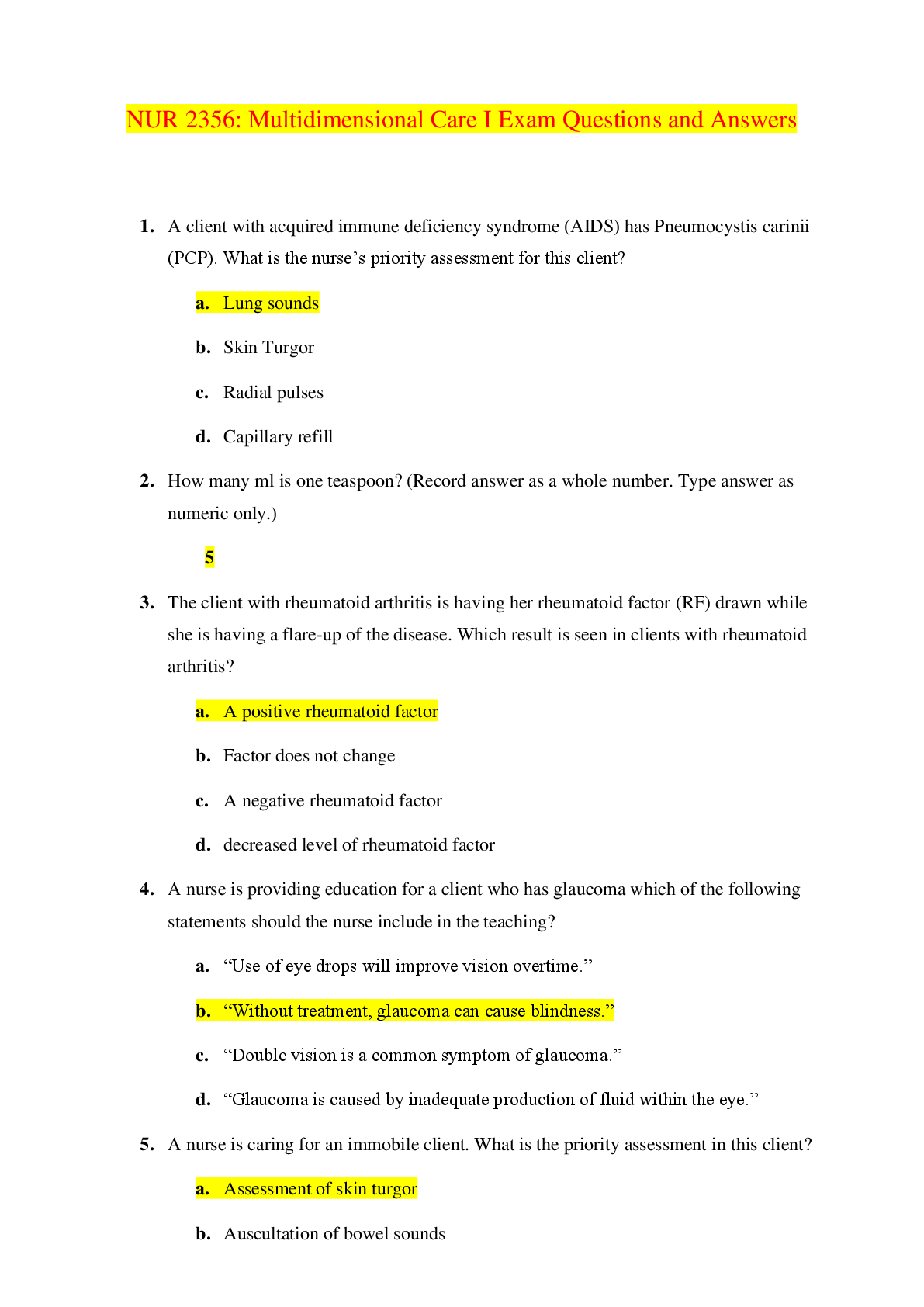
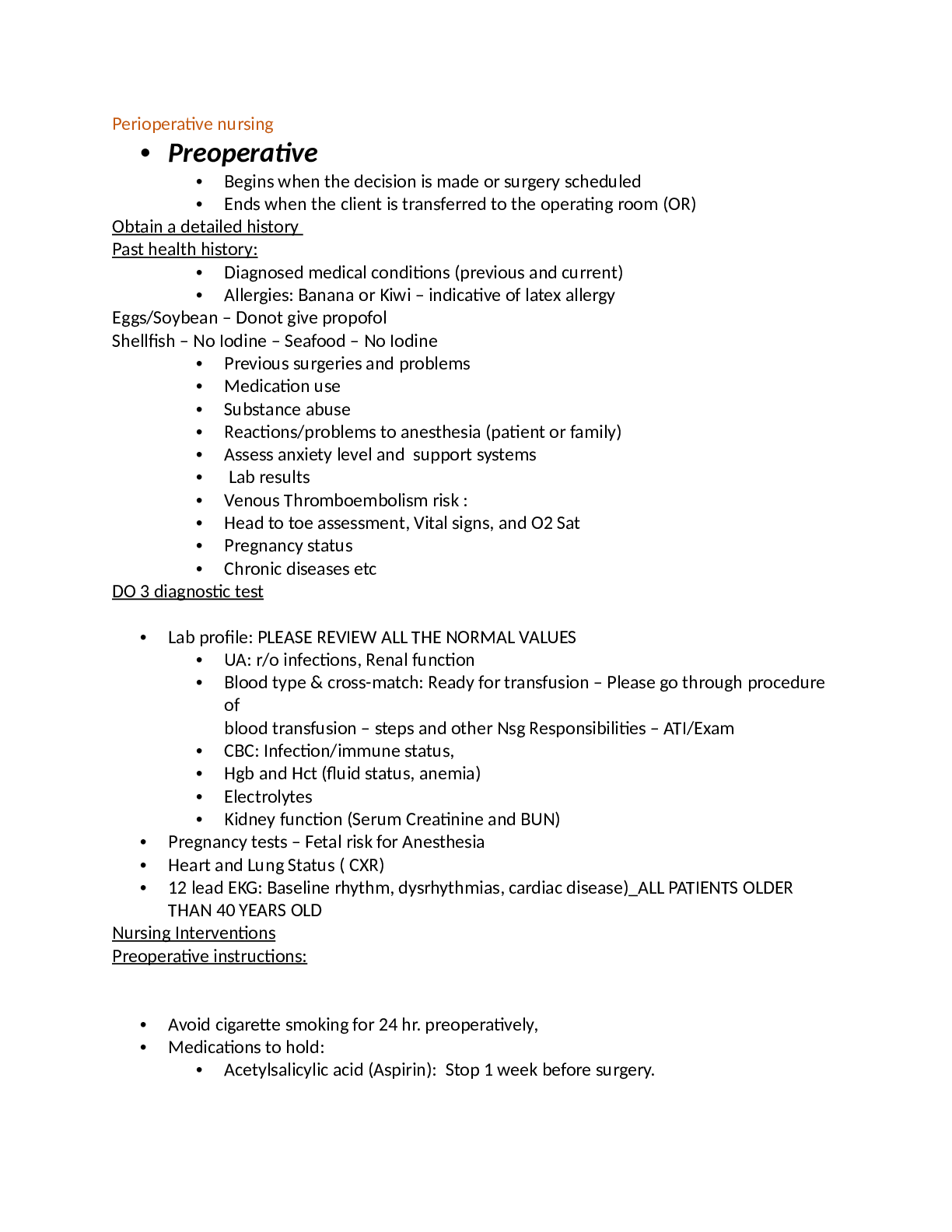
• Preoperative
• Begins when the decision is made or surgery scheduled
• Ends when the client is transferred to the operating room (OR)
Obtain a detailed history
Past health history:
• Diagnosed medical conditions (
...
