*NURSING > QUESTIONS & ANSWERS > NURS 611 Exam 4 Questions & Answers (test-bank) Latest 2019/20 verified guide, Answers explained - M (All)
NURS 611 Exam 4 Questions & Answers (test-bank) Latest 2019/20 verified guide, Answers explained - Maryville University Of St. Louis.
Document Content and Description Below
NURS 611 Exam 4 Questions & Answers Chapter 24: Structure and Function of the Reproductive Systems MULTIPLE CHOICE 1. The initial reproductive structures of the male and female embryos appear the ... same until which week of gestation? a. Third c. Twentieth b. Eighth d. Thirtieth 2. The absence of which major hormone is a determinant of sexual differentiation (wolffian system) in utero? a. Estrogen c. Growth hormone b. Progesterone d. Testosterone 3. Which gland produces the associated hormones that are found in high levels in a female fetus? a) Posterior pituitary excretes gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH). b) Hypothalamus excretes luteinizing hormone (LH) and gonadotropin-releasing hormone (GnRH). c) Anterior pituitaryfollicle-stimulating hormone (FSH) and luteinizing hormone (LH). d) Hypothalamus excretes gonadotropin-releasing hormone (GnRH) and follicle-stimulating hormone (FSH). 4. Which hormone is linked to an increase in appetite during puberty? a. Inhibin c. Activin b. Leptin d. Follistatin 5. The Skene glands are located on either side of which structure? a. Introitus c. Clitoris b. Urinary meatus d. Vestibule 6. What is the function of the mucus secreted by the Bartholin glands? a) Enhancement of the motility of sperm b) Lubrication of the urinary meatus and vestibule c) Maintenance of an acid-base balance to discourage proliferation of pathogenic bacteria d) Enhancement of the size of the penis during intercourse 7. Which change is a result of puberty and defends the vagina from infection? a) The pH stabilizes between 7 and 8. b) A thin squamous epithelial lining develops. c) V aginal pH becomes more acidic. d) Estrogen levels are low. 8. What happens to the vagina’s lining at puberty? a) It becomes thinner. c. It assumes a neutral pH. b) It becomes thicker. d. It undergoes atrophy. 9. Which structure is lined with columnar epithelial cells? a. Perimetrium c. Myometrium b. Endocervical canal d. Vagina 10. Where is the usual site of fertilization of an ovum? a) Trumpet end of the fallopian tubes c. Ampulla of the fallopian tubes b) Fimbriae of the fallopian tubes d. Os of the fallopian tubes 11. Where is the usual site of cervical dysplasia or cancer in situ? a) Squamous epithelium of the cervix meets the cuboidal epithelium of the vagina. b) Columnar epithelium of the cervix meets the squamous epithelium of the uterus. c) Squamous epithelium of the cervix meets the columnar epithelium of the uterus. d) Columnar epithelium of the cervix meets the squamous epithelium of the vagina. 12. Having ejected a mature ovum, the ovarian follicle develops into a(n): a) Atretic follicle c. Corpus luteum b) Thecal follicle d. Functional scar 13. The mucosal secretions of the cervix secrete which immunoglobulin? a. IgA c. IgG b. IgE d. IgM 14. The equivalent to the female gonad is the male: a) Epididymis c. Vas deferens b) Spermatic cord d. Testes 15. A surge of which hormone causes the corpus luteum to produce progesterone? a) Follicle stimulating hormone c. Gonadotropin-releasing hormone b) Luteinizing hormone d. Estrogen 16. What directly causes ovulation during the menstrual cycle? a) Gradual decrease in estrogen levels c. Sharp rise in progesterone levels b) Sudden increase of LH d. Gradual increase in estrogen levels 17. Which anatomic structure secretes follicle stimulating hormone (FSH) and luteinizing hormone (LH)? a) Hypothalamus c. Anterior pituitary b) Ovaries d. Adrenal cortex 18. During the time that ovulation occurs, which statement concerning basal body temperature (BBT) is true? a) BBT increases. b) BBT decreases. c) BBT fluctuates around 37° C (98° F). d) BBT rises consistently above 37.8° C (100° F). 19. What structure in the male lies posterior to the urinary bladder? a) Seminal vesicles c. Cowper glands b) Prostate glands d. Parabladder glands 20. When do penile erections begin? a) Before birth b) Shortly after birth c) Shortly before puberty d) After puberty 21. Which statement is true regarding the major difference between male and female sex hormone production? a) Luteinizing hormone has no apparent action in a man. b) In a man, sex hormone production is relatively constant. c) Estradiol is not produced in a man. d) In a man, gonadotropin-releasing hormone does not cause the release of follicle stimulating hormone. 22. Where in the male body does spermatogenesis occur? a) Epididymis c. Seminiferous tubules b) Rete testes d. Vas deferens 23. Which immunoglobulin is contained in breast milk? a. IgA c. IgG b. IgE d. IgM 24. Which hormone promotes the development of the lobular ducts in the breasts? A.Progesterone c. Oxytocin b. Prolactin d. Estrogen 25. What causes the vasomotor flushes (hot flashes) that are associated with declining ovarian function with age? a) Decreased estrogen levels c. Increased estrogen levels b) Absence of estrogen d. Rapid changes in estrogen levels 26. When does the male body begin to produce sperm? a) Before birth c. At puberty b) Shortly after birth d. When erection is possible 27. The human zygote has a total of how many chromosomes? a. 23 c. 46 b. 25 d. 50 28. Which hormone promotes the development of testosterone in both males and females? a. Progesterone c. Oxytocin b. Prolactin d. Estrogen 29. Which hormone stimulates gonads to produce both male and female hormones? a) Gonadotropin-releasing hormone (GnRH) b) Follicle-stimulating hormone (FSH) c) Luteinizing hormone (LH) d) Estrogen 30. Which hormone relaxes the myometrium and prevents lactation until the fetus is born? a) Gonadotropin-releasing hormone (GnRH) b) Follicle-stimulating hormone (FSH) c) Progesterone d) Estrogen 31. A Sims-Huhner test is of particular interest to a patient experiencing which condition? a) Infertility c. Venereal disease b) Possible HIV infection d. Perimenopause MULTIPLE RESPONSE 32. Estrogen has many biological effects on the female body including: (Select all that apply.) a) Maturation of reproductive organs b) Differentiating female physical characteristics c) Postpuberty closure of short bones d) Regulation of the menstrual cycle e) Endometrial regeneration after menstruation 33. Which statements about the human papillolmavirus (HPV) and vaccine are true? (Select all that apply.) a) Currently, two HPV vaccines have been approved for use in the United States. b) HPV is believed to be responsible for the majority of the diagnosed cases of cervical cancer. c) A form of the vaccine has been approved for use in males to prevent genital warts. d) The administration of the vaccine is a one-dose intramuscular injection. e) The recommended age for vaccination of girls is between 11 and 12 years of age. 34. Which statements are true regarding the female menstrual cycle? (Select all that apply.) a) Initial cycles may dramatically vary in length. b) By adulthood, the commonly accepted cycle average is 28 (27 to 30) days. c) The length of a cycle varies among women. d) Up to 8 years before menopause, the intervals of the menstrual cycle begin to lengthen. e) Menopause is achieved when a woman is without a period for 2 years. 35. Testosterone is believed to have a role in: (Select all that apply.) a) Male-patterned baldness b) Libido levels c) Acne development d) Altered cholesterol metabolism 36. What are normal characteristics of aging of the male reproductive system? (Select all that apply.) a) Reduced sperm count b) Slower, less forceful ejaculations c) Testicular atrophy and softening d) Longer time to achieve full erection e) Decreased levels of testosterone Chapter 25: Alterations of the Female Reproductive System MULTIPLE CHOICE 1. In 95% of children of delayed puberty, the problem is caused by: a) Disruption in the hypothalamus c. Deficit in estrogen or testosterone b) Disruption of the pituitary d. Physiologic hormonal delays 2. What is the first sign of puberty in girls? a) Breast enlargement c. Menstruation b) Growth of pubic hair d. Vaginal discharge 3. Which type of precocious puberty causes the child to develop some secondary sex characteristics of the opposite sex? a. Mixed c. Isosexual b. Incomplete d. Homosexual 4. The release of which chemical mediator causes primary dysmenorrhea? a. Leukotrienes c. Bradykinin b. Prostaglandins d. C-reactive protein 5. Considering the pathophysiologic characteristics of primary amenorrhea, what anatomic structure is involved in compartment II? a. Ovary c. Hypothalamus b. Anterior pituitary d. Vagina 6. Considering the pathophysiologic characteristics of primary amenorrhea, what anatomic structure is involved in compartment IV? a) V agina c. Ovary b) Hypothalamus d. Anterior pituitary 7. Which condition is considered a clinical cause of amenorrhea? a) Disorder in the endometrium c. Lack of physical exercise b) Obstruction of the fallopian tubes d. Failure to ovulate 8. Clinical manifestations that include irregular or heavy bleeding, the passage of large clots, and the depletion of iron stores support which diagnosis? a) Premenstrual syndrome c. Polycystic ovary syndrome b) Dysfunctional uterine bleeding d. Primary dysmenorrhea 9. What statement concerning the pathogenetic mechanisms of polycystic ovarian syndrome (POS) is true? a) POS causes a decrease in leptin levels; this decrease reduces the hypothalamic pulsatility of gonadotropin-releasing hormone, which reduces the number of follicles that mature. b) POS is a result of a disorder in the anterior pituitary that increases the follicle-stimulating hormone, which reduces the luteinizing hormone released. c) POS is a result of a combination of conditions that include oligo-ovulation or anovulation, elevated levels of androgens, or clinical signs of hyperandrogenism and polycystic ovaries. d) POS inhibits testosterone, which stimulates androgen secretion by the ovarian stroma and indirectly reduces sex hormone–binding globulin. 10. What is the leading cause of infertility in women? a) Pelvic inflammatory disease c. Salpingitis b) Endometriosis d. Polycystic ovary syndrome 11. Considering the mediating factors of premenstrual syndrome (PMS), which medication may be used either continually or only during the menstrual period as a treatment for the condition? a. NSAIDs c. SSRIs b. Estrogen d. Progesterone 12. Which statement regarding pelvic inflammatory disease (PID) is true? a) An episode of mild PID can decrease the possibility of a successful pregnancy by 80%. b) Such an inflammation results in temporary changes to the ciliated epithelium of the fallopian tubes. c) PID has not been associated with an increased risk of an ectopic pregnancy. d) Contracting this infection increases the risk of uterine cancer. 13. When a woman’s uterus is assessed as protruding through the entrance of the vagina to the hymen, which grade of prolapse does this indicate? a. 0 c. 2 b. 1 d. 3 14. Which term is used to identify the descent of the posterior bladder and trigone into the vaginal canal? a. Rectocele c. Cystocele b. V aginocele d. Enterocele 15. What type of cyst develops when an ovarian follicle is stimulated but no dominant follicle develops and completes the maturity process? a. Follicular c. Corpus albicans b. Corpus luteal d. Benign ovarian 16. Which term is used to identify benign uterine tumors that develop from smooth muscle cells in the myometrium and are commonly called uterine fibroids? a) Endometrial polyps c. Leiomyomas b) Myometrial polyps d. Myometriomas 17. What theory is used to describe the cause of endometriosis? a) Obstruction within the fallopian tubes prevents the endometrial tissue from adhering to the lining of the uterus. b) Endometrial tissue passes through the fallopian tubes and into the peritoneal cavity and remains responsive to hormones. c) Inflammation of the endometrial tissue develops after recurrent sexually transmitted diseases. d) Endometrial tissue lies dormant in the uterus until the ovaries produce sufficient hormone to stimulate its growth. 18. Which virus is a precursor for developing cervical intraepithelial neoplasia (CIN) and cervical cancer? a) Human papillomavirus (HPV) c. Herpes simplex II virus (HSV) b) Epstein-Barr virus (EBV) d. Cytomegalovirus (CMV) 19. Which description is used when a progressive neoplastic change involves the full epithelial thickness of the cervix? a) Cervical intraepithelial neoplasia c. Cervical carcinoma in situ b) Cervical dysplasia d. Invasive carcinoma of the cervix 20. Which factor increases the risk for ovarian cancer after the age of 40 years? a) Use of fertility drugs c. Multiple pregnancies b) Oral contraceptive use d. Prolonged lactation 21. Infertility is defined as the inability to conceive after how many months of unprotected intercourse with the same partner? a. 6 c. 18 b. 12 d. 24 22. Which of the following is not considered a cause of galactorrhea? a) Proliferation of the lactiferous ducts of the breast b) Hypothyroidism, resulting from a decrease in thyroid-releasing hormone c) Excess prolactin secretion from the pituitary d) Drugs such as high-dose oral contraceptives and phenothiazines 23. Fluid-filled squishy sacs characterize which breast disorder? a) Paget disease c. Nonproliferative breast lesions b) Cysts d. Lobular carcinoma in situ 24. What are typical findings on breast palpation of a woman diagnosed with simple fibroadenoma? a) Painful, round, movable, and fluid-filled mass b) Painless, movable, hard, and irregular mass c) Smooth, solid, mobile, and well-circumscribed mass d) Smooth, nonmovable, irregular, and soft mass 25. Which benign breast tumor affects postmenopausal women and is characterized by the principal lactiferous ducts becoming dilated and filled with cellular debris? a) Mammary duct ectasia c. Phyllodes tumor b) Intraductal papilloma d. Fibroadenoma 26. The majority of the small percentage of ovarian cancers that are associated with a known pattern of inheritance are associated with: a) Susceptibility of the BRCA1 gene b) Mutations of the BRCA2 gene c) Hereditary nonpolyposis colorectal cancer (HNPCC) syndrome d) Low progesterone levels 27. What is usually the first clinical manifestation of breast cancer? a) Nipple dimpling c. Enlargement of one breast b) Nipple discharge d. Painless lump MULTIPLE RESPONSE 28. What is a recognized treatment for the symptoms often associated with pelvic organ prolapse? (Select all that apply.) a) Pessary b) Kegel exercises c) Estrogen therapy d) Surgical repair e) Bearing down exercises 29. Dysfunctional uterine bleeding (DUB), secondary to ovarian dysfunction, is abnormal uterine bleeding resulting from: (Select all that apply.) a) Endometriosis b) Progesterone deficiency c) Sexually transmitted infections d) Congenital abnormalities in the uterine structure e) Estrogen excess 30. The size of benign uterine tumors, such as leiomyomas, is thought to be caused by the influence of which hormone? (Select all that