Pharmacology Exam 3 Study Guide Cardiovascular Digoxin How does this medication work? Force of contraction in ventriclesWhat is it used for? Manage Cardiac dysrhythmias . Slows and strengthens the heart. How do you know
...
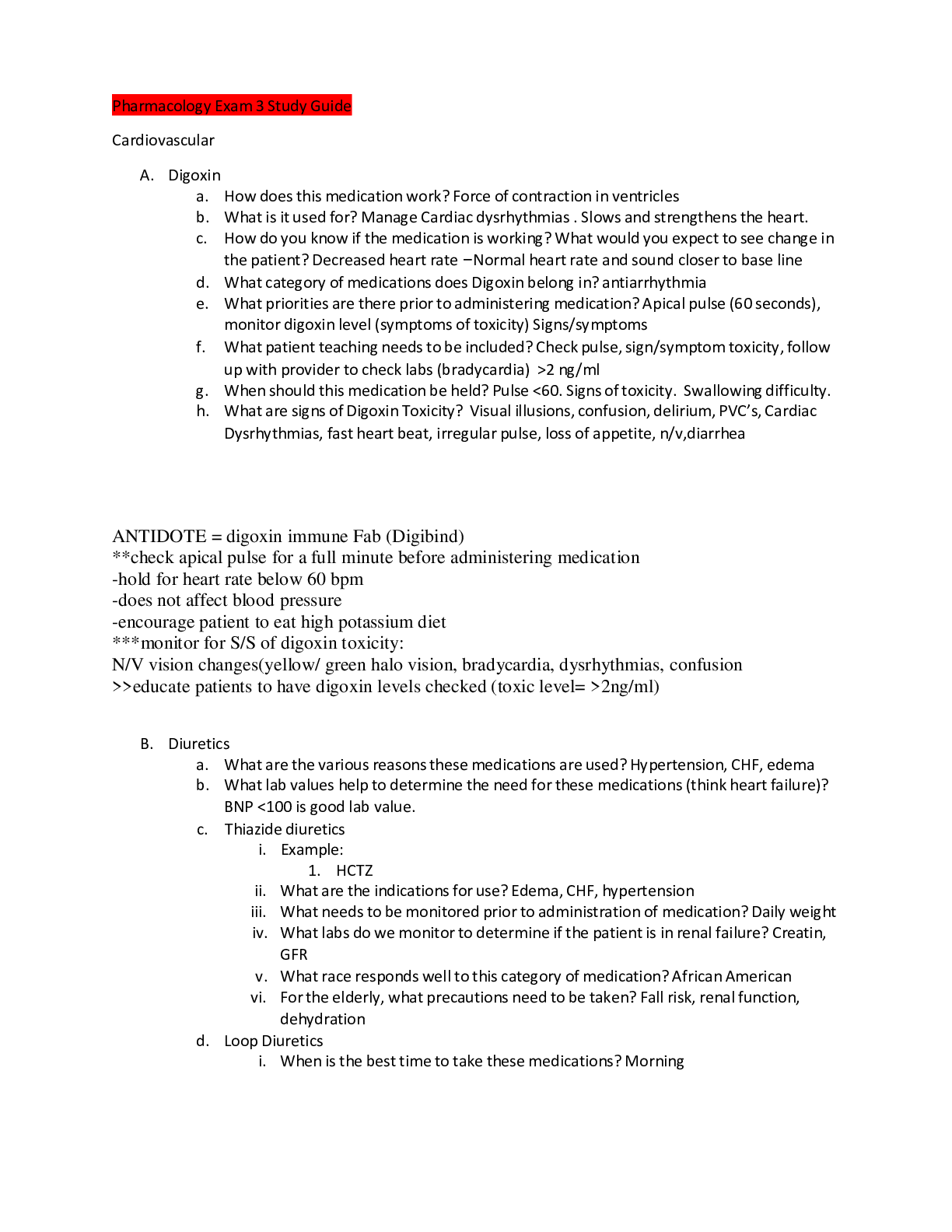
Pharmacology Exam 3 Study Guide Cardiovascular Digoxin How does this medication work? Force of contraction in ventriclesWhat is it used for? Manage Cardiac dysrhythmias . Slows and strengthens the heart. How do you know if the medication is working? What would you expect to see change in the patient? Decreased heart rate –Normal heart rate and sound closer to base line What category of medications does Digoxin belong in? antiarrhythmia What priorities are there prior to administering medication? Apical pulse (60 seconds), monitor digoxin level (symptoms of toxicity) Signs/symptoms What patient teaching needs to be included? Check pulse, sign/symptom toxicity, follow up with provider to check labs (bradycardia) >2 ng/mlWhen should this medication be held? Pulse <60. Signs of toxicity. Swallowing difficulty. What are signs of Digoxin Toxicity? Visual illusions, confusion, delirium, PVC’s, Cardiac Dysrhythmias, fast heart beat, irregular pulse, loss of appetite, n/v,diarrhea ANTIDOTE = digoxin immune Fab (Digibind)**check apical pulse for a full minute before administering medication-hold for heart rate below 60 bpm-does not affect blood pressure-encourage patient to eat high potassium diet***monitor for S/S of digoxin toxicity:N/V vision changes(yellow/ green halo vision, bradycardia, dysrhythmias, confusion>>educate patients to have digoxin levels checked (toxic level= >2ng/ml)Diuretics What are the various reasons these medications are used? Hypertension, CHF, edema What lab values help to determine the need for these medications (think heart failure)? BNP <100 is good lab value. Thiazide diuretics Example:HCTZ What are the indications for use? Edema, CHF, hypertension What needs to be monitored prior to administration of medication? Daily weight What labs do we monitor to determine if the patient is in renal failure? Creatin, GFRWhat race responds well to this category of medication? African American For the elderly, what precautions need to be taken? Fall risk, renal function, dehydration Loop Diuretics When is the best time to take these medications? Morning What is an important way to monitor fluid retention (also can do this with thiazide diuretics)? Daily weight Examples: Furosemide (Lasix), Bumetanide, piretanide, torasemideWhat is a symptom that the patient should report immediately if experiencing while on this medication (or aspirin)? TinnitusPotassium Sparing Diuretics What food substitute should be avoided with this group of medications? Sodium With many diuretics, potassium needs to be replaced. What are the normal levels of potassium? When should it be administered? Should you ever chew potassium tablets? Normal Potassium Levels 3.5-5.5 mEQ/L. Never chew or crush potassium tablets but may be dissolved. <2.5 is criticalCalcium Channel BlockersWhat are they used for? Hypertension, cardiac arrhythmias, THEY ARE A VASODIALATORBest to treat HTN in African Americans if HCTZ doesn’t workWhat patient education is important for this group of medications? Monitor bp, heart rate, rise slow.Side effects: Orthostatic hypotension, peripheral edema, increased fall risk, flushingWhat are examples of this category of medications?Nifedipine (Procardia)DiltiazemBeta Blockers : Ends in LOL. Inderal (Propanolol) , Coreg (carvidilol)What are they used for? hypertensionWhat needs to be monitored/checked prior to administration? Monitor BP, PulseWhat do you need to teach your patient to check prior to taking medication at home?Monitor bp pulse and when to hold it . Hold is <60 bpm and SBP <90When do you hold these