Health Care > AHIP > AHIP test MEDICARE | Already graded answers | 17 pages (All)
AHIP test MEDICARE | Already graded answers | 17 pages
Document Content and Description Below
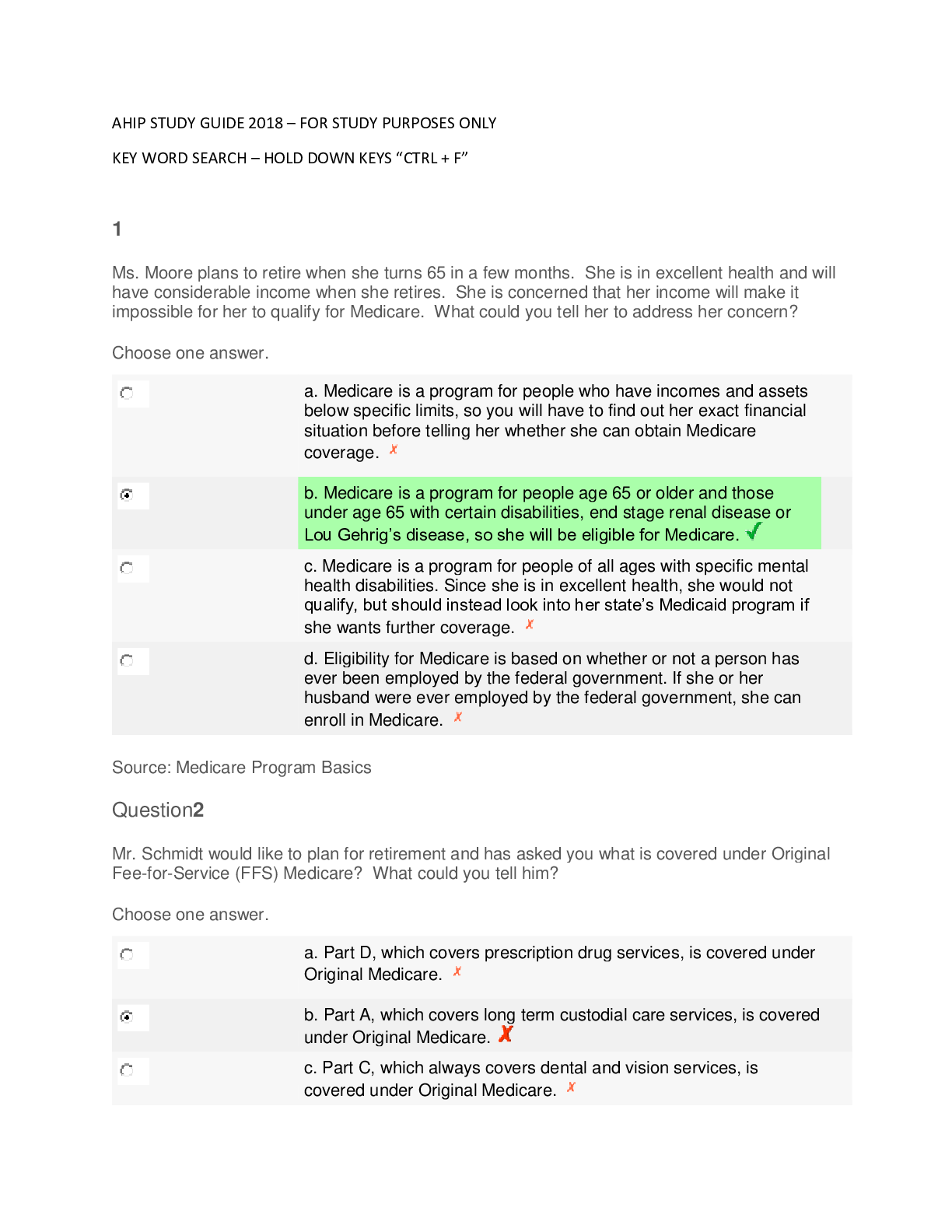
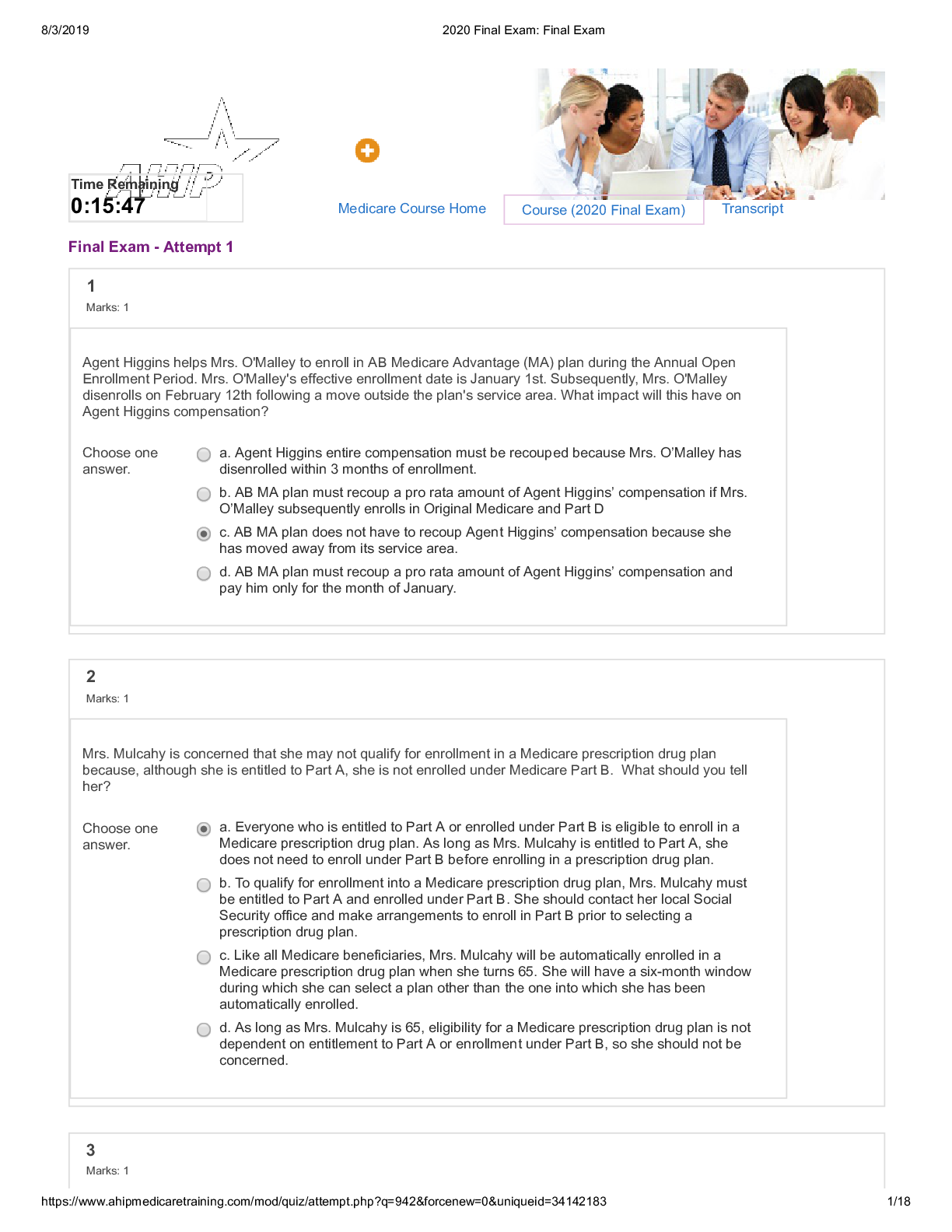
Ms. Gardner is currently enrolled in an MA-PD plan. However, she wants to disenroll from the MA-PD plan and instead enroll in a Part D only plan and go back to Original Medicare. According to Medicar... e's enrollment guidelines, when could she do this? Choose one answer. a. She may make such a change during the Annual Election Period that runs from Oct. 15 to December 7, or during the MA Open Enrollment Period which takes place from January 1- March 31 of each year (beginning in 2019). b. Any time that she is dissatisfied with the plan’s network coverage or customer service she may make such a change. c. She may do it only during the MA Disenrollment Period, which runs from January 1 to February 14 of each year. d. She may only make such a change during her “initial coverage election period,” which occurred when she first became entitled to Medicare. Question2 Mrs. Wu was primarily a homemaker and employed in jobs that provided taxable income only sporadically. Her husband worked full-time throughout his long career. She has heard that to qualify for Medicare Part A she has to have worked and paid Medicare taxes for a sufficient time. What should you tell her? Choose one answer. a. She will have to obtain a job and work enough years to qualify for Medicare Part A. b. Since her husband paid Medicare taxes during the entire time he was working, she will automatically qualify for Medicare Part A without having to pay any premiums. c. Because her husband paid Medicare taxes, and she rarely did, she will have to pay Part A premiums but will do so at a reduced rate. d. She will have to pay the monthly Part A premium in order to obtain the coverage. Question3 Mr. Cole has been a Medicaid beneficiary for some time, and recently qualified for Medicare as well. He is concerned about changes in his cost-sharing. What should you tell him? Choose one answer. a. He should know that Medicaid will pay cost sharing only for services provided by Medicaid participating providers. b. Medicaid will no longer pay any cost sharing once he is eligible for Medicare, so he will need to rely only on Medicare providers. c. For Medicaid beneficiaries, Medicare reduces its cost-sharing amounts to match those charged by the state Medicaid program so there will be no change in his cost-sharing amounts. d. Medicaid will cover his cost-sharing, regardless of from which physician or hospital he receives his Medicare-covered services. [Show More]
Last updated: 2 years ago
Preview 1 out of 17 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Bundle for AHIP tests compilation | everything you need
Bundle for AHIP tests compilation | everything you need
By Dr Medina Reed 2 years ago
$29.5
13
Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 24, 2022
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Aug 24, 2022
Downloads
0
Views
127