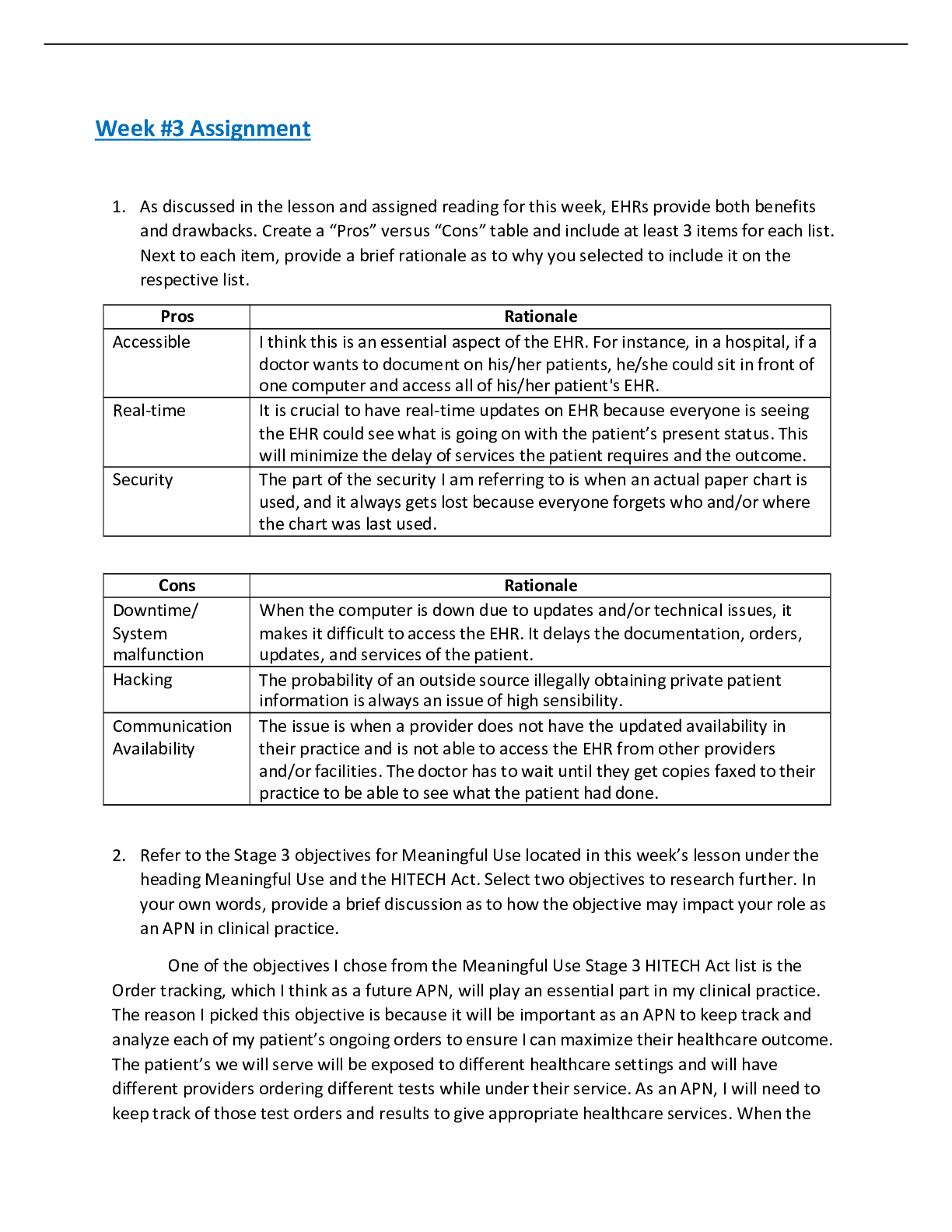
Acute Abdominal pain
History of Present Illness
Miss. JR, 47-year-old female complains of generalized abdominal pain with diarrhea that started 3 days ago. The patient has been able to eat, with some nausea afterwards
...
Acute Abdominal pain
History of Present Illness
Miss. JR, 47-year-old female complains of generalized abdominal pain with diarrhea that started 3 days ago. The patient has been able to eat, with some nausea afterwards and he states that the pain is a 5/10 today but has been as much as 9/10 when it first started. He has not taken any medications because he did not know what to take.
PMH: HTN, Diabetes, and hx of GI bleed 4 years ago Allergies: NKDA
Current Medications: Lisinopril 10mg, Amlodipine 5 mg, Metformin 1000mg, Lantus 10 units QHS. Family History: No hx of colon cancer, Father hx DMT2, HTN, Mother hx HTN, Hyperlipidemia, GERD. Social: Denies tobacco use; occasional EtOH, married, 3 children (1 girl, 2 boys).
Required additional information:
When did the pain start? Was the onset sudden or gradual? Ans: Gradual pain 3 days ago Have you ever had this pain before? Ans: No
What makes the pain worse and what relieves the pain? Ans: When cough comes pain gets worse and rest relieves pain.
Is the pain radiating to anywhere? Ans: All over body.
Is it just nausea or you vomited in the 3 days? What is the color of the vomitus? Is pain occurring before or after vomiting? Ans: No vomiting.
