*NURSING > EXAM > NURSING 428 Module 8 Exam 100 Questions and Answers {GRADED A} Solutions plus Rationales | Download (All)
NURSING 428 Module 8 Exam 100 Questions and Answers {GRADED A} Solutions plus Rationales | Download To Score A
Document Content and Description Below
Module 8 Exam 1.A nurse notes that the site of a client’s peripheral intravenous (IV) catheter is reddened, warm, painful, and slightly edematous near the insertion point of the catheter. On the ba... sis of this assessment, the nurse should take which action first? • Remove the IV catheter Correct • Slow the rate of infusion • Notify the health care provider • Check for loose catheter connections Rationale: Phlebitis is an inflammatory process in the vein. Phlebitis at an IV site may be indicated by client discomfort at the site or by redness, warmth, and swelling in the area of the catheter. The IV catheter should be removed and a new IV line inserted at a different site. Slowing the rate of infusion and checking for loose catheter connections are not correct responses. The health care provider would be notified if phlebitis were to occur, but this is not the initial action. 2. A nurse hangs a 500-mL bag of intravenous (IV) fluid for an assigned client. One hour later the client complains of chest tightness, is dyspneic and apprehensive, and has an irregular pulse. The IV bag has 100 mL remaining. Which action should the nurse take first? • Remove the IV • Sit the client up in bed • Shut off the IV infusion Correct • Slow the rate of infusion Rationale: The client’s symptoms are indicative of speed shock, which results from the rapid infusion of drugs or a bolus infusion. In this case, the nurse would note that 400 mL has infused over 60 minutes. The first action on the part of the nurse is shutting off the IV infusion. Other actions may follow in rapid sequence: The nurse may elevate the head of the bed to aid the client’s breathing and then immediately notify the health care provider. Slowing the infusion rate is inappropriate because the client will continue to receive fluid. The IV does not need to be removed. It may be needed to manage the complication. 3. A nurse discontinues an infusion of a unit of packed red blood cells (RBCs) because the client is experiencing a transfusion reaction. After discontinuing the transfusion, which action should the nurse take next? • Remove the IV catheter • Contact the health care provider Correct • Change the solution to 5% dextrose in water • Obtain a culture of the tip of the catheter device removed from the client Rationale: If the nurse suspects a transfusion reaction, the transfusion is stopped and normal saline solution infused at a keep-vein-open rate pending further health care provider prescriptions. The nurse then contacts the health care provider.. Dextrose in water is not used, because it may cause clotting or hemolysis of blood cells. Normal saline solution is the only type of IV fluid that is compatible with blood. The nurse would not remove the IV catheter, because then there would be no IV access route through which to treat the reaction. There is no reason to obtain a culture of the catheter tip; this is done when an infection is suspected. 4. The nurse determines that the client is exhibiting signs of a hemolytic transfusion reaction while receiving a blood transfusion. The nurse should perform these actions in which priority order? Arrange the actions in the order that they should be performed. All options must be used. The correct order is: 1. Stopping the infusion of blood 2. Hanging an IV bag of normal saline solution (NS) at a keep-vein-open (KVO) rate 3. Notifying the health care provider 4. Obtaining vital signs/oxygen saturation 5. Documenting the findings Rationale: If a transfusion reaction is suspected, the transfusion is immediately stopped and NS infused, pending further primary health care provider prescriptions. Ensuring patent IV access also helps maintain the client’s intravascular volume. NS is the solution of choice, rather than solutions containing dextrose, because red blood cells do not clump with NS. Next, the primary health care provider should be notified because this is an emergency situation. Vital signs and oxygen saturation are monitored closely. Finally, the nurse documents the findings and the client’s response to the interventions. 5.A client with heart failure is being given furosemide and digoxin. The client calls the nurse and complains of anorexia and nausea. Which action should the nurse take first? • Administer an antiemetic • Administer the daily dose of digoxin • Discontinue the morning dose of furosemide • Check the result of laboratory testing for potassium on the sample drawn 3 hours ago Correct Rationale: Anorexia and nausea are symptoms commonly associated with digoxin toxicity, which is compounded by hypokalemia. Early clinical manifestations of digoxin toxicity include anorexia and mild nausea, but they are frequently overlooked or not associated with digoxin toxicity. Hallucinations and any change in pulse rhythm, color vision, or behavior should be investigated and reported to the health care provider. The nurse should first check the results of the potassium level, which will provide additional when the nurse calls the health care provider, an important follow-up action. The nurse should also check the digoxin reading if one is available. The nurse would not administer an antiemetic without further investigating the client’s problem. Because digoxin toxicity is suspected, the nurse would withhold the digoxin until the health care provider has been consulted. The nurse would not discontinue a medication without a prescription to do so. 6. The health care provider (HCP) prescribes the administration of total parenteral nutrition (TPN), to be started at a rate of 50 mL/hr by way of infusion pump through an established subclavian central line. After the first 2 hours of the TPN infusion, the client suddenly complains of difficulty breathing and chest pain. The nurse should take which immediate action? • Obtain blood for culture • Clamp the TPN infusion line Correct • Obtain an electrocardiogram (ECG) • Obtain a sample for blood glucose testing Rationale: One complication of a subclavian central line is embolism, caused by air or thrombus. Sudden onset of chest pain shortly after the initiation of TPN may mean that this complication has developed. The infusion is clamped (the line should not be discontinued, however), the client turned on the left side with the head down, and the HCP notified immediately. Depending on agency protocol, the rapid response team would also be called. Blood cultures are not necessary in this situation, because infection is not the concern. Likewise, there is no useful reason for checking the blood glucose level. An ECG may be obtained, but this is not the immediate priority. If the client shows signs of an air embolism, the nurse should examine the catheter to determine whether an open port has allowed air into the circulatory system. 7. The health care provider prescribes 2000 mL of 5% dextrose and normal saline 0.45% for infusion over 24 hours. The drop factor is 15 gtt/mL. At how many drops per minute does the nurse set the flow rate? (Round to the nearest whole number). Correct Rationale: Use the IV flow rate formula: 8.A nurse is assessing a peripheral intravenous (IV) site and notes blanching, coolness, and edema at the insertion site. What should the nurse do first? • Remove the IV Correct • Apply a warm compress • Check for blood return • Measure the area of infiltration Rationale: Blanching, coolness, and edema of the IV site are all signs of infiltration. Because infiltration may result in damage to the surrounding tissue, the nurse must first remove the IV cannula to prevent any further damage. The nurse should not depend solely on the blood return for assurance that the cannula is in the vein, because blood return may be present even if the cannula is only partially in the vein. Compresses may be used, but the compress (warm or cool) depends on the type of solution infusing and health care provider preference. The nurse should measure the area of infiltration after the IV has been removed so that further tissue damage is prevented. 9.A home care nurse has been assigned a client who has been discharged home with a prescription for total parenteral nutrition (TPN). Which parameters does the nurse plan to check at each visit as a means of identifying complications of the TPN therapy? Select all that apply. • Weight Correct • Glucose test Correct • Temperature Correct • Peripheral pulses • Hemoglobin and hematocrit Rationale: When a client is receiving TPN therapy, the nurse monitors the client’s weight to determine the effectiveness of the therapy. The nurse should weigh the client at each visit to make sure that the client has not gained or lost an excessive amount of weight. Because the formula contains a large amount of dextrose, the health care provider should check the client’s glucose level frequently. The nurse caring for a client receiving TPN at home should also monitor the temperature to detect infection, which is a potential complication of this therapy. An infection in the intravenous line could result in sepsis, because the catheter is in a blood vessel. The peripheral pulses and hemoglobin and hematocrit readings may provide data but are unrelated to complications associated with TPN therapy. 