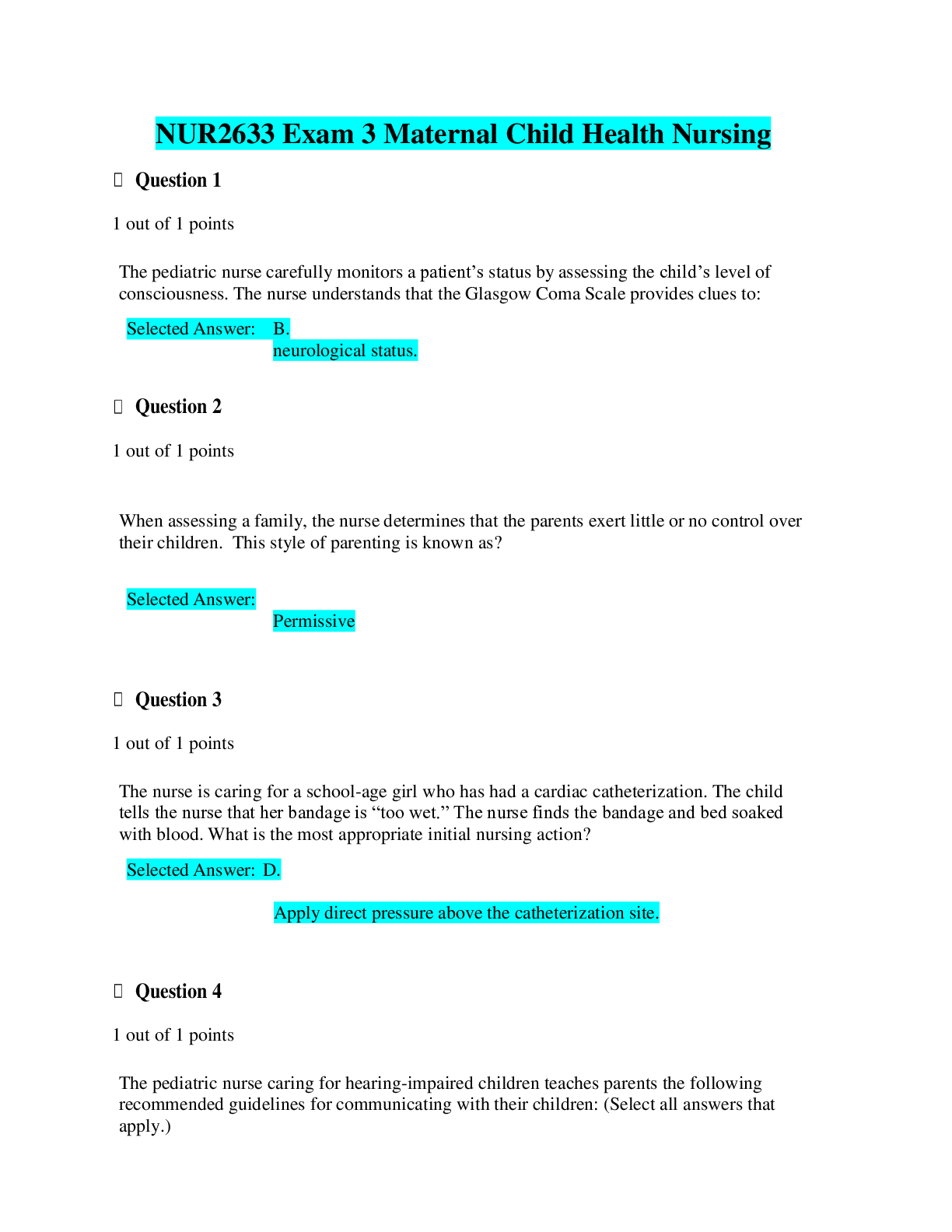
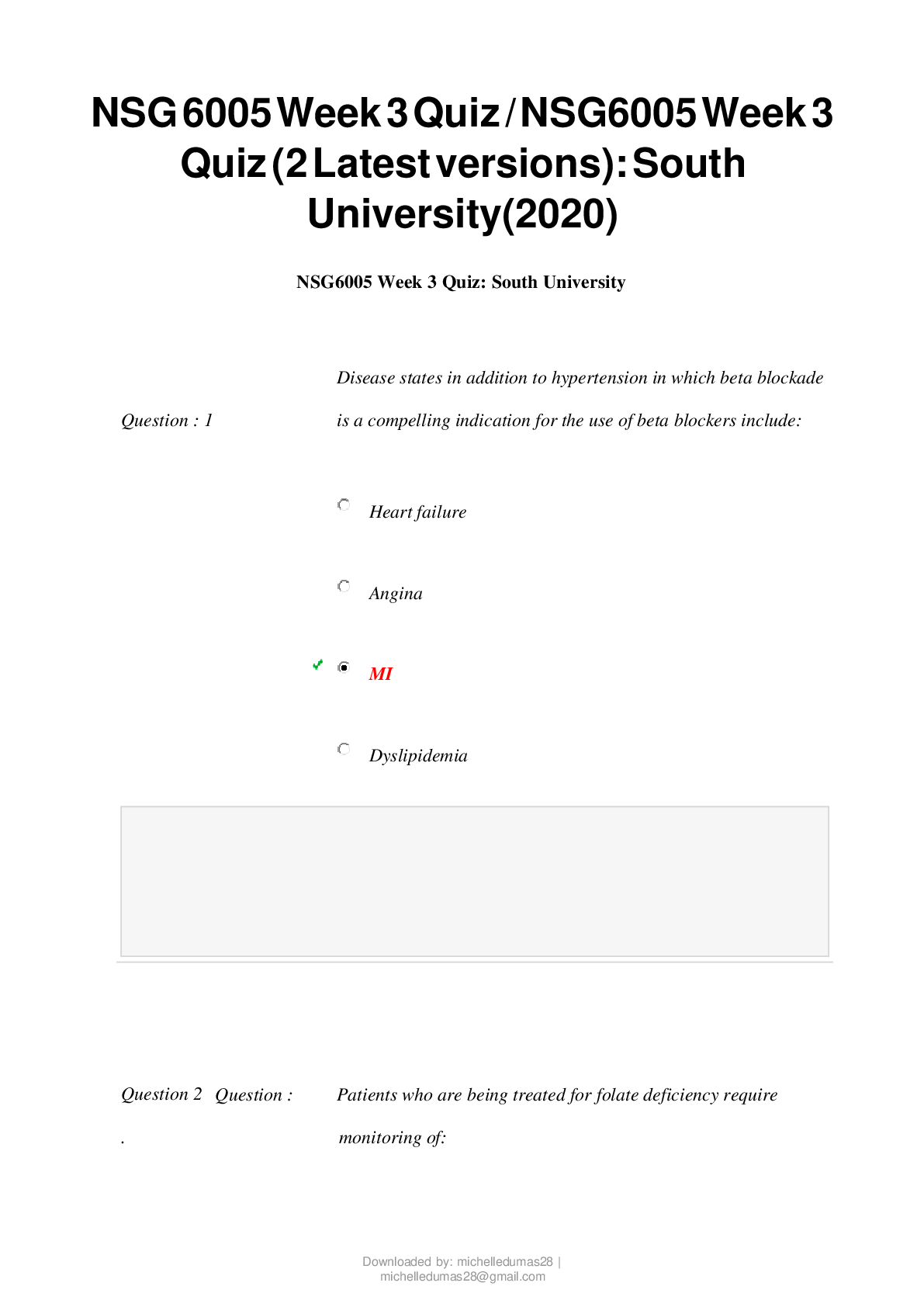
*NURSING > EXAM > NSG 6005 WEEK 3 QUIZ (2 VERSIONS)/ NSG6005 WEEK 3 QUIZ (LATEST): SOUTH UNIVERSITY |100% CORRECT ANSW (All)
NSG 6005 WEEK 3 QUIZ (2 VERSIONS)/ NSG6005 WEEK 3 QUIZ (LATEST): SOUTH UNIVERSITY |100% CORRECT ANSWERS, DOWNLOAD TO SCORE A |
Document Content and Description Below
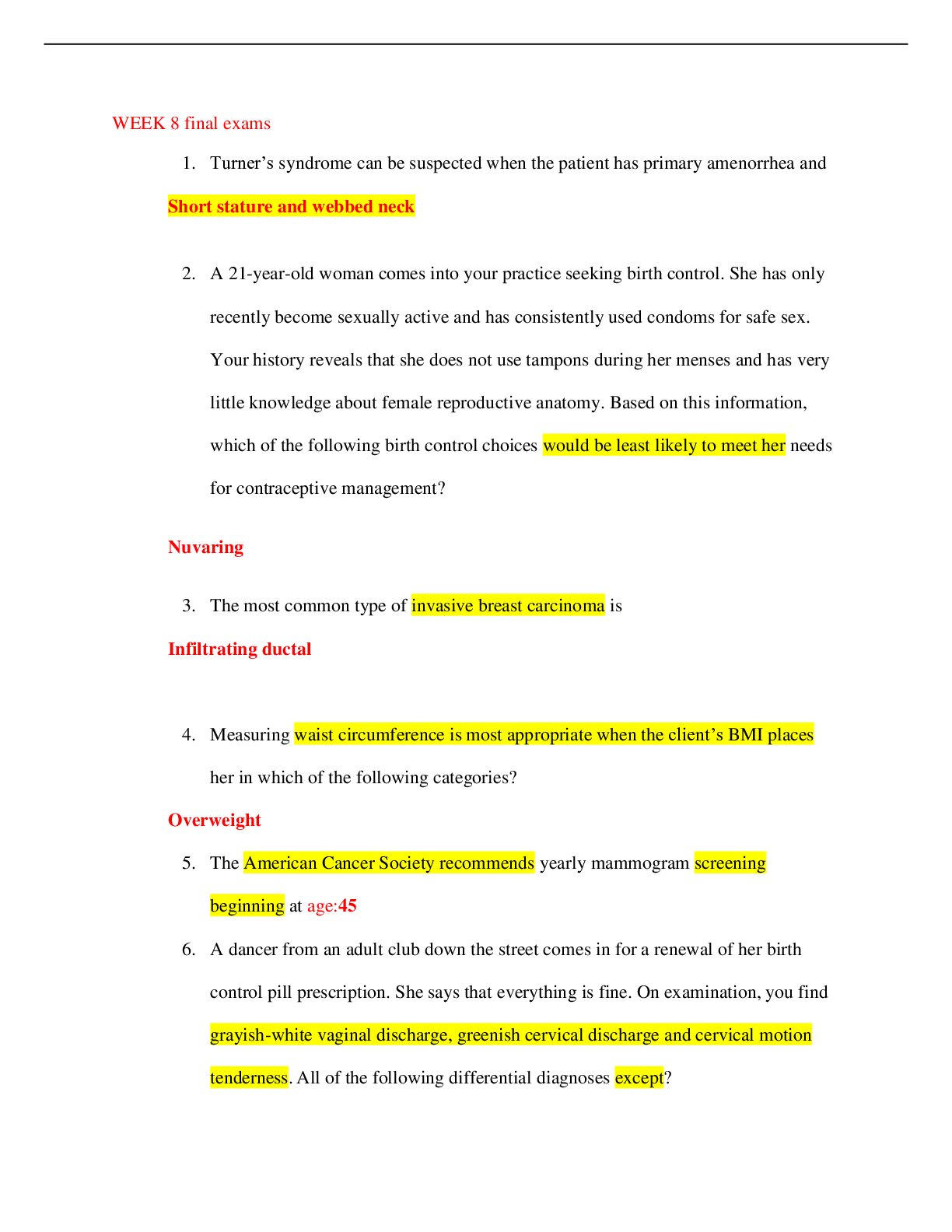
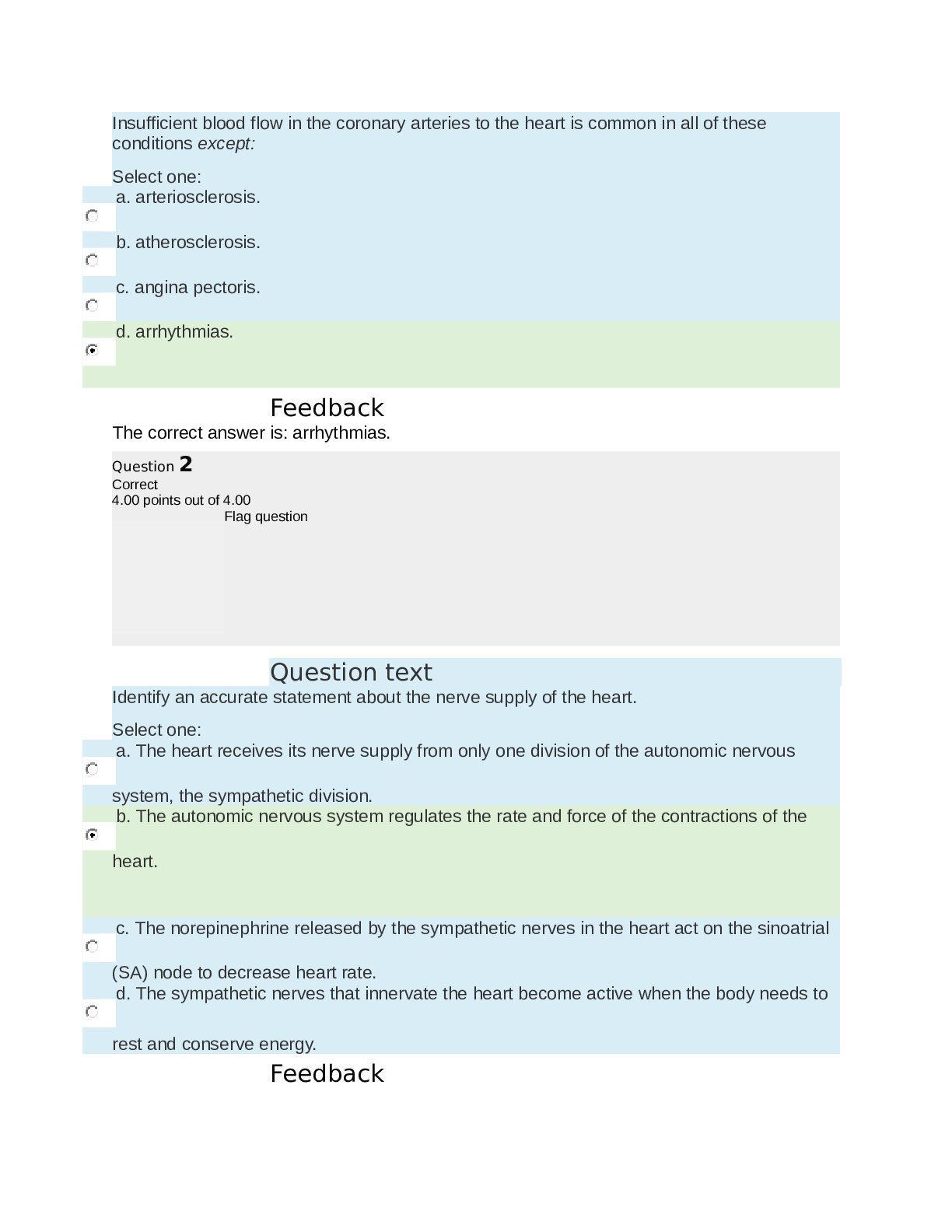
NSG 6005 Week 3 Quiz / NSG6005 Week 3 Quiz (Latest): South University South University NSG 6005 Week 3 Quiz / South University NSG6005 Week 3 Quiz (Latest) Question : 1 Disease states in addition to h ... ypertension in which beta blockade is a compelling indication for the use of beta blockers include: Heart failure Angina MI Dyslipidemia Question 2. Question : Patients who are being treated for folate deficiency require monitoring of: Complete blood count every four weeks Hematocrit and hemoglobin at one week and then at eight weeks Reticulocyte count at one week Folate levels every four weeks until the hemoglobin stabilizes Question 3. Question : A potentially life-threatening adverse response to ACE inhibitors is angioedema. Which of the following statements is true about this adverse response? Swelling of the tongue and hoarseness are the most common symptoms. It appears to be related to a decrease in aldosterone production. The presence of a dry, hacky cough indicates a high risk for this adverse response. Because it takes time to build up a blood level, it occurs after being on the drug for about one week. Question 4. Question : The treatment for vitamin B12 deficiency is: 1,000 mcg daily of oral cobalamin 2 gm/day of oral cobalamin 100 mcg/day vitamin B12 IM 500 mcg/dose nasal cyanocobalamin two sprays once a week Question 5. Question : Scott is presenting for follow-up on his lipid panel. He had elevated total cholesterol, elevated triglycerides, and an LDL of 122 mg/dL. He has already implemented diet changes and increased physical activity. He has mildly elevated liver studies. An appropriate next step for therapy