*NURSING > HESI > Exit HESI (Actual hesi hints), EXIT HESI 2, Questions and answers, Graded A+ (All)
Exit HESI (Actual hesi hints), EXIT HESI 2, Questions and answers, Graded A+
Document Content and Description Below
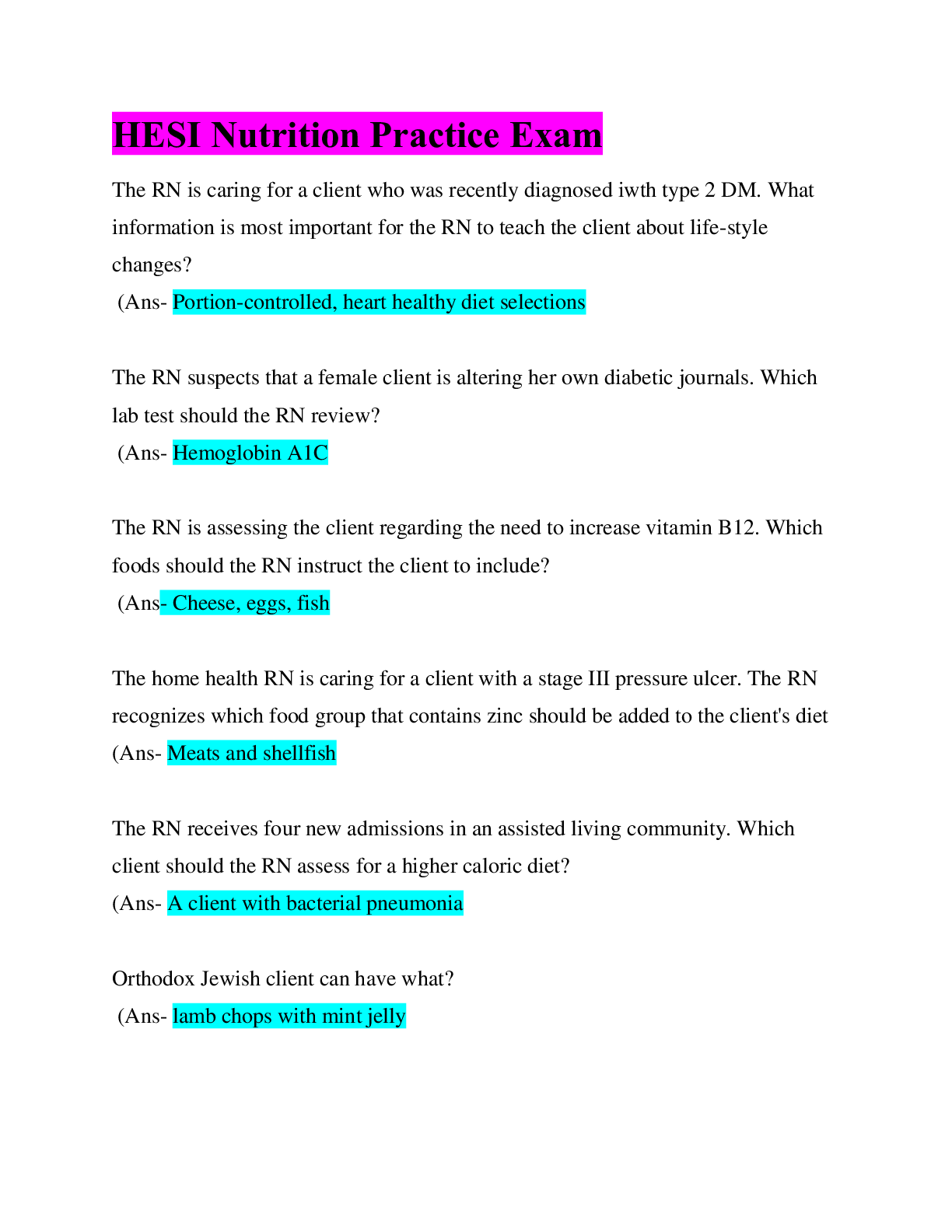
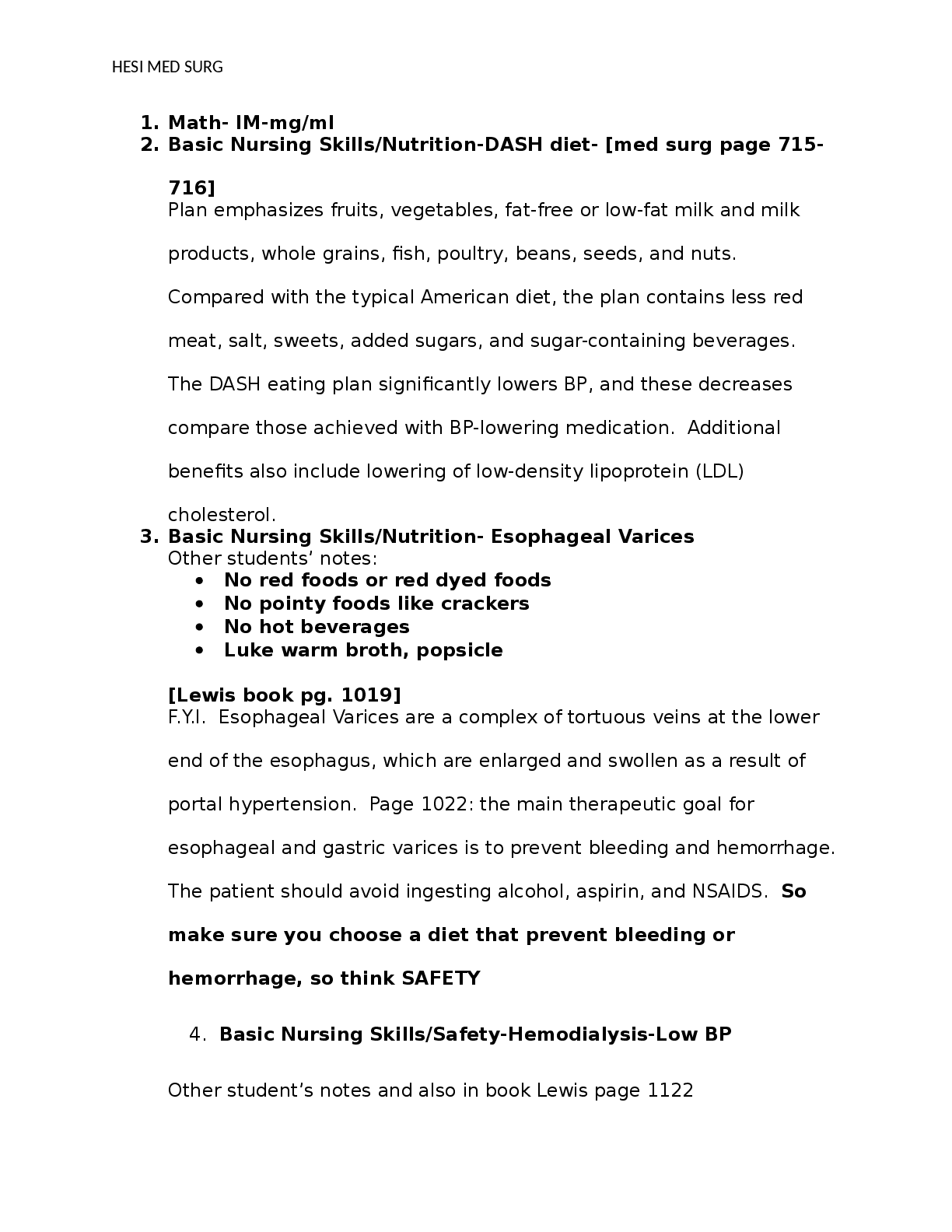
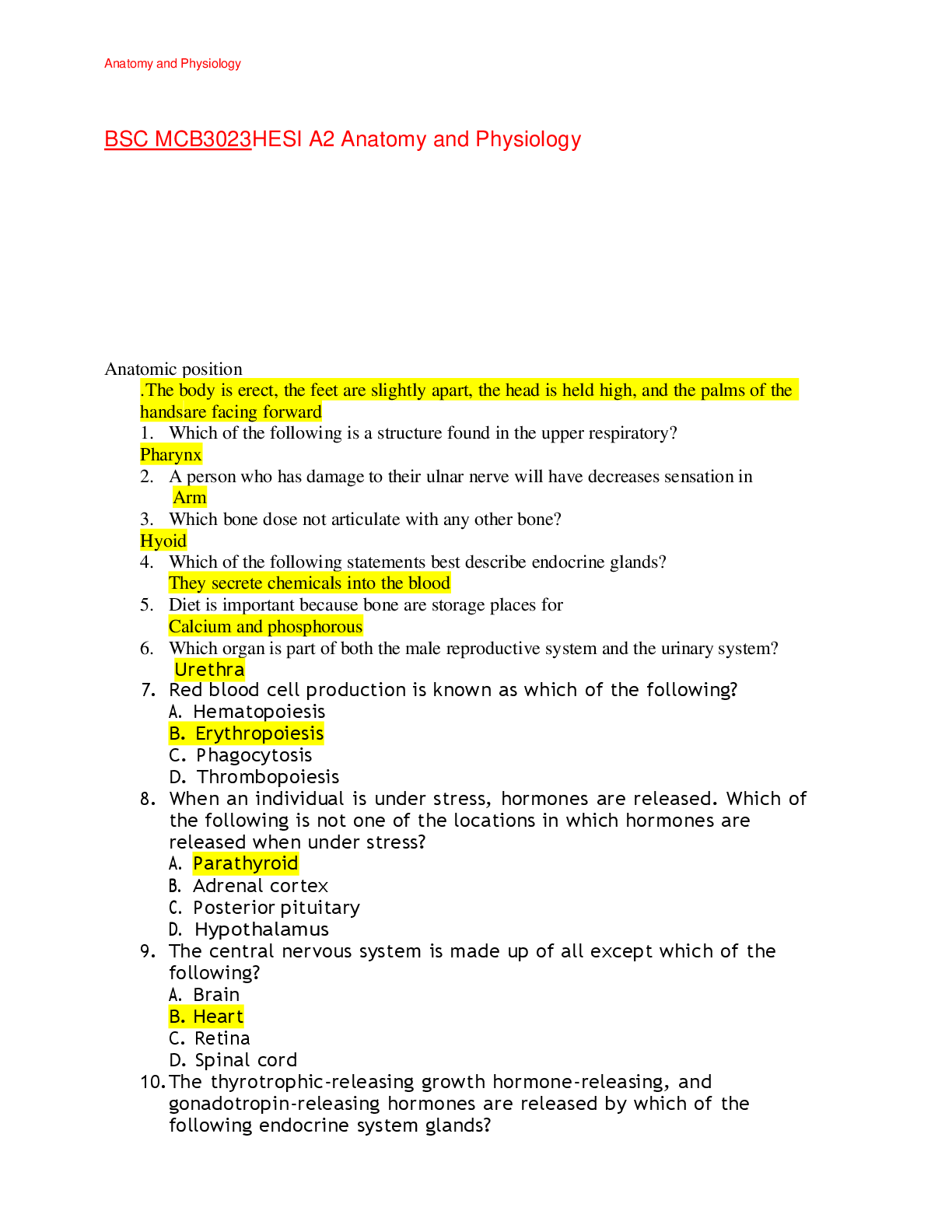
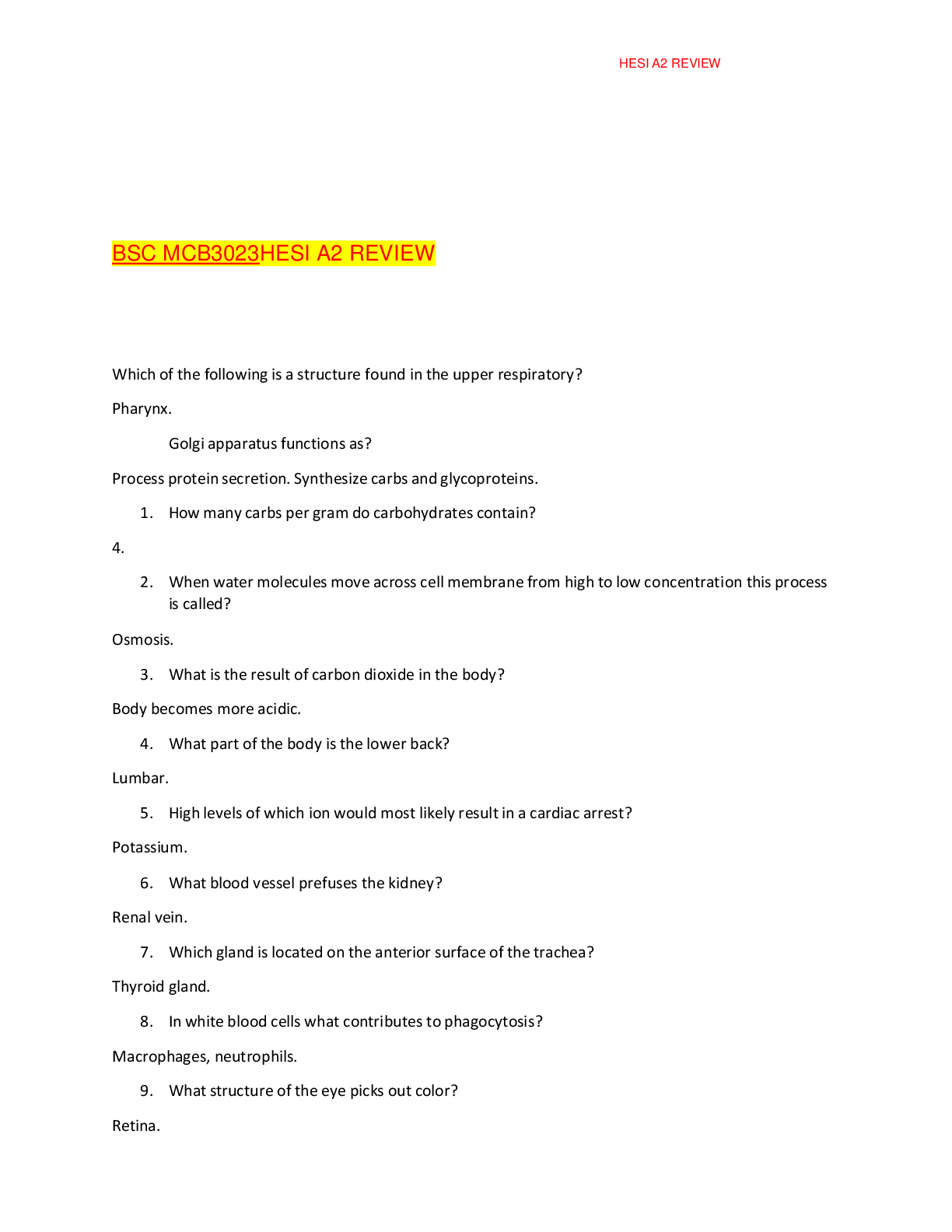
Exit HESI (Actual hesi hints), EXIT HESI 2, Questions and answers, Graded A+ what is considered a postpartum infection? - ✔✔a fever on 2 consecutive days for the first 10 days postpartum not ... including the first day wound infections mastitis endometritis UTIs respiratory tract infections what do you suspect in a child with an irregular pulse? - ✔✔Kawasaki disease what do you screen for on a newborn baby? - ✔✔hypothyroidism check T4 level (decreased) what is an expected side effect of Solu-Medrol? - ✔✔bleeding, bruising what does Pilocarpine treat? - ✔✔glaucoma antidote is atropine sulfate may get a dry mouth TPN - ✔✔central venous catheter check for cloudiness refrigerate- warm before administration monitor electrolytes everyday monitor for hyperglycemia and infection change tubing with each new bag nothing else goes through this line what drug would you give is extravasation has occurred? - ✔✔phentolamine (Regitine)- it's a vasodilator and will increase blood flow to the area to prevent necrosis what diet would be chosen for a pt with CKD? - ✔✔bread & cream of wheat pt receiving a blood transfusion develops fluid volume excess and dyspnea, what do you do? - ✔✔increase O2 what should you be monitoring in a client who has had a nephrectomy? - ✔✔UOP it is more important than drainage what is important when caring for pt in skeletal traction? - ✔✔pin care; sterile technique; remove crust; serous drainage is ok how do you deal with a rude doctor that is avoided by the nurses? - ✔✔staff meeting what is confrontation? - ✔✔calling attention to inconsistent behaviors what is reflecting? - ✔✔paraphrasing or repeating what client said what client would most likely be experiencing delirium? - ✔✔a client with constant pain or insomnia what is the priority for a depressed client who has not slept? - ✔✔sleep a client who is bipolar is going home for the weekend to adjust for discharge. what do you tell the family? - ✔✔continue normal daily activities if a client has a pulse with absent breath sounds on the left side what do you do? - ✔✔prepare to reposition ETT what do you monitor for in adrenal insufficiency (no steroids)? - ✔✔shock hyperkalemia increase sodium in diet if a client suddenly withdraws from steroids what do you do? - ✔✔check VS what do you teach a client taking prednisone? - ✔✔monitor for hyperglycemia take in morning you are caring for a client with AIDS and you accidentally stick yourself with a sterile needle. what do you do? - ✔✔go get a new needle- no need to report what do you teach a pt taking an antipyretic for and increased temp? - ✔✔give with fluids because fever can cause dehydration what is suspected if there is an increase in serosanguineous drainage? - ✔✔dehiscence what would you expect in a client with an epidural hematoma? - ✔✔temporary loss of consciousness, followed by a lucid period, and then gradually leading to coma for maximum effectiveness, what should older clients use for dry skin? - ✔✔petroleum based ointment what are signs of pain in an infant? - ✔✔grimacing tachycardia restlessness irritability difficulty feeding/sleeping increased RR diaphoresis decreased O2 levels what is priority for a client with renal lithiasis? - ✔✔address pain- these pts get pain meds immediately (don't teach important of straining urine- that's RNs job) what do you do for a pt on Amph B? - ✔✔monitor UOP- it's nephrotoxic what is the priority