Bronchiolitis: diagnosis and management of bronchiolitis in children
Document Content and Description Below
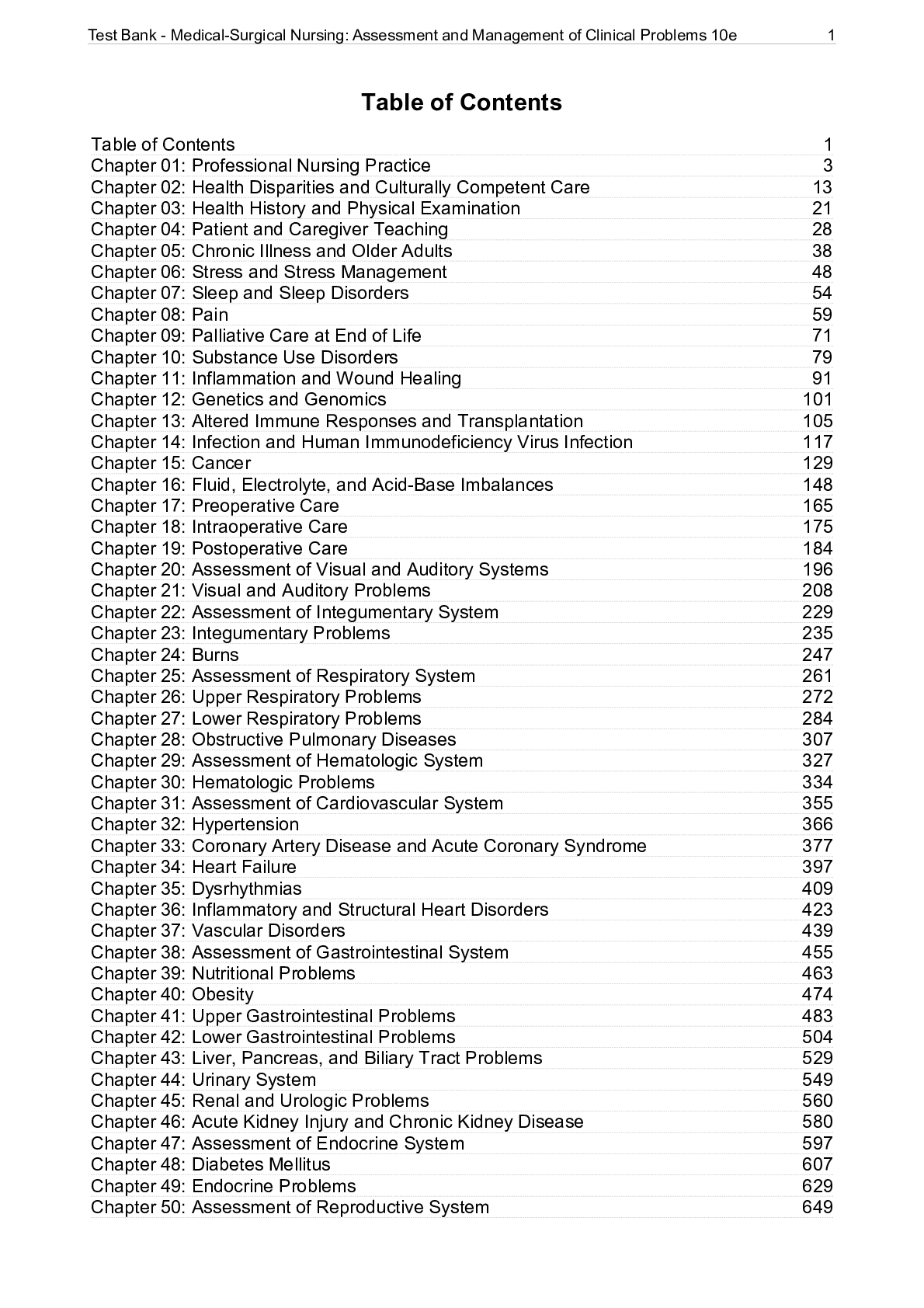
A.1 Treatment of bronchiolitis A.1.1 Review question What is the efficacy of inhaled bronchodilator therapy? What is the efficacy of systemic corticosteroid therapy? What is the efficacy of combin... ed bronchodilator and corticosteroid therapy? A.1.2 Introduction A.1.2.1 Review of published evaluations One cost effectiveness analysis was identified for this question (Sumner et al. 2010). This analysis was based on the RCT by Plint et al. 2009. This was a Canadian study comparing nebulized epinephrine plus oral dexamethasone, nebulized epinephrine alone, oral dexamethasone alone and no active treatment. The trial included infants between 6 weeks and 12 months of age. The effectiveness was measured as a combined outcome of days without symptoms and this included: difficulties in infant feeding, sleeping, coughing and noisy breathing. The results of the clinical evaluations did not show statistical significance for all differences in outcomes. The perspective for the analysis was societal, including costs to the healthcare system and costs borne by the families of children with bronchiolitis. The analysis was also run from the health care perspective. All costs were presented in 2009 Canadian dollars. The time horizon of the model was 22 days after enrolment into the trial. The results showed that the combination of epinephrine and dexamethasone was both less expensive than all other treatments including no active treatment and also more effective, with the lowest average time to relief of all symptoms (12.17 days compared with 12.69 for no active treatment, 12.62 for oral dexamethasone and 13.02 for nebulized epinephrine). The length of hospital stay and re-admissions were not reported separately and so it is not possible to adapt this model to the UK setting. A.1.2.2 New economic evaluation A network meta-analysis (Hartling et al. 2011) was published comparing bronchodilators and corticorsteroids, alone and in combination, with no treatment. This clinical evidence was used to develop a model to consider the cost effectiveness of various treatment strategies. A.1.2.3 Methods A decision tree model was developed in Excel based on the outcomes of the network meta-analysis (Figure 1). The following comparisons were considered in the model: no treatment adrenaline adrenaline plus steroid steroid steroid plus salbutamol salbutamol Bronchiolitis appendices Health economics @NCC_WCH 6 Figure 1: Decision tree model The model was developed from the perspective of the UK NHS, using 2013/14 costs. The time horizon for the model was less than a year and so no discount rate was applied. The clinical evidence was presented as odds ratios (ORs). Using the baseline risk of admission from all studies of 20% as reported in Hartling et al. 2011, the relative risks for each treatment strategy were calculated: (OR admission x OR treatment) / (1−(OR admission x OR treatment) = risk of admission given treatment Risk of admission given treatment / baseline risk of admission = relative risk of admission given treatment Table 1: Risk of admission Treatment strategy OR Lower 95% CI Upper 95% CI Calculated RR Admissions at day 1 Adrenaline 0.48 0.18 1.01 0.54 Adrenaline plus steroid 0.52 0.15 1.57 0.58 Steroid 0.84a) 0.33 2.05 0.87 Steroid plus salbutamol 0.92 0.28 3.4 0.93 Salbutamol 1.04 0.46 2.35 1.03 Admissions at day 7 Adrenaline 0.85 0.18 3.85 0.88 Adrenaline plus steroid 0.56 0.12 2.6 0.61 Admit [Show More]
Last updated: 2 years ago
Preview 1 out of 713 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$22.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 23, 2021
Number of pages
713
Written in
Additional information
This document has been written for:
Uploaded
Sep 23, 2021
Downloads
0
Views
112






.png)




.png)