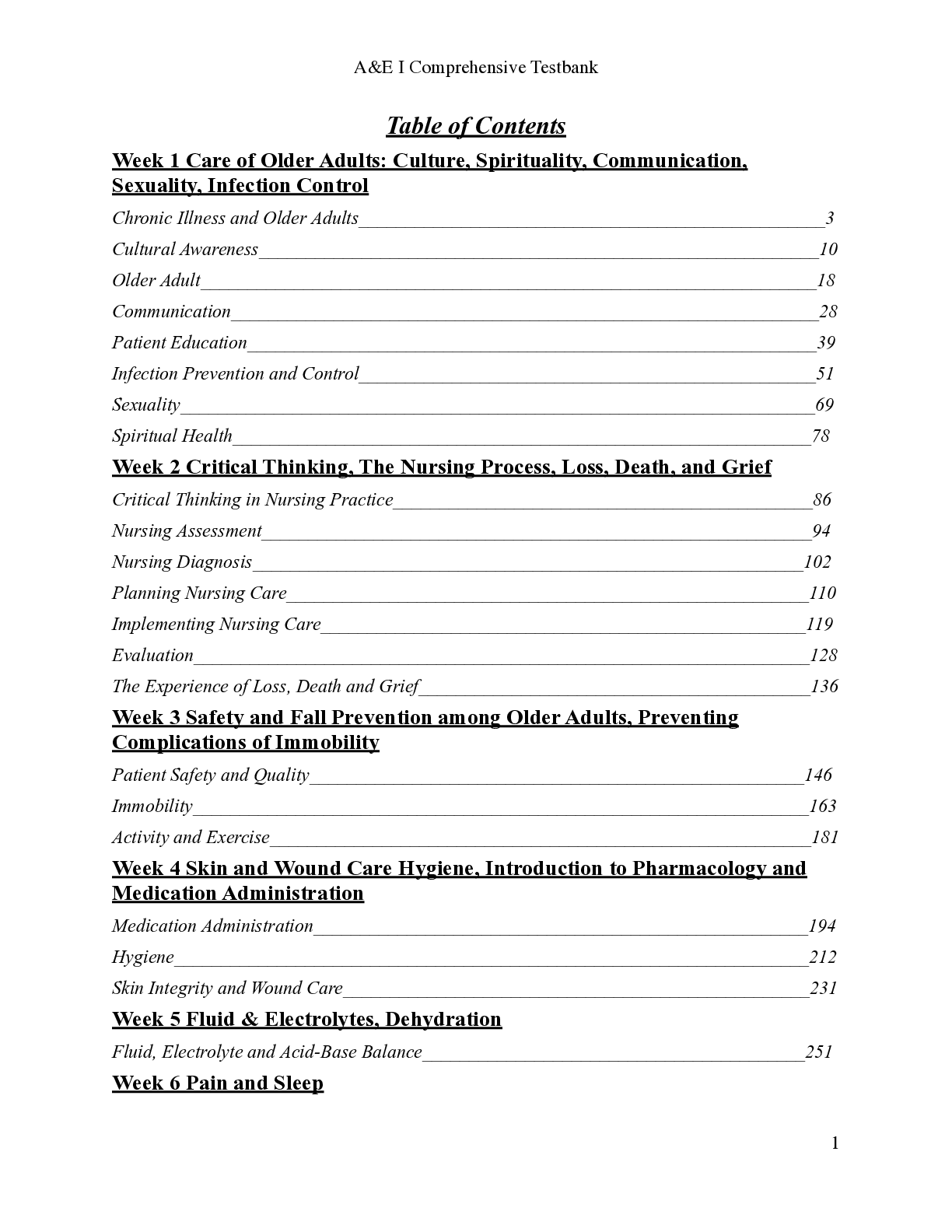
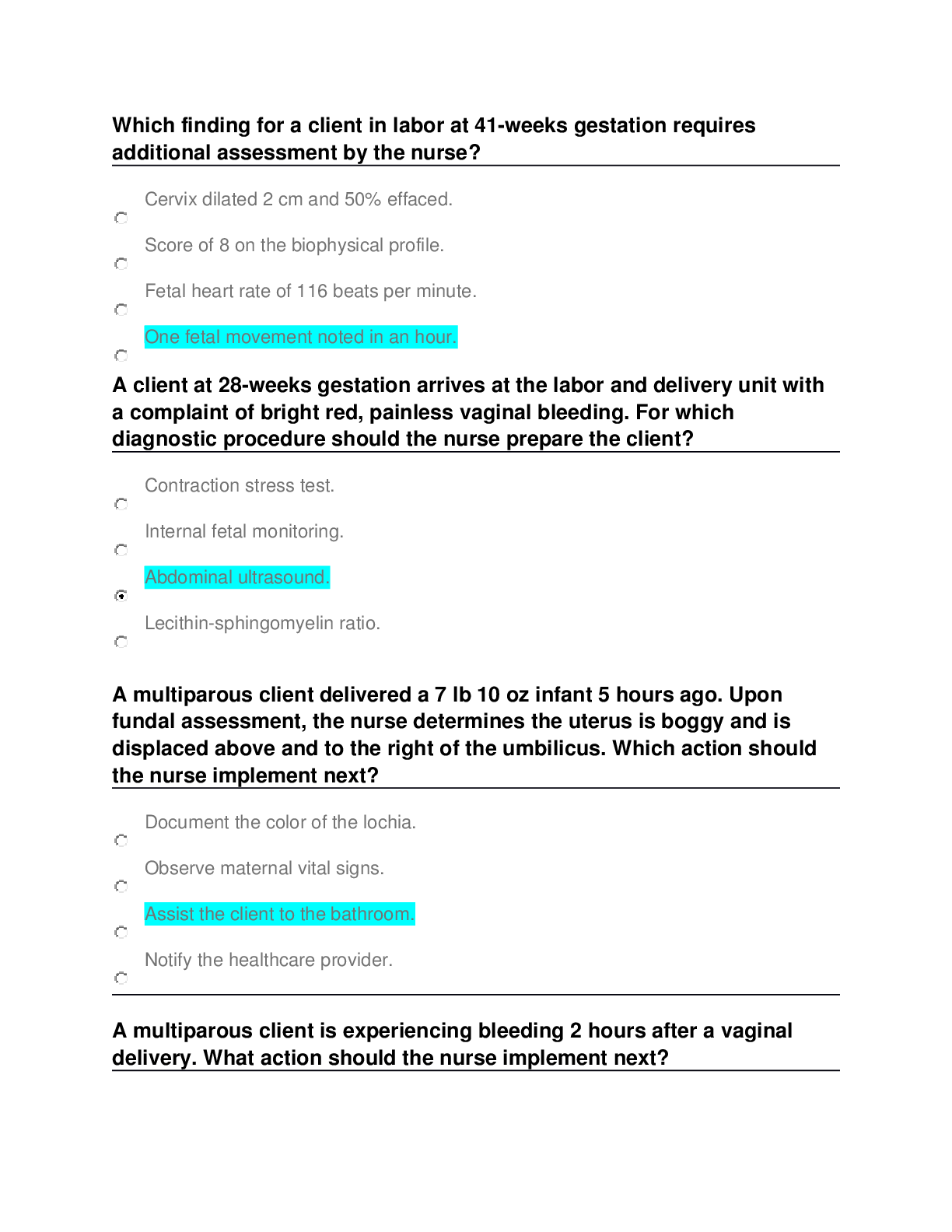
Which finding for a client in labor at 41weeks gestation requires
additional assessment by the nurse?
Cervix dilated 2 cm and 50% effaced.
Score of 8 on the biophysical profile.
Fetal heart rate of 116 beats per
...
Which finding for a client in labor at 41weeks gestation requires
additional assessment by the nurse?
Cervix dilated 2 cm and 50% effaced.
Score of 8 on the biophysical profile.
Fetal heart rate of 116 beats per minute.
One fetal movement noted in an hour.
A client at 28weeks gestation arrives at the labor and delivery unit with
a complaint of bright red, painless vaginal bleeding. For which
diagnostic procedure should the nurse prepare the client?
Contraction stress test.
Internal fetal monitoring.
Abdominal ultrasound.
Lecithinsphingomyelin ratio.
A multiparous client delivered a 7 lb 10 oz infant 5 hours ago. Upon
fundal assessment, the nurse determines the uterus is boggy and is
displaced above and to the right of the umbilicus. Which action should
the nurse implement next?
Document the color of the lochia.
Observe maternal vital signs.
Assist the client to the bathroom.
Notify the healthcare provider.
A multiparous client is experiencing bleeding 2 hours after a vaginal
delivery. What action should the nurse implement next?
Determine the firmness of the fundus.
Give oxytocin (Pitocin) intravenously.
Inform the healthcare provider of the bleeding.
Assess the vital signs for indicators of shock.
The nurse notes a pattern of the fetal heart rate decreasing after each
contraction. What action should the nurse implement?
