*NURSING > QUESTIONS & ANSWERS > GRNU 615 Study Guide (2019-20) Graduate Nursing 615 | Maryville University of St. Louis. This study (All)
GRNU 615 Study Guide (2019-20) Graduate Nursing 615 | Maryville University of St. Louis. This study guide contains 230+ pages organised in 1762 questions and answers deigned for the quick exam-study sessions.
Document Content and Description Below
GRNU 615 Study Guide (2019-20) What are black box warnings on NSAIDS? GI bleed + What are the black box warnings on NSAIDs What are the black box warnings on NSAIDS What are the black box wa... rnings on NSAIDS? What lab values should be monitored with gout? What lab values should be monitored with gout What lab values should be monitored with gout? What lab values should be monitored with gout? Differentiate between low dose and high dose colchicine? Differentiate between low dose and high dose colchicine Differentiate between low dose and high dose colchicine. What patient education should you provide when prescribing colchicine? What patient education should you provide when prescribing colchicine? What patient education should you provide when prescribing colchicine? What patient education should you provide when prescribing colchicine? What patient teaching will you provide when prescribing febuxostat (uloric)? What patient teaching will you provide when prescribing febuxostat (Uloric)? What patient teaching will you provide when prescribing febuxostat (Uloric)? What are the adverse effects of corticosteroids if administered for 6 months or more? What are the adverse effects of corticosteroids if administered for six months or more What are the adverse effects of corticosteroids if administered for 6 months or more? What are the adverse effects of corticosteroids if administered for 6 months or more? What are the adverse effects of corticosteroids if administered for 6 months or more? Why is it important to taper the corticosteroid? Why is it important to taper the corticosteroid? Why is it important to taper the corticosteroid? What are the drug interactions with digoxin (cardiac glycoside)? What are the recommendations in the treatment of pain? What are the recommendations in the treatment of pain What are the recommendations in the treatment of pain? What are the recommendations in the treatment of pain? What is the mechanism of action of ibuprofen? What is the mechanism of action for ibuprofen What is the mechanism of action of ibuprofen? What is the mechanism of action of ibuprofen? What are the serious side effects associated with acetaminophen (APAP)? How is amlodipine (norvasc) metabolized? What are the side effects of dihydropyridine {i.e. amlodipine (norvasc)}? What patient teaching will you provide when prescribing amiodarone? What patient teaching will you provide when prescribing amiodarone What patient teaching will you provide when prescribing amiodarone? What patient teaching will you provide when prescribing amiodarone? What is the purpose of a thyroid panel with amiodarone? What's the purpose of thyroid panel with amiodarone? What is the purpose of a thyroid panel with amiodarone? What is the purpose of a thyroid panel with amiodarone? What is nitrate tolerance? Nitrate tolerance What is nitrate tolerance? What is nitrate tolerance? Nitrate tolerance nitrate tolerance What are the contraindications to therapy with coumadin? hemorrhagic tendencies ( What are the contraindications to therapy with Coumadin? What are the contraindications to therapy with Coumadin? What classes of medications are used in the treatment of CHF? Identify the symptoms of hypoglycemia? Identify symptoms of hypoglycemia Identify the symptoms of Diabetic Ketoacidosis. Identify the symptoms of Hyperglycemia. How does metformin work? How does metformin work? How does metformin work? What diagnostic testing is required before and throughout therapy with metformin? What diagnostic testing is required before and throughout therapy with metformin What diagnostic testing is required before and throughout therapy with metformin? What diagnostic testing is required before and throughout therapy with metformin? What is the action of gliptin (dipeptidyl peptidase-4 inhibitor (DPP-4)? How do GLP agonists work? How do GLP agonists work How do GLP agonists work? How do GLP agonists work? - When should exenatide (GLP-1 receptor agonist) be administered? What are the adverse effects of propylthiouracil (PTU)?hyperthyroid tx: graves dz What are the adverse effects of levothyroxine? What are the adverse effects of levothyroxine? What are the adverse effects of levothyroxine? - What are the treatment recommendations with toxic goiter? What are the adverse effects of PTU and methimazole? What are the adverse effects of PTU and What are the adverse effects of PTU and methimazole? What is the dosage schedule for alpha-glucosidase inhibitors? (Acrobose) Describe the pharmacodynamics of meglitinides. Describe the pharmacodynamics of meglitinides Describe the pharmacodynamics of meglitinides. What is the mechanism of action of propyltiouracil (PTU)? What are the contraindications to therapy with alpha-glucosidase inhibitors (Acarbose)? What patient education is important relative to the administration of levothyroxine? What patient education is important relative the administration of levothyroxine What patient education is important relative to the administration of levothyroxine? What patient education is important relative to the administration of levothyroxine What black box warning has the FDA issued regarding the administration of TZDs (thiazolidinediones)? What symptoms may indicate that a patient is taking too much thyroid replacement hormone? What symptoms may indicate that a patient is taking too much thyroid replacement hormone What symptoms may indicate that a patient is taking too much thyroid replacement hormone? What symptoms may indicate that a patient is taking too much thyroid replacement hormone? What is the mechanism of action of metformin? ) What is the mechanism of action of metformin? What is the mechanism of action of metformin? What lab values will be used to monitor a patient on levothyroxine? What lab values will be used to monitor a patient on levothyroxine What lab values will be used to monitor a patient on levothyroxine? What lab values will be used to monitor a patient on levothyroxine? What is low dose colchicine What is high dose colchicine what is the difference between high dose and low dose colchicine? What lab value should be monitored with gout? What are serious side effects associated with acetaminophen? What are the serious side effects associated with acetaminophen? What are the serious side effects associated with acetaminophen? Identify the signs of hyperglycemia identify the signs of ketoacidosis how is metformin processed in the body What is the action of gliptin The first agent in the class, sitaglipin, was approved by the FDA in 2006 what is the benefit of using meglitinides . What are GLP agonist used to treat When should exenatide be administered When should exenatide be administered what is the mechanism of action of exenatide What are the adverse effects of propylthiouracil or PTU what is the mechanism of action of PTU what are the side effects of levothyroxine? which hormone is levothyroxine chemically identical to Where is T4 secreted what is levothyroxine used to treat A patient develops toxic goiter. What's the recommended treatment A patient develops a toxic goiter. What is the recommended treatment? A patient develops a toxic goiter. What is the recommended treatment? What are the adverse effects Methimazole? What are the adverse effects of PTU What is the dosage schedule for alpha-glucosidase inhibitors What is the dosage schedule for alpha-glucosidase inhibitors? What is the dosage schedule for alpha-glucosidase inhibitors? in what population is alpha-glucosidase inhibitors contraindicated What are the common side effects of alpha-glucosidase inhibitors What is the mechanism of action of propylthiouracil . What is the mechanism of action of propylthiouracil? What is the mechanism of action of propylthiouracil? - where does propylthiouracil (PTU) work What are the contraindications for therapy with alpha-glucosidase inhibitors What are the contraindications to therapy with alpha-glucosidase inhibitors? What are the contraindications to therapy with alpha-glucosidase inhibitors? What black box has the FDA issued regarding administration of TZDs (thiazolidinediones)? What is the onset of action peak of action and duration of action of Rapid acting insulin: Lispro(humalog)/Aspart (Novolog)/Glulisine (Apidra) what is the onset of action, peak of action, and duration of intermediate action insulin (NPH) What is the onset of action, peak of action, and duration of action of What is the onset of action, peak of action, and duration of action of Lispro? What is the onset of action, peak of action, and duration of action of regular insulin? 30-60 min 2-3 hours 3-7 What is the onset of action, peak of action, and duration of action of Regular U-500? 30-45 min 8-24 hours 8-24 What is the onset of action, peak of action, and duration of action of NPH? 30-60 min 10-16 hours 10-16 What is the onset of action, peak of action, and duration of action of Glarline? 60 none 24 What is the onset of action, peak of action, and duration of action of affreza? 0-12 min 2-3 hours 2-3 What is the onset of action, peak of action, and duration of action of rapid acting insulin preparation? Onset of action - > 15 minutes, usually around 5 Peak of action - peaks at 1 hour or 30-90 minutes Duration of action - about 3-5 hours What is the onset of action, peak of action, and duration of action of regular acting insulin preparation? Onset of action - taken around meal time 30-45 minutes before eating Peak of action - 3-4 hours Duration of action - 4-10 hours What is the onset of action, peak of action, and duration of action of each intermediate insulin preparation? Onset of action - 1-2 hours Peak of action - 4-10 hours Duration of action - 12-24 hours What is the onset of action, peak of action, and duration of action of long acting insulin preparation? Onset of action - 2-4 hours Peak of action - little to no peak Duration of action - 24 hours what is the onset of action, peak of action, and duration of Short acting insulin: Regular (humulin) Onset 30-45 minutes Peak 3-4 hours Duration 4- 10 hours what is the onset of action, peak of action, and duration of long acting insulin (Glargine/ Levemir or detemir) Onset 2-4 hours Peak (not documented) Duration up to 24 hours 2When changing from NPH to Glargine insulin, how will you adjust the patient's dose The initial dose of glargine is reduced by twenty percent to avoid hypoglycemia. Insulin glargine long-acting basal insulin analog given once daily to help control blood sugar levels. It consists of microcrystals that slowly releases insulin giving a long duration of action of 18 to 26 hours. Pharmacokinetic it resembles basal insulin secretion of a non-diabetic pancreatic beta cells. Insulin Glargine Lantus Why are ACE inhibitors the drug of choice and diabetic patients with hypertension They reduce the adverse effects of diabetes on the kidneys. ACE inhibitors slow the onset of diabetic nephropathy in patients with microalbuminuria and type 1 diabetes Why are ACE inhibitors the drug of choice in diabetic patients with hypertension? helps to decrease the effects that diabetes has on the kidneys because it affects the RAS system. Why are ACE inhibitors the drug of choice in diabetic patients with hypertension? -slow the onset of diabetic neuropathy in patients with microalbuminuria DM 1 -reduce the adverse effects of DM on the kidneys What are the side effects of insulin therapy? hypoglycemia and hypokalemia What are side effects of insulin therapy? Hypoglycemia (confusion, sweating, tachycardia, result in coma, seizures, cardiac arrhythmias, neurological deficits, and death)Ocular disturbance (presbyopia-blurry vision)weight gaindermatologic (lipohypertrophy or lipoatrophy)hypersensitivity What are side effects of insulin therapy? Hypoglycemia and diabetic ketoacidosis What assessment should be made before prescribing in any antihypertensive agent a thorough assessment of their liver and renal function. The real function especially for ace inhibitors and ACE receptor blockers which are primarily in the kidneys What assessments should be made before prescribing any antihypertensive agents? Race (d/t response=African Am. + Asian have higher risk of angioedema with ACE)DMHFAnginaIschemic heart disease What assessments should be made before prescribing any antihypertensive agent? If they have hyperglycemia because some drugs for HTN can make this worse What assessments should be made before prescribing any antihypertensive agent? BP Renal function (primary) head to toe assessment diet sodium intake electrolytes sodium level potassium levels 6. What's the most common adverse effect of ACE inhibitors? A dry, hacking cough. That's the most common reason to change treatment from an ace inhibitor to an ace receptor blocker. What is the most common adverse effect of an ACE inhibitor? associated with hypotension. tachyphylaxis with continued therapy. dry hacking cough What is the most common adverse effect of an ACE inhibitor? Hypotension is most common and can cause dizziness, headache, fatigue, orthostatic hypotension What is the mechanism of ACE inhibitors? systematic process triggered by kidneys due to low blood volume.begins w/ secretion of insulin from renal cortex. Once released renin cleaves off angiotensinogen 2 form Angiotensin-I it is then catalyzed by angotensin converting enzyme in pulm vasculature to angotensin 2 basil constrictor effects are > by ACE inhibition 9. What is the mechanism of action of calcium channel blockers Calcium channel blockers prevent or reduce the opening of calcium channels reducing the effects. What is the mechanism of action of calcium channel blockers block the influx of calcium by binding to channels and slow them down so they do not open as many or as fast and cause prolong vascular and smooth muscle relaxing What is the mechanism of action of calcium channel blockers? vasodilation: acting on vascular smooth muscle reducing contraction in the arteries and causing an increase in arterial diameter reduce the force of contraction by acting on cardiac muscles of the myocardium slow HR by slowing conduction of electrical activity reduce aldosterone production which lower BP by blocking calcium signals on the adrenal cortex (dihydropyridines): nifedipine and nicardipine mainly affect arterial vascular smooth muscle and lower blood pressure by causing vasodilation (phenylalanine): verapamil mainly affect the cells of the heart and have negative inotropic effects (strength of heart muscle), and negative chronotropic effects (how quickly heart beats) what effect do calcium channel blockers have on vascular smooth muscle they reduce contraction the arteries and causes an increase in arterial diameter a phenomenon called vasodilatations. Calcium channel blockers do not work on Venus smooth muscle what effect do calcium channel blocker have on cardiac muscles by acting on cardiac muscles or the myocardium they reduce the force of the contraction of the heart What effect do calcium channel blockers have on the electrical activity of the heart? by slowing down the conduction of electrical activity within the heart they slow down the heart rate; reducing the aldosterone production by blocking the calcium signals on the adrenal cortex allows calcium channel blockers to decrease after load decreases which in turn decreases how hard the heart pumps decreasing oxygen requirements (helpful in treatment of angina pectoris). what is the class of calcium channel blockers that affect arterial vascular smooth muscle dihydropyridines What is the effect of dihydropyridines? lower blood pressure by causing vasodialation which drugs are in the phenylalanine class of calcium channel blockers verapamil what is the effect of phenylalanine drugs affect the cells of the heart and have a negative inotropic and negative chronotropic effect what is a inotropic effect how strong the heart muscle works what is a negative chronotropic effect. controls how quickly the heart beats. what is a benzothiazepine class of calcium channel blockers Diltiazem What class does the following drugs belong to?:1) Nifedipine2) Amlodipine 3) Felodipine4) Clevidipine5) Diltiazem6) Verapamil 1. dihydropyridine 2. dihydropyridine3. 4.5.benzothiazepine6. phenylalanine What are the adverse effects of dihydropyridine-type calcium channel blockers reflex tachycardia which can be detrimental for patients with the ischemic symptoms because the resulting increase in myocardial oxygen demand. work on the vasculature and do not work on the heart. can worsen proteinuria + increase edema in hands and feet. What are the adverse effects of dihydropyridine-type calcium channel blockers? vasodilation effect (hypotension, dizziness, HA, syncope, decreased myocardial contractility, cough, SOB, congestion, and palpitations Peripheral edema, dysthymia, N/V, dry mouth, constipation Rare: sex dysfunction, gynecomastia, and hyperglycemia What are the adverse effects of dihydropyridine-type calcium channel blockers? due to good vasodilation they can cause pooling of the blood in extremities and also cause reflux tachycardia. What are the adverse effects of dihydropyridine-type calcium channel blockers? since they reduce SVR and arterial pressure they can cause vasodilation and hypotension which can lead to a reflex tachycardia this can be detrimental for patients with ischemic symptoms bc of the increase in myocardial oxygen demand can worsen proteinuria with patients with neuropathy which can increase edema in the hands and feet What are the adverse effects of statins rhabdomyolysis; you can also see an increased risk of diabetes and increase the liver enzymes the blood due to liver damage. Other possible adverse effects include cognitive loss, neuropathy, pancreatic and other hepatic dysfunction and sexual dysfunction What are the adverse effects of statins? cutaneous flushing (face + upper body)GI symptoms (dyspepsia, abdominal pain, diarrhea, flatulence, N/V)CholelithiasisConstipation d/t bile acid sequestrates What are the adverse effects of statins? myalgia with higher doses, GI disturbances What are the adverse effects of statins. main adverse reaction is rhabdomyolysis can also cause increased risk of DM increased liver enzymes in the blood due to liver damamge cognitive loss, neuropathy, pancreatic and other hepatic dysfunction, sexual dysfunction What patient education would you provide for client in which you have prescribed a statin Instruct the patient to report any muscle weakness or tenderness and dark urine to the provider immediately What patient education will you provide for a client in which you have prescribed a statin? Take as prescribed and do not miss a dose or double up on missed doses. Best taken in evening d/t action on cholesterol synthesis.Lovastatin take with foodatorvastatin take anytime and no regard to foodReport muscle pain and tenderness What patient education will you provide for a client in which you have prescribed a statin? Take it at the same time every day, if have a lot of GI upset can use fiber or CQ10. May interact with some antibiotics. Do not take them with grapefruit, or antacids What patient education will you provide for a client in which you have prescribed a statin? report any muscle weakness or tenderness and dark urine What patient education will you provide for a client in which you have prescribed a statin? take med as prescribed, do not skip or double doses, sequestrants taken before meals, mixed with liquid. take at bedtime, lovastatin take with food for improved absorption. niacin-flushing, aspirin. Sequestrants-stool softener, increased fiber muscle tenderness or pain, important to regular follow up to make sure effective and no adverse rx. P368. 15. What lipid disorders do bile acid sequestrants treat? cholestyramine or cholybar lowers plasma cholesterol levels. what is the mechanism of action of bile acid sequestrants? bile acid sequestrants which binds bile in the GI tract to prevent its reabsorption. removes bile acids from the body forming insoluble complexes with bile acids in the intestine then excreted in the feces. As a result of this loss of bile acids or plasma cholesterol is converted to bile acids in the liver to normalize levels. What would you recommend to a patient who is experiencing flushing with niacin therapy 300 mg of aspirin 30 min before taking niacin What would you recommend to a patient who is experiencing flushing with niacin therapy? Change to extended release.Take ASA, NSAIDs or COX-1 inhibitor 30 mins prior What would you recommend to a patient who is experiencing flushing with niacin therapy? gradually increasing initial low doses over a few weeks helps, taking ASA 325-650 range 30-60 minutes prior, with meals, or taking it at night. What would you recommend to a patient who is experiencing flushing with niacin therapy? take 300 mg of ASA a half hour before taking niacin flushing usually lasts 15-30 minutes although it can sometimes last up to 2 hours; accompanied by prickling or itching When changing from NPH daily to glargine insulin (Lantus), how will you adjust the patient's dose? The initial dose is not changed. How is amlodipine metabolized It's metabolized in the liver to inactive metabolites vs cyp3a4; grapefruit juice inhibits the cyp3a4 or 384 increasing the amount of amlodipine in the bloodstream. How is amlodipine metabolized? in the liver via the CYP 3A4 channel. Eliminated via the urine and feces. Binds to protein 93%, half-life is 30-50 hrs How is amlodipine metabolized? Metabolized by the liver to inactive metabolites vs CYP3a4 what is amlodipine used for Amlodipine is a medication used to treat high blood pressure and prevent chest pain; it can also be used for heart failure. what is amlodipine used for? atherosclerosis, hf what are the side effects of amlodipine peripheral edema, dizziness and palpitations, and flushing; common not dose-related: include fatigue, nausea, abdominal pain, and somnolence; and rare side effects include: blood disorders, impotence, depression, insomnia, tachycardia, gingival enlargement, hepatitis, and jaundice What are the side effects of amlodipine? photosensitivity, facial telangiectasia, hyperpigmentation. s/s of hypotension (dizziness, headache, syncope) that may cause HF. What are the side effects of amlodipine? Common dose related:peripheral edema, dizziness, palpitations, flushing Common not dose related: fatigue, nausea, abd pain, and somnolence Rare: blood disorders, impotence, depression, insomnia, tachycardia, gingival enlargement, hepatitis and jaundice When changing from NPH BID to glargine (lantus), how will you adjust the patient's dose? To avoid hypoglycemia the initial dose should be reduced by 20% and then adjusted based on patients response. what is the action of amlodipine By widening blood vessels, it lowers blood pressure What is the drug of choice in diabetic patients with hypertension? ACE inhibitors 4. What are the drug interactions with digoxin? Digoxin has potentially serious interactions with verapamil, amiodarone, erythromycin, and epinephrine as would be injected by a local with a local in the anesthetic. The digoxin level should be monitored while taking albuterol; need to monitor renal functions as it's excreted in the kidneys What are the drug interactions with digoxin? Drugs that cause hypokalemia, hypercalcemia or hypomagnesemia, antiarrhythmic, increase serum cg level, induce bradycardia. These include phenobarbital, Dilantin, rifampin, thiazide and loop diuretics, mezlocillin, piperacillin, What are the drug interactions with digoxin? Verapamil, Amiodarone, Erythromycin, Epinephrine (local), and Albuterol What is the mechanism of action of ACE inhibitors? Inhibits ACE activity which decreases production of angiotensin ii and aldosterone.Plays role in kinin-kallilrein-bradykinin system. What is the mechanism of action of ACE inhibitors? Breaks down bradykinin and reduces the effects it has on the system including dilation, smooth muscle contraction, increased vascular permeability, increased leukocyte chemotaxis What is the mechanism of action of ACE inhibitors? "PRIL": inhibit the conversion of angiotensin-1 to angiotensin-2, causing vasodilation, decreased aldosterone levels, Na+ and fluid wasting, and K+ retention what is the most common indication for digoxin? are a fib and a flutter with that rapid ventricular response although beta blockers and calcium channel blockers are a better first choice. what are the potential risks with using digoxin tentative evidence that digoxin may increase the risk of death. High ventricular rate leads to insufficient diastolic filling time. By slowing down the conduction of the AV node and increasing its refractory period digoxin can reduce the ventricular rate. How do you avoid nitrate tolerance long-term nitrate therapy regimens should be tailored to provide a 10 to 12-hour nitrate-free interval level when possible Warfarin Sodium (Coumadin) Contraindications Hemorrhage tendencies vitamin C or K deficiencies active peptic ulcer disease (GI bleed) Uncontrolled hypertension (promotes bleeding) Severe hepatic or renal disease (liver wont produce vitamin K and kidneys wont be able to clear it) Recent brain or spine surgery What is the mechanism of action angiotensin receptor blockers? Do not affect ACE activity but block the angiotensin ii receptor.Similar actions as ACEI on vasoconstriction and aldosterone secretion but no activity r/t bradykinin What is the mechanism of action angiotensin receptor blockers? They do the same thing as ACE only they do not break down the action to decrease it, they bind to the receptors so it cannot do its job. They do not affect bradykinin but affect the aldosterone secretion and do not affect cardiac output What is the mechanism of action angiotensin receptor blockers? Block the angiotensin II receptor -increasing vascular tone and stimulating vascular smooth muscle contraction; One of the greatest advantages-does not produce the dry, hacking cough that ACE inhibitors do. Angiotensin II receptor blockers (ARBs) help relax your blood vessels, which lowers your blood pressure and makes it easier for your heart to pump blood. Angiotensin is a chemical in your body that affects your cardiovascular system in various ways, including narrowing your blood vessels. This narrowing can increase your blood pressure and force your heart to work harder. Angiotensin II receptor blockers block the action of angiotensin II, allowing blood vessels to widen (dilate). What classes of medications are used in the treatment of congestive heart failure? ACE inhibitors, ARBs, BB, diuretics What classes of medications are used in the treatment of congestive heart failure? Diuretics are first line to treat HF. The most common are thiazine, aldosterone antagonists and loop. What classes of medications are used in the treatment of congestive heart failure? 1st line therapy due to reduced systolic function should include ACE inhibitors or ACE receptor blockers what type of drug is procainamide pharmaceutical anti arrhythmic agent used for medical treatment of cardiac arrhythmias classified as a 1a What is the mechanism of action of CCB (calcium channel blockers)? Calcium triggers smooth muscle contraction.Block the influx of calcium=decreasing trans-membranous calcium and prolonging vascular smooth muscle relaxation.Decrease after loaddecrease contractility and decrease SA and AV nodal conduction velocity what is procainamide used for used for both supraventricular and ventricular arrhythmias. For example, it can be used to convert new onset a-fib though it is sub- optimal for this purpose. must have adequate serum concentration. how is procainamide dosed Because of its short half-life it must be dose every three to four hours how should procainamide doses be taken? around the clock to keep even levels what are the side effects of procainamide may also lead to drug induced fever and other allergic responses. There is also a chance the systemic lupus erythematosus can occur, which at the same time leads to polyarthralgia, myalgia, and pleurisy—most of these side effects may occur due to the aestivation of procainamide. What are dihydropyridine-type calcium channel blockers? A greater degree of vasodilation than CCB causing sufficient reflex increase in sympathetic tone to overcome the negative inotropes. What are the side effects of CCBs? Lightheadedness, low BP, low HR, drowsiness, constipation, swelling of feet, ankles, legs, increased appetite, GERD, tender or bleeding gums, sexual dysfunction What lipid disorder do fibric acid derivatives treat? (Tricor) lipid lowering. Main action to decrease triglyceride levels. also reduce LDL and raise HDL What lipid disorders do bile acid sequestrants treat? Cholestyramin (Questran) Reduce LDL cholesterol levels. Bind to bile acids in intestines and prevent their reabsorption into the body Insulin aspart (novolog)Rapid-Acting Onset (h) 0.25Peak (h) 1-3Duration (h) 3-5Elimination in urine Insulin glulisine(rapid acting) Onset (h) 0.25Peak (h) 0.5-1.5Duration (h) 1-2.5Elimination in urine Lispro (Humalog)(rapid acting) Onset (h) 0.25Peak (h) 0.5-1.5Duration (h) 2-5Elimination ??? Regular (short-acting) Onset (h) 0.5-1 Peak (h) 2-4 Duration (h) 8-12 Elimination in urine NPH(intermediate acting) Onset (h) 1-1.5Peak (h) 4-12Duration (h) 24Elimination in urine Insulin glargine (Lantus) Long-acting Onset (h) 1.1Peak (h) 5Duration (h) 24Elimination in urine Insulin determirlong-acting Onset (h) 1.3Peak (h) 3-8Duration (h) 15.5-23.2Elimination in urine PZIlong acting Onset (h) 4-8Peak (h) 14-24Duration (h) 36Elimination in urine why should you choose a low dose colchicine vs a high dose? a) had a better treatment results after 24 hoursb) fewer adverse effects (diarrhea & N/V)c) "the lower dose the better" what are you going to address with gout? either uric acid build up or inflammatory response. what should you do the first time that some one might have gout and it isn't listed as a historical dx? they need a joint aspiration to confirm before it is diagnosed the first time. what issues are specific to probenecid and sulfinpyrazone ? blood dyscrasias bone marrow, anemia, hemolytic anemia, sulfa allergies what is the difference between macule rash vs papule? macules are flatpapules are raised what gout med, if it causes a rash could be deadly? allopurinol what foods should be avoided with gout? steak, alcohol, oxalate rich foods, shellfish, mushrooms, high purines, organ meats if someone has gout and heart failure what meds would you not want to give them NSAID but can give glucocorticoids in the joint. what meds should you use for gout if someone is on anticoags? colchicine. what parts of the body do glucocorticoids affect? metabolicant-inflammatorygrowth when is a time that you can stop steroids abruptly when on an oral instead of tapering it down? on an inhaled corticosteroid, and on the oral for less than 3 week. what effects do chronic steroid use have for diabetics and cardiac? insulin resistance, increased build up of cholesterol in blood vessels. what side effects can you have with NSAIDS? IGE with ibuprofen and hypersensitivity. if u mix indomethacin and asa what sx do you need to watch for tinnitus Identify the symptoms of hypoglycemia, hyperglycemia, and ketoacidosis Hypoglycemia: decreased LOC, hunger, sweating, weakness, dizziness, tachycardia, loss of vision, confusion. Ketoacidosis: drowsiness, dim vision, kussmaul respirations. Hyperglycemia: polyuria, polydipsia, sweet breath, weight loss, fatigue, dehydration. Identify the symptoms of hypoglycemia, hyperglycemia, and ketoacidosis. Hypoglycemia - dizziness, confusion, diaphoresis, and tachycardia Hyperglycemia - polyuria, polydispia, weight loss Ketoacidosis - fruity breath odor, rapid respiration's; neurological symptoms including lethargy, focal signs, and obtundation can progress to a coma What is the action of gliptin? Act on the incretin hormone system that is from the gut and stimulates glucose-dependent insulin secretion, enhances insulin gene transcription and insulin biosynthesis, enhances cellular transformation from pancreatic ductal tissues to beta cell tissues, increases beta cell mass by cellular exogenesis and proliferation, inhibits gastric empting and reduces appetite and food intake. What is the action of gliptin? -DPP-4 inhibitors; - Increases incretin levels which inhibit glucagon release, in turn increasing insulin secretion; -Decreases gastric emptying and blood glucose levels what can happen when someone is on metformin and get contrast dye? lactic acidosis. What are the adverse effects of propylthiouracil? Agranulocytosis and aplastic anemia. Drug induced hepatitis, abnormal hair loss, live failure is a black box warning. Less severe are drowsiness, HA, paresthesia, vertigo, diarrhea, nausea, arthralgia, itchy rash. Edema and localized pain, dry mouth. What are the adverse effects of propylthiouracil? fever and sore throat which can be fatal granulocytopenia or agranulocytosis - acna positive vasculitis; -temporary alopecia - rash - aplastic anemia - ARF What black box warning has the FDA issued regarding the administration of TZDs? Increased risks for heart failure and side effects of MI and angina are higher. What black box warning has the FDA issued regarding the administration of TZDs? Should be cautiously used because of the potential for cardiovascular problems. Close monitoring of heart failure signs and symptoms associated with a class effect of fluid retention. How does Celebrex differ from other NSAIDs? No GI issues since selective Cox2 Inhibitor what is the most difficult thing to get a diabetic to do to better their disease process? diet and exercise what type of diet is best for a diabetic medditerian Actions of Bile Acid Sequestrants Bind acids in GI tract. Not recommended for 1st line therapy ADR with high dose dihydropyridine (i.e. amlodipine)? Edema What do you monitor with Allopurinol? Monitor RFTs + LFTs (liver toxicity) prior and periodically.BUN, Serum Creatinine, CCr Monitoring with ACE inhibitors? Potassium=could cause hyperkalemia d/t renal function impairment Target HA1C <7% (last 120 days) what level if ha1c must you consider insulin? HA1C @9 what diabetic meds are way down the line because of their side effects? TZDs What lipid disorder(s) do bile acid sequestrants treat? helps to decrease high LDL those seen in cardiac patients What lipid disorder(s) do bile acid sequestrants treat? lower plasma cholesterol level by removing bile from the body by forming insoluble complexes with bile acids in the intestines which are then excreted in the feces What lipid disorder(s) do bile acid sequestrants treat? helps to decrease high LDL those seen in cardiac patients hyperlipidemia What lipid disorder(s) do fibric acid derivatives treat reduces triglyceride levels those with pancreatic issues. What lipid disorder(s) do fibric acid derivatives treat? mainly treat elevated triglycerides many times used in combination with statins; are also indicated