Exit HESI Practice Questions with answers, Graded A+, 2022 update
Document Content and Description Below
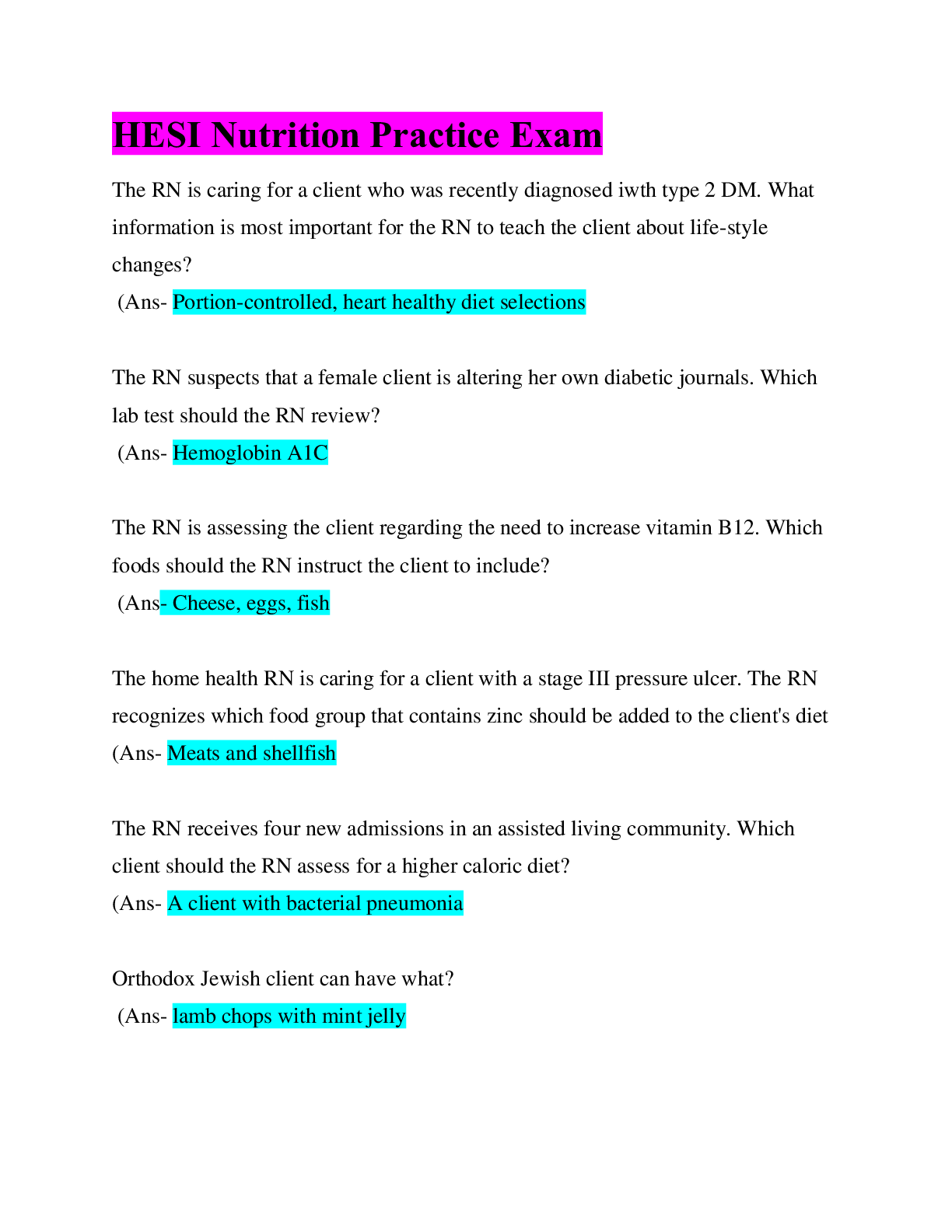
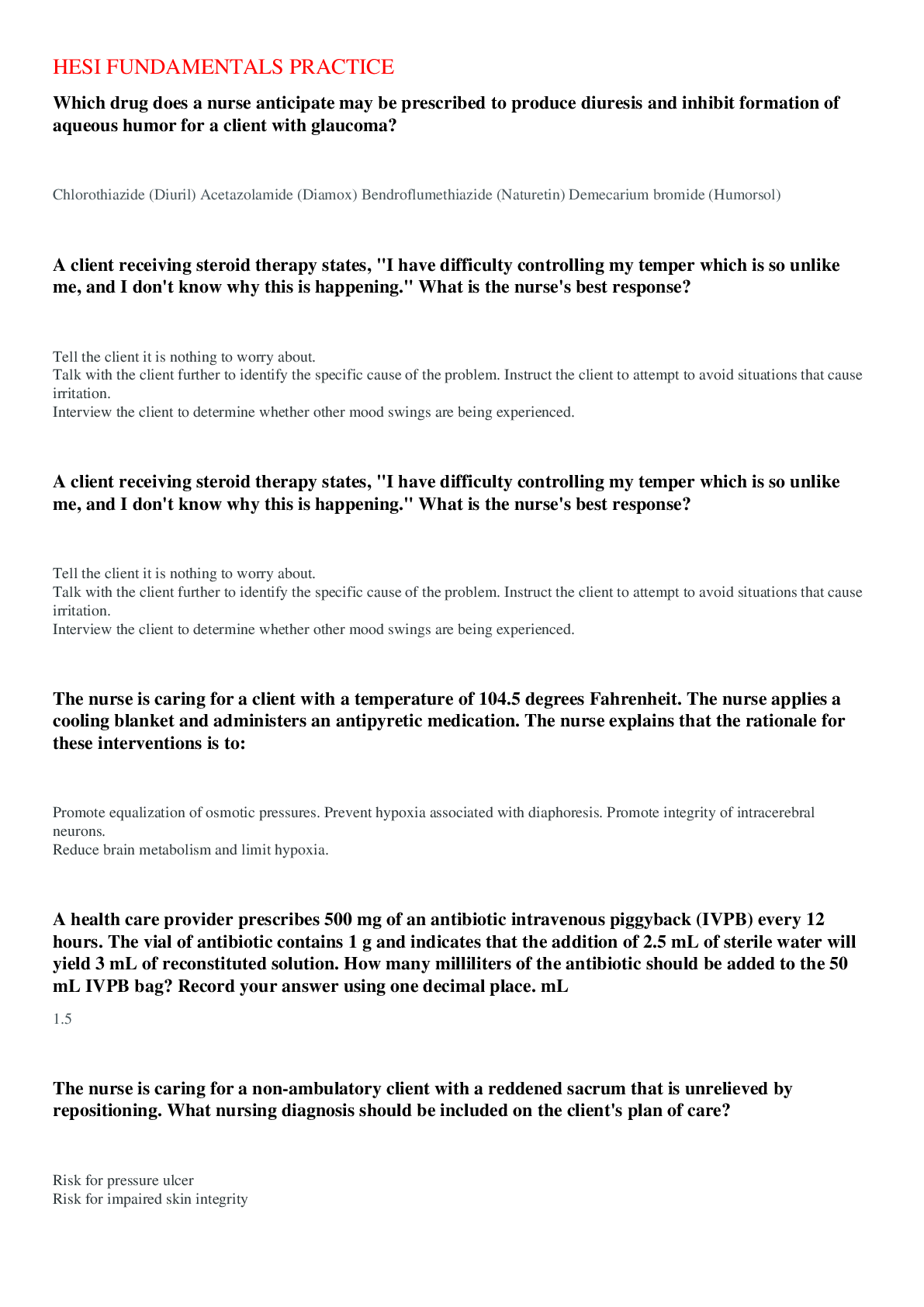
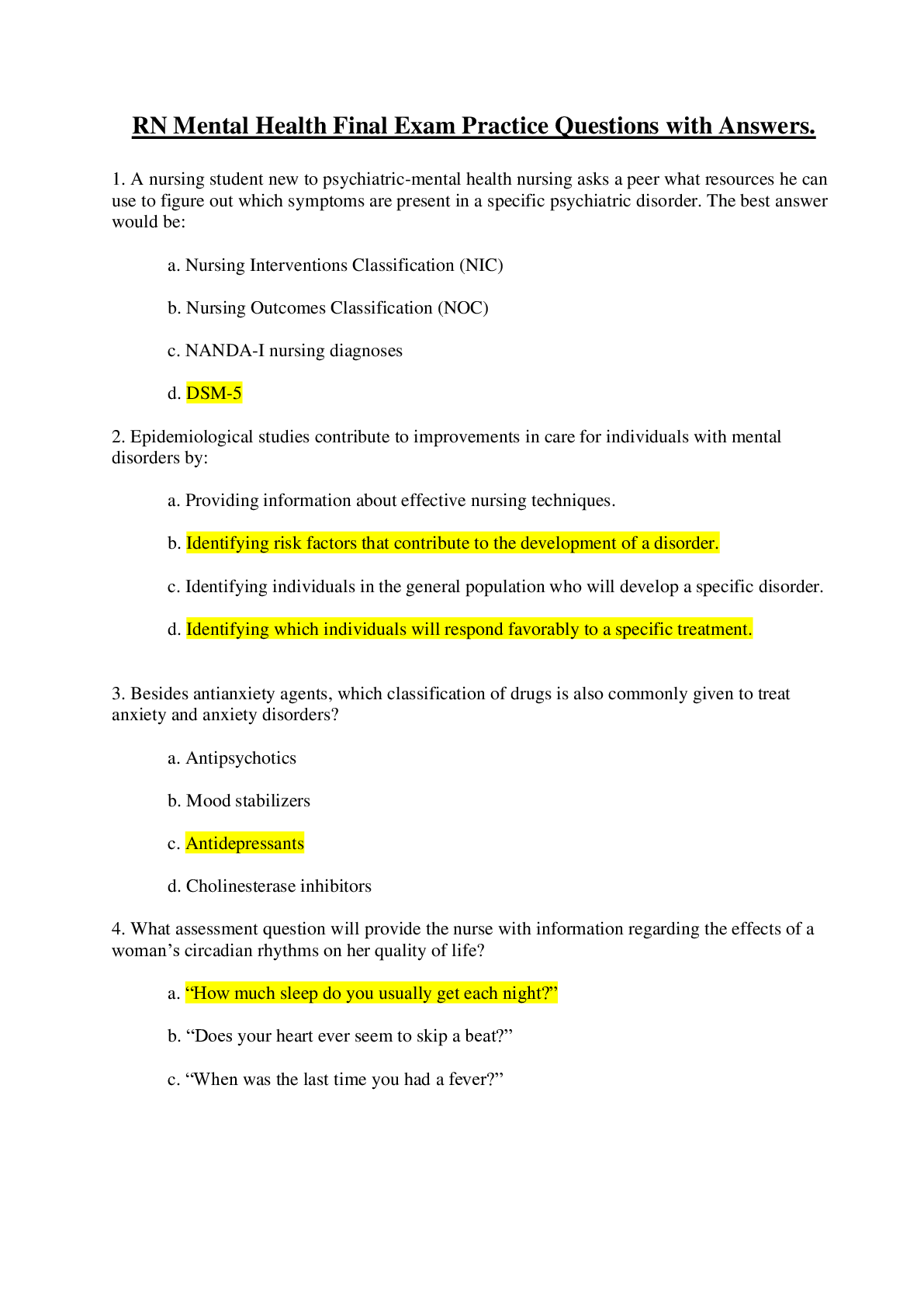
Exit HESI Practice Questions with answers, Graded A+, 2022 update A client presents at the ED complaining of a raspy voice, cold intolerance, and fatigue. Lab tests indicate an elevated TSH and l... ow T3 and T4 levels. After the client is admitted to the telemetry unit, which intervention is most important for the nurse to implement? A) Assess for presence of non-pitting edema. B) Administer the prescribed dose of levothyroxine. C) Offer additional blankets and a warm drink. D) Note client's most recent hemoglobin levels. - ✔✔B) Administer the prescribed dose of levothyroxine. Rationale: In the negative feedback mechanism of hypothyroidism, a low level of thyroid hormone stimulates TSH production by the hypothalamus and results in an elevated TSH level, but the thyroid gland does not respond with adequate production of T3 and T4 to regulate basal metabolic rate. These serum hormone levels indicate the need to administer supplementary thyroid hormone as soon as possible to avert possible myxedema coma. Non-pitting edema is seen in chronic hypothyroidism and assessment of the presence and location of the edema (A) is not a top priority. Providing warmth (C) is beneficial but of less priority than (B). Anemia is common in hypothyroidism, but (D) is of lower priority than initiating treatment to prevent myxedema coma. The nurse suspects that a client might be hemorrhaging internally. Which findings of an orthostatic tilt test are a most likely indication of a major bleed (> 1000 ml)? A) A decrease in the systolic BP of 10 mm Hg with a corresponding increase in the HR of 20. B) A decrease in the systolic BP of 10 mm Hg with a corresponding decrease in the HR of 20. C) A decrease in the systolic BP of 20 mm Hg with a corresponding decrease in the HR of 10. D) A decrease in the systolic BP of 20 mm Hg with a corresponding increase in the HR of 10. - ✔✔Ans: A) A decrease in the systolic BP of 10 mm Hg with a corresponding increase in the HR of 20. Rationale: The loss of circulatory volume results in a 10 mm Hg drop in the systolic pressure, while the HR increases by 20 % above normal as a compensatory response to the low pressure. When conducting diet teaching for a client who is on a postoperative full liquid diet, which foods should the nurse encourage the client to eat? SATA. A) Canned fruit cocktail B) Creamy peanut butter C) Vegetable juice D) Vanilla frozen yogurt E) Clear beef broth - ✔✔Ans: C, D, E A full liquid diet includes all liquids that are not clear such as vegetable juice and frozen yogurt, as well as clear liquids. Pieces of fruit as found in fruit cocktail and peanut butter are not considered liquids. A client is receiving ophthalmic drops preoperatively for a cataract extraction and asks the nurse why he is prescribed all these medications? SATA. A) One of the medications