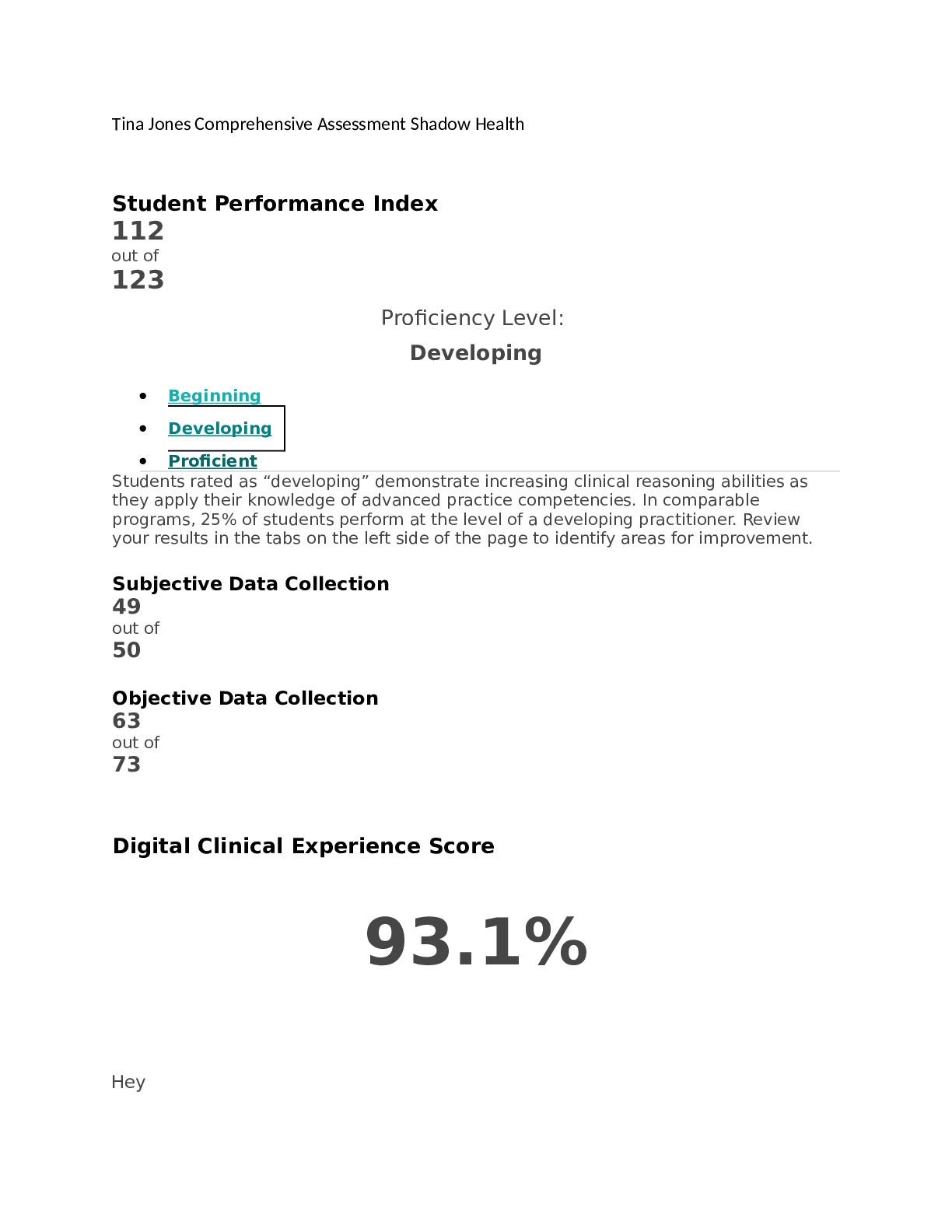
*NURSING > SHADOW HEALTH > Esther Parks abdominal pain - EHR documentation. (All)
Esther Parks abdominal pain - EHR documentation.
