*NURSING > HESI > BIO MED SURG 1/ HESI P 1 (GRADED A) Questions and Answer solution | 100% Guaranteed Pass. (All)
BIO MED SURG 1/ HESI P 1 (GRADED A) Questions and Answer solution | 100% Guaranteed Pass.
Document Content and Description Below
BIO MED SURG 1/ HESI P 1 1. A client with gout experiences an acute attack. The client reports he has been trying to lose weight. Which client information is most important for the nurse to obtain?... • Serum cholesterol level (not related to the acute attack gout) • Capillary glucose level (not related to the acute attack gout) • Daily caloric intake (Starvation diet can cause an acute attack of gout) • Daily calcium intake (not related to the acute attack gout) 2. A male client with a C-6 spinal cord injury is in rehabilitation. In the middle of the night he reports a severe, pounding headache, and has observable goose bumps. The nurse should assess for which trigger? • Loud hallway noise (Not manifestation of autonomic hyperreflexia) • Fever (Not manifestation of autonomic hyperreflexia) • Full bladder • Frequent cough (Not manifestation of autonomic hyperreflexia) * A pounding headache is a sign of autonomic hyperreflexia, an acute emergency that occurs because of an exaggerated sympathetic response in a client with a high-level spinal cord injury. Any stimulus below the level of injury can trigger autonomic hyperreflexia, but the most common cause is an overly distended bladder. 3. After learning that she as terminal pancreatic cancer, a female client becomes very angry and says to the nurse, “God has abandoned me. What did I do to deserve this”? Based on this response, the nurse deicides to include Which nursing problem in the client’s plan of care? • Acute pain (physical pain less than 6 month) • Spiritual distress (indicates anger toward God for her disease) • Ineffective coping (not reflect) • Complicated grieving (not reflect) 4. A nurse working on an Endocrine Unit should see which client first? • An Adolescent male with type 1 diabetes who is arguing about his insulin dose (dealt with at a later time) • A older client with Addison’s disease whose current blood sugar level is 62 mg/dl (blood sugar level is low (normal 60 -110 mg/dl, but is not critical) • An adult with a blood sugar of 384 mg/dl and a urine output of 350 ml in the last hour (exhibiting sign of diabetes insipidus, which include hyperglycemia & urine output, but this patient can be seen after corticosteroid pt) • A client taking corticosteroids who has become disoriented in the last two hours (safety) * Rationale: safety is a priority intervention. Mania & psychosis can occur during corticosteroid therapy, which places the client at risk for injury, so this should be first seen. 5. A young boy who is in a chronic vegetative state and living at home is readmitted to the hospital with pneumonia and pressure ulcers. The mother insists that she is capable of caring for her son and that she is going to take him home when he is discharged. Which action should the nurse implement next? • Report the incident to the local Child Protective Service (further assessment is needed before implementing) • Find a home health agency that specializes in brain injuries (further assessment is needed before implementing) • Determine the mother’s basic skill level in providing care (client is manifesting disease syndrome complications, and the mother’s skill in providing basic care should be determined) • Consult the ethics committee to determine how to proceed (further assessment is needed before implementing) 6. A male client with persistent low back pain has received a prescription for an electronic stimulator (TENS) unit. After the nurse applies the electrodes and turns on the power, the client reports feeling a tingling sensation. How should the nurse respond? • Determine if the sensation feels uncomfortable (Electronic stimulators, such as a transelectrial nerve stimulator (TENS) unit, effective in reducing low back pain by “closing the gate” to pain stimuli. A tingling sensation should be felt when the power is turned on, and the nurse should assess whether the sensation is too strong, causing discomfort or muscle twitching) • Decrease the strength of the electrical signals (indicated if the sensation is too strong) • Remove electrodes and observe for skin redness (not necessary because the tingling sensation is expected) • Check the amount of gel coating on the electrodes (not necessary because the tingling sensation is expected) 7. A male client returns to the mental health clinic for assistance with his anxiety reaction that is manifested by a rapid heartbeat, sweating, shaking, and nausea while driving over the bay bridge. What action in the treatment plan should the nurse implement? • Tell client to drive over the bridge until fear is manageable • Teach client to listen to music or audio books while driving • Encourage client to have spouse drive in stressful places • Recommend that the client avoid driving over the bridge 8. The nurse preparing to administer 1.6 ml of medication IM to a 4-month-old infant. Which action the nurse include? • Select a 22 gauge 1 ½ inch (3.8 cm) needle for the intramuscular injection A short, small gauge needle should be to inject into the small muscle mass of an infant rather than which is used for an adult) • Administer into the deltoid muscle while the parent holds the infant securely (deltoid muscle site in the arm should not be used in infants whose muscle mass is underdeveloped) • Divide the medication into two injections with volumes under 1 ml • Use a quick dart-like motion to inject into the dorsogluteal site (dorsoglutel site is not recommended due to the proximity to nerves and blood vessels) * IM injection for children under 3 year of age should not exceed 1 ml, so the prescribed dose should be divided into smaller volumes for injection in two different sites. 9. Which problem reported by a client taking lovastatin requires the most immediate follow-up by the nurse? • Diarrhea and flatulence (are also side effect of lovastatin that require intervention, but are of loss priority) • Abdominal cramps (are also side effect of lovastatin that require intervention, but are of loss priority) • Muscle pain (Lovastatin main priority of side effect) • Altered taste (are also side effect of lovastatin that require intervention, but are of loss priority) * Statins can cause rhabdomyolysis, a potentially fatal disease of skeletal muscle characterized by myoglobinuria and manifested with muscle pain, so this symptom should immediately be reported to the health care provider 10. The nurse is triaging victims of a tornado at an emergency shelter. An adult woman who has been wandering and crying comes to the nurse. What action should the nurse take? • Check the client’s temperature, blood sugar, and urine output • Transport the client for laboratory tests and electrocardiogram (EKG) • Delegate care of the crying client to an unlicensed assistant • Send the client to the shelter’s nutrient center to obtain water and food 11. The nurse is collecting a sterile sample for culture and sensitivity form a disposable three chamber-seal drainage system connected to a pleural chest tube. The nurse should obtain the sample from which site on the drainage system? • Tubing located on the top of the suction chamber (do not provide access to chest drainage) • Plastic tubing located at the chest insertion site (should not be disconnected or accessed to collect a sample) • Stopper port located above the water-seal level (do not provide access to chest drainage) • Rubberized port at the bottom of collection chamber (with one-way value) 12. The healthcare provider prescribes a low-fiber diet for a client with ulcerative colitis. Selection of which food items indicates to the nurse that the client understands the prescribed diet? • Roasted turkey, canned vegetables (low-fiber diet) • Baked potato with skin, raw carrots (not low-fiber diet) • Pancakes, whole-grain cereals (not low-fiber diet) • Roast pork, fresh strawberries (not low-fiber diet) 13. A client exposed to tuberculosis is scheduled to begin prophylactic treatment with isoniazid. Which information is most important for the nurse to note before administering the initial dose? • Conversion of the client’s PPD test from negative to positive (indication for prophylactic treatment) • Length of time of the exposure to tuberculosis (do not provide data indicating the need to question or hold the prescribed treatment) • Current diagnosis of hepatitis B (contraindicated for a person with liver disease because it may cause liver damage. The nurse should hold the prescribed dose and contact healthcare provider) • History of intravenous drug abuse (do not provide data indicating the need to question or hold the prescribed treatment) 14. After placing a client at 26-weeks’ gestation in the lithotomy position, the client complains of dizziness and becomes pale and diaphoretic. What action should the nurse implement? • Place the client in the Trendelenburg position (not alleviate pressure on the vena cava and aorta) • Instruct the client to take deep breathe (not alleviate pressure on the vena cava and aorta) • Place a wedge under the client’s hip • Remove the client’s legs from the stirrups (not alleviate pressure on the vena cava and aorta) * the client is likely to be experiencing supine hypotensive syndrome due to pressure of enlarging uterus on the vena cava and aorta. Placing a wedge under either hip tilts the uterus off these large vessels and relieves symptoms. 15. A gravida 2 para 1, at 38-weeks’ gestation, scheduled for a repeat cesarean section in one week, is bought to the labor and delivery unit complaining of contraction every 10 minutes. While assessing the client, the client’s mother enters the labor suite and says in a loud voice, “I’ve had children and I know she is in labor. I want her to have her cesarean section right now!” What action should the nurse take? • Request the mother to leave the room (The nurse should ask the family member to leave the room because the behavior is disruptive to the nurse and to the client. After the assessment is completed, the nurse should then address the family member’s concerns) • Tell the mother to stop speaking for the client (is confrontational and could escalate the situation) • Request security to remove her from the room (are not indicated at this time unless the situation with the family member escalates) • Notify the charge nurse of the situation (are not indicated at this time unless the situation with the family member escalates) 16. A client with a chronic health problem has difficulty ambulating short distances due to generalized weakness but is able to bear weight on both legs. To assist with ambulation and provide the greatest stability, what assistive device is best for this client? • A quad cane (used to when there is partial or complete leg paralysis or some hemiplegia • Crutches with 2-point gait (requires at least partial weight bearing on each foot, but does not provide the stability) • Crutches with 3-point gait (useful when the client must bear all of the weight on one foot, and this is not the problem experienced by this client) • Crutches with 4-point gait (provide stability and require weight bearing on both legs, which this client should be able to provide) 17. A female nurse who took drugs from the unit for personal use was temporarily released from duty. After completion of mandatory counseling, the nurse has asked administration to allow her to return to work. When the nurse administrator approaches the charge nurse with impaired nurse’s request, what action is best for the charge nurse to take? • Since treatment is completed, assign the nurse to routine RN responsibilities • Ask to meet with impaired nurse’s therapist before allowing her back on the unit • Allow the impaired nurse to return to work and monitor medication administration (provides essential monitoring and helps ensure nurse compliance and promote client safety) • Meet with staff to assess their feeling about the impaired nurse’s return to the unit 18. A client had subtotal parathyroidectomy two days ago and is now preparing for discharge. Which assessment finding is most important for the nurse to provide to the healthcare provider? • No bowel movement since surgery (are signs of discomfort, but are not as important as a positive Chvostek’s sign) • Afebrile with normal pulse (is an expected finding) • No Appetite for breakfast (are signs of discomfort, but are not as important as a positive Chvostek’s sign) • A positive Chvostek’s sign * A positive Chvostek’s sign is spasm of the cheek muscle when the facial nerve is tapped indication a decreased serum calcium caused by lack of parathyroid hormone. This critical information should be relayed to the healthcare provider. 19. A client with cirrhosis is receiving a low protein diet. The nurse should explain to the family that this diet restriction is implemented to reduce the risk of which complication of cirrhosis? • Delirium tremors (decreased protein intake does not prevent) • Abdominal ascites (decreased protein intake does not prevent) • Hepatic encephalopathy • Esophageal varices (decreased protein intake does not prevent) * Protein end-products (amino acids) are converted (deaminated) by the liver to a fuel source by the removal of ammonia (NH3), which accumulates in the blood in those with cirrhosis and contributes to the potentially fatal complication of hepatic encephalopathy. 20. While completing an admission assessment for a client with unstable angina, which closed ended questions should the nurse ask about the client’s chest pain? • Tell me about the activities that cause your pain? • When did you first notice the pain your chest? • Does your pain occur when walking short distances? (yes or no question) • How do you feel when the pain becomes noticeable? 21. A 59-year-old male client comes to the clinic and reports his concern over a lump that, “just popped up on my neck a week ago.” In performing and examination of the lump, the nurse palpates a large, nontender, hardened left subclavian lymph node. There is no overlying tissue inflammation. What do these finding suggest? • Lymphangitis • Malignancy • Bacterial infection • Viral infection * - Rapid enlargement of a lymph node, particularly the subclavian node with no tenderness or inflammation is suggestive of malignancy. - Lymphangitis: is characterized by pain and inflammation - In infectious processes (Bacterial and Viral infection), the involved nodes become warm and tender to touch 22. An older client with atrial fibrillation receives a new prescription for dabigatran to reduce risk of blood clot formation. What information should the nurse include in this client’s medication teaching plan? (select all that apply) • Medication injections are self-administered daily • Plan to monitor and record the pulse rate daily • Contact the healthcare provider if bruising occurs • Report bleeding in the urine or stool right away • Inform dentist of medication usage before procedures * Dabigatran is an oral anticoagulant used to decrease clot formation in atrial fibrillation, thus reducing the risk for stoke. As an anticoagulant, excessive bleeding may occur and bruising and bleeding should be reported to the healthcare provider promptly, as well as all practitioners, such as dentist, who should be aware of the increased risk for bleeding prior to any scheduled procedures. 23. A morbidly obese woman is scheduled for gastric bypass surgery. She completes the required preoperative nutritional counseling and signs the operative permit. To promote effective discharge planning, which intervention is most important for the nurse to implement? • Discuss small, low fat, low sugar meal preparation techniques • Encourage the client to keep a daily dietary for two weeks • Suggest that the client’s husband do the family grocery shopping • Advise the client to arrange for dietary counseling after discharged 24. After reviewing the Braden Scale finding of residents at a long-term facility, the charge nurse should to tell unlicensed assistive personal (UAP) to prioritize skin care for which client? • An older adult who is unable to communicate elimination needs • A older man whose sheets are damp each time he is turned (risk for skin breakdown) • A woman with osteoporosis who is unable to bear weight • A poorly nourished client who requires liquid supplements 25. The husband of an older woman, diagnosed with pernicious anemia, calls the clinic to report that his wife still has memory loss and some confusion since she received the first dose of nasal cyanocobalamin two days ago. He tells the nurse that he is worried that she may be getting Alzheimer’s disease. What action should the nurse take? • Explain the memory loss and confusion is common with Vitamin B12 deficiency • Ask if the client experiencing any change in bowl habits • Determine if the client is taking iron and folic acid supplements • Encourage the husband to bring the client to the clinic for a complete blood count * Pernicious anemia is related to the absence of the intrinsic factor in gastric secretion, leading to malabsorption of vitamin B12, and commonly causes memory loss, confusion, cognitive problem, and GI manifestations. 26. A male client who sustained a head injury following an automobile collision is admitted to the hospital. The nurse includes the client’s risk for developing increased intracranial pressure (ICP) in the plan of care. Which signs indicated to the nurse that ICP has increased. • Increased Glasgow coma scale score (improvement in neurologic status) • Nuchal rigidity and dystonia (do not necessarily reflect increased ICP) • Confusion and papilledema (Papilledema is always an indicator of increased ICP, and confusion is usually the first sign of increased ICP • Periorbital ecchymosis (do not necessarily reflect increased ICP) * Papilledema is always an indicator of increased ICP, and confusion is usually the first sign of increased ICP 27. At 0715, after receiving report on four medical clients, the nurse is preparing a prioritized “to do” list. Which action should the nurse plan to do first? (click on each chart tab for additional information. Please scroll to the bottom right corner of each tab to view all information contained in the client’s medical records) • Administer metformin to client D • Insert the IV in a new location for client C • Complete a focused assessment for client A (The client with heart failure is exhibiting signs for worsening failure evidenced by his HR, RR, and scattered infiltrates on the chest x-ray, so a focused assessment is the highest priority) • Validate the blood pressure for client D 28. The nurse is preparing to send a client to the cardiac catheterization lab for an angioplasty. Which client report is most important for the nurse to explore further prior to the start of the procedure? • Drank a glass of water in the past 2 hours • Experiences facial swelling after eating crab (allergy to shellfish, is critical to the prevention of a life-threatening complication, anaphylactic shock, induced by iodine- based dyes used to visualize the coronary arteries during the cardiac catherization. While NPO precaution are routinely taken prior to the procedure.) • Reports left chest wall pain prior to admission • Verbalizes a fear of being in confined space 29. A client who has a below-the-knee amputation is experiencing severe phantom limb pain (PLP) and as the nurse it mirror therapy will make the pain stop. Which response by the nurse is likely to be most helpful? • Research indicates that mirror therapy is effective in reducing phantom limb pain (due to the activation of neurons in the hemisphere of the brain that is contralateral to the amputated limb when visual input reduces the activity of systems that perceive protopathic pain. Research findings indicate that mirror therapy significantly reduces PLP in those who have undergone amputation of lower limbs) • You can try mirror therapy, but do not expect complete elimination of the pain (is not true) • Transcutaneous electrical nerve stimulators (TENS) has been found to be more effective • Where did you learn about the use of mirror therapy in treating phantom limb pain? 30. One hour ago, while walking on the treadmill in the cardiac rehabilitation unit, a client began to exhibit signs of a cerebrovascular accident (CVA). The client is transported to the emergency department. Which client behavior is indicative of increased intracranial pressure (ICP) and deteriorating condition? • Calls out for family members who are outside the room • Falls asleep while answering health history questions • Becomes agitated when blood specimen is collected • Cries and grasps the nurse’s hand during vital signs *increased ICP often occurs following a cerebral bleed or clot. A change in level of consciousness (B, falls asleep while answering health history questions) is an early sign of changes in ICP, which requires immediate treatment. 31. During change of shift report, the oncoming nurse learns that soft restraints were applied to a combative client at 0600 after multiple alternatives were attempted and the client’s healthcare provider was notified. The nurse and unlicensed assistive personnel (UAP) initially enter the client’s room at 0800. In what order should the nurse implement these interventions? (Arrange from first action on top to last on the bottom. 32. A client with a history of dementia has become increasing confused at night and is picking at an abdominal surgical dressing and the tape securing the intravenous (IV) line. The abdominal dressing is no longer occlusive, and the IV insertion site is pink. What intervention should the nurse implement? • Replace the IV site with a smaller gauge (should be assessed to ensure that it has not been dislodged and a dressing reapplied, if needed) • Redress the abdominal incision (the abdominal incision should be redressed using aseptic technique) • Leave the lights on the room at night (may interfere with the client’s sleep and increased confusion) • Apply soft bilateral wrist restraints (are not indicated and should only be used as a last resort to keep client from self-harm) 33. When should intimate partner violence (IPV) screening occur? • As soon as the clinician suspects a problem • Only when a client present with an unexplained injury • As a routine part of each health care provider (universal screening for IPV, is a vital means to identify victims of abusive relationship) • Once the clinician confirms a history of abuse (Although history of abuse is difficult to confirm, screening should occur regardless, and this incident may be the initial case of abuse) 34. A male client who weighs 325 pounds (148 kg) is admitted because of ureteral colic and is now complaining of sharp pain radiating toward his genitalia. His has hematuria and is hypertensive. Which intervention is most important for the nurse to include in the client’s plan of care? • Manage pain • Encourage low calorie diet • Monitor hematuria • Document blood pressures *- Sharp, severe pain (Renal colic) radiating toward the genitalia and thigh is caused by urethral distention and smooth muscle spasm making pain relief (A, manage pain) the priority intervention. • - Encourage low calorie diet, monitor hematuria, and Document blood pressures are important and should be included in the plan of care, but they do not have the priority 35. A client with a lower respiratory tract infection receives a prescription for ciprofloxacin 500 mg PO q12 hours. When the client requests an afternoon snack, which dietary choice should the nurse provide? • Vanilla-flavored yogurt (Contains calcium) • Low-fat chocolate milk (Contains calcium) • Calcium-fortified juice (Contains calcium) • Cinnamon applesauce (Contains NO calcium) * Diary products and calcium-fortified dairy products decrease the absorption of cipro. Cinnamon applesauce contains no calcium. 36. A male client presents to the clinic with large draining ulcers on his lower legs that are characteristic of Kaposi’s sarcoma lesions. He is accompanied by two family members. Which action should the nurse take? • Ask the family members to wear gloves when touching the client • Send the family to the waiting area while the client’s history is taken (Pts privacy) • Obtain a blood sample to determine if the client is HIV positive • Complete a head to toe assessment to identify other signs of HIV 37. A client with Type 2 diabetes mellitus is admitted for frequent hyperglycemic episodes and a glycosylated hemoglobin (HbA1c) of 10. Insulin glargine 10 units subcutaneously once a day at bedtime and a sliding scale with insulin aspart q6h prescribed. What actions should the nurse include in this client’s plan of care? (Select all that apply) • Fingerstick glucose assessments q6h with meals • Mix bedtime does of insulin glargine with insulin aspart sliding scale dose • Review with the client proper foot care and prevention of injury • Do not contaminate the insulin aspart so that it is available for IV use • Coordinate carbohydrate-controlled meals at consistent times and intervals • Teach subcutaneous injection technique, site rotation, and insulin management 38. A mother calls the nurse to report that at 0900 she administered a PO dose of digoxin to her 4-month-old infant, but at 0920 the baby vomited the medicine. What instruction should the nurse provide to this mother? • Give another dose • Withhold this dose • Administer a half dose now • Mix the nest dose with food * - This dose should be withheld because the amount absorbed by the infant is unknown. • - Give another dose and Administer a half dose now are pose safety concerns due to the unknown absorption 39. A preeclamptic client who delivered 24 hours ago remains in the labors and delivery recovery room. She continues to receive magnesium sulfate at 2 grams per hours. Her total input is limited to 125 ml per hour, and her urinary output for the last hour was 850 ml. What intervention should the nurse implement? • Discontinue the magnesium sulfate immediately (not indicated at this time) • Decrease the client’s IV rate to 50 ml per hour (not indicated at this time) • Continue with plan of care for this client (diuresis in 24 to 48 hours after birth is a sign of improvement in the preeclamptic client. As relaxation of arteriolar spasms occurs, kidney perfusion increases. With improved perfusion, fluid is drawn into intravascular bed from the interstitial tissue and then cleared by the kidneys.) • Change the client’s diet to NPO status (not indicated at this time) 40. While changing a client’s tube dressing, the nurse notes a crackling sensation when gentle pressure is applied to the skin at the insertion site. What action would be best for the nurse to take? • Apply a pressure dressing around the chest tube insertion site (not indicated for crepitus. Since this not an allergic reaction) • Assess the client for allergies to topical cleaning agents (are not indicated) • Measure the area of swelling and cracking • Administer an oral antihistamine per PRN protocol (are not indicated) • * A crackling sensation, or crepitus, indicates subcutaneous emphysema, or air leaking into the skin, this area should be measured (C, Measure the area of swelling an cracking) and the finding documented 41. The nurse is developing an educational program for older client who are being discharged with antihypertensive medications. The nurse should ensure that the educational materials include which characteristics? (select all that apply) • Written at a 12-grade reading level • Contains a list with definitions of unfamiliar terms • Uses common words with few syllables • Printed using a 12-pint type font • Uses pictures to help illustrate complex ideas * Contains a list with definitions of unfamiliar terms, uses common words with few syllables and Uses pictures to help illustrate complex ideas. During the aging process, older client often experiences sensory or cognitive change, such as decreased visual or hearing acuity, slower thought or reasoningoricesses, and shorter attention span. Materials for this age group should include a list of terms, such as medical terminology that a client may not know and use common words that express information clearly and simply. Simple, attractive pictures help hold learner’s attention. 42. An older adult male with emphysema who continues to smoke cigarettes returns to the medical unit after a physical therapy session and is complaining of being short of breath. The nurse notes that the client is lying supine with the head of the bed elevated to 45 degrees. Oxygen is flowing via nasal cannula at 3L/minute, his pulse respiratory rate is 14 breaths/minutes, and his vital signs are stable. Which intervention should the nurse implement? • Notify the physician for the low pulse oximetry value ( is unnecessary since a low pulse is common for clients with emphysema and providers the hypoxic drive to breathe) • Administer a prescribed albuterol inhaler • Assess lung sounds for signs of infection (infection is not the primary concern at this time) • Encourage client to initiate a smoking cessation program (not indicated at this time) * the immediate issue is the client’s shortness of breath, probably due physical exertion and fatigue after physical therapy. Albuterol (Administer a prescribed albuterol inhaler), a short- acting rescue inhaler, relaxes the airway quickly and is used for clients with asthma and COPD. 43. Assessment by the home health nurse of an older client who lives alone indicates that the client has choric constipation. The client’s fluid and fiber intake is deficient and he eat microwaved foods at home and frequents fast-food restaurants. Daily medications include furosemide for hypertension and heart failure and laxatives. To manage the client’s constipation, which suggestions should the nurse provide? (select all that apply) • Decrease laxative use to every other day, and use oil retention enemas needed • Include oatmeal with stewed prunes for breakfast as often as possible (increases dietary fiber and bowel stimulation, thereby decreasing need for laxatives) • Increase fluid intake by keeping water glass next to recliner (decrease constipation) • Recommend seeking help with regular shopping and meal preparation (might help the client eat more fresh fruits and vegetables and result on less reliance on microwaved and fast food, which are usually high in sodium and fate with little fiber) • Report constipation to healthcare provider related to cardiac medication side effects. 44. The nurse is preparing a 4-day-old infant with a serum bilirubin level of 19 mg/dl discharge from the hospital. When teaching the parents about home phototherapy, which instruction should the nurse include in the discharge teaching plan? • Reposition the infant every 2 hours • Perform diaper changes under the light (Bonding with parents) • Feed the infant every 4 hours (Bonding with parents) • Cover with a receiving blanket (Bonding with parents) * An infant who is receiving phototherapy for hyperbilirubinemia, should be repositioned every two hours. Reposition ensure that the phototherapy lights reach all of the body surface areas. 45. The nurse who is working on a surgical unit receives change-of-shirt report on a group of clients for the upcoming shirt. Which client requires the most immediate attention by the nurse? • Gunshot wound three hours ago with dark drainage of 2 cm noted on the dressing (not life threatening) • Mastectomy 2 days ago with 50 ml bloody drainage noted in the Jackson-Pratt drain (not life threatening) • Collapsed lung after a fall 8 hours ago with 100 ml blood in the chest tube collection container (not life threatening) • Abdominal-perineal resection 2 days go with no drainage on dressing who has fever and chills * is a risk for peritonitis and needs to be immediately assessed for other signs and symptoms for sepsis 46. The nurse identifies the presence of clear fluid on the surgical dressing of a client who just returned to the unit following lumbar spinal surgery. What action should the nurse implement immediately? • Change the dressing using a compression bandage (the nurse should not implement, based on this finding) • Document the findings in the electronic medical record (this is not a priority action) • Test the fluid on the dressing for glucose using chernstrip • Mark the drainage are with pen and continue to monitor (delays necessary intervention) * Which could be cerebrospinal fluid. if the fluid on the dressing is positive for glucose, this verifies that it is cerebrospinal fluid and the surgeon should be notified immediately 47. The nurse has received funding to design a health promotion project for African American women who are at risk of developing breast cancer. Which recourse is most important designing this program? • A listing of African American women who live in the community • Participation of community leaders in planning the program • Morbidity date for breast cancer in women of all access • Technical assistance to produce a video on breast self-examination 48. The nurse is caring for a client who is entering the second stage of labor. Which action should the nurse implement first? • Convey to the client that birth is imminent • Prepare the client for spinal anesthesia (prior to delivery) • Empty the client’s bladder using a straight catheter (prior or after delivery) • Prepare the coach to accompany the client to delivery (only for support) * the second stage of labor occurs when the client is fully dilated and the fetus is crowning, so completing preparations and informing the client that birth is imminent is first action. 49. A client with coronary artery disease who is experiencing syncopal episodes is admitted for a electrophysiology study (EPS) and possible cardiac ablation therapy. Which intervention should the nurse delegate to the unlicensed assistive personnel (UAP)? • Prepare skin for procedure (could be done by a UAP) • Identify client’s pulse points (by a nurse) • Witness consent for procedure (by a nurse) • Check telemetry monitoring (by a nurse) 50. An 18-year old female client is seen at the health department for treatment of condylomata acuminate (perineal warts) caused by the human Papillomavirus (HPV). Which intervention should the nurse implement? • Tell the client that the vaccine for HPV is not indicated • Inform the client that warts do not return following cryotherapy • Recommend the use of latex condoms to prevent HPV transmission • Reinforce the importance of annual Papanicolaou (Pap) smears * Because the human Papillomavirus (HPV) is associated w/cervical cancer, close follow up, including yearly Pap smears should be recommended. 51. A client presents at the emergency department complaining of raspy voice, cold intolerance, and fatigue. Laboratory test indicate an elevated thyroid stimulating hormone (TSH) and low T3 and T4 levels, After the client is admitted to the telemetry unit, which intervention is most important for the nurse to implement? • Assess or presence of non-pitting edema • Administer prescribed dose of levothyroxine • Offer additional blankets and a warm drink • Note client’s most recent hemoglobin level * in the negative feedback mechanism of hypothyroidism, a low level of thyroid hormone stimulates TSH production by the hypothalamus and results in an elevated TSH level, but the thyroid gland does not respond with adequate production of thyroid hormones (T3 and T4) to regulate basal metabolic rate. These serum hormone levels indicate the need to administer supplemental thyroid hormones, such as levothyroxine. As soon as possible myxedema coma. 52. The nurse suspects that a client might be hemorrhaging internality. Which finding of an orthostatic tilt test are the most likely indication of a major bleed (> 1,000 ml)? • A decrease in the systolic BP of 10 mm Hg with a corresponding increase in the HR of 20 • A decrease in the diastolic BP of 10 mm Hg with a corresponding decrease in the HR of 20 (does not correctly characterize the VS changes associated with a major bleed) • A decrease in the systolic BP of 20 mm Hg with a corresponding decrease in the HR of 10 (does not correctly characterize the VS changes associated with a major bleed) • A decrease in the diastolic BP of 20 mm Hg with a corresponding increase in the HR of 10 (does not correctly characterize the VS changes associated with a major bleed) * the loss of circulatory volume results in a 10 mm Hg drop in the systolic pressure, while the heart rate increase by 20% above normal as a compensatory response to the low pressure. 53. When conducting diet teaching for a client who is on a postoperative full liquid diet, which foods should the nurse encourage the client to eat? (Select all that apply) • Canned fruit cocktail (not considered liquids) • Creamy peanut butter (not considered liquids) • Vegetable juice • Vanilla frozen yogurt • Clear beef broth * A full liquid diet includes all liquids that are not clear, such as vegetable and vanilla frozen yogurt, as well as clear liquids 54. The nurse is caring for a 17-year-old male who fell 20 feet 5 months ago while climbing the side of cliff and has been in a sustained vegetative state since the accident. Which intervention should the nurse implement? • Talk directly to the adolescent while providing care • Monito vital signs and neuro status every 2 hours (not warranted for a non-acute comatose client) • Inquire about food allergies and food likes and dislikes (has nothing to do with a vegetative state) • Initiate open communication with the teen’s parents (this just supporting the parents) * talking directly to the adolescent who is an sustained vegetative state providers environmental stimulation and includes him in an interpersonal relationship because he may still be able to hear and process verbal communications. 55. A client is receiving ophthalmic drops preoperatively for a cataract extraction and ask the nurse why the healthcare provider has prescribed all these medications. Which information should the nurse included when responding to this client? (select all that apply) • One of the medications is used to anesthetize the corneal surface • The iris must be paralyzed during surgery to prevent it from reacting to light • A medication is used to induce sleep during the produce ( A sedative may be administered to reduce anxiety but is not used to sleep) • Pupillary dilation is necessary to access the eye chamber for lens removal • These medications assist in obstructing client’s vision during the surgery (cloudy vision may be a side effect of these agents, but the client will still be able to see during the surgery) * Cataract surgery is accessed through the cornea using eyelid retractors, while the client is awake. It is necessary to anesthetize the corneal surface. 56. The community health nurse is planning how to address the issue of child abuse in a large metropolitan area. Which primary presentation program should the nurse develop? • From weekly support group meeting for abused children • Start home visits for families identified at risk for violence • Develop an anger management class for abusive parents • Create a child development class for high school students 57. A male client with HIV, who is receiving saquinavir PO in combination with order antiretroviral therapy, tells the home health nurse that he is always hungry and thirsty but seems to be losing weight. What action should the nurse implement? • Use a glucometer to determine the client’s capillary glucose level • Reassure the client that he will gain weight as his viral load decrease (if the pt has developed diabetes mellitus) • Explain to the client that he may require an increased dose of this medication (not indicated if the client has developed adverse effects from medications) • Teach the client strategies to ensure that he measures his weight accurately (less concern than the symptoms reflecting hyperglycemia that the client is manifesting) * The nurse should determine the client’s blood glucose before taking further action. Protease inhibitors such as saquinavir may increase blood glucose, producing symptoms such as polyphagia, polydipsia, polyuria and weight loss. 58. When assessing an IV site that is used for fluid replacement and medication administration, the client complains of tenderness when the arm is touched above the site. Which additional assessment finding warrants immediate intervention by the nurse? • A sluggish blood return • Client uses the arm cautiously • Spot of dried at insertion site • Red streak tracking the vein (indicates vein irritation and necessities discontinuing the IV at the present site) 59. The nurse is triaging clients in an urgent care clinic. The client with which symptoms should be referred to the health care provider immediately? • High fever, skin rash, and a productive cough • Headache, photophobia, and nuchal rigidity (signs and symptoms of a meningeal infection) • Nausea vomiting, and poor skin turgor • Malaise, fever, and stiff, swollen joints 60. A nurse is planning discharge care for a male client with metastatic cancer. The client tells the nurse that he plans to return to work despite pain, fatigue, and impending death. Which goal is most important to include in this client’s plan of care? • implements decisions about future hospice services within the next 3 months • Maintains pain level below 4 when implementing outpatient pain clinic strategies. (providers the interdisciplinary services needed to manage chronic pain) • Request home health care if independence become compromised for 5 days • Arranges for short term counseling stressors impact work schedule for 2 weeks 61. A client with liver abscess develops septic shock. A sepsis resuscitation bundle protocol is initiated, and the client receives a bolus of IV fluids. Which parameter should the nurse monitor to assess effectiveness of the fluid bolus? • Blood cultures • Oxygen saturation • White blood cell count • Mean arterial pressure (MAP) * - The cornerstone of initial sepsis resuscitation is fluid volume administration to restore and them maintain arterial pressure Mean arterial pressure of at least 65 mmHg. • - Blood cultures, Oxygen saturation and White blood cell count are also important parameters to monitor in the overall management of septic shock, but mean arterial pressure is the most direct measure of the effective of fluid volume resuscitation 62. A client presents in the emergency room with right-sided facial asymmetry. The nurse asks the client to perform a series of movement that require use of the facial muscles. What symptoms suggest that the client has most likely experienced a Bell’s palsy rather than a stroke? • Slow onset of facial drooping associated with headaches (More indicative of stroke) • Inability to close the affected eye, raise brow, or smile • A flat nasolabial fold on the right resulting in facial asymmetry (more w/both Bell’s palsy and stoke) • Drooling is present on right side of the mouth, but not on the left (more w/both Bell’s palsy and stoke) *Because the motor functions controlling eye closure, brow movement, and smiling are all carried on the 7th cranial (Facial) nerve, the combination of symptoms directly relating to an impairment of the facial indicate the Bell’s palsy has occurred 63. When attempting to establish risk reduction strategies in a community, the nurse notes that regional studies indicate a high number of persons with growth stunting and irreversible mental deficiencies (cretinism) caused by hypothyroidism. The nurse should seek funding to implement which screening measure? • T4 levels in newborns (screening for low T4 levels in newborns with follow up treatment can reduce the risk for irreversible growth stunting and mental deficiencies (cretinism) caused by congenital hypothyroidism) • TSH levels in women over 45 • T3 levels in school aged children • Iodine levels in all person over 60 (B,C and D) do not reduce the risk for congenital hypothyroidism, which is often the result of low iodine intake in women of child bearing age) 64. For the past 24 hours, an antidiarrheal agent, diphenoxylate, has been administered to a bedridden, older client with infectious gastroenteritis. Which finding requires the nurse to take further action? • Loss of appetite (expected finding w/infectious gastroenteritis) • Serum K+ 4.o mEq/ or mmol/L (SI) (Normal and should keep monitoring) • Loose, runny stools (expected finding w/infectious gastroenteritis) • Tented skin turgor * Tented skin turgor indicates dehydration; a serious complication follows prolonged diarrhea that requires further intervention by the nurse 65. An older woman who was recently diagnosed with end stage metastatic breast cancer is admitted because she is experiencing shortness of breath and confusion. The client refuses to eat and continuously asks to go home. Arterial blood gas indicate hypoxia. Which intervention is most important for the nurse to implement? • Prepare for emergent oral intubation • Clarify end of life desires (who is terminally ill is the most important intervention and should be done first before any further intervention are implemented) • Initiate comfort measures • Offer sips of favorite beverages 66. After an elderly female client receives treatment for drug toxicity, the healthcare provider prescribes a 24-hour creatinine clearance test. Prior to starting the urine collection, the nurse notes that the client’s serum creatinine is 0.3 mg/ dl. What action should the nurse implement? • Initiate the urine collection as prescribed (even though the serum creatinine is low. Elderly client may develop drug toxicity due to impaired renal function (best evaluated by completing a 24-hour creatinine clearance), because decreased muscle mass often results in a lower serum creatinine) • Notify the healthcare provider of the results (is not necessary) • Evaluate the client’s serum BUN level (is a less specific indicator of renal function than the serum creatinine or creatinine tests) • Assess the client for signs of hypokalemia 67. Following a motor vehicle collision (MVC), an unrestrained female client is admitted to the intensive care unit with altered mental status. She has multiple rib fractures and bruising across her lower abdomen. Which assessment finding warrants immediate intervention by nurse? (Please scroll and view each tab’s information in the clients’ medical record before selecting the answer.) • Several apnea episodes lasting ten seconds • A large amount of gross hematuria • Delayed peripheral capillary refill • Numbness of the left lower extremity (Normal ABG are pH 7.35 to 7.45; pCO2 35 to 45 mmHg; HCO3 22 to 26 mEq/L (mmol/L) and pO2 80 to 100 mmHg. The ABG results reveal partially compensated respiratory acidosis as evidenced by a low pH, high PaCO2, and high HCO3 due to the kidneys attempting to compensate by retaining HCO3 to normalize the PH. Increasing PaCO2 decreases the client’s desire to breath, as evidenced by periods of apena that can progress to respiratory arrest, so this the priority assessment finding.) 68. An adult male who fell from a roof and fractured his left femur is admitted for surgical stabilization after having a soft cast applied in the emergency department. Which assessment finding warrants immediate intervention by the nurse? • Pale, diaphoretic skin (pain or blood loss warrants further investigation) • Pain score 8 out of 10 (normal finding and needs to be treated) • Onset of mild confusion • Weak palpable distal pulses (normal finding and needs to be treated) * onset of any confusion or change in level of consciousness may indicate a life-threatening situation, such as massive loss of blood that often occur with femur fractures or a head injury resulting from the fall. 69. Which assessment finding is most important when planning to provide a complete bed bath to a bedfast client? • 2+ pitting edema of the feet (assessment finding) • Right-sided paralysis (assessment finding) • Orthopnea • Pallor (assessment finding) pale skin * orthopnea: the inability to breath effectively while lying flat, has the greatest implication for the nurse when planning to provide a bed bath to a bedfast client. 70. The nurse is assessing a 3-month-old infant who had a pylorotomy yesterday. This child should be medicated for pain based on which finding(s)? (Select all that apply) • Restlessness • Clenched fists • Increased pulse rate • Increased temperature (sign of infection, not pain) • Peripheral pallor of the skin (more consistent with vasoconstriction related to exposure to cold, anemia, or decreased circulation) • Increased respiratory rate Physiologic responses to pain include restlessness, increased muscle tone, such as clenching fists, an increased pulse rate and respiratory rate all of which occur as the result of stimulation of the sympathetic nervous system. 71. A male client with ulcerative colitis received a prescription for a corticosteroid last month, but because of the side effects he stopped taking the medication 6 days ago. Which finding warrants immediate intervention by the nurse? • Fluid retention (common side effect of taking corticosteroid) • Hypotension and fever (1st sign of precipitous withdrawal) • Anxiety and restlessness (common side effect of taking corticosteroid) • Increased blood glucose (common side effect of taking corticosteroid) * Sudden withdrawal from a corticosteroid can cause sudden decrease adrenal function resulting in low serum sodium, high serum potassium, and low blood pressure, which can lead to shock and possible death. 72. Azithromycin is prescribed for an adolescent female who has lower lobe pneumonia and recurrent chlamydia. What information is most important for the nurse to provide to this client? • Have partners screened for human immunodeficiency virus • Report a sudden onset arthralgia to the healthcare provider • Decrease intake of high-fat foods, caffeine, and alcohol • Use two forms of contraception while taking this drug (antibiotics, especially broad spectrum drugs like azithromycin, decrease the effectiveness of oral contraceptives and some spermicides, so the adolescent should be encouraged to use at least two contraction to prevent pregnancy.) 73. Answer: Observe color of urine Rationale: Prasugrel, a platelet inhibitor, can cause hemorrhage, so it is critical to monitor for signs and symptoms of bleeding such as pink tinged urine 74. A young adult client is admitted to the emergency room following a motor vehicle collision the client’s head hit the dashboard. Admission assessments include: blood pressure 65/45 mm Hg, oral temperature 98.6 F, pulse 124 beats/minutes and respirations 22 breaths/minute. based on these data the nurse formulates the first portion of a nursing diagnosis as “Risk for injury.” What form best expression the “related to” portion of the nursing diagnosis? • Infection • Increased intracranial pressure • Shock • Head injury (is correct BUT is vague and is not specifically related to the assessment data described, so it is not the best answer) * Two signs of shock: decrease BP and increase (often weak and thread) pulse: this client has both symptoms 75. The nurse includes assessment or fat embolism syndrome (FES) in the plan of care for a client with a fractured femur. Which finding should the nurse include that are often the earliest indication of FES? • Confusion, restlessness (also Memory loss) • Tachycardia, fever (also sign of FES but occur later after confusion and restlessness) • Pulmonary crackles (also sign of FES but occur later after confusion and restlessness) • Petechial rash (also sign of FES but occur later after confusion and restlessness) * In FES fat globules transported to the lungs cause a hemorrhagic interstitial pneumonitis, acute respiratory distress syndrome (ARDS), poor oxygen exchanges, and hypoxemia resulting in poor cerebral perfusion. Memory loss, restlessness and confusion 76. Staff report to the charge nurse that they suspect temperature are being measured incorrectly by a certain machine. Which action would be best for the charge nurse to take? • Tell staff to obtain a machine from another unit and use it to take temperature • Call the maintenance department and ask them to pick up the machine for repair • Ask those taking vital signs to compare results of two different machines ( the worker to actually producing the work is the one with the greatest knowledge and the greatest potential for solving the problem) • Spend time at shift change to personally assess the accuracy of the machines 77. The nursing staff on a medical unit includes a register nurse (RN), practical nurse (PN), and an unlicensed assistive personnel (UAP). Which task should the charge nurse assign to the RN? • Supervise a newly hired graduate nurse during an admission assessment (assigned RN) • Transport a client who is receiving IV fluids to the radiology department (assigned UAP) • Administer PRN oral analgesics to a client with a history of chronic pain (assigned PN) • Complete ongoing focused assessments of a client with wrist restraints (assigned PN) 78. After several months on a waiting list, an adult male received a liver transplant a week ago. The nurse notes that he has developed a maculopapular rash on his hands and palms, which client reports itch and hurt. Which finding of graft-versus-host-disease (GVHD) is most important for the nurse to report to the health care provider? • Next cyclosporine dose due tomorrow • White blood cell and differential count • Abdominal pain and frequent diarrhea • Presences of fine tremor of hands GVHD can occur a week to 30 days after transplantation when immune competent cells from transplanted organs attack the immunosuppressed host cells. Which include targeted skin, liver, and gastrointestinal (GI) organs. Assessment for and prevention of infection is the priority intervention for client with possible GVH, so the client’s white blood cell count (WBC) with differential cell counts should be reported. 79. A male client with terminal cancer is brought to the emergency department manifesting a Cheyne-Stoke respiratory pattern. His wife tells the nurse that her husband has an advance directive that indicates a “Do not resuscitate” (DNR) status, but the documents are at home. When the client become apneic and pulseless, what action should the nurse take? • Ask the wife if her husband’s wishes ever changed • Call the healthcare provider for a DNR prescription • Begin cardiopulmonary resuscitation (CPR) • Determine if the family want hospice care If a client’s signed documents, such as a living will or advances, are unavailable, resuscitation efforts should be implemented. 80. Question is a Video Answer: Picking up the second glove 81. The nurse is teaching a mother of a newborn with a cleft lip how to bottle feed her baby using a Medela Haberman feeder, which has a valve to control the release of milk and a slit nipple opening. The nurse discusses placing the nipple’s elongated lip in the back of the oral cavity. What instructions should the nurse provide the mother about feedings? • Squeeze the nipple base to introduce milk into the mouth • Position the baby in the left lateral position after feeding • Alternate milk with water during the feeding • Hold the newborn in an upright position (prevent aspiration) 82. In assessing an older female client with complications associated with chronic obstructive pulmonary disease (COPD), the nurse notices a change in the client’s appearance. Her face appears tense and she begs the nurse to leave her alone. Her pulse rate is 100, and respirations are 26 per minute. What is the primary nursing diagnosis? • Impaired gas exchange related to narrowing of small airways • Death anxiety related to concern about prognosis • Anxiety related to fear of suffocation (A common problem w/clients who have COPD is anxiety. These client cannot aerate their lungs and adequately oxygenate their bodies, so they feed a perpetual state of suffocation which is worse during exacerbation of their COPD) • Ineffective coping related to knowledge deficit about COPD 83. Which intervention should the nurse implement for a client with superficial (First degree) burns? • Spray an anesthetic agent over the burn every 3 to 4 hours • Position the burn victim in front of a cool fan to decrease discomfort • Apply ice packs for 30 minutes to lower surface temperature • Place wet cloths on the burned areas for short periods of time (provides comfort and helps to relieve the pain of a first degree burn, which involves only the epidermal layer skin) 84. Following breakfast, the nurse is preparing to administer 0900 medication to clients on a medical floor. Which medication be held until a later time? • The loop-diuretic furosemide (Lasix), for a client with serum potassium level of 4.2 mEq/L • The mucosal barrier, sucralfate (Carafate), for a client diagnosed with peptic ulcer disease • The antiplatelet agent aspirin, for a client who is scheduled to be discharge within the hour • The antifungal mystatin (Mycostatin) suspension, for a client who has just brushed his teeth Carafate coasts the mucosal lining prior to eating a meal, so this medication should be held until prior to the next meal. 85. A female client is taking alendronate, a bisphosphonates, for postmenopausal osteoporosis. The client tells the nurse…. Experiencing jaw pain. How should the nurse respond? • Determine how the client is administering the medication • Confirm that this is a common symptom of osteoporosis • Report the client’s jaw pain to the healthcare provider • Advise the client to gargle with warm salt water twice daily * Bisphosphonates, including alendronate can cause osteonecrosis of the jaw, resulting in jaw pain for evaluation. 86. A client with a cervical spinal cord injury (SCI) has Crutchfield tongs and skeletal traction applied as a method of closed reduction, which intervention is most important for the nurse to include in the client’s plan of care? • Provide daily care of tong insertion sites using saline and antibiotic ointment • Modify the client’s diet to prevent constipation (plan of care but less importance than prevention infection) • Encourage active range of motion q2 to 4 hours (plan of care but less importance than prevention infection) • Instruct the client to report any symptoms of upper extremity paresthesia(plan of care but less importance than prevention infection) Crutchfield tongs, a skeletal traction device for cervical immobilization, requires daily care of the surgically inserted tongs to minimize the risk of infection of the insertion site and cranial bone. Daily cleansing with normal saline solution and antibiotic ointment application minimizes bacterial colonization and helps to prevent infection. 87. An adult woman who is seen in the clinic with possible neuropathic pain of the right leg rates her pain as a 7 on a 10-point scale. Which action should the nurse take? • Elevate the foot and leg on two pillows • Measure the client’s capillary glucose • Ask the client to dorsiflex the right food • Encourage the client to describe the pain (Neuropathic pain is caused by damage within the nervous system. Descriptions of pain, such as burning, tingling, or numbness help identify the pain as neuropath, allowing appropriate treatment to be initiated. 88. Correct answer 89. A nine-day-old infant with congenital adrenal hyperplasia (CAH) develops dehydration and is admitted to the hospital for aldosterone replacement therapy. The healthcare provider prescribes fludrocortisone acetate (Florinel) 0.05 mg PO daily. Which finding indicates the newborn is experiencing a therapeutic response? • Resting blood pressure of 62/41 mmHg (are not therapeutic responses to aldosterone replacement therapy) • Plasma glucose 45 mg/dl (are not therapeutic responses to aldosterone replacement therapy) • Serum sodium 142 mEq/L (newborns norm 134-146 mEq/L) • Capillary refill greater than 3 seconds (are not therapeutic responses to aldosterone replacement therapy) Infants with CAH produce inadequate cortisol and aldosterone that leads to dehydration and salt-losing crises, which require urgent medical intervention. Aldosterone replacement therapy is prescribed to promote increase reabsorption of sodium and water in the distal renal tubules, which should result in a normalization of serum sodium 90. The nurse requests a meal tray for a client who follow Mormon beliefs and who is on clear liquid diet following abdominal surgery. Which menu items should the nurse request for this client? (select all that apply) • Hot chocolate (not allowed in clear liquid diet) • Apple juice (clear diet and consumed by Mormons) • Chicken broth (clear diet and consumed by Mormons) • Orange juice (not allowed in clear liquid diet) • Black coffee (yes clear diet but not consumed by Mormons) 91. While eating breakfast, a client admitted with syncope and a 2-month history of vertigo complains of dizziness. Using the standard communication tool SBAR (Situation, Background, Assessment, Recommendation), which statement is best for the nurse to provide the healthcare provider about the client’s background • Blood pressure is 80/40 mmHg, and heart rate is 132 beats/minute • The client’s significant history includes atrial fibrillation and hypoglycemia • While eating breakfast, the client complained of feeling dizzy • If the client has recurrent vertigo, a PRN prescription may be needed 92. At 0600 while admitting a woman for scheduled repeat cesarean section (C-section), the client tells the nurse that she drank a cup of coffee at 0400 because she wanted to avoid getting a headache, which action should the nurse take first? • Ensure preoperative lab results are available (the nurse should then implement) • Start prescribed IV with Lactated Ringer’s (based on the anesthesia provider’s decision, the nurse may then proceed with this choice) • Inform the anesthesia care provider • Contact the client’s obstetrician (the nurse should then implement) Surgical preoperative instruction include NPO after midnight the day of surgery to decrease the risk of aspiration should vomiting occur during anesthesia. While it is possible the C-section will be done schedule or rescheduled for later in the day, the anesthesia provider should be notified first to make that decision. 93. Which fetal heart rate pattern requires immediate nursing intervention? • A fetal heart rate deceleration that mirrors the contraction • An increase in the fetal heart to 180 that quickly returns to baseline • A fetal heart rate deceleration that occurs at the acne of the contraction • A decrease in the fetal heart rate that occurs after the peak of a contraction A decreased fetal heart rate after the peak of a contraction is an ominous sign and indicates fetal distress (hypoxia) 94. A newborn infant is receiving positive pressure ventilation after delivery. Based on which assessment finding should the nurse initiate chest compressions? • Apgar score 7 • Heart rate 54 • Central cyanosis • Limp muscle tone Chest compression should be initiated when a newborn’s HR is less than 60 beats/minutes, despite the use of positive pressure ventilation 95. A primigravida at 36-weeks gestation, who is Rh negative experienced abdominal trauma in a motor vehicle collision. Which assessment finding is most important for the nurse to report to the healthcare provider? • Positive fetal hemoglobin testing • Fetal heart rate of 162 beats/minute • Trace of protein in the urine • Mild contractions every 10 minutes 96. A couple who is trying to have a baby ask the nurse when they are most likely to conceive a child. The woman has a regular 36-day menstrual cycle, and the first day of her last menstrual period was on January 16. Which information should the nurse provide? Answer: Plan to have intercourse on February 7, as this is when ovulation should occur 97. Which action should the school nurse implement to provide secondary prevention for school-aged children? Answer: initiate a hearing and vision screening program for first graders 98. The nurse is caring for a one-week-old infant who has ventriculoperitoneal (VP) shunt that was place 2 days after birth. Which finding are an indication of postoperative complication? (select all that apply) • Poor feeding and vomiting • Leakage of CSF from the incisional site • Hyperactive bowel sounds • Abdominal distention • White blood cell count of 10,000/mm3 99. A young female college student visits the health clinic in early winter to obtain birth control pills. The clinic nurse ask if the student has received an influenzas vaccination. The student states she did not receive a vaccination because she has asthma. How should the nurse response? Answer: Offer to provide the influenza vaccination to the student while she is at the clinic 100. An adult male is admitted to psychiatric unit from the emergency department because he is in the manic stage of bipolar disorder. He has lost 10 pounds in the last two weeks and has not bathed in a week because he has been “trying to start a new business” and is “too busy to eat.” He is alert and oriented to time, place and person, but no situation. What nursing problem has the greatest priority? • Hygiene self-care deficit • Imbalance nutrition • Disturbed sleep pattern • Self-neglect 101. A 12-year old boy who had an appendectomy two days ago is receiving 0.9% normal saline at 50 ml/hour. His urine specific gravity is 1,035. What action should the nurse implement? Answer: Encourage popsicles and fluids of choice 102. In assessing an infant 10 hours after birth, the nurse note the infant slight cyanotic and has a large amount of mucous. Which intervention should the nurse implement first? • Begin oxygen at 2 L/minute • Insert a nasogastric tube • Suction the infant as needed • Assess the heart rate 103. A client with eczema is experiencing severe pruritus. Which PRN prescriptions should the nurse administer? (Select all that apply) Answer: • Topical corticosteroid • Oral antihistamine 104. A female client is taken to the urgent care clinic after a fainting while exercising at the gym. She is weak, pale, and diaphoretic. Which intervention should the nurse implement first? • Offer an oral hydration drink • Auscultate heart sounds • Check blood glucose level • Perform a 12-lead electrocardiogram 105. An adult male is admitted to the emergency department after falling from a ladder. While waiting to have a computed tomography (CT) scan, he requests something for a severe headache. When the nurse offers him a prescribed does of acetaminophen, he asks…something stronger. Which intervention should the nurse implement? • Request that the CT scan be done immediately • Review client’s history for use of illicit drug • Assess client’s pupils for their reaction to light • Explain the reason for using only non-narcotics 106. A nurse who is working in the emergency department triage area during the evening shift is presented with four clients at the same time. The client presenting with which symptoms requires the most immediate intervention by the nurse? • Low-grade fever, headache, and malaise for the past 72 hours • Unable to bear weight on the left foot, with swelling and bruising • Chest discomfort one hour after consuming a large, spicy meal • One-inch bleeding laceration on the chin of a crying 5-year-old 107. A client with cirrhosis of the liver is admitted with complication related to end stage liver disease. Which interventions should the nurse implement? (Select all that apply) • Monitor abdominal girth • Increase oral fluid intake to 1,500 ml daily • Report serum albumin and globulin levels • Provide diet low in phosphorus • Note signs of swelling and edema 108. The charge nurse is observing the care provided for a client with acquired immune deficiency syndrome (AIDS) who was admitted yesterday with Pneumocystis carinii pneumonia. Which observation is an indication that staff education is needed? • An environmental service technician wears gloves to use a bleach solution to wipe up blood • A nursing student is wearing a mask while taking the client’s blood pressure (mask and gloves are only necessary when there is the possibility of direct contact with the client’s blood and body fluids, which not likely to occur while taking a BP) • A laboratory technician is wearing gloves while performing a venipuncture • The staff nurse is allowing visitors to enter the client’s room without donning personal protection 109. The nurse is explaining the need to reduce a salt intake to client with primary hypertension. What explanation should the nurse provider? • High salt can damage the lining of the blood vessels • Too much salt can cause the kidneys to retain fluid • Excessive salt can cause blood vessels to construct • Salt can cause inflammation inside the blood vessels 110. An older adult male is admitted to the stroke unit after recovery from the acute phrase of an ischemic cerebral vascular accident (CVA). Which interventions should the nurse include in the plan of care during convalescence and rehabilitation? (Select all that apply) • Suction oral cavity q4 hours • Place a bedside commode next to bed (safety) • Play classical music in room while client is awake • Measure neurological vital signs q4 hours (Monitor neurological status guides care, monitors client’s progress, and identifies early sign of complications) • Encourage family to participate in the client’s care (Helps prepare for home care and demonstrates the values of family members providing participative care for the client) 111. Before leaving the room of a confused client, the nurse notes that a half bow knot was used to attach the client’s wrist restraints to movable portion of the client’s bed frame. What action should the nurse take before leaving the room? • Ensure that the knot can be quickly released (Maintain client safety) • Tie the knot with a double turn or square knot (requires more time to release if a rapid response is needed) • Move the ties so the restraints are secured to the side rails (may cause harm to the client if the side rail is moved without first releasing the restraint) • Ensure that the restraints are snug against the client’s wrists (restraints should fit loosely (Two fingers should fit under the restraint) to prevent damage to the client’s skin) 112. The healthcare provider prescribes a maintenance dose of norepinephrine bitartrate at 4 mcg/minute for a client with septic shock. The pharmacy provides a solution containing 8 mg in 250 ml of D5W. The nurse should program the infusion pump to deliver how many ml/hr? Answer: 7.5 ml/hour 4 mcg/min x 60 min = 240 mcg/hr 8 mg x 1000 mcg = 8000 mcg 8000 mcg: 250 ml = 240 mcg: X ml 8000X = 60,000 X = 7.5 ml/hour 113. A client with a prescription for “do not resuscitate” (DNR) begins to manifest signs of impending death. After notifying the family of the client’s status, what priority action should the nurse implement? a. The impending signs of death should be documented b. The client’s need for pain medication should be determined c. The nurse manager should be updated on the client’s status d. The client’s status should be conveyed to the chaplain 114. A 62-year-old male client who has been diagnosed with emphysema, asks the nurse to tell him about the symptoms of hid disease. Which statement should be included in the nurse’s description of emphysema to this client? a. “Breathing through pursed lips causes lung expansion and decreased physical exertion.” b. “Tolerance for oxygen deprivation results in an increased ability to carry out daily activities.” c. “A barrel chest results because of using a hyperventilating breathing pattern.” d. “Oxygen requirements decrease because of the overexpansion of alveoli.” 115. A client who is admitted to the intensive care unit with a right chest tube attached to a THORA-SEAL chest drainage unit becomes increasingly anxious and complains of difficulty breathing. The nurse determines the client is tachypneic with absent breath sounds in the client’s right lung fields. Which additional finding indicates that the client has developed a tension pneumothorax? a. Continues bubbling in the water-seal chamber- indicates that there is a loose connection in the chest drainage system b. Decreased bright red bloody drainage- occurs with an obstructor or a displaced chest tube c. Tachypnea with difficulty breathing- are early signs of respiratory distress, which can result from a variety of causes, including a pneumothorax d. Tracheal deviation toward the left lung- tracheal deviation toward the unaffected left lung with absent breath sounds over the affected right lung are classic late signs of a tension pneumothorax 116. Prior insertion of an indwelling urinary catheter, what client information is most important for the nurse to obtain? a. Client allergies to antiseptic solutions- knowledge of all allergies prior to cleansing with a medication or solution is the highest priority because it may present a possible allergic reaction b. Previous history of urinary tract infections c. Client’s ability to increase fluid intake d. Color, clarity and odor of urine 117. A young woman with multiple sclerosis just received several immunizations in preparation for moving into a college dormitory. Two days later, she reports to the nurse that she is experiencing increasing fatigue and visual problems. What teaching should the nurse provide? a. Plans to move into the dormitory need to be postponed for at least a semester b. These early signs of an infection may require medical treatment with antibiotics c. These are common side effects of the vaccines and will resolve in a few days d. Immunization can trigger a relapse of the disease, so get plenty of extra rest 118. A young adult male was admitted 36 hours ago for a head injury that occurred as the result of a motorcycle accident. In the last 4 hours, his urine output has increased to over 200 ml/hour. Before reporting the finding to the healthcare provider, which intervention should the nurse implement? a. Evaluate the urine osmolarity and the serum osmolarity values b. Obtain blood pressure and assess for dependent edema c. Measure oral secretions suctioned during last 4 hours d. Obtain capillary blood sample q2 hour for glucose monitoring 119. A client at 30-weeks gestation is admitted due to preterm labor. A prescription of terbutaline sulfate 0.25 mg is given subcutaneously. Based on which finding should the nurse withhold the next dose of this drug? a. Maternal blood pressure of 90/60 b. Fetal heart rate of 170 beats per minute for 15 minutes c. Maternal pulse rate of 162 beats per minute d. Serum potassium of 2.8 mg/dl 120. Medical asepsis requires that the nurse include what handwashing technique? a. Hold hands higher than the elbows and scrub vigorously b. Use hot water to ensure that pathogens are killed c. Use circular motion, washing from clean to dirty areas d. Rinse soap off keeping hands and forearms lower than elbows 121. When assessing a male client, the nurse notes that he has unequal lung expansion. What conclusion regarding this finding is most likely to be accurate? The client has a. Collapsed lung b. History of COPD c. A chronic lung infection d. Normally functioning lungs 122. Which conditions are most likely to respond to treatment with antihistamines? Select all that apply. a. Allergic rhinitis b. Contact dermatitis c. Otitis media d. Bronchitis e. Myocarditis 123. A client arrives on the surgical floor after major abdominal surgery. What intervention should the nurse perform first? a. Administer prescribed pain medication b. Assess the surgical site c. Determine the client’s vital signs d. Apply warmed blankets 124. An older woman who lives alone in a two-story home is admitted after falling while shopping. X-rays reveal a fractured left hip. With no immediate family in the area, the client is concerned about her pets. Which intervention should the nurse implement? Select all that apply. a. Palpate and mark pedal pulses b. Alert social worker of client’s concerns c. Assess ability to bear weight when standing d. Evaluate pain using a standard pain scale e. Support left leg with two pillows 125. A client with chronic obstructive lung disease who is receiving oxygen at 1.5 liters/minute by nasal cannula, is currently short of breath. What action should the nurse take? a. Increase oxygen to three liters/minute -increasing the oxygen level decreases the hypercarbia drive to breathe b. Have the client breathe into a paper bag c. Ask the client to take short, rapid breaths d. Instruct the client in pursed lip breathing -keeps the aveoli open by maintaining positive pressure in thoracic cavity 126. A middle-aged woman, diagnosed with Graves’ disease, asks the nurse about this condition. Which etiological pathology should the nurse include in the teaching plan about hyperthyroidism? Select all that apply. a. Graves’ disease, an autoimmune condition, affects thyroid stimulating- b. Large protruding eyeballs are a sign of hyperthyroid function c. Early treatment includes levothyroxine d. T3 and T4 hormone levels are increased e. Weight gain is a common complaint in hyperthyroidism Graves’ disease is an autoimmune disorder in which thyroid stimulating antibodies activate thyroid simtulating hormone (TSH) receptors causing an increased production of thyroid hormone (T3 and T4). Manifestations include exophthalmos and weight loss, not weight gain. Treatment includes medication to block synthesis of thyroid hormone, so levothyroxine is contraindicated 127. An adult woman suffered burns to her face and chest resulting from a grease fire. On admission, airway protection with endotracheal intubation was required and a 2 liter bolus of normal saline was administered. Currently the normal saline is infusing at 250 ml/hour. The client’s heart rate is 120 beats/minute, blood pressure 90/50 mmHg, respirations are 12 breaths/minute over the ventilated 12 breaths for a total of 24 breaths/minute, and the central venous pressure (CVP) is 4 mm H2O. Which intervention should the nurse implement? a. Infuse an additional bolus of normal saline- burns require a massive amount of fluid resuscitation. A low CVP (normal 5-12 mm H2O) and low blood pressure indicate the need for additional IV fluids b. Increase the oxygen delivered by the ventilator- the ventilator respirations may need to be increased, but there is no evidence to support increasing the oxygen c. Bring a tracheotomy tray to the bedside- not necessary d. Lower head of the bed to recumbent position- is contraindicated 128. At 1130, the nurse assumes care of an adult client with diabetes mellitus who was admitted with an infected foot ulcer. After reviewing the client’s electronic health record, which priority nursing action should the nurse implement? a. Obtain antibiotic peak and trough levels b. Administer insulin per sliding scale- a blood glucose level of 450 mg/dl or 25 mmol/L indicates significant hyperglycemia that requires immediate treatment with insulin c. Assess appearance of foot wound d. Initiate hourly urine output measurements- indicated in response to the onset of hypotension, and should be implemented after 129. A client who weighs 176 pounds receives a prescription for enoxaparin sodium 80 units subcutaneously daily at 0900. What action should the nurse take before administering this medication? a. Explain the client the painful effects of administering enoxaparin sodium- if given correctly, subcutaneous enoxaparin sodium should not cause pain b. Clarify the correct dosage with the healthcare provider- Enoxaparin sodium 80 units is within the recommended dosage range, 1 mg/kg c. Determine if the client is receiving heparin or warfarin- before initiating therapy with an anticoagulant such as enoxaparin sodium, current use of another anticoagulant, like heparin or warfarin, should be determined because concomitant use of two anticoagulants can result in hypocoagulation. d. Use a filter needle to give the subcutaneous injection- Enoxaparin sodium is available as a prefilled syringe with an attached needle so is not needed 130. A 15-year-old male is attending an after-school adolescent group session because he frequently loses his temper, argues with his teachers, and refuses to comply with classroom rules. During the group session, the adolescent repeatedly blames others regardless of the situation. To help modify the adolescent’s behavior, what action should the nurse implement? a. Encourage the client to ventilate his feelings of anger- it is important for clients to verbalize feelings b. Describe the consequences of his behavior in concrete terms-to proactively manage this adolescent’s oppositional behavior, the nurse should describe the consequences for specific, offensive behaviors c. Ignore blaming behavior and praise the client’s appropriate behavior- although providing positive feedback for appropriate behavior is a reinforcer that helps shape behavior and increase self esteem, the blaming behavior should not be ignored d. Explain that blaming others limits his psychological growth- is likely to elicit defensiveness 131. A female client is admitted to the hospital for evaluation of severe abdominal pain. Laparoscopy examination reveals multiple ovarian cysts and a total abdominal hysterectomy with bilateral salpingo-oophorectomy is scheduled for the next day. In providing care for this client the evening before surgery, what nursing action has the highest priority? a. Assess IV sites for administration of fluids- not as important b. Administer a douche and an enema to the client- may be prescribed preoperatively, but clients often choose to self-administer these procedures c. Ask the client about her thoughts or concerns- promoting a positive body image and decreasing anxiety related to impending surgery are important factors related to preoperative care d. Discuss prevention of infection after surgery- most dependent on the medical and nursing care provided during and after surgery 132. Dopamine hydrochloride 2 mcg/kg/minute is prescribed to promote renal perfusion for a client weighing 198 lbs. The pharmacy sends a pre-mixed bag of dopamine containing 400 mg in 250 ml D5W. An IV pump is available that provides a precision infusion rate to a tenth of a ml. The nurse should set the IV pump to deliver how many ml/hour? Answer: 6.8 198 lb/2.2lb/kg = 90 kg x 2 mcg = 180 mcg/min x 60 min = 10,800 mcg/hr = 10.8 mcg 10.8 mg/hr / 400 mg x 250 ml = 2,700 / 400 = 6.75 = 6.8 ml/hr 133. (AUDIO) The nurse is auscultating a client’s heart sounds. Which description should the nurse use to document this sound? (please listen to the audio file to select the option that applies. a. S1 S2 b. S1 S2 S3 c. Murmur d. Pericardial friction rub 134. The nurse is counseling a family whose 5-year-old daughter was killed by a hit and run driver. The 10-year old daughter child tells the nurse that she should have been watching her sister better. After the nurse tells the child that she did not cause the accident, which response is best for the nurse to provide? a. Explain to the child that the accident was the fault of the person driving b. Inquire if the parents or others were watching when the accident occurred c. Ask the child to share what could have done to stop this from happening- exploring the child’s feelings by asking the child what could have been done to prevent this tragic accident is the first response to help the child and family cope with their grief and underlying guilt about the accident d. Question the parents if the child had the duty to watch her sister- can cause the parents to feel guilty 135. A woman at 12-weks gestation comes to the clinic for her first prenatal visit. After completing a health history, the nurse should also discuss which issue about pregnancy at this initial visit? a. Cultural practices related to childbearing- to ensure culturally competent care, information that is specific to the client’s cultural beliefs, practices, and family values should be discussed to ensure client care is culturally sensitive b. Concerns about parenting c. Knowledge about labor and delivery d. Complications associated with childbirth 136. A 38-week gestational age infant of a diabetic mother (IDM) is admitted to the newborn nursery weighing 8 pounds and 2 ounces, and is transitioning without respiratory distress. Within the first hours of transition after birth, what priority nursing assessment is necessary for this infant? a. Congenital anomalies b. Hypoglycemia c. Birth injuries d. Hyperbilirubinemia 137. The public health nurse receives funding to initiate a primary prevention program in the community. Which program best fits the nurse’s proposal? a. Case management and screening for clients with HIV- secondary prevention b. Regional relocation center for earthquake victims- tertiary prevention, such as recovery efforts c. Vitamin supplements for high- risk pregnant women- primary prevention activities focus on health promotion and disease prevention, so vitamin supplementation for high-risk pregnant women provides adequate vitamins and minerals for fetal development d. Lead screening for children in low-income housing- secondary prevention 138. An IV infusing in a client’s left forearm becomes infiltrated. After removing the IV, which sites should the nurse select as possible sites to insert another IV catheter? Select all that apply a. Right hand- should be inserted in the opposite extremity b. Left hand- may result in continued infiltration of IV fluids c. Right forearm- should be inserted in the opposite extremity d. Right subclavian- sites used for insertion of central venous catheters e. Left subclavian- sites used for insertion of central venous catheters 139. Which medication should the nurse anticipate administering to a client who is diagnosed with myxedema coma? a. Intravenous administration of thyroid hormones- the high mortality of myxedema coma requires immediate administration of IV thyroid hormones b. Oral administration of hypnotic agents- is contraindicated, because even small doses can cause profound somnolence lasting longer than expected c. Intravenous bolus of hydrocortisone- is administered to clients diagnosed with adrenal insufficiency (Addison crisis) d. Subcutaneous administration of vitamin K- to clients who have had an overdose of warfarin 140. Which environment factor is most significant when planning care for a client with osteomalacia? a. Cool, moist air b. Adequate sunlight- a client with osteomalacia is lacking adequate Vitamin D, so treatment should include short periods of exposure to sunlight c. Quiet, calm surroundings d. Stimulating sounds and activity 141. A woman who had bariatric surgery 2 months ago is admitted because of vomiting and inability to tolerate food and liquids. She states that she is pain free. Which intervention should the nurse include in the client’s plan of care? a. Encourage positive self accolades for dietary adherence b. Determine if the client is over-hydrating to feel satiated c. Maintain the client on an NPO status d. Administer daily vitamin supplements 142. When a blood transfusion is prescribed for a client with large uterine fibroids, she states that she is afraid of getting acquired immunodeficiency disease (AIDS) from the blood transfusion. What response is best for the nurse provide? a. Ask the client to talk about her feelings regarding AIDS b. Have the healthcare provider explain the risks involved c. Inquire about client’s exposure through sexual partners d. State that rigorous blood product screening negates risks 143. The nurse who working in the emergency department is obtaining evidence for a rape kit from a woman who reports that she was raped while returning to her dormitory from the university library. Which intervention is most important for the nurse to implement? a. Do not allow client to shower until all evidence is obtained (it is most important to gather evidence, and a shower distorts such evidence) b. Report the incident to the university’s security department c. Listen attentively to the client’s description of the event d. Determine the client’s personal reaction to the reported rape 144. The nurse is assigned to care for a client diagnosed with psoriasis. What behavior by the nurse addresses this client’s psychosocial need for acceptance? a. Encouraging the client to join a support group b. Shaking the client’s hand during an introduction (touch, more than any other gesture, communicates acceptance of the client with a skin problem such a psoriasis) c. Wearing gloves when interviewing client d. Allowing the client to ventilate feelings 145. The nurse is preparing to gavage feed a premature infant through an orogastric tube. During insertion of the tube, the infant’s heart rate drops to 60 beats/minute. Which action should the nurse take? a. Continue the insertion since this is a typical response (may precipitate further bradycardia) b. Insert the feeding tube into the infant’s nasal passage (Traumatizes the nasal mucosa, which can cause edema that obstructs nasal breathing) c. Pause and monitor for a continued drop of the heart rate (Insertion of an orogastic tube for gavage feedings often trigger vagus stimulation, which can result in bradycardia. Pausing during insertion and monitoring the infant’s HR and color nay be all that is necessary for the HR to return to normal) d. Postpone the feeding until the infant’s vital signs are stable (The feeding should be given since a HR drop alone does not indicate instability) 146. A client who weighs 75 kg is receiving IV dopamine at 2 mcg/kg/minute. The concentration of the dopamine solution is 200 mg/250 ml of D5NS. How many ml/hour should the nurse program the infusion pump? Answer: 11 2 mcg x 75 kg = 150 mcg/minute 150 mcg x 60 minutes = 9000 mcg/hour = 9 mg/hour 9 mg/hour / 200 mg x 250 ml = 11.25 = 11 ml/hour 147. Immediately after extubation, a client who has been mechanically ventilated is placed on a 50% non-rebreather. The client is hoarse and complaining of a sore throat. Which assessment finding should the nurse report to the healthcare provider immediately? a. Oxygen saturation 90%- should be titrated to achieve an oxygen saturation of 94% b. Upper airway stridor- consistent with airway swelling and obstruction that if not resolved is life-threatening and should be reported to the HCP immediately c. Expiratory wheezing- not life threatening d. Blood-tinged sputum- common following extubation and results from mucosal trauma 148. A client who has a tracheal stoma is complaining of mouth pain. While performing oral care, the nurse determines that the client has mouth ulcers and that the oral mucosa is irritated. The client also has halitosis. Which intervention should the nurse implement? a. Encourage frequent use of a mouthwash- routine mouth care is necessary but should not be done too frequently b. Apply viscous gel to ulcers during mouth care- an oral viscous gel such as lidocaine anesthetic can be used to temporarily relieve the pain c. Provide flavored oral swabs to use q2 hours d. Rinse out mouth with liquid germicide daily 149. The nurse brings an oral medication prescribed to be given daily to a male client who tells the nurse that he will take his medications later. What action should the nurse implement? a. Inform the client that his medication is scheduled to be taken now b. Leave the medication on the bedside table with a fresh glass of water c. Note the client’s noncompliance with medications in the nurse’s notes d. Agree upon a time to return to the client’s room with the medication (Direct observation of a client ingesting medication is a safe practice of medication administration that validates administration time and client compliance, so the nurse should return with the medication later. Preferably at a time agreed upon by the nurse and client) 150. An adult male is admitted to a rehabilitation center after 3 weeks in an acute care hospital. The client suffered a right-sided brain injury that occurred as the result of a fall from a ladder. Which intervention should the nurse include in this client’s plan of care? a. Maintain elastic stockings continuously b. Apply a hand splint for finger extension (the client suffered a right-sided brain, so his left hand is likely to experience some degree of paralysis. The use of a hand splint keep finger in extension and prevents contractures that can impede any rehabilitation efforts to reestablish some degree of dexterous function.) c. Monitor blood pressure every 4 hours d. Give antithrombolytic injections daily A,C and D are interventions that should be included in the client’s plan of care, especially during the acute phase of treatment, but may not be necessary during rehabilitation [Show More]
Last updated: 2 years ago
Preview 1 out of 49 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 13, 2022
Number of pages
49
Written in
Additional information
This document has been written for:
Uploaded
Mar 13, 2022
Downloads
0
Views
116


.png)


.png)

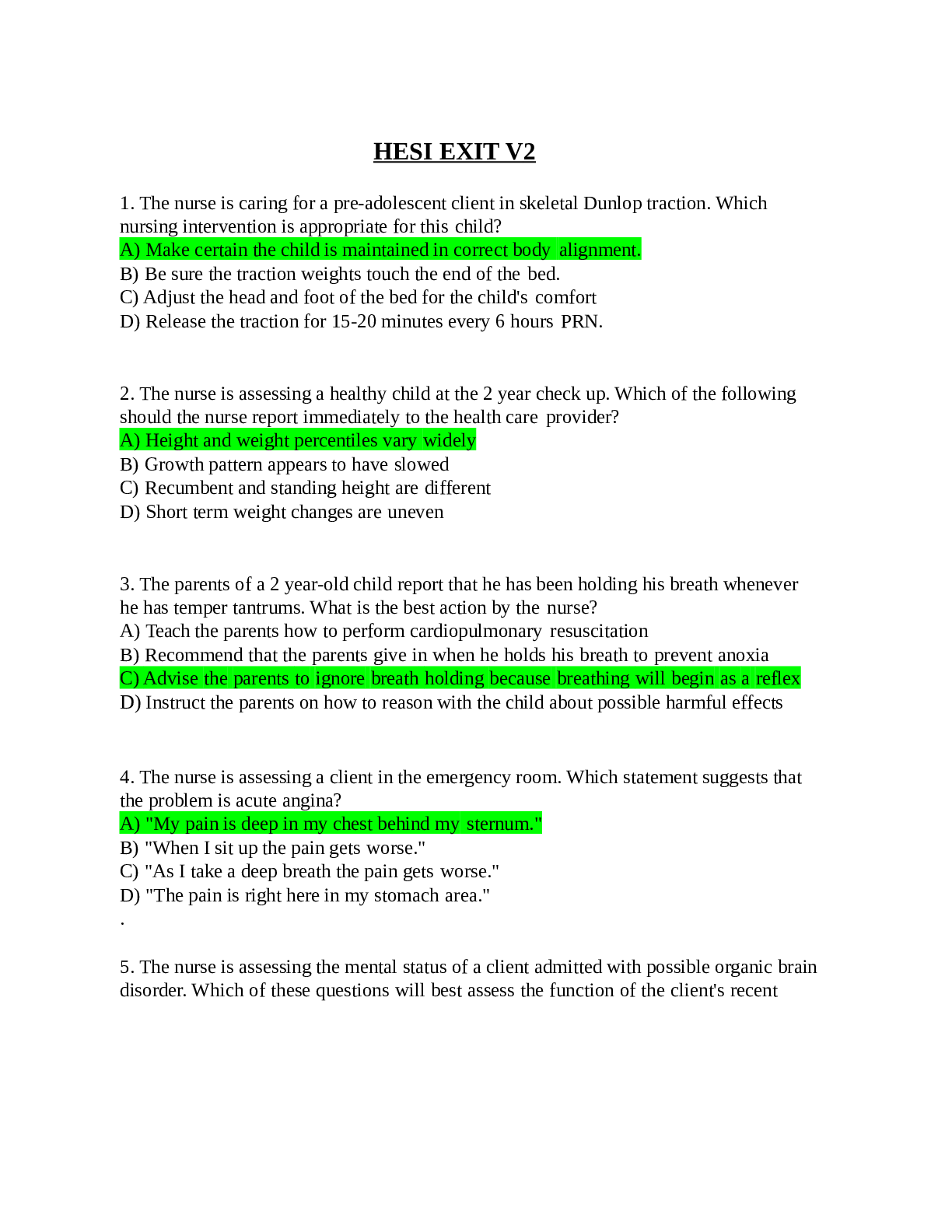





 Questions and Answers with elaborations.png)