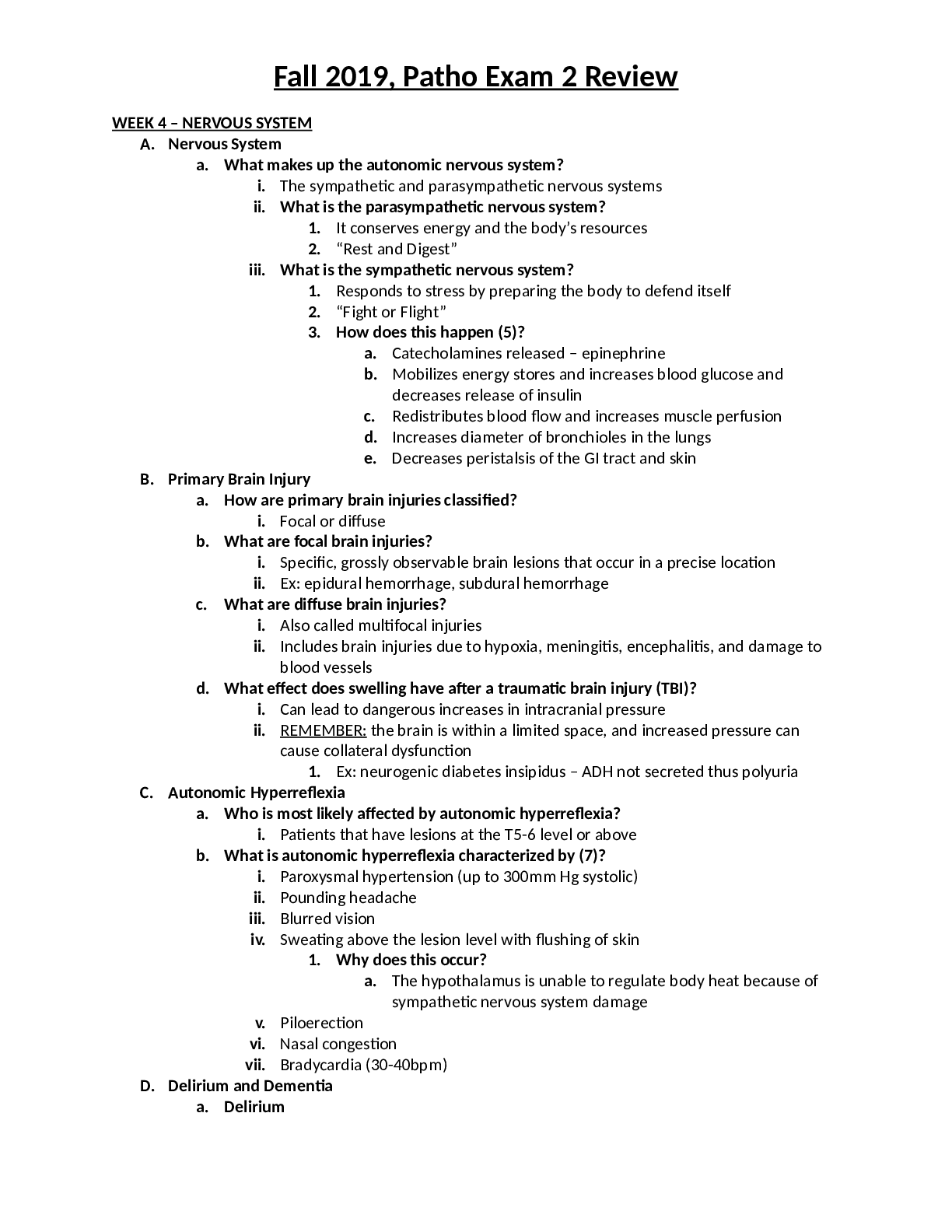
WEEK 4 – NERVOUS SYSTEM
A. Nervous System
a. What makes up the autonomic nervous system?
i. The sympathetic and parasympathetic nervous systems
ii. What is the parasympathetic nervous system?
1. It conserves energy
...
WEEK 4 – NERVOUS SYSTEM
A. Nervous System
a. What makes up the autonomic nervous system?
i. The sympathetic and parasympathetic nervous systems
ii. What is the parasympathetic nervous system?
