Mid-Term Study Guide Week 4
review concepts related to anticholinergic drugs and the treatment for asthma,
bronchitis and associated pathogenesis; chronic bronchitis and related acid/base
disturbances, perfusion, bloo
...
Mid-Term Study Guide Week 4
review concepts related to anticholinergic drugs and the treatment for asthma,
bronchitis and associated pathogenesis; chronic bronchitis and related acid/base
disturbances, perfusion, blood flow between the heart and lungs, asthma signs and
symptoms, bronchioles, alveolar hyperinflation with asthma, polycythemia vera;
mechanism of action of anticholinergic drugs to treat asthma
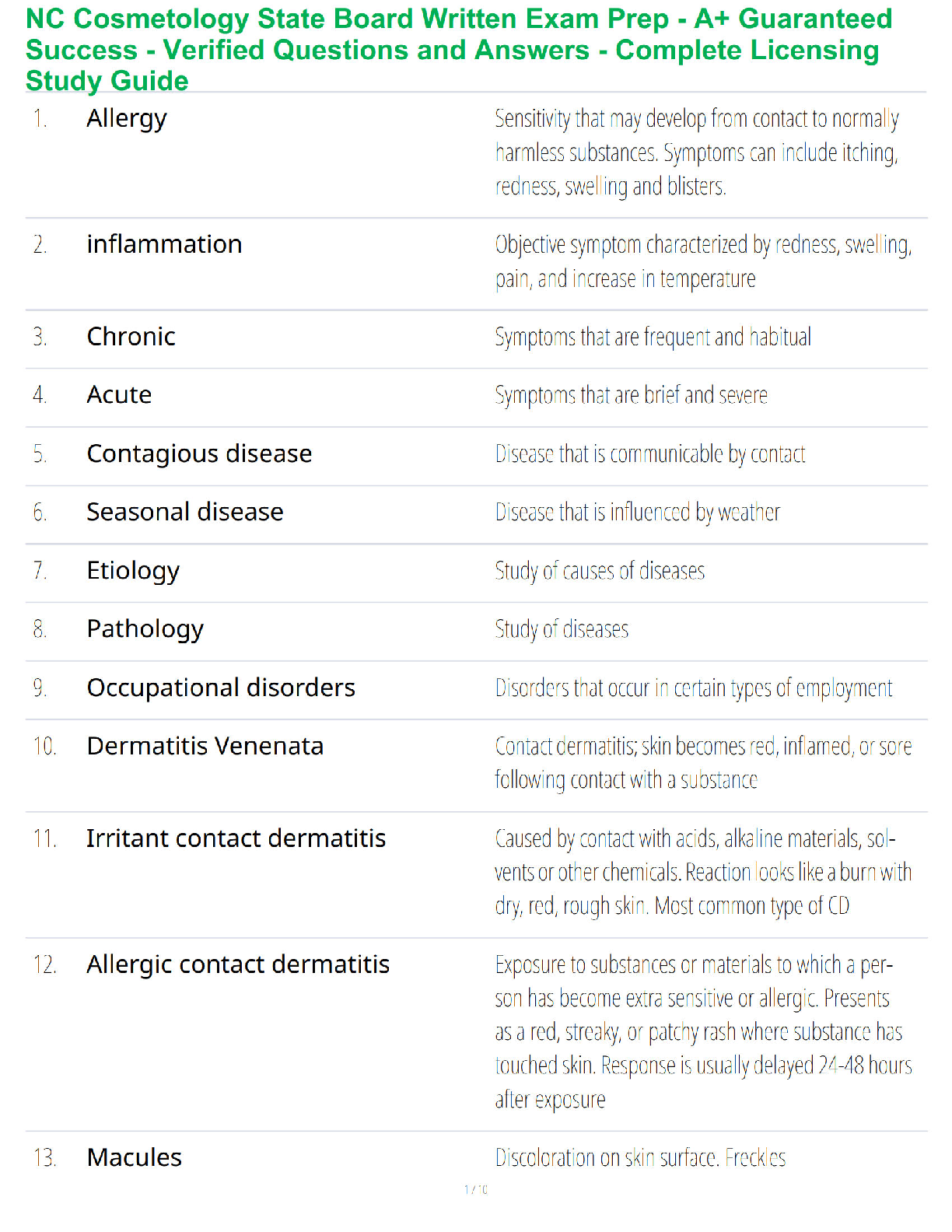
Asthma is a chronic inflammatory disease characterized by sensitization to
allergens, bronchial hyperreactivity, and reversible airway obstruction. Asthma is
initiated by a type I hypersensitivity reaction primarily mediated by IgE. Airway
epithelial exposure to antigen initiates both an innate and an adaptive immune
response in sensitized individuals. Many cells and cellular elements contribute to
the persistent inflammation of the bronchial mucosa and hyperresponsiveness of
the airways, including macrophages (dendritic cells), T helper 2 (Th2)
lymphocytes, B lymphocytes, mast cells, neutrophils, eosinophils, and basophils.
There is both an immediate (early asthmatic response) and a late (delayed)
response. In young children, airway obstruction can be more severe because of the
smaller diameter of their airways.
Asthma is caused by complex interaction of genetic and environmental factors.
Asthma results in excess mucus production and accumulation hypertrophy of
bronchial smooth muscle airflow obstruction decreased alveolar ventilation.
Asthma can take two forms: extrinsic and intrinsic. The most common symptoms
of both extrinsic and intrinsic asthma are: coughing, wheezing shortness of breath
rapid breathing chest tightness
Extrinsic: The plugs of mucus and pus from this inflammatory process can block
alveolar passageways,
leading to air-trapping and hyperinflation more signs and symptoms consistent
with the diagnosis of asthma
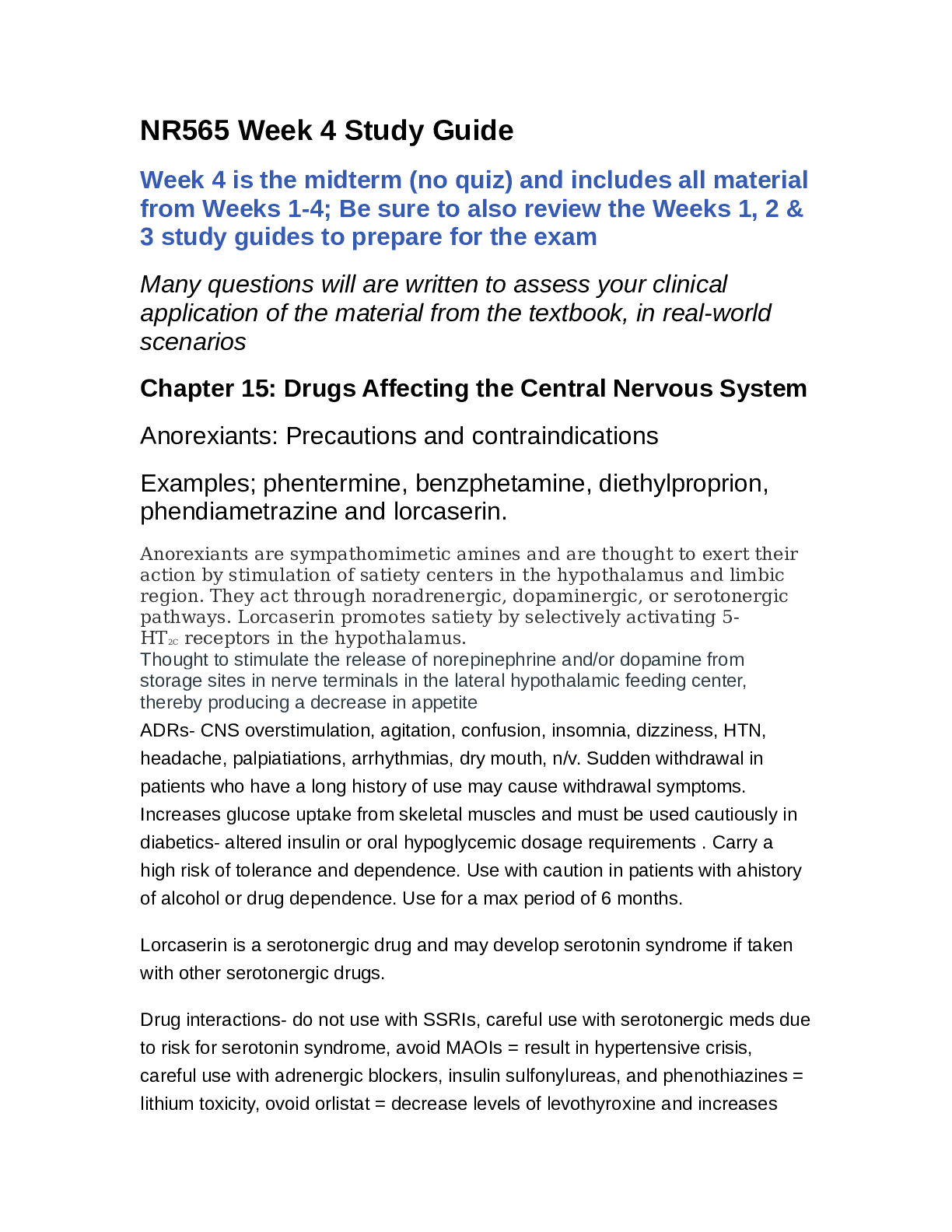
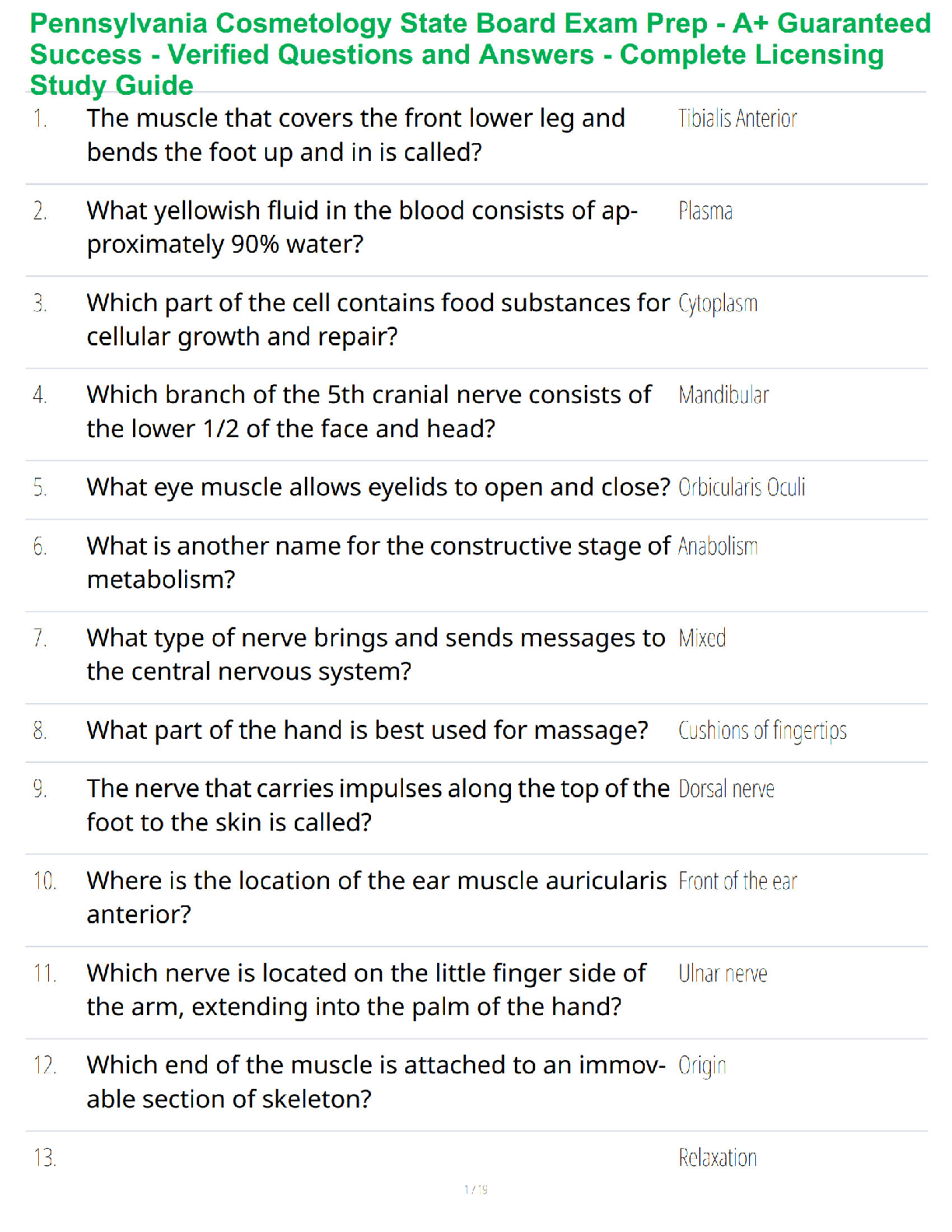
This process is illustrated in this image which shows the airway pathology in its
entirety mast cell degranulation triggered by the excessive amounts of IGE that
have airingly formed this individual that will bind that allergen as it enters the
airway that mast cell degranulation releases chemicals that releases mucus
production and accumulation as well as chemicals that contribute to smooth muscle
constriction that smooth muscle constriction along with mucus plugs that form
result in hyperinflation of the alveoli and eventual erosion of airway tissue
Intrinsic: can be triggered by a variety of non-allergic factors, each causing a
slightly different variation on the inflammatory process.
Regardless of the underlying cause of asthma, the disease process has both a
bronchoconstriction component and an inflammation component.
Pharmacotherapy focuses on one or both of these components to provide fast relief
for acute bronchospasms, as well as long-term control to reduce the frequency of
asthma attacks.
Chronic Bronchitis:
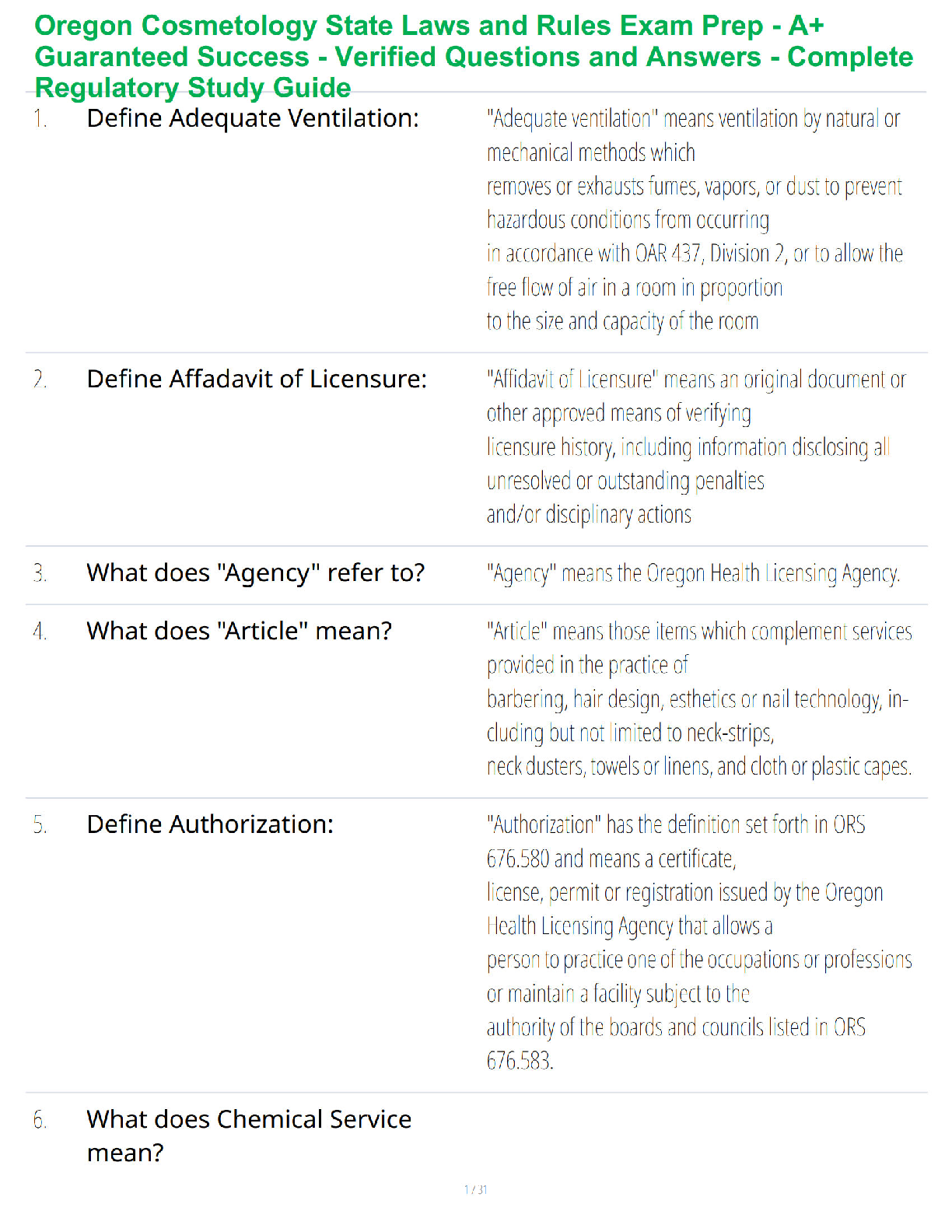
pathogenesis of chronic bronchitis which begins with some sort of exposure to
airborne irritants which activates bronchial smooth muscle constriction, mucus
secretion, and release of inflammatory mediators (histamine, prostaglandins,
leukotrienes, interleukins) from immune cells located in the lamina propria
These airborne irritants can include air pollution or industrial chemicals & fumes.
But the most common irritant is smoke from cigarettes and other tobacco products.
Keep in mind that all of these bronchial responses are, in fact, normal responses to
occasional inhalation of airborne irritants.
Smooth muscle constriction is important to limit passage of the irritant deeper into
the respiratory tract.
Secretion of mucus and release of inflammatory chemicals are also important to
help trap and defend against a potentially harmful substance.
The transition from a normal, protective respiratory response to a detrimental effect
occurs with ….
long-term exposure to airborne irritants which promotes
• smooth muscle hypertrophy à increased bronchoconstriction
• hypertrophy and hyperplasia of goblet cells à mucus hypersecretion
• epithelial cell metaplasia à non-ciliated squamous cells
• migration of more WBCs to site à inflammation & fibrosis in bronchial wall
• thickening and rigidity of bronchial basement membrane à narrowing of
bronchial passageways
the smooth muscle constriction, bronchial wall inflammation, and mucus plugs
lead to another issue: alveolar hyperinflation.
Because of the anatomical changes in the bronchioles associated with chronic
irritation ventilation, especially exhalation, is compromised.
Pressure differences during inhalation are high enough to force air into the alveoli.
However, during exhalation the narrowing and collapse of the air passageways
causes air to be trapped in the alveoli resulting in.
• alveolar hyperinflation à expanded thorax
• hypercapnia, (CO2 retention) and, respiratory acidosis
The high concentration of CO2 creates unfavorable conditions for gas exchange, so
there is
• decreased O2 exchange à ventilation/perfusion (V/Q) mismatch
Decreased perfusion of the pulmonary capillaries with oxygenated blood results in
• chronic pulmonary hypoxia à cyanosis
Poor ventilation, leading to decreased perfusion, causes Right to Left “shunting” to
occur. This is the phenomenon where deoxygenated blood passes from the RV to
lungs to the LV without adequate perfusion (gas exchange)
Similar to other obstructive pulmonary disorders, chronic bronchitis has both a
bronchoconstriction component and an inflammation component.
Pharmacotherapy includes:
• antitussives and expectorants – can be useful to help thin the secretions for
easier expulsion and to help control coughing episodes
• bronchodilators – fast- and long-acting agents are mainstays of chronic
bronchitis treatment
• systemic corticosteroids – particularly useful during an acute flareup/exacerbation.
• antibiotics – as needed for treatment of bacterial infections; critical to
prevent any excessive immune stimulation
Prophylactic immunizations (especially the pneumococcus vaccine and annual flu
vaccines) are important to reduce likelihood of exacerbations triggered by
respiratory infections.
Clients also benefit from working with respiratory and physiotherapists to learn
relatively simple physical measures that can help optimize quality of life for clients
with chronic bronchitis.
These physical measures include:
• chest physiotherapy using postural drainage (changes in body position) and
gravity to facilitate movement of mucus from the congested lower bronchial
airways to the trachea for easier expulsion AND
• relaxation and breathing techniques, including pursed lip breathing, similar
to how you would blow a bubble, to prolong the exhalation period
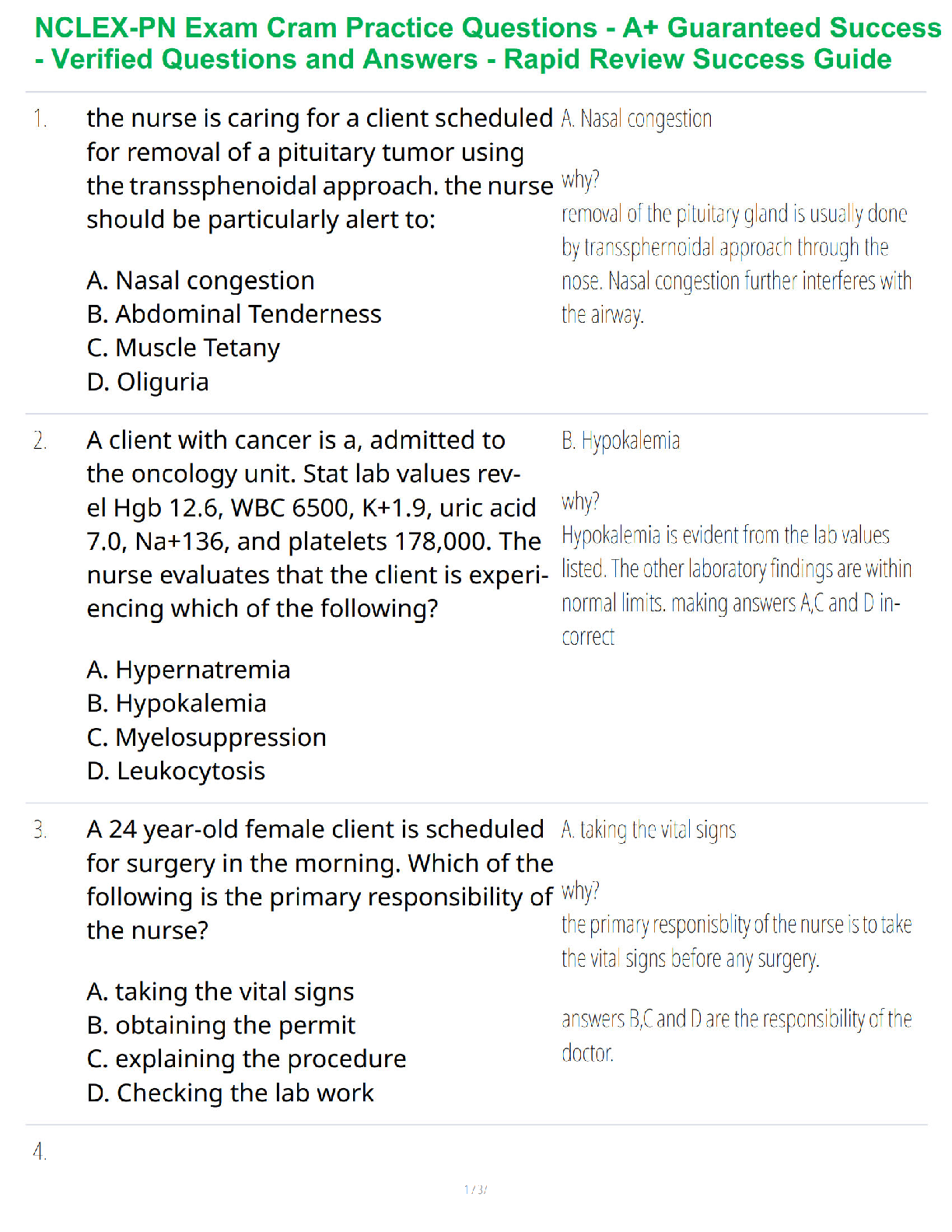
An anticholinergic agent is a substance that blocks the neurotransmitter
acetylcholine in the central and the peripheral nervous system. These agents inhibit
parasympathetic nerve impulses by selectively blocking the binding of the
neurotransmitter acetylcholine to its receptor in nerve cells. The nerve fibers of the
parasympathetic system are responsible for the involuntary movement of smooth
muscles present in the gastrointestinal tract, urinary tract, lungs, and many other
parts of the body. Anticholinergics are divided into three categories in accordance
with their specific targets in the central and peripheral nervous system:
antimuscarinic agents, ganglionic blockers, and neuromuscular blockers
[Show More]