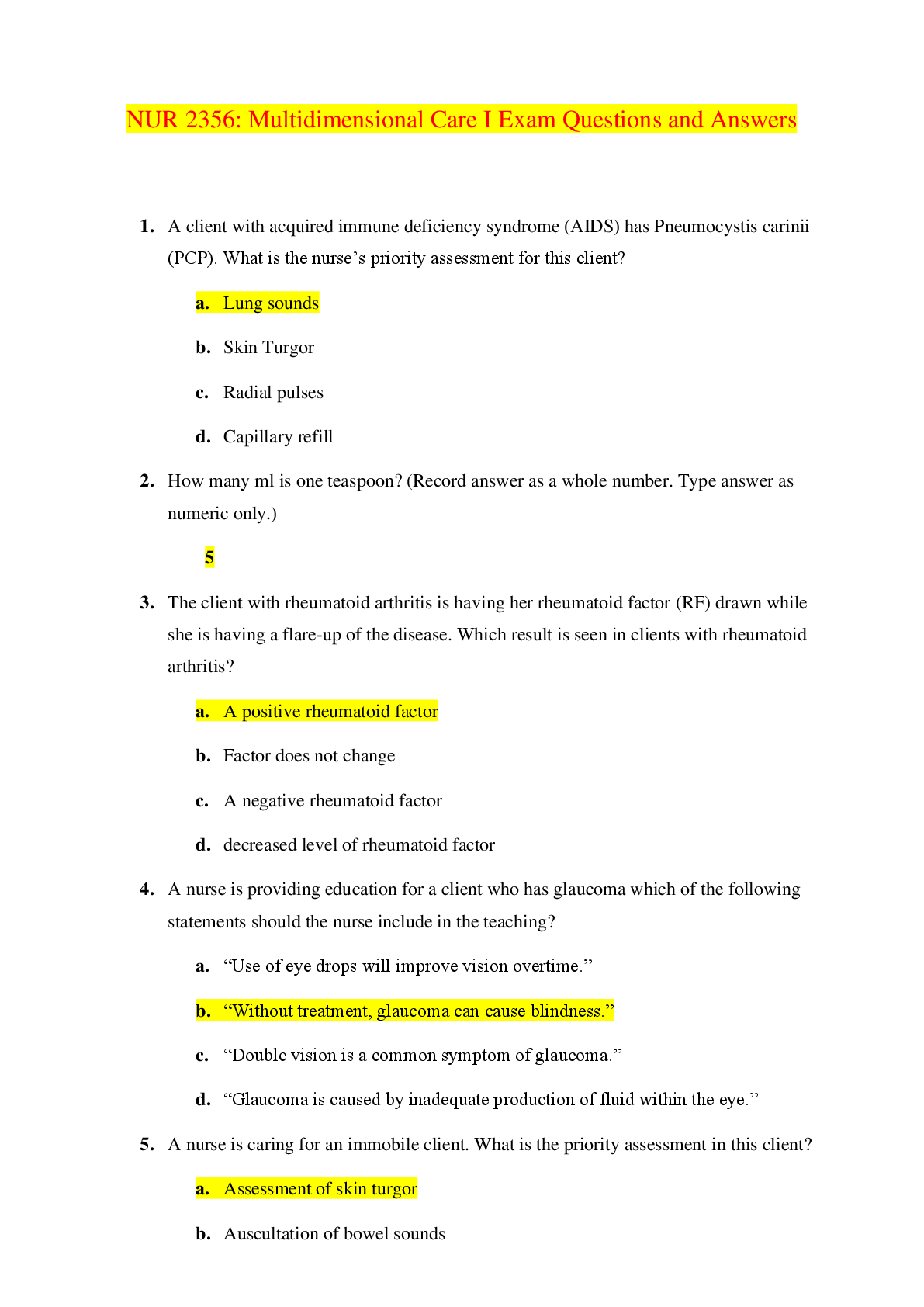
Review
headaches
o vascular headaches: migraines, cluster, HPT
migraines: prodromal (early s/s): aura, visual field defects,
unusual smells or sounds, disorientation, paresthesia
o tension headaches
o traction-
...