Document Content and Description Below
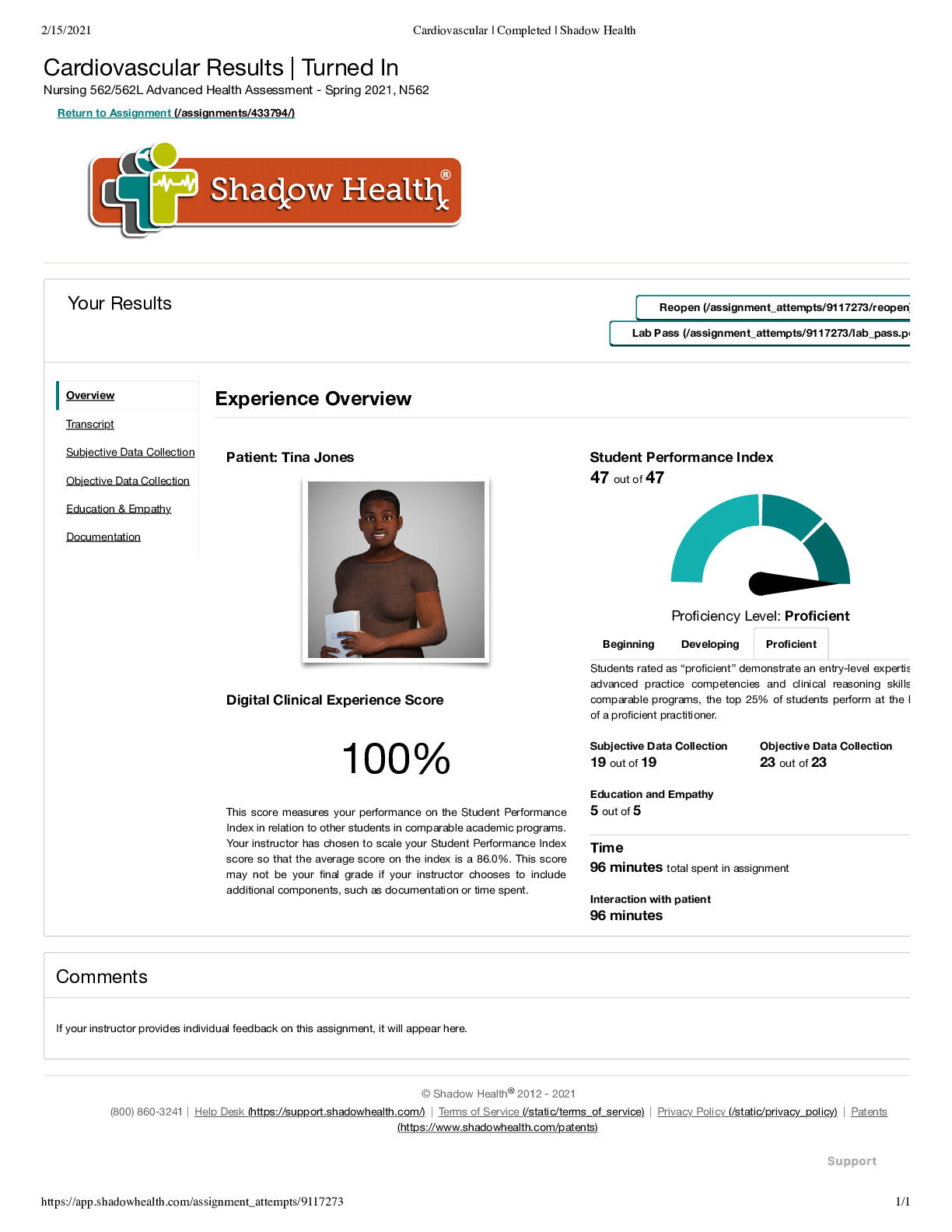
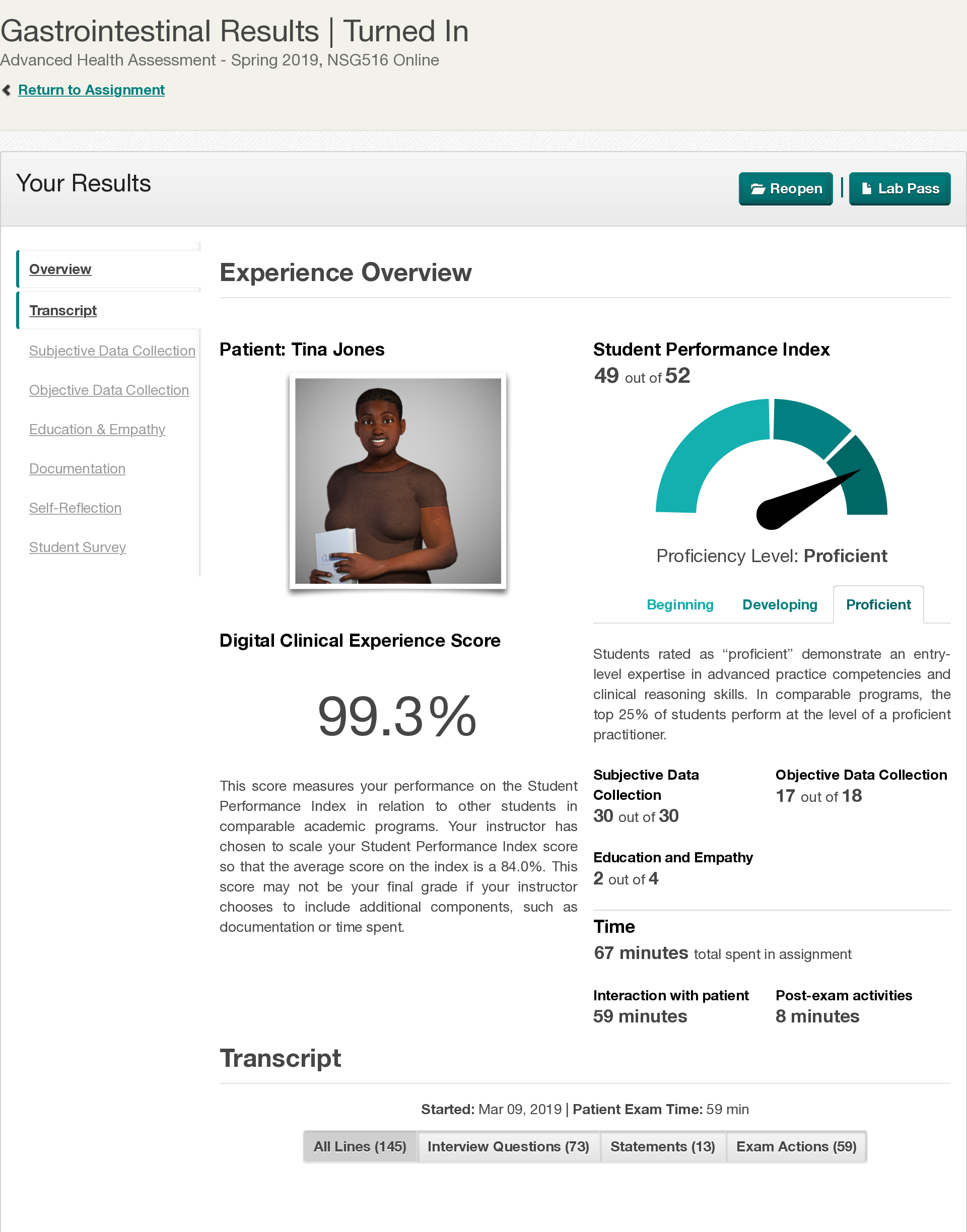
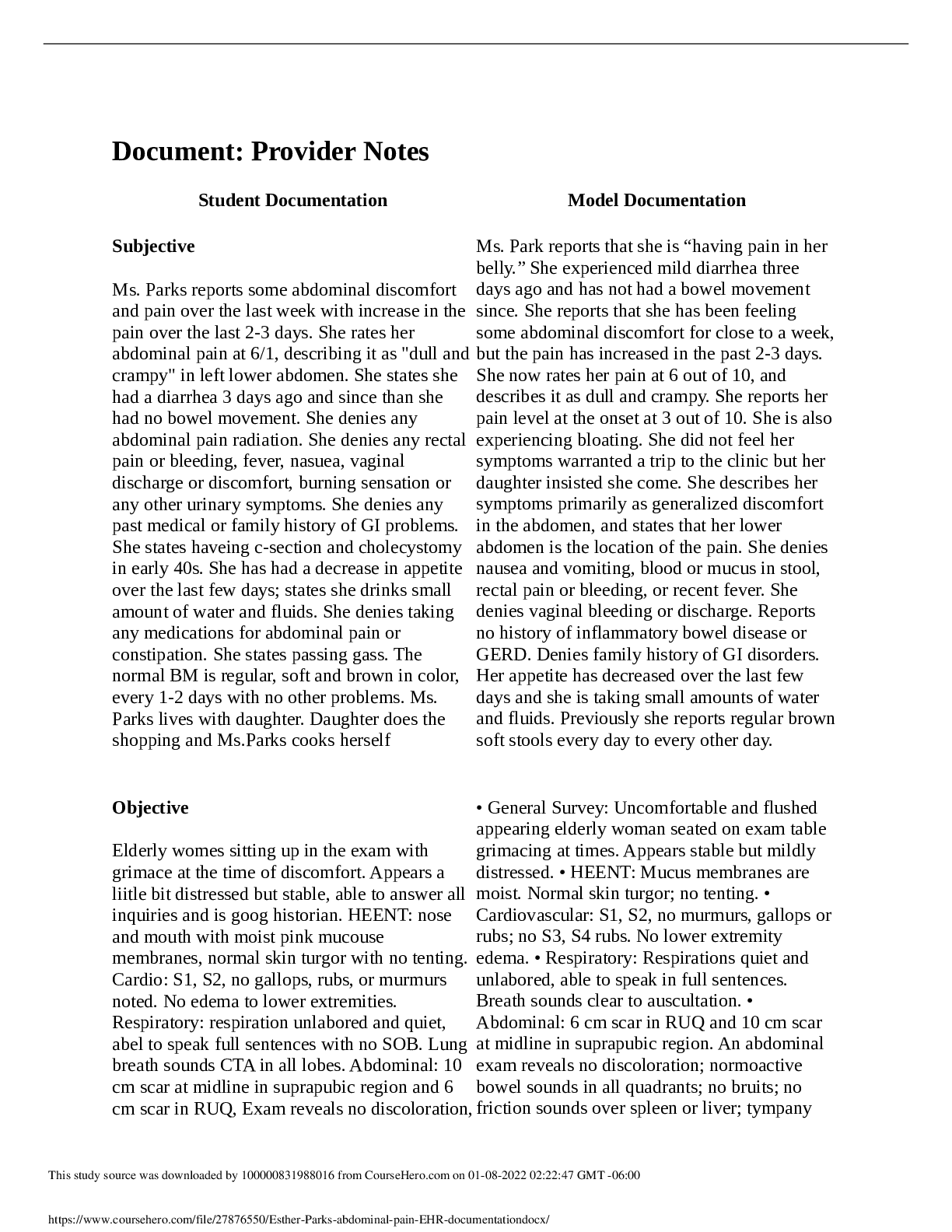
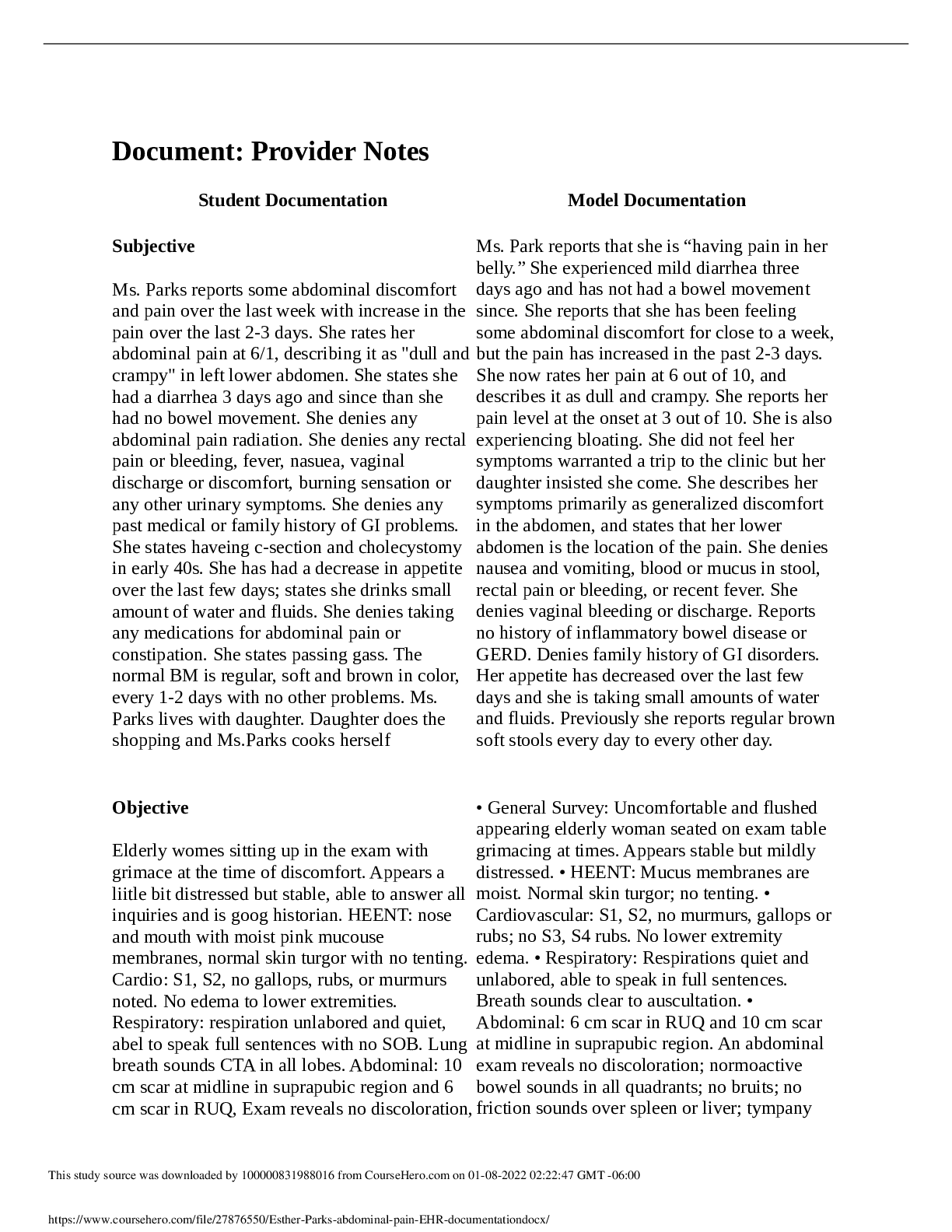
Document: Provider Notes Student Documentation Model Documentation Subjective Ms. Parks reports some abdominal discomfort and pain over the last week with increase in the pain over the last 2-3 d ... ays. She rates her abdominal pain at 6/1, describing it as "dull and crampy" in left lower abdomen. She states she had a diarrhea 3 days ago and since than she had no bowel movement. She denies any abdominal pain radiation. She denies any rectal pain or bleeding, fever, nasuea, vaginal discharge or discomfort, burning sensation or any other urinary symptoms. She denies any past medical or family history of GI problems. She states haveing c-section and cholecystomy in early 40s. She has had a decrease in appetite over the last few days; states she drinks small amount of water and fluids. She denies taking any medications for abdominal pain or constipation. She states passing gass. The normal BM is regular, soft and brown in color, every 1-2 days with no other problems. Ms. Parks lives with daughter. Daughter does the shopping and Ms.Parks cooks herself Ms. Park reports that she is “having pain in her belly.” She experienced mild diarrhea three days ago and has not had a bowel movement since. She reports that she has been feeling some abdominal