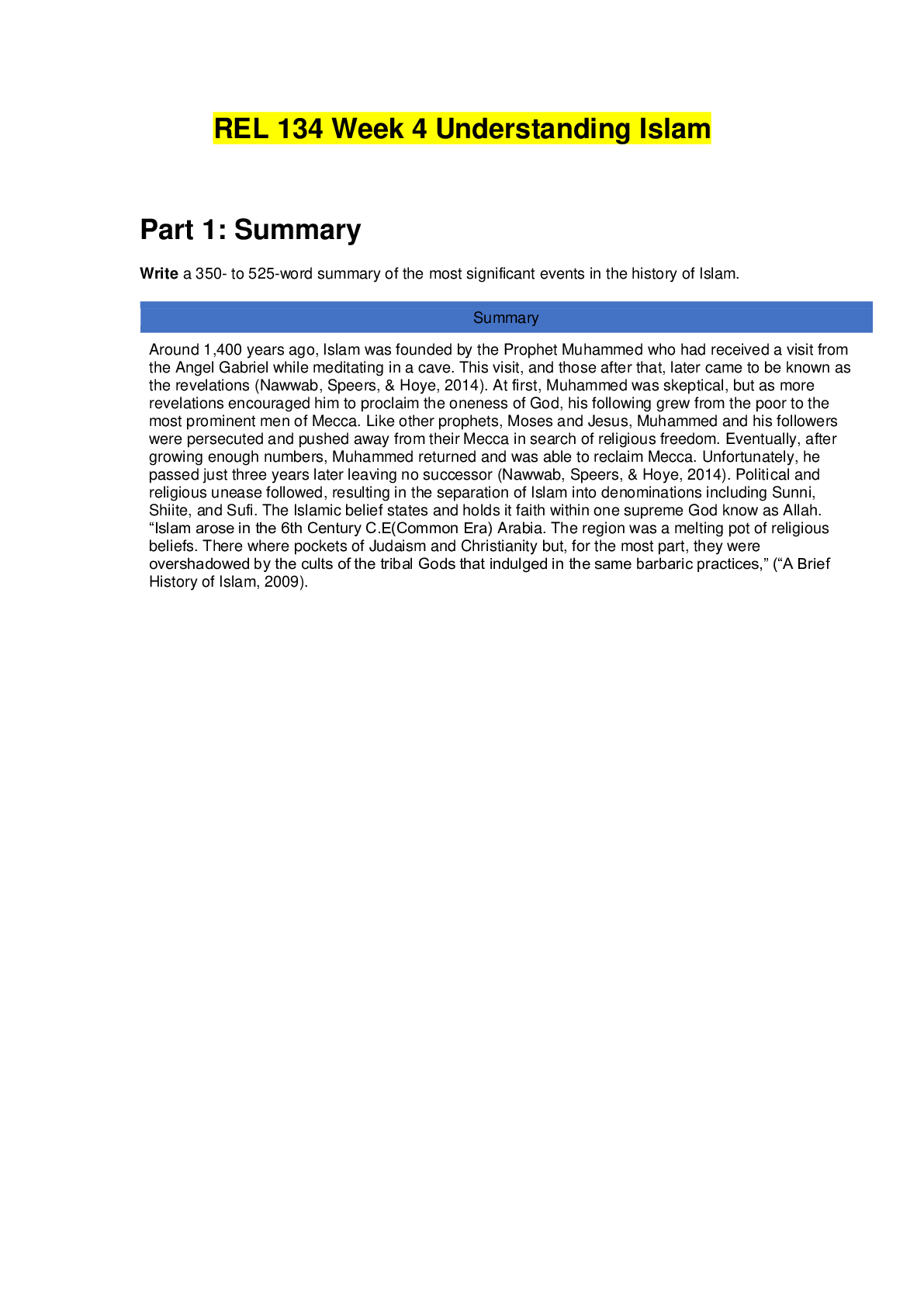
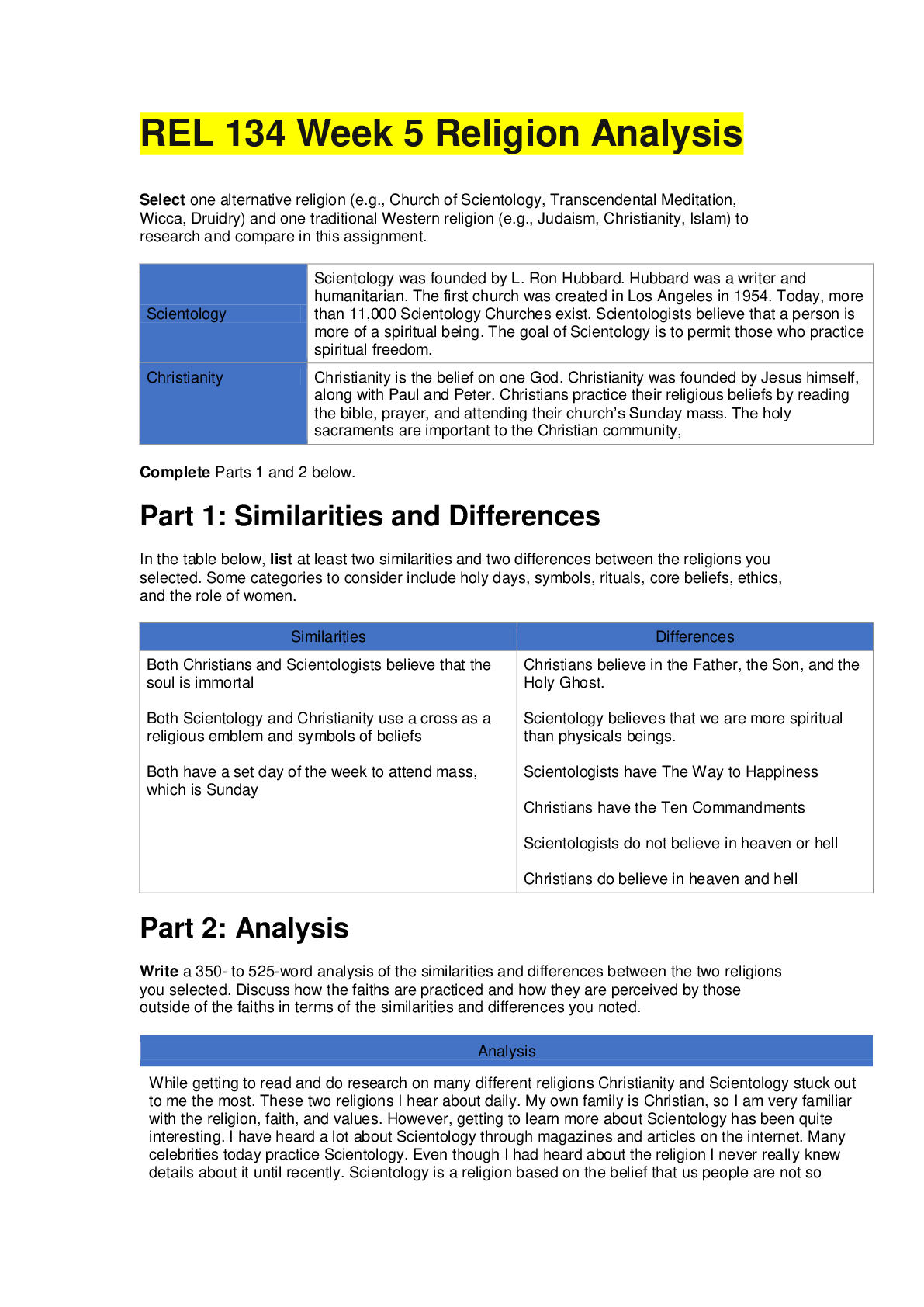
