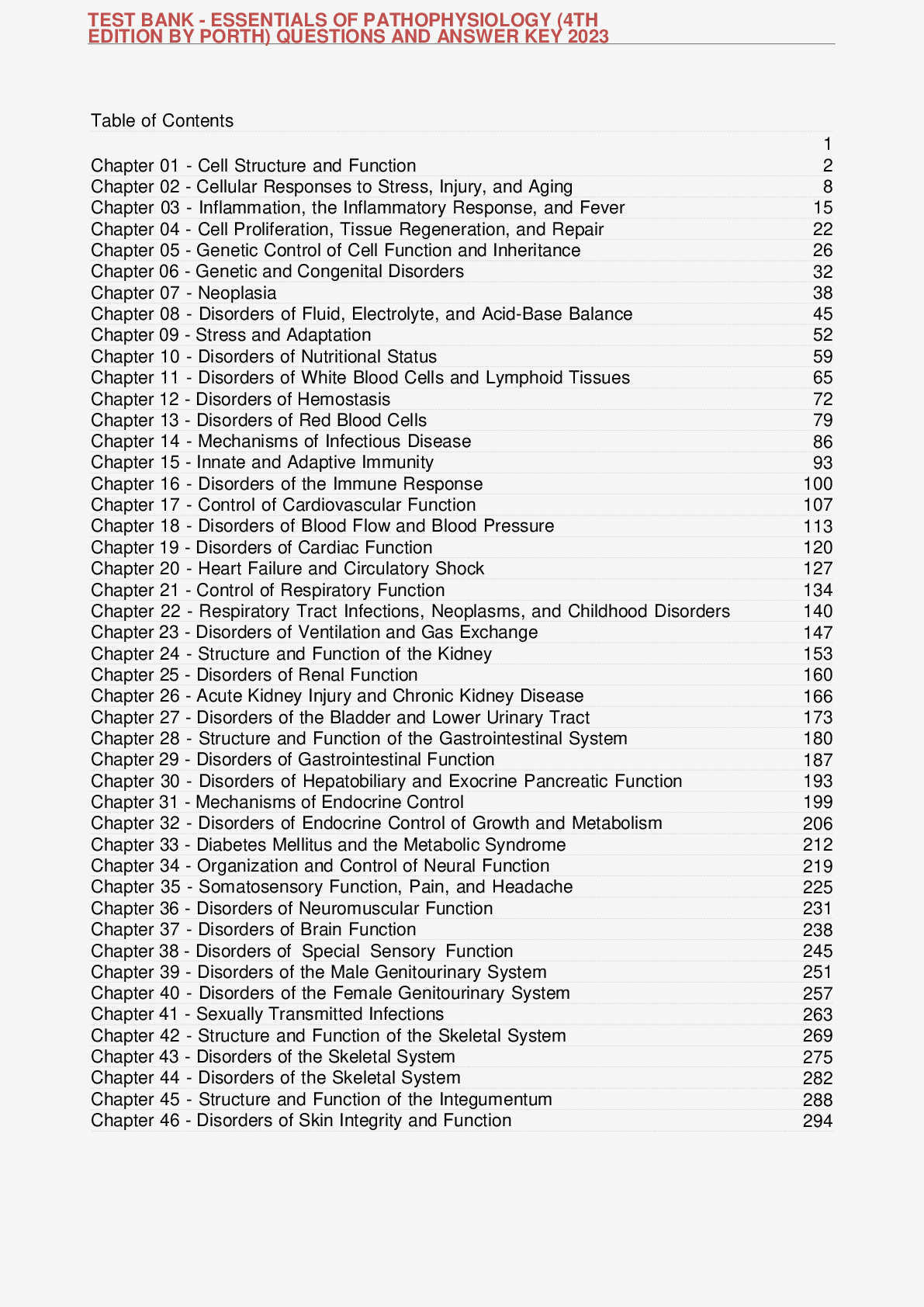
TEST BANK - ESSENTIALS OF PATHOPHYSIOLOGY (4TH EDITION BY PORTH) QUESTIONS AND ANSWER KEY 2023
$ 13

PROPHECY EKG 2022