would be: Atorvastatin (Lipitor) Niacin (Niaspan) Simvastatin and ezetimibe (Vytorin) Gemfibrozil (Lopid) Question 6. Question : The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as: Stage A Stage B Stage C Stage D Question 7. Question : ACE inhibitors are the drug of choice in treating hypertension in diabetic patients because they: Improve insulin sensitivity Improve renal hemodynamics Reduce the production of angiotensin II All of the above Question 8. Question : Beta blockers treat hypertension because they: Reduce peripheral resistance. Vasoconstrict coronary arteries. Reduce norepinephrine. Reduce angiotensin II production. Question 9. Question : At which stage/classification of hypertension should drug therapy be instituted according to the JNC-7 Report? Prehypertension Stage 1 Stage 2 Any stage where the blood pressure is greater than 120/80 mm Hg Question 10. Question : Despite good blood pressure control, a nurse practitioner might change a patient’s drug from an ACEI to an ARB because the ARB: Is stronger than the ACEI Does not produce a dry, hacky cough Has no effect on the renal system Reduces sodium and water retention Question 11. Question : Furosemide is added to a treatment regimen for heart failure, which includes digoxin. Monitoring for this combination includes: Hemoglobin Serum potassium Blood urea nitrogen Serum glucose Question 12. Question : Kyle has Crohn’s disease and has a documented folate deficiency. Drug therapy for folate deficiency anemia is: Oral folic acid 1 to 2 mg/day Oral folic acid 1 gm/day IM folate weekly for at least six months Oral folic acid 400 mcg daily Question 13. Question : Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: Symptoms markedly worsen or the patient becomes hypotensive and has syncope. There is evidence of progressive renal insufficiency or failure. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic. All the above options are correct. Question 14. Question : Dulcea has type II diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? Reactive airway disease/asthma Inflammatory bowel disease Allergy to aspirin Gallbladder disease Question 15. Question : An ACE inhibitor and what other class of drug may reduce proteinuria in patients with diabetes better than either drug alone? Beta blockers Diuretics Nondihydropyridine calcium channel blockers Angiotensin II receptor blockers Question 16. Question : Art is a fifty-five-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: “This is a parasympathetic response to the vasodilating effects of the drug.” “Headaches are common side effects with these drugs. How severe are they?” “This is associated with your smoking. Let’s work on having you stop smoking.” “This is not related to your medication. Are you under a lot of stress?” Question 17. Question : Digoxin has a very limited role in the treatment of heart failure. It is used mainly for patients with: Ejection fractions above 40% An audible S3 Mitral stenosis as a primary cause for heart failure Renal insufficiency Question 18. Question : Jose is a twelve-year-old overweight child with a total cholesterol level of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____ with a reevaluation in six months. statins niacin sterols bile acid-binding resins Question 19. Question : In teaching about the use of sublingual nitroglycerine, the patient should be instructed: To swallow the tablet with a full glass of water To place one tablet under the tongue if chest pain occurs and allow it to dissolve To take one tablet every five minutes until the chest pain goes away That it should “burn” when placed under the tongue or it is no longer effective Question 20. Question : Which of the following classes of drugs is contraindicated in heart failure? Nitrates Long-acting dihydropyridines Calcium channel blockers Alpha-beta blockers NSG 6005 Week 3 Quiz / NSG6005 Week 3 Quiz (Latest): South University South University NSG 6005 Week 3 Quiz / South University NSG6005 Week 3 Quiz (Latest) Question1. Question : Jose is a twelve-year-old overweight child with a total cholesterol level of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____ with a reevaluation in six months. statins