NURS 200 Final Exam Review
1. Know hand hygiene pg. 612 (no matter how old always use hand hygiene)
• #1 way to prevent infection, always use hand hygiene before patient contract (no matter the age)
2. Know standard p
...
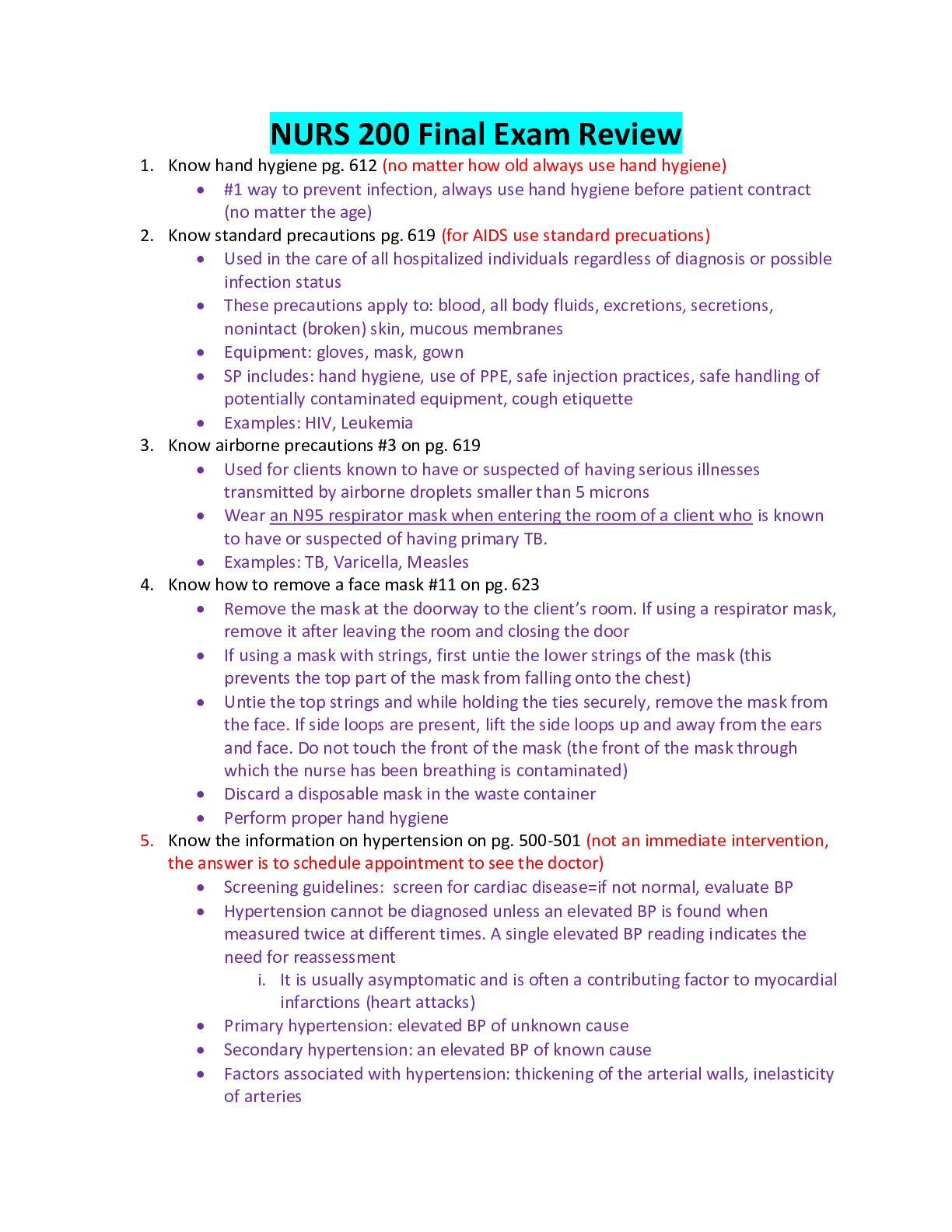
NURS 200 Final Exam Review
1. Know hand hygiene pg. 612 (no matter how old always use hand hygiene)
• #1 way to prevent infection, always use hand hygiene before patient contract (no matter the age)
2. Know standard precautions pg. 619 (for AIDS use standard precuations)
• Used in the care of all hospitalized individuals regardless of diagnosis or possible infection status
• These precautions apply to: blood, all body fluids, excretions, secretions, nonintact (broken) skin, mucous membranes
• Equipment: gloves, mask, gown
• SP includes: hand hygiene, use of PPE, safe injection practices, safe handling of potentially contaminated equipment, cough etiquette
• Examples: HIV, Leukemia
3. Know airborne precautions #3 on pg. 619
• Used for clients known to have or suspected of having serious illnesses transmitted by airborne droplets smaller than 5 microns
• Wear an N95 respirator mask when entering the room of a client who is known to have or suspected of having primary TB.