for those who cannot tolerate statins increase HDL and lower triglycerides which seems to reduce insulin resistance when dyslipidemia is associated with other features of a metabolic syndrome like HTN and DM2 What lipid disorder(s) do fibric acid derivatives treat? hyperlipidemia *not suitable for patients with low HDL levels What are the side effects of the calcium channel blockers? hypotension, reflux tachycardia, GI disturbances, hyperglycemia, worse HF. What are the side effects of the calcium channel blockers? -Constipation -Headache -Palpitations -Dizziness -Rash -Drowsiness -Flushing -Nausea -Swelling in the feet and lower legs what do you need to be aware of when starting a fibexostat or allopurinol? can cause a gout attack unless you also put them on NSAID When changing from NPH to glargine insulin, how will you adjust the patient’s dose? Total the amount of insulin they are using in a day of NPH, divide that in half and that is your one time a day starting dose of glargine. The rest of the amount they have been taking is then spread out in the day of the NPH. P 562 Another maneuver can be to take 20% of the total dose and start there but not decrease the NPH When changing from NPH to glargine insulin, how will you adjust the patient’s dose? the initial dose of glargine is reduced by 20% to avoid hypoglycemia is it hyper or hypo for toxic goiter? hyper what is the most common s/e of ace inhibitors? cough if the patient has the cough from a ace what med then do you try for HTN? angiotensin receptor blocker s/e of ace inhibitor that can be life threating angioedema in airway when you inhibit angiotensin with an ace what does it do tot he body? less production of angiotensin II and aldosterone. Why is ACE inhibitors preferred with DM pts? Decrease risk of neuropathy than other meds What do you monitor before prescribing ACEI? RFTs and K what is a common issue with amlodipine? many interactions due to it attaching to a common receptor. what is a common se of amiodarone? hyper and hyperthyroidism. what do you administer before radioactive iodine? you need to increase TSH by stopping meds and let it increase it on own also can give thyrogen. What is Black Box warning of Metformin? Lactic Acidosis Fibrate Acids (Tricor) are used to treat? Decrease triglycerides in combo therapy with statins. With electrolytes to monitor with Amiodarone? K, Mg, Ca Why is Metformin the 1st line of DM2 treatment? bc doesn't cause hypoglycemia What tests prescribe prior to Radioactive Iodine therapy? TSH DM agent taken with first bite of meal? Acarbose (precose) what order do you use meds for chf? 1) loop2) ace3) arb4) arni (last)5) beta after stable what is a se of dihydropyridine when given in high doses? edema how are cox 2 different from other nsaids less risk of bleeding what is black box for metformin lactic acidosis, monitor RFT's what does fibric acid do to triglycerides? increase them what do you need to monitor with amioarone thyroid levels because t4 doesn't convert to t3 and K, Mg, Ca what effect do glistens have? dpp4 inhibitors, incretin system to have indirect effect to increase insulin production what is a contraindication with acarbose? bowel disease or renal impairment. normal BUN 24-29 normal creatinine .6-1.2 normal creatinine clearence 107-139 normal thyroid levels thyroxine: 4-11T4: 3.2-7.2 normal TSH normal hct & hmg 37-5412-18 normal phosphate 3-4.5 normal mg 1.3-2.1 explain how cox-2 meds help it is an inducible enzyme from pain. name the stages of gout 1) asymptomatic hyperuricemia2) acute gouty arthritis3) tophaceous gout (chronic disease) tx of gout 1) anti inflammatory2) xanthine oxidase inhibitors3) colchicine 4) joint hydrocortisones5) non weight bearing reduce wt and diet issues what do steroids do in the body labile emotions, decreased memory, increase cbg, stimulate gluconeogenesis in the liver, stimulate protein breakdown, decrease serum calcium levels s/s of asa od respiratory alkalosis, hyperpnea, tachypnea, n/v, hypokalemia, tinnitus, disorientation, irritability, seizures, dehydration, hyperthermia, thrombocytopenia. treatment for asa od induce vomiting, activated charchoal, acid-base balance, fluids, electrolyte levels, forced alkaline diuresis, sodium bicarb, sever would get dialysis what is the treatment of diabetic ketoacidosis acid-base balance/correction of acidosis, correction of hypotension via fluids, low dose reg insulin what insulins can you mix? clear to cloudy. do not mix U-500, LAI. RAI can be mixed with NPH stopping metformin b4 dye can cause lactic acidosis, hold 48 hours before especially with renal failure s/s of diabetic ketoacidosis drowsiness, dim vision, kussmaul respirations, why do you not want to give acarbose with gi or renal issues due to toxicity issues. how do glucagon -like peptide 1 agonist work? incretin system binds to this receptor in pancreatic beta cell to augment glucose mediated insulin release. this works well with hyperglycemia cuase helps to decrease insulin demand. What is the first line of defense for African Americans with HTN? Calcium Channel Blockers with HCTZ what drug interations do cardiac glycosides have? phenobarb, Dilantin, rifampin and dig are a no. calcium preps cause toxicity and stones, adlactone increases dig, beta andre cause bradycardia, thyroid meds can cause irrethmias, diuretics apt and steroids cause hypokalemia. what food does dig interact with ? bran what meds does dig interact with rifampin, sulfasalazine, st john wart what are nitrates used for? chf, htn what are beta blockers used for? chf, arrhythimas, atrial tachy, htn, stage fright, migrains, hyperthyroidism when are beta blockers used? pts with diastolic dysfunction or cardiomyopathy where redused hr can inprove cardiac output what are ace inhibitors used for? DM, chf, hyperlipidemia, htn when are ace inhibitors used? initial therapy or not relieved from diuretic or a diabetic what are direct renin inhibitors used for? htn what are statins used for hyperlipidemia, htn what are dihydropyridines CCB used for? HTN, isolated systolic htn, systolic hf, daynaud's disease, pvd what are vereapamil ccb used for? atrial tachy, htn, mitrains, mi what are diltiazem ccb used for? atrial tachy, dm, mi when in hctz used:? for volume overload initial therapy when are loop diuretics used? added therapy for decompensation when are angiotensin II receptor antagonis used? 1) cozaar, diovan, if intolerant to ace2) dig if not relieved from ace and diuretic3) hydralazine: with IMDUR for intolerance to ace4) imdur: with HCTz for intolerance to ace when are aldosterone antagonist used? diastolic HF what CCB are used for htn? Norvasc, Cardizem, felodipine, isradipine, cardene, Procardia, verapamil what ccb are used for angina? verapamil er and short acting, Norvasc, Cardizem short, cd, er, cardene, nifedipine/procardia what ccb has strongest negative inotropic effect? verapamil what should you monitor with procainamide? dyspnea, JVD, peripheral edema/s/s of chf what side effects does amiodarone have? dizziness, avoid hot showers what s/s of rabdo are there if statins cause? dark urine, muscle weakness. what dose should ccb be started at? 1/2 regular dose. 1. What is tiotropium used to treat? Tiotropium (Spiriva) is used to treat COPD and bronchospasm (Chronic bronchitis and emphysema). 1. What is tiotropium used to treat? Tiotropium (Spiriva) is used to treat COPD and bronchospasm (Chronic bronchitis and emphysema). Anticholinergic bronchodilator 2. What are the adverse effects with montelukast (Singular)?erm Neuropsychiatric effects include depression, anxiety, and suicide. A rapid conversion from steroids to montelukast may cause Churg- Strauss Syndrome. Signs and symptoms of Churg-Strauss syndrome include weight loss, flu-like symptoms, and pulmonary vessel inflammation 2. What are the adverse effects with montelukast (Singular)?erm Neuropsychiatric effects include depression, anxiety, and suicide. A rapid conversion from steroids to montelukast may cause Churg- Strauss Syndrome. Signs and symptoms of Churg-Strauss syndrome include weight loss, flu-like symptoms, and pulmonary vessel inflammation. Diarrhea, Laryngitis, Pharyngitis, Nausea, Sinusitis, Viral Infection 3. What patient teaching should accompany the prescription of montelukast (Singulair)? To take as prescribed, these medications are not for acute episodes of asthma. Patients are not to decrease or discontinue any other asthma medications without talking with their provider. Pregnant or nursing women should not take these medications. 3. What patient teaching should accompany the prescription of montelukast (Singulair)? To take as prescribed, these medications are not for acute episodes of asthma. Patients are not to decrease or discontinue any other asthma medications without talking with their provider. Pregnant or nursing women should not take these medications. St John's Wart -> Decrease serum levels 4. What patient teaching should be provided when prescribing inhaled corticosteroids? Use a spacer, wait at least a minute in between puffs, patients need to rinse their mouth after administration to prevent oral candidiasis. 4. What patient teaching should be provided when prescribing inhaled corticosteroids? Use a spacer, wait at least a minute in between puffs, patients need to rinse their mouth after administration to prevent oral candidiasis. Use decongestant drops prior to use. Monitor for signs of Respiratory Infection. Continue to take med -> may take 2-3 weeks to reach effective level. 5. What ethnic background should not be prescribed long-acting beta agonists? African Americans, increased incidence of death in this population 6. What medication would you prescribe for bronchospasm for a patient taking propranolol? Ipratropium bromide (Atrovent) 6. What medication would you prescribe for bronchospasm for a patient taking propranolol? Ipratropium bromide (Atrovent); Salmeterol 7. What is the mechanism of action of albuterol? Selectively binds to beta 2 adrenergic receptors, resulting in bronchodilation. 7. What is the mechanism of action of albuterol? Selectively binds to beta 2 adrenergic receptors, resulting in bronchodilation. Relaxes smooth muscle in bronchial tree and peripheral vasculature. Redistribution; intracellular shift (hyperkalemia 8. What is the mechanism of action of inhaled corticosteroids? Anti-inflammatory: They inhibit the immunoglobulin E (IgE) and mast cell–mediated migration of inflammatory cells into the bronchial tissue producing smooth muscle relaxation. 9. When is it appropriate to use a short acting beta agonist? Used for acute symptoms of shortness of breath. 9. When is it appropriate to use a short acting beta agonist? Used for acute symptoms of shortness of breath. Prevention of exercise-induced bronchospasm an effect begins almost immediately (within 5 minutes), peaks in 30-60 minutesShort-term control of bronchospasm due to reversible airway disease. Used for quick relief - considered "reliever" or rescue medications. Most effective drugs available for relief of acute bronchoconstriction and bronchospasm associated with asthma and COPD 9/1/2020 StudyBlue printing of GRNU 615 Study Guide (2016-17 Frandsen) 10. What is the mechanism of action of inhaled muscarinic receptor antagonists (Anticholinergic bronchodilators)? The medication binds to the muscarinic receptors, resulting in the drying up of secretions and the dilation of the airway. Examples include tiotropium bromide (Atrovent) and Tiotropium (Spiriva). 11. What are the adverse effects associated with inhaled corticosteroids? All of the inhaled corticosteroids have associated xerostomia, hoarseness, tongue and mouth irritation, flushing, and dysgeusia (altered taste sensation). Oral candidiasis 12. What special populations should not be prescribed pseudoephedrine? Pseudoephedrine is no longer recommended for use in children younger than 4 years, but if prescribing, the dose of pseudoephedrine is 4 mg/kg per day divided in four-times-a-day doses. 13. What drug should be prescribed for a patient with nasal congestion with hypertension? Claritin, Zyrtec, any second generation antihistamine, Flonase, Oceans Spray. Cloricidin HBP 14. What are the adverse effects of antihistamines? First generation antihistamines: Sedation, dizziness, tinnitus, lassitude, disturbed coordination, fatigue, headache, irritability, nervousness, blurred vision, diplopia, tremors, dry mouth, urinary retention, and dysuria. 15. What conditions should cause a patient to avoid the use of antihistamines? Patients with a predisposition to urinary retention, history of bronchial asthma, increased intraocular pressure, hyperthyroidism, cardiovascular disease, or hypertension should exercise caution due to the anticholinergic effects. Any conditions using CNS depressants. 16. What is the mechanism of action of codeine in the suppression of a cough? Codeine works as an antitussive through direct action on receptors in the cough center of the medulla, at lower doses than is required for analgesia. 17. Which medications are considered antitussives? Antitussive are also called “cough medicine”, which include: dextromethorphan, codeine, and benzonatate. 7. How are upper respiratory infections treated? Decongestants, expectorants, antitussives (cough medicine) When using the “Step-Up” approach in caring for patients with GERD, the “step up” from OTC antacid use is:A.Prokinetic (metoclopramide) for 4 to 8 weeksB.Proton pump inhibitor (omeprazole) for 12 weeksC.Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeksD.Cytoprotective drug (misoprostol) for 2 weeks DefinitionC.Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks When using the “Step-Up” approach in caring for patients with GERD, the “step up” from OTC antacid use is:A. Prokinetic (metoclopramide) for 4 to 8 weeks B. Proton pump inhibitor (omeprazole) for 12 weeks C. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks D. Cytoprotective drug (misoprostol) for 2 weeks C. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks A patient presents to the clinic with a temperature of 101 oral, feeling “achy” all over, fatigue, sore throat, cough and headache. The patient reports these symptoms have been persistent for 24 hours. What drug would be indicated?A) Tamiflu B) Pseudoephedrine C) Solu-Cortef D) Prednisone A: Tamiflu; this patient is exhibiting strong s/s of the flu. Tamiflu must be started within 48 hours of symptom onset so this patient is within the window to begin treatment. Which OTC medications should be used in extreme caution when taking beta blockers?A.TylenolB.Cold medicationsC.Eye dropsD.IBU B. Cold medications When is it safe to give an antihistamine during pregnancy? Which one should be prescribed if one is given? a) Anytime during the pregnancy, they are safe b) Never- they are Category D c) Third trimester- they have no risk d) First and second trimester- less likey to cause seizure activity in the fetus d) Antihistamines should not be given in the third trimester of pregnancy related to the increase potential for seizures in the fetus. What conditions contraindicate the use of albuterol?a. Left ventricular heart failure b. Narrow-angle glaucoma c. COPD d. Diabetes b. Beta 2 agonist are not recommended in patients with narrow-angle glaucoma 1. Janice Monroe, 22 year old female that is 24 weeks pregnant comes to the office for evaluation of her asthma symptoms. As the nurse practitioner you discuss how to monitor her symptoms and prescribe which drug? a. Terbutaline b. Montelukast; Singulair c. Prednisone injection d. Inhaled corticosteroid: budesonide Correct Answer D: (Woo & Wynn, pg 1008). Long-term control medication of choice. The inhaled corticosteroid has the most data available in pregnant woman. What is considered the “Hallmark of Asthma” a. Airway Hyperresponsiveness b. Airflow Obstruction c. COPD A – Airway hyperresponsiveness is a hallmark of asthma, which leads to wheezing, dyspnea, and chest tightness. A patient is at home with complaints of an asthma exacerbation. What would be the first line drug to help treat this condition? a. Inhaled corticosteroid b. Inhaled beta2 agonist c. Theophylline B – An inhaled beta2 agonist is the first line treatment in acute asthma attack after the patient determines severity. In asthmatic’s lungs, inflammatory changes are controlled by all of the following medications except: a. Cryomolyn sodium inhaler (Intal) b. Triamcinolone (Azmacort) c. Albuterol inhaler (Proventil) d. Montelukast (Singulair) c. Albuterol (Proventil) is a short-acting bronchodilator used as a rescue medication for shortness of breath. It’s method of action is to dilate the tubes in the lungs. Whereas the remaining medications contain leukotrienes and steroids and are therefore preventative medications 1. What of the following drugs should the Nurse Practitioner consider as a first line treatment for allergic rhinitis? A. Flonase B. Medrol Dose Pack C. Albuterol D. Benadryl A. Nasal corticosteroids are “used to manage the inflammatory response associated with seasonal or perennial allergies” (Woo & Wynne, 2012, p. 414). None of the nasal corticosteroids are more preferred than the other; therefore the choice ultimately lies with patient and prescriber preferences. What is the rational for advising patients not to smoke while taking Theophylline? A. Taking Theophylline increases the patient’s risk for respiratory side effects B. Nicotine competes for receptors with Theophylline C. Theophylline levels may be increased when patients smoke D. There is an increased risk for cardiovascular side effects C. Theophylline levels may be increased when patients smoke and should be closely monitored if patients smoke while taking theophylline. This includes nicotine replacement products such as gum, patches, or lozenges. are absolutely contraindicated for patients on concurrent MAOI therapy? A. Oral Decongestants B. Antihistamines C. Corticosteroids D. Respiratory inhalants D. oral decongestants are contraindicated in concurrent therapy with MAOI therapy because they can result in severe headache, hypertension and hyperpyrexia, and possibly hypertensive crisis You are caring for a 24 weeks pregnant woman that is in need of long-term control of her asthma. You are going to prescribe an inhaled corticosteroid. Which of the choices below would be best prescribed? A. Beclomethasone (QVAR) B. Budesonide (Pulmicort) C. Flunisolide (AeroBid) D. Fluticasone (Flovent) B. Budesonide (Pulmicort) has more available data for use in pregnancy You are caring for Joey, a 4-year-old child that has been diagnosed with asthma. According to the Stepwise approach for managing asthma long-term in children, what should be the first step in managing this child? A. Medium-dose inhaled corticosteroid (ICS) B. Low-dose inhaled corticosteroid (ICS) C. Cromolyn or Montelukast D. Short acting beta2 agonist (SABA) PRN D. According to the Stepwise Approach for managing Asthma Long Term in Children, 0-4 Years of Age and 5-11 Years of Age (2007), the first step for managing Joey’s asthma would be a SABA as needed Mr. Ray is a 68-year-old farmer. He is at the clinic today because he has a non-productive cough that he just can’t seem to get to subside and he wants something to help. He has a known medical history of asthma and Parkinson’s. His medications consist of Azilect daily and Advair twice a day. What cough preparation would you prescribe as the primary care provider for Mr. Ray? A. Dextromethorphan B. Codeine C. Benzonatate D. Guaifenesin D. Antitussives such as dextromethorphan, codeine and benzonatate, should not be used for asthmatic cough, which is not ruled out in Mr. Ray’s case. Antitussives should also NOT be taken concurrently with MAOIs, of which Azilect belongs in this drug class. The best choice within this category of preparations would be guaifenesin for Mr. Ray’s non-productive cough 19. What patient education should be provided to the patient taking antacids? Antacids should be taken 1 to 3 hours after meals and at bedtime. Aluminum- and calcium-based antacids may cause constipation. Magnesium-based antacids may cause diarrhea. They often include avoiding: smoking, flat-lying body position while sleeping, foods that increase acid. 20. What is the action of loperamide? Loperamide binds to the opiate receptors of the intestinal wall, leading to slowed gastric motility. It also reduces fecal volume, increases viscosity and bulk, and diminishes the loss of fluid and electrolytes. 21. What are the adverse effects of bismuth subsalicylate? Gray/black stools and black tongue, the results of the bismuth. Patients should be told to expect this reaction and that it does not indicate GI bleeding. 22. What special population should not be administered bismuth subsalicylate? Avoid bismuth subsalicylate in pediatric patients with influenza or chicken pox because of the risk of Reye syndrome. 23. When should bismuth subsalicylate be administered? When a patient has acute diarrhea. 24. What lab values should be monitored with long-term administration of proton pump inhibitors? Pts should be tested for H. pylori infection. Therapy should be stopped two weeks before urea breath testing-Can lead to the false-negative result. 25. Why is osteoporosis a risk when taking omeprazole Calcium deficiency can result from omeprazole, therefore increasing a patient's risk for osteoporosis. 26. What is the most rapid-acting laxative and why? Stimulants due to the direct action on intestinal mucosa by stimulating the mesenteric plexus. Drugs in the stimulant class include cascara, senna, bisacodyl, and castor oil. 27. How does metoclopramide improve GERD? The principal effect of metoclopramide in the management of GERD is on symptoms of postprandial and daytime heartburn. For adults, if symptoms occur throughout the day, a dose of 10 mg taken 30 minutes prior to each meal and at bedtime is recommended. 28. What is the Step-Down Approach with GERD? Start with lifestyle modifications and PPI for 8 weeks. If symptom free for 4 weeks, step down to H2RA. If symptoms not relieved, increase PPI to BID for 4-8 weeks. If symptom free for 4 weeks, step down to daily PPI and reassess in 6-12 months. 29. What is the Step Up Approach with GERD? First antacids, lifestyle & OTC antacids, H2 receptor agonists and proton pump inhibitors (If no errosive disease present) 4-8 weeks. If better go back to H2 receptor agonists, if worse continue treatment and make a referral. 30. What is the first line therapy for peptic ulcer disease with a positive H. pylorus? PPI and antimicrobial therapy; Acid suppression by the PPI in conjunction with the antimicrobial helps alleviate the ulcer-related symptoms, heals the gastric mucosal inflammation, and may enhance the efficacy of the antimicrobial agents against H pylori at the mucosal surface. 31. How will you treat nausea and vomiting First-generation antihistamines with strong anticholinergic properties bind to central cholinergic receptors and produce antiemetic effects, decreasing nausea and vomiting. The antiemetic drugs in this class are dimenhydrinate, diphenhydramine, hydroxyzine, and meclizine. 32. How will you treat constipation in children? Bulk form laxatives are the safest and produces physiologic effect similar to increasing fiber in the diet. Bulk-forming are used for management of chronic diarrhea in adults. Lactulose can be administered to children if bulk is ineffective. Dose is 7.5mL every day. 33. What are the disadvantages of using stimulant laxatives for prolonged periods of time? Abuse and dependency 34. What is the mechanism of action of the phenothiazine anti-emetics? Phenothiazines block dopamine receptors in the chemoreceptor trigger zone (CTZ). They also bind to and block cholinergic, alpha1- adrenergic, and histamine1 receptors. Examples include prochlorperazine and promethazine. 35. What is the mechanism of action of docusate sodium? They reduce the surface tension of the oil–water interface on the stool and facilitate admixture of fat and water into the stool, producing an emollient action. 36. What is the mechanism of action of proton pump inhibitors? Proton pump inhibitors suppress gastric acid secretion These drugs reduce H+ secretion by inhibition of the H +/K+/ATPase enzyme system at the secretory surface of the parietal cell itself to block the final step in H+ secretion. 37. What is the mechanism of action of ondansetron? Ondansetron blocks 5-HT3 in the central nervous system in the chemoreceptor trigger zone and in the peripheral nervous system on nerve terminals of the vagus nerve. 38. What are the contraindications to the use of misoprostol? Renal impairment and adults older than 65 years of age. It may cause abortion, premature birth, or birth defects. Uterine rupture has been reported in women who were administered misoprostol to induce labor. 39. How will you choose a diuretic in the treatment of hypertension? Based kidney function. GFR rates higher than the mid -40 mL/min range=Thiazide, GFRs less than the mid-40 mL/min =Loop diuretics, All classes of diuretics have been used to treat HTN, but the best results are with thiazide-type diuretics. 40. Mechanism of action of loop diuretics The loop diuretics inhibit sodium reabsorption in the ascending loop of Henle. These drugs are short-acting and cause a large natriuresis. Loop diuretics increase potassium excretion . 41. Mechanism of action of thiazide diuretics The thiazide-type diuretics act on the distal renal tubule to inhibit sodium reabsorption. Their effect is generally longer-lasting, and they cause less brisk diuresis. Both of these classes increase potassium excretion. 42. Mechanism of action of potassium sparing diuretics The potassium-sparing diuretics include aldosterone antagonists and agents like amiloride that inhibit excretion of potassium distally. These agents are weak diuretics, often used in combination with thiazides to reduce potassium loss. A nurse is having difficulty hearing differences while percussing over lung fields. What should the nurse do? Increase pressure on the finger in contact with the patient’s skin A nurse is testing the deep tendon reflexes of a preschool-aged child. What is the appropriate instrument to use to check the patellar reflex Examiner’s finger When does the nurse use inspection during a health assessment When the examiner sees the patient and continuously throughout the examination Which position is commonly used to conduct a pelvic examination of a female patient? Lithotomy Which part of the hand is most sensitive and used in performing palpation Finger pads A nurse is performing percussion while examining a patient. Over which body organ would the examiner expect to hear tympany Stomach hyperresonant sounds are heard where? Lungs Dull sounds are heard over organs liver and kidneys What is the purpose of using a monofilament during a physical examination Determine the ability to perceive sensation in the feet A reflex hammer is used to elicit deep tendon reflexes ophthalmoscope is used to exam the fundus of the eye. A goniometer is used to measure joint range of motion. A nurse uses an electronic sphygmomanometer during an examination. Further assessment is needed to obtain which data? Pulse rhythm electronic sphygmomanometer displays what vitals? display the pulse rate and the systolic and diastolic blood pressure readings The nurse plans to test the client’s tympanic membrane for compliance. Which piece of equipment is required to perform this task otoscope with a pneumatic attachment is used to inject air while the examiner observes movement of the tympanic membrane in the ear. Sclera A dense, avascular structure that appears anteriorly as the white of the eye. Cornea The anterior sixth of the globe. It is continuous with the sclera. Choroid The thin, highly vascular membrane that covers the posterior five sixths of the eye between the retina and sclera. Retina The sensory network of the eye. It transforms light impulses into electrical impulses, which are transmitted through the optic nerve to consciousness in the cerebral cortex. Pupil The opening in the form of a circle in the iris of the eye. It lies behind the cornea and in front of the lens. It is the window of the eye through which light passes to the lens and the retina. Lens A cellular structure that contains crystalline matter located behind the iris. Iris muscle A circular, contractile muscular disc that contains pigmented cells that produce the color of the eye. Contracture or relaxation of the iris muscle permits variation in the amount of light entering the eye. Conjunctiva A thin membrane that covers most of the anterior surface of the eye and the surface of the eyelid in contact with the globe. Ciliary muscle This muscle changes the shape of the lens so that light focuses on the retina. Anterior chamber The chamber of the eye between the cornea and the iris. It contains the aqueous humour. Central retinal artery & vein A primary blood supply to and from the eye. Medial rectus muscle The muscles that move, when contracted, to rotate the eye toward the nose. Lateral rectus muscle The muscles that move, when contracted, to rotate the eye toward the ear. Vitreous body A clear jelly-like substance contained in a thin membrane that fills the space behind the crystal-like lens of the eye. Retinal artey The vessel that supplies arterial blood to the eye. Retinal vein A vessel that drains venous blood from the eye. Optic nerve The second cranial nerve that starts in the retina, travels through the thalamus, and joins with the visual cortex at the back of the brain. The visual cortex works to sense light, shade, and color, and to decode the nerve signals from the retina. Xanthelasma A soft, yellow spot or plaque that usually occurs in groups around the eyelids. Subconjunctival hemorrhage Bleeding under or into the conjunctiva of the eye. Severe papilledema Swelling of the optic disc caused by increased intracranial pressure. Arcus senilis A dull-looking grey or white ring that surrounds the edges of the cornea of the eye. Caused by deposits of fat in the cornea or by breakdown of tissue Acute purulent conjunctivitis Swelling in the surface of the eye due to allergy or infection. Corneal ulcer Disruption in the corneal epithelium and stroma caused by bacterial or viral infection or by physical injury. Diabetic retinopathy (proliferative) A disorder in the blood vessels in the retina of the eye. This occurs most frequently when diabetes is poorly controlled. Repeated bleeding may lead to partial or complete blindness Which test assesses a patient’s peripheral vision Confrontation test What is the common cause of a hordeolum? nfection due to Staphylococcus aureus Pterygium is an abnormal growth of the conjunctiva caused by exposure to ultraviolet light. Which instruction is given to a patient for the Snellen test Testing will be done with and without the corrective lens Which finding during an ophthalmoscopic examination suggests the patient has hypertension Narrowed retinal arteries Which condition of the eye is associated with impaired vision? Corneal scar Which patient concern suggests the development of a cataract? Poor night vision The nurse asks the patient to close his eyes and gently palpates the eyes simultaneously. This is a screening test for which condition? Open-angle glaucoma An increased number of drusen in the macular area are noted on ophthalmoscopic examination. What action should follow? Ask the patient to self-test using the Amsler grid.An increased number of drusen (benign degenerative deposits) suggests the development of macular degeneration The nurse begins the eye exam using an ophthalmoscope. What is observed? Examining the Retina 1 Red reflex Which finding on the assessment of a patient’s eye suggests hyperthyroidism? Positive eyelid lag assessment finding Fine tremor noted when patient shuts eyes Using a nasal speculum, the nurse observes the nasal mucosa to be blue-gray in color. With what is this finding associated? Allergy The nurse palpates the areas of the skull behind the ears and is able to identify the mastoid processes, which are nontender. What is the significance? This is a normal finding. Which description is correct regarding the use of the otoscope on an adult? Use the largest speculum that fits comfortably in the patient’s ear.The otoscope is held with the handle up. The pinna of the adult ear should be pulled upward during insertion Which finding upon inspection of the external ear is considered normal? Darwin tubercle is small painless nodules atop the helix that are a normal finding Which finding is considered normal when visualizing the tympanic membrane? Visible handle of malleus.The normal tympanic membrane is pearly gray in color, and the light reflex is visible in the anteroinferior quadrant. White patches are scar tissue from previous ear infections. What condition of the oral mucous membranes is characterized by thickened white patches that cannot be wiped away Leukoplakia Which is the most exact testing of hearing acuity? Pure tone audiometry Chronic insufflation of cocaine is associated with which assessment finding? Perforated nasal septum Which finding is associated with Meniere disease? (Select all that apply.) Vertigo Tinnitus Hearing loss Which sinuses are accessible to palpation during physical examination? (Select all that apply.) Frontal Maxillary Select the correct description of S2, the second heart sound. Corresponds to the “dubb” sound A patient has a holosystolic murmur. Which statement is correct about this murmur? The sound is heard with mitral regurgitation A ventricular heave is detected by which assessment technique? Palpation What effect on the radial pulse is a usual finding for a client with atrial fibrillation There is a fluctuation in strength and quality of the pulse The nurse hears a pericardial friction rub while listening to heart sounds. Which characteristic is correct about this sound Occurs throughout the heart sound cycle. The sound is enhanced when the patient holds their breath on expiration while sitting up and leaning forward. When does the nurse expect to hear an S4 heart sound Just before S1. It may be present with S3 or heard without S3. Where is the point of maximum impact heard in most normal adult patients Fifth intercostal space midclavicular line The nurse auscultates heart sounds of a client with a heart rate of 110 beats/min. What should the nurse do to identify which sound is S1 Determine which sound is louder with inspiration. During which segment of the electrical conduction of a heartbeat does ventricular systole occur? QRS How does a nurse convey courtesy to a patient during an appointment Knocking on the door before entering From a questionnaire the patient completed, the nurse learns that the patient uses illicit drugs. What technique is appropriate to explore this health concern during the interview? Reassure the patient that all information will be kept confidential. A patient must wait 45 minutes after the scheduled appointment time because the office is running late. Select the best way the nurse should address the issue Thank the patient for his patience. A patient tells the nurse that his wife, who is the patient’s caregiver, becomes irritable when more assistance is needed. How should the nurse respond to the patient initially Ask the patient how he feels when his wife becomes irritated. Health care professionals discuss that a patient obtains secondary gain from an illness. What is meant by secondary gain from an illness Attention and caring from others because of the illness A patient is curt, avoids eye contact, and states that he does not know why he bothered to seek medical attention. How should the nurse address this behavior? Tell the patient he seems angry and ask him to state his concerns Which communication technique is most appropriate to use while conducting an interview with a patient? Use active listening techniques, including clarification and reflection What is the goal of using a screening tool during a patient health history interview To determine if the patient has a problem related to the issue Research findings show that a family history for which conditions increases the risk to develop diabetes type 2 and cardiovascular disease? (Select all that apply.) Obesity Dyslipidemia Select the data included in a sexual history. (Select all that apply.) Sexual partners Sexual practices Methods used to prevent pregnancy Past history of sexual transmitted infections Protection used against sexual transmitted infections Select the best way a nurse demonstrates cultural competence in communication during a health examination. Listening and allowing time to understand and be understood Which is the best method to determine what culture a patient identifies with? Ask the patient if there is an ethnic group he or she identifies with A patient from an ethnic minority culture comes to a clinic appointment accompanied by two other persons of the same ethnicity. How should the nurse approach the people with the patient? Introduce oneself, greet them and the patient, and find out their relationship Which is the best way a health care provider can become culturally competent? Be respectful and open to understanding the ways of all patients A patient belonging to a specific ethnic group tells the nurse that she has been eating cold foods since developing a respiratory infection last month. What does the patient mean? An infection is a hot disease, so treatment includes foods that are cold. Which is good practice when the nurse communicates with patients from other cultures? Allow time for greeting exchange at the beginning and ending of encounters. An ethnic minority client comes to the health clinic. The client does not speak or understand the language of the health care provider. What should the health care provider do? Obtain the services of a trained translator to be present during the examination. Select the best manner to address the use of home remedies by a patient. Tell me how you have been treating this and how it has been working. Which of the characteristics are considered to be components of a patient’s cultural identity? (Select all that apply.) Gender Religion Sexual orientation A patient who eats traditional Hispanic foods is prescribed a diet that is low in saturated fat and low in sodium. How should the nurse intervene to assist the patient? (Select all that apply.) Include the person who prepares meals in teaching. Refer to and inform the dietician of patient’s ethnicity and new diet. Discuss how traditional foods can be modified to lower fat and sodium what does 20/30 vision mean If you have 20/30 vision, that means what you see comfortably at 20 feet, can be seen by a person with "normal" vision at 30 feet. Cardinal field of gaze assess for? - extra-ocular muscle function test the cranial nerves CN III, IV, VI. What are grades for pulses? 