1. It conserves energy and the body’s resources
2. “Rest and Digest”
iii. What is the sympathetic nervous system?
1. Responds to stress by preparing the body to defend itself
2. “Fight or Flight”
3. How does this happen (5)?
a. Catecholamines released – epinephrine
b. Mobilizes energy stores and increases blood glucose and
decreases release of insulin
c. Redistributes blood flow and increases muscle perfusion
d. Increases diameter of bronchioles in the lungs
e. Decreases peristalsis of the GI tract and skin
B. Primary Brain Injury
a. How are primary brain injuries classified?
i. Focal or diffuse
b. What are focal brain injuries?
i. Specific, grossly observable brain lesions that occur in a precise location
ii. Ex: epidural hemorrhage, subdural hemorrhage
c. What are diffuse brain injuries?
i. Also called multifocal injuries
ii. Includes brain injuries due to hypoxia, meningitis, encephalitis, and damage to
blood vessels
d. What effect does swelling have after a traumatic brain injury (TBI)?
i. Can lead to dangerous increases in intracranial pressure
ii. REMEMBER: the brain is within a limited space, and increased pressure can
cause collateral dysfunction
1. Ex: neurogenic diabetes insipidus – ADH not secreted thus polyuria
C. Autonomic Hyperreflexia
a. Who is most likely affected by autonomic hyperreflexia?
i. Patients that have lesions at the T5-6 level or above
b. What is autonomic hyperreflexia characterized by (7)?
i. Paroxysmal hypertension (up to 300mm Hg systolic)
ii. Pounding headache
iii. Blurred vision
iv. Sweating above the lesion level with flushing of skin
1. Why does this occur?
a. The hypothalamus is unable to regulate body heat because of
sympathetic nervous system damage
v. Piloerection
vi. Nasal congestion
vii. Bradycardia (30-40bpm)
D. Delirium and Dementia
a. Delirium
2
i. What age does delirium occur?
1. Usually older
ii. What is the onset?
1. Acute – most common during hospitalizations
iii. Are there any associated conditions (9)?
1. UTI
2. Thyroid disorders
3. Hypoxia
4. Hypoglycemia
5. Toxicity
6. Fluid-electrolyte imbalance
7. Renal insufficiency
8. Trauma
9. Multiple medications
iv. What is the course?
1. Fluctuating; remits with treatment
v. What is the duration?
1. Hours to weeks
vi. How is the patient’s attention?
1. Impaired
vii. How is their sleep-wake cycle?
1. Disrupted
viii. How is their alertness and orientation?
1. Impaired
ix. What is their behavior like?
1. Agitated, withdrawn/depressed
x. What is their speech like?
1. Incoherent
2. Can be rapid or slowed
xi. What are their thoughts like?
1. Disorganized with delusions
xii. What are their perceptions like?
1. Hallucinations/illusions
b. Dementia
i. What age does dementia occur?
1. Usually older
ii. What is the onset?
1. Usually insidious
2. Acute in some cases of strokes/trauma
iii. Are there any associated conditions (9)?
1. May have no other conditions
2. Brain trauma
iv. What is the course?
1. Chronic slow decline
v. What is the duration?
1. Months to years
vi. How is the patient’s attention?
1. Intact early
3
2. Often impaired late
vii. How is their sleep-wake cycle?
1. Usually normal or fragmented
viii. How is their alertness?
1. Normal
ix. How is their orientation?
1. Intact early
2. Impaired late
x. What is their behavior like?
1. Intact early
xi. What is their speech like?
1. Word-finding problems
xii. What are their thoughts like?
1. impoverished
xiii. What are their perceptions like?