discomfort for close to a week, but the pain has increased in the past 2-3 days. She now rates her pain at 6 out of 10, and describes it as dull and crampy. She reports her pain level at the onset at 3 out of 10. She is also experiencing bloating. She did not feel her symptoms warranted a trip to the clinic but her daughter insisted she come. She describes her symptoms primarily as generalized discomfort in the abdomen, and states that her lower abdomen is the location of the pain. She denies nausea and vomiting, blood or mucus in stool, rectal pain or bleeding, or recent fever. She denies vaginal bleeding or discharge. Reports no history of inflammatory bowel disease or GERD. Denies family history of GI disorders. Her appetite has decreased over the last few days and she is taking small amounts of water and fluids. Previously she reports regular brown soft stools every day to every other day. Objective Elderly womes sitting up in the exam with grimace at the time of discomfort. Appears a liitle bit distressed but stable, able to answer all inquiries and is goog historian. HEENT: nose and mouth with moist pink mucouse membranes, normal skin turgor with no tenting. Cardio: S1, S2, no gallops, rubs, or murmurs noted. No edema to lower extremities. Respiratory: respiration unlabored and quiet, abel to speak full sentences with no SOB. Lung breath sounds CTA in all lobes. Abdominal: 10 cm scar at midline in suprapubic region and 6 cm scar in RUQ, Exam