Which of the following is considered the final determination of the issues involving settlement of an insurance claim? - Ans-Adjudication
A form that contains charges, DOS, CPT codes, ICD codes, fees and copayment inf
...
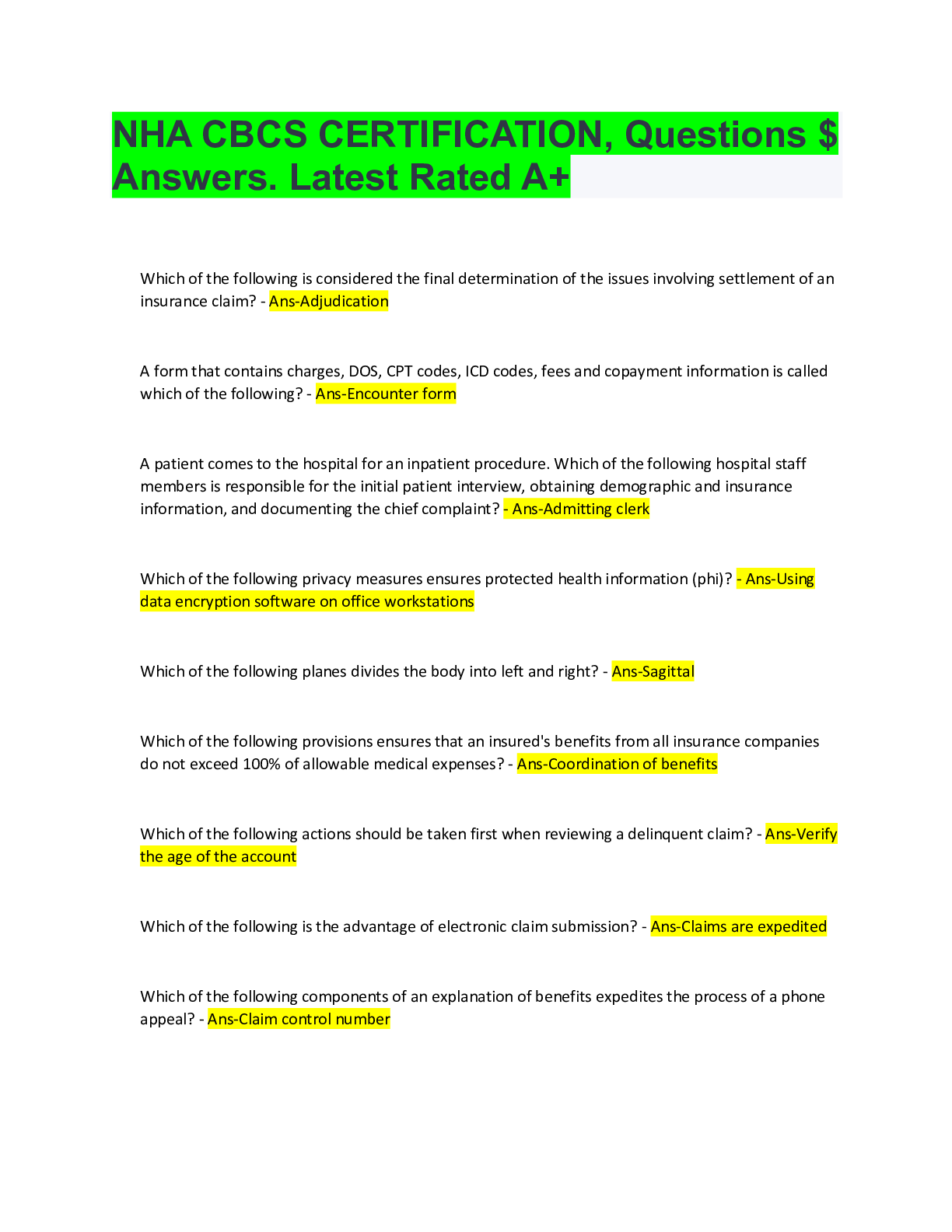
Which of the following is considered the final determination of the issues involving settlement of an insurance claim? - Ans-Adjudication
A form that contains charges, DOS, CPT codes, ICD codes, fees and copayment information is called which of the following? - Ans-Encounter form
A patient comes to the hospital for an inpatient procedure. Which of the following hospital staff members is responsible for the initial patient interview, obtaining demographic and insurance information, and documenting the chief complaint? - Ans-Admitting clerk
Which of the following privacy measures ensures protected health information (phi)? - Ans-Using data encryption software on office workstations
Which of the following planes divides the body into left and right? - Ans-Sagittal
Which of the following provisions ensures that an insured's benefits from all insurance companies do not exceed 100% of allowable medical expenses? - Ans-Coordination of benefits
Which of the following actions should be taken first when reviewing a delinquent claim? - Ans-Verify the age of the account
Which of the following is the advantage of electronic claim submission? - Ans-Claims are expedited
Which of the following components of an explanation of benefits expedites the process of a phone appeal? - Ans-Claim control number
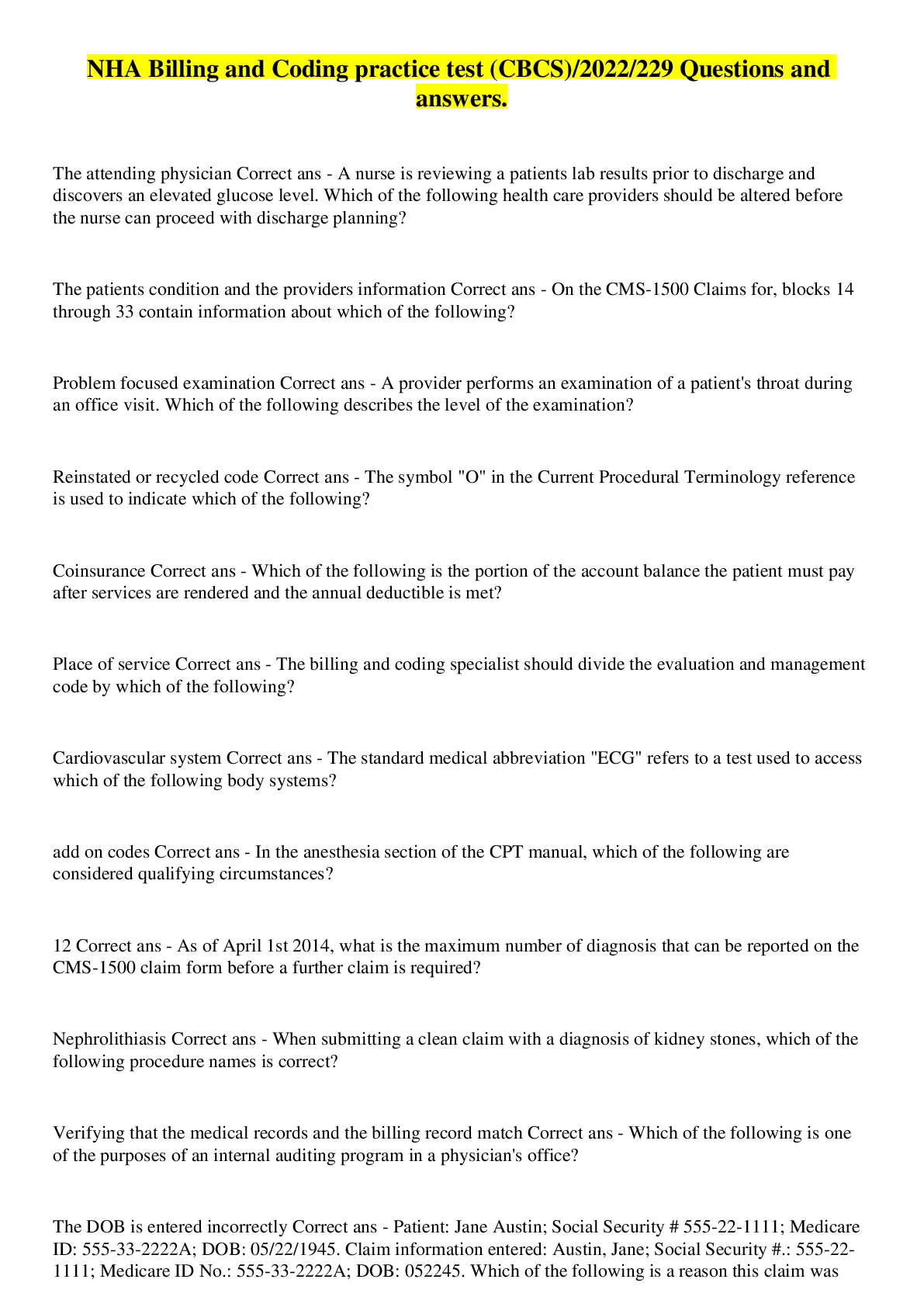
The standard medical abbreviation ECG refers to a test used to assess which of the following body systems? - Ans-Cardiovascular system
Which of the following actions by a billing and coding specialist would be considered fraud? - Ans-Billing for services not provided
The >< symbol is used to indicate a new and revised test other than which of the following? - Ans-Procedure descriptors
On the CMS-1500 claim form, blocks 14 through 33 contain information about which of the following? - Ans-The patient's condition and the provider's information
Which of the following includes procedures and best practices for correct coding? - Ans-Coding Compliance Plan
