*NURSING > EXAM > Chapter 32: Alterations of Cardiovascular Function. Question and Correct Answers. (All)
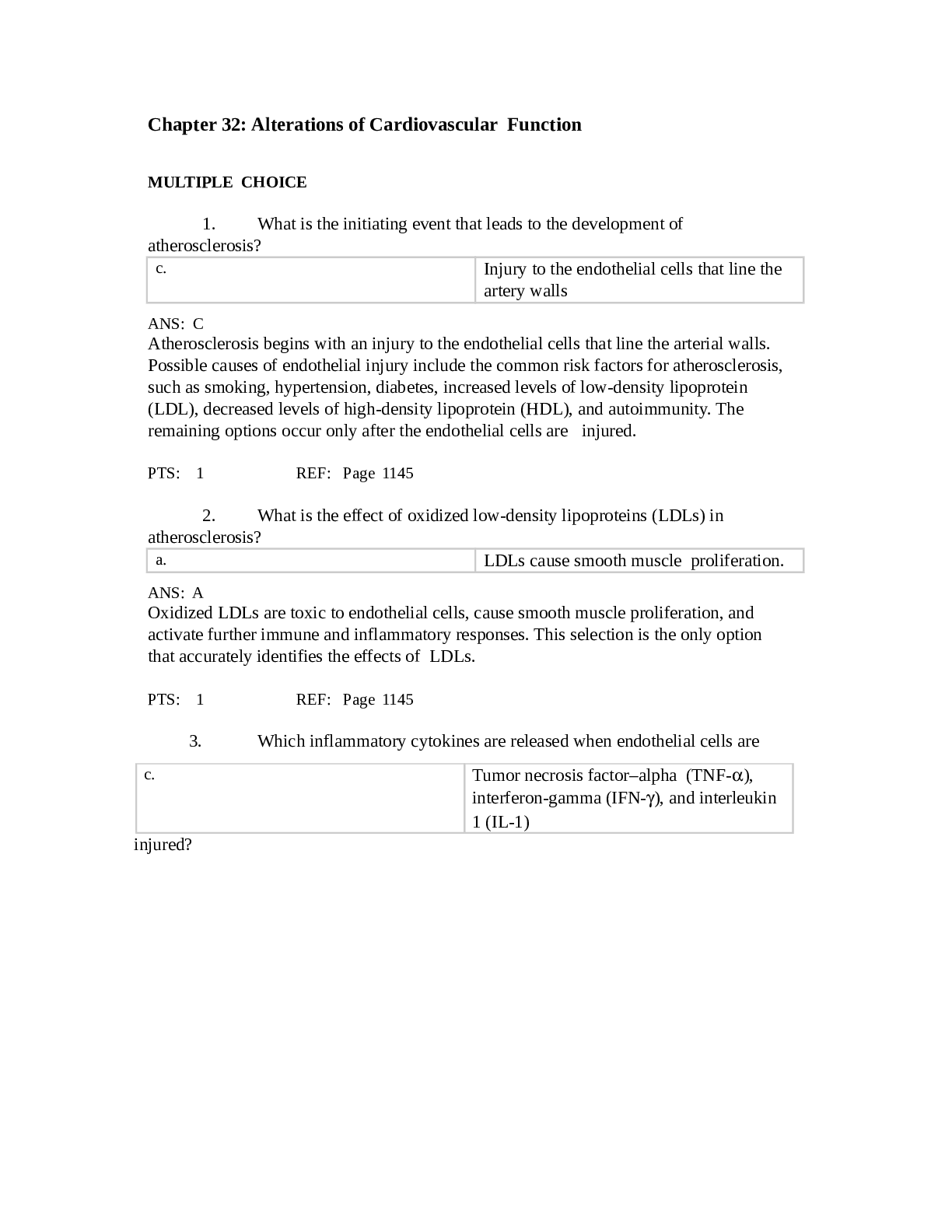
Chapter 32: Alterations of Cardiovascular Function. Question and Correct Answers.