• Preoperative
• Begins when the decision is made or surgery scheduled
• Ends when the client is transferred to the operating room (OR)
Obtain a detailed history
Past health history:
• Diagnosed medical conditions (previous and current)
• Allergies: Banana or Kiwi – indicative of latex allergy
Eggs/Soybean – Donot give propofol
Shellfish – No Iodine – Seafood – No Iodine
• Previous surgeries and problems
• Medication use
• Substance abuse
• Reactions/problems to anesthesia (patient or family)
• Assess anxiety level and support systems
• Lab results
• Venous Thromboembolism risk :
• Head to toe assessment, Vital signs, and O2 Sat
• Pregnancy status
• Chronic diseases etc
DO 3 diagnostic test
• Lab profile: PLEASE REVIEW ALL THE NORMAL VALUES
• UA: r/o infections, Renal function
• Blood type & cross-match: Ready for transfusion – Please go through procedure
of
blood transfusion – steps and other Nsg Responsibilities – ATI/Exam
• CBC: Infection/immune status,
• Hgb and Hct (fluid status, anemia)
• Electrolytes
• Kidney function (Serum Creatinine and BUN)
• Pregnancy tests – Fetal risk for Anesthesia
• Heart and Lung Status ( CXR)
• 12 lead EKG: Baseline rhythm, dysrhythmias, cardiac disease)_ALL PATIENTS OLDER
THAN 40 YEARS OLD
Nursing Interventions
Preoperative instructions:
• Avoid cigarette smoking for 24 hr. preoperatively,
• Medications to hold:
• Acetylsalicylic acid (Aspirin): Stop 1 week before surgery.
• Herbal medications (G’s: Ginkgo biloba, Ginseng, Garlic): stop taking 2 to 3
weeks before surgery to prevent hemorrhage.
• Feverfew : Stop taking 2-3 weeks (adverse affects to the anesthetic)
• Regular medications for chronic conditions maybe taken before surgery.
• Bowel preparation instructions ( if needed)
• Pain Scale
• Intraoperative
• Begins when the client is transferred to the OR
• Ends when the client is transferred to a post anesthesia care unit (PACU)
Risk Factors
• General anesthesia:
• Malignant hyperthermia
• Respiratory disease ( hypoventilation)
• Cardiac disease (dysrhythmias)
• GI ( aspiration of gastric content)
• Alcohol or drug use ( interactions)
• Local anesthesia:
• Allergy to ester-type anesthetics
• Alterations in peripheral circulation
• Airway patency is the main priority in all situations but cardiovascular problems can
also arise
• 3 phases:
• Induction, Maintenance, Emergence.
• Anesthetics used during general anesthesia are classified as:
• Injectable : benzodiazepines, propofol ( don’t use with allergy to eggs or
soybean oil), fentanyl.
• inhaled (halothane, isoflurane).
Antidotes -
naloxone hydrochloride (Narcan) - Opioids
flumazenil (Romazicon) - Benzodiazepines
Anesthetics
• Opoids – eg – Fentanyl, Sufentanil, Alfentanil
• Uses – Sedation, Analgesics to releive post op and pre op pain.
• Adverse effect – Depresses the CNS – Resp depression or distress
• Delays regain of conscious after surgery
• Can trigger N/V
• Benzodiazepines – Eg- Diazepam, Midazolam
• Uses: Reduce anxiety pre-op
• Promote amnesia
• Produce mild sedation with mod to little respiratory depression when titrated
• Adv Effects – Cardiac/Resp arrest if not administered slowly or if doses are administered
without waiting for full effect to develop
Sedatives
• Eg – Pentobarbital, Secobarbital
• Uses – Sedative effect for preanesthesia sedation or amnesia effect
• Induction of General Anesthesia
• Adv Effect – Avoid giving within 14 days of starting or stopping MOA inhibitor,
Respiratory depression
• Neuromuscular blocking agents – Eg – Succinylcholine Vencuronium
• Uses – Skeletal muscle relaxation for surgery
• Airway placement
• In conjunction with IV anesthetics agents
• Adv Effects – Total flaccid paralysis
• Requires mechanical ventilation because blocks contraction of muscles including the
diaphragm and respiratory system.