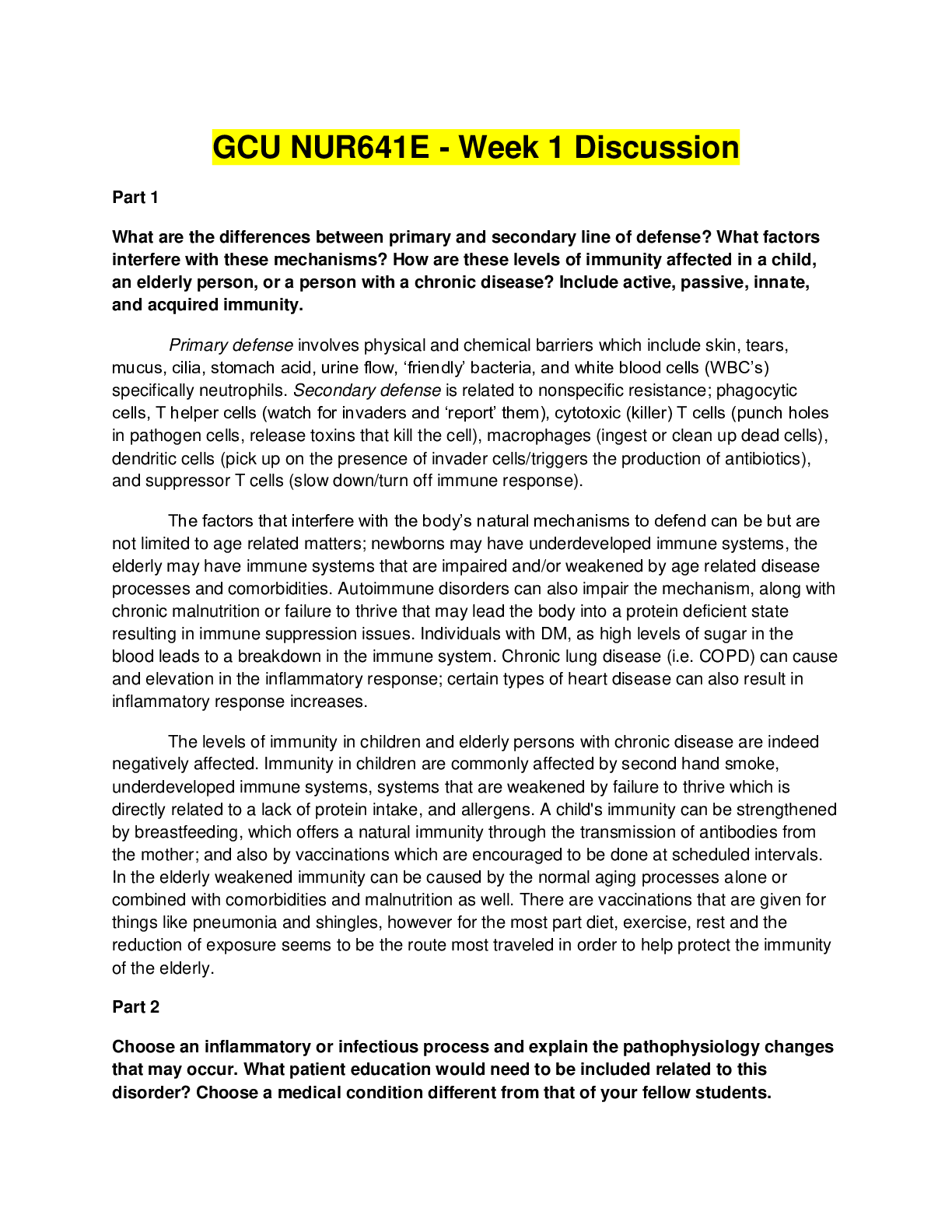
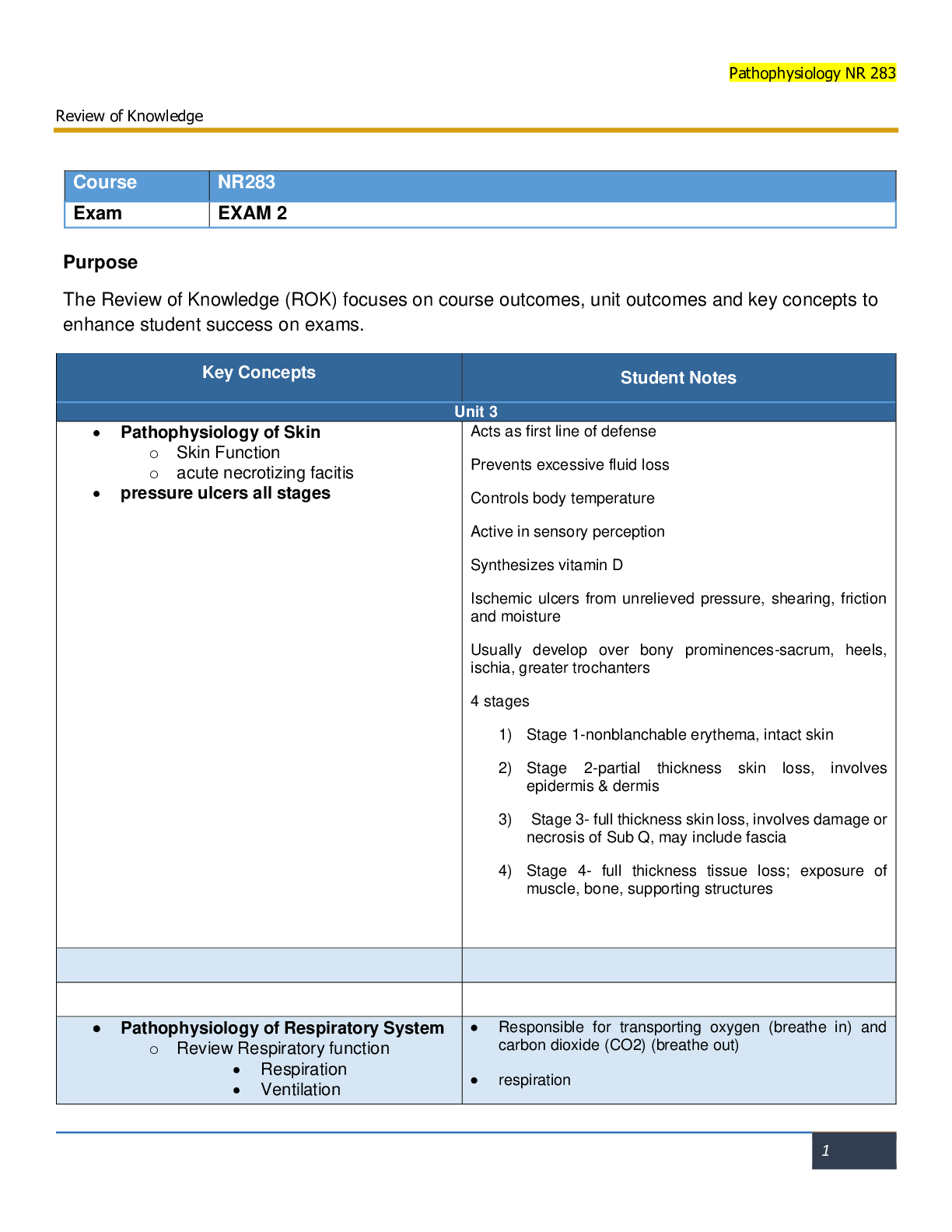
*NURSING > STUDY GUIDE > NR 507 week7 notes |NR 507 Advanced Pathophysiology Week 7 Outline, detailed full complete guide, Fa (All)
NR 507 week7 notes |NR 507 Advanced Pathophysiology Week 7 Outline, detailed full complete guide, Fall 2020.