Document Content and Description Below
Chapter 32: Alterations of Cardiovascular Function MULTIPLE CHOICE 1. What is the initiating event that leads to the development of atherosclerosis? Injury to the endothelial cells that line t... he artery walls Atherosclerosis begins with an injury to the endothelial cells that line the arterial walls. Possible causes of endothelial injury include the common risk factors for atherosclerosis, such as smoking, hypertension, diabetes, increased levels of low-density lipoprotein (LDL), decreased levels of high-density lipoprotein (HDL), and autoimmunity. The remaining options occur only after the endothelial cells are injure PTS: 1 REF: Page 1145 2. What is the effect of oxidized low-density lipoproteins (LDLs) in atherosclerosis? LDLs cause smooth muscle proliferation. Oxidized LDLs are toxic to endothelial cells, cause smooth muscle proliferation, and activate further immune and inflammatory responses. This selection is the only option that accurately identifies the effects of LDLs. PTS: 1 REF: Page 1145 3. Which inflammatory cytokines are released when endothelial cells are Tumor necrosis factor–alpha (TNF-), interferon-gamma (IFN-), and interleukin 1 (IL-1) injured? Numerous inflammatory cytokines are released, including TNF-, IFN-, IL-1, toxic oxygen radicals, and heat shock proteins. This selection is the only option that accurately identifies which inflammatory cytokines are associated with endothelial cell injury. PTS: 1 REF: Page 1145 4. When endothelia cells are injured, what alteration contributes to atherosclerosis? Cells are unable to make the normal amount of vasodilating cytokines. Injured endothelial cells become inflamed and cannot make normal amounts of antithrombotic and vasodilating cytokines. This selection is the only option that accurately identifies the factor that contributes to atherosclerosis. PTS: 1 REF: Page 1145 5. Which factor is responsible for the hypertrophy of the myocardium associated with hypertension? Of the available options, only angiotensin II is responsible for the hypertrophy of the myocardium and much of the renal damage associated with hypertension. PTS: 1 REF: Pages 1132-1138 6. What pathologic change occurs to the kidney’s glomeruli as a result of hypertension? Ischemia of the tubule In the kidney, vasoconstriction and resultant decreased renal perfusion cause tubular ischemia and preglomerular arteriopathy. This selection is the only option that accurately identifies the pathologic change to the kidney that occurs as a result of hypertension. PTS: 1 REF: Pages 1134-1136 7. What effect does atherosclerosis have on the development of an aneurysm? Atherosclerosis erodes the vessel wall. Atherosclerosis is a common cause of aneurysms because plaque formation erodes the vessel wall. This selection is the only option that accurately identifies the effect that atherosclerosis has on aneurysm development. PTS: 1 REF: Pages 1141-1142 8. Regarding the endothelium, what is the difference between healthy vessel walls and those that promote clot formation? Inflammation and roughening of the endothelium of the artery are present. Invasion of the tunica intima by an infectious agent also roughens the normally smooth lining of the artery, causing platelets to adhere readily. This selection is the only option that accurately describes the mechanism that