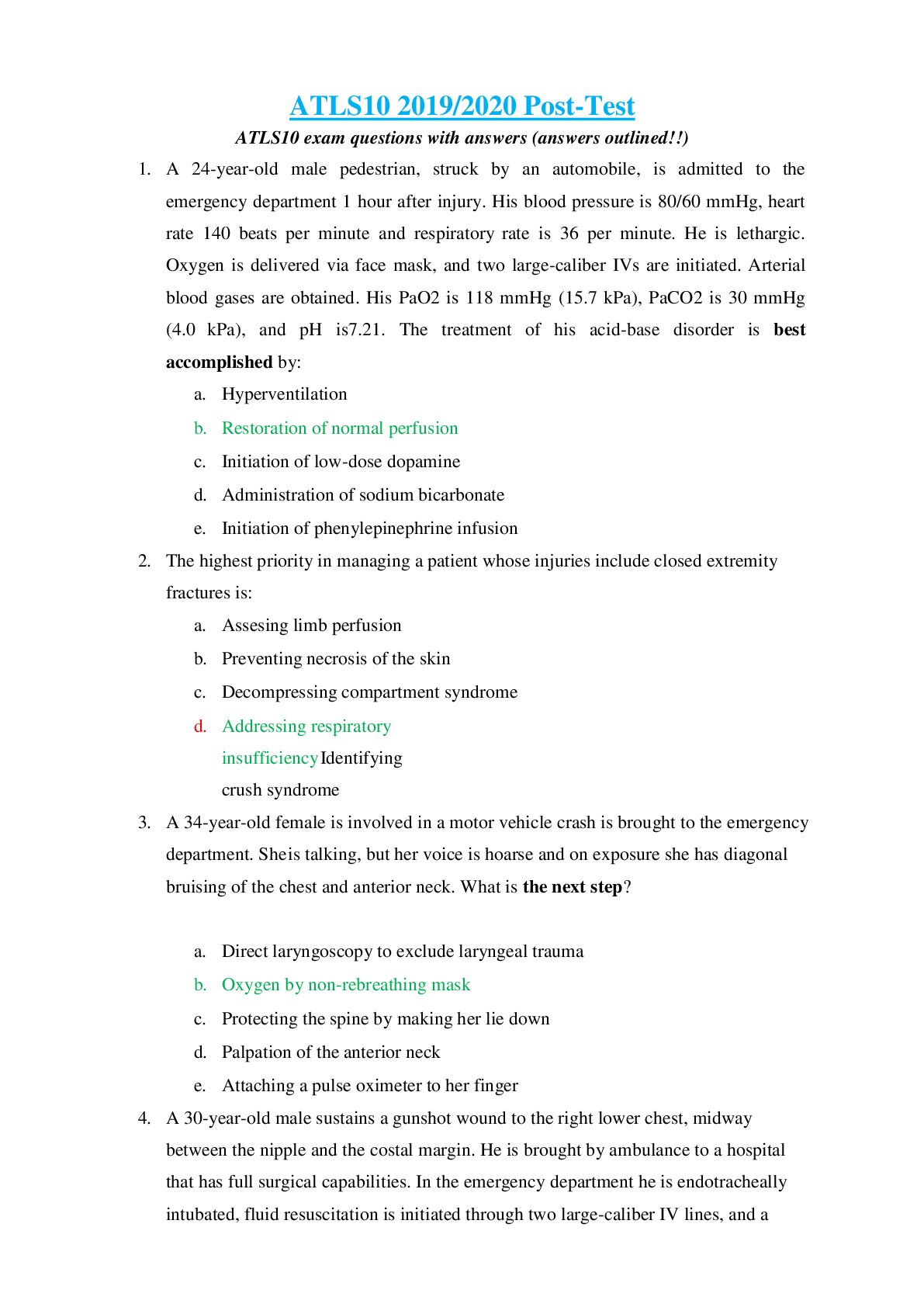
Cardiac tamponade after trauma
a. is seldom life-threatening
b. can be excluded by an upright, AP chest x-ray
c. can be confused with a tension pneumothorax
d. causes a fall in systolic pressure of > 15 mm Hg with ex
...
Cardiac tamponade after trauma
a. is seldom life-threatening
b. can be excluded by an upright, AP chest x-ray
c. can be confused with a tension pneumothorax
d. causes a fall in systolic pressure of > 15 mm Hg with expiration
e. most commonly occurs after blunt injury to the anterior chest wall
2. Which one of the following statements regarding patients with thoracic spine
injuries is TRUE?
a. Log-rolling may be destabilizing to fractures from T-12 to L-1.
b. Adequate immobilization can be accomplished with the scoop stretcher.
c. Spinal cord injury below T-10 usually spares bowel and bladder function.
d. Hyperflexion fractures in the upper thoracic spine are inherently
unstable.
e. These patients rarely present with spinal shock in association with cord
injury.
