Test Bank For Mastering Competencies in Family Therapy 4th International Edition By Diane R. Gehart
$ 30
Solutions manual For Modern Compressible Flow With Historical Perspective 4th Indian Edition By John Anderson
$ 30

ATI MATERNAL NEWBORN PROCTORED 2019
$ 12
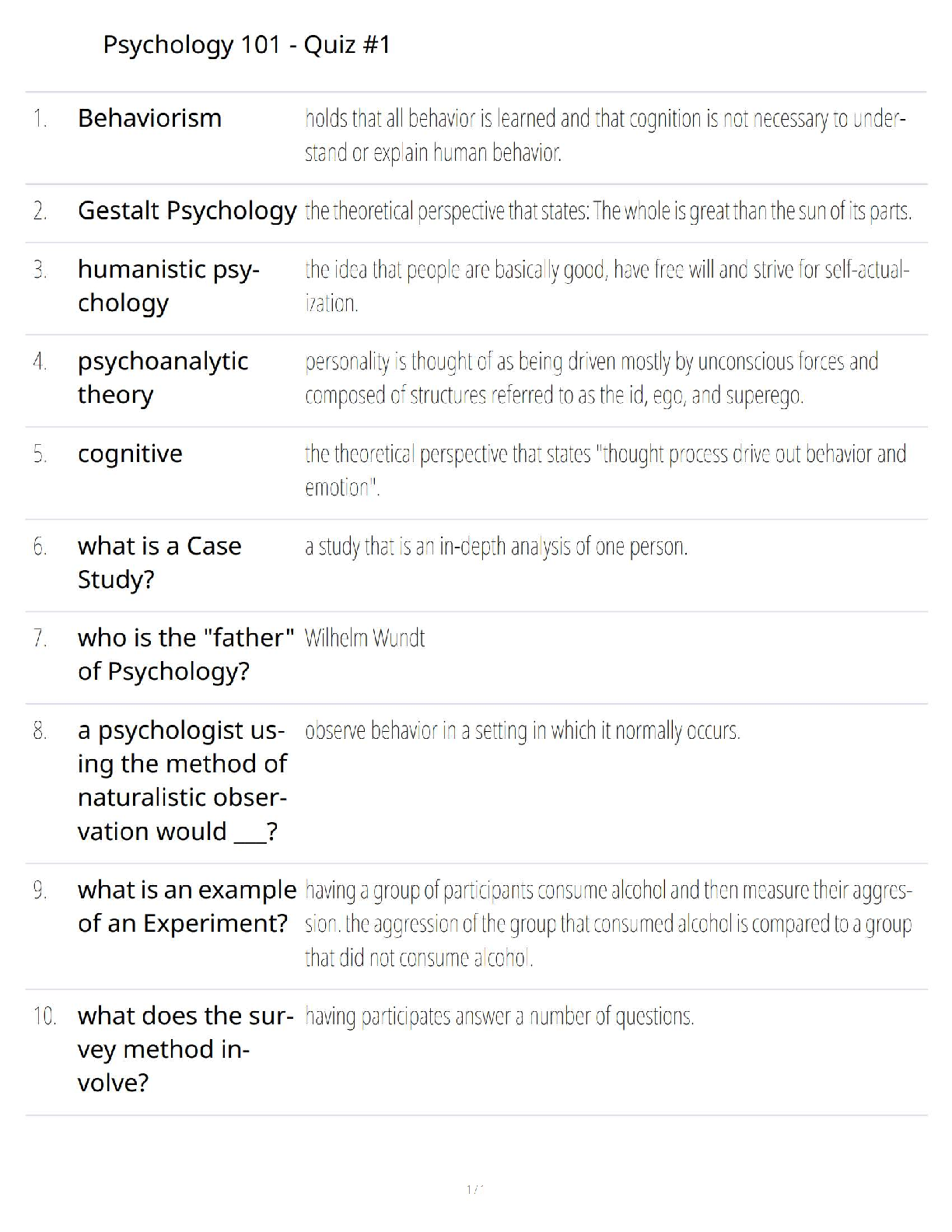
Psychology 101 Quiz 1 Study Guide: Score 100% with Correct Answers – Updated 2025/2026 Version
$ 15
Test_Bank_for_Introduction_to_Clinical_Pharmacology,_11th_Edition
$ 15
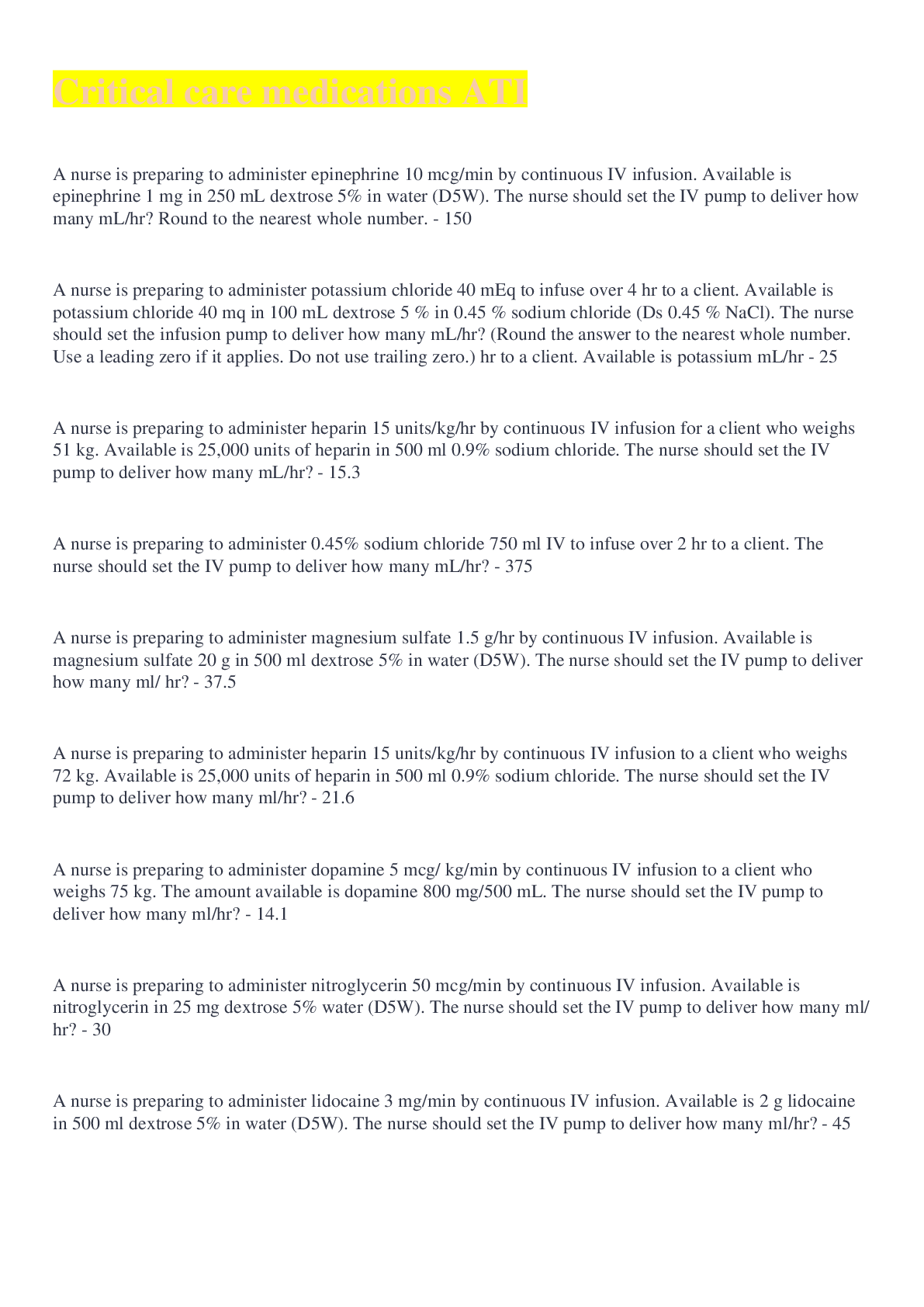