Review
headaches
o vascular headaches: migraines, cluster, HPT
migraines: prodromal (early s/s): aura, visual field defects,
unusual smells or sounds, disorientation, paresthesia
o tension headaches
o traction-inflammation headaches
respiratory disease- interventions- respiratory alteration? O2 status
o can only administer 2-4L of oxygen without prescription needed
o listen to lung sounds, position pt to high fowlers
delegation
o what uaps can and can’t do- can help with ADLs, basic care and vitals
of stable pts, no medications
hypovolemic shock- interventions- restoring blood volume- replace loss hmt
and hgb- manifestation- roles of RBCs
o can be caused due to hypovolemia-dehydration- due to vomiting,
diarrhea, hemorrhage, polyuria, inadequate fluid intake. Increase BP,
threading pulse (weak pulse), tachycardia, cold calmly skin and fleshy
skin, sunken eyes, tenting packed RBCs given to restore blood volume
and replace HMT and HGB levels- give more fluids, give albumin to
increase BP, oxygen to prevent hypoxia, sodium-bicarb due to
increase acidosis, orthostatic hypotension, oliguria, diaphoresis,
weight every 8 hrs, vitals every 15 min
HPT- risk factors- values- assessment-intervention-teaching
o Exercise 5x/ week 30 min
o High level of potassium-obtain 12 ECG- indication of abnormal
rhythm: dysrhythmia. Typical abnormalities in
o Risk factors: smoking, race (African), obesity, stress, family history,
sedentary lifestyle, alcohol, age >60 or postmenopausal, excessive
alcohol
o Interventions: reduce BP and prevent or lessen extent of organ
damage, 12L EKG/ECG monitor for heart rhythm and report changes
o Teaching: diet, stress reduction
o Assessment: may be asymptomatic, headache, visual disturbance,
dizziness, chest pain, tinnitus (noise or ringing in ears), flushed face,
epistaxis (nosebleed)
o Parameters
Normal: <120/ <80
Pre-HPT: 120-129 systolic OR 80-89 diastolic
HPT Stage 1: >140-159/ >90-99
HPT Stage 2: >160/ >100
Medications for HPT- beta blockers- ace inhibitors-s/e-assessmentintervention-teaching- Labs-meds- risk factors
o “-il” = ace inhibitor, “-olol” = beta blockers
o Lisinopril- ACE inhibitor
Prevents vasoconstriction
Can cause sexual dysfunction and impotence
Swelling on tongue
o Metoporlol and Ateneolol- Beta Blockers
Beta blockers such as atenolol dilate peripheral arteries, sudden
position changes can cause dizziness, lightheadedness, or
syncope. These responses are most prominent when beginning
the drug. To promote safety, especially for older adults, the
nurse should teach the patient taking beta blocker to change
position very slowly.
Blocks sympathetic nervous system (beta adrenergic receptors)
and produces a slower heart rate
Monitor for bradycardia
Can increase risk of bleeding
Gathering subjective and objective data- assessment/physical
o Objective: heart rate, blood pressure, respirations, wound appearance,
ambulation description
o Subjective: pain, any data gathered from pt telling you something
Pre-op consent/ pt teaching incentive/ understanding procedure- intra-opthings to do, things happening, do for pts in post-op
o Incentive spirometer: take deep breath, inhale with device, exhale out
prevents atelectasis, improves lung expansion/oxygenation. Pt turn
and cough deep breath, ever 2 hrs, turn pts side-back-side cough
forcefully and splint if needed. Do not do in pts with ICP pressure
surgeries or ent spin surgeries.