3. Absence of breath sounds and dullness to percussion over the left hemithorax
are fmdings best explained by
a. Left hemothorax.
b.
c.
d.
e.
f.
g. cardiac contusion
h. left simple pneumothorax
i. left diaphragmatic rupture
j. right tension pneumothorax.
4. A young man sustains a gunshot wound to the abdomen and is brought
promptly to the emergency department by prehospital personnel. His skin is
cool and diaphoretic, and he is confused. His pulse is thready and his femoral
pulse is only weakly palpable. The defmitive treatment in managing this
patient is to
a. administer 0-negative blood
b. applyextemal warming devices.
c. Control internal hemorrhage operatively
d. apply the pneumatic antishock garment
e. infuse large volumes of intravenous crystalloid solution.
5. To establish a diagnosis of shock,
a. systolic blood pressure must be below 90 mm Hg.
b. the presence of a closed head injury should be excluded
c. acidosis should be present by arterial blood \gas analysis
d. the patient must fail to respond to intravenous fluid infusion.
e. clinical evidence of inadequate organ perfusion must be present.
6. A 23-year-old man is brought immediately to the emergency department from
the hospital' s parking lot where he was shot in the lower abdomen.
Examination reveals a single bullet wound. He is breathing and has a thready
pulse. However, he is unconscious and has no detectable blood pressure.
Optimal immediate management is to
a. perform diagnostic peritoneal lavage.
b. initiate infusion of packed red blood cells.
c. insert a nasogastric tube and urinary catheter.
d. transfer the patient to the operating room, while initiating fluid
therapy.
e. initiate fluid therapy to return his blood pressure to normotensive
7. An electrician is electrocuted by a downed power line after a thunderstorm.
He apparently made contact with the wire at the level of the right mid thigh.
In the emergency department, his vital signs are normal and no dysrhythmia
is noted on ECG. On examination, there is an exit wound on the bottom of the
right foot. His urine is positive for blood by dip stick but no RBCs are seen
microscopically. Initial management should include
a. immediate angiography.
b. aggressive fluid infusion.
c. intravenouspyleography.
d. debridement of necrotic muscle.
e. admission to the intensive care unit for observation.
8. An 8-year-old girl is an unrestrained passenger in a vehicle struck from
behind. In the emergency department, her blood pressure is 80/60 mm Hg,
heart rate is 80 beats per minute, and respiratory rate is 16 breaths per
minute. Her GCS score is 14. She complains that her legs feel "funny and
won't move right;" however, her spine x-rays do not show a fracture or
dislocation. A spinal cord injury in this child
a. is most likely a central cord syndrome.
b. must be diagnosed by magnetic resonance imaging.
c. can be excluded by obtaining a CT of the entire spine.
d. may exist in the absence of objective findings on x-ray studies.
e. is unlikely because of the incomplete calcification of the vertebral bodies.
9. Immediate chest tube insertion is indicated for which of the following
conditions?
a. Pneumothorax
b. Pneumomediastinum
c. Massive hemothorax
d. Diaphragmatic rupture
e. Subcutaneous emphysema
10.A 32-year-old man is brought to the hospital unconscious with severe facial
injuries and noisy respirations after an automobile collision. In the emergency
department, he has no apparent injury to the anterior aspect of his neck. He
suddenly becomes apneic, and attempted ventilation with a face mask is
unsuccessful. Examination of his mouth reveals a large hematoma of the
pharynx with loss of normal anatomic landmarks. Initial management of his
airway should consist of
a. inserting an oropharyngealairvvay.
b. inserting a nasopharyngeal airway.
c. performing a surgical cricothyroidotomy.
d. performingfiberoptic-guided nasotracheal intubation.
e. performingorotracheal intubation after obtaining a lateral c-spine x-ray.
11.The primary indication for transferring a patient to a higher level trauma
center is
a. unavailability of a surgeon or operating room staff.
b. multiple system injuries, including severe head injury.
c. resource limitations as determined by the transferring doctor.
d. resource limitations as determined by the hospital administration.
e. widened mediastinum on chest x-ray following blunt thoracic trauma.
