Annual CE/ Medicare CE, Q&As-Confirming the consumer's Medicaid level and that the consumer is entitled to Medicare Part A and enrolled in Medicare Part B is a requirement of:
- Selling DSNPs
The consumer states the
...
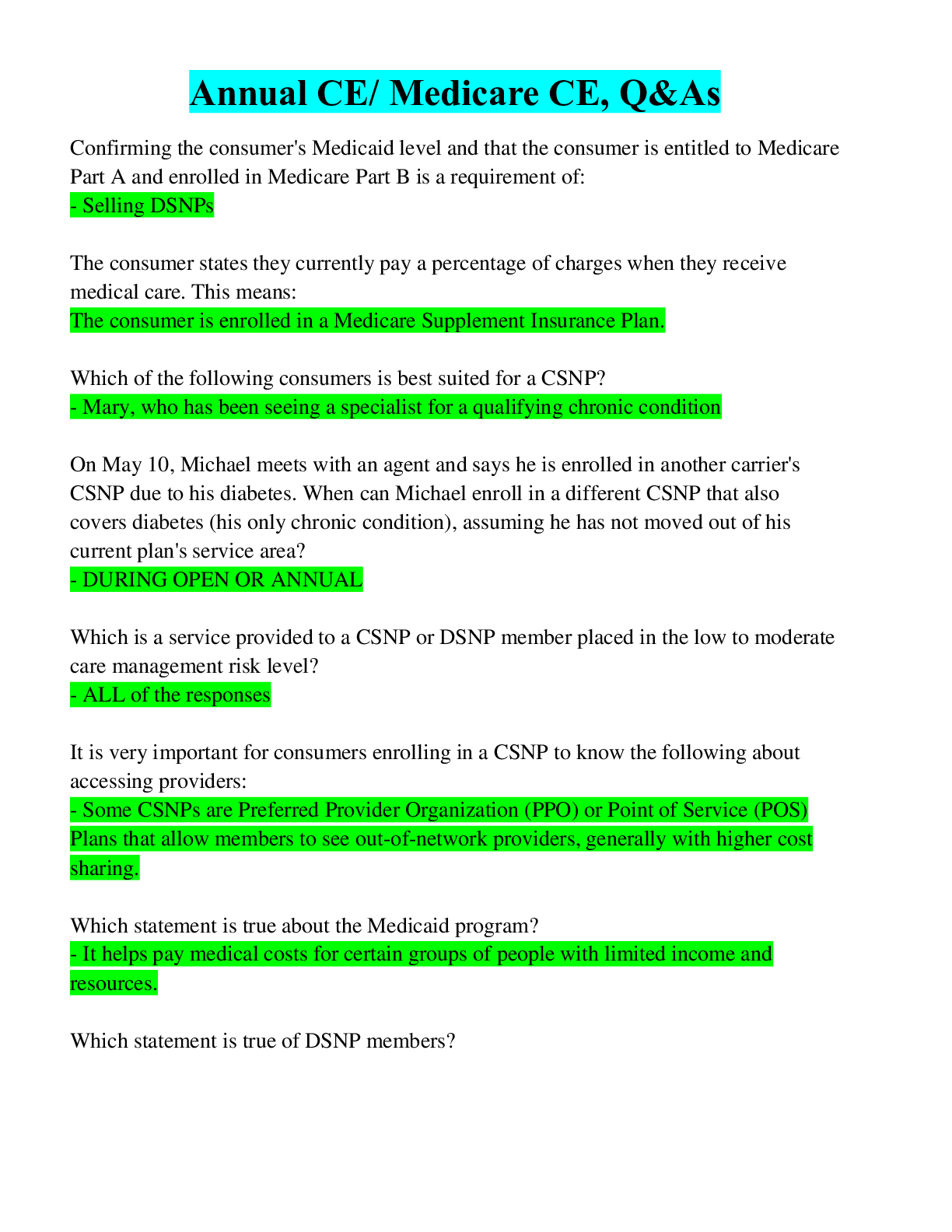
Annual CE/ Medicare CE, Q&As-Confirming the consumer's Medicaid level and that the consumer is entitled to Medicare Part A and enrolled in Medicare Part B is a requirement of:
- Selling DSNPs
The consumer states they currently pay a percentage of charges when they receive medical care. This means:
The consumer is enrolled in a Medicare Supplement Insurance Plan.
Which of the following consumers is best suited for a CSNP?
- Mary, who has been seeing a specialist for a qualifying chronic condition
On May 10, Michael meets with an agent and says he is enrolled in another carrier's CSNP due to his diabetes. When can Michael enroll in a different CSNP that also covers diabetes (his only chronic condition), assuming he has not moved out of his current plan's service area?
- DURING OPEN OR ANNUAL
Which is a service provided to a CSNP or DSNP member placed in the low to moderate care management risk level?
- ALL of the responses
It is very important for consumers enrolling in a CSNP to know the following about accessing providers:
- Some CSNPs are Preferred Provider Organization (PPO) or Point of Service (POS) Plans that allow members to see out-of-network providers, generally with higher cost sharing.
Which statement is true about the Medicaid program?
- It helps pay medical costs for certain groups of people with limited income and resources.
Which statement is true of DSNP members?
- Members who are QMB+ or are Full Dual-Eligible are not required to pay copayments for Medicare-covered services obtained from a DSNP in-network provider. Their provider should bill the state Medicaid program, as appropriate, for these costs.
[Show More]