10.A nurse is caring for a group of adult clients on an acute care nursing unit. Which clients does the nurse recognize as the most likely candidates for total parenteral nutrition (TPN)? Select all that apply. • A client with pancreatitis Correct • A client with severe sepsis Correct • A client with renal calculi • A client who has undergone repair of a hiatal hernia • A client with a severe exacerbation of ulcerative colitis Correct Rationale: TPN is indicated in the client whose gastrointestinal tract is not functional or who cannot tolerate an enteral diet for extended periods. The client with sepsis is very ill and may require TPN. Other candidates include clients who have undergone extensive surgery, sustained multiple fractures, or have advanced cancer or AIDS. The client who has undergone hiatal hernia repair is not a candidate, because this client would resume a normal diet within a relatively short period after the hernia repair. The client with renal calculi also is not a candidate because the client would be able to eat. 11.A client with a peripheral intravenous (IV) line in place has a new prescription for infusion of total parenteral nutrition (TPN), a solution containing 25% glucose. Which action should be taken by the nurse? • Hanging the IV solution as prescribed • Questioning the health care provider about the prescription Correct • Diluting the solution with sterile water to half-strength • Hanging the IV solution but setting the infusion at just half the prescribed rate Rationale: TPN solutions containing as much as 10% glucose can be infused through peripheral vessels. A TPN solution containing 25% glucose is hypertonic. The nurse should question the prescription in the absence of a central venous catheter or a peripherally inserted central catheter. Diluting the solution with sterile water to half-strength and hanging the IV solution as prescribed are both inappropriate. The nurse must not alter a prescribed solution independently. 12. The first bag of total parenteral nutrition (TPN) solution has arrived on the clinical unit for a client beginning this nutritional therapy. The solution is to be infused by way of a central line. Which essential piece of equipment should the nurse obtain before hanging the solution? • Pulse oximeter • Blood glucose meter • Electronic infusion device Correct • Noninvasive blood pressure monitor Rationale: The nurse obtains an electronic infusion device before hanging a TPN solution. Because of the high glucose load, it is necessary to use an infusion device to ensure that the solution does not infuse too rapidly or fall too far behind. Because the client’s blood glucose is checked every 6 to 8 hours during administration of PN, a blood glucose meter will also be needed, but it is not essential before the solution is hung. A noninvasive blood pressure cuff is unnecessary for this procedure. Although oxygen saturation is important, in this situation, it is not the most important equipment to use at this time. 13.A nurse is monitoring a client who is receiving total parenteral nutrition (TPN). Which t signs and symptoms causes the nurse to suspect that the client is experiencing hyperglycemia as a complication? • Pallor, weak pulse, and anuria • Nausea, vomiting, and oliguria • Nausea, thirst, and increased urine output Correct • Sweating, chills, and decreased urine output Rationale: The high glucose concentration in TPN puts the client at risk for hyperglycemia. Signs of hyperglycemia include polyuria, polydipsia, polyphagia, blurred vision, nausea and vomiting, and abdominal pain. The nurse checks the blood glucose level immediately if these symptoms develop. The signs and symptoms identified in the other options are unrelated to hyperglycemia. 14. At 1600 the nurse checks a client’s total parenteral nutrition (TPN) infusion bag and notes that the solution is running at a rate of 100 mL/hr. The bag was hung the previous day at 1800. The nurse plans to change the infusion bag and tubing this evening at what time? • 1700 • 1800 Correct • 2000 • 2100 Rationale: The TPN solution should be changed every 24 hours as a means of helping prevent infection. Infection is also prevented with the use of aseptic technique during bag and tubing changes. Most agencies recommend that tubing be changed every 24 hours along with the TPN infusion bag. Specific agency policies should always be followed. The nurse should also use a filter when administering TPN in accordance with hospital protocol. Therefore the remaining options are incorrect. 15.A nurse is changing the central line dressing of a client receiving total parenteral nutrition (TPN). The nurse notes moisture under the dressing covering the catheter insertion site. What should the nurse assess next? • Temperature • Time of the last dressing change • Expiration date on the infusion bag • Tightness of the tubing connections Correct Rationale: A loose tubing connection — the most obvious cause of the moisture that could be readily detected and fixed by the nurse — is the first thing the nurse should look for. The client’s temperature would be assessed if the nurse were looking for signs of infection. The expiration date on the infusion bag and the time of the last dressing change are routine observations but have nothing to do with the subject of the question. 16. A client receiving total parenteral nutrition (TPN) requires fat emulsion (lipids), which will be piggybacked to the TPN solution. On obtaining a bottle of fat emulsion, the nurse notes that fat globules are floating at the top of the solution. Which action should the nurse take? • Shake the bottle vigorously • Request a new bottle from the pharmacy Correct • Rotate the bottle gently back and forth to mix the globules • Run the bottle under warm water until the globules disappear Rationale: The nurse should not hang a fat emulsion that contains visible fat globules. Another bottle of solution should be obtained and used in its place. When TPN is combined with fat emulsion, the solution should not be used if there is a visible “ring” noted in the container of solution. The actions in the other options are incorrect. • 17.ID: 9476963029 A nurse is preparing a client for the insertion of a central intravenous line into the subclavian vein by the health care provider. The nurse gathers the equipment, places it at the bedside, and prepares to assist the health care provider with the procedure. As further preparation for the procedure, the nurse places the client in which position? • Flat on the left side • In the prone position • In the supine position • In a slight Trendelenburg position Correct Rationale: Unless contraindicated, the client is placed in a slight Trendelenburg position. This position is used to increase dilation of the veins and positive pressure in the central veins, reducing the risk of air embolus during insertion. Note that Trendelenburg position is contraindicated in clients with head injuries, increased intracrainial pressure, certain respiratory conditions, and spinal cord injuries. If the client had any of these conditions then an alternative position as prescribed would need to be used for insertion. The other options are incorrect because they will not achieve this goal. • 18.ID: 9476959516 A client is receiving total parenteral nutrition (TPN) with fat emulsion (lipids) piggybacked to the TPN solution. For which signs of an adverse reaction to the fat emulsion should the nurse monitor the client? Select all that apply. • Chills Correct • Pallor • Headache Correct • Chest and back pain Correct • Nausea and vomiting Correct • Subnormal temperature Rationale: Signs of an adverse reaction to fat emulsion include chest and back pain, chills, fever, dyspnea, cyanosis, diaphoresis, flushing, headache, nausea and vomiting, pressure over the eyes, vertigo, and thrombophlebitis at the infusion site. • 19.ID: 9476959599 The nurse is preparing to change the solution bag and intravenous tubing of a client receiving total parenteral nutrition (TPN) through a left subclavian central venous line. Which essential action does the nurse ask the client to perform just before switching the tubing? • Turn the head to the left • Turn the head to the right • Exhale slowly and evenly • Take a deep breath and hold it Correct Rationale: The nurse must ask the client to take a deep breath and hold it. This effectively achieves the Valsalva maneuver during tubing changes, which helps prevent air embolism. If the line is on the left, it may be helpful to have the client turn the head to the right and vice versa. This allows more room for the nurse to work. However, it is not the most essential action. The other options are incorrect. • 20.ID: 9476961270 A nurse suspects that a client receiving total parenteral nutrition (TPN) through a central line has an air embolism. The nurse immediately places the client in which position? • Left side with the head lower than the feet Correct • Left side with the head higher than the feet • Right side with the head lower than the feet • Right side with the head higher than the feet Rationale: When air embolism is suspected, the client should be placed in a left side–lying position with the head lower than the feet. This position is used to minimize the effect of the air traveling as a bolus to the lungs by trapping it in the right side of the heart. The positions in the other options are incorrect. 