supports abnormal clot formation. PTS: 1 REF: Pages 1142-1143 9. What is the usual source of pulmonary emboli? Pulmonary emboli originate in the venous circulation (mostly from the deep veins of the legs) or in the right heart. This selection is the only option that accurately identifies the usual source of pulmonary emboli. PTS: 1 REF: Page 1143 10. Which factor can trigger an immune response in the bloodstream that may result in an embolus? Of the options available, only amniotic fluid displaces blood, thereby reducing oxygen, nutrients, and waste exchange; however, it also introduces antigens, cells, and protein aggregates that trigger inflammation, coagulation, and the immune response in the bloodstream. PTS: 1 REF: Pages 1143-1144 11. Which statement best describes thromboangiitis obliterans (Buerger disease)? Inflammatory disorder of small- and medium-size arteries in the feet and sometimes in the hands Buerger disease is an inflammatory disease of the peripheral arteries. Inflammation, thrombus formation, and vasospasm can eventually occlude and obliterate portions of small- and medium-size arteries. The digital, tibial, and plantar arteries of the feet and the digital, palmar, and ulnar arteries of the hands are typically affecte This selection is the only option that accurately describes Buerger diseas PTS: 1 REF: Page 1144 12. Which statement best describes Raynaud disease? Vasospastic disorder of the small arteries and arterioles of the fingers and, less commonly, of the toes Attacks of vasospasm in the small arteries and arterioles of the fingers and, less commonly, of the toes characterize Raynaud phenomenon and Raynaud disease and is the only option that accurately describes this diseas PTS: 1 REF: Page 1144 13. What change in a vein supports the development of varicose veins? If a valve is damaged, permitting backflow, then a section of the vein is subjected to the pressure exerted by a larger volume of blood under the influence of gravity. The vein swells as it becomes engorged, and the surrounding tissue becomes edematous because increased hydrostatic pressure pushes plasma through the stretched vessel wall. This selection is the only option that accurately describes the development of varicose veins. PTS: 1 REF: Pages 1129-1130 14. Superior vena cava syndrome is a result of a progressive increase of which process? Superior vena cava syndrome (SVCS) is a progressive occlusion of the superior vena cava (SVC) that leads to venous distention in the upper extremities and hea The remaining options are not associated with this disorder. PTS: 1 REF: Page 1131 15. What term is used to identify when a cell is temporarily deprived of blood supply? Coronary artery disease (CAD) can diminish the myocardial blood supply until deprivation impairs myocardial metabolism enough to cause ischemia, a local state in which the cells are temporarily deprived of blood supply. This term is the only option that is used to identify a temporarily deprived blood supply. PTS: 1 REF: Page 1148 16. The risk of developing coronary artery disease is increased up to threefold by which factor? Hypertension is the only factor responsible for a twofold-to-threefold increased risk of atherosclerotic cardiovascular diseas PTS: 1 REF: Page 1151 17. Which risk factor is associated with coronary artery disease (CAD) because of its relationship