*NURSING > EXAM > Paramedic Care- Principles & Practice, V5, 5e Bledsoe Lesson Plan, Test Bank, Quiz, Chapter Review, (All)
Paramedic Care- Principles & Practice, V5, 5e Bledsoe Lesson Plan, Test Bank, Quiz, Chapter Review, And Answer Key. Chapter 1-16. Questions And Answers468 Pages.
Document Content and Description Below
Paramedic Care- Principles & Practice, V5, 5e Bledsoe Lesson Plan, Test Bank, Quiz, Chapter Review, And Answer Key. Chapter 1-16. 468 Pages. Detailed Lesson Plan Gynecology 85–110 Minutes Cha pter 1... objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture. 5 II. Introduction A. The term gynecology is derived from Greek gynaik, meaning woman. B. Branch of medicine that deals with health and diseases of women and their reproductive organs C. Obstetrics is the branch that deals with care of women throughout pregnancy. D. Most patients experience abdominal pain or vaginal bleeding. 15 III. Anatomy and Physiology A. Understanding of anatomy and physiology of the female reproductive system will allow better understanding, recognition, and treatment of emergencies as they arise B. Female Reproductive Organs 1. External genitalia have accessory functions and include the perineum, mons pubis, labia majora and minora, clitoris, and urethra. a. Perineum – skin-covered tissue that separates the vagina and anus; term may include entire vulvar area; may be torn during childbirth or sexual assault b. Mons pubis – fatty layer over the symphysis pubis that protects symphysis pubis during intercourse c. Labia majora – structure that is located laterally and protects Teaching Tips Use an anatomic model, picture, etc. to show students the female reproductive system, which will allow them a visual of how close all organs are to each other and why internal bleeding can be hidden. MASTER TEACHING NOTES Teaching Tips Discussion Topics Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes vagina and urethra d. Labia minora – structure that is located medial and protects vagina and urethra e. Clitoris – highly innervated, major site of sexual stimulation f. Urethra – located superior and anterior to vagina; drains the urinary bladder; owing to decreased length, females are more susceptible to bladder infections 2. Internal organs are located within pelvic cavity and include ovaries, fallopian tubes, uterus, and vagina. a. Vagina – three functions: female organ of copulation, final passageway during childbirth, and outlet for menstrual blood and tissue b. Uterus – primary function: to provide site for fetal development; muscle of pregnancy that has a body (fundus) and neck (cervix); innermost layer called endometrium, middle layer called myometrium, and outer layer called perimetrium c. Ovaries – primary female sex glands that are situated laterally on either side of uterus; two functions: secretion of estrogen and progesterone and development and release of eggs for reproduction d. Fallopian tubes – flexible tubes that extend from uterus to each ovary; function of tubes: to conduct egg from ovary into uterine cavity using peristalsis 15 IV. The Menstrual Cycle A. Hormonal cycle generally occurring every 28 days B. Prepares uterus to receive fertilized egg C. Onset of menstrual cycle, menarche, usually begins between 10 and 14 years of age. D. A normal menstrual cycle varies for each woman, so it is important to inquire as to the normal length for the woman in question. E. Female sex hormones estrogen and progesterone control the ovarian menstrual cycle, pregnancy, and lactation (estrogen and progesterone Teaching Tips Cover with students the various hormones related to the female cycle, explaining which hormones are secreted by the ovaries and which by the pituitary.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes secretion controlled by follicle-stimulating hormone [FSH] and luteinizing hormone [LH] secretion). F. Proliferative Phase 1. First two weeks of menstrual cycle 2. Dominated by estrogen, which causes lining of uterus to thicken 3. Ovulation takes place due to surge of LH at day 14. a. Immature ovarian follicles, graafian follicles, are present in female at birth and gradually used up during lifetime. b. Follicle reaches maturity due to FSH and increased estrogen. c. Follicle ruptures and discharges egg through ovary. d. Ruptured follicle develops the corpus luteum (body of cells). e. If not fertilized, corpus luteum will atrophy within 3 days. f. If fertilized, corpus luteum produces progesterone until placenta takes over. G. Secretory Phase 1. Stage immediately surrounding ovulation 2. If egg is not fertilized, estrogen levels drop while progesterone dominates. 3. Uterine vascularity increases in anticipation of fertilized egg. H. Ischemic Phase 1. If fertilization does not occur, estrogen and progesterone levels drop 2. Endometrium undergoes vascular changes that cause small blood vessel rupture. I. Menstrual Phase 1. Ischemic endometrium is shed. 2. Menstrual flow usually lasts 3–5 days. 3. Average blood loss is 50 mL. 4. Premenstrual syndrome can be experienced, and includes physical changes related to changing hormone levels. 5. Absence of a menstrual cycle in a sexually active woman of childbearing years should raise suspicion of pregnancy. J. Premenstrual Dysphoric Disorder (PMDD) 1. Condition similar to premenstrual syndrome, but symptoms more©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes severe 2. Includes a wide range of physical and/or emotional symptoms K. Menopause 1. Cessation of menses, marks cessation of ovarian function 2. Menses declines around 45–55 years old, until menses stops 3. End of reproductive life 4. Sexual hormones decline 15 V. Assessment of the Gynecologic Patient A. Most common complaints are abdominal pain and vaginal bleeding 1. Dysmenorrhea – severe discomfort during menstrual periods 2. Dyspareunia – painful sexual intercourse B. Complete primary and secondary assessments; specific questions must be asked regarding reproductive function and dysfunction C. History D. OPQRST for chief complaint E. SAMPLE for past medical history F. Any associated symptoms? G. Obstetrical history H. Last menstrual period I. Sexually activity J. Possibility of pregnancy K. Contraceptive use L. Physical exam M. Exam limited in the field N. Patient comfort guide’s exam O. Always have a chaperone if an examination is necessary. and explain to the patient what you will be doing. P. Indicators during the assessment include: 1. Mental status 2. Skin, mucous membranes 3. Pulse rate, blood pressure 4. Orthostatic changes in vital signs 5. Evidence of vaginal bleeding (how many vaginal pads used?) Class Activities Have students break into groups, and ask the specific questions that would be related to the gynecologic patient. Afterward, discuss whether any students were uncomfortable asking the questions, and discuss ways to lessen this discomfort. Obtain several types of feminine care products (various size maxi/mini pads, tampons). Using blue- or green-tinted water and a 100-cc syringe, place water on each item in 10- to 20-cc increments until the item is saturated. This allows students to have an estimated approximation of the amount of blood these items can hold, allowing a better idea of blood loss when asking the patient, “How many pads have you gone through?”©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 6. Abdominal examination; palpate, auscultate 7. NEVER perform an internal vaginal exam in the field 5 VI. Management of Gynecologic Emergencies A. Majority of care will be supportive. B. Primary assessment survey will guide care decisions. 1. O2, EKG, IV, analgesics, etc. C. Monitor and evaluate serious bleeding; do not pack vagina with dressings. D. Patient positioning may include left lateral recumbent with knees bent, which decreases tension on peritoneum. E. Transport for evaluation F. Psychological support Discussion Topics Discuss with students why the left lateral/knees bent position may be most comfortable and why bleeding in the abdomen may cause shoulder pain. 30 VII. Specific Gynecologic Emergencies A. Medical Gynecological Emergencies 1. Pelvic inflammatory disease: infection of reproductive tract a. Bacterium, virus, or fungus b. Most common cause of nontraumatic abdominal pain c. Common causes: gonorrhea, chlamydia d. Signs and symptoms include diffuse abdominal pain, shuffling gait, fever, chills, nausea, vomiting, vaginal discharge. e. Treatment includes ABCs, supportive care, comfort, transport, antibiotics. 2. Ruptured ovarian cyst: fluid-filled pockets on ovary that rupture a. Cyst that ruptures may spill small amount of blood into abdomen. b. Signs and symptoms include moderate to severe unilateral abdominal pain, pain that may radiate to back, dyspareunia, irregular bleeding, delayed menstrual period. c. Treatment includes ABCs, supportive care, comfort, transport, surgical interventions. 3. Cystitis: urinary bladder infection Discussion Topics Ask students why they think their patient may be uncomfortable with the gynecologic emergency and/or exam. Discuss with students ways to make the patient more comfortable. Knowledge Application Create a chart with each emergency listed. Have three columns: for Definition, Signs and Symptoms, and Treatment. Have students complete the chart for homework. Points to Emphasize Stress to students how their behavior in treating a sexual assault patient could cause further harm to the patient.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. Common cause of abdominal pain b. Signs and symptoms include abdominal pain, urinary frequency, dysuria, low-grade fever, hesitancy in urination, blood in urine. c. Treatment includes ABCs, supportive care, comfort, transport, antibiotics. 4. Mittelschmerz – midcycle abdominal pain at ovulation a. Peritoneal irritation due to follicle rupture b. Signs and symptoms include unilateral lower quadrant pain, midcycle spotting, low-grade fever (although body temperature normally increases during ovulation) c. Treatment includes ABCs, supportive care, comfort, transport 5. Endometritis – infection of uterine lining a. Occasional complication from miscarriage, childbirth, dilation and curettage (D&C) b. May mimic pelvic inflammatory disease (PID) c. Complications can include sterility, sepsis, death. d. Signs and symptoms include lower abdominal pain; bloody, foulsmelling discharge; fever (101–104°F); appearance of symptoms 48–72 hours after gynecologic event. e. Treatment includes ABCs, supportive care, comfort, transport, antibiotics, surgical interventions. 6. Endometriosis – endometrial tissue found outside of uterus a. Most commonly found in abdomen and pelvis but can be found anywhere b. Tissue responds to hormone changes, causing cyclic inflammation, scarring of tissues, adhesions. c. Signs and symptoms include dull, cramping pelvic pain usually related to menstruation, dyspareunia, abnormal vaginal bleeding, painful bowel movements. d. Treatment includes ABCs, supportive care, comfort, transport, hormones, analgesics, anti-inflammatory drugs, surgery. 7. Ectopic pregnancy – implantation of fetus outside of uterus a. Most common site is fallopian tube©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes b. Surgical emergency c. Signs and symptoms include severe unilateral pain, radiation of pain to shoulder on affected side, late or missed period, possible vaginal bleeding. d. Treatment includes ABCs, supportive care, comfort, transport, surgical intervention. 8. Nontraumatic vaginal bleeding – vaginal bleeding not associated with menstruation a. Called dysfunctional uterine bleeding b. Most common cause is spontaneous abortion (miscarriage) c. Other causes include uterine fibroids (noncancerous tumors in uterus), cancerous lesions, PID, onset of labor. d. Signs and symptoms include vaginal bleeding, abdominal pain. e. Treatment includes ABCs, supportive care, comfort, transport, possible surgical interventions. 9. Management for medical gynecological emergencies may include oxygen, IV and fluids, electrocardiogram (ECG), transport (remember to NEVER pack vagina with dressing), absorb bleeding with pads. B. Traumatic Gynecological Emergencies 1. Causes of gynecologic trauma include straddle injuries, sexual assault, blunt force to lower abdomen, direct blows to perineal area, foreign body insertion, self-attempts at abortion, lacerations following childbirth. 2. Management for gynecologic traumatic includes direct pressure over laceration or chemical cold pack to hematoma, oxygen, IV and fluids for signs of shock, transport, possible surgical intervention. 3. Sexual assault a. Most rapidly growing crime in America b. No “typical” victim c. Common element is sexual contact without consent, resulting in crime of violence with serious physical and psychological implications. d. Assessment: unique patient with unique needs i. As a rule, do not question about the incident in©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 8 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes the field. ii. Confine questions to physical injuries. iii. Patient may be withdrawn, hysterical, in denial, angry, or fearful. iv. Be calm and professional in your approach. v. Do not examine genitalia unless life-threatening hemorrhage is present. vi. Look for possible signs of “date-rape” drug symptoms. e. Management: In most situations, psychological and emotional support it the most important help you can offer. i. Try to use same-gender paramedic for care. ii. Disturb crime scene as little as possible. iii. Bag clothing or other evidence in paper bags. iv. Do not allow patient to change clothes or bathe. f. Documentation: state patient remarks accurately, state observations, document evidence, do not include opinions. 5 VIII.Summary A. Majority of gynecologic emergency patients will present with abdominal pain and/or bleeding B. This area of care may be uncomfortable for patient, but a detailed history is beneficial to care. C. Best historian is patient. D. Very few things paramedic can do for gynecologic emergencies, outside of ABCs, O2, IV/fluids if necessary, ECG, comfort, and transport. E. Treat patient symptomatically and with dignity . 5 IX. Case Study Class Activities Discuss the case with the students now that they are familiar with the chapter.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 9 Chapter 1 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 X. You Make the Call Class Activities Read and discuss the call and questions as a group. 5 XI. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 1 Detailed Lesson Plan Chapter 2 Obstetrics 220–230 Minutes Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture. 5 II. Introduction A. The focus of this chapter is pregnancy, childbirth, and potential complications B. Pregnancy is a natural, normal process that occurs daily and normally requires only the most basic assistance 5 III. The Prenatal Period A. Prebirth period from time of conception until delivery of fetus B. Significant changes in mother, along with fetal development C. Health care visits during this period are referred to as prenatal visits or prenatal care. 10 IV. Anatomy and Physiology of the Obstetric Patient A. Ovulation 1. Release of egg from ovary, which, if fertilized, becomes implanted in uterus and pregnancy begins 2. Ovulation usually occurs on average 14 days from menstrual cycle, but may vary by several days B. Fertilization 1. Ovum begins cellular division. 2. Becomes blastocyst (hollow ball of cells), and implants in uterine lining C. Placenta 1. Organ of pregnancy Teaching Tips Use an anatomy and physiology model so students can visualize the structures of pregnancy. MASTER TEACHING NOTES Teaching Tips Discussion Topics Class Activities Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. Develops on uterine wall at site of blastocyst attachment 3. Temporary structure that transfers heat, exchanges O2 and CO2, delivers nutrients, carries away wastes, serves as endocrine gland during pregnancy, serves as protective barrier against some harmful substances 4. When expelled following delivery of child, referred to as afterbirth D. Umbilical Cord 1. Connects placenta to fetus 2. Flexible, rope-like cord that is 2 feet in length 3. Normally contains two arteries and one vein 4. Vein transports oxygenated blood to fetus, and arteries return deoxygenated blood to placenta E. Amniotic Sac 1. Fetus develops within this sac, which is filled with amniotic fluid. 2. Referred to as “bag of waters” F. Amniotic Fluid 1. Surrounds and protects fetus during development 2. Volume of fluid by 20th week of gestation: 500–1,000 mL 3. Allows fetal movement 4. Secretions from fetus (lungs and urination) contribute to fluid 5. Rupture of membranes usually occurs during labor, with flow of fluid from vagina 10 V. Physiologic Changes of Pregnancy A. Due to altered hormonal state, mechanical effects of enlarging uterus and vascularity, and increasing metabolic demands on mother B. Reproductive System 1. Most significant change occurs in uterus. 2. By end of pregnancy, uterus will weigh 1,000 grams. 3. Vascular system of uterus contains 1/16 of mother’s total blood volume during pregnancy. 4. Formation of mucus plug in cervix, which protects fetus and prevents infection, and is expelled when cervical dilation begins 5. Estrogen causes thickened vaginal mucosa, increased vaginal secretions, and loosens connective tissue to allow for delivery. 6. Breasts enlarge as mammary glands prepare for lactation. Class Activities As you discuss the changes that pregnancy causes for each body system, ask your students what aspects of their assessment and care need to be altered, if any, for a pregnant patient.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes C. Respiratory System 1. Maternal oxygen demand increases. 2. Decrease in airway resistance as a result of progesterone 3. 20% increase in O2 consumption and 40% increase in tidal volume 4. Slight increase in respiratory rate 5. Diaphragm pushed up by enlarging uterus D. Cardiovascular System 1. Cardiac output increases by 30–50% throughout pregnancy, peaking at 6–7 L/minute by pregnancy term. 2. Systemic vascular resistance decreases. 3. Maternal blood volume increases 45%. 4. Relative anemia occurs, due to slightly more plasma increase than RBC increase. 5. Due to increase in blood volume, mother may suffer an acute blood loss of 30–35% without significant changes in vital signs. 6. Maternal heart rate increases 10–15 beats/minute. 7. Blood pressure is slightly decreased during first two trimesters, then rises to normal levels during third trimester. 8. Supine hypotensive syndrome occurs when the uterus compresses the inferior vena cava while mother lies in the supine position. E. Gastrointestinal System 1. Nausea and vomiting are common in first trimester due to hormone levels. 2. Delayed gastric emptying is present, resulting in bloating or constipation. 3. As the uterus grows, abdominal organs are compressed. F. Urinary System 1. Renal blood flow increases. 2. Glomerular filtration rate (GFR) increases 50% 3. Urinary bladder displaced, causing urinary frequency G. Musculoskeletal System 1. Loosened pelvic joints results from hormonal influences, giving mother a waddling gait. 10 VI. Fetal Development A. Begins immediately after fertilization and is complex©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes B. Normal duration of pregnancy is 40 weeks from first day of mother’s last menstrual period, equaling 280 days. C. Estimated birth date is called due date, or estimated date of confinement. D. Pregnancy is divided into three trimesters, each three calendar months long. E. Preembryonic stage: first 14 days after conception F. Embryonic stage: day 15 and ends at 8 weeks G. Fetal stage: 8 weeks until delivery H. Sex of infant is usually determined by 16 weeks of gestation. I. Fetal heart tones are detected by stethoscope by 20 weeks of gestation, and mother has felt movement. J. Infant may be able to survive by 24 weeks of gestation, and if born after 28 weeks, there is an excellent chance of survival. K. Baby is considered term by 38th week of gestation. L. Most fetal organs develop during first trimester, which is when fetus is most vulnerable to development of birth defects . 10 VII. Fetal Circulation A. Fetus receives O2 and nutrients from mother through placenta. B. Fetus does not need respiratory or gastrointestinal (GI) tract while in utero. C. Fetal circulation shunts blood around lungs and GI. 1. Umbilical vein connects directly to inferior vena cave by ductus venosis, allowing blood to enter right atrium and pass through tricuspid and into right ventricle, exiting right ventricle and traveling through pulmonic valve into pulmonary artery. 2. Fetal heart has a hole between right and left atria, called the foramen ovale, allowing oxygenated blood in right atrium to mix with blood leaving left ventricle, which is bound for aorta. 3. Oxygenated blood now in pulmonary artery will enter the ductus arteriosus, which connects pulmonary artery with aorta, causing blood to bypass the uninflated lungs. D. Fetal circulation changes immediately at birth. 1. First breath of fetus causes lungs to inflate, decreasing pulmonary vascular resistance, and closure of specialized circulation structures occurs. Teaching Tips Use an anatomic model to explain the specialized structures of fetal circulation. Discussion Topics Discuss with students what they might see in a newborn when the specialized structures of circulation do not close appropriately.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 20 VIII.General Assessment of the Obstetric Patient A. Primary Assessment 1. Same as for nonobstetric patients 2. Special attention is paid to the developing fetus. a. SAMPLE history b. General information to include gravidity, parity, length of gestation, estimated due date, any known GYN/OB complications in past, any current prenatal care, medications/allergies, and so forth B. Preexisting or Aggravated Medical Conditions 1. Diabetes a. May become unstable during pregnancy b. Mother may develop gestational diabetes (diabetes developed during pregnancy). c. Poorly controlled diabetes can result in large infants and possibly birth defects. 2. Heart disease a. Congestive heart failure (CHF) may develop in a mother who has serious preexisting heart disease due to the increased cardiac output. 3. Hypertension (HTN) a. Preexisting HTN is aggravated by pregnancy. b. Preeclampsia may contribute to maternal HTN. c. Persistent HTN can affect placenta, compromising fetus. 4. Seizure disorders a. Most patients with seizure disorders are controlled by medication and have uneventful pregnancies. 5. Neuromuscular disorders a. Disorder may be aggravated by pregnancy, but more likely mother will experience remission of symptoms. 6. Pain a. Determination of when pain started, character of pain, location, duration, radiation is of utmost importance. 7. Vaginal bleeding a. Vaginal bleeding or spotting is major concern in obstetrics. b. Color, amount, duration of bleeding, events prior to event, passing Teaching Tips Go over all of the special vocabulary related to pregnancy. Class Activities Have students break into groups and perform an obstetric assessment.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes of tissues/clots, any other discharge present 8. Active labor a. Assess whether mother feels need to push, or move bowels, if membranes have ruptured. 9. Physical examination a. Protect patient’s modesty and dignity. b. Measurement of fundal height allows for estimated date of pregnancy. c. Vital signs taken with patient on left side and orthostatic vital signs may be helpful in determining shock (not to be done if patient is in obvious shock). d. Examination of genitals may include vaginal discharge, progression of labor, prolapsed cord, crowning (bulging of fetal head past vaginal opening, an indication of impending delivery). 5 IX. General Management of the Obstetric Patient A. Two patients present: mother and fetus B. Fetal well-being depends on mother’s well-being. C. Management includes ABCs, O2, IV, fluids, electrocardiogram (ECG), position of comfort, analgesic use must be done with caution, transport . 30 X. Complications of Pregnancy A. Trauma 1. Motor vehicle collisions (MVCs), falls, physical abuse 2. Most frequent nonobstetric cause of death in pregnant women 3. Primary cause of fetal death is maternal death 4. Anticipation of shock necessary on basis of mechanism of injury (MOI) rather than vital signs, due to physiologic changes in mother 5. Direct abdominal trauma may result in separation of placenta from uterine wall, preterm labor, abortion, uterine rupture, and possible fetal death. 6. Signs and symptoms may include vaginal bleeding, tender abdomen, MOI. 7. Management includes C-collar, spinal immobilization (with board and patient tilted onto left side), oxygen if patient is hypoxic, IV and fluids, reassessment, monitoring of fetus, and transport. Teaching Tips Go over the definitions for the terms for medical abortions. Knowledge Application Create a chart with each complication; have three columns: for Definition, Signs and Symptoms, and Treatments. Have students complete the chart for homework.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes B. Medical Conditions 1. Abdominal pain is most common complaint, due to stretching of ligaments. 2. Appendicitis and cholecystits can occur. 3. Signs and symptoms may include right upper quadrant or back pain. 4. Management includes ABCs, O2, comfort, and transport. C. Bleeding in Pregnancy 1. May occur due to abortion, ectopic pregnancy, placenta previa, or abruptio placentae. 2. Vaginal bleeding associated with potential fetal loss 3. Signs and symptoms may include vaginal bleeding, pain, or shock. 4. Management includes ABCs, O2, IV and fluids, comfort, and transport. D. Abortion 1. Expulsion of fetus before 20 weeks 2. Most common cause of bleeding in first and second trimester 3. Abortion and miscarriage used interchangeably (abortion generally considered termination of pregnancy at mother’s request, whereas miscarriage seen as accident of nature) 4. Spontaneous abortion commonly seen between 12 and 14 weeks 5. Signs and symptoms include cramping abdominal pain, backache, vaginal bleeding. 6. Management includes ABCs, O2 if hypoxic, position of comfort, IV and fluids if needed, save any tissues/clots to transport with mother, emotional support, orthostatic vital signs. E. Ectopic Pregnancy 1. Abnormal implantation of fertilized egg outside of uterus 2. Significant life threat to mother 3. 95% implanted in fallopian tube 4. Predisposing factors can include pelvic inflammatory disease (PID), previous ectopic pregnancy, pelvic or tubal surgery, endometriosis, intrauterine device (IUD) use. 5. Signs and symptoms include abdominal pain on affected side, missed period or last menstrual period (LMP) four to six weeks ago, rigid abdomen, syncope, vaginal bleeding, shock. 6. Management includes ABCs, O2 if patient hypoxic, IV and fluids,©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 8 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes comfort, transport; definitive care includes surgical interventions. F. Placenta Previa 1. Abnormal implantation of placenta on lower half of uterine wall, partially or completely covering cervical opening 2. Predisposing factors may include history of placenta previa, multiparity, increased maternal age, uterine scar tissue, large placenta, defective development of blood vessels on uterine wall. 3. Signs and symptoms include third trimester of pregnancy, painless and bright red vaginal bleeding (note: hallmark of placenta previa). 4. Management includes ABCs, O2 as needed, IV and fluids, treat for shock, and transport to hospital with obstetrical surgical capability. G. Abruptio Placentae 1. Premature separation of normally implanted placenta from uterine wall 2. Potential life threat to both mother and fetus 3. Predisposing factors may include multiparity, maternal HTN, trauma, cocaine use, increasing maternal age, and history of previous abruption. 4. Signs and symptoms include sharp, sudden, tearing pain, stiff, boardlike abdomen, vaginal bleeding, maternal hypotension. 5. Management includes ABCs, O2, IV and fluids, left lateral recumbent (LLR) position, transport to hospital with obstetrical and high-risk neonatal care. H. Hypertensive Disorders of Pregnancy 1. Preeclampsia a. Progressive disorder b. Defined by increased blood pressure, protein in urine, and edema 2. Eclampsia a. HTN, protein in urine, edema, visual disturbances that precede generalized tonic–clonic seizures 3. Chronic HTN a. Blood pressure 140/90 or higher before pregnancy or before 20th week of gestation 4. Transient HTN a. Temporary rise in blood pressure occurring during labor or postpartum 5. Signs and symptoms include excessive weight gain, headaches, visual©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 9 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes disturbances, apprehension, upper right quadrant pain, seizures, pale, and hyperactive reflexes. 6. Management includes ABCs, O2 if hypoxic, keep patient calm, dim lights and any sensory stimulation, IV and fluids, LLR position, antihypertensive may be ordered by medical control, and transport. E. Supine Hypotensive Syndrome 1. Usually occurs during third trimester 2. Uterus compresses vena cava when mother is in supine position 3. Signs and symptoms include late in pregnancy, supine position, dizziness, syncopal episode. 4. Management includes ABCs, O2 if hypoxic, IV and fluids if needed, LLR position, check orthostatic vital signs, ECG, and transport. F. Gestational Diabetes 1. Placental hormones become resistant to increase in insulin production, causing decreased glucose tolerance. 2. Signs and symptoms include ketones present in urine, altered mental status, diaphoresis, tachycardia. 3. Management includes ABCs, O2 if hypoxic, IV and fluids if needed, blood glucose level (BGL), D50 if hypoglycemic, and prenatal care required for diabetes management. G. Braxton-Hicks Contractions 1. Painless, irregular contractions that are thought to be conditioning uterus and enhancing placental circulation 2. Do not cause cervical changes 3. Impossible to distinguish false labor from true labor in the field 4. Signs and symptoms include tightening of uterus. 5. Management includes ABCs, reassurance, transport. H. Preterm Labor 1. True labor that begins before 38th week of gestation 2. Signs and symptoms include contractions that occur every 10 minutes or less, low abdominal cramping, sensation of pelvic pressure, low backache, changes in vaginal discharge, rupture of membranes may occur. 3. Management includes should be stopped with tocolytics if possible, although infrequently done in the field; ABCs; O2 if hypoxic; IV and fluid©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 10 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes bolus of 1 liter to help inhibit release of oxytocin; magnesium sulfate or terbutaline; transport to facility with obstetric and high-risk neonatal capabilities . 10 XI. The Puerperium A. Time period surrounding birth of fetus B. Labor 1. Process by which delivery occurs (mechanical and physiologic) 2. Delivery of fetus is culmination of pregnancy 3. Excretion of bloody show is usually sign of imminent labor. C. Stages of Labor 1. Stage one (dilation stage) Begins with onset of true labor contractions and ends with complete dilation (10 cm or about 4 inches) and effacement of cervix. a. Usually lasts 8–10 hours in woman in first labor b. Usually lasts 5–7 hours in woman who has given birth before 2. Stage two (expulsion stage) a. Begins with complete dilation of cervix and ends with delivery of fetus b. Usually lasts 50–60 minutes in nullipara and 25–30 minutes in multipara c. Urge to push usually begins, and membranes tend to rupture. d. Crowning present 2. Stage three (placental stage) a. Third and final stage of labor b. Begins immediately after birth of infant and ends with delivery of placenta c. Placenta generally delivers within 5–20 minutes. 5 XII. Management of a Patient in Labor A. One of the most important decisions will be whether to deliver infant in field versus transport. B. Signs of imminent delivery include crowning, maternal urge to push, number of previous pregnancies, frequency of contractions.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 11 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes C. Indications of prompt immediate transport, despite threat of delivery include prolonged rupture of membranes (> 24 hours), abnormal presentation, fetal distress, and multiple fetuses. 15 XIII.Field Delivery A. Prepare equipment quickly and set up delivery area (keeping patient on the cot is recommended, if possible). B. Administer O2 if mother is hypoxic, and establish IV if time permits. C. Place patient on back with buttocks slightly raised, and drape mother with toweling. D. Monitor fetal heart rate (drop of rate < 90 bpm indicates prompt immediate transport). E. If no delivery after 20 minutes of contractions that are every 2 minutes, transport immediately. F. Prepare OB kit, and use universal precautions. G. As head crowns, apply gentle pressure to avoid explosive delivery and tearing of mother’s perineum. H. If amniotic sac still in place, tear open with finger. I. Slide your finger along infant’s head and neck to ensure that the umbilical cord is not wrapped around the infant’s neck (nuchal cord). If the cord is wrapped around neck, try to remove it by slipping it over infant’s head; if cord is wrapped too tight, clamp the cord and cut. J. Support baby’s head as it rotates. K. Gently guide baby’s head downward to allow delivery of shoulders, and then guide baby’s body upward to allow delivery of lower shoulder. Rest of baby’s body will follow rapidly. L. Support baby’s body, and keep at level of vagina. M. Place first umbilical cord 10 cm from baby and second 5 cm above first; cut cord between clamps. N. Wipe baby’s face clean, and suction mouth and nose until airway clear. O. Dry and cover infant, keeping baby warm and positioned on side. P. Maternal blood loss is expected at 500 mL, and once separation of placenta from uterine wall takes place, the umbilical cord will appear to lengthen—DO Classroom Activities Obtain an OB kit, and have students go through each piece of equipment, describing the use of each. Then take students through the steps of a delivery.