assessment in a client who has lost a tooth and has an eye injury? - ✔✔check pupils where should the level of water be in the water seal chamber? - ✔✔at 2cm where should the level of water be in the suction control chamber? - ✔✔at 20cm how does a client present with DM2? - ✔✔usually come back to doctor for wounds that won't heal or vaginal infections don't have enough insulin insulin doesn't work a client in hypovolemic shock would present with what? - ✔✔weak thready pulse how would you teach someone to use an inhaler? - ✔✔shake well for 5 seconds (if MDI) exhale completely press canister once and inhale deeply and slowly hold breath for 10 seconds wait 1 min between each puff if using MDI- rinse mouth & gargle after each use nebulizers are better for peds and clients with severe asthma because it allows you to breath normally what is the appropriate action for a burn client in the emergent phase whose UOP and BP are dropping? - ✔✔immediately call the HCP what do you monitor for in a client with HHS and DKA with insulin drip? - ✔✔hypokalemia U wave what is priority discharge teaching for a client with HHS? - ✔✔monitor for signs of dehydration what activity would you choose for a person who attempting suicide? - ✔✔punching bag choose most exerting answer what would you teach a client on peritoneal dialysis about self care? - ✔✔warm fluid before administration increase protein and fiber in diet report any fever, abdominal pain that persists after 1-2 weeks, bloody, cloudy, urine colored outflow, outflow that is great than inflow, leakage around catheter site what do you suspect with coffee ground emesis? - ✔✔peptic ulcer stomach cancer what medications do you give with coffee ground emesis? - ✔✔'prazole (proton pump inhibitors) 'tidine (h2 antagonist) antacids mylanta carafate what is the G&D of a toddler? - ✔✔toilet training magical thinkers, egocentrism dramatic, pretend and parallel play learn to behave through restrictions gender identity let child touch and hold equipment walks without help, creeps up stairs, kneels without support builds tower of cubes, holds two cubes in one hand, scribbles, uses cups, but struggles with spoons uses 4-5 words, uses 10 or more words, uses 2-3 phrases points and ask for objects understand simple commands talk all the time tolerates separation from parents temper tantrums are normal dependency on security items (blanket) what is suspected in a pediatric client with croup and how do you treat? - ✔✔retractions & barking cough riding with windows down at night steamy hot showers cool temp therapy nebulized epinephrine, corticosteroids what do you assess for a femoral artery sheath? - ✔✔bleeding and hemorrhage how do you care for a hemiparesis client? - ✔✔ambulate encourage independence with ADL's increase mobility as tolerated what do you teach a client with asthma about taking beta agonists? - ✔✔if administered with theophylline cardiac dysrythmias can occur avoid if taking beta blockers, MAOIs or tricyclic antidepressants observe for chest, jaw, arm pain or palpitations report increase in pulse of 20-30bpm how do you communicate with a client who has had a CVA has developed receptive aphasia? - ✔✔picture board- they can't understand spoken or written words left hemisphere what does tadalafil (Cialis) treat? - ✔✔erectile dysfunction BPH pulmonary HTN what is the side effect of ondansetron (Zofran)? - ✔✔hives, chest tightness, trouble breathing if family refuses to discuss funeral arrangements what do you do? - ✔✔remain with family member without discussing (don't show acceptance of family member's feelings) how do you treat a client with swollen tongue, dry mouth and excessive thirst? - ✔✔IV hypotonic solution 0.2% NaCl 0.45% NaCl D5W what do you teach a client with thrombocytopenia? - ✔✔watch