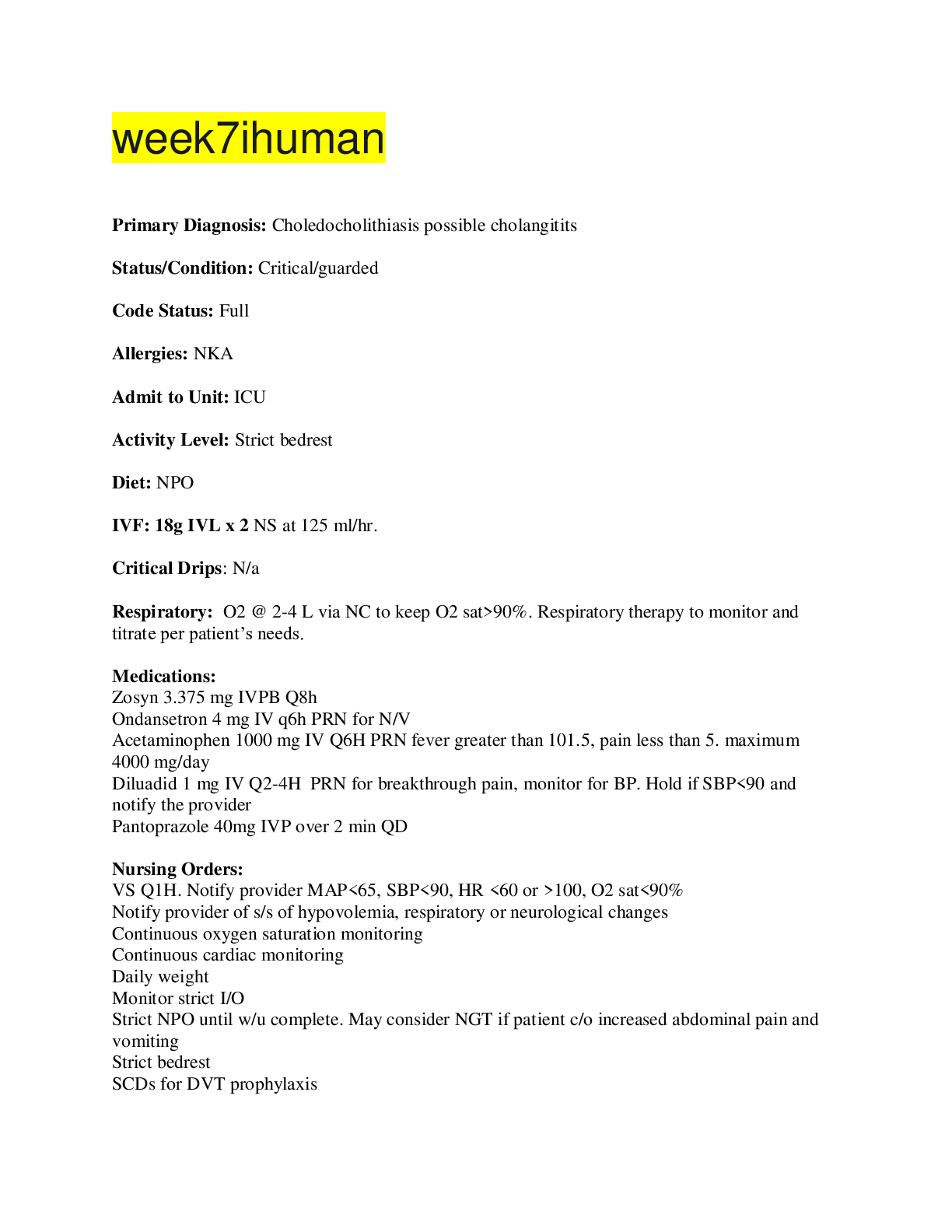
week7ihuman
Primary Diagnosis: Choledocholithiasis possible cholangitits
Status/Condition: Critical/guarded
Code Status: Full
Allergies: NKA
Admit to Unit: ICU
Activity Level: Strict bedrest
Die
...
week7ihuman
Primary Diagnosis: Choledocholithiasis possible cholangitits
Status/Condition: Critical/guarded
Code Status: Full
Allergies: NKA
Admit to Unit: ICU
Activity Level: Strict bedrest
Diet: NPO
IVF: 18g IVL x 2 NS at 125 ml/hr.
Critical Drips: N/a
Respiratory: O2 @ 2-4 L via NC to keep O2 sat>90%. Respiratory therapy to monitor and titrate per patient’s needs.
Medications:
Zosyn 3.375 mg IVPB Q8h
Ondansetron 4 mg IV q6h PRN for N/V
Acetaminophen 1000 mg IV Q6H PRN fever greater than 101.5, pain less than 5. maximum 4000 mg/day
Diluadid 1 mg IV Q2-4H PRN for breakthrough pain, monitor for BP. Hold if SBP<90 and notify the provider
Pantoprazole 40mg IVP over 2 min QD
Nursing Orders:
VS Q1H. Notify provider MAP<65, SBP<90, HR <60 or >100, O2 sat<90%
Notify provider of s/s of hypovolemia, respiratory or neurological changes
Continuous oxygen saturation monitoring
Continuous cardiac monitoring
Daily weight
Monitor strict I/O
Strict NPO until w/u complete. May consider NGT if patient c/o increased abdominal pain and vomiting
Strict bedrest
SCDs for DVT prophylaxis
Follow Up Lab tests:
Amylase, lipase, type and screen for PRBCs, CBC and CMP daily, PT/PTT/INR now.
Lipid panel, Blood cultures x 2 sets prior to initiating the antibiotics
Diagnostic testing:
ERCP with papillotomy with stone extraction ASAP-removal of stone from bile duct
Consults:
Gastroenterologist consult stat- Choledocholithiasis, ERCP and papillotomy
General surgery stat- Choledocholithiasis possible cholecystectomy
Patient Education and Health Promotion
Pathophysiology of gallbladder disease
risk factors of the disease
advanced age,
obesity,
diet
heredity
hyperlipidemia.
Symptoms of gallbladder disease
Prevention of progression of gallbladder disease
Discharge planning and required follow-up care
Discharge patient home on PO medications when stable
F/U with PCP within 24-48 hours.
F/U with surgeon per his order
Take medications as ordered.
Do not stop or skip the medications even if you feel better without consulting the PCP.
Call your healthcare provider right away if you have any of the following:
Tiredness that persists for 2 to 3 days,
decreased exercise tolerance,
chest pain or pressure feeling,
persistent SOB at rest or with mild activities,
fever over 100.4°F (38.0°C),
sweats,
increase and pounding heart rate,
difficulty catching breath,
persistent cough,
blood in the sputum
feeling of impending doom.
Discharge patient home when symptoms have resolved and patient is hemodynamically stable.
F/U with general surgery after discharge
References
Doherty, G. M. (2015). Current diagnosis & treatment: Surgery (14th ed.). New York:
McGraw Hill Education.
Papadakis, M. A., McPhee, S. & Rabow, M.W. (2019). Current medical diagnosis &
treatment 2019 (58th ed.). New York: McGraw Hill Education.
Sabatine, M. S. (2017). Pocket Medicine. The Massachusetts General Hospital Handbook of Internal Medicine (6th ed.). Philadelphia: Wolters Kluwer.
[Show More]