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 12 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes NOT PULL ON CORD; once placenta is delivered, transport with mother to hospital; if placenta does not deliver immediately, transport does not have to be delayed. Q. To further decrease vaginal bleeding, massage the uterus or allow infant to nurse; both will stimulate uterine contractions. R. After delivery, inspect mother for perineum tears, and apply vaginal pad to absorb bleeding; continuously monitor vital signs. S. Pitocin may be ordered by medical control in cases of postpartum hemorrhage. 10 XIV. Neonatal Care A. Routine Care of the Neonate 1. Maintain warmth a. Cold infants become distressed very quickly. b. Dry infant, and then wrap in clean, warm towels/blankets. c. Keep head warm. 2. Clear the airway. a. Routine suctioning of neonate when amniotic fluid is clear is no longer recommended unless neonate has obvious obstruction to spontaneous breathing. b. Drying and tactile stimulation should cause infant to “pink up.” c. Extremities may still appear dusky (acrocyanosis). d. Normal respiratory rate:30–60 breaths/minute; heart rate:100–180 beats/minute 3. APGAR scoring a. Appearance, Pulse, Grimace, Activity, Respiration b. APGAR score taken at 1 minute and 5 minutes after birth c. Normal APGAR is usually between 7 and 10; infants between 4 and 6 are moderately depressed and require O2 and stimulation; infants between 0 and 3 are severely depressed and require immediate ventilator and circulatory assistance. Classroom Activities Using a newborn mannequin, have students practice neonatal care.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 13 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 10 XV. Neonatal Resuscitation A. Factors that contribute to resuscitation include prematurity, pregnancy and delivery complications, maternal health problems, and inadequate prenatal care. B. If tactile stimulation does not increase neonate respiratory rate, immediately assist with bag-valve mask (BVM); assess heart rate using stethoscope to auscultate apical pulse, feeling for pulse at base of umbilical cord or palpating brachial/femoral. C. If heart rate > 100 bpm with spontaneous respirations, continue assessment. D. If heart rate < 100 bpm, continue positive pressure ventilations. E. Initiate chest compressions if heart rate is < 60 bpm and not responding to ventilations. F. Make every effort to expedite transport. G. Vascular access may be necessary if transport time is long; most accessible is umbilical vein. H. Maintain warmth of infant at all times. 15 XVI. Abnormal Delivery Situations A. Breech Presentation 1. Most infants present head first and face down. 2. In breech presentation, buttocks or both feet present first. 3. Increase risk for delivery trauma to mother, prolapsed cord, cord compression, anoxia to infant 4. Commonly associated with preterm birth, placenta previa, multiple gestation, uterine and fetal anomalies 5. Management includes position mother with buttocks at edge of cot/bed, with legs in flexed position, support infant’s legs as they deliver; as head passes pubis, apply gentle upward traction until mouth appears; if head does not deliver and baby begins breathing spontaneously, insert index and middle fingers into vagina in V shape, pushing against vaginal wall—this will allow unrestricted respiration; continue during transport; if shoulders deliver first, you may have to support infant’s body and extract 4–6 inches of umbilical cord. B. Prolapsed Cord Classroom Activities Using an OB mannequin, have students practice going through each abnormal delivery presented.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 14 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Occurs when umbilical cord precedes the fetal presenting part, causing compression of cord, cutting off fetal circulation 2. Commonly associated with prematurity, multiple births, premature rupture of membranes 3. Serious emergency that can cause fetal death quickly without prompt intervention 4. Management includes: insert two fingers into vagina to raise presenting part of fetus off the cord, while checking cord for pulsations; place mother in Trendelenburg position or knee-chest position, administer O2 if hypoxic, and transport immediately, while holding presenting part off of cord; if possible, apply moistened dressing to exposed cord. C. Limb Presentation 1. If baby in transverse position, arm or leg may be presenting part. 2. May be associated with preterm birth, multiple gestation 3. Management includes: place mother in knee-chest position, administer O2 if hypoxic, transport immediately—cesarean section is necessary— do not touch presenting extremity, as touching may cause infant to gasp, inhaling and aspirating amniotic fluid. D. Occipital Posterior 1. Descending of infant facing forward 2. Management includes early recognition, reassurance, O2 if hypoxic, immediate transport. 15 XVII. Other Delivery Complications A. Multiple Births 1. Presence of more than one fetus 2. Management includes normal delivery guidelines but will need additional personnel and equipment; may be one shared placenta or two placentas; after delivery of first baby, clamp and cut cord, then deliver second baby. B. Cephalopelvic Disproportion 1. Infant’s head is too big to pass through the maternal pelvis easily. 2. May be associated with primigravida, diabetes, multiparity, postmaturity 3. Management includes O2 if hypoxic, IV access, and immediate transport. Classroom Activities Using an OB mannequin, have students go through the delivery complications.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 15 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes C. Precipitous Delivery 1. Delivery that occurs after less than 3 hours of labor 2. May be associated with grand multipara 3. Management includes: be prepared and control delivery of infant’s head. D. Shoulder Dystocia 1. Infant’s shoulders are larger than its head. 2. May be associated with diabetic and obese mothers and postterm pregnancies 3. Management includes O2 if mother is hypoxic, have mother drop buttocks off edge of cot/bed and flex thighs upward; apply firm pressure with open hand above symphysis pubis (McRobert’s maneuver); if delivery does not occur, transport immediately. E. Meconium Staining 1. Fetus passes feces into amniotic fluid. 2. Indicative of a fetal hypoxic incident 3. May be associated with prolonged labor but can be seen in term, postterm, or low-birth-weight infants 4. Presence of yellowish-green or dark green amniotic fluid 5. Management includes: if meconium is thin and light colored, no further treatment is generally required; if meconium is thick, suction is necessary until meconium clear from airway. 15 XVIII. Maternal Complications of Labor and Delivery A. Postpartum Hemorrhage 1. Loss of > 500 mL immediately following delivery 2. May be associated with lack of uterine muscle, can occur following multiple births or births of large infants, placenta previa, abruptio placentae, retained placental parts, clotting disorders of mother B. Vaginal/Cervical Tears 1. Signs and symptoms include history, predisposing factors, clinical appearance of patient, vital signs, soft and boggy uterus, steady flow of bleeding from vagina. 2. Management includes ABCs, O2 if hypoxic, IV and fluids, administration of oxytocin per medical direction. C. Uterine Rupture Knowledge Application Create a chart with each complication; have three columns: for Definition, Signs and Symptoms, and Treatments. Have students complete the chart for homework.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 16 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Actual tearing or rupture of uterus 2. May occur with onset of labor, as result of abdominal trauma, or due to prolonged uterine contractions of surgically scarred uterus 3. Signs and symptoms include excruciating abdominal pain, shock, cessation of labor contractions, possible external hemorrhage, absent fetal heart tones, tender and rigid abdomen. 4. Management include: ABCs, O2 at high flow, IV and fluids, monitor vital signs and fetal heart tones, transport rapidly. D. Uterine Inversion 1. Rare emergency 2. Uterus turns inside out after delivery and extends through the cervix. 3. May result from pulling on umbilical cord while awaiting delivery of fetus or placenta 4. Signs and symptoms include profound shock. 5. Management includes: place patient in supine position, O2 if patient hypoxic, IV and fluids; make one attempt to replace uterus by pushing the fundus of inverted uterus toward vagina using palm of hand; if unsuccessful, cover uterus with moistened towels and transport. E. Pulmonary Embolism 1. Presence of blood clot in pulmonary vascular system 2. One of most common causes of maternal death 3. Appears more frequently following cesarean section, but may occur at any time during pregnancy 4. Signs and symptoms include sudden onset of severe dyspnea, sharp chest pain, sense of impending doom, tachycardia, tachypnea, jugular venous distention (JVD), hypotension. 5. Management includes high-concentration O2 and ventilator support as needed, IV and fluids, ECG, monitoring of vital signs and SPO2. XIX. Cardiac Arrest in Pregnancy A. Estimation of Gestational Age 1. Estimate gestational age by comparing the uterine fundal height to the mother’s symphysis pubis 2. Each measured centimeter corresponds to 1 week of gestation. 3. Less accurate when patient is beyond 36 weeks gestation.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 17 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes B. Chest Compressions in Pregnancy 1. Chest compressions should be performed at a rate of at least 100 per minute and at a depth of at least 2 inches (5 centimeters). 2. Full recoil should be allowed before the next compression. 3. Interruptions should be limited. 4. Compression to ventilation ratio of 30:2 C. Aortocaval Compression 1. A large gravid uterus can compress the aorta and the vena cava when the patient is supine. 2. Pregnant patients in cardiac arrest with an estimated gestational age of 20 weeks or greater should receive a procedure called manual lateral uterine displacement (LUD) if technically feasible. 3. Manual LUD can be accomplished from either side of the patient. D. Defibrillation in Pregnancy 1. In cases of cardiac arrest that are due to ventricular fibrillation or pulseless ventricular tachycardia, survival is most likely when rapid defibrillation is provided. 2. Defibrillation and cardioversion are generally considered safe in all stages of pregnancy. E. Airway Management in Pregnancy 1. Hypoxia develops much more quickly in the pregnant patient than in those who are not pregnant. 2. The pregnant patient has limited oxygen reserves, so supplemental oxygen should be provided early in resuscitation. 3. During endotracheal intubation, consider the use of passive oxygenation techniques. F. Use of Emergency Drugs in the Pregnant Cardiac Arrest Patient 1. Pharmacologic therapy for cardiac arrest in the pregnant patient differs little from that for patients who are not pregnant. 2. Epinephrine is preferred over vasopressin because of the effects of vasopressin on the gravid uterus. G. Transport Destinations for the Pregnant Cardiac Arrest Patient 1. The pregnant cardiac arrest patient should be transported to a hospital that has the appropriate staffing and capabilities to manage this type of emergency.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 18 Chapter 2 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 XX. Summary A. Childbirth is a normal process, and emergencies are fairly uncommon B. Complications are unpredictable, and recognition of these emergencies is important in the care of mother and child. C. Vast majority of EMS calls may include obstetric patients who have not received prenatal care. D. When delivery occurs, warmth of infant is imperative to his survival. 5 XXI. Case Study Class Activities Discuss the case with students now that they are familiar with the chapter. 5 XXII. You Make the Call Class Activities Read and discuss the call and questions as a group. 5 XXIII. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 1 Detailed Lesson Plan Chapter 3 Neonatology 170–190 Minutes Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students the case will be reviewed after the lecture 5 II. Introduction A. Neonates—babies less than 1 month old B. Newborns (newly born infants)—first few hours of life C. Two patients to manage with an unexpected field delivery—mother and baby D. This chapter will cover initial care of newborns, focusing on special needs of distressed and premature newborns Class Activities If possible, arrange for an OB/NICU nurse to come in and discuss various newborn situations with the class. 10 III. General Pathophysiology, Assessment, and Management A. Care of newborns follows same priorities as for all patients B. Correct problems detected in primary assessment C. Majority of newborns require no resuscitation beyond suctioning of airway, mild stimulation, and body temperature maintenance D. Quick action of paramedic can make difference between life and death in distressed newborn Discussion Topics Discuss with students possible emergencies that they may encounter with unexpected field deliveries. 15 IV. Epidemiology A. Of newborns, 10% require some assistance to begin breathing at birth B. Less than 1% will require extensive resuscitation, with medications rarely indicated C. As newborn birth weight decreases, complications increase 1. Of newborns < 1500 g (3lbs, 5 ounces), 80% will require resuscitation Teaching Tips Focus on the antepartum and intrapartum risks that can occur. Discussion Topics Discuss with students what measures they can take to resuscitate preterm MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. Antepartum and intrapartum factors can help indicate possible complications D. Successful resuscitation of newly born is aided by training, ongoing practice, and proper supplies 1. OB kit, with resuscitation equipment in various sizes 2. Knowledge of types of facilities available to transport to that specialize in high-risk newborns newborns if available preterm-sized equipment is not stocked on the ambulance. Class Activities Go through the OB kit with students, focusing on resuscitation equipment. Obtain equipment for full-term and preterm infants, and compare the difference in sizes. 20 V. Pathophysiology A. Dramatic changes occur at birth that prepare newborn for extrauterine life 1. Respiratory system must initiate and maintain respirations 2. One-third of fetal lung fluid removed through compression of chest during vaginal delivery 3. Newborn takes first breath within first few seconds after delivery 4. Timing of first breath unrelated to cutting of umbilical cord 5. Factors that stimulate baby’s first breath include: a. Mild acidosis b. Initiation of stretch reflexes in lungs c. Hypoxia d. Hypothermia 6. With first breath, lings rapidly fill with air, displacing remaining fluid 7. Blood flow diverted from ductus arteriosus to lungs, where O2 is picked up 8. If hypoxia or severe acidosis is present, ductus may reopen, which will retrigger fetal circulation, causing ongoing hypoxia (called persistent fetal circulation) 9. Paramedic must facilitate the first few breaths and prevent hypoxia and acidosis by being alert at all times to signs of respiratory distress a. Hypoxemia can lead to permanent brain damage 10. Infant rapidly gasps for breath after initial hypoxia; if asphyxia continues, respiratory movement will cease, heart rate will decrease, Teaching Tips Make sure to cover the special vocabulary associated with neonatology. Discussion Topics Discuss with students what signs and symptoms they may see if one of the specialized fetal circulation structures doesn’t close. Class Activities Have students practice oxygenation of newly born patients with a bag-valve mask on a manikin. Points to Emphasize Make sure students understand that a cold baby is unable to maintain life on its own; when an infant is delivered, the ambulance should be warm to the point that the paramedic is sweating, and infant still needs to be warmed.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes and muscle tone will diminish a. Primary apnea simple stimulation and exposure to oxygen will reverse bradycardia and assist with development of pulmonary perfusion b. Secondary apnea—ongoing hypoxia where infant has several deep gasping respirations; heart rate, blood pressure, and SPO2 continue to fall and infant will become unresponsive to stimulation, and will not spontaneously breath on own; death will occur unless prompt resuscitation is initiated 11. Always assume apnea is secondary in nature and treat rapidly 12. Changes of intrauterine structures occur after birth a. Ductus arteriosus—ligamentum arteriosum b. Foramen ovale—fossa ovalis c. Ductus venosus—ligamentus venosum d. Umbilical vein—ligamentum teres e. Umbilical arteries—constrict 15 VI. Congenital Anomalies A. Two percent of infants born with some congenital problem, which typically arose from a problem in fetal development 1. These defects are the leading cause of death in infants 2. Several anomalies will make resuscitation of newborn more difficult 3. Most common include congenital heart defects a. Patent ductus arteriosus—ductus arteriosus fails to close b. Atrial syndrome septal defects—hole in wall between artria c. Ventricular septal defects—hole in wall between ventricle d. Tetralogy of Fallot—four congenital conditions that decrease ability of lungs to oxygenate blood e. Transposition of the great vessels-—normal right and left ventricle tracts are switched f. Coarctation of aorta—narrowed arch of aorta, obstructs blood flow g. Mitral, pulmonary, or aortic stenosis—problem with mitral, pulmonary, or aortic valve that can cause blood flow obstruction h. Hypoplastic left heart—left side of heart is underdeveloped Discussion Topics Discuss with students during which trimester most fetal development occurs, and what factors can affect this development. Class Activities Obtain photographs of various anomalies. Have students point out what signs and symptoms may be present, along with ways resuscitation may take place. Points to Emphasize Stress to students the importance of prenatal care, such as knowing the anomalies a child may present with, which allows the paramedic to gather©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Noncardiac congenital anomalies a. Diaphragmatic hernia—defect in diaphragm that allows abdominal contents to enter chest b. Meningomyelocele—spinal cord and associated structures may be exposed c. Omphalocele—defect where abdominal contents fill area of umbilicus d. Choanal atresia—presence of bony of membranous septum between nasal cavity and pharynx e. Cleft palate—failure of lip and palate to close f. Cleft lip—failure of upper lip to close g. Pierre Robin syndrome—small jaw, large tongue in conjunction with cleft palate appropriate equipment and adapt treatment. Knowledge Application Create a chart with the listed anomalies. For homework, have students chart definition, signs and symptoms, and treatment for each. 10 VII. Assessment A. Make mental note of time of birth B. Quickly obtain vital signs C. Newborns are SLIPPERY, so support infant with both hands D. Respiratory rate should be 40–60 breaths/minute; if respirations not adequate, or infant is gasping, begin positive pressure ventilation E. Heart rate should be 150–180 beats/minute, slowing to 130–140 beats/minute; < 100 beats/minute indicates distress with emergency intervention required F. Look at skin color—cyanosis of extremities is common immediately after birth G. Pulse oximetry a better indication of O2 saturation—will not reach normal levels until about 10 minutes after birth Critical Thinking Questions Why would it take up to 10 minutes for a newborn’s pulse oximetry reading to reach normal? What other signs can you use to determine adequate oxygenation? 5 VIII.Normal Newborn Vital Signs A. Respirations: 30–60 B. Heart rate: 100–180 C. Blood pressure: 60–90 systolic D. Temperature: 36.7–37.8°C or 98–100°F E. APGAR: 1 minute and 5 minutes after birth 1. A—Appearance Discussion Topics Discuss what steps students can take in resuscitative measures for newborns, from applying O2 to using a BVM. Class Activities©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. P—Pulse Rate 3. G—Grimace 4. A—Activity 5. R—Respirations 6. Score of 0, 1, or 2 for each parameter 7. Minimum total is 0, maximum is 10 8. Score of 7–10 indicates active and vigorous newborn 9. Score of 4–6 indicates moderately distressed newborn who requires O2 and stimulation 10. Score of < 4 indicates newborn requiring immediate resuscitation Give students various scenarios of newborns with different resuscitation needs. Have them score the infants using APGAR. 15 IX. Treatment A. Starts prior to delivery by preparing the environment and gathering equipment B. Most newborns require only suctioning, mild stimulation, and maintenance of body temperature 1. Establishing the airway a. One of most critical steps b. Suctioning of airway indicated when there is obstruction to spontaneous breathing, positive pressure ventilation required, or meconium is present c. Drying and tactile stimulation usually initiates respirations in most newborns (flicking of feet or gently rubbing back) 2. Preventing Heat Loss a. Heat loss can be life-threatening in a newborn b. Cold infants become distressed infants quickly c. Most heat loss occurs through evaporation and convection for the newborn d. Dry newborn immediately, maintain ambient temperature at a minimum of 74°F, close all windows/doors, swaddle newborn in warm and dry blanket, cover head, and, if indicated due to colder environment, place well-insulated water bottles or gloves filled with warm water around infant 3. Cutting the umbilical cord a. Performed once airway is stabilized and heat loss minimized Discussion Topics Discuss with students other ways the newborn can be kept warm, and what sort of materials might be used. Class Activities Obtain a newborn /OB manikin and have students go through the steps of treatment for the newborn, including clamping and cutting the cord. Points to Emphasize Remember that routine suctioning is no longer indicated in the care of the vigorous newborn due to risks of bradycardia.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes b. Maintain infant at level of mother’s vagina to avoid over- or under-transfusion of blood c. Do not milk the cord, which will lead to polycythemia, which may in turn lead to hyperbilirubinemia d. Apply clamps 30–45 seconds after delivery e. Place first clamp 10 cm from newborn, with second clamp about 5 cm from first; cut cord between two clamps, and inspect to make sure bleeding has stopped 10 X. The Distressed Newborn A. May by full-term or preterm B. Meconium indicates fetal distress at some point in pregnancy 1. Particulate meconium may indicate that distress has occurred recently 2. Meconium aspiration can cause significant respiratory problems C. Most common problem experienced is ventilation 1. Resuscitation usually consists of ventilation, and, if needed, oxygenation 2. IV fluids, drugs, or cardiac equipment usually not indicated 3. Most important procedures include suctioning, drying, and stimulating D. Fetal heart rate most important indicator of distress 1. Newborn has relatively fixed stroke volume, so cardiac output tends to depend on heart rate 2. Bradycardia, if caused by hypoxia, decreases cardiac output, and leads to poor perfusion 3. Pulse rate less than 60 beats/minute in distressed newborn should be treated with chest compressions 4. Monitor the heart rate with an ECG monitor or pulse oximetry. Class Activities Go over the steps of newborn resuscitation, having students practice compressions and ventilations. Points to Emphasize Remember to stress to students that for a distressed newborn, cause must be found. Most babies aren’t born with something wrong. 20 XI. Resuscitation A. Majority of newborns do not require resuscitation outside of maintenance airway, stimulation, and body temperature control B. Difficult to predict which newborns may need care C. Equipment needed for newborn resuscitation includes: Teaching Tips Using the board, draw out the inverted pyramid, so that students can visualize the steps of newborn resuscitation.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Neonatal BVM, bulb syringe, laryngoscope blades 0 and 1, endotracheal (ET) tubes 2.5–4, ET stylet, tape or ET securing device, laryngeal mask airway (LMA), umbilical catheter, three-way stopcock, 20-mL syringe and 8-French, glucometer, various sizes of syringes, sterile towels, epinephrine 1:10,000 and 1:1000, Lactated Ringer’s Solution or Normal Saline D. Inverted Pyramid for Resuscitation 1. Drying, warming, positioning, suctioning, and tactile stimulation a. Minimize heat loss, place newborn in skin-to-skin contact with mother; if not possible place newborn in a warm, dry blanket away from drafts b. If further resuscitation is required, clamp and cut cord, position infant on back in “sniffing position” using blanket under shoulders to help maintain position c. Assess: respiratory effort, heart rate, color, APGAR score 2. Ventilation a. Begin positive pressure ventilation if heart rate is < 100, apnea, SPO2 less than expected post-birth, persistence of central cyanosis b. BVM is device of choice (pop-off valve may have to be disabled for prolonged ventilation), various sizes of face masks available, c. ET intubation indicated: after chest compressions, ventilations through mask not effective, if tracheal suctioning indicated, prolonged ventilation, diaphragmatic hernia suspected, ineffective respiratory effort found d. Use of capnography with ET intubation e. Gastric distention may occur with ET, use of naso- or orogastric tube may be indicated 3. Supplemental oxygen a. If central cyanosis or SPO2 levels less than expected for age, administer only enough O2 to reach normal range SPO2 b. Avoid both hypoxia and hypoxemia c. If possible, use warm and humidified O2 4. Chest compressions a. Initiate chest compressions if heart rate is less than 60 Class Activities Have students perform all of the skills (BVM, compressions, pediatric intubation, pediatric IO, umbilical cannulation). Create a scenario involving a distressed newborn with an APGAR of 3. Have students do hands-on care, including all necessary skills required. Have students practice the epinephrine dose with medmath, and drawing up the correct amount of medication to give. Have students practice assembling all of the equipment for the IO, including how the three-way stopcock works. Points to Emphasize Review the normal SPO2 levels for newborns and how important it is to maintain these levels.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 8 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes beats/minute b. Encircle newborn’s chest, placing both thumbs on lower third of sternum. If baby is small you may need to overlap fingers, and if baby is large you may need to perform two-finger compressions. c. Compress lower half of sternum at a compressions-to-ventilation ratio of 3:1 with accompanying ventilations d. Use a 3:1 ratio of compressions to ventilation at 90 compressions and 30 breaths per minute to achieve approximately 120 events per minute for maximize ventilation e. Reassess heart rate, respiration, and color every 30 seconds and coordinate with chest compressions and ventilation f. Discontinue compressions if spontaneous heart rate exceeds 80 beats/minute 5. Medications and fluids a. Administered when ventilation and oxygenation fail b. Vascular access managed most readily using the umbilical vein c. If umbilical catheter unable to be placed, some medications can go down the ET tube, or other options include peripheral vein cannulation and intraosseus (IO) d. Fluid therapy consists of 10 mL/kg of NS or LR given as slow IV push 6. Maternal narcotic use a. Illegal or prescribed abuse of narcotics can complicate field deliveries b. Shown to have low-birth-weight infants, and infants may demonstrate withdrawal symptoms such as tremors, startles, decreased alertness, and risk of respiratory depression at birth c. Use of Narcan is not indicated in neonatal resuscitation 7. Neonatal transport a. Healthy newborns should be allowed to begin bonding process with mother b. Distressed newborns must be positioned on side and rapidly transported c. Transport includes maintaining airway, body temperature, oxygen, and ventilation©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 9 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes d. Isolette often available with transport, allowing heat, light, and oxygen source 25–35 XII. Specific Neonatal Situations A. Meconium-stained Amniotic Fluid 1. Bowel movement that occurs in utero, and carries risk of aspiration or obstruction; indicates some form of fetal distress 2. Signs and symptoms may include: stained amniotic fluid (either thin or particulate), respiratory distress in newborn, airway obstruction 3. Treatment: if infant vigorous, treatment may not be indicated; if infant non-vigorous, apply suction to meconium aspirator that is attached to an ET tube and intubate/suction until meconium clears (usually not more than two times); if infant able to breathe on own, ventilate and oxygenate as needed to maintain target SPO2; if infant hypotensive, consider fluids, prevent hypothermia, transport B. Apnea 1. Common finding in preterm infants, infants < 1500 g, infants exposed to drugs, or infants born after prolonged labor and delivery (L&D) 2. Infant fails to breath spontaneously after stimulation or respiratory pauses of > 20 seconds 3. Other causes include: central nervous system (CNS) depressants or narcotics, weakness of respiratory muscles, sepsis, metabolic disorders, CNS disorders 4. Signs and symptoms include: failure to breathe spontaneously, respiratory pauses > 20 seconds, cyanosis, decreasing heart rate 5. Treatment includes: tactile stimulation, BVM, chest compression if heart rate < 60, ET, circulatory access, ECG, prevent hypothermia, transport C. Diaphragmatic Hernia 1. Failure of diaphragm to completely close, resulting in abdominal contents in chest cavity 2. Signs and symptoms include: little to severe distress at birth, dyspnea and cyanosis unresponsive to ventilations, scaphoid Teaching Tips Obtain photographs for each situation listed. With students, go over each situation, focusing on signs/symptoms and treatment. Discussion Topics Discuss with students different ways that they can assess mental status and urinary output in the newborn. Critical Thinking Questions How would you feel if a parent watches the full resuscitation of his or her child? What reasons would you have for removing the parent? Class Activities Have students perform all care on a newborn manikin, covering all of the specific situations and skills involved. Have students practice their assessment of a newborn, and any required care, by having one student portray the mother while paramedic students asks appropriate questions. This will help students remember that the mother may be asking questions, and that they actually have two patients, not one.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 10 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes abdomen, bowel sounds in chest cavity, heart sounds displaced to right 3. Treatment includes: position infant head and thorax higher than abdomen/feet, nasogastric (NG) or orogastric tube placement, low intermittent suctioning, if necessary, intubation with cautious positive pressure ventilation; DO NOT use BVM unless infant intubated D. Bradycardia 1. Most commonly caused by hypoxia 2. Other causes include: increased intracranial pressure (ICP), hypothyroidism, acidosis 3. Signs and symptoms include: decreased heart rate 4. Treatment includes: follow inverted pyramid, check airway, ventilation, oxygenation if needed, medications E. Prematurity 1. Infant born prior to 37 weeks of gestation or weighing from 1 lb 5 oz to 4 lb 13 oz 2. Risks associated with prematurity include: respiratory suppression, head or brain injury caused by hypoxemia, changes in blood pressure, intraventricular hemorrhage, fluctuations in serum osmolarity 3. Signs and symptoms include: larger head relative to body size, large trunks, short extremities, transparent skin, few wrinkles, birth occurring weeks before due date 4. Treatment includes: resuscitation with any signs of life, maintain patent airway, avoid aspiration, maintain body temperature, transport to specialty facility F. Respiratory Distress/Cyanosis 1. Prematurity single most common cause due to immature central respiratory control center and effects of environmental or metabolic changes 2. Contributing factors include: lung/heart disease, CNS disorders, meconium aspiration, metabolic problems, obstruction of nasal passages, shock and sepsis, diaphragmatic hernia 3. Signs and symptoms include: tachypnea, paradoxical breathing, intercostal retractions, nasal flaring, expiratory grunt Points to Emphasize Remind students again how important prevention of hypothermia in the newborn is, and how some of the situations presented can be caused by hypothermia. Knowledge Application Create a chart listing all of the specific situations. For homework, have students list the definition, signs and symptoms, and treatments for each specific situation.