for bleeding gums, hematuria, black stools use electric razor use soft toothbrush no IM injections how do you care for a client with AKI? - ✔✔restrict protein intake monitor for hyperkalemia if there is a staff conflict what do you do? - ✔✔attend client assignments first what is initially used for a co-worker who is abusing narcotics? - ✔✔employee assistance program a client is having a precipitate delivery and you are waiting for the doctor. how do you position the client? - ✔✔lateral sims a client who has a family history of malignant hyperthermia is going in to surgery and receiving general anesthesia. how do you prepare? - ✔✔cooling blanket fluids when are febrile seizures most common? - ✔✔9 months - 5 years old triggered by ear infection or viral illness what is the priority of a client with febrile seizure? - ✔✔bring fever down a client with pancreatic cancer should monitor for what? - ✔✔hypoglycemia with high levels of insulin and c-peptide dizziness, fatigue, uncontrolled shaking, weakness, hunger, history of fainting what do you assess for in a client with a facial injury? - ✔✔violence abuse what is suspected in a pediatric client with diaphoresis? - ✔✔diabetes what interventions do you implement for a client in shock? - ✔✔O2 is priority- place client on high flow oxygen (100% nonrebreather) monitor VS, skin color, temp, cap refill, LOC, UOP, cardio) place flat with legs elevated prepare for intubation maintain patent IV- isotonic fluids what is a PICC used for? - ✔✔chemo blood transfusion antibiotics IV fluids liquid food frequent blood draws what do you teach a person about their PICC line? - ✔✔can go home with- stays in 3 week to months flush once a week use waterproof cover when showering clamp should always be closed when not in use report swelling, redness, pain, discolored fluid at site or fever how do you provide hospice care? - ✔✔talk about what the client wants to talk about listen with compassion focus on creating a peaceful environment touch and facial expression are important use lotion, give back rub, offer cool towel nutrition is less important when body is shutting down- offer liquids and soft foods teach family that this is a normal process how do you care for a pediatric client who is impulsive? - ✔✔distract by redirecting to other activities consequences for bad behavior reward for good behavior what do you assess for in a victim of partner abuse? - ✔✔chronic pain when can a venipuncture be given to a pediatric client? - ✔✔2 years old median cubital, cephalic veins dorsal hand veins basilic vein on pinkie side of arm only used when there is not another more prominent arm vein foot and ankle veins used as last resort Grave's disease treatment - ✔✔-Goal: inhibit production of thyroid hormones and block effect on the body -Radioactive iodine therapy: destroys overactive thyroid cells over time -Propylthiouracil, methimazole -Betablockers -Subtotal or full thyroidectomy (risk of damaging vocal cords and parathyroid glands) Describe Lupus and pt education - ✔✔-*Autoimmune disorder -Could have a decreased WBC count; increased risk for infection -Avoid crowds, avoid sick people, avoid sunlight (trigger) Assessment points for pt with constipation - ✔✔-Assess current medications -Check measures that they're currently taking (daily enemas, laxatives, etc) -Assessment: no bowel sounds, abd distention -Make a doctors appointment -Assess current nutrition, diet, and exercise -Drink more water Osteomalacia and implications for pt teaching - ✔✔-Focus on nutritional support -Sunlight is a good source of vitamin D -Vitamin D is important to absorb calcium and phosphorous -Check vitamin D levels Osteomyelitis - ✔✔-Bone infection -Treat with antibiotics -Poor healing, injury entered the bone UTI - ✔✔-Pt