Antiemetics
• Odensteron, Metoclopramide, Promethazine
• Uses: Decrease post Anesthesia N/V
• Metoclopramide – enhances gastric emptying
• Promethazine – Induces sedation
• Decreases risk of aspiration.
• Adv Effects – Dry Mouth, Dizziness
• Use metoclopramide with caution if history of parkinsonism disease and asthma
• Promethazine can cause resp depression and apnea
Anticholinergics
• eg Atropine, Glycopyrolate
• Uses: Decrease risk of Bradycardia during surgery and at times vagal slowing of the heart
due to parasympathetic response to surgical manipulation
• Block Muscarinic response to acetylcholine by decreasing salivation, bowel movement
and GI secretions
• Slow mobility of GI system
• Decrease salivation, Pancreatic juices and gastric juices
• Decrease risk of aspiration
• Adv Effects –
• Urinary retention
• Tachycardia
• Dry mouth
• Decreased levodopa effects
• Contraindicated with glaucoma and urinary problems
Malignant Hyperthermia
• Malignant Hyperthermia -
• Acute life threatening medical emergency
• Hypermetabolic condition causing an alteration in calcium activity in muscle cells –
muscle rigidity and hyperthermia causing damage to CNS
• Anesthetics – Trigger
• Increased CO2 – Decreased O2 – Tachycardia – Dysrhythmias – Muscle Rigidity –
Hypotension – Tachypea – skin mottling – cyanosis – muscle break down and
myoglobinuria
• Extremely High temperature – 111 F
Nursing Actions for malignant hypothermia –
• Terminate Surgery – Inform the Anethesiologist
• Administer Dantrolene IV – relaxes muscles
• O2 – 100 % - Monitor ABG – Met Acidosis
• Iced – NS 0.9%
• Cooling blanket
• Monitor Urine output and BP
Postoperative
• Begins when client leaves the OR for the PACU
• Ends when the client is transferred to Med-Surg Unit or discharged home
(outpatient)
• Who can transfer a client from OR to PACU?
• Anesthesia provider (anesthesiologist or CRNA)
• Circulating nurse gives the verbal “hand-off” report to PACU nurse.
• Postoperative care is provided initially in the PACU by a ACLS certified RN.
• Initial postoperative care:
• assessments, administering medications, managing client’s pain,
preventing complications, and determining when a client is ready to be
discharged from the PACU.
• PRIORITIES During the immediate postoperative stage:
• airway patency
• ventilation
• circulatory status
Common Post-OP Complications: Immediate to 48 hr:
• Respiratory depression
• Hypoxia
• Wound Hemorrhage
• Nausea
• Shock
• Urinary retention (up to 3days)
First 48hr:
• Atelectasis
After 48 hr:
• Hypostatic pneumonia
2-4 days:
• Paralytic ileus (decreased peristalsis)
3-5 days:
• Wound infection
• > 4 days:
• UTIs
• Thrombophlebitis
• Wound dehiscence/evisceration
Risk FactorsUrinary retention (up to 3days)
First 48hr:
• Atelectasis
After 48 hr:
• Hypostatic pneumonia
2-4 days:
• Paralytic ileus (decreased peristalsis)
3-5 days:
• Wound infection
• > 4 days:
• UTIs
• Thrombophlebitis
• Wound dehiscence/evisceration
Risk Factors for Postoperative complications
• Immobility (respiratory compromise, thrombophlebitis, pressure ulcer)
• Anemia (blood loss, inadequate/decreased oxygenation, and healing factors).
• Hypovolemia (tissue perfusion).
• Hypothermia (surgical wound infection, altered absorption of medication, coagulopathy,
and cardiac dysrhythmia).