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 11 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Treatment includes: follow inverted pyramid, airway and ventilation, suction as need, O2, BVM, ET, chest compressions if necessary, D10 if hypoglycemic, maintain body temperature, transport, sodium bicarbonate if indicated by medical control G. Hypovolemia 1. Leading cause of shock in newborns that can result from dehydration, hemorrhage, or third spacing of fluids 2. Signs and symptoms include: pale color, cool skin, diminished peripheral pulses, delayed capillary refill with normal ambient temperature, change in mental status 3. Diminished urination 4. Treatment includes: fluid bolus of 10 mL/kg of isotonic fluid administered over 5–10 minutes, assess response, additional fluid may be necessary H. Seizures 1. Usually indicate a serious underlying abnormality, medical emergency abnormality, or drug withdrawal 2. Causes include: sepsis, fever, hypoglycemia, hypoxic-ischemic encephalopathy, metabolic disturbances, meningitis, developmental abnormalities, or drug withdrawal 3. Signs and symptoms include: decreased level of consciousness, seizure activity as listed below a. Subtle seizures—chewing motions, excessive salivation, blinking, sucking, swimming motions of arms, pedaling motions of legs, apnea, color changes b. Tonic seizures—rigid posturing of extremities and trunk, possible deviation of eyes; more common in premature infants c. Focal clonic seizures—rhythmic twitching of muscle groups, usually face and extremities d. Multifocal seizures—similar to focal clonic seizures, except multiple muscle groups involved; primarily seen in full-term newborns e. Myoclonic seizures—brief focal or generalized jerks of extremities or parts of body with distal muscle groups 4. Treatment includes: airway management, oxygen saturation, medical©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 12 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes order for anticonvulsant, D10 for hypoglycemia, benzodiazepine for status epilepticus, prevent hypothermia, transport I. Fever 1. Rectal temperature of 100.4°F or 38°C or higher 2. Any fever in neonate requires extensive evaluation 3. May be caused by: pneumonia, sepsis, meningitis 4. Signs and symptoms include: fever of 100.4°F or higher, mental status changes, decreased feedings, skin warm to touch, rashes or petechiae, beads of sweat only at brow of full-term infants 5. Treatment includes: patent airway, adequate ventilation, if bradycardiac provide chest compressions, transport J. Hypothermia 1. Increased surface-to-volume relationship in newborns make them extremely sensitive to environmental temperatures 2. A common and life-threatening condition for newborn 3. Signs and symptoms include: pale color, skin cool to touch, acrocyanosis, respiratory distress, possible apnea, bradycardia, central cyanosis, initial irritability, lethargy (note: newborns cannot shiver) 4. Treatment includes: warm the infant, adequate ventilations and oxygenation, chest compressions may be indicated, warm IV fluids in indicated, D10 if hypoglycemic, transport K. Hypoglycemia 1. Only age group that can develop severe hypoglycemia without having diabetes mellitus 2. Causes include: prematurity, diabetic mother, respiratory illness, hypothermia, toxemia, CNS hemorrhage, asphyxia, meningitis, sepsis 3. Signs and symptoms include: twitching/seizure, limpness, lethargy, eye rolling, high-pitched cry, apnea, irregular respirations, possible cyanosis, BGL < 45 mg/dL 4. Treatment includes: airway management, ventilation, chest compressions if indicated, D10 with medical direction, prevent hypothermia, transport L. Vomiting©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 13 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Forceful ejection of stomach contents 2. Causes include: anatomic abnormality, increased cranial pressure, infection 3. Signs and symptoms include: distended stomach, signs of infection, increased intracranial pressure, drug withdrawal 4. Treatment includes: airway management, ventilation, suction of vomitus from airway, fluid administration, placement of infant on side, prevent hypothermia, transport M. Diarrhea 1. Can cause severe dehydration and electrolyte imbalances 2. Five to six stools per day is normal 3. Causes include: bacterial/viral infection, gastroenteritis, lactose intolerance, phototherapy, neonatal abstinence syndrome, thyrotoxicosis, cystic fibrosis 4. Signs and symptoms include: loose stools, decreased urinary output, prolonged capillary refill time, cool extremities, listless, lethargy 5. Treatment includes: airway, ventilations, adequate oxygenation, chest compression if indicated, fluid therapy with medical control, prevent hypothermia, transport N. Common Birth Injuries 1. Risk factors for birth injury include: prematurity, postmaturity, cephalopelvic disproportion, prolonged labor, breech presentation, explosive delivery, shoulder dystocia, diabetic mother 2. Injuries can include: cranial injuries, erythema, ecchymosis, hemorrhage of retina or subconjunctival, fracture of skull, intracranial hemorrhage, scalp hematoma, damage to spinal cord, peripheral nerve injury, injury to liver, rupture of spleen, adrenal hemorrhage, clavicle fractures, extremity fractures, hypoxia-ischemia 3. Signs and symptoms include: swelling of soft tissue around scalp, paralysis of extremities, paralysis of upper arm with or without forearm paralysis, diaphragmatic paralysis, movement of only one side, inability to move arm freely on injured side, lack of spontaneous movement to body or extremity, hypoxia, shock 4. Treatment includes: protection of airway, adequate ventilation and oxygenation, chest compression if needed, medications per medical©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 14 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes control, treatment of particular traumatic injuries, prevent hypothermia, transport O. Cardiac Resuscitation, Post-resuscitation, and Stabilization 1. Neonatal cardiac arrest primarily related to hypoxia 2. Risk factors for cardiac arrest include: bradycardia, intrauterine asphyxia, prematurity, maternal drug use, congenital disorders and malformations, intrapartum hypoxemia, primary or secondary apnea 3. Signs and symptoms include: peripheral cyanosis, inadequate respiratory effort, ineffective or absent heart rate 4. Treatment includes: inverted pyramid, ABCs, administer drugs or fluids per medical direction, prevention of hypothermia, transport P. When Parents Request Baptism 1. The paramedic may baptism infant in an emergency setting by dipping a finger into water and saying “I baptize you in the name of the Father and of the Son and of the Holy Spirit. Amen” 2. You do not have to be same religion as parents or infant 5 XIII.Summary A. After the delivery, paramedic has two patients; mother and infant B. Newborns airway must be protected, ventilations ensured, and hypothermia prevented C. Most newborns only require some stimulation, oxygen, and possible ventilation D. If newborn distressed, he will require more aggressive resuscitation 5 XIV. Case Study Class Activities Discuss the case with students now that they are familiar with the chapter. 5 XV. You Make the Call Class Activities Read and discuss the call and questions as a group.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 15 Chapter 3 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 XVI. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Then go over the questions again after the lecture, to assess their understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 1 Detailed Lesson Plan Chapter 4 Pediatrics 260-–280 Minutes Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture. 5 II. Introduction A. Leading causes of death in pediatrics are age specific. B. Many of these injuries and deaths could have been prevented by early intervention. C. Pediatric tragedies can account for some of the most stressful incidents in the prehospital setting D. Special concerns in dealing with pediatric patients are including parents, patient inability to communicate, size, and others. 15 III. Role of Paramedics in Pediatric Care A. Two key concepts for paramedic role: Pediatric injuries have become major health concerns, and children are at higher risk of injuries and more likely to be adversely affected by injuries. B. Some factors and dangers can be eliminated by getting all involved in methods that prevent injuries. C. Some medical illnesses are unique to children. D. Continuing Education and Training 1. PALS, PEPP, APLS, PPC 2. Improving pediatric knowledge will allow improved patient care. E. Improved Health Care and Injury Prevention 1. Emergency Medical Services of Children federally funds programs that improve the health of pediatric patients by identifying numerous pediatric concerns, including community education, prehospital care, Discussion Topics Discuss with students the different skills they will obtain when taking specialized pediatric courses. Critical Thinking Questions What role do you believe the parent has in preventable injuries/illnesses? Do you think that when a child is injured in a preventable injury, the parent/caregiver should be held accountable? MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes injury prevention, and so forth. 2. Injury prevention or community programs 3. Teachable moments 4. Research studies or registries F. Advanced Life Support Skills in Pediatrics 1. 85% of prehospital pediatric calls require only basic life support (BLS). 2. Pediatric ALS skills should be practiced frequently, because when they are needed, the skills must be done competently. Class Activities Have students list the various prevention programs available for pediatric injuries/illnesses, along with the engineering concepts that have created different safety equipment. Knowledge Application For homework, have students create scenarios in which teachable moments would be applicable 25 IV. General Approach to Pediatric Emergencies A. Approach varies with age of patient and problem B. Consideration of patient’s emotional and physiologic development, along with family members and/or caregivers C. Communication and Psychological Support 1. Includes communication and interaction throughout assessment and management 2. Obtain information as accurately and quickly as possible, usually through parents/caregivers, although older children can be a good source of information. 3. Treat pediatric patients with respect, allowing them to express opinions and ask questions. D. Responding to Patient Needs 1. Common fear responses of children includes: a. Separation from parents/caregivers b. Removal from family place, with fear of never returning c. Being hurt, or being mutilated or disfigured d. Fear of unknown 2. Fears can intensify if child detects fear/anxiety from parents/caregivers. 3. Using honesty and age-appropriate language will help reduce feelings of helplessness. B. Responding to Parents or Caregivers 1. Reactions may vary from shock, grief, denial, anger, guilt, fear, to complete loss of control. Discussion Topics Discuss with students the different fears a pediatric patient may present with. Class Activities With students, practice responding to pediatric scenarios with different parental responses. Have students practice how they would calm the scene. Points to Emphasize Remember that you do not have just one patient; with a pediatric patient, you must include family/caregivers.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. Paramedic communication is key to a calm scene. 3. Allow one of the parents/caregivers to remain with the child, as long as the parent does not interfere with care. 4. Be suspicious of abuse/neglect if patient shows patterned injury. 25 V. Growth and Development A. Newborns (First Hours after Birth) 1. Most frequently used assessment tool is the APGAR scoring system B. Neonates ( Birth to 1 month) 1. Major state of development that centers on reflexes 2. Common signs and symptoms: jaundice, vomiting, respiratory distress (note: fever may be only sign) 3. Age-group approaches: keep warm, observe skin, respiratory activity. C. Infants (1–5 months) 1. Doubled birth weight by 6 months; muscle control begins at head and moves toward tail 2. Common illnesses and accidents: sudden infant death syndrome (SIDS), vomiting, dehydration, meningitis, child abuse, household accidents 3. Age-group approaches: keep warm and comfortable, allow infant to stay with caregiver, if possible. D. Infants (6–12 months) 1. May stand or walk with assistance; active and explore the environment 2. Foreign body obstruction is major risk factor in this age group. 3. Common illness/injuries: febrile seizures, vomiting, diarrhea, dehydration, bronchiolitis, car crashes, croup, child abuse, poisoning, falls, and airway obstruction 4. Age-group approaches: examine while sitting in lap of parents/caregivers, use toes-to-head assessment, to allow for child to get comfortable with you (as long as ABCs are intact). E. Toddlers (1–3 years) 1. Gross motor skill development, can run, more curious 2. Beginning of language development, understanding of verbal language better than spoken language Teaching Tips Use pictures, slides, or other visuals to show students the difference in sizes between each age group. Discussion Topics Discuss with students the various injuries associated with each age group. Have students discuss ways to prevent each injury. Critical Thinking Questions How will knowing the developmental stages allow you to determine correct mental responses in each age group? Class Activities Show slides of each age group. After students have determined the age group, have them list the developmental factors, common illnesses/injuries, and approaches for each group. Points to Emphasize Stress to students that the determination of mental status of particular age groups may solely focus on their response to parents. Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 3. Common illness/injuries: accidents of all types are leading cause of death, motor vehicle collisions, homicides, burns, drowning, pediatric collisions, vomiting, diarrhea, febrile fevers, poisoning, falls, child abuse, croup, foreign body airway obstruction (FBAO) 4. Age-group approaches: approach slowly to gain confidence (as long as ABCs intact), toe-to-head assessment, use simple words, speak quietly and in very basic terms; if possible, avoid dominant hand procedures. F. Preschoolers (3–5 years) 1. Tremendous increase of fine and gross motor development, greatly increased language skills 2. Vivid imagination, fear of mutilation; avoid frightening comments 3. Common illness/injuries: croup, asthma, poisoning, auto collisions, burns, child abuse, ingestion of foreign bodies, drowning, and febrile seizures 4. Age-group approaches: avoid baby talk, use doll to assist in examination, let child sit on lap, start examination with chest and evaluate head last, explain what you are doing (all of this can be done as long as ABCs intact), keep parents/caregivers with you. G. School-age Children (6–12 years) 1. Active and carefree, growth spurts that can result in clumsiness 2. Value peers but are proud of family and need their support 3. Common illness/injuries: asthma, drowning, auto collisions, bicycle accidents, falls, fractures, sports injuries, child abuse, burns 4. Age-group approaches: give the patient responsibility of providing history, with parents to fill in pertinent information; respect modesty; use honesty. H. Adolescence (13–18 years) 1. Covers end of childhood to start of adulthood 2. Puberty is child specific and can begin at various ages. 3. Teenagers are body conscious, worry about physical image, have strong desire to be liked by peers. 4. Common illness/injuries: mononucleosis, asthma, auto collisions, sports injuries, drug and alcohol problems, suicide gestures, sexual abuse, pregnancy 5. Age-group approaches: vital signs close to an adult’s, interview patient For homework, have students list each age group and the common illnesses/injuries associated with that group, along with ageappropriate approaches.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes away from parents/caregivers, use tact and compassion when interviewing adolescent, have same-sex paramedic interview/exam if patient shows modesty or body shame. 25 VI. Anatomy and Physiology A. Differences in pediatric versus adult anatomy and physiology are the basis for the differences in emergency medical care. B. Pediatric patients tend to have healthier bodies, ability to compensate for most illnesses, and softer, more flexible tissues. C. Head 1. Proportionally larger, with occipital region significantly larger, smaller faces and flatter noses 2. Infants have soft fontanelles, which allow for compression of head during childbirth and rapid growth of brain during early life. 3. Heavy head relative to body size places infant/child at risk of blunt head trauma. 4. Anatomic consideration for head: tight, bulging fontanelle may indicate increased intracranial pressure; sunken fontanelle may indicate dehydration; head size may affect airway positioning; head size may propel more forcefully than body, causing higher incidence of brain injury; thin layer of padding under back for children < 3 years old will obtain neutral position; medically ill children > 3 years old, folded sheet or towel under occipital will obtain sniffing position. D. Airway 1. Narrower airway, which is easily blocked; infants obligate nose breathers 2. Tongue takes up more space in child’s mouth, can easily obstruct breathing; trachea softer and more flexible, can collapse in neck/head hyperextended 3. Larynx higher and extends into pharynx, cricoid ring narrowest part of airway(below the cords), epiglottis is omega-shaped and more floppy 4. Anatomic considerations for airway: keep nares of infants < 6 months clear; do not overextend neck; airway swelling can occur from airway Teaching Tips Using slides and pictures, compare adult and pediatric anatomy and physiology, which allows students to view the differences. Discussion Topics Discuss with students the anatomy and physiology of pediatric patients; stress to students that having an understanding of pediatric anatomy and physiology will allow for high-quality patient care. Critical Thinking Questions How can anatomic consideration improve your pediatric patient care? Class Activities Using mannequins, have students perform various pediatric skills as they note the differences in the anatomy and physiology of the pediatric patient. Make sure that students use padding, appropriate sized equipment, and so forth. Points to Emphasize As a group, show students, by using infant and child mannequins, how inappropriately sized equipment can further harm your©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes device placement. E. Chest and Lungs 1. Tissues and muscles more immature, chest muscles tire easily; lung tissue more fragile; soft, pliable ribs offer less protection to organs 2. Anatomic considerations for chest: diaphragmatic breathers; prone to gastric distention; rib fractures infrequent, but not uncommon in abuse; internal injury present without external signs; pulmonary contusions more common; lungs more prone to tension pneumothorax; trachea will shift more with tension pneumothorax; easily transmitted breath sounds F. Abdomen 1. Liver and spleen larger, abdominal organs closer together, immature abdominal muscles 2. Anatomic considerations for abdomen: more frequent damage to liver and spleen, more multiple-organ injuries G. Extremities 1. Softer, more porous bones 2. Anatomic considerations for extremities: injuries to growth plate may disrupt bone growth; use caution when inserting IO H. Skin and Body Surface Area (BSA) 1. Skin is thinner, less subcutaneous fat, larger BSA-to-weight ratio 2. Anatomic considerations for skin and body surface: greater risk of injury from extremes in temperature of thermal exposure; lose fluid and heat more quickly; greater risk of dehydration and hypothermia; burn more easily and deeply (note: accounts for why burns are one of the leading causes of death in pediatric patients) I. Respiratory System 1. Require double the metabolic oxygen; smaller oxygen reserves 2. Anatomic considerations for respiratory system: infants and children susceptible to hypoxia J. Cardiovascular System 1. Rate-dependent in infants and small children; limited cardiac reserves; absolute blood volume smaller 2. Maintains blood pressure longer but may still be at risk for shock 3. Anatomic considerations for cardiovascular system: smaller absolute volume fluid/blood loss needed to cause shock; hypotension is late sign pediatric patient. This is a great visual that students remember. Knowledge Application For homework, have students list the anatomic considerations for each system/organ listed.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes of shock and is an ominous sign of imminent cardiopulmonary arrest; may be in shock despite normal blood pressure; shock assessment based on clinical signs of tissue perfusion; suspect shock if tachycardia present; bleeding that would not be dangerous in an adult may be serious and life threatening in pediatrics. K. Nervous System 1. Develops continually throughout childhood; neural tissue more fragile; skull and spinal cord offer less protection to brain and spinal cord. 2. Anatomic considerations for nervous system: greater force can be transmitted to neural tissue; injuries can occur without injury to skull or spinal column. L. Metabolic Differences 1. Limited stores of glycogen and glucose; prone to hypothermia due to greater BSA-to-weight ratio; significant volume loss can result from vomiting and diarrhea; newborns/neonates lack ability to shiver. 2. Anatomic considerations for metabolic differences: prevent heat loss by covering pediatric head and maintaining ambulance temperatures. 25 VII. General Approach to Pediatric Assessment A. Basic Considerations 1. Many components can be visually examined upon arrival 2. Involve parent/caregiver if possible and warranted; pay attention to interactions of all on scene. 3. Scene safety is always first. B. Scene Size-Up 1. Use dispatch information and your own observations to determine scene safety. 2. Look for mechanism of injury (MOI) or nature of illness (NOI) to help guide assessment and interventions. 3. Note any dangerous substances, environmental hazards. 4. Be alert to possible abuse. 5. Keep the child’s comfort in mind when beginning assessment. C. Primary Assessment 1. Patient condition guides primary assessment. 2. General impression Teaching Tips Draw out the Pediatric Assessment Triangle (PAT) and Glasgow Coma Scale (GCS) on the board. Reinforce to students how these two tools enhance the assessment and allow guidance of care. As a group, create problems within the PAT and GCS, and have students decide what type of assessment would be warranted. Discussion Topics Discuss with students what type of dangers they may face on a pediatric call. Discuss with students ways the paramedic can determine urine output for an infant or©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 8 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. Pediatric Assessment Triangle (PAT) is a quick tool to evaluate level of severity and need for intervention. b. Components include appearance (mental status and muscle tone); breathing (respiratory rate and effort); circulation (skin signs and color, capillary refill). 3. Vital function a. Level of consciousness: AVPU (alert, verbal response, painful response, unresponsive) to evaluate level of consciousness (LOC); techniques to determine LOC may have to be adjusted for age. b. Airway: Airway and respiratory problems are most common cause of cardiac arrest in infants and children. Look for patent airway—is airway maintainable by child? c. Breathing: Look at chest rise and fall, listen for breath sounds (normal and abnormal), feel for air movement; look for lifethreatening chest injuries; assess respiratory rate, effort, and child’s color. d. Circulation: Check color, capillary refill; evaluate heart rate, peripheral circulation, end-organ perfusion (skin, kidneys, and brain) 4. Anticipating cardiopulmonary arrest a. Primary assessment and repeated assessments allow you to recognize and prevent cardiopulmonary arrest. b. Early recognition is one of the main goals of PALS. c. Conditions that place patient at risk include respiratory rate > 60 breaths/minute, heart rate > 180 or < 80 (under age 5 years), heart rate > 180 or < 60 (over age 5 years), respiratory distress, trauma, burns, cyanosis, altered LOC, seizures, fever with petechiae. d. Cardiopulmonary arrest usually not a sudden event, more of a progressive deterioration. 5. Transport priority a. Urgent: rapid trauma assessment, immediate transport, further assessment and treatment en route b. Nonurgent: Complete secondary assessment at scene, then transport. 6. Transitional phase a. Intended for conscious, nonacutely ill child toddler. Discuss with students different ways in which you can assess level of consciousness in the various pediatric age groups. Critical Thinking Questions Why would your assessment be more difficult if you did not keep the child’s comfort in mind? If the child is not comfortable during the exam, could patient care be compromised? Why or why not? Class Activities Create pediatric scenarios and have students perform assessments, along with any skills necessary. During pediatric assessments, have students practice using parents (other students) to assist with exam. Points to Emphasize Remember that early recognition is key to preventing cardiopulmonary arrest in pediatric patients. Knowledge Application For homework, have students list ways that they can make pediatric patients comfortable. There are no correct answers, just different comfort ideas.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 9 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes b. Allows infant or child to become familiar with you and equipment c. This step is skipped in dealing with an unconscious or acutely ill patient. D. Secondary Assessment 1. Completed once patient care is prioritized at end of primary assessment 2. If medical illness, history usually precedes physical exam. 3. If trauma, physical exam usually takes precedence. 4. History a. Family or caregiver usually involved b. SAMPLE, presence of fever, behavior changes, bowel/urine changes, vomiting/diarrhea 1. Physical exam a. Focused exam: carried out after all life-threatening conditions identified; toe-to-head approach in younger children; include pupils, capillary refill, hydration, pulse oximetry b. Glasgow Coma Scale (GCS): Use in cases of trauma; allows a scoring system for neurological status in patients with possible head injuries; modifications will have to be made in younger pediatric patients; (mild = GCS 13–15, moderate = GCS 9–12, severe = GCS 8 or <); elements of GCS are verbal response, motor functions, eye movements. c. Vital signs: Take with patient in resting state if possible; include pulse, respirations, blood pressure, temperature; use appropriately sized blood pressure (BP) cuff; pay attention to pulse pressure; feel pulse for 30 seconds to 1 minute; use family to give weight of child, or use a good estimate; observe respiratory rate before exam starts and note any retractions, patterns, and so forth; take temperature early in exam and repeat at end; continue observation of child’s LOC. d. Noninvasive monitoring: pulse oximeter, capnography, automated BP device, self-registering thermometers, electrocardiograms (ECGs) e. Reassessment: Continuous reassessment is crucial due to rapid condition changes in pediatric patients.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 10 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 25 VIII.General Management of Pediatric Patients A. Top priorities are airway, breathing, circulation. B. Basic Airway Management 1. Manual positioning a. Position of comfort; avoid hyperextension of neck. 2. Foreign body airway obstruction a. Determine if FBAO is mild versus severe b. Children with severe FBAO require abdominal thrusts; infants with severe FBAO require five back blows and five chest thrusts; no blind finger sweeps. 3. Suctioning a. Use bulb-syringe, flexible catheter, rigid-tip catheter. b. Suction < 100 mmHg, suction time < 10 seconds, suction no deeper than you can see, check patient pulse for bradycardia frequently. 4. Oxygenation a. Use pulse oximetry to guide supplemental administration. b. Provide enough oxygen to maintain SpO2 of 94% or higher. c. Use 100% O2 for resuscitation when possible, with the exception of newborns. 5. Airway adjuncts a. Use adjuncts only if prolonged artificial ventilations required. 6. Oropharyngeal airways a. Only used in patients who lack a gag reflex. b. Size accurately; too small will obstruct airway, and too big will block airway and cause trauma. c. Use a tongue blade to depress tongue and jaw. 7. Nasopharyngeal airways a. Use in patients with intact gag who require prolonged ventilation. b. Do not use on patients with midface or head trauma. 8. Ventilation a. Avoid hyperventilation, and use capnography to monitor and guide. b. Use properly sized mask and look at chest rise with each breath. c. Allow full chest recoil and exhalation. d. Do not use bag-valve masks (BVMs) with pop-off valves unless they can readily be occluded; ensure correct positioning of airway. Teaching Tips All equipment presented must be covered with students, especially when to use each. Discussion Topics Discuss with students how they can adapt particular pieces of equipment to fit their pediatric patients. Critical Thinking Questions Why is oxygen therapy based on pulse oximetry and patient presentation? What could happen to pediatric patient if oxygen is provided when none is needed? Class Activities With the class, bring out all of the pediatric equipment, and go over each piece, listing indications and contraindications. Using infant and child mannequins, have students practice all BLS, ALS airway, IV and IO therapy, immobilization, and electrical therapy skills presented. Have students practice Med Math and drawing up accurate medications. Points to Emphasize Equipment must fit the patient. Ill-fitting equipment can further hinder patient care. Knowing when to use equipment is just as important as knowing how to use it.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 11 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes C. Advanced Airway and Ventilatory Management 1. Foreign body airway obstruction a. Visualization of airway with laryngoscope and Magill forceps to remove obstruction if BLS procedures are ineffective. b. Intubation around object may be attempted if object cannot be removed. 2. Needle cricothyrotomy a. Anatomical landmarks may be more difficult to identify. b. Only indication is failure to obtain airway by any other method. 3. Endotracheal intubation a. Allows direct visualization of lower airway b. Most effective method to control the airway c. Anatomic and physiologic concerns: straight blade; resuscitation tapes for estimate of correct ET sizes d. Indications: need for prolonged ventilation; inadequate ventilations with BVM; cardiac/respiratory arrest; medication route; gain access to suction e. Techniques for pediatric intubation: Steps mimic those for adults, allowing no more than 30 seconds without ventilating patient. f. Tube placement verification in the pediatric patient: Always verify placement and ensure tube stays in place throughout care; remember to go through all steps of tube verification; remember the DOPE mnemonic to remember possible causes of tube displacement. 4. Rapid-sequence intubation a. May be indicated with significant LOC and presence of gag reflex; use of paralytics and sedatives may be authorized to allow for intubation. 5. Extraglottic airways a. Laryngeal mask airway (LMA) may be used as alternative airway 6. Nasogastric intubation a. Consider placement if gastric distention is present. b. Not to be used in patients with sustained head or facial trauma D. Circulation 1. Look for end-organ changes that may indicate respiratory and Knowledge Application For homework, have students list the various equipment and techniques available for pediatric care.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 12 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes cardiovascular function. 2. Vascular access a. Veins of neck, scalp, arms, hands, feet may be accessed in infant. b. External jugular should only be used in life-threatening situations. 3. Intraosseous (IO) infusion a. Insertion occurs at medial aspect of tibia, 1–3 cm below tibial tuberosity. b. PALS medications can be placed IO. 4. Fluid therapy a. In hypovolemic patient, 20 cc/kg of LR or NS b. Monitor closely for fluid overload. 5. Medications a. Certain medications may be indicated due to patient need. b. Pediatric medications are based on weight. E. Electrical Therapy 1. Ventricular fibrillation = 2–4 j/kg 2. Make sure that hypoxia and acidosis are being corrected. F. C-Spine Stabilization 1. Cervical spine is vulnerable to injury due to heavier and larger head. 2. A spinal cord injury could be present without noticeable damage to vertebral column. 