reveals no discoloration, • General Survey: Uncomfortable and flushed appearing elderly woman seated on exam table grimacing at times. Appears stable but mildly distressed. • HEENT: Mucus membranes are moist. Normal skin turgor; no tenting. • Cardiovascular: S1, S2, no murmurs, gallops or rubs; no S3, S4 rubs. No lower extremity edema. • Respiratory: Respirations quiet and unlabored, able to speak in full sentences. Breath sounds clear to auscultation. • Abdominal: 6 cm scar in RUQ and 10 cm scar at midline in suprapubic region. An abdominal exam reveals no discoloration; normoactive bowel sounds in all quadrants; no bruits; no friction sounds over spleen or liver; tympany This study source was downloaded by 100000831988016 from CourseHero.com on 01-08-2022 02:22:47 GMT -06:00 https://www.coursehero.com/file/27876550/Esther-Parks-abdominal-pain-EHR-documentationdocx/ Student Documentation Model Documentation bowel sounds WNL in all quadrants; no friction sounds over spleen or liver, no bruits in any areas; tympany presides; Liver span at 7 cm; Guarding to light touch at LLQ; 2x4 mass in LLQ with deep palpation; strong sphincter tone, fecal mass detected in rectal vault. GU: bilateral kindey nontender; urine clear and dark yellow, normal odor, no nitrites, WBCs, RBCs, or keatones, pH 6.5, SG 1.017. presides with scattered dullness over LLQ; abdomen soft in all quadrants; an oblong mass is noted in the LLQ with mild guarding, distension; no