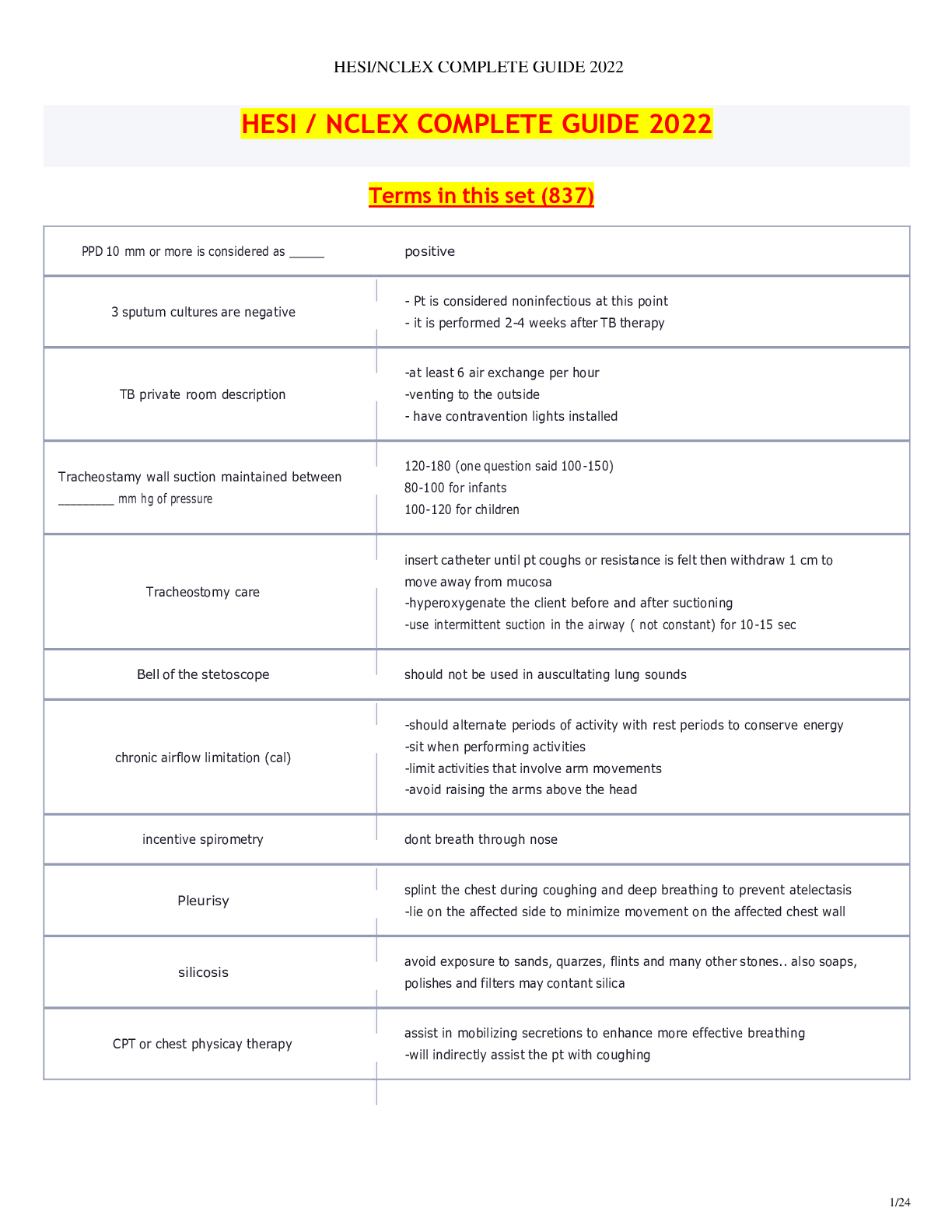
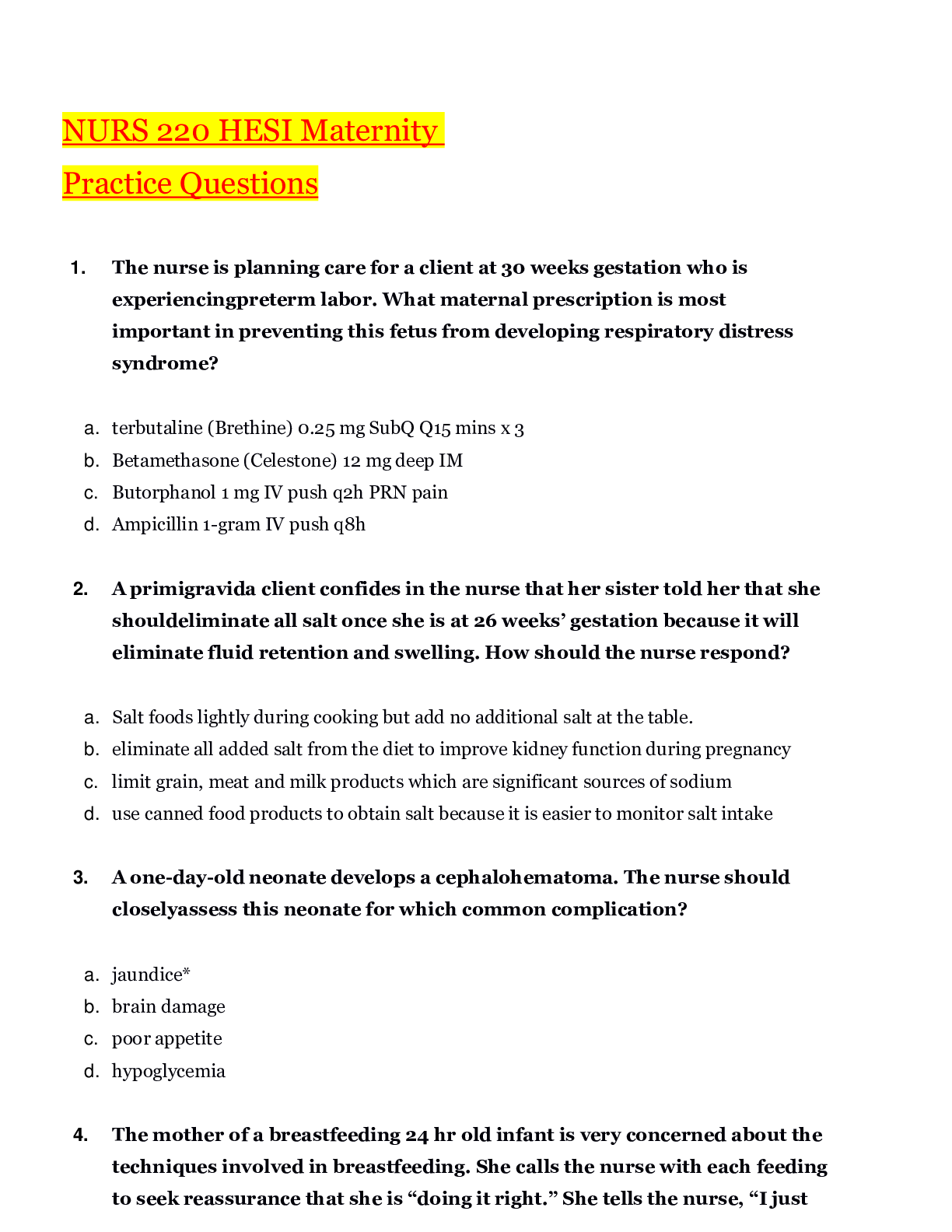
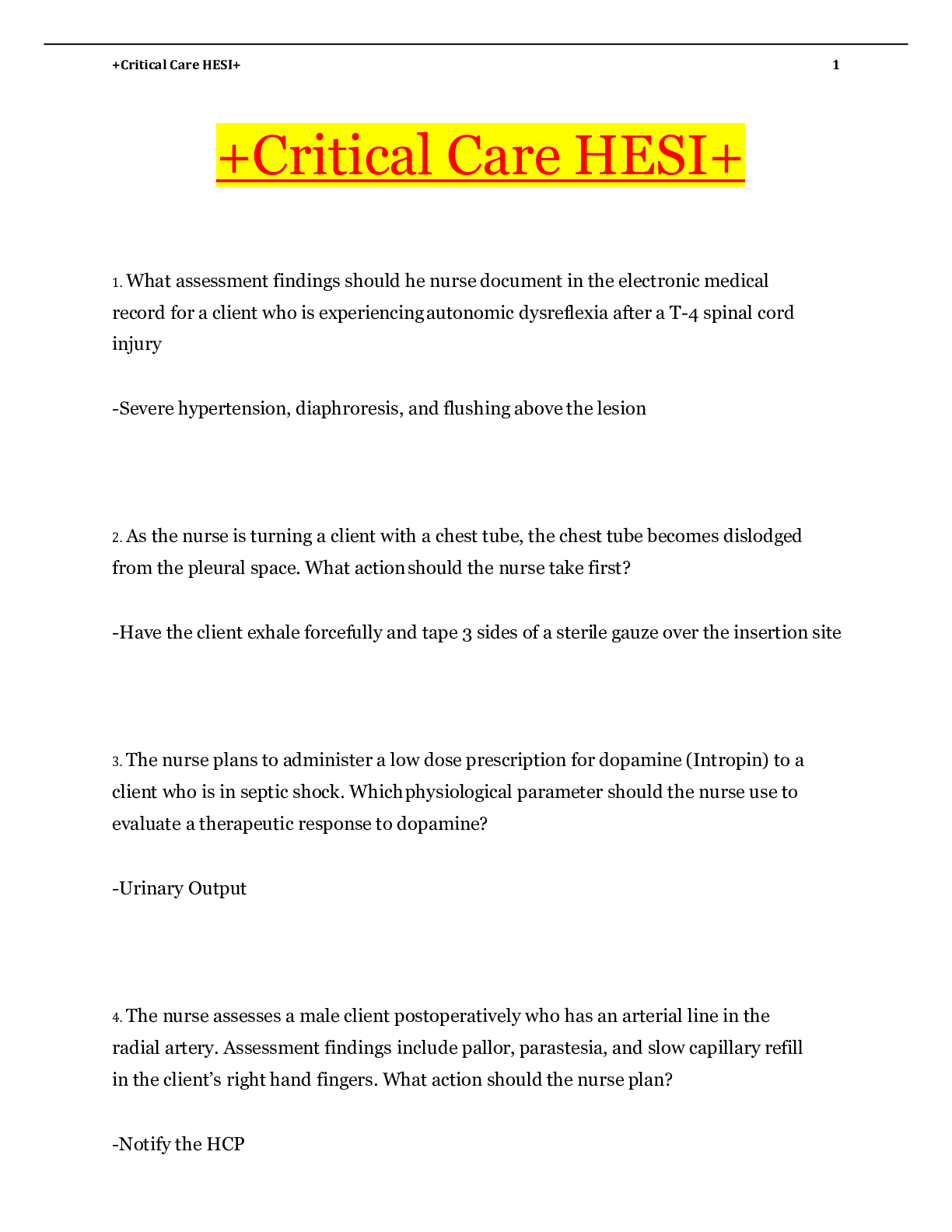
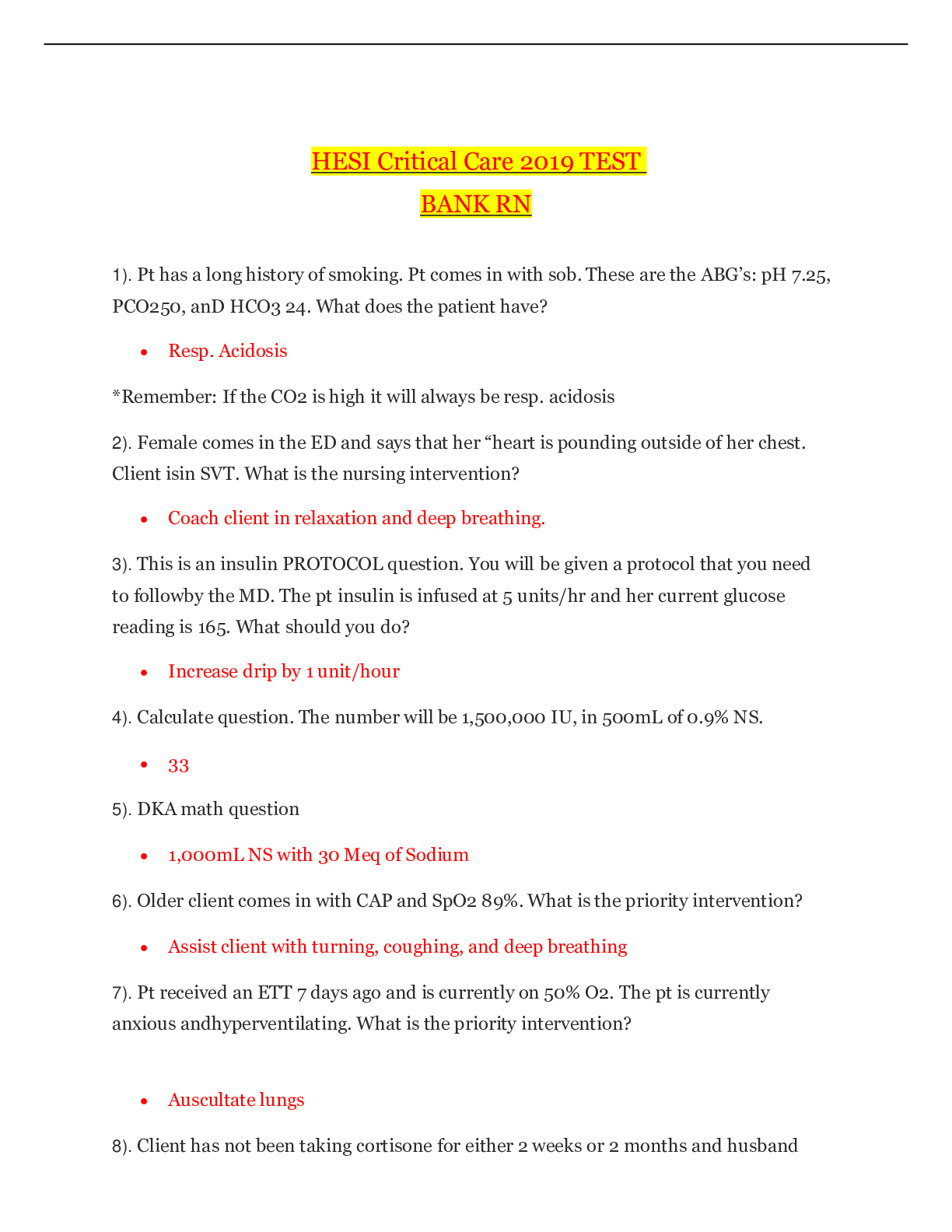
*NURSING > HESI > NURS 3410 HESI Exam 5 (2020 updated) – University of Arizona | NURS3410 HESI Exam 5 (2020 updated) (All)
NURS 3410 HESI Exam 5 (2020 updated) – University of Arizona | NURS3410 HESI Exam 5 (2020 updated)
Document Content and Description Below
NURS 3410 HESI Exam 5 (2020 updated) – University of Arizona Chapter 30 Endocrine Drugs Pituitary Drugs • Anterior pituitary drugs o cosyntropin o somatropin o octreotide • Po... sterior pituitary drugs – fyi… also makes oxytocin which can be used to induce labor o vasopressin o desmopressin Mechanism of Action • Differs depending on the drug o Either augments or antagonizes the natural effects of the pituitary hormones Anterior Pituitary Drug Profile Cosyntropin Indication-Used for diagnosis of adrenocortical insufficiency Stimulates release of cortisol from adrenal cortex- Hydrocortisone (Solu-Cortef) is the drug from of cortisol Anti-inflammatory effect- reduce leukocyte function and scare tissue formation Promotes renal retention of sodium which can result in edema and hypertension Once adrenal insufficiency is diagnosed, pt treated with adrenal steroids (fludrocortions, prednisone) Somatropin and Somatrem Forms: Typically, Subq (some) IM Indication-Recombinantly made growth hormone (GH) Stimulate anabolic (tissue building processes) Liver glycogenolysis Lipid mobilization from body fat Retention of sodium, potassium and phosphorus Stimulate skeletal growth in patients with deficient GH, such as hypopituitary dwarfism Also used for wasting associated with HIV Contraindications-Children with closed growth plates, patients with tumors, or acute illnesses Adverse Effects- HA, hyper/hypoglycemia, hypothyroidism, hypercalciuria, rash, urticarial, development of antibodies to GH, inflammation at injection site, flulike syndrome Assess, Implement, Edu • Obtain baseline thyroid, glucose and calcium levels • Pay close attention to growth, motor skills, height, and weight of peds pt. • Do not shake medication!! Octreotide Forms: IV, IM and Subq Indications- Antagonizes natural growth hormone by inhibiting release Carcinoid tumors secrete VIP (vasoactive intestinal polypeptide). VIP causes profuse, watery diarrhea. Octreotide reduces this severe diarrhea, flushing, and potentially life-threatening hypotension that may occur with a carcinoid crisis. - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -- lso cause: drowsiness, HA, vertigo, paresthesia, N/V/D, hepatitis, loss of taste, smoky urine, decreased OP, blood disorders, rash, pruritis, myalgia, arthralgia, increased BUN/Cr, enlarged thyroid, nephritis Assess, Implement, Edu Propylthiouracil (PTU) • Dose with meals to prevent stomach upset • Report any fever, sore throat, mouth ulcers, skin eruptions, bleeding or bruising immediately • Monitor CBC & LFT • Avoid iodized salt or seafood with iodine • Monitor for S/S of hypothyroidism • Never stop abruptly All Thyroid and Antithryoid Drugs Assess, Implement, Edu • Assess for drug allergies, contraindications, and potential drug interactions. • Obtain baseline vital signs and weight. • Cautious use is advised for those with cardiac disease or hypertension and for pregnant women. • During pregnancy, treatment for hypothyroidism should continue. • Fetal growth may be retarded if maternal hypothyroidism is untreated during pregnancy. o Adjust dosage every 4 weeks to keep TSH at the lower end of the normal range. • Teach patients to take thyroid drugs once daily in the morning on empty stomach 30 mins before breakfast to decrease the likelihood of insomnia if taken later in the day. • Teach patients to take the medications at the same time every day and not to switch brands without primary care provider approval. • Teach patients to report any unusual symptoms, chest pain, or heart palpitations. • Teach patients not to take over-the-counter medications without primary care provider approval. • Teach patients that therapeutic effects may take several weeks to occur. • Teach patients the importance of alerting health care providers of thyroid medication use. o May enhance activity of anticoagulants o Patients with diabetes may need increased dosages of hypoglycemic medications. o May decrease serum digoxin levels • Antithyroid medications o Better tolerated when given with food o Give at the same time each day to maintain consistent blood levels. o Never stop these medications abruptly. o Avoid eating foods high in iodine (seafood, sushi, anything soy, soy sauce, tofu, and iodized salt). • Monitor for therapeutic response. o Thyroid drugs: decreased symptoms of hypothyroidism, improved energy levels, improved mental and physical stamina o Antithyroid drugs: no evidence of hyperthyroidism • Monitor for adverse effects. o Thyroid drugs: cardiac dysrhythmia o Antithyroid drugs: leukopenia (manifested as fever, sore throat, lesions) Chapter 33 Adrenal Drugs Adrenal Gland • Adrenal cortex o Glucocorticoids o Mineralocorticoids (primarily aldosterone) • Adrenal medulla o Epinephrine o Norepinephrine • Each portion has different functions and secretes different hormones. • Feedback process of hormone regulation Adrenal Cortex Disorders • Oversecretion leads to Cushing’s syndrome. o Too much cortisol & aldosterone o Typical cause is the over use of exogenous steroids • Undersecretion leads to Addison’s disease. o Not enough cortisol & aldosterone o Many times autoimmune, can also be caused by excessive exogenous steroids o Can cause an Addison’s/Adrenal crisis which is life-threatening Corticosteroids • Can be either synthetic or natural • Many different drugs and forms • Glucocorticoids o Topical, systemic, inhaled, nasal • Mineralocorticoid o Systemic • Adrenal steroid inhibitors o Systemic Glucocorticoids adrenocorticotropic hormone betamethasone cortisone dexamethasone hydrocortisone methylprednisolone prednisolone triamcinolone Mineralocorticoids aldosterone desoxycorticosterone fludrocortisone Corticosteroids Drug Profile Most corticosteroids exert their effects by modifying enzyme activity. Glucocorticoids differ in their potency, duration of action, and the extent to which they cause salt and fluid retention. Glucocorticoids inhibit or help control inflammatory and immune responses. Indications- Adrenocortical deficiency Bacterial meningitis ,Cerebral edema Collagen diseases (e.g., systemic lupus erythematosus), Dermatologic diseases (e.g., exfoliative dermatitis, pemphigus) “itis”: Endocrine disorders (thyroiditis), Gastrointestinal (GI) diseases (e.g., ulcerative colitis, regional enteritis) Exacerbations of chronic respiratory illnesses such as asthma and chronic obstructive pulmonary disease Hematologic disorders (reduce bleeding tendencies) Organ transplantation (decrease immune response to prevent organ rejection) Leukemias and lymphomas (palliative management) Nephrotic syndrome (remission of proteinuria) Spinal cord injury Glucocorticoids Administration By inhalation for control of steroid-responsive bronchospastic states (not a rescue inhaler) Nasally for rhinitis and to prevent the recurrence of polyps after surgical removal Topically for inflammations of the eye, ear, and skin Oral (prednisone) Contraindications- Drug allergies, Serious infections, including septicemia, systemic fungal infections, and varicella However, in the presence of tuberculous meningitis, glucocorticoids may be used to prevent inflammatory central nervous system (CNS) damage. Cautious use in :Cataracts, glaucoma, PUD, Mental health disorders, DM* (need to increase DM meds), Gastritis, reflux, PUD, Cardiac, renal, liver impairment Adverse Effects- Potent effects on all body systems, wide variety Cardiovascular: heart failure, cardiac edema, hypertension—all caused by electrolyte imbalances (hypokalemia, hypernatremia) CNS: convulsions, headache, vertigo, mood swings, nervousness, insomnia Endocrine: growth suppression, Cushing’s syndrome, menstrual irregularities, carbohydrate intolerance, hyperglycemia, hypothalamic–pituitary–adrenal axis suppression GI: peptic ulcers, pancreatitis, ulcerative esophagitis, abdominal distension Integumentary: fragile skin, petechiae, ecchymosis, facial erythema, poor wound healing, hirsutism, urticaria Musculoskeletal: muscle weakness, loss of muscle mass, osteoporosis Ocular: increased intraocular pressure, glaucoma, cataracts Other: weight gain Interactions- Non–potassium-sparing diuretics (e.g., thiazides, loop diuretics) can lead to severe hypocalcemia and hypokalemia. Aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), and other ulcerogenic drugs produces additive GI effects and an increased chance of gastric ulcer development. Anticholinesterase drugs produce weakness in patients with myasthenia gravis. Immunizing biologics inhibit the immune response to the biologic. Antidiabetic drugs may reduce the hypoglycemic effects of the latter and result in elevated blood glucose levels. Prednisone Most commonly used oral glucocorticoid for anti-inflammatory or immunosuppressant purposes Intermediate acting Also used to treat exacerbations of chronic respiratory illnesses Inadequate for the management of adrenocortical insufficiency (Addison’s disease) Lacks mineralocorticoid properties Prednisolone liquid form Methylprednisolone (Solu-Medrol) Most commonly used injectable glucocorticoid drug Primary use: antiinflammatory or immunosuppressant drug Usually administered intravenously Available in a long-acting (depot) formulation Most injectable formulations contain a preservative (benzyl alcohol) that cannot be given to children younger than 28 days of age. All Adrenal