Medical Studies > QUESTIONS & ANSWERS > Certified Coding Associate (CCA) Exam Preparation 2022- with rationale (All)
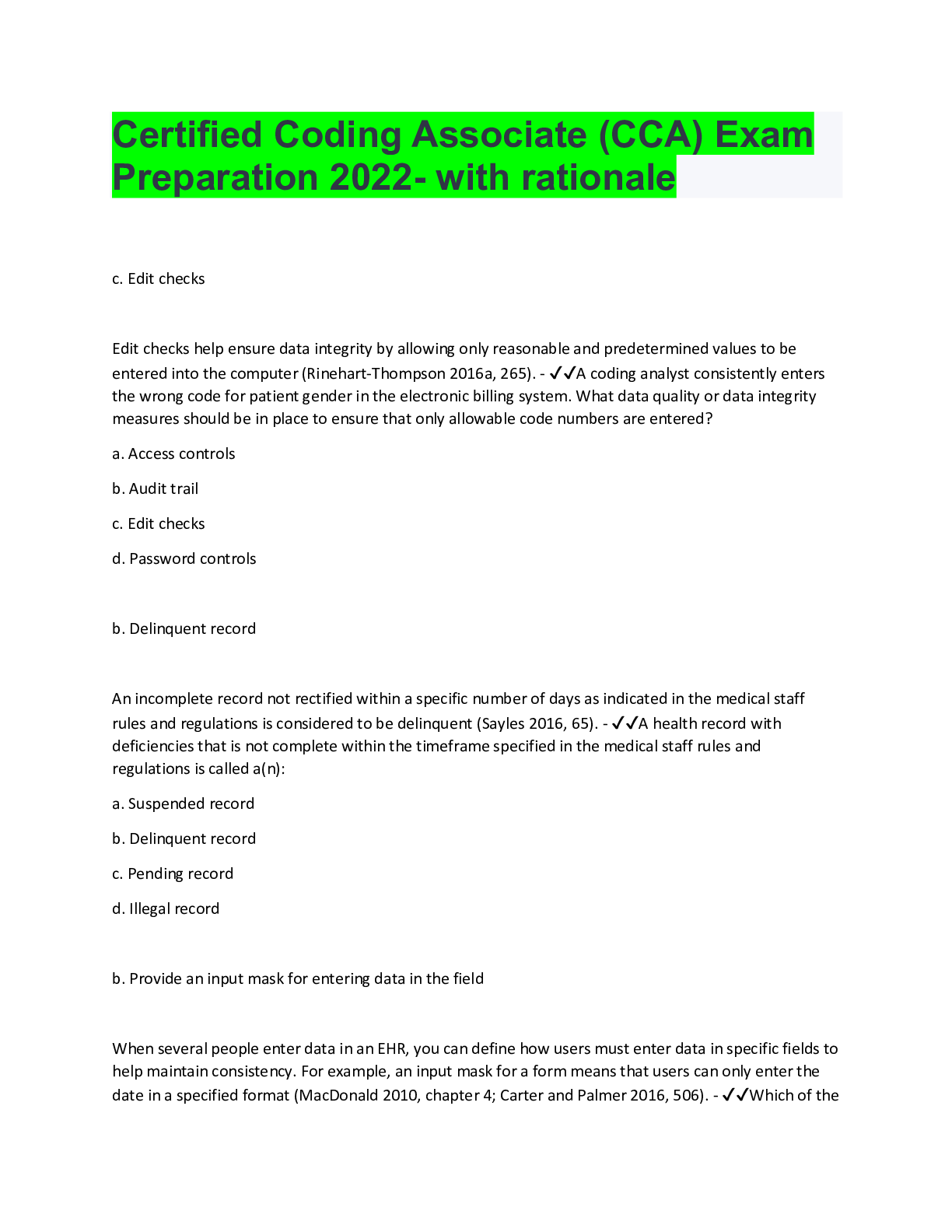
Certified Coding Associate (CCA) Exam Preparation 2022- with rationale
Document Content and Description Below
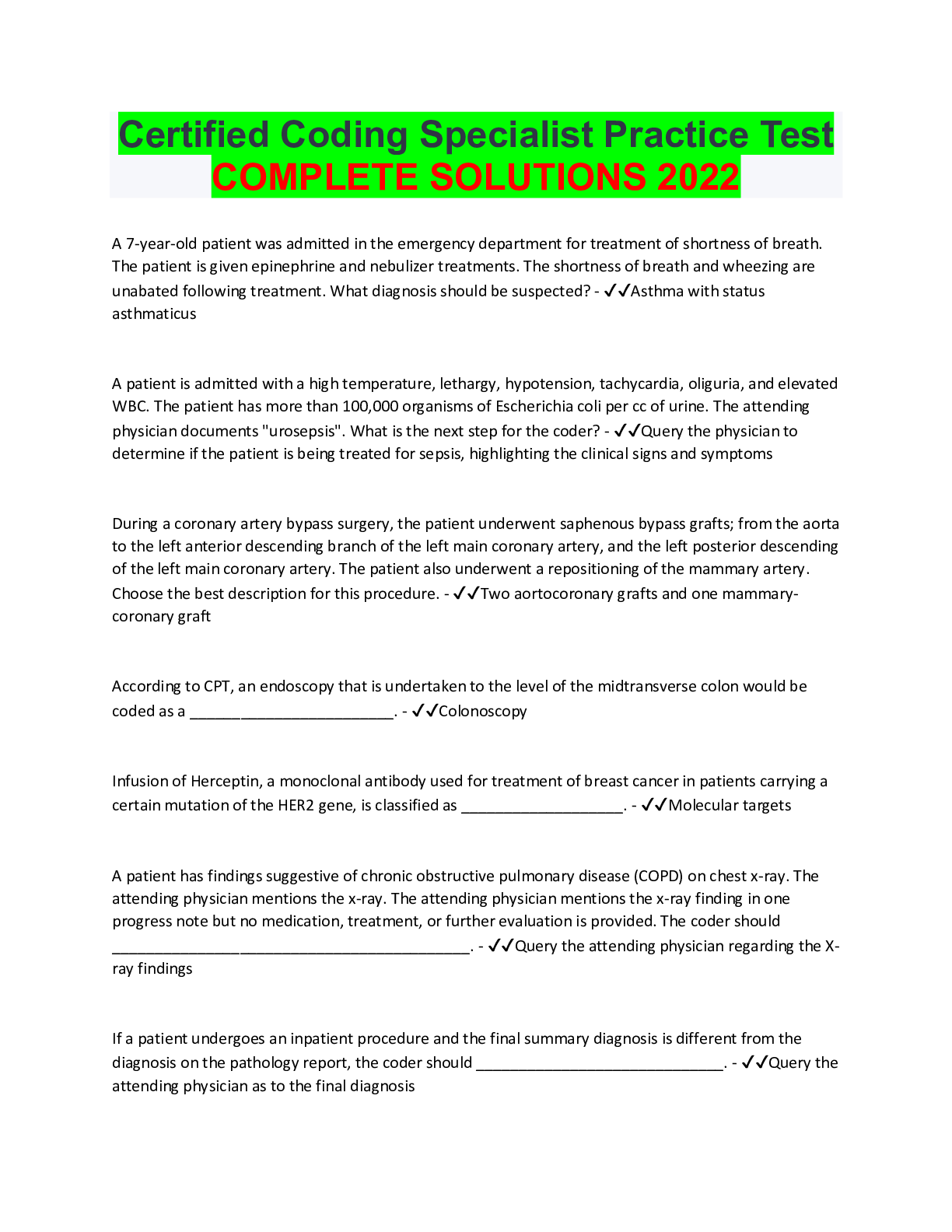
Certified Coding Associate (CCA) Exam Preparation 2022- with rationale c. Edit checks Edit checks help ensure data integrity by allowing only reasonable and predetermined values to be entered into... the computer (Rinehart-Thompson 2016a, 265). - ✔✔A coding analyst consistently enters the wrong code for patient gender in the electronic billing system. What data quality or data integrity measures should be in place to ensure that only allowable code numbers are entered? a. Access controls b. Audit trail c. Edit checks d. Password controls b. Delinquent record An incomplete record not rectified within a specific number of days as indicated in the medical staff rules and regulations is considered to be delinquent (Sayles 2016, 65). - ✔✔A health record with deficiencies that is not complete within the timeframe specified in the medical staff rules and regulations is called a(n): a. Suspended record b. Delinquent record c. Pending record d. Illegal record b. Provide an input mask for entering data in the field When several people enter data in an EHR, you can define how users must enter data in specific fields to help maintain consistency. For example, an input mask for a form means that users can only enter the date in a specified format (MacDonald 2010, chapter 4; Carter and Palmer 2016, 506). - ✔✔Which of thefollowing would be the best technique to ensure that registration clerks consistently use the correct notation for assigning admission date in an