o Pre-op:
Things that should be reported: cardiac problems, airway
concerns, recent airway infections, COPD or asthma, history or
smoking, pregnancy, eating/drinking prior to surgery
Prophylactic antibiotics within 1 hr of a surgical incision
Informed consent: LEGAL PREP
Provider: discuss procedure, describe risks and benefits,
their ability to refuse, any alternatives
RN: can only CLARIFY, witness consent after client
acknowledges understanding, it is OUT OF SCOPE if pt
doesn’t understand
PT: pt with mental illness does not mean they cant
consent. Once consent is signed, it can still be withdrawn
Before anesthesia- ask pt to confirm name, DOB,
surgical procedure, site and consent
Wrong surgical procedure and surgery performed on
wrong body part or wrong pt are defined as a sentinel
events
Manifestations hypovolemic shock- thromboembolism risk factors
o
VTE-what do you look out for- teaching/ manifestations dos and don’t
o Development of blood clot in deep veins- starts at DVT then develops
to embolism
o Risk factors: venous stasis, hypercoagulability, trauma of a blood
vessel, immobilization after surgery
o Manifestations: pain, edema, erythema, warmth, tenderness along vein
o Do not massage legs, anti-embolic stockings
o Measure stockings: from heel to popliteal space
Deep vein thrombosis- most important aspect/ open-reduction internal
fixation
o Elevate the extremity above heart level
o At risk for pulmonary embolism
o Compression stocking, frequent position changes, early ambulation
o Do not massage pt legs-can travel
o Dull aching calf pain
o Compare legs size, temp, edema
o Pt at risk: given blood thinners: warfarin & heparin together due to
effectiveness- for therapeutic levels (anti-coagulant meds)
o Warfarin & ginkgo: bad reaction-cannot take with it
o Warfarin & glucosine cannot be taken together
Differentiate between clear, full liquid diets
o Clear: only liquids you can see through/ little residue-broth, clear fruit
juices, gelatin
o Full: thicker, clear liquids plus liquid dairy products, all juices.
ABGs
o Role- measures acidity (pH) and levels of oxygen and carbon dioxide
in the blood from an artery- used to check how well lungs are able to
move oxygen into the blood and remove carbon dioxide from the
blood
o Ph: 7.35-7.45
<7.35= acidosis
>7.45= alkalosis
o HCO3: 22-26
<22: metabolic acidosis
>26: metabolic alkalosis
o CO2: 35-45
<35: respiratory alkalosis
>45: respiratory acidosis
Skin assessment- stage 1, 2,3, 4- teaching
o Stage 1: intact skin with non-blanchable redness. Possible indicatorsskin temp., tissue consistency, pain. May appear with: red, blue, or
purple hues in darker skin tones
Dressing changes: transparent & hydrocolloid
o Stage 2: Partial-thickness loss of dermis. Shallow open ulcer with red
pink wound bed. Presents as an intact or ruptured serum-filled blister
Dressing changes: composite film, hydrocolloid, hydrogel
o Stage 3: full-thickness loss can extend down to, but not through,
underlying fascia. Presents as a deep crater with possible undermining
of adjacent tissue. Depth of ulcer varies by anatomic location
Dressing changes: hydrocolloid, hydrogel w/ foam, gauze,
growth factors
o Stage 4: full thickness loss can extend to muscle, bone, supporting
structures. Bone, tendon, or muscle may be visible or palpable.