Drugs Assess, Implement, Edu • Perform a physical assessment to determine baseline weight, height, intake and output status, vital signs (especially blood pressure), hydration status, and immune status. • Obtain baseline laboratory studies. • Assess for edema and electrolyte imbalances. • Assess for contraindications to adrenal drugs, especially the presence of peptic ulcer disease. • Assess for drug allergies and potential drug interactions (prescription and over-the-counter drugs). • Be aware that these drugs may alter serum glucose and electrolyte levels. • Systemic forms may be given by oral, intramuscular, intravenous, or rectal routes (not subcutaneous). • Prepare and administer according to manufacturer’s directions. o Oral forms should be given with food or milk to minimize GI upset. o For topical applications, follow instructions about use and type of dressing, if any, to apply. o Clear nasal passages before giving a nasal corticosteroid. o After using an orally inhaled corticosteroid, instruct patients to rinse their mouths to prevent possible oral fungal infections. • Teach patients taking corticosteroids to avoid contact with people with infections and to report any fever, increased weakness, lethargy, or sore throat. • Patients should be taught to take all adrenal medications at the same time every day, usually in the morning, with meals or food. • Patients should not take adrenal medications with alcohol, aspirin, or NSAIDs. • Sudden discontinuation of these drugs can precipitate an adrenal crisis caused by a sudden drop in serum levels of cortisone. • Doses are usually tapered before the drug is discontinued. • Monitor for therapeutic responses. • Monitor for adverse effects. Chapter 32 Antidiabetic Drugs Diabetes Mellitus • Diabetes mellitus (DM) actually is not a single disease but a group of progressive diseases. It is often regarded as a syndrome rather than a disease. • Two types o Type 1 o Type 2- most common 90%, caused by insulin deficiency and insulin resistance • Gestational- hyperglycemia that develops during pregnancy S/S: Elevated fasting blood glucose (higher than 126 mg/dL) or a hemoglobin A1C (HbA1C) level greater than or equal to 6.5% Polyuria, Polydipsia, Polyphagia, Glycosuria, Unexplained weight loss, Fatigue, Blurred vision Several comorbid conditions: Obesity Coronary heart disease Dyslipidemia Hypertension Microalbuminemia (protein in the urine) Increased risk for thrombotic (blood clotting) events These comorbidities are collectively referred to as metabolic syndrome, insulin-resistance syndrome, or syndrome X. Major Long-Term Complications of Both Types of Diabetes • Macrovascular (atherosclerotic plaque) o Coronary arteries o Cerebral arteries o Peripheral vessels • Microvascular (capillary damage) o Retinopathy o Neuropathy o Nephropathy Glycemic Goal of Treatment • HbA1C of less than 7% • Fasting blood glucose goal for diabetic patients of 70 to 130 mg/dL • - - - - - - - - - - - - - - - - - - - - - - -- - - - - - - - - -- rition or enteral tube feedings • SQ insulin is ordered in an amount that increases as the blood glucose increases • Disadvantage delays insulin administration until hyperglycemia occurs; results in large swings in glucose control Basal-Bolus Insulin Dosing • Preferred method of treatment for hospitalized patients with DM • Mimics a healthy pancreas by delivering basal insulin constantly as a basal and then as needed as a bolus • Basal insulin is a long-acting insulin (insulin glargine) • Bolus insulin (insulin lispro or insulin aspart) Oral Antidiabetic Drugs • Used for type 2 DM • Effective treatment involves several elements o Careful monitoring of blood glucose levels o Therapy with one or more drugs o Treatment of associated comorbid conditions such as high cholesterol and high blood pressure • 2013 American Diabetes Association guidelines o New-onset type 2 DM treatment 1st used - Lifestyle interventions 2nd used- Oral Biguanide drug metformin 3rd used -If lifestyle modifications and the maximum tolerated metformin dose do not achieve the recommended HbA1C goals after 3 to 6 months, additional treatment should be given with a second oral agent, GLP-1 agonist (liraglutide, exenatide, abliglutide) or insulin. Biguanides Insulin Drug Profile Metformin (Glucophage) Indication-First-line drug and is the most commonly used oral drug for the treatment of type 2 DM Decreases glucose production by liver Decreases intestinal absorption of glucose Improves insulin sensitivity Adverse effects-Abdominal bloating, nausea, cramping, a feeling of fullness, and diarrhea Metallic taste, hypoglycemia, and a reduction in vitamin B12 levels after long-term use Lactic acidosis is an extremely rare complication. Contraindications- Renal disease or dysfunction, Alcoholism, metabolic acidosis, hepatic disease, heart failure, risk for lactic acidosis