4+ bounding3+ full, increased2+ normal1+ weak, thread0 absent Stenotic valve narrowed valve turbulent flow=murmur incompetent valves A regurgitant (incompetent, insufficient, or leaky) valve does not close completely, letting blood move backward through the valve. Sclerotic valve valve thickening (sclerosis) without stenosis is common in elderly adults. It is often detected either as a systolic murmur murmur grades 1.) very soft2.) soft3.) moderate4.) mod loud- can feel thrill 5.) very loud-steth sideways 6.) extremely loud-steth off chest and still hear Tonsil grading 1+ or 2+ in HEALTHY 3+ touching uvula 4+ touching each other - both 3 ,4 mean possible accute infection PMI (apical pulse) pulse of maximal impulse 5th intercostal space at midclavicular line. S3 heart sounds is a low-frequency, brief vibration occurring in early diastole at the end of the rapid diastolic filling period of the right or left ventricle gallop S4 heart sounds is a low-pitched sound coincident with late diastolic filling of the ventricle due to atrial contraction. occurs shortly before the first heart sound. Heart sounds are created by? The “ lub” is the first heart sound, S1, caused by turbulence caused by the closure of mitral and tricuspid valves at the start of systole. The second sound,” dub” or S2, is caused by the closure of aortic and pulmonic valves, marking the end of systole. How to assess for sinus tenderness? Use thumbs over sinus and maxillary Rinne test 1) Test compares air and bone conduction hearing.2) Strike a 512 Hz tuning fork softly.3) tuning fork on the base of the mastoid bone.4) pt to tell you when the sound is no longer heard.5) Note the time interval6) PT to tell you when no lonnger heard..7) Note the time interval and findings Ear assessment of a child the pinna of a child under 2 years of age is pulled downward Ear assessment in adult with the otoscope Pull the pinna UP and BACK How do you assess for accommodation and convergence? Hold finger out in front of nose and bring towards nose, testing for eyes to go inward and pupils to dilate What is the Rosenbaum test Numbers on a card checks for near visual acuity used after cataract surgery Unilateral Pitting Edema (Local) - lymphedema - venous insufficiency - cellulitis - abscess - osteomyelitis - DVT - Tourniquet Bilateral Pitting edema CHFCirrhosisRenal FailurePericardial EffusionNephrotic Syndrome Claudication Pain caused by a decrease of blood flow. Improves with rest. Carotid pulse coincides with what heart sound? S1 thrill vibration accompanying a murmur carotid bruit turbulent blood flow heard from ausculating over the carotid artery. due to narrowing in the artery. Test eyes for peripheral vision use the confrontation test How should you adjust the lens of your ophthalmoscope if the pt is hyperopic (farsighted)? rotate the lens disc clockwise to the plus diopters How should you adjust the lens of your ophthalmoscope if the pt is myopic (nearsighted)? rotate the lens disc counterclockwise to the minus diopters The choice of diuretic to use in treating hypertension is based on: A. Presence of diabetes with loop diuretics being used for these patients B. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40 mL/min range C. Ethnicity with aldosterone antagonists best for African Americans and older adults D. Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL B. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40 mL/min range Furosemide is added to a treatment regimen for heart failure which includes digoxin. Monitoring for this combination includes: A. Hemoglobin B. Serum potassium C. Blood urea nitrogen D. Serum glucose B. Serum potassium Education of patients with COPD who use inhaled corticosteroids includes: A. Doubling dose at the first sign of a URI B. Use their inhaled corticosteroid first and then their bronchodilator C. Rinsing mouth after use D. They should not smoke for at least 30 minutes after using C. Rinsing mouth after use Patients with COPD require monitoring of: A. Beta-2-agonist use B. Serum electrolytes C. Blood pressure D. All of the above A. Beta-2-agonist use Patients with a COPD exacerbation may require: A. Doubling of inhaled corticosteroid dose B. Systemic corticosteroid burst C. Continuous inhaled beta-2-agonists D. Leukotriene therapy B. Systemic corticosteroid burst Medications used in the management of patients with COPD include: A. Inhaled beta-2-agonists B. Inhaled anticholinergics (ipratropium) C. Inhaled corticosteroids D. All of the above D. All of the above One goal of asthma management in children is: A. They independently manage their asthma B. Participation in school and sports activities C. No exacerbations D. Minimal use of inhaled corticosteroids B. Participation in school and sports activities Oral terbutaline B. Prednisone C. Inhaled corticosteroids (budesonide) D. Montelukast (Singulair) C. Inhaled corticosteroids (budesonide) Patients who are at risk of a fatal asthma attack include patients: A. With moderate persistent asthma B. With a history of requiring intubation or ICU admission for asthma C. Who are on daily inhaled corticosteroid therapy D. Who are pregnant B. With a history of requiring intubation or ICU admission for asthma Asthma exacerbations at home are managed by the patient by: A. Increasing frequency of beta-2-agonists and contacting their provider B. Doubling inhaled corticosteroid dose C. Increasing frequency of beta-2-agonists D. Starting montelukast (Singulair) A. Increasing frequency of beta-2-agonists and contacting their provider Monitoring a patient with persistent asthma includes: A. Monitoring how frequently the patient has a URI during treatment B. Monthly in-office spirometry testing C. Determining if the patient has increased use of his or her long-acting beta-2-agonist due to exacerbations D. Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy D. Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing with their provider or a pharmacist first? A. Patients with kidney stones B. Pregnant patients C. Patients with heartburn D. Post-menopausal women A. Patients with kidney stones You have a patient who has been treated for many years with glucocorticoids. She has a severe chronic obstructive pulmonary disease and you are the home care nurse practitioner visiting the patient. What disorders is the patient at risk for developing and what signs and symptoms would you expect. The patient is at risk for the development of Cushing syndrome and long term use of glucocorticoids will result in abdominal distension, fat deposit, hirsutism, loss of muscle mass, moon face, thin fragile skin, weight gain, thick torso. Prior to prescribing metformin, the provider should: A. Draw a serum creatinine to assess renal function B. Try the patient on insulin C. Tell the patient to increase iodine intake D. Have the patient stop taking any sulfonylurea to avoid dangerous drug interactions A. Draw a serum creatinine to assess renal function The first-line therapy for mild-persistent asthma is: A. High-dose montelukast B. Theophylline C. Low-dose inhaled corticosteroids D. Long-acting beta-2-agonists C. Low-dose inhaled corticosteroids Treatment for mild intermittent asthma is: A. Daily inhaled medium dose corticosteroids B. Short-acting beta-2-agonists (albuterol) as needed C. Long-acting beta-2-agonists every morning as a preventative D. Montelukast (Singulair) daily B. Short-acting beta-2-agonists (albuterol) as needed A stepwise approach to the pharmacologic management of asthma: A. Begins with determining the severity of asthma and assessing asthma control B. Is used when asthma is severe and requires daily steroids C. Allows for each provider to determine their personal approach to the care of asthmatic patients D. Provides a framework for the management of severe asthmatics, but is not as helpful when patients have intermittent asthma A. Begins with determining the severity of asthma and assessing asthma control One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is: A. Ability to use albuterol daily to control symptoms B. Minimize exacerbations to once a month C. Keep nighttime symptoms at a maximum of twice a week D. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms D. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur: A. At nighttime one to two times a month B. At nighttime three to four times a month C. Less than twice a week D. Daily B. At nighttime three to four times a month Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur: A. Daily B. Daily and limit physical activity C. Less than twice a week D. More than twice a week and less than once a day D. More than twice a week and less than once a day The first-line treatment for cough related to a URI in a 5 year old is: A. Fluids and symptomatic care B. Dextromethorphan and guaifenesin syrup (Robitussin DM for Kids) C. Guaifenesin and codeine syrup (Tussin AC) D. Chlorpheniramine and dextromethorphan syrup (Nyquil for Kids) A. Fluids and symptomatic care Martin is a 60 year old with hypertension. The first-line decongestant to prescribe would be: A. Oral pseudoephedrine B. Oral phenylephrine C. Nasal oxymetazoline D. Nasal azelastine C. Nasal oxymetazoline Cough and cold medications that contain a sympathomimetic decongestant such as phenylephrine should be used cautiously in what population: A. Older adults B. Hypertensive patients C. Infants D. All of the above D. All of the above Decongestants such as pseudoephedrine (Sudafed): A. Are Schedule III drugs in all states B. Should not be prescribed or recommended for children under 4 years of age C. Are effective in treating the congestion children experience with the common cold D. May cause drowsiness in patients of all ages B. Should not be prescribed or recommended for children under 4 years of age When recommending dimenhydrinate (Dramamine) to treat motion sickness, patients should be instructed to: A. Take the dimenhydrinate after they get nauseated B. Drink lots of water while taking the dimenhydrinate C. Take the dimenhydrinate 15 minutes before it is needed D. Double the dose if one tablet is not effective C. Take the dimenhydrinate 15 minutes before it is needed First generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they are: A. More effective than first generation antihistamines B. Less sedating than the first generation antihistamines C. Prescription products, therefore are covered by insurance D. Able to be taken with CNS sedatives, such as alcoho B. Less sedating than the first generation antihistamines 15.Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: A. Urinary retention B. Cardiac output C. Peripheral edema D. Skin for rash A. Urinary retention Patients with allergic rhinitis may benefit from a prescription of: A. Fluticasone (Flonase) B. Cetirizine (Zyrtec) C. OTC cromolyn nasal spray (Nasalcrom) D. Any of the above D. Any of the above When educating patients who are starting on inhaled corticosteroids, the provider should include: A. They need to get any live vaccines before starting the medication. B. Inhaled corticosteroids need to be used daily during asthma exacerbations to be effective. C. Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush. D. They can triple the dose number of inhalations of medication during colds to prevent needing systemic steroids. C. Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush The known drug interactions with the inhaled corticosteroid beclomethasone (QVAR) include: A. Albuterol B. MMR vaccine C. Insulin D. None of the above D. None of the above Montelukast (Singulair) may be prescribed for: A. A 6 year old with exercise-induced asthma B. A 2 year old with moderate persistent asthma C. An 18 month old with seasonal allergic rhinitis D. None of the above; montelukast is not approved for use in children B. A 2 year old with moderate persistent asthma When prescribing montelukast (Singulair) for asthma, patients or parents of patients should be instructed: A. Montelukast twice a day is started when there is an asthma exacerbation B. Patients may experience weight gain on montelukast C. Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast C. Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast Christy has exercise and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes: A. Use one to two puffs of albuterol per day to prevent an attack with no more than eight puffs per day B. Beclomethasone needs to be used every day to treat her asthma C. Report any systemic side effects she is experiencing, such as weight gain D. Use the albuterol MDI immediately after her corticosteroid MDI to facilitate bronchodilation B. Beclomethasone needs to be used every day to treat her asthma Tiotropium bromide (Spiriva) is an inhaled anticholinergic: A. Used for the treatment of COPD B. Used in the treatment of asthma C. Combined with albuterol for treatment of asthma exacerbations D. Combined with fluticasone for the treatment of persistent asthma A. Used for the treatment of COPD i takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: A. Reassure him this is probably a viral infection and should be better soon B. Have him seen the same day for an assessment and theophylline level C. Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better D. Order a theophylline level at the lab for him B. Have him seen the same day for an assessment and theophylline level James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin’s diet for weight loss. The appropriate response would be: A. Congratulate him on making a positive change in his life B. Recommend he try stopping smoking instead of the Atkin’s diet C. Schedule him for regular serum theophylline levels during his diet due to increased excretion of theophylline D. Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels C. Schedule him for regular serum theophylline levels during his diet due to increased excretion of theophylline The bronchodilator of choice for patients taking propranolol is: A. Albuterol B. Pirbuterol C. Formoterol D. Ipratropium D. Ipratropium Long-acting beta-agonists (LTBAs) received a Black Box warning from the U.S. Food and Drug Administration due to the: A. Risk of life-threatening dermatological reactions B. Increased incidence of cardiac events when LTBAs are used C. Increased risk of asthma-related deaths when LTBAs are used D. Risk for life-threatening alterations in electrolytes C. Increased risk of asthma-related deaths when LTBAs are used Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? A. Betamethasone, an inhaled corticosteroid B. Salmeterol, an inhaled long-acting beta-agonist C. Albuterol, a short-acting beta-agonist D. Montelukast, a leukotriene modifier B. Salmeterol, an inhaled long-acting beta-agonist Patients with pheochromocytoma should avoid which of the following classes of drugs due to the possibility of developing hypertensive crisis? A. Expectorants B. Beta-2-agonists C. Antitussives D. Antihistamines B. Beta-2-agonists Digoxin levels need to be monitored closely when the following medication is started: A. Loratadine B. Diphenhydramine C. Ipratropium D. Albuterol D. Albuterol Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true? A. Diuretics reduce preload associated with fluid retention. B. Diuretics can be used earlier than Stage C when the goal is control of hypertension. C. Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism. D. Diuretics from the potassium-sparing class should be used when using an ARB. D. Diuretics from the potassium-sparing class should be used when using an ARB. Patrick is a 10 year old who presents with constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10 year old would be: A. PEG 3350 (Miralax) B. Bisacodyl (Dulcolax) suppository C. Docusate (Colace) suppository D. Polyethylene glycol electrolyte solution A. PEG 3350 (Miralax) Sadie is a 72 year old who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: A. Megaloblastic anemia B. Osteoporosis C. Hypertension D. Strokes B. Osteoporosis Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for: A. Iron deficiency anemia, vitamin B12 and calcium deficiency B. Folate and magnesium deficiency C. Elevated uric acid levels leading to gout D. Hypokalemia and hypocalcemia A. Iron deficiency anemia, vitamin B12 and calcium deficiency Jim presents with complaints of “heart burn” that is minimally relieved with Tums (calcium carbonate) and is diagnosed with GERD. An appropriate first step therapy would be: A. Omeprazole (Prilosec) twice a day B. Ranitidine (Zantac) twice a day C. Famotidine (Pepcid) once a day D. Metoclopramide (Reglan) four times a day B. Zantac BID Josie is a 5 year old who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie? A. Prochlorperazine (Compazine) B. Meclizine (Antivert) C. Promethazine (Phenergan) D. Ondansetron (Zofran) D. Zofran Hannah will be traveling to Mexico with her church group over Spring Break to build houses. She is concerned she may develop traveler's diarrhea. Advice includes normal food and water precautions as well as:Select one:a. Loperamide four times a day throughout the tripb. Bismuth subsalicylate with each meal and bedtimec. A prescription for diphenoxylate with atropine to use if she gets diarrhead. None of the above b. Bismuth subsalicylate with each meal and bedtime Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate: A. May lead to toxicity if taken with aspirin B. Is contraindicated in children with flu-like illness C. Has antimicrobial effects against bacterial and viral enteropathogens D. All of the above D. All of the above Kelly has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide: A. Can be given to all age patients, including infants and children, for viral gastroenteritis B. Slows gastric motility and reduces fluid and electrolyte loss from diarrhea C. Is the treatment of choice for the diarrhea associated with E. coli 0157 D. May be used in pregnancy and by lactating women B.Slows gastric motility and reduces fluid and electrolyte loss from diarrhea Patients taking antacids should be educated regarding these drugs, including: A. They may cause constipation or diarrhea B. Many are high in sodium C. Separate antacids from other medications by 1 hour D. All of the above D. All of the above If a patient with H. pylori positive peptic ulcer disease fails first-line therapy the second-line treatment is: A. Proton pump inhibitor BID plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days Treatment failure in patients with peptic ulcer disease associated with H. pylori may be due to:A. Antimicrobial resistance B. Ineffective antacid C. Overuse of proton pump inhibitors D. All of the above A. Antimicrobial resistance An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is:A. Histamine2 receptor antagonists for 4 to 8 weeks B. Proton pump inhibitor BID for 12 weeks until healing is complete C. Proton pump inhibitor BID plus clarithromycin plus amoxicillin for 14 days D. Proton pump inhibitor BID and levofloxacin for 14 days C. Proton pump inhibitor BID plus clarithromycin plus amoxicillin for 14 days Long-term use of proton pump inhibitors may lead to:A. Hip fractures in at-risk persons B. Vitamin B6 deficiency C. Liver cancer D. All of the above A. Hip fractures in at-risk persons Infants with reflux are initially treated with:A. Histamine2 receptor antagonist (ranitidine) B. Proton pump inhibitor (omeprazole) C. Anti-reflux maneuvers (elevate head of bed) D. Prokinetic (metoclopramide) C. Anti-reflux maneuvers (elevate head of bed) When using “Step-Up” therapy for GERD, the next “step up” in treatment when a patient has been on proton pump inhibitors for 12 weeks is:A. Add a prokinetic (metoclopramide) B. Referral for endoscopy C. Switch to another proton pump inhibitor D. Add a cytoprotective drug B. Referral for endoscopy When using the “Step-Up” approach in caring for patients with GERD, the “step up” from once daily proton pump inhibitor use is:A. Prokinetic (metoclopramide) for 8 to 12 weeks B. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks C. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks D. Cytoprotective drug (misoprostol) for 4 to 8 weeks B. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks When treating patients using the “Step-Down” approach the patient with GERD is started on first.A. Antacids B. Histamine2 receptor antagonists C. Prokinetics D. Proton pump inhibitors D. Proton pump inhibitors Antacids treat GERD by:A. Increasing lower esophageal tone B. Increasing gastric pH C. Inhibiting gastric acid secretion D. Increasing serum calcium level B. Increasing gastric pH Metoclopramide improves GERD symptoms by:A. Reducing acid secretion B. Increasing gastric pH C. Increasing lower esophageal tone D. Decreasing lower esophageal tone C. Increasing lower esophageal tone Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Foods that may aggravate GERD include:A. Eggs B. White bread C. Chocolate D. Chicken B. White bread Gastroesophageal reflux disease (GERD) may be aggravated by the following medication that effects lower esophageal sphincter (LES) tone:A. Calcium carbonate B. Estrogen C. Furosemide D. Metoclopramide B. Estrogen Varenicline (Chantix) MOA Partial agonist at the alpha4beta2 nicotinic ACh receptor; blocks effect of additional nicotine challenge while causing release of mesolimbic dopamine; most effective single drug Adverse effects of Varenicline Most common is self-limiting nausea; depression, suicidal ideation, and emotional lability have been reported; CV-related death, non- fatal MI, and non-fatal stroke Bupropion MOA Norepinephrine and dopamine re-uptake inhibitor; decreases cravings and withdrawal symptoms while interacting with pathways underlying addiction; thought to reduce depressive symptoms of nicotine withdrawal; better than nicotine replacement but less effective than varenicline Adverse effects of Bupropion Insomnia, dry mouth, nausea; neuropsychiatric effects include increased risk of suicidal ideation in patients with/without pre-existing psychiatric disorders Clonidine MOA Blocks cravings, anxiety, restlessness, tension, and hunger; potential utility for anxious agitated ex-smokers who are likely to benefit from the sedative effects; it is an oral antihypertensive drug Clonidine adverse effects Sedation, dry mouth, dizziness Mecamylamine MOA Nicotine antagonist (ganglionic blocker); can moderate smoking cue-induced emotional responses in smokers; nicotine + mecamylamine is superior to nicotine alone in smoking cessation Mecamylamine adverse effects Contraindicated in coronary or renal insufficiency, glaucoma, uremia; adverse effects include orthostatic hypotension, fatigue, sedation, constipation, dry mouth, N/V Naltrexone MOA Opiate antagonist; no effect based on clinical trials in smoking cessation Nicotine replacement therapy Alternative delivery prevents withdrawal symptoms; levels attained high enough to prevent withdrawal but not high enough to produce dependence; gradually taper off consumption; includes gum, patch, oral lozenge, nasal spray, and oral vapor inhaler; patches produce most constant nicotine blood level Nicotine patch 12 week course with step down titration; application site reactions, headaches, cold and flu symptoms common; caution advised with CV disease, diabetes, hepatic impairment, peptic ulcers, pheochromocytoma, and uncontrolled hyperthyroidism, esp. if you smoke while on patch Nicotine gum 2 mg dose with no more than 24 pieces/day; 12 week course; jaw pain/orodental problems from chewing; headache, indigestion, nausea common; patients may transfer their nicotine addiction from cigarettes to gum Nicotine inhaler/spray inhaler:12 week course; spray: 3 month course; localized irritation in mouth or nostrils; mild symptoms of headache, nausea, heartburn and hiccups reported; more beneficial than other NRTs Glucopeptides have excellent activity against both aerobic and anaerobic gram + bacteria Vancomycin resistance has become a problem for which organisms? Enterococcus spp. and S. aureus All B-lactam antibiotics act by preventing proper construction of the bacterial peptidoglycan Unlike vancomycin, telavancin possess a lipophilic side chain which classifies it as a lipoglycopeptide The structure of Daptomycin cyclic lipopeptide Daptomycin has excellent activity against aerobic gram + bacteria. Colistin binds to and disrupts in the bacterial outer membrane. lipopolypeptide Colistin has activity against aerobic bacteria. gram negative Rifampin binds bacterial and inhibits synthesis of . RNA plymerase, mRNA Rifampin is used primarily in the treatment of disease caused by and . mycobacteria,staphlycocci The rifamycins are usually used in conjunction with other antimircobials agents because to rifamycins develop during mono therapy. resistance The amino glycosides have excellent activity against aerobic bacteria. gram negative The aminoglyocides are used at synergistic doses along with cell wall-active agents to treat some aerobic bacteria. gram postive The major toxicities associated with amino glycosides are and . nephrotoxicityand ototoxicity Among the macrocodes has the best aerobic gram - coverage and is therefore useful against . azithromycin, Haemophilus influenzae and are macrocodes that are better tolerated than erythromycin. azithromycin, clarithromycin Macrolides have relatively poor activity against aerobic gram negative bacilli and bacteria. anaerobic Telithromcyin is a member of the class of antimicrobial agents. ketolides Because of its spectrum of activity, telithromycin is most useful in treating infections. respiratory Tetracycline inhibits bacterial growth by binding to bacterial . ribosomes Tetracyclines have an excellent activity against bacteria. atypical Because of problems with discoloration of teeth and deposition in bones, tetracycline should not be used in and should be used with caution in . pregnant women, children less than 9 years of age. Tetracycline is a member of the class of antibiotics called . glycylclines Tigeclycline has activity against many highly resistant aerobic and bacteria. Gram +, Gram - Chloramphenicol inhibits bacterial growth by binding the bacterial . ribosomes Chloramphenicol has excellent activity against and bacteria. It is also active against many aerobic gram + and aerobic gram - bacteria.. Resistance to chloramphenicol may occur when bacteria acquire the ability to inactivate the drug by or produce that prevent accumulation. acetylation, efflux pump The major factor limiting the use of chloramphenicol is its which is primarily consists of reversible , suppression and irreversible . toxicity, bone marrow, aplastic anemia Clindamycin is active against many aerobic bacteria and bacteria. gram +, anaerobic Resistance to may also lead to resistance to clindamycin in some bacteria. macrolides or erythromycin Use of clindamycin may lead to life-threatening . psuedomembranous colitis Streptogramins consist of antibiotics that work synergistically together. two Quinupristin/dalfopristin has excellent activity against aerobe . gram + The strength of quinupristin/dalfopristin is its activity agasint resistance staphylococci, resistanct streptoccuc pneumoniae and some resistant enterococci. methicillin, penicillin, vancomycin Linezolid has excellent activity against gram + bacteria such as resistant staphylococci and resistant enterococci. methicillin and vancomycin This agent binds to bacterial and inhibits protein synthesis. ribosomes One advantage of linezolid is it achieves similar high serum levels whether given or . intravenously, orally. Nitrofurantoin has excellent activity against many of the aerobic and bacteria that commonly cause acute cystitis. gram - and gram + Nitrofurantoin does not achieve high levels and therefore should not be used to treat systemic infections or pyelonephritis. blood Despite decades of use, very little to nitrofurantoin has emerged. resistance Which of the following antibiotics is NOT a B-lactam? ampicillinmeropenemceftriaxoneaztreonam vancomycin Which of the following antibiotics has little activity against anaerobic bacteria? imipenemmetronidazoleceftriazoneclinidamycinamoxicillin/clavulnate ceftriaxone Which of the following antibiotics could you use in someone who has a history of developing anaphylaxis after taking penicillins? aztreonamertapenempiperacillin/tazobactrumcefotetan aztreonam Which of the following agents is NOT useful in the treatment of enterococci infections? penicillincefazolinampicillingentamycinvancomycin cefazolin Which of the following quinolines has the greatest activity against Pseudomonas aeruginosa? levofoxacinmoxifloxacingatifloxacingemifloxacinciproflaxacin ciprofloxacin Rifampin is useful in treatment or prophylaxis against all of the following bacteria except:staphylococcus aureusstaphylococcus epidermisbactericides fragilisneisseria meningitismycobacterium tuberculosis bactericides fragilis Which of the following agents is NOT useful in treating infections caused by Mycobacterium avium complex? clarithromycinisoniazidehtambutolrifabutinciprofloxacin isoniazid which of the following would be useful in the treatment of an infection cause by an Escherichia coli strain that produces an evened spectrum B-lactamase? meropenem Which does not inhibit bacterial cell wall synthesis?gentamicinactreonamimipenem gentamicin Which antibiotics would you use to treat haemiphilus influenza? amoxicillin/clavunatecefuroxime doxycyclinecefotaxime NOT ampicillin What antibiotic can be safely used in children? azithromycin Common adverse effects of aminoglycosides auditory impairment, nephotoxicity, vestibular toxocity Pyrazinamide is used to treat infections caused by ? mycobacterium tuberculosis Chlymida should not be treated by what antibiotic? Ceftriaxone Empiric use vancomycin in infective endocarditits would fail to cover which for the following organisms? covers staph aureus, staph epidermis, virdians group strep, enterococci, BUT NOT HACEK organism Which antibiotic targets the bacterial ribosomes? tetracycline Doxycyline does not treat pseudomonas Which of the following antibiotics targets bacterial RNA polymerase?cefotetanamikacinrifampinazithromycin rifampin What antx combo to use for pseudomonas? ceftazidine and tobramycin Using good clinical judgment, what questions should you ask yourself before prescribing a medication for a patient? 1. Is there a clear indication for drug therapy? 