12.A young man sustains a ritle wound to the mid-abdomen. He is brought
promptly to the emergency department by prehospital personnel. His skin is
cool and diaphoretic, and his systolic blood pressure is 58 rnm Hg. Warmed
crystalloid fluids are initiated without improvement in his vital signs. The
next, most appropriate step is to perform
a. celiotomy.
b. an abdominal CT scan.
c. diagnostic laparoscopy.
d. abdominal ultrasonography.
e. a diagnostic peritoneal lavage.
13.A teen-aged bicycle rider is hit by a truck traveling at a high rate of speed. In
the emergency department, she is actively bleeding from open fractures of
her legs, and has abrasions on her chest and abdominal wall. Her blood
pressure is 80/50 mm Hg, heart rate is 140 beats per minute, respiratory rate
is 8 breaths per minute, and GCS score is 6. The first step in managing this
patient is to
a. obtain a lateral cervical spine x-ray.
b. insert a central venous pressure line.
c. administer 2 liters of crystalloid solution.
d. perform endotracheal intubation and ventilation.
e. apply the PASG and inflate the leg compartments.
14.An 8-year-old boy falls 4.5 meters (15 feet) from a tree and is brought to the
emergency department by his family. His vital signs are normal, but he
complains of left upper quadrant pain. An abdominal CT scan reveals a
moderately severe laceration of the spleen. The receiving institution does not
have 24-hour-a-day operating room capabilities. The most appropriate
management of this patient would be to
a. type and crossmatch for blood.
b. request consultation of a pediatrician.
c. transfer the patient to a trauma center.
d. admit the patient to the intensive care unit.
e. prepare the patient for surgery the next day.
15.A 17-year-old helmeted motorcyclist is struck broadside by an automobile at
an intersection. He is unconscious at the scene with a blood pressure of
140/90 mm Hg, heart rate of 90 beats per minute, and respiratory rate of 22
breaths per minute. His respirations are sonorous and deep. His GCS score is
6. Immobilization of the entire patient may include the use of all the following
EXCEPT
a. air splints.
b. bolstering devices.
c. a long spine board.
d. a scoop-style stretcher.
e. A semirigid cervical collar.
16.Which of the following statements regarding injury to the central nervous
system in children is TRUE?
a. Children suffer spinal cord injury without x-ray abnormality more
commonly than adults.
b. An infant with a traumatic brain injury may become hypotensive from
cerebral edema.
c. Initial therapy for the child with traumatic brain injury includes the
administration of methylprednisolone intravenously.
d. Children have more focal mass lesions as a result of traumatic brain injury
when compared to adults .
e. Young children are less tolerant of expanding intracranial mass lesions
than adults.
17.During an altercation, a 32-year-old man sustains a gunshot wound to the
right upper hemithorax, above the nipple line with an exit wound posteriorly
above the scapula on the right. He is transported by ambulance to a
community hospital. He is endotracheally intubated, closed tube
thoracostomy is performed, and 2 liters of Ringer's lactate solution are
infused through 2 large-caliber IVs. His blood pressure now is 60/0 mm Hg,
heart rate is 160 beats per minute, and respiratory rate is 14 breaths per
minute (ventilated with 100% 02). The most appropriate next step in
managing this patient is
a. celiotomy.
b. diagnostic peritoneal lavage.
c. arterial blood gas determination.
d. administer packed red blood cells.
e. chest x-ray to confinn tube placement.
18.A 42-year-old man, injured in a motor vehicle crash, suffers a closed head
injury, multiple palpable left rib fractures, and bilateral femur fractures. He is
intubated orotracheally without difficulty. Initially, his ventilations are easily
assisted with a bag¬valve device. It becomes more difficult to ventilate the
patient over the next 5 minutes, and his hemoglobin oxygen saturation level
decreases from 98% to89 % . The most appropriate next step is to
a. obtain a chest x-ray.
b. decrease the tidal volume.
c. auscultate the patient's chest.
d. increase the rate of assisted ventilations.
e. perform needle decompression of the left chest.
19.A 24-year-old woman passenger in an automobile strikes the wind screen with
her face during a head-on collision. In the emergency department, she is
talking and has marked facial edema and crepitus. The highest priority should
be given to
a. lateral, c-spine x-ray.
b. upper airway protection.
c. carotid pulse assessment.
d. management of blood loss.
e. determination of associated Injuries.
20.Twenty-seven patients are seriously injured in an aircraft accident at a local
airport. The basic principle of triage should be to
a. treat the most severely injured patients first.
b. establish a field triage area directed by a doctor.
c. rapidly transport all patients to the nearest appropriate hospital.
d. treat the greatest number of patients in the shortest period of time.
e. produce the greatest number of survivors based on available
resources.