• Examples: TB, Varicella, Measles
4. Know how to remove a face mask #11 on pg. 623
• Remove the mask at the doorway to the client’s room. If using a respirator mask, remove it after leaving the room and closing the door
• If using a mask with strings, first untie the lower strings of the mask (this prevents the top part of the mask from falling onto the chest)
• Untie the top strings and while holding the ties securely, remove the mask from the face. If side loops are present, lift the side loops up and away from the ears and face. Do not touch the front of the mask (the front of the mask through which the nurse has been breathing is contaminated)
• Discard a disposable mask in the waste container
• Perform proper hand hygiene
5. Know the information on hypertension on pg. 500-501 (not an immediate intervention, the answer is to schedule appointment to see the doctor)
• Screening guidelines: screen for cardiac disease=if not normal, evaluate BP
• Hypertension cannot be diagnosed unless an elevated BP is found when measured twice at different times. A single elevated BP reading indicates the need for reassessment
i. It is usually asymptomatic and is often a contributing factor to myocardial infarctions (heart attacks)
• Primary hypertension: elevated BP of unknown cause
• Secondary hypertension: an elevated BP of known cause
• Factors associated with hypertension: thickening of the arterial walls, inelasticity of arteries
• Lifestyle factors: smoking, obesity, heavy alcohol consumption, lack of physical exercise, high blood cholesterol levels, stress
6. Know table 29-4 on pg. 501 priority risk factor (know the numbers of hypertension)
• Normal: <120 mmHg systolic and <80 mmHg diastolic
• Prehypertensive: 120-139 mmHg systolic or 80-89 mmHg diastolic
• Hypertension stage 1: 140-159 mmHg systolic or 90-99 mmHg diastolic
• Hypertension Stage 2: >160 mmHg systolic or >100 mmHg diastolic
7. Know how age and temperature are related on pg. 479 #1 Age (know that factors that affect body temp is age)
• Infants are greatly influenced by the temperature of the environment and must be protected from extreme changes
• Children’s temperatures vary more than those of adults do until puberty
• Many older people, particularly those over 75 years, are at risk of hypothermia (temperatures below 36 degrees Celsius or 96.8 degrees Fahrenheit)
i. For a variety of reasons such as: inadequate diet, loss of subcutaneous fat, lack of activity, reduced thermoregulatory efficiency
ii. Older adults are also particularly sensitive to extremes in the environmental temperature due to decreased thermoregulatory controls