apply.) a) Progesterone b) Estrogen c) Luteinizing hormone d) Gonadotropin-stimulating hormone e) Growth factors 31. What are the common clinical manifestations of endometriosis? (Select all that apply.) a) Back and flank pain b) Infertility c) Dysuria d) Amenorrhea e) Dysmenorrhea Chapter 26: Alterations of the Male Reproductive System MULTIPLE CHOICEf 1. In the 95% of those with delayed puberty, the problem is caused by which condition? a. Disruption in the hypothalamus c. Deficit in estrogen or testosterone b. Disruption of the pituitary d. Physiologic hormonal delays 2. What is the first sign of puberty in boys? a. Thickening of the scrotal skin c. Enlargement of the testes b. Growth of pubic hair d. Change in voice 3. Which type of precocious puberty causes the child to develop some secondary sex characteristics of the opposite sex? a. Mixed c. Isosexual b. Incomplete d. Homosexual 4. What term is used to identify a condition in which the foreskin cannot be retracted over the glans penis? a. Paraphimosis c. Prephimosis b. Priapism d. Phimosis 5. What term is used to identify a fibrotic condition that causes lateral curvature of the penis during erection, which is associated with a local vasculitis-like inflammatory reaction and decreased tissue oxygenation? a. Phimosis c. Lateral paraphimosis b. Lateral phimosis d. Peyronie disease 6. What term is used to identify an inflammation of the glans penis? a. Glanitis c. Priapism b. Balanitis d. Hydrocelitis 7. Cryptorchidism can be defined as which of the following? a. Normal developmental state of the testes b. Abnormal state in which the testes are overdeveloped c. Lack of scrotum d. Testicular maldescent 8. What is the most common infectious cause of orchitis and one that usually affects postpubertal boys? a. Herpes c. Mumps b. Escherichia coli d. Cytomegalovirus 9. The risk of which cancer is greater if the man has a history of cryptorchidism? a. Penile c. Prostate b. Testicular d. Epididymal 10. What are the clinical manifestations of testicular cancer? a. Firm, nontender testicular mass c. Painful fluid-filled testicular mass b. Painful, mobile, firm testicular mass d. Soft, nontender testicular mass 11. How does the epididymis become infected? a. The pathogenic microorganisms ascend the vasa deferentia from an already infected urethra or bladder. b. The pathogenic microorganisms are attached to sperm that travel through the genital tract. c. The pathogenic microorganisms from the tunica vaginalis are transported to the epididymis. d. The pathogenic microorganisms from the prostate fluid ascend to the epididymis. 12. Symptoms of benign prostatic hyperplasia (BPH) are a result of which pathophysiologic condition? a. Infection of the prostate c. Ischemia of the urethra b. Obstruction of the urethra d. Compression of the urethra 13. Which infection has clinical manifestations that include the sudden onset of malaise, low back pain, and perineal pain with high fever and chills, dysuria, nocturia, and urinary retention? a. Orchitis c. Epididymitis b. Balanitis d. Bacterial prostatitis 14. Priapism has been associated with the abuse of what substance? a. Marijuana c. Cocaine b. Alcohol d. Heroin 15. Which age group should be targeted for testicular cancer education and screening? a. 15 to 35 year olds c. 30 to 55 year olds b. 20 to 45 year olds d. 45 to 70 year olds 16. What is the reason breast cancer in men has such a poor prognosis? a. Breast cancer is extremely aggressive in men. b. Treatment is usually delayed as a result of late detection. c. Chemotherapies are not as effective in men. d. Breast tumors tend to be small and hard to isolate. MULTIPLE RESPONSE 17. Which are clinical manifestations of male breast cancer? (Select all that apply.) a. Ulceration present on the breast b. Retraction of breast tissue c. Nipple discharge d. Palpable mass midline of the nipple e. Unilateral solid mass 18. Which statements are true regarding urethritis? (Select all that apply.) a. A purulent drainage may be present. b. A clear mucus-like discharge may be present. c. Symptoms include urethral tingling and itching or burning on urination. d. A 24-hour urine test is required to diagnose the disorder. e. Treatment includes appropriate antibiotic therapy. 19. Which statements are true regarding prostate cancer? (Select all that apply.) a. It ranks second to lung cancer as being most common among American men. b. A familial history of prostate cancer is a risk factor. c. Dietary habits seem to play a role in its development. d. African-American men have an increased risk for its development. e. Being over 65 years of age increases the risk for developing prostate cancer. MATCHING Match the description with the disorder. A. Painless diverticulum of the epididymis located between the head of the epididymis and the testis- Spermatocele- A spermatocele is a painless diverticulum of the epididymis located between the head of the epididymis and the testis. B. Collection of fluid in the tunica vaginalis- Hydrocele- A hydrocele is a collection of fluid within the tunica vaginalis C. Rotation of a testis, which twists blood vessels of the spermatic cord- Testicular torsion- Torsion of the testis is rotation of a testis, which twists blood vessels in the spermatic cord. D. Abnormal dilation of the vein within the spermatic cord- Varicocele- A varicocele is an abnormal dilation of a vein within the spermatic cord and is classically described as a bag of worms Chapter 27: HIV Infection, Hepatitis, Tuberculosis, and Sexually Transmitted Diseases Test Bank MULTIPLE CHOICE 1. Which of the following sexually transmitted diseases can be prevented through immunization? a. Chlamydia b. Gonorrhea c. Hepatitis B d. Herpes 2. Which of the following provides the best explanation as to why people do not immediately seek medical treatment when they first become ill with HIV? a. They are afraid to get tested for fear results will be positive. b. They avoid the problem (maybe it will go away). c. They don’t recognize their symptoms as possibly being due to HIV. d. It is too expensive to get an HIV test. 3. A client was clearly very relieved when an HIV test came back negative. “Thank goodness. I’ve had sex several times without a condom, and when one of my friends said he was sick, I think I panicked.” Which of the following would be most important to emphasize to the client immediately? a. Abstinence is the only way to be certain you are HIV-free. b. Sex should be restricted to one partner. c. The test could be wrong and the client might still have an HIV infection. d. The test would not cover any recent infection, so if the client has had recent unprotected sex, the test should be repeated in 3 months. 4. A student asks the nurse at the student health clinic how AIDS is diagnosed. Which of the following statements would be the best response by the nurse? a. “A diagnosis of AIDS is made when a screening test called an enzyme-linked immunosorbent assay (ELISA) is confirmed by the Western blot test.” b. “A diagnosis of AIDS is made when antibodies to HIV are detected about 6 weeks to 3 months following possible exposure.” c. “A diagnosis of AIDS is made when antibodies to HIV reach peak levels of 1000/ml of blood.” d. “A diagnosis of AIDS is made when CD4 T lymphocytes drop to less than 200/ml.” 5. The correctional health nurse is doing a quick assessment on a newly admitted inmate who is HIV positive. Which of the following diseases should the inmate receive screening for immediately? a. Herpes zoster b. Hepatitis B c. Hepatitis C d. Tuberculosis 6. A school nurse asks a class about the ways HIV can be transmitted. Which of the following comments by a student indicates a need for additional teaching? a. “I wouldn’t sit next to someone with HIV.” b. “Having unprotected sex with someone who is infected spreads HIV.” c. “Sharing needles when shooting up drugs spreads HIV.” d. “Transfusions of blood products that are contaminated can spread HIV.” 7. In the United States, which demographic group has the highest risk for HIV infection? a. African-American homosexual men b. Hispanic IV drug abusers c. White homosexual men d. White lesbians 8. Which of the following best explains why some health clinics allow clients to be tested for HIV anonymously with no record of the client’s name, address, or contact information? a. Client doesn’t actually ever have to be told the results of the test. b. Client may be engaged in illegal activities (drug use). c. Client plans on not paying for the test and collection agencies will not be able to harass them. d. Client wants to be sure care providers don’t share results with their family. 9. A nurse is providing education to a client about the use of PrEP. Which of the following statements would the nurse include as part of this teaching? a. ”Side effects of PrEP include extreme lethargy and joint pain.” b. ”PrEP has been shown to be effective in preventing transmission of the disease from sharing needles.” c. ”The effectiveness of PrEP will depend on your adherence to the medication regimen.” d. ”PrEP will prevent you from contracting HIV and Hepatitis B.” 10. A male client visits the clinic office complaining of a yellow, green discharge from his penis. Which of the following STDs has the client most likely contracted? a. Gonorrhea b. Syphilis c. Herpes simplex virus 2 d. Human papillomavirus 11. A client is being treated for secondary syphilis. Which of the following signs and symptoms would the nurse anticipate the client would exhibit? a. Chancre at the site of entry b. Jaundice c. Difficulty coordinating muscle movements d. Skin rash without itching 12. Which of the following best explains why chlamydia is a major focus of public health efforts? a. It has more serious long-term outcomes than other STDs b. It can cause problems in infants born to infected mothers c. It is not frequently seen in the United States d. It is so difficult and expensive to treat 13. Which of the following statements best explains why HSV-2 infection is more challenging for a client than gonorrhea infection? a. HSV-2 is a viral infection that is both chronic and incurable. b. HSV-2 is extremely expensive to treat. c. HSV-2, like HIV, is almost impossible to diagnosis in the early stages. d. Once a person has been treated for HSV-2, the person is immune to further outbreaks. 14. When a nurse discovers that a woman has been treated for cervical cancer, the nurse asks the woman whether she has ever been tested for HIV or other STDs. The woman is offended and asks why the nurse would ask her such a thing. Which of the following statements would be the best response from the nurse? a. “Cervical cancer treatments may decrease immunity, so that it is easier to acquire STDs.” b. “Cervical cancer usually is caused by HPV, and often the presence of one STD is accompanied by other STDs.” c. “The presence of an STD in women with cervical cancer may lead to congenital defects in offspring.” d. “The presence of an STD in a woman with a history of cervical cancer has been associated with a relapse of the cancer after treatment.” 15. Which of the following best describes the characteristic appearance of lesions of human papillomavirus (HPV)? a. Solitary growth with elevated borders and a central depression b. Elevated growths with a “cauliflower” appearance c. Thin-walled pustules that rupture to form honey-colored crusts d. Vesicles that ulcerate and crust within 1 to 4 days 16. A client who is very upset says to the nurse, “But we always used a condom! How could I have genital warts?” Which of the following would be the best response by the nurse? a. “Are you positive you always used a condom?” b. “Condoms don’t always work.” c. “The condom might have had a tear in the latex.” d. “Skin to skin contact to a wart may have occurred outside the area that the condom covers.” 17. Which of the following statements best explains why many health care providers are more afraid of getting hepatitis B than HIV? a. Everyone would assume the person infected with hepatitis B is a drug user. b. Having HBV would mean no further employment in health care. c. The fatality rate is higher and occurs sooner with HBV. d. There is no treatment for HBV, which can be a very serious illness. 18. A nurse explained to a new mother that because she had tested positive for the hepatitis B virus, her newborn son would need the hepatitis B vaccine immediately and then also an immune globulin injection. “Wait,” said the new mother. “Why is my son getting two shots?” Which of the following statements would be the best response by the nurse? a. “One injection protects your son, while the other encourages his body to build up immunity.” b. “One shot keeps your son from getting sick, while the other is a typical vaccine to prevent you from accidentally infecting him.” c. “Since you’ve already been infected with the virus, your son needs twice as much protection.” d. “The second shot is just to make sure the first one works.” 19. A client with tuberculosis (TB) asks why the nurse is required to watch the client swallow the medication each day. Which of the following statements is the best response by the nurse? a. “Clients with TB are often noncompliant, so if I directly observe, you will be sure to take the drugs that have been ordered.” b. “This therapy is recommended to make sure that you receive the treatment you need and the infection doesn't become resistant to the drugs.” c. “This is to make sure you take your medication if your condition becomes so advanced that you do not have enough cerebral oxygenation to remember.” d. “Tuberculosis medications are very expensive so this method ensures that government money doesn't get wasted on those who will not take the drugs.” 20. A nurse is concerned about the prevalence of tuberculosis among migrant farmworkers. Which of the following activities would be best to use when implementing tertiary prevention? a. Administer purified protein derivative (PPD) to contacts of those with tuberculosis. b. Initiate directly observed therapy (DOT) for tuberculosis treatment. c. Provide education about the prevention of tuberculosis to members of the migrant community. d. Use skin tests to screen migrant health workers for tuberculosis infection. 