Critical care medications ATI 2022 Med math fully solved
$ 11
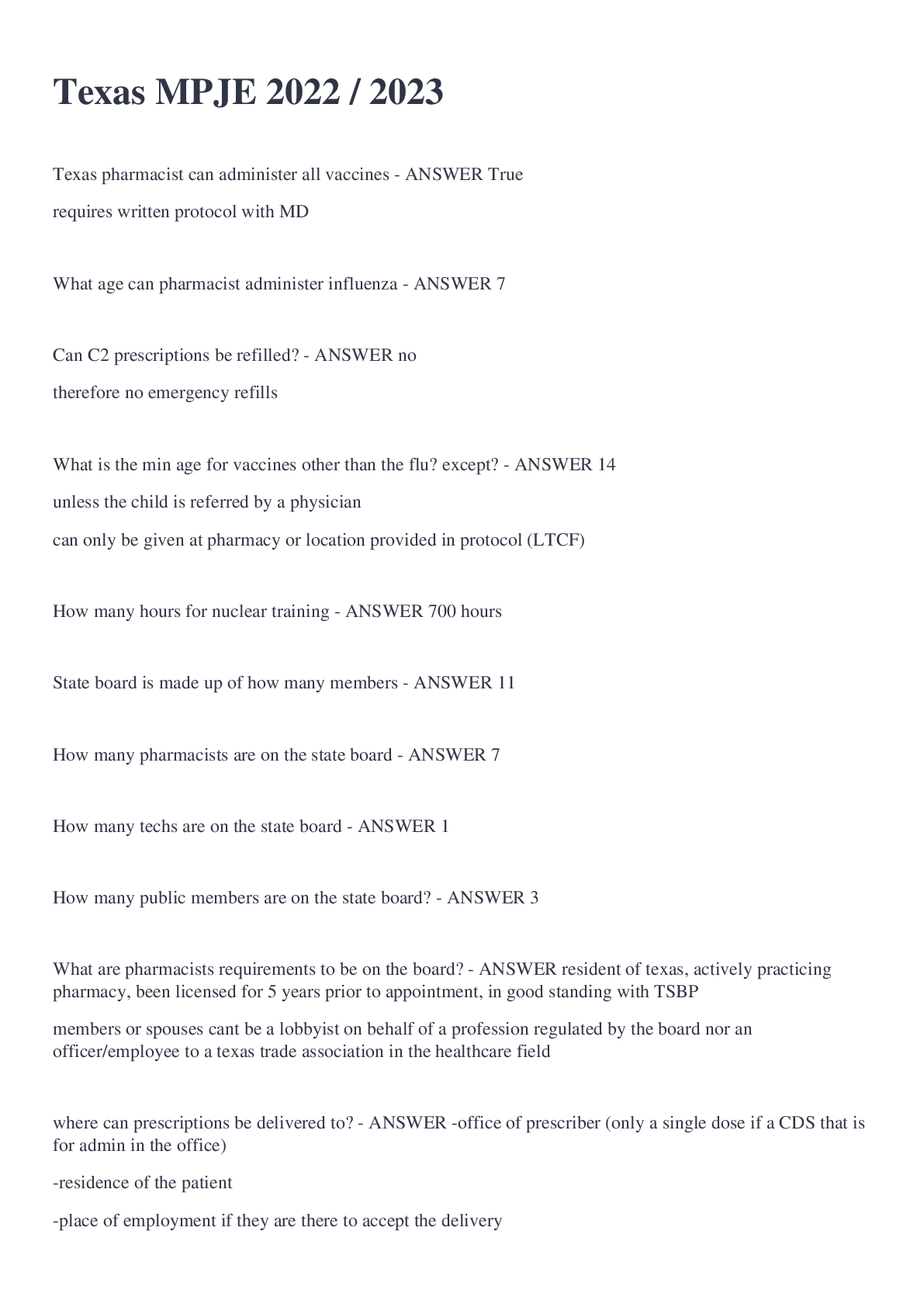
Texas MPJE Exam 2022/2023 Q&A Solved 100% Correct
$ 10
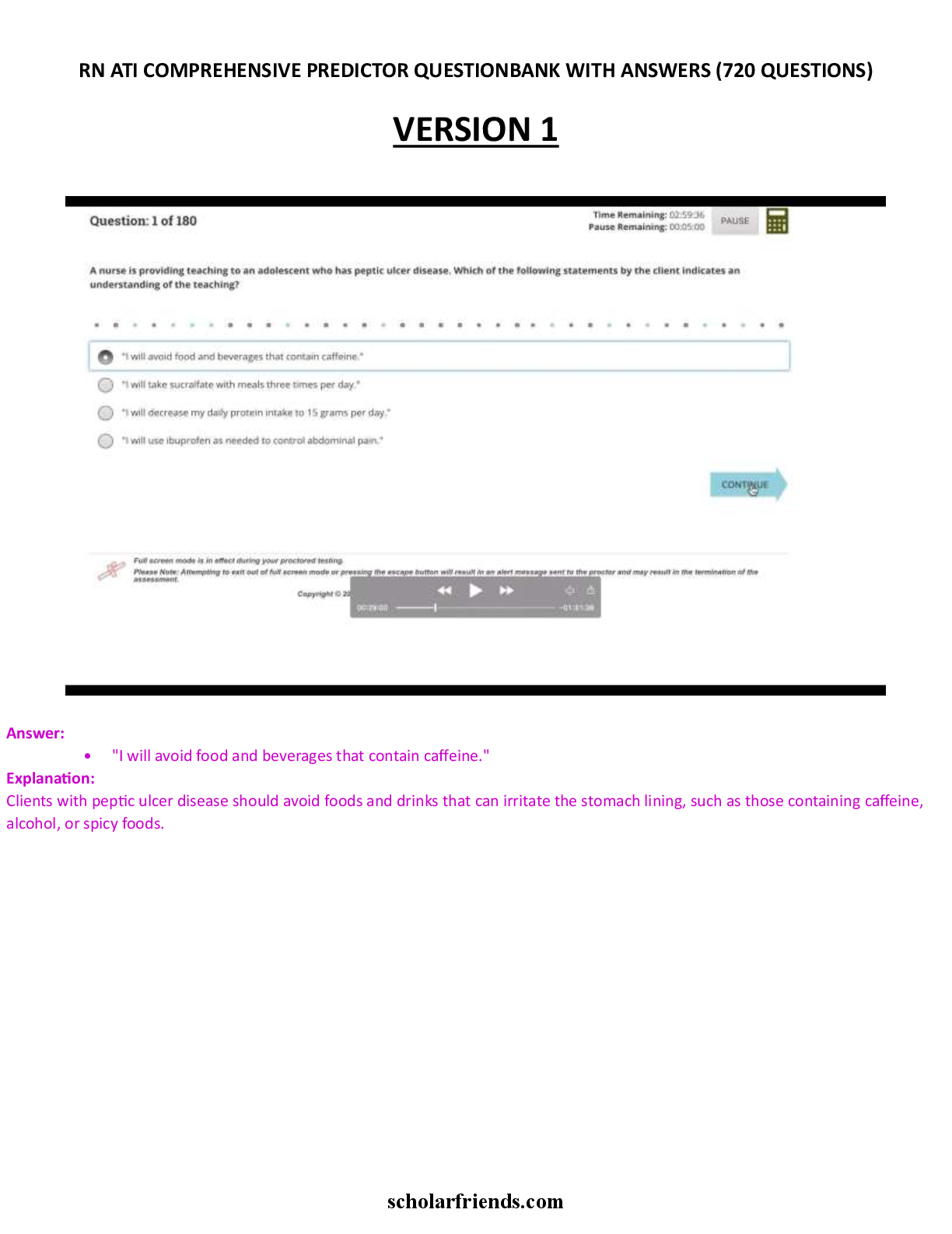
ATI RN Comprehensive Predictor Question Bank (720QAs)
$ 29.5
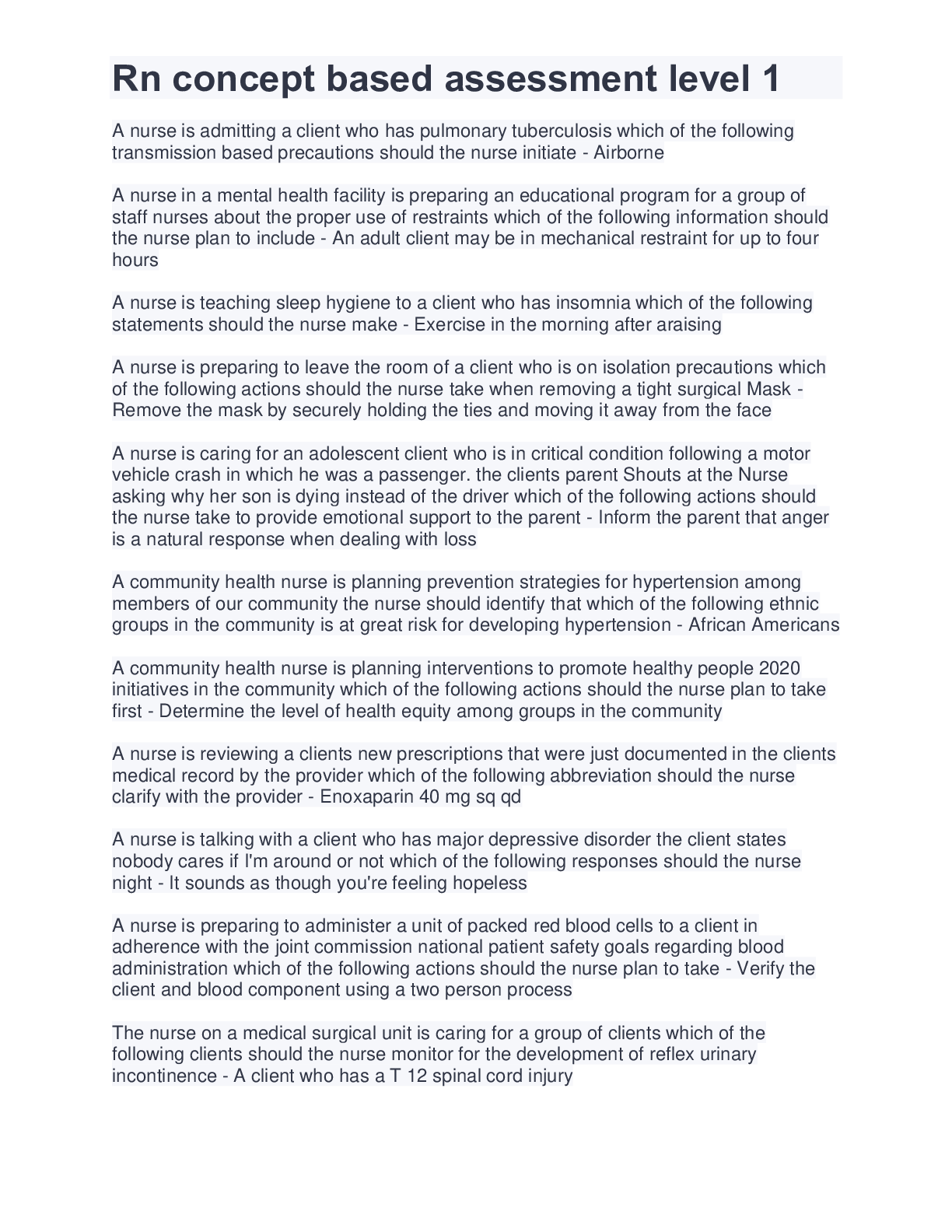
RN CONCEPT BASED ASSESSMENT LEVEL 1 ONLINE PRACTICE QUESTIONS AND ANSWERS( COMPLETE SOLUTION RATED A)
$ 11
.png)
Arkansas Esthetics State Board Written Test #1 Questions and Answers Graded A+
$ 10