When was your last bowel movement? Ans: Yesterday evening.
Do you have any diarrhea, constipation, abdominal distention, rectal bleeding or any recent changes in bowel habits before?
Have you had any recent weight loss?
Do you have any cough or shortness of breath?
Review of Systems:
General: complaint of malaise and fever.
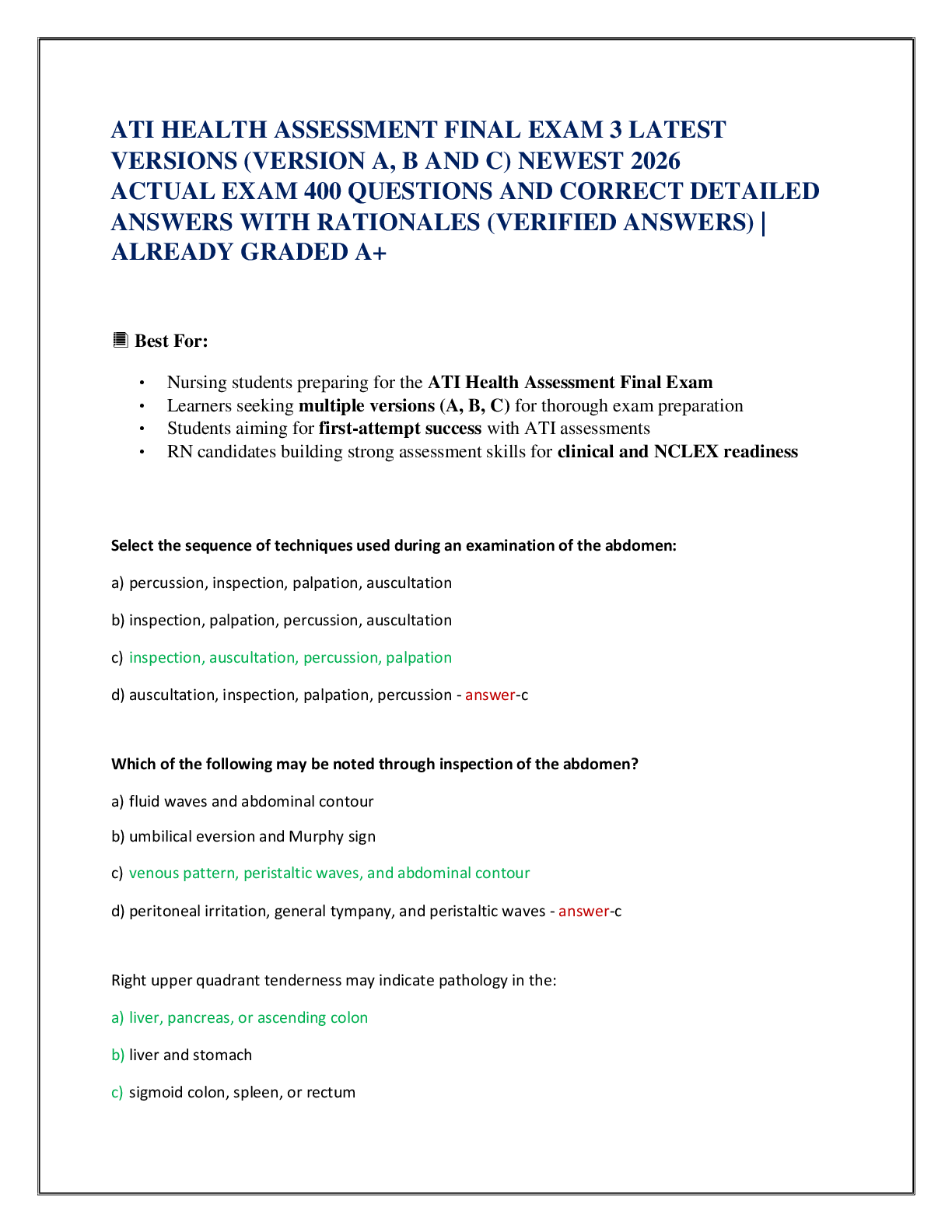
Gastrointestinal: Abdominal pain, nausea, vomiting, and anorexia. Abdomen is soft, hyperactive bowel sounds, pos pain in the LLQ
Genitourinary: Ask about urinary characteristics including color, frequency, volume congruent with fluid intake, force of stream and ability to empty the bladder (Ball et al.,2015).
Endocrine: Blood sugar 156mg/dl. Cardiovascular: normal heart rate, no murmur. Skin: Intact without lesions, no urticaria.
Lungs: CTA, chest wall symmetrical.
Objective data
Physical Exam:
Assess general appearance of patient and observe whether Miss. JR look sick. Check vital signs: Temp 99.8; BP 160/86; RR 16; P 92; HT 5’10”; WT 248lbs.
Observe abdominal musculature and note abdominal distention: Non-tender abdomen. Assess the exact location of pain: Left lower quartan.
Heart: RRR, no murmurs.
Assess Lungs: CTA, chest wall
............................................................CONTINUED.............................................
[Show More]



.png)