with the alteration of hepatic lipoprotein? Of the available options, only diabetes mellitus is associated with CAD because of the resulting alteration of hepatic lipoprotein synthesis; it increases triglyceride levels and is involved in low-density lipoprotein oxidation. PTS: 1 REF: Pages 1148-1151 18. Nicotine increases atherosclerosis by the release of which neurotransmitter? Nicotine stimulates the release of catecholamines (g., epinephrine, norepinephrine), which increases the heart rate and causes peripheral vascular constriction. As a result, blood pressure increases, as do both cardiac workload and oxygen deman None of the other options are associated with this mechanism. PTS: 1 REF: Page 1151 19. Which substance is manufactured by the liver and primarily contains cholesterol and protein? Low-density lipoproteins (LDLs) A series of chemical reactions in the liver results in the production of several lipoproteins that vary in density and function. These include VLDLs, primarily triglycerides and protein; LDLs, mostly cholesterol and protein; and HDLs, mainly phospholipids and protein. LDLs are the only lipoproteins that are manufactured by the liver and primarily contain cholesterol and protein. PTS: 1 REF: Page 1149 20. Which elevated value may be protective of the development of atherosclerosis? High-density lipoproteins (HDLs Low levels of HDL cholesterol are also a strong indicator of coronary risk, whereas high levels of HDLs may be more protective for the development of atherosclerosis than low levels of LDLs. Neither VLDLs nor elevated triglycerides are associated with a protective mechanism. PTS: 1 REF: Pages 1149-1151 21. Which laboratory test is an indirect measure of atherosclerotic plaque? C-reactive protein (CRP) Highly sensitive CRP (hs-CRP) is an acute phase reactant or protein mostly synthesized in the liver and, of the available options, is an indirect measure of atherosclerotic plaque- related inflammation. PTS: 1 REF: Page 1152 22. Cardiac cells can withstand ischemic conditions and still return to a viable state for how many minutes? Cardiac cells remain viable for approximately 20 minutes under ischemic conditions. If blood flow is restored, then aerobic metabolism resumes, contractility is restored, and cellular repair begins. If the coronary artery occlusion persists beyond 20 minutes, then myocardial infarction (MI) occurs. PTS: 1 REF: Page 1153 23. Which form of angina occurs most often during sleep as a result of vasospasms of one or more coronary arteries? Of the options available, only Prinzmetal angina (also called variant angina) is chest pain attributable to transient ischemia of the myocardium that occurs unpredictably and almost exclusively at rest. PTS: 1 REF: Page 1154 24. When is the scar tissue that is formed after a myocardial infarction (MI) most vulnerable to injury? During the recovery period (10 to 14 days after infarction), individuals feel more capable of increasing activities and thus may stress the newly formed scar tissu After 6 weeks, the necrotic area is completely replaced by scar tissue, which is strong but unable to contract and relax like healthy myocardial tissu PTS: 1 REF: Page 1160 25. An individual who is demonstrating elevated levels of troponin, creatine kinase–isoenzyme MB (CK-MB), and lactic dehydrogenase (LDH) is exhibiting indicators associated