medications? Systolic under 100 pulse under 60What effect does wine have with this type of medication? Increase effect. Drops vital signs.Examples:Metoprolol (Lopressor)Atenolol ( Tenormin)Propanolol (Inderal)Carvidilol (Coreg)***Don’t stop abruptly Can cause HypertensionACE inhibitors (ALL END IN PRIL) Lisinopril (Zestril)What is the medication given for? Hypertension & HF How does it work? Blocks acetylcholine receptors, dilates vessels to lower bp. Prevents vasoconstriction DiuresisWhat is a common side effect of this group of meds that can be bothersome to patients? Persistent Dry cough. Adverse: angioedema (life threatening), Hypotension, orthohypo, hyperkalemia in diabetics, renal failure and with potassium-sparing diuretics.NitroglycerinHow does this medication work? Dialates blood vesselsWhat different forms are available of this medication? Sublingual Tablets, ointment, patches When is an appropriate time to give this medication? Onset of chest painWhat patient education is necessary in the use of this medication? Rotate sites for patch, 3 doses of sublingual every 5 minutes.What precautions should be advised? Don’t swallow, don’t stand up too fast.What side effects should the nurse educate the patient on prior to administering? What should the patient expect to experience? Nausea, light headed.What medication should NOT be given if a patient is using nitro? Erectile dysfunction Can cause sudden drop in BP Headache is common Tabs should be protected from heat and lightStatinsWhat side effects need to be monitored for and the patient needs to be educated to report immediately if experiencing? Muscle pain, weakness (rhabdomyolysis). Life threatening muscle damage.What could these side effects lead to?HeparinWhat lab values are used to monitor normal levels? INR, XaWhat is the antidote? Protamine SulfateCoumadinWhat foods, meds, etc. can alter the effects of coumadin? Vitamin K, leafy greens, antibiotics, NSAIDSWhat is the antidote? Vitamin KWhy might a patient be taking this medication? Afib, TIA,What lab value is used to monitor normal levels? What is a typical normal range we would expect?( 0.8-1.2 normal ) Coumadin (2-3) is therapeuticWhat are the various ways that could indicate the patient’s INR levels are off? Brusing, bleedingPlavixWhat is the indications for use? AntiplateletWhat other medication should be used in combination with this one if the patient has a history of ulcers? PPI,When should this be stopped if a patient is having surgery? 7-10 daysRespiratoryAlbuterolWhen is this indicated for use? Acute bronchospasmWhat is the expected outcome after use? ReliefWhat are the expected side effects of the medication? Tachycardia, palpationsSereventMaintenance inhaler: Long actingWhat medication category does this fall into? Beta 2.AtroventWhat can you do to help a patient manage the bitter taste that is common with this medication? Rinse mouthDuonebsAnticholinergic effects – what are they? Dries up mucous membranes Theophylline Why is this used? EmphysemaWhat adverse effects might occur?What are signs of toxicity? Vomiting , abdominal pain, seizure,Singulair (Montelukast)What organ can be damaged with this medication? LiverHow is it used in asthma? Frequency, time of administration, etc. Evening .It is anti inflammatory and is only used for prophylactic and maintenance therapy.Fluticasone (inhaled)What is a major risk with inhaled steroids? Thrush How is this treated (with what medication and how should you instruct the patient to use)? Swish after.What should you teach patients to do after using inhalers? Good oral cares afteradministrationGeneral instructions for inhalersWhat sequence should be used? Short acting bronchodialators, steroid lastCodeine with robitussinWhen is this advised to be given as a cough suppressant? Nonproductive, dry cough. Short term
[Show More]