[SOLVED] HIEU 201 / HIEU201 Chapter 10 Quiz (LATEST 2022 Graded A+)
$ 10
ACCUPLACER TEST STUDY GUIDE 2024 COMPLETE STUDY GUIDE ALL SUBJECTS INCLUDED WITH PRACTICE QUESTIONS AND CORRECT ANSWERS
$ 19

SOLUTION TO END OF CHAPTER EXERCISES FOR: Introduction to Econometrics, 3rd Edition James H. Stock, and Mark W. Watson. Questions And Answers
$ 13

ATI Leadership Proctored Exam 2020
$ 10.5

ATI TEAS Study Guide
$ 13

ATI Med surg 2 exam1 2022 UPDATED
$ 16

Answered Quiz Version 1 - Integration Study Guide 2022. Liberty University
$ 16.5
.png)
Esthetics State Board Exam California 2022/2023 Graded A
$ 10

Educational Research Qualitative, Quantitative, and Mixed Methods Approaches Seventh Edition by R. Burke Johnson solutions
$ 22
D027 WGU | 80 QUESTIONS AND ANSWERS
$ 12
Test-Bank-Principles-Of-Human-Physiology-
$ 18
Google Analytics Certification 2024 / GAIQ Exam Prep / GA4 & Universal Analytics Test Bank / Pass Guaranteed
$ 18.5