21.Which one of the following statements is FALSE concerning Rh
isoimmunization in the pregnant trauma patient?
a. It occurs in blunt or penetrating abdominal trauma.
b. Minor degrees of fetomaternal hemorrhage produce it.
c. A negative Kleihauer-Betke test excludes Rh isoimmunization.
d. This is not a problem in the traumatized Rh-positive pregnant patient.
e. initiation of Rh immunoglobulin therapy does not require proof of
fetomaternal hemorrhage.
22.A 30-year-old man is struck by a car traveling at 56 kph (35 mph). He has
obvious fractures of the left tibia near the knee, pain in the pelvic area, and
severe dyspnea. His heart rate is 180 beats per minute, and his respiratory
rate is 48 breaths per minute with no breath sounds heard in the left chest. A
tension pneumothorax is relieved by immediate needle decompression and
tube thoracostomy. Subsequently, his heart rate decreases to 140 beats per
minute, his respiratory rate decreases to 36 breaths per minute, and his
blood pressure is 80/50 inm Hg. Warmed Ringer's lactate is administered
intravenously. The next priority should be to:
a. perform a urethrogram and cystogram.
b. perform external fixation of the pelvis.
c. obtain abdominal and pelvic CT scans.
d. perform arterial embolization of the pelvic vessels.
e. perform diagnostic peritoneal lavage or abdominal ultrasound.
23.Regarding shock in the child, which of the following is FALSE?
a. Vital signs are age-related.
b. Children have greater physiologic reserves than do adults.
c. Tachycardia is the primary physiologic response to hypovolemia.
d. The absolute volume of blood loss required to produce shock is
the same as in adults.
e. An initial fluid bolus for resuscitation should approximate 20 mL/kg of
Ringer's lactate
24.A 30-year-old man sustains a severely comminuted, open distal right femur
fracture in a motorcycle crash. The wound is actively bleeding. Normal
sensation is present over the lateral aspect of the foot but decreased over the
medial foot and great toe. Normal motion of the foot is observed.
Dorsalispedis and posterior tibial pulses are easily palpable on the left, but
heard only by Doppler on the right. Immediate efforts to improve circulation
to the injured extremity should involve
a. immediate angiography.
b. tamponade of the wound with a pressure dressing.
c. wound exploration and removal of bony fragments.
d. realignment of the fracture segments with a traction splint.
e. fasciotomy of all four compartments in the lower extremity.
25.A crosstable, lateral x-ray of the cervical spine
a. must precede endotracheal intubation.
b. excludes serious cervical spine injury.
c. is an essential part of the primary survey.
d. is not necessary for unconscious patients with penetrating cervical
injuries.
e. is unacceptable unless 7 cervical vertebrae and the C-7 to T-1
relationship are visualized.
26.An 18-year-old, helmeted motorcyclist is brought by ambulance to the
emergency department following a high-speed crash. Prehospitalpersormel
report that he was thrown 15 meters (50 feet) off his bfice. He has a history
of hypotension prior to arrival in the emergency department, but is now
awake, alert, and conversational. Which of the following statements is TRUE?
a. Cerebral perfiision is intact
b. Intravascular volume status is normal.
c. The patient has sensitive vasomotor reflexes.
d. Intraabdominal visceral injuries are unlikely.
e. The patient probably has an acute epidural hematoma.
27.Which one of the following is the recommended method for initially treating
frostbite?
a. Vasodilators
b. Anticoagulants
c. Warm (40°C) water
d. Padding and elevation
e. Topical application of silvasulphadiazine
28.The driver of a single car crash is orotracheally intubated in the field by
prehospital personnel after they identify a closed head injury and determine
that the patient is unable to protect his airway. In the emergency department,
the patient demonstrates decorticate posturing bilaterally. He is being
ventilated with a bag-valve device, but his breath sounds are absent in the
left hemithorax. His blood pressure is 160/88 mm Hg, heart rate is 70 beats
per minute, and the pulse oximeter displays a hemoglobin oxygen saturation
of 96% . The next step in assessing and managing this patient should be to
a. determine the arterial blood gases.
b. obtain a lateral cervical spine x-ray.
c. assess placement of the endotracheal tube.
d. perform needle decompression of the left chest.
e. insert a thoracostomy tube in the left hemithorax.
29.Early central venous pressure monitoring during fluid resuscitation in the
emergency department has the greatest utility in a
a. patient with a splenic laceration.
b. patient with an inhalation injury.
c. 6-year-old child with a pelvic fracture.
d. patient with a severe cardiac contusion.
e. 24-year-old man with a massive hemothorax.