niacin sterols bile acid-binding resins Question 2. Question : Donald has been diagnosed with hyperlipidemia. On the basis of his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: Become a vegetarian since this disorder is associated with eating red meat Stop taking the drug if abdominal cramps and diarrhea develop Report muscle weakness or tenderness and dark urine to his provider immediately Expect “hot flash” sensations during the first two weeks of therapy Question 3. Question : Patients who have angina, regardless of class, who are also diabetic should be on: Nitrates Beta blockers ACE inhibitors Calcium channel blockers Question 4. Question : Beta blockers treat hypertension because they: Reduce peripheral resistance. Vasoconstrict coronary arteries. Reduce norepinephrine. Reduce angiotensin II production. Question 5. Question : The treatment for vitamin B12 deficiency is: 1,000 mcg daily of oral cobalamin 2 gm/day of oral cobalamin 100 mcg/day vitamin B12 IM 500 mcg/dose nasal cyanocobalamin two sprays once a week Question 6. Question : Isosorbidedinitrate is a long-acting nitrate given twice daily (BID). The schedule for administration is 7 a.m. and 2 p.m. because: Long-acting forms have a higher risk for toxicity. Orthostatic hypotension is a common adverse effect. It must be taken with milk or food. Nitrate tolerance can develop. Question 7. Question : Despite good blood pressure control, a nurse practitioner might change a patient’s drug from an ACEI to an ARB because the ARB: Is stronger than the ACEI Does not produce a dry, hacky cough Has no effect on the renal system Reduces sodium and water retention Question 8. Question : Premature infants require iron supplementation with: 10 mg/day of iron 7 mg/day in diet 1 mg/kg per day until there is adequate intake of iron from foods Question 9. Question : Scott is presenting for follow-up on his lipid panel. He had elevated total cholesterol, elevated triglycerides, and an LDL of 122 mg/dL. He has already implemented diet changes and increased physical activity. He has mildly elevated liver studies. An