• Cardiovascular diseases (fluid overload, deep-vein thrombosis, arrhythmia)
• Respiratory disease (respiratory compromise)
• Comorbidities affecting Post-Operative period:
• Immune disorder (risk for infection, delayed healing)
• Diabetes mellitus (gastroparesis, delayed wound healing)
• Coagulation defect (increased risk of bleeding)
• Malnutrition (delayed healing)
• Obesity (wound healing, dehiscence, evisceration)
• Older adults ( more susceptible)
PACU Assessments and Nursing interventions:
• Full Head to Toe assessment with priority given to airway, breathing, and circulation
(ABCs)
• Nursing monitoring and management:
• Airway and Breathing:
• ( artificial airway, O2 Sat (>92% or at preop. levels)
• Respiratory pattern ,breath sounds, chest wall movement, and
Auscultate lung sounds
• Administer humidified oxygen.
• If unable to cough:
• Suctioning with Yankauer suction ( thick oral secretions), or
• Large French suction catheter (nasopharyngeal or nasotracheal
secretions)
• Circulation: Monitor
• S & S of internal bleeding (abdominal distention, visible hematoma
under/near the surgical site, tachycardia, hypotension, increased pain).
• External Bleeding.
• Assess for hypervolemia and hypovolemia.
• Assess skin color, temperature, sensation, and capillary refill.
• Check mucous membranes, lips, and nail beds for cyanosis.
• Assess and compare peripheral pulses for impaired circulation, deep-vein
thrombosis (continue DVT prevention measures)
• ECG readings and apical pulse
Fluid and electrolyte balance.
• Vital Signs:
• Until stable (every 15 min) and assess for trends.
• Prevent hypothermia
• Positioning:
• If responding to verbal stimuli: Semi Fowler’s if not contraindicated
(facilitate chest expansion)
• If unresponsive or unconscious: Right or Left Lateral position (to prevent
aspiration)
• If hypotension or shock develop: Elevate legs and lower the head of the
bed.
• If recovering from spinal anesthesia: Do not elevate legs higher than
placement on a pillow
• Avoid placing a pillow under the knees or engaging the knee gatch of
the bed ( decrease venous return).
• Response to anesthesia (sedation, nausea and/or vomiting), Monitor
• LOC
• Movement, sensation
• Antiemetics
• I & O: Monitor
• Fluid and electrolyte balance
• Skin turgor, diaphoresis
• Emesis, drains, NG tubes, IV fluids, urine, Blood products.
• Isotonic IV fluids (0.9% sodium chloride, lactated Ringer’s, dextrose 5% in
lactated Ringer’s)
• Palpate bladder for distention.
• Urinary catheters patency: Urine output less than 30 mL/hr may indicate hypovolemia.
• Surgical wound, incision site, and/or dressing
• Pain
• Monitor recovery from anesthesia by using the Aldrete scoring system.
• Criteria indicating readiness for discharge from the PACU
• Aldrete Score of 8 to 10
• Stable vital signs
• No evidence of bleeding
• Return of reflexes (gag, cough, swallow)
• Minimal to absent nausea and vomiting
• Wound drainage that is minimal to moderate
• Urine output of at least 30 mL/hr
• The anesthesiologist must sign out the client before transfer to another unit or
discharged to home.