3. Use appropriately sized stabilization devices. 4. Padding is necessary to ensure a supine, neutral position. 5. Stabilization may cause emotional stress; keep parents close by if possible. G. Transport Guidelines 1. Do not delay transport for a procedure that can be done en route 2. Consider time of transport, specialized facilities, and specialized personnel when determining transport decision. 40 IX. Specific Medical Emergencies A. Infections 1. Frequent infections due to relative immaturity of immune system 2. May be virus, bacteria, fungus, or parasite 3. Life-threatening infections include meningitis, pneumonia, septicemia. These Teaching Notes will cover pages 116–136, due to the length of the medical and traumatic emergencies section. Most of the teaching notes can be applied to all emergencies.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 13 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Signs and symptoms may include fever, chills, tachycardia, cough, sore throat, nasal congestion, malaise, tachypnea, cool or clammy skin, petechiae, respiratory distress, poor appetite, vomiting, diarrhea, dehydration, hypoperfusion, purpura, seizures, severe headaches, irritability, stiff neck, bulging fontanelle. 5. Management includes body substance isolation (BSI), ABCs, fluid if needed, comfort, transport. B. Respiratory/Upper Airway 1. Respiratory emergencies are the most common reason for EMS care. 2. Stages of respiratory compromise include respiratory distress, respiratory failure, respiratory arrest. 3. Respiratory distress a. Mildest form of respiratory impairment b. One of the earliest indications is an increase in respiratory rate. c. Signs and symptoms include normal LOC that deteriorates into irritability, anxiety, tachypnea, retractions, nasal flaring, poor muscle tone, tachycardia, head bobbing, grunting, cyanosis or hypoxia that improves with oxygen. d. Management includes increasing ventilation and oxygenation, airway positioning, patency of airway, high-concentration oxygen, more aggressive airway and ventilation if child does not improve. 4. Respiratory failure a. Respiratory system unable to meet the demands of the body for oxygen intake and CO2 removal b. Characterized by inadequate ventilation and oxygenation c. Signs and symptoms include irritability or anxiety deteriorating into lethargy, tachypnea deteriorating into bradypnea, retractions deteriorating into agonal respirations, poor muscle tone, tachycardia deteriorating into bradycardia, central cyanosis, hypoxia. d. Management includes establishment of airway, high-flow O, BVM, ET if BVM does not improve condition, gastric decompression if abdominal distention impeding BVM, needle decompression if tension pneumothorax present, cricothyrotomy if complete airway obstruction present and airway cannot be obtained, IV access, transport, reassessment en route. Teaching Tips Go over all of the specific medical/trauma emergencies, using slides, pictures, and other visuals to describe signs and symptoms. Explain the phases of the pedestrian–car collision to students, focusing on injuries sustained. Go over the pediatric rule of nines with students; have students practice computing BSA burned. Discussion Topics Have students explain why they think respiratory emergencies are common reasons for EMS response. Discuss with students the various safety equipment that provides injury prevention for pediatrics. Discuss with students different traumas sustained by pediatric patients, along with scenarios of occurrence and prevention strategies. Use current news that reflects pediatric trauma. Critical Thinking Questions Why would day care centers and preschools have influence in the spreading of infection among children? In what ways can the spread of infection in these areas©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 14 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5. Respiratory arrest a. End result of respiratory impairment; cessation of breathing b. Signs and symptoms include unresponsiveness deteriorating to coma, bradypnea deteriorating to coma, absent chest wall movement, bradycardia deteriorating to asystole, profound cyanosis. c. Management includes establishment of airway, high-flow O2, BVM, ET if BVM does not improve condition, gastric decompression if abdominal distention impeding BVM, needle decompression if tension pneumothorax present, cricothyrotomy if complete airway obstruction present and airway cannot be obtained, IV access, transport, reassessment en route. 6. Upper airway obstruction a. May be partial or complete b. May be caused by infection (swelling of tissues), aspirated foreign body c. Signs and symptoms include stridor, drooling, ineffective cough, inability to move air. d. Management includes FBAO removal techniques. 7. Croup a. Medically termed laryngotracheobronchitis b. Viral infection of upper airway that commonly occurs in children 6 months to 4 years of age and prevalent in the fall and winter months c. Causes inflammation of upper respiratory tract that leads to edema beneath glottis and larynx d. Signs and symptoms include history of mild cold or infection, harsh and barking cough, inspiratory stridor, low-grade fever. e. Steroids are recommended for moderate to severe croup. f. Management includes airway maintenance; position of comfort; cool mist air or blow-by O2; if severe, racemic epinephrine or albuterol may be ordered; do not agitate child, to prevent airway from swelling further. 8. Epiglottitis a. Acute infection of epiglottis, potentially life threatening b. Caused by bacterial infection (Hib), tends to occur in children 3–7 be stopped or limited? What vaccination is responsible for preventing epiglottitis? Class Activities Create medical emergency scenarios, allowing students to recognize signs and symptoms, identify the emergency, and begin treatment. This will take several labs, as there will be numerous scenarios to cover. Using PowerPoint, create a signs/symptoms slide show that lists signs and symptoms, and have students figure out the emergency based on the clues. Invite a pediatric ICU nurse to come in and go over various emergencies common to the pediatric patient. Obtain a CD of lung sounds to play for students. Have students identify each sound that corresponds with each respiratory emergency. Using PALS algorithms, have students go through each cardiac scenario, performing all skills pertinent to call, along with drawing up medication using Med Math. Have students practice immobilizing child/infant on backboard and in car seat. Make sure that padding is used correctly.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 15 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes years old c. Signs and symptoms include brassy cough, pain on swallowing, sore throat, high fever, shallow breathing, dyspnea, inspiratory stridor, drooling, tripod position, signs of respiratory distress. d. Management includes: DO NOT attempt to visualize the airway, as this will cause more swelling of airway and could cause complete obstruction; airway maintenance; humidified O2 by facemask or blow-by; keep child comfortable; two-rescuer BVM if airway obstructed; ET only if complete obstruction present; gentle handling; transport. 9. Bacterial tracheitis a. Bacterial infection of airway in subglottic region, most likely to occur following episodes of viral croup, afflicting mainly ages 1–5 years b. Signs and symptoms include possible history of recent croup, high fever, coughing up of pus and mucus, hoarse voice, sore throat, stridor (inspiratory or expiratory). c. Management includes: manage airway and breathing, provide oxygenation, high-pressure ventilation may be necessary to adequately ventilate patient, ET considered only if complete airway obstruction presents, transport. 10. Foreign body aspiration a. Young children tend to put objects in mouth, increasing their risk for aspirating foreign bodies b. FBAO is the leading cause of in-home accidental deaths in children under 6 years of age c. Common foods and objects associated with FBAO include hard candy, nuts, seeds, hot dogs, sausages, grapes, coins, balloons, small objects. d. Signs and symptoms include minimal to no air movement (complete) or stridor, muffled voice, drooling, pain in throat, retractions, cyanosis (partial). e. Management includes: assess respiratory efforts—if partial, make child comfortable, administer O2, transport; if complete, use BLS techniques to attempt to clear airway, visualize airway with laryngoscope, Magills forceps for removal of object, ET if necessary, Have students do a rotation at a pediatric emergency room. Points to Emphasize Stress to students that each medical/trauma emergency has a specific sign or symptom that leads to recognition and treatment. Focus on respiratory distress, failure, and arrest in the pediatric patient; stress to students the signs and symptoms of each respiratory impairment and treatment to be provided. Knowledge Application For homework, create a chart that lists each medical emergency. Have students list the definition, signs and symptoms, and treatment of each. Create a matching homework with one column listing emergencies and the other column listing signs and symptoms. Create a matching homework with one column listing pediatric medications and the other column listing dosages.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 16 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes needle cricothyrotomy as last resort and per medical direction. C. Respiratory/Lower Airway 1. Asthma a. Chronic inflammatory disorder of lower respiratory tract b. Characterized by bronchospasm and excessive mucus production, can be triggered by environmental allergens, cold air, exercise, food, irritants, emotional stress, medications c. Within minutes after exposure, bronchoconstriction and bronchial edema occur; if attack is not treated immediately, inflammation of bronchioles causes more edema and further decreases expiratory airflow. d. Signs and symptoms include: history, asthma medication, tripod position, tachypneic, unproductive cough, accessory muscle usage, wheezing (no wheezing heard is an ominous sign), tachycardia e. Management includes: establish airway, administer O2, nebulized bronchodilators, ECG, pulse oximetry, steroid administration per medical direction 2. Status Asthmaticus a. Severe, prolonged attack that cannot be broken with aggressive pharmacologic agents b. Serious medical emergency c. Signs and symptoms include greatly distended chest, breath sounds and wheezing may be absent, exhaustion, acidotic, dehydrated d. Management includes: establish airway, administer O2, nebulized bronchodilators, steroid administration per medical direction, prepare for ET, ECG, pulse oximetry, immediate transport. 3. Bronchiolitis a. Infection of bronchioles that occurs early in childhood b. Caused by viral infection, commonly respiratory syncytial virus (RSV), and spreads quickly through day cares and preschools c. Characterized by expiratory wheezing and clinically resembles asthma; most commonly affects children < 2 years old d. Signs and symptoms include history to distinguish from asthma, low-grade fever, age (asthma rarely occurs in children < 1 year old), wheezes or crackles.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 17 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes e. Management include: humidified O2, position of comfort, ventilate as necessary, administration of bronchodilator, pulse oximetry, ECG, transport. f. Nasal suctioning in an infant can improve respiratory distress. 4. Pneumonia a. Infection of lower airway and lungs; can be caused by bacterium or virus, most commonly appears in infants, toddlers, and preschoolers b. Most cases viral and self-limiting, but older children can contract bacterial pneumonia c. Pneumonia vaccine is available and highly effective for children under 5 and those of increased risk. d. Signs and symptoms include history of respiratory infection, lowgrade fever, decreased breath sounds, crackles, rhonchi, pain in chest area, increased respiratory rates or tachycardia. e. Management includes supportive care, position of comfort, patent airway and O2, ET and BVM if indicated. 5. Foreign Body Lower Airway Obstruction a. Same patients at risk for upper airway obstruction at risk for lower airway obstruction due to foreign body too small to lodge in upper airway b. Signs and symptoms include history of possible foreign body in mouth that disappears, respiratory distress, considerable coughing, anxiousness, diminished breath sounds in area of foreign body, unilateral crackles or rhonchi, unilateral wheezing. c. Management includes supportive care, position of comfort, avoid agitation, provide O2, transport to facility that can perform pediatric fiber-optic bronchoscopy. D. Shock 1. Shock is the second major cause of cardiopulmonary arrest in pediatrics, after respiratory impairment. 2. Shock is an inadequate perfusion of the tissues with oxygen, which ultimately results in tissue hypoxia and metabolic acidosis 3. Causes of shock in pediatrics include loss of body heat (newborns/neonates), dehydration, infection, trauma, blood loss, allergic reactions, poisoning, cardiac events (rare).©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 18 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Shock is classified by severity as compensated, decompensated, and irreversible. 5. Compensated shock a. Early shock that the body is able to compensate for through various physiologic measures b. Blood pressure will be normal at this stage; compensated shock is generally reversible if appropriate treatment is rendered. c. Signs and symptoms include irritability, anxiety, tachycardia, tachypnea, weak peripheral pulse, full central pulses, delayed capillary refill, cool and pale extremities, systolic blood pressure within normal limits, decreased urinary output. d. Management includes ABCs, O2, IV access, fluid replacement; definitive care takes place at hospital. 6. Decompensated Shock a. Develops when body can no longer compensate for decreased tissue perfusion b. Hallmark of decompensated shock is a fall in blood pressure. c. Pediatric patient’s compensatory mechanisms function very efficiently, so when decreased blood pressure occurs, a significant loss of fluid or impairment of cardiac output has occurred. d. Signs and symptoms include lethargy or coma; marked tachycardia or bradycardia; absent peripheral pulses and weak central pulses; markedly delayed capillary refill; cool, pale, dusky, and mottled extremities; hypotension; markedly decreased urinary output; absence of tears. e. Management includes treatment of underlying cause, ABCs, O2, IV access, fluid replacement, BVM and ET if indicated; definitive care takes place at hospital. 7. Irreversible Shock a. Occurs when treatment measures are inadequate or too late to prevent significant tissue damage and death b. Best treatment for irreversible shock is prevention. 8. Hypovolemic Shock (caused by decreased blood or fluid volume) a. Loss of intravascular fluids b. Most common cause is severe dehydration from vomiting and©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 19 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes diarrhea and blood loss as result of trauma or burns. c. Signs and symptoms include irritability, anxiety, tachycardia, tachypnea, weak peripheral pulse, full central pulses, delayed capillary refill, cool and pale extremities, systolic blood pressure within normal limits, decreased urinary output. d. Management includes ABCs, O2, IV, 20-cc/kg bolus of NS or LR, reassess, second bolus if necessary, transport. 9. Distributive shock (caused by abnormal distribution and return of blood resulting from vasodilation, vasopermeability, or both); includes septic, anaphylactic, and neurogenic shock 10. Septic shock (caused by infection of bloodstream by pathogen) a. Toxins from infection cause peripheral vasodilation. b. Signs and symptoms include ill appearance, irritability or altered mental status, fever, vomiting, diarrhea, cyanosis, pallor, mottled skin, nonspecific respiratory distress, poor feeding, tachycardia, delayed capillary refill, inability to recognize parents, acidosis. c. Management includes prevention of septic shock, ABCs, O2, IV, 20 cc/kg of NS/LR, consider pressor therapy; definitive treatment includes antibiotics. 11. Anaphylactic shock (caused by exposure to antigen that impairs tissue perfusion) a. Primarily occurs as result of histamine and other chemicals that cause vasodilation and capillary permeability b. Signs and symptoms include tachycardia, tachypnea, wheezing, urticaria, anxiousness, edema, hypotension, exposure. c. Management includes ABCs, administration of Epi 1:1000 SQ, antihistamine, O2, IV; if patient in decompensated shock, Epi 1:10,000 IV administered. 12. Neurogenic shock (caused by sudden peripheral vasodilation from interruption of nervous control of peripheral vascular system) a. Most common cause is injury to spinal cord. b. Signs and symptom includes history of injury, paralysis, warm, dry skin below injury site, low blood pressure, normal to below normal heart rate. c. Management includes ABCs, stabilization of injury, O2, IV, pressor©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 20 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes agents to stabilize blood pressure. 13. Cardiogenic shock (caused by impaired pumping power of heart) a. Inadequate cardiac output; usually resulting from secondary cause such as near-drowning or toxic ingestion b. Primary causes include congenital heart disease and cardiomyopathy. 14. Congenital heart disease a. Primary cause of heart disease in children b. Most heart problems are detected at birth, although some may not be discovered until later in childhood. c. Signs and symptoms include cyanosis, respiratory distress, congestive heart failure (CHF), “cyanotic spell,” which includes irritability, inconsolable crying, altered mental status, progressive cyanosis with severe dyspnea, seizures, coma, cardiac arrest, tachycardia, drowsiness, fatigue, pallor, and decreased end-organ perfusion. d. Management includes ABCs, O2, ventilator support if indicated, ECG, IV, position for increased cardiac return (knee-chest downward facing or squatting), transport. 15. Cardiomyopathy a. Disease or dysfunction of cardiac muscle b. Can result from congenital heart disease or infection, and causes mechanical pump failure c. Signs and symptoms include early fatigue, crackles, jugular venous distention (JVD), engorgement of liver, peripheral edema, signs and symptoms of shock. d. Management includes ABCs, O2, fluid restriction, IV, furosemide, pressor agents, transport. E. Arrhythmias 1. Uncommon in children, but when they occur, bradyarrhythmias are most common 2. Can cause pump failure, leading to cardiogenic shock due to children having very limited capacity to increase stroke volume 3. Tachyarrhythmias a. Rate is greater than estimated normal heart rate for child.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 21 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes b. Result from primary cardiac disease or secondary causes c. Supraventricular tachycardia (SVT) is narrow complex with rate typically 220 or greater d. Usually result of problem in conductive system, but can be result of drug ingestion or other conditions e. Rapid rates do not allow for adequate cardiac filling, causing CHF and cardiogenic shock. f. Signs and symptoms include irritability, poor feeding, JVD, hepatomegaly, hypotension, ECG with narrow-complex SVT g. Management includes: depends on clinical findings; stable patients. require O2 if hypoxic, vagal maneuvers, adenosine; unstable patients require O2 if hypoxic, cardioversion at 0.5–1 j/kg, increased to 2 j/kg if initial shock unsuccessful; amiodarone or procainamide may be indicated if vagal, adenosine, or cardioversion unsuccessful. h. Ventricular tachycardia with a pulse is almost always due to a secondary cause. i. Signs and symptoms include poor feeding, irritability, rapid, widecomplex tachycardia, with child unable to tolerate very long, signs of shock. j. Management includes ABCs, O2 if hypoxic, IV, stable patients require supportive care and transport; unstable patients require amiodarone, procainamide, lidocaine, and cardioversion. 4. Bradyarrhythmias a. Most common type of pediatric arrhythmia b. Most frequently result of hypoxia or result from vagal stimulation (rare) c. Signs and symptoms include slow heart rate (< 60 bpm). d. Lethargic, early signs of CHF e. Management includes AB’s, O2 if hypoxic, IV access; if patient stable: supportive care, ventilation, and oxygenation; if patient unstable: BVM,O2, epinephrine IV or IO. 5. Asystole a. Absence of rhythm; may be initial rhythm seen in pediatrics b. Signs and symptoms include pulseless, apneic, straight line on cardiac monitor (check in two leads).©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 22 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes c. Often due to a respiratory cause d. Management includes ABCs, CPR, IV/IO, ET/BVM, epinephrine, consider causes. 6. Ventricular fibrillation/pulseless ventricular tachycardia a. Very rare in children; causes include electrocution and drug overdoses. b. Signs and symptoms include pulseless, apneic, wide-complex tachycardia or fibrillation on monitor. c. Management includes ABCs, CPR, IV/IO, ET/BVM, defibrillation at 2 j/kg, with subsequent doses 4 j/kg, epinephrine, amiodarone, or lidocaine. 7. Pulseless electrical activity a. Presence of cardiac rhythm with no associated pulse b. Usually due to hypoxia, pericardial tamponade, tension pneumothorax, trauma, acidosis, hypothermia, hypoglycemia c. Signs and symptoms include pulseless, apneic. d. Management includes ABCs, CPR, IV/IO, ET/BVM, epinephrine, consider causes. F. Neurologic Emergencies 1. Neurologic problems are fairly uncommon in childhood, although seizures can and do occur. 2. Seizures a. Abnormal discharge of neurons in the brain b. Common reason for EMS care c. Risk factors for seizures include fever, hypoxia, infections, idiopathic epilepsy, electrolyte disturbances, head trauma, hypoglycemia, toxic ingestions or exposure, tumor, CNS malformations. d. Partial seizures – focal motor seizures, sudden jerking of particular body part, lip smacking, eye blinking, staring, confusion, lethargy, no loss of consciousness e. Generalized seizures – sudden jerking of whole body, tenseness and relaxation of body, positive loss of consciousness f. Status epilepticus – series of one or more generalized seizures without any period of consciousness in between; medical emergency due to prolonged period of apnea©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 23 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes g. Febrile seizures – result of sudden increase in body temperature, most common between 6 months to 6 years of age h. Signs and symptoms include history, high fever (if febrile seizure suspected), condition and position of child, irritability, lethargy, level of consciousness (LOC). i. Management includes ABCs, protect from injury if still seizing, O2 if hypoxic, vital signs; if status epilepticus: IV, blood glucose level (BGL), diazepam or lorazepam; if febrile with long transport, may be directed to administer acetaminophen. 3. Meningitis a. Infection of meninges, the lining of brain and spinal cord b. May be bacterial or viral c. Signs and symptoms include recent illness, high fever, lethargy, irritability, severe headache, stiff neck, extreme discomfort with movement. d. Management includes ABCs, O2 if hypoxic, IV access, fluids, supportive care. G. Gastrointestinal Emergencies 1. Nausea and vomiting a. Not a disease, but symptoms of other disease process b. Common causes include fever, ear infections, respiratory infections. c. Risks include dehydration. d. Management includes ABCs, supportive care, IV, fluids at 20 cc/kg of NS or LR. 2. Diarrhea a. Common occurrence; > 10 or more stools per day b. Risk includes dehydration. c. Management includes ABCs, supportive care, IV, fluids at 20 cc/kg of NS or LR. H. Metabolic 1. Diabetes can occur in young children. 2. Young children can develop hypoglycemia without having diabetes. 3. Hypoglycemia a. Abnormally low concentration of sugar in the blood b. True medical emergency that must be treated immediately©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 24 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes c. Risk of hypoglycemia: diabetic patients: strenuous exercise, too much insulin meningitis, pneumonia and dehydration from illness; nondiabetic patients: physical activity, diet changes, illness, growth d. Signs and symptoms include change in mental status, tachycardia, cool and clammy skin, diaphoresis, low BGL, coma. e. Management includes ABCs, O2 if hypoxic, IV, fluids; if conscious and alert, given oral fluids with sugar, or oral glucose; if patient has altered mental status, administer D25 or D10 via IV or IM glucagon. 2. Hyperglycemia a. Abnormally high concentration of blood sugar b. Hyperglycemia and diabetic ketoacidosis are the most common finding in new-onset diabetics. c. Hyperglycemia is commonly associated with too much food relative to injected insulin, missing insulin injection, defective insulin pump, illness or stress. d. Signs and symptoms include history, fruity breath odor, altered level of consciousness, warm and dry skin, dehydration, polyuria, polydipsia. e. Management includes ABCs, vital signs, BGL, IV, fluids. I. Poisoning and Toxic Exposure 1. Common reason for summoning EMS that result from accidental ingestion 2. Leading cause of preventable death in children < 5 years old, with ironcontaining supplements leading cause of poisoning 3. Best prevention is by teaching people to “poison-proof” their homes. 4. Signs and symptoms include depending on substances, may present with respiratory depression, circulatory depression or collapse, impairment of CNS, effects on thoughts and behavior, injury to gastrointestinal (GI) system, liver necrosis. 5. Management includes: responsive patient: O2 if hypoxic, contact poison control, consider activated charcoal, transport and monitor patient; unresponsive patient: ABCs, patent airway, O2 if hypoxic, BVM if indicated, contact poison control, transport and monitor patient. J. Trauma Emergencies 1. Number one cause of death in infants and children, most of which result©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 25 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes from blunt trauma 2. Mechanism of injury (MOI): most common MOIs include falls, motor vehicle collisions (MVC), car vs. pedestrian, drowning, penetrating injuries, burns, physical abuse. 3. Best way to stop traumatic injuries is to prevent them. 4. Falls a. Most common cause of injury; falls from bicycles account for significant number of injuries. 5. Motor vehicle collisions a. One-third of children who die from trauma do so from motor vehicle collisions, which makes MVCs the leading cause of traumatic death and leading cause of permanent brain injury in children. 6. Pedestrian injuries a. More common in cities where children play near the street. b. Injuries are lethal trauma due to phases of collisions. c. First phase: Vehicle connects with child; child is propelled from vehicle or pushed underneath vehicle. d. Second phase: Child connects with ground or is run over by vehicle. 7. Submersion/Immersion Injuries a. Leading cause of death in boys aged 1–4 years b. Drowning – “the process of experiencing respiratory impairment as the result of submersion/immersion in a liquid medium” c. Drowning has 3 outcomes: no morbidity, morbidity, or mortality; is either “fatal” or “nonfatal” d. Older terms such as “near-drowning” are no longer used. e. Severe and irreversible brain injuries occur as a result of anoxia. 8. Penetrating injuries a. Increase in violent crimes has resulted in increasing number of children with penetrating trauma. b. Risk of death increases with age, and children are usually innocent victims of crimes, although they may be intended victims. c. Visual inspection of external injuries does not provide adequate evaluation of internal injuries. 9. Burns a. Leading cause of accidental death in home for children under 14©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 26 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes years old 10. Physical abuse a. Risk for physical abuse by adults and older children b. Factors include poverty, domestic disturbances, younger parents, substance abuse, community violence. c. Remember to document all pertinent findings, treatments, and interventions, and report to proper authorities 20 X. Special Considerations A. Airway Control 1. Maintain in-line stabilization in neutral position. 2. Administer O2 if patient hypoxic. 3. Maintain patent airway with suctioning and jaw-thrust maneuver. 4. Prepare to assist ineffective respirations (may be necessary to depress pop-off valve). 5. Intubate if airway cannot be maintained. 6. Gastric tube for stomach decompression 7. Needle cricothyrotomy is rarely indicated in pediatrics. B. Stabilization 1. Padding from shoulders to the hips 2. Use appropriately sized equipment C. Fluid Management 1. Use large-bore IV catheter into peripheral vein 2. Do not delay transport to gain IV 3. IO is alternative if IV cannot be accessed 4. 20-cc/kg fluid bolus D. Pediatric Analgesia and Sedation 1. Commonly used analgesics include morphine and fentanyl 2. Consult medical direction when considering pediatric analgesic E. Traumatic Brain Injury 1. Increased risk due to large and heavy head 2. Injuries classified as mild—GCS 13–15; moderate—GCS 9–12; severe—GCS of 8 or less 3. Signs of increased intracranial pressure include: elevated BP, bradycardia, rapid and deep respirations, bulging fontanelles in infants Teaching Tips Focus on analgesic drug dosages, indications, contraindications, and side effects. Discussion Topics Discuss traumatic brain injury in pediatric patients, along with correct Glasgow Coma Scale (GCS) scores based on verbal, motor, and eye movement criteria. Critical Thinking Questions When dealing with a sudden infant death syndrome (SIDS) patient, at what point does care become futile? Class Activities Have students practice nasogastric (NG) tube insertion. Have students practice chest decompression using actual pork or beef ribs and an inner tube. Have students practice intraosseus (IO) insertion using raw chicken drumsticks.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 27 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Signs of herniated brain injury include asymmetrical pupils, decorticate and decerebrate posturing. 5. Management includes O2 if hypoxic, ventilation, consider ET if GCS 8 or less, rapid-sequence intubation (RSI) if GCS 8 or < but muscle tone prevents intubation. 6. Hyperventilation is considered only if child has asymmetrical pupils, active seizures, or neurologic posturing. F. Specific Injuries 1. Head, face, and neck a. Injuries to head most common cause of death in pediatric trauma b. Risk factors include bicycle collisions, falls from trees, car– pedestrian collisions, sporting events, abuse, MVCs. c. Diffuse injuries are more common that focal injuries due to softer, more compliant skull. d. Common facial injuries are lacerations secondary to falls. e. If child sustains severe head injury, suspect cervical injury as well. 2. Chest and abdomen a. Most injuries result from blunt trauma. b. Rib fractures are less likely, with increased risk of intrathoracic injuries due to flexibility of ribs. c. Little protection of abdominal organs due to underdeveloped abdominal muscles 3. Injuries to chest a. Second cause of pediatric trauma deaths b. Severe intrathoracic trauma may be present with no signs of external injuries. c. Pneumothorax and hemothorax can occur in pediatric patients, especially in MVCs. d. Signs and symptoms of tension pneumothorax include diminished breath sounds over affected lung, shift of trachea to opposite side, progressive decrease in ventilator compliance. e. Signs and symptoms of cardiac tamponade include hypotension. 4. Injuries to abdomen a. Significant blunt trauma can result in injury to spleen or liver. b. Spleen is most commonly injured organ in pediatrics. (Make sure that gloves are worn and aseptic techniques are used. Clear this with your supervisor before bringing raw chicken into class.) Practice with students the use of the BVM with the pop-off valve disabled. Points to Emphasize Make sure students understand the anatomic differences in pediatric patients and how injuries may appear in different patterns or without the normal signs that would be seen in an adult. Knowledge Application Have students define the vocabulary of pediatrics.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 28 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes c. Signs and symptoms of splenic injury include tenderness in left upper quadrant (LUQ), abrasions to abdomen, hematoma to abdominal wall. d. Signs and symptoms of liver injury include right upper quadrant (RUQ) pain, right lower chest pain. e. Management includes positioning, fluids, maintenance of temperature. 5. Extremities a. These injuries are limited to fractures and lacerations. b. Types of fractures include bend, buckle, or greenstick fractures (incomplete) or growth plate fractures. 