21.A nurse is making initial rounds on a group of assigned clients. Which client should the nurse see first? • A client receiving total parenteral nutrition (TPN) at a rate of 50 mL/hr for the last 24 hours • A client receiving TPN at a rate of 50 mL/hr whose temp was 99° F (37.2°C) on the previous shift • A client receiving TPN at a rate of 100 mL/hr who has complained of needing frequent trips to the bathroom to void • A client whose TPN solution was decreased to a rate of 25 mL/hr who is now complaining of weakness, headache, and sweating Correct Rationale: The nurse should assess the client complaining of weakness, headache, and sweating first, because these are signs of hypoglycemia, which could be caused by the decrease in the TPN rate. The client who has been receiving TPN at a rate of 50 mL/hr for the last 24 hours should be assessed but does not need to be seen first. The client who complains of frequent trips to the bathroom should be assessed for hyperglycemia, one of the side effects of TPN, but should not take precedence over the client showing signs of hypoglycemia. A client with an increased temperature should be monitored closely but does not take precedence over the client exhibiting signs of hypoglycemia. . • 22.ID: 9476964581 A nurse answers a call bell and finds that the total parenteral nutrition (TPN) solution bag of an assigned client is empty. The new prescription was written for a new bag at the beginning of the shift, but it has not yet arrived from the pharmacy. Which action should the nurse take first? • Call the health care provider • Call the pharmacy for further instructions • Hang a solution of 10% dextrose in water Correct • Hang a solution of 5% dextrose in 0.9% sodium chloride Rationale: The solution containing the highest amount of dextrose should be hung until the new bag of TPN becomes available. Because TPN solutions contain high glucose concentrations, the 10% dextrose solution is the best solution to infuse because it will minimize the risk of hypoglycemia. The pharmacy and health care provider should also be called, but care of the client is the immediate priority of the nurse. • 23.ID: 9476957513 A young female client with schizophrenia says to the nurse, “Since I started on olanzapine last year, I’m doing well in school and all, but I’ve gained so much weight, and it’s really bothering me. What can I do about this?” Which response by the nurse would be therapeutic? • “Well, I think you’re overreacting. Today people think they should be skinny- minnies, even though it’s not healthy.” • “Weight gain can be a side effect of the medication, so you need to watch your diet and exercise. How much weight have you gained?” Correct • “That medication isn’t any more likely to cause weight gain than the others you’re taking. Perhaps we could go over your diet and exercise habits.” • “I want you to stop taking this medication immediately, and I’m calling the doctor, because this is a very serious side effect and you may need dialysis.” Rationale: Olanzapine is an antipsychotic agent that causes weight gain, a disadvantage of the medication. Weight gain, especially in a young woman, for whom it may have an especially serious affect on self-image, may lead to noncompliance with the medication regimen. “That medication isn’t any more likely to cause weight gain than the others you’re taking” offers incorrect information. “I think you’re overreacting” minimizes the client’s complaints. “I want you to stop taking this medication immediately” gives incorrect information and is presented in an unprofessional style. • 24.ID: 9476961262 A client with schizophrenia has been taking an antipsychotic medication for 2 months. For which adverse effect should the nurse monitor the client closely? • Akathisia Correct • Pelvic thrusts • Athetoid limbs • Protruding tongue Rationale: Approximately 5 to 60 days after starting an antipsychotic medication, the client may exhibit the adverse effect of akathisia, manifested by motor restlessness (continually tapping a foot, rocking back and forth in a chair, or shifting weight from one foot to another). Pelvic thrusts, athetoid limbs, and a protruding tongue are effects that may occur after 6 to 24 months of an antipsychotic medication. . • 25.ID: 9476957544 A client with schizophrenia who has been taking an antipsychotic medication calls the clinic nurse and says, “I need to cancel my appointment with the psychiatrist again, because I still have this awful sore throat. It’s so bad that my mouth has a sore.” How does the nurse respond to the client? • “I wouldn’t be upset. It happens when you aren’t drinking enough water.” • “I think you need to come in for blood work today, because this may be an adverse effect of your medicine.” Correct • “Do you remember when you started this medication? Your psychiatrist told you how important it is to keep your appointments with him.” • “You probably have a simple flu, but it might help if you gargle with some antiseptic mouthwash every 2 hours or so and drink plenty of water.” Rationale: Agranulocytosis, an adverse effect of antipsychotic medications, is characterized by a sore throat with mouth sores, fever, and malaise. Any client taking such a medication who complains of flulike symptoms should be evaluated carefully. For this reason, the psychiatrist usually prescribes periodic blood tests while a client is taking antipsychotic medications. The incorrect options ignore the client’s complaints. • 26.ID: 9476967709 The client rings the call bell and complains of pain at the site of an IV infusion. The nurse assesses the site and determines that phlebitis has developed. Which actions should the nurse take? Select all that apply. • Removing the IV catheter at that site Correct • Applying warm, moist compresses to the IV site Correct • Notifying the health care provider about the finding Correct • Encouraging the client to scrub the site while in the shower • Starting a new IV line in a proximal portion of the same vein Rationale: The nurse should remove the IV from the phlebitic site and apply warm, moist compresses to the area to speed resolution of the inflammation and absorb the fluid from the tissues. The nurse also notifies the primary health care provider of this complication. The nurse should restart the IV line in a vein other than the one in which phlebitis has developed. The nurse should discourage the client from rubbing the site while in the shower, because this could cause sloughing of the tissue. 27.A nurse notes that the site of a client’s peripheral IV catheter is reddened, warm, painful, and slightly edematous in the area of the insertion site. After taking appropriate steps to care for the client, the nurse documents in the medical record that the client has experienced which problem? • Phlebitis of the vein Correct • Infiltration of the IV line • Hypersensitivity to the IV solution • An allergic reaction to the IV catheter material Rationale: Phlebitis at an IV site can be identified by client discomfort at the site, as well as by redness, warmth, and swelling in the area of the catheter. The IV should be removed and a new one inserted at a different site. The remaining options are incorrect. Coolness and swelling would be noted if infiltration had occurred. The symptoms of hypersensitivity and allergic reaction depend on whether these complications are local or systemic. . • 28.ID: 9476957517 A nurse has a written prescription to remove an intravenous (IV) line. Which item should the nurse obtain from the unit supply area for use in applying pressure to the site after removing the IV catheter? • Alcohol swab • Adhesive bandage • Sterile 2 × 2 gauze Correct • Povidone-iodine (Betadine) swab Rationale: A dry sterile dressing such as a 2 × 2 is used to apply pressure to the discontinued IV site. This material is absorbent, sterile, and nonirritating. An adhesive bandage may be used to cover the site once hemostasis has occurred. A povidone-iodine swab or alcohol swab would irritate the opened puncture site and would not stop the blood flow. • 29.ID: 9476961274 A client has just undergone insertion of a central venous catheter by the health care provider at the bedside. Which result would the nurse be sure to check before initiating infusion of the IV solution that the health care provider has prescribed? • Serum osmolality • Serum electrolytes • Portable chest x-ray Correct • Intake and output record Rationale: Before beginning the administration of any volume of IV solution through a central venous catheter, the nurse should determine whether the results of the chest x-ray reveal that the catheter is in the proper place. This is necessary to prevent inadvertent infusion of IV fluid into pulmonary or subcutaneous tissues. The other options are items that are useful for the nurse in the general care of the client, but they are not related to this procedure. • 30.ID: 9476970196 A nurse has obtained a unit of blood from the blood bank and properly checked the blood bag with another nurse. Which parameter should the nurse assess just before hanging the transfusion? • Skin color • Vital signs Correct • Latest platelet count • Urine output over the last 24 hours Rationale: A change in vital signs may indicate that a transfusion reaction is occurring. This is why the nurse assesses vital signs before the procedure, every 15 minutes for the first half-hour, and every half-hour thereafter. The other options do not need to be assessed just before the start of a transfusion. The nurse should be aware of fluid volume status, as well as weight to help identify fluid volume overload, but this is not the priority before start of a blood infusion. • 31.ID: 9476963068 A nurse has just received a prescription to transfuse a unit of packed red blood cells for an assigned client. For how long does the nurse plan to stay with the client after the unit of blood is hung? • 5 minutes • 15 minutes Correct • 45 minutes • 60 minutes Rationale: The nurse must remain with the client for the first 15 minutes of a transfusion, the time frame during which most transfusion reactions occur. This will enable the nurse to quickly detect a reaction and intervene quickly. Five minutes is too short; the nurse would not be present during the critical 15 minutes. Staying with the client for 45 or 60 minutes is unnecessary. • 32.ID: 9476957575 A client has a prescription for a unit of packed red blood cells (RBCs). Which IV solution should the nurse obtain to hang with the blood product at the client’s bedside? • 0.9% sodium chloride Correct • Lactated Ringer’s solution (LR) • 5% dextrose in 0.9% sodium chloride • 5% dextrose in water in 0.45% sodium chloride Rationale: Sodium chloride (normal saline, NS) 0.9% is an isotonic solution that is typically used both to precede and follow infusion of a blood product. Dextrose is not used because it could result in clumping and subsequent hemolysis of RBCs. LR is not the solution of choice for this procedure, even though it is an isotonic solution. • 33.ID: 9476964591 The health care provider prescribes 1000 mL of normal saline 0.45% for infusion over 8 hours. The drop factor is 10 gtt/mL. At how many drops per minute does the nurse set the flow rate? (Round to the nearest whole number). Correct Rationale: Use the IV flow rate formula: Formula: • 34.ID: 9476961213 A nurse discontinues an infusion of a unit of blood after the client experiences a transfusion reaction. Once the incident has been documented appropriately, where does the nurse send the blood transfusion bag? • Blood bank Correct • Risk management • Microbiology laboratory • Infection-control department Rationale: The nurse returns the transfusion bag, containing any remaining blood, to the blood bank. This allows the blood bank to perform any follow-up testing needed in the event of a documented transfusion reaction. The other options are incorrect because they do not handle post transfusion reaction procedures or testing. . • 35.ID: 9476963006 Packed red blood cells have been prescribed for a client with low hemoglobin and hematocrit values. The nurse takes the client’s temperature orally before hanging the blood transfusion and notes that it is 100.0° F (37.7 C). What should the nurse do next? • Call the health care provider Correct • Begin the transfusion as prescribed • Administer an antihistamine and begin the transfusion • Administer 2 tablets of acetaminophen and begin the transfusion Rationale: If the client has a temperature of 100.0° F (37.7 C) or higher, the unit of blood should not be hung until the health care provider has been notified and had the opportunity to give further prescriptions. It is likely that the health care provider will prescribe the blood to be administered despite the temperature, but it is not within the nurse’s scope of practice to make that determination. Therefore the other options are incorrect. Additionally, medications are not administered to the client without a prescription. • 36.ID: 9476961252 A nurse has just hung a transfusion of packed red blood cells and stayed with the client for the appropriate amount of time. Before leaving the room, the nurse tells the client that it is most important to immediately report which specific signs if it occurs? Select all that apply. • Rash Correct • Chills Correct • Fatigue • Backache Correct • Tiredness Rationale: The nurse should instruct the client to report signs of a transfusion reaction, such as a backache, chills, itching, or rash, immediately. If a transfusion reaction occurs, the nurse would stop the transfusion immediately. Fatigue and tiredness are not specifically related to a transfusion reaction. • 37.ID: 9476961290 At 1300, the nurse is documenting the receipt of a unit of packed blood cells at the hospital blood bank. The nurse calculates that the transfusion must be started by which time? • 1315 • 1330 Correct • 1345 • 1400 Rationale: Blood must be hung within 30 minutes after obtaining it from the blood bank. After that time, the temperature of the blood becomes warm and could be unsafe for use. Therefore 1345 and 1400 are incorrect. It is not necessary to hang the blood within 15 minutes of receiving it from the blood bank. • 38.ID: 9476959502 A client who needs to receive a blood transfusion has experienced a pruritic rash during previous transfusions. The client asks the nurse whether it is safe to receive the transfusion. Which medication does the nurse anticipate will most likely be prescribed before the transfusion? • Ibuprofen • Acetaminophen • Diphenhydramine Correct • Acetylsalicylic acid Rationale: An urticarial reaction is characterized by a rash accompanied by pruritus. This type of transfusion reaction is prevented by pretreating the client with an antihistamine, such as diphenhydramine. Acetaminophen and acetylsalicylic acid are analgesics; ibuprofen is a nonsteroidal antiinflammatory medication. The health care provider prescribes 1000 mL of 5% dextrose in water to be infused over 8 hours. The drop factor is 15 gtt/mL. At how many drops per minute does the nurse set the flow rate? (Round to the nearest whole number). Correct Rationale: Use the IV flow rate formula: . • 40.ID: 9476967788 The health care provider prescribes an intramuscular dose of 200,000 units of penicillin G benzathine for an adult client. The label on the 10-mL ampule sent from the pharmacy reads, “Penicillin G benzathine,300,000 units/mL.” How many milliliters of medication does the nurse prepares to ensure administration of the correct dose? (Round to the nearest tenth.) Correct • 41.ID: 9476964522 The health care provider’s prescription for an adult client reads, “Potassium chloride 15 mEq by mouth.” The label on the medication bottle reads, “20 mEq potassium chloride/15 mL.” How many milliliters of KCl does the nurse prepare to ensure administration of the correct dose of medication? (Round to the nearest whole number.) Correct Rationale: Use the medication formula: • 42.ID: 9476961236 The health care provider prescribes 1000 mL of 5% dextrose in water, to be infused over 24 hours. The drop factor is 60 gtt/mL. At how many drops per minute does the nurse set the flow rate? (Round to the nearest whole number). Correct Rationale: Use the IV flow rate formula: . • 43.ID: 9476959549 The health care provider’s prescription reads, “Clindamycin phosphate 0.3 g in 50 mL NS, to be administered IV over 30 minutes.” The medication label reads, “Clindamycin phosphate 150 mg/mL.” How many milliliters of medication does the nurse prepare to ensure that the correct dose is administered? Correct Rationale: Convert 0.3 g to milligrams: 1000 mg = 1 g and therefore 0.3 g = 300 mg. Next, use the medication formula: . • 44.ID: 9476970182 The health care provider’s prescription reads, “Phenytoin 0.1 g by mouth twice daily.” The medication label indicates that the bottle contains 100-mg capsules. How many capsules does the nurse prepare for administration of one dose? Correct Rationale: Convert 0.1 g to milligrams: 1000 mg = 1 g; therefore 0.1 g = 100 mg. Next use the medication formula: • 45.ID: 9476959572 A nurse is preparing a plan of care for a client who will be receiving meperidine hydrochloride. Which side/adverse effects does the nurse make a note of needing to be alert to in the plan of care? Select all that apply. • Hypotension Correct • Constipation Correct • Bradycardia • Urine retention Correct • Respiratory depression Correct Rationale: Side/adverse effects of meperidine hydrochloride respiratory depression, orthostatic hypotension, tachycardia, drowsiness and mental clouding, constipation, and urine retention. • 46.ID: 9476957583 A nurse is preparing a plan of care for a client with a diagnosis of cancer who is receiving morphine sulfate for pain. Which action does the nurse identify as a priority in the plan of care for this client? • Monitoring urine output • Encouraging increased fluids • Monitoring the client’s temperature • Monitoring the client’s respiratory rate Correct Rationale: Morphine sulfate suppresses respiration, and monitoring respirations is a priority nursing action. Although the other options may be a component of the plan of care for this client, monitoring the client’s respiratory rate is the priority nursing action. • 47.ID: 9476964563 A client who has been taking lisinopril complains to the nurse of a persistent dry cough. What should the nurse tell the client? • This is a side effect of therapy Correct • He probably has an upper respiratory infection • He needs to have his blood counts checked • A chest x-ray is required because the cough is a sign of heart failure Rationale: One common side effect of therapy with any of the angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril, is a persistent dry cough. The cough generally does not improve while the client is taking the medication. Clients are advised to notify the health care provider if the cough becomes troublesome to them. The cough is reversible with discontinuation of the therapy. The other options are incorrect interpretations of the client’s complaint. • 48.ID: 9476961266 A client has been given a prescription to begin using nitroglycerin transdermal patches for the management of angina pectoris. What should the nurse tell the client about the medication? • Place the patch in the area of a skin fold to promote adherence • Apply the patch at the same time each day and leave it in place for 12 to 16 hours as directed Correct • If the patch becomes dislodged, do not reapply and wait until the next day to apply a new patch. • Alternate daily dose times between the morning and the evening to prevent the development of tolerance to the medication Rationale: Nitroglycerin is a coronary vasodilator used in the management of angina pectoris. The client is generally advised to apply a new patch at the same time each day (usually each morning) and leave in place for 12 to 16 hours as per health care provider directions. This prevents the client from developing tolerance (such as that which happens with 24-hour use). The client should avoid placing patches in skin folds or excoriated areas. The client benefits from removing the patch for sleep as well, because the nitroglycerin may cause a headache, which could disrupt sleep. The client may apply a new patch if the old one is dislodged, because the dose is released continuously in small amounts through the skin. • 49.ID: 9476970178 A client with newly diagnosed angina pectoris has taken 2 sublingual nitroglycerin tablets for chest pain. The chest pain is relieved, but the client complains of a headache. What should the nurse tell the client? • This is an indication that the medication should not be used again • Headache indicates medication tolerance, and the dosage must be increased • This may be an allergic reaction to the nitroglycerin, and the health care provider must be notified • This is an expected side effect of the nitroglycerin, and the client can relieve it by taking acetaminophen Correct Rationale: Headache is a frequent side effect of nitroglycerin, a result of the vasodilating action of the medication. Headaches, which may be treated effectively with the use of acetaminophen, usually diminish in frequency as the client becomes accustomed to the medication. The other options are incorrect. • 50.ID: 9476970192 A client has been taking metoprolol. Which finding indicates