NR509 Week 6 SOAP Note - NR 509
Document Content and Description Below
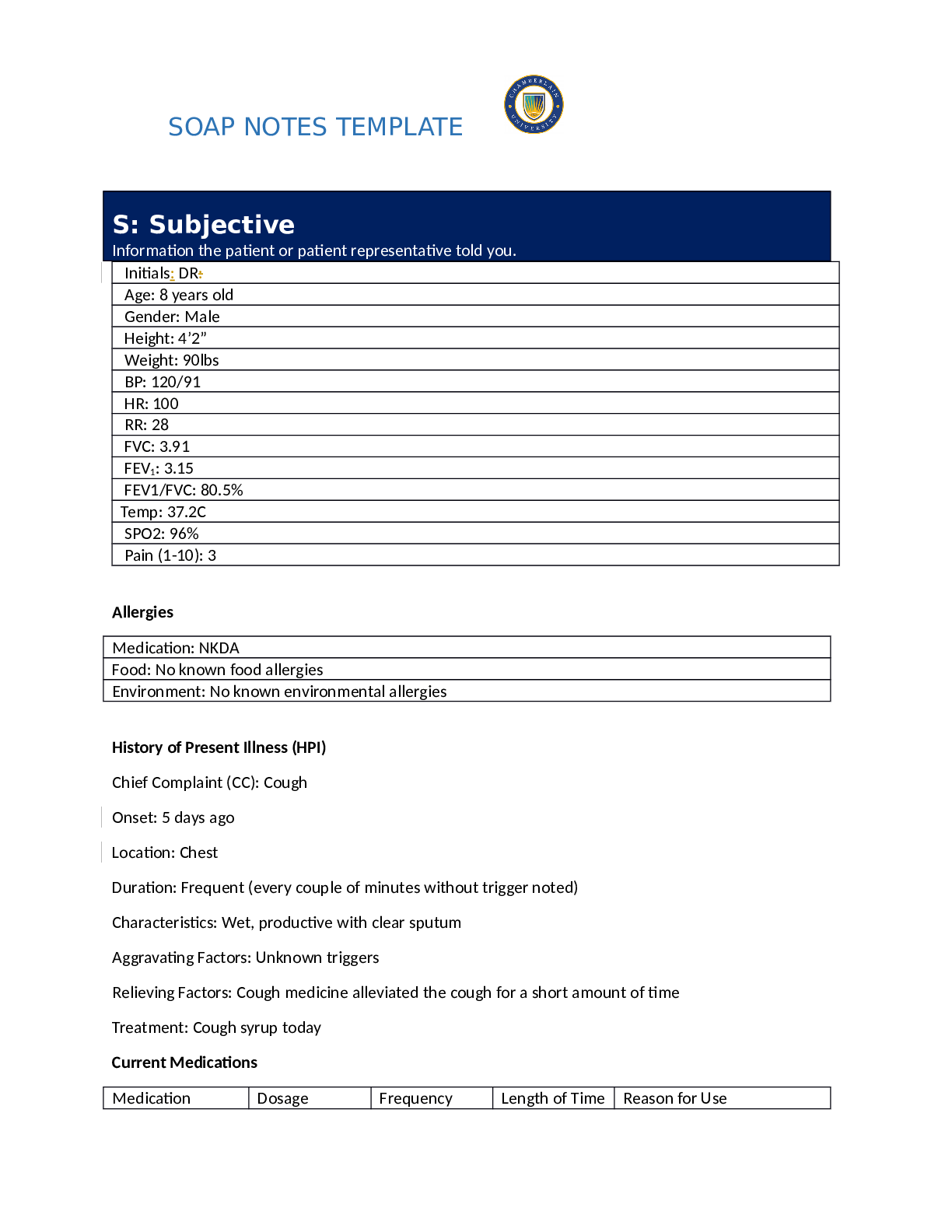
SOAP NOTES TEMPLATE S: Subjective Information the patient or patient representative told you. Initials: DR: Age: 8 years old Gender: Male Height: 4’2” Weight: 90lbs BP: 120/91 HR: ... 100 RR: 28 FVC: 3.91 FEV1: 3.15 FEV1/FVC: 80.5% Temp: 37.2C SPO2: 96% Pain (1-10): 3 Allergies Medication: NKDA Food: No known food allergies Environment: No known environmental allergies History of Present Illness (HPI) Chief Complaint (CC): Cough Onset: 5 days ago Location: Chest Duration: Frequent (every couple of minutes without trigger noted) Characteristics: Wet, productive with clear sputum Aggravating Factors: Unknown triggers Relieving Factors: Cough medicine alleviated the cough for a short amount of time Treatment: Cough syrup today [Show More]
Last updated: 3 years ago
Preview 1 out of 13 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 03, 2022
Number of pages
13
Written in
All
Additional information
This document has been written for:
Uploaded
Jun 03, 2022
Downloads
0
Views
109