6. Burns a. Second leading cause of death in children and leading cause of accidental death in the home for children < 14 years old b. May be chemical, thermal, or electrical, with scalding being the most common type of burn injury encountered by EMS c. Rule of nines allows for estimation of burn surface area; remember to use pediatric scale; use the child’s palm as a 1% guide for less extensive burns. d. Management includes prompt management of airway, maintain body heat, spinal stabilization with electrical burns, ET with smaller tube if necessary. G. Sudden Infant Death Syndrome (SIDS) 1. Sudden death of infant during first year of life from an illness of unknown etiology 2. Leading cause of death between 2 weeks and 1 year of age 3. Most frequently occurs in fall and winter; more common in boys 4. Signs and symptoms include normal nutrition and hydration, mottled skin, frothy and possibly blood-tinged fluid in mouth/nose, vomitus may be present, unusual position, intrathoracic petechiae found at autopsy. 5. Management includes ABCs, CPR, family support. H. Apparent Life-Threatening Event 1. Sudden event that is characterized by apnea, cyanosis, loss of muscle tone, coughing, gagging. 2. Incident cause is unknown.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 29 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 3. Management includes treating any immediate life threats . 15 XI. Child Abuse and Neglect A. Intended physical and psychological harm B. Common characteristics for abused child include labeled different from others, less than 5 years old (common), children with special needs, different gender from what parents wanted. C. Perpetrators of Abuse or Neglect 1. Parents, caretakers, institutions, legal guardians, foster parents, babysitter, and others 2. Person can come from any geographical area, race, religion, occupation, education, socioeconomic background 3. Certain traits that tend to be shared by abusers include usually parent or full-time caregiver, usually abused as children. 4. Three conditions for potential of abuse include parent or adult with evasive or hostile behavior, child in one of high-risk categories, presence of a crisis. D. Types of Abuse 1. Psychological, physical, sexual, and neglect 2. Physical abuse uses any object that can serve as weapon; deprived of food or toilet; may be burned, shaken, thrown, shot, stabbed, suffocated 3. Sexual abuse ranges from exposing self to sexual acts to sexual torture. 4. Sexual abusers tends to be someone the child knows. E. Assessment of the Potentially Abused or Neglected Child 1. Signs and symptoms include obvious or suspected fractures in child < 2 years old, multiple injuries in various stages of healing, more injuries than normally seen in child of same age, bruises or burns that indicate intentional infliction, increased intracranial pressure, suspected intraabdominal trauma, any injury that does not fit with description of cause given, history does not match injury, delay in seeking help, child dressed inappropriately for situation, comments by siblings or patient, vague parental accounts, accusations that child harmed himself. 2. Signs and symptoms of neglect include extreme malnutrition, longstanding skin infections, extreme lack of cleanliness, verbal/social skills below child of similar age, lack of appropriate medical care, multiple Teaching Tips Using slides or pictures, show students classical patterns of abuse involving burns, cords, ropes, and so forth. These pictures will be disturbing, so bring your students back to the care that needs to be provided. Discussion Topics Discuss with students lists of resources available for child abuse. Critical Thinking Questions How will you as the paramedic answer your abuse patient when they ask whether the abuse is their fault? Class Activities Have students practice various scenarios involving abuse, focusing on identification of the signs of abuse and neglect. Points to Emphasize Remind students that in abuse cases, tensions and emotions can run high. Forcing altercations with alleged abusers does nothing for your patients and puts all of you in danger. Make sure your students know what resources to contact in situations of abuse or neglect.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 30 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes insect bites. F. Management of the Potentially Abused or Neglected Child 1. Appropriate treatment for injuries, protection of child from further abuse, notification of proper authorities; be nonjudgmental, document all statements, findings, and treatments; NEVER leave transport to alleged abuser; report your suspicions to ED and authorities. G. Resources for abuse and neglect 1. Local child protection agencies, Internet resources, children’s hospitals Knowledge Application Have students research cases of pediatric abuse from their local newspapers or the Internet. 15 XII. Infants and Children with Special Needs A. Medical technology has lowered infant mortality rates and allows greater number of children with special needs to live at home B. Children with special needs include: premature infants and children with lung disease, heart disease, neurological disorders, cystic fibrosis, asthma, spina bifida, other congenital birth defects, cerebral palsy, cancer C. Common Home Care Devices 1. Tracheostomy tubes a. Surgically placed tube in inferior trachea b. Complications include: obstruction, site bleeding, site leakage, dislodged tube, infection c. Management includes: maintain open airway, suctioning of tube, position of comfort, O2 for respiratory distress, assisting ventilations in respiratory failure/arrest 2. Apnea monitors a. Used to alert parents or caregivers of the cessation of breathing in infant, some also signal changes in heart rate b. EMS may be summoned when alarm goes off 3. Home artificial ventilators a. Demand ventilators, positive end-expiratory pressure (PEEP) b. Complications include: mechanical failure, shortage of energy c. Management includes: maintain open airway, artificial ventilations 4. Central intravenous lines a. Used for long-term IV therapy, such as IV nutrition, antibiotics, chemotherapy b. Complications include cracked lines, loss of patency, infection, Teaching Tips If possible, obtain several of the home care devices to discuss with the class. Use pictures or slides to show the different home care devices. Critical Thinking Questions If your special needs child has a do not resuscitate order (DNR), is the DNR indicated in an emergency situation regarding equipment failure? Class Activities Invite a home health care nurse in to go over the various home care devices used. Points to Emphasize Remember that the parents/caregivers are familiar with the pediatric patient’s special needs, so use their knowledge and expertise when dealing with the special needs patient.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 31 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes hemorrhage, air embolism. c. Management includes bleeding control, clamp line if air cannot be removed, clamp between crack and patient, positioning child on left side with head down. 5. Gastric feeding tubes and gastrostomy tubes a. Placed to provide nutrition in child who cannot eat or swallow b. Gastric tube – placed through nose into stomach; gastrostomy tube – placed through abdominal wall directly into stomach c. Complications include bleeding at site, dislodged tube, respiratory distress if tube backs up into esophagus and is aspirated, altered mental status if patient diabetic and feeding missed. d. Management includes ABCs, suctioning, O2, position sitting or lying on right side with head elevated. 6. Shunts a. Surgical connection that runs from brain to abdomen, allowing excess cerebrospinal fluid (CSF) to drain b. Complications include blocked shunt, leading to increased intracranial pressure (ICP), shunt failure. c. Signs and symptoms include: increased ICP, altered mental status, drowsiness, respiratory distress, pupil dysfunction or posturing d. Management includes open airway, ventilations, transport. 7. General assessment and management practice a. Same assessment as everyone else b. ABCs, primary assessment, secondary assessment, history c. Involve parents or caregivers, as they are familiar with patient’s illness. 10 XIII.Multiple-Casualty Incidents (MCIs) Involving Children A. JumpSTART 1. Objective tool developed specifically for triage of children in MCI 2. Objectives include optimize primary triage of injured children; enhance effectiveness of resource allocation; reduce emotional burden on triage personnel. B. Using the JumpSTART System 1. Identify and direct all ambulatory patients to designated area. Critical Thinking Questions What officer involved in an MCI is going to be most emotionally taxed? Class Activities Create several scenarios of pediatric patients in an MCI. Have students apply the objectives of JumpSTART.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 32 Chapter 4 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. Assess breathing. 3. Assess respiratory rate. 4. Assess perfusion. 5. Assess mental status. C. Modifications for Nonambulatory Children 1. All nonambulatory children must be evaluated immediately using JumpSTART algorithm. 2. Red, yellow, green D. Reassessing Dead/Nonsalvageable Victims 1. Reassess dead/nonsalvageable victims unless suffering from injuries incompatible with life. Points to Emphasize Remind students that during an MCI, assessment changes affect the greatest number of patients. 5 XIV. Summary A. Pediatric emergencies can be stressful for you, the patient, and family members. B. Pediatric emergencies are often caused by airway or breathing problems. C. Look for signs and symptoms of abuse, and report those findings. D. Approach, assessment, and management may have to be modified for age of patient. 5 XV. Case Study Class Activities Discuss the case with students now that they are familiar with the chapter. 5 XVI. You Make the Call Class Activities Read and discuss the call and questions as a group. 5 XVII. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 1 Detailed Lesson Plan Chapter 5 Geriatrics 200–230 Minutes Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture 5 II. Introduction A. Aging: the gradual decline of biological functions B. Aging varies by individual C. Some functional losses are caused by age-related changes; others are the result of disease, lifestyle, diet, behavior, and environment D. Important to distinguish between normal age-related changes and abnormal changes Knowledge Application Go through the chapter and list chapterspecific vocabulary terms. For homework, have students list the definition of each term. 20 III. Epidemiology and Demographics A. Because of medical and technological advances, life expectancy has increased. B. The growing number of elderly will present a challenge not only to EMS, but also to society’s resources C. Population Characteristics 1. By late 2014, elderly population reached more than 45 million. 2. “Graying of America” is the process in which the number of elderly is pushing up the average age of the U.S. population. 3. Several reasons: increase survival rate, birth rate declining, absence of major wars and catastrophes, improved health care and standard of living 4. By 2030, 70 million people will be age 65 years or older. 5. Number of old-old (age 85 or older) will increase. D. Gerontology: study of the effect of aging on humans E. Geriatrics: specialized aspect of medicine that focuses on the care of the Discuss Topics With students, discuss how the decrease in population and increase in survival have affected medical costs. Discuss with students the different programs available for elderly patients. Discuss with students the risks of poverty to the elderly, especially medical care (not taking medications properly, lack of heat, etc.) Critical Thinking Questions What medical conditions do you think you may respond to in the elderly home health MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes elderly F. Today, 36% of EMS calls involve elderly. G. Societal Issues 1. Ageism: societal label of “old person” 2. Retirement may be one-third of average life span 3. Many people will live happy, productive elderly lives; whereas others may suffer physical and financial difficulties. 4. Treatment of elderly must involve social situation. H. Living Environments 1. Independent and dependent living situations 2. “Oldest” elderly members tend to live alone, majority being women. I. Poverty and Loneliness 1. Elderly living alone represent one of most impoverished and vulnerable parts of society. 2. Income may be depleted by death of partner, long illness, decrease of retirement benefits. 3. Low incomes tend to make elderly choose among food, shelter, medications. 4. Lack of family members add to feelings of loneliness and depression. 5. Elderly may fear loss of independence, being burden to family; may feel that illness is part of aging J. Social Support 1. Of elderly living alone, 74% receive no forms of assistance. 2. Interaction with family, friends, other people encouraged to avoid social isolation. 3. Some elderly turn to dependent care arrangements such as live-in nursing, assisted living, life-care communities, congregate care, nursing homes, or personal-care homes. 4. Tight finances and lack of mobility may result in accidental hypothermia, carbon monoxide (CO) poisoning, fires, inadequate nutrition, or reduction of medications. 5. Many state have few to no restrictions on personal-care aides or others who provide services, resulting in risk to elderly of criminal activity. 6. Adult community or nursing home removes some worries of self-care care patient? Class Activities Have a representative from your local senior center come in to discuss with students the resources available for the elderly. Have students create a home for the elderly patient, listing all of the prevention measures that would be in place. If possible, visit an assisted living home, so that students can observe the programs in place for the elderly. If available, have students participate in a blood pressure clinic, prevention program, or similar program focused on the elderly. Knowledge Application Have students list the various ways in which an elderly patient can feel a loss of independence.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes but includes degree of loss of independence, exposure to illness, lack of contact with young people. K. In responding to the elderly, remember that living conditions will be part of patient history, and that illness carries special meaning to them, more aware of death L. Ethics 1. Ethical concerns include multiple decision makers, patient competency, advanced directives. 2. Usually, honoring the wishes of the patient is best if the patient is competent. 3. Follow state and local laws regarding advanced directives. M. Financing and Resources for Health Care 1. Social Security pays significant portion of monthly bills, with medical support provided by four publicly funded programs: a. Medicare – operates in two parts: A covers in-hospital care; B provides medical insurance to cover physician, outpatient care, therapy, durable medical equipment b. Medicaid – federal and state government share responsibility; provides largest share of public funding for long-term care; contributes 45% for nursing home care c. Veterans Administration – health care to veterans with disabilities or service-related problems; free or sliding scale d. Local government – publically funded hospitals and clinics provide care for those unable to find health care; usually less than 65 years old 2. With number of younger taxpaying workers shrinking, publically funded programs face uncertain future. N. Health Care Alternatives 1. Big debate centers on question of preventing death at all costs. 2. Advised by agencies that money may be better spent on prevention of disease rather than preventing death. 3. To decrease health care costs, patient care has been shifted to home care. 4. With more home care, EMS will be responding to more complicated care for patients.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes O. Prevention and Self-Help 1. Best intervention is prevention 2. Goal is to keep people from becoming sick or injured 3. Taking part in community education programs can help reduce morbidity among elderly P. Senior centers – provide social atmosphere for education, recreation, and entertainment; support health care Q. Religious organizations – may provide care for elderly members R. National and state associations – AARP, Alzheimer’s Association, Association for Senior Citizens; provide advocacy for retired individual S. Governmental agencies – Department of Health and Human Services, Office of Aging; being familiar with these agencies and what they offer will allow you to provide further care to your elderly patient. 5 IV. General Pathophysiology, Assessment, and Management A. Medical disorders often present as functional impairment and should be treated as an early warning of undetected problem. B. Signs and symptoms do not necessarily point to underlying cause. C. Thorough evaluation must always be done to detect possible cause of impairment. Class Activities Have students practice assessment skills on each other. 35 V. Pathophysiology of the Elderly Patient A. Generalizations about age-related changes and disease process include: 1. Multiple-System Failure a. Body less efficient with age; increasing likelihood of malfunction b. Maintenance, defense, and repair processes weaker in elderly c. May suffer from more than one illness at a time d. Average of 6 medical disorders may coexist e. Comorbidity: concomitant diseases f. Common complaints include fatigue, weakness, dizziness, vertigo, syncope, falls, headache, insomnia, dysphagia, loss of appetite, inability to void, constipation, diarrhea. g. May not monitor condition, owning to illness as part of aging concept 2. Pharmacology of elderly a. Use of multiple medications; average is 4.5 per day, not including Discussion Topics Discuss with students the age-related changes seen in the elderly. Using pictures/models, compare the mid- 20s to 30s adult with the elderly patient, focusing on the changes that occur with age. Discuss with students the accommodations that can be made for the elderly patient’s skin in securing an IV. Discuss with students situations they may©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes over-the-counter (OTC) or herbal remedies. b. Polypharmacy: multiple medications c. Sensitivity to drugs increases with age, causing more drug-to-drug interactions, drug reactions, drug-disease interactions. d. Drug dosages must be adjusted to prevent toxicity. e. Ask whether patient is taking prescription drug as prescribed. f. Reasons for decreased drug compliance include limited income, memory loss, limited mobility, sensory impairment, multiple/complicated drug therapies, fear of toxicity, childproof containers, duration of drug therapy. g. Factors that can increase compliance include good physician– patient communications, belief that illness/injury is serious, drug calendar, compliance counseling, easy-open packaging, pillbox compartments, transportation to pharmacy, simple directions, ability to read. 3. Problems with mobility and falls a. Two of the most effective prevention measures are regular exercise and a good diet. b. Lack of mobility can cause poor nutrition, difficulty with elimination, poor skin integrity, greater disposition for falls, loss of independence/confidence, depression, isolation. c. Fall-related injuries are the leading cause of accidental death in the elderly; intrinsic falls (related to patient) or extrinsic falls (related to environment) d. Intrinsic factors: dizziness, sense of weakness, impaired vision, altered gait, central nervous system (CNS) problems, decreased mental status, medications e. Extrinsic factors: slippery floors, lack of handrails, loose throw rugs, and so forth 4. Communication difficulties a. Normal changes include impaired vision, blindness, impaired or loss of hearing, lower sensitivity to pain 5. Problems with continence and elimination a. Respect patient’s dignity, as elderly may find it embarrassing to encounter in which elderly patients decrease their heart rate (bowel movements, coughing, etc.). Class Activities Gather empty medication bottles, and label them with common prescriptions taken by the elderly. Have students list the medical conditions that are usually seen with the medications. Smear Vaseline over a pair of glasses. Have students wear these to simulate visual changes in the elderly. Have students walk across the room with these on to show how falls can occur with vision changes. Have students wear a leg immobilizer and attempt to walk up and down the stairs. Demonstrate the dangers of slip rugs to students and ways the rugs can be made more safe (tape, etc.). Using the average of $1,600 per month, have students create a budget that their elderly patient may live on, including a $350 prescription medication amount, and what the elderly patient may do to save money. Create scenarios that involve an elderly©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes discuss problems. b. Incontinence: may be urinary or fecal; can lead to rashes, skin infections, skin breakdowns, urinary tract infections (UTIs), sepsis, falls, fractures c. Factors that predispose: medical disorders, multiple medications, decreased bladder capacity, urinary flow rate, and ability to postpone voiding d. Management can include surgery, absorptive devices, catheters. e. Elimination: may be a sign of a serious underlying condition, leading to other complications f. Straining to eliminate can seriously effect cerebral, coronary, and peripheral arterial circulation. g. Transient ischemic attacks (TIAs) or syncopal episodes can occur when bearing down for bowel movement. h. Drugs that can cause difficult elimination include opioids, anticholinergics, antacids, calcium, iron, anticonvulsants, diuretics. B. Assessment Considerations 1. Standard Precautions with all patients; HEPA or N-95 may be necessary if tuberculosis (TB) is risk factor. 2. Be alert to environment and temperature. C. General Health Assessment 1. Look at living situation, level of activity, social support, level of independence, medication history, sleep patterns, nutrition. 2. Conditions that may complicate eating include breathing/respiratory problems, abdominal pain, nausea/vomiting, poor dental care, medical problems, medications, alcohol/drug abuse, psychological disorders, poverty, problems with shopping or cooking. 3. By-products of poor nutrition include vitamin deficiencies, dehydration, hypoglycemia. D. Pathophysiology and Assessment 1. Try to distinguish chief complaint from primary problem. 2. Multiple diseases complicate the assessment, chronic problems making acute problems more difficult to assess. 3. Always treat the patient complaint on a threat-to-life basis when medical patient with communication issues (hard of hearing, visual impairments, etc.). Using real time, have students perform an assessment to experience the time delays and assessment changes that may have to be made. Knowledge Application Have students list various signs that their elderly patients are having difficulty living on their own.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes information is not known. 4. Other complications may include decreased response to pain and altered temperature regulation, causing absence of fever and being more prone to environmental problems. 5. Always use patience, respect, and kindness during your interview. E. History 1. You may have to spend more time gathering information, with periods of rest if your patient gets fatigued. 2. Find patient’s medications, as they can be good indicator of patient’s disease. F. Communication Challenges 1. Cataracts (clouding of lens) and glaucoma (increased pressure) can diminish sight; level of anxiety increases in patient with visual impairments; make sure to place yourself where patient can see or touch you. 2. Overall hearing decreases, and patient may suffer from tinnitus or Menière’s disease; deafness or impaired hearing can make obtaining a history almost impossible; use notes, family/friends, gestures to communicate. 3. Speech difficulties may include difficulty in retrieving words, slow speech, changes in voice quality, dentures not in place. 4. Techniques for improved communication include: introduce yourself; speak slowly, distinctly, and respectfully; speak to patient first and speak face-to-face and at eye level; retrieve hearing aids, glasses; have patient use stethoscope while you speak into it; turn on lights; use verbal and nonverbal signs; be polite; preserve dignity; explain what you are doing; observe signs of anxiety. G. Altered Mental Status 1. Age may sometimes diminish mental status; confusion can occur with noise, equipment, strange voices. 2. Common symptoms include delirium, confusion, distractibility, restlessness, excitability, hostility. 3. Try to determine whether mental status change is new; depression may affect mental status©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 8 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes H. Concluding the History 1. If time allows, try to verify history with credible source; usually less offensive to patient if done out of his presence. 2. Observe patient’s surroundings for self-sufficiency. I. Physical Examination 1. Patient may be easily fatigued and unable to tolerate long examination. 2. Several layers of clothing may be worn. 3. Patient may minimize or deny symptoms—fears of loss of independence. 4. Peripheral pulses may be difficult to feel, owing to peripheral artery disease. 5. Increase in mouth breathing and loss of skin elasticity 5 VI. Management Considerations A. Management plan will be tailored to fit each patient’s illness, injury, and general health B. Conditions must be spotted and corrected quickly, owing to elderly patients’ potential for rapid deterioration. C. Primary assessment, changes in neurologic status, vital signs, cardiac status D. Transport tends to be more stressful to elderly; avoid lights and sirens if possible, remain calm, and provide emotional support . Critical Thinking Questions What worries do you think elderly patients may have during an emergency? What can you do to help alleviate their fears? 30 VII. System Pathophysiology in the Elderly A. Age-related changes in structure and function of organs increases probability of disease. B. Respiratory System 1. Decreased chest wall compliance, loss of lung elasticity, increased air trapping due to collapse of smaller airways, reduces strength and endurance of respiratory muscles. 2. Vital capacity may be reduced by 50% by age 65. 3. Maximum breathing capacity may decrease by 60%; maximum O2 uptake may decrease by 70%. 4. Decrease in cough reflex and cilia activity 5. Kyphosis, pollutants, and cigarette smoking decrease pulmonary Discussion Topics Discuss with students what signs and symptoms may be missing in an elderly patient on beta-blockers. Review with students the organ system changes and the treatment accommodations that must be made. Critical Thinking Questions Why would a diminished cough reflex make your elderly patient more prone to©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 9 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes function. 6. Changes result in decreased ventilation and progressive hypoxemia. 7. Management includes position for adequate breathing, use breathing patterns to assist in exhalation, bronchodilators, O2, monitor ventilation for fatigue, fluids if needed, using caution not to overload. C. Cardiovascular System 1. Variables include diet, smoking, alcohol use, education, socioeconomic status, personality traits, physical activity. 2. Age-related changes include left ventricular wall thickening and enlargement, fibrosis in heart and peripheral vascular system, hypertension, arteriosclerosis, decreased cardiac function, stiffened and lengthened aorta, ventricular filling pattern changes, loss of atrial kick, exercise intolerance, degeneration of conductive system. 3. Changes result in declining stroke volume, decreased cardiac output, diminished ability of heart to respond to stress. 4. Management includes O2 if patient is hypoxic, have patient stop all activity, start IV, medications, vital signs, electrocardiogram (ECG), calm and comforting response. D. Nervous System 1. Cells in CNS cannot reproduce. 2. People experience 10% reduction in brain weight from age 20 to 90. 3. Do not assume that an elderly patient possesses less cognitive ability. 4. Changes that occur include difficulty with recent memory, psychomotor slowing, forgetfulness, decreased reaction times. 5. Reduced brain size leaves room for increased bleeding after an injury to head; elderly are more prone to subdural hematomas. 6. Management includes: determine baseline mental status; question patient in environment with minimal distractions; observe for weakness, chronic fatigue, changes in sleep pattern, syncope, signs of stroke; apply O2 if hypoxic; capnography. E. Endocrine System 1. Early diagnosis offers greatest opportunities to prevent disability. 2. Diabetes, menopause, thyroid disorders, Marfan syndrome 3. Altered mental status may be only real presentation. pneumonia? What cardiac dysrhythmia leaves elderly patients at a higher risk for clots? Why is the elderly patient more prone to hypothermia? What brain injury is the elderly patient more prone to, owing to structural changes in the brain? Knowledge Application For homework, have students list each organ system and the age-related changes that occur with the elderly.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 10 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Management includes ABCs, ECG, O2 if hypoxic, blood glucose level (BGL), vital signs. F. Gastrointestinal System 1. Changes include decreased saliva production, dry mouth, predisposition to choking, decreased gastric secretions, intestinal motility decreases, difficulty swallowing, delayed digestive process, reduced production of hydrochloric acid, gum atrophy, decreased taste buds, hiatal hernia, diminished liver function, reduced clotting proteins 2. Management includes: ABCs, shock protocols G. Thermoregulatory System 1. Highly susceptible to variations in environmental temperature due to altered or impaired thermoregulatory mechanism 2. Changes include reduced effectiveness of sweating to cool body, deterioration of autonomic nervous system, decreased shivering, lower resting peripheral blood flow, diminished perception of cold, medication that affects response to temperature, hyperthermia and hypothermia. 3. Common cause of EMS response H. Integumentary System 1. Skin loses collagen, thus becoming more subject to injuries from bumps and tearing. 2. Injury to skin more severe, increased healing time and greater risk of secondary infection, skin tumors, drug-induced eruptions, and viral or fungal infections. I. Musculoskeletal System 1. Loss of 2–3 inches of height 2. Osteoporosis results in softening of bones, causing increased risk of fractures. 3. Kyphosis revealed as increased curvature of spine 4. Demineralization of bones makes patient more susceptible to fractures. 5. Management includes O2 if hypoxic, IV, pain control, immobilization. J. Renal System 1. Reduced number of functioning nephrons by 30–40% 2. Renal blood flow reduced, increasing waste products in blood. 3. Decreased renal function can result in anemia or hypertension.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 11 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Management includes adequate oxygenation, fluid status, monitoring output, pain control, vital signs. K. Genitourinary System 1. Progressive loss of bladder sensation and tone, feel frequent need to urinate, increasing risk of falls, especially at night 2. UTI and sepsis increased owing to lack of emptying. 3. In males, prostate may become enlarged, causing difficulty with urination. L. Immune System 1. Function of T cells declines, making them less able to notify immune system of invasion. 2. Immune senescence: diminished immune response 3. Best prevention is adequate nutrition, infection control measures, and exercise; vaccinations may be indicated. M. Hematologic System 1. Affected by failure of renal system to stimulate production of red blood cells (RBCs), and inadequate nutrition 2. Blood volume decreased due to less body water, making recovery more complicated 3. Management includes O2 if hypoxic, prepare for increased bleeding times, monitor. 60 VIII.Common Medical Problems in Elderly A. Illness may be more severe, complications more likely, and classic signs and symptoms absent or altered B. More likely to react adversely to stress and deteriorate more quickly C. Pulmonary/Respiratory Disorders 1. Pneumonia a. Infection of lung, usually caused by bacterium or virus; aspiration may develop as result of difficulty swallowing. b. Serious disease for elderly, fourth leading cause of death in patients older than 65. c. More frequent due to decreased immune response, reduced pulmonary function, increased colonization of Gram-negative bacteria, abnormal or ineffective cough reflex, decreased These Master Teaching Notes cover outline pages 172 through 193 and can be altered to cover any of the medical problems covered Teaching Tips Discuss the fact that the typical signs and symptoms that are usually seen with these medical conditions may not be present in the elderly patient. Pull up statistics on elderly alcohol and drug abuse.