8. What tasks can be delegated to a UAP?
• Never assessment, education, teaching, medication
• Pick the answer that does not have the above mentioned
9. Know hearing aids, skill 33-7 #1 on pg. 705 (help them be as independent as possible)
• Prior to performing the procedure, introduce self and verify the client’s identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how he or she can participate
• Always give freedom to patient and encourage as much independence as possible
10. Know partial bed bath pg. 675 (what to do for partial bed bath and who gets a partial bed bath)
• Also known as “abbreviated bath”
• Only the parts of the client’s body that might cause discomfort or odor, if neglected, are washed: the face, hands, axillae, perineal area, and back
i. Omitted from the bath: arms, chest, abdomen, legs, and feet
ii. The nurse provides this care for dependent clients and assists self-sufficient clients confined to bed by washing their backs
iii. Some ambulatory clients prefer to take a partial bath at the sink. The nurse can assist them by washing their backs
• Used for patients who are dependent clients, and self-sufficient clients who are confined to the bed
11. Know practice guidelines for bed making on pg. 709 (used linens do not go on the ground)
• Wear gloves while handling a client’s used bed linen. Linens and equipment that have been soiled with secretions and excretions harbor microorganisms that can be transmitted to others directly or by the nurse’s hands or uniform. Wash hands after removing gloves
• Hold soiled linen away from uniform
• Linen for one client is never placed on another client’s bed
• Place soiled linen directly in a portable linen hamper or tucked into a pillow case at the end of the bed before it is gathered up for disposal
• Do not shake soiled linen in the air because shanking can disseminate secretions and excretions and the microorganisms they contain
• When stripping and making a bed, conserve time and energy by stripping and making up one side as much as possible before working on the other side
• To avoid unnecessary trips to the linen supply area, gather all linen before starting to strip a bed
12. Know client teaching related to skin rashes on pg. 684 (read options very carefully)
• Keep the area clean by washing it with a mild soap. Rinse the skin well and pat it dry
• To relieve itching, try a tepid bath or soak. Some over the counter preparations such as Caladryl lotion may help but should be used with full knowledge of the product
• Avoid scratching the rash to prevent inflammation, infection, and further skin lesions
• Choose clothing carefully. Too much can cause perspiration and aggravate a rash
• Keep site dry and do not rub, provide extra care and take time with rash site
13. Know attentive listening book 26-1 “E” on pg. 420 (the answer is maintaining eye contact)
• Maintain good eye contact. In north American culture, mutual eye contact, preferably at the same level, recognizes the other person and denotes willingness to maintain communication. Eye contact neither glares at nor stares down another but is natural. In other cultures, too much eye contact especially with someone in a position of authority is out of order.
14. Know table 26-1 on pg. 420, using silence (being silent allows the patient to collect their thoughts and feelings and put them into words)
• Accepting pauses or silences that may extend for several seconds or minutes without interjecting any verbal response
• Examples: sitting quietly (or walking with the client) and waiting attentively until the client is able to put thoughts and feelings into words
• Helps patient gather thoughts
15. Know stereotyping in Table 26-2 on pg. 422
• Offering generalized and oversimplified beliefs about groups of people that are based on experiences too limited to be valid. These responses categorize clients and negate their uniqueness as individuals
• Examples
i. “Two-year-olds are brats”
ii. “Women are complainers”
iii. “Men don’t cry”
iv. “Most people don’t have any pain after this type of surgery”
16. Table 26-1 on pg. 421 seeking clarification perception checking and seeking consensual validation (this will be a scenario that you will have to choose the seeking clarification comment form the scenario)
• Seeking clarification
i. A method of making the client’s broad overall meaning of the message more understandable. It is used when paraphrasing is more difficult or when the communication is rambling or garbled. To clarify the message, the nurse can restate the basic message or confess confusion and ask the client to repeat or restate the message. Nurses can also clarify their own message with statements
ii. Examples:
1. “I’m puzzled”
2. “Would you please say that again?”
3. “I meant this rather than that”
4. I’m not sure I understand that”
• Perception checking or seeking consensual validation
i. A method similar to clarifying that verifies the meaning of specific words rather than the overall meaning of a message
ii. Examples:
1. Client: “My husband never gives me any presents.”
2. Nurse: “You mean he has never given you a present for your birthday or Christmas?”
3. Client: “Well- not never. He does get me something for my birthday and Christmas, but he never thinks of giving me anything at any other time”
4. Nurse: “how dare he…..”
• Both are used to elicit more information from the client
17. Know open-ended questions pg. 420 Table 26-1 (knowing the type of technique, using silence and opened ended questions, and what technique is being used either using silence or the open ended questions)
• Asking broad questions that lead or invite the client to explore (elaborate, clarify, describe, compare, or illustrate) thoughts or feelings. Open-ended questions specify only the topic to be discussed and invite answers that are longer than one or two words
• Examples:
i. “I’d like to hear more about that”
ii. “Tell me more”
iii. “How have you been feeling lately?”
iv. “What is your opinion?”
v. “What brought you to the hospital?”
18. Know Ensuing confidentiality of computer records on pg. 222 (never ever share your password with anyone)
• The Security Rule of HIPAA became mandatory in 2005, this rule governs the security of electronic PHI (protected health information), ways to ensure the confidentiality and security of computerized records:
i. A personal password is required to enter and sign off computer filed. Do not share this password with anyone including other health team members
ii. After logging on, never leave a computer terminal unattended
iii. Do not leave client information displayed on the monitor where others may see it
iv. Shred all unneeded computer-generated worksheets
v. Know the facilities policy and procedure for correcting an entry error
vi. Follow agency procedures for documenting sensitive material such as a diagnosis of AIDS
vii. Information technology (IT) personnel must install a firewall to protect the server from unauthorized access.