2. What drugs are effective in treating this disorder 3. What is the goal of therapy with this drug? 4. Under what conditions is it determined that a drug is not meeting the goal and a different therapy or drug should be tried 5. Are there unnecessary duplications with other drugs the patient is already taking 6. Would an OTC drug be just as useful as a prescription drug? 7. What about cost? 8. Where is the information to answer these questions? Criteria for choosing drug High efficacy (>95%)Low costOrganism resistance unlikely to develop or likely to be delayedSingle dosePO administrationNot CI for pregnancy or lactation Identify the major phasesand key activities in each phase for human drug discoveryand development o Discovery § Compound Selection § nGLP Tox Support o Preclinical § Compound enters development § IND-Enabling Studies § Drug Safety Review preIND (DSC) o Clinical trials § Phase I ú Phase II Support § Phase II ú Phase III Support ú Drug Safety Review EOPII (FDA) § Phase III ú NDA Support ú Drug Safety Review PreNDA (FDA) FDA review (NDA) How does Hypoalbuminemia affect anesthesia? hypoalbuminemia= decreased colloid oncotic pressure and inc for edema, inc unbound fraction of drugs in bloods that are highly protein bound (most sedatives/anesthetic drugs), ie inc amount of drug avail to produce effect, so careful to not overdose. What is the Prescription Drug Marketing Act (PDMA)? Allows for reimportation by ONLY the manufacturer. If Pfizer sends it out, Pfizer is the only one who can bring it back into the US. Passed in 1987. Also requires state licensing of wholesale distributors of prescription drugs. How will you stay up to date with medication administration and prescribing? continuing education, article review, etc. What is the role of the FDA? -content and labeling of food, drugs, and medical devices -food is safe and wholesome -cosmetics won't harm us -medicines and medical devices are safe and effective -radiation emitting products are not harmful -products are labeled truthfully What is the primary purpose of the Food and Drug Administration? To protect the patient and ensure drug effectiveness What happens with albumin and how does this effect drugs? Albumin decreases, lowering the dosage needed for toxicity in patients. It makes the drug inactive so it can't bind to the receptor site, and won't have the physiological effect. What is the drug’s half-life? the time it takes for the amount of drug in the body to decrease to 1/2 of the peak level it previously achieved How does a drugs half-life effect the frequency of administration If longer the half-life the less frequent the medication Differentiate onset, peak, and duration of action. Onset: When the drug starts working after administeredPeak: When the drug is working at its maximal capacityDuration of action: The length of time that the effect of the drug lasts Pharmacokinetics: Metabolism.Explain first-pass effect - Refers to the rapid hepatic inactivation of certain oral drugs- Remember, when oral drugs are absorbed from the GI tract, they are carried directly to the liver via the hepatic portal vein- When drugs are highly metabolized during the first circulation to the liver (first pass), little or not active drug is sent to the general circulation What is meant by a synergistic effect? Give an example and explain what each hormone does. is two hormones/drugs acting together for a greater effect. An example is gastrin and histamine What is the Steady state? when all the highest concentrations and lowest concentrations are the same what is an additive effect? Each chemical expresses same toxicity as it would alone Factors affect a drug’s absorption: –Route given–Perfusionof tissue–Solubility–Ionizationand Ph–Absorbing surface–Concentrationof drug Effect of P450 on drug and alcohol metabolism Ethanol competitively inhibits P450 in drug metabolism. Causes increased level of drugs in body when drinking heavily What is drug efficacy? maximum effect one can expect from a drug (regardless of dose); 2 drugs with different potencies can have the same efficacy On the drug concentration curve what is the first sign of a therapeutic effect? onset of action or first sign of effect what is a peak and trough level? peak - time required for a drug to reach its maximum therapeutic response trough - lowest blood level of a drug What is the minimum toxic concentration (MTC)? the lowest blood concentration level that significant adverse effects of a drug usually occcur blood-brain barrier and fetal placental barrier anatomic barriers prevent chemicals and medications from entering ◦Physiologic Barriers – lipid soluble substances only –Blood Brain – protects CNS, difficult to treat some disorders –Blood Placental – protects fetus, many drugs can cross What is the difference in distribution for each medication route? Oral: Medications are taken by mouth (in pill, capsule or liquid form) and absorbed into the system through the digestive system. Absorption is slow. Medications that use this option cannot be used if vomiting is occurring. Enteral: Medications are administered into the rectum (via a suppository) and absorbed by the lower digestive tract. Mucosal: Medications are delivered through the nose or inhaled and are absorbed through the nasal mucosa or bronchioles, respectively. Vaginal administration of a medication is also considered mucosal. Parenteral: Any medication administration that involves injecting a drug directly into a vein (intravenous), muscle (intramuscular), artery (intrarterial), abdominal cavity (intrperitoneal), heart (intracardiac) or into the fatty tissue beneath the skin (subcutaneous). Best methods IV & SQ Percutaneous: Medications are absorbed directly through the skin into the blood stream. Some hormone replacements are administered by patches that are absorbed slowly and evenly, for example. How does renal insufficiency affect drug distribution? Can have alterations in distribution volume due to decreased or increased protein binding. also changes in body composition (increased total body water) Decrease or slow drug elimination (low albuminism) What is the additive (indifferent) effect? It is the interaction of two antibiotics the produces a combined effect that is no greater than the sum of their separately measured individual effects. What is the synergistic effect? Where the effects of two or more drugs are multiplied beyond what is expected if each were taken alone (1+1=5) what is antagonistic effect? drugs work much more poorly together than they do individually PCN + Chloramphenicol Describe the drug effects based on the route of administration. See #25 isoenzymes enzymes that catalyze the same reaction with different proteins- ex: fetal hemoglobin; medication can be more active or interactive with these. According to the WHO what is the prescribing process. (1) define the patient’s problem; (2) specify the therapeutic objective; (3) verifythe suitability of your P-drug and choose a treatment for this individual patient; (4) writea prescription; (5) inform and instruct the patient; and (6) monitor and/or stop thetreatment. What is approved by the FDA? regulation of food, drugs and medical devices What is "off-label prescribing"? prescribing a medication for a disorder when it is known to work, but there is no formal FDA indication. It is perfectly legal and quite common. Effects not always well-known, especially in less studied populations What factors place an infant and child at risk when prescribing medications? weight and how physiological development affects absorption, distribution, metabolism and excretion in children What factors place an infant and child at risk when prescribing medications? More water, less fat Immature liver-make less plasma proteins: Less albuminLess able to metabolize drugs -Renal function not fully developed until 30m-Neonates-Drugs bind to bilirubin and can cause issue with excretion-kernicterus Body surface areaImmature Blood-brain barrier leading to risk for CNS toxicity Fewer Binding sites, lead to high blood concentrationmany drugs not studies in children Drugs requiring oxidation: Phenobarbitol, phenytoin, methylxanthines- due to faster respiratory rate they may need more medication or more frequent schedule Phase of development: Tetracycline stains teeth from 4months to 8 years and steroids will affect growth What adverse drug reactions (ADRs) is the elderly client at risk for developing? Drug toxicity and death What are the components of each of the Adverse Drug Reactions related to special populations? babies, elderly, and renal compromise. Text 116-117 List and define the different types of potential adverse drug reactions and provide examples of each type. (chronic and delayed) Chronic—w/ prolonged use (EX: osteoporosis w/ glucocorticoids, dyskinesiastypical w/ antipsychotics Delayed—months/years aftertreatment (EX: leukemia w/ alkylating agents (chemo), baby cleft palate w/isotretinoin, Fetal alcohol syndrome w/ ethanol) passed down=teratogenic Which medications interact with St. John’s Wort? Depression primarily AEs: Drug interactions frequent and potentially serious. Induces CYP3A4 and likely other enzymes. Mania or hypomania in some predisposed patients; fatigue, dry mouth, constipation, confusion AVOID in pts. already taking antidepressants; protease inhibitors; oral contraceptives. Which medications interact with St. John’s Wort? St. John's Wort Indications: Reduces depression, reduce anxiety, anti-inflammatory Drug interactions: DECREASE EFFECT OF WARAFIN antidepressants, antiretrovirals, CNS depressants, and analgesics, phenytoin Teaching: decreased anticoagulant effects, increased sedation, decreased antiretroviral activity What drugs does ginseng interact with Increases effects of anticoagulants and antiplatelets, insulin, oral antidiabetic agents.Decreased effects with concurrent use of furosemide.May interfere with immunosuppresants. What are the drug reactions with licorice root? Uses - respiratory infections, asthma, liver disease aid, lowers cholesterol, antioxidant, antiviral, antiinflammatory, for skin disorders; used as food additive/flavoring mostly Contraindications - Interferes with a large amount of meds (ACE inhibitors, insulin, laxatives, oral contraceptives), not to be used when pregnant, suffering from high BP, kidney and liver disease; lowers potassium levels and causes sodium retention What is the role of the NP in caring for patients who take herbal supplements? Watch for potential reactions; educate for appropriate sources of care. What ailment generates the greatest use of over-the-counter medications? Cough & cold how do doxazosin and terasosin work? by blocking alpha-1 receptors in the bladder neck and in vascular smooth muscle of blood vessels which causes vasodilatation. Not selective What does Minipress (prazosin) do? Alpha-adrenergic receptor blockers relax the smooth muscle in the bladder neck, thus facilitating urinary flow through the prostatic urethra. Side effects: blocking the adrenergic receptors could include dizziness, postural hypotension, urinary frequency, impotence, dry mouth, blurred vision What is the action of beta blockers? decrease myocardiac O2 demand by decreasing force of contractions (neg inotrope); improve filling time by decreasing AV conduction (neg. chronotrope), decreasing afterload by vasodilating peripheral vessels what are the adverse effects of beta blockers? heart failure and symptoms of cns depression. agranulocytosis, throbocytopenia, hyper/hypo glycemia, hyperlipedemia, impotene, alopecia, wheezing, dry mouth Explain the rapid withdrawal syndrome associated with the sudden stopping of a beta blocker. rebound sensitivity to adrenergic stimulation- leads to increase of O2 consumption, angina, possible MI, even if no prior heart disease What patient teaching should be provided when prescribing clonidine or any centrally acting adrenergic blocker? • Teach patient not to stop drug abruptly, and to maintain compliance of the medication and dosage schedule • Take first dose at bedtime to decrease orthostatic B/P changes • take the med and then lay down. What are the adverse effects of a beta 1 selective blocker? ADVERSE CARDIAC EFFECTS DUE TO BETA BLOCKADE Heart failure Negative chronotropic effects Beta blocker withdrawal ADVERSE NONCARDIAC EFFECTS DUE TO BETA BLOCKADE Increased airways resistance Exacerbation of peripheral artery disease Facilitation of hypoglycemia Hyperkalemia Depression, fatigue, sexual dysfunction Lipid metabolism Weight gain Why should beta-blockers be used cautiously in diabetics? Beta-blockers can mask the warning signs, i.e. tachycardia, for insulin-induced hypoglycemia. Which medication used in the treatment of Alzheimer’s Disease is not an anticholinergic agent? Namenda or memantine What are the anticholinesterase agents used to treat? To treat myasthenia gravis. In myasthenia gravis, they are used to increase neuromuscular transmission. To treat glaucoma To treat Postural Tachycardia Syndrome As an antidote to anticholinergic poisoning To reverse the effect of non-depolarising muscle relaxants To treat Apathy To increase chances of lucid dreaming What are the anticholinesterase agents used to treat?#2 To treat Alzheimer's diseaseTo treat cognitive impairments in patients with schizophrenia. As a treatment for autism and to increase the percentage of Rapid eye movement sleep in autistic children What effect does nicotine have on nicotinic acetylcholine receptors? 1 Stimulates locus serulius2 -enhances dopamine release-stimulates then depresses3 increase motility of GIvasoconstriction Cholinergic blockers do what? block action of parasympathetic system How do cholinergic blockers manage extrapyramidal symptoms? Pseudoparkinsonism or dystonic reactions What do cholinesterase inhibitors do? treat dementia and alzhimer's by delaying cognitive loss and maintaining function What is the action of cholinesterase inhibitors? Prevents destruction of acetylcholine in the synapses of the CNS by inhibiting cholinesterase. Slows progress of mild-to-moderate Alzheimer's dementia. Also temporarily improves symptoms of Parkinson's disease. How is scopolamine normally administered? As a transdermal patch to prevent systemic anticholinergic effects Can medications be administered during pregnancy for myasthenia gravis? Yes, but cautiously and only when clearly needed Why are elderly at higher risk of developing Adverse Drug Reactions (ADRs)? - Poly-pharmacy - Lower weight - Higher fat % - Lower water/plasma % - Muscle atrophy - Changes in pharmacokinetics (ADME) - Confusion/Alzimers - (Women are more susceptible!) What are the ADRS related to special populations? PEDS ADRS related to pregnancy, elderly and children. Mostly related to Pharmacokinetics-Absorption is different Children/infants: Gastric pH does not reach adult levels until age 1-if drug needs acid to absorb, less med will be absorbed Greater Body surface area and HAVE greater absorption of topical medication Infants skin is more permeable to water leading to increased absorption Immature peripheral circulation will prevent absorption of IM or SC medication Bilirubin binds to plasma proteins Phase 1 drug metabolism - Cytochrome P-450, CYP 3A play a major role in metabolism The Earliest enzyme to show activity is CYP 3A7 -present in utero and declines after birth with an increase in CYP3 A4 and CYP 3A5-ADULT LEVELS NOT REACHED FOR YEARS. MEDS that need first pass metabolism NEED TO BE REDUCEDErythromycin Drugs and Pregnancy Progesterone decreases gastric tone & Motility, prolonged stomach emptying-Alters Pharmacokinetics -Progesterone-Increases tidal volumeIncreases Pulmonary vasodilation-inhaled drugs absorb more quickly Distribution/Metabolism in pregnancy HR is increased by 10-15 BPM50% increase in blood volume causing hemodilution of plasma albumin to potentiate drug distributionIncrease in plasma lipids altering drug transport & distributionDrugs compete for recepotr site occupied by HORMONE resulting in unbound and free drug Drugs that are not lipophilic enter fetal circulation DRUG METABOLISM IS NOT ALTERED BY PREGNANCY Pregnancy and lactation -Treat Pre-existing condition-Treat Pregnancy-related complication During lactation: use only if needed and treatment cannot be delayed until the infant is weaned Instruct mother to take medicine AFTER Nursing to lower concentration at next feeding Drugs that are lipid soluble and Low protein binding such as CNS agents pass into breast mild Drugs with low molecular weight PASS into breast milk Low pH- produce increase concentrations FDA categories for Drugs & Pregnancy CAT A: Controlled studies in pregnant women and NO RISK CAT B-Animal Studies show NO RISK but not controlled studies in pregnant women CAT C: Animal studies; SHOW RISK. No HUMAN STUDIESBENEFIT MUST OUTWEIGH RISK CAT D: RISK/BENEFIT-may outweigh in serious situation CAT X: FETAL ABNORMALITIES, RISK OUTWEIGHS BENEFITNOT USED What blood values should be monitored with carbamazepine? CBC, chemistry, Liver function tests (LFTs), thyroid stimulating hormone (TSH) Check every 3-4 months if results remain normal What is the pharmacodynamics of carbamazepine? Effects NA channels slowing influx of NA in the cortical neurons and slowing the spread of abn activity Depresses transmission in the nucleus ventralis anterior of the thalmus This area is associated with the spread of seizure discharge What should families be taught regarding the monitoring of seizure activity? Monitor frequency, duration, and severity You may continue to have seizures during treatment May need to avoid activities such as swimming, driving, or climbing so you do not harm yourself or others What electrolyte imbalance is noted with the administration of topiramate? Decreased serum bicarbonate concentrations due to inhibition of carbonic anhydrase and increased renal bicarb loss leading to hyperchloremic metabolic acidosis What is the pregnancy category for valproate? With regard to valproate use in pregnant women with epilepsy or bipolar disorder, valproate products should only be prescribed if other medications are not effective in treating the condition or are otherwise unacceptable. Valproate products will remain in pregnancy category D for treating epilepsy and manic episodes associated with bipolar disorder. What instructions will you provide to a woman who wants to get pregnant and has a seizure disorder controlled with valproate? pregnancy category D - risk versus benefit - 1st trimester- can cause neural tube defects - spina bifida. Used with caution and only if life threatening without valproate. If taking and would like to become pregnant - reduce dosage or switch meds prior to conception all woman of child-bearing age should take 0.4 mg of folic acid a day to prevent neural tube defects How long does it take for selective serotonin reuptake inhibitors to produce an effect in patients with depression? as long as 3 to 4 weeks What are the precautions and contraindications for the tricyclic antidepressants? tylines, pines, pramines heart problems due to quinidine like effect on myocardium, direct alpha adrenergic blocking effect, sinus tachy, prolong qrs, pr, qt intervals acetylcholine blocking effect used in caution for glaucoma, prostatic hypertrophy, urinary incontinence not administered with MAOIs or those with hypersensitivity with this class elderly increase risk of confusion, hypotension, falls Phenelzine (Nardil) is an MAO inhibitor. What are the cautions and contraindications? How is it used to treat recalcitrant depression? Use cautiously with severe hepatic or renal impairment. Avoid in first and last trimesters of pregnancy. The MAO inhibitor exert their effect by irreversibly inactivating the enzymes that metabolize norepinephrine, serotonin, and dopamine to increase the bioavailability of these neurotransmitter. What are the symptoms of hypertensive crisis? BP greater than 160/94 strong, bounding pulse severe headache chest pain neural deficits Nosebleed ringing in ears When are buspirone (Buspar) and an SSRI combined? Although buspirone can be used as the sole pharmacotherapeutic modality for anxiety, it is frequently used adjunctively with SSRIs in treatment-resistant depression because of the combined serotonergic mechanisms, that is postsynaptic reuptake inhibition and receptor agonism. What type of diet is recommended with the administration of lithium? Must be taken with food to prevent GI upset Lithium may decreased with the use of NA salts and bulking agents Sweat a lot increase water intake and maintain adequate salt intake Low fat, low carb, low calorie, high protein, sugar free 13. What are the main side effects of each of classes of antidepressants? All have black box warning for suicidalideation. TCAs: Drymouth, constipation, urinary hesitancy, urinary retention, blurred vision, sedation, orthostatic hypotension, weight gain, nausea, vomiting, gynecomastia, and libido changes. SSRIs: Nausea, vomiting, HA, lightheadedness, dizziness, dry mouth, increased sweating, weight gain, exacerbation of anxiety, agitation. MAOIs: insomnia, anxiety, agitation, dry mouth, blurred vision, urinary retention, constipation, dizziness, HA, insomnia, restlessness, and hypotension. SNRIs: HA, somnolence, dizziness, insomnia, nausea, dry mouth, constipation and abnormal ejaculation. What receptors do the benzodiazepines act on? Benzodiazepines (BZs) act on gamma-aminobutyric acid type A (GABAA) receptors such as alpha1beta2gamma2 through key residues within the N-terminal region of alpha subunits, to render their sedative and anxiolytic actions. They attach to the GABA and decrease the excitability of the receptor. In the GABA receptor they attach to the benzodiazepine receptor. What factors will place the patient at risk for antibiotic resistance? Increasing population of immunocompromised patients, increase of invasive medical procedures, increase survival, chronic disease, daycare, overcrowding, travel, use of antibiotics in children under 2 and older than 65, ^ broad spectrum antibiotics use 2. What factors place the patient at risk for hypersensitivity reactions with penicillins and cephalosporins? - the risk for allergic like event after penicillin is increased about 10 fold who had a prior event - cross sensitivity to cephalosporins, imipinem or beta-lactamase inhibitors. -cephalosporins are generally not recommended for those who have type 1 reaction to any penicillin. - What are the safest antibiotics to prescribe to a woman who is pregnant? Antibiotics agents in class A or B Amoxicillin, Ampicillin, Clindamycin, Erythromycin, Penicillin, Nitrofurantoin Amino penicillin, ampicillin, amoxicillin are active against wide range of gram-positive and limited range of gram-negative organisms Which antibiotics inhibit bacterial cell wall synthesis? These are beta-lactam antibiotics, glycopeptides, daptomycin and colistin. These antibiotics attract the protective cell membrane, turning it into a liability for the bacteria. Cephalasporins Why is clavulanate added to Amoxicillin? inactivate the B-lactamases of many gram +, gram -, and anaerobic bacteria as a result they dramatically broaden the antimicrobial spectrum of the aminopenicillins What antibiotics are appropriate to prescribe to children? Cephalosprins, amoxicillin, clindamycin, erythromycin According to the American College of Cardiology and the American Heart Association, what are the guidelines related to prophylactic antibiotics prior to a dental appointment? The only people who should have prophylactic antibiotic therapy are pt with heart valves, previous endocarditis, congenital heart disease, cardiac transplant, valve regurg who will have tissue or root works Central nervous system (CNS) consists of the brain and the spinal cord (ch 12, go 129) peripheral nervous system consists of all nervous tissue, sensory and motor neurons (ch 12, pg 129) somatic nervous system consists of the nerves that provide voluntary control over skeletal muscle (ch 12, pg 130) autonomic nervous system Include involuntary control; cardiac muscle, the heart, digestive tract, respiratory tract, arteries, glands....(ch 12, pg 130) Limbic system located in middle brain, responsible for emotional expression, learning and memory; signals pass to hypothalamus (ch 14, pg 162) Reticular formation connects w/ the hypothalamus; its a network of neurons found along the entire length of the brainstem; inhibition causes drowsiness and sleep (ch 14, pg 163) Reticular activating system (RAS) Where the reticular formation is found; responsible for sleeping and wakefulness, helping a person focus on individual tasks (ch 14, pg 163) Anxiolytics Drugs that are quite effective in reducing anxiety levels in patients; used when anxiety begins to effect ADL's (ch 14, slide 10) CNS depressants alcohol, anasthetic, barbiturates, benzodiazepines (Valium) (ch 14, pg 166) Lexapro SSRI- Increases the amount of seratonin available at a specific postsynaptic receptor within the CNS (ch 15, slide 31) Benzodiazepines Most widely prescribed drug class; used to treat anxiety and insomnia (pg 169) Barbiturates sedatives and hypnotics; Binds to GABA receptors and suppress the CNS; many include schedule II drugs (ch 14, page 171) REM rapid eye movement sleep; this is the stage when dreaming occurs (ch 14, page 166) Seizures a sudden, involuntary movement with loss of awareness, caused by uncontrolled neuronal discharge in the brain (ch 15, page 181) Gamma-amnniobutyric acid (GABA) the primary inhibitory neurotransmitter in the brain (ch 15, pg 185) Myoclonic seizures large jerking movements of a major muscle group, such as an arm (ch 15, slide 26) Status Epilepticus A continuous seizure which can lead to death, considered a medical emergency (ch 15, slide 17) What type of seizures indicate the use of benzodiazepines? Absence and myoclonic seizures (ch 15, page 187) Succinimides medications that suppress seizures by delaying calcium influx into neurons (most effective in absence seizures) (ch 15, pg 191) Phenothiazines Pharmacologic class of drugs that are the most effective in treating positive signs of schizophrenia (ch 17, page 27) Chlorpromazine Therapeutic Class: Conventional antipsychotic Pharmacologic class: D2 dopamine receptor antagonist (ch 17, pg 228) Nonphenothiazines consists of drugs whose chemical structures are dissimilar to the phenothiazines but actions are the same as phenothiazines (ch 17, slide 27) Atypical Antipsychotic Drugs Preferred for treating psychoses, do not cause EPS symptoms and fewer side effects than conventional drugs, treat both positive and negative symptoms(ch 17, page 231) what should the nurse monitor in a patient taking an atypical antipsychotic drug? Hematologic side effects, anticholergenic side effects, decrease of psychoses Sx, for alcohol or drug abuse Dopamine-serotonin system stabilizers the newest antipsychotic class that was approved in 2002, controls both positive and negative, grouped with atypical antipsychotic (ch 17, page 235) What patient teaching will you provide to a patient who is experiencing non- infectious diarrhea related to antibiotic administration? Term If severe diarrhea occurs, pt should contact the prescriber before initiating any treatment. For mild diarrhea, they can use adsorbent antidiarrheal agents containing attapulgite (Donnagel) but should avoid antiperistaltic agent that promotes retention of toxins (C. diff). call if more than 4-6 stools a day or bloody stools increase fluids, eat plain yogurt A patient is taking a fluoroquinolone; what are the most serious adverse effects? It is important to consider in patients who present diarrhea, especially if it contains blood, pus, or mucus. GI: abdominal pain, nausea, and altered taste. Stevens-Johnson syndrome Phototoxicity Cardiovascular: angina, A-flutter, cardiopulmonary arrest, cerebral thrombosis, MI, and ventricular ectopy. CNS: sleep disorders, nervousness, and vertigo. Increased or decreased blood sugars in diabetics. What population should not be administered tetracyclines and why? Renal impairment – may lead to excessive accumulation of drugs, increased BUN, azotemia, hyperphosphatemia, and acidosis. Hepatic Impairment – Hepatotoxicity, monitor liver function tests. Pregnancy – should not be used during pregnancy, tetracyclines found in fetal tissue, and can produce retardation of skeletal development in the fetus and staining of deciduous teeth. Lactating women – expressed in breast milk, may affect milk production or composition. Children – 8 years or younger should not use any tetracycline, this drug form a stable calcium complex in any bone-forming tissue, decreasing bone growth. May cause permanent yellow/gray/brown discoloration of deciduous and permanent teeth. Enamel hypoplasia has also been reported. What are the most common drug interactions with levofloxacin? NSAIDs, Warfarin, Cyclosporin, Antacids, bismuth subsalicylate, iron salts, sevalamer, sucrafalate, and zinc salts. Cimetidine with all Fluroquinolones, Caffeine and warfarin with all, antacids, bismuth subsalicylate, iron salts, sucralfate, and zinc salts for an insoluble chelate. Levofloxacin interacts with NSAIDS and causes increase CNS stimulation and seizures. Antidiabetic drugs cause increase or decrease blood sugar. Increases PT and INR. Do not use in renal impairment, take with full glass of water. Community acquired pneumonia is levofloxacin, best choice. A patient is administered gentamicin and complains of sudden hearing loss. What should the nurse practitioner do?Term Discontinue (stop) the medication due to ototoxicity. Which medications interact with linezolid? MAOI interact as well as the other meds that interact with MAOI. Increases serotonin and can cause serotonin hypertensive crisis. Tirazine or aged foods. Which medications interact with linezolid? Adrenergic drugs (dopamine & epinephrine), MAOIs, SSRIs, TCIs, Ondansetron, Meperidine, Buspirone, Methadone, and Tramadol. New drug class approved 2000 (Zyvox) (class of antibiotics= oxazolidinones-synthetic antibiotics decrease naturally occurring drug resistance) interacts with Adrenergic drugs “vasopressors” or “dopaminergic” (dopamine and epinephrine), serotonergic ”Indirect- acting sympathomimetics” (SRIs), Food interactions are Tyramine rich foods and drinks. What is the course of treatment with doxycycline for the treatment of Lyme Disease? Early and aggressive antibiotic treatment. Doxycycline 100mg twice daily is the first-line drug of choice for early treatment. Children 8 years or older doxycycline 4mg/kg/d divided into twice daily. 23. What is the course of treatment with doxycycline for the treatment of Lyme Disease? 100 mg BID for 14-28 days depending on patient: Amoxicillin is the alternative in pregnant women and in children younger than 8 years old. Birth control becomes ineffective, patients can develop photosensitivity, patient needs to avoid dairy and iron, and separate dosing from thyroid medication if a part of the drug regimen. What are the main side effects of doxycycline? Phototoxicity, headache, and blurred vision. nausea, vomiting, upset stomach, mild diarrhea, skin rash or itching, and vaginal itching or discharge. Differentiate between oral and parenteral vancomycin. Oral vancomycin is poorly absorbed. Prenancy Class B low excretion in breast milk,125 mg -500mg every 6 hours for 7-10 days. Excreted in feces, some in urine and serum half-life is increase with renal impairment. Monitor for relief of diarrhea from coloitis c diff. IV Vanccomycin- Pregnancy class C. can cause ototoxicity, high excretion in breast milk, can cause red man syndrome if infused too fast, 2-3 grams infused divided into doses every 6-8 hours with dosage adjust for renal impairment. 90% of elimination if glomular filtration. Monitor peak and trough levels. Can cause decrease in platelets. Oral vancomycin is administered for C-Diff Parental administration it’s uses for systemic infection. Be sure to assess renal function and white blood cell count for inflammatory responses. What is the mechanism of action of azithromycin? Reversibly binds to the P site of the 50S ribosome subunit of susceptible organisms and may inhibit RNA-dependent protein synthesis by stimulating the dissociation of peptidyl-tRNA from ribosomes. Bacteriostatic, may be bacteriocidal depending on drug concentrations and the bacterial species tested. Treats bacterial infections. Active against gram-positive organisms. Which antibiotics block bacterial protein production? Rifamycins, Aminoglycocides, Macrolides, Ketolides, Tetracyclines, Glycyclines, Chloramphenicol, Stretogramins, Linezolid TThe U.S. Food and Drug Administration (FDA) regulates:erm The official labeling for all prescriptions and over-the-counter drugsDefinition Nurse practitioner prescriptive authority is regulated by: DThe State Board of Nursing for each stateefinition Electronic health records (EHRs) Allow for all patient data to be centralized in one location for access by multiple providers Alterations in drug metabolism among Asians may lead to Slower metabolism of antidepressants, requiring lower doses Pharmacokinetics among Asians are universal to all the Asian ethnic groups. B. False Gender differences between men and women in pharmacokinetics include: Higher proportion of body fat so that lipophilic drugs have relatively greater volumes of distributionDefinition The factor that has the greatest effect on males developing male sexual characteristics is: Androgen production An advantage of prescribing a sublingual medication is that the medication is: A. Absorbed rapidly Infants and young children are at higher risk of ADRs due to: B. Lack of safety and efficacy studies in the pediatric population Pharmacokinetic factors that affect prescribing include: C. Bioavailability Carbamazepine has a Black Box warning recommending testing for the HLA-B*1502 allele in patients with Asian ancestry prior to starting therapy due to: C. Increased risk for Stevens-Johnson syndrome in Asian patients with HLA-B*1502 allele Genetic polymorphisms account for differences in metabolism, including: D. All of the above A patient may develop neutropenia from using topical Silvadene for burns. Neutropenia is a(n): A. Cytotoxic hypersensitivity reaction The elderly are at high risk of ADRs due to: D. Age-related decrease in renal function The time required for the amount of drug in the body to decrease by 50% is called: Half-life The angiotensin converting enzyme (ACE) inhibitor lisinopril is a known teratogen. Teratogens cause Type ADR D Common OTC pain relievers such as acetaminophen or ibuprofen: Are harmful if taken in higher than recommended amounts A patient’s nutritional intake and lab work reflect hypoalbuminemia. This is critical to prescribing because: Distribution of drugs to target tissue may be affected Warfarin resistance may be seen in patients with VCORC1 mutation, leading to: Decreased response to warfarin The first step in the prescribing process according to the World Health Organization is: C. Diagnosing the patient’s problem A nurse practitioner would prescribe the liquid form of ibuprofen for a six-year-old because: A six-year-old may have problems swallowing a pill The point in time on the drug concentration curve that indicates the first sign of a therapeutic effect is the: COnset of Action When obtaining a drug history from Harold, he gives you a complete list of his prescription medications. He denies taking any other drugs, but you find that he occasionally takes aspirin for his arthritis flare-ups. This is an example of A common misconception that intermittently taken OTC medications are not an important part of his drug history Which one of the following statements about bioavailability is true? *Bioavailability issues are especially important for drugs with narrow therapeutic ranges or sustained release mechanisms All brands of a drug have the same bioavailability Drugs that are administered more than once a day have a greater bioavailability than drugs given once daily Combining an active drug with an inert substance does not affect bioavailability eta blockers treat hypertension because they: Reduce peripheral resistance Which of the following is true about procainamide and its dosing schedule? Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. Dulcea has type II diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? Gallbladder disease Patients who have angina, regardless of Class who are also diabetic should be on ? ACE Inhibitors Donald has been diagnosed with hyperlipidemia. On the basis of his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: Report muscle weakness or tenderness and dark urine to his provider immediately ACE inhibitors are the drug of choice in treating hypertension in diabetic patients because they: A. Improve insulin sensitivity B. Improve renal hemodynamics C. Reduce the production of angiotensin II D. All of the above Definition First-line therapy for hyperlipidemia is: Lifestyle changes Isosorbide dinitrate is a long-acting nitrate given twice daily (BID). The schedule for administration is 7 a.m. and 2 p.m. because Nitrate tolerance can develop Jamie is a thirty-four-year-old pregnant woman with familial hyperlipidemia and elevated LDL levels. What is the appropriate treatment for a pregnant woman? Bile acid-binding resins Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: Symptoms markedly worsen or the patient becomes hypotensive and has syncope. There is evidence of progressive renal insufficiency or failure. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic. All the above options are correct. Rodrigo has been prescribed procainamide after an episode of MI. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: Onset of congestive heart failure Compelling indications for an ACE inhibitor as treatment for hypertension based on clinical trials include: Renal parenchymal disease Which of the following disease processes could be made worse by taking a nonselective beta blocker? Asthma might worsen. Diabetes might worsen. Both might worsen. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as: A. Stage A B. Stage B C. Stage C D. Stage D C. Stage C Phil is a fifty-four-year-old male with multiple risk factors who has been on a high-dose statin for three months to treat his high LDL level. His LDL is 135 mg/dL, and his triglycerides are elevated. A reasonable change in therapy would be to: DeContinue the statin and add in ezetimibe.finition Which of the following drugs has been associated with increased risk for MI in women? Estrogen replacement Treatments for heart failure, including drug therapy, are based on the stages developed by the American Heart Association and the American College of Cardiology. Stage A patients are: DeTreated with drugs for hypertension and hyperlipidemia, if they existfinition A potentially life threatening adverse response to ACE inhibitors is angioedema. Which of the following statements is true about this adverse response? Swelling of the tongue and hoarseness are the most common symptoms A stepwise approach to the pharmacologic management of asthma: Begins with determining the severity of the asthma and assessing asthma controlDefinition A patient with a COPD exacerbation may require: Systemic corticosteroid burst The first-line treatment for cough related to a upper respiratory infection in a five-year-old is: Fluids and symptomatic careDefinition When treating a patient using the “step-down” approach, the patient with GERD is started on first PPIs In five- to eleven-year-old children, mild-persistent asthma is diagnosed when asthma symptoms occur: When using the “step-up” approach in caring for a patient with GERD, the “step up” from OTC antacid use is: Histamine 2 receptor antagonist (ranitidine) for four to eight weeks If a patient with H. pylori positive PUD fails first-line therapy, the second-line treatment is: DA PPI BID plus metronidazole plus tetracycline plus bismuth subsalicylate for fourteen daysefinition Howard is a seventy-two-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: Urinary retention Treatment failure in patients with PUD associated with H. pylori may be due to: Antimicrobial resistance Sadie is a seventy-two-year-old who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: A) Megaloblastic anemia B) Osteoporosis C) Hypertension D) Strokes Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing with their providers or a pharmacist first? A. Patients with kidney stones B. Pregnant patients C. Patients with heartburn D. Post-menopausal women Patients with allergic rhinitis may benefit from a prescription of : A. Fluticonase (Flonase)B. Certizine (Zyrtec)C. OTC cromoly nasal spray (Nasalcrom) D. Any of the above Tiotropium bromide (Spiriva) is an inhaled anticholinergic: Used for the treatment of COPD Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the National Heart, Lung, and Blood Institute (NHLBI) Expert Panel 3 guidelines. In adults, mild-persistent asthma is classified as asthma symptoms that occur: More than twice a week and less than once a day Pregnant patients with asthma may safely use throughout their pregnancies. inhaled corticosteroids (budesonide) Josie is a five-year-old who presents to the clinic with a forty-eight-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down, and her weight is 4 pounds less than her last recorded weight. Besides intravenous (IV) fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie? Ondansetron (Zofran) Judy is being prescribed phenytoin for seizures. Monitoring includes: Assessing for phenytoin hypersensitivity syndrome three to eight weeks after starting treatment When a patient is on selective-serotonin reuptake inhibitors: There is no laboratory monitoring required. Jaycee has been on escitalopram (Lexapro) for a year and is willing to try tapering off of the selective-serotonin reuptake inhibitors. What is the initial dosage adjustment when starting a taper off antidepressants? DReduce the dose by 50% for three to four days.efinition Cecilia presents with depression associated with complaints of fatigue, sleeping all the time, and lack of motivation. An appropriate initial antidepressant for her would be: Cymbata/Duloxetine Jake, a forty-five-year-old patient with schizophrenia, was recently hospitalized for acute psychosis due to medication noncompliance. He was treated with intramuscular (IM) long-acting haloperidol. Besides being monitored for his schizophrenia symptoms, the patient should be assessed by his primary care provider: With the Abnormal Involuntary Movement Scale (AIMS) for extrapyramidal symptoms (EPS) symptoms Selma, who is overweight, recently started taking topiramate for seizures and at her follow-up visit you note she has lost 3 kg. The appropriate action would be: A.Tell her to increase her caloric intake to counter the effects of the topiramate B.Consult with a neurologist, as this is not a common adverse effect of topiramate C.Decrease her dose of topiramate D.Reassure her that this is a normal side effect of topiramate and continue to monitor her weight D.Reassure her that this is a normal side effect of topiramate and continue to monitor her weight An appropriate first-line drug to try for mild to moderate generalized anxiety disorder would be: Buspirone (Buspar) When prescribing Adderall (amphetamine and dextroamphetamine) to adults with ADHD the nurse practitioner will need to monitor: A. Blood pressure B. Blood glucose levels C. Urine ketone levels D. Liver function Cynthia is taking valproate (Depakote) for seizures and would like to get pregnant. What advice would you give her? Valproate is a known teratogen but may be taken after the first trimester if necessary. Levetiracetam has known drug interactions with: A. Oral contraceptives B. Carbamazepine C. Warfarin D. Few, if any, drugs D. Few, if any, drugs A nineteen-year-old male was started on risperidone. Monitoring for risperidone includes observing for common side effects, including: Bradykinesia, akathisia, and agitation Sarah, a forty-two-year-old female, requests a prescription for an anorexiant to treat her obesity. A trial of phentermine is prescribed. Prescribing precautions include understanding that: Anorexiants may cause tolerance and should only be prescribed for six months. Prior to starting antidepressants, patients should have laboratory testing to rule out: Hypothyroidism Jack, eight years old, has attention deficit disorder (ADD) and is prescribed methylphenidate (Ritalin). He and his parents should be educated about the side effects of methylphenidate, which are: Insomnia and decreased appetite An appropriate drug for the treatment of depression with anxiety would be: Escitalopram (Lexapro) An appropriate drug for the treatment of depression with anxiety would be Lexapro The tricyclic antidepressants should be prescribed cautiously in patients with: Heart disease Anticholinergic agents, such as benztropine (Cogentin), may be given with a phenothiazine to: Reduce the chance of tardive dyskinesia. Six-year-old Lucy has recently been started on ethosuximide (Zarontin) for seizures. She should be monitored for: A. Increased seizure activity, as this drug may auto-induce seizures B. Altered renal function, including renal failure C. Blood dyscrasias, which are uncommon but possible D. Central nervous system excitement, leading to insomnia Henry is eighty-two years old and takes two aspirin every morning to treat the arthritis pain in his back. He states that the aspirin helps him to “get going” each day. Lately, he has had some heartburn from the aspirin. After ruling out an acute GI bleed, what would be an appropriate course of treatment for Henry? Add an H2 blocker such as ranitidine to his therapy. TermPatients need to be questioned about all pain sites because . patients tend to report the most severe, or important, in their perception When prescribing any headache therapy, appropriate use of medications needs to be discussed to prevent medication-overuse headaches. The clinical characteristics of medication-overuse headaches include . headaches recurring when medication wears off Different areas of the brain are involved in specific aspects of pain. The reticular and limbic systems in the brain influence . the motivational aspects of pain Narcotics are exogenous opiates. They act by . attaching to receptors in the afferent neuron to inhibit the release of substance P Juanita presents to clinic with a complaint of headaches off and on for months. She reports she feels like someone is “squeezing” her head. She occasionally takes Tylenol for the pain but usually just “toughs it out.” Initial treatment for tension headache includes asking her to keep a headache diary and a prescription for . naproxen (Aleve) Pathological similarities and differences between acute pain and chronic pain include which of the following options? Chronic pain has a predominance of C-neuron stimulation. Henry presents to clinic with a significantly swollen, painful great toe and is diagnosed with gout. Of the following, which would be the best treatment for Henry? Low-dose colchicines Pain assessment to determine adequacy of pain management is important for all patients. This assessment is done to determine which of the following options? If the diagnosis of source of pain is correct If the current regimen is adequate or different combinations of drugs and nondrug therapy are required If the patient is willing and able to be an active participant in his or her pain management All the given option Kirk sprained his ankle and is asking for pain medication for his mild-to-moderate pain. The appropriate first-line medication would be . ibuprofen (Advil) Chemical dependency assessment is integral to the initial assessment of chronic pain. Which of the following raises a “red flag” about potential chemical dependency? Multiple times when prescriptions are lost with requests to refill Phil is starting treatment with febuxostat (Uloric). Education of patients starting febuxostat includes which one of the following instructions? Gout may worsen with therapy. Kelly is a fourteen-year-old who presents to clinic with a classic migraine. She says she is having a headache two to three times a month. The initial plan would be which of the following? Prescribe NSAIDs as abortive therapy and have her keep a headache diary to identify her triggers. Patients prescribed aspirin therapy require education regarding the signs of aspirin toxicity. An early sign of aspirin toxicity is . tinnitus Which of the following statements is true about age and pain? Acetaminophen is especially useful in both children and adults because it has no effect on platelets and has fewer adverse effects than NSAIDs. When prescribed an opioid analgesic such as acetaminophen and codeine (Tylenol #3), which of the following instructions should the patient follow? The medication may cause sedation, so the patient should not drive. Constipation is a common side effect, so the patient should increase fluids and fiber. The patient should not take any other acetaminophen-containing medications at the same time. CORRECT All the given options are correct. Patients who are on or who will be starting chronic corticosteroid therapy need monitoring of: Serum glucose One of the main drug classes used to treat acute pain is NSAIDs. They are used due to which of the following reasons? Inflammation is a common cause of acute pain. Prophylactic use of bisphosphonates is recommended for patients with early osteopenia related to long-term use of which of the following drugs? Glucocorticoids Ashley comes to the clinic with a request for oral contraceptives. She has successfully used oral contraceptives before and has recently started dating a new boyfriend so would like to restart contraception. She denies recent intercourse and has a negative urine pregnancy test in the clinic. An appropriate plan of care would be: Prescribing oral contraceptives and having her start them the same day, with a back-up method used for the first seven days A woman who has migraine with aura: Should not be prescribed estrogen due to an increased risk of stroke occurring with estrogen use A contraindication to the use of combined contraceptives is: A history of clotting disorder Angela is a black woman who has heard that women of African descent do not need to worry about osteoporosis. What education would you provide Angela about her risk? Black women are at risk of developing osteoporosis due to their lower calcium intake as a group. Which of the following is the mechanism of action of oral combined contraceptives that prevent pregnancy? Progestins thicken cervical mucous and slow tubal motility. When starting a patient with hypothyroidism on thyroid replacement hormones, patient education would include the following: It may take four to eight weeks to get to euthyroid symptomatically and by lab testing. Inadequate vitamin D intake can contribute to the development of osteoporosis by: Altering calcium metabolism Absolute contraindications to estrogen therapy include: Clotting disorders The drug recommended as primary prevention of osteoporosis in men over seventy years is: Alendronate (Fosamax) Men who are prescribed sildenafil (Viagra) need ongoing monitoring for: The development of chest pain or dizziness Elderly patients who are started on levothyroxine for thyroid replacement should be monitored for: Tachycardia and angina Dosage changes of conjugated equine estrogen (Premarin) are made at intervals. six to eight week Infants with congenital hypothyroidism are treated with Levothyroxine Progesterone-only pills are recommended for women who: Are breastfeeding Have a history of migraine Have a medical history that contradicts the use of estrogen All of the above The ongoing monitoring of patients over the age sixty-five years taking alendronate (Fosamax) or any other bisphosphonate is: Annual renal function evaluation Sallie has been diagnosed with osteoporosis and is asking about the once-a-month pill to treat her condition. How do bisphosphonates treat osteoporosis? By reducing bone resorption and inhibiting osteoclastic activity Medroxyprogesterone (Depo Provera) injection has an US Food and Drug Administration (FDA) black box warning due to: Decreased bone density while on Depo GLP-1 agonists: Directly bind to a receptor in the pancreatic beta cell. Prior to prescribing metformin, the provider should: Draw a serum creatinine to assess renal function. The action of “gliptins” is different from other antidiabetic agents because they: Act on the incretin system to indirectly increase insulin production DPP-4 inhibitors (gliptins) act on the incretin system to improve glycemic control. Advantages of these drugs include: Low risk for hypoglycemia Hypoglycemia can result from the action of either insulin or an oral hypoglycemic. Signs and symptoms of hypoglycemia include: Dizziness, confusion, diaphoresis, and tachycardia When the total daily insulin dose is split and given twice daily, which of the following rules may be followed? Give two-thirds of the total dose in the morning and one-third in the evening. The American Diabetic Association has recommended which of the following tests for ongoing management of diabetes? Fasting blood glucose and Hemoglobin A1c Lispro is an insulin analogue produced by recombinant deoxyribonucleic acid (DNA) technology. Which of the following statements about this form of insulin is not true? The duration of action is increased when the dose is increased. The drugs recommended for older adults with type II diabetes include: Third-generation sulfonylureas The decision may be made to switch from twice a day (BID) NPH insulin to insulin glargine to improve glycemia control throughout the day. This is effective when: The initial dose of glargine is reduced by 20% to avoid hypoglycemia. Type I diabetes results from autoimmune destruction of the beta cells. Eighty-five to 90% of type I diabetics have: Autoantibodies to two tyrosine phosphatases Metformin is a primary choice of drug to treat hyperglycemia in type II diabetes because it: Decreases glycogenolysis by the liver Studies have shown that control targets that reduce the HBA1c to less than 7% are associated with fewer long-term complications of diabetes. Patients who should have such a target include: Those with no significant cardiovascular disease Type II diabetes is a complex disorder involving: A suboptimal response of insulin-sensitive tissues especially in the liver Both ACE inhibitors and some angiotensin-II receptor blockers have been approved in treating: Hypertension in diabetic patients Diabetic nephropathy Both A and B Before prescribing metformin, the provider should: Draw a serum creatinine level to assess renal function. Unlike most type II diabetics where obesity is a major issue, older adults with low body weight have higher risks for morbidity and mortality. The most reliable indicator of poor nutritional status in older adults is: Involuntary loss of 10% of body weight in less than six months Diagnostic criteria for diabetes include: Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl Sadie is an 82-year-old patient who has herpes zoster (shingles) and would benefit from an antiviral such as valacyclovir. Prior to prescribing valacyclovir she will need assessment of: Renal function The first-line drug choice for a previously healthy adult patient diagnosed with community acquired pneumonia would be: Azithromycin Monitoring for patients who are on long-term antifungal therapy with ketoconazole includes which of the following lab assessments: AST, ALT, alkaline phosphatase, and bilirubin Rose is a 3 year old with an upper respiratory infection (URI). Treatment for her URI would include: Amoxicillin atients who should be cautious about using decongestants for an upper respiratory infection include: Patients with cardiac disease Nicole is a 16 year old who is taking minocycline for acne. She comes to the clinic complaining of a headache. What would be the plan of care? Evaluate for pseudotremor cerebri Which of the following patients may be treated with a 3-day course of antibiotic therapy for their urinary tract infection? Jamie, a 24-year-old female Tetracyclines are contraindicated in children younger than 8 years because of: Adverse effects on bone growth The most common bacterial pathogen in community acquired pneumonia is: Streptococcus pneumoniae When prescribing acyclovir, patients should be educated regarding: Need to drink lots of fluids during treatment Fluoroquinolones have a Black Box warning regarding even months after treatment. Tendon rupture Nicholas has been diagnosed with Type A influenza. Appropriate prescribing of oseltamivir (Tamiflu) would include: Starting oseltamivir within the first 48 hours of influenza symptoms A factor that places a patient at risk of developing an antimicrobial resistant organism include: Inappropriate use of antimicrobials When prescribing metronidazole (Flagyl) to treat bacterial vaginosis, patient education would include: Consuming alcohol in any form may cause a severe reaction Jonathan has been diagnosed with strep throat and needs a prescription for an antibiotic. He says the last time he had penicillin he developed a red, blotchy rash. The appropriate antibiotic to prescribe would be: Erythromycin Samantha is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe? Azithromycin Sarah is a 25-year-old female who is 8 weeks pregnant and has a urinary tract infection. What would be the appropriate antibiotic to prescribe for her? Amoxicillin (Trimox) The chest circumference of a 12-month-old chest is 1-2 smaller than head circumference The NP is examining a 3-month old infant that has normal development. She has identified an alopecic area at the occiput . What should be done? Encourage the caregiver to change the infant's head position An infant is brought to the NP because his gaze is asymmetrical which finding indicates a need for referral He has persistent strabismus A tympanic membrane is erythematous which factor is not the cause of erythematous tympanic membrane? Coughing How long should a 6-year-old with AOM be treated with an antibiotic? 5-7 days The most common cause of acute pharyngitis in children is Respiratory virus Epstein-Barr virus is responsible for Mononucleosis A 6-year-old with sore throat, coryza, hoarseness, and diarrhea. What is the most likely etiology? Viral etiology A 3-year-old has been diagnosed with AOM. She is penicillin allergic (Type 1) hypersensitivity reaction. How should she be managed? Claithromycin Hand-foot-mouth and herpangina are viral infection caused by Coxsackie virus A young child with an audible murmur. the NP describes it as a grade 4. How should this be managed? Child should be referred to cardiology The NP identifies a satellite lesion in a 6-month-old infant. These are indicative of Candidal infection A 3-year-old female has a fever of 102F for three days. today she woke up from a nap and is febrile. She had a maculopapular rash? The rash will blanch(roseola or exanthema subitum) A 3-day old infant weighed 8 pounds at birth. Today he weighs 7.5 pounds. How should this be managed? Continue feeding every 2-4 hours. At what age is unusual to see thrush? Birth Cranial nerve II could be assessed in a young infant by? Assessing squinting response to bright light Which reflexes might a one-month-old infant be expected to exhibit? Moro, stepping, and rooting A 2-month-old infant has an asymmetric Moro reflex. What statement is true? The infant could have birth injuries What would be the appropriate anticipatory guidance for a 9 month old? Discuss weaning from the bottle When does a child's vision approximate 20/20? 5-6 years Conjunctivitis? usually begin with a viral infection The reflex that may be present in a 9 months of age during sleep Rooting A child that is 15 months old is referred to as a? Toddler A child is probably that can stack a maximum of 5 blocks is probably a 2 year old a young female has breast buds bilaterally. This represents a Tanner Stage 2 A what age does a child first walk backwards? 18 months When can a child be able to stand on 1 foot? age 3 At what age should initial BP screening take place? 3 years old what is the earliest age that an average child would appropriately receive construction paper and a pair of scissors with rounded point? Age 4 What is the earliest age that an average child would be able to copy a triangle, know his colors and count on his fingers? Age 5 What Tanner stage corresponds to an average 8 year old? Stage 1 The average age for pubertal growth spurt in a North American boy? 12-14 years A 6-month-old male has a palpable cystic mass in his scrotum. His mother states that sometimes the size of the scrotum seems larger than today during the exam. How should this be managed? Referral to urology if this has not resolved in 6 months An infant with diaper dermatitis with satellite lesions visible. This should be treated with a topical antifungal An NP has successfully reduced a nursemaid's elbow. How can an NP know that it was successful? Child moves the affected elbow. A congenital heart abnormality is often discovered during the newborn period is coaction of the aorta, How is this assessed? By comparing upper and lower extremity blood pressures A mother presents with her one-month-old infant she reports that he cries inconsolably every evening after his first evening feeding she asks for help. What would be done? Education, parental reassurance, and encouragement. A four-year-old female is brought into the clinic by mother who reports that she is constantly scratching" her privates"The patient states they itches. On exam the vagina is red and irritated. How should the NP proceed? Collect vaginal swab of the external vagina for microscopic evaluation. I this child has vaginitis. There are many diagnosis in the differential including pinworms, yeast, contact irritants form soap or bubble bath, et. Since the dx is not clear, some evaluation must occur in order to determine the dx so proper treatment can be initiated. Since the description of the problem does not indicate what the dx it is inappropriate to treat with a cortisone or topical antifungal.D A 3 days-old full-term infant has a bilirubin level of 16mg/ld. How should his be managed? Order phototherapy for the infant. A 2 year old has sudden onset of high fever while at daycare. The daycare attendant describes a seizure in the child. The child is brought to the clinic, neurologically he appears normal, and his body temperature is 99.9 F after receiving Ibuprofen. He is dx with otitis media, How should the nurse practitioner mange this? Treat the otitis media and give education about fever management. A 6 months old has a dis conjugate gaze. The Np observes that the 6 month old tilts his heads when looking at objects in the room. Which statement is true? The infant will have an abnormal cover/uncover test. A young child has developed a circumferential lesion on her inner forearm, it is slightly raised, and red and is pruritic. It is about 2.5 cm in diameter. This is probably related to: The child’s new cat (this describes ringworm, it is a fungal infection that is common in children. A typical precipitant is a new animal like a cat. Since it appears on the inner forearm it like the child got this from holding the cat. It should be treated with a topical antifungal At what age should screening for oral health begin? 6 months What vitamin will decrease peripheral neuropathy? Vitamin B6 Pyridoxine prevents the development of peripheral neuropathy secondary to use of Antimycobacterials such as Ethionamide and Ethambutol. What lab values should be assessed when administering valacyclovir? BUN and sodium creatinine may be assessed prior to therapy for those with risk factors for renal impairment and periodically during prolonged therapy to detect changes in renal function. When should oseltamivir phosphate be prescribed? Prophylaxis or treatment of Influenza A. According to the chart on 843 it is used for both Influenza A and B. Dosage for Prophylaxis - 75 mg PO every day for 4 weeks Treatment of Influenza Adults - 75 mg PO BID for 5 days Peds - ≤ 15 kg - 30 mg susp BID, <15-23 kg 45 mg BID, .23-40 kg 60 mg BID, >40 kg 75 mg BID. For what is rifampin prescribed? Tuberculosis as part of combined drug therapy. bactericidal against susceptible mycobacteria, Gonorrhea, Staphyloccous, Mycobacterium leprae (cause of leprocy), MAC, and H. Flu type B. Meningococcal meningitis prophylaxis, haemophilus influenzae meningitis prophylaxis. Infections involving prosthetic material caused by staphylococci. What are the adverse effects of isoniazid (INH)? Hepatotoxicity Peripheral neuropathy Give with pyridoxine (vit B6) to decrease neuropathy When is prophylactic oseltamivir recommended? For the prophylaxis after exposure to influenza A/B. Administer flu vaccine and 75mg PO daily once daily x 4 weeks. When prescribing ketoconazole, how should it be administered? Should be taken with food to alleviate GI symptoms and promote absorption. Do not give with antacids or statin drugs. Should not be given for patients with prostatic cancer. Should not be administered during pregnancy and children < 2 years of age. What is hypochlorhydria? When the stomach is unable to produce hydrochloric acid. What lab values should be monitored when administering antifungal agents? Need to monitor: AST, ALT, alkaline phosphate, and bilirubin should be monitored prior to initiation of therapy and monthly for 3-4 months and frequently after treatment. Even the slightest elevation in liver enzymes requires discontinuation of antifungal agents Identify which antihelmintic is used to treat parasitic worms. Pinworm- pyrantel pamoate, albendazole, and mebendazole Whipworm-pyrantel pamoate, albendazole, mebendazole Roundworm-mebendazole Hookworm-pyrantel pamoate, albendazole and mebendazole Threadworm-ivermectin and thiabendazole. Ivermectin is the drug of choice Thiabendazole in AIDS What antifungal medications can be used topically to treat fungal infections? Imidazole What are the main side effects of ethambutol? Optic neuritis, loss of visual acuity, color blindness Visual problems- check at baseline and then recheck throughout therapy Hyperuricemia (increased uric acid) gout Skin rash Not recommended for use in children (more difficult to assess visual Disturbances) What medication is used to treat scabies? Ivermectin 200 mcg/kg x1 and repeat in 1-2 weeks Worked well with immunocompromised but must be repeated 1- 2 weeks What are the side effects of rifampin? Anorexia, nausea, vomiting, diarrhea, flatulence, and abdominal pain. Hepatoxicity leading to hepatitis A harmless orange-red discoloration of body fluids – tears, saliva, urine, sweat, CSF, and feces. Hematuria Blood dyscrasias, headache, drowsiness, and inability to concentrate, pruritic rash, visual disturbances, lupus erythematosus, and exudative conjunctivitis. What are the bacterial cell wall composed of? Peptidoglydan What enzymes cross-linked by peptidoglydan polymers? Penicillin-binding proteins (PBPs) What are the rod-shaped bacteria? bacilli All beta-lactam antibiotics act by preventing the proper construction of the bacterial layer. peptidoglycan The four major classes of beta-lactam antibiotics are? penicillins cephalosporins carbapenems monobactems All beta-lactam antibiotics exert their effect by binding to? Penicillin-binding proteins (PBPs) The enzymes that cleave beta-lactam antibiotics thus inactivating them? beta-lactamases Penicillins all share the same basic structure which consist of a thiazolidine ring linked to a with a modifiable . bacto-lactomase ring side chain Natural penicillins have moderate activity against aerobic gram positive bacteria and anaerobic bacteria but poor activity against aerobic bacteria and most atypical bacteria gram-negative How are the cephalosporins grouped? They are grouped in generation In what class of antibiotics are cephalosporins? beta-lactamases What do cephalosporins bind to? Pencillin-binding proteins (PBPs) First generation cephlosporins are most useful in treatment of infections caused by? aerobic gram-positive bacteria Daptomycin has an excellent activity against aerobic bacteria gram positive Colistin binds to and disrupts in the bacterial outer membrane. lipopolysaccharide Colistin has activity against aerobic bacteria gram negative What will you instruct the patient related to rifamycins? They will turn the urine, tears, and body fluids orange-red color and Rifabutin is associated with uveitis The aminoglycosides have excellent activity against aerobic bacteria gram negative The aminoglycosides are used synergistic doses along with cell wall active agents to treat some aerobic bacteria gram positive The two major toxicities associated with the aminoglycosides are and . nephrotoxicity and ototoxicity RESPA is primarily involved with the disclosure of and the prevention of closing costs; kickbacks Who enforces RESPA regulations and who used to enforce? The Consumer Financial Protection Bureau currently enforces and HUD used to RESPA requires which 3 pre-settlement disclosures? Special information booklet, Loan Estimate, and the Mortgage Servicing Disclosure Statement What is required if a loan servicer sells or assigns the servicing rights to another loan servicer? Who requires this? Servicing Transfer Statement; required by RESPA According to , the loan servicer must notify the borrower days before the effective date of the loan transfer. RESPA; 15 days As long as the borrower makes timely payments to the old servicer within days of the loan transfer, the borrower cannot be penalized. 60 days Overages of $ or more discovered in a borrower's escrow account during the annual audit analysis must be refunded to the borrower. $50 What are the 2 disclosures that must be given at settlement? Who requires it? Closing Disclosure and Initial Escrow Statement; RESPA The HUD-1 Settlement Statement must be made available _ day(s) prior to closing and the Closing Disclosure must be delivered _ day(s) prior to closing. 1 day; 3 days prohibits a person from giving or accepting any part of a charge for services that are not performed. These illegal activities and referral fees are called . RESPA; kickbacks In order to protect itself from escrow shortages, the lender may require a cushion that doesn't exceed an amount equal to (fraction) of the total disbursements for the year. 1/6 What is Regulation B? Part of ECOA; specifies a borrower is entitled to copy of appraisal report, 3 business days before closing. ECOA Equal Credit Opportunity Act; prohibits discrimination based off race, gender, religion, etc. Who specifies that the borrower is entitled to a copy of the appraisal report before closing? How many days prior to closing must it be received? ECOA; 3 days What are the three choices available on the application regarding marital status? Married, unmarried, separated Who enforces ECOA? the CFPB Enforces the ECOA? Consumer Financial Protection Bureau A lender has days after receipt of an application to notify the applicant of it's action on the application. 30 days An application can request a statement of reasons within days of receiving the original adverse action notice. 60 days A lender has days after an application's request for an adverse action statement to provide that information 30 days What Act was passed by Congress in 1968 as part of the Consumer Credit Protection Act? TILA TILA was implemented by . The Federal Reserve Board TILA is administered by the CFPB (Consumer Financial Protection Bureau) Who administers TILA? The CFPB Regulation Z covers 3 general areas: 1. Disclosure of financing charges 2. Distribution of the Consumer Handbook on Adjustable-Rate Mortgages booklet 3. The right of rescission. APR disclosure must occur within business days of . 3 business days of receiving an application If the APR is quoted incorrectly by more than % (fraction) for a fixed rate loan, it must be re-disclosed before settlement. 