AVIA 245 Quiz 4 Liberty > Latest fall 2020, all answers correct.
$ 7
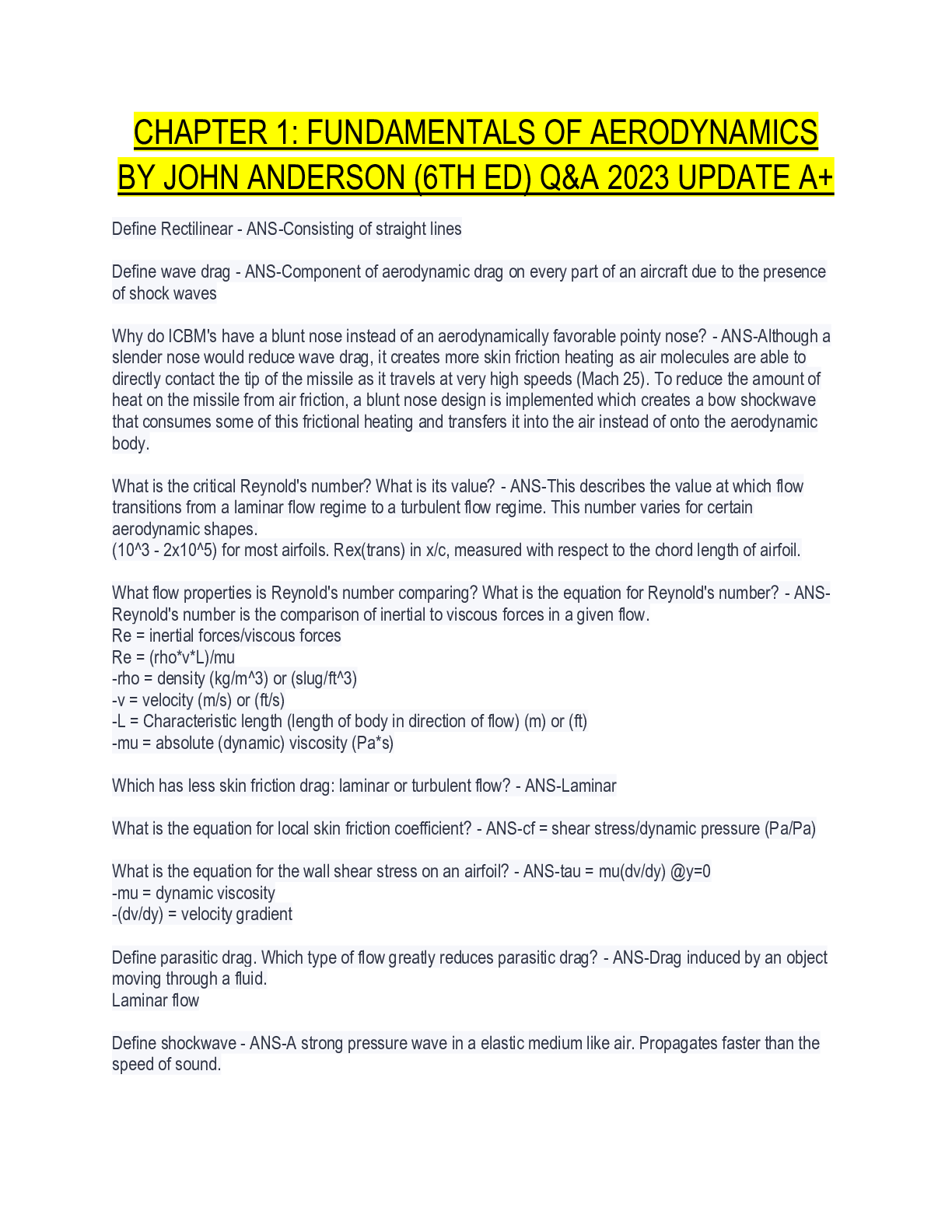
FUNDAMENTALS OF AERODYNAMICS BY JOHN ANDERSON (6TH ED) Q&A 2023 UPDATE A+
$ 9
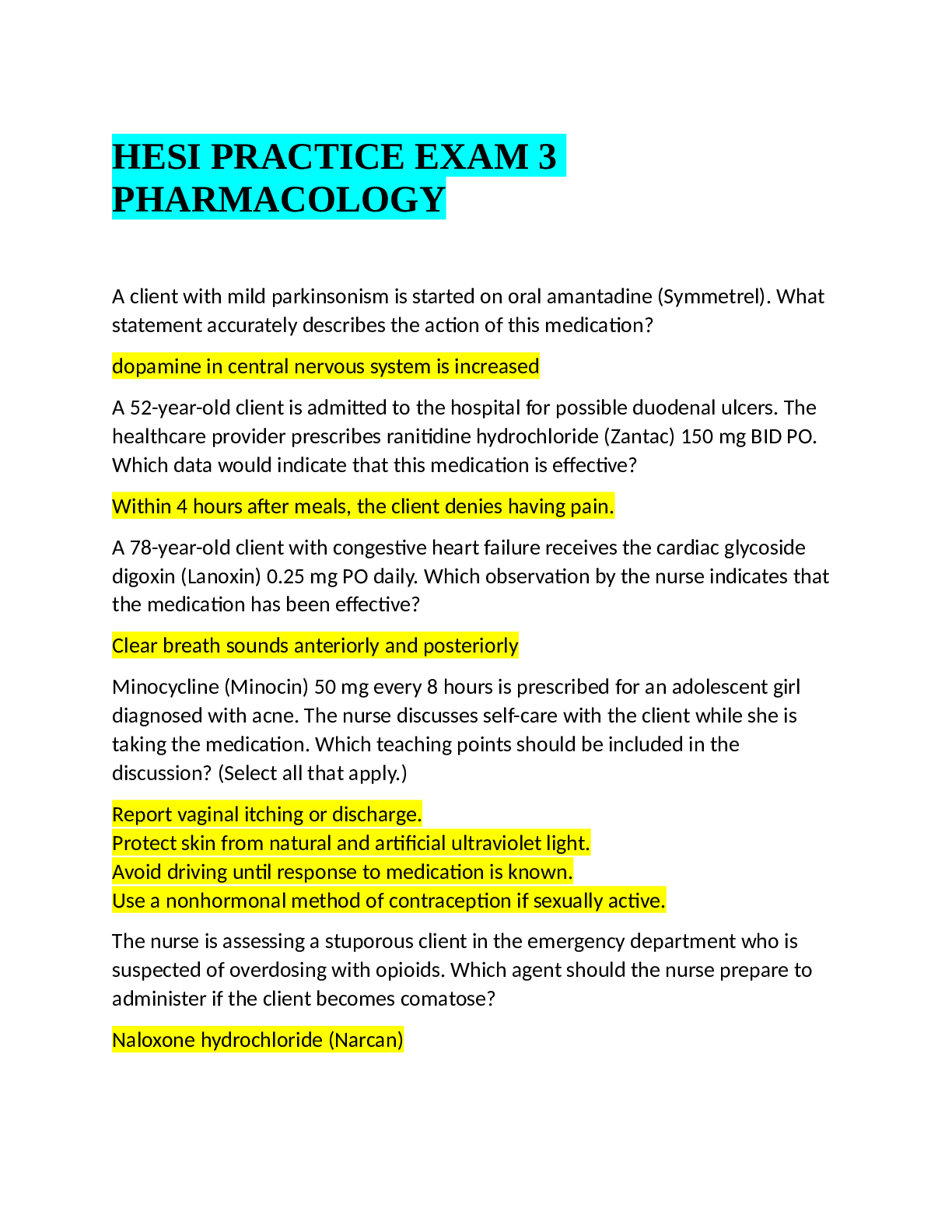
Nursing_knowledge_Assessment_Practice_Exam PRACTICE EXAM 3 PHARMACOLOGY
$ 7
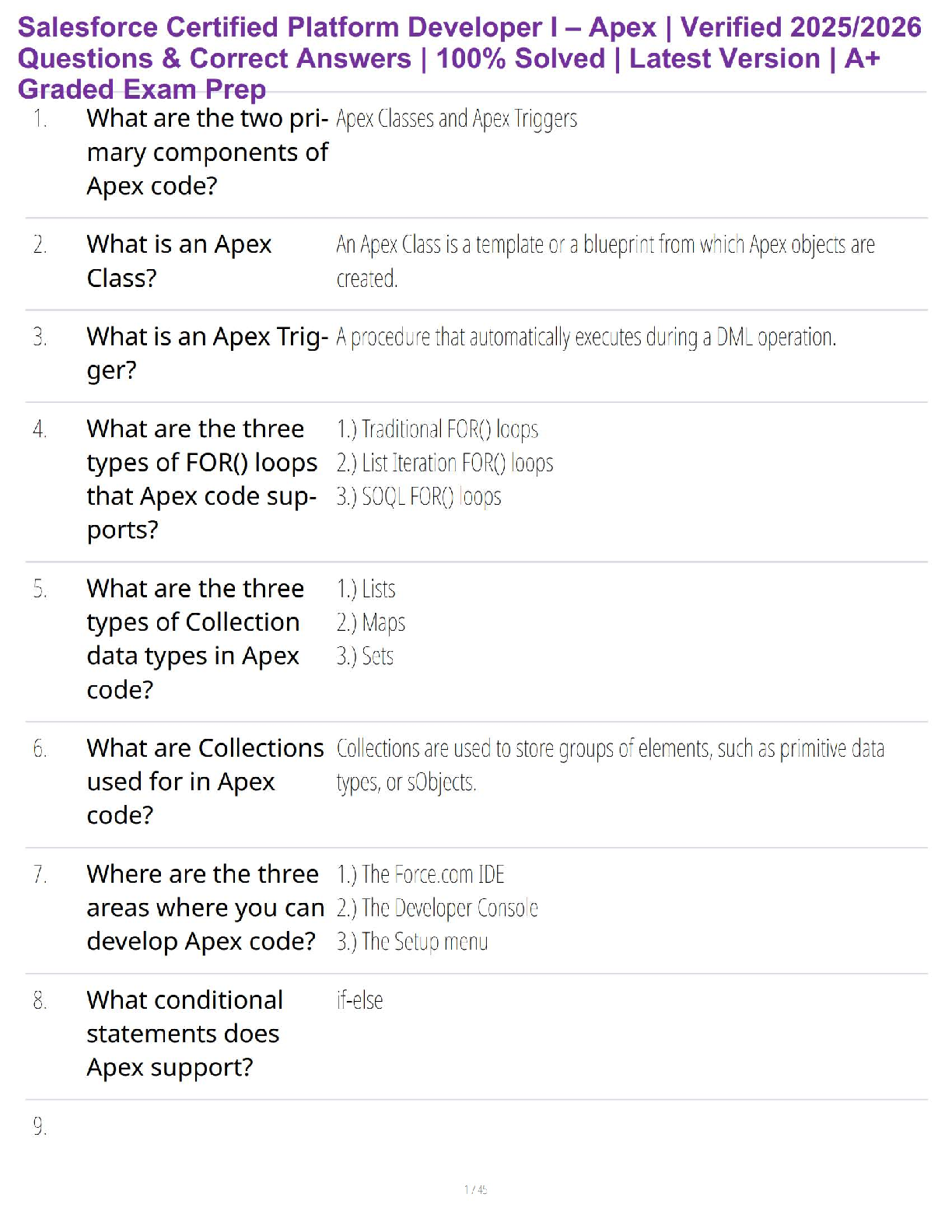