electronic health record (EHR)? a. Make admission date a required field b. Provide an input mask for entering data in the field c. Make admission date a numeric field d. Provide sufficient space for input of data a. UHDDS In 1974, the federal government adopted the UHDDS as the standard for collecting data for the Medicare and Medicaid programs. When the Prospective Payment Act was enacted in 1983, UHDDS definitions were incorporated into the rules and regulations for implementing diagnosis-related groups (DRGs). A key component was the incorporation of the definitions of principal diagnosis, principal procedure, and other significant procedures, into the DRG algorithms (Oachs and Watters 2016, 223). - ✔✔Mary Smith, RHIA, has been charged with the responsibility of designing a data collection form to be used on admission of a patient to the acute-care hospital in which she works. The first resource that she should use is _____. a. UHDDS b. UACDS c. MDS d. ORYX a. Meaning of data Data definition means that the data and information documented in the health record are defined; users of the data must understand what the data mean and represent (Sayles 2016, 52). - ✔✔Data definition refers to: a. Meaning of data b. Completeness of data c. Consistency of data d. Detail of dataa. Provide the medical records in paper format The covered entity must provide access to the personal health information in the form or format requested when it is readily producible in such form or format. When it is not readily producible in the form or format requested, it must be produced in a readable hard-copy form or such other form or format agreed upon by the covered entity and the individual (Gordon and Gordon 2016b, 615-616). - ✔✔A patient requests copies of her personal health