1/8% If the APR is quoted incorrectly by more than % (fraction) for an adjustable-rate loan, it must be re-disclosed before settlement. 1/4% What must be disclosed if a triggering term is specified? The APR and the amount and terms of repayment The provides a 3 business day cooling-off period for a consumer who uses his primary residence as security for a refinance, home improvement, or second mortgage loan Right of Rescission The rescission period does not apply to a first mortgage on a purchase of a property The must be delivered at least business days prior to funding for reverse mortgages, equity lines of credit, mortgages secured by a mobile home, and dwellings not attached to land. The Truth-in-Lending Disclosure; 7 business days The APR must be finalized at least days before closing. 3 days HOEPA The Home Ownership and Equity Protection Act of 1994 What amends TILA and establishes requirements for certain loans with high rates and/or fees? HOEPA A high-cost home loan is one that charges the borrower more than % of the total loan amount for points and fees. 5% HMDA The Home Mortgage Disclosure Act The Home Mortgage Disclosure Act is implemented by The Federal Reserve Board's Regulation C HMDA requires lending institutions to report public loan data What was passed in 1970 to protect an individual's privacy rights and to ensure accurate and fair credit reporting? FCRA - Fair Credit Reporting Act Who is FCRA enforced by? The Federal Trade Commission Which act regulates the actions of the Credit Reporting Agencies and protects the rights of consumers to dispute incorrect information? The Fair Credit Reporting Act Bankruptcies can be kept in the credit report for years. 10 years Tax liens can be kept in the credit report for years from the time they were . 7 years; paid Which two commissions established a national Do-Not-Call Registry? Federal Communication Commission (FCC) & Federal Trade Commission (FTC) Telemarketers and sellers are required to search the registry at least once every and drop from their call lists the phone numbers of consumers who have registered. 31 days Violators of the telemarketing rules may be subject to fines of up to $ per violation $16,000 A company with which a consumer has an established business relationship may call for up to after the consumer's last purchase, delivery, or payment unless the consumer asks the company not to call again. 18 months Which act allows every individual to have a free copy of their credit report once a year from each of the three credit reporting agencies? The Fair and Accurate Credit Transaction Act (FACT Act) requires that financial institutions and creditors to develop written identity theft programs? The Red Flag Rule Who must manage The Red Flags program and include appropriate staff training and oversight of service providers? the Board of Directors or senior employees of the financial institution or creditor A finance charge is a fee the buyer would not pay if it were a cash deal. (Ex: Wire transfers and mortgage interest payments contribute to calculation of APR whereas hazard insurance and home inspections do not) A telephone call is sufficient for an adverse action notice? True or False False, it must be in writing What are the 4 loss mitigation options? 1. Refinance 2. Loan modification 3. Short sale 4. Deed-in-lieu If the servicer receives the mitigation application days before a foreclosure sale, the borrower's situation must be evaluated for app applicable options within days. The borrower may appeal a decision if the complete application package was submitted at least days before a schedule sale. 37 days; 30 days; 90 days High-cost home loans have which 3 restrictions? 1. Most balloon mortgages are prohibited 2. the borrower must prove an ability to repay 3. borrower must speak to a HUD-approved housing counselor Flipped homes are defined as resells within days with the seller paying a minimum of _% price increase or _% increase within 91- 180 days 90 days; 10%; 20% A qualified mortgage is one that follows stated guidelines intended to reduce a lender's liability (ex: positive amortization, no balloon payments, maximum 30 years, etc) MARS Mortgage Assistance Relief Services The Bank Secrecy Act and Anti-Money Laundering laws require companies to file a Currency Transaction Report with the IRS for cash purchases exceeding $ in one day. $10,000 Zero variance allowance 1. Real estate transfer taxes 2. Loan origination fees 3. Interest rate (Can have NO difference between Loan Estimate and Closing Disclosure) 10% variance limit -fees that the lender chooses or identifies (gov. recording fees, title, insurance) -cannot vary between LE and CD between 10% No limit on variance -Fees for services that owners choose themselves (ex: hazard insurance) The lender has business days after the closing for TRID-compliant loans to refund any portion of the charges that exceeded the acceptable amount of variance. business days for reverse mortgages. 60; 30 Higher priced loans are ones in which the APR exceeds the average prime rate by at least % for first-lien loans. 1.5% TIL disclosure includes: 1. APR 2. Finance charge 3. Amount financed 4. Total amount of payments In (MM/YY), the TRID went into effect and modified disclosure requirements for most closed-end loans, but not for reverse mortgages The TRID Loan Estimate combines and the initial TILA disclosure and the GFE The TRID Closing Disclosure combines and the final TILA disclosure and HUD-1 Settlement Statment The loan estimate must be delivered or mailed to no later than _ business days after an application is submitted and no later than _ business days prior to loan consummation. 3; 7 Lenders must ensure that the revised Loan Estimate is received _ business days prior to loan consummation (mailed at least _ business days prior) 4; 7 Changes in the APR, loan product or the addition of a prepayment penalty trigger a revised Closing Disclosure and an additional _ business day waiting period. 3 Non-numeric clerical errors and tolerance violations trigger a new Closing Disclosure that must be delivered without calendar days following loan consumption. Refunds must also be sent within days. 60 days When a consumer requests the cancellation of their escrow account, the lender must deliver an Escrow Closing notice no later than _ business days before closure. 3 days If the escrow account is closed for reasons beyond cancellation (refi, repayment, rescission) an Escrow Closing Notice must be sent business days prior to closure. 30 days Lenders must retain the Closing Disclosure and related documents for _ years, the Loan Estimate for _ years, and the Escrow Cancellation Notice and Partial Payment Policy for _ years 5; 3; 2 SAFE Act Secure And Fair Enforcement The SAFE Act is a part of the Act of 2008 Housing and Economic Recovery Act (HERA) Who oversees compliance with the SAFE act? (3) 1. The Conference of State Bank Supervisors (CSBS) 2. The American Association of Residential Mortgage Regulators (AARMR) 3. The Consumer Financial Protection Bureau (CFPB) Federal banking agencies include: 1. Federal Reserve System Board of Governors 2. National Credit Union Administration 3. Comptroller of the Currency 4. The Federal Deposit Insurance Corporation Define "immediate family members" spouse, parents, stepparents, child, stepchild, sibling, stepsibling, grandparent, grandchild, and adopted members A nontraditional mortgage product is any offer that is not a 30 year fixed-rate loan Who maintains the registry, approves mortgage schools and courses, and oversees state compliance? CSBS & AARMR A loan originator license application must meet either a net worth or requirement, or pay into the state fund. surety bond Pre-licensing education must include: -3 hours federal law -3 hours ethics -2 nontraditional mortgage products A minimum of _ hours of annual continuing education is required for all loan originators. 8 hours Continuing education must include: -3 hours federal law -2 hours ethics -2 hours nontraditional mortgage products Loan originators who are approved continuing education course instructors may receive hours of CE credit for every 1 hour taught 2 Loan originator organizations can receive compensation for selling additional products such as title insurance, but individual loan originators may not. True or False True Loan originator organizations must keep a record of payments from a creditor and payments to individual originators for years. 3 The is the mortgagor. Borrower The is the mortgagee. lender The two types of documents associated with a loan are the and the . mortgage; the note The is the legal evidence of the debt and is not recorded. note The is not included in the note. APR A occurs when a borrower obtains a mortgage from the seller to purchase a home. Purchase Money Mortgage There is an unlimited possible number of junior mortgages and no restrictions on terms. True or false? True Lien Theory states allow the borrower to obtain the at closing and agrees to allow the lender to place a on the property in exchange for the loan. The is the security instrument. deed; lien; mortgage States where the borrower does not receive the deed at closing are known as . Title Theory states. A is the enforcement of a lien. foreclosure is the choice by the lender not to take action even though the borrower is in default of the loan. Forbearance The equitable right of redemption allows the mortgagor in default to to keep the property from being foreclosed. pay the entire balance due A allows the lender to claim other assets from the borrower when the proceeds of the foreclosure sale are insufficient to satisfy the mortgage lien. deficiency judgment The mortgage acceleration clause allows the lender to if the borrower is in default. call the entire loan balance due The mortgage escalation clause allows the lender to under certain conditions. increase the interest rate of the loan The clause requires that the loan balance is paid off when the title is transferred. due-on-sale The mortgage defeasance clause: (2) 1. prevents the lender from foreclosing unless the borrower is in default 2. requires the lender to send a Satisfaction of Mortgage notice to a borrower within 60 days of paying off the loan The grantor is the owner of a property. The grantee is the party receiving the title transfer. A is a written instrument used to convey title or transfer ownership. deed What is it called when the mortgagor voluntarily conveys the deed to the lender in exchange for satisfaction of the debt? A Deed in Lieu of Foreclosure The FHA is a government agency within the Department of Housing and Urban Development The FHA provides 100% insurance to it's approved lenders. The lenders recover any losses experienced during a foreclosure or shore sale because the FHA makes up the difference to the lenders. True or false. True FHA loans have a required and regardless of the down payment amount. UFMIP; MIP FHA loans have a % late fee. 4% The downpayment for an FHA loan cannot be a gift from a relative. True or false? False FHA loans require the use of a FHA appraiser. True or False? True VA loans require a monthly insurance premium. True or False? False VA loans require a one time funding fee at closing. True or False? True VA loans require a veteran to produce a , which shows the amount of their entitlement. Certificate of Eligibility A VA appraisal is known as a . Certificate of Reasonable Value (CRV) VA loans have a % late fee 4 A mortgage is not insured or guaranteed by the government. conventinal Most conventional mortgage are not ; they do have a clause. assumable; due-on sale A conventional mortgage has a % late fee. 5 Sub-prime loans are the riskiest and are associated with poor . credit scores An ARM consists of two parts: an which fluctuates and a which is fixed. + = fully indexed rate index; margin and are two common indices. US Treasuries Securities rate; London Inter-Bank Offered Rate (LIBOR) The margin is expressed in basis points where points equals 1%. 100 A is a form of revolving credit, in which the home serves as collateral. The amount of the available credit line usually depends on the borrowers in the home. Home Equity Line of Credit; Equity The loan is the FHA's reverse mortgage loan. HECM The Gramm-Leach-Bliley Act is part of of 1999 The Financial Modernization Act Which act protects individuals' (not a business's) personal financial information held by financial institutions? Gramm-Leach-Bliley Act Who enforces the Gramm-Leach-Bliley Act laws for institutions that aren't already regulated by federal or state agencies? The FTC HPA Homeowner's Protection Act (1998) Homeowner's Protection Act 1998 - Protects people who buy primary residences using PMI The function of a wholesale lender is to provide servicing and pricing. (provides relief to the broker) A loan originator has years within which he can reinstate an expired license without retesting. 5 years What are the mortgage loan originator testing requirements? 20 hours of pre-licensing education which includes: 3 hours of federal law, 3 hours of ethics, and 2 hours of nontraditional mortgage products. What are the mortgage loan originator retesting requirements? 8 hours of pre-licensing education which includes: 3 hours of federal law, 2 hours of ethics, and 2 hours of nontraditional mortgage products. Mortgage loan originator applicants may not have had a felony in the last years. 7 years The NMLS was established by the CSBS & AARMR Who is responsible for determining that each state has mortgage loan originator licensing standards and that each state is participating in the NMLS? The CFPB State the purpose of the SAFE Act. (4) -increases uniformity in licensing & registration requirements among the states -reduces the regulatory burden of states -enhances consumer protection -reduces fraud Yearly RESPA is administered by the CFPB In an affiliated business arrangement, a provider of settlement services may have more than 1% ownership interest in another settlement service provider. True or false? True The Special Information Booklet must be given to only one or both borrowers? only one The CFPB Special Information Booklet cannot be part of other larger documents. Prepaids (and examples) -costs paid before 1st payment, usually in escrow ex: HOIP, MIP, Prepaid interest, property taxes Services you can shop for (3) -pest inspections -survey -a closing agent Services you cannot shop for (6) -appraisals -securing a credit report -flood determination -government funding (guarantee fee) -Homeowners Association certification -services rendered by the lender's attorney On the Loan Estimate, what are the charges called that are paid to the creditor or loan originator, including points to lower the rate? Origination charges Origination charges must be expressed both as a & . percentage of the amount credited; a dollar amount In order to discourage appraisal fraud caused by loan originator pressure, the FHA discourages flipping by determining that a property resold within days is not eligible for FHA. 90 days An originating lender may be required to return the SRP if . (Service Release Premium); the borrower defaults within the first 3 months The ARM index based on the interest expense on savings deposits reported by member savings banks in the Federal Home Loan Bank System's 11th District is called the . COFI - The 11th District Monthly Weighted Average Cost of Funds Index In a mortgage transaction subject to RESPA that is secured by the consumer's dwelling, a Closing Disclosure must be delivered or mailed within 3 business days after application and no later than . the 7th business day before the transaction is consummated. Under the Bank Secrecy Act, each institution must develop a written compliance program, which must be approved by . Anti-Money-Laundering; the institution's board of directors RESPA does not require lender disclosures of closing costs and procedures for . temporary construction loans After initiation of foreclosure on a consumer's principle dwelling, the finance charge and other disclosures affected by the finance charge are considered accurate if they are understated no more than or are . $35; greater than the amount required to be disclosed Federal Emergency Management Agency Which agency produces maps showing the floodplains? FEMA (Federal Emergency Management Agency) Who determines whether flood insurance is required for a particular property? the lender Under the rules for the Do-Not-Call Registry, a mortgage broker may make an unsolicited call to a client with whom he's established business with for up to from his last transaction. 18 months If a consumer makes an inquiry or submits an application to a company, the company can call for . 3 months TILA provides that the APR advertised for a mortgage loan can deviate from the actual rate offered by %. 0% A loan secured by vacant or unimproved property is covered under RESPA only if the loan proceeds will be used to . construct or place a structure or manufactured home on the real property within 2 years from loan settlement The minimum number of comparables needed for an appraisal is . 3 FNMA requires employment and income documentation to be dated no earlier than prior to the note date for loans. 120 days or 4 months What is the "principal-agent problem"? This exists because there is a relative lack of consequences for mortgage brokers and loan originators as they have no long-term interest in the performance of a loan. According to , loan applicants must be provided with the status of their application within . ECOA; 30 days The statement "You are not required to complete this agreement merely because you have received these disclosures or signed a loan application." is required by Regulation on loans. z; HOEPA loans What is a non-traditional mortgage? Any loan product other than a 30 year fixed. Interest only loan is a non-traditional mortgage. True or false? False. It's traditional because it has a 30 year term and a fixed rate. A loan originator who provided a revised Loan Estimate must retain documented reason for revision for . 3 years after settlement. For a new home purchase where the settlement is expected to be more than 60 days from the time the Loan Estimate is provided, the loan officer can provide a revised Loan Estimate any time up until . 60 calendar days to closing The terms each member serves on the Mortgage Broker Advisory Committee is . 3 years The Mortgage Broker Advisory Committee is composed of members; are mortgage brokers and are real estate brokers or sales people. 6; 4; 2 A mortgagee's Title Policy, issued by a title company at closing, is for who's benefit? the lender A mortgage loan that meets the underwriting requirements of Fannie Mae & Freddie Mac is known as a . conforming loan The penalty for red-lining is sever reprimand by , a $ fine, and loss of . the Federal Reserve; $10,000; charter to do business TILA is a body of Federal law passed as a part of the Act, and implemented by the . Federal Reserve Board Which Federal law was enacted to ensure that consumers are given uniform, understandable information about the cost of credit and that all disclosure are clear? TILA Section of RESPA requires the lender to perform an escrow analysis once per and notify the borrowers of any shortage and refund any overages over $ . 10; year; $50 Section of RESPA prohibits the from requiring the buyer to use a particular as condition of sale. 9; seller; title company Section 8 of RESPA prohibits . kickbacks For an ARM, the interest rate adjustments are tied to an independent . index For an ARM, the is fixed and is the percentage added to index rate. margin The power of sale clause gives the lender the right to . foreclose without first going to court A deed of trust is a three-party mortgage instrument that provides for non-judicial . foreclosure The promissory note is secured by the execution and recording of the . deed of trust The mortgagor holds the and the mortgagee holds . legal title; equitable interest The Federal National Mortgage Association was originally created in by the US government to purchase insured loans from loan originators & provide for lending institutions. 1930; FHA; liquidity FNMA purchases which types of loans? FHA; VA; & conforming conventional loans What are the duties of the Federal Reserve? (3) -Conduct the nation's monetary policy -regulate banking institutions -protect consumer credit rights Who must be members of the Federal Reserve System? All national, federally chartered, or FDIC insured banks. (Federal Deposit Insurance Corporation) All national, federally chartered, or FDIC insured banks must be members of . The Federal Reserve System FDIC Federal Deposit Insurance Corporation Usury laws are established by to determine the amount of that can be charged on loans and set caps on the max that can be charged. state legislators; interest; interest are established by state legislators to determine the amount of interest that can be charged on loans and set caps on the max interest that can be charged. Usury laws prohibits financial institutions from refusing to make loans in specific areas due to racial make up of area. Home Mortgage Disclosure Act is refusing to make loans in specific areas due to racial make up of area. Red-lining requires that the loan originator fill in to the best of their ability the applications race on the 1003 if the applicant does not fill it out themselves. HMDA The is interest and fees charged on a loan annually. APR The annual percentage rate is the interest and fees charged on a loan annually and includes paid by the borrower. points and other fees What are the 4 types of triggers in advertising? 1. amount of down payment 2. number of payments or period of repayment 3. amount of monthly payments 4. amount of any finance charges What must be disclosed if a trigger term is used in advertising? (3) 1. the amount or percentage of down payment 2. the terms of repayment 3. APR During a service transfer, the borrower cannot be penalized for making a timely payment to the prior servicer within days. 60 Define: state, individual, & person State: any state in the US or any territory of the US Individual: a natural person (1 person) Person: a natural person, corporation, company, partnership, or association A subordinate loan can have a higher or lower balance than the loan having priority. True or false? True A junior mortgage, or subordinate loan, may be given or at the same time as the primary loan. after A subordinate loan, or 2nd mortgage, has a greater risk to the lender and because of that it generally has a . higher rate In the event of a foreclosure, a subordinate loan may be removed as a lien if . the foreclosure proceeds can't pay it off Name the 4 Federal Banking Agencies. 1. The Board of Governers of the Federal Reserve System 2. The Comptroller of the currency 3. The National Credit Union Administration 4. The Federal Deposit Insurance Corporation HERA Housing & Economic Revovery Act of 2008 Title V The SAFE Act RESPA Real Estate Settlement Proceedures Act Real Estate Settlement Procedures Act was passed by in to provide consumer protection for loans on residential properties. congress; 1974 Which act is primarily involved with closing costs and kickbacks? RESPA Who enforces RESPA? The CFPB TILA was created in as part of the . 1968; Consumer Credit Protection Act TILA applies to commercial or other non-residential loans. True or false? False Which law covers disclosures, distribution of the Consumer Handbook on ARMs, and the right of rescission? TILA NMLS is developed and maintained by . CSBS & AARMR CFPB Consumer Financial Protection Bureau CFPB promotes financial , takes consumer , and researches consumer . education; complaints; behavior In , Obama signed the Dodd-Frank Street Reform and the Consumer Protection Act 2010 GNMA Government National Mortgage Association GNMA was created in and does not buy or sell loans, only guarantees them, and is a part of . 1968; HUD FHLMC Federal Home Loan Mortgage Corporation Federal Home Loan Mortgage Corporation or otherwise known as was created in . Freddie Mac; 1970 Freddie Mac buys and sells which types of loans? FHA, VA, & USDA Who controls the country's monetary policy? The Federal Reserve What is it called when a broker originates, processes, closes, and records a loan in its own name, but the loan is underwritten by, funded by, and assigned to a secondary lender at closing? table funding Upon repayment of the debt in full, the mortgage will voided. This is called . the defeasance clause When a borrower offers his property as security for a debt but does not give equitable title or possession to the lender, it is called . Hypothecation The transfer of title to real property from one party to another is called . conveyance How do you determine the housing or upfront ratio? PITI (+ HOA, PMI, or MIP if applicable) divided by gross monthly income How is LTV determined? loan amount divided by the property value or sales price (whichever is less) Piggyback loans, or simultaneous seconds, are not likely to be used anymore but are usually made when the LTV is over % and the borrower wants to avoid . 80%; PMI Discount points, or buydown, is defined as . prepaid interest at closing 1 discount point = % of the loan amount. 1% discount point(s) will reduce the interest rate by 1%. 6 The interest rate that would be charged if there were no additions or subtractions to the rate because of discount points is called . the par rate YSP Yield Spread Premium Yield Spread Premium is defined as . the points credited for an interest rate above it's par rate "No closing cost loans" usually result from applying the to pay the borrowers closing costs. Yield Spread Premium The Special Information Booklet is not required for . Refinances and reverse mortgages The Special Information Booklet is published by . the CFPB A is defined as a business entity that controls, is controlled by, or is under common control with. It also includes spouses, parents, and children, or anyone who has an agreement regarding referrals. associate The servicer must attempt loss mitigation by contacting the delinquent borrower within days and must sent written notice no later than the th day of delinquency. 36; 45 The Loan Estimate must be kept for years after settlement. 3 years The Closing Disclosure must be kept for years after settlement. 5 years Other disclosures besides the LE and CD must be kept for years after settlement. 2 years Assumption is defined as . whether or not the new owner can assume the seller's loan under original terms For ARMs, borrowers must be notified days before the first payment is due at adjusted level, and days for ARMs with adjustments every 60 days or more frequently. 60-120 days; 25-120 days The process of separating the criminal proceeds from their criminal origins using financial transactions in one or more accounts. (ex: a deposit of cash followed by a transfer of funds in almost the same amount) Layering The process of combining criminal proceeds with legal funds to provide legitimate ownership. Integration The process of introducing unlawful proceeds into the financial system. (ex: loan balances quickly reduced by multiple cash payments under reporting thresholds) Placement FinCEN is a bureau within the and is delegated the admin of the . US Treasury Department; BSA (Bank Secrecy Act) CTR Currency Transaction Report Currency Transaction Report are sent to for transactions with $ or more within days. A copy of these reports must be retained for years. FinCEN; $10,000; 15 days; 5 years On ARMs, when the rate increases but is capped off, the remaining interest not paid this term is called , and the borrower may have to repay what was missed when the rate decreases. carryover Prepayment penalties may not exceed _% of amount prepaid if paid within the first 2 years of the loan and may not exceed _% of the amount prepaid if paid within the 3rd year of the loan. 2%; 1% The appraisal approach, also known as the "market data" approach, is consider the most reliable and compares properties similar in , , , and . Sales Comparison; location; time of sale; conditions of sale; physical characteristics (size, amenities, condition of improvements) The approach for appraisals can be used for any appraisal but is best for new builds or buildings which can't be compared. cost How is the property value estimated in an appraisal with the cost approach? Replacement/Reproduction cost - Depreciation = Depreciated value Value of land - Depreciated value = Estimated property value The appraisal approach, otherwise known as the capitalization approach, is used to appraise properties that produce rental income. income How do you calculate the value using the income approach for appraisals? Gross income -allowance for vacancies and bad debts -fixed expenses (taxes and insurance) -operating expenses (repairs and management) -reserves to replace items =annual net income. Annual net income - capitalization rate = value Appraisal comparable adjustment limitations are as follows. Gross adjustments (positive and negative) are not to exceed % of the sales price and net adjustments are not to exceed % 25%; 15% Chapter bankruptcy is the implementation of a payment plan over years to pay off debts. 13; 3-5 Chapter bankruptcy involves the liquidation of assets so a person can start fresh. 7 What are the 4 "C"s of underwriting? 1. Capacity 2. Capital 3. Character 4. Collateral Regarding the 4 "C"s of underwriting, what does each one mean? (Capacity, Capital, Character, Collateral) 1. Capacity - ability to repay (income2. Capital - cash and assets3. Character - credit history4. Collateral - property used for the loan secured by appraisal What are the 4 actions used by Fannie Mae Desktop Underwriter? approve, refer, eligible, ineligible What are the 4 actions used by Freddie Mac Loan Prospector? accept, accept plus, caution, refer Which type of lender funds loans and sells to wholesale lenders? Correspondent lender A correspondent lender . funds loans and sells to wholesale lenders Which type of lender funds loans applied for through mortgage brokers? Wholesale lenders A wholesale lender . funds loans applied for through mortgage brokers A retail lender . interacts directly with the borrower and actually makes the loan The lender that interacts directly with the borrower and actually makes the loan is called the . Retail lender HECM Home Equity Conversion Mortgage A Home Equity Conversion Mortgage is also known as a . reverse mortgage A converts equity into cash for living expenses. Home Equity Conversion Mortgage (HECM), or reverse mortgage The loan originator charges for a HECM are %, plus 1% after the first $ , with a total cap of $ . 2%; 1%; $200,000; $6,000 One or both of the applicants for a HECM must be over 62? Only one Applicants for an HECM must receive . There are no requirements and no monthly . The factors considered in granting a HECM are: , , & . counseling; income; payments; age; property value; initial rate The borrowers promise to repay is called . the note The promissory note creates a lien. True or false? False The promissory note contains: -The terms of the loan, including the interest rate, but not APR Payment due dates -Late payment penalties -The right to repay along with any repayment penalties. AARMR Anerican Associate of Residential Mortgage Regulators CSBS Conference of State Bank Supervisors LLPA fee Loan Level Price Adjustment fee The fee is paid as a percentage from the borrower for increased-risk loans. LLPA VA DTI 41% FHA DTI 43% Conforming loan DTI 36% Jumbo loan DTI 38-40% Conforming loan housing ratio 28% FHA housing ratio 31% Jumbo housing ratio 33% USDA DTI 41% USDA housing ratio 29% USDA Front/Back end ratios 29%/41% FHA Front/Back end ratios 31%/43% VA Front/Back end ratios 41% DTI; no front end ratio Conforming loan Front/Back end ratios 28%/36% Jumbo Front/Back end ratios 33%/38-40% The punishment for an individual violating the BSA can be years in prison and up to $ . 20 years; $500,000 The punishment for covered financial institutions violating the BSA can be loss of , fines up to $ , and subject to . institution charter; $1,000,000; cease and desist order The punishment for covered financial institution employees violating the BSA can be , may be from industry, years in prison, and up to $ . termination; barred; 10 years; $500,000 The consequences for violating ECOA can be $ for an individual or for a corporation, $ or % net worth (whichever is ). $10,000; $500,000; 1%; less The penalties for violations of RESPA (kickbacks, fee-splitting, and unearned fees) can be up to $ and imprisonment for . $10,000; 1 year Punishments for false statements can be up to years prison and a $ fine. 5 years; $100,000 Punishment for a false mortgage loan application, conspiracy, bank fraud, etc, is up to years prison and/or a $ fine. 30 years; $1,000,000 What is the maximum find for violations to the SAFE act, per violation? $25,000 each What is the difference between closing costs and cash to close? Closing costs are the costs to do business and cash to close is closing costs plus down payment. Retirement and pension income must continue for years beyond the application date in order to be included as income. 3 years Receipt of alimony or child support payments must continue for years beyond the application date in order to be included as income. 3 years % of rental income from an investment property can be included. Rent from boarders in their primary residence or second home may not be included. 75% Generally, all installment debt should be considered part of the borrower's recurring monthly debt unless there are less than monthly payments remaining on the account. 10 The IRS 4506-T is the and the IRS 8821 is the . These documents can be signed by the borrower and used by the lender to verify income. Request for Transcript of Tax Return; Tax Information Authorization A first-time homebuyer can not have purchased a home in the past. True or false? False, a first-time homebuyer is someone who is purchasing a primary residence who has not had an interest in owning a primary residence in the last 3 years. years is generally the minimum time required by Fannie Mae between a bankruptcy charge or short sale and filing a mortgage loan application. This is years following a foreclosure. 4 years; 7 years If the entire down payment is a gift, the borrower must put at least % down unless it's a loan. 20%; FHA Cash-on-hand is not an acceptable source of funds for the down payment. True or false? True is the illegal practice of obtaining consumer information from financial institutions under false pretenses. Pre-texting The lender must provide a copy of the appraisal report to the borrower within business days prior to closing. 3 What information must be collected for demographics? What form is it on? race, ethnicity, and sex (when face to face). 