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 12 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes effectiveness of mucociliary cells. d. Greatest risk include frail adults, chronic multiple diseases, patients in hospitals or nursing homes. e. Signs and symptoms include dyspnea, congestion, fever, chills tachypnea, sputum production, altered mental status; occasionally, abdominal pain may be only symptom; fever may be absent. f. Treatment includes management of all life threats, maintain adequate oxygenation, transport. 2. Chronic obstructive pulmonary disease (COPD) a. Collection of diseases characterized by chronic airflow obstruction with reversible/irreversible components b. Usually refers to emphysema, chronic bronchitis, asthma. c. Factors include cigarette smoking, childhood respiratory disease, environmental pollutants, genetic predisposition. d. Exacerbation of COPD: condition that can rapidly lead to death because accompanying hypoxia and hypercapnia alter acid-base balance and deprive tissues of O2 e. Signs and symptoms include accessory muscle use, cough, dyspnea, exercise intolerance, increased sputum production, pleuritic chest pain, pursed-lip breathing, tachypnea, tripod positioning, wheezing. f. Treatment includes supplemental O2 to correct hypoxia, drug therapy. 3. Pulmonary embolism a. Always consider in patient with respiratory distress b. Blood clots are most frequent cause of pulmonary embolism. c. Risk factors include atrial fibrillation, deep vein thrombosis (DVT), fractures of the pelvis, hip, or leg, major surgery, malignancy (tumors), obesity, paralysis, presence of a venous catheter, prolonged immobility, trauma to leg vessels, use of hormones. d. Usually originate in deep veins of calves and thighs e. Signs and symptoms include acute onset of dyspnea, chest pain, right heart failure, cardiac arrhythmias, cardiovascular collapse f. Treatment includes: O2, IV, morphine sulfate, anticoagulants, Using pictures, show the different stages of decubitus ulcers. Discussion Topics Discuss with students the topic of suicide in the elderly. Focus on risk factors, along with signs of a potential suicide. With students, discuss the different conditions that can present as altered mental status. Discuss with students the different drugs that can cause skin problems in the elderly (beta-blockers, PCN, sulfa drugs, etc.). Discuss with students the different medications that have to be altered in dose because of the age-related changes in the elderly liver and kidneys. Critical Thinking Questions What drug can be given to an elderly patient who overdoses on beta-blockers? Why is an elderly patient more prone to medication toxicity? What medication, commonly used in the elderly patient, has a very narrow therapeutic index? What medication causes visual changes,©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 13 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes dopamine per medical direction, upright position, avoid lifting legs or knees, transport, monitor vital signs and any changes. 4. Pulmonary edema a. Effusion or escape of serous fluids into alveoli and interstitial tissues of lungs b. Can develop rapidly in elderly c. Commonly associated with acute myocardial infarction (AMI), pulmonary infection, inhaled toxins, narcotic overdoses, pulmonary embolism, and decreased atmospheric pressure d. Signs and symptoms include dyspnea with congestion, rapid labored breathing, cough with blood-stained sputum, cyanosis, cold extremities, moist crackles, accessory muscle usage, rhonchi e. Treatment includes altering cause of condition, ABCs. 5. Lung cancer a. Highest incidence in the world is in U.S. and increases with age. b. Leading cause is cigarette smoking. c. Signs and symptoms include progressive dyspnea, hemoptysis, chronic cough, weight loss. d. Treatment includes occurs in hospital setting, prehospital includes ABCs, comfort. D. Cardiovascular Disorders 1. Leading cause of death in elderly; assessment and treatment often complicated by non-age-related factors and disease processes in other organ systems; determine level of cardiac function; look for hypertension and orthostatic changes, dehydration, and edema; listen for bruits, heart sounds. 2. Angina pectoris a. Development increases with age. b. Usually triggered by physical activity, after a meal, or after exposure to very cold weather and may vary in frequency. c. Defined as “pain in the chest,” although only 10–20% of elderly will feel angina; dyspnea will be the more likely symptom. d. Develops when narrowing of coronary vessels as a result of plaque or vasospasms leads to inability to meet O2 demand of heart muscle including complaints of “seeing colors,” when at a toxic level? Class Activities Create a scenario for the various medical problems listed. Have students perform assessments, identify the problems, and treat accordingly. Have students complete a run report and radio report as well. (This will take time, so plan these activities during lab skills.) Create a drug box that includes the commonly prescribed medications, along with flashcards that list the indications for each drug. Have students match up the drugs with the conditions. Use tissue paper as an example of the fragility of the elderly patient’s skin. Have students attempt to manipulate the paper without tearing it. Using rubber tubing, have students attempt to start an IV, while an instructor continues to “roll” the vein. Knowledge Application Create a chart that lists the common medical problems in the elderly. For homework, have students list signs and symptoms, definitions, and treatment. For homework, have students list the©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 14 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes (pain represents buildup of lactic acid). e. Signs and symptoms include dyspnea, exercise intolerance, chest pain (10–20%). f. Treatment includes ABCs. 3. Myocardial infarction (STEMI and non-STEMI) a. Actual death of muscle tissue owing to a partial or complete occlusion of one or more of the coronary arteries b. Greatest number of patients over age 65 c. Signs and symptoms include absence of pain, confusion/dizziness, dyspnea (common in patients over age 85), exercise intolerance, fatigue/weakness, neck, dental, or epigastric pain, syncope (note: elderly patients less likely to present with classic symptoms). d. Mortality rate doubles after age 70; elderly more likely to suffer silent myocardial infarctions; majority of deaths that occur in first few hours caused by arrhythmias. e. Treatment includes ABCs, MONA. 4. Heart failure a. Takes place when cardiac output cannot meet body’s metabolic demands b. Rises exponentially after age 60; widespread among elderly; most common diagnosis in hospitalized patients over 65 c. Causes include impairment to flow, inadequate cardiac filling, volume overload, myocardial failure. d. At-risk factors include anemia, arrhythmias, hypoxic, infection, ischemic, noncompliance with drug therapy, hypothermia or hyperthermia, nonsteroidal anti-inflammatory drugs (NSAIDs), arrhythmias. e. Signs and symptoms include edema, fatigue (left-side failure), twopillow orthopnea, dyspnea on exertion, dry and hacking cough progressing to productive cough, dependent edema (right side), nocturia, anorexia, hepatomegaly, ascites. f. Treatment includes ABCs, diuretics, vasodilators, antihypertensive agents, inotropic medications. 5. Arrhythmias common drugs that patients can overdose on, along with signs and symptoms and indicated treatments.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 15 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. May occur with age; atrial fibrillation most common in elderly patients. b. Occur primarily as a result of degeneration of conduction system; anything that decreases myocardial blood flow can produce arrhythmia; may also be caused by electrolyte imbalance. c. Elderly do not tolerate extremes in heart rate. d. Treatment depends on type of arrhythmia; pacemakers, drug therapy, defibrillators. e. Pacemaker complications include electrode disgorgement, battery failure, fibrosis around catheter site, lead fracture. 6. Aortic dissection/aneurysms a. Aortic dissection: degeneration of wall of aorta, at either thoracic or abdominal level b. Aneurysm: rupture of vessel c. Of aneurysms, 80% are the result of atherosclerosis and hypertension. d. Distal portion of aorta is most common site for abdominal aneurysms. e. Signs and symptoms include tearing sensation, back pain, numbness, tingling, pain in legs, pulsating mass (abdominal), abnormal pulses and/or blood pressures. f. Treatment includes ABCs, gentle handling, IV, drug therapy. 7. Hypertension a. Product of industrial society; experts do not believe that it is a normal age-related change. b. Affects 50% of people over age 65 c. Defined as blood pressure greater than 140/90 mmHg d. Hypertensive patients are at risk for heart failure, stroke, blindness, renal failure, coronary heart disease, peripheral vascular disease e. Contributing factors include atherosclerosis, obesity, diabetes. f. Signs and symptoms include often a silent disease that shows no clinical signs; nonspecific complaints include headache, tinnitus, epistaxis, slow tremors, nausea, and vomiting (note: acute onset of high blood pressure [BP] without kidney involvement is a telltale©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 16 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes indicator of thyroid disease). g. Treatment includes beta-blockers, diuretics, prevention (modified diet, exercise, smoking cessation, compliance with medications). 8. Syncope a. Common complaint among elderly b. Condition results when blood flow to the brain is temporarily interrupted or decreased. c. Most often caused by problems with nervous system or cardiovascular system d. Common presentations include vasodepressor syncope, orthostatic syncope, vasovagal syncope, cardiac syncope, seizures, TIAs. E. Neurologic Disorders 1. Most disorders will exhibit as an alteration in mental status. 2. Underlying causes may range from stroke to degenerative brain disease. 3. Cerebrovascular disease (stroke/TIAs) a. Strokes are the third leading cause of death in U.S. b. Incidence of stroke and risk of death increases with age. c. Occlusive strokes are more common in elderly. d. Higher risk of stroke comes from atherosclerosis, hypertension, immobility, limb paralysis, congestive heart failure (CHF), atrial fibrillation. e. TIAs are more common in elderly, and more than one-third will develop a major stroke. f. Brain ischemia strokes – injury to brain tissue caused by an inadequate supply of O2 and nutrients g. Subarachnoid or intracerebral hemorrhage – bleeding within the brain h. Signs and symptoms include altered mental status, coma, paralysis, slurred speech, change in mood, seizures. i. Treatment includes: prehospital stroke screen, rapid transport, ABCs, fibrinolytics. j. Prevention of strokes includes cessation of recreational drugs, cessation of smoking, control of hypertension (HTN), good eating©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 17 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes habits, moderate use of alcohol, regular exercise, treatment of blood disorders, treatment of cardiac disorders. 4. Seizures a. Can be easily mistaken as strokes, and first-time seizures may occur as a result of damage from previous stroke. b. Common causes include alcohol withdrawal, hypoglycemia, mass lesion, head trauma, epilepsy, stroke, syncope. c. Signs and symptoms include generalized to subtle. d. Treatment includes ABCs, transport, immobilization if trauma present. 5. Dizziness/vertigo a. Frightening and a frequent complaint of elderly b. Vertigo may be accompanied by sweating, pallor, nausea, vomiting, spinning sensation. c. Causes include impaired visual input, inner-ear function, peripheral sensory input, CNS impairment, prescription drugs, hypoglycemia, alcohol. d. Virtually impossible to distinguish dizziness, syncope, and presyncope in prehospital setting 6. Delirium, dementia, and Alzheimer’s disease a. Of all Americans over age 65, 15% have some degree of dementia or delirium. b. Dementia – chronic global cognitive impairment, often progressive or irreversible (best known is Alzheimer’s) c. Delirium – global mental impairment of sudden onset and selflimited duration d. Delirium: may be organic brain disease or disorders that occur elsewhere in body; serious condition in elderly; causes include subdural hematoma, tumors, drugs, intoxication, CNS infections, electrolyte abnormalities, heart failure, fever, metabolic disorders, chronic endocrine disorders, postconcussion. e. Delirium: presentation varies; signs and symptoms include acute onset of anxiety, inability to focus, disordered thinking, irritability, inappropriate behavior, fearfulness, excessive energy, psychotic©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 18 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes behaviors, hallucinations, paranoia, aphasia, slurring of speech. f. Dementia: more prevalent in elderly; usually caused by underlying neurologic disease; often called organic brain syndrome, senile dementia, or senility; causes include small strokes, atherosclerosis, age-related neurologic changes, neurologic diseases, hereditary diseases, Alzheimer’s disease. g. Dementia: signs and symptoms include progressive disorientation, shortened attention span, aphasia, nonsense talking, hallucinations, hampered ability to communicate; EMS may have to rely on caregivers for information. h. Alzheimer’s disease: chronic degenerative disorder that attacks the brain, resulting in impaired memory, thinking, and behavior; three stages: early stage (recent memory loss, inability to learn new things, mood swings, personality changes); intermediate stage (complete inability to learn new material, wandering, loss of selfcare abilities); terminal stage (inability to walk, regression to infant stage, loss of eating and swallowing) i. Alzheimer’s disease: Treat both patient and family, as care can pose high stress levels. 7. Parkinson’s disease a. Degenerative disorder characterized by changes in muscle response, tremors, loss of facial expression, and gait disturbances b. Primary cause is unknown, but it does affect the basal ganglia in brain. c. Primary and secondary Parkinson’s disease d. Secondary Parkinson’s disease has known causes, including viral encephalitis, atherosclerosis of cerebral vessels, reactions to certain drugs or toxins, metabolic disorders, tumors, head trauma, degenerative disorders (Shy-Drager syndrome). e. Signs and symptoms include initial sign is resting tremor combined with a pill-rolling motion, rigid muscles, slower movements, jerky movements, shuffled gait, kyphotic deformity, mask-like face devoid of expression, slow and monotone voice. f. Treatment includes: manage treatable conditions and transport.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 19 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes F. Endocrine Disorders 8. Diabetes mellitus a. Primarily type II diabetes b. Development occurs as a result of poor diet, decreased physical activity, loss of lean body mass, impaired insulin production, resistance by body cells to actions of insulin. c. Signs and symptoms include fatigue, weakness, elevated glucose levels. d. Treatment includes ABCs, BGL monitoring. e. Increased risk of atherosclerosis, retinopathy, delayed healing, blindness, altered renal function, peripheral vascular disease, foot ulcers, amputations 9. Thyroid disorders a. Result from inadequate levels of thyroid hormones b. May experience hypothyroidism or hyperthyroidism c. Signs and symptoms include mental confusion, anorexia, falls, incontinence, decreased mobility, increased muscle or joint pain; hyperthyroidism may be result of medication errors, with typical complaint of heat intolerance, atrial fibrillation, failure to thrive, abdominal distress, diarrhea, exhaustion, and depression. d. Treatment includes ABCs, medical evaluation. G. Gastrointestinal (GI) Disorders 1. Common among elderly, with GI bleeding most frequent emergency 2. Significant risk of hemorrhage and shock; managed aggressively 3. Upper GI bleed a. Peptic ulcer: injury to mucous lining of upper part of GI tract due to stomach acids, digestive enzymes, inflammatory drugs, and other causes b. Gastritis: inflammation of lining of stomach c. Esophageal varices: abnormal dilation of veins in lower esophagus; common complication of cirrhosis of liver d. Mallory-Weiss tear: tear in lower esophagus that is often caused by severe and prolonged retching 4. Lower GI bleed©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 20 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. Diverticulosis: small pouches on colon; cause 70% of lifethreatening lower GI bleeds b. Tumors: can cause bleeding when tumor erodes into blood vessels within intestines c. Ischemic colitis: inflammation of colon resulting from impaired blood supply d. Arteriovenous malformations: abnormal link between artery and vein 5. Signs and symptoms of GI bleed include coffee-ground emesis, black and tarlike stools (melena), blood in emesis or stool, orthostatic hypotension, pulse greater than 100 (unless patient on beta-blockers), confusion. 6. Complications include angina symptoms, CHF, weakness, dyspnea. 7. Bowel obstruction a. Typically involves the small bowel b. Causes include tumors, prior abdominal surgery, medications, vertebral compression fractures. c. Signs and symptoms include diffuse abdominal pain, bloating, nausea, vomiting, distended abdomen, hypoactive or absent bowel sounds, fever, weakness, shock, electrolyte disturbances. 8. Mesenteric ischemia/infarct a. Occurs when a portion of the bowel does not receive enough blood to survive b. Age-related changes make elderly more vulnerable to condition. c. Signs and symptoms include bloody diarrhea, tachycardia (although vagal effect may mask), abdominal distention, risk of shock, massive infection. 9. Treatment of gastrointestinal disorders a. Airway management, support of breathing and circulation, supplemental O2 if patient is hypoxic b. IV fluid replacement, rapid transport H. Skin Disorders 1. Age-related changes to immune system make elderly more prone to skin diseases and infection, including pressure ulcers (bedsores). 2. Skin diseases©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 21 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a. Pruritus (itching) is common complaint in elderly. caused by dermatitis, environmental conditions, may be sign of systemic disease. b. Slower healing and decreased tissue perfusion make elderly more susceptible to bacterial infections, cellulitis, impetigo, staphylococcal scalded skin, fungal infections, herpes zoster (shingles). c. Treatment includes questions about medical history and medications (certain medications may induce skin disorders). 3. Pressure ulcers (decubitus ulcers) a. Usually occur in people over 70 years old; highest incidence occurs in nursing homes. b. Typically develop from waist down, usually over bony prominences in bedridden patients, but can occur anywhere on body c. Result from tissue hypoxia and affect the skin, subcutaneous tissues, and muscles d. Increased risks include external compression of tissues, altered sensory perception, maceration (caused by excessive moisture), decreased activity, decreased mobility, poor nutrition, friction or shear e. Reducing development of pressure ulcers or alleviating condition involves: changing patient position frequently, using a pull sheet to move patient, padding areas of skin before moving, cleaning and drying excessive moisture, cleaning ulcers with normal saline solution and dressing I. Musculoskeletal Disorders 1. Musculoskeletal diseases are the leading cause of functional impairment in the elderly, producing chronic disability, leading to a context for illness 2. Osteoarthritis a. Leading cause of disability in patients over 65 b. Contributing causes include wear and tear, age-related changes, obesity, primary disorders of the joint, trauma, congenital abnormalities. c. Signs and symptoms include joint pain that worsens with exercise©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 22 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes and improves with rest, diminished mobility, joint deformity, crepitus, grating sensation, tenderness on palpation or passive motion. d. Treatment includes prevention strategies such as stretching and strengthening, drug therapy, surgery. 3. Osteoporosis a. Largely responsible for hip, wrist, and vertebral fractures following a fall or other injury b. Risk factors include age, gender (higher risk for women), race (White and Asian higher risk), body weight, family history. c. Signs and symptoms include usually asymptomatic until fracture occurs. d. Treatment includes prevention of fractures through exercise and drug therapy, pain management. 4. Ankylosing spondylitis a. Form of arthritis that primarily affects the spine, causing inflammation of joints between the vertebrae of spine and sacroiliac joints in pelvis b. As condition worsens, new bone forms as part of healing process, resulting in bony ridges throughout spine, causing a stiff and inflexible spine (known as “bamboo spine”). c. Treatment includes modified accommodation of patient for airway techniques, splinting and transport; padding must be used for immobilization, and airway techniques applied without extension. d. EMS care MUST be done properly, as devastating results can occur if patient’s spine is not protected accordingly. J. Renal Disorders 1. Most common diseases include renal failure, glomerulonephritis, renal blood clots. 2. Two age-related factors are loss in kidney size and changes in wall of renal arteries and arterioles serving glomeruli; most of loss occurs in tissues that filter the blood. 3. With renal changes, toxins and medications are more likely to accumulate in bloodstream; kidneys are ineffective in clearing wastes. 4. Risks factors in acute renal failure include hypotension, heart failure,©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 23 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes major surgery, sepsis, angiographic procedures, use of nephrotoxic antibiotics, hypertension. K. Urinary Disorders 1. Most infections result from bacteria and can easily lead to urosepsis, due to reduced immune system function. 2. Factors that contribute include atrophic vaginitis, bladder obstruction from prostate, dementia, diabetes, immobilization, stroke, upper urinary tract stone, use of indwelling catheters. 3. Signs and symptoms include cloudy and foul-smelling urine, bladder pain, frequent urination, fever, chills, abdominal discomfort. 4. Treatment includes IV catheter, fluids, antibiotics, transport, maintenance of adequate blood pressure and fluids. L. Environmental Emergencies 1. Great health risk to elderly; 50% of all heatstroke deaths in people over age 50 and hypothermia and winter risks (pneumonia, influenza) responsible for > 750,000 deaths each year 2. Hypothermia a. Factors that predispose elderly are accidental exposure to cold, atrioventricular (AV) shunts, chronic illness, CNS disorders, medications, endocrine disorders, forced inactivity, inflammatory dermatitis, low or fixed income, malnutrition or starvation. b. Signs and symptoms include slow speech, confusion, sleepiness, hypertension, and increased heart rate in early stages; in later stages the blood pressure and heart rate will slow, sometimes to barely detectable level, cool skin (note: patient may not shiver). c. Treatment includes rewarming, ABCs, reassessment (note: death commonly results from cardiac arrest or ventricular fibrillation). 3. Hyperthermia a. At risk for heat stress from changes in sweat glands and increased incidence of heart disease b. Development of heat cramps, heat exhaustion, or heatstroke c. Risk factors include alcoholism, altered sensory output, medications that inhibit sweating (e.g., antihistamines, tricyclic antidepressants), concomitant medical disorders, decreased functioning of©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 24 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes thermoregulatory center, inadequate liquid intake, low or fixed income, diuretics. d. Signs and symptoms include nausea, light-headedness, dizziness, headache, absence of sweating, neurologic impairment; use high temperature as reliable indicator. e. Treatment includes adequate fluid intake, reduced activity in heat, shelter in air-conditioning, light clothing; if hyperthermia present, immediate cooling, ABCs, transport. M. Toxicologic Emergencies 1. Aging alters pharmacokinetics and pharmacodynamics in elderly, with functional changes in kidneys, liver, and GI that slow absorption and elimination 2. Of hospital admissions, 30% are result of drug-related illness; accidental overdose occurs more frequently in the aged due to confusion, vision impairment, self-selection, forgetfulness, and concurrent drug use. 3. Assessment of geriatric patient must include full list of medications, newly prescribed medications, past medical history, and your knowledge of medications (note: try to take all medications to hospital with patient). 4. Beta-blockers – treatment for hypertension, angina, cardiac arrhythmias a. Propranolol, hydrochloride, nadolol, sotalol, esmolol, timolol, metroprolol, penbutolol, labetalol b. Signs and symptoms include depression, lethargy, sleep disorders, orthostatic hypotension, inability to increase cardiac output with sympathetic response, decreased intraocular pressure. c. Treatment includes ABCs, removal of gastric contents, cardiorespiratory support, fluids, nonadrenergic inotropic agents (glucagon), atropine for bradycardia. 5. Antihypertensives/diuretics – treatment of hypertension and CHF a. Hydrochlorothiazide (HCTZ), furosemide, bumetanide, torsemide b. Signs and symptoms include postural hypotension, circulatory collapse, potassium depletion, renal function impairment. 6. Angiotensin-converting enzyme inhibitors – treatment of hypertension and CHF a. Captopril, enalapril, lisinopril, fosinopril, benazepril, quinapril,©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 25 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes ramipril b. Signs and symptoms include hypotension; vomiting; diarrhea; possible anaphylactic reactions (hemodialysis patients); dizziness; light-headedness; rash; muscle cramps; swelling of hands, feet, or eyes; cough; headache; stomach upset; fatigue (note: Captopril can cause loss of taste). 7. Digitalis – treatment of CHF, atrial fibrillation, atrial flutter, paroxysmal atrial tachycardia, cardiogenic shock a. Digoxin, Lanoxin b. Positive inotropic effect, negative chronotropic effect, slows conduction and increases refractory period c. Low therapeutic index, so dose must be adjusted for each patient. d. Signs and symptoms include change in kidney function, visual disturbances, fatigue, weakness, nausea, loss of appetite, abdominal discomfort, dizziness, abnormal dreams, headache, vomiting, hypokalemia, sinoatrial (SA) block, SA arrest, second- or third-degree AV block, atrial fibrillation, accelerated AV junction, premature ventricular contractions (PVCs) V-tach, atrial tachycardia. e. Treatment includes gastric lavage with activated charcoal, correction of confirmed hypokalemia, treatment of bradycardia with transcutaneous pacing (TCP) or atropine, treatment of rapid ventricular with lidocaine, digoxin-specific FAB fragment antibodies treatment (Digibind)-antidote. 8. Anticoagulants a. Aspirin is used as a common antiplatelet inhibitor. b. Warfarin is difficult to dose and requires routine monitoring; Vitamin K can be used to reverse toxicity. c. Newer anticoagulants do not need monitoring but do not have reversal agent (dabigatran, rivaroxaban, and apixaban). d. Patients on anticoagulants (besides aspirin) are at increased risk for hemorrhage. 9. Antipsychotics/antidepressants – treatment for psychiatric disorders, depression e. Depression is most common mental disorder in elderly.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 26 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes f. Fluoxetine (Prozac) and bupropion (Wellbutrin) – selective serotonin reuptake inhibitors (SSRIs) g. Amitriptyline (Elavil) and imipramine (Tofranil) – tricyclic antidepressants h. Isocarboxazid (Marplan) and phenelzine (Nardil) – monoamine oxidase inhibitors (MAOIs) i. Signs and symptoms include sedation, lethargy, muscle weakness, dry mouth, constipation, urinary retention, confusion, orthostatic hypotension. j. Lithium – treatment for manic depression k. Signs and symptoms include metallic taste in mouth, hand tremors, nausea, muscle weakness, fatigue, blurred vision, lack of coordination, coma, death. l. Chlorpromazine (Thorazine), thioridazine (Mellaril), chlorprothixene (Taractan), thiothixene (Navane), haloperidol (Haldol) – antipsychotic medications m. Signs and symptoms include restlessness, involuntary muscle movements, sedation, anticholinergic effects. n. Sedative-hypnotic medications – used to relax patient, allay anxiety by decreasing anxiety without producing sedation o. Benzodiazepines most common; flurazepam (Dalmane), temazepam (Restoril), triazolam (Halcion), diazepam (valium), lorazepam (Ativan), chlordiazepoxide (Librium) p. Signs and symptoms include drowsiness, sluggishness, addiction if used over long period of time. q. Field treatment includes ABCs, airway management, transport. 10. Medications for Parkinson’ s disease a. Parkinson’s in a common disorder in the elderly; caused by a breakdown of dopamine-secreting neurons located in the basal ganglia, leading to an imbalance in other neurotransmitters b. This imbalance leads to rigidity, bradykinesia, resting tremors, and postural instability. c. Carbidopa/levodopa (Sinemet), bromocriptine (Parlodel), benztropine mesylate (Congentin), amantadine (Symmetrel)©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 27 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes d. Signs and symptoms include dyskinesia, visual hallucinations, nightmares, orthostatic hypotension. e. Tolcapone (Tasmar) given in combination with Sinemet can cause liver failure in patients presenting with acute jaundice. f. Treatment includes decrease patient anxiety, supportive environment, ABCs, continued reassessment. 11. Anti-seizure medications a. Cause of seizure may be from previous CNS injury; anti-seizure medication depends on type of seizures present. b. Signs and symptoms include sedation, GI distress, headache, dizziness, lack of coordination, rashes. c. Treatment includes airway management and supportive therapy. 12. Analgesics and ant-inflammatory agents a. Used in the treatment of pain and inflammation for chronic conditions such as osteoarthritis and rheumatoid arthritis b. Include narcotics and nonnarcotic analgesics and corticosteroids c. Narcotic analgesics: codeine, meperidine (Demerol), morphine, hydrocodone (Vicodin), oxycodone (Percodan, Percocet), hydromorphone (Dilaudid) – alter pain perception d. Signs and symptoms include sedation, mood changes, nausea, vomiting, constipation, orthostatic hypotension, respiratory depression. e. NSAIDs and acetaminophen (Tylenol) – prescribed for mild to moderate pain f. Signs and symptoms include gastric irritation, renal and hepatic toxicity, confusion. g. Aspirin signs and symptoms include ringing or buzzing in ears, GI hemorrhage. 13. Corticosteroids a. Powerful anti-inflammatory agents used to treat rheumatoid arthritis and other inflammatory conditions b. Signs and symptoms include hypertension, peptic ulcer, aggravation of diabetes mellitus, glaucoma, increased risk of infection, suppression of normally produced corticosteroids.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 28 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes c. Cortisone (Cortone), hydrocortisone (Hydrocortone), prednisone (Deltasone) N. Substance Abuse 1. Widespread problem in U.S. 2. Up to 17% over age of 60 addicted to substance 3. Factors that contribute are age-related changes, loneliness, loss of employment, loss of spouse or partner, malnutrition, moving from home to other living arrangement, multiple prescriptions. 4. Elderly may abuse substances to escape pain or life, may be accidental. 5. May involve drugs, alcohol, or both 6. Drug abuse a. Polypharmacy increases likelihood of complications, such as drug– drug interactions, drug–disease interactions, and drug–food interactions. b. Signs and symptoms of abuse include decreased vision/hearing, drowsiness, falling, memory changes, mood changes, orthostatic hypotension, poor dexterity, restlessness, weight loss. c. Treatment includes document all findings, collect medications for identification, transport, referral for substance abuse treatment. 7. Alcohol abuse a. Use or abuse of alcohol places elderly at high risk of toxicity, due to physiologic changes to the body, interaction with medications. b. Signs and symptoms include anorexia, confusion, history of falls, insomnia, mood swings, denial, hostility when questioned about drinking, nausea, visible anxiety. c. Treatment includes: do not judge patient, evaluate for fluid therapy, consider possibility of withdrawal, transport. O. Behavioral/Psychological Disorders 1. Behavioral and/or psychological disorders that occur later in life are often dismissed as normal age-related change, which is untrue, and places the elderly patient at risk for a missed diagnosis and correction of a treatable condition. 2. Emotionally stressful incidents for elderly may be isolation, loneliness, loss of independence, strength, fear of future, and so forth.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 29 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 3. Common classifications of disorders are affective disorders, dissociative disorders, organic brain syndrome, personality disorders. 