is used to anesthetize the corneal surface. B) The iris must be paralyzed during the surgery to prevent it from reacting to light. C) Medication is used to induce sleep during the procedure. D) Pupillary dilation is necessary to access the eye chamber for lens removal. E) These meds assist in obstructing the client's vision during the surgery. - ✔✔Ans: A, B, D Cataract surgery is accessed through the cornea using eyelid retractors while the client is awake. It is necessary to anesthetize the corneal surface (A), paralyze the ciliary body (B), and provide pupil dilation (D)(mydriasis) to facilitate access to the lens which ties behind the iris (posterior chamber of the anterior cavity). A sedative may be administered to reduce anxiety but it is not used to induce sleep. (C) Cloudy vision may be a side effect of these agents, but the client will still be able to see during the surgery (E). When assessing an IV site that is sued for fluid replacement and medication administration, the client complains of the tenderness when the arm is touched above the site. Which additional assessment warrants immediate intervention by the nurse? A) Sluggish blood return B) Client uses the arm cautiously C) Spot of dried blood at the insertion site D) Red streak tracking the vein - ✔✔Ans: D A red streak (D) indicates vein irritation and necessitates discontinuing the IV at the present site. A, B, and C are indications for relocating the IV site or other immediate intervention. A client with a liver abscess develops septic shock. A sepsis resuscitation bundle protocol is initiated and the client receives a bolus of IV fluids. Which parameter should the nurse monitor to assess effectiveness of the fluid bolus? A) Blood cultures. B) Oxygen saturation. C) White blood count. D) Mean arterial pressure (MAP). - ✔✔D) Mean arterial pressure (MAP) The cornerstone of initial sepsis resuscitation is fluid volume administration to restore and then maintain MAP of at least 65 mmHg. When attempting to establish risk reduction strategies in a community, the nurse notes that regional studies indicate a high number of persons with growth stunting and irreversible mental deficiencies (cretinism) caused by hypothyroidism. The nurse should seek funding to implement which screening measure? A)T4 levels in newborns. B) TSH levels in women over 45. C) T3 levels in school-aged children D) Iodine levels in all persons over 60. - ✔✔A) T4 levels in newborns. Screening for low T4 levels in newborns with follow-up treatment can reduce the risk for irreversible growth stunting and mental deficiencies caused by congenital hypothyroidism. For the past 24 hours, an antidiarrheal agent, diphenoxylate, has been administered to a bedridden, older client with infectious gastroenteritis. Which finding requires the nurse to take further action? A) Loss of appetite B) Serum K+ 4.0 mEq/L or mmol/L (SI) C) Loose, runny stools. D) Tented skin turgor. - ✔✔D) Tented skin turgor. Indicates dehydration, a serious complication following prolonged diarrhea that requires further