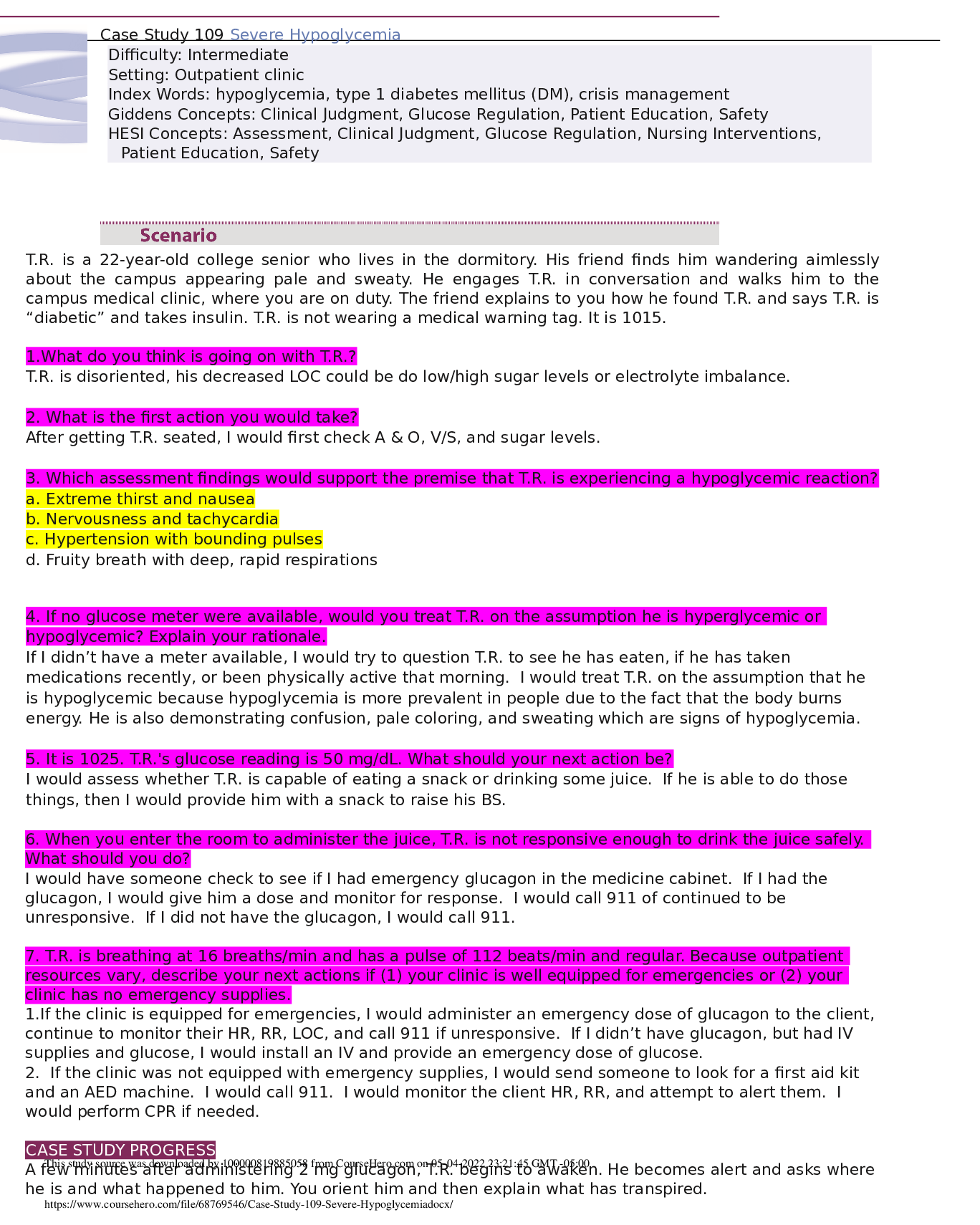
T.R. is a 22-year-old college senior who lives in the dormitory. His friend finds him wandering aimlessly
about the campus appearing pale and sweaty. He engages T.R. in conversation and walks him to the
campus medical
...
T.R. is a 22-year-old college senior who lives in the dormitory. His friend finds him wandering aimlessly
about the campus appearing pale and sweaty. He engages T.R. in conversation and walks him to the
campus medical clinic, where you are on duty. The friend explains to you how he found T.R. and says T.R. is
“diabetic” and takes insulin. T.R. is not wearing a medical warning tag. It is 1015.
1.What do you think is going on with T.R.?
T.R. is disoriented, his decreased LOC could be do low/high sugar levels or electrolyte imbalance.
2. What is the first action you would take?
After getting T.R. seated, I would first check A & O, V/S, and sugar levels.
3. Which assessment findings would support the premise that T.R. is experiencing a hypoglycemic reaction?
a. Extreme thirst and nausea
b. Nervousness and tachycardia
c. Hypertension with bounding pulses
d. Fruity breath with deep, rapid respirations
4. If no glucose meter were available, would you treat T.R. on the assumption he is hyperglycemic or
hypoglycemic? Explain your rationale.
If I didn’t have a meter available, I would try to question T.R. to see he has eaten, if he has taken
medications recently, or been physically active that morning. I would treat T.R. on the assumption that he
is hypoglycemic because hypoglycemia is more prevalent in people due to the fact that the body burns
energy. He is also demonstrating confusion, pale coloring, and sweating which are signs of hypoglycemia.
5. It is 1025. T.R.'s glucose reading is 50 mg/dL. What should your next action be?
I would assess whether T.R. is capable of eating a snack or drinking some juice. If he is able to do those
things, then I would provide him with a snack to raise his BS.
6. When you enter the room to administer the juice, T.R. is not responsive enough to drink the juice safely.
What should you do?
I would have someone check to see if I had emergency glucagon in the medicine cabinet. If I had the
glucagon, I would give him a dose and monitor for response. I would call 911 of continued to be
unresponsive. If I did not have the glucagon, I would call 911.
7. T.R. is breathing at 16 breaths/min and has a pulse of 112 beats/min and regular. Because outpatient
resources vary, describe your next actions if (1) your clinic is well equipped for emergencies or (2) your
clinic has no emergency supplies.
1.If the clinic is equipped for emergencies, I would administer an emergency dose of glucagon to the client,
continue to monitor their HR, RR, LOC, and call 911 if unresponsive. If I didn’t have glucagon, but had IV
supplies and glucose, I would install an IV and provide an emergency dose of glucose.
2. If the clinic was not equipped with emergency supplies, I would send someone to look for a first aid kit
and an AED machine. I would call 911. I would monitor the client HR, RR, and attempt to alert them. I
would perform CPR if needed.
[Show More]