appropriate next step for therapy would be: Atorvastatin (Lipitor) Niacin (Niaspan) Simvastatin and ezetimibe (Vytorin) Gemfibrozil (Lopid) Question 10. Question : Because primary hypertension has no identifiable cause, treatment is based on interfering with the physiological mechanisms that regulate blood pressure. Thiazide diuretics treat hypertension because they: Increase renin secretion. Decrease the production of aldosterone. Deplete body sodium and reduce fluid volume. Decrease blood viscosity. Question 11. Question : Art is a fifty-five-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: “This is a parasympathetic response to the vasodilating effects of the drug.” “Headaches are common side effects with these drugs. How severe are they?” “This is associated with your smoking. Let’s work on having you stop smoking.” “This is not related to your medication. Are you under a lot of stress?” Question 12. Question : Patients who are being treated for folate deficiency require monitoring of: Complete blood count every four weeks Hematocrit and hemoglobin at one week and then at eight weeks Reticulocyte count at one week Folate levels every four weeks until the hemoglobin stabilizes Question 13. Question : Rodrigo has been prescribed procainamide after an episode of MI. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: Widening of the area of infarction Onset of congestive heart failure An electrolyte imbalance involving potassium Renal dysfunction Question 14. Question : Dulcea has type II diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? Reactive airway disease/asthma Inflammatory bowel disease Allergy to aspirin Gallbladder disease Question 15. Question : Which of the following is true about procainamide and its dosing schedule? It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. GI adverse effects are common, so the drug should be taken with food. Adherence can be improved by using a sustained-release formulation that can be given once daily. Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. Question 16. Question : In teaching about the use of sublingual nitroglycerine, the patient should be instructed: To swallow the tablet with a full glass of water To place one tablet under the tongue if chest pain occurs and allow it to dissolve To take one tablet every five minutes until the chest pain goes away That it should “burn” when placed under the tongue or it is no longer effective Question 17. Question : Treatments for heart failure, including drug therapy, are based on the stages developed by the American Heart Association and the American College of Cardiology. Stage A patients are: Treated with drugs for hypertension and hyperlipidemia, if they exist Taught lifestyle management, including diet, exercise, and smoking cessation only Treated with ACE inhibitors to directly affect the heart failure only Not given any drugs in this early stage Question 18. Question : Phil is a fifty-four-year-old male with multiple risk factors who has been on a high-dose statin for three months to treat his high LDL level. His LDL is 135 mg/dL, and his triglycerides are elevated. A reasonable change in therapy would be to: Discontinue the statin and change to a fibric acid derivative. Discontinue the statin and change to ezetimibe. Continue the statin and add in ezetimibe. Refer him to a specialist in managing patients with recalcitrant hyperlipidemia. [Show More]
Last updated: 3 years ago
Preview 1 out of 27 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
.png)
NSG 6005 WEEK 1 QUIZ TO WEEK 10 QUIZ, NSG 6005 FINAL EXAM (2 VERSIONS), NSG 6005 MIDTERM EXAM (2 VERSIONS), NSG 6005 MIDTERM EXAM AND FINAL EXAM STUDY GUIDE & NSG 6005 EXAM QUESTION BANK (LATEST, 2020): SOUTH UNIVERSITY |100% CORRECT ANSWERS |
NSG 6005 WEEK 1 QUIZ TO WEEK 10 QUIZ, NSG 6005 FINAL EXAM (2 VERSIONS), NSG 6005 MIDTERM EXAM (2 VERSIONS), NSG 6005 MIDTERM EXAM AND FINAL EXAM STUDY GUIDE & NSG 6005 EXAM QUESTION BANK (LATEST, 2020...
By kofee 5 years ago
$96.5
15
Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Dec 13, 2020
Number of pages
27
Written in
All
Additional information
This document has been written for:
Uploaded
Dec 13, 2020
Downloads
0
Views
99