doesn't always report sx! -Urine sample is foul smelling and cloudy -Send sample to lab for urinalysis -Order a secondary test (culture and sensitivity) to choose the correct tx Assessment and nursing interventions for hip fx - ✔✔-Assess for pain -Hip fracture sometimes shortens the leg/rotates it -Treat like its a hip fracture even if no testing done yet -Assess circulation (pulse, cap refill, feeling, movement, wiggle toes, color) -Don't elevate the leg -No extra motion until hip is stabilized -Assess skin and circulation if in traction Care and assessment for adrenalectomy - ✔✔-Pt at risk for electrolyte abnormalities -Put on telemetry -Daily serum electrolytes -Monitor VS -Watch for dysrhythmias Tracheostomy pt teaching - ✔✔-Maintain airway: suctioning -Communicate with white boards -Cough and suction on the way out -No more than 10 seconds Steps of the chain of infection - ✔✔-Causative agent -Reservoir -Portal of exit: ex: wound, dressing change -Mode of transmission: nurse could be mode if they wear a gown in the hallway -Portal of entry -Susceptible host: decreased immune system, also have wounds (entry site) *Ways to block transmission: precautions, wash hands Aseptic handwashing - ✔✔-Wash clean to dirty -Point arms down so dirty water runs from clean to dirty Chrones Diet - ✔✔-Low fat -High-calorie: dried fruit increases calories and nutrients -High nutrient foods -Ex: eggs w/o yolk, lean meat, fish, seafood, chicken Heart Failure Diet - ✔✔-No canned/processed food -No cheese or salami -Limit sodium (fluid retention) -Vegetables and fruits Mormon Diet - ✔✔-No alcohol -No caffeine -Give milk, juice, or water -If diabetic, no juice -Church = latter day saints Enema administration and nursing considerations - ✔✔-Monitor pt for cramping and abd pain -Coach and support pt through this pain -Need to get procedure done, take break, deep breaths, then continue Trapeze bar and considerations - ✔✔-Need upper body strength/upper extremities -Get history from pt: make sure they don't have any problems with dislocated shoulder -Allows more independence and participation with repositioning Manual bladder irrigation and CBI - ✔✔-CBI: 3 way catheter -Check for kinks if not flowing properly -Manually irrigate CBI if there's a clot -If a clot is blocking, the pressure in the bladder could cause leakage around the catheter site AKI assessment - ✔✔-Decreased kidney function because of secondary condition and output decreases -Oliguria: less than 400 cc in 24 hrs -Kidneys aren't producing urine -Possibly can't produce urine sample AKI Interventions - ✔✔-Follow up and look at what drugs they're on -Monitor electrolytes -Monitor weight and edema -Monitor VS: HTN/HypoTN, increased HR -Aggressive fluids: watch for fluid overload, check lung sounds and vitals -Lasix or Mannitol IM Injections - ✔✔-If you stick yourself, fill out appropriate paper work and get pts blood sample -If you think you're in the wrong space, get a larger needle -If you aspirate and get blood return, take out and throw everything away Safety concerns with Parkinson's - ✔✔-Early: falls, decreased mobility, risk for aspiration -Late: wheelchair bound, ulcers, decreased muscle, decreased mobility Distracting Injury - ✔✔-Ex: traumatic amputation, so focused on treating that you don't realize the pt isn't breathing -ABCs -C: know the cause and how to control it 3 Middle ear bones - ✔✔Incus, Maleus (hammer), Stapes Hearing - ✔✔-Maleus (hammer) is first small bone hit from the eardrum vibrations -Sound waves go to tiny hair cells in cochlea and communicate with the brain to perceive sound Stapedectomy - ✔✔-Performed for otosclerosis -Incision behind inner ear, stapes removed and implant inserted -Allows sound and vibrations to pass from eardrum to inner ear fluids Stapedectomy