When completing a CMS-1500 paper claim form, which of the following is an acceptable action for the billing and coding specialist to take? - Ans-Use arial size 10 font
A participating blue cross/blue shield (BC/BS) provider receives an explanation of benefits for a patient account. The charged amount was $100. BC/BS allowed $80 and applied $40 to the patient's annual deductible. BC/BS paid the balance at 80%. How much should the patient expect to pay? - Ans-$48
Which of the following indicates a claim should be submitted on paper instead of electronically? - Ans-The claim requires an attachment
According to HIPAA standards, which of the following identifies the rendering provider on the CMS-1500 claim form in block 24j? - Ans-NPI
Which of the following blocks should the billing and coding specialist complete on the CMS-1500 claim form form for procedures, services or supplies (CPT/HCPCS)? - Ans-Block 24D
Which of the following terms describes when a plan pays 70% of the allowed amount and the patient pays 30%? - Ans-Coinsurance
A provider charged $500 to claim that had an allowable amount of $400. In which of the following columns should the billing and coding specialist apply the non-allowed charge? - Ans-Adjustment column of the credits
Which of the following is a HIPAA compliance guideline affecting electronic health records? - Ans-The electronic transmission and code set standards require every provider to use the healthcare transactions ,code sets and identifiers
Patient: Jane Austin; Social Security # 555-22-1111; Medicare ID: 555-33-2222A; DOB: 05/22/1945. Claim information entered: Austin, Jane; Social Security #.: 555-22-1111; Medicare ID No.: 555-33-2222A; DOB: 052245. Which of the following is a reason this claim was rejected? - Ans-The DOB is entered incorrectly
Why does correct claim processing rely on accurately completed encounter forms? - Ans-They streamline patient billing by summarizing the services rendered for a given date of service
A patient's health plan is referred to as the "payer of last resort." The patient is covered by which of the following health plans? - Ans-Medicaid
Which of the following color formats is acceptable on the CMS-1500 claim form? - Ans-Red
Which of the following is an example of a violation of an adult patient's confidentiality? - Ans-Patient information was disclosed to the patient's parents without consent.