21. A mother felt very guilty that her baby was born HIV positive. When the nurse suggested the usual DPT and MMR immunizations, the mother was extremely upset. “Don’t you know HIV children are immunosuppressed?” she exclaimed. Which of the following would be the nurse’s best response? a. “All children have to have these immunizations before they can attend school.” b. “Being HIV positive, your child is more likely to catch an infection and be very ill if not immunized.” c. “I’m so sorry; I forgot for a moment your child was HIV positive.” d. “The American Pediatric Association requires all health care providers to offer these immunizations to all parents; it is your choice whether or not to accept them.” 22. A nurse was reading PPD tests 24 hours after another nurse had administered them. Which of the following findings would cause the nurse to interpret the test as positive? a. 15 mm of erythema in a client with HIV infection b. 5 mm of induration in an immigrant from a country where TB is endemic c. A 5-mm ruptured pustule with purulent drainage in a homeless client d. 10 mm of swelling and increased firmness in a client recently released from a correctional facility 23. A high school student is planning to volunteer at the hospital after school, so she needs to have a Mantoux test before beginning. Which of the following information should the nurse provide to the new volunteer? a. “I will be using tiny tines to administer the TB antigen to the skin on your arm.” b. “Notify the clinic immediately if you experience any redness or itching at the test site.” c. “The areas should be kept dry until you return; cover it with plastic wrap when bathing.” d. “You will need to return in 2 to 3 days to have any reaction interpreted.” MULTIPLE RESPONSE 1. In which of the following cases would the school nurse be correct to advise the parents of an HIV-infected child to keep the child home from school? (Select all that apply.) a. The child develops allergies with sneezing. b. The child persists in biting behavior or is unable to control body secretions. c. The nurse is not comfortable with being responsible for the child. d. There is an outbreak of chickenpox in the school. 2. A woman and man who have come to the health clinic begin to argue loudly. “You gave me an STD!” the man yells. The woman screams back, “Not me. I don’t have an STD!” Which of the following statements would be most appropriate for the nurse to say to them? (Select all that apply.) a. “Actually, you’re very fortunate to have been tested so you and your partner can begin treatment before more serious damage is done.” b. “Some STDs may not have any symptoms, so you need to be tested for other conditions and treated if necessary.” c. “Sometimes the test is inaccurate, so before getting too upset, you should ask to be tested again.” d. “You may be able to get treatment from your pharmacist so you won’t have to be embarrassed like this again.” 3. The public health nurse comes to the hospital to see a client just diagnosed with hepatitis A. The nurse says, “I’m sorry to bother you when you’re not feeling well, but I need to ask you a few questions.” Which of the following questions would be most appropriate for the nurse to ask the client? (Select all that apply.) a. “Do you know how you got this infection?” b. “Who lives with you?” c. “Where are you employed?” d. “Where do you usually eat?” Chapter 27: Sexually Transmitted Infections MULTIPLE CHOICE 1. What unique factor causes adolescent girls to have a high risk for sexually transmitted infections (STIs)? a) They are in an experimental phase with sexual intercourse and believe they are resistant to developing STIs. b) The adolescent cervix is immature and lacks immunity. c) The length of the vaginal canal is short in adolescents, allowing a greater concentration of microorganisms within the internal genitalia. d) In adolescent girls, the anus to the vaginal introitus are in close proximity. Partly, perhaps, because of risk-taking behavior (unprotected intercourse or selection of high-risk partners), many adolescents have an increased risk for STI exposure and infection. The unique factor for adolescent women is that they have a physiologically increased susceptibility to infection because of increased cervical immaturity and lack of immunity. The remaining options are not considered legitimate risk factors for STIs. 2. How is gonorrhea transmitted from a pregnant woman to her fetus? a) Unbound in the blood via the placenta b) Attached to immunoglobulin G (IgG) via the placenta c) Across amniotic membranes by the direct inoculation with the fetal scalp electrodes during labor monitoring d) Predominately through infected cervical and secretions during the birth process 3. Which statement is false about the factors that facilitate the ascent of gonococci into the uterus and fallopian tubes? a) Ascent of gonococci is facilitated because the cervical plug disintegrates during menstruation. b) Ascent of gonococci is facilitated because the vaginal pH decreases to 2 or 3. c) Ascent of gonococci is facilitated because the uterine contractions may cause d) retrograde menstruation into the fallopian tubes. e) Ascent of gonococci is facilitated because the bacteria may adhere to sperm and be transported to the fallopian tubes. Several factors can facilitate the ascent of gonococci into the uterus and the fallopian tubes, where they cause pelvic inflammatory disease (PID). Among these factors are (1) disintegration of the cervical mucous plug and (2) a rise in vaginal pH greater than 4.5 during menstruation. The other options are accurate statements. 4. In women, what is the usual site of original gonococcal infection? a) Endocervical canal c. Fallopian tube b) Vagina d. Labia majora 5. What is the primary site for uncomplicated local gonococci infections in men? a. Epididymis c. Urethra b. Lymph nodes d. Prostate 6. What local complication of a gonococcal infection is diagnosed in approximately 10% of affected women? a. Acute salpingitis c. Vaginitis b. Cystitis d. Cervicitis 7. Which laboratory test is considered adequate for an accurate and reliable diagnosis of gonococcal urethritis in a symptomatic man? a) Ligase chain reaction (LCR) c. Polymerase chain reaction (PCR) b) Gram-stain technique d. DNA testing 8. How does an established gonococcal infection usually express itself in newborns? a) Generalized skin rash 4 to 6 days after birth b) Systemic infection with fever c) Bilateral corneal ulceration d) Yellow vaginal or penile discharge approximately 10 days after birth 9. What is the major concern regarding the treatment of gonococci infections? a) Development of antibiotic resistance c. Changes in pathogenicity b) Changes in virulence d. Mutations into different strains 10. Which sexually transmitted infection frequently coexists with gonorrhea? a. Syphilis c. Chlamydia b. Herpes simplex virus d. Chancroid 11. During which stage of syphilis do bloodborne bacteria spread to all the major organ systems? a. Primary c. Latent b. Secondary d. Tertiary Bloodborne bacteria spread to all major organ systems during only stage II, secondary syphilis (see Box 26-2). 12. In which stage of syphilis would the following clinical manifestations be found: destructive skin, bone and soft tissue lesions, aneurysms, heart failure, and neurosyphilis? a. Primary c. Latent b. Secondary d. Tertiary 13. Which organism is responsible for the development of syphilis? a) Neisseria syphilis c. Haemophilus ducreyi b) Treponema pallidum d. Chlamydia trachomatis 14. Which is a characteristic lesion of secondary syphilis? a) Condylomata lata c. Chancroid b) Gummas d. Donovan bodies 15. By which method is the organism that causes syphilis best identified? a) Acid-fast stain c. In vitro culture b) Gram-stained slide d. Darkfield microscopy 16. When a patient has small, vesicular lesions that last between 10 and 20 days, which sexually transmitted infection is suspected? a. Genital herpes c. Syphilis b. Chancroid d. Chlamydia 17. Which statement is false regarding the risk of transmission of the herpes simplex virus (HSV) from mother to fetus? a) Neonatal infection of HSV rarely occurs in the intrapartum or postpartum period. b) The risk is higher in women who have a primary HSV infection. c) The risk is higher in women who experience ruptured membranes more than 6 hours before delivery. d) d. The risk is higher when internal fetal monitoring devices are used. 18. During the latent period of a herpes virus infection, where in the host cell is the genome of the virus maintained? a. Mitochondria c. Nucleus b. Lysosomes d. Cytoplasm 19. During reactivation (release from latency), herpes virus genomes are transported through which nerves to the dermal surface? a. Somatic c. Autonomic b. Peripheral sensory d. Peripheral motor Only during reactivation are the viral genomes transported through the peripheral sensory nerves back to the dermal surface. 20. Which statement provides the most accurate information regarding the transmission of herpes simplex virus (HSV)? 1. HSV is transmitted only when vesicles are present. 2. HSV is transmitted only while lesions are present. 3. The use of condoms prevents the transmission of HSV. 4. The risk of transmission is present even during latent periods. . 21. Which drug may be prescribed orally for outbreak management of herpes simplex viral (HSV) infections? a) Acyclovir (Zovirax) c. Zidovudine (AZT) (Retrovir) b) 5-Fluorouracil (5-FU) d. Bichloroacetic acid (BCA) 22. Which of the following causes condylomata acuminata or genital warts? a) Chlamydia c. Human papillomavirus (HPV) b) Adenovirus d. Herpes simplex virus 1 (HSV-1) 23. Which treatment is used for trichomoniasis? a) Topical application of 5-Fluorouracil (5-FU) b) Topical application of acyclovir c) Systemic metronidazole d) Systemic tetracycline 24. A woman diagnosed with trichomoniasis asks if her sexual partner should be treated as well. What is the appropriate response? a) Sexual partners should be treated only if symptoms are present. b) Sexual partners should be treated even if they are asymptomatic. c) Infections in men are self-limiting; therefore a male sexual partner does not require treatment. d) Sexual partners should be treated to prevent infection. Sexual partners, even if asymptomatic, are also treated and examined for coexisting sexually transmitted infections. 25. Which microorganism is sexually transmitted, primarily by homosexual men, through infected feces? a) Shigellosis c. Giardia lamblia b) Cytomegalovirus (CMV) d. Entamoeba histolytica 26. Which hepatitis virus is known to be sexually transmitted? a. A c. C b. B d. D 27. Which sexually transmitted disease occasionally causes clinical manifestations of scant intermittent penile discharge, slight pruritus, and mild dysuria? a. Campylobacter enteritis c. Cytomegalovirus enteritis b. Shigellosis d. Trichomoniasis MULTIPLE RESPONSE 28. Which statements are true regarding the hepatitis B infection? (Select all that apply.) a) Hepatitis B poses a significant risk for chronic liver disease. b) Hepatocellular cancer is a common comorbid condition. c) Universal vaccination of infants and children is recommended. d) The preventive method of choice is immunization. e) Universal vaccination of sexually active adults is recommended. 29. What are the common modes of transmission for the hepatitis B virus (HBV)? (Select all that apply.) a) Needle punctures b) Blood transfusions c) Contact with infected body fluids d) Skin cuts e) Ingestion of infected substances 30. Which statements are true regarding the parasitic infection referred to as scabies? (Select all that apply.) a) Scabies is spread through skin-to-skin contact. b) The crab lice, Phthirus pubis, cause scabies. c) Severe pruritus is its major clinical manifestation. d) Symptoms worsen at night. e) Treatment is provided through oral medication therapy. 31. Which statements are true concerning the sexually transmitted infection (STI) lymphogranuloma venereum? (Select all that apply.) a) Lymphogranuloma venereum is an STI commonly diagnosed in the United States. b) It begins as a skin infection. c) Lymphogranuloma venereum spreads to lymph tissues. d) Primary and secondary lesions are apparent with this STI. e) A 60-day course of oral erythromycin is the recommended treatment. MATCHING 32. Treponema pallidum - Syphilis- T. pallidum is the cause of syphilis. 33. Haemophilus ducreyi – Chancroid-- H. ducreyi, a gram-negative bacillus, causes chancroid 34. Calymmatobacterium granulomatis -- Granuloma inguinale--- Granuloma inguinale (donovanosis) is a chronic, progressively destructive bacterial infection caused by Calymmatobacterium granulomatis 35. Entamoeba histolytica--- Amebiasis-- E. histolytica is the cause of amebiasis 36. Trichomonas vaginalis—Trichomoniasis--- Trichomoniasis is a result of infection caused by T. vaginalis. Chapter 35: Structure and Function of the Pulmonary System MULTIPLE CHOICE 1. What pulmonary defense mechanism propels a mucous blanket that entraps particles moving toward the oropharynx? a. Nasal turbinates c. Cilia b. Alveolar macrophages d. Irritant receptors on the nares 2. Which term is used to identify the movement of gas and air into and out of the lungs? a. Perfusion c. Respiration b. Ventilation d. Diffusion 3. When an individual aspirates food particles, where would the nurse expect to hear decreased or absent breath sounds? a. Left lung c. Trachea b. Right lung d. Carina 4. Aspiration is most likely to occur in the right mainstem bronchus because it: a. Extends vertically from the trachea. b. Is narrower than the left mainstem bronchus. c. Comes into contact with food and drink first. d. Is located at the site where the bronchi bifurcate. 5. Air passage among alveoli is collateral and evenly distributed because of the function of which structures? a. Type I alveolar cells c. Acinus pores b. Pores of Kohn d. Alveolar pores 6. Where in the lung does gas exchange occur? a. Trachea c. Alveolocapillary membrane b. Segmental bronchi d. Main bronchus 7. Surfactant produced by type II alveolar cells facilitates alveolar distention and ventilation by which mechanism? a. Decreasing thoracic compliance b. Attracting water to the alveolar surface c. Decreasing surface tension in the alveoli d. Increasing surface tension in the alveoli 8. Which part of the brainstem provides basic automatic rhythm of respiration by sending efferent impulses to the diaphragm and intercostal muscles? a. Dorsal respiratory group (DRG) c. Pneumotaxic center b. Ventral respiratory group d. Apneustic center 9. Which structures secrete surfactant? a. Type I alveolar cells c. Alveolar macrophages b. Type II alveolar cells d. Stretch receptors 10. Which structure is not associated with any lymphatic vessels? a. Trachea c. Acinus b. Bronchi d. Terminal bronchioles 11. Which describes the pressure in the pleural space? a. Atmospheric c. Above atmospheric b. Below atmospheric d. Variable 12. The adequacy of a person’s alveolar ventilation is assessed best by monitoring which mechanism? a. Ventilatory rate c. Respiratory effort b. Ventilatory pattern d. Arterial blood gas 13. Which normal physiologic change occurs in the aging pulmonary system? a. Decreased flow resistance c. Stiffening of the chest wall b. Fewer alveoli d. Improved elastic recoil 14. How is most of the oxygen in the blood transported? a. Dissolved in plasma c. In the form of carbon dioxide (CO2) b. Bound to hemoglobin d. Bound to protein 15. Stretch receptors and peripheral chemoreceptors send afferent impulses regarding ventilation to which location in the brain? a. Pneumotaxic center in the pons b. Apneustic center in the pons c. Dorsal respiratory group (DRG) in the medulla oblongata d. Ventral respiratory group (VRG) in the medulla oblongata 16. Which substances cause airway epithelium to constrict? a. Epinephrine and acetylcholine c. Bradykinin and thromboxane A b. Histamine and prostaglandin d. Leukotrienes and prostacyclin 17. If a patient develops acidosis, the nurse would expect the oxyhemoglobin dissociation curve to react in which manner? a. Shift to the right, causing more oxygen (O2) to be released to the cells b. Shift to the left, allowing less O2 to be released to the cells c. Show no change, allowing the O2 concentration to remain stable d. Show dramatic fluctuation, allowing the O2 concentration to increase 18. How is most carbon dioxide (CO2) in the blood transported? a. Attached to oxygen c. Combined with albumin b. In the form of bicarbonate d. Dissolved in the plasma 19. The sternocleidomastoid and scalene muscles are referred to as which group? a. Diaphragmatic muscles c. Intercostal muscles b. Muscles of expiration d. Muscles of inspiration 20. An increase in surface tension caused by decreased surfactant production results in which alteration? a. Decrease in alveolar macrophage production b. Increase in lung compliance c. Decrease in alveoli collapse d. Increase in alveoli fluid collection 21. Decreased lung compliance means that the lungs are demonstrating which characteristic? a. Difficult deflation c. Stiffness b. Easy inflation d. Inability to diffuse oxygen 22. The lung is innervated by the parasympathetic nervous system via which nerve? a. Vagus c. Brachial b. Phrenic d. Pectoral 23. What event is characteristic of the function in Zone 1 of the lung? a. Blood flow through the pulmonary capillary bed increases in regular increments. b. Alveolar pressure is greater than venous pressure but not greater than arterial pressure. c. The capillary bed collapses, and normal blood flow ceases. d. Blood flows through Zone 1, but it is impeded to a certain extent by alveolar pressure. 