with which condition? Cardiac troponins (troponin I and troponin T) are the most specific indicators of MI. Other biomarkers released by myocardial cells include CK-MB and LDH, but they are not associated with the other options. PTS: 1 REF: Pages 1160-1161 26. What is the expected electrocardiogram (ECG) pattern when a thrombus in a coronary artery permanently lodges in the vessel and the infarction extends through the myocardium from the endocardium to the epicardium? ST elevation myocardial infarction (STEMI) Individuals with this pattern on an ECG usually have significant elevations in the ST segments and are categorized as having STEMI. The other options are not associated with the described pathologic condition. PTS: 1 REF: Pages 1157-1158 27. How does angiotensin II increase the workload of the heart after a myocardial infarction (MI)? By increasing the peripheral vasoconstriction Angiotensin II is released during myocardial ischemia and contributes to the pathogenesis of a myocardial infarction (MI) in several ways. First, it results in the systemic effects of peripheral vasoconstriction and fluid retention. These homeostatic responses are counterproductive in that they increase myocardial work and thus exacerbate the effects of the loss of myocyte contractility. Angiotensin II is also locally released, where it is a growth factor for vascular smooth muscle cells, myocytes, and cardiac fibroblasts; promotes catecholamine release; and causes coronary artery spasm. This selection is the only option that accurately describes how angiotensin II increases workload after a MI. PTS: 1 REF: Page 1159 28. The pulsus paradoxus that occurs as a result of pericardial effusion is caused by a dysfunction in which mechanism? Diastolic filling pressures of the left ventricle and reduction of blood volume in all four heart chambers. Pulsus paradoxus means that the arterial blood pressure during expiration exceeds arterial pressure during inspiration by more than 10 mm Hg. This clinical finding reflects impairment of diastolic filling of the left ventricle plus a reduction of blood volume within all four cardiac chambers. This selection is the only option that accurately describes the mechanism. PTS: 1 REF: Page 1164 29. A patient reports sudden onset of severe chest pain that radiates to the back and worsens with respiratory movement and when lying down. These clinical manifestations describe: Most individuals with acute pericarditis describe several days of fever, myalgias, and malaise, followed by the sudden onset of severe chest pain that worsens with respiratory movements and with lying down. Although the pain may radiate to the back, it is generally felt in the anterior chest and may be initially confused with the pain of an acute MI. Individuals with acute pericarditis also may report dysphagia, restlessness, irritability, anxiety, and weakness. This selection is the only option with these symptoms. PTS: 1 REF: Page 1163 30. Ventricular dilation and grossly impaired systolic function, leading to dilated heart failure, characterize which form of cardiomyopathy? Only dilated cardiomyopathy (congestive cardiomyopathy) is characterized by ventricular dilation and grossly impaired systolic function, leading to dilated heart failur PTS: 1 REF: Page 1165 31. A disproportionate thickening of the interventricular septum is the hallmark