In the anesthesia section of the CPT manual, which of the following are considered qualifying circumstances? - Ans-Add-on codes
Ambulatory surgery centers, home health care, and hospice organizations use the - Ans-UB-04 claim form
Which of the following is a private insurance carrier? - Ans-Blue Cross/ Blue Shield
Which of the following shows outstanding balances? - Ans-Aging report
Which of the following is one of the purposes of an internal auditing program in a physician's office? - Ans-Verifying that the medical records and the billing record match
The star symbol in the CPT code book is used to indicate which of the following? - Ans-Telemedicine
Medigap coverage is offered to Medicare beneficiaries by which of the following? - Ans-Private third party payers
A patient's portion of the bill should be discussed with the patient before a procedure is performed for which of the following reasons? - Ans-To ensure the patient understands his portion of the bill
The physician bills $500 to a patient. After submitting the claim to the insurance company, the claim is sent back with no payment. The patient still owes $500 for this year. This amount is called - Ans-Deductible
A patient who is an active member of the military recently returned from overseas and is in need of specialty care. The patient does not have anyone designated with power of attorney. Which of the following is considered a HIPAA violation? - Ans-The billing and coding specialist sends the patient's records to the patient's partner.
A patient is upset about a bill she received. Her insurance company denied the claim. Which of the following actions is an appropriate way to handle the situation? - Ans-Inform the patient of the reason of the denial
A patient presents to the provider with chest pain and SOB. After an unexpected ECG result, the provider calls a cardiologist and summarizes the patient's symptoms. What portion of HIPAA allows the provider to speak to the cardiologist prior to obtaining the patient's consent? - Ans-TITLE II
A physician ordered a comprehensive metabolic panel for a 70 year old patient who has Medicare as her primary insurance. Which of the following forms is required so the patient knows she may be responsible for payment? - Ans-Advanced Beneficiary Notice
Which of the following describes the reason for a claim rejection because of Medicare NCCI edits? - Ans-Improper code combinations
Which of the following is the purpose of running an aging report each month? - Ans-It indicates which claims are outstanding
Which of the following do physicians use to electronically submit claims? - Ans-Clearinghouses
Which of the following should the billing and coding specialist include in an authorization to release information? - Ans-The entity to whom the information is to be released
Which of the following information is required on a patient account record? - Ans-Name and address of guarantor
Which of the following forms should the billing and coding specialist transmit to the insurance carrier for reimbursement of inpatient hospital services? - Ans-UB-04
An insurance claims register (aged insurance report) facilitates which of the following? - Ans-Follow up of insurance claims by date
When posting payment accurately, which of the following items should the billing and coding specialist include? - Ans-Patient's responsibility
Which of the following should the billing and coding specialist complete to be reimbursed for the provider's services? - Ans-CMS-1500 claim form
As of April 1st 2014, what is the maximum number of diagnosis that can be reported on the CMS-1500 claim form before a further claim is required? - Ans-12
Which of the following describes an obstruction of the urethra? - Ans-Urethratresia
Which of the following options is considered proper supportive documentation for reporting CPT and ICD codes for surgical procedures? - Ans-Operative report
Which of the following describes a delinquent claim? - Ans-The claim is overdue for payment
All dependents 10 year of age or older are required to have which of the following for TRICARE? - Ans-Military identification
Which of the following types of claims is 120 days old? - Ans-Delinquent
HIPAA transaction standards apply to which of the following entities? - Ans-Health care clearinghouse
Which of the following actions should be taken when a claim is billed for a level four office visit and paid at a level three? - Ans-Submit an appeal to the carrier with supporting documentation
When submitting a clean claim with a diagnosis of kidney stones, which of the following procedure names is correct? - Ans-Nephrolithiasis
All e-mail correspondence to a third party payer containing patients' protected health information (PHI) should be - Ans-Encrypted
The billing and coding specialist should divide the evaluation and management code by which of the following? - Ans-Place of service
[Show More]