Document Content and Description Below
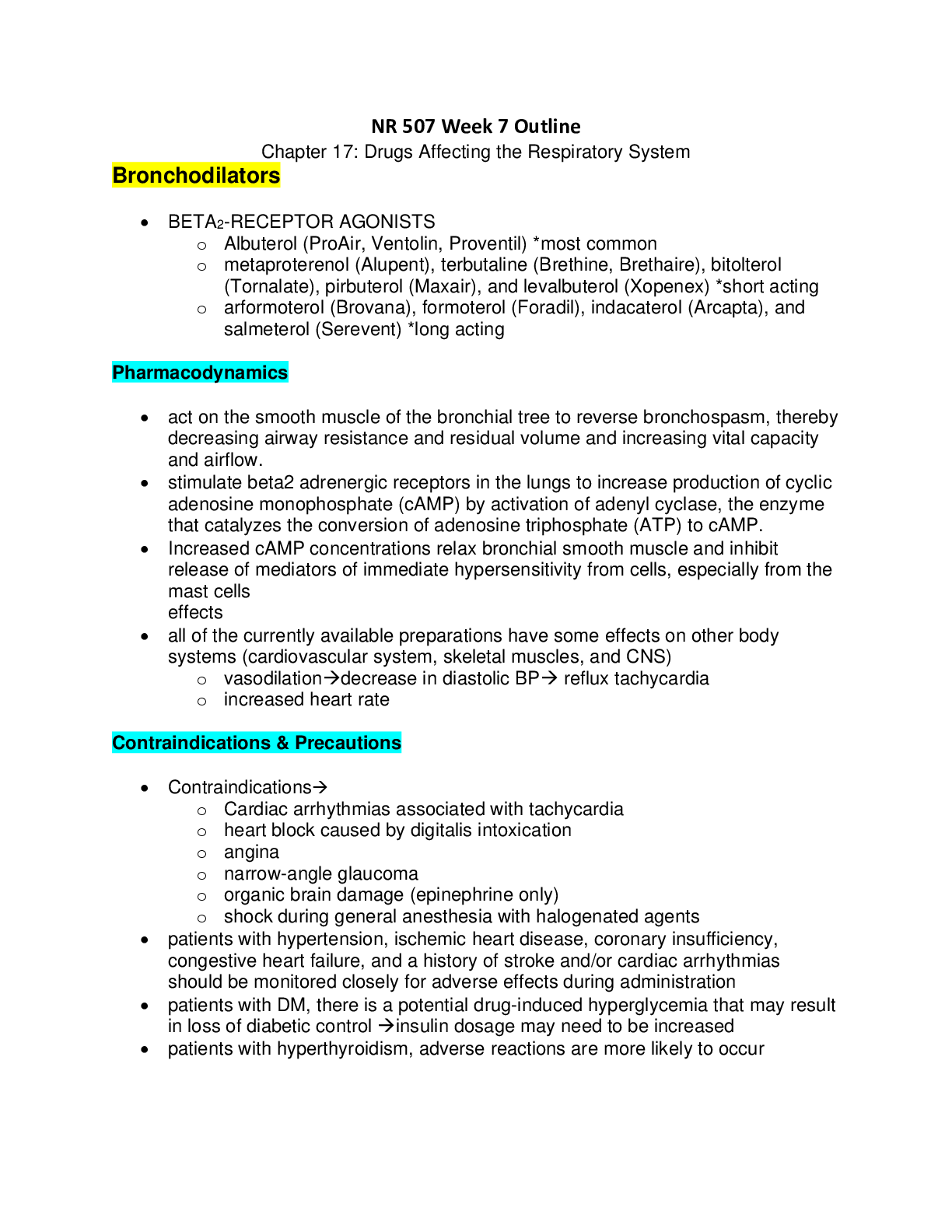
Week 7 Outline Chapter 17: Drugs Affecting the Respiratory System Bronchodilators • BETA2-RECEPTOR AGONISTS o Albuterol (ProAir, Ventolin, Proventil) *most common o metaproterenol (Alupent), t ... erbutaline (Brethine, Brethaire), bitolterol (Tornalate), pirbuterol (Maxair), and levalbuterol (Xopenex) *short acting o arformoterol (Brovana), formoterol (Foradil), indacaterol (Arcapta), and salmeterol (Serevent) *long acting Pharmacodynamics • act on the smooth muscle of the bronchial tree to reverse bronchospasm, thereby decreasing airway resistance and residual volume and increasing vital capacity and airflow. • stimulate beta2 adrenergic receptors in the lungs to increase production of cyclic adenosine monophosphate (cAMP) by activation of adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cAMP. • Increased cAMP concentrations relax bronchial smooth muscle and inhibit release of mediators of immediate hypersensitivity from cells, especially from the mast cells effects • all of the currently available preparations have some effects on other body systems (cardiovascular system, skeletal muscles, and CNS) o vasodilationdecrease in diastolic BP reflux tachycardia o increased heart rate Contraindications & Precautions • Contraindications o Cardiac arrhythmias associated with tachycardia o heart block caused by digitalis intoxication o angina o narrow-angle glaucoma o organic brain damage (epinephrine only) o shock during general anesthesia with halogenated agents • patients with hypertension, ischemic heart disease, coronary insufficiency, congestive heart failure, and a history of stroke and/or cardiac arrhythmias should be monitored closely for adverse effects during administration • patients with DM, there is a potential drug-induced hyperglycemia that may result in loss of diabetic control insulin dosage may need to be increased • patients with hyperthyroidism, adverse reactions are more likely to occur • Patients taking digoxin require close monitoring when albuterol is started because it increases the volume of distribution of digoxin and can cause up to a 30% decrease in blood digoxin levels. • FDA released a safety announcement regarding LABAs (Long acting beta agonists) o To ensure the safe use of these products: Single-ingredient LABAs should only be used in combination with an asthma controller medication; they should not be used alone. should only be used long-term in patients whose asthma cannot be adequately controlled on asthma controller medications. should be used for the shortest duration of time required to achieve control of asthma symptoms and discontinued, if possible, once asthma control is achieved. Patients should then be maintained on an asthma controller medication. Pediatric and adolescent patients who require the addition of a LABA to an inhaled corticosteroid should use a combination product containing both an inhaled corticosteroid and a LABA, to ensure compliance with both medications ADR • usually transient temporary reduction in dose may alleviate some of the side effects • palpitations • supraventricular & ventricular ectopic beats • CNS excitation tremors, dizziness, shakiness, nervousness, and restlessness • headache Drug interactions • digitalis glycosides increased risk of cardiac arrhythmiasmonitor ECG carefully • Beta agonists used with beta-adrenergic blocking agents (including ophthalmic preparations) may result in mutual inhibition of therapeutic effects • Tricyclic antidepressants and MAOIs used with albuterol, metaproterenol, or terbutaline may potentiate the effects of the bronchodilator on the vascular system. • Hypokalemia or electrocardiogram changes may be seen with coadministration of the beta agonists with drugs that lower the potassium level, such as diuretics. Clinical Use and Dosing • Bronchospasm: most often associated with asthma, bronchitis (acute or chronic), and COPD o dose of albuterol metered-dose inhaler (MDI) in