4. Emotional health is imperative to physical well-being. 5. Signs and symptoms include lapses in memory, cognitive difficulty, changes in sleep patterns, fear of death, changes in sexual interest, thoughts of suicide, withdrawal from society. 6. Treatment includes ABCs, supportive care, transport. 7. Depression a. Up to 15% of noninstitutionalized and 30% of institutionalized elderly experience depression. b. Inquire about crying episodes, feelings of sadness or despair, current stressful events, any sensory changes, duration of depression or history, any treatment, hypochondriasis, emotional pain, dysphoria. c. Treatment includes supportive care, transport, psychotherapy, antidepressants (note: question about thoughts of suicide in a delicate and tactful manner). 8. Suicide a. Highest suicide rate in U.S. is among people over age 65, especially men. b. Third leading cause of death among elderly c. Depression is leading cause of suicide; other stressors include bereavement, chronic illness, family history of suicide, family issues, financial problems, isolation and loneliness, living in a youthoriented society, low serotonin levels, physical impairment, substance abuse, unrelieved pain. d. Warning signs include loss of interest in enjoyable activities; curtailing of social interaction, grooming, and self-care; breaking medical or exercise routine; grieving personal loss; feeling useless; putting affairs in order; stockpiling medications or other lethal means of self-destruction. e. Higher incidence of suicide among terminally ill f. Prevention involves intervention from all involved; recognition of warning signs is critical.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 30 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes g. Treatment includes: first priority for paramedic is to protect themselves and then protect patient from self-harm; use law enforcement to protect scene; do not rule out use of firearm among elderly suicide; do not leave suicidal patient alone; transport. 10 IX. Trauma in the Elderly Patient A. Leading cause of death in the elderly B. Contributing factors are slower reflexes, arthritis, diminished eyesight and hearing. C. Falls, motor vehicle collisions (MVCs), criminal assault all contribute to injuries. D. Age-related factors: osteoporosis, muscle weakness, reduced cardiac reserve, decreased respiratory function, impaired renal function, decreased elasticity in the peripheral blood vessels E. General Assessment 1. Determine mechanism of injury (MOI); leading causes include falls, MVCs, burns, assaults, underlying medical conditions. 2. Blood pressure may be higher in elderly patients; elevated pulse may not be present due to heart disease or medications; pain sensation may be decreased, masking fractures (note: best indicator of shock in elderly is altered mental status or changes in consciousness during assessment). F. Observing for Abuse/Neglect 1. Observe scene for signs of abuse and/or neglect. 2. Geriatric abuse – syndrome in which an elderly person has received serious physical or psychological injury from family members or other Teaching Topics Pull up pictures of elderly patients involved in motor vehicle collisions. Discussion Topics Discuss with students medications that will alter the elderly patient’s vital signs presentation when involved in a trauma. Critical Thinking Questions Do you believe that the decreased reflex time of elderly patients make them a risk on the road? Is this any different from younger patients who text and drive?©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 31 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes caregivers 3. Signs and symptoms include unexplained trauma. 4. Risk factors include average age over 80, multiple medical problems, dementia. 5. If abuse suspected, do NOT confront family; document all findings, report suspicions to emergency department and appropriate authority (note: most states consider it a crime to NOT report abuse). 10 IX. General Management A. Keep in mind age-related changes in the elderly, along with presence of chronic disease. B. Cardiovascular Considerations 1. Recent or past myocardial infarctions (MIs) may contribute to arrhythmias or CHF in trauma patient. 2. Decreased response of heart in adjusting rate and stroke volume in hypovolemia 3. May require higher than usual arterial pressure for perfusion of vital organs due to increased peripheral vascular resistance and HTN 4. Caution with fluid administration due to decreased myocardial reserves 5. Hypotension, hypovolemia, and hypervolemia poorly tolerated C. Respiratory Considerations 1. Consider physical changes such as dentures, decreased chest wall movement, decreased vital capacity. 2. Reduction of tolerance for anoxia to all organs; COPD widespread among elderly 3. Adjustments may be needed in oxygenation, CO2 removal; monitor pulse oximetry and capnography. D. Renal Considerations 1. Decreased ability to maintain normal acid–base balance and compensate for fluid changes 2. Decreased renal function and decreased cardiac reserves increases elderly risk of fluid overload and pulmonary edema, along with medication toxicity E. Transport Considerations 1. Modification of positioning, immobilization, and packaging Critical Thinking Questions How would you care for an elderly patient who has an injury to the cervical spine and congestive heart failure (CHF)? Class Activities Have students practice immobilization skills, using padding and alternate forms of immobilization equipment (vacuum splints, etc.).©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 32 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. Physical deformities from chronic conditions can cause pain or require special care. 3. Skin frailty can cause pressure sores or tearing. 4. Hypothermia is increased risk for elderly; keep patient warm. 10 X. Specific Injuries A. Orthopedic Injuries 1. Elderly suffer greatest mortality and morbidity from falls, with hip or pelvis most common fall-related fracture. 2. Signs and symptoms include tenderness over affected joint, shortening and external rotation of leg, non-weight-bearing. 3. Other fractures from falls include proximal humerus, distal radius, proximal tibia, thoracic and lumbar bodies. 4. Treatment includes questions about underlying medical conditions, immobilization, and packaging. B. Burns 1. Patients age 60 and older more likely to suffer death from burns (except neonates and infants). 2. High mortality rate results from slower reaction time, preexisting conditions, age-related skin changes that allow deeper burns and slower healing time, immunologic and metabolic changes that increase risk of infection, reduced reserves of vital organ systems. 3. Treatment includes ABCs, stop the burning process, administration of appropriate measures of fluids; delayed response in elderly burn patients increases risk of infection and systemic failure. C. Head and Spinal Injuries 1. Elderly suffer more head injuries, even from minor trauma. 2. Major factor is difference in proportion between brain and skull, as brain size decreases with age but skull remains constant in size, creating room for brain to move 3. Cervical spine more susceptible to injury due to osteoporosis and spondylosis (degeneration of vertebral body) 4. Changes in cervical spine can cause compression of nerve roots or spinal cord 5. Sudden neck movement can cause spinal cord injury, even without Discussion Topics Discuss with student the risks of osteoporosis, arthritis, and brittle bones in the elderly patient. Have students list the medical procedures that could actually cause harm to these patients. Critical Thinking Questions What are the causes for the high mortality rate among burned elderly patients? What is the normal fluid resuscitation amount in a burned elderly patient? Class Activities Create scenarios specific to listed injuries. Have students perform assessments, identify the problems, treat, and document. Knowledge Application Have students create a list of specific injuries, presentations, and treatments.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 33 Chapter 5 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes fracture 6. Provide appropriate spinal precautions (based upon local protocols) at time of primary assessment. 5 XI. Summary A. Because of “graying of America,” there is greater number of people age 65 and older. B. Keep in mind the anatomic, physiologic, and emotional changes that occur with age. C. Elderly patients are more susceptible to medication side effects, trauma, environmental stressors, abuse/neglect. D. Elderly patients may present with variety of scenarios that are unique to population. E. Knowledge and understanding of this population will allow you to make more accurate assessments and treatment plans. 5 XII. Case Study Class Activities Discuss the case with students now that they are familiar with the chapter. 5 XIII.You Make the Call Class Activities Read and discuss the call and questions as a group. 5 XIV. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Detailed Lesson Plan Chapter 6 Abuse, Neglect and Assault 160–180 Minutes Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture 5 II. Introduction A. Obtaining accurate statics is difficult, owing to underreporting. B. Almost five children die per day from child abuse, elder abuse occurs at 700,000 to 1.1 million/year, and between 2 and 4 million women are battered each year. C. Abuse transcends gender, race, age, and socioeconomic status. D. Paramedic’s responsibilities include identification of victims of abuse, initiation of action, and reporting of incident to proper authorities. E. Early detection is critical to breaking abuse cycle. 5 III. Partner Abuse A. Results when man or women subjects domestic partner to some form of physical or psychological violence B. May be wife, husband, girlfriend, boyfriend, roommate, same-sex partner C. Most widespread form of abuse is against women, but men can be abused by women. D. Abusive relationships follow same patterns and cycles. Points to Emphasize Stress to students that there are multiple forms of abuse. 10 IV. Reasons for Not Reporting Abuse A. Fear of reprisals to themselves or children B. Humiliation at powerlessness and inability to stop abuse C. Hope that abuse will end, especially when abuser promises to change D. Abuser may justify abuse, stating that victim deserved it. E. May lack financial means, job skills to seek help. F. Report of abuse is usually last resort. Discussion Topics Discuss with students the different reasons why someone might not report abuse. Discussion Topics Discuss with students the laws in your area regarding domestic violence. MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes G. If intervention does not occur, victims are all too often are killed by abuser. 10 V. Identification of Partner Abuse A. Several categories of abuse: physical, verbal, sexual B. Physical – application of force in many ways C. Verbal – words chosen to control or harm a person D. Sexual – forced sexual contact and includes marital and date rape E. Ten generic risk factors: 1. Male who is unemployed 2. Male uses illegal drugs at least once a year 3. Different religious backgrounds 4. Family income below poverty level 5. Unmarried 6. Either partner violent toward children at home 7. Male did not graduate from high school 8. Male unemployed or has blue-collar job 9. Male between 18 and 30 years old 10. Male saw father hit mother 10 VI. Characteristics of Partner Abusers A. Abuse occurs in all demographic groups. B. Some characteristics of abusers include: 1. Trouble paying bills, or holding jobs 2. Unable to keep pace with technological changes, making their jobs obsolete 3. History of family violence 4. Abuser does not like being out of control, but powerless to change 5. Overly aggressive personality 6. Feelings of low self-esteem, insecurities, jealousy, unpredictable rages 7. Alcohol or drug use that increases feelings 8. Sense of remorse and shame after abusive episode, with promises to change 9. Cycle of violence repeats Critical Thinking Questions Why might the abuser call 911 several times before the abuse occurs? Class Activities Have a police officer who specializes in domestic violence speak to the class.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 10 VII. Characteristics of Abused Partners A. Primary risk factor is history of violence between parents. B. Pregnancy increases risk in abusive relationship. C. Substance abuse D. Emotional disorders E. May attempt to protect attacker F. May avoid eye contact, exhibit nervous behavior, or watch abuser G. Verbal clues: “I am always causing trouble,” “We have been having problems lately.” Critical Thinking Questions What fears can you think of that might be felt by a person involved in an abusive relationship and prevent that person from leaving the relationship? 10 VIII. Approaching the Battered Patient A. Direct questioning is best during assessment. B. Convey your awareness that partner may have caused harm, and be willing to discuss it; avoid judgmental statements. C. Listen to abused patients, and encourage them to regain control over their lives. D. Share your knowledge of community resources, such as shelters, counseling, support services. E. Do not leave scene without advising patient to take all necessary precautions by rehearsing the quickest way to leave home, where patient will go/call, and so forth. F. Abuser may be reported and taken into custody by police; you must inform patient that abuser can be released, and provide patient information about available protection programs. Discussion Topics Discuss with students the various domestic abuse programs available in your area. Class Activities Create a scenario involving domestic violence, including care provided. Have students compete a run report, focusing on appropriate documentation. 5 IX. Elder Abuse A. Elder abuse is a widespread medical and social problem that is caused by many factors, such as: 1. Increased life expectancies, increased dependency on others, decreased productivity in later years 2. Physical and mental impairments, limited resources, economic factors that strain family resources, stress on middle-aged caregivers B. Elder abuse is expected to grow along with elderly population. C. Paramedic responsibility includes remaining alert to signs of elder abuse. Knowledge Application For homework, have students list signs and symptoms they may observe in an elder abuse victim.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 X. Identification of Elder Abuse A. Domestic abuse – takes place when elder is being cared for in a homebased setting, usually by relatives B. Institutional elder abuse – elder being cared for by a person with legal or contractual responsibility to provide care, such as caregivers, nursing home staff, other professionals C. Both types of abuse can be acts of commission (physical, sexual, or emotional violence) or acts of omission (neglect). D. Some signs are subtle, such as theft of belongings or loss of freedom; others are obvious, such as wounds, decubitus ulcers, poor hygiene. Knowledge Application Have students research on the Internet different cases of elder abuse, including cases of financial abuse. 5 XI. Theories about Domestic Elder Abuse A. Four main theories about causes of domestic elder abuse: 1. Caregivers feel stressed and overburdened 2. Patient’s physical and or mental impairment 3. Family history of violence 4. Personal problems of caregivers Class Activities Have a representative from your local senior agency come in to discuss elder abuse. 5 XII. Characteristics of Abused Elders A. Affects all demographic groups B. Difficult to outline an accurate profile of abused elder C. Most common cases: 1. Elderly women abused by their sons 2. Elderly dependent on others for care 3. Elderly who are mentally and or physically challenged D. In cases of neglect: 1. Abused elders commonly live alone. 2. Fear asking for help due relatives complaining about helping, or threats to place in nursing home E. Elderly abuse victims tend to be reluctant to give information about abusers for fear of retaliation. Critical Thinking Questions Is abandoning an elderly family member in a safe place considered neglect? What responses regarding injuries would you likely expect to hear from a patient who has suffered abuse? 5 XIII. Characteristics of Elder Abuse A. Difficult to profile abusers of elderly B. Several characteristics are commonly found in abusers: 1. Exhibit alcoholic behavior, drug addiction, or mental impairment 2. Dependent on income of elder, causing resentment, anger, or violence Discussion Topics Discuss with students the different stress factors that could be present in an elder abuser.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 XIV. Child Abuse A. One of most difficult circumstances faced as a paramedic B. Child abuse ranges from physical, emotional, to neglect of child’s basic needs. C. May be afflicted by parents, caregivers, foster parents, babysitters, stepparents, siblings, other relatives, or peers D. Damage lasts a lifetime; perpetuates a cycle of violence for generations Teaching Tips This is one of the most difficult responses that EMS will have to deal with. Go over ways in which the EMS provider can cope with abuse. 10 XV. Characteristics of Child Abusers A. Cannot relate child abuse to social class, income, or education B. Patterns that do emerge include: 1. History of abuse within own family 2. Physically or emotionally abused as children 3. Prefer to use other forms of discipline but buckle under stress 4. Tend to be male 5. One or both of abuser’s parents are abusers C. Behavioral traits include: 1. Use or abuse of drugs/alcohol 2. Immaturity or preoccupied with self 3. Lack of obvious feeling for the child, rarely looking at or touching child 4. Apparent lack of concern about child’s injury, treatment, or prognosis 5. Open criticism of child, with little indication of guilt or remorse for involvement in child’s condition 6. Little identification with the child’s pain, whether physical or emotional Discussion Topics Discuss with students ways they think that the cycle of violence could be stopped. Go over with students the various child abuse prevention programs. 10 XVI. Characteristics of Abused Children A. Child’s behavior is one of the most important indicators of abuse. 1. Under age 6 usually appear excessively passive 2. Over age 6 seem aggressive B. Other behavioral clues include: 1. Hopeless crying during treatment, or no crying at all 2. Avoiding the parents or showing little concern for parental absence 3. Unusual wariness or fear of physical contact 4. Apprehension and/or constant alertness for danger 5. Prone to sudden behavior changes, absence of nearly all emotions 6. Neediness, constantly requesting favors, food, or things C. Use your instincts and knowledge of age-appropriate behavior to guide first impression. Discussion Topics Go over the age-appropriate behaviors observed in children. Class Activities Have students list ways in which they may be able to gain the confidence of a child.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 20 XVII. Identification of the Abused Child A. Not all injured children are abused. 1. Child volunteers story of injury without hesitation. 2. Child’s story matches story told by parents. B. Cases of parental or child behavior that raise index of suspicion create a challenge for the paramedic to distinguish between intentional injury and authentic accident C. Conditions that are commonly mistaken for abuse: 1. Car seat burns, staphylococcal scalded skin syndrome 2. Chickenpox, hematologic disorders that can cause bruising D. Physical Exam 1. Signs of physical mistreatment of child most often easiest to recognize 2. Soft tissue injuries, multiple bruises, bites, burns, and defensive wounds E. Burns and Scalds 1. Burn tend to be in certain common locations with distinct patterns. 2. Soles of the feet, palms of hands, back, or buttocks; may or may not present with other injuries 3. Children scald more easily due to thinner skin. 4. Home water tends to be 140°F, which will scald in about 5 seconds for an adult. 5. Accidental burns tend to have “splash” patterns created by spattering water. 6. Intentional scalding is characteristic of lack of “splash” patterns referred to as “dipping injuries” and are a common form of child abuse. F. Fractures 1. Second most common form of abuse 2. Sites of fractures include skull, nose, facial structures, upper extremities, ribs. 3. Twisting and jerking the upper extremity 4. Neck injuries from shaking 5. Ribs are very pliable in children; with fractures at this site, maintain high index of suspicion for abuse. G. Head Injuries 1. Over time, abuse injuries progress from extremities and trunk to the head. 2. Head injuries commonly found include scalp wounds, skull fractures, subdural hematomas, and repeated concussions. Teaching Tips Using pictures of injury patterns, go over with students the various injuries sustained in child abuse cases (this may be difficult for some students to view). Discussion Topics Discuss with students the neglect of a child. Have students list the signs of neglect. Class Activities Have a social worker, police officer, or medical professional who deals with abuse of children come in to speak with students. Points to Emphasize Remember that emotional abuse is just as damaging as any other abuse. Knowledge Application Create a chart with the various injuries listed. For homework, have students list the identifying markers associated with each injury, along with treatment.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 3. Head injuries claim the largest number of lives among abused children and account for most of the long-term disability. H. Shaken Baby Syndrome 1. Frequently occurs when a parent or caregiver becomes frustrated with a crying infant and all other attempts to quiet the child have failed 2. Occurs when person picks up infant and shakes baby vigorously 3. Movement causes permanent brain damage, such as subdural hematomas or diffuse swelling, injuries to neck and spine, and retinal hemorrhage, leading to blindness 4. If shaken hard enough or repeatedly, child may die. I. Abdominal Injuries 1. Small proportion of injuries suffered by child but usually very serious when they occur 2. Blunt trauma can cause injury to liver, spleen, or mesentery. 3. Look for swelling, pain, vomiting, and hemodynamic compromise. J. Maternal Drug Abuse 1. Drug use during pregnancy is a subtle but devastating form of child abuse (fetal alcohol syndrome, “crack babies”). 2. Cocaine and alcohol use during pregnancy are associated with longterm problems in child. K. Signs of Neglect 1. Child not provided with adequate food, clothing, shelter, or medical care 2. EMS has position to observe child’s home environment 3. Signs of neglect: a. Malnutrition, severe diaper rash, diarrhea/dehydration b. Hair loss; untreated medical conditions; inappropriate, dirty, or torn clothing or lack of clothing c. Tired and listless attitude, near constant demands for physical contact or attention L. Signs of Emotional Abuse 1. Often hardest form of abuse to identify 2. Six forms of emotional abuse: a. Ignore child, show indifference to needs, fail to provide stimulation b. Reject, humiliate, or criticize child c. Child isolated and deprived of normal human contact or nurturing d. Terrorized or bullied through verbal assaults and threats, creating fear and anxiety©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes e. Parent/caregiver encourages destructive or antisocial behavior f. Child overpressured by unrealistic expectations of success 5 XVIII. Recording and Reporting Child Abuse A. Paramedics have responsibility to report suspected cases of child abuse and may have opportunity to provide early intervention. 1. Abusive adult may actively seek help by calling EMS several times within 24-hour period. 2. May summon help for inconsequential symptoms or demonstrate inability to handle impending crisis 3. Warning signs should be noted. B. As the paramedic, conduct examination of abused child with another colleague present C. Keep personal reactions to yourself, document only objective observations; do not put assumptions in your report. D. Final document should be objective, legible, and written with knowledge that it may be used in court. E. Always put child’s interest first, treating with kindness and gentleness. Teaching Tips Obtain the number of the local agency to report suspected abuse. Points to Emphasize Remember that documentation must be done in a professional manner with no opinions of others. Knowledge Application Give students a child abuse scenario, along with the care provided. Have students complete a run report for homework, focusing on proper and complete documentation. 15 XIX. Sexual Assault A. Males and females of all backgrounds, from infancy to old age, can be victims of sexual assault B. Sexual assault – unwanted sexual contact, whether genital, oral, rectal, or manual (prosecuted as a crime) C. Rape – penile penetration of the genitalia or rectum without the consent of the victim (felony offense) D. Characteristics of victims of sexual assault/rape 1. Statistical patterns show that adolescent females younger than 18 are most likely group to be victimized; rape occurs every 2 minutes on average; most likely to be raped by someone she knows 2. One-third of all juvenile sexual abuse victims are younger than 6 years old; children raised in families where there is domestic violence are 8 times more likely to be sexually molested 3. Sexual assault victims may be physically injured or killed and commonly Discussion Topics Discuss with students the steps they can take to preserve evidence in a sexual abuse case. Discuss with students the different date rape drugs used in sexual assault, along with the medical side effects the patient may present with. Critical Thinking Questions What range of emotions do you think you may see when administering care to a victim of sexual abuse?©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes suffer internal injuries, infections, sexually transmitted diseases (STDs), unwanted pregnancies. 4. Psychological damage includes shame, anger, lack of trust. 5. Children find it difficult to speak about molestation; likely they know the person and fear reprisal; causes confusion of situation, and child fears no one will believe him. 6. Symptoms of sexual abuse include nightmares, restlessness, withdrawal tendencies, hostility, phobias, regressive behaviors, truancy, promiscuity, drug and alcohol abuse. E. Characteristics of Sexual Assailants 1. Assailants come from every background. 2. Some characteristics include abused as children, believe that domination is part of relationship, under influence of drugs or alcohol. 3. Victims may be drugged by assailant, which will cause signs of extreme intoxication without smell of alcohol, or drug-induced amnesia, which will make questioning difficult. F. Date Rape Drugs 1. Medications that facilitate a sexual assault by rendering a person unresponsive, weaken the ability to resist attacker, cause amnesia of event 2. Drugs associated with rape (predator drugs) include Rohypnol, GHB, ketamine, MDMA. 3. Note any suspicions or observations that suggest use of date rape drugs. G. EMS Responsibilities 1. Primary responsibility is safety for yourself, crew, and patient. 2. Provide safe environment. 3. Provide proper psychosocial care and privacy. 4. Use open-ended questions that allow patient to reestablish a sense of control. H. Human Trafficking 1. Human trafficking including sex trafficking, labor trafficking, forced marriages, similar abuses. 2. Traffickers use violence, threats, deception, debt bondage, other manipulative tactics. 3. Vulnerable populations: children under 18 induced into commercial sex, adults over 18 induced into commercial sex, children and adults induced Class Activities Have a police officer from your community who specializes in investigation of sexual assault speak with students about the characteristics of this abuse. Points to Emphasize Remember to be nonjudgmental when dealing with sexual abuse patients. Knowledge Application Give students a sexual abuse scenario, with the care provided. Have students complete a run report for homework, focusing on proper and complete documentation.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes to perform labor or services 4. Indicators: disconnected from friends, family and activities, stopped attending school, sudden change in behavior, engaged in commercial sex acts, disoriented or confused, show signs of abuse, act fearful or submissive, denied of care, someone else is in control of the situation, coached on what to say, live in unsuitable conditions, lack personal possessions, able to leave where they live, or unreasonable security measures 5. If you have identified someone in a human trafficking situation, contact law enforcement immediately. I. Hate Crimes 1. Crime of hatred or prejudice in which target is particular victim(s) because of perceived membership in certain social group 2. Groups include racial, religious, sexual orientation, political, disability, other social groups. 3. Based on bias and referred to as bias-motivated crime 4. Involve vandalism, intimidation, assault, violence 5. EMS safety requires treating hate crimes as dangerous situations and involving law enforcement early. J. Legal Considerations 1. Abuse and assault are crimes. 2. You have a responsibility for reporting suspected cases, accurately documenting your findings, and learning about available resources in your area. 3. Remember that evidence must be maintained. 5 XX. Summary A. You will likely experience an abuse case during your paramedic career. B. Remember that you have a duty to report abuse situations, whether or not you transport the patient. C. It is important to recognize the significant physical and emotional assessment findings, as well as the characteristics of victims and assailants, as you may be the only chance a victim has of being saved from further abuse. 5 XXI. Case Study Class Activities Discuss the case with students now that they are familiar with the chapter.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. Chapter 6 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 XXII. You Make the Call Class Activities Read and discuss the call and questions as a group. 5 XXIII. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 1 Detailed Lesson Plan Chapter 7 The Challenged Patient 100–120 Minutes Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture. 5 II. Introduction A. During your EMS career, you will encounter patients who live with a variety of special needs. B. Treating the “challenged” patient involves understanding and recognizing the special condition of your patient and making any needed accommodations. 25 III. Physical Challenges A. Physical impairment – condition that limits the use of one or more parts of the body B. Important to quickly recognize impairment and adjust assessment accordingly C. Hearing Impairments 1. Decrease or loss in ability to distinguish or hear sounds 2. Inability to hear is called deafness (complete or partial); can be present at birth or result from aging, accident, or illness. 3. Two types of deafness are conductive deafness and sensorineural a. Conductive – any condition that prevents sound waves from being transmitted from external ear to middle/inner ear; can be temporary or permanent (otitis media, earwax, swimmer’s ear, obstructions, etc.) b. Sensorineural deafness – inability of nerve impulses to reach auditory center of brain due to damage to inner ear or brain; usually Teaching Tips Pull up common words used in EMS that are transferred to American Sign Language. Discussion Topics Discuss with students ways in which they can avoid injuring themselves and their patients when providing care for individuals who are obese. Discuss with students the different medical tests and assessments that may need to be altered in an obese patient (e.g., electrocardiogram [ECG] placement, blood pressure cuff size, lung sounds, etc.). MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 2 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes a permanent condition (congenital defect, birth injury, illness, tumor, concussion, injury, loud noises, presbycusis) 4. Recognition of deafness – repeat of questions, misunderstand answers, respond inappropriately, hearing aids, poor diction, use of hands for gesturing or sign language 5. Accommodations for deaf patients: Identify yourself, face patient, speak in normal voice or use low-pitched voice directly into ear, turn off background noises, offer pen and paper, use interpreter for sign language, notify hospital. D. Visual Impairments 1. Important to note whether visual impairment is a permanent disability or new symptom 2. Many causes for visual impairments, such as injury, disease, congenital conditions, infection, and degeneration of retina, optic nerve, or nerve pathway 3. Injury – Penetrating injuries can cause enucleation (removal of eyeball); chemical/thermal burns can damage cornea and lead to permanent vision loss if not treated quickly. 4. Disease – Glaucoma increases intraocular pressure on optic nerve, leading to loss of peripheral vision and blindness if not treated (primary and secondary glaucoma); diabetic retinopathy results from diabetes, which causes disorders in blood vessels leading to retina, leading to slow loss of vision and blindness. 