intervention by the nurse. A male client with ulcerative colitis received an Rx for a corticosteroid last month but because of the S/E, he stopped taking the medications 6 days ago. Which finding warrants immediate intervention by the nurse? A) Fluid retention B) Hypotension and fever C) Anxiety and restlessness D) Increased blood glucose - ✔✔B) Hypotension and fever Sudden withdrawal from a corticosteroid can cause sudden decreased adrenal function resulting in low serum sodium, high serum potassium, and low blood pressure which can lead to shock and possible death. Hypotension and fever (B) are the first signs of precipitous withdrawal. Fluid retention (A), anxiety and restlessness (C), and glucose intolerance (D) are common S/E of taking corticosteroids. The nurse who working in the ED is obtaining evidence for a rape kit from a woman who reports that she was raped. Which intervention is most important for the nurse to implement? A) Do not allow client to shower until all evidence is obtained. B) Report incident to the university's security department. C) Listen attentively to the client's description of the event. D) Determine the client's personal reaction to the reported rape. - ✔✔A) Do not allow client to shower until all evidence is obtained. It is most important to gather evidence and a shower distorts such evidence. The client should not be allowed to shower until all the evidence is collected. The nurse is preparing to gavage feed a premature infant through an orogastric tube. During insertion of the tube, the infant's HR drops to 60 bpm. Which action could the nurse take? A) Continue the insertion since this is a typical response. B) Insert the feeding tube into the infant's nasal passage. C) Pause and monitor for a continued drop of the HR D) Postpone the feeding until the infant's vital signs are stable. - ✔✔C) Pause and monitor for a continued drop of HR. Insertion of an orogastric tube for gavage feedings often triggers vagus stimulation which can result in bradycardia. Pausing during insertion and monitoring (C) the infant's HR and color may be all that is necessary for the HR to return to normal. A client who has a tracheal stoma is c/o of mouth pain. While performing oral care, nurse determines that the client has mouth ulcers and that oral mucosa is irritated. The client also has halitosis. Which intervention should the nurse implement? A) Encourage frequent use of mouthwash. B) Apply viscous gel to ulcers during mouth care. C) Provide flavored oral swabs to use Q2H D) Rinse out mouth with a liquid germicide daily. - ✔✔B) Apply viscous gel to ulcers during mouth care. Mouth ulcers and irritation of the lining of the mucous membranes are very painful. An oral viscous gel such as a lidocaine anesthetic can be used to temporarily relieve the pain. (B) Routine mouth care is necessary but should not be done too frequently because it may cause further irritation of the mucous membranes. An adult male is admitted in a rehab center after 3 weeks in an acute care hospital. The client suffered a