information on CD. When the patient goes home, she finds that she cannot read the CD on her computer. The patient then requests the hospital to provide the medical records in paper format. How should the hospital respond? a. Provide the medical records in paper format b. Burn another CD because this is hospital policy c. Provide the patient with both paper and CD copies of the medical record d. Review the CD copies with the patient on a hospital computer b. Objective Objective information may be measured or observed by the healthcare provider (Amatayakul 2016, 294). - ✔✔A notation for a diabetic patient in a physician progress note reads: "FBS 110mg%, urine sugar, no acetone." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan d. Query the physician as to the method used. It is not appropriate for the coder to assume the removal was done by either snare or hot biopsy forceps. The ablation code is only assigned when a lesion is completely destroyed and no specimen is retrieved. The coding professional must query the physician to assign the appropriate code (AHIMA 2016, 454). - ✔✔When the physician does not specify the method used to remove a lesion during an endoscopy, what is the appropriate procedure? a. Assign the removal by snare technique code. b. Assign the removal by hot biopsy forceps code [Show More]
Last updated: 2 years ago
Preview 1 out of 125 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 16, 2022
Number of pages
125
Written in
Additional information
This document has been written for:
Uploaded
Nov 16, 2022
Downloads
0
Views
171


 with Complete Solution.png)
 Career Information with Complete Solution.png)


 for E-6 Career Information_watermark.png)


 Exam Preparation 2023- with rationale.png)
 Exam With Questions And Answers.png)