to the nurse that the medication is effective? • The client’s ankles are swollen. • The client’s weight has increased. • The client’s blood pressure has decreased. Correct • The client has wheezes in the lower lobes of the lungs. Rationale: Metoprolol is a cardioselective beta-blocking agent used after myocardial infarction, as well as for hypertension and angina. Side/adverse effects include bradycardia and such symptoms of heart failure as weight gain and increased edema. . • 51.ID: 9476970174 A nurse has taught a client taking a methylxanthine bronchodilator about beverages that must be avoided. Which beverage choices by the client indicate to the nurse that the client needs further education? Select all that apply. • Cocoa Correct • Coffee Correct • Lemonade • Orange juice • Chocolate milk Correct Rationale: Cola, coffee, and chocolate contain xanthine and should therefore be avoided by the client taking a methylxanthine bronchodilator, because they will enhance the effects of the medication, increasing the likelihood of cardiovascular and central nervous system side/adverse effects. Lemonade and orange juice are acceptable choices. • 52.ID: 9476972011 A client taking hydrochlorothiazide reports to the clinic for follow-up blood tests. For which side/adverse effect of the medication does the nurse monitor the client’s laboratory results? • Hypokalemia Correct • Hypocalcemia • Hypernatremia • Hypermagnesemia Rationale: The client taking a potassium-losing diuretic such as hydrochlorothiazide must be monitored for reductions in the potassium level. Other fluid and electrolyte imbalances that may occur with use of this medication are hyponatremia, hypercalcemia, hypomagnesemia, and hypophosphatemia. The nurse should also educate the client about foods that are rich in potassium. • 53.ID: 9476970145 A nurse has taught a client who is taking lithium carbonate about the medication. The nurse determines that the client needs additional teaching if the client makes which comment to the nurse? • The medication should be taken with meals • The lithium blood levels must be monitored very closely • It is important to decrease fluid intake while taking the medication to avoid nausea Correct • The health care provider must be called if excessive diarrhea, vomiting, or diaphoresis occurs Rationale: Because the therapeutic and toxic dosage ranges are so close, the blood level of lithium in a client taking the medication must be monitored closely; assessments are performed frequently at first and every several months after that. The client should be instructed to stop taking the medication if excessive diarrhea, vomiting, or diaphoresis occurs and to inform the health care provider if any of these problems develops. Lithium is irritating to the gastric mucosa; therefore lithium should be taken with meals. A normal diet and normal salt and fluid intake (1500 to 3000 mL/day of fluid) should be maintained, because lithium decreases sodium reabsorption in the renal tubules, which may result in sodium depletion. Low sodium intake causes an increase in lithium retention and could lead to toxicity. • 54.ID: 9476967714 A nurse is developing a plan of care for a client, hospitalized with heart failure, who has a history of Parkinson disease and is taking benztropine mesylate daily. Which intervention does the nurse identify as a priority in the plan? • Monitoring intake and output Correct • Monitoring the client’s pupillary response • Placing the client in a right side-lying position • Checking the client’s hemoglobin level daily Rationale: Urine retention is a side effect of benztropine mesylate. The nurse must be alert for infrequent voiding of small amounts, which may be indicative of urine retention, dysuria, abdominal distention, or overflow incontinence. This monitoring is also an important intervention for the client with heart failure. Monitoring pupillary response and checking the client’s hemoglobin level daily are not interventions specific to this medication. The client with heart failure is placed in an upright position to facilitate breathing. • 55.ID: 9476964528 A nurse is providing instructions to a client regarding quinapril hydrochloride. The nurse should teach the client to implement which measure? • To take the medication with meals • To rise slowly from a lying to a sitting position Correct • To discontinue the medication if nausea occurs • That a therapeutic effect will be felt immediately Rationale: Quinapril hydrochloride is an angiotensin-converting enzyme (ACE) inhibitor used in the treatment of hypertension. The client should be instructed to rise slowly from a lying to a sitting position and to permit the legs to dangle from the bed momentarily before standing to reduce the hypotensive effect. The medication does not need to be taken with meals. It may be given without regard to food. If nausea occurs, the client should be instructed to drink a noncola carbonated beverage and eat some salted crackers or dry toast. The full therapeutic effect may take place in 1 to 2 weeks. • 56.ID: 9476959557 Methylergonovine intramuscularly is prescribed for a postpartum client. Before administering the medication, the nurse explains to the client that the medication will promote which effect? • Reduce lochial drainage • Prevent postpartum bleeding Correct • Maintain a normal blood pressure • Decrease the strength of uterine contractions Rationale: Methylergonovine, an ergot alkaloid /oxytocic agent, is used to prevent or control postpartum hemorrhage by inducing uterine contraction and enhancing myometrial tone. The immediate dose is usually administered intramuscularly, and then, if needed, the medication is given again by mouth. Methylergonovine increases the strength and frequency of contractions and may increase blood pressure. One priority before the administration of methylergonovine is assessment of the client’s blood pressure. There is no relationship between the action of this medication and lochial drainage. • 57.ID: 9476957528 Carbamazepine is prescribed for a client with trigeminal neuralgia. Which side/adverse effects does the nurse instruct the client to report to the health care provider? Select all that apply. • Fever Correct • Nausea • Headache • Sore throat Correct • Mouth sores Correct Rationale: Drowsiness, headache, nausea, and vomiting are frequent side effects of carbamazepine. Adverse reactions include blood dyscrasias; fever, sore throat, mouth ulcerations, unusual bleeding or bruising, or joint pain may be indicative of a blood dyscrasia, and the health care provider should be notified. • 58.ID: 9476964506 Disulfiram is prescribed for a client. Which questions does the nurse make a priority of asking the client before administering this medication? Select all that apply. • “When did you have your last full meal?” • “Do you have a history of diabetes insipidus?” • “When was your last drink of alcohol?” Correct • “Do you have a history of thyroid problems?” Correct • “Do you have a history of cancer in your family?” Rationale: Disulfiram is used as an adjunct treatment for selected clients with alcoholism who want to remain in a state of enforced sobriety. Clients must abstain from alcohol intake for at least 12 hours before the initial dose of the medication is administered. The most important question is when the client had his last drink of alcohol. The medication is used with caution in clients with diabetes mellitus, hypothyroidism, epilepsy, cerebral damage, nephritis, and hepatic disease. It is also contraindicated in cases of severe heart disease, psychosis, or hypersensitivity to the medication. • 59.ID: 9476964558 A nurse is assessing a client who is being hospitalized with a diagnosis of pneumonia. The client’s husband tells the nurse that the client is taking donepezil hydrochloride. The nurse should ask the husband about the client’s history of which disorder? • Dementia Correct • Seizure disorder • Diabetes mellitus • Posttraumatic stress disorder Rationale: Donepezil hydrochloride is a cholinergic agent that is used in the treatment of mild to moderate dementia of the Alzheimer type. It enhances cholinergic function by increasing the concentration of acetylcholine, slowing the progression of Alzheimer disease. The disorders in the other options are not treated with this medication. • 60.ID: 9476967730 Fluoxetine hydrochloride is prescribed for a client, and the nurse provides instruction regarding the use of the medication. The nurse tells the client that it is best to take the medication at what time? • At lunchtime • In the morning Correct • With the evening meal • Midafternoon, with an antacid Rationale: Fluoxetine hydrochloride is a selective serotonin reuptake inhibitor that elicits an antidepressant response. It is best administered in the early morning, and there is no need to coordinate the dose with a meal. (If the medication causes lightheadedness or dizziness, the healthcare provider may advise the client to take it at bedtime.) The other options are incorrect. • 61.ID: 9476964511 A nurse is teaching a client how to mix regular and NPH insulin in the same syringe. The nurse should provide the client with which information about the insulin? • Keep insulin refrigerated at all times • Draw the regular insulin into the syringe first Correct • Shake the NPH insulin bottle before mixing the two types • Remove all of the air from the bottle before mixing the two types Rationale: Before different types of insulin are mixed, the bottle should be rotated for at least one minute between the hands. This resuspends the insulin and helps warm the medication. The bottles should not be shaken; shaking causes the formation of bubbles, which may trap particles of insulin and alter the dosage of the medication. Insulin may be maintained at room temperature. A 25- to 28-gauge 5/8-inch (1.6 cm) needle should be used for subcutaneous injection of insulin. Bottles of insulin intended for future use should be stored in the refrigerator. Regular insulin is drawn up before NPH insulin to ensure