pt teaching - ✔✔-Improvement of hearing isn't immediate, can initially be worse -Hearing improves in 3 weeks, maximum hearing takes 6 months -Dressing on the ear Polycystic Kidney Disease treatments - ✔✔-Need pain relievers -NO NSAIDS (advil, naproxin sodium, motrin) -Can have tylenol Neurogenic Diabetes Insipidus assessment - ✔✔-Very high urine output, very dilute -Monitor sodium *Monitor osmolarity and osmolality: abnormal means its dilute urine -Mostly from trauma to hypothalamus Emphysema treatment - ✔✔-Sit pt up in bed -Pursed lip breathing doesn't make the pt work less -Need to rest...might need bipap Trouble shooting for pulse ox - ✔✔-Warm up the extremity -Change site: nose, toes, earlobes Trouble shooting for BP machine - ✔✔-Get a different machine! Herpes Zoster - ✔✔-Rash along the nerves of the side of the body (usually one side) -Very painful Herpes Zoster treatment - ✔✔-Try to stop the replication of the virus; can still have symptoms -Pain meds throughout: narcotics Wernicke's syndrome - ✔✔-Common in alcoholics -Sx: confusion, memory loss, ataxia, nystagmus, ptosis, abnormal gait Degenerative Joint Disease - ✔✔-Assess kidney function before giving pain meds -Assess pain -Pain meds: NSAIDS (motrin, aspirin, naproxin sodium) are better for inflammation -Nonpharmacological measures: ice, rest, warm compresses Assessing radial and pedal pulses - ✔✔-If you can't find a pulse, use doppler ultrasound; keep looking! -Don't take pulse at same time as BP -Compare pulses bilaterally Influences on blood sugar levels - ✔✔-Illness/infection: check glucose more frequently -Check sugar levels before/after meals and at night -Exercise can decrease sugar: monitor before Palliative care patient care - ✔✔-Goal: improve quality of life, caring not curing -Still treat symptoms like pain/whatever impacts QOL -Still take meds for managing problems Herniated disc - ✔✔-Thorough pain assessment -Assess quality of pain -Radiating pain and numbness bc the bulge is pressing on nerves Teaching points for multiple sclerosis - ✔✔-Need more rest periods -They will have periods of exacerbation -Be aware of triggers: infection, trauma, immunization, childbirth, stress, change in climate Neuropathic pain - ✔✔-Numbing, burning, shooting, stabbing, sharp pain -Caused by trauma, inflammation, infection (herpes zoster, HIV), diabetes -Get a good pain assessment Treatment for anaphylaxis - ✔✔-Need meds! -1st: epinepherine for emergent anaphylaxis; can be given IM, SubQ, IV -Benedryl -H2 blocker to stop histamine release Decorticate posturing - ✔✔-Flexing towards core -3 on GCS -Indicates brain injury Decerebrate posturing - ✔✔-Extension of extremities -2 on GCS (worse than decorticate) -Indicates brain injury DNR - ✔✔-Do not resuscitate -Need a document stating they're DNR, otherwise you're "failing to rescue" -Can't just take family's word for the pts code status Job responsibilities only LPN can do - ✔✔-Take the more stable patients -Insert NG tubes, foleys, IVs -Wound care Job responsibilities only UAP can do - ✔✔-Vitals -Can do home visits to help a pt shower -No dressing changes Hospital emergency response plan in case of an external disaster - ✔✔-Central control center manages care to decrease chaos How the nurse provides continuity of care - ✔✔-Verbal reports -Pt handoff: verbal and continuity of care form -Communication ensures continuity of care Actions of a supervisor when an employer has poor behavior - ✔✔-Talk to employer 1:1 -Document the incident (time, day, exactly what happened) Primary interventions - ✔✔-Aimed to prevent -Immunizations, education (ex: posters around the hospital) Secondary interventions - ✔✔-Reduce a problem that already exists -Screenings Ecoli investigation - ✔✔-Infected from eating/drinking something