Interactions- Other hypoglycemic ,Cimetidine, Diuretics, steroids, & CONTRAST MEDIA (AKI & lactic acidosis) D/C on day of test and 48 h post procedure Sulfonylurea Oldest group Second generation: glimepiride (Amaryl), glipizide (Glucotrol), glyburide (DiaBeta) Stimulate an increase in the release of insulin Decrease secretion of glucagon Indications- Used in conjunction with other agents Should not be given concurrently with insulin (pancreas no longer working) Contraindications- Hypoglycemia, NPO, ? Cross allergy of sulfa Adverse effects: hypoglycemia, weight gain, skin rash, nausea, epigastric fullness, and heartburn Interactions- Beta blockers (remember hypoglycemia?), Cimetidine, erythromycin, flonazole, sulfonamides, DPP4 inhibitors, garlic, ginger, ginseng, carbamazepine, phenobarbital, phenytoin, rifampin Glinides Repaglinide (Prandin), nateglinide (Starlix) Indication: type 2 DM Similar mech of action to sulfonylurea but shorter duration must be taken with every meal Thiazolidinediones (Glitazones) Pioglitazone (Actos) Rosiglitazone (Avandia) Only available through specialized manufacturer programs Insulin-sensitizing drugs Enhance sensitivity of insulin receptors Stimulate peripheral uptake of glucose Affect gene regulation ( slow onset and max activity might not be seen for several months) Contraindicated in advanced HF Adv effects- HF, peripheral edema and weight gain, reduced bone mineral density Alpha-glucosidase inhibitors Acarbose (Precose), miglitol (Glyset) Inhibit enazyme that is in small intestine responsible for glucose metabolism which then delays glucose absorption MUST be taken with food Contraindications- Inflammatory bowel disease, malabsorption syndromes or intestinal obstructions Adverse effects- High incidence of flatulence, diarrhea, abdominal pain, May elevate LFT Rare to cause hypoglycemia (but must be tx with simple sugars) Dipeptidyl peptidase-IV (DPP-IV) inhibitors (gliptins) sitagliptin (Januvia) saxagliptin (Onglyza) linagliptin (Tradjenta) alogliptin (Nesina) Delay breakdown of incretin hormones by inhibiting enzyme Contraindication: allergy Adverse effects: upper respiratory infections, headache, diarrhea Interactions: depends on agent Sodium Glucose Cotransporter (SGLT2) Inhibitors • Inhibition of SGLT2 leads to a decrease in blood glucose caused by an increase in renal glucose excretion. • SGLT2 inhibitors: new class of oral drugs for the treatment of type 2 DM • Canaglifozin (Invokana), dapaglifozin (Farxiga), and empagliflozin (Jardiance) • Mechanism of Action: work independently of insulin to prevent glucose reabsorption from the glomerular filtrate, resulting in a reduced renal threshold for glucose and glycosuria • Other effects: may increase insulin sensitivity and glucose uptake in the muscle cells and decrease gluconeogenesis • Results: improved glycemic control, weight loss, and a low risk of hypoglycemia Injectable Amylin Agonist Pramlintide (Symlin) Form- SQ injection Slows gastric emptying Suppresses glucagon secretion, reducing hepatic glucose output Centrally modulates appetite and satiety Used when other drugs have not achieved adequate glucose control Adverse effects: Nausea, vomiting, anorexia, headache Injectable Incretin Mimetics Exenatide (Byetta): injection pen device Liraglutide (Victoza) Enhances glucose-driven insulin secretion from beta cells of the pancreas Only used for type 2 DM Adverse effects- Nausea, vomiting, and diarrhea; Rare cases of hemorrhagic or necrotizing pancreatitis Weight loss Hypoglycemia • Abnormally low blood glucose level (below 50 mg/dL) • Mild cases can be treated with diet—higher intake of protein and lower intake of carbohydrates—to prevent rebound postprandial hypoglycemia • Early o Confusion, irritability, tremor, sweating • Late o Hypothermia, seizures o Coma and death will occur if not treated Glucose-Elevating Drugs • Oral forms of concentrated glucose o Buccal tablets, semisolid gel • IV 50% dextrose in water (D50W) • Glucagon subcutaneous injections o Can cause vomiting so roll on side first o Good to give if patient unconscious and can’t establish IV access All Anti-Diabetic Drugs Assess, Implement, Edu • Before giving drugs that alter glucose levels, obtain and document: o A thorough history, Vital signs, HbA1C level o Potential complications and drug interactions o Risk for hypoglycemia Blood glucose level Assess the patient’s ability to consume food. Assess for nausea or vomiting. a patient is NPO for a test or procedure, consult the primary care provider to clarify orders for antidiabetic drug therapy o Keep in mind that overall concerns for any patient with DM increase when the patient: o Is under stress o Has an infection o Has an illness or trauma o Is pregnant or lactating • Thorough patient education is essential regarding: o Disease process o Diet and exercise recommendations o Self-administration