R sided brain injury that occurred as the result of a fall from a ladder. Which intervention should the nurse include in this client's plan of care? A) Maintain elastic stockings continuously. B) Apply a hand splint for finger extension. C) Monitor BP every 4 hours. D) Give antithrombolytic injections daily. - ✔✔B) Apply a hand splint for finger extension. The nurse is explaining the need to reduce salt intake for a client with primary HTN. What explanation should the nurse provide? A) high salt can damage the lining of the blood vessels. B) Too much salt can cause the kidneys to retain fluid. C) Excessive salt can cause blood vessels to constrict. D) Salt can cause inflammation inside the blood vessels. - ✔✔B) Too much salt can cause the kidneys to retain fluid. Excessive salt intake can contribute to primary HTN by causing renal salt retention which influences water retention that expands blood volume and pressure. A client with cirrhosis of the liver is admitted with complications related to end-stage liver disease. Which interventions should the nurse implement? SATA. A) Monitor abdominal girth. B) Increase oral fluid intake to 1,500 mL daily. C) Report serum albumin and globulin levels. D) Provide a diet low in phosphorus. E) Note signs of swelling and edema. - ✔✔Ans: A, C, E Ad adult male is admitted to the ED after falling from a ladder. While waiting to have a CT scan, he requests for stronger pain medication. Which intervention should the nurse implement? A) Request that the CT scan be done immediately. B) Review client's history for use of illicit drugs. C) Assess client's pupils for their reaction to light. D) Explain the reason for using only non-narcotics. - ✔✔D) Explain the reason for using only non-narcotics. The patient needs to understand that any pain medication that can mask declining neurological symptoms such as narcotics should be avoided. A client with eczema is experiencing severe pruritus. Which PRN prescriptions should the nurse administer? SATA. A) Topical corticosteroid B) Topical acobicide C) Topical alcohol rub D) Transdermal analgesic E) Oral antihistamine - ✔✔Ans: A, E Which patient requires most immediate attention by the nurse? A) Gunshot wound three hours ago with dark drainage of 2 cm noted on dressing. B) Mastectomy 2 days ago with 50 ml bloody drainage noted in the Jackson-Pratt drain. C) Collapsed lung after a fall 8 hours ago with 100 ml in the chest tube collection container. D) Abdominal perineal resection 2 days ago with no drainage on dressing who has fever and chills. - ✔✔D) Abdominal perineal resection 2 days ago with no drainage on dressing who has fever and chills. Risk for peritonitis and needs to be immediately assessed for other signs and symptoms for sepsis. In assessing an infant 10 hours after birth, the nurse notes that the infant is slightly cyanotic and has a large amount of mucus. Which interventions should the nurse implement first? A) Begin O2 at 2 L/min B) Insert a nasogastric tube. C) Suction the infant as needed. D) Assess the heart rate. - ✔✔C) Suction