5. Congenital and degenerative disorders – cerebral palsy, premature birth, aging, cytomegalovirus (seen in AIDS) 6. Recognizing and accommodating visual Impairments – Identify yourself as you approach, describe everything you are doing, do not pet service dog and ask permission of patient to touch animal, have person take your arm for guidance. E. Speech Impairments 1. Difficulty with communication can hinder treatment and information 2. Types of speech impairments include language, articulation, voice production, and fluency disorders. 3. Language disorders – Impaired ability to understand spoken or written word; loss of ability to communicate in speech, writing, or signs is known Discuss with students the different speech impairments listed. Have students list various medical conditions that can present with speech difficulties. Discuss with students patients with halo devices. Have students discuss various ways they may have to make accommodations for transport. Critical Thinking Questions What are ways in which you can prevent hearing loss as a result of your job? Class Activities Have a student use ear plugs to limit hearing and wear a blindfold to limit sight. Have another student interview the first student and perform an assessment, using various communication techniques. Have students practice their lifting techniques using a stretcher, stair chair, Reeves, and other equipment. Blindfold a student and have another student practice how to guide a patient with sight limitations. Points to Emphasize Emphasize to students that patients who have visual, hearing, or speech limitations usually have normal intelligence. Stress how the other senses are usually heightened in these patients.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 3 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes as aphasia. a. Sensory aphasia – can no longer understand spoken word b. Motor aphasia – can no longer use the symbols of speech; will understand what you are saying, but cannot clearly articulate response c. Global aphasia – patient has both sensory and motor aphasia; cannot understand nor respond 4. Articulation disorders – dysarthria; affect the way a person’s speech is heard by others 5. Voice production disorders – quality of person’s voice is affected (hoarseness, harshness, inappropriate pitch, abnormal nasal resonance, total loss of speech) 6. Fluency disorders – stuttering 7. Accommodations for speech impairments: Do not assume that patient lacks intelligence, may be impossible to complete a thorough interview, do not rush patient or predict answers, use questions that require short and direct answers, look directly at patient, ask to repeat if you do not understand, have patient write information. F. Obesity 1. More than 40% of people in U.S. are considered obese. 2. Obesity more difficult for EMS in regard to lifting; exacerbation of medical problems from excess weight; leads to hypertension (HTN), heart disease, diabetes, joint and muscle problems 3. Etiologies a. Occurs when person has an abnormal amount of body fat and weight is 20–30% heavier than normal b. Occurs from caloric intake greater that amount of calories needed, genetic factors, low basal metabolic rate 4. Accommodations for obese patients: medical history, equipment accommodations due to excess adipose tissue (electrocardiogram [ECG] placement, large blood pressure [BP] cuff, lung sounds), lifting assistance, special weight-bearing stretchers G. Paralysis 1. Paraplegic (paralyzed from waist down) or quadriplegic (paralysis of all four extremities) Knowledge Application Create a definition list of the various impairments. For homework, have students list the meaning of each impairment listed.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 4 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 2. May be ventilator dependent if C3–C5 injury (keep suction close) 3. Halo traction may be in place if injury recent; call physician on how to assist if patient unable to inform. 4. May have colostomy appliance 15 IV. Mental Challenges and Emotional Impairments A. Present a special challenge to EMS providers B. Developmental Disabilities 1. Individuals with impaired or insufficient development of brain who are unable to learn at usual rate 2. May live in residential settings, on their own, with family, or in group homes 3. Causes include genetics, brain injury, or traumatic event C. Accommodations for Developmental Disabilities 1. May be difficult to recognize until you begin interview 2. Treat patient as you would anyone else 3. May need to obtain history and chief complaint from others if patient has severe disability 4. Establish trust with patient. 5. Keep primary caregiver with you at all times if disability is severe so that patient is comfortable and you can gather information. D. Down Syndrome 1. Extra chromosome (chromosome 21 or 22) 2. Incident increases with increased age of mother. 3. Down syndrome presents with recognizable features: a. Eyes sloped at outer corners, folds of skin on side of nose that cover inner corner of eyes, small face and facial features b. Large and protruding tongue, flattening of back of head, short and broad hands c. Mild to moderate developmental disabilities; may have heart defects, intestinal defects, and chronic lung problems; and can develop cataracts, blindness, and Alzheimer’s at an early age Discussion Topics Discuss with students the characteristics of Down syndrome and fetal alcohol syndrome (FAS), along with typical medical conditions they may expect to respond to with these patients. Class Activities Have a representative from your local board of developmental disabilities come in to discuss with students the different developmental disabilities.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 5 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 4. Remember to consider the level of developmental delay during assessment and transport. E. Fetal Alcohol Syndrome (FAS) 1. Preventable disorder caused by excessive alcohol consumption during pregnancy 2. Characteristics of FAS children include: a. Small head with multiple facial abnormalities, small eyes with short slits, wide and flat nose bridge b. Lack of groove between nose and lip, small jaw 3. Often exhibit delayed physical growth, mental disabilities, and hyperactivity 35 V. Pathological Challenges A. Patients with chronic conditions will be encountered by EMS, with interventions and transports possibly being higher than average. B. Arthritis 1. Three common types include juvenile (before age 16), rheumatoid (autoimmune), osteoarthritis (degenerative) 2. Causes painful swelling and irritation of joints, joint stiffness, and limited range of motion; some smaller joints may become deformed 3. Treatment includes: aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids; some treatment may be for side effects of medications (upset stomach, vomiting, hyperglycemia); transport in position of comfort C. Cancer 1. Blanket term for many diseases that have a common ground of abnormal growth of cells in normal tissue; site of origin determines type of cancer; carcinoma – starts in epithelial tissue; sarcoma – starts in connective tissue 2. Signs of cancer may be difficult to see, although signs of cancer treatment may appear, such as hair loss, loss of appetite, weight loss, radiation tattoos, removal of tissue. 3. Treatment includes reduce exposure to infection because patient may be neutropenic (low levels of neutrophils), keep mask on patient, use sterile technique if you must start IV. D. Cerebral Palsy Teaching Tips Using pictures, go over polio with students, including the use of iron lungs. Critical Thinking Questions What medical procedures could increase the risk of infection in a patient undergoing chemotherapy? Class Activities Create scenarios for each common chronic condition listed. Focus on signs and symptoms, and have students perform complete assessments, including treatment options. (This should be done over several lab sessions, as it can be time consuming.) Hot glue tongue depressors into the fingers of a pair of gloves. Have students wear these gloves and attempt to pick up objects, button a coat, tie a shoe, and write with a pen (arthritis example).©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 6 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Group of disorders caused by damage to cerebrum in utero or trauma during birth (any event that leads to hypoxia in the fetus) 2. Causes include premature birth, brain damage from difficult delivery, encephalitis, meningitis, head injury 3. Patient have difficulty controlling motor functions, spasticity of muscles, may affect one or more limbs or entire body; some patients may have below-normal intellectual capacity, seizures; some patients highly intelligent 4. Three types of cerebral palsy: a. Spastic – most common form, muscles in state of permanent stiffness and contracture b. Athetosis – involuntary writhing movement c. Ataxia – rarest form, problems with coordination of gait and balance 5. Treatment includes: do not assume patient cannot communicate with you, special devices may be used for mobility, make accommodations in transporting to prevent further injury. E. Cystic Fibrosis (Mucoviscidosis) 1. Inherited disorder that involves exocrine glands, primarily in lungs and digestive system; causes thick mucus to form in lungs, obstructing bronchioles and collapsing alveoli; also causes blockages in the pancreas, leading to malnutrition. 2. History includes high concentration of chlorine in sweat (sweat test), lung infections, clay-colored stools, clubbing of fingers/toes 3. Medical advances have extended life of cystic fibrosis patient into 30s 4. Treatment includes: remember developmental stage of patient, comfort, O2, suctioning. F. Multiple Sclerosis 1. Disorder of central nervous system (CNS) that usually strikes between ages 20and 40, affecting women more than men 2. Cause unknown, considered autoimmune 3. Characteristics include inflammation of myelin sheaths surrounding nerves, blocking nerve impulses to affected areas. 4. Slow onset, with slight change in strength of muscle, numbness/tingling, increasingly tired, unsteady gait, slurred speech, eye problems 5. Initial signs usually temporary, with return more frequent and lasting Make a mold of a kyphotic back using plaster of Paris. Insert this mold into a vest jacket. Have students immobilize each other wearing this vest (demonstrates the importance of padding when immobilizing patients). Have a nurse who specializes in special needs patients come in to discuss the different emergencies seen by EMS. Knowledge Application Create a chart that lists each common chronic condition listed. For homework, have students list signs and symptoms, definitions, and treatment.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 7 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes longer; symptoms become more permanent, leading to weakness or paralysis. 6. Treatment includes supportive care, O2, comfort, bring assistive devices with you. G. Muscular Dystrophy (MD) 1. Group of hereditary disorders characterized by progressive weakness and wasting of muscle tissue 2. Most common form is Duchenne MD, which affects boys between ages 3 and 6. 3. Progressive muscle weakness that leads to paralysis, affecting heart, and causing death at an early age 4. Other forms of MD are classified by age and muscles affected. 5. Treatment includes complete history, respiratory support, comfort. H. Poliomyelitis 1. Communicable disease that affects gray matter of brain and spinal cord 2. Highly contagious, but immunization makes polio very rare in developed nations. 3. People born before polio vaccination may be affected. 4. Characteristics: enters through gastrointestinal (GI) tract, circulates, enters bloodstream, is carried to CNS, and alters nerve cells; paralytic polio causes asymmetrical muscle weakness and permanent paralysis 5. Signs include permanent paralysis of affected limb, use of assistive device, muscle atrophy, respiratory paralysis with tracheostomies and ventilators. 6. Post-polio syndrome develops in patients who suffered from polio more than 30 years ago; a condition that results from long-term weakness in affected nerves; patients tire easily, develop intolerance to cold. 7. Treatment includes supportive care. I. Previous Head Injury 1. May be difficult to recognize initially; usually apparent once patient begins to speak 2. Signs include symptoms similar to a stroke without the hemiparalysis, aphasia, slurred speech, loss of vision or hearing, learning disability, short-term memory loss. 3. Treatment includes history, slow physical assessment, comfort.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 8 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes J. Spina Bifida 1. Congenital abnormality that falls under neural tube defects; defect in closure of backbone and spinal cord 2. Symptoms include depends on what part of spinal cord is protruding; may have paralysis of lower extremities, lack of bowel or bladder control; possible collection of fluid in brain, with shunt present. 3. Treatment includes: many spina bifida patients have latex allergy; take any assistive devices patient uses. K. Myasthenia Gravis 1. Autoimmune disease characterized by chronic weakness of voluntary muscles and progressive fatigue 2. Results from problem with neurotransmitters, causing blockage of nerve signals to muscles; commonly occurs in women age 20–50. 3. Signs and symptoms include lack of energy, especially at night; eyelid drooping; difficulty chewing/swallowing; double vision; severe cases may include respiratory muscle paralysis. 4. Treatment includes supportive care, accommodation, assisted ventilation if in respiratory arrest.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 9 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 10 VI. Other Challenges A. Special situations that will affect quality of patient service provided B. Culturally Diverse Patients 1. Ethically required to care for all patients, regardless of race, gender, religion, ethnicity, or living condition 2. Remember that your patient who has decision-making capabilities has a right to self-determination. 3. Accommodating cultural diversity requires patience and ingenuity C. Terminally Ill Patients 1. Emotional challenge 2. Family may call ambulance at last minute, new condition may arise that can be treated, or medication may change. D. Patients with Communicable Diseases 1. Always withhold personal judgment. 2. Take Standard Precautions as you would with any patient. E. Patients with Financial Challenges 1. Part of your job is to inform patients where and how they can obtain medical care, regardless of financial situation. 2. Always treat the patient, not the financial condition of the patient. Discussion Topics Discuss with students different cultures and medical beliefs. Discuss with students the various resources available in your area for patients with no health insurance. Critical Thinking Questions Why might a patient with a communicable disease feel offended when you use universal precautions? Class Activities Create a scenario in which a student has to provide care to an individual from a culture that does not accept blood products, male providers to female patients, and so forth. Have students role-play their responses, and discuss how they can modify assessment and care to accommodate patients. 5 VII. Summary A. More and more patients with special challenges are living at home rather than in medical facilities. B. EMS may be summoned for complications of chronic illnesses. C. Keeping patients’ best interests in mind includes physical, emotional, financial, and spiritual aspects. D. It is your responsibility to treat all patients with respect and dignity. 5 VIII.Case Study Class Activities Discuss the case with students now that they are familiar with the chapter.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed.. 10 Chapter 7 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 IX. You Make the Call Class Activities Read and discuss the call and questions as a group. 5 X. Review Questions Class Activities Pass out review questions before the lesson starts. Have students answer them. Go over the questions again after the lecture to assess students’ understanding of the information.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 1 Detailed Lesson Plan Chapter 8 Acute Interventions for the Chronic Care Patient 110–130 Minutes Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 5 I. Case Study Teaching Tips Have a student read the scenario. Tell students that the case will be reviewed after the lecture. 5 II. Introduction A. Major trend in modern medicine is to place patients back in their homes as soon as possible, which has caused a huge increase in home health care needs. B. More and more patients will receive treatment in out-of-hospital setting. 35 III. Epidemiology of Home Care A. Growth of home care includes enactment of Medicare; growth of health maintenance organizations (HMOs); improved medical technology, improved recovery rate, and lower costs with home care B. Implications of EMS include assumption of greater responsibility for treatment and ALS intervention. C. In home care setting, numerous medical devices may be encountered. D. Must be familiar with basic functions of medical devices to be able to provide patient care. E. Patients Receiving Home Care 1. Almost 75% of home care patients are > 65 years old, almost two-thirds female and receive acute and chronic care from paid providers and family members/volunteers. 2. Average assistance is 4 hours per day, 7 days a week. 3. Government reduction of home health care has put tremendous strain on EMS and is partially responsible for hospital emergency department Discussion Topics With students, discuss the benefits and disadvantages of continuing care at home. Attempt to obtain an estimated hospital bill for a 5-day stay for congestive heart failure (CHF). Compare this bill to a bill for the same length of time for a patient with the same condition who is being cared for at home. Critical Thinking Questions What do you think the stress risks are for family members who care for other family members at home? What are ways to control the stress? MASTER TEACHING NOTES Teaching Tips Discussion Topics Critical Thinking Questions Class Activities Points to Emphasize Knowledge Application©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 2 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes (ED) overcrowding. F. ALS Response to Home Care Patients 1. Some situations that may require treatment include equipment failure, unexpected complication, absence of caregiver, need for transport, inability to operate device, and so forth. 2. Primary role of paramedic is to identify and treat any life-threatening problems. 3. Use home care providers as important source of information, as they are familiar with patient condition. G. Typical Response 1. Home care patient usually in more fragile medical state 2. Monitor patient carefully, and be ready to intervene. 3. Typical responses include: a. Airway complications – always utmost concern; problems include inadequate pulmonary output, alveolar ventilation, and alveolar oxygenation b. Respiratory failure – most common includes: emphysema, bronchitis, asthma, cystic fibrosis, congestive heart failure (CHF), pulmonary embolus, sleep apnea, Guillain-Barré syndrome, myasthenia gravis c. Cardiac decompensation – true medical emergency that can lead to life-threatening shock; patient at risk if cardiac demand more than cardiac ability; causes include CHF, acute myocardial infarction (AMI), hypertrophy, calcification of conduction system, heart transplant, sepsis d. Alterations in peripheral circulation – limited mobility causes entire circulatory system to be weaker and less effective; as muscle tone decreases, so does flow of blood, which can lead to increased risk of infection and gangrene e. Altered mental status – subtle or obvious change in mental status; always suspect other causes in addition to exacerbation of condition; risks include hypoxia, hypotension, sepsis, altered electrolytes, hypoglycemia, Alzheimer’s, tumor in brain, overdose, stroke f. Gastrointestinal (GI)/genitourinary (GU) crisis – often revolves What role does the caregiver play in your care? Do you think that it is to the patient’s advantage to include the caregiver in decisions? Why or why not? Class Activities Obtain equipment and/or pictures of equipment that is commonly found in the home (e.g., oxygen concentrators, ventilators, continuous positive airway pressure [CPAP], apnea monitors, etc.). With students, review the uses and common equipment failures of each. Points to Emphasis Stress to students that these patients’ immune systems may already be compromised, due to condition and medication. Infection control is indicated with all patient care. Knowledge Application Have students create a chart that lists the typical emergencies EMS may respond to, and what the causes may be.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 3 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes around misplaced or removed catheter; inability to eat or urinate can compromise an already weakened patient g. Infections/septic complications – always maintain high suspicion of infection, due to decreased immune response, poor general health, specific disease; be alert for infections involving indwelling devices h. Patients with decreased sensorium are at risk for infection due to inability to feel area; general signs of infection include: redness or swelling at site, purulent discharge, warm skin at site, fever; sepsis signs include: redness, fever, altered mental status, poor skin turgor or color, signs of shock, vomiting, diarrhea i. Equipment failure – power may go out, resulting in machine not functioning; machine may break; examples include ventilators, O2 delivery systems, apnea monitors, home dialysis machines j. Other medical disorders and home care patients: brain or spinal trauma, arthritis, psychological disorders, cancers, hepatitis, AIDS, transplants, and so forth H. Commonly Found Medical Devices 1. If unfamiliar with a patient’s medical device, ask questions about its usage; do not endanger the patient by pretending to know the equipment if you don’t. 2. Glucometers, IV infusions and indwelling IVs, nebulizers, aerosol medication administrators, shunts, fistulas, venous grafts, O2 concentrators, O2 tanks, liquid oxygen systems, O2 masks, tracheostomies, home ventilators, G-tubes, colostomies, urostomies, surgical drains, apnea monitors, cardiac monitors, pulse oximetry, wheelchairs, canes, walkers I. Intervention by a Home Health Care Practitioner or Physician 1. Usually require acute intervention for problems such as inadequate respiratory support, acute respiratory events, cardiac events, sepsis, GI/GU crisis 2. Determine whether another health care professional was present before your arrival and, if so, what instructions were conveyed 3. Hospice patients have special psychological needs due to situation. 4. Be alert for pharmacologic emergencies. J. Injury Control and Prevention©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 4 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 1. Most effective intervention is prevention 2. Ten steps to injury prevention: a. Prevent creation of hazard. b. Reduce amount of hazard. c. Prevent release of existing hazard. d. Modify rate of distribution of hazard. e. Separate hazard and protect from time and space. f. Separate hazard and protect by barrier. g. Modify qualities of hazard. h. Make protection resistant to hazard. i. Counter damage already done. j. Stabilize and repair/rehabilitate damage. 20 IV. General System Pathophysiology, Assessment, and Management A. Management 1. Becoming familiar with the pathophysiology of the particular diseases commonly found in the home care setting will allow for a more confident assessment 2. Emotional needs of patients and caregivers can affect patent condition 3. Sensitivity must be expressed, which will allow an efficient assessment B. Assessment 1. Same steps as with any other patient 2. Modify your assessment to look for unique conditions that may be observed in a home care patient. C. Scene Size-Up 1. Look for any equipment alerting you to chronic problems (e.g., wheelchair ramp, O2 equipment, sharps container, hospital bed). 2. Make personal contact with all on scene. 3. Be aware of special hazards with infectious wastes, medical supplies, and equipment. 4. Observe patient environment (patient milieu) for cleanliness and safety. D. Primary and Secondary Assessment 1. ABCs, existing problem versus new problem, treat patient as you see him, vital signs 2. Mental status evaluation may include caregivers and or family members; secondary assessment may show treatable cause if problem. Discussion Topics Using pictures or PowerPoint, show slides of various medical equipment, and discuss with students what condition the patient may have that necessitates the particular piece of equipment. Critical Thinking Questions Would it be poor patient care to transport a patient in his own equipped vehicle if there are no issues with the ABCs? Class Activities Create a scenario with a patient who suffers from a chronic illness. Make the patient complaint acute and not pertaining to chronic illness. Review the scenario with students, focusing on the ABCs.©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 5 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes 3. Inquire about do not resuscitate (DNR) orders. E. Transport and Management Treatment Plan 1. Replacement of home care treatment with ALS 2. May have to support mechanisms on ambulance. 3. Use caregivers during transport to aid in care. 40 V. Specific Acute Home Health Situation A. Respiratory Disorders 1. Account for > 600,000 patients 2. Devices used include O2 equipment, suctioning, aerosol and nebulizers, incentive spirometers, home ventilators, tracheostomy tubes and collar. 3. Chronic diseases requiring home respiratory support: a. Chronic obstructive pulmonary disease (COPD), bronchitis and emphysema, asthma, congestive heart failure (CHF), cystic fibrosis, bronchopulmonary dysplasia, neuromuscular degenerative diseases, muscular dystrophy, Guillain-Barré syndrome, myasthenia gravis, sleep apnea, patients awaiting lung transplants 4. Medical therapy found in the home setting: a. Home oxygen therapy, artificial airways/tracheostomies 5. Management a. If EMS has been called, it usually means that the caregiver and/or patient has not been able to solve the problem. b. Ensure that ventilations are adequate. c. Check all oxygen equipment for loose connections or tubing, and check patient for any obstructions. d. Intubation of stoma may be necessary. 6. Home ventilation a. Positive and negative pressure ventilators may be encountered. b. Common reasons for ventilator include decreased respiratory drive, (spinal cord injury), ventilator muscle weakness (muscular dystrophy, polio, myasthenia gravis, Guillain-Barré syndrome), obstructive pulmonary disorders (COPD, sleep apnea, cystic fibrosis, bronchopulmonary dysplasia), other disorders (pediatric sleep apnea, chest wall deformities). c. Positive pressure ventilators push air into lungs through face mask, Teaching Tips Using pictures or equipment, go over vascular access devices (VADs), urinary and gastrointestinal (GI) catheters, and feeding tubes and their various uses and complications. Discussion Topics Discuss with students the common medications used by the home health care patient. Critical Thinking Questions When would using a patient’s VAD be beneficial? What do you think the risks might be? Class Activities Have students practice tracheal suctioning, removal and replacement, aerosols, CPAP, bilevel positive airway pressure (BiPAP), and bag-valve mask (BVM) through a stoma techniques during skills lab, along with any other special equipment indicated in your protocol. When practicing suctioning, have students practice going through a stoma and the correct measurement of tubing, along with©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 6 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes nasal mask, or tracheostomy; features include variations in tidal volume, respiratory rate, flow rate, and pressure. d. Negative pressure ventilators: with expansion, pull on chest, causing it to expand and allowing air to flow into lungs, mimicking normal breathing process; iron lung, poncho-wrap are examples, commonly used at night. e. Positive end-expiratory pressure (PEEP), continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP): add pressure at various times in respiratory cycle; may be used full-time or part-time; danger of pneumothorax exists due to increased pulmonary pressure f. PEEP: used to keep alveoli from collapsing; provides back pressure at end of expiration; can be used in premature newborns with insufficient surfactant, washout from acute pulmonary edema, acute respiratory distress syndrome (ARDS), drowning, COPD (pursed lips in a COPD patient is PEEP) g. CPAP: used to keep pharyngeal structures from collapsing at end of a breath; often used for sleep apnea (Idea of CPAP same as PEEP; just that CPAP is through a mask, and PEEP is through an endotracheal tube [ET] tube.) h. BiPAP: provides two levels of pressure, one on inspiration and one on expiration; used when higher levels of pressure are required 7. General management considerations a. Primary assessment includes ABCs, level of consciousness (LOC), breathing and circulatory distress, including equipment used by patient. B. Vascular Access Devices(VADs) 1. Used to provide any parenteral treatment on a long-term basis 2. Device depends on treatment and disease 3. Types of VADs a. Hickman, Broviac, Groshong catheters – single, double or triple lumen; inserted into any central vein in trunk of body, subclavian most common; external port that looks like typical IV port; external hub sutured to skin; highest risk of infection is first 2 weeks; care consists of keeping site clean and dry, along with anticoagulant insertion of normal saline to loosen secretions. Have students practice assembling CPAP and BiPAP devices. Create several scenarios using equipment that requires electricity. Focus your scenario on power failures and how students would provide care to patients when there is no electricity. Using an extension set, have students practice flushing a line, along with locking it off. Have a student sit in a wheelchair, hooked up to a nasal cannula and an oxygen cylinder. Have two other students attempt to pick the student up and transfer him or her to a stretcher. Discuss the difficulties and accommodations that must be made. Ask a home health nurse to speak to the class to discuss care and equipment, along with the role of EMS. Points to Emphasize Stress to students that if they do not know the equipment, they should ask. NEVER touch equipment you do not know. Knowledge Application Create a list of various home health care equipment; for homework, have students©2017 Pearson Education, Inc. Paramedic Care: Principles & Practice, Volume 5, 5th Ed. 7 Chapter 8 objectives can be found on the opening chapter page. These objectives, which form the basis of each chapter, were developed from the new Education Standards and Instructional Guidelines. Minutes Content Outline Master Teaching Notes therapy. b. Peripherally inserted central catheter (PICCs) – PICC lines, inserted into peripheral vein; allow for catheter to be inserted into central venous circulation; low complication rate due to insertion by radiology c. Surgically implanted medication delivery system – Port-A-Cath, Medi-Port; infusion port is implanted below skin and requires a specially shaped needle to access; usually found in upper chest; never access unless protocol allows. d. Dialysis shunts – used for patients undergoing hemodialysis to filter blood; AV shunt is a loop connecting an artery and vein, usually in distal arm; fistula connects an artery and a vein, creating an artificial blood vessel, usually found in upper extremity; both are surgically created and very delicate; avoid application of blood pressure and vascular access on extremity. 4. Anticoagulant therapy – used to flush device to prevent clot formation; patient’s natural clotting mechanism may be suppressed, leading to bleeding disorders. 5. VAD complication – most commonly result from obstructions; other complications include catheter kinking, catheter tip embolism, infection, hemorrhage. 6. Potential for air embolism – signs and symptoms include headache, shortness of breath (SOB) with clear lungs, hypoxia, chest pain, indications of myocardial infarction (MI), altered mental status. C. Cardiac Conditions 1. Conditions for home health patients include post-MI recovery, postcardiac surgery, heart transplant, CHF, hypertension, implanted pacemaker, atherosclerosis, congenital malformation. 2. Equipment may include O2, electrocardiogram (ECG), bedside monitor, halter monitor, defibrillator. D. GI/GU Disorders 1. Response may be ALS or a needs-based assessment. 2. Urinary tract devices a. Devices that support patients with urinary tract dysfunction b. External catheters – Texas catheter (condom catheter) list the different medical reasons a patient may require the equipment Show Less [Show More]
Last updated: 2 years ago
Preview 1 out of 468 pages
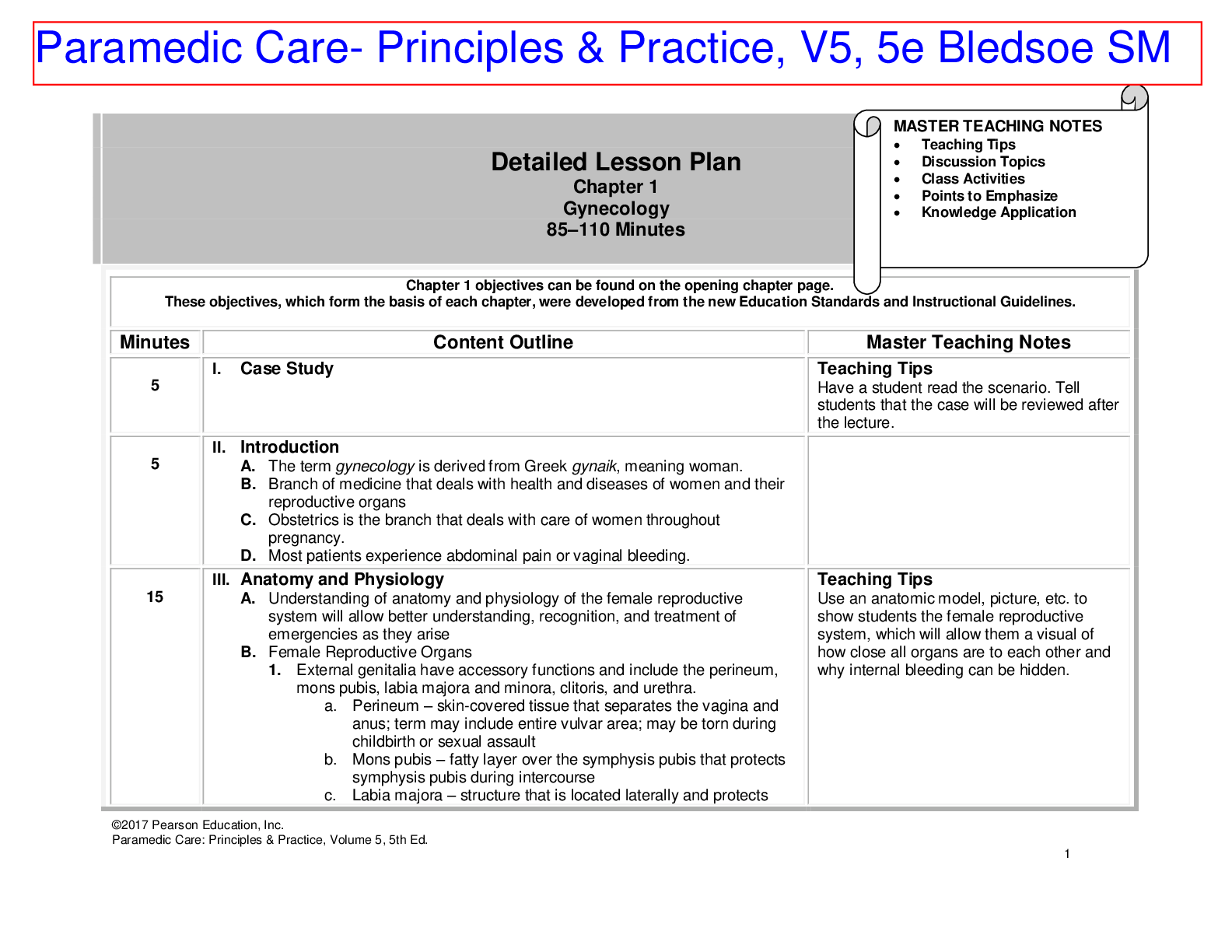
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 20, 2021
Number of pages
468
Written in
Additional information
This document has been written for:
Uploaded
Jul 20, 2021
Downloads
0
Views
201

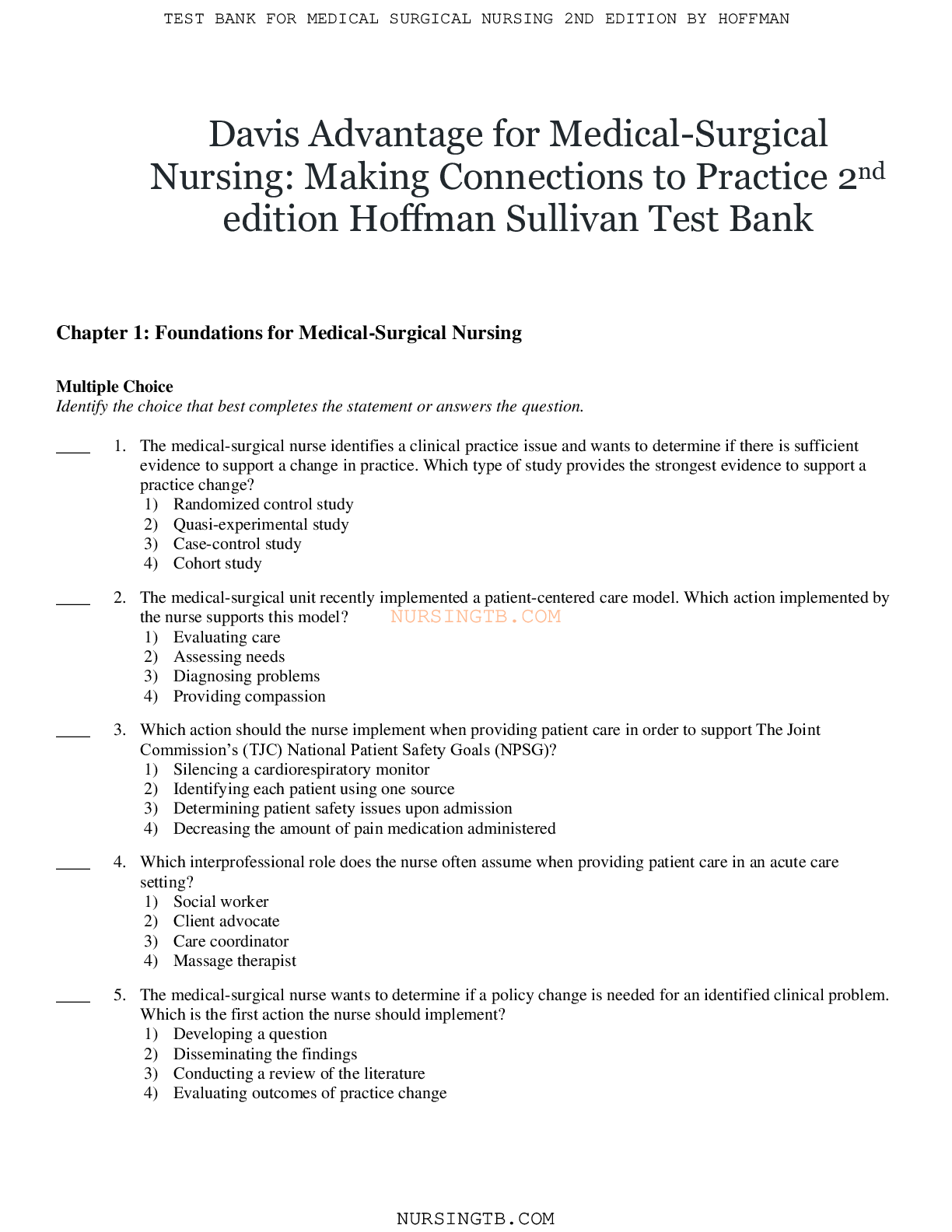
.png)
.png)
.png)



.png)



.png)
.png)
.png)
.png)
.png)