contaminated with animal/human fecal matter -Look at method of storage -Temperature of storage Normal lymph node characteristics - ✔✔-Pea sized, nontender, movable Concerning lymph node characteristics - ✔✔-Enlarged, tender, nonmovable BMI assessment - ✔✔-Age/sex specific -Assess pts nutrition -Do they have money for food? -Assess activity level -Assess who is providing the pt with food and assess their knowledge of food/educate that person on healthy choices Viral meningitis - ✔✔-Supportive care, rest, fluids -Sx: fever, lethargy -Biggest risk factor: being exposed to other viruses/having other infection -Vaccinations decrease the risk of getting this Congenital adrenal hyperplasia - ✔✔-A healthy baby starts to develop problems: start telemetry -Severe form symptoms: abnormal heart rhythm, change in electrolytes, poor feeding, vomiting, dehydration -Exams: check electrolytes -Treatment: goal is to return hormones to normal/near normal, cortisol, steroids Risk for adrenal crisis - ✔✔-When pt with congenital adrenal hyperplasia becomes symptomatic -Stopping steroid treatment abruptly Von Willebrand's disease signs/symptoms - ✔✔-Sx: recurrent/prolonged nose bleeds, bleeding gums, increased menstrual flow, excessive bleeding from cut, blood in stool/urine Lithium Carbonate - ✔✔-Mood stabilizer, antimanic, antidepressive -For bipolar disorder: affects storage, relsease, and reuptake of neurotransmitters -Adverse reactions/side effects: nausea, fatigue, hand tremors, weight gain, hypothyroid, renal impairment -Toxicity: diarrhea, muscle weakness, unsteady gait, slurred speech -Nursing considerations: maintain adequate serum levels (0.6-1.2), toxicity over 1.5, check renal, cardiac, thyroid levels, Na, do not use with diuretics Displacement - ✔✔-Transference of feelings to another group/object -Ex: after being yelled at by supervisor, person comes home and kicks dog for barking Identification - ✔✔-Attempt to be like someone else -Ex: teenager dresses like favorite singer Intellectualization - ✔✔-Using reason to avoid emotional conflicts -Ex: wife of substance abuser describes the dynamics of enabling behavior yet continues to call her husband's work and report he was missing bc of illness Introjection - ✔✔-Incorporation of values or qualities of an admired person/group into one's own ego -Ex: young man deal with business in same fashion father did Isolation - ✔✔-Separation -Ex: ER nurse is able to care for pts by isolating feelings and emotions r/t pts injuries Passive-aggression - ✔✔-Indirectly expressing aggression toward others -Ex: employee arrives late and disrupts others after being reminded of the meeting earlier that day and promising to be on time Projection - ✔✔-Attributing one's own thoughts or impulses to another person -Ex: sexual feelings toward her teacher tells her friends the teacher is coming onto her Rationalization - ✔✔-Offering an acceptable, logical explanation for unacceptable feelings/behavior -Ex: Student did bad on test and says the course was poorly taught Reaction formation - ✔✔-Conscious attitudes and behaviors that are the opposite of what if really felt -Ex: a person who dislikes animals volunteers for Humane Society Sublimation - ✔✔-Substitution of an acceptable feeling by a more socially acceptable one -Ex: a student who feels to small to play football becomes a marathon swimmer; pt takes unacceptable feelings and takes them out during contact sports Undoing - ✔✔-Communication or behavior done to negate a previously unacceptable act -Ex: young man who used to hunt animals is now on committee for protecting them; mom yells at child then offers to get icecream Teaching for mom breast feeding - ✔✔-If engorged, feed the baby or pump Education early in pregnancy - ✔✔-Assess their support system -Are they