children over age 4 years and adults is two puffs every 4 to 6 hours albuterol (Ventolin, Proventil) o delivered via nebulizer for children over age 12 years as well as for adults is 2.5 mg (0.5 mL) in 2 mL normal saline; for younger children up to 15 kg, the dose is 0.1 to 0.15 mg/kg per dose. o Inhaled forms of albuterol may be repeated once after 5 to 10 minutes, up to 2 times (three doses total) during exacerbations. o oral albuterol dose in adults is 2 to 4 mg 3 or 4 times a day, up to a maximum of 32 mg/day. For children aged 6 to 12, 2 mg albuterol 3 or 4 times a day may be prescribed, (oral albuterol is rarely used in children) o Aformoterol is not approved for use in children and should not be used for acute asthma exacerbation o recommended dose of levalbuterol (Xopenex) inhalation solution in adolescents over age 12 years and adults is 0.63 mg 3 times a day, every 6 to 8 hours. Dosing for children aged 6 to 11 is 0.31 mg 3 times a day per the manufacturer's label, with routine dosing not to exceed 0.63 mg 3 times a day. o Salmeterol is not to be used for short-term bronchospasm relief. If prescribing salmeterol for persistent asthma, the drug must be prescribed in conjunction with an inhaled corticosteroid or other asthma controller medication o Hospital admission may be avoided by the addition of ipratropium to the treatment regimen in cases of exacerbation seen in the clinic or emergency department. o Ipratropium is the bronchodilator of choice in patients who are taking beta blockers or who do not tolerate beta2 agonists. • Exercise-Induced Bronchospasm: o used just before exercise can prevent exercise-induced bronchospasm o inhaled albuterol or other short-acting beta2 agonist and salmeterol o albuterol MDI to prevent EIB is two puffs 15 minutes prior to exercise, should prevent EIB for 2 to 3 hours. o The dose of salmeterol is two puffs 30 to 60 minutes prior to exercise. should prevent EIB for 10 to 12 hours. o Salmeterol and other long-acting beta2 agonists have a shortened duration of action if used on a daily basis Rational Drug Selection • the only short-acting bronchodilators that can be prescribed for children under age 4 are albuterol and metaproterenol. • Levalbuterol is labeled to be used in children older than age 4 • Albuterol is by far the most often used medication in clinical practice and is safe to use even in infants • albuterol is the least expensive, especially if a generic formula is prescribed Patient Education • Overuse of bronchodilators will lead to increased adverse effects • using less than prescribed may lead to increased bronchospasm and decreased pulmonary function. • MDILearning to coordinate the release of the medication from the inhaler with a deep breath is difficult • patient should first exhale and then tilt the head slightly back and place the inhaler mouthpiece either about 2 inches from the open mouth or between the open lips. While inhaling, the patient should press down on the canister, breathe in slowly and deeply, and hold his or her breath for 10 seconds (count of 10) or as long as comfortable. • If two puffs are prescribed, then the patient should wait at least 1 full minute between inhalations. • The Foradil capsule is placed into the aerolizer, then the aerolizer is squeezed to break the capsule. The patient inhales the medication.Patients should receive clear instructions not to swallow the capsule • The patient needs to self-monitor respiratory status with a peak flowmeter to determine the effectiveness of the prescribed medication. • The patient should avoid or quit smoking. • The patient should avoid environmental triggers for asthma at home, work, and school. Xanthine Derivatives • Methylxanthines o theophylline o aminophylline o caffeine Pharmacodynamics • believed to be mediated by selective inhibition of specific phosphodiesterases (PDEs). produces an increase in cAMP, leads to bronchial smooth muscle and pulmonary vessel relaxation • Theophylline and caffeine have an impact on