that there is no contamination of the rapid-acting insulin by the intermediate-acting insulin. It is not necessary to remove air from the insulin bottle. • 62.ID: 9476964518 A nurse provides instructions to a client who will be taking furosemide. Which statement by the client indicates to the nurse that the client needs additional instruction? • “I need to sit or stand up slowly.” • “I need to maintain my fluid intake.” • “This medication will make me urinate.” • “I should expect to have ringing in my ears.” Correct Rationale: Furosemide is a loop diuretic. Adverse effects of furosemide therapy include orthostatic hypotension and ototoxicity. Therefore the client should change positions slowly to help prevent lightheadedness. The client must also contact the health care provider if signs of ototoxicity, such as hearing loss or ringing in the ears, occur. Fluid intake should be maintained to prevent dehydration. • 63.ID: 9476957539 A client is receiving heparin sodium by way of continuous IV infusion. For which adverse effects of the therapy does the nurse assess the client? Select all that apply. • Tinnitus • Tarry stools Correct • Slowed pulse • Bleeding from the gums Correct • Increased blood pressure Rationale: Heparin is an anticoagulant, and the client who receives continuous IV heparin is at risk for bleeding. The nurse must be alert for signs of bleeding: bleeding from the gums, ecchymoses on the skin, cloudy or pink-tinged urine, tarry stools, and body fluids that test positive for occult blood. • 64.ID: 9476967737 A client has a prescription for short-term therapy with enoxaparin . The nurse explains to the client that this medication is being prescribed for which purpose? • Prevent pain • Relieve back spasms • Increase the client’s energy level • Reduce the risk of deep vein thrombosis Correct Rationale: Enoxaparin is an anticoagulant that is administered to prevent deep vein thrombosis and thromboembolism in selected at-risk clients. It is not used to prevent pain, relieve back spasms, or increase the energy level. • 65.ID: 9476963055 Metoprolol has been prescribed for a client with hypertension. For which common side effects of the medication does the nurse monitor the client? Select all that apply. • Fatigue Correct • Dry eyes • Weakness Correct • Impotence Correct • Nightmares Rationale: One common side effect of beta-adrenergic–blocking agents, such as metoprolol, is impotence. Fatigue and weakness are also common. Rarer central nervous system side effects include mental status changes, nervousness, depression, and insomnia. Altered taste, dry eyes, and nightmares are rare side effects. . • 66.ID: 9476964597 A client with HIV infection has been started on therapy with zidovudine. The nurse tells the client to report to the laboratory in 3 months for testing to detect adverse effects of the therapy. Which laboratory test is most important to monitor for this client? • Creatinine • Serum potassium • Blood urea nitrogen (BUN) • Complete blood count (CBC) Correct • 67.ID: 9476959537 A nurse is reading the medical record of a client receiving haloperidol. The nurse notes that the health care provider has documented that the client is experiencing signs of akathisia. On the basis of the health care provider’s note, which clinical manifestation would the nurse expect to find during assessment of the client? • Motor restlessness Correct • Puffing of the cheeks • Puckering of the mouth • Protrusion of the tongue Rationale: Akathisia —motor restlessness, or the desire to keep moving —may appear within 6 hours of administration of the first dose of haloperidol. It may be difficult to distinguish from psychotic agitation. Tardive dyskinesia is uncontrolled rhythmic movements of the mouth, face, and extremities, including lip smacking or puckering, puffing of the cheeks, uncontrolled chewing, and rapid or wormlike movements of the tongue. The health care provider should be notified if any of these symptoms occurs. • 68.ID: 9476964554 Phenelzine sulfate is being administered to a client with depression. The client suddenly complains of a severe frontally radiating occipital headache, neck stiffness and soreness, and vomiting. On further assessment, the client exhibits signs of hypertensive crisis. Which medication should the nurse prepare to administer, anticipating that it will be prescribed as the antidote to treat phenelzine-induced hypertensive crisis? • Phentolamine Correct • Acetylcysteine • Protamine sulfate • Calcium gluconate Rationale: The antidote to treat phenelzine-induced hypertensive crisis is phentolamine. Hypertensive crisis may manifest as hypertension, frontally radiating occipital headache, neck stiffness and soreness, nausea, vomiting, sweating, fever and chills, clammy skin, dilated pupils, and palpitations. Tachycardia or bradycardia and constricting chest pain may also be present. • 69.ID: 9476964515 Risperidone is prescribed for a client with a diagnosis of schizophrenia. Which laboratory study does the nurse expect to see among the health care provider’s prescriptions? • Platelet count • Creatinine level Correct • Sedimentation rate • Red blood cell count Rationale: Baseline assessment includes renal and liver function parameters. Risperidone is used with caution — often at a reduced dosage — in clients with renal or hepatic impairment, clients with underlying cardiovascular disorders, and in older or debilitated clients. The laboratory tests identified in the other options are not necessary. • 70.ID: 9476963078 Betaxolol eye drops have been prescribed for the treatment of a client’s glaucoma. The nurse tells the client to return to the clinic for follow-up for which purpose? • To have weight checked • To give a sample for urinalysis • To have the blood glucose level checked • For measurement of blood pressure and apical pulse Correct Rationale: Betaxolol is an antiglaucoma medication and a beta-adrenergic blocker. Hypotension (manifested as dizziness), nausea, diaphoresis, headache, fatigue, constipation, and diarrhea are side/adverse effects of the medication. Nursing interventions include blood pressure monitoring to detect hypotension and assessment of the pulse for strength, weakness, irregularity, and bradycardia. Blood glucose testing is not a part of follow-up with this medication; neither are weighing and urinalysis. 71. Intravenous tobramycin sulfate is prescribed for a client with a respiratory tract infection. For which of the following symptoms, indicative of an adverse effect, does the nurse monitor the client? ▪ Nausea ▪ Vertigo Correct ▪ Vomiting ▪ Hypotension Rationale: Ringing in the ears and vertigo are two symptoms that may indicate dysfunction of the eighth cranial nerve. Ototoxicity, a common adverse effect of therapy with the aminoglycosides, may result in permanent hearing loss. If signs of ototoxicity occur, the nurse should hold the next dose of the medication and notify the health care provider. Nausea, vomiting, and hypotension are rare side effects of the medication. 72.ID: 9476957560 A client who is taking bupropion in an attempt to stop smoking tells a nurse that he has been doubling the daily dose to make it easier to resist smoking. The nurse warns the client that doubling the daily dosage is dangerous. Of which adverse effect of the medication does the nurse warn the client? ▪ Insomnia ▪ Seizures Correct ▪ Weight gain ▪ Orthostatic hypotension Rationale: Bupropion is an antidepressant. Seizure activity is common with dosages greater than 450 mg/day. It does not cause significant orthostatic blood pressure changes. Bupropion frequently causes a drop in body weight. Insomnia is a side effect, but seizure activity is more dangerous to the client. 73.ID: 9476970154 A nurse is caring for a client with histoplasmosis who is receiving intravenous amphotericin B . What should the nurse do while the medication is being administered? ▪ Monitor the client’s urine output Correct ▪ Monitor the client for hypothermia ▪ Check the client’s neurological status ▪ Check the client’s blood glucose level Rationale: Amphotericin B can produce medication toxicity during administration and exhibit symptoms such as chills, fever, headache, vomiting, and impairment of renal function. The medication is also irritating to the IV site, commonly causing thrombophlebitis. The nurse administering this medication watches for all of these problems. The other options are not specifically related to the administration of this medication. 74.ID: 9476961244 A client with rheumatoid arthritis is taking high doses of acetylsalicylic acid. While assessing the client for aspirin toxicity, which question should the nurse ask the client? ▪ “Are you constipated?” Incorrect ▪ “Are you having any diarrhea?” ▪ “Do you have any double vision?” ▪ “Do you have any ringing in the ears?” Correct Rationale: Mild intoxication with acetylsalicylic acid, called salicylism, is common when the daily dose is more than 4 g. Tinnitus (ringing in the ears) is the effect most frequently noted with intoxication. Hyperventilation may also occur, because salicylate stimulates the respiratory center. The client may have a fever, because salicylate interferes with oxygen consumption and heat production. Test-Taking Strategy: Focus on the subject, aspirin toxicity. Recalling that this medication is ototoxic will direct you to the correct option. Review the signs of aspirin toxicity. 75.ID: 9476970120 A nurse is reviewing the laboratory results of a client receiving intravenous chemotherapy. Which laboratory finding prompts the nurse to initiate neutropenic precautions? ▪ A clotting time of 10 minutes ▪ An ammonia level of 20 mcg N/dL (14.6 μmol N/L) ▪ A platelet count of 100 × 103/μL (100× 109/L). ▪ A white blood cell (WBC) count of 2.0 × 103/μL (2.0 × 109/L). Correct Rationale: The normal WBC count is 4.0 to 11.0 × 103/μL (4.0 to 11.0 × 109/L).. When the WBC count drops, neutropenic precautions — including protective isolation to protect the client from infection — must be implemented. Bleeding precautions must be initiated when the platelet count drops. With bleeding precautions, traumatic procedures such as injections and rectal temperatures are avoided. The normal platelet count is 150 to 400 × 103/μL (150 to 400 × 109/L).. The normal clotting time is 8 to 15 minutes. The normal ammonia value is 15 to 45 mcg N/dL (11-32 μmol N/L). 