3rd page of 1003 loan application. Who does Reg Z apply to? Who not? 3 National Credit Reporting Agencies: Experian, Transunion, and Equifax Define- Gramm-Leach-Bliley Act protect consumers personal, financial information held by financial institutions These calls are not limited by the DNC Registry political organizations, charities, or telephone surveyors Range of FICO scores 300-850 The HPA requires what? PMI cancelled when LTV reaches 78% original purchase price Prepares the closing disclosure Lenders or closing agents What does the USA Patriot Act require? mortgage applications provide name, address, SS#, and Photo ID. Allows electronic records and signatures to be valid, as long as its use is consented The E-Sign Act Who performs clerical/support tasks, and cannot negotiate loan terms? Underwriters, and loan processors Mortgage Companies and lenders must submit mortgage call reports to the NMLSR The senior mortgage is known as the mortgage FIRST This mortgage covers multiple tracks of land. blanket A valid contract has these (4) elements 1) competent parties 2) mutual agreement 3) legal object 4) consideration is an assumption in which the original borrower is released from all liability. novation Requires a down payment of 3.5% FHA Loan A 2/3/6 rate cap is initial adjustment, then every adjustment period after, with a lifetime cap OF 2%, 3%, 6% This loan is partially guaranteed, allows for 100% financing, one time funding fee, and no PMI USDA Loan USDA Loans are (3): 1) Lower income 2) Owner-occupied 3)30 year fixed rate loans Not insured or guaranteed by the government. Conventional Mortgage T/F- A conventional mortgage requires a 5% down payment. FALSE- 3% This loan exceeds Fannie/Freddie maximum loan amount. What loans are characterized by reduced documentation, high ratios, or limited assets? Alt-A The process of fully paying off a loan in regular payments over a specified period of time. Amortization occurs when the monthly mortgage payment decreases the loan. occurs when payments amount to less than the interest due. Positive amortization. Negative amortization. What does PITI stand for? Principle, interest, taxes and hazard/flood/mortgage insurance. A 360/180 loan is a amortized over years with a lump sum due after years. balloon; 30; 15 What is a term mortgage? a non-amortizing interest only loan. Balance is due at end of term in a balloon. Has a fixed rate and increasing payments so the loan balance is paid off more quickly. GEM (Growing Equity Mortgage) Mortgage interest in paid in arrears How is housing expense ratio determined? PITI/Gross Monthly Income What are the housing expense ratios for Fannie, FHA, and VA? 28% Fannie, 31% FHA, and VA doesn't consider. = PITI + other monthly debt/ Gross Monthly income Total Debt to Income Ratio What is the max Total Debt to Income Ratio for Fannie, FHA, and VA? Fannie- 36%, FHA- 43%, VA- 41% Who buys Conventional, FHA and VA loans? Fannie Mae Commission, Overtime, Bonus, Part-time, interest and dividend income must be averaged over years. 2 Fannie Mae emphasizes total obligations ratio at a maximum of ? 36% T/F- An applicant's interest rates can be locked in. TRUE- They can also float Fannie Mae requires a year history for all credit and public record info. 7 years Fair Isaac Corporation developed: FICO Credit Scores How is the late charge calculated? On the P&I portion only. T/F- An FHA Streamline Refinance doesn't require an appraisal, or income, and credit verification. TRUE What is the Underwriter's responsibility? evaluating the risk of the property and borrower. Fannie Mae's automated underwriting system is known as: Desktop Underwriter (DU) Freddie Mac's automated underwriting system is known as: Loan Prospector (LP) T/F- Appraisers are paid based on the appraisal value. FALSE- paid a flat fee Name the 7 protected classes under the Fair Housing Law: race, color, religion, sex, handicap, familial status, and national origin What 2 distinct areas does the FBI investigate mortgage fraud in? Fraud for profit, and fraud for housing Pushing a client into a transaction that makes more sense for the MLO than the client's long term interest. Steering A non-amortizing interest-only loan which balance is due at the end of term in a balloon payment. Term Mortgage The primary toxicity leading to death from an acetaminophen overdose is? Hepatocellular necrosis. Forms used by an appraiser to certify construction is complete 442 OR 1004D The TILA Disclosure must be given to the applicant within days after receiving the signed application for a reverse mortgage 3 business days The HMDA was implemented by Federal Reserve Board A guarantor or co-signer signs the: Note You have a patient who has been admitted to the Emergency Department with nausea, vomiting, muscle weakness, hypotension, dehyd ration and vascular collapse. Her family states she has Addison disease and recently experienced a mild case of Flu. The patient is experiencing acute renal crisis. You would prescribe the hormone replacement therapy that includes glucocorticoids, corti coid and mineral corticoids.Definition You have a patient who is administered prednisone for the treatment of inflammation. After taking the medication for one week he abruptly stops. What is the patient risk for? There is a risk for development of acute adrenoco rtical insufficiency Monitoring for Long term use of corticosteroids hyperglycemia, tuberculosis, peptic ulcer disease Adverse effects of corticosteroids Suppression of the physiologic response to infection, increased susceptibility, tuberculosis, herpes virus and varicella virus. GI complaints, nausea, vomiting, exacerbation of gastric ulcers, acne, osteoporosis, delayed wound healing, increased risk of fracture, sodium and fluid retention, increased blood glucose, anxiety and insomnia. Diabetics will need more insulin and nondiabetics are susceptible to increased blood sugar also and may need short term sliding scale. Adverse effects of nitrates include headache, flushing, dizziness, weakness, orthostatic hypotension, reflex tachycardia, skin irritation. Use caution with vasodilators such as Viagra, Lev itra, and Cialis T/F- Age is required HMDA borrower information. FALSE TILA disclosure requirements do NOT apply to these (3) loans. HELOCs, reverse mortgages, or chattel-dwelling loans (secured by mobile home or not attached to real property) A violation of Section 8 of RESPA may result in fines of $ and year(s) in prison. $10,000 1 Year In RESPA Class actions, total damages may not exceed... $1,000,000 OR 1% of the net worth of the servicer. When creditors refuse to make loans in certain neighborhoods due to personal characteristics of the residents Redlining Reverse Redlining: targeting neighborhoods with elderly, immigrant, and minority populations to make risky loans. applies to extensions of credit for business, commercial, and agriculture use. Which (2) do NOT? ECOA does. Respa & Tila do not. What are the central nervous system adverse effects with montelukast (Singular)? Suicidal ideations: Instruct the patient and family to assess for aggression, anxiety, and depression When administering albuterol and metformin, what should the patient be taught? To assess blood sugar due to drug induced hyperglycemiaDefinition When administering albuterol and metformin, what should the patient be taught? To assess blood sugar due to drug induced hyperglycemia What daily medication will control asthma? Inhaled steroids such as beclomethasone. What are the adverse effects of amiodarone? Pulmonary disease, Hypothyroidism, Hyperthyroidism, Sinus bradycardia, Prolongation of the QT interval, Ocular changes with corneal microdeposits, Optic nerve injury, Hepatotoxicity, Photosensitivity, Nausea, Vomiting, Diarrhea What medication is combined with a long- acting beta agonist? Inhaled corticosteroid should be combined with the long-acting beta agonist. What are the precautions and contraindications when administering beta receptor agonists? > Cardiac arrhythmias with tachycardia or heart block causes digitalis intoxication, angina, >narrow angle glaucoma > Diabetic patients can have drug-induced hyperglycemia > Patients taking digoxin and albuterol have a possible 30% decrease in blood digoxin levels > Patients with pheochromocytoma should avoid beta-adrenergic agonist due to severe hypertension >Long-acting beta agonists (Salmeterol) have been proven to have an increased risk of asthma-related> death >Long-acting beta agonists should not be used long term > Long-acting beta agonist must be combined with an inhaled corticosteroid Ipratropium (an inhaled anticholinergic agent) What is the bronchodilator of choice in a patient taking a beta blocker? Pseudoephedrine and phenylephrine What decongestant is contraindicated in children under the age of 4 years? What are the adverse effects of antihistamines? Drowsiness, urinary retention, hypertension, dizziness, headache, fatigue, cardiovascular collapse, insomnia, confusion Constipation is an adverse effect. Alkalosis may occur but tends to only in patients with renal impairment. What is the most common adverse effect when prescribing calcium carbonate antacids? Constipation is an adverse effect. Alkalosis may occur but tends to only in patients with renal impairment. Take as prescribed: 1-3 hours after meals and at bedtime Chewable tablets should be chewed not swallowed Shake suspensions Antacids may bind to other drugs separate from other medications by 2 hours Do not administer calcium based antacids with oxalic acid (spinach, rhubarb) or phytic acid (bran cereals); do not administer with milk or diary productions leads to milk alkali syndrome (nausea, vomiting, confusion, headache) Administering acidic fruit juice may improve absorption.Definition What is the action of loperamide? Loperamide binds to the opiate receptors of the intestinal wall leading to slowed gastric motility. It also reduces fecal volume, increases viscosity and bulk, and diminishes the loss of fluid and electrolytes. Gray black stools and black tongue What are the adverse effects of bismuth subsalicylate? Children (children should only need oral rehydrating solutions. What special population should not be administered bismuth subsalicylate? After each loose stoolAdminister with each meal and bedtime When should bismuth subsalicylate be administered? Does bismuth subsalicylate provide antimicrobial effects? It has antibacterial effect and antisecretory properties and is used to treat traveler’s diarrhea. Differentiate between ranitidine and famotidine. Ranitidine is 5-12 times more potent and famotidine is 30-60 times more potent than cimetidine to control gastric secretion. What lab values should be monitored with long-term administration of proton pump inhibitors? Assess for B12 deficiency and calcium deficiency. The patient is at risk for developing megaloblastic anemia. The patient is also at risk for developing hip fractures and osteoporosis. Due to calcium deficiency Why is osteoporosis a risk when taking omeprazole? Stimulants due to the direct action on intestinal mucosa by stimulating the mysenteric plexus. What is the most rapid-acting laxative and why? How does metoclopramide improve GERD? It stimulates motility in the upper GI tract. It sensitizes tissue to the action of acetylcholine. It increases tone and amplitude of gastric contractions and relaxes the pyloric sphincter and duodenal bulb, and increases peristalsis of the duodenum and jejunum, resulting in accelerated gastric emptying and increase speed of gastric transit. How do antacids improve GERD? Anatacids increase lower esophageal sphincter tone to manage GERD. Hip Which bone is likely to be fractured with long term proton pump inhibitor therapy? PPI and antimicrobial therapy What is the first line therapy for peptic ulcer disease with a positive pylori? first line therapy for peptic ulcer disease with positive pylori triple drug regimen or quadruple drug regimen that includes bismuth subsalicylate. Acid suppression by the PPI in conjunction with the antimicrobial helps alleviate the ulcer related symptoms, heals the gastric mucosal inflammation, and may enhance the efficacy of the antimicrobial agents against H.pylori at the mucosal surface. What is the first line therapy for peptic ulcer disease with a positive pylori? PPI and antimicrobial therapy Will antimicrobial resistance prevent the successful treatment of pylori? Limited antimicrobial resistance appears to be clarithromycin plus amoxicillin, plus a PPI, all taken twice a day for 10-14 days. Resistance to metronidazole is most common and higher in women, due to its use in treating genital infections. T/F: Conventional loans are insured OR guaranteed. FALSE. Conventional loans are not insured or guaranteed. What patient education should be provided to the patient taking antacids? Take as prescribed: 1-3 hours after meals and at bedtime Chewable tablets should be chewed not swallowed Shake suspensions Antacids may bind to other drugs separate from other medications by 2 hours Do not administer calcium based antacids with oxalic acid (spinach, rhubarb) or phytic acid (bran cereals); do not administer with milk or diary productions leads to milk alkali syndrome (nausea, vomiting, confusion, headache) Administering acidic fruit juice may improve absorption. Ranitidine is 5-12 times more potent and famotidine is 30-60 times more potent than cimetidine to control gastric secretion. Differentiate between ranitidine and famotidine. Assess for B12 deficiency and calcium deficiency. The patient is at risk for developing megaloblastic anemia. The patient is also at risk for developing hip fractures and osteoporosis What lab values should be monitored with long term administration of proton pump inhibitors? Why is osteoporosis a risk when taking omeprazole? Due calcium deficiency What is the most rapid acting laxative and why? Stimulants due to the direct action on intestinal mucosa by stimulating the mysenteric plexus. Acid suppression by the PPI in conjunction with the antimicrobial helps alleviate the ulcer related symptoms, heals the gastric mucosal inflammation, and may enhance the efficacy of the antimicrobial agents against H.pylori at the mucosal surface. How does the treatment with triple and quadruple regimen act Limited antimicrobial resistance appears to be clarithromycin plus amoxicillin, plus a PPI, all taken twice a day for 10-14 days. Resistance to metronidazole is most common and higher in women, due to its use in treating genital infections . Will antimicrobial resistance prevent the successful treatment of pylori? How do bronchodilators work? by acting on the bronchial smooth muscle of the bronchial tree to reverse bronchospasm, thereby decreasing airway resistance and residual volume & increasing vital capacity and airflow. How do leukotriene-receptor agents work? Act to decrease inflammation in the lungs What conditions are Beta 2-receptor-agonist bronchodilator agents used for? Asthma Reactive airway dx (RAD) COPD What is the most commonly prescribed Beta 2-receptor agonist? Albuterol What are the short acting Beta 2-receptor agonists? metaproterenol terbutaline bitolterol pirbuterol levalbuterol What are the long acting Beta 2-receptor agonists? arformoterol formoterol indacterol salmeterol How to Beta 2-agonists work? Beta agonists stimulate beta2 adrenergic receptors in the lungs to increase production of cyclic adenosine monophosphate (cAMP) by activation of adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cAMP. Increased cAMP concentrations relax bronchial smooth muscle and inhibit the release of mediators of intermediate hypersensitivity from cells, especially mast cells. What are the other body systems are affected by Beta 2 agonists? Cardiovascular Skeletal muscles Central nervous system Albuterol is a selective beta 2 agonist with some minor . beta 1 activity The international nonproprietary name for albuterol is . salbutamol How does albuterol affect beta receptors? Increases HR by stimulating beta 2 receptors in the heart Decreases BP and increases HR by stimulating beta 2 receptors in vascular smooth muscle causing vasodilation. Causes tremors by activation of beta 2 receptors of skeletal muscle The effect of albuterol on beta 2 receptors occurs only at because . high serum levels of low affinity for receptors and fewer beta 2 receptors than beta 1 receptors in the heart. has fewer cardiac and CNS effects than some of the other respiratory beta agonists and is, therefore, often the drug of choice for first line therapy. albuterol Levalbuterol is similar to , where the from racemic albuterol is removed, leaving the , which has less . albuterol (S)-isomer (R)-isomer Describe pirbuterol selective beta 2 agonist that is structurally identical to albuterol, except for the substitution of a pyridine ring for the benzine ring in its chemical make-up Describe terbutaline Selective beta 2 agonist with minor beta 1 activity Also known inhibit uterine contractions Describe metaproterenol Selective beta 2 agonist with some minor beta 1 activity Less selective than albuterol or terbutaline Describe bitolerol Hydrolyzed by the esterases in the lung to colterol or terbutylnorepinephrine which are selective beta 2 agonists are long-acting inhaled bronchodilators with a half-life ranging from . Salmeterol, formoterol, indacaterol, aformoterol 10 hours (fomoterol) - more than 40 hours (indacaterol) Describe salmeterol more selective for beta 2 receptors than albuterol and has minor beta 1 activity Describe formoterol 200-fold greater activity at beta 2 receptors than at beta 1 receptors Describe Aformoterol (R,R)-enantiometer of formoterol with twice the potency formoterol Describe indacterol 24-fold greater agonist activity at beta 2 receptors than beta 1 receptors exert long-lasting brochoprotection effects against allergen-, exercise-, histamine-, and methacholine-caused bronchospasm. Sameterol & formoterol Beta 1 receptor locations and effects of stimulation? • Cardiac pacemaker – increasing the heart rate • Myocardium – myocardium contracts more forcefully, increased ejection fraction • Salivary gland ducts – reabsorbs some water in the slowly passing saliva making it more viscous • Eccrine and apocrine sweat glands – increased sweat production. • Kidneys – increased renin release • Stomach - increased gherlin from stomach causing increased hunger Beta 2 receptor locations and effects of stimulation? • GI tract – decreased muscle tone and motility • Urinary bladder – decreased muscle tone enables greater filling, contraction of urethral sphincter • Skeletal muscle arteries – dilates blood vessels resulting in enhanced blood flow, decreased BP • Bronchial tree – bronchodilation • Some coronary vessels - increasing hormonally induced blood flow within the musculature of the heart • Uterus – relaxation • Kidneys – increased renin release which stimulates the production of angiotensin II and the subsequent release of aldosterone by the adrenal cortex. • Liver- glycogenolysis = increased glucose • Pancreas - release of glucagon = increased glucose What are the contraindications for beta 2 agonists? Cardiac arrhythmias associated with tachycardia Heart block caused by digitalis intoxication Angina Narrow-angle glaucoma Organic brain injury (decreased mental functioning not d/t mental illness) with epinephrine only Shock during general anesthesia with halogenated agents What patients should closely monitored during administration of respiratory beta agonists? Patients with: HTN Ischemic heart dx Coronary insufficiency CHF Hx of CVA or cardiac arrhythmias When taking bronchodilators, patients with diabetes may experience . hyperglycemia When taking bronchodilators, patients with hyperthyroidism may experience . more adverse reactions When taking bronchodilators, patients taking digoxin may experience . 30% decrease in blood digoxin levels Patients with pheochromocytoma should avoid . beta-adrenergic antagonists because severe HTN may occur doses of bronchodilators may be necessary in older adults because of sympathomimetic sensitivity. Lower increased What are the black-box warnings for bronchodilators? LABAs: salmeterol, formoterol, aformoerol, & indacterol respiratory & asthma-related intubation and death When should LABAs be introduced and why are they used? Only used long-term in patients whose asthma cannot be adequately controlled on asthma controller medications; not to be used alone. Used for shortest duration of time required to achieve control of asthma symptoms, then discontinued. Pediatric and adolescents should use a combination product containing both an inhaled corticosteroid and a LABA. What are the pregnancy categories of respiratory beta agonists? Terbutaline is a class B, all others are class C is used during pregnancy to prevent contractions r/t preterm labor. terbutaline Terbutaline to prevent pre-term contractions is not . FDA-approved What respiratory agonists are safe for use in children? Albuterol: infants & children (minimal adverse effects) Metaproterenol: young children Levabuterol: children 6 years & older Terbutaline Pirbuterol & Bitolterol: >12 years old Salmeterol: 4 years and older Formoterol: >5 years old Adverse reactions to the beta-agonist bronchodilators are usually . How are these adverse effects managed? transient Temporarily decrease dose, then slowly increase dose after rx to optimal dosing What are the adverse effects of beta agonist bronchodilators? Supraventricular and ventricular ectopic beats Tachycardia and palpitations CNS excitation - tremors, dizziness, shakiness, nervousness, restlesness Headaches Insomnia Post-inhalation cough Increased risk of exacerbation of severe asthma symptoms if the patient is deteriorating with salmeterol None of the LABAs should be started in patients with . acutely deteriorating asthma What precautions must be taken for patients taking beta agonist bronchodliators and digitalis glycosides? ECG monitoring for cardiac arrhythmias MAOI & TCA usage with certain beta agonists may . Which beta agonists? potentiate the bronchodilator effect on the vascular system. albuterol, metaproterenol, terbutaline Coadministration of drugs that lower potassium levels, such as diuretics, with beta agonists may cause . hypokalemia or ECG changes What drugs should not be used with aformoterol? Beta blockers MAOIs QT prolonging drugs What drugs should not be used with albuterol? Other sympathomimetics MAOIs TCAs BBs Thyroid hormones Ritodrine What drugs shouldn't be used with bitolterol? Other sympathomimetics MAOIs TCAs BBs What drugs shouldn't be used with indacterol? MAOIs QT prolonging drugs BBs What drugs shouldn't be used with levalbuterol? BBs MAOIs Other sympathomimetics What drugs shouldn't be used with metaproterenol? Other sympathomimetics MAOIs TCAs BBs Inhaled anesthetics What drugs shouldn't be used with pirbuterol? BBs MAOIs/TCAs within 14 days Which drugs shouldn't be used with salmeterol? BBs MAOIs TCAs What drugs shouldn't be used with terbutaline? Halogenated anesthetics MAOIs/TCAs maprotiline BBs & antihypertensive agents Cardiac gylcosides & levodopa What drugs shouldn't be used with respiratory anticholinergics? aclidinium - anticholinergics Ipratropium - Cromolyn Inhalation Solution (precipitates) Tiotropium - anticholinergics Doses of theophylline may need to be temporarily decreased after adminstration of . influenza vaccine Charlie is a 65-year-old male who has been diagnosed with hypertension and benign prostatic hyperplasia. Doxazosin has been chosen to treat his hypertension because it Relaxes smooth muscle in the bladder neck. To reduce potential adverse effects, patients taking a peripherally acting alpha1 antagonist should do all of the following EXCEPT: Monitor their blood pressure and skip a dose if the pressure is less than 120/80 Jim is being treated for hypertension. Because he has a history of heart attack, the drug chosen is atenolol. Beta blockers treat hypertension by: Reducing vascular smooth muscle tone Richard is 70 years old and has a history of cardiac dysrhythmias. He has been prescribed nadolol. You do his annual lab work and find a CrCl of 25 ml/min. What action should you take related to his nadolol? Extend the dosage interval Dwayne has recently started on carbamazepine to treat seizures. He comes to see you and you note that while his carbamazepine levels had been in the therapeutic range, they are now low. The possible cause for the low carbamazepine levels include: Carbamazepine auto-induces metabolism, leading to lower levels in spite of good compliance Selma, who is overweight, recently started taking topiramate for seizures and at her follow-up visit you note she has lost 3 kg. The appropriate action would be Reassure her that this is a normal side effect of topiramate and continue to monitor her weight Scott's seizures are well controlled on topiramate and he wants to start playing baseball. Education for Scott regarding his topiramate includes He should monitor his temperature and ability to sweat in the heat while playing Common mistakes practitioners make in treating anxiety disorders include Thinking a partial response to medication is acceptable Jamison has been prescribed citalopram (Celexa) to treat his depression. Education regarding how quickly SSRI antidepressants work would be Appetite and concentration improve in the first 1 to 2 weeks An appropriate first-line drug for the treatment of depression with fatigue and low energy would be Effexor Vicky, age 56 years, comes to clinic requesting a refill of her Fiorinal (aspirin and butalbital) that she takes for migraines. She has been taking this medication for over 2 years for migraine and states one dose usually works to abort her migraine. What is the best care for her? Assess how often she is using Fiorinal and refill medication Xi, a 54-year-old female, has a history of migraine that does not respond well to OTC migraine medication. She is asking to try Maxalt (rizatriptan) because it works well for her friend. Appropriate decision making would be Prescribe Maxalt and arrange to have her observed in the clinic or urgent care with the first dose Jayla is a 9-year-old who has been diagnosed with migraines for almost 2 years. She is missing up to a week of school each month. Her headache diary confirms she averages four or five migraines per month. Which of the following would be appropriate Prescribe propranolol (Inderal) to be taken daily for at least 3 months James has been diagnosed with cluster headaches. Appropriate acute therapy would be O2 100% for 15-30 minutes Age is a factor in different responses to pain. Which of the following age-related statements about pain is NOT true? Preterm and newborn infants do not yet have functional pain pathways Chronic pain is a complex problem. Some specific strategies to deal with it include Scheduling return visits on a regular basis rather than waiting for poor pain control to drive the need for an appointment Patients need to be questioned about all pain sites because Patients tend to report the most severe or important in their perception albuterol is rarely used in children. Oral Frequent use of for exercise-induced asthma is discouraged. LABAs The FDA recommends that pediatrics and adolescents who require the addition of a LABA be prescribed a . combination product to increase compliance (LABA & corticosteroid) is an inhaled anticholinergic that may be used in combination with to treat asthma exacerbations in the ER. Ipratropium albuterol is the bronchodilator of choice in patients who are taking beta blockers or who do not tolerate beta 2 agonists. Ipratropium have a shortened duration of action if used on a daily basis. LABAs What is the recommended treatment for prevention of exercise-induced asthma? Inhaled albuterol (2 puffs 15 minutes prior) or other SABA Salmeterol (2 puffs 30-60 minutes prior). Choosing an appropriate bronchodilator is a matter of . the age of the patient and cost The only SABAs that can be prescribed to children under 4 are . albuterol & metaproterenol Levalbuterol can only be used in children older than . 4 is the most common SABA given to infants albuterol Of all the SABAs, is the least expensive. albuterol Response to SABAs should be monitored with . a peak flowmeter It is recommended that a be used with MDIs to . spacer device increase deposition of medication into the lungs rather than the mouth Teaching on how to use an inhaler properly. Exhale first, tilt head slightly back Place the inhaler mouthpiece either 2 inches from open mouth or between open lips While inhaling, press down on canister, breathe in slowly and deeply, and hold breath for 10 seconds If 2 puffs prescribed, wait 1 min between inhals Describe Aerochamber tube-like device that has pictures drawn on outside to remind the patient of proper technique for using inhaler. Emits a whistling sound if the patient is taking too rapid of a breath Describe InspirEase Spacer gives a visual cue of the spacer of the spacer bag deflating to help in taking a deep-enough breath, Emits a whistling sound if the patient is taking too rapid of a breath What key points should be taught about nebulizer usage? Accurate measurement of medication & appropriate cleaning of equipment Teaching about Advair Diskus? Do not exhale or blow into Diskus Diskus should not be washed or taken apart Teaching about Neohaler Capsule must be removed from a blister pack immediately before inserting into Neohaler Indacterol capsules that are exposed to air for prolonged periods should be discarded Do not swallow capsules Overuse of beta 2 agonists can cause . seizures hypokalemia anginal pain HTN What symptoms should patients report when using beta 2 agonist bronchodilators? palpitations tachycardia chest pain muscle tremors dizziness headache flushing What are the methylxanthines? theophylline aminophylline caffeine Two life threating adverse drug reactions hypoglycemia diabetic ketoacidosis Patient education regarding prescribed medication includes: B. Discussion of expected adverse drug reactions Which of the following patients would be at higher risk of experiencing adverse drug reactions (ADRs): C. A 3-month-old female Adverse drug reactions and patients’ perceptions of them are likely to produce non-adherence. Which of the following ADRs are least likely to produce non-adherence? A. Severe hypotension and anaphylaxis What adverse drug reactions (ADRs) are the elderly at risk of developing? physiologic changes: increase the proportion of body fat so you have increase storage of fat soluble drugs, increased cardiovascular effects, decrease drug metabolism in the liver, decrease renal function, increase effect of drugs on the CNS drug toxicity and death A genetic variation in how the metabolite of the cancer drug irinotecan SN-38 is inactivated by the body may lead to: B. Increased adverse drug reactions, such as neutropenia Adverse drug reactions in elderly people are the result of: changes in drug metabolism due to diminished hepatic function List 4 risk factors for adverse drug reactions Elderly, very young, severe illness, multiple drug use Beer's criteria helps indicate medications that may be inappropriately prescribed for the elderly patient; serves as "red flags" beers criteria list of potentially inappropriate meds to use with 65+ Beers Criteria potentially inappropriate medication (PIM) in older patients Beers criteria -basic guidelines for identifying drugs that are "potentially inappropriate medications" for the elderly-Davis -> medication safety tools - > Beers Criteria-DAvis-> medication safety tools -> drugs associated with increased risk of falls in the elderly-risk/benefit ratio-used for pateints greater to or = 65 Beers Criteria To reduce medication related risks For all ambulatory settings Monitoring of adverse effects Developed in 1991 for SNF's 53 medications "Start low and go slow" BEERS criteria avoid these drug in elderly: first gen antihistamine, GI antispasmodics, antithrombotics dipyramole ticlopidine, a blocker(ortho hypo), central alpha agonists, antiarrhythmics; TCA, anti psychotics, barbs, benzo; sliding scale insulin, sulfonylureas; indomethacin, muscle relaxants (sedation), meperidine Widely used criteria for medication use in the elderly, aimed at decreasing adverse drug events. Beers Criteria What are some criteria that tell whether a med is appropriate for the elderly pop Beers Criteria Polycythemia Increased RBI production hemoglobin and hematocrit Causes of polycythemia Primary polycythemia: polycythemia Vera, primary familial polycythemia Secondary (physiologic adaptation): high altitude, hypoxia induced (chronic, copd) Non-adaptation: neoplasm, anabolic steroid abuse, EPO administration What is the anemic effect HGB level approximates potential negative consequences of anemia; however clinical assessment is key to determine consequences in the individual patients How to assess for anemia effect Symptoms objective findings co-morbidities General causes anemia Increased destruction (hemolytic anemias) like sickle cell blood transfusion reaction Increased loss like hemorrhage Ex: trauma, gi bleed, menstruation Fluid overload: Late pregnancy, excess fluid intake/admin What does testing the rbcs do? Narrow the differential diagnosis Subjective symptoms. Primary Primarily related to two factors Decreased oxygen delivery to tissues Hypovolemia and compensatory General subjective symptoms Fatigue Hyper dynamic state like pallor palpitations Severe symptoms Lethargy confusion medical complications like HF. MI Sure history subjective Trauma Chronic subjective history PHM. Alcohol chronic disease coagulopathy nutrition significant family history medicine Blood loss: occult or non-occult blood loss Physical exam findings Pallor Hyper dynamic state- tachycardia Hypoperfusion- pallor conjunctiva Blood loss- abdominal source Coagulopathy- petichiae Jaundice Neurological findings - vit B12 deficiency Adenopathy CBC testing Hot HGB Because RBc indices, MCV. RBc size, MCHC a& MCH HGB concentration Retic count ( when available on CBC) Plasma volume is blank with dilution Increased Plasma volume is blank with concentration Decreased With an acute bleed you would expect to see your over all volume what Decreased deficit Late in pregnancy you would expect to see an increase or decrease in your plasma volume Increase What could possibly mask your underlying anemia with regards to volume status Add a pleated volume my mask underlying anemia fluid status until it is restores Populations that may have a skewed normal CBC interpretation High altitude smokers African-Americans compared to Caucasians older adults athletes these are all considerations in determining polycythemia evaluations What is the reticulocyte And assessment of the red blood cells production by the bone marrow What is the reticulocyte Rbc recently released from the bone marrow Hi reticulocyte count Increase production responding to red blood cell loss or deficient red blood cell production or hemolysis What does the peripheral blood smear indicate or show It allows more detailed morphology and other characteristics additional evaluation for Normocytic and macrocytic anemia abnormal findings consider Milo dysplastic syndrome malignancy multiple myeloma bone marrow biopsy How would you perform our studies no I really performed fasting it assesses iron levels Panel to assess our studies consist of Ferritin serum iron level and a total iron binding capacity transferrin (TiBC). transferrin saturation What test indicate early vitamin B 12 deficiency earlier than the anemia development Methyl malonate (MMA). And homocysteine Homocysteine Commonly used classification due to availability on the CBC panel hemoglobin concentration MCHC equals chromic what is the most commonly used starting portion of