19. Know SBAR Box 15-6 on pg. 238 (know that R stands for)
• S: Situation
i. State your name, unit, and client name
ii. Briefly state the problem
• B: Background
i. State client admission diagnosis and date of admission
ii. State pertinent medical history
iii. Provide brief summary of treatment to date
iv. Code status (if appropriate)
• A: Assessment
i. Vital signs
ii. Pain scale
iii. Is there a change from prior assessments?
• R: Recommendation
i. State what you would like to see done or specify that the care provider needs to come and assess the client
ii. Ask if health care provider wants to order any tests or medications
iii. Ask health care provider if she or he wants to be notified for any reason
iv. Ask, if no improvement, when you should call again
20. Know heart failure on pg. 1297 (left sided heart failure is failure of the lungs –respiratory system)
• May develop if the heart is unable to keep up with the body’s need for oxygen and nutrients to the tissues. Heart failure usually occurs because of MI but it may also result from chronic overwork of the heart such as in clients with uncontrolled hypertension or extensive arteriosclerosis. If left-sided heart failure the vessels of the pulmonary system become congested or engorged with blood. This may cause fluid to escape into the alveoli and interfere with gash exchange, a condition known as pulmonary edema
• S/S
i. Pulmonary congestion: adventitious lung sounds
ii. SOB
iii. Dyspnea on exertion (DOE)
iv. S3 heart sound
v. Increased respiratory rate
vi. Nocturia
vii. Orthopnea
viii. Distended neck veins
• Gender and Race disparities: African Americans experience symptoms of heart failure (HF) earlier possibly because of the higher rate of uncontrolled hypertension. African Americans have higher BMI than Caucasians due to their views on body size (larger the body the more it is valued positively)
21. Know assessing the heart #6 on pg. 564 (mitral value)
• S1: heart loudest in mitral area (5th intercostal space, Left mid-clavicular line)
• Assessment
i. Auscultate the heart in all four anatomic sites: aortic, pulmonic, tricuspid, and apical (mitral)
ii. Auscultation need to be limited to these areas; however, the nurse may need to move the stethoscope to find the most audible sounds for each client
1. Eliminate all sources of room noise (heart sounds are of low intensity and other noise hinders the nurse’s ability to hear them)
2. Keep the client in a supine position with head elevated 15-45 degrees
3. Use both the diaphragm and the bell to listen to all areas
4. In every area of auscultation, distinguish both S1 and S2 sounds
5. When auscultating, concentrate on one particular sound at a time in each area; the first heart sound followed by systole and then the second heart sound then diastole. Systole and diastole are normally silent intervals
6. Later reexamine the heart while the client is in the upright sitting position (certain sounds are more audible in certain positions)
iii. Normal Findings
1. S1: usually heart at all sites, usually louder at apical (mitral) area
2. S2: usually hear at all sites, usually louder at base of heart
3. Systole: silent interval; slightly shorter duration than diastole at normal heart rate (60-90 BPM)
4. Diastole: silent interval: slightly longer duration than systole at normal heart rates
5. S3 in children and young adults
6. S4 in many older adults
iv. Deviations from normal
1. Increased or decreased intensity
2. Varying intensity with different beats
3. Increased intensity at aortic area
4. Increased intensity at pulmonic area
5. Sharp-sounding ejection clicks
6. S3 in older adults
7. S4 may be a sign of hypertension
22. Know impaired tissue perfusion physical assessment on pg. 1298 (know the bullet points)
• Atherosclerosis is the most common cause of impaired blood flow to organs and tissues. As vessels narrow and become obstructed, distal tissues receive less blood, oxygen, and nutrients
i. Any artery in the body may be affected by atherosclerosis however the effects are most associated with coronary arteries, vessels supplying blood to the brain and arteries in peripheral tissues
ii. Partial obstruction of coronary arteries causes myocardial ischemia often resulting in angina pecotris; if the obstruction is complete a heart attack (MI) occurs.
iii. Partial obstruction of cerebral vessels may cause a TIA; if the obstruction is complete, a stroke occurs.