24. Hypoventilation that results in the retention of carbon dioxide will stimulate which receptors in an attempt to maintain a normal homeostatic state? a. Irritant receptors c. Peripheral chemoreceptors b. Central chemoreceptors d. Stretch receptors 25. What is the most important cause of pulmonary artery constriction? a. Low alveolar partial pressure of arterial oxygen (PaO2) b. Hyperventilation c. Respiratory alkalosis d. Epinephrine 26. Where does the tracheal bifurcation occur? a. Larynx c. Carina b. Bronchi d. Nasopharynx 27. How low must the partial pressure of arterial oxygen (PaO2) drop before the peripheral chemoreceptors influence ventilation? a. Below 100 mm Hg c. Below 70 mm Hg b. Below 80 mm Hg d. Below 60 mm Hg 28. Which receptors are located in the smooth muscles of airways? a. Central chemoreceptors c. Peripheral chemoreceptors b. Stretch receptors d. J-receptors 29. Which receptors are located near the respiratory center? a. Peripheral chemoreceptors c. Central chemoreceptors b. Stretch receptors d. J-receptors 30. Which receptors are located in the aortic bodies, aortic arch, and carotid bodies? a. Central chemoreceptors c. J-receptors b. Stretch receptors d. Peripheral chemoreceptors 31. What is the purpose of the spirometry measurement? a. To evaluate the cause of hypoxia b. To measure the volume and flow rate during forced expiration c. To measures the gas diffusion rate at the alveolocapillary membrane d. To determine pH and oxygen and carbon dioxide concentrations MULTIPLE RESPONSE 32. Which structures belong to the upper conduction airway? (Select all that apply.) a. Oropharynx b. Larynx c. Nasopharynx d. Trachea e. Bronchi 33. Regarding the respiratory process referred to as remodeling, which statements are true? (Select all that apply.) a. Remodeling involves the vascular walls. b. Scarring and thickening occurs during this respiratory process. c. Remodeling results in a permanent change. d. Pulmonary artery hypotension results. e. Remodeling increases blood flow resistance. 34. What are the effects of aging on the pulmonary system? a. Decreased chest wall compliance b. Decreased lung recoil c. Reduced ventilatory reserve d. Decreased partial pressure of arterial oxygen (PaO2) e. Reduced respiratory rate MATCHING 35. Initiates rapid, shallow breathing- J-receptors- J-receptors are sensitive to increased pulmonary capillary pressure, which stimulates them to initiate rapid, shallow breathing; hypotension; and bradycardia. 36. Monitors pH, partial pressure of carbon dioxide (PaCO2), and partial pressure of oxygen (PaO2) in arterial blood- Peripheral chemoreceptors- Although the peripheral chemoreceptors are sensitive to changes in PaCO2 and pH, they are primarily sensitive to oxygen levels in arterial blood (PaO2) and are responsible for all of the increase in ventilation that occurs in response to arterial hypoxemia. 37. Initiates cough reflex- Irritant receptors- Irritant receptors are sensitive to noxious aerosols (vapors), gases, and particulate matter (e.g., inhaled dusts), which cause them to initiate the cough reflex. 38. Senses pH of cerebrospinal fluid- Central chemoreceptors- Central chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of cerebrospinal fluid (CSF). 39. Hering-Breuer expiratory reflex- Stretch receptors- Stretch receptors decrease ventilatory rate and volume when stimulated, an occurrence sometimes referred to as the Hering-Breuer expiratory reflex. Chapter 36: Alterations of Pulmonary Function MULTIPLE CHOICE 1. Besides dyspnea, what is the most common characteristic associated with pulmonary disease? a. Chest pain c. Cough b. Digit clubbing d. Hemoptysis 2. Sitting up in a forward-leaning position generally relieves which breathing disorder? a. Hyperpnea c. Apnea b. Orthopnea d. Dyspnea on exertion 3. Kussmaul respirations as a respiratory pattern may be associated with which characteristic(s)? a. Alternating periods of deep and shallow breathing b. Pulmonary fibrosis c. Chronic obstructive pulmonary disease d. Slightly increased ventilatory rate, large tidal volumes, and no expiratory pause 4. Respirations that are characterized by alternating periods of deep and shallow breathing are a result of which respiratory mechanism? a. Decreased blood flow to the medulla oblongata b. Increased partial pressure of arterial carbon dioxide (PaCO2), decreased pH, and decreased partial pressure of arterial oxygen (PaO2) c. Stimulation of stretch or J-receptors d. Fatigue of the intercostal muscles and diaphragm 5. With a total hemoglobin of 9 g/dl, how many grams per deciliter of hemoglobin must become desaturated for cyanosis to occur? a. 3 c. 7 b. 5 d. 9 6. Which statement is true regarding ventilation? a. Hypoventilation causes hypocapnia. b. Hyperventilation causes hypercapnia. c. Hyperventilation causes hypocapnia. d. Hyperventilation results in an increased partial pressure of arterial carbon dioxide (PaCO2). 7. What term is used to describe the selective bulbous enlargement of the distal segment of a digit that is commonly associated with diseases that interfere with oxygenation of the blood? a. Edema c. Angling b. Clubbing d. Osteoarthropathy 8. Pulmonary edema and pulmonary fibrosis cause hypoxemia by which mechanism? a. Creating alveolar dead space b. Decreasing the oxygen in inspired gas c. Creating a right-to-left shunt d. Impairing alveolocapillary membrane diffusion 9. High altitudes may produce hypoxemia through which mechanism? a. Shunting c. Decreased inspired oxygen b. Hypoventilation d. Diffusion abnormalities 10. Which condition is capable of producing alveolar dead space? a. Pulmonary edema c. Atelectasis b. Pulmonary emboli d. Pneumonia 11. What is the most common cause of pulmonary edema? a. Right-sided heart failure c. Mitral valve prolapse b. Left-sided heart failure d. Aortic stenosis 12. Pulmonary edema usually begins to develop at a pulmonary capillary wedge pressure or left atrial pressure of how many millimeters of mercury (mm Hg)? a. 10 c. 30 b. 20 d. 40 13. The collapse of lung tissue caused by the lack of collateral ventilation through the pores of Kohn is referred to as what type of atelectasis? a. Compression c. Absorption b. Perfusion d. Hypoventilation 14. In what form of bronchiectasis do both constrictions and dilations deform the bronchi? a. Varicose c. Cylindric b. Symmetric d. Saccular 15. Which pleural abnormality involves a site of pleural rupture that acts as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing during expiration? a. Spontaneous pneumothorax c. Open pneumothorax b. Tension pneumothorax d. Secondary pneumothorax 16. In which type of pleural effusion does the fluid become watery and diffuse out of the capillaries as a result of increased blood pressure or decreased capillary oncotic pressure? a. Exudative c. Transudative b. Purulent d. Large 17. Which condition involves an abnormally enlarged gas-exchange system and the destruction of the lung’s alveolar walls? a. Transudative effusion c. Exudative effusion b. Emphysema d. Abscess 18. Which term is used to identify a circumscribed area of suppuration and destruction of lung parenchyma? a. Consolidation c. Empyema b. Cavitation d. Abscess 19. Which condition is not a cause of chest wall restriction? a. Pneumothorax c. Gross obesity b. Severe kyphoscoliosis d. Neuromuscular disease 20. What causes pneumoconiosis? a. Pneumococci bacteria c. Exposure to asbestos b. Inhalation of inorganic dust particles d. Inhalation of cigarette smoke 21. Which condition is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury? a. Acute respiratory distress syndrome (ARDS) b. Pneumonia c. Pulmonary emboli d. Acute pulmonary edema 22. Which structure(s) in acute respiratory distress syndrome (ARDS) release inflammatory mediators such as proteolytic enzymes, oxygen-free radicals, prostaglandins, leukotrienes, and platelet-activating factor? a. Complement cascade c. Macrophages b. Mast cells d. Neutrophils 23. Pulmonary edema in acute respiratory distress syndrome (ARDS) is the result of an increase in: a. Levels of serum sodium and water c. Capillary hydrostatic pressure b. Capillary permeability d. Oncotic pressure 24. In acute respiratory distress syndrome (ARDS), alveoli and respiratory bronchioles fill with fluid as a result of which mechanism? a. Compression on the pores of Kohn, thus preventing collateral ventilation b. Increased capillary permeability, which causes alveoli and respiratory bronchioles to fill with fluid c. Inactivation of surfactant and the impairment of type II alveolar cells d. Increased capillary hydrostatic pressure that forces fluid into the alveoli and respiratory bronchioles 25. Which type of pulmonary disease requires more force to expire a volume of air? a. Restrictive c. Acute b. Obstructive d. Communicable 26. Which immunoglobulin (Ig) may contribute to the pathophysiologic characteristics of asthma? a. IgA c. IgG b. IgE d. IgM 27. Which statement about the late asthmatic response is true? a. Norepinephrine causes bronchial smooth muscle contraction and mucus secretion. b. The release of toxic neuropeptides contributes to increased bronchial hyperresponsiveness. c. The release of epinephrine causes bronchial smooth muscle contraction and increases capillary permeability. d. Immunoglobulin G initiates the complement cascade and causes smooth muscle contraction and increased capillary permeability. 28. Clinical manifestations of inspiratory and expiratory wheezing, dyspnea, nonproductive cough, and tachypnea are indicative of which condition? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma 29. The most successful treatment for chronic asthma begins with which action? a. Avoidance of the causative agent b. Administration of broad-spectrum antibiotics c. Administration of drugs that reduce bronchospasm d. Administration of drugs that decrease airway inflammation 30. Which factor contributes to the production of mucus associated with chronic bronchitis? a. Airway injury c. Increased Goblet cell size b. Pulmonary infection d. Bronchospasms 31. Clinical manifestations of decreased exercise tolerance, wheezing, shortness of breath, and productive cough are indicative of which respiratory disorder? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma 32. Clinical manifestations that include unexplained weight loss, dyspnea on exertion, use of accessory muscles, and tachypnea with prolonged expiration are indicative of which respiratory disorder? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma 33. Which of the following is the most common route of lower respiratory tract infection? a. Aspiration of oropharyngeal secretions b. Inhalation of microorganisms c. Microorganisms spread to the lung via blood d. Poor mucous membrane protection 34. What is the initial step in the management of emphysema? a. Inhaled anticholinergic agents c. Cessation of smoking b. Beta agonists d. Surgical reduction of lung volume 35. In tuberculosis, the body walls off the bacilli in a tubercle by stimulating which action? a. Macrophages that release tumor necrosis factor–alpha (TNF- b. Phagocytosis by neutrophils and eosinophils c. Formation of immunoglobulin G to initiate the complement cascade d. Apoptotic infected macrophages that activate cytotoxic T cells 36. The progression of chronic bronchitis is best halted by which intervention? a. Regular use of bronchodilators b. Smoking cessation c. Postural chest drainage techniques d. Identification of early signs of infection 37. Clinical manifestations of inspiratory crackles, increased tactile fremitus, egophony, and whispered pectoriloquy are indicative of which respiratory condition? a. Chronic bronchitis c. Pneumonia b. Emphysema d. Asthma 38. Pulmonary artery hypertension (PAH) results from which alteration? a. Narrowed pulmonary capillaries c. Destruction of alveoli b. Narrowed bronchi and bronchioles d. Ischemia of the myocardium 39. Squamous cell carcinoma of the lung is best described as a tumor that causes which alterations? a. Abscesses and ectopic hormone production b. Airway obstruction and atelectasis c. Pleural effusion and shortness of breath d. Chest wall pain and early metastasis 40. What medical term is used to identify the accumulation of air in the pleural space? a. Flail chest c. Pleural effusion b. Pneumothorax d. Exudate effusion 41. What medical term is used to identify the presence of pus in the pleural space? a. Plural effusion c. Empyema b. Asthma d. Pneumonia 42. Fluid in the pleural space characterizes which condition? a. Pleural effusion c. Bronchiectasis b. Atelectasis d. Ischemia 43. Which statement is true regarding hypoxemia? a. Hypoxemia results in the increased oxygenation of arterial blood. b. Respiratory alterations cause hypoxemia. c. Hypoxemia results in the decreased oxygenation of tissue cells. d. Various system changes cause hypoxemia. 