Health Care > QUESTIONS & ANSWERS > AHIP FWA Questions and Answers with Certified Solutions (All)
AHIP FWA Questions and Answers with Certified Solutions
Document Content and Description Below
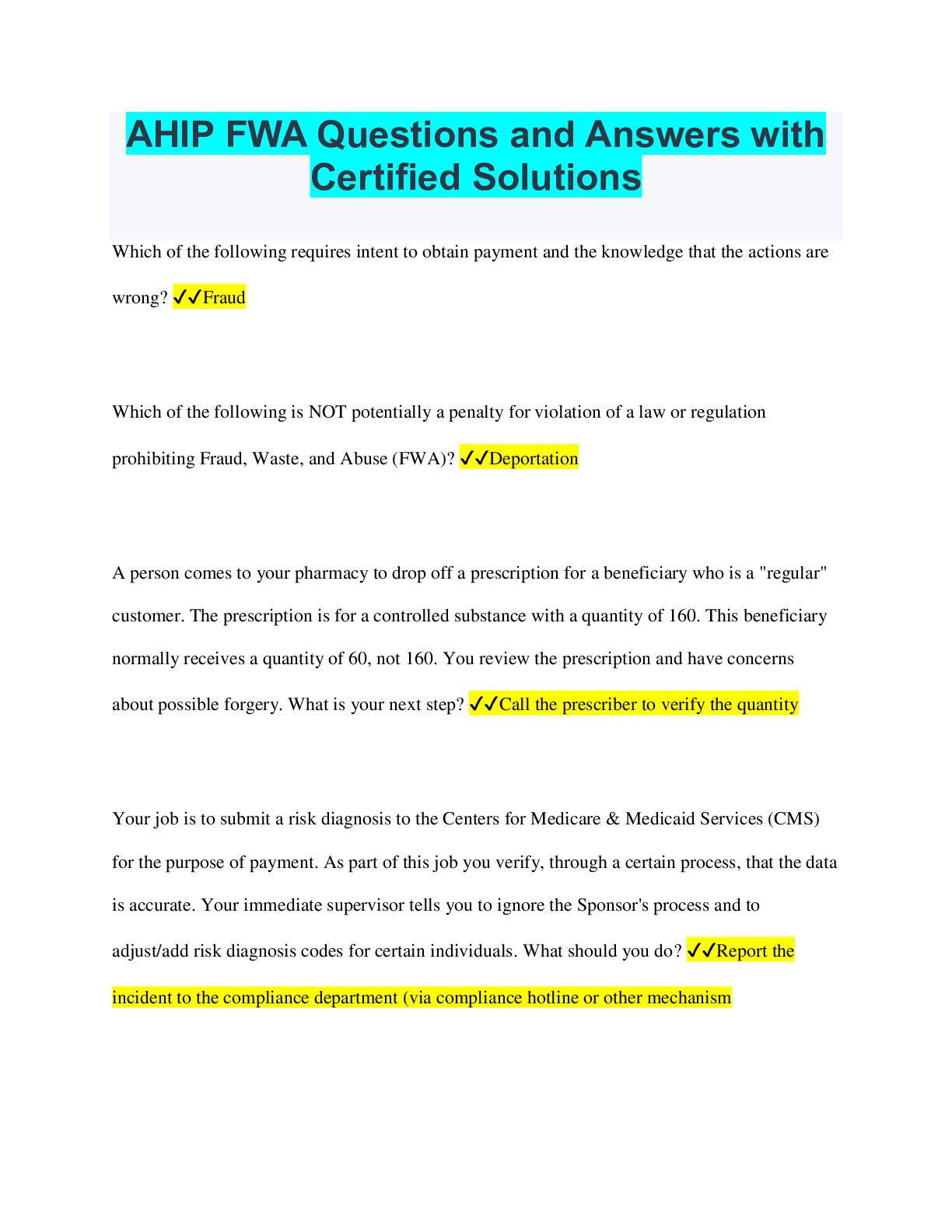
AHIP FWA Questions and Answers with Certified Solutions Which of the following requires intent to obtain payment and the knowledge that the actions are wrong? ✔✔Fraud Which of the following is... NOT potentially a penalty for violation of a law or regulation prohibiting Fraud, Waste, and Abuse (FWA)? ✔✔Deportation A person comes to your pharmacy to drop off a prescription for a beneficiary who is a "regular" customer. The prescription is for a controlled substance with a quantity of 160. This beneficiary normally receives a quantity of 60, not 160. You review the prescription and have concerns about possible forgery. What is your next step? ✔✔Call the prescriber to verify the quantity Your job is to submit a risk diagnosis to the Centers for Medicare & Medicaid Services (CMS) for the purpose of payment. As part of this job you verify, through a certain process, that the data is accurate. Your immediate supervisor tells you to ignore the Sponsor's process and to adjust/add risk diagnosis codes for certain individuals. What should you do? ✔✔Report the incident to the compliance department (via compliance hotline or other mechanism You are in charge of payment of claims submitted by providers. You notice a certain diagnostic provider ("Doe Diagnostics") requested a substantial payment for a large number of members. Many of these claims are for a certain procedure. You review the same type of procedure for other diagnostic providers and realize that Doe Diagnostics' claims far exceed any other provider that you reviewed. What should you do? ✔✔Consult with your immediate supervisor for next steps or contact the compliance department (via compliance hotline, Special Investigations Unit (SIU), or other mechanism) You are performing a regular inventory of the controlled substances in the pharmacy. You discover a minor inventory discrepancy. What should you do? ✔✔Follow your pharmacy's procedures Compliance is the responsibility of the Compliance Officer, Compliance Committee, and Upper Management only. ✔✔False Ways to report a compliance issue include: ✔✔All of the above What is the policy of non-retaliation? ✔✔Protects employees who, in good faith, report suspected non-compliance These are examples of issues that can be reported to a Compliance Department: suspected Fraud, Waste, and Abuse (FWA); potential health privacy violation, and unethical behavior/employee misconduct. ✔✔True Once a corrective action plan begins addressing non-compliance or Fraud, Waste, and Abuse (FWA) committed by a Sponsor's employee or First-Tier, Downstream, or Related Entity's (FDR's) employee, ongoing monitoring of the corrective actions is not necessary. ✔✔False Medicare Parts C and D plan Sponsors are not required to have a compliance program. ✔✔False At a minimum, an effective compliance program includes four core requirements. ✔✔False Standards of Conduct are the same for every Medicare Parts C and D Sponsor. ✔✔False Correcting non-compliance ______________. ✔✔Protects enrollees, avoids recurrence of the same non-compliance, and promotes efficienc What are some of the consequences for non-compliance, fraudulent, or unethical behavior? ✔✔All of the above [Show More]
Last updated: 2 years ago
Preview 1 out of 3 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)

Fraud Waste and Abuse (FWA) Bundled Exams Questions and Answers 100% Pass
Fraud Waste and Abuse (FWA) Bundled Exams Questions and Answers 100% Pass
By Nutmegs 2 years ago
$20
13
Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 12, 2023
Number of pages
3
Written in
Additional information
This document has been written for:
Uploaded
Apr 12, 2023
Downloads
0
Views
99