of which form of cardiomyopathy? Only hypertrophic cardiomyopathy is characterized by a thickening of the septal wall, which may cause outflow obstruction to the left ventricle outflow tract. PTS: 1 REF: Page 1166 32. Amyloidosis, hemochromatosis, or glycogen storage disease usually causes which form of cardiomyopathy? Restrictive cardiomyopathy may occur idiopathically or as a cardiac manifestation of systemic diseases, such as scleroderma, amyloidosis, sarcoidosis, lymphoma, and hemochromatosis, or a number of inherited storage diseases. This characterization is not true of the other forms of cardiomyopathy. PTS: 1 REF: Page 1167 33. Which condition is a cause of acquired aortic regurgitation? Rheumatic heart disease, bacterial endocarditis, syphilis, hypertension, connective tissue disorders (g., Marfan syndrome, ankylosing spondylitis), appetite suppressing medications, trauma, or atherosclerosis can cause acquired aortic regurgitation. This selection is the only available option that is known to cause acquired aortic regurgitation. PTS: 1 REF: Page 1169 34. Which predominantly female valvular disorder is thought to have an autosomal dominant inheritance pattern, as well as being associated with connective tissue disease? Mitral valve prolapse tends to be most prevalent in young women. Studies suggest an autosomal dominant and X-linked inheritance pattern. Because mitral valve prolapse often is associated with other inherited connective tissue disorders (g., Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta), it is thought to result from a genetic or environmental disruption of valvular development during the fifth or sixth week of gestation. This provided history is not associated with any of the other options. PTS: 1 REF: Page 1170 35. Which disorder causes a transitory truncal rash that is nonpruritic and pink with erythematous macules that may fade in the center, making them appear as a ringworm? Rheumatic fever Erythema marginatum is a distinctive truncal rash that often accompanies acute rheumatic fever. It consists of nonpruritic, pink erythematous macules that never occur on the face or hands. This presentation is not associated with any of the other options. PTS: 1 REF: Page 1172 36. What is the most common cause of infective endocarditis? Infective endocarditis is a general term used to describe infection and inflammation of the endocardium—especially the cardiac valves. Bacteria are the most common cause of infective endocarditis, especially streptococci, staphylococci, or enterococci. PTS: 1 REF: Page 1173 37. What is the most common cardiac disorder associated with acquired immunodeficiency syndrome (AIDS) Pericardial effusion and left heart failure are the most common complications of human immunodeficiency virus (HIV) infection. Other conditions include cardiomyopathy, myocarditis, tuberculous pericarditis, infective and nonbacterial endocarditis, heart block, pulmonary hypertension, and nonantiretroviral drug-related cardiotoxicity. PTS: 1 REF: Page 1175 38. A patient is diagnosed with pulmonary disease and elevated pulmonary vascular resistanc Which form of heart failure may result from pulmonary disease and elevated pulmonary vascular resistance? Right heart failure is defined as the inability of the right ventricle to provide adequate blood flow into the pulmonary circulation at a normal