$ 12
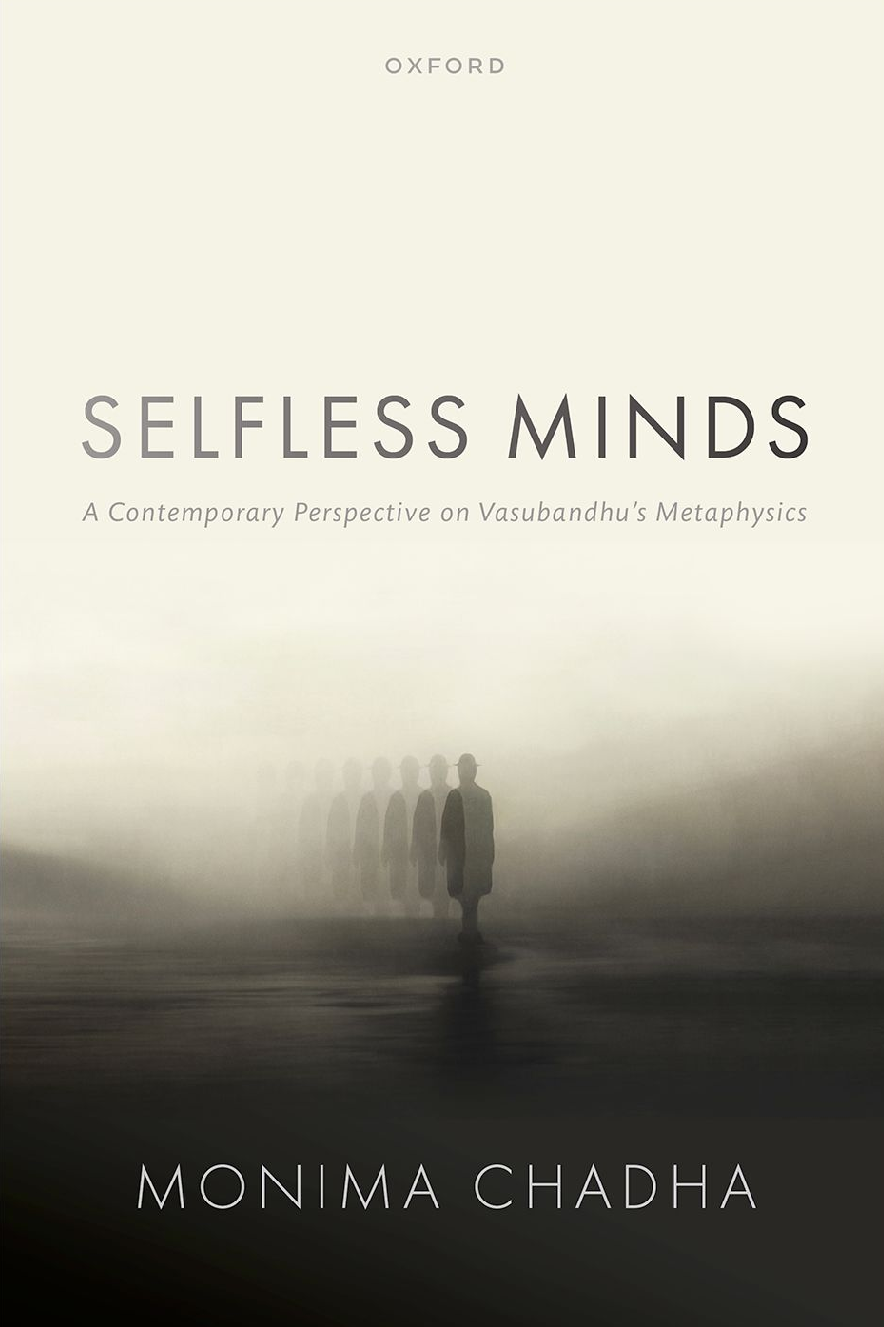
eBook Selfless Minds, A Contemporary Perspective on Vasubandhu's Metaphysics 1st edition by Monima Chadha
$ 30