iv. Peripheral vascular disease leads to ischemia of distal tissues such as legs and feet
1. Gangrene and amputation may result
• Ischemia: lack of blood supply due to obstructed circulation
• S/S of impaired peripheral arterial circulation in the legs and feet
i. Decreased peripheral pulses
ii. Pain or paresthesia
iii. Pale skin color (pallor)
iv. Cool extremities
v. Decreased hair distribution
• Risk factors for peripheral atherosclerosis
i. Smoking
ii. Obesity
iii. Hypertension
iv. Diabetes
• On the venous side
i. Incompetent valves may allow blood to pool in veins causing edema and decreasing venous return to the heart. Veins can also become inflamed, reducing blood flow and increasing the risk of thrombus (clot) formation
ii. Thrombi can break free and become emboli which can occlude blood supply to the capillaries.
23. Know a priority assessment if someone has numbness in their fingers or toes pg. 1299 (check circulation and pulse r/t peripheral circulation)
• Check pulses and circulation
• Examine the cardiovascular system
i. BP in both arms (should be within 10mmHg of each other)
ii. Palpate peripheral pulses for strength and equality
iii. Apical pulse auscultated for rate, rhythm, and quality of the heart
iv. Assess skin for color, temperature, hair distribution
v. Clients with extensive peripheral vascular disease may have cool feet with weak pulses, and shiny, hairless shins and feet; Pitting edema of feet and ankles may be noted with clients with heart failure
vi. Interview: past or current cardiovascular problems & Medical history, lifestyle habits (smoking, drinking, recreational drug use)
24. What would a patient be at risk for if they would be receiving fluids and not eating? (fluid retention and imbalance)
• Fluid retention and imbalances
25. Know that a least invasive task that does not require an assessment can be delegated to a UAP (assisting with pt meals / feeling)
• Sitting patient up in bed, ambulating with patient
26. Skin fold measurements on pg. 1146 (must be months to years)
• Anthropometric measurement
• Months years rather than days weeks
• Changes in anthropometric measurements occur slowly and reflect chronic rather than acute changes in nutritional status. They are used to monitory client’s progress for months to years. Ideally, initial and subsequent measurements need to be taken by the same clinician. Measurements obtained need to be interpreted with caution. Fluctuations in hydration status that often occur during illness can influence the accuracy of results. Normal standards often do not account for normal changes in body composition such as those that occur with aging
27. What is a priority of the nurse if a patient is not tolerating a tube feeding? (the patient has a tube and suction and their stomach hurts, so check the equipment to make sure it is working properly)
• Stop feeding and check the machine for malfunctions
28. Know Lifespan considerations bullet 6 on pg. 528 (check skin turgor on sternum and clavicle for older adults)
• Due to the normal loss of peripheral skin turgor in older adults, assess for hydration by checking skin turgor over the sternum or clavicle
29. Know table 30-8 on pg. 557 (know crackles)
• Crackles: fine, short, interrupted crackling sounds; alveolar rales are high pitched. Sound can be simulated by rolling a lock of hair near the ear. Best heard on inspiration but can be heard on both inspiration and expiration. May not be cleared by coughing
• Cause: air passing through fluid or mucus in any air passage
• Location: most commonly heard in the bases of the lower lung lobes
30. What class of medications could decrease respiratory rate (answer is a narcotic do not pick digoxin)
• Narcotics: opioids: pain medication
31. Know what to teach a patient about the use of an incentive spirometer pg. 1254 (explain the purpose of the activity/ therapy)
• AKA sustained maximal inspiration devices (SMIs): measure the flow of air inhaled through the mouthpiece and are used to:
i. Improve pulmonary ventilation
ii. Counteract the effects of anesthesia or hypoventilation
iii. Loosen respiratory secretions
iv. Facilitate respiratory gaseous exchange
v. Expand collapsed alveoli
32. Know venturi mask pg. 1261
• Delivers oxygen concentrations varying from 24% to 40% or 50% at liter flows of 4 to 10 L/min
• The Venturi mask has wide-bore tubing and color-coded jet adapters that correspond to a precise oxygen concentration and liter flow.