30.The response to catecholamines in an injured, hypovolemic pregnant woman
can be expected to result in
a. placental abruption.
b. fetal hypoxia and distress.
c. fetal/maternal dysrhythmia.
d. improved uterine blood flow.
e. increased maternal renal blood flow.
31.A 5-year-old boy is struck by an automobile and brought to the emergency
department. He is lethargic, but withdraws purposefully from painful stimuli.
His blood pressure is 90 mm Hg systolic, heart rate is 140 beats per minute,
and his respiratory rate is 36 breaths per minute. The preferred route of
venous access in this patient is
a. percutaneous femoral vein cannulation
b. cutdown on the saphenous vein at the ankle.
c. intraosseous catheter placement in the proximal tibia.
d. percutaneous peripheral veins in the upper extremities.
e. central venous access via the subclavian or interna1 jugular vein.
32.A 22-year-old man is brought to the hospital after crashing his motorcycle
into a telephone pole. He is unconscious and in profound shock. He has no
open wounds or obvious fractures. The cause of his shock is MOST LIKELY
caused by
a. a subdural hematoma.
b. an epidural hematoma.
c. a transected lumbar spinal cord.
d. a transected cervical spinal cord.
e. hemorrhage into the chest or abdomen.
33.A 42-year-old man is trapped from the waist down beneath his overtumed
tractor for several hours before medical assistance arrives. He is awake and
alert until just before arriving in the emergency department. He is now
unconscious and responds only to painful stimuli by moaning. His pupils are 3
mm in diameter and symmetrically reactive to light. Prehospital personnel
indicate that they have not seen the patient move either of his lower
extremities. On examination in the emergency department, no movement of
his lower extremities is detected, even in response to painful stimuli. The
most likely cause for this fmding is
a. an epidural hematoma.
b. a pelvic fracture.
c. central cord syndrome.
d. intracerebral hemorrhage.
e. bilateral compartment syndrome.
34.All of the following signs on the chest x-ray of a blunt injury victim may
suggest aortic rupture EXCEPT:
a. mediastinal emphysema.
b. presence of a "pleural cap."
c. obliteration of the aortic knob.
d. deviation of the trachea to the right.
e. depression of the left mainstem bronchus
35.A young woman sustains a severe head injury as the result of a motor
vehicular crash. In the emergency department, her GCS score is 6. Her blood
pressure is 140/90 mm Hg and her heart rate is 80 beats per minute. She is
intubated and is being mechanically ventilated. Her pupils are 3 mm in size
and equally reactive to light. There is no other apparent injury. The most
important principle to follow in the early management of her head injury is to
a. administer an osmotic diuretic.
b. prevent secondary brain injury.
c. aggressively treat systemic hypertension.
d. reduce metabolic requirements of the brain.
e. distinguish between intracranial hematoma and cerebral edema.
36.A 25-year-old woman is brought to the emergency department after a motor
vehicle crash. She was initially lucid at the scene and then developed a
dilated pupil and contralateral extremity weakness. In the emergency
department, she is unconscious and has a GCS score of 6. The initial
management step for this patient should be to
a. obtain a CT scan of the head.
b. administerdecadron 20 mg IV.
c. perform endotracheal intubation.
d. initiate an W line and administer Mannitol 1 g/kg.
e. perform an emergency linar hole on the side of the dilated pupil.
37.Contraindication to nasogastric intubation is the presence of a
a. gastric perforation.
b. diaphragmatic rupture.
c. open depressed skull fracture.
d. fracture of the cervical spine.
e. fracture of the cribriform plate.
38.A 24-year-old man sustains multiple fractured ribs bilaterally as a result of
being crushed in a press at a plywood factory. Examination in the emergency
department reveals a flail segment of the patient's thorax. Primary
resuscitation includes high-flow oxygen administration via a nonrebreathing
mask, and initiation of Ringer' s lactate solution. The patient exhibits
progressive confusion, cyanosis, and tachypnea. Management at this time
should consist of
a. intravenous sedation.
b. external stabilization of the chest wall.
c. increasing the F102 in the inspired gas.
d. intercostal nerve blocks for pain relief.
e. endotracheal intubation and mechanical ventilation.
39.During resuscitation, which one of the following is the most reliable as a
guide to volume replacement?
a. Pulse rate
b. Hematocrit
c. Blood pressure
d. Urinary output
e. Jugular venous pressure
40.Which one of the following physical findings suggests a cause of hypotension
other than spinal cord injury?
a. priapism.
b. bradycardia.
c. diaphragmatic breathing.
d. presence of deep tendon reflexes.
e. ability to flex forearms but inability to extend them
[Show More]
.png)


.png)