1. Usually intact early
E. Alzheimer’s Disease
a. What is Alzheimer’s Disease
i. The leading cause of dementia
ii. One of the most common causes of severe cognitive dysfunction in older adults
iii. Late onset causes about 90%
b. What are risk factors of Alzheimer’s?
i. Greatest risk factors are age and family history
ii. Other risk factors: diabetes, hypertension, hyperlipidemia, obesity, smoking,
depression, cognitive inactivity or low education attainment, female gender,
estrogen deficit at the time of menopause, physical inactivity, head trauma,
elevated serum homocysteine and cholesterol levels, oxidative stress, and
neuroinflammation
c. What is the cause of AD?
i. Exact cause is unknown and no real understanding of disease process
ii. Early onset familial AD is autosomal dominant
1. What gene defects are linked to AD (3)?
a. Amyloid precursor protein (APP) on chromosome 21
b. Presenilin 1 (PSEN1) on chromosome 14
c. PSEN2 on chromosome ___
d. How is AD diagnosed?
i. FIRST, rule out ALL other causes of dementia
F. Stroke
a. What is the incidence of stroke?
i. Two times higher in blacks than whites
ii. Tends to run in families
b. What is the most common type or stroke?
i. Ischemic – thrombotic or embolic
1. What is the diagnostic cause?
a. No identifiable cause established by conventional diagnostics
and are classified as “undetermined” or “cryptogenic”
c. What are possible outcomes of stroke?
i. The mildest outcome can be almost unnoticed
4
ii. The most severe outcomes include hemiplegia, coma, and death
d. How are strokes classified?
i. According to pathology
1. Ischemic – thrombotic or embolic
2. Global hypoperfusion – as in shock
3. Intracerebral hemorrhage
e. What is the most commonly involved artery?
i. Middle cerebral artery
f. What is the single greatest risk factor for stroke?
i. Uncontrolled hypertension
g. What are other risk factors for stroke (13)?
i. Insulin resistance and diabetes mellitus
ii. High total cholesterol or low high-density lipoprotein (HDL) cholesterol level,
elevated lipoprotein-A level
iii. Hyperhomocysteinemia
iv. Congestive heart disease and peripheral vascular disease
v. Asymptomatic carotid stenosis
vi. Polycythemia and thrombocytopenia
vii. Atrial fibrillation
viii. Postmenopausal hormone therapy
ix. High sodium intake, low potassium intake
x. Smoking
xi. Physical inactivity
xii. Obesity
xiii. Chronic sleep deprivation
G. Guillain-Barre Syndrome (GBS)
a. What is GBS?
i. An autoimmune disease triggered by a preceding bacterial or viral infection
b. What are first manifestations?
i. Numbness, pain, paresthesias, or weakness in the limbs
c. How do motor signs manifest?
i. As an acute or subacute progressive paralysis
ii. Proximal muscles may be involved earlier and more significantly than distal
muscles
iii. Paresis/paralysis may be present in an ascending pattern involving limbs,
respiratory muscles, and bulbar muscles
d. How does weakness progress?
i. Usually plateaus or improves by the 4th week in 90% of cases
1. After plateau, strength improves over a period of days to months, with
the majority reaching levels similar to their pre-disease state
ii. Respiratory weakness leads to need for ventilator support in 10-30% of cases
iii. Cranial nerve weakness manifests as facial weakness and bulbar weakness in
chewing, swallowing, and coughing
H. Multiple Sclerosis
a. What is MS?
i. A chronic inflammatory disease involving degeneration of CAN myelin, scarring
or formation of plaque, and loss of axons
5
b. What is the cause of MS?
i. An autoimmune response to self-antigens in genetically susceptible individuals
c. What is the first demyelinating event?
i. AKA “clinically isolated syndrome”
ii. A single episode of neurologic dysfunction lasting greater than 24 hours that can
be a prelude to MS
d. Are there replases or remissions?
i. Initially, 90% present with remissions and exacerbations
ii. 10% present with a primary progressive course
iii. 90% will develop a progressive course 10-20 years after onset
iv. Once walking problems develop, progression occurs quickly regardless of type
I. Myasthenia Gravis
a. What is MG?
i. A chronic autoimmune disease mediated by acetylcholine receptor (AchR)
antibodies that act at the neuromuscular junction
b. What is the onset?
i. Typically insidious
c. What do clinical manifestations begin?
i. May first appear during pregnancy, postpartum period
ii. In conjunction with administration of certain anesthetic agents
d. What are hallmark symptoms (2)?
i. Exertional fatigue
ii. Weakness that worsens with activity, improves with rest, and recurs with
resumption of activity
e. What are typical complaints?
i. Fatigue after exercise
ii. Recent history of recurring upper respiratory tract infections
f. What muscles are affected?
i. Muscles of the eyes, face, mouth, throat, and neck are affected first
ii. What muscles are most affected?