Salesforce Certified Platform Developer I (2025) | Verified Exam Questions & Detailed Answers | 100% Pass Guarantee
$ 21.5
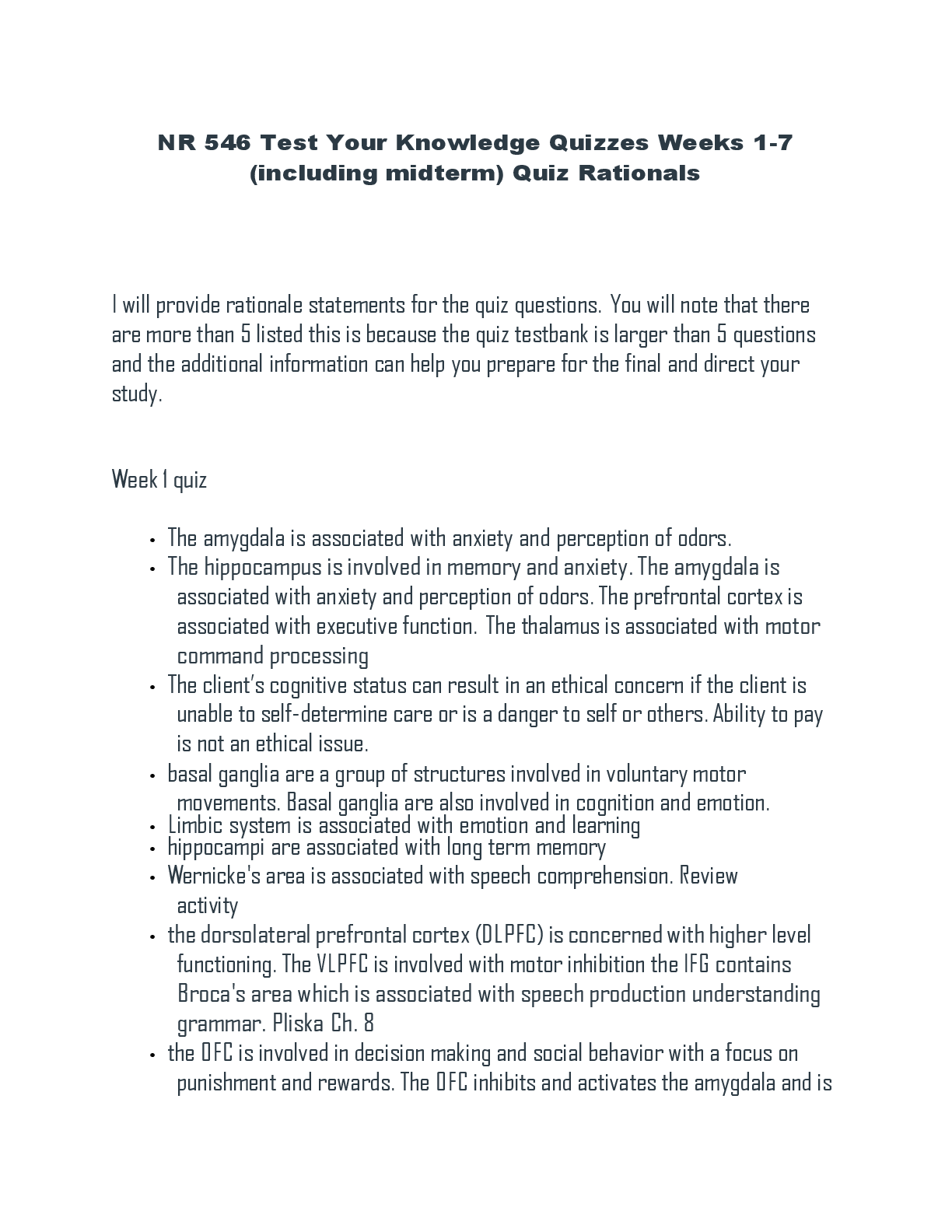
NR 546 Test Your Knowledge Quizzes Weeks 1-7 (including midterm) Quiz Rationals
$ 21.5
Test Bank For Organizational Leadership Second Edition By John Bratton
$ 19
Leadership Exam 2 gelen
$ 31.5