Give 10 liters of oxygen via face mask.
Prepare for an emergency cesarean section.
Continue to monitor the fetal heart rate pattern.
Obtain an oral maternal temperature.
A client at 28weeks gestation experiences blunt abdominal trauma.
Which parameter should the nurse assess first for signs of internal
hemorrhage?
Vaginal bleeding.
Complaints of abdominal pain.
Changes in fetal heart rate patterns.
Alteration in maternal blood pressure.
Which client should the nurse report to the healthcare provider as
needing a prescription for Rh Immune Globulin (RhoGAM)?
Woman whose blood group is AB Rhpositive.
Newborn with rising serum bilirubin level.
Newborn whose Coombs test is negative.
Primigravida mother who is Rhnegative.
The nurse is caring for a client whose labor is being augmented with
oxytocin (Pitocin). Which finding indicates that the nurse should
discontinue the oxytocin infusion?
The client needs to void.
Amniotic membranes rupture.
Uterine contractions occur every 8 to 10 minutes.
The fetal heart rate is 180 bpm without variability
A client in labor receives an epidural block. What intervention should the
nurse implement first?
Encourage oral fluids.
Assess contractions.
Monitor blood pressure.
Obtain a radial pulse.
A multiparous client is admitted to the postpartum unit after a rapid
labor and birth of an infant weighing 4,000 grams. The client's fundus is
boggy, lochia is heavy, and vital signs are unchanged. After having the
client void and massaging the uterus, the client's fundus remains
difficult to locate, and the rubra lochia remains heavy. What action
should the nurse implement next?
Recheck the client's vital signs.
Notify the healthcare provider.
Insert an indwelling urinary catheter.
Massage the fundus in 30 minutes.
The nurse is providing discharge teaching for a gravid client who is
being released from the hospital after placement of cerclage. Which
instruction is the most important for the client to understand?
Plan for a possible cesarean birth.
Arrange for home uterine monitoring.
Make arrangements for care at home.
Report uterine cramping or low backache.
The nurse assesses a male newborn and determines that he
has the following vital signs: axillary temperature 95.1 F,
heart rate 136 beats/minute and a respiratory rate 48
breaths/minute. Based on these findings, which action
should the nurse take first?
Check the infant's arterial blood gases.
Notify the pediatrician of the infant's vital signs.
Assess the infant's blood glucose level.
Encourage the infant to take the breast or sugar water.
Rationale
The nurse should first assess the infant's blood glucose level (C),
because the infant is displaying signs of hypothermia (normal
newborn axillary temperature is 96 to 98 F) and hypoglycemia may
occur as glucose is metabolized in an effort to meet cellular energy
demands. The infant's respiratory and heart rates are within normal
limits, so (A) is not a priority. (B and D) would be implemented after
information regarding the blood sugar level has been obtained.
What action should the nurse implement when caring for a
newborn receiving phototherapy?
Reposition every 6 hours.
Place an eyeshield over the eyes.
Limit the intake of formula.
Apply an oil-based lotion to the skin.
Rationale
Phototherapy converts unconjugated bilirubin, which is deposited in
the skin, to a water-soluble form that is more easily excreted by the
liver. Exposure to the light source can increase the risk for ocular
damage, so an eyeshield (B) is placed while the infant is under the
light source. To ensure all body surfaces are exposed to the lights,
the newborn should be reposition every 2 to 4 hours, not every 6
hours (A). Phototherapy can increase insensible water loss, and to
prevent dehydration, fluid intake should be encouraged, not
restricted (C). Lotions (D) absorb heat and can potentially cause
burns and should not be used on the skin while phototherapy is in
progress.
The nurse is caring for a client in active labor and observes
V shape decelerations in the fetal heart rate occurring with
the peak of each contraction. What action should the nurse
implement?
Notify the healthcare provider of fetal status.
Give oxygen at 10 L per nasal cannula.
Place the client in a side-lying position.
Increase the flow rate of intravenous fluids.
Rationale
Variable decelerations are caused by compression of the umbilical
cord and are evidenced by V shape appearance, characterized by a
rapid descent and ascent to and from the depth of the deceleration.
To alleviate the pressure on the umbilical cord, the nurse should
reposition the client into a side-lying position (C). Once the client is
repositioned and evaluated, then (A, B, and D) should be
implemented.
A multiparous client delivered a 7 lb 10 oz infant 5 hours
ago. Upon fundal assessment, the nurse determines the
uterus is boggy and is displaced above and to the right of
the umbilicus. Which action should the nurse
[Show More]


.png)