the infant as needed. To clear the airway, nurse should first suction the mucous. A 12 year-old boy who had an appendectomy two days ago is receiving 0.9% normal saline at 50 ml/hr. His urine specific gravity is 1.035. What action should the nurse implement? A) Evaluate postural blood pressure measurements. B) Obtain a specimen for urinalysis. C) Encourage popsicles and fluids of choice. D) Assess bowel sounds in all quadrants. - ✔✔C) Encourage popsicles and fluids of choice. Specific gravity of urine is a measurement of hydration status (NR 1.010 to 1.025) which is indicative of fluid volume deficit); when Sp Gr increases as urine become more concentrated. The nurse should continue the prescribed IV fluids and increase PO intake. The nurse is caring for a one-week-old infant who has a ventriculoperitoneal (VP) shunt that was placed 2 days after birth. Which findings are an indication of a postoperative complication? SATA. A) Poor feeding and vomiting. B) Leakage of CSF from the incisional site. C) Hyperactive bowel sounds. D) Abdominal distention. E) White blood count of 10,000/mm3. - ✔✔Ans: A, B, D are signs of postoperative complications. A couple who is trying to have a baby asks the nurse when they are most likely to conceive a child. The woman has a regular 36 day cycle and the first day of her LMP was on January 15. Which information should the nurse provide? A) Have intercourse every other morning because this is when sperm count is higher. B) Plan to have intercourse on February 7, as this is when ovulation should occur. C) Have intercourse every 3 days to ensure that ovulation and intercourse coincide. D) The woman should ovulate mid-cycle, so plan to have intercourse on February 3. - ✔✔B) Plan to have intercourse on February 7, as this is when ovulation should occur. Ovulation usually occurs 14 days before the first day of the menstrual cycle. The client's next menstrual period should begin on February 21 so ovulation should occur on February 7. A newborn infant is receiving positive pressure ventilation after delivery. Based on which assessment finding should the nurse initiate chest compressions? A) Apgar score of 7 B) Heart rate of 54 C) Central cyanosis D) Limp muscle tone - ✔✔Ans: B) Heart rate of 54 Chest compressions should be initiated when a newborn's heart rate is less than 60 bpm (B) despite the use of positive pressure ventilation. The Apgar score is obtained at 1 minutes and 5 minutes but a score of 7 is not the criterion used to determine neonatal response to ventilation. Which fetal heart pattern requires immediate nursing intervention? A) An FHR deceleration that mirrors the contraction. B) An increase in the FHR to 100 that quickly returns to baseline. C) An FHR deceleration that occurs at the same time of contraction. D) A decrease in the FHR that occurs after the peak of a contraction. - ✔✔D) A decrease in the FHR that occurs after the peak of contraction. A decreased FHR after the peak of contraction is an ominous sign and indicates fetal distress (hypoxia). A and C are