organomegaly; no CVA tenderness; liver span 7 cm @ MCL; no hernias. • Rectal: No hemorrhoids, no fissures or ulceration; strong sphincter tone, fecal mass in rectal vault. • Pelvic: No inflammation or irritation of vulva, abnormal discharge, or bleeding; no masses, growths, or tenderness upon palpation. • Urinalysis: Urine clear, dark yellow, normal odor. No nitrites, WBCs, RBCs, or ketones detected; pH 6.5, SG 1.017. Assessment Primary: Constipation Secondary: Small Bowel Obstruction Mrs. Park’s bowel sounds are normoactive in all quadrants, with no bruits or friction sounds. Scattered dullness in LLQ during percussion is suggestive of feces in the colon; otherwise, her abdomen is tympanic. Her abdomen is soft to palpation; mild guarding and oblong mass suggesting feces were discovered in LLQ. No CVA tenderness; liver span 7 cm @ MCL; no splenic dullness. Digital rectal exam revealed a fecal mass in the rectal vault. No abnormalities were noted during the pelvic exam, so pelvic inflammatory disease is not suspected. Ms. Park’s urinalysis was normal, which rules out a urinary tract infection. No signs of dehydration or cardiovascular abnormalities. Mrs. Park’s symptoms and health history suggest she has constipation. Differential diagnoses are constipation, diverticulitis, and intestinal obstruction. Plan Encourage to drink more fluids at tleast 8-10 glasses water a day Encourage to drink prune juice Prescription for stool softener Docuset 100 