*NURSING > Class Notes > Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 4,100% CORRECT (All)
Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 4,100% CORRECT
Document Content and Description Below
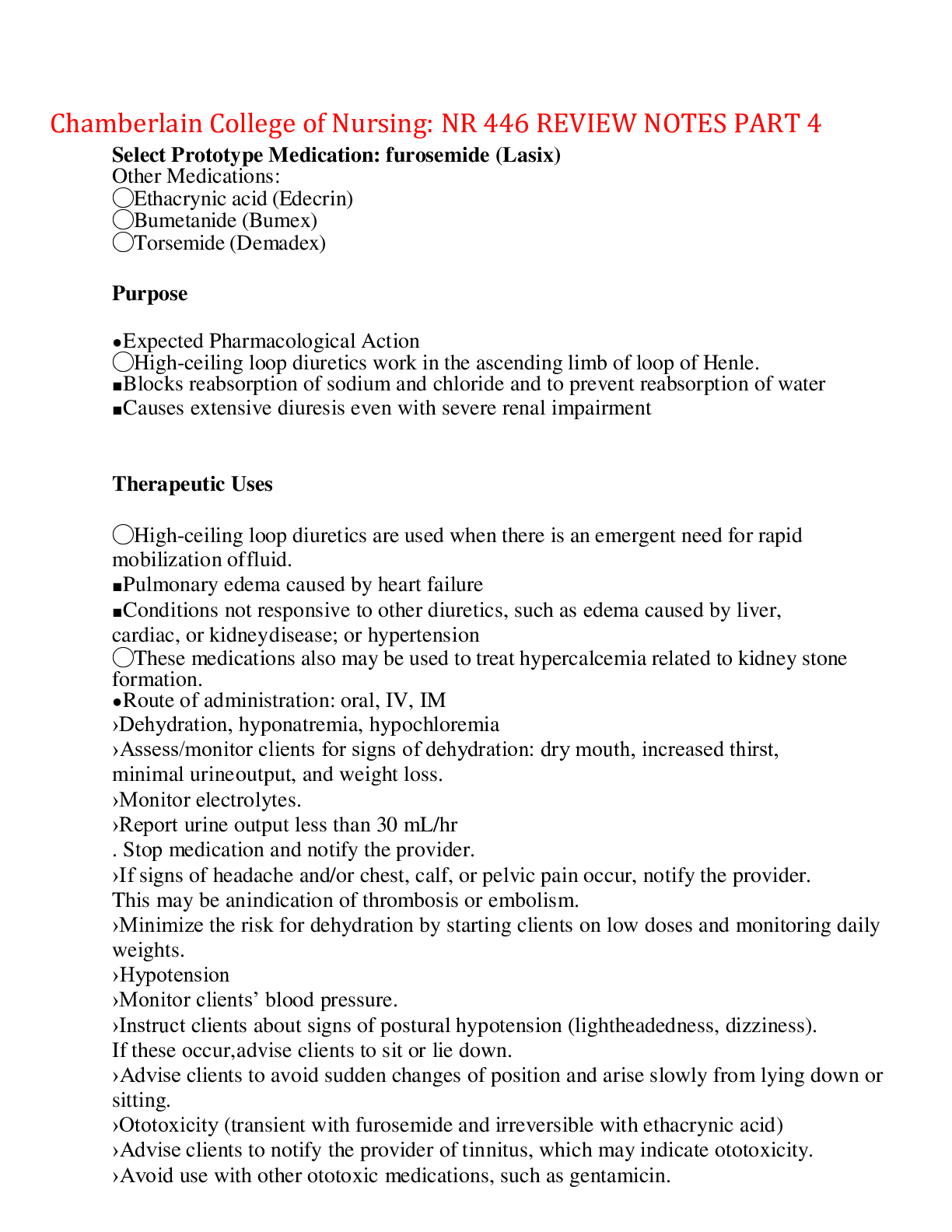
Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 4 Select Prototype Medication: furosemide (Lasix) Other Medications: ◯Ethacrynic acid (Edecrin) ◯Bumetanide (Bumex) ◯Torsemide (Dema ... dex) Purpose ● Expected Pharmacological Action ◯High-ceiling loop diuretics work in the ascending limb of loop of Henle. ■ Blocks reabsorption of sodium and chloride and to prevent reabsorption of water ■ Causes extensive diuresis even with severe renal impairment Therapeutic Uses ◯High-ceiling loop diuretics are used when there is an emergent need for rapid mobilization of fluid. ■ Pulmonary edema caused by heart failure ■ Conditions not responsive to other diuretics, such as edema caused by liver, cardiac, or kidney disease; or hypertension ◯These medications also may be used to treat hypercalcemia related to kidney stone formation. ● Route of administration: oral, IV, IM ›Dehydration, hyponatremia, hypochloremia ›Assess/monitor clients for signs of dehydration: dry mouth, increased thirst, minimal urine output, and weight loss. ›Monitor electrolytes. ›Report urine output less than 30 mL/hr . Stop medication and notify the provider. ›If signs of headache and/or chest, calf, or pelvic pain occur, notify the provider. This may be an indication of thrombosis or embolism. ›Minimize the risk for dehydration by starting clients on low doses and monitoring daily weights. ›Hypotension ›Monitor clients’ blood pressure. ›Instruct clients about signs of postural hypotension (lightheadedness, dizziness). If these occur, advise clients to sit or lie down. ›Advise clients to avoid sudden changes of position and arise slowly from lying down or sitting. ›Ototoxicity (transient with furosemide and irreversible with ethacrynic acid) ›Advise clients to notify the provider of tinnitus, which may indicate ototoxicity. ›Avoid use with other ototoxic medications, such as gentamicin. ›Hypokalemia (K+ less than 3.5 mEq/L) ›Monitor clients’ cardiac status and potassium levels. ›Report a decrease in potassium level (K+ less than 3.5 mEq/L). ›Teach clients to consume high-potassium foods (e.g., bananas, potatoes, dried fruits, nuts, spinach, and citrus fruit). ›Teach clients signs of hypokalemia, such as nausea/vomiting and general weakness. ›Other adverse effects (hyperglycemia, hyperuricemia, decrease in calcium and magnesium levels) ›Monitor clients’ blood glucose, uric acid, and calcium andmagnesium levels. ›Report elevated levels Contraindications/Precautions ● Avoid using these medications during pregnancy unless absolutely required. ● Use cautiously in clients who have diabetes and/or gout. ›Digoxin (Lanoxin) toxicity (ventricular dysrhythmias) can occur in the presence of hypokalemia. ›Monitor the client’s cardiac status and potassium and digoxin levels. ›Potassium-sparing diuretics often are used in conjunction with loop diuretics to reduce the risk of hypokalemia. ›Administer potassium supplements as prescribed by the provider. ›Concurrent use of antihypertensives can have additive hypotensive effect. ›Monitor the client’s blood pressure. ›Lithium carbonate (Eskalith) serum levelscan increase, which may lead to toxicity, if hyponatremia occurs due to the loop diuretic. ›Monitor the client’s lithium levels. Dosage may need to be adjusted. ›NSAIDs decrease blood flow to the kidneys, which reduces the diuretic effect. ›Watch for a decrease in the effectiveness of the diuretic, such as a decrease in urine output. Nursing considerations ● Obtain the client’s baseline data, including orthostatic blood pressure, weight, electrolytes, and location and extent of edema. ● Weigh clients at the same time each day with same amount of clothing and bed linen (if using a bed scale), usually upon awakening. ● Monitor the client’s blood pressure and I&O. ● Avoid administering the medication late in the day to prevent nocturia. Usual dosing time is 0800 and 1400. ● Administer furosemide orally, IV bolus dose, or continuous IV infusion. Infuse IV doses at 20 mg/min or slower to avoid abrupt hypotension and hypovolemia. ● If potassium level drops below 3.5 mEq/L, monitor the client’s potassium level, and notify the provider because the client may need to be placed on a potassium supplement. ● If the medication is used for hypertension, teach clients to self-monitor blood pressure and weight by keeping a log. ● Advise clients to get up slowly to minimize postural hypotension and check orthostatic blood pressure to assess for hypovolemia. If faintness or dizziness occurs, instruct clients to sit or lie down. ● Teach clients to report significant weight loss, lightheadedness, dizziness, GI distress, and/or general weakness to the provider, which may indicate hypokalemia or hypovolemia. ● Encourage clients to consume foods high in potassium. ● Instruct clients with diabetes to monitor for elevated blood glucose levels. ● Instruct clients to observe for signs of low magnesium levels (e.g., weakness, muscle twitching, and tremors). ● Depending on therapeutic intent, effectiveness may be evidenced by ◯Decrease in pulmonary or peripheral edema ◯Weight loss ◯Decrease in blood pressure ◯Increase in urine output Identify early and late signs of intracranial pressure. Early signs: Altered level of consciousness, tachycardia, rise in blood pressure, headache, abnormal respirations, elevated temperature, vomiting, pupil change, and headache. Late Signs: Increased systolic blood pressure, widened pulse pressure and slowed heart rate (Cushing triad), changes in motor function such as weakness, hemiplegia, positive babinski reflex, decorticate or decerebrat e posturing, and seizures. Interventions: 1. Maintain Patent Airway and prevent hypoxia 2. Elevate head of bed 30-40 degrees, Avoid extreme flexion, extension or rotation of the head and maintain the body in midline neutral position 3. Report presence of CSF 4. Maintain body temperature 5. Instruct client to avoid straining activities such as coughing or sneezing. 6. Decrease environmental stimuli 7. Monitor Input & output 8. Maintain body temperature and alignment Medications: 1. Mannitol (Osmitrol):Is a plasma expander by reducing the Htc and blood viscosity (increasing CBF and cerebral O2 delivery) Is a vascular osmotic, moving fluid from tissues into the blood vessels ( ICP) 2. Dexamethasone (Decadron) :Corticosteroid that improves neuronal function by improving CBF and restoring autoregulatio-Reduce cerebral edema :Monitor for infection, GI bleeding, intake and Na+, glucose levels regularly ,Give antacids or H2-receptor blockers or PPI to prevent GI ulcers and bleeding 3. Phenobarbital (Nembutal):Used to induce a barbiturate coma to decrease cerebral metabolic demands (Last resort) 4. Phenytoin (Dilantin):Prevent or tx seizures that can occur 5. Morphine sulfate:Control pain and restlessness, use if pt is receiving ventilationAvoid the use of opioids due to CNS depressant effect that will make a neurological assessment difficult Nutritional therapy: 1. Pt w/ ICP is in a hypermetabolic and hypercatabolic state that the need for glucose to provide fuel for metabolism of the injured brain a. Nutritional replacements should begin w/in 3 days after injury to reach full nutritional replacement w/in 7 days after injury Interventions for a person who is having hallucinations. Interventions: 1. Intervene with one-on-one contact 2. Decrease stimuli or move the client to another area 3. Avoid conveying the client that others also are experiencing the hallucination 4. Respond verbally to anything real the client talks about 5. Avoid touching the client 6. Administer medication as prescribed 7. Tell the client you understand they are seeing or hearing things but you do not see them. *for a client with hallucinations, safety is the first priority- Ensure that the client does not have auditory command telling him or her to harm self or others. Caring for a pt w/ Clostridium difficile Precautions Standard/contact Duration of precautions Duration of illness Reservoir Feces Nursing Considerations Hand hygiene; PPE if in contact with potentially contaminated materials Contact Precautions • Prevent transmission of infectious agents that are spread by direct or indirect contact with the client or the client’s environment. These precautions are applied in the presence of wound drainage, fecal incontinence, or other bodily discharges that suggest an increased potential for environmental contamination and risk of contamination. • PPE: gloves, gown; as needed use of mask and goggles. o Order of PPE application: gown, mask, goggles/face shield, gloves o Order of PPE removal: gloves, goggles/face shield, gown, mask • Nursing interventions: (in addition to standard precautions) o Private room preferred; may cohort with client who has infection with same organism. o Gloves and gown worn by caregivers and visitors. o Disposal of infectious dressing material into nonporous bag. o Dedicated equipment for the patient or disinfect after each use. o Client to leave room only for essential clinical reasons. • Protective isolation: o Used to protect clients who have an increased susceptibility to infections, are receiving chemotherapy, or are immunosuppressed or neutropenic. o Nursing interventions: Follow standard precautions. Institute maximum protection, which may include the use of sterile linens, food, and other supplies. Minimize exposure to microorganisms found on the outer layers of fresh flowers, fruits, and vegetables. Wear sterile gloves and gown/mask when in contact with client. Maximum protection will require ventilated/positive pressure room. RhoGAM administration Rh-negative mothers • RhO (D) immune globulin (RhoGAM) – suppresses immune response of clients who are Rh- negative • Administer RhO(D) immune globulin (RhOGAM) to the client if she is Rh-negative (standard practice after an amniocentesis (or any invasive procedure) for all women who are Rh- negative to protect against Rh isoimmunization). • Administer RhO(D) immune globulin (RhoGAM) IM around 28 weeks of gestation for clients who are Rh-negative. • Review the Rh status – All Rh-negative mothers who have newborns who are Rh-positive must be given RHO(D) immune globulin (RhoGAM) administered IM within 72 hr of the newborn being born to suppress antibody formation in the mother & to prevent sensitization in future pregnancies. • Test the client who receives both the rubella vaccine and RhoGAM after 3 months to determine whether immunity to rubella has been developed. • The Kleihauer-Betke test determines the amount of fetal blood in maternal circulation if a large fetomaternal transfusion is suspected. If 15 mL or more of fetal blood is detected, the mother should receive an increased RhoGAM dose to suppress the maternal immune response to fetal Rh-positive blood. • Laboratory tests may include CBC with monitoring of Hgb, Hct, and WBC and platelet counts ANTIDIUERTIC HORMONE Care of a newborn at Birth • INITIAL CARE(immediately after birth): Airway, breathing, circulation (ABC’s) • Thermoregulation • Umbilical cord: two arteries, one vein • Apgar: 1& 5 min of life o Ratings: 7-10 (WNL) 4-6 (moderately distressed) 0-3(severely distressed) SCORE 0 1 2 HR Absent < than 100 > than 100 RR Absent Slow, weak cry Good cry Muscle tone Flaccid Some flexion Well-flexed Reflex irritability None Grimace Cry Color Blue, pale Pink body, cyanotic hands and feet (acrocyanosis) Completely pink • Equipment needed for assessment o Bulb syringe o Stethoscope o Axillary thermometer (Rectal temperatures are avoided) o Blood pressure cuff 2 o Scale with protective cover in place (Scale should be at 0) o Tape measure in centimeters – Measure length, head circumference, chest, and abdominal circumference above the umbilicus. o Clean gloves • Expected reference ranges of physical measurements o Weight – 2,500 to 4,000 g o Length – 45 to 55 cm (18 to 22 in) o Head circumference – 32 to 36.8 cm (12.6 to 14.5 in) o Chest circumference – 30 to 33 cm (12 to 13 in) o Temperature: 37C Variations: 36.5-37.2 C Abnormal if temp not stabilized after 10 hrs Prevent heat loss, dry thoroughly, cover head, place on warm, dry environment, skin to skin encouraged o Blood Pressure: SBP 60-80; DBP 40-50 Variations occur w/crying & sleeping Hypotension- potential sepsis/hypovolemic Hypertension in upper extremities- potential coarctation of aorta Assess all 4 extremities on admission, check arm & leg- significant difference between lower and upper extremities • Physical assessment • VS o HR: 100-160/min Normal variations 100/min (sleeping) 180/min (crying Assess pulses bilaterally, apical pulse for 1 min, assess for murmur o RR: 40-60/min Bradypnea: <25/min TachypneaL >60/min Assess rate, rhythm & adventious breath sounds RR will be shallow & irregular in newborn Nasal flaring, grunting, intercostals retractions or see-saw breathing= signs of distress • Reflexes • Reactivity o 1st period of reactivity-NB alert & exhibits exploring activity, makes sucking sound, rapid heartbeat & RR, lasts 15-30mins after birth o Period of relative inactivity- sleep, HR & RR decrease, last about 30min-2hr post birth o 2nd period or reactivity- reawakes, often gags& chokes on mucus that accumulates in mouth, lasts 2-8hrs after birth • Gestational age assessment (New ballard score) o Physical ( skin, lanugo, plantar surfaces, breast, eye/ear, genitals) o Neuromuscular (posture, square window, arm recoil, popliteal angle, scarf sign, heel to ear) o Medications (erythromycin/tetracycline admin w/in 1 hr of birth, vitamin K IM w/in 1 hr, hepatitis w/in 12hr of birth) • Monitor for s/s of resp distress • Promote patent airway o Oral/nasal suction PRN Remember MOUTH before NOSE • Promote thermoregulation • Monitor glucose levels • Monitor nutrition o Initiate feeds immediately after birth o Maintain fluid intake of 100-140 mL/kg/24hr • Monitor elimination o Keep perineal area clean and dry o 1st void and stool w/in 24hrs • Provide skin care o Core care- clean with neutral pH cleanser and sterile H2O. cord should be kept clean and dry to prevent infection o First bath after temperature stabilizes • Promote bonding o Encourage mothers/family to hold newborn • Promote safety & security for NB and family o ID bands correctly placed o All facility staff assisting w/care should have an ID badge DESMOPRESSIN (DDVAP, Stimuate) • Antidiuretic Hormone (ADH) o Produced by the posterior pituitary, promotes reabsorption of H2O w/in the kidney o Natural ADH causes vasoconstriction because of the contraction of vascular smooth muscle o Desmopressin cause much less vasoconstriction o Therapeutically used to treat Diabetes Insipidus (DI) o ADH sometimes used during CPR to temporarily decrease blood flow to the periphery & increase flow to the brain & heart o Admin routes= PO, intranasal, SQ, IV Adverse Effects RN Interventions/ Pt Education Reabsorption of too much H2O Monitor for overhydration (sleepiness, pounding headache) Generally, pt should reduce fluid intake during therapy Pt should use smallest effective dose of desmopressin Myocardial ischemia from excessive vasoconstriction Monitor ECG & BP Advise pt to notify the HCP of chest pain, tightness, or diaphoresis • The use of vasopressin contraindicated in pts who have CAD (risk for angina, MI), peripheral circulation (Risk for gangrene) or chronic nephritis Medication/food interactions RN interventions/ Pt teaching Carbamazepine & TCA’s may increase diuretic action Use cautiously together Concurrent use of alcohol, heparin, lithium, and phenytoin may decrease antiduretic effects Establish baseline I&O and weight and monitor frequently • Nursing Administration o Monitor VS, CVP, I&O, specific gravity, and Lab studies (K, Na, BUN, Creatinine, Specific gravity, osmolality) o Monitor BP & HR o Monitor for headache, confusion, or other indications of water intoxication o w/ IV admin of vasopressin, monitor IV site carefully because extravasation can lead to gangrene o Intranasal desmopresin starts w/a bedtime dose. I&O monitored. When nocturia is controlled, doses are given twice daily • RN evaluation of medication effectiveness o Depending on therapeutic intent, evidence of effectiveness includes: A reduction in the large volumes of Urine output associated w/ DI to normal levels of Urine output (1.5-2L/ 24hrs) Cardiac arrest survival • Desmopressin avoided during Esophageal varices due to multiple adverse effects • Used during DI, which results from a deficiency of ADH o Decreased ADH reduces the ability of collecting and distral renal tubules in the kidneys to concentrate uring, resulting in excessive diluted urination, excessive thirst, and excessive fluid intake o Desmopressing increases H2O reabsorption from kidneys and decreases urine output o Pt to monitor weight daily and report gain > 0.9 kg (2lb) in 24hrs o RN to monitor for indications of thrombocytopenia (sore throat, bruising, fever) o Can be taken w/food to reduce gastric distrewss o Use caution when driving or operating heavy machinery until effects of med established o Notify HCP of sore throat, bleeding, fever Signs / Symptoms of Pericarditis Commonly follows a respiratory infection. Can be due to a myocardial infarction. Findings include chest pressure/pain, friction rub auscultated in the lungs, shortness of breath, and pain relieved when sitting and leaning forward. Laboratory Tests Blood cultures to detect a bacterial infection. An elevated WBC count can be indicative of a bacterial infection. Cardiac enzymes can be elevated with pericarditis. Elevated ESR and CRP indicate inflammation in the body. Throat cultures to detect a streptococcal infection, which can lead to rheumatic fever Nursing Care Auscultate heart sounds (listen for murmur). Assess breath sounds in all lung fields (listen for friction rub). Review ABGs, SaO2, and chest x-ray results. Administer oxygen as prescribed. Monitor vital signs (watch for fever). Monitor ECG, and notify the provider of changes. Monitor for cardiac tamponade and heart failure. Obtain throat cultures to identify bacteria to be treated by antibiotic therapy. Administer antibiotics, antipyretics and pain as prescribed. Assess onset, quality, duration, and severity of pain. Encourage bed rest. Sedative Hypnotics -- adverse effects Benzodiazepines; triazolam (Halcion) CNS depression (lightheadedness, drowsiness, incoordination). Anterograde amnesia. Paradoxical response such as insomnia, excitation, euphoria, anxiety, rage. Respiratory depression, especially with IV administration. Physical dependence. Acute toxicity; oral toxicity (drowsiness, lethargy, confusion); IV toxicity (respiratory depression) Nonbenzodiazepines zolpidem (Ambien) Daytime sleepiness and lightheadedness Melatonin Agonist ramelteon (Rozerem) Sleepiness, dizziness, fatigue. Hormonal effects (amenorrhea, decreased libido, infertility, and galactorrhea) Intravenous Anesthetics Respiratory and cardiovascular depression with high risk for hypotension. Bacterial infection (with propofol). Psychologic reactions (with ketamine). Hallucinations and mental confusion. Risk Factor related to ethnicity: Different ethnicities have the potential to be a risk factor for different medical conditions. • The cancer incidence rate among African Americans is 10% higher than among European Americans • Latinos have higher rates of diabetes, liver disease, and infectious diseases • African Americans and Latinos have approximately twice the risk as European Americans of developing diabetes • Asian Americans are 60% more likely to being at risk of developing diabetes in comparison to European Americans and are more likely to develop the disease as lower BMIs and lower body weights. South Asians are especially more likely to developing diabetes as it is estimated South Asians a four times more likely to developing the disease in comparison to European Americans • Native Americans suffer from higher rates of diabetes, tuberculosis, pneumonia, influenza, and alcoholism than does the rest of the • European Americans die more often from heart disease and cancer than do Native Americans, Asian Americans, or Hispanics • White Americans have far higher incident rates of melanoma of the skin or skin cancer than any other race/ethnicity in the US. • Cystic fibrosis, the most common life-limiting autosomal recessive disease among people of European heritage • Sickle-cell anemia, most prevalent in populations with sub-Saharan African ancestry but also common among Latin-American, Indian, and Saudi Arab populations, as well as those people of Mediterranean regions such as Turkey, Greece, and Italy • Thalassemia, most prevalent in populations having Mediterranean ancestry • Tay–Sachs disease, an autosomal recessive disorder more frequent among Ashkenazi Jews • Hereditary hemochromatosis, most common among persons having Northern European ancestry, in particular those people of Celtic descent Mania is severe enough to cause marked impairment in activities or relationships that may necessitate hospitalization to prevent harm to self or others. Presenting symptoms: Inflated self-esteem or grandiosity Decreased need for sleep More talkative than usual Flight of ideas Increase in goal directed activity Excessive involvement in unrestrained buying sprees, poor business investments, or sexual indiscretions due to loss of impulse control. Nursing interventions: Assess whether client is danger to self or others Assess the need to protect client from uninhibited behaviors Assess for coexisting medical conditions such as substance use disorder Therapeutic interventions: Use firm calm approach Provide frequent high-calorie fluids Maintain low-level stimuli Medications: Lithium Anticonvulsants: valproic acid (Depakote) Atypical antipsychotics: aripiprazole (Abilify) and risperidone (Risperdal) Antianxiety agents: clonazepam (Klonopin) Antiemetic: Metoclopramide (Reglan) Action: Multiple classifications of medications that affect the GI tract or the “vomiting center” of the brain to reduce nausea/vomiting. Therapeutic Uses: Postop, chemotherapy, and nausea/vomiting associated with disease process. Side/Adverse Effects: Drowsiness, anticholinergic effects, restlessness, EPSs, and tardive dyskinesia Nursing Interventions: Instruct client about rapid GI emptying and discontinue with signs of EPSs. EPSs: Abnormal body movements may include: involuntary fine motor tremors, rigidity, uncontrollable restlessness, and acute dystonias (spastic movements and/or muscle rigidity affecting the head, neck, eyes, facial area, and limbs). These may occur within a few hr or may take months to develop. These symptoms are more often associated with medications affecting the CNS, such as those used to treat mental health disorders. Endocrine disorders Monitoring for theraputic effect: Anterior pituitary gland: Serum GH CT/MRI/X-RAYS Posterior pituuitary gland: WATER FLUID DEPREVATION MONITOR BODY WEIGHT HOURLY URINE OUTPUT SERUM AND URINE OSMOLARITY VASSOPRESSIN TEST MRI OF HYPOTHALAMUSAND PITUITARY 24 HR UNRINE OUTPUT Addrenal cortex DEXAMETHASONE SUPPRESSION TEST. Addrenal medula ABDOMINAL CT/ECG/SERUM ALDOSTERONE/RENIN/POTASSIUM/URINE ALDOSTERONE Thyroid gland Diagnostic Procedures – Laboratory Tests Serum T3 Serum T4 Free T4 index T3 resin uptake Thyroid antibodies THR stimulation test TSH Serum cholesterol CBC Parathyroid gland Laboratory Tests Calcium level less than 9.0 mg/Dl Diagnostic Procedures Electrocardiogram ECG changes – prolonged QT interval and prolonged ST interval Pancreas Laboratory Tests WBC increased with left shift indicates inflammation Direct, indirect, and total serum bilirubin (increased if bile duct obstructed) Amylase and lipase (increased with pancreatic involvement) Aspartate aminotransferase (AST), lactate dehydrogenase (LDH), and alkaline phosphatase (ALP) (increased with liver dysfunction) may indicate the common bile duct is obstructed. Serum cholesterol (greater than 200 mg/dL) Diagnostic Procedures Ultrasound visualizes gall stones and a dilated common bile duct. An abdominal x-ray or CT scan can visualize calcified gallstones and an enlarged gall bladder. A hepatobiliary scan (HIDA) assesses the patency of the biliary duct system after an IV injection of contrast. An endoscopic retrograde cholangiopancreatography (ERCP) allows for direct visualization using an endoscope that is inserted through the esophagus and into the common bile duct via the duodenum. A sphincterotomy with gall stones removal may be done during this procedure. (Refer to the chapter on Gastrointestinal Diagnostic Procedures.) A percutaneous transhepatic cholangiography (PTC) involves the direct injection of contrast into the biliary tract through the use of a flexible needle. The gallbladder and ducts can be visualized. Intervening in bonding, how to promote? It is important for a nurse to provide comfort measures for the client during the fourth stage of labor. This maternal recovery period starts with the delivery of the placenta and lasts from 1 to 4 hr. Also during this stage, parent-newborn bonding should begin to occur. The main goal during the immediate postpartum period is to prevent postpartum hemorrhage. Other goals include assisting in a client’s recovery, identifying deviations in the expected recovery process, providing comfort measures and pharmacologic pain relief as prescribed, providing client education about newborn and self-care, and providing baby-friendly activities to promote infant/family bonding. 0The postpartum period, also known as the puerperium, includes physiological and psychological adjustments. This period begins after the delivery of the placenta and ends when the body returns to the prepregnant state. This process takes approximately 6 weeks. Assess for behaviors that facilitate and indicate mother-infant bonding. Considers the infant a family member. Holds the infant face-to-face (en face), maintaining eye contact. Assigns meaning to the infant’s behavior and views positively. Identifies the infant’s unique characteristics and relates them to those of other family members. Naming the infant indicates that bonding is occurring. Touches the infant and maintains close physical proximity and contact. Provides physical care for the infant such as feeding and diapering. Responds to the infant’s cries. Smiles at, talks to, and sings to the infant. Assess for behaviors that impair and indicate a lack of mother-infant bonding. Apathy when the infant cries. Disgust when the infant voids, stools, or spits up. Expresses disappointment in the infant. Turns away from the infant. Does not seek close physical proximity to the infant. Does not talk about the infant’s unique features. Handles the infant roughly. Ignores the infant entirely Assess for signs of mood swings, conflict about maternal role, and/or personal insecurity. Feelings of being “down.” Feelings of inadequacy. Feelings of anxiety related to ineffective breastfeeding. Emotional lability with frequent crying. Flat affect and being withdrawn. Feeling unable to care for the infant. Nursing interventions to assist with maternal-infant bonding. Facilitate the bonding process by placing the infant skin-to-skin in the en face position with the client immediately after birth. Promote rooming-in as a quiet and private environment that enhances the family bonding process. Promote early initiation of breastfeeding, and encourage the client to recognize infant readiness cues. Offer assistance as needed. Teaching the client about infant care facilitates bonding as the client’s confidence improves. Encourage the parents to bond with their infant through cuddling, bathing, feeding, diapering, and inspection. Provide frequent praise, support, and reassurance to the client as she moves toward independence in caring for her infant and adjusting to her maternal role. Encourage the client/parents to express their feelings, fears, and anxieties about caring for their infant. Mass Casualty Triage • Triage must be rapid and conducted in 15 seconds • Categorized by their acuity o Emergent or Class I Life-threatening or limb-threatening situation Identified with a red tag o Urgent or Class II Major injuries that require immediate treatment Identified with a yellow tag o Nonurgent or Class III Minor injuries that do not require immediate treatment Identified with a green tag o Expectant or Class IV Indicates those who are expected to die Identified with a black tag IV (excretory) urography • Used to detect obstruction, assess for a paraenchymal mass, and assess size of kidney • IV contrast dye (iodine-based) used to enhance images • Preprocedure o Encourage increased fluids the day before procedure. o Bowel cleansing with laxative or enema to remove fecal contents, fluid, and gas from the colon for a more clear visualization. o NPO after midnight. o Determine client allergy to iodine, seafood, eggs, milk, chocolate; or if client has asthma. o Check the client’s creatinine and BUN levels. o Hold metformin (Glucophage) for 24 hr before procedure (risk for lactic acidosis from contrast dye with iodine). • Postprocedure o Administer parenteral fluid, or encourage oral fluids to flush dye through the renal system and prevent complications. o Diuretics may be administered to increase dye excretion. o Follow-up creatinine and BUN serum levels before metformin is resumed. • Physical Abuse Safety Concerns in Long Term Care Facility o Spiral fracture- occurs from twisting motion o Bruises/burns healing at different stages • Falls o Older adult clients have an increased risk of falls related to impaired balance, generalized weakness, gait changes, and impaired vision and hearing. Assess the home environment for safety (remove throw rugs, provide adequate lighting, clear walkways) to prevent falls, which may result in fractures. Reinforce the use of safety equipment and assistive devices. Instruct the client to avoid inclement weather (ice, slippery surfaces). Clearly mark thresholds, doorways, and steps. • Nutrition o At an increase risk for altered nutrition due to the physiologic changes of aging, cognitive and functional decline, environmental factors, and social isolation Weight loss Poor dental hygiene/ poor-fitted or no dentures Dysphagia- difficulty swallowing • Aspiration • Skin break down- increase risk of pressure ulcer Treatment of Sinus Tachycardia • Sinus Tachycardia: o Rhythm- normal o Rate- higher than 100 o P-wave- normal o PRI- normal o QRS- normal • Cause: o Pain o Anxiety o Fever o Hypovolemia • Treatment: o Treat the underlying cause o Sit down o Antipyretics o Analgesics o ANXIOLYTIC o FLUIDS • Signs and Symptoms: o Decreased CO o Dizziness o Hypotension Information Security Mandatory adherence with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) began in 2003 to help ensure the confidentiality of health information. A major component of HIPAA, the Privacy Rule, promotes the use of standard methods of maintaining the privacy of protected health information (PHI) among health care agencies. It is essential for nurses to be aware of clients’ rights to privacy and confidentiality. Facilities’ policies and procedures help ensure adherence with HIPAA regulations. The Privacy Rule requires that nurses protect all written and verbal communication about clients. Only health care team members directly responsible for a client’s care may access that client’s record. Nurses may not share information with other clients or staff not caring for the client. Clients have a right to read and obtain a copy of their medical record. Nurses may not photocopy any part of a medical record except for authorized exchange of documents between facilities and providers. Staff must keep medical records in a secure area to prevent inappropriate access to the information. They may not use public display boards to list client names and diagnoses. Electronic records are password protected. The public may not view them. Staff must use only their own passwords to access information. Nurses must not disclose clients’ information to unauthorized individuals or family members who request it in person or by telephone or e-mail. Many hospitals use a code system to identify those individuals who may receive information about a client. Nurses should ask any individual inquiring about a client’s status for the code and disclose information only when the individual can give the code. Communication about a client should only take place in a private setting where unauthorized individuals cannot overhear it. To adhere to HIPAA regulations, each health care facility has specific policies and procedures to monitor staff adherence, technical protocols, computer privacy, and data safety. Log off from the computer before leaving the workstation to ensure that others cannot view protected health information on the monitor. Never share a user ID or password with anyone. Never leave a medical record or other printed or written PHI where others can access it. Shred any printed or written client information for reporting or client care after use. Bacterial Vaginosis • Bacterial vaginosis is an abnormal vaginal condition that is characterized by vaginal discharge and results from an overgrowth of unusual bacteria in the vagina. • Bacterial vaginosis is not dangerous, but it can cause disturbing symptoms. • Symptoms of bacterial vaginosis are vaginal discharge and odor, although most women with the condition experience no symptoms. • In diagnosing bacterial vaginosis, it is important to exclude other serious infections, such as gonorrhea and Chlamydia. • Treatment options for bacterial vaginosis include oral antibiotics and vaginal gels. Certain factors have been identified that increase the chances of developing bacterial vaginosis. These include: • multiple or new sexual partners, • IUDs (intrauterine devices) for birth control, • recent antibiotic use, • vaginal douching, and • cigarette smoking. While up to 1/3 of cases of bacterial vaginosis may resolve on their own, it is recommended that medical treatment be given if symptoms are present or during pregnancy to avoid the development of complications. Antibiotics are the recommended treatment for bacterial vaginosis. A few antibiotic remedies are routinely used and include: • metronidazole (Flagyl) taken by either oral (pill) form or vaginallymetronidazole gel (Metrogel). The oral metronidazole can cause some minor but unpleasant side effects, but is believed to be the most effective treatment. The gels do not typically cause side effects, although yeast vaginitis can occur as a side effect of the medication • vaginal clindamycin cream (Cleocin) • tinidazole (Tindamax) is an antibiotic that appears to be effective in treating bacterial vaginosis, and may have fewer side effects than metronidazole. Recurrence of bacterial vaginosis is possible even after successful treatment. More than half of those treated experience recurrent symptoms within 12 months. It is unclear why so many recurrent infections develop. With recurrent symptoms, a second course of antibiotics is generally prescribed. Closed Intermittent Irrigation • Prepare a sterile syringe with irrigant • Clamp the catheter between the injection port and the extension tubing • Cleanse the injection port with an antiseptic swab or wipe • Insert the needle of the syringe with the irrigant into the injection port • Slowly inject the irrigant into the catheter • Withdraw the syringe and remove the clamp • Allow the irrigant to drain into the drainage bag GI therapeutic procedures/diet plan • Enteral Feedings o Enteral feedings are instituted when a client can no longer take adequate nutrition orally o Complications Overfeeding results from infusion of greater quantity of feeding that can be readily digested by the client, resulting in abdominal distention, nausea, and vomiting • Check residual every 4 to 6 hr • Follow protocol for withholding excess residual volumes as directed (typically 100 to 200 mL) • Withhold feeding as prescribed and resume at reduced rate as prescribed • Total parenteral nutrition (TPN) o TPN is a hypertonic IV bolus solution. The purpose of TPN administration is to prevent or correct nutritional deficiencies and minimize the adverse effects of malnourishment Contains complete nutrition, including calories (in a high concentration [20% to 50%] of dextrose), lipids/essential fatty acids, proteins, electrolytes, vitamins, and trace elements. Standard IV bolus therapy is typically less than or equal to 700 calories/day. o The flow rate is gradually increased and gradually decreased to allow body adjustment (usually no more than a 10& hourly increase in rate) Never abruptly stop TPN. Speeding up/slowing down the rate is contraindicated. An abrupt rate change can alter blood glucose levels significantly o Check capillary glucose every 4 to 6 hr for at least the first 24 hr Client receiving TPN frequently need supplemental regular insulin until the pancreas can increase its endogenous production of insulin Monitor for hypoglycemia • Paracentesis o Performed by inserting a needle or trocar through the abdominal wall into the peritoneal cavity. The therapeutic goal is relief of abdominal ascites pressure. Low sodium diet (1.5 to 2 grams/day) Limit amount of fluids if kidney problems present (1 liter or less/day) • Nasogastric decompression o Clients who have intestinal obstruction require NG decompression. An NG tube is inserted, then suction is applied to relieve abdominal distention. Treatment continues until the obstruction resolves or is removed The client is to remain NPO • Bariatric surgeries o Treatment for morbid obesity when other weight control methods have failed Instruct the client on limitations regarding liquids or pureed foods for the first 6 weeks, as well as the volume that can be consumed (often not to exceed 1 cup) Remind the client that overeating can dilate the surgically created pouch causing weight to be regained Instruct the client to take vitamin and mineral supplements Tell the client to eat two servings of protein a day Tell the client to eat only nutrition-dense foods. Avoid empty calories, such as colas and fruit juice drinks. • Ostomies o An ostomy is a surgical opening from the inside of the body to the outside and can be located in various areas of the body. Ostomies can be permanent or temporary o Educate the client regarding dietary changes and ostomy appliances that can help manage flatus and odor Foods that can cause odor include fish, eggs, asparagus, garlic, beans, and dark green leafy vegetables Foods that can cause gas include dark green leafy vegetables, beer, carbonated beverages, dairy products, and corn. Yogurt can be ingested to decrease gas After an ostomy involving the small intestine is placed, the client should be instructed to avoid high-fiber foods for the first 2 months after surgery, chew food well, increase fluid intake, and evaluate for evidence of blockage when slowly adding high-fiber foods to the diet Contraindications for MMR vaccination http://www.cdc.gov/vaccines/recs/vac-admin/contraindications-vacc.htm The Advisory Committee on Immunization Practices (ACIP) has recommended that all vaccines can be administered to persons with minor illnesses such as diarrhea, mild upper respiratory infection with or without low-grade fever, or other low-grade febrile illness. Use precautions to MMR vaccination: • Moderate or severe acute illness with or without fever • Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) • History of thrombocytopenia or thrombocytopenic purpura • Need for tuberculin skin testing MMR contraindicated: • Hypersensitivity to any component of the vaccine, including gelatin. • Anaphylactic reactions after a previous dose, to any component, or to neomycin. • Pregnancy. Postpubertal females: pregnancy should be avoided for three months following vaccination. • Known severe immunodeficiency (e.g., from hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, or long-term immunosuppressive therapy or patients with human immunodeficiency virus [HIV] infection who are severely immunocompromised). • Individuals with blood dyscrasias, leukemia, lymphomas of any type, or other malignant neoplasms affecting the bone marrow or lymphatic systems. Stages of labor Primigravida – primi Multigravida – multi ° - hour '– minute "– second Stage Duration Beginning Contractions Ending Maternal characteristics Nursing interventions First Latent phase Active phase Transition phase 12.5° Primi: 6° Multi: 4° Primi: 3° Multi: 2° 20' -40' Onset of labor Cervix: 0 cm Cervix: 4 cm Cervix: 8 cm Irregular, mild to moderate. Frequency 5'-30' Duration 30"-45" Regular, moderate to strong Frequency 3' -5' Duration 40" - 70" Strong to very strong. Frequency 2'- 3' Duration 45"- 90" Complete cervix dilation Cervix: 3 cm Cervix: 7 cm Complete cervix dilation 10 cm On average cervical dilation: Primi – 1 cm/hr. Multi – 1.5 cm/hr. Some dilation and effacement. Talkative and excited. Rapid dilation and effacement. Some fetal descent. In pain. Feelings of helplessness. Anxiety and restlessness increase as contractions become stronger. Tired, restless, and irritable. May have nausea and vomiting. Urge to push. Increased bloody show. Most difficult part of labor. Admission assessment. Informed consent. Birth plan. Continue assessing maternal/fetal status Assess amniotic fluids status. Nitrazine paper used if ROM (will turn blue in presence of alkaline amniotic fluids: pH 6.5-7.5). Assist with non-pharm. pain management. Active phase considered an emergency med. condition by the Emergency Medical Treatment & Active Labor Act (EMTALA). FHR Normal: 110-160/min Variability best indicator of well-being. Moderate= 6-25/min. External: auscultation, ultrasound transducer Internal: spiral electrode, requires raptured membraine, ↑risk of infection. UTERINE CONTRACTIONS External: manual/tocotransducer Internal: intrauterine pressure cath. (IUPC) CERVIX Exams done with sterile gloves. Limit exams due To risk of infection. Second “pushing” Primi: 30'- 2° Multi: 5'- 30' Complete cervix dilation Progresses to intense every 1' - 2' Delivery of baby Pushing results in birth of fetus Assess FHR Q15' Assist with pushing, breathing. Record delivery time, medications, episiotomy or lacerations. Third 5' - 30' Delivery of baby Mild Delivery of placenta Placental separation and expulsion. Schultz presentation: shiny fetal surface of placenta emerges first. Duncan presentation: dull maternal surface of placenta emerges first. Pt focused on her baby. Patient: assessment of VS, bleeding, fundus. Newborn: ABC, Apgar score, warm environment, safety, infection control. Fourth 1° – 2° Delivery of placenta None Maternal stabilization of vital signs Achievement of vital sign homeostasis. Lochia scant to moderate rubra Assessment: Maternal vital signs, Fundus, Lochia, Perineum, Urinary output, Maternal & newborn baby-friendly activities. Interventions: Assess maternal vital signs, fundus, lochia every 15' x 4; every 30' x 2; and in 60'. ■ Hemorrhage is priority concern. Massage the uterine fundus and/or administer oxytocics as prescribed to maintain uterine tone to prevent hemorrhage. ■ Assess the client’s perineum, and provide comfort measures as indicated. ■ Encourage voiding to prevent bladder distention. ■ Encourage breastfeeding & promote maternal/newborn bonding. Offer assistance with breastfeeding, and provide reassurance. ■ Instruct the client to notify the nurse of increased vaginal bleeding or passage of blood clots. Confidentiality and Information Security Nursing Role in Confidentiality • It is essential for nurses to be aware of the rights of clients in regard to privacy and confidentiality. Facility policies and procedures are established in order to ensure compliance with HIPAA regulations. It is essential that nurses know and adhere to the policies and procedures. HIPAA regulations also provide for penalties in the event of noncompliance with the regulations. • The Privacy Rule of HIPAA requires that nurses protect all written and verbal communication about clients. Components of the privacy rule include: o Only health care team members directly responsible for the client’s care should be allowed access to the client’s records. Nurses may not share information with other clients or staff not involved in the care of the client. o Clients have a right to read and obtain a copy of their medical record, and agency policy should be followed when the client requests to read or have a copy of the record. o No part of the client record can be copied except for authorized exchange of documents between health care institutions. For example: -Transfer from a hospital to an extended care facility -Exchange of documents between a general practitioner and a specialist during a consult o Client medical records must be kept in a secure area to prevent inappropriate access to the information. Using public display boards to list client names and diagnoses is restricted. o Electronic records should be password-protected, and care must be taken to prevent public viewing of the information. -Health care workers should use only their own passwords to access information. o Client information may not be disclosed to unauthorized individuals, including family members who request it and individuals who call on the phone. -Many hospitals use a code system in which information is only disclosed to individuals who can provide the code. - Nurses should ask any individual inquiring about a client’s status for the code and disclose information only when an individual can give the code. o Communication about a client should only take place in a private setting where it cannot be overheard by unauthorized individuals. The practice of “walking rounds,” where other clients and visitors can hear what is being said, is no longer sanctioned. Taped rounds also are discouraged because nurses should not receive information about clients for whom they are not responsible. Change-of-shift reports can be done at the bedside as long as the client does not have a roommate and no unsolicited visitors are present. Information Security o Health information systems (HIS) are used to manage administrative functions and clinical functions. The clinical portion of the system is often referred to as the clinical information systems (CIS). The CIS may be used to coordinate essential aspects of client care. o In order to comply with HIPAA regulations, each health care facility has specific policies and procedures designed to monitor staff adherence, technical protocols, computer privacy, and data safety. o Information security protocols include: - Logging off from the computer before leaving the workstation to ensure that others cannot view protected health information (PHI) on the monitor - Never sharing a user ID or password with anyone -Never leaving a client’s chart or other printed or written PHI where others can access it -Shredding any printed or written client information used for reporting or client care after it is no longer needed Newborn: Hyperbilirubinemia • Hyperbilirubinemia is an elevation of serum bilirubin levels resulting in jaundice. Jaundice normally appears in the head (especially the sclera and mucous membranes), and then progresses down the thorax, abdomen, and extremities. • Jaundice can be either physiologic or pathologic o Physiologic jaundice is considered benign (resulting from normal newborn physiology of increased bilirubin production due to the shortened lifespan and breakdown of fetal RBCs and liver immaturity). The newborn with physiological jaundice has no other manifestations and shows evidence of jaundice after 24 hr of age. o Pathologic jaundice is a result of an underlying disease. Pathologic jaundice appears before 24 hr of age or is persistent after day 7. In the term newborn, bilirubin levels increase more than 0.5 mg/dL/hr, peaks at greater than 13 mg/dL, or is associated with anemia and hepatosplenomegaly. Pathologic jaundice is usually caused by a blood group incompatibility or an infection, but may be the result of RBC disorders. • Kernicterus (bilirubin encephalopathy) can result from untreated hyperbilirubinemia with bilirubin levels at or higher than 25 mg/dL. It is a neurological syndrome caused by bilirubin depositing in brain cells. Survivors may develop cerebral palsy, epilepsy, or mental retardation. They may have minor effects such as learning disorders or perceptual-motor disabilities. Risk Factor Objective Data Lab Tests/Diagnostic procedure/Treatment -Increased RBC production or breakdown -Rh or ABO incompatibility, -Decreased liver function - Ineffective breastfeeding -Sibling with diagnosed jaundice -Certain medications (maternal ingestion of aspirin tranquilizers, and sulfonamides) - Hypoglycemia -Hypothermia -Anoxia - Prematurity Physical assessment findings: • Yellowish tint to skin, sclera, and mucous membranes. • To verify jaundice, press the newborn’s skin on the cheek or abdomen lightly with one finger. Then, release pressure, and observe the newborn’s skin color for yellowish tint as the skin is blanched. • Note the time of jaundice onset to distinguish between physiologic and pathologic jaundice. • Assess the underlying cause by reviewing the maternal prenatal, family, and newborn history. • Hypoxia, hypothermia, hypoglycemia, and metabolic acidosis can occur as a result of hyperbilirubinemia and may increase the risk of brain damage. Clinical findings of kernicterus: • Very yellowish or orange skin • Lethargy • Hypotonic • Poor suck reflex • Increased sleepiness • If untreated, the newborn will become hypertonic with backward arching of the neck and trunk. • High-pitched cry • Fever Laboratory tests • An elevated serum bilirubin level may occur (direct and indirect bilirubin). Monitor the newborn’s bilirubin levels every 4 hr until the level returns to normal. • Assess maternal and newborn blood type to determine whether there is a presence of ABO incompatibility. This occurs if the newborn has blood type A or B, and the mother is type O. • Review Hgb and Hct. • A direct Coombs’ test reveals the presence of antibody-coated (sensitized) Rh-positive RBCs in the newborn. • Check electrolyte levels for dehydration from phototherapy Diagnostic procedures • Transcutaneous bilirubin level is a noninvasive method to measure a newborn’s bilirubin level. Treatment • Phototherapy is the primary treatment for hyperbilirubinemia. It is prescribed if a newborn’s serum bilirubin is greater than 15 mg/dL prior to 48 hr of age, greater than 18 mg/dL prior to 72 hr of age, and greater than 20 mg/dL at any time. Nursing Care • Observe the newborn’s skin and mucous membranes for jaundice. • Monitor the newborn’s vital signs. • Set up phototherapy if prescribed. o Maintain an eye mask over the newborn’s eyes for protection of corneas and retinas. o Keep the newborn undressed with the exception of a male newborn. A surgical mask should be placed (like a bikini) over the genitalia to prevent possible testicular damage from heat and light waves. Be sure to remove the metal strip from the mask to prevent burning. o Avoid applying lotions or ointments to the skin because they absorb heat and can cause burns. o Remove the newborn from phototherapy every 4 hr, and unmask the newborn’s eyes, checking for inflammation or injury. o Reposition the newborn every 2 hr to expose all of the body surfaces to the phototherapy lights and prevent pressure sores. o Check the lamp energy with a photometer per facility protocol. o Turn off the phototherapy lights before drawing blood for testing. • Observe the newborn for effects of phototherapy. o Bronze discoloration – not a serious complication o Maculopapular skin rash – not a serious complication o Development of pressure areas o Dehydration (poor skin turgor, dry mucous membranes, decreased urinary output) o Elevated temperature - Encourage the parents to hold and interact with the newborn when phototherapy lights are off. - Monitor elimination and daily weights, watching for evidence of dehydration. - Check the newborn’s axillary temperature every 4 hr during phototherapy because temperature may become elevated. - Feed the newborn early and frequently – every 3 to 4 hr. This will promote bilirubin excretion in the stools. - Encourage continued breastfeeding of the newborn. Supplementation with formula may be prescribed. - Maintain adequate fluid intake to prevent dehydration. - Reassure the parents that most newborns experience some degree of jaundice. - Explain hyperbilirubinemia, its causes, diagnostic tests, and treatment to parents. - Explain that the newborn’s stool contains some bile that will be loose and green. • Administer an exchange transfusion for newborns who are at risk for kernicterus. • Discharge Instructions o Educate the parents regarding the newborn’s plan of care. [Show More]
Last updated: 3 years ago
Preview 1 out of 47 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
47
Written in
All
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
144