describing the same contraction pattern and both are normal signs of fetal descent. B is a description of FHR acceleration which is normal. The nurse requests a meal tray for a client who follows Mormon beliefs and who is on a clear liquid diet following abdominal surgery. Which menu items should the nurse request for this client? SATA. A) hot chocolate B) apple juice C) chicken broth D) orange juice E) black coffee - ✔✔Ans: B, C Apple juice and chicken broth are included in a clear liquid diet and are consumed by Mormons. Black coffee (E) is included in a clear liquid diet, but caffeinated beverages are not consumed by Mormons. A nine-day old infant with congenital adrenal hyperplasia (CAH) develops dehydration and is admitted to the hospital for aldosterone replacement therapy. The HCP prescribes fludrocortisone acetate (Florinef) 0.05 mg PO daily. Which finding indicates the newborn is experiencing a therapeutic response? A) Resting blood pressure of 62/41 mmHg B) Plasma glucose 45 mg/dl C) Serum sodium 142 mEq/L D) Capillary refill is greater than 3 seconds. - ✔✔C) Serum sodium 142 mEq/L Infants with CAH produce inadequate cortisol and aldosterone that leads to dehydration and salt-losing crises which require urgent medical intervention. Aldosterone replacement therapy is prescribed to promote increased reabsorption of sodium and water int eh distal renal tubules, which should result in a normalization of serum sodium (134-146). A client with a cervical spinal cord injury has Crutchfield tongs and skeletal traction applied as a method. Which intervention is most important for the nurse? A) Provide daily care of tong insertion site using saline and antibiotic ointment. B) Modify the client's diet to prevent constipation. C) Encourage active ROM Q2-4 hours. D) Instruct the client to report any symptoms of upper extremity paresthesia. - ✔✔A) Provide daily care of tong insertion site using saline and antibiotic ointment. Crutchfield tongs, a skeletal traction device for cervical immobilization requires daily care of the surgically inserted tongs to minimize the risk of infection of the insertion sites and cranial bone. Daily cleansing with normal saline solution and antibiotic ointment applications minimize the bacterial colonization and helps to prevent infections. Following breakfast, the nurse is preparing to administer 0900 medications to clients on a medical floor. Which medications should the nurse hold until a later time? A) Loop diuretic furosemide (Lasix) for a client with a serum potassium level of 4.2 B) The mucosal barrier, sucralfate (Carafate) for a client diagnosed with PUD. C) The antiplatelet agent aspirin for a client discharged within the hour. D) The antifungal nystatin suspension for a client who has just brushed his teeth. - ✔✔B) The mucosal barrier, sucralfate (Carafate) for a client diagnosed with PUD. Carafate coasts the mucosal lining prior to eating a meal, so this med should be held until prior to the next meal. Since the potassium level is (A) within normal limits, there is no