76.ID: 9476964575 Cyclophosphamide has been prescribed for a client with a diagnosis of breast cancer, and the nurse is providing instructions to the client. The nurse should provide which information to the client? ▪ To avoid salt while taking this medication ▪ That it is best to take the medication with food ▪ To increase fluid intake to 2000 mL to 3000 mL/day Correct ▪ To drink at least 2 glasses of orange juice every day Rationale: Hemorrhagic cystitis is a toxic effect of cyclophosphamide. The client must be instructed to drink copious amounts of fluid during administration of this medication. The client should also monitor her urine for hematuria. The medication should be taken on an empty stomach, unless gastrointestinal upset occurs. Hyperkalemia may also result from the use of the medication; therefore the client would not be encouraged to increase potassium intake (i.e., bananas and orange juice). The client also would not be instructed to alter her sodium intake. 77.ID: 9476964567 A client is receiving intravenous bleomycin sulfate. During administration of the chemotherapy, nursing assessment is the priority? ▪ Heart rate ▪ Lung sounds Correct ▪ Peripheral pulses ▪ Level of consciousness Rationale: Bleomycin sulfate, an antineoplastic medication, can cause interstitial pneumonitis that may progress to pulmonary fibrosis. Pulmonary function parameters, along with hematologic, hepatic, and renal function tests, must be monitored. The nurse should monitor lung sounds for dyspnea and wheezes, indicative of pulmonary toxicity. The medication must be discontinued immediately if pulmonary toxicity occurs. 78.ID: 9476961294 The serum theophylline level of a client who is taking the medication (Theo-24) is 16 mcg/mL. On the basis of this result, the nurse should take which action initially? ▪ Document the normal value on the chart Correct ▪ Call the health care provider immediately ▪ Call the rapid response team to help with the emergency ▪ Call the pharmacy to alert the pharmacist regarding the client’s theophylline level Rationale: The normal therapeutic range for theophylline is 10 to 20 mcg/mL. A level above 20 mcg/mL is considered toxic. A value of 16 mcg/mL is within the therapeutic range. 79.ID: 9476970188 A client with tuberculosis is being started on isoniazid and the nurse stresses the importance of returning to the clinic for follow-up blood testing. Which blood test will be performed? ▪ Liver enzymes Correct ▪ Serum creatinine ▪ Blood urea nitrogen ▪ Red blood cell count Rationale: Isoniazid therapy can increase hepatic enzymes and cause hepatitis. Therefore the client’s liver enzymes are assessed when therapy is initiated and during the first 3 months of therapy. Monitoring may be continued further in the client who is older than 50 or abuses alcohol. The other options are not specifically related to the use of this medication. 80.ID: 9476961298 Baclofen is prescribed for a client with a spinal cord injury who is experiencing muscle spasms. While providing instructions to the client, which side effect does the nurse tell the client is possible? ▪ Photosensitivity ▪ Nasal congestion Correct ▪ Increased appetite ▪ Increased salivation Rationale: Common side effects of baclofen include drowsiness, dizziness, weakness, and nausea. Occasional side effects include headache, paresthesia of the hands and feet, constipation or diarrhea, anorexia, hypotension, confusion, and nasal congestion. Paradoxical central nervous system excitement and restlessness may occur, along with slurred speech, tremor, dry mouth, nocturia, and impotence. Photosensitivity is not a side effect of this medication. 81. A nurse is caring for a client with myasthenia gravis who is exhibiting signs of cholinergic crisis. Which medication does the nurse ensure is available to treat this crisis? ▪ Acetylcysteine ▪ Atropine sulfate Correct ▪ Protamine sulfate ▪ Pyridostigmine bromide Rationale: The treatment for cholinergic crisis is atropine sulfate. Protamine sulfate is the antidote for heparin, and acetylcysteine is the antidote for acetaminophen. Pyridostigmine bromide is an anticholinesterase agent used in the treatment of myasthenia gravis to improve muscle strength. An overdose of this medication can cause cholinergic crisis. 82.ID: 9476964532 A nurse is providing instruction to a client who is taking codeine sulfate for severe back pain. Which instruction should the nurse provide to the client? ▪ Decrease fluid intake ▪ Maintain a high-fiber diet Correct ▪ Avoid all exercise to help prevent lightheadedness ▪ Avoid the use of stool softeners to help prevent diarrhea Rationale: Codeine sulfate can cause constipation. The client is instructed to increase fluid intake and maintain a high-fiber diet to help prevent constipation. The other options are incorrect because they do not address the side effects associated with the use of this medication. Although lightheadedness may occur with the use of this medication, all exercise is not avoided; in fact, the client should ambulate frequently. 83.ID: 9476967721 A nurse is preparing a plan of care for a pregnant client who will be given oxytocin to induce labor. Which occurrence does the nurse include in the plan of care as a reason for immediate discontinuation of the oxytocin infusion? ▪ Uterine atony ▪ Severe drowsiness ▪ Uterine hyperstimulation Correct ▪ Early decelerations of the fetal heart rate Rationale: Oxytocin, a synthetic hormone that stimulates uterine contractions, is a commonly used pharmacological means of inducing labor. One major concern associated with oxytocin is hyperstimulation of uterine contractions. Hyperstimulation of the uterus, which may result in diminished placental perfusion, may cause fetal distress. Therefore an oxytocin infusion must be stopped if there are any signs of uterine hyperstimulation. Early decelerations of the fetal heart rate are a reassuring sign and do not indicate fetal distress. Uterine atony and severe drowsiness are not indications of the need to discontinue the infusion. 84.ID: 9476970141 A home health nurse provides instructions to a client who is taking allopurinol for the treatment of gout. Which instruction should the nurse provide to the client? ▪ Place an ice pack on the lips if they swell ▪ Drink at least 8 glasses of fluid every day Correct ▪ Take the medication on an empty stomach 2 hours before meals ▪ Use an over-the-counter (OTC) antihistamine lotion if a rash develops Rationale: Clients taking allopurinol are encouraged to drink 3000 mL/day of fluid. Allopurinol is to be given with or immediately after meals or milk. If a rash, irritation of the eyes, or swelling of the lips or mouth develops, the client should contact the health care provider because this development may indicate hypersensitivity. 85.ID: 9476961278 A client taking metronidazole for the treatment of trichomoniasis vaginalis calls the clinic nurse to express concern because her urine has turned dark in color. The nurse should provide which information to the client? ▪ To increase her fluid intake ▪ To discontinue the medication ▪ That darkening of the urine is a harmless side effect Correct ▪ To report to the clinic to see the health care provider Rationale: Metronidazole can produce a variety of untoward effects, but they rarely require termination of treatment. Harmless darkening of the urine may occur, and the client should be forewarned of this effect. The nurse would not instruct the client to discontinue the medication. It is not necessary that the client see the health care provider. Increasing fluid intake is a good health measure but will not prevent this expected side effect. 86.ID: 9476964502 Erythromycin is prescribed for a client with a respiratory tract infection. The nurse provides instructions to the client regarding the administration of the oral medication and tells the client that it is best to take the medication in which way? ▪ With juice ▪ With a meal ▪ On an empty stomach Correct ▪ At bedtime, with a snack Rationale: Oral erythromycin should be taken on an empty stomach with a full glass of water. Some preparations may be administered with food if gastrointestinal upset occurs, but it is best to administer the drug on an empty stomach. 87.ID: 9476964550 A nurse is monitoring a client who is receiving a continuous intravenous infusion of morphine sulfate. Which finding should cause the nurse to contact the health care provider? ▪ Temperature of 97.6° F (36.4°C) ▪ Urine output of 30 mL/hr ▪ Blood pressure of 100/60 mm Hg ▪ Respiratory rate of 10 breaths/min Correct Rationale: Before an opioid is administered, respiratory rate, blood pressure, and pulse rate should be measured. The medication should be withheld and the health care provider notified if the respiratory rate is 12 breaths/min or slower, if the blood pressure is significantly below the pretreatment value, or if the pulse rate is significantly above or below the pretreatment value. A urine output of 30 mL/hr is normal. A temperature of 97.6° F (36.4°C) is below normal, but it is not necessary to notify the health care provider of this reading. 