44. Which medication classification is generally included in the treatment of silicosis? a. Corticosteroids c. Bronchodilators b. Antibiotics d. Expectorants 45. What medical term is used for a condition that results from pulmonary hypertension, creating chronic pressure overload in the right ventricle? a. Hypoxemia c. Bronchiectasis b. Hypoxia d. Cor pulmonale MULTIPLE RESPONSE 46. What are the causes of dyspnea? (Select all that apply.) a. Decreased pH, increased partial pressure of arterial carbon dioxide (PaCO2) and decreased partial pressure of arterial oxygen (PaO2) b. Decreased blood flow to the medulla oblongata c. Stimulation of stretch or J-receptors d. Presence of anxiety e. Presence of pain 47. Which inflammatory mediators are produced in asthma? (Select all that apply.) a. Histamine b. Bradykinin c. Leukotrienes d. Prostaglandins e. Neutrophil proteases 48. Which clinical manifestation is associated with pulmonary hypertension? (Select all that apply.) a. Systemic blood pressure greater than 130/90 mm Hg b. Rhonchi bilaterally c. Dyspnea on exertion d. Peripheral edema e. Jugular venous distention 49. Which statements are true regarding exudative effusion? (Select all that apply.) a. Exudative effusion contains high concentrations of white blood cells. b. Exudative effusion produces a very thick exudate. c. Exudative effusion may occur in response to an inflammatory process. d. The presence of a malignant cancer can trigger exudative effusion. e. Exudative effusion is a result of increased capillary permeability. 50. Which characteristics are symptomatic of a flail chest? (Select all that apply.) a. Involves the fracture of several consecutive ribs. b. Involves multiple fractures to individual ribs. c. Can involve the fracture of the sternum. d. Is generally a result of the inflammatory process. e. Is more common among the older adult population. 51. Which statements regarding Mycobacterium tuberculosis are true regarding the bacilli’s ability to go into dormancy? (Select all that apply.) a. Neutrophils and macrophages all play a role in its dormancy. b. Mycobacterium tuberculosis is capable of dormancy but for only a short period. c. The immune system is the controlling factor regarding its length of dormancy. d. The bacilli are sealed off in tubercles to allow for dormancy. e. An attack by lymphocytes brings the bacilli out of their dormant state. MATCHING 52. Pulmonary fibrosis-- Excessive amount of connective tissue in the lung-- Pulmonary fibrosis is an excessive amount of fibrous or connective tissue in the lung. 53. Atelectasis--- Lung tissue collapse--- Atelectasis is the collapse of lung tissue. 54. Bronchiectasis-- Abnormal dilation of the bronchi-- Bronchiectasis is persistent abnormal dilation of the bronchi. 55. Aspiration--- Passage of fluid and solid particles into the lung 56. Bronchiolitis--- Inflammatory obstruction of small airways--- Bronchiolitis is inflammation of the small airways or bronchioles. MULTIPLE CHOICE- additional questions 1. A 10-year-old female develops pneumonia. Physical exam reveals subcostal and intercostal retractions. She reports that breathing is difficult and she feels she cannot get enough air. What term should the nurse use to document this condition? a. Cyanosis b. Dyspnea c. Hyperpnea d. Orthopnea 2. A 20-year-old male presents to his primary care provider reporting difficulty breathing when lying down. What term should the nurse use to document this condition? a. Dyspnea b. Orthopnea c. Apnea d. Tachypnea 3. A 50-year-old diabetic male did not take his medication and is now in metabolic acidosis. He is experiencing Kussmaul respirations. What type of breathing will the nurse observe upon assessment? a. Audible wheezing or stridor b. A slightly increased ventilatory rate, large tidal volumes, and no expiratory pause c. Rapid respirations with periods of apnea d. Very slow inhalations and rapid expirations 4. A 30-year-old female received a severe head injury in a motor vehicle accident. She is now experiencing respiratory abnormalities characterized by alternating periods of deep and shallow breathing with periods of apnea. What term should the nurse use when charting this condition? a. Cheyne-Stokes b. Frank-Starling c. Apnea d. Orthopnea 5. Which patient would the nurse assess for paroxysmal nocturnal dyspnea (PND)? A patient with: a. Pulmonary fibrosis b. Asthma c. Left ventricular failure d. Hypotension 6. A 20-year-old male is in acute pain. An arterial blood gas reveals decreased carbon dioxide (CO2) levels. Which of the following does the nurse suspect is the most likely cause? a. Hyperventilation b. Hypoventilation c. Apnea d. Cyanosis 7. A 65-year-old female with emphysema presents to the ER for difficulty breathing. Physical exam reveals bluish skin and mucous membranes. How should the nurse chart this condition? Patient has: a. Cyanosis b. Hemoptysis c. Hematemesis d. Ischemia 8. A 28-year-old male reports to his primary care provider that he has had a cold for a week and is coughing up bloody secretions. When giving report, what term should the nurse use to describe this condition? a. Hematemesis b. Cyanosis c. Rhinitis d. Hemoptysis 9. A nurse is reviewing the results of an ABG and finds reduced oxygenation of arterial blood. What term should the nurse use to describe this condition? a. Ischemia b. Hypoxia c. Hypoxemia d. Hypocapnia 10. A group of mountain climbers experience confusion, tachycardia, edema, and decreased renal output after climbing Mount Rainier. A nurse recalls this condition is caused by: a. Bronchoconstriction b. Hypoventilation c. Decreased inspired oxygen d. Diffusion abnormalities 11. A nurse remembers a low ventilation-perfusion ratio results in: a. Increased dead space b. Shunting c. Alveolar collapse d. Bronchoconstriction 12. When the pulmonologist discusses the condition in which a series of alveoli in the left lower lobe receive adequate ventilation but do not have adequate perfusion, which statement indicates the nurse understands this condition? When this occurs in a patient it is called: a. A right-to-left shunt b. Alveolar dead space c. A low ventilation-perfusion ratio d. Pulmonary hypotension 13. A 30-year-old male is involved in a motor vehicle accident and sustains trauma to the lungs and chest wall. He experiences respiratory failure. Which of the following lab values would the nurse expect? a. Electrolyte imbalances b. Elevated PaCO2 c. Low hematocrit d. Elevated pH 14. A nurse is teaching staff about pulmonary edema. Which information should the nurse include? The most common cause of pulmonary edema is: a. Right heart failure b. Left heart failure c. Asthma d. Lung cancer 15. A 47-year-old male is diagnosed with pulmonary edema. Which assessment findings will the nurse observe? a. Thick mucus secretions b. Pink, frothy sputum c. Hypocapnia d. Wheezing 16. A 65-year-old male recently had a cerebrovascular accident that resulted in dysphagia. He now has aspiration of gastric contents. The nurse assesses the patient for which complication? a. Pneumonia b. Bronchiectasis c. Pneumothorax d. Emphysema 17. A 26-year-old female recently underwent surgery and is now experiencing dyspnea, cough, fever, and leukocytosis. Tests reveal that she has a collapsed lung caused by removal of air from obstructed alveoli. What condition will the nurse observe on the chart? a. Compression atelectasis b. Bronchiectasis c. Absorption atelectasis d. Hypoventilation 18. A 45-year-old male undergoes lung transplantation. He now suffers from airway occlusion secondary to fibrosis. Which diagnosis will the nurse see on the chart? a. Compression atelectasis b. Bronchiectasis c. Bronchiolitis d. Bronchiolitis obliterans 19. A 50-year-old male presents with hypotension, hypoxemia, and tracheal deviation to the left. Tests reveal that the air pressure in the pleural cavity exceeds barometric pressure in the atmosphere. Based upon these assessment findings, what does the nurse suspect the patient is experiencing? a. Pleural effusion b. Tension pneumothorax c. Open pneumothorax d. Transudative pneumothorax 20. A 60-year-old female with a history of cirrhosis presents with dyspnea, impaired ventilation, and pleural pain. A diagnosis of pleural effusion is made, and a watery fluid is drained. When giving report, the nurse will refer to this fluid as: a. Exudative b. Purulent c. Infected d. Transudative 21. An 80-year-old female develops pneumonia in the hospital. She becomes cyanotic, tachycardic, and develops a fever and cough. Chest x-ray reveals pus in the pleural space. Which of the following is the most likely diagnosis documented on the chart? a. Empyema b. Emphysema c. Pleurisy d. Chyle 22. A 54-year-old male is diagnosed with empyema. Upon receiving and reviewing the culture result, which organism does the nurse suspect is the most likely cause? a. Virus b. Staphylococcus aureus c. Klebsiella pneumonia d. Moraxella catarrhalis 23. A 15-year-old female is diagnosed with restrictive lung disease caused by fibrosis. The patient had a pulmonary functions test. Which of the following findings is expected? a. Increased compliance b. Increased tidal volume c. Decreased respiratory rate d. Decreased functional residual capacity 24. A 57-year-old male presents with cough, sputum production, dyspnea, and decreased lung volume. He is diagnosed with pneumoconiosis. When taking the patients history, which finding is the most probable cause of his illness? a. Inhalation of silica, asbestos, mica b. Autoimmune disease c. Allergic reactions d. Flail chest 25. A 42-year-old female presents with dyspnea; rapid, shallow breathing; inspiratory crackles; decreased lung compliance; and hypoxemia. Tests reveal a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Acute respiratory distress syndrome (ARDS) b. Sarcoidosis c. Postoperative respiratory failure d. Malignant respiratory failure 26. Which of the following shows a correct cause and effect sequence in the development of acute respiratory distress syndrome (ARDS)? a. Impaired alveolar compliance causing decreased surfactant production b. Alveolocapillary membrane injury causing a massive inflammatory response c. Hyaline membrane formation and fibrosis causing pulmonary edema d. Increased alveolocapillary membrane permeability causing metabolic alkalosis 27. A 60-year-old female with emphysema is having difficulty expiring a given volume of air. When giving report, the nurse will relay that the patient is most likely experiencing _____ pulmonary disease. a. Restrictive b. Obstructive c. Atelectatic d. Pleuritic 28. When the nurse is asked what causes asthma, how should the nurse respond? Asthma is thought to be caused by: a. An autosomal recessive trait b. Autoimmunity c. Excessive use of antibiotics as a young child d. Interactions between genetic and environmental factors ANS: D Asthma is an interaction between genetic and environmental factors. 29. A nurse recalls asthma is classified by: a. Pathophysiologic differences b. Clinical severity c. Genetic traits d. Treatment outcomes 30. A nurse is preparing to teach the staff about asthma. Which information should the nurse include? Airway hyper-responsiveness in asthma is related to: a. Increased sympathetic nervous system response b. The release of stress hormones c. Exposure to an allergen causing mast cell degranulation d. Hereditary decrease in IgE responsiveness . 31. A nurse is preparing to teach the staff about asthma. Which information should the nurse include? Airway obstruction contributing to increased airflow resistance and hypoventilation in asthma is caused by: a. Type II alveolar cell injury and decreased surfactant b. Alveolar fibrosis and pulmonary edema c. Mucus secretion, bronchoconstriction, and airway edema d. Collapse of the cartilaginous rings in the bronchi 32. A 10-year-old male is brought to the ER with prolonged bronchospasm and severe hypoxemia. The most likely diagnosis on the chart is: a. Exercise-induced asthma b. Chronic obstructive pulmonary disease (COPD) c. Status asthmaticus d. Bronchiectasis 33. A 22-year-old female presents with chronic bronchitis. Tests reveal closure of the airway during expiration. While planning care, a nurse recalls this condition is most likely caused by: a. Thick mucus from hypertrophied glands b. Ventilation-perfusion mismatch c. Hyperventilation d. Thinning smooth muscle in the bronchioles 34. A 25-year-old male presents with chronic bronchitis of 5 months duration. When obtaining the patients history, which of the following findings is most likely to cause this condition? a. Chronic asthma b. Air pollution c. Cigarette smoke d. Recurrent pneumonias 35. A 25-year-old male presents with chronic bronchitis of 5 months duration. Which of the following is the most significant concern for the nurse to monitor in this patient? a. Left heart failure b. Pulmonary embolus c. Immunosuppression d. Recurrent pulmonary infections 36. A 53-year-old male with a 20-year history of smoking is diagnosed with emphysema. When a staff member asks why the patients airways are obstructed, how should the nurse respond? The airways are obstructed because of: a. Excessive mucus production b. Loss of elastic recoil c. Infection and inflammation d. Airway edema 37. A 53-year-old male with a 20-year history of smoking is diagnosed with emphysema. When the nurse is asked what causes this, what is the nurses best response? Changes in his lungs are caused by: a. Viral infections b. Destruction of alveolar macrophages c. Alpha-1-antitrypsin deficiency d. Fibrotic lung disease 38. Individuals with a recent diagnosis of emphysema should be assessed for which most common presenting factor? a. A productive cough b. Cyanosis c. Dyspnea d. Cor pulmonale 39. A 60-year-old female with a 25-year history of smoking is diagnosed with emphysema. She has an increased anterior-posterior chest diameter. The nurse attributes this finding to: a. Air trapping b. Decreased inspiratory reserve volumes c. Increased flow rates d. Alveolar destruction 40. A patient asks what causes pneumonia. How should the nurse reply? Pneumonia is caused by: a. Use of anesthetic agents in surgery b. Atelectasis c. Chronic lung changes seen with aging d. Viral or bacterial infections 41. When the nurse observes a diagnosis of nosocomial pneumonia, the patient generally acquires this pneumonia: a. At day care centers b. On airplanes c. During hospitalization d. In the winter season 42. A 30-year-old male prison inmate contracted tuberculosis during an outbreak. When the nurse reviews the lab results, the organism that caused this condition is a: a. Bacterium b. Fungus c. Virus d. Parasite 43. A 30-year-old male prison inmate contracted tuberculosis during an outbreak. While planning interactions, the nurse realizes the patient can transmit this disease through: a. Skin contact b. Fecal-oral contact c. Airborne droplets d. Blood transfusions 44. A 70-year-old female is in the hospital for pelvic fracture. She develops pulmonary thromboembolism. The nurse realizes this embolus is composed of: a. Fat b. Air c. Tissue fragment d. Blood clot 45. Which of the following patients is at highest risk for developing pulmonary embolism (PE)? a. 21-year-old male with a hemophilia bleeding disorder b. 28-year-old woman who had a baby 6 months earlier c. 36-year-old woman with a history of alcohol abuse who is recovering from a gastric ulcer d. 72-year-old male who is recovering from hip replacement surgery in the hospital 46. An 80-year-old female is in the hospital for a bone fracture. While there she develops a large, nonlethal pulmonary embolus. Which of the following is a direct result of the obstruction to pulmonary blood flow? a. Pulmonary hypertension b. Systemic hypertension c. Pulmonary edema d. Risk of cerebral emboli 47. When a patient has a massive pulmonary embolism (PE), what complications will the nurse monitor for? a. Damage to the lung microcapillaries b. Chronic obstructive pulmonary disease (COPD) c. Disseminated intravascular coagulation (DIC) d. Shock and death 48. A 50-year-old male is diagnosed with pulmonary embolism (PE). Which of the following symptoms most likely occurred before treatment? a. Dry cough and inspiratory crackles b. Shallow respirations and wheezing c. Chest pain and shortness of breath d. Kussmaul respirations and back pain 49. A 60-year-old male undergoes surgery for a bone fracture. Which of the following nursing measures would be most effective for preventing pulmonary embolism (PE) in this patient? a. Ensure that patient uses supplemental oxygen. b. Prevent deep vein thrombosis formation. c. Check hematocrit and hemoglobin levels frequently during the postoperative period. d. Promote aggressive fluid intake. 