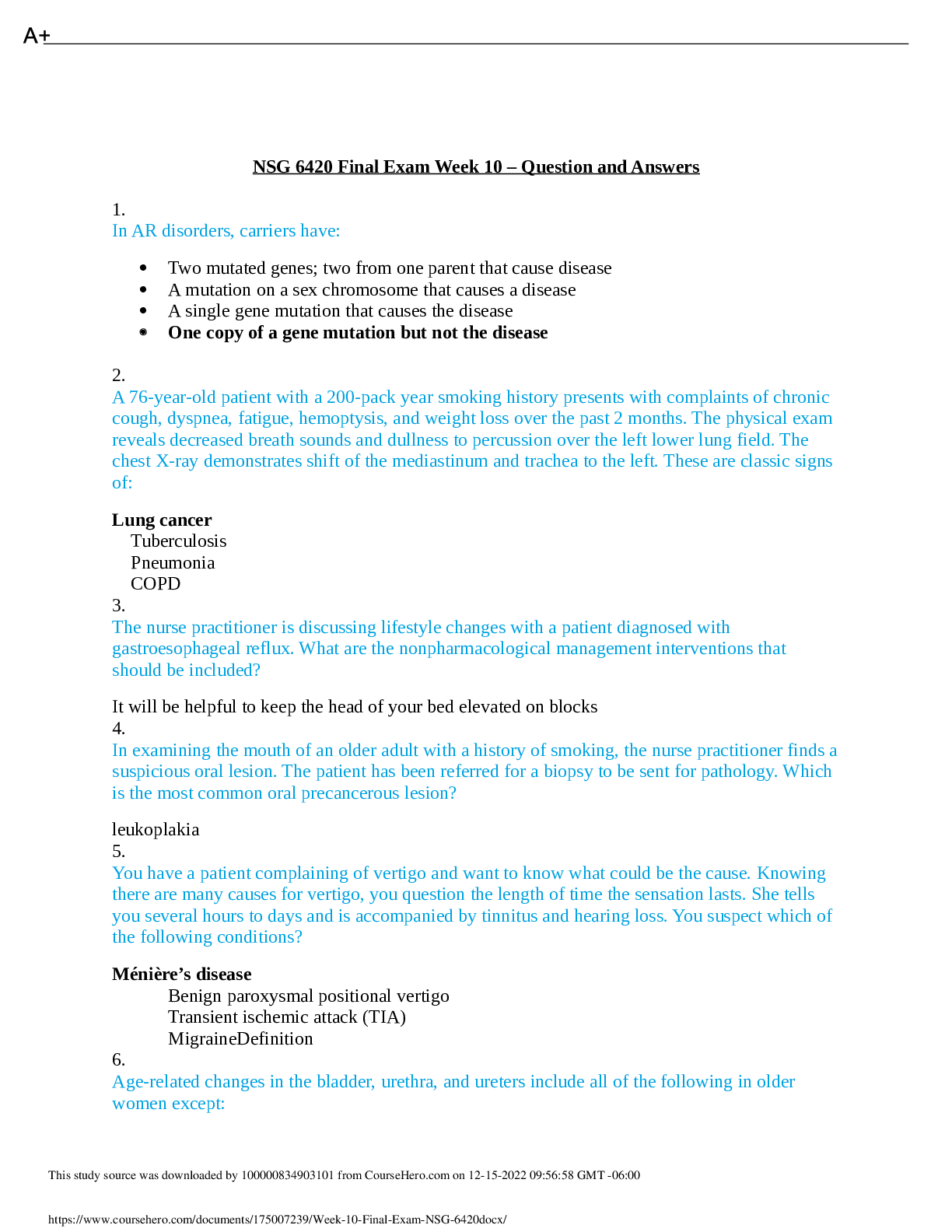
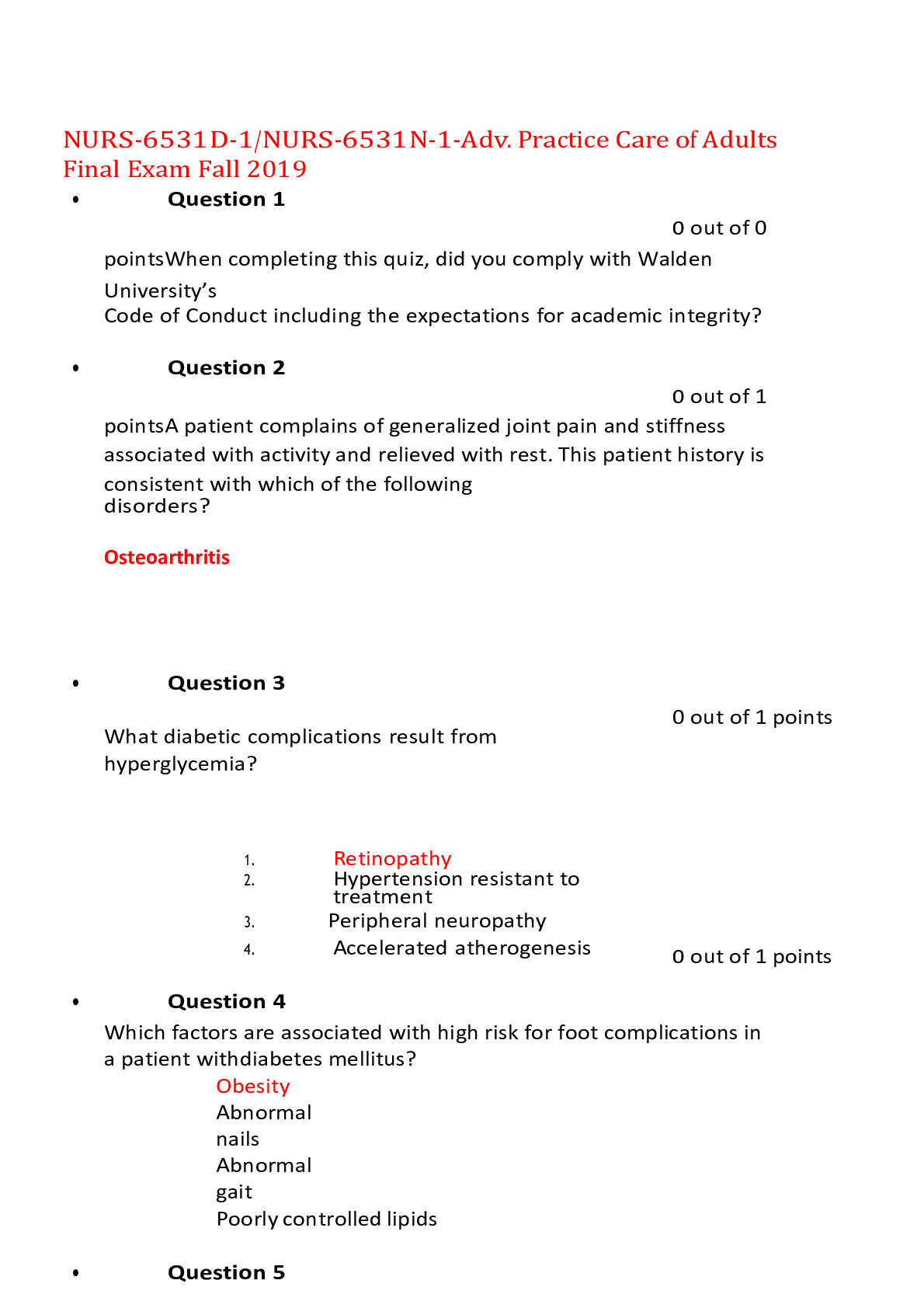
DIABETES
• Type 2 – Impaired insulin production/Impaired insulin use
Etiology and Risk Factors
• Type 2 –
• Insulin production is less or use is impaired or reduces insulin sensitivity
o Hereditary – major role
o Obesity
o Eating habits
o Sedentary life style
Pathophysiology
• Type 2 –
• Causes – leading to high glucose
• Stages – Desensitization – Failure of beta cells to respond to high glucose levels
• Insulin Resistance – Production of glucose by liver despite of high glucose levels
• Inability of fat and muscle tissue to take up glucose – peripheral insulin resistance
Clinical Manifestations
• 3 p’s – Polydipsia, Polyuria and Polyphagia
• ^ Hyperglycemia S/S: Fatigue, Blurred vision, Slow wound healing, Itchy skin-“Hot and
dry, blood sugar high”
• v Hypoglycemia S/S: Sweating, Hunger, Trembling, Anxiety, Confusion, Blurred
vision-“Cool and clammy, need some candy”
• Weight loss
• Ketone bodies- Diabetic Keto Acidosis
• Fruit breath odor, headache, N,V, Abd. Pain, fatigue, weakness, slow wound healing
To diagnose
Diagnostic criteria include:
• TWO findings (on separate days) of at
[Show More]











 JN21.png)