the CBC for anemia Mean corpuscle value MCV MCV in microcytic is increased or decreased Microcytic is decreased To test the best discriminate IDA or iron deficiency anemia Ferritin in the TIBC microcytic and hypochromic with a low Redtip count likely to be which kind of anemia Iron When your ferritin is normal or your TIBC is low to normal what test would you order next A peripheral blood smear and see reactive proteins for inflammation a BUN and creatinine level and a hemoglobin electrophoresis A normal reticulocyte Count Normal is 1 to 2% Increased reticular account Greater than 2% Hemoglobin of less than 12 and an MVC less than 81 could mean Iron deficiency Thalassemia sideroblastic anemia lead intoxication chronic disease late Hemoglobin less than 12 in mCV 81 to 100. Could mean Acute blood loss chronic disease chronic renal insufficiency hypothyroidism bone marrow suppression Hemolysis G6DP deficiency a plastic anemia Hemoglobin less than 12 MCV greater than 100 could mean Vitamin B 12 deficiency folate deficiency liver disease reticulocytosis Myelodysplastic syndrome's alcohol abuse drugs chemotherapy agents hydroxyurea Microcytic blood smear. Decreased iron increase TIBC decreased ferritin equals Iron deficiency anemia To prevent the development of peripheral neuropathy in patients taking isoniazid for tuberculosis the patient is also prescribed: Pyridoxine (Vitamin B6) Pong-tai is a 12 month old who is being treated with amoxicillin for acute otitis media. His parents call the clinic and say he has developed diarrhea. The appropriate action would be to: Advise the parents that some diarrhea is normal with amoxicillin and try feeding him yogurt daily Lauren is a 13 year old who comes to clinic with a 4-day history of cough, low grade fever, and rhinorrhea. When she blows her nose or coughs the mucous is greenish-yellow. The appropriate antibiotic to prescribe would be: None Both men and women experience bone loss with aging. The bones most likely to demonstrate significant loss are: A. Cortical bone B. Femoral neck C. Cervical vertebrae D. Pelvic bones B. Femoral neck Bisphosphonates treat or prevent osteoporosis by: A. Inhibiting osteoclastic activity B. Fostering bone resorption C. Enhancing calcium uptake in bone D. Strengthening the osteoclastic proton pump A. Inhibiting osteoclastic activity Prophylactic use of bisphosphonates is recommended for patients with early osteopenia related to long-term use of which of the following drugs? A. Selective estrogen receptor modulators B. Aspirin C. Glucocorticoids D. Calcium supplements C. Glucocorticoids Patients with cystic fibrosis are often prescribed enzyme replacement for pancreatic secretions. Each replacement drug has lipase, protease, and amylase components, but the drug is prescribed in units of: A. Lipase B. Protease C. Amylase D. Pancreatin A. Lipase Brands of pancreatic enzyme replacement drugs are: A. Bioequivalent B. About the same in cost per unit of lipase across brands C. Able to be interchanged between generic and brand-name products to reduce cost D. None of the above B. About the same in cost per unit of lipase across brands When given subcutaneously, NPH insulin begins to take effect (onset of action): A. 15 to 30 minutes after administration B. 60 to 90 minutes after administration C. 3 to 4 hours after administration D. 6 to 8 hours after administration B. 60 to 90 minutes after administration Hypoglycemia can result from the action of either insulin or an oral hypoglycemic. Signs and symptoms of hypoglycemia include: A. “Fruity” breath odor and rapid respiration B. Diarrhea, abdominal pain, weight loss, and hypertension C. Dizziness, confusion, diaphoresis, and tachycardia D. Easy bruising, palpitations, cardiac dysrhythmias, and coma Dizziness, confusion, diaphoresis, and tachycardia Nonselective beta blockers and alcohol create serious drug interactions with insulin because they: A. Increase blood glucose levels B. Produce unexplained diaphoresis C. Interfere with the ability of the body to metabolize glucose D. Mask the signs and symptoms of altered glucose levels D. Mask the signs and symptoms of altered glucose levels Lipro is an insulin analogue produced by recombinant DNA technology. Which of the following statements about this form of insulin is NOT true? A. Optimal time of preprandial injection is 15 minutes. B. Duration of action is increased when the dose is increased. C. It is compatible with NPH insulin. D. It has no pronounced peak. B. Duration of action is increased when the dose is increased. The decision may be made to switch from BID NPH insulin to insulin glargine to improve glycemia control throughout the day. If this is done: A. The initial dose of glargine is reduced by 20% to avoid hypoglycemia B. The initial dose of glargine is 2 to 10 Units per day C. Patients who have been on high doses of NPH will need tests for insulin antibodies D. Obese patients may require more than 100 Units per day A. The initial dose of glargine is reduced by 20% to avoid hypoglycemia When blood glucose levels are difficult to control in Type 2 diabetes some form of insulin may be added to the treatment regimen to control blood glucose and limit complications risks. Which of the following statements are accurate based on research? A. Premixed insulin analogues are better at lowering HbA1C and have less risk for hypoglycemia. B. Premixed insulin analogues and the newer premixed insulins are associated with more weight gain than the oral antidiabetic agents. C. Newer premixed insulins are better at lowering HbA1C and post-prandial glucose levels than are long-acting insulins. D. Patients who are not controlled on oral agents and have post-prandial hyperglycemia can have NPH insulin added at bedtime. C. Newer premixed insulins are better at lowering HbA1C and post-prandial glucose levels than are long-acting insulins. Insulin preparations are divided into categories based on onset, duration, and intensity of action following subcutaneous inject. Which of the following insulin preparations has the shortest onset and duration of action? A. Insulin lispro B. Insulin glulisine C. Insulin glargine D. Insulin detemir B. Insulin glulisine Metformin is a primary choice of drug to treat hyperglycemia in Type 2 diabetes because it: A. Substitutes for insulin usually secreted by the pancreas B. Decreases glycogenolysis by the liver Increases the release of insulin from beta cells D. Decreases peripheral glucose utilization B. Decreases glycogenolysis by the liver The action of “gliptins” is different from other antidiabetic agents because they: A. Have a low risk for hypoglycemia B. Are not associated with weight gain C. Close ATP-dependent potassium channels in the beta cell D. Act on the incretin system to indirectly increase insulin production D. Act on the incretin system to indirectly increase insulin production Sitagliptin has been approved for: A. Monotherapy in once daily doses B. Combination therapy with metformin C. Both A and B D. Neither A nor B C. Both A and B GLP-1 agonists: A. Directly bind to a receptor in the pancreatic beta cell B. Have been approved for monotherapy C. Speed gastric emptying to decrease appetite D. Can be given orally once daily A. Directly bind to a receptor in the pancreatic beta cell Avoid concurrent administration of exenatide with which of the following drugs? A. Digoxin B. Warfarin C. Lovastatin D. All of the above D. All of the above Administration of exenatide is by subcutaneous injection: A. 30 minutes prior to the morning meal B. 60 minutes prior to the morning and evening meal C. 15 minutes after the evening meal D. 60 minutes before each meal daily B. 60 minutes prior to the morning and evening meal Potentially fatal granulocytopenia has been associated with treatment of hyperthyroidism with propylthiouracil. Patients should be taught to report: A. Tinnitus and decreased salivation B. Fever and sore throat C. Hypocalcemia and osteoporosis D. Laryngeal edema and difficulty swallowing B. Fever and sore throat Elderly patients who are started on levothyroxine for thyroid replacement should be monitored for: A. Excessive sedation B. Tachycardia and angina C. Weight gain D. Cold intolerance B. Tachycardia and angina ACE inhibitors are a central part of the treatment of heart failure because they have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors? A. Changes in the structure of the left ventricle so that it dilates, hypertrophies, and uses energy less efficiently. B. Reduced formation of cross-bridges so that contractile force decreases. C. Activation of the sympathetic nervous system that increases heart rate and preload. D. Decreased renal blood flow that decreases oxygen supply to the kidneys. C. Activation of the sympathetic nervous system that increases heart rate and preload. One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include: A. Myocardial ischemia and injury secondary to myocardial infarction B. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction C. Increased demands of the heart beyond its ability to adapt secondary to anemia D. Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension A. Myocardial ischemia and injury secondary to myocardial infarction Diagnosis of heart failure cannot be made by symptoms alone since many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is: A. Chest x-rays that show cephalization and measure heart size B. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction C. Complete blood count, BUN, and serum electrolytes that facilitate staging for end-organ damage D. Measurement of brain natriuretic peptide to distinguish between systolic and diastolic dysfunction B. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with: A. Drugs for hypertension and hyperlipidemia, if they exist B. Lifestyle management including diet, exercise, and smoking cessation only C. ACE inhibitors to directly affect the heart failure only D. No drugs are used in this early stage A. Drugs for hypertension and hyperlipidemia, if they exist Class I recommendations for Stage A heart failure include: A. Aerobic exercise within tolerance levels to prevent the development of heart failure B. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention C. Beta blockers for all patients regardless of cardiac history D. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias D. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias Stage B patients should have beta blockers added to their heart failure treatment regimen when: A. They have an ejection fraction less than 40% B. They have had a recent MI C. Both A and B D. Neither A nor B C. Both A and B Increased life expectancy for patients with heart failure has been associated with the use of: A. ACE inhibitors, especially when started early in the disease process B. All beta blockers regardless of selectivity C. Thiazide and Loop diuretics D. Cardiac glycosides A. ACE inhibitors, especially when started early in the disease process Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with: A. Ejection fractions above 40% B. An audible S3 C. Mitral stenosis as a primary cause for heart failure D. Renal insufficiency B. An audible S3 Which of the following classes of drugs is contraindicated in heart failure? A. Nitrates B. Long-acting dihydropyridines C. Calcium channel blockers D. Alpha-beta blockers C. Calcium channel blockers Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is: A. Aldosterone antagonists B. Eplerenone C. ACE inhibitors D. ARBs C. ACE inhibitors ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes are considered to be safe, at least in the later parts of pregnancy? A. Diuretics B. Beta blockers D. Nitrates C. Beta blockers Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: A. Symptoms markedly worsen or the patient becomes hypotensive and has syncope B. There is evidence of progressive renal insufficiency or failure C. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic D. Any of the above D. Any of the above Type 1 diabetes results from autoimmune destruction of the beta cells. Eighty-five to 90 percent of Type 1 diabetics have: A. Autoantibodies to two tyrosine phosphatases B. Mutation of the hepatic transcription factor on chromosome 12 C. A defective glucokinase molecule due to a defective gene on chromosome 7p D. Mutation of the insulin promoter factor A. Autoantibodies to two tyrosine phosphatases Type 2 diabetes is a complex disorder involving: A. Absence of insulin production by the beta cells B. A suboptimal response of insulin-sensitive tissues in the liver C. Increased levels of glucagon-like peptide in the post-prandial period D. Too much fat uptake in the intestine B. A suboptimal response of insulin-sensitive tissues in the liver Diagnostic criteria for diabetes include: A. Fasting blood glucose greater than 140 mg/dl on two occasions B. Post-prandial blood glucose greater than 140 mg/dl C. Fasting blood glucose 100 to 125 mg/dl on two occasions D. Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl D. Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl Routine screening of asymptomatic adults for diabetes is appropriate for: A. Individuals who are older than 45 and have a BMI less than 25 kg/m2 B. Native Americans, African Americans, and Hispanics C. Persons with HDL cholesterol greater than 100 mg/dl D. Persons with pre-diabetes confirmed on at least two occasions B. Native Americans, African Americans, and Hispanics Screening criteria for children who meet the following criteria should begin at age 10 and occur every 3 years thereafter: A.BMI above the 85th percentile for age and sex B.Family history of diabetes in first- or second-degree relative D.Any of the above D.Any of the above Insulin is used to treat both types of diabetes. It acts by: A. Increasing beta cell response to low blood glucose levels B. Stimulating hepatic glucose production C. Increasing peripheral glucose uptake by skeletal muscle and fat D. Improving the circulation of free fatty acids C. Increasing peripheral glucose uptake by skeletal muscle and fat Adam has Type 1 diabetes and plays tennis for his university. He exhibits a Knowledge deficit about his insulin and his diagnosis. He should be taught that: A. He should increase his CHO intake during times of exercise B. Each brand of insulin is equal in bioavailability, so buy the least expensive C. Alcohol produces hypoglycemia and can help control his diabetes when taken in small amounts D. If he does not want to learn to give himself injections, he may substitute an oral hypoglycemic to control his diabetes A. He should increase his CHO intake during times of exercise The drug of choice for Type 2 diabetics is metformin. Metformin: A. Decreases glycogenolysis by the liver B. Increases the release of insulin from beta cells C. Increases intestinal uptake of glucose D. Prevents weight gain associated with hyperglycemia A. Decreases glycogenolysis by the liver Before prescribing metformin, the provider should: A. Draw a serum creatinine level to assess renal function B. Try the patient on insulin C. Prescribe a thyroid preparation if the patient needs to lose weight D. All of the above A. Draw a serum creatinine level to assess renal function Sulfonylureas may be added to a treatment regimen for Type 2 diabetics when lifestyle modifications and metformin are insufficient to achieve target glucose levels. Sulfonylureas have been moved to Step 2 therapy because they: A. Increase endogenous insulin secretion B. Have a significant risk for hypoglycemia C. Address the insulin resistance found in Type 2 diabetics D. Improve insulin binding to receptors B. Have a significant risk for hypoglycemia Dipeptidyl peptidase-4 inhibitors (gliptins) act on the incretin system to improve glycemic control. Advantages of these drugs include: A. Better reduction in glucose levels than other classes B. Less weight gain than sulfonylureas C. Low risk for hypoglycemia D. C. Low risk for hypoglycemia Control targets for patients with diabetes include: A. HbA1C between 7 and 8 B. Fasting blood glucose levels between 100 and 120 mg/dl C. Blood pressure less than 130/80 mm Hg D. LDL lipids less than 130 mg/dl C. Blood pressure less than 130/80 mm Hg Establishing glycemic targets is the first step in treatment of both types of diabetes. For Type 1 diabetes: A. Tight control/intensive therapy can be given to adults who are willing to test their blood glucose at least twice daily B. Tight control is acceptable for older adults if they are without complications C. Plasma glucose levels are the same for children as adults D. Conventional therapy has a fasting plasma glucose target between 120 and 150 mg/dl D. Conventional therapy has a fasting plasma glucose target between 120 and 150 mg/dl Treatment with insulin for Type 1 diabetics: A. Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight B. Divides the total doses into three injections based on meal size C. Uses a total daily dose of insulin glargine given once daily with no other insulin required D. Is based on the level of blood glucose A. Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight When the total daily insulin dose is split and given twice daily, which of the following rules may be followed? A. Give two-thirds of the total dose in the morning and one-third in the evening. B. Give 0.3 units per kg of premixed 70/30 insulin with one-third in the morning and two-thirds in the evening. C. Give 50% of an insulin glargine dose in the morning and 50% in the evening. D. Give long-acting insulin in the morning and short-acting insulin at bedtime. A. Give two-thirds of the total dose in the morning and one-third in the evening. Studies have shown that control targets that reduce the HbA1C to less than 7% are associated with fewer long-term complications of diabetes. Patients who should have such a target include: A. Those with long-standing diabetes B. Older adults C. Those with no significant cardiovascular disease D. Young children who are early in their disease C. Those with no significant cardiovascular disease Prevention of conversion from pre-diabetes to diabetes in young children must take highest priority and should focus on: A. Aggressive dietary manipulation to prevent obesity B. Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl to prevent cardiovascular disease C. Maintaining a blood pressure that is less than 80% based on weight and height to prevent hypertension D. All of the above B. Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl to prevent cardiovascular disease The drugs recommended by the American Academy of Pediatrics for use in children with diabetes (depending upon type of diabetes) are: A. Metformin and insulin B. Sulfonylureas and insulin glargine C. Split-mixed dose insulin and GPL-1 agonists D. Biguanides and insulin lispro A. Metformin and insulin Unlike most Type 2 diabetics where obesity is a major issue, older adults with low body weight have higher risks for morbidity and mortality. The most reliable indicator of poor nutritional status in older adults is: A. Weight loss in previously overweight persons B. Involuntary loss of 10% of body weight in less than 6 months C. Decline in lean body mass over a 12-month period D. Increase in central versus peripheral body adiposity B. Involuntary loss of 10% of body weight in less than 6 months The drugs recommended for older adults with Type 2 diabetes include: A. Second generation sulfonylureas B. Metformin C. Pioglitazone D. Third generation sulfonylureas D. Third generation sulfonylureas Ethnic groups differ in their risk for and presentation of diabetes. Hispanics: A. Have a high incidence of obesity, elevated triglycerides, and hypertension B. Do best with drugs that foster weight loss, such as metformin C. Both A and B D. Neither A nor B C. Both A and B The American Heart Association states that people with diabetes have a 2- to 4-fold increase in the risk of dying from cardiovascular disease. Treatments and targets that do not appear to decrease risk for micro- and macro-vascular complications include: A. Glycemic targets between 7% and 7.5% B. Use of insulin in Type 2 diabetics C. Control of hypertension and hyperlipidemia D. Stopping smoking A. Glycemic targets between 7% and 7.5% All diabetic patients with known cardiovascular disease should be treated with: A. Beta blockers to prevent MIs B. ACE inhibitors and aspirin to reduce risk of cardiovascular events C. Sulfonylureas to decrease cardiovascular mortality D. Pioglitazone to decrease atherosclerotic plaque buildup B. ACE inhibitors and aspirin to reduce risk of cardiovascular events All diabetic patients with hyperlipidemia should be treated with: A. HMG-CoA reductase inhibitors B. Fibric acid derivatives C. Nicotinic acid D. Colestipol A. HMG-CoA reductase inhibitors Both ACE inhibitors and some Angiotensin-II receptor blockers have been approved in treating: A. Hypertension in diabetic patients B. Diabetic nephropathy C. Both A and B D. Neither A nor B C. Both A and B Protein restriction helps slow the progression of albuminuria, GFR decline, and ESRD is some patients with diabetes. It is useful for patients who: A. Cannot tolerate ACE inhibitors or ARBs B. Have uncontrolled hypertension C. Have HbA1C levels above 7% D. Show progression of diabetic nephropathy despite optimal glucose and blood pressure control D. Show progression of diabetic nephropathy despite optimal glucose and blood pressure control Diabetic autonomic neuropathy (DAN) is the earliest and most common complication of diabetes. Symptoms associated with DAN include: A. Resting tachycardia, exercise intolerance, and orthostatic hypotension B. Gastroparesis, cold intolerance, and moist skin C. Hyperglycemia, erectile dysfunction, and deficiency of free fatty acids D. Pain, loss of sensation, and muscle weaknes A. Resting tachycardia, exercise intolerance, and orthostatic hypotension Drugs used to treat diabetic peripheral neuropathy include: A. Metoclopramide B. Cholinergic agonists C. Cardioselective beta blockers D. Gabapentin D. Gabapentin The American Diabetic Association has recommended which of the following tests for ongoing management of diabetes? A. Fasting blood glucose B. HbA1C C. Thyroid function tests D. Electrocardiograms B. HbA1C Angina is produced by an imbalance between oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS? A. Calcium channel blockers B. Beta blockers C. ACE inhibitors D. Aspirin Not all chest pain is caused by myocardial ischemia. Non-cardiac causes of chest pain include: A. Pulmonary embolism B. Pneumonia C. Gastroesophageal reflux D. All of the above D. All of the above The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is: A. Class I B. Class II C. Class III D. Class IV B. Class II Patients at high risk for developing significant coronary heart disease are those with: A. LDL values between 100 and 130 B. Systolic blood pressure between 120 and 130 C. Class III angina D. Obesity C. Class III angina To reduce mortality, all patients with angina, regardless of Class, should be on: A. Aspirin 81 to 325 mg/d B. Nitroglycerin sublingually for chest pain C. ACE inhibitors or ARBs D. Digoxin A. Aspirin 81 to 325 mg/d Patients who have angina, regardless of Class, who are also diabetic, should be on: A. Nitrates B. C. Both A and B Beta blockers are especially helpful for patients with exertional angina who also have: A. Arrhythmias B. Hypothyroidism C. Hyperlipidemia D. Atherosclerosis A. Arrhythmias Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use? A. These drugs are useful for immediate symptom relief when the patient is certain it is angina. B. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away. C. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the hospital. D. All of the above C. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the hospital. Isosorbide dinitrate is a long-acting nitrate given BID. The schedule for administration is 7 AM and 2 PM because: A. Long-acting forms have a higher risk for toxicity B. Orthostatic hypotension is a common adverse effect C. It must be taken with milk or food D. Nitrate tolerance can develop D. Nitrate tolerance can develop Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because: A. Nitrates increase MOS and beta blockers increase MOD B. Their additive affects permit lower doses of both drugs and their adverse reactions cancel each other out. C. They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease D. All of the above B. Their additive affects permit lower doses of both drugs and their adverse reactions cancel each other out. Although they are often described as helpful in the lay media, which of the following therapies have not been shown to be helpful based on clinical evidence? A. Vitamins C and E B. Co-enzyme Q10 C. Folic acid D. All of the above D. All of the above Drug choices to treat angina in older adults differ from those of younger adults only in: A.Consideration of risk factors for diseases associated with and increased in aging B.The placement of drug therapy as a treatment choice before lifestyle changes are tried C.The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult D.Those with higher risk for silent myocardial infarction (MI) A. Consideration of risk factors for diseases associated with and increased in aging Which of the following drugs has been associated with increased risk for myocardial infarction (MI) in women? A. Aspirin B. Beta blockers C. Estrogen replacement D. Lipid-lowering agents C. Estrogen replacement Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT: A. Patients often require multiple drugs B. A large number of angina patients are older adults on fixed incomes C. Generic formulations may be cheaper but are rarely bioequivalent D. Lack of drug selectivity may result in increased adverse reactions C. Generic formulations may be cheaper but are rarely bioequivalent Five questions should be asked during the follow up of any angina patient. They include: A. Have there been any changes in lab data since the last visit? B. Has the level of physical activity associated with the angina changed since the last visit? C. Have new risk factors come to light in producing the angina? D. Is the patient filling prescriptions and taking the drugs as prescribed? B. Has the level of physical activity associated with the angina changed since the last visit? Situations that suggest referral to a specialist is appropriate include: A. of choice in treating hypertension in diabetic patients because they: A. Improve insulin sensitivity B. Improve renal hemodynamics Reduce the production of angiotensin II D. All of the above D. All of the above A potentially life-threatening adverse response to ACE inhibitors is angioedema. Which of the following statements is true about this adverse response? A. Swelling of the tongue or hoarseness are the most common symptoms. B. It appears to be related to the decrease in aldosterone production. C. Presence of a dry, hacky cough indicates a high risk for this adverse response. D. Because it takes time to build up a blood level, it occurs after being on the drug for about 1 week. A. Swelling of the tongue or hoarseness are the most common symptoms. ACE inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use? A. Stable angina because it decreases the thickening of vascular walls to decreased MOD. B. Heart failure because it reduces remodeling of injured myocardial tissues. C. Both A and B are true and the reasons are correct D. Both A and B are true but the reasons are wrong E. Neither A nor B are true C. Both A and B are true and the reasons are correct Despite good blood pressure control, a NP might change a patient’s drug from an ACEI to an angiotensin II receptor blocker (ARB) because the ARB: A. Is stronger than the ACEI B. Does not produce a dry, hacky cough C. Has no effect on the renal system D. Reduces sodium and water retention B. Does not produce a dry, hacky cough While taken an ARB, patients need to avoid certain over-the-counter drugs without first consulting the provider because: A. Cimetidine is metabolized by the CYP 3A4 isoenzymes B. Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels C. Both A and B D. Neither A nor B C. Both A and B Laboratory monitoring for patients on ACEIs or ARBs should include: A. White blood cells counts with the drug dose increased for elevations above 10,000 B. Liver function tests with the drug dose stopped for ALT values 2× normal C. Serum creatinine levels with the drug dose reduced for values above 2.5 mg/dL D. Serum glucose levels with the drug dose increased for levels above 120 mg/dL C. Serum creatinine levels with the drug dose reduced for values above 2.5 mg/dL Jacob has hypertension for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it: A. Decreases the amount of calcium inside the cell B. Reduces stroke volume C. Increases the activity of the Na+/K+/ATPase pump indirectly D. Decreases heart rate A. Decreases the amount of calcium inside the cell Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker? A. Bradycardia B. Hlt D. Withheld if she experiences gastroesophageal reflux A. Started at about half the usual dose Larry has heart failure which is being treated with digoxin because it exhibits: A. Negative inotropism B. Positive chronotropism C. Both A and B D. Neither A nor B D. Neither A nor B Which of the following create higher risk for digoxin toxicity? Both the cause and the reason for it must be correct. A. needed in adjusting a dose C. After three half-lives from the starting of the drug D. When a patient has stable renal function B. Because a reference point is needed in adjusting a dose Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: A. Widening of the area of infarction B. Onset of congestive heart failure C. An electrolyte imbalance involving potassium D. Renal dysfunction B. Onset of congestive heart failure Which of the following is true about procainamide and its dosing schedule? A. It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. B. Gastrointestinal adverse effects are common so the drug should be taken with food. C. A Take a hot shower or bath if you feel dizzy The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response? A. “Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism.” B. “Amiodarone damages the thyroid gland and can result in inflammation of that gland causing hyperthyroidism.” C. “Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given.” D. “Amiodarone can cause corneal deposits in up to 25% of patients.” A. “Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism.” Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 AM and 2 PM because: A. It ing. Let’s work on having you stop smoking.” D. “This is not related to your medication. Are you under a lot of stress?” B. “Headaches are common side effects with these drugs. How severe are they?” In teaching about the use of sublingual nitroglycerine, the patient should be instructed: A. To swallow the tablet with a full glass of water B. To place one tablet under the tongue if chest pain occurs and allow it to dissolve C. To take one tablet every 5 minutes until the chest pain goes away D. That it should “burn” when placed under the tongue or it is no longer effective B. To place one tablet under the tongue if chest pain occurs and allow it to dissolve Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: A. B B. Twice daily in the morning and the evening C. With each meal and at bedtime D. In the morning before eating A. In the evening in a single daily dose Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following labs should be monitored? A. Ser Which of the following statements is true? A. Niacin is a B-complex vitamin and taking double the dose of the over-the-counter vitamin will lower LDL and save money. B. Niacin has been shown to reduce all-cause mortality for patients with CAD if taken in prescription strength. C. Niacin should be given on an empty stomach to avoid GI irritation. D. All of the above B. Niacin has been shown to reduce all-cause mortality for patients with CAD if taken in prescription strength. Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? A. Reactive airway disease/asthma B. Inflammatory bowel disease C. Allergy to aspirin D. Gallbladder disease D. Gallbladder disease Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct. A. Reductase inhibitors, due to an increased risk for rhabdomyolysis B. Bile-acid sequestering resins, due to interference with folic acid absorption C. Grapefruit juice, due to interference with metabolism D. Niacin, due to decreased gemfibrozil activity A. Reductase inhibitors, due to an increased risk for rhabdomyolysis Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug: A. Blocks synthesis of cholesterol in the liver B. Exchanges chloride ions for negatively charged acids in the bowel C. Increases HDL levels the most among the classes D. Blocks the lipoprotein lipase pathway B. Exchanges chloride ions for negatively charged acids in the bowel Because of their site of action, bile acid sequestering resins: A. Should be administered separated from other drugs by at least 4 hours B. May increase the risk for bleeding C. Both A and B D. Neither A nor B A. Should be administered separated from other drugs by at least 4 hours what can loss of smell be related to? nasal discharge, head trauma, smoking, aging, cocaine what is cranial nerve II (and is it sensory or motor)? optic, sensory what CN conveys visual information from the retina II, optic nerve how do you test the optic nerve (CNII)? snellen chart, rosenbaum chart/Jaeger near vision chart, peripheral vision which cranial nerves are responsible for extra ocular movements of the eye? III, IV, VI (occulomotor, trochlear, abducens) CN responsible for controlling direct and consensual response to light and accommodation, pupillary constriction, change in lens shape based on stimuli Oculomotor III what is the motor function of CNV (trigeminal) innervates temporal and masseter muscles, clenching jaw What is the sensory function of CNV (trigeminal) pain sensation (sharp dull, light touch) corneal pain sensation how do you assess sensory aspect of CN V? cotton wisp to test corneal reflex face sensation: eyes closed, touch scalp, cheek and chin with sharp/dull how do you test motor function of CN 7? (and which nerve is it) facial nerve. ask patient to raise eyebrows, squeeze eyes shut, wrinkle forehead, smile, show teeth which CN is responsible for taste on the anterior portion of the tongue CN 7 (facial nerve) which CN is responsible for secretion of salvia and tears? CN 7, facial CN VIII (acoustic) how is cranial nerve VIII (acoustic) assessed? whisper test which way will the tongue deviate in a unilateral lesion? towards the side of weakness (our notes say away but every resource I've seen online say towards? not sure...) [Show More]
Last updated: 2 years ago
Preview 1 out of 234 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 01, 2020
Number of pages
234
Written in
Additional information
This document has been written for:
Uploaded
Sep 01, 2020
Downloads
1
Views
120

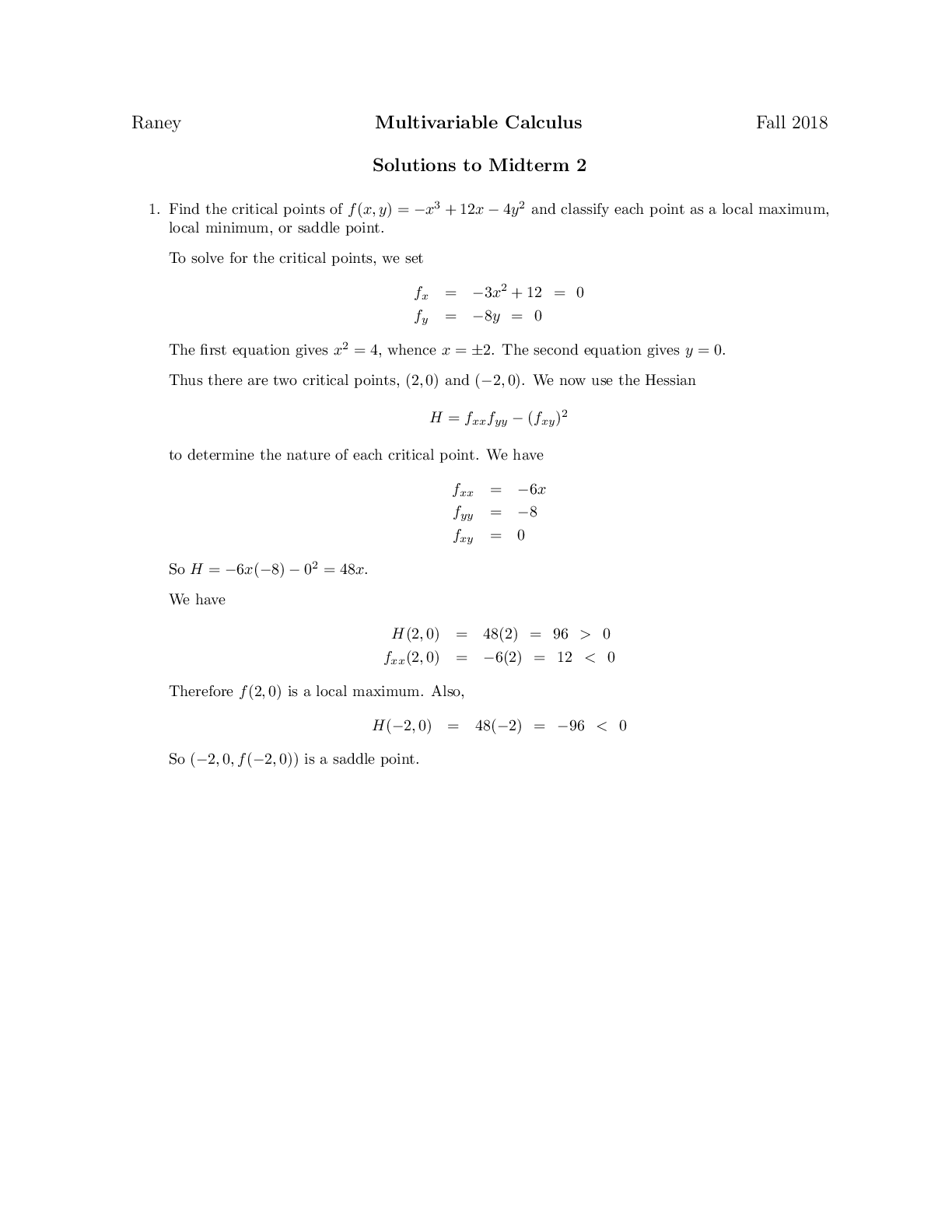


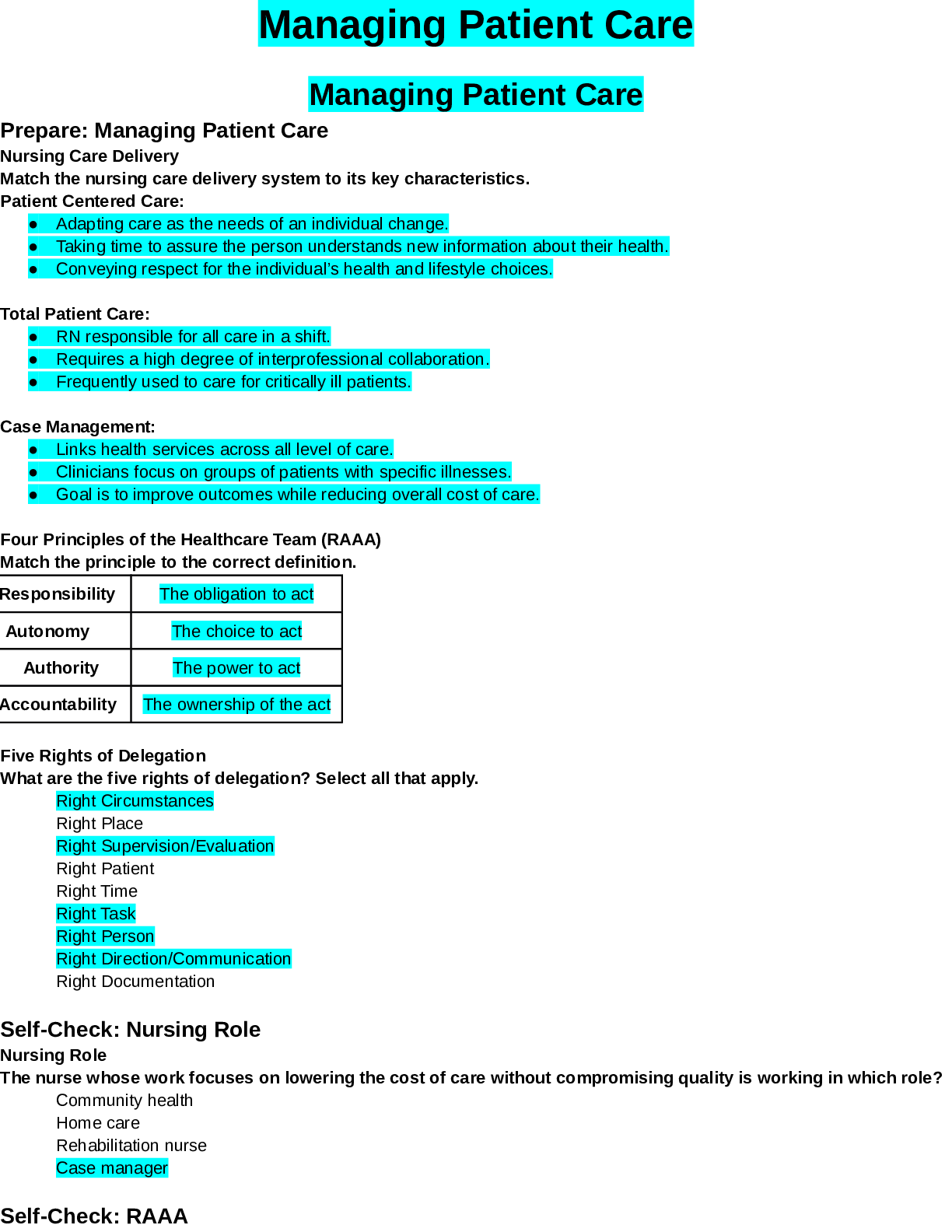



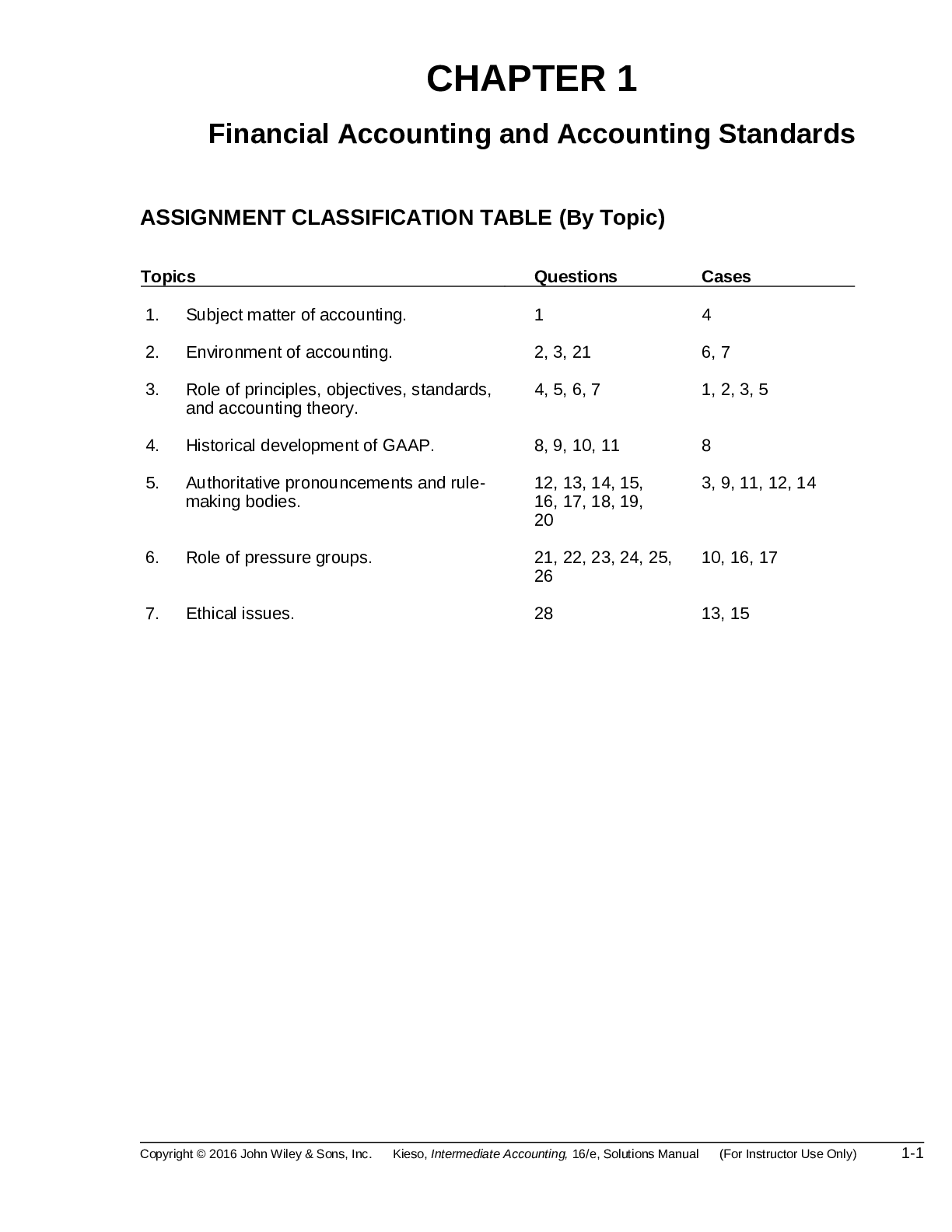
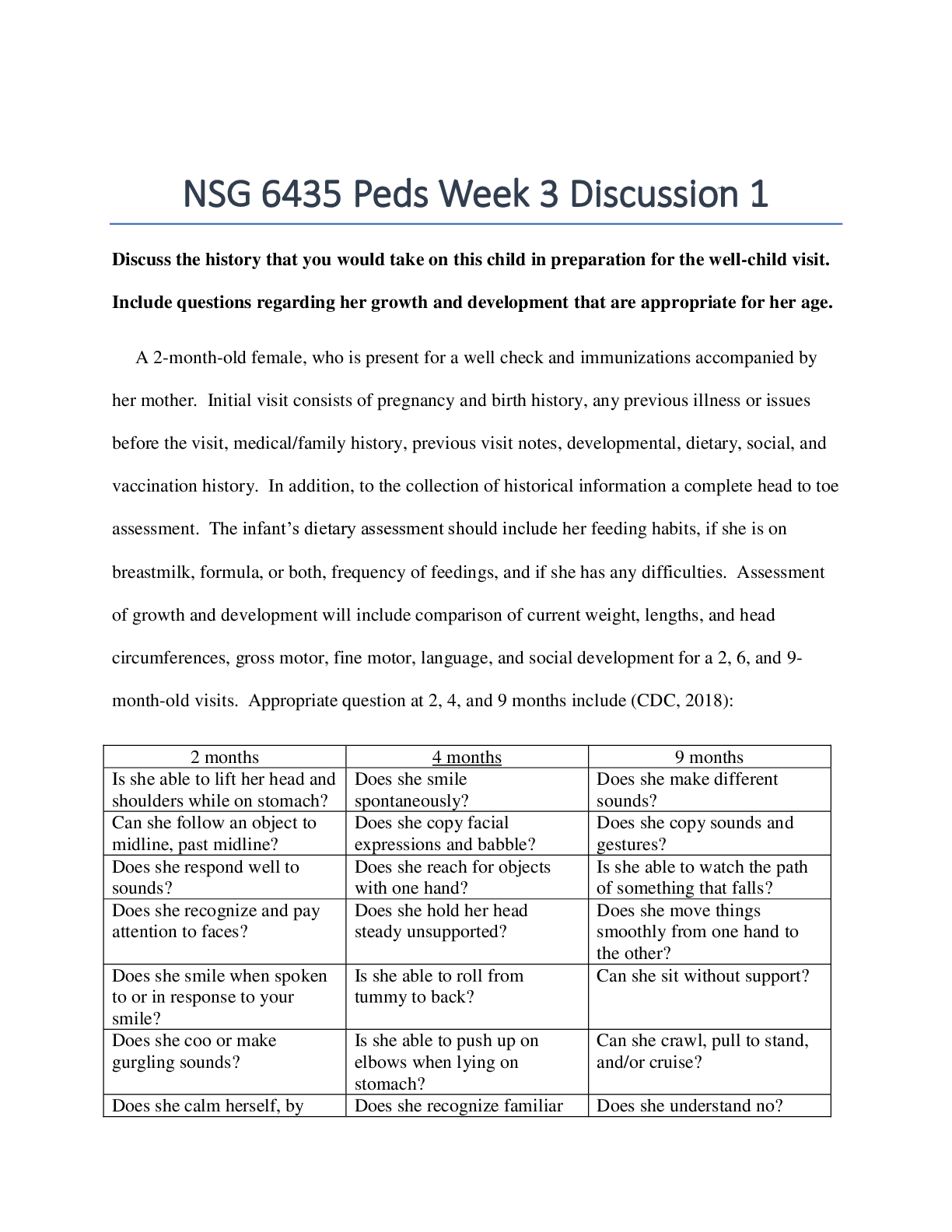
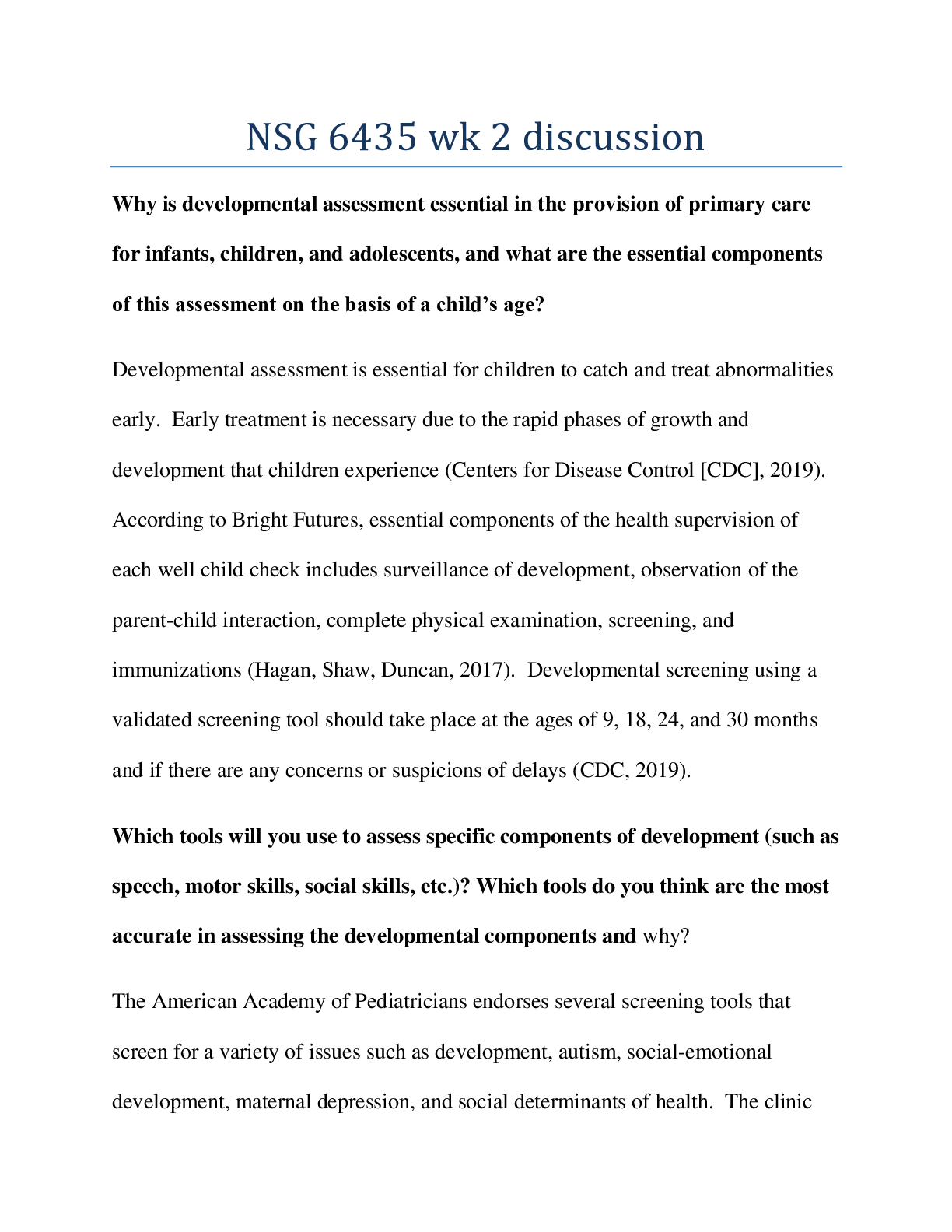
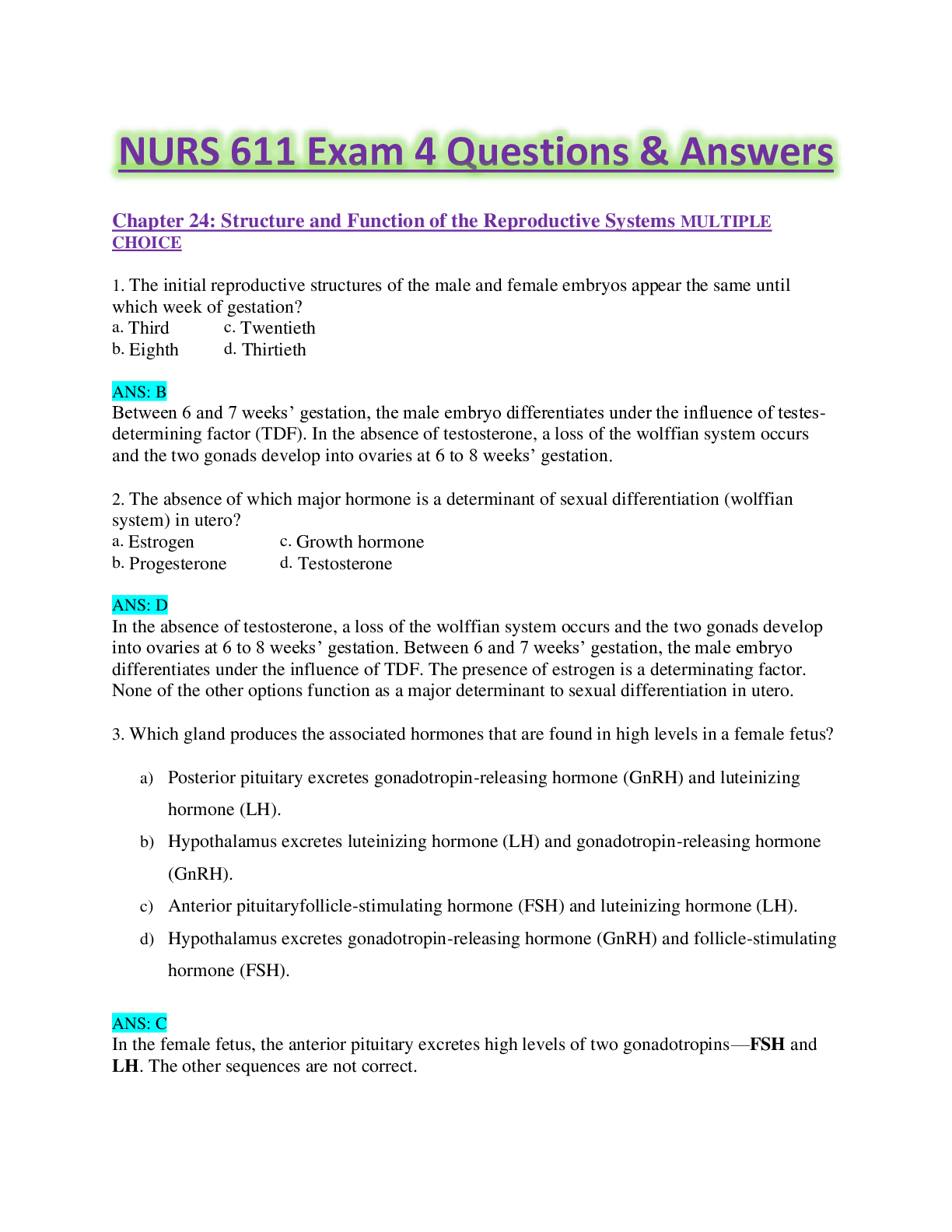
.png)