VSIM RED YODER part 2 Guided Reflection 6.16( Complete Solution)
$ 10.5

ABO Test Practice with COMPLETE SOLUTION
$ 9
AVIA 245 Aviation Leadership Final Exam set iii > latest fall 2020, A+ answers
$ 12

Hyperbilirubinemia Case Study group 3 answers
$ 11.5
eBook Research Design & Statistical Analysis 2nd Edition By Arnold D. Well, Jerome L. Myers
$ 29

Middle Tennessee State University MBAE 6865 Economic Decisions for Managers. Module One Quizzes - KW. All Answers Correct.
$ 11
AQA MARK SCHEMES AS BIOLOGY PAPER1 2022
$ 10
HUM 111 Week 9 Quiz 8 - Questions & Answers
$ 15
Test Bank for Microbiology, A Systems Approach, 6th Edition, Marjorie Kelly Cowan, Heidi Smith 2024 latest revised update
$ 16
eBook [PDF] Bernard Shaw Automata Robots and Artificial Intelligence 1st Edition By Kay Li
$ 29

ATI Capstone Content Review: Mental Health
$ 9
Airport ID Badges [DFW SIDA Training Pocket Guide]with Questions and Answers! RATED A+
$ 7
test bank for Microbiology an introduction 13th edition By tortora
$ 19
Burns' Pediatric Primary Care 7th Edition Test Bank
$ 19.5
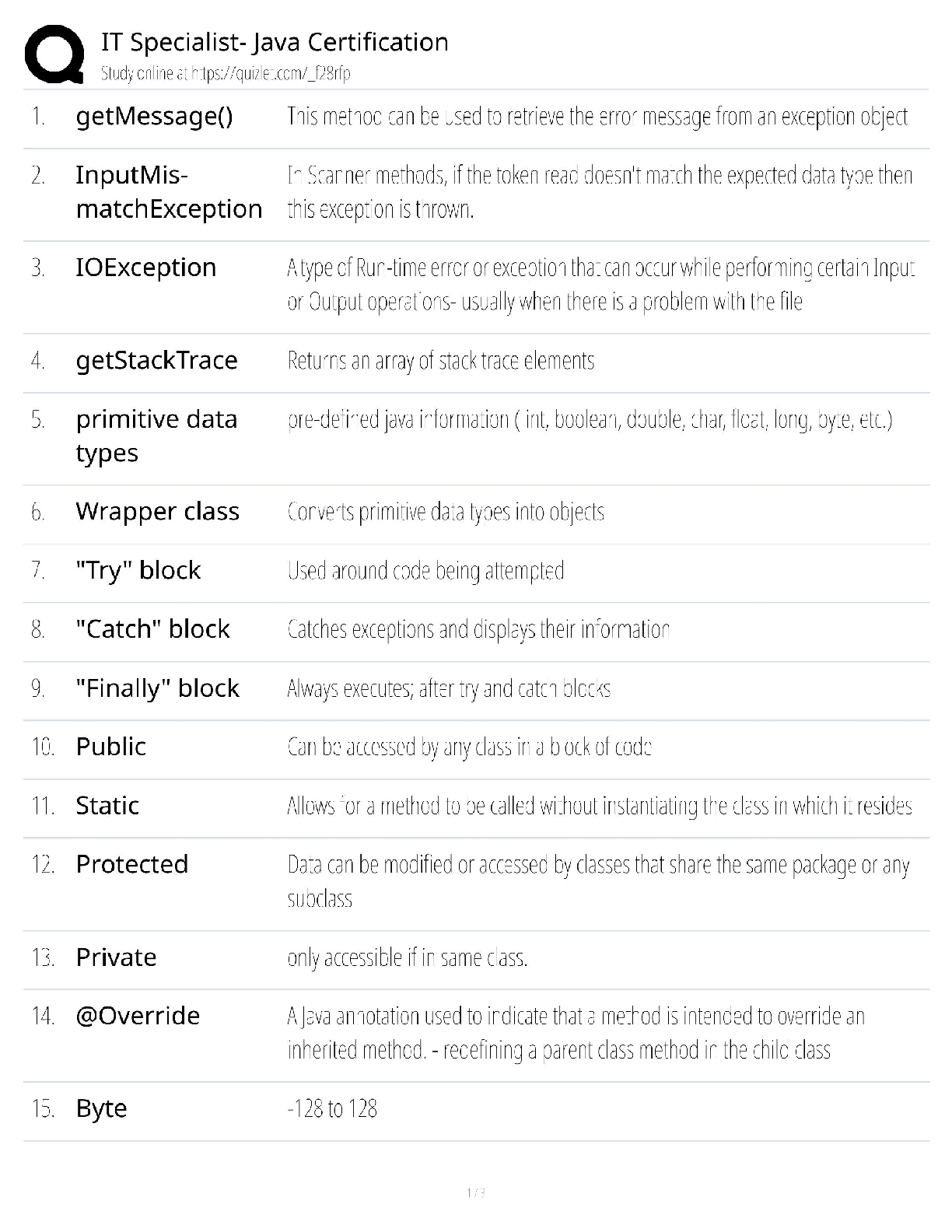
IT Specialist – Java Certification / Score 100% / 2025 Update / Study Guide & Exam Prep
$ 18.5
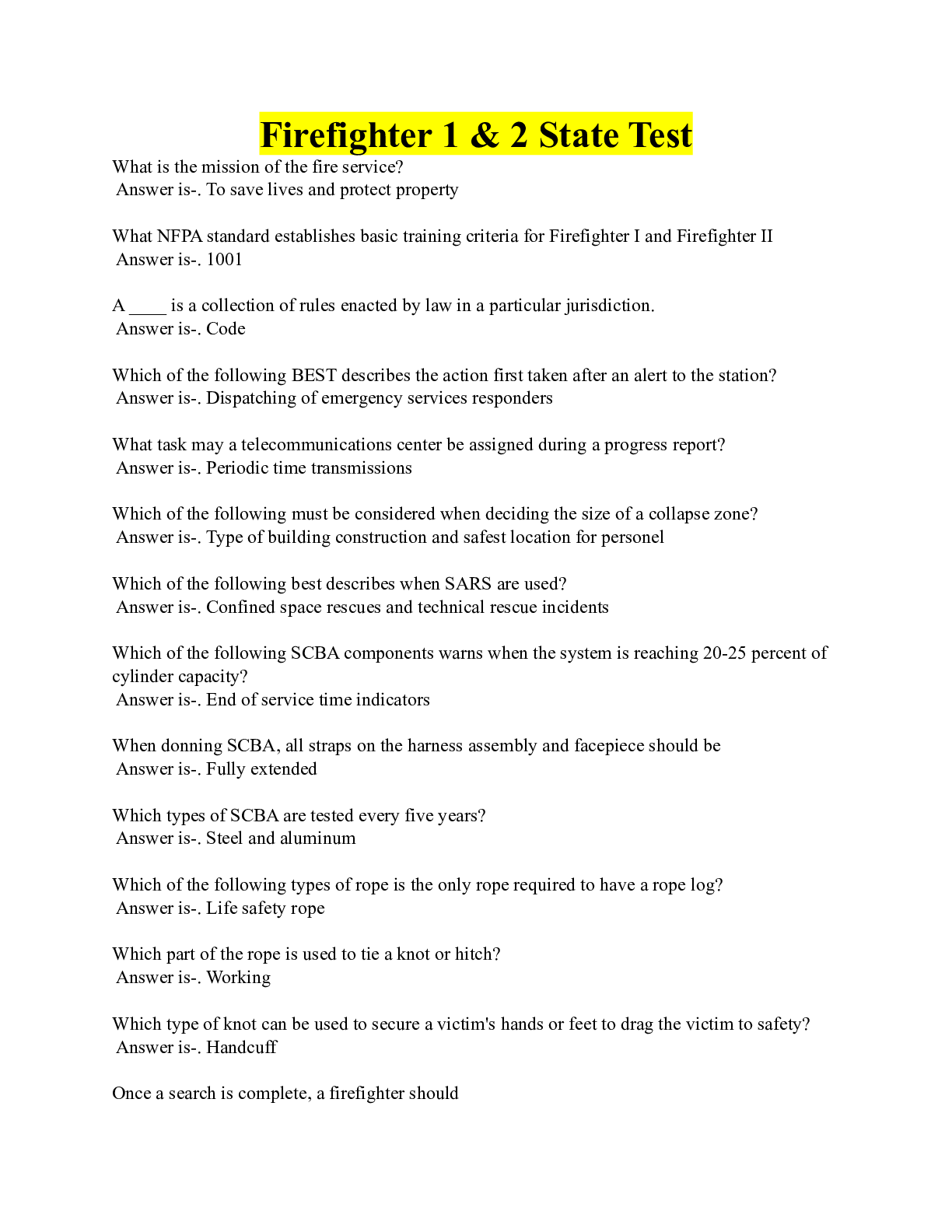
Firefighter 1 & 2 State Test (Questions and Answers with solutions)
$ 9.5