central venous pressur This condition is often a result of pulmonary disease and the resulting elevated pulmonary vascular resistanc PTS: 1 REF: Page 1181 39. What cardiac pathologic condition contributes to ventricular remodeling? Of the options available, myocardial ischemia contributes to inflammatory, immune, and neurohumoral changes that mediate a process called ventricular remodeling. PTS: 1 REF: Page 1175 40. In systolic heart failure, what effect does the renin-angiotensin-aldosterone system (RAAS) have on stroke volume? Increases preload and increases afterloa Activation of the RAAS not only causes an increase in preload and afterload, but it also causes direct toxicity to the myocardium. This selection is the only option that accurately identifies the effect that the RAAS has on stroke volume in this situation. PTS: 1 REF: Page 1175 | Page 1177 41. What is the cause of the dyspnea resulting from a thoracic aneurysm? Clinical manifestations depend on the location of the aneurysm. Pressure of a thoracic aneurysm on surrounding organs cause symptoms of dysphagia (difficulty in swallowing) and dyspnea (breathlessness). This selection is the only option that accurately describes the cause of dyspnea resulting from a thoracic aneurysm. PTS: 1 REF: Page 1142 42. Which statement is true concerning the cells’ ability to synthesize cholesterol? Most body cells are capable of producing cholesterol. Although cholesterol can easily be obtained from dietary fat intake, most body cells can also manufacture cholesterol. This selection is the only option that accurately describes the cellular role in cholesterol synthesis. PTS: 1 REF: Page 1149 43. What is the trigger for angina pectoris? Angina pectoris is chest pain caused by myocardial ischemi None of the other options are considered triggers for angina pectoris. PTS: 1 REF: Page 1154 44. Individuals being effectively managed for type 2 diabetes mellitus often experience a healthy decline in blood pressure as a result of what intervention? Insulin-sensitivity medication therapy Many people with type 2 diabetes mellitus, who are treated with drugs that increase insulin sensitivity, experience a decline in their blood pressure without taking antihypertensive drugs. Although the other medications may be included in the management plan, the other options are not associated with a decrease in hypertension. PTS: 1 REF: Page 1136 MULTIPLE RESPONSE 45. Which statements are true regarding fatty streaks? (Select all that apply.) Fatty streaks progressively damage vessel walls. Fatty streaks are capable of producing toxic oxygen radials. When present, inflammatory changes occur to the vessel walls. Oxidized low-density lipoproteins (LDLs) are involved in their formation. , B, C, D The oxidized LDLs penetrate the intima of the arterial wall and are engulfed by macrophages. Macrophages filled with oxidized LDLs are called foam. Once these lipid- laden foam cells accumulate in significant amounts, they form a lesion called a fatty streak. Once formed, fatty streaks produce more toxic oxygen radicals and cause immunologic and inflammatory changes, resulting in progressive damage to the vessel wall. PTS: 1 REF: Page 1145 | Page 1147 46. What factors contribute to the development of orthostatic hypotension? (Select all that apply.) Altered body chemistry Drug action of certain antihypertensive