reason to hold the lasix. The nurse can safely administer (C). In (D), the client should rinse the mouth prior to administering nystatin swish and swallow but the medication does not need to be held. Which interventions should the nurse implement for a client with a superficial (first degree) burn? A) Spray an anesthetic agent over the burn every 3-4 hours. B) Position the burn victim in front of a cool fan to decrease discomfort. C) Apply ice packs for 30 minutes to lower surface temperature. D) Place wet cloths on the burned areas for short periods of time. - ✔✔D) Place wet cloths on the burned areas for short periods of time. Placing wet cloths on the burned areas for short periods of time (D) provides comfort and helps to relieve the pain of a first degree burn, which involves only the epidermal layer of the skin. (A and B) are not likely to provide pain relief. (C) Applying ice for 30 minutes is too long and can result in additional skin damage. The nurse is teaching a mother of a newborn with a cleft lip on how to bottle feed her baby using a Haberman feeder that has a valve to control the release of milk and a slit nipple opening. The nurse discusses placing the nipple's elongated lip to the back of the oral cavity. What instructions should the nurse provide the mother about feedings? A) Squeeze the nipple base to introduce milk into the mouth. B) Position the baby in the left lateral position after feeding. C) Alternate milk with water during the feeding. D) Hold the newborn in an upright position. - ✔✔D) Hold the newborn in an upright position. The mother should be instructed to hold the infant during feedings in a sitting or upright position to prevent aspiration. Impaired sucking is compensated by the use of special feeding appliances and nipples, such as Haberman feeder that prevents aspiration by adjusting the flow of milk according to the effort of the neonate. Squeezing the nipple base may introduce a value that is greater than the neonate can coordinate swallowing (A). The preferred position of an infant after feeding is on the right side (B) to facilitate stomach emptying. Suckling difficulty impedes the neonate's intake of adquate nutrient needed for weight gain, and water should be provided after the feeding (D) to cleanse the oral cavity and not fill up the neonate's stomach. A male client with terminal cancer is brought to the ED manifesting a Cheyenne Stokes respiratory pattern. The wife tells the nurse that her husband has an advanced directive that indicates "Do not resuscitate (DNR) status," but the documents are at home. When the client becomes apneic and pulseless, what action should the nurse take? A) Ask the wife if her husband's wishes ever changed. B) Call the HCP for a DNR prescription. C) Begin CPR. D) Determine if the family wants hospice care [Show More]
Last updated: 2 years ago
Preview 1 out of 50 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 27, 2022
Number of pages
50
Written in
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Aug 27, 2022
Downloads
0
Views
225