homeless? This impacts care -Assess environment, living situation, age, cultural/religious expectations -Are they happy about the pregnancy? Magnesium Sulfate - ✔✔-Pharmacological treatment for preterm labor -Therapeutic level is 4-7.5 -Watch for adverse effects: loss of DTR, resp rate <12, UO <30 ml/hr -Anecdote = calcium gluconate Terbutaline - ✔✔-Causes uterine muscle relaxation -Helps delay birth for hours/days -Increases mom/fetal HR -d/c if HR mom HR is >130 -Notify HCP Biophysical profile - ✔✔-Assessment of the fetus -Failure of stress test indicates you need the biophysical profile -Scores 0-10; 2 points for normal, 0 for abnormal -Low score = increased rate of infant mortality; possible emergent c-section -High score = continued monitoring 5 variables of biophysical profile - ✔✔1. Fetal breathing movements 2. Gross body movements 3. Fetal tone 4. Reactive FHR 5. Qualitative amniotic fluid volume Interventions for low biophysical profile score - ✔✔-<2: labor induction -4: labor induction if >32 weeks; repeat the test the same day if <32 weeks then induce labor if <6 -6: Labor induction if >36 weeks, repeat testing in 24 hrs if <36 weeks -8: labor induction if presence of oligohydramnios (lack of amniotic fluid surrounding fetus) Vaginal laceration care plan considerations - ✔✔-No straining, stool softeners -Ice packs to minimize edema -Sitz baths -Stitches Apgar scale - ✔✔-Performed at 1 min and 5 min -7-10 is good -4-6 needs moderate resuscitative efforts -0-3 is severe need for resuscitation -5 Components: heart rate, resp effort, muscle tone, reflex irritability, color Apgar score for Heart Rate - ✔✔0 = absent 1 = <100 2 = >100 Apgar score for resp effort - ✔✔0 = no cry 1 = weak cry 2 = vigorous cry Apgar score for muscle tone - ✔✔0 = flaccid 1 = some flexion 2 = total flexion Apgar score for reflex irritability - ✔✔0 = no response to foot tap 1 = slight response (grimace) 2 = quick foot removal Apgar score for color - ✔✔0 = dusky/cyanotic 1 = acrocyanotic 2 = pink Assessment of postpartum pt - ✔✔-Massage the fundus -Soft or boggy = concern, massage -If fundus is off to the side, empty bladder -Fundus should be midline -Assess blood: saturating a pad in an hour is too much Prednisone - ✔✔-Class: Adrenal corticosteroid -Inhibits accumulation of inflammatory cells at inflammation site -Prevents/suppresses immune reactions -Frequent side effects: puffy round face, insomnia, nervousness, mood swings, increased appetite, delayed wound healing, increased susceptibility to infection -Adverse effects: muscle wasting, cushings syndrome, rebound inflammation, abrupt withdrawal, could be fatal -Nursing implications: watch for mania, monitor BP, serum electrolytes, glucose, bone mineral density test, ht/wt in children, increased risk for candida, be alert to infection, avoid alcohol, minimize use of caffeine Diphenhydramine (Benedryl) - ✔✔-Class: antihistamine -Indications/Action: decreases inflammatory reaction associated with allergy, decreases urticaria -Adverse reactions/side effects: dry mouth, may have paradoxical effect in children (euphoria, agitation), may cause drowsiness, confusion, dizziness, watch for CNS depression with overdose -Nursing implications: avoid alcohol, safety considerations associated with drowsiness, dizziness Orlistat (Xenical, Alli) - ✔✔-Class: obesity management agent, gastric/pancreatic lipase inhibitor) -Indications/Action: inhibits absorption of dietary fats, may improve weight loss -Adverse reactions: headache, flatulence, abd discomfort, fatty stool, fecal urgency -Nursing implications: for use with reduced calorie diet, fat soluble vitamins should be taken at least two hours apart from med to allow for absorption, administer during or up to 1 hr after meal containing fat Ezetimibe (Zetia) - ✔✔-Class: antihyperlipidemic -Indications/Actions: reduces serum cholesterol, inhibits cholesterol absorption in small intestine -Adverse reactions: may increase liver enzyme, hepatitis, arthralgia, rhabdomyolysis -Nursing implications: don't use with pt with liver disease/damage, get baseline hepatic function labs, monitor cholesterol, report muscle/bone pain Ramelteon (Rozeram) - ✔✔-Class: hypnotic, melatonin receptor agonist -Indications/action: prevents insomnia, characterized with difficulty falling asleep -Adverse reactions: may cause sleepwalking, sleepcooking, sleepeating (somnambulism), may decrease testosterone, increase prolactin -Nursing implications: don't use with alcohol, take 30 min before bed, provide restful and quiet environment Linezolid (Zyvox) - ✔✔-Class: antibiotic -Indications/actions: treatment of nosocomial infections, VRI -Adverse reactions: thrombocytopenia, myelodepression -Other superinfections: watch for severe watery diarrhea (may result from altered bacterial balance in gut) -Nursing implications: monitor bowel consistency, GI effects, monitor CBC, platelets, hgb, electrolytes, monitor for superinfections, avoid tyramine containing foods/alcohol Sulcrafate (Carafate) - ✔✔-Class: antiulcer -Indications/action: protective agent in stomach, forms adhesive barrio on mucosa in stomach/duodenum, treatment of ulcer, ulcer prevention -Adverse reactions: constipation, can make bezoars -Nursing implications: take 1 hr before meals and before bedtime Mesalamine (5-aminosalicylic acid) - ✔✔-Class: antiinflammatory, salicylic acid derivative -Indications: blocks prostaglandins, diminishes inflammation in colon, used for tx of ulcerative colities, sigmoiditis, and proctitis -Adverse reaction/side effects: abd cramping, flatulence, alopecia (rare) -D/c if rash, fever, abd pain -Nursing implications: encourage fluids, monitor bowel activity, assess for GI disturbances, may turn urine yellow/brown Penicillin G Potassium - ✔✔-Class: antibiotic -Indications/action: treatment of infections, including sepsis, meningitis, endocarditis, pneumonia -Adverse reactions/side effects: electrolyte imbalances, may increase liver enzymes, risk for seizures (rare) -Nursing implications: monitor I&O, use caution in renal/hepatic impairment, hypersensitivity to cephalosporins, seizure disorder Colorectal cancer - Surgical Care and care of Colostomy - ✔✔Monitor vital signs, stoma, Q 4 hours Should be Beefy Red (normal) Dusky appearance (necrotic) Small amount of bleeding is normal NG suctioning until bowel sounds are present No lifting greater than 10 lbs or pulling for 6 weeks wash with mild soap, warm H20, pat dry do not wash off markings KNOW! Low fat, high fiber cruciferous diet (Brussel Sprouts, cauliflower, broccoli, cabbage ) Osteoporosis plan of care - ✔✔RISK IS LOW CALCIUM INTAKE Watch for stairs, waxed floor, rugs, medicate for pain High Protein, High calcium, High iron diet Weight bearing and strengthening exercises fall prevention: Non-skid socks encourage activity of D.L. Side rails in bathrooms Ectopic Pregnancy - ✔✔HCG Elevation Transvaginal ultrasound unilateral or bilateral abd. pain medical emergency Burn Neck Contractures - ✔✔Neck stabilized and aligned Airway management Splinting, neck collars Pedicuosis (head lice) - ✔✔Direct contact No sharing personal items Nits (whitish sacs) Keeping staff separate SCHOOL NURSE - send note home to parents Date Rape - ✔✔Ask if consensual - had any conceptual sex recently DKA Labs - ✔✔ANION GAP Metabolic Acidosis - PH < 7.15 [Show More]
Last updated: 3 years ago
Preview 1 out of 72 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 27, 2022
Number of pages
72
Written in
All
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Aug 27, 2022
Downloads
0
Views
168