50. A 50-year-old male with a 30-year history of smoking was diagnosed with lung cancer. He was previously exposed to air pollution, asbestos, and radiation at his job. Which of the following should the nurse realize had the greatest impact on the development of his cancer? a. Radiation b. Cigarette smoke c. Asbestos d. Air pollution 51. A 60-year-old male with a 40-year history of smoking presents with chest pain, cough, sputum production, and pneumonia. Tests reveal widespread metastatic cancer, and the primary care provider plans radiation therapy. Which of following is the most likely type of cancer to be documented on the chart? a. Adenoma b. Non-small cell carcinoma c. Small cell carcinoma d. Basal cell carcinoma MULTIPLE RESPONSE 1. Which of the following assessment findings would be expected in pulmonary embolism (PE)? (Select all that apply.) a. Chest pain b. Tachycardia c. Tachypnea d. Fever e. Hemoptysis 2. Which of the following are characteristic of idiopathic pulmonary arterial hypertension (IPAH)? (Select all that apply.) a. Male gender b. Fatigue c. Dyspnea d. Jugular vein distention e. Weight gain Chapter 41: Structure and Function of the Digestive System MULTIPLE CHOICE 1. In the mouth and stomach, salivary -amylase initiates the digestion of which nutrients? a. Proteins c. Fats b. Carbohydrates d. Fiber 2. Which elements in saliva protect against tooth decay? a. Salivary -amylase and ptyalin b. Secretin and IgA c. Endogenous enamelin and salivary -amylase d. Exogenous fluoride and a pH of 7.4 3. Saliva contains which immunoglobulin (Ig)? a. IgA c. IgG b. IgE d. IgM 4. What effect is a result of inhibiting the parasympathetic nervous system with a drug such as atropine? a. Salivation becomes thinner. c. The pH of saliva changes. b. Salivation decreases. d. Digestive enzymes are inhibited. 5. Food enters the stomach via which sphincter? a. Cardiac c. Gastric b. Upper esophageal d. Fundal 6. Which gastric cells secrete hydrochloric acid and intrinsic factor? a. Parietal c. G b. Chief d. H 7. Which cells in the stomach secrete histamine? a. Oxyntic c. D b. Chief d. Enterochromaffin-like 8. The presence of chyme in the duodenum stimulates which hormones? a. Motilin and histamine b. Secretin and cholecystokinin c. Enteroglucagon and gastric inhibitory peptide d. Somatostatin and acetylcholine 9. Which gastric hormone inhibits acid and pepsinogen secretion, as well as decrease the release of gastrin? a. Bombesin c. Somatostatin b. Histamine d. Acetylcholine 10. Which enzyme breaks down protein-forming polypeptides in the stomach? a. Acetylcholine c. Gastrin b. Pepsin d. Secretin 11. Exposure to which substance protects the mucosal barrier of the stomach? a. Prostaglandins c. Helicobacter pylori b. Aspirin d. Regurgitated bile 12. The ileum and jejunum are suspended by folds of the peritoneum that contain an extensive vascular and nervous network. What are these folds called? a. Ligament of Treitz c. Auerbach folds b. Mesentery d. Lamina propria 13. Where in the small intestines are lymphocytes, plasma cells, and macrophages produced? a. Brush border c. Lamina propria b. Microvilli d. Crypts of Lieberkühn 14. Why are water and electrolytes transported in both directions through tight junctions and intercellular spaces rather than across cell membranes? a. The intercellular hydrostatic pressure is inadequate to push the water and electrolytes across the cell membranes. b. A balance of cations and ions among the electrolytes on each side of the cell membranes cannot be maintained. c. The epithelial cell membranes are formed of lipids that are hydrophobic and therefore repel water. d. Receptors on those cell membranes are occupied with a diffusion of amino acids and monosaccharides. 15. Which statement best describes the gastrointestinal tract? a. The gastrointestinal tract is a muscular tube that transports food from the mouth to the stomach. b. The gastrointestinal tract is a hollow tube that extends from the mouth to the anus. c. The gastrointestinal tract is a baglike structure that propels partially digested food (chyme). d. The structure is 5 m long and consists of three segments. 16. Glucose transport enhances the absorption of which electrolyte? a. Sodium c. Potassium b. Phosphate d. Chloride 17. What process is capable of increasing both intrathoracic and intraabdominal pressure, thereby facilitating defecation? a. Relaxation of the internal anal sphincter b. Intestinal peristalsis c. Valsalva maneuver d. Ileogastric reflex 18. Which pancreatic enzyme is responsible for the breakdown of carbohydrates? a. Trypsin c. Lipase b. Amylase d. Chymotrypsin 19. The formation of water-soluble molecules to facilitate the absorption of the by-products of lipid hydrolysis is accomplished by: a. Micelles c. Chylomicrons b. Phospholipase d. Colipase 20. What is the primary source of physiologic iron? a. Transferrin from plasma c. Bile from bilirubin b. Pepsin form pepsinogen d. Heme from animal protein 21. Which statement is incorrect regarding the characteristics of vitamin B12? a. Vitamin B12 is absorbed in the terminal ileum. b. Vitamin B12 is absorbed in its free (unbound) form but only in small amounts. c. Vitamin B12 is necessary for platelet maturation. d. Vitamin B12 binds to intrinsic factor. . 22. Which water-soluble vitamin is absorbed by passive diffusion? a. Vitamin B6 c. Vitamin K b. Vitamin B1 d. Folic acid 23. Which vitamin facilitates the absorption of iron by the epithelial cells of the duodenum and jejunum? a. B6 c. E b. C d. B12 24. What is the role of the normal intestinal bacterial flora? a. Metabolizing bile salts, estrogens, and lipids b. Breaking down proteins into amino acids c. Facilitating the motility of the colon d. Metabolizing aldosterone and insulin 25. Kupffer cells are best described as: a. Natural killer cells that produce interferon-gamma (IFN-) b. Contractile and therefore capable of regulating the sinusoid blood flow c. Bactericidal and therefore central to innate immunity d. Able to metabolize estrogen, progesterone, and androgens 26. Bilirubin is a by-product of the destruction of which aged cells? a. Platelets c. Leukocytes b. Protein d. Erythrocytes 27. The process of conjugation of bilirubin in the liver is best described as which transformation? a. Unconjugated (fat-soluble) bilirubin into urobilinogen b. Unconjugated (fat-soluble) bilirubin into conjugated (water-soluble) bilirubin c. Conjugated (water-soluble) bilirubin into unconjugated (fat-soluble) bilirubin d. Conjugated (water-soluble) bilirubin into urobilinogen 28. Which statement is incorrect regarding gallbladder function? a. Within 30 minutes of eating, the gallbladder forces bile into the stomach. b. Cholinergic branches of the vagus nerve mediate gallbladder contraction. c. Cholecystokinin provides hormonal regulation of gallbladder contraction. d. The sphincter of Oddi controls the flow of bile from the gallbladder. 29. Which structure synthesizes clotting factors and the vitamin K necessary for hemostasis? a. Colon c. Gallbladder b. Spleen d. Liver 30. How many days does it take for the entire epithelial population of the small intestines to be replaced? a. 30 to 45 c. 7 to 15 b. 15 to 25 d. 4 to 7 31. Which statement is true regarding the state of the intestinal tract at birth? a. The intestinal tract is colonized by Escherichia coli. b. The intestinal tract is sterile. c. Clostridium welchii is present in the intestinal tract but in very small numbers. d. Streptococcus colonization in the intestinal tract has begun. MULTIPLE RESPONSE 32. Gastric emptying is delayed by the presence of which substances? (Select all that apply.) a. Solids b. Carbohydrates c. Nonisotonic solutions d. Bacteria e. Fats 33. Which statements are true regarding the ileogastric reflex? (Select all that apply.) a. The purpose of ileogastric reflex is to inhibit gastric motility. b. Ileum distension triggers the ileogastric reflex. c. The ileogastric reflex causes the relaxation of the ileocecal sphincter. d. Increased gastric secretion triggers the ileogastric reflex. e. The ileogastric reflex stimulates an increase in ileal motility. 34. Which hormones are involved in the relaxation of the stomach’s fundus during swallowing? (Select all that apply.) a. Progesterone b. Glucagon c. Motilin d. Gastrin e. Cholecystokinin 35. Which hormones are involved in regulating gastric motility by making the threshold potential of muscle fibers more negative? (Select all that apply.) a. Estrogen b. Secretin c. Somatostatin d. Gastrin e. Motilin 36. What requirements are necessary for calcium to be absorbed through the ileum at concentrations of less than 5 mmol/L? (Select all that apply.) a. Receptor site on the ileum b. Vitamin D3 c. Vitamin K d. Carboxypeptidase e. A carrier protein 37. Which water-soluble vitamins are dependent on sodium for absorption? (Select all that apply.) a. Pantothenic acid b. Vitamin B1 c. Vitamin C d. Vitamin B12 e. Folic acid 38. Which statement is correct regarding the functions of the pancreas? (Select all that apply.) a. Cholecystokinin stimulates the release of pancreatic enzymes. b. Bilirubin and S cells inhibit the secretion of pancreatic enzymes. c. Pancreatic polypeptide is released after eating. d. Acetylcholine (ACh) is liberated from the pancreatic branches of the vagus nerve. e. ACh stimulates the release of pancreatic enzymes. Chapter 42: Alterations of Digestive Function MULTIPLE CHOICE 1. Where in the brain is the vomiting center located? a. Hypothalamus c. Pons b. Medulla oblongata d. Midbrain 2. Antiemetic agents, such as domperidone and haloperidol, are antagonists for which receptors? a. 5-Hydroxytryptamine (5-HT) serotonin b. Histamine-2 c. Acetylcholine d. Dopamine 3. What type of vomiting is caused by the direct stimulation of the vomiting center by neurologic lesions involving the brainstem? a. Retch c. Duodenal b. Periodic d. Projectile 4. Considering the normal frequency of bowel evacuation, how infrequently can evacuation occur and still be considered within normal range? a. Once a day c. Once a week b. Once every 2 days d. Once every 2 weeks 5. How many stools per day are considered the upper limits of normal? a. Two c. Five b. Three d. Seven 6. The adult intestine processes approximately how many liters of luminal content per day? a. 3 c. 9 b. 6 d. 12 7. A person who has cholera would be expected to have which type of diarrhea? a. Osmotic c. Small volume b. Secretory d. Motility 8. What type of diarrhea is a result of lactase deficiency? a. Motility c. Secretory b. Osmotic d. Small-volume 9. Which statement is false concerning how abdominal pain is produced? a. Chemical mediators, such as histamine, bradykinin, and serotonin, produce abdominal pain. b. Edema and vascular congestion produce abdominal pain by stretching. c. Ischemia, caused by distention of bowel obstruction or mesenteric vessel thrombosis, produces abdominal pain. d. Low concentrations of anaerobes, such as Streptococci, Lactobacilli, Staphylococci, Enterobacteria, and Bacteroides, produce abdominal pain. 10. How can abdominal pain that is visceral in nature best be described? a. Abdominal pain that is visceral in nature is diffused, vague, poorly localized, and dull. b. It travels from a specific organ to the spinal cord. c. The pain lateralizes from only one side of the nervous system. d. Abdominal pain is associated with the peristalsis of the gastrointestinal tract. 11. What is the cause of gastroesophageal reflux disease? a. Excessive production of hydrochloric acid b. Zone of low pressure of the lower esophageal sphincter c. Presence of Helicobacter pylori in the esophagus d. Reverse muscular peristalsis of the esophagus 12. What term is used to identify frank bleeding of the rectum? a. Melena c. Occult bleeding b. Hematochezia d. Hematemesis 13. What is the cause of functional dysphagia? a. Intrinsic mechanical obstruction c. Tumor b. Extrinsic mechanical obstruction d. Neural or muscular disorders 14. What is the cause of reflux esophagitis? a. Immune response to gastroesophageal reflux b. Delayed gastric emptying c. Congenital anomaly d. Secretory response to gastroesophageal reflux . 15. By what mechanism does intussusception cause an intestinal obstruction? a. Telescoping of part of the intestine into another section of intestine, usually causing strangulation of the blood supply b. Twisting the intestine on its mesenteric pedicle, causing occlusion of the blood supply c. Loss of peristaltic motor activity in the intestine, causing an adynamic ileus d. Forming fibrin and scar tissue that attach to the intestinal omentum, causing obstruction 16. What is the most immediate result of a small intestinal obstruction? a. Vomiting c. Electrolyte imbalances b. Dehydration d. Distention 17. An intestinal obstruction at the pylorus or high in the small intestine causes metabolic alkalosis by causing which outcome? a. Gain of bicarbonate from pancreatic secretions that cannot be absorbed b. Excessive loss of hydrogen ions normally absorbed from gastric juices c. Excessive loss of potassium, promoting atony of the intestinal wall d. Loss of bile acid secretions that cannot be absorbed 18. What are the cardinal symptoms of small intestinal obstruction? a. Constant, dull pain in the lower abdomen relieved by defecation b. Acute, intermittent pain 30 minutes to 2 hours after eating c. Colicky pain caused by distention, followed by vomiting d. Excruciating pain in the hypogastric area caused by ischemia 19. What is a cause of chronic antral gastritis? a. Helicobacter pylori bacteria b. Development of autoantibodies to gastric H+/K+ ATPase c. Pernicious anemia d. Reflux of bile and alkaline pancreatic secretions 20. What is the primary cause of peptic ulcers? a. Hypersecretion of gastric acid c. Helicobacter pylori b. Hyposecretion of pepsin d. Escherichia coli 21. A peptic ulcer may occur in all of the following areas except the: a. Stomach c. Jejunum b. Duodenum d. Esophagus 22. Which statement is false regarding the contributing factors of duodenal ulcers? a. Bleeding from duodenal ulcers causes hematemesis or melena. b. Gastric emptying is slowed, causing greater exposure of the mucosa to acid. c. The characteristic pain begins 30 minutes to 2 hours after eating when the stomach is empty. d. Duodenal ulcers occur with greater frequency than other types of peptic ulcers. 