1. Extraocular muscles and levator muscles
2. What are manifestations of this (3)?
a. Diplopia
b. Ptosis
c. Ocular palsies
iii. What muscles are next most involved?
1. Muscles of facial expression, mastication, swallowing, and speech
g. What are later signs of disease progression?
i. Respiratory distress and difficulty breathing
J. Parkinson’s Disease
a. What is the pathogensis of PD?
i. Unknown
ii. Several genes have been identified
iii. What is the primary pathology?
1. Degeneration of basal ganglia (corpus striatum, globus pallidus,
subthalamic nucleus, substantia nigra)
iv. What are hallmark pathologic features?
1. Loss of dopaminergic pigmented neurons
6
2. Dopamine loss includes: brainstem, thalamus, and cortex
b. What are classic motor manifestations (5)?
i. Resting tremor
ii. Pill-rolling tremors
iii. Bradykinesia/akinesia (poverty of movement)
iv. Rigidity (muscle stiffness)
v. Postural abnormalities
c. What is the characteristic appearance?
i. Wide-eyes, unblinking, staring expression with facial muscles smoothed out and
almost immobile
ii. Saliva frequently drools
iii. Skin of face is frequently greasy
iv. Gait is pathognomonic: individual walks with slow, short, shuffling steps; arms
are flexed, abducted, and held stiffly at side; and trunk is bent slightly forward
1. Person may break into a run spontaneously or when pushed forward or
backward
v. Tendency is to fall to the side
d. What are some of the most common depressing symptoms (3)?
i. Postural instability
ii. Sleep disorders
iii. Difficulty concentrating
K. Pain
a. Acute Pain
i. What is a characteristic experience?
1. An event
ii. What is the source of pain?
1. External agent or internal disease usually known
iii. What is the onset?
1. Usually sudden
iv. What is the duration?
1. Transient but up to 6 months
v. What are the clinical signs (5)?
1. Increased pulse rate
2. Elevated blood pressure
3. Increased respiratory rate
4. Diaphoresis
5. Dilated pupils
vi. What is the clinical course?
1. Suffering but usually decreases over time
vii. What is the prognosis?
1. Likelihood of eventual complete relief
b. Chronic Pain
i. What is a characteristic experience?
1. A situation; state of existence
ii. What is the source of pain?
1. Unknown
2. If known, treatment is prolonged or ineffective
7
iii. What is the onset?
1. May be sudden or develop insidiously
iv. What is the duration?
1. Prolonged and persistent (months to years)
v. What are the clinical signs?
1. Response patterns vary
2. Fewer overt signs (adaptation)
vi. What is the clinical course?
1. Suffering usually increases over time
vii. What is the prognosis?
1. Complete relief usually not possible
c. Neuropathic Pain
i. What is neuropathic pain?
1. Chronic pain initiated or caused by a primary lesion or dysfunction in the
nervous system and leads to long-term changes in pain pathway
structures (neuroplasticity) and abnormal processing of sensory
information
ii. What happens to the pain experienced?
1. It is amplified without stimulation by injury or inflammation
iii. How is it described?
1. Burning, shooting, shock-like, or tingling
iv. What are the characteristics?
1. Hyperalgesia
2. Increased sensitivity to a normally painful stimulus (touch, pressure,
pinprick, cold, and heat)
3. Allodynia – the induction of pain by normally nonpainful stimuli
L. Headaches
a. Migraine (with or without aura)
i. What is the age of onset?
1. Childhood, adolescence, or young adulthood
ii. What is the common gender affected?
1. Female
iii. Is there a family history of headaches?
1. Yes
iv. What is the onset and evolution?
1. Slow to rapid
v. What is the time course?
1. Episodic
vi. What is the quality?
1. Usually throbbing
vii. What is the location?
1. Variable, often unilateral
viii. Are there any associated features (2)?
1. Prodrome
2. Vomiting
b. Cluster headache/Proximal hemicrania
i. What is the age of onset?
1. Young adulthood, middle age
[Show More]