mg BID PO Abdominal x-ray Abdominal CAT scan Blood draw CBC, BMP, Hep/Lip panel Mrs. Park should receive diagnostic tests to rule out differentials: CBC to assess for elevated WBCs associated with diverticulitis, electrolyte profile to evaluate electrolyte and fluid status, and a CT scan to assess for obstruction. If Mrs. Park has diverticulitis I recommend IV fluids and bowel rest. If she has bowel obstruction, I recommend NPO, IV fluids, and general This study source was downloaded by 100000831988016 from CourseHero.com on 01-08-2022 02:22:47 GMT -06:00 https://www.coursehero.com/file/27876550/Esther-Parks-abdominal-pain-EHR-documentationdocx/ Student Documentation Model Documentation surgical consult. If she has constipation, I recommend that she increase fluids, increase fiber, and increase activity as tolerated. [Show More]
Last updated: 3 years ago
Preview 1 out of 3 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
Esther Parks Abdominal Pain Care Plan,subjective data collection,Objective Data&EHR documentation
Focused Exam: Abdominal Pain Results | Turned In Health Assess - Spring 1 2020, 322301 Return to Assignment (/assignments/289775/) Care Plan : 13 of 13 (100.0%) Nursing Diagnoses: Definitions & Cl...
By Nutmegs 4 years ago
$30
4
Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 08, 2022
Number of pages
3
Written in
All
Additional information
This document has been written for:
Uploaded
Jan 08, 2022
Downloads
0
Views
201