agents Prolonged immobility Effects of aging on postural reflexes , B, C, D Orthostatic hypotension may be acute or chroni Acute orthostatic hypotension (temporary type) may result from (1) altered body chemistry, (2) drug action (g., antihypertensives, antidepressants), (3) prolonged immobility caused by illness, (4) starvation, (5) physical exhaustion, (6) any condition that produces volume depletion (g., massive diuresis, potassium or sodium depletion), and (7) venous pooling (g., pregnancy, extensive varicosities of the lower extremities). Older adults are susceptible to this type of orthostatic hypotension, in which postural reflexes are slowed as part of the aging process. PTS: 1 REF: Page 1140 47. Which assessment findings are clinical manifestations of aortic stenosis? (Select all that apply.) Angina Syncope ANS: D, E The classic manifestations of aortic stenosis are angina, syncope, and heart failur None of the other options are associated with aortic stenosis. PTS: 1 REF: Pages 1168-1169 48. Which risk factors are associated with infective endocarditis? (Select all that apply.) Intravenous drug use Long-term indwelling catheterization Heart valve disease , C, E Risk factors for infective endocarditis include acquired valvular heart disease, intravenous drug abuse, long-term indwelling catheterization (g., for pressure monitoring, hyperalimentation, or hemodialysis), and recent cardiac surgery. Neither rheumatic fever nor aortic regurgitation is considered a risk factor for infective endocarditis. PTS: 1 REF: Page 1173 | Box 32-3 MATCHING Match the descriptions with the corresponding terms. Impairs flow from left atrium to left ventricle Impairs flow from the left ventricle Backflow into left atrium Backflow into right atrium Backflow into left ventricle 49. Aortic stenosis 50. Aortic regurgitation 51. Mitral stenosis 52. Tricuspid regurgitation 53. Mitral regurgitation 49. PTS: 1 REF: Page 1168 MSC: Outflow obstruction increases pressure within the left ventricle as it tries to eject blood through the narrowed opening. Left ventricular hypertrophy develops to compensate for the increased workloa 50. PTS: 1 REF: Pages 1169-1170 MSC: During systole, blood is ejected from the left ventricle into the aort If the aortic semilunar valve fails to close completely, then some of the ejected blood flows back into the left ventricle during diastol 51. PTS: 1 REF: Page 1169 MSC: Mitral stenosis impairs the flow of blood from the left atrium to the left ventricl 52. PTS: 1 REF: Page 1170 MSC: Tricuspid regurgitation is more common than tricuspid stenosis and is usually associated with cardiac failure and dilation of the right ventricle, secondary to pulmonary hypertension. 53. PTS: 1 REF: Page 1170 MSC: Mitral regurgitation permits the backflow of blood from the left ventricle into the left atrium during ventricular systole, giving rise to a loud pansystolic (throughout systole) murmur heard best at the apex that radiates into the back and axilla [Show More]
Last updated: 2 years ago
Preview 1 out of 17 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 01, 2021
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Apr 01, 2021
Downloads
0
Views
77

 HESI VI EXIT EXAM.png)
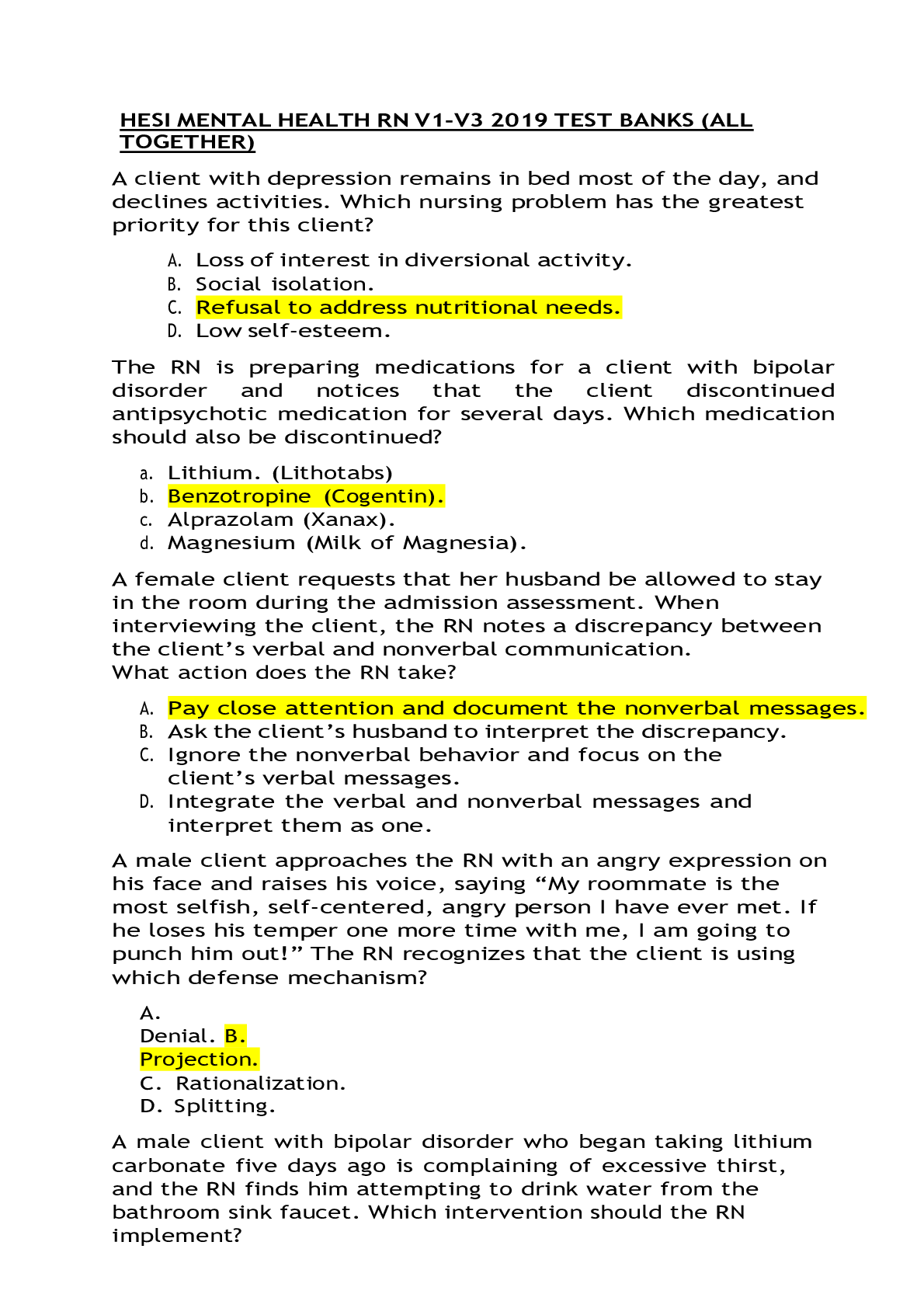
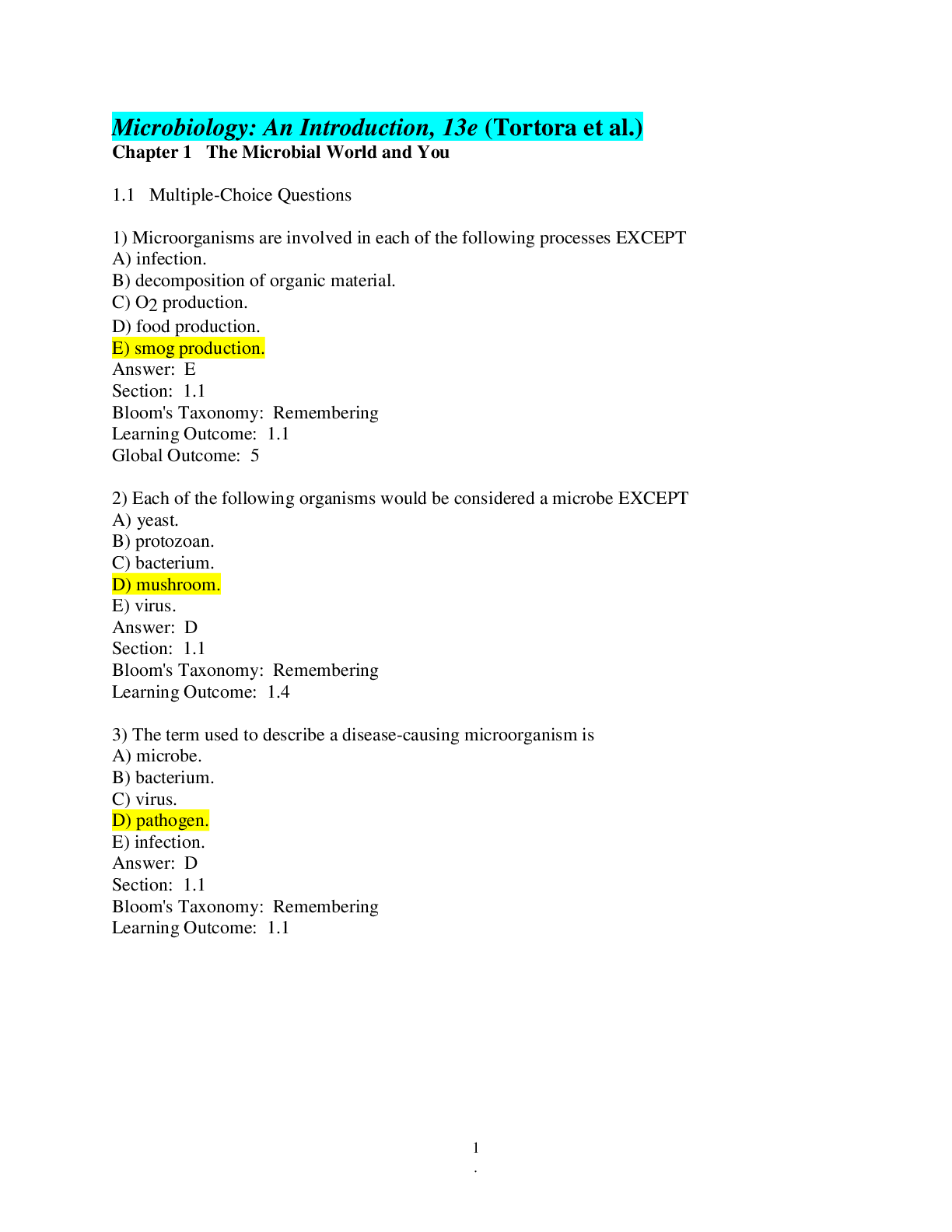
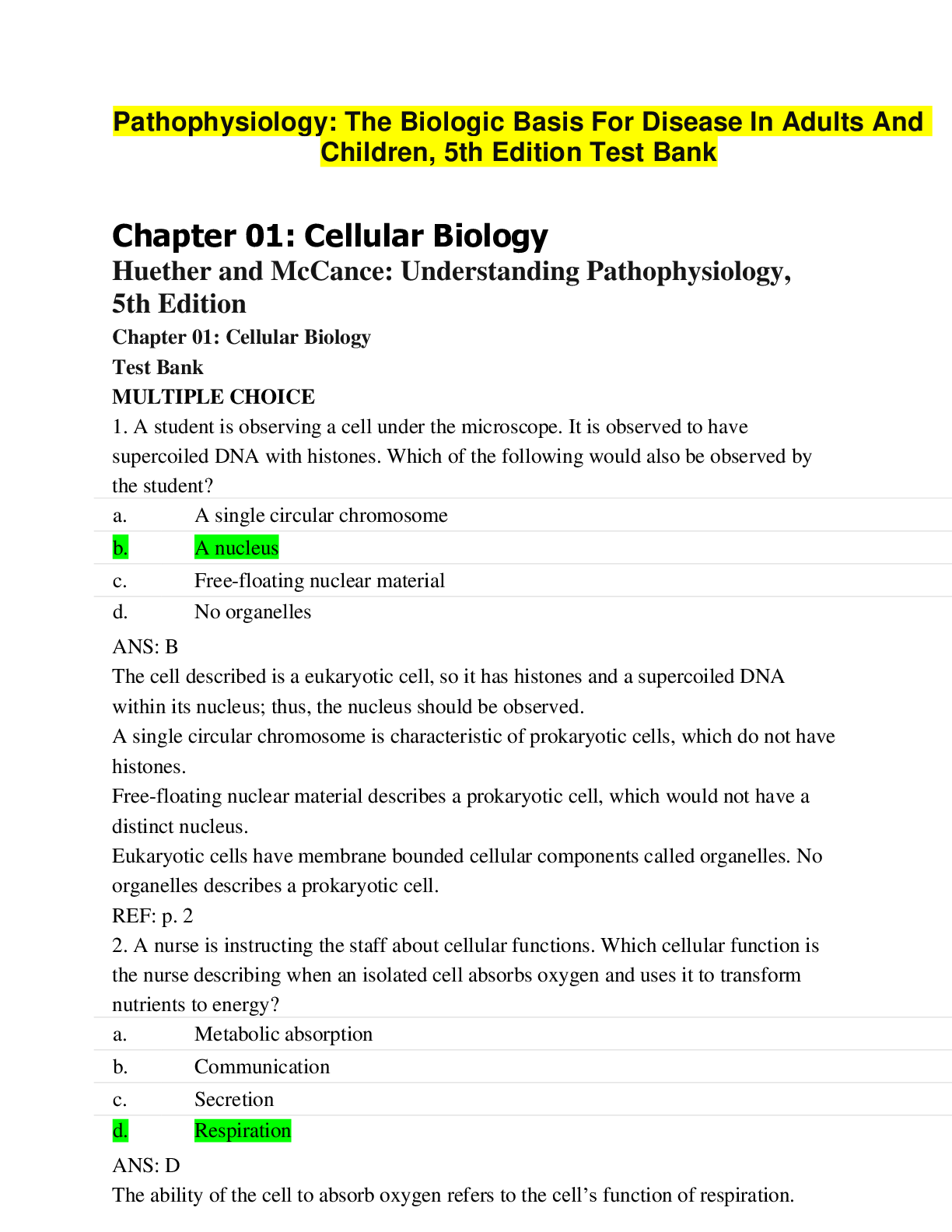


, MSN 570.png)