Undermining and tunneling may occur
Hydrogel, calcium alginate, gauze
o Unstageable: cannot determine depth of damage due to exudates,
necrosis, or eschar
Adherent film, gauze, enzymes
Albumin, protein, vitamin C, on skin ulcers
o Promotes wound healing
Assess respiratory status on elders
o
Assess for falls- what to identify
o Assess room for any risks
Manifestation GI bleeding (what to look for when someone is bleeding
internally)
o dark tarry stools and red blood in stool- if dark it is from upper GI
GERD- teaching-manifestations-assessments
o Backflow of gastric and duodenal contents into the esophagus
o Causes: Incompetent LES/lower esophageal sphincter, Pyloric
stenosis, Hiatal hernia, Excessive intra-abdominal or intragastric
pressure, Motility problems
o Assessments: heartburn, epigastric pain (upper abdomen), dyspepsia,
nausea, regurgitation, pain/difficulty swallowing, hyper salivation
o Teachings: avoid coffee, chocolate, fried or fatty foods, carbonated
beverages or alcoholic beverages, cigarette smoking. Pt should eat
low fat, high fiber diet, avoid eating and drinking 2hrs before bedtime
and wearing tight clothes
o Elevate head of bed, emesis basin,
o Ice chips- do not eat within 2-3hrs before bed
o Radiating pain-neck/jaw/back
IBD diet question-food choices
o Functional disorder characterized by chronic or recurrent diarrhead,
constipation, and/or abdominal pain & bloating
o Increase dietary fiber, drink 8-10 cups of liquids per day
Diabetes- type 1 and type 2- risks- hypoglycemic/ hyperglycemic
o Type 1: insulin dependent, autoimmune disorder, destruction of B
cells occurring for months to years before symptoms occur,
manifestations develop when pancreas can no longer produce
sufficient insulin to maintain normal glucose. 3 Ps: polydipsia
(excessive thirst), polyphagia (excessive hunger), polyuria (frequent
urination)
o Type 2: non-insulin dependent. Pancreas continues to produce
endogenous insulin but not enough insulin is produced OR body does
not use insulin effectively. relative lack on insulin or resistance to the
action of insulin, insulin is sufficient to stabilize fat and protein
metabolism but not carbohydrate metabolism
Risk factors: abdominal obesity, hyperglycemia, HPT, high
triglyceride level, a lowered HDL cholesterol level
o Assessments: polyuria, polydipsia, polyphagia- all more common in
type 1 DM. Hyperglycemia, weight loss (common in type 1, rare in
type 2), blurred vision, slow wound healing, vaginal infections,
weakness and paresthesia (tingling, pricking, chilling numbness),
signs of inadequate circulation to feet
o Hypoglycemia occurs when the blood glucose level falls below
70mg/dL or when the blood glucose levels drop rapidly from an
elevated level, can be caused by too much insulin or too large an
amount of an oral hypoglycemic agent, too little food, or excessive
activity-pt should carry emergency foods (fast-acting simple
carbohydrates)
o Dietary adjustments for pts with nephropathy and DM- consume less
than 08. g/kg of body weight of protein per day, 45%-65% carbs per
day, less than 200 mg of cholestrol per day, 25 g per day of fiber for
women and 38 g per day for men
o Hypoglycemia-sweating, tremor, tachycardia, palpitations, headache,
fatigue, nervousness, hunger
o Hyperglycemia- dehydration, fruity breath odor, nausea, vomiting,
warm, moist skin
Teaching medication- Biguanides- metformin(Glucophage)- when is it given
o Most common for type 2- take with food-never crush or chew
o Reduces glucose production by liver-enhancing insulin sensitivitymay cause weight loss- take with food never crush or chew
o May need to be discontinue 48 hrs before surgery (can increase risk
on renal failure) and may not be restarted until renal function is
normal postop
o Monitor for serum creatinine
Glipizide- s/e what is it for- pt teaching
o Stimulates insulin release from pancreas causing decrease in blood
sugar levels. Major s/e: hypoglycemia
o Administer 30 mins before meals, avoid alcohol
Manifestations of diabetes insipidus- peeing like no tomorrow
o Excretion of large amount of dilute urine, polydipsia, dehydration
(decreased skin turgor and dry mucous membranes), inability to
concentrate urine
o Fatigue, muscle pain, weakness
Diabetic teaching-diet/ time for insulin and time of breakfas
[Show More]




.png)













 JN21.png)