88.ID: 9476964544 A nurse is providing dietary instructions to a client taking spironolactone. Which foods does the nurse instruct the client are acceptable to consume? Select all that apply. ▪ Rice Correct ▪ Cereal Correct ▪ Carrots Correct ▪ Bananas ▪ Citrus fruits Incorrect Rationale: Spironolactone is a potassium-retaining diuretic. Hyperkalemia is the principal adverse effect. Clients are instructed to restrict their intake of potassium-rich foods, such as citrus fruits and bananas. Rice, cereal, and carrots are appropriate foods for the daily diet. 89.ID: 9476967701 A nurse is caring for a client with a diagnosis of chronic kidney disease who is receiving dialysis. Epoetin alfa, to be administered subcutaneously, has been prescribed, and the nurse is drawing the medication from a single-use vial. What should the nurse do to prepare the medication? ▪ Shake the vial before drawing up the medication ▪ Draw up the medication and discard the unused portion Correct ▪ Obtain the medication from the medication freezer and allow it to thaw ▪ Mix the medication with 0.1 mL of heparin before administration to prevent clotting Rationale: Epoetin alfa is dispensed in a 1-mL vial for subcutaneous or IV injection. The vial should not be shaken, because epoetin alfa is a protein that can be denatured with agitation. The nurse should use only one dose per single-dose vial and discard the unused portion. Epoetin alfa is not to be mixed with other medications. The medication should be stored at 2° to 8 °C (35° to 46° F) and should not be frozen. 90.ID: 9476961257 Zidovudine (is prescribed for an adult client with HIV infection. The nurse should provide which instruction to the client about the medication? ▪ That the medication must be taken with milk ▪ That aspirin can be taken to treat headache ▪ To discontinue the medication if nausea occurs ▪ To space the doses evenly around the clock Correct Rationale: The adult dosage of zidovudine is usually 200 mg every 8 hours or 300 mg every 12 hours. The client is instructed to space doses of the medication evenly around the clock. Food or milk does not affect the gastrointestinal absorption of the medication. The client is instructed to continue therapy for the full prescribed duration of treatment. The client is also instructed not to take any medication, including aspirin, without the health care provider’s approval. 91.ID: 9476961223 A nurse is to administer a dose of digoxin to a client with atrial fibrillation and notes that the client has a potassium level of 4.6 mEq/L (4.6 mmol/L). The nurse determines which about the administration of the dose? ▪ Should be withheld that day ▪ Should be administered as prescribed Correct ▪ Should be preceded with a dose of potassium ▪ Should be withheld and the health care provider notified Rationale: Hypokalemia can make the client more susceptible to digoxin toxicity, so the nurse monitors the client’s potassium level. The normal reference range of potassium for an adult is 3.5 to 5.0 mEq/L (3.5 to 5.0 mmol/L). If the potassium level is low, the dose is withheld and the health care provider is notified. In this situation, the dose should be administered as prescribed, because the potassium level is within the normal range. 92.ID: 9476970133 A client with heart failure being discharged home will be taking furosemide. Which statement by the client indicates to the nurse that the teaching has been effective? ▪ “I’ll weigh myself every day.” Correct ▪ “I’ll take my pulse every day.” ▪ “I’ll measure my urine output.” ▪ “I’ll check my ankles every day for swelling.” Rationale: A client taking furosemide must be able to monitor fluid status throughout therapy. Weighing oneself each day is the easiest and most accurate way to accomplish this. Checking the ankles for swelling and measuring urine output are incorrect because of the difficulty of assessing fluid status accurately in these ways. Taking daily pulse is not necessary and unrelated to the administration of furosemide. 93.ID: 9476967705 A client who has undergone adrenalectomy is prescribed prednisone. Which finding indicates that the client is experiencing an adverse effect of the medication? ▪ Dry mouth ▪ Tarry stools Correct ▪ Hypotension ▪ Hypoglycemia Rationale: Corticosteroids increase gastric secretion, which may result in the development of peptic ulcers and gastrointestinal bleeding. Corticosteroids increase blood glucose. Dry mouth and hypotension are not side effects of corticosteroid therapy. 94.ID: 9476964578 A pregnant client is receiving magnesium sulfate for the management of preeclampsia. Which assessment finding indicates to the nurse that the client is experiencing magnesium toxicity? ▪ Proteinuria of +3 ▪ Sudden drop in fetal heart rate Correct ▪ Presence of deep tendon reflexes ▪ Serum magnesium level of 2.5 mEq/L (1.25 mmol/L) Rationale: Magnesium toxicity may result from magnesium sulfate therapy. Signs of magnesium sulfate toxicity, related to the central nervous system–depressant effects of the medication, include respiratory depression, loss of deep tendon reflexes, sudden drop in fetal or maternal heart rate, and decreased blood pressure. The normal serum range for magnesium is 1.5-2.5 mEq/L 0.75-1.25 mmol/L)Proteinuria of 3+ is likely to be noted in a client with preeclampsia. 95.ID: 9476970149 A client with a thoracic spinal cord injury is receiving dantrolene sodium. Which statement by the client indicates to the nurse that the client is experiencing an adverse effect of the medication? ▪ “I’m feeling really drowsy.” Correct ▪ “My legs are very relaxed.” ▪ “I can’t seem to get enough to eat.” ▪ “I urinate about the same amount as I always did.” Rationale: Drowsiness, diarrhea, and hepatotoxicity are the adverse effects of this muscle relaxant, which is used to treat the chronic spasticity seen with spinal cord injury. The drowsiness may interfere with the client’s rehabilitation. Relaxed legs are a desired effect. Some clients experience anorexia and urinary frequency. 96.ID: 9476957554 The emergency department staff prepares for the arrival of a child who has ingested a bottle of acetaminophen. Which medication does the nurse ensure is available? ▪ Pancreatin ▪ Phytonadione ▪ Acetylcysteine Correct ▪ Protamine sulfate Rationale: Acetylcysteine is the antidote to acetaminophen. Pancreatin is a pancreatic enzyme replacement or supplement. Phytonadione is the antidote to warfarin sodium. Protamine sulfate is the antidote to heparin. 97.ID: 9476957571 A nurse is caring for a client who has been taking acetazolamide for glaucoma. Which, if documented in the assessment data, indicates to the nurse that the client may be experiencing an adverse effect of the medication? ▪ Tinnitus ▪ Jaundice Correct ▪ No change in peripheral vision ▪ Pupillary constriction in response to light Rationale: Acetazolamide is a carbonic anhydrase inhibitor used in the treatment of glaucoma to reduce the rate of aqueous humor formation and to lower intraocular pressure. Adverse effects include nephrotoxicity, hepatotoxicity, and bone marrow depression. Jaundice is a sign of hepatotoxicity. Tinnitus is not related to this medication. Pupillary constriction in response to light is a normal response. Diminished peripheral vision would signal a complication of glaucoma. 98.ID: 9476963002 A nurse instructs a client with hypothyroidism about the dosage, method of administration, and side effects of levothyroxine sodium. Which statement by the client indicates an understanding of the nurse’s instructions? ▪ “I should take the medication in the evening.” ▪ “I can expect diarrhea, insomnia, and excessive sweating.” ▪ “If I feel nervous or have tremors, I should only take half the dose.” ▪ “I need to report any episodes of palpitations, chest pain, or dyspnea.” Correct Rationale: One major concern when initiating thyroid hormone–replacement therapy is that the dose is too high, which can lead to cardiovascular problems. For this reason, clients need to be made aware of the early signs and symptoms of toxicity and urged to report these findings immediately to the health care provider. Diarrhea, insomnia, and excessive sweating are signs and symptoms of hyperthyroidism; though they may occur with thyroid-replacement therapy, they are not expected and should be reported. Tremors and nervousness are also signs of toxicity, which should be reported. Clients should never take it upon themselves to adjust hormone dosage. Levothyroxine sodium is administered in the morning. 99.ID: 9476959589 Warfarin sodium has been prescribed, and the nurse teaches the client about the medication. Which statement by the client indicates that further teaching is necessary? ▪ “I won’t play football anymore.” ▪ “I won’t take any over-the-counter medications except aspirin.” Correct ▪ “I’ll use an electric shaver until the doctor stops the Coumadin prescription.” ▪ “I’ll buy one of those medication alert tags that tells people I’m taking an anticoagulant.” Rationale: No over-the-counter medications of any kind should be ingested by a client taking an anticoagulant. This is especially true of aspirin and aspirin-containing products (because of the potential for bleeding). The other options are correct statements. Strenuous games (e.g., contact sports) that may result in bruising and skin breakdown should be avoided. Electric shavers are less irritating to the skin than razors and less likely to cause skin breakdown. Medication alert tags are recommended in case of emergency. The client should also be taught to carry an identification card listing all medications currently being taken. 100.ID: 9476961286 A client is taking a folic acid supplement. Which laboratory parameter does the nurse use to evaluate the effectiveness of this therapy? Select all that apply. ▪ Magnesium ▪ Hemoglobin Correct ▪ Blood glucose ▪ Hematocrit Correct ▪ Alkaline phosphatase Rationale: Folic acid, necessary for red blood cell production, is classified as a vitamin and as an antianemic agent. Both hematocrit and hemoglobin are appropriate parameters by which to assess the blood count. The nurse can gauge the effectiveness of therapy by monitoring the results of periodic complete blood counts, in particular the hematocrit. [Show More]
Last updated: 2 years ago
Preview 1 out of 61 pages
 (1).png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 23, 2021
Number of pages
61
Written in
Additional information
This document has been written for:
Uploaded
Sep 23, 2021
Downloads
0
Views
77



 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)








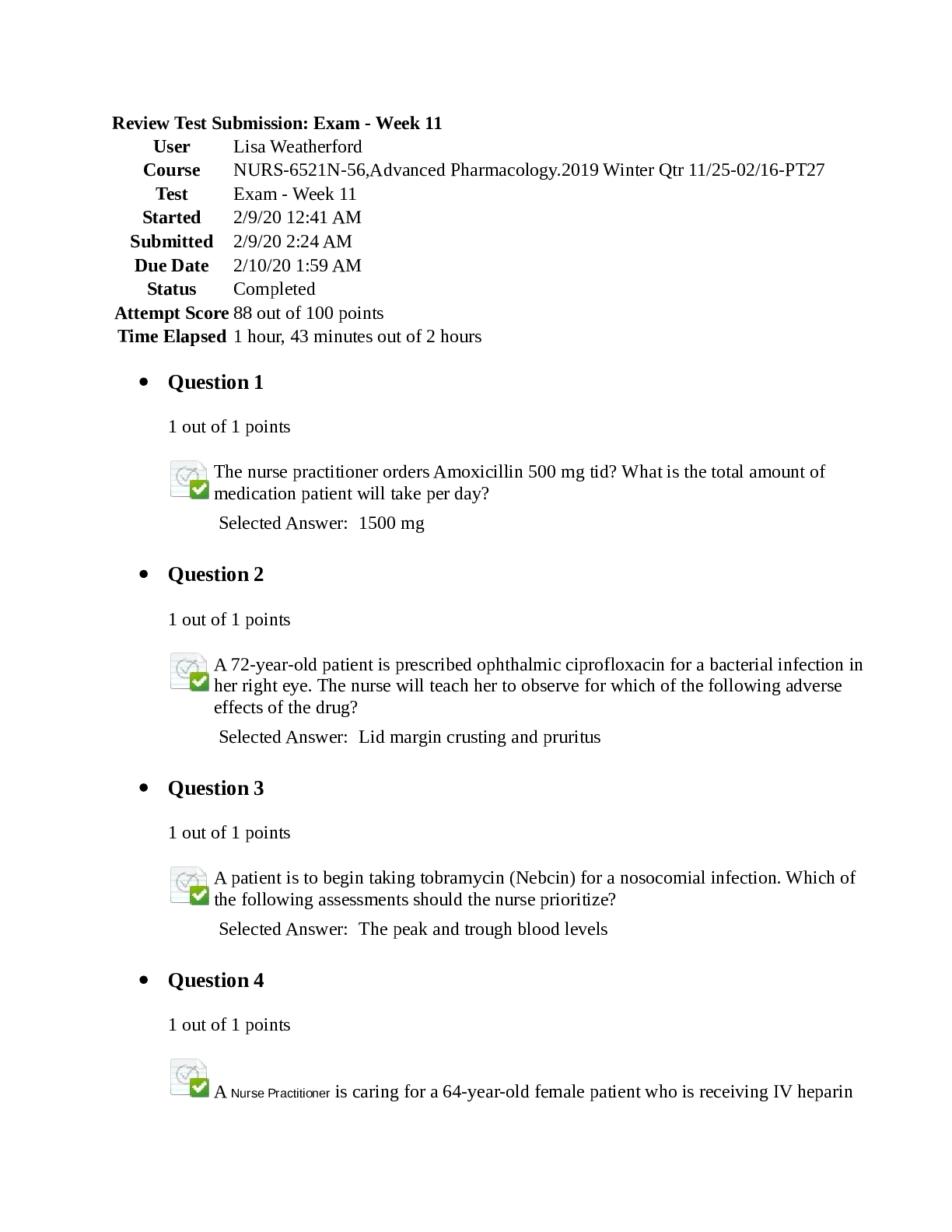

 _ Dermatology Prescription (100 Questions and Answers) – South University Savannah.png)