of insulin or oral drugs o Potential complications • When insulin is ordered, ensure: o Correct route o Correct type of insulin o Timing of the dose o Correct dosage Insulin order and prepared dosages are second checked with another nurse. • Insulin o Check blood glucose level before giving insulin. o Roll vials between hands instead of shaking them to mix suspensions. o Ensure correct storage of insulin vials. o Only use insulin syringes, calibrated in units, to measure and give insulin. o Ensure correct timing of insulin dose with meals. o Once opened, keep vial at room temperature o Change vials every month or per policy • When drawing up two types of insulin in one syringe, always withdraw the regular or rapid-acting insulin first. o Provide thorough patient education regarding self-administration of insulin injections, including timing of doses, monitoring blood glucose levels, and injection site rotations. • Oral antidiabetic drugs o Always check blood glucose levels before giving o Usually given 30 minutes before meals o Alpha-glucosidase inhibitors are given with the first bite of each main meal. o Metformin is taken with meals to reduce GI effects. o Metformin will need to be discontinued if the patient is to undergo studies with contrast dye because of possible renal effects; check with the prescriber. • Assess for signs of hypoglycemia. • If hypoglycemia occurs: o Administer oral form of glucose if the patient is conscious. o Give the patient glucose tablets or gel, corn syrup, honey, fruit juice, or non-diet soft drink or have the patient eat a small snack, such as crackers or a half sandwich. o Deliver D50W or glucagon IV if the patient is unconscious. o Monitor blood glucose levels. • Monitor for therapeutic response: o Decrease in blood glucose levels to the level prescribed by physician o Measure HbA1C to monitor long-term compliance with diet and drug therapy. o Monitor for hypoglycemia and hyperglycemia. Chapter 11 General and Local Anesthetics Drugs Overview • Anesthetics: Drugs that reduce or eliminate pain by depressing nerve function in the central nervous system (CNS) and peripheral nervous system • Anesthesia: A state of reduced neurologic function o General: complete loss of consciousness and body reflexes o Local: no paralysis of respiratory function. Anesthetized nerves eliminates pain in tissues supplied by those nerves o Balanced anesthesia: use of general anesthetics and adjuncts to decrease amount of both agents needed and maintain a more balanced controlled state General Anesthesia • Drugs that induce a state in which the CNS is altered to produce varying degrees of: o Pain relief o Depression of consciousness o Skeletal muscle relaxation o Reflex reduction • Inhalational anesthetics o Volatile liquids or gases that are vaporized in oxygen and inhaled • Parenteral anesthetics o Administered intravenously • Adjunct anesthetics o Drug that enhances clinical therapy when used simultaneously with another drug Mech of Act- Overton-Meyer theory - For all anesthetics, potency varies directly with lipid solubility. Fat-soluble drugs are stronger anesthetics than water-soluble drugs. Nerve cell membranes have high lipid content, as does the blood–brain barrier. Lipid-soluble anesthetic drugs can therefore easily cross the blood–brain barrier to concentrate in nerve cell membranes. Reactions on the Body Systems - Depresses airway protective mechanisms, airway irritation, possible laryngospasm Hypotension, tachycardia, bradycardia with vagal response, Increased ICP, reduced hepatic blood flow and clearance, Decreased GFR, Relaxation of skeletal muscle, CNS depression blurred vision, nystagmus Older adults have more adversely affected r/t decreased liver function, comorbidities and polypharmacy Adverse Effects- Vary, hypotension, Post- op N/V, Substance abuse predisposes to anesthetic induced complication, Malignant hyperthermia (uncommon but fatal) Malignant Hyperthermia • Occurs during or after volatile inhaled general anesthesia or use of the neuromuscular blocking drug (NMBD) succinylcholine • Sudden elevation in body temperature (greater than 104° F) • S/S- Tachypnea, tachycardia, muscle rigidity • Life-threatening emergency • Treated with cardiorespiratory supportive care and dantrolene (skeletal muscle relaxant) – Children, adolescents and individuals with muscular or skeletal abnormalities at higher risk Toxicity and Management of overdose- In large doses, anesthetics are potentially life threatening. Cardiac and respiratory arrest ultimate causes of death in an overdose. Administered in a controlled environment Interactions- Antihypertensives: increased hypotensive effects, Beta blockers: increased myocardial depression General Anesthesia Drug Profile Dexmedetomidine (Precedex) Alpha-2 adrenergic receptor agonist Dose-dependent sedation, decreased anxiety, and analgesia