23. After a partial gastrectomy or pyloroplasty, clinical manifestations that include increased pulse, hypotension, weakness, pallor, sweating, and dizziness are the results of which mechanism? a. Anaphylactic reaction in which chemical mediators, such as histamine, prostaglandins, and leukotrienes, relax vascular smooth muscles, causing shock b. Postoperative hemorrhage during which a large volume of blood is lost, causing hypotension with compensatory tachycardia c. Concentrated bolus that moves from the stomach into the small intestine, causing hyperglycemia and resulting in polyuria and eventually hypovolemic shock d. Rapid gastric emptying and the creation of a high osmotic gradient in the small intestine, causing a sudden shift of fluid from the blood vessels to the intestinal lumen 24. Which statement is consistent with dumping syndrome? a. Dumping syndrome usually responds well to dietary management. b. It occurs 1 to 2 hours after eating. c. Constipation is often a result of the dumping syndrome. d. It can result in alkaline reflux gastritis. 25. What stimulates the desire to eat? a. Agouti-related protein (AgRP) b. Alpha-melanocyte–stimulating hormone (-MSH) c. Cocaine- and amphetamine-regulated transcript (CART) d. Peptide YY (PYY) 26. Which structure regulates eating behavior and energy metabolism? a. Anterior pituitary c. Posterior pituitary b. Hypothalamus d. Parietal lobe 27. Which symptom is characteristic of bulimia nervosa? a. Recurrent episodes of binge eating with fears of not being able to stop eating. b. Fear of becoming obese, despite progressive weight loss. c. Perception that the body is fat when it is actually underweight. d. Absence of three consecutive menstrual periods. 28. The most common clinical manifestation of portal hypertension is what type of bleeding? a. Rectal c. Esophageal b. Duodenal d. Intestinal 29. What is the most common manifestation of portal hypertension–induced splenomegaly? a. Leukopenia c. Erythrocytopenia b. Thrombocytopenia d. Pancytopenia 30. Which statement is false concerning the accumulation of fluid in the peritoneal cavity? a. Impaired excretion of sodium by the kidneys promotes water retention. b. Decreased oncotic pressure and increased hepatic sinusoidal hydrostatic pressure cause the movement of fluid into the peritoneal cavity. c. Decreased blood flow to the kidneys activates aldosterone, which retains sodium. d. Circulating nitric oxide causes vasoconstriction, which forces fluid from the capillaries into the peritoneal cavity. 31. Which statement is false regarding the sources of increased ammonia that contribute to hepatic encephalopathy? a. End products of intestinal protein digestion are sources of increased ammonia. b. Digested blood leaking from ruptured varices is a source of increased ammonia. c. Accumulation of short-chain fatty acids that is attached to ammonia is a source of increased ammonia. d. Ammonia-forming bacteria in the colon are sources of increased ammonia. 32. Hepatic fat accumulation is observed in which form of cirrhosis? a. Biliary c. Postnecrotic b. Metabolic d. Alcoholic 33. Which statement is false concerning the pathophysiologic process of alcoholic cirrhosis? a. Inflammation and damage leading to cirrhosis begin in the bile canaliculi. b. Alcohol is transformed to acetaldehyde, which promotes liver fibrosis. c. Mitochondrial function is impaired, decreasing oxidation of fatty acids. d. Acetaldehyde inhibits export of proteins from the liver. 34. Which statement is false regarding the pathophysiologic process of acute pancreatitis? a. Bile duct or pancreatic duct obstruction blocks the outflow of pancreatic digestive enzymes. b. Acute pancreatitis can also result from direct cellular injury from drugs or viral infection. c. Acute pancreatitis is an autoimmune disease in which immunoglobulin G (IgG) coats the pancreatic acinar cells; consequently, the pancreatic enzymes destroy the cells. d. Acute pancreatitis is usually mild and spontaneously resolves. 35. The mutation of which gene is an early event associated with the pathogenetic origin of esophageal cancer? a. K-ras mutation c. myc b. TP53 d. HER2 36. Obesity is defined as a body mass index (BMI) greater than what measurement? a. 22 c. 28 b. 25 d. 30 MULTIPLE RESPONSE 37. Which statements are true regarding parietal pain? (Select all that apply.) a. Parietal pain arises from the parietal peritoneum. b. It is generally more localized than visceral pain. c. Parietal pain is usually less intense than visceral pain. d. Nerve fibers that travel to the spinal cord are involved in parietal pain. e. Parietal pain corresponds to dermatomes T6 and L1. 38. Which statements are true regarding chronic gastritis? (Select all that apply.) a. Chronic gastritis tends to occur in older adults. b. It causes thinning and degeneration of the stomach wall. c. Chronic gastritis results in chronic inflammation and mucosal atrophy. d. Mucosal atrophy is a common outcome of chronic gastritis. e. Epithelial metaplasia is often observed with chronic gastritis. 39. Which hormones are natural appetite suppressants? (Select all that apply.) a. Insulin b. Cortisol c. Galanin d. Calcitonin e. Serotonin 40. Which are the early (prodromal) clinical manifestations of hepatitis? (Select all that apply.) a. Fatigue b. Vomiting c. Itching d. Splenomegaly e. Hyperalgia 41. Which clinical manifestations are consistent with cancer of the cecum and ascending colon? (Select all that apply.) a. Mahogany-colored blood mixed with stool b. Anemia c. Pain d. Constipation e. Palpable mass in the lower right quadrant Chapter 38: Structure and Function of the Renal and Urologic Systems MULTIPLE CHOICE 1. The area of the kidneys that contains the glomeruli and portions of the tubules is called the: a. Medulla c. Pyramids b. Cortex d. Columns 2. What is the functional unit of the kidney called? a. Glomerulus c. Collecting duct b. Nephron d. Pyramid 3. Which cells have phagocytic properties similar to monocytes and contract like smooth muscles cells, thereby influencing the glomerular filtration rate? a. Principle cells c. Mesangial cells b. Podocin cells d. Intercalated cells 4. The only surface inside the nephron where cells are covered with microvilli to increase the reabsorptive surface area is called the: a. Proximal convoluted tubules c. Ascending loop of Henle b. Distal tubules d. Descending loop of Henle 5. What part of the kidney controls renal blood flow, glomerular filtration, and renin secretion? a. Macula densa c. Juxtaglomerular apparatus (JGA) b. Visceral epithelium d. Filtration slits 6. Kidney stones in the upper part of the ureter would produce pain referred to which anatomical area? a. Vulva or penis c. Thighs b. Umbilicus d. Lower abdomen 7. Innervation of the bladder and internal urethral sphincter is supplied by which nerves? a. Peripheral nerves c. Sympathetic nervous system b. Parasympathetic fibers d. Tenth thoracic nerve roots 8. How much urine accumulates in the bladder before the mechanoreceptors sense bladder fullness? a. 75 to 100 ml c. 250 to 300 ml b. 100 to 150 ml d. 350 to 400 ml 9. What is the trigone? a. A smooth muscle that comprises the orifice of the ureter b. The inner mucosal lining of the kidneys c. A smooth triangular area between the openings of the two ureters and the urethra d. One of the three divisions of the loop of Henle 10. The glomerular filtration rate is directly related to which factor? a. Perfusion pressure in the glomerular capillaries b. Diffusion rate in the renal cortex c. Diffusion rate in the renal medulla d. Glomerular active transport 11. On average, what percent of cardiac output do the kidneys receive? a. 10% to 20% c. 20% to 25% b. 15% to 20% d. 30% to 35% 12. What effects do exercise and body position have on renal blood flow? a. Exercise and body position activate renal parasympathetic neurons and cause mild vasoconstriction. b. They activate renal sympathetic neurons and cause mild vasoconstriction. c. Both activate renal parasympathetic neurons and cause mild vasodilation. d. They activate renal sympathetic neurons and cause mild vasodilation. 13. Blood vessels of the kidneys are innervated by the: a. Vagus nerve c. Somatic nervous system b. Sympathetic nervous system d. Parasympathetic nervous system 14. When renin is released, it is capable of which action? a. Inactivation of autoregulation b. Direct activation of angiotensin II c. Direct release of antidiuretic hormone (ADH) d. Formation of angiotensin I 15. What effect do natriuretic peptides have during heart failure when the heart dilates? a. Stimulates antidiuretic hormones. c. Stimulates renin and aldosterone. b. Inhibits antidiuretic hormones. d. Inhibits renin and aldosterone. 16. What is the direct action of atrial natriuretic hormone? a. Sodium retention c. Water retention b. Sodium excretion d. Water excretion 17. What term is used to identify the movement of fluids and solutes from the tubular lumen to the peritubular capillary plasma? a. Tubular secretion c. Tubular reabsorption b. Ultrafiltration d. Tubular excretion 18. How high does the plasma glucose have to be before the threshold for glucose is achieved? a. 126 mg/dl c. 180 mg/dl b. 150 mg/dl d. 200 mg/dl 19. Which hormone is required for water to be reabsorbed in the distal tubule and collecting duct? a. Antidiuretic hormone c. Cortisol b. Aldosterone d. Adrenocorticotropin hormone . 20. Which glycoprotein protects against urolithiasis and is a ligand for lymphokines? a. Uromodulin c. Urodilatin b. Nephrin d. Cystatin 21. What is the end-product of protein metabolism that is excreted in urine? a. Glucose c. Bile b. Ketones d. Urea 22. What is the action of urodilatin? a. Urodilatin causes vasoconstriction of afferent arterioles. b. It causes vasodilation of the efferent arterioles. c. Urodilatin inhibits antidiuretic hormone secretion. d. It inhibits salt and water reabsorption. 23. The concentration of the final urine is determined by antidiuretic hormone (ADH), which is secreted by which gland? a. Posterior pituitary c. Parathyroid b. Thyroid d. Anterior pituitary 24. Which statement is true regarding urodilatin? a. Urodilatin inhibits sodium chloride and water reabsorption in the medullary part of the collecting duct. b. It inhibits antidiuretic hormone (ADH) to prevent water reabsorption in the medullary part of the collecting duct. c. Urodilatin is stimulated by a rise in blood pressure and an increase in extracellular volume. d. It is stimulated by a fall in blood pressure and a decrease in extracellular volume. . 25. What substance stimulates renal hydroxylation in the process of producing vitamin D? a. Erythropoietin c. Calcitonin b. Thyroid hormone d. Parathyroid hormone 26. Which hormone is synthesized and secreted by the kidneys? a. Antidiuretic hormone c. Erythropoietin b. Aldosterone d. Angiotensinogen 27. What provides the best estimate of the functioning of renal tissue? a. Glomerular filtration rate b. Hourly urine output c. Serum blood urea nitrogen and creatinine d. The specific gravity of the solute concentration of the urine 28. Which renal change is found in older adults? a. Sharp decline in glomerular filtration rate b. Sharp decline in renal blood flow c. Decrease in the number of nephrons d. Decrease in urine output 29. Compared with a younger individual, how is the specific gravity of urine in older adults affected? a. Specific gravity of urine in older adults is increased. b. Specific gravity of urine in older adults is considered high normal. c. Specific gravity of urine in older adults is considered low normal. d. Specific gravity of urine in older adults is decreased. 30. What process allows the kidney to respond to an increase in workload? a. Glomerular filtration b. Secretion of 1,25-dihydroxyvitamin D3 c. Increased heart rate d. Compensatory hypertrophy . 31. Which process makes it possible for ureters to be transplanted successfully? a. Compensatory hypertrophy c. Peristalsis b. Erythropoietin secretion d. Collateral circulation MULTIPLE RESPONSE 32. Which structures are parts of the nephron? (Select all that apply.) a. Loop of Henle b. Renal corpuscle c. Proximal convoluted tubule d. Calyx e. Collecting duct 33. Which forces create passive transport of water in the proximal tubule? (Select all that apply.) a. Peritubular capillary hydrostatic pressure b. Peritubular capillary oncotic pressure c. Interstitial hydrostatic pressure d. Interstitial osmotic pressure e. Peritubular capillary osmotic pressure 34. Which hormones are produced by the kidney? (Select all that apply.) a. Renin b. Erythropoietin c. 1,25-dihydroxyvitamin D3 d. Calcitonin e. Aldosterone 35. Which statements are true regarding renal circulation? (Select all that apply.) a. The interlobar arteries travel down into the renal columns. b. The arcuate arteries branch to form the interlobar arteries. c. The arcuate arteries arch over the base of the pyramids. d. The interlobar arteries run parallel to the surface of the kidneys. e. The interlobar arteries run between the pyramids. 5th ed MULTIPLE CHOICE 1. A nurse is teaching the staff about the kidneys. Which information should the nurse include? The region of the kidneys that contains the glomeruli is the: a. Medulla b. Cortex c. Pyramids d. Columns 2. When the nurse is discussing the functional unit of the kidney, what other term should the nurse use? a. Calyx b. Nephron c. Collecting duct d. Pyramid 3. The urologist is teaching about the nephrons that determine the concentration of the urine. The urologist is discussing the _____ nephrons. a. Juxtamedullary b. Midcortical c. Cortical d. Medullary 4. A urologist is discussing the phagocytic cells that lie between the layers of the renal corpuscle. What is the urologist describing? a. Podocytes b. Macula densa cells c. Mesangial cells d. Filtration slits 5. When the nurse discusses the glomerulus and Bowman capsule together, it is referred to as the renal: a. Corpuscle b. Capsule c. Medulla d. Pyramid Together, the glomerulus and Bowman capsule are called the renal corpuscle. 6. When a nurse is checking the urinalysis, plasma proteins should be absent from the urine because: a. All proteins filtered are subsequently reabsorbed. b. All of the plasma proteins are too large to fit through the filtration slits. c. All proteins filtered are subsequently degraded before elimination. d. The negative charge of the glomerular filtration membrane repels the plasma proteins. . 