i. For example, in some cases, a blue adapter delivers a 24% concentration of oxygen at 4L/min and a green adapter delivers a 35% concentration of oxygen at 8L/min. However, colors and concentrations may vary
ii. The nurse must find a mask of appropriate size. Limitations of masks include difficulty in achieving a proper fit and poor tolerance by some clients who may complain of feeling hot or “smoldering”
33. Know how to perform nasopharyngeal suctioning #8 on pg. 1270 (its going to ask you how long can you suction, the answer is 15 seconds)
• Apply your finger to the suction control port to start suction and gently rotate the catheter (gentle rotation of the catheter ensures that all surfaces are reached and prevents trauma to any one area of the respiratory mucosa due to prolonged suction)
• Apply suction for 5-10 seconds while slowly withdrawing the catheter, then remove your finger from the control and remove the catheter (intermittent suction reduces the occurrence of trauma or irritation to the trachea and nasopharynx)
• A suction attempt should last only 10-15 seconds (should not exceed 15 seconds) during this time, the catheter is inserted, the suction applied and discontinued, and the catheter removed.
34. Know the steps on inserting an oropharyngeal airway pg. 1265 #3 bullet point (know bullet points 3-7)
• Hold the lubricated airway by the outer flange, with the distal end pointing up or curved upward
35. Know the lifespan considerations on pg. 102: Assessing older adults’ section (asks about ADL’s since ADL’s are self care the answer is how well they perform self care)
• Assessing the functional levels of older adults on an ongoing basis will provide guidelines for detecting needs for special care, resources, and services. It helps to determine their level of independence and changes as they occur. The two most common assessments are to evaluate the following activities of daily living and instrumental activities of daily living
i. Activities of daily living: bathing, dressing, toileting, transferring, continence, feeding
ii. Instrumental activities of daily living: ability to use the telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medication, ability to handle finances
• Help the patient be as independent as possible
• ADLs= self-care
36. Know the musculoskeletal assessment on pg. 514 and what would not be normal (older patients have brand new symptoms)
• Normal: bilateral strength of pulses however in older adults this gets weaker due to decreased perfusion. Osteoarthritis is also considered normal in older adults
• Abnormal findings: make sure to document, report, and address abnormalities as found.
• Purposes of physical assessment
i. To obtain a baseline data about client’s functional abilities
ii. To supplement, confirm or refute data obtained in the nursing history
iii. To obtain data that will help establish nursing diagnoses and plans of care
iv. To evaluate the physiological outcomes of health care and thus the progress of a client’s health problem
v. To make clinical judgements about client’s health status
vi. To identify areas for health promotion and disease prevention
37. Know expressive aphasia pg. 581
• Any defects in or loss of the power to express oneself by speech, writing, or signs, or to comprehend spoken or written language due to disease or injury of the cerebral cortex is called aphasia.
• Categories of aphasia
i. Sensory or receptive aphasia: the loss of the ability to comprehend written or spoken words
1. Auditory (acoustic) aphasia
a. Lost ability to understand the symbolic content associated with sounds
2. Visual aphasia
a. Lost ability to understand printed or written words
• Pick out patient that displays expressive aphasia
i. Motor or expressive aphasia involves loss of the power to express oneself by writing, making signs, of speaking. Clients may find that even though they can recall words, they have lost the ability to combine speech sounds into words
38. Know the home care considerations on pg. 1055 (2 questions) (the things that will help them stay safe the most) (the things that will cause the most harm to them)
• When making a home visit assess carefully for safety issues concerning ambulation. Counsel the client and family about inadequate lighting, unfastened rugs, slippery floors, and loose objects on the floors
• Check the surroundings for adequate supports such as railings and grab bars
• Recommend that nonskid strips be placed on outside steps and inside stairs that are not carpeted
• Ask to see the shoes the client intends to wear while ambulating. They should be in good repair and should support the foot
39. Know the home care considerations related to applying restraints on pg. 665 (know bullet point 2 for restraints)
• Restraints may be necessary for clients in wheelchairs or in the home. Safety guidelines apply in all cases. Assess the knowledge and skill of all caregivers in the use of restraints and educate as indicated
i. Use means other than restraints as much as possible, and stay with the client
ii. Pad bony prominences, such as wrists and ankles, if needed before applying a restraint over them
iii. Tie restraints with knots that will not tighten when pulled and to parts of the wheelchair that do not move and release quickly in case of emergency
iv. Assess restrained limbs for signs of impaired blood circulation
v. Always stay with
[Show More]