most of the major body systems. o powerful CNS stimulants, often causing insomnia and excitability o Theophylline directly stimulates the myocardium and increases myocardial contractility and heart rate. o By relaxing vascular smooth muscle, theophylline dilates the coronary, pulmonary, and systemic blood vessels. o Both theophylline and caffeine increase gastric acid secretion and may produce nausea and vomiting, reaction is probably due to CNS effect o Theophylline acts directly on the renal tubules to cause increased sodium and chloride excretion. o By increasing renal blood flow (from increased heart rate) and the glomerular filtration rate, theophylline and caffeine also cause diuresis. Precautions and Contraindications • true contraindications to theophylline are hypersensitivity to any xanthine, peptic ulcer disease, and underlying seizure disorder. • Contraindications to caffeine include hypersensitivity to caffeine and use of caffeine sodium benzoate formulation in neonates • patients with hypertension, ischemic heart disease, coronary insufficiency, congestive heart failure, or a history of stroke and cardiac arrhythmias should be monitored closely for adverse effects while taking theophylline • Excessive doses may lead to toxicity. Incidence of toxicity increases when serum theophylline levels are above 20 mcg/mL. Toxicity is found if serum theophylline levels reach 25 mcg/mL in 75% of patients. • Toxicity should not occur at recommended dosages but may occur if theophylline clearance is decreased (hepatic impairment, chronic lung disease, cardiac failure, patients older than age 55, and infants under age 1 year). Theophylline clearance may be decreased in patients over age 55. • Theophylline is used to treat apnea in preterm infants, with a therapeutic serum theophylline range of 5 to 10 mcg/mL Infants younger than 1 year have decreased theophylline clearance and should have close monitoring of serum theophylline levels. Adverse Drug Reactions • The CNS adverse effects that may be seen include irritability, restlessness, seizures, and insomnia. • Gastroesophageal reflux may occur. • The cardiovascular adverse effects that may occur include palpitations, tachycardia, hypotension, and life-threatening arrhythmias. • Other adverse effects include rash, diuresis, and tachypnea • serum theophylline levels above 20 mcg/mL, patients may experience nausea, vomiting, diarrhea, headache, insomnia, and irritability. • At levels above 35 mcg/mL, the patient may have hyperglycemia, hypotension, cardiac arrhythmias, tachycardia, seizures, brain damage, and death • Adverse effects of caffeine include cardiac arrhythmias, tachycardia, insomnia, agitation, irritability, headache, nausea, vomiting, and gastric irritation. Food/Drug Interactions • smoking tobacco increases theophylline clearance. o Theophylline levels should be monitored closely if the patient begins or quits smoking while on theophylline. o Nicotine replacement products (gum or patch) also affect theophylline clearance. o Theophylline clearance may not return to normal for 3 months to 2 years after smoking cessation • sedative effects of benzodiazepines may be antagonized by theophylline. • Concurrent use of theophylline with beta2-agonist bronchodilators may result in additive toxicity. • Lithium levels may be reduced by theophylline. • The concurrent use of tetracyclines with theophylline may lead to an increased incidence of theophylline adverse reactions • A diet that is low in carbohydrates and high in protein increases the elimination (shortens the half-life) of theophylline. • A diet high in carbohydrates and low in protein decreases the elimination (lengthens the half-life) of theophylline. • A diet that contains a lot of charcoal-broiled foods accelerates the hepatic metabolism of theophylline because of the high polycyclic hydrocarbon content. • cimetidine, ketoconazole, fluconazole, mexiletine, and phenylpropanolamine may impair caffeine metabolism, leading to increased serum levels. • Caffeine elimination may be increased by coadministration of phenobarbital and phenytoin Clinical Use and Dosing • Theophylline and COPD o Theophylline is not recommended for first-line therapy in the COPD patient, although if the patient has been stable on theophylline, there is no reason to discontinue the medication as long as serum theophylline levels are monitored o The adult patient >16 is started on a dose of 6 mg/kg per 24 hours or 400 mg/24 hours, whichever is less, divided at 6 to 8 hour intervals. The dose is increased every 3 days in 25% increments until the desired serum theophylline levels are achieved (ideally between 10 and 20 mcg/mL). o Dosing adjustments are made based on the serum theophylline level. o If the level is 5 to 10 mcg/mL, then the dose of theophylline is increased by 25% every 3 days until desired serum concentrations of theophylline are reached. o If the serum concentration is between 10 and 15 mcg/mL, maintain dosage if tolerated and recheck at 6 to 12 month intervals. o If the serum theophylline level is 15 to 19.9 mcg/mL, consider decreasing the dose by 10% to provide a greater margin of safety. o If the serum theophylline level is 20 to 25 mcg/mL, then decrease the dose by 10% and recheck the level in 3 days. o If the serum level is 25 to 30 mcg/mL, skip the next dose and decrease subsequent doses by 25%; redraw the theophylline level in 3 days. o If the theophylline level is above 30 mcg/mL, then skip the next two doses and decrease the dose by 50%; recheck in 3 days. • Apnea of prematurity o A loading dose of caffeine citrate 10 to 20 mg/kg is given in the treatment of apnea of prematurity, with a maintenance dose of 5 mg/kg per day. o If theophylline has been given to the patient in the previous 3 days, the loading dose is decreased by 50% to 70%. o If theophylline is used to treat apnea of prematurity, the patient is given a loading dose of 4 mg/kg per dose, with a maintenance dose of 4 mg/kg per day in the premature infant or newborn up to age 6 weeks. Rational Drug Selection • immediate-release, timed-release, and liquid formulas • Capsules that can be opened and sprinkled on soft foods are convenient for some patients. Patient Education • Missed doses or irregular timing of doses can cause wide variations in the serum theophylline level, resulting in either subtherapeutic or toxic levels. • The patient may take the medication either with or without food, but consistency is important because food can alter the absorption of the medication. • Patients who are having signs of toxicity may mistakenly think they have a viral illness. Instead, patients with any unusual symptoms should contact their provider. The symptoms to report include nausea, vomiting, insomnia, jitteriness, headache, rash, severe GI pain, restlessness, convulsions, or irregular heartbeat. • avoid large amounts of caffeine-containing beverages, which can increase the adverse effects of theophylline Anticholinergics • Ipratropium bromide (Atrovent) • Tiotropium bromide (Spiriva) and aclidinium bromide (Tadorza Pressair) --inhaled Pharmacodynamics • acts to block the muscarinic cholinergic receptors by antagonizing the action of acetylcholine. • Blocking the cholinergic receptors decreases the formation of cyclic guanosine monophosphate (cGMP), which leads to decreased contractility of the smooth muscle of the lungs, probably because of the actions of cGMP on intracellular calcium. • amount of bronchodilation caused by ipratropium inhalation is thought to reflect the level of parasympathetic tone. • When inhaled, ipratropium's actions are confined to the mouth and airways. ************************************************************CONTINUED*********************************************** [Show More]
Last updated: 3 years ago
Preview 1 out of 118 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 16, 2020
Number of pages
118
Written in
All
Additional information
This document has been written for:
Uploaded
Oct 16, 2020
Downloads
0
Views
90