7. When the nurse is discussing the sodium-sensing cells of the glomerulus, what term should the nurse use? a. Podocytes b. Macula densa c. Mesangial cells d. Loop of Henle 8. When a nurse is preparing to teach about urine, which information should the nurse include? Just before entering the ureter, urine passes through the: a. Collecting duct b. Renal pelvis c. Urethra d. Major calyx 9. A urologist is discussing a structure that supplies blood to the medulla. What is the urologist describing? a. Renal arteries b. Arcuate arteries c. Peritubular capillaries d. Vasa recta 10. A nurse is describing the trigone. Which information should be included? The trigone is defined as: a. The orifice of the ureter b. The inner area of the kidney c. A triangular area between the openings of the two ureters and the urethra d. The three divisions of the loop of Henle 11. When describing the male urinary anatomy, which information should the nurse include? The portion of the male urethra that is closest to the bladder is the _____ portion. a. Membranous b. Prostatic c. Cavernous d. Vas deferens . 13. While reviewing urine lab results, the nurse remembers the glomerular filtration rate (GFR) is directly related to the: a. Perfusion pressure in the glomerular capillaries b. Oncotic pressure in the glomerular capillaries c. Vascular resistance in the glomerular arterioles d. Hydrostatic pressure in the Bowman capsule 14. A nurse recalls the blood vessels of the kidneys are innervated by the: a. Vagus nerve b. Sympathetic nervous system c. Somatic nervous system d. Parasympathetic nervous system 15. While planning care for a patient with urinary problems, the nurse recalls that the renin-angiotensin system will be activated by: a. Increased blood volume b. Elevated sodium concentrations c. Decreased blood pressure in the afferent arterioles d. Renal hypertension 16. When a patients renal system secretes rennin, what effect will that cause in the body? It causes the direct activation of: a. Angiotensin I b. Angiotensin II c. Antidiuretic hormone d. Aldosterone 17. A nurse is reviewing urinalysis results and notices glucose is present in the urine. A nurse realizes glucose will be excreted in the urine when: a. The maximum rate of glucose filtration is achieved b. The carrier molecules have reached their maximum c. Glucose is consumed d. The ability of the kidneys to regulate blood glucose is lost 18. When teaching about sodium reabsorption, which information should the nurse include? The majority of sodium reabsorption takes place in the: a. Proximal tubule b. Loop of Henle c. Distal tubule d. Collecting duct 19. A kidney has a glomerular capillary hydrostatic pressure of 50 mm Hg, a Bowman capsule hydrostatic pressure of 15 mm Hg, and a glomerular capillary oncotic pressure of 12 mm Hg. The net filtration pressure is ____ mm Hg. a. 23 b. 27 c. 35 d. 38 20. A nurse is preparing to teach about the loop of Henle. Which information should be included? The descending segment of the loop of Henle primarily allows for: a. Sodium secretion b. Potassium secretion c. Hydrogen ion reabsorption d. Water reabsorption 21. When a staff member asks which of the following substances are actively secreted by the renal tubules, what is the nurses best response? a. Sodium and chlorine b. Phosphate and calcium c. Hydrogen and potassium d. Bicarbonate and carbonic acid 22. A nurse is preparing to teach about the collecting ducts. Reabsorption of water in the collecting ducts requires which of these hormones? a. Antidiuretic hormone (ADH) b. Atrial natriuretic factor (ANP) c. Renin d. Aldosterone 23. When a patient asks what role the kidneys play in vitamin D function, how should the nurse reply? a. Synthesizes vitamin D from cholesterol b. Activates intestinally absorbed vitamin D c. Metabolizes and breaks down vitamin D d. Excretes excess vitamin D 24. A 35-year-old hypertensive male begins taking a diuretic. Which of the following common side effects of this medication should the nurse monitor? a. Hypokalemia b. Hyponatremia c. Increased uric acid secretion d. Hypermagnesemia 25. A patient has searched the Internet for hormones. The patient has a good understanding when she knows that the hormone _____ is synthesized and secreted by the kidneys to stimulate bone marrow production of red blood cells. a. Creatinine b. Aldosterone c. Erythropoietin d. Renin 26. If a nurse wants to obtain the best estimate of renal function, which test should the nurse monitor? a. Glomerular filtration rate (GFR) b. Circulating antidiuretic hormone (ADH) levels c. Volume of urine output d. Urine-specific gravity The GFR provides the best estimate of functioning renal tissue. 27. A nurse recalls the glomerular filtration rate (GFR) and plasma creatinine (Pcr) concentration are _____ related. a. Directly b. Indirectly c. Inversely d. Not The GFR and Pcr are inversely related. MULTIPLE RESPONSE 1. When a student asks what the components of the nephron are, how should the nurse respond? The components of the nephron include (select all that apply): a. Loop of Henle b. Renal corpuscle c. Proximal tubule d. Renal pelvis e. Convoluted tubule 2. When a staff member asks how the urine gets from the nephrons to the calyces, what is the nurses best response? The renal structure that drains directly into the calyces is (are) the (select all that apply): a. Distal tubule b. Collecting duct c. Pyramid d. Renal pelvis e. Loop of Henle COMPLETION 1. A nurse recalls the superficial cortical nephrons account for ____% of all nephrons. 2. On average, _____% of renal plasma flow (RPF) to the glomerulus is filtered into the Bowman capsule. 3. A nurse would chart a patient is experiencing oliguria when a 24-hour urine output is less than ________. Chapter 39: Alterations of Renal and Urinary Tract Function MULTIPLE CHOICE 1. How does progressive nephrons injury affect angiotensin II activity? a) Angiotensin II activity is decreased. b) It is elevated. c) Angiotensin II activity is totally suppressed. d) It is not affected. 2. Which mineral accounts for the most common type of renal stone? a) Magnesium-ammonium-phosphate c. Calcium oxalate b) Uric acid d. Magnesium phosphate 3. Regarding the formation of renal calculi, what function does pyrophosphate, potassium citrate, and magnesium perform? a) They inhibit crystal growth. b) Pyrophosphate, potassium citrate, and magnesium stimulate the supersaturation of salt. c) They facilitate the precipitation of salts from a liquid to a solid state. d) Pyrophosphate, potassium citrate, and magnesium enhance crystallization of salt crystals to form stones. 4. Hypercalciuria is primarily attributable to which alteration? a) Defective renal calcium reabsorption b) Intestinal hyperabsorption of dietary calcium c) Bone demineralization caused by prolonged immobilization d) Hyperparathyroidism 5. Detrusor hyperreflexia develops from neurologic disorders that originate where? a) Spinal cord between C2 and S1. c. Above the pontine micturition center b) Spinal cord between S2 and S4 d. Below the cauda equina 6. Considering the innervation of the circular muscles of the bladder neck, which classification of drug is used to treat bladder neck obstruction? A. -Adrenergic blocking medications c. Parasympathomimetic medications B. -Adrenergic blocking medications. d. Anticholinesterase medications 7. Renal cell carcinoma, classified as clear cell tumors, arises from epithelial cells in which structure? a) Proximal tubule c. Nephron b) Distal tubule d. Glomerulus Renal cell carcinoma, classified as clear cell tumors according to cell type and extent of metastasis, arises from the proximal tubular epithelium. These tumors are not associated with the other options. 8. Bladder cancer is associated with the gene mutation of which gene? a) c-erbB2 b) Human epidermal growth factor receptor 2 (HER2) c) TP53 d) myc 9. What is the most common cause of uncomplicated urinary tract infections? a. Staphylococcus c. Proteus b. Klebsiella d. Escherichia coli 10. Which differentiating sign is required to make the diagnosis of pyelonephritis from that of cystitis? a) Difficulty starting the stream of urine b) Spasmodic pain that radiates to the groin c) Increased glomerular filtration rate d) Urinalysis confirmation of white blood cell casts 11. Considering host defense mechanisms, which element in the urine is bacteriostatic? a) High pH (alkaline urine) c. High glucose b) High urea d. High calcium 12. Which clinical manifestations of a urinary tract infection may be demonstrated in an 85-year-old individual? a) Confusion and poorly localized abdominal discomfort b) Dysuria, frequency, and suprapubic pain c) Hematuria and flank pain d) Pyuria, urgency, and frequency 13. Pyelonephritis is usually caused by which type of organism? a. Bacteria c. Viruses b. Fungi d. Parasites Pyelonephritis is usually caused by the bacteria Escherichia coli, Proteus, or Pseudomonas. 14. Which abnormal laboratory value is found in glomerular disorders? a) Elevated creatinine concentration c. Elevated immunoglobulin A (IgA) b) Low blood urea nitrogen (BUN) d. Low serum complement 15. Which glomerular lesion is characterized by thickening of the glomerular capillary wall with immune deposition of immunoglobulin G (IgG) and C3? a. Proliferative c. Mesangial b. Membranous d. Crescentic The thickening of the glomerular capillary wall characterizes only membranous lesions. 16. Goodpasture syndrome is an example of which of the following? a) Antiglomerular basement membrane disease b) Acute glomerulonephritis c) Chronic glomerulonephritis d) Immunoglobulin A (IgA) nephropathy 17. A patient exhibits symptoms including hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin as the major protein. These data suggest the presence of which disorder? a. Cystitis c. Glomerulonephritis b. Chronic pyelonephritis d. Nephrotic syndrome 18. Hypothyroidism, edema, hyperlipidemia, and lipiduria characterize which kidney disorder? a) Nephrotic syndrome c. Chronic glomerulonephritis b) Acute glomerulonephritis d. Pyelonephritis Symptoms of nephrotic syndrome include edema, hyperlipidemia, lipiduria, vitamin D deficiency, and hypothyroidism. These symptoms do not support the other options. 19. Which antibiotics are considered “major culprits” in causing nephrotoxic acute tubular necrosis (ATN)? a) Penicillin and ampicillin c. Gentamicin and tobramycin b) Vancomycin and bacitracin d. Cefazolin and cefepime 20. Which urine characteristics are indicative of acute tubular necrosis (ATN) caused by intrinsic (intrarenal) failure? a) Urine sodium >30 mEq/L b) Urine osmolality >500 mOsm c) Fractional excretion of sodium (FENa) <1% d) Urine sediment has no cells, some hyaline casts 21. How are glucose and insulin used to treat hyperkalemia associated with acute renal failure? a) Glucose has an osmotic effect, which attracts water and sodium, resulting in more dilute blood and a lower potassium concentration. b) When insulin transports glucose into the cell, it also carries potassium with it. c) Potassium attaches to receptors on the cell membrane of glucose and is carried into the cell. d) Increasing insulin causes ketoacidosis, which causes potassium to move into the cell in exchange for hydrogen. 22. Creatinine is primarily excreted by glomerular filtration after being constantly released from what type of tissue? a. Nervous system c. Muscle b. Kidneys d. Liver 23. Which statement is false concerning the skeletal alterations caused by chronic renal failure when the glomerular filtration rate (GFR) declines to 25% of normal? a) Parathyroid hormone is no longer effective in maintaining serum phosphate levels. b) The parathyroid gland is no longer able to secrete sufficient parathyroid hormone. c) The synthesis of 1,25-vitamin D3, which reduces intestinal absorption of calcium, is impaired. d) The synthesis of 1,25-vitamin D3, which impairs the effectiveness of calcium and phosphate resorption from bone by parathyroid hormone, is impaired. 24. Anemia of chronic renal failure can be successfully treated with which element? a) Intrinsic factor c. Vitamin D b) Vitamin B 12 d. Erythropoietin 25. When the right kidney is obstructed, how will the glomeruli and tubules in the left kidney compensate? a) Increase in number c. Develop collateral circulation b) Increase in size d. Increase speed of production 26. What medical term is used to identify a functional urinary tract obstruction caused by an interruption of the nerve supply to the bladder? a) Neurogenic bladder c. Necrotic bladder b) Obstructed bladder d. Retrograde bladder Neurogenic bladder is a general term for bladder dysfunction caused by neurologic disorders. The types of dysfunction are related to the sites in the nervous system that control sensory and motor bladder function (see Figure 38-3). None of the other options correctly identify the described condition. MULTIPLE RESPONSE 27. In glomerulonephritis, what damages the epithelial cells resulting in proteinuria? (Select all that apply.) a) Ischemia b) Lysosomal enzymes c) Compression from edema d) Activated complement e) Altered membrane permeability 28. Which statements are true concerning struvite stones? (Select all that apply.) a) They are more common in women than in men. b) Struvite stones are associated with chronic laxative use in women. c) They grow large and branch into a staghorn configuration in renal pelvis and calyces. d) Struvite stones are closely associated with urinary tract infections caused by urease-producing bacteria, such as Pseudomonas. e) They are more common in men than in women. 29. Which statements are true regarding renal colic? (Select all that apply.) a) Renal colic results in mild-to-moderate pain. b) Pain originates in the flank area. c) Renal colic indicates the presence of renal stones. d) Pain radiated to the groin. e) Renal colic indicates obstruction of the renal pelvis or proximal ureter. 30. Which conditions related to the bladder would result from the effects of lesions of the sacral segments below S1? (Select all that apply.) a) Frequency b) Urge incontinence c) Bladder distension d) Urgency e) Urinary retention 31. What are considered risk factors for developing bladder and kidney cancers? (Select all that apply.) a) Cigarette smoking b) Hypertension c) Exposure to aniline dyes d) Below normal body weight e) Male gender 32. Which renal disorders are considered causes of intrarenal renal failure? (Select all that apply.) a) Acute glomerulonephritis b) Allograft rejection c) Tumors d) Acute tubular necrosis (A TN) e) Prostatic hypertrophy 33. Prerenal injury from poor perfusion can result from which condition? (Select all that apply.) a) Bilateral ureteral obstruction b) Renal vasoconstriction c) Renal artery thrombosis d) Hemorrhage e) Hypotension [Show More]
Last updated: 2 years ago
Preview 1 out of 127 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$20.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 20, 2020
Number of pages
127
Written in
Additional information
This document has been written for:
Uploaded
Apr 20, 2020
Downloads
1
Views
122

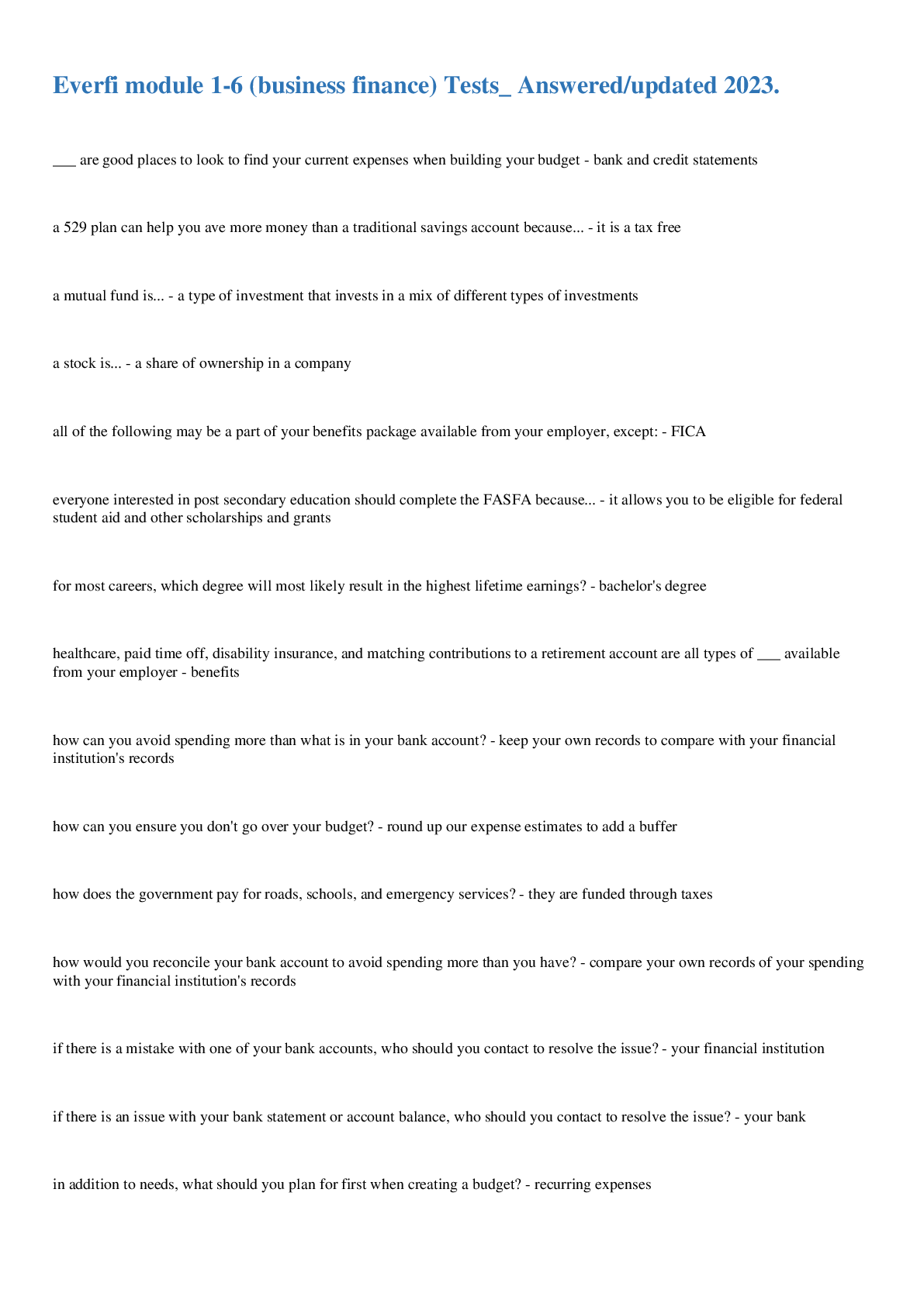

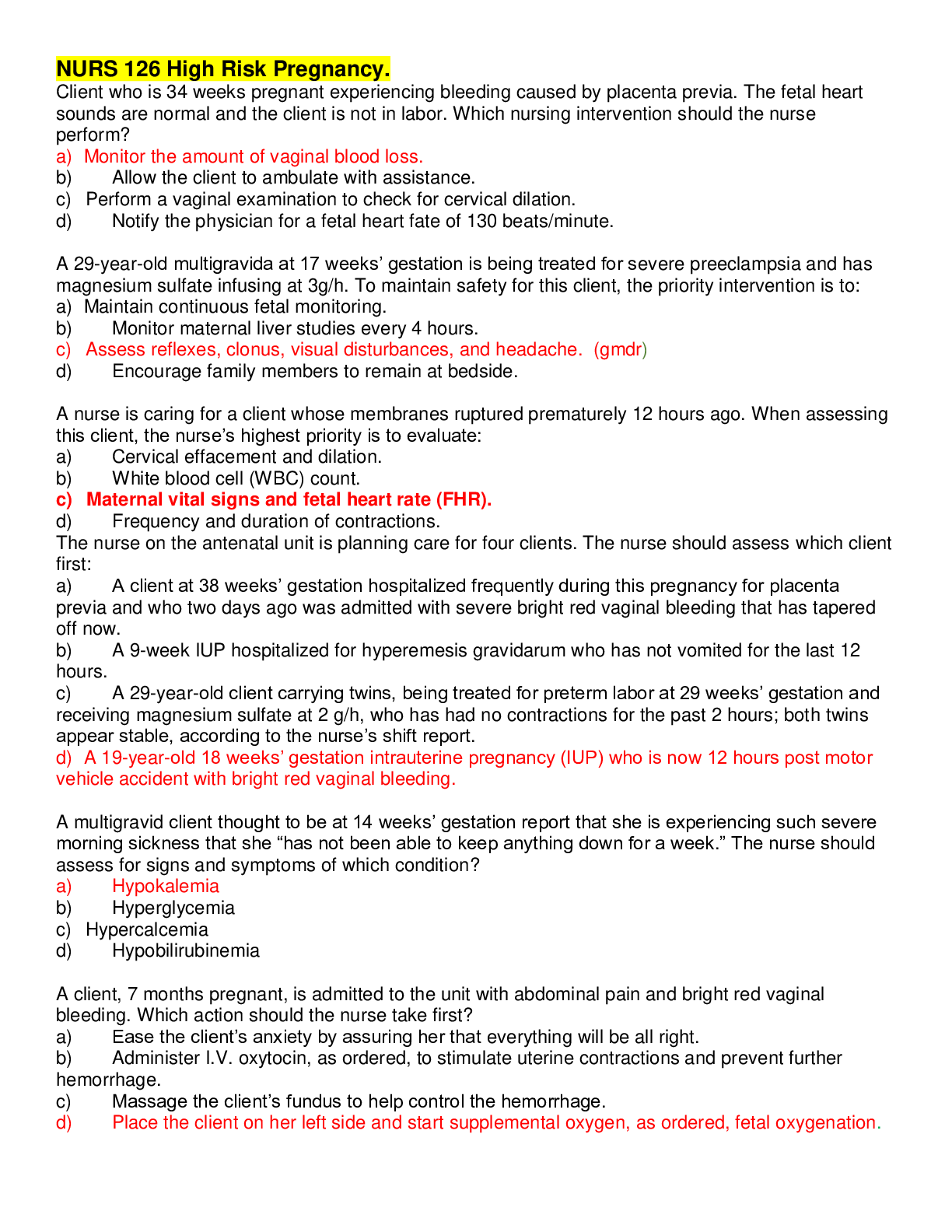


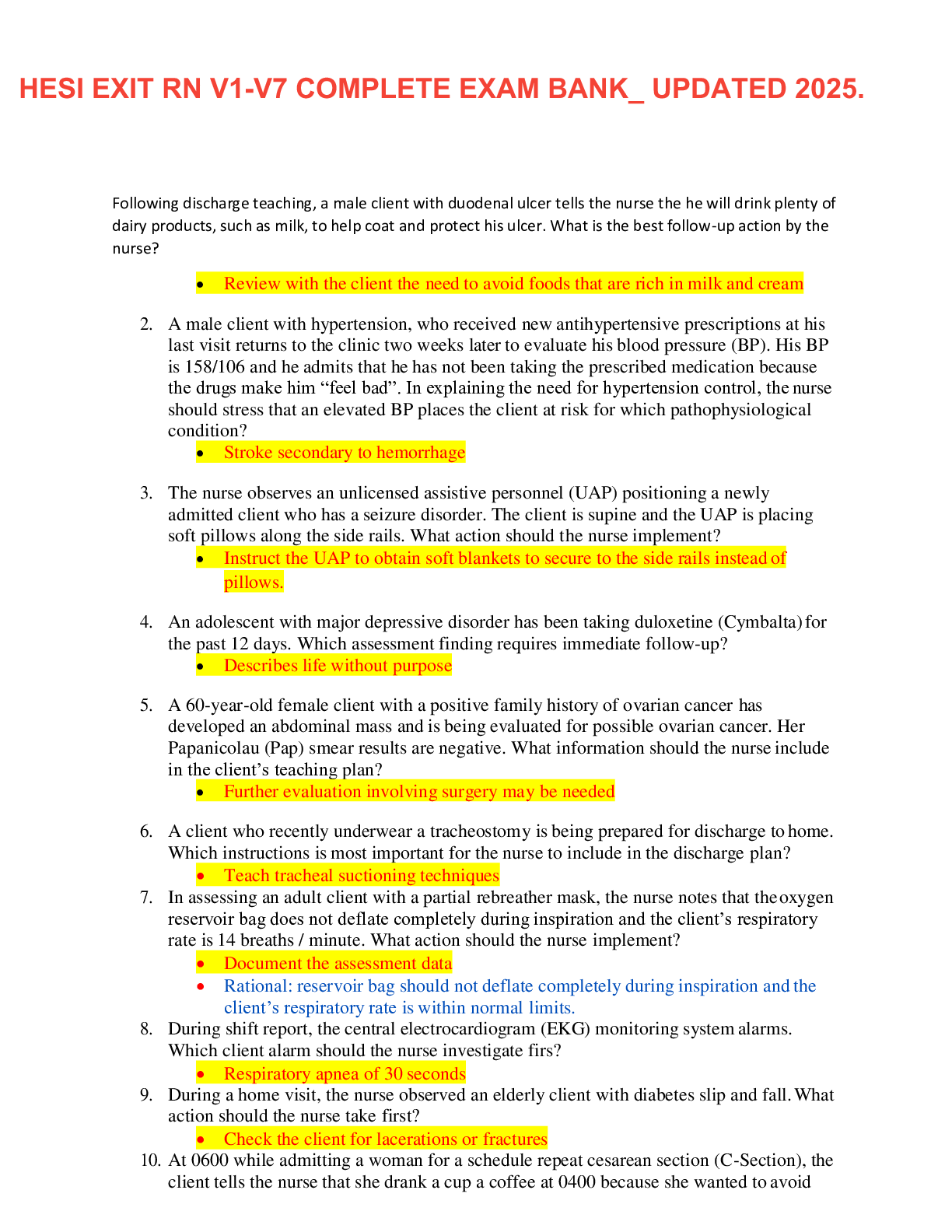
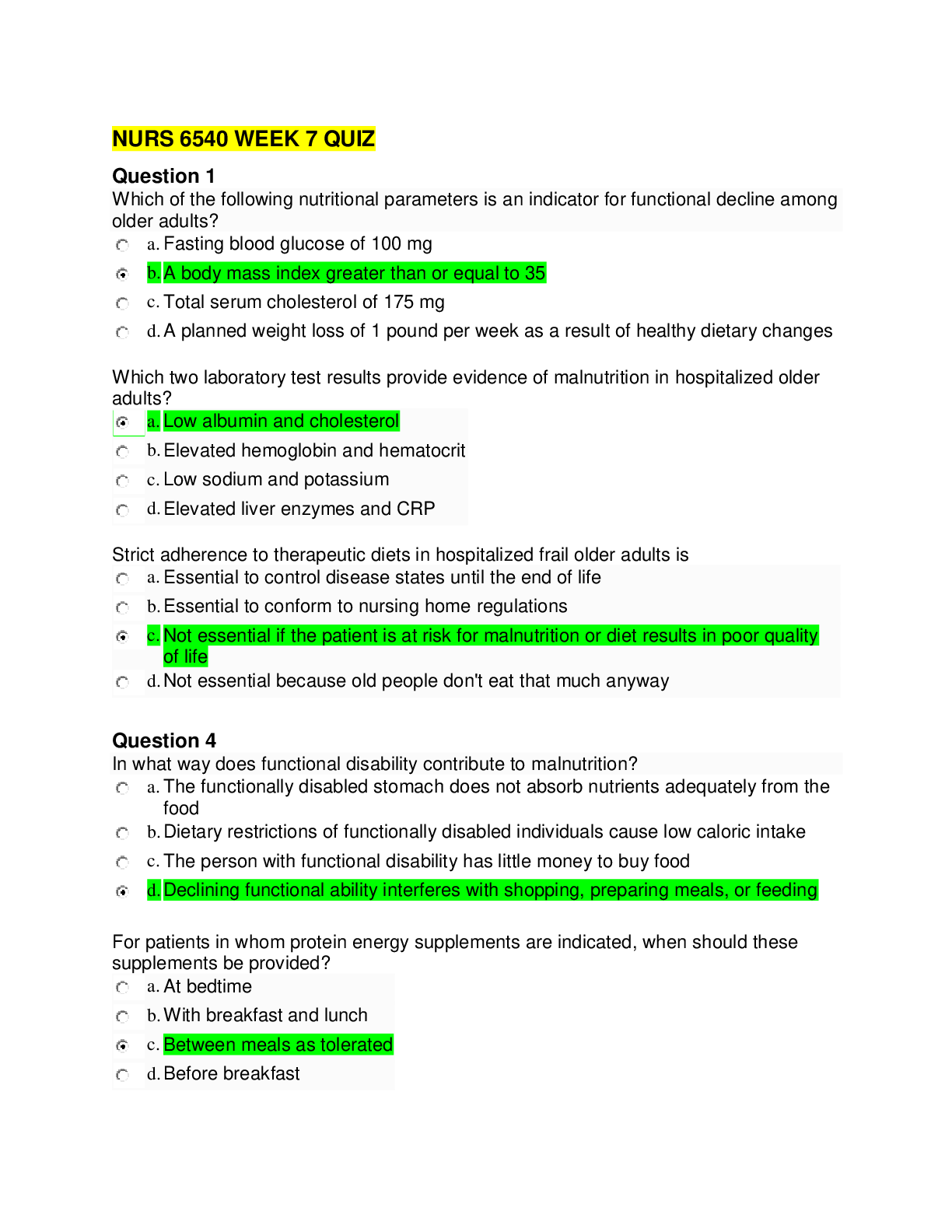
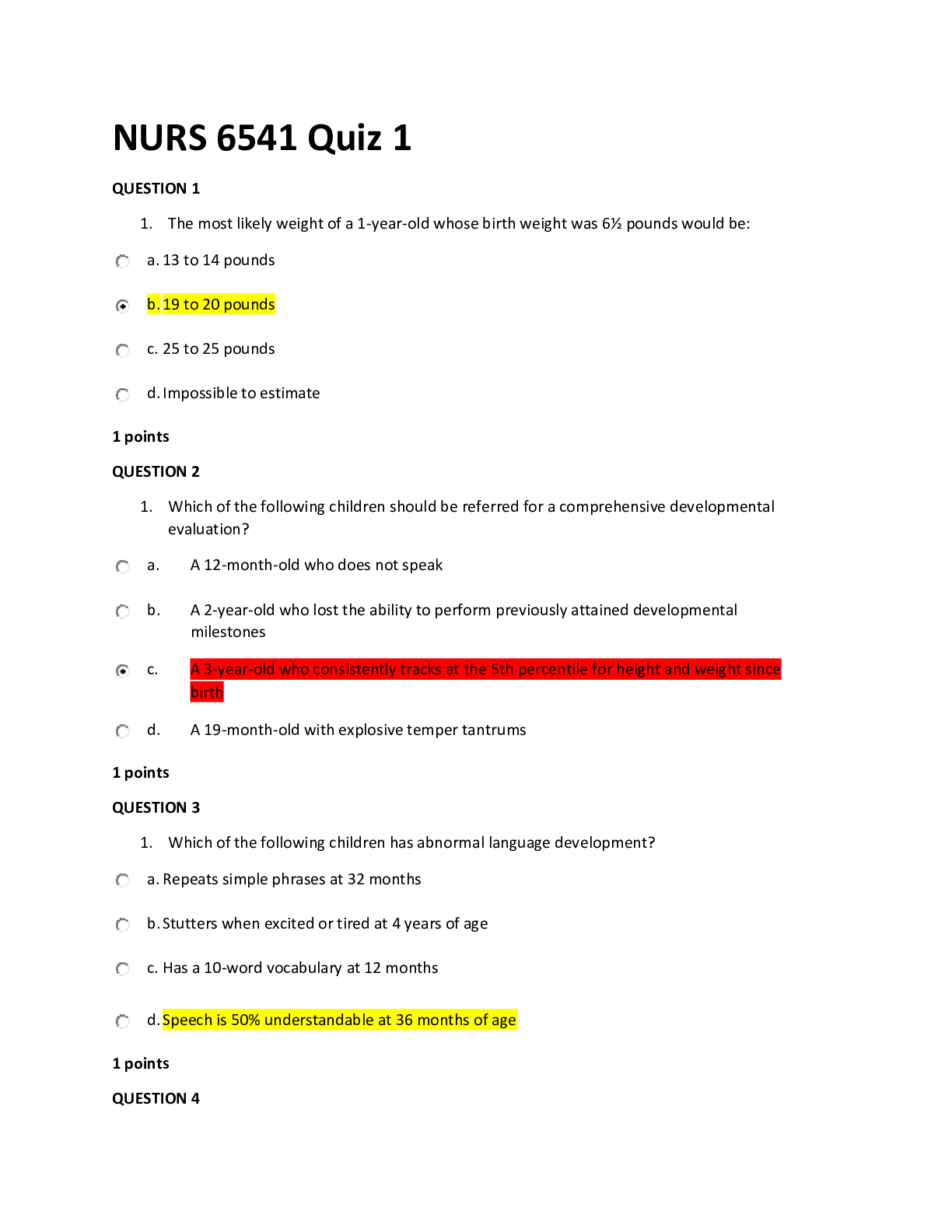
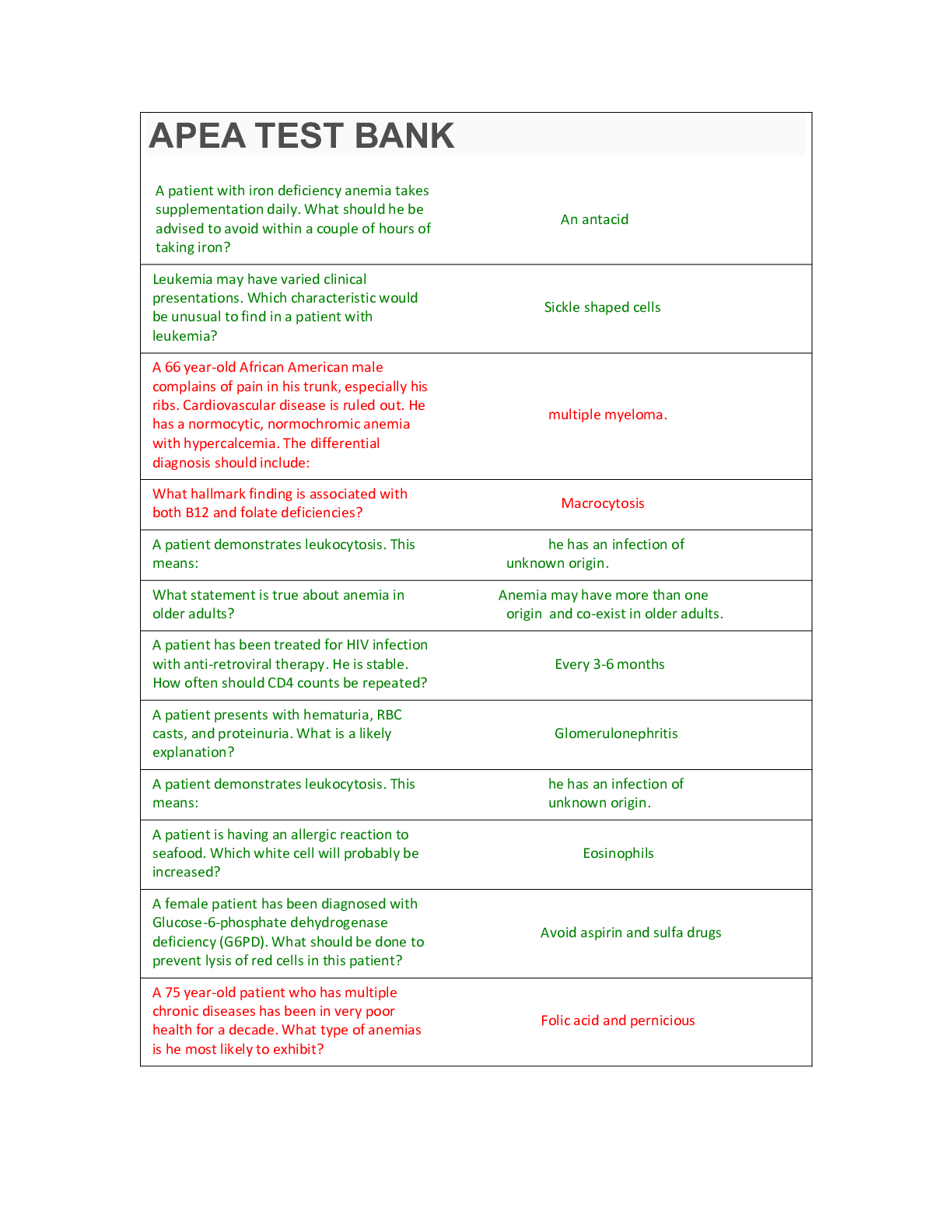
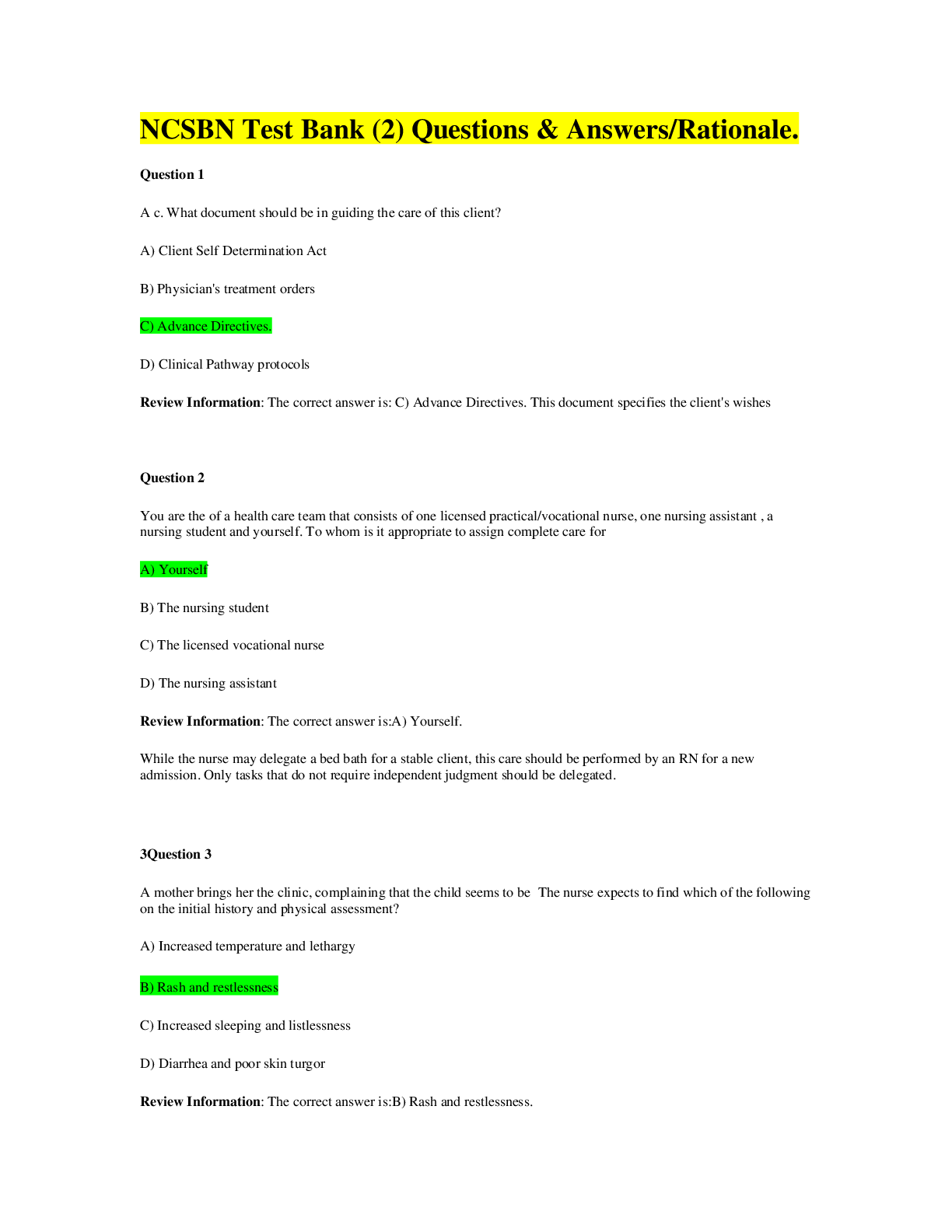
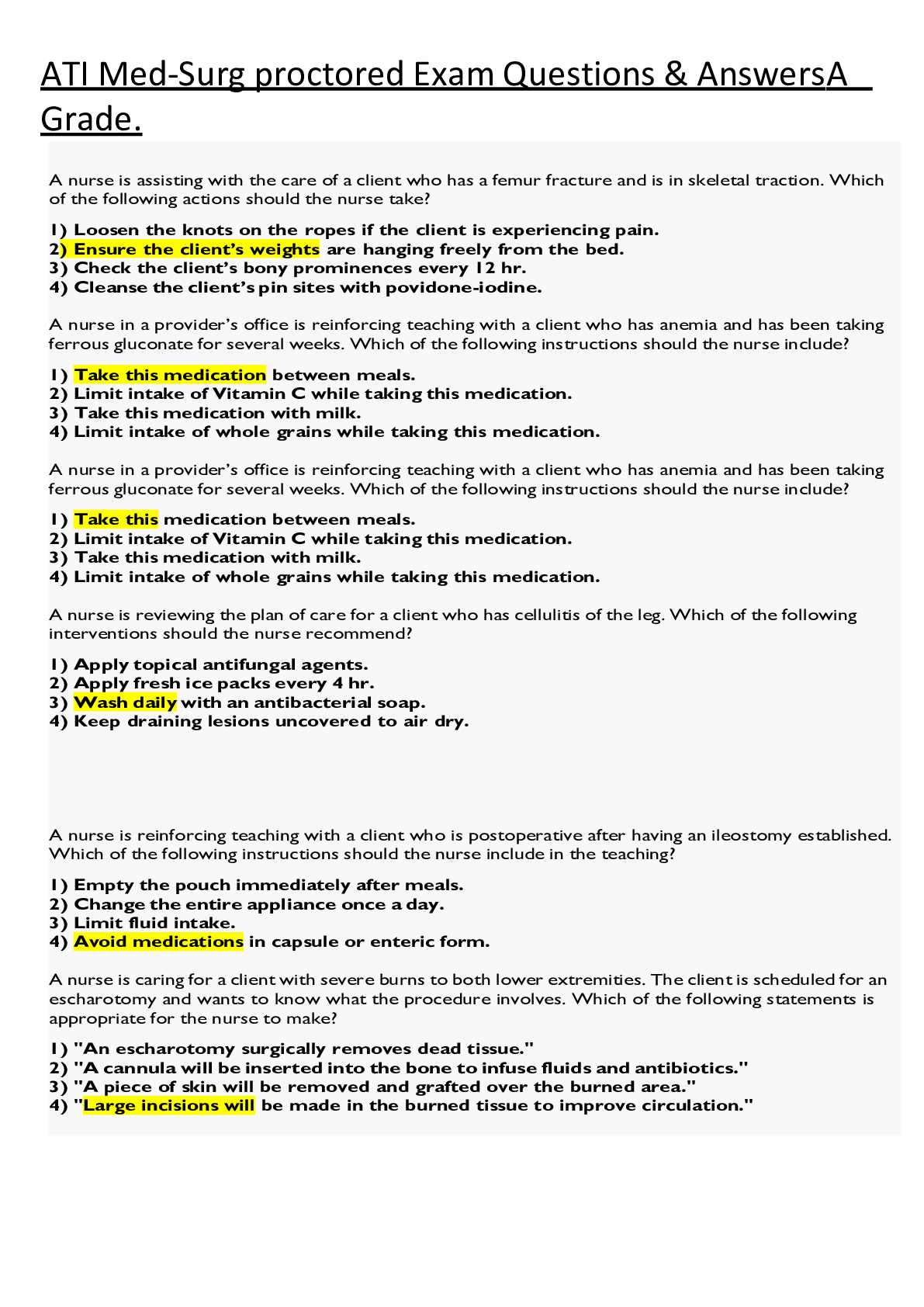
.png)
.png)