Leadership__ _Proctored__ Complete questions and answers to ace the exams
$ 10
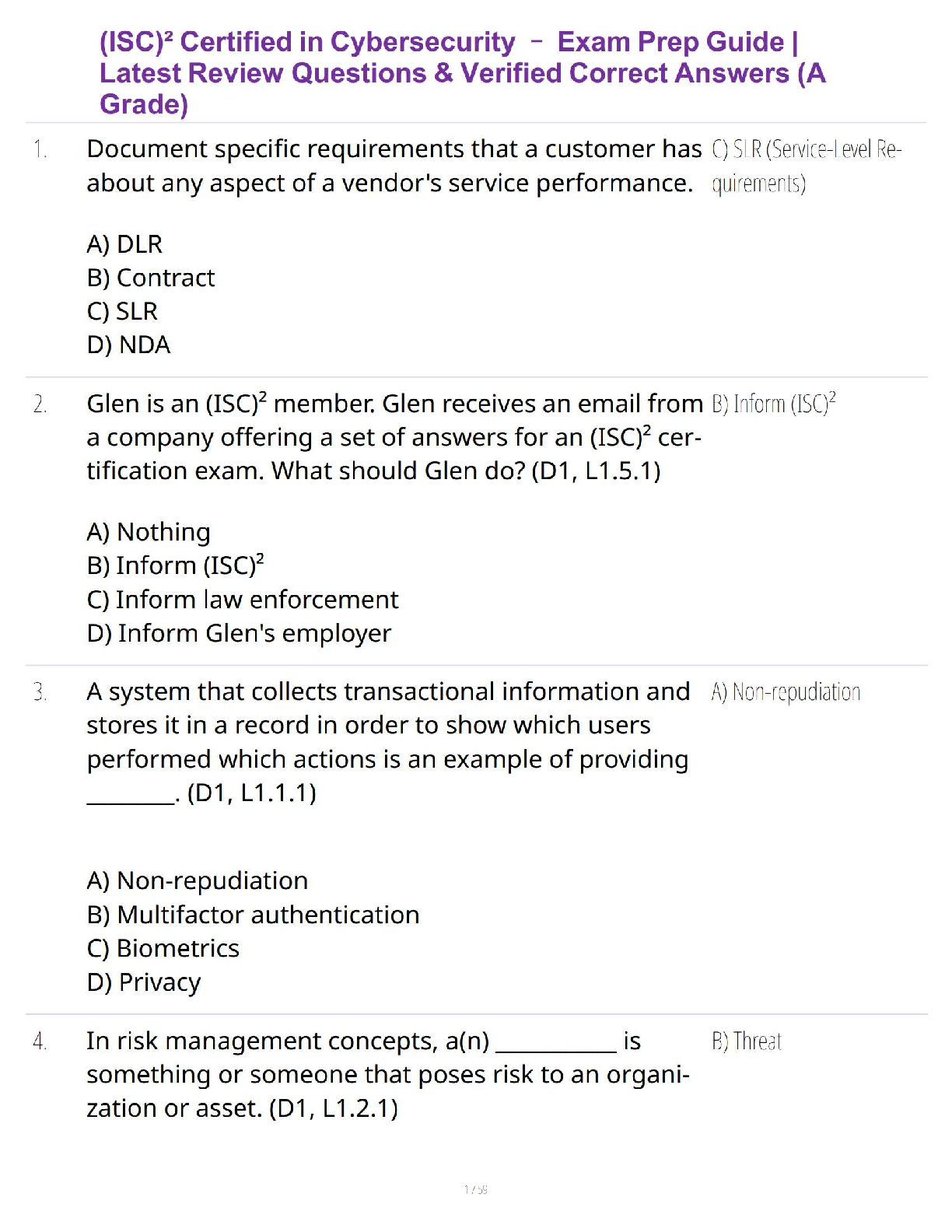
(ISC)² Certified in Cybersecurity – Exam Prep Guide | Latest Review Questions & Verified Correct Answers (A Grade)
$ 27.5
LDR 615 week 1 topic 2.,WELL EXPLAINED.
$ 12
Review Questions in Blood Banking
$ 30

Final_Epidemiology_module[1]/ Complete Solution
$ 13.5

Medtech Laws Exam
$ 30
LDR 615 week 7 topic 1.,GRADED A.
$ 12
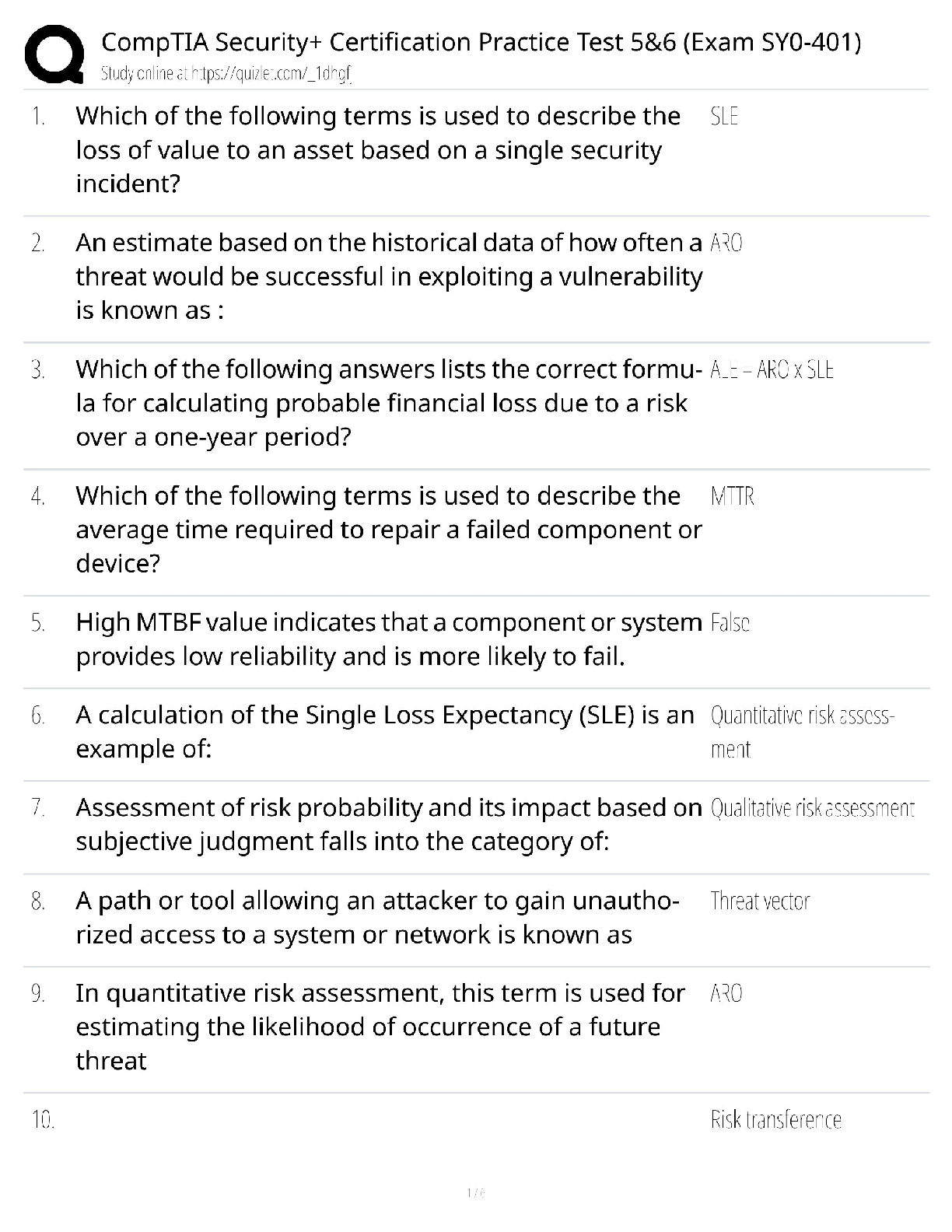
CompTIA Security+ Practice Tests 5 & 6 (2024) / SY0-701 Exam Prep / 500+ Questions / Pass Guaranteed
$ 18.5
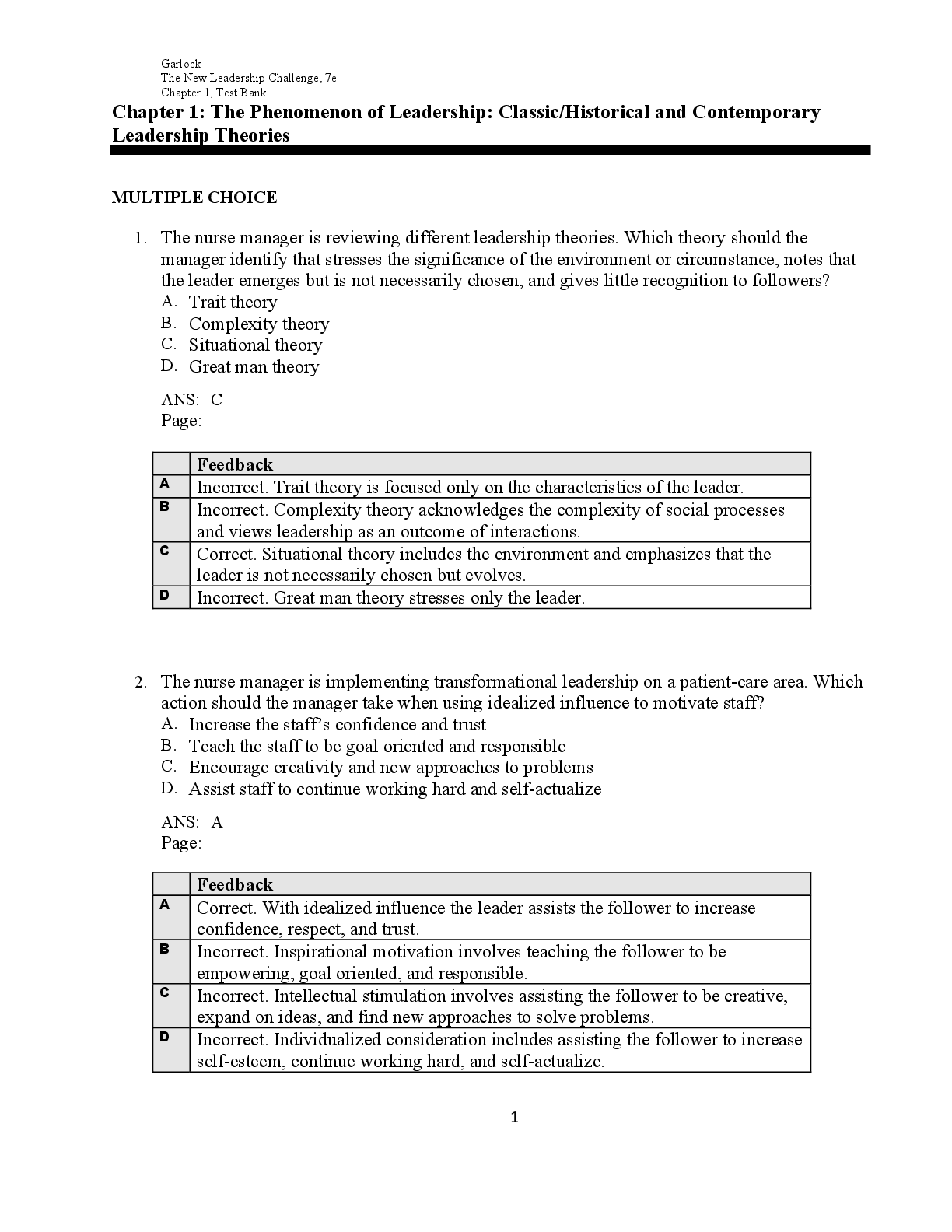
Test Bank For The New Leadership Challenge Creating the Future of Nursing 7th Edition By Abby E. GarlockDNP, Nicole P. Waters
$ 19

NURS 618 - Saunders Med Surg Cardiovascular Revised 2020.
$ 12
Dell Client 2025 Assessment Test | Latest Update | 100% Correct Questions and Answers
$ 7.5
.png)
WGU C724 Unit 2 Test Latest 2022 Rated A
$ 8
MKT 571 week 6 FINAL Exam Solution docs questions and answers 2020
$ 15.5

STOCK WATSON –INTRODUCTION TO ECONOMETRICS 3 RD EDITION ANSWER TO EMPIRICAL EXERCISE
$ 9.5
Adjuster Pro - Insurance adjuster test
$ 22

PDHPE Exam Revision 2022/2023 Graded A+
$ 8

NURS-6512-Advanced-Health-Assessment-FInal Exam



 (1).png)