without respiratory depression Indications- procedural sedation, surgeries of short duration. Short half-life, and the patient awakens quickly upon withdrawal of the drug. Sedation of mechanically ventilated patients in the intensive care unit (ICU) Use for only 24 hours, but also safe and effective for longer durations Adverse Effects- Hypotension, bradycardia, transient hypertension, nausea Ketamine Indications-Intravenous administration use for both general anesthesia and moderate sedation Rapid onset of action Low incidence of reduction of cardiovascular, respiratory, and bowel function Has bronchodilating properties so great for asthmatic anesthesia Adverse effects- disturbing psychomimetic effects, including hallucinations Reduced if given concurrently with benzo Propofol (Diprivan) Parenteral (IV) general anesthetic Indication- Used for the induction and maintenance of general anesthesia Sedation for mechanical ventilation in ICU settings Lower doses: sedative-hypnotic for moderate sedation Monitor triglycerides if administered with total parenteral nutrition Nitrous Oxide “Laughing gas” Only inhaled gas currently used as a general anesthetic Weakest of the general anesthetic drugs Indications- Used primarily for dental procedures or as a supplement to other, more potent anesthetics Primarily for its analgesic properties High concentrations can increase risk of post op N/V Sevoflurane (Ultane) Fluorinated ether Indications- Widely used, Especially useful in outpatient surgery settings Rapid onset and rapid elimination Nonirritating to the airway Greatly facilitates induction of an unconscious state, especially in pediatric patients Moderate Sedation • Also called conscious sedation and procedural sedation • Does not cause complete loss of consciousness and does not normally cause respiratory arrest. • Combination of an IV benzodiazepine (e.g., midazolam) or propofol and an opiate analgesic (e.g., fentanyl or morphine) o Concurrent opioid reduces benzo dose by 30-50% o If patient regularly consumes ETOH, benzo dose might need to be increased • Anxiety and sensitivity to pain are reduced, and the patient cannot recall the procedure. o Always behave and speak as though patient was totally awake • Preserves the patient’s ability to maintain own airway and to respond to verbal commands • Used for diagnostic procedures and minor surgical procedures that do not require deep anesthesia • Rapid recovery time and greater safety profile than general anesthesia • HCP need ACLS certification, one to one care, someone who can intubate must be present Local Anesthetics “-caine” • Also called regional anesthetics • Used to render a specific portion of the body insensitive to pain • Interfere with nerve impulse transmission to specific areas of the body • Work on peripheral nerves • Do not cause loss of consciousness Topical ■ Applied directly to skin or mucous membranes ■ Creams, solutions, ointments, gels, ophthalmic drops, powders, suppositories Parenteral ■ Injected intravenously or into the CNS by various spinal injection techniques Spinal or intraspinal ■ Intrathecal ■ Epidural • Infiltration (local- multiple, small amount in the tissue) or Nerve block (deep injections into areas close to the major nerve trucks or ganglia) • Peripheral nerve catheter attached to a pump containing the local anesthetic: Pain Buster and On-Q pump Types: Lidocaine, bupivacaine, chlorprocaine, mepivacaine, prilocaine, procaine, tetracaine, ropivacaine Mech of Act- First, autonomic activity is lost. Then pain and other sensory functions are lost. Last, motor activity is lost. As local drugs wear off, recovery occurs in reverse order (motor, sensory, then autonomic activity are restored). Indications- Local anesthetics are used for: Surgical, dental, and diagnostic procedures Treatment of certain types of chronic pain Spinal anesthesia: to control pain during surgical procedures and childbirth • Local anesthetics are given by: Infiltration anesthesia Nerve block anesthesia • Infiltration anesthesia Minor surgical and dental procedures Injection of the anesthetic solution intradermally, subcutaneously, submucosally, or intramuscularly across the path of nerves supplying target area May be given in a circular pattern around operative area • Infiltration anesthesia and epinephrine (vasoconstrictor) Some local anesthetics used for infiltration or nerve block are combined with vasoconstrictors To prevent systemic absorption of anesthetic To help confine local anesthetic to injected area To reduce local blood loss during procedure • Nerve block anesthesia Used for surgical, dental, and diagnostic procedures Also used for therapeutic management of pain The anesthetic drug is injected directly into or around the nerve trunks or nerve ganglia that supply the area to be numbed. Adverse Effects- Usually limited • Adverse effects result if: o Inadvertent intravascular injection o Excessive dose or rate of injection o Slow metabolic breakdown o Injection into highly vascular tissue • Spinal anesthesia can cause “Spinal headache” 70% of patients who either experience inadvertent dural puncture during epidural anesthesia or undergo intrathecal anesthesia. Usually self-limiting Treatment: bed rest, analgesics [APA(Tylenol)], caffeine, blood patch Neuromuscular Blocking Drugs (NMBDs) • Prevent nerve transmission in skeletal and smooth muscle, resulting in muscle paralysis • Also paralyze the skeletal muscles required for breathing: the intercostal muscles and the diaphragm- pt. need to be on a ventilator • Used with anesthetics during surgery • When used during surgery, artificial mechanical ventilation is required. o These drugs paralyze respiratory and skeletal muscles. o The patient cannot breathe on his or her own. o They do not cause sedation or pain relief. o The patient may be paralyzed yet conscious. Mech of Act- classified into two groups • Depolarizing drugs o Bind to acetylcholine receptors (agonists)- think about malignant hyperthermia o 2 phases: muscle twitching and then paralysis o Succinylcholine • Nondepolarizing drugs (antagonists) o Block acetylcholine receptors o Short acting o Intermediate acting o Long acting Indications- Main use: facilitating controlled ventilation during surgical procedures Endotracheal intubation (short-acting) To reduce muscle contraction in an area that needs surgery Diagnostic drugs for myasthenia gravis Contraindicated- Hx of malignant hyperthermia, Penetrating eye injuries & narrow angle glaucoma, Burns, crush trauma, CVA Adverse effects- Muscle spasms that can damage muscles, causing hyperkalemia, Possible release of histamine causing bronchospasm, hypotension, excessive bronchia land salivary secretion Interactions- Aminoglycosides and tetracyclines, CCB, Many others Toxicity and management of overdose- Respiratory support Antidotes for nondepolarizing NMBDs anticholinesterase drugs such as neostigmine, pyridostigmine, and edrophonium No antidote for succinlycholine NMBDs Drug Profile Succinylcholine Works similarly to neurotransmitter acetylcholine (ACh), causing depolarization Metabolism is slower than ACh, so as long as succinylcholine is present, repolarization cannot occur. Result: flaccid muscle paralysis Quick onset, typically used for rapid endotracheal intubation Can cause muscle fasciculations and malignant hyperthermia Rocuronium Non-depolarizing Rapid to intermediate acting Adjunct to general anesthesia Can also be used to reduce muscle contraction and facilitate diagnostic procedures All Anesthetics Assess, Implement, Edu. • Always assess past history of surgeries and response to anesthesia. • Assess past history, allergies, and medications. • Assess use of alcohol, illicit drugs, and opioids • Assessment is vital during preoperative, intraoperative, and postoperative phases o Vital signs o Baseline lab work, ECG o Oxygen saturation o ABCs (airway, breathing, circulation) o Monitor all body systems • Each perioperative phase has its own complex and very specific nursing actions. • Provide preoperative teaching about the surgical procedure and anesth • Perform close and frequent observation of the patient and all body systems. • During a procedure, monitor vital signs and ABCs. • Watch for sudden elevations in body temperature, which may indicate malignant hyperthermia • During recovery, monitor for cardiovascular depression, respiratory depression, and complications of anesthesia. • Implement safety measures during recovery, especially if motor or sensory loss occurs because of local anesthesia. • Reorient patient to his or her surroundings. • Teach the patient about postoperative turning, coughing, and deep breathing. Chapter 45 & 46 Chemotherapeutic Cancer Overview • Group of diseases characterized by cellular transformation, uncontrolled cellular growth, possible invasion into surrounding tissue and metastasis to other tissues or organs distant to original body site • Lack cellular differentiation • Carcinoma (epithelial), Sarcoma (connective), Lymphoma (lymphatic), Blood and Bone Marrow (leukemia, multiple myeloma) • Paraneoplastic syndromes • Etiology remains mystery • Age and sex • Genetic and ethnic factors • Oncogenic viruses • Occupational and environmental carcinogens • Radiation • Immunologic factors Antineoplastic • Also called cancer drugs, anticancer drugs, cytotoxic chemotherapy or chemotherapy • Cancer typically treated with surgery, radiation, chemotherapy (pharm), or combinations of three • Chemo divided into two groups o Cell cycle-nonspecific- cytotoxic( cell killing) in any phase of the cycle o Cell cycle specific- cytotoxic during a specific cell cycle phase • Goal is to kill every neoplastic cell to “cure” but not achieve in most cases • Some patient’s immune systems can clear remaining tumor • If cure not possible, goal is to control growth while maintaining best QOL with least possible discomfort and adverse effects as possible • Research constantly being done and protocols, dosages, etc changing • Most have low therapeutic index • Most are more susceptible to combination therapy • Toxicities • Stem from the drugs affecting rapidly dividing cells • Hair, GI tract, bone marrow • Hair loss, N/V, infections, fatigue, bleeding • Nadir: lowest level of WBC following treatment- risk for infection • Targeted therapy growing (monoclonal antibodies & cancer specific drugs) • Extravasation risk Extravasation • Leaking of an antineoplastic drug into surrounding tissues during - - - - - - - - - - - -- - - - - - - - - - - - - - - - - - - - - - - -erons (IFNs) • Monoclonal antibodies (MABs) • Interleukin (IL) receptor agonists and antagonists • Miscellaneous drugs • Work by • Enhancement or restoration of the host’s immune system defenses against the tumor • Direct toxic effect on the tumor cells, which causes them to lyse, or rupture • Adverse modification of the tumor’s biology, which makes it harder for the tumor cells to survive and reproduce • Therapeutic Effect • Enhancement of hematopoietic function • Regulation or enhancement of the immune response, including cytotoxic or cytostatic activity against cancer cells • Inhibition of metastases, prevention of cell division, or inhibition of cell maturation Hematopoietic Drugs • HDs are used to: • Decrease the duration of chemotherapy-induced anemia, neutropenia, and thrombocytopenia • Enable higher doses of chemotherapy to be given • Decreases bone marrow recovery time after bone marrow transplantation or irradiation • Erythropoietic drugs • epoetin alfa &darbepoetin alfa • Colony-stimulating factors (CSFs)-WBC • Filgrastim, pegfilgrastim, sargramostim • Platelet-promoting drugs • Oprelvekin, romipliostim Adverse Effects- usually mild, most common include, fever, muscle aches, bone pain, and flushing Colony-Stimulating Factors Drug Profile Filgrasim(Neupogen) Granulocyte colony-stimulating factor (G-CSF) Stimulates precursor cells for the type of white blood cells known as granulocytes (including basophils, eosinophils, and neutrophils) Administered before patient develops infection Pepfilgrastim (Neulasta) Longer acting form of filgrastim Sargramostim Granulocyte-macrophage colony-stimulating factor (GM-CSF) Stimulates bone marrow precursor cells that make both granulocytes and phagocytic (cell-eating) cells; known as monocytes Indicated for promoting bone marrow recovery after autologous (own marrow) or allogenic (donor marrow) bone marrow transplantation in patients with leukemia and lymphoma Platelet-Promoting Drug Profile Oprelvekin (Neumega) Both a hematopoietic drug and one of the ILs (IL-11) Enhances synthesis of platelets Indicated for the prevention of chemotherapy-induced severe thrombocytopenia and avoidance of the need for platelet transfusions Stimulates the bone marrow cells, specifically megakaryocytes that eventually give rise to platelets Immunomodulating Drugs • Medications that therapeutically alter a patient’s immune response to malignant tumor cells • Drugs that modify the body’s own immune response so that it can destroy various viruses and cancerous cells • Fourth part of cancer therapy, in addition to: • Surgery • Chemotherapy • Radiation • Also used for other diseases • Autoimmune • Inflammatory • Infectious Interferons (IFN) • Proteins with three basic properties • Antiviral • Antitumor • Immunomodulating • Alpha, beta, and gamma IFNs • Protect human cells from virus attack • Prevent cancer cells from dividing and replicating • Increase the activity of other cells in the immune system, such as macrophages, neutrophils, and NK cells Mech of Act- Restore the immune system’s function if it is impaired. • Augment the immune system’s ability to function as the body’s defense. • Inhibit the immune system from working. Helpful in autoimmune disorders Indications-Viral infections, Cancer, Autoimmune disorders Adverse Effects- Flulike effects (Fever, chills, headache, myalgia) • Dose-limiting adverse effect is fatigue • Anorexia, Dizziness, Nausea, Vomiting, Diarrhea Interferons Drug Profile IFN alfa products: “leukocyte IFNs”—produced from human leukocytes • IFN alfa-2a (Roferon-A) • IFN alfa-2b (Intron-A) • IFN alfa-n3 (Alferon-N) • IFN alfacon-1 (Infergen) • peginterferon alfa-2a (Pegasys) • peginterferon alfa-2b (PEG-Intron) - - - - - - - - - - - - [Show More]
Last updated: 2 years ago
Preview 1 out of 48 pages
 – University of Arizona.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Dec 02, 2020
Number of pages
48
Written in
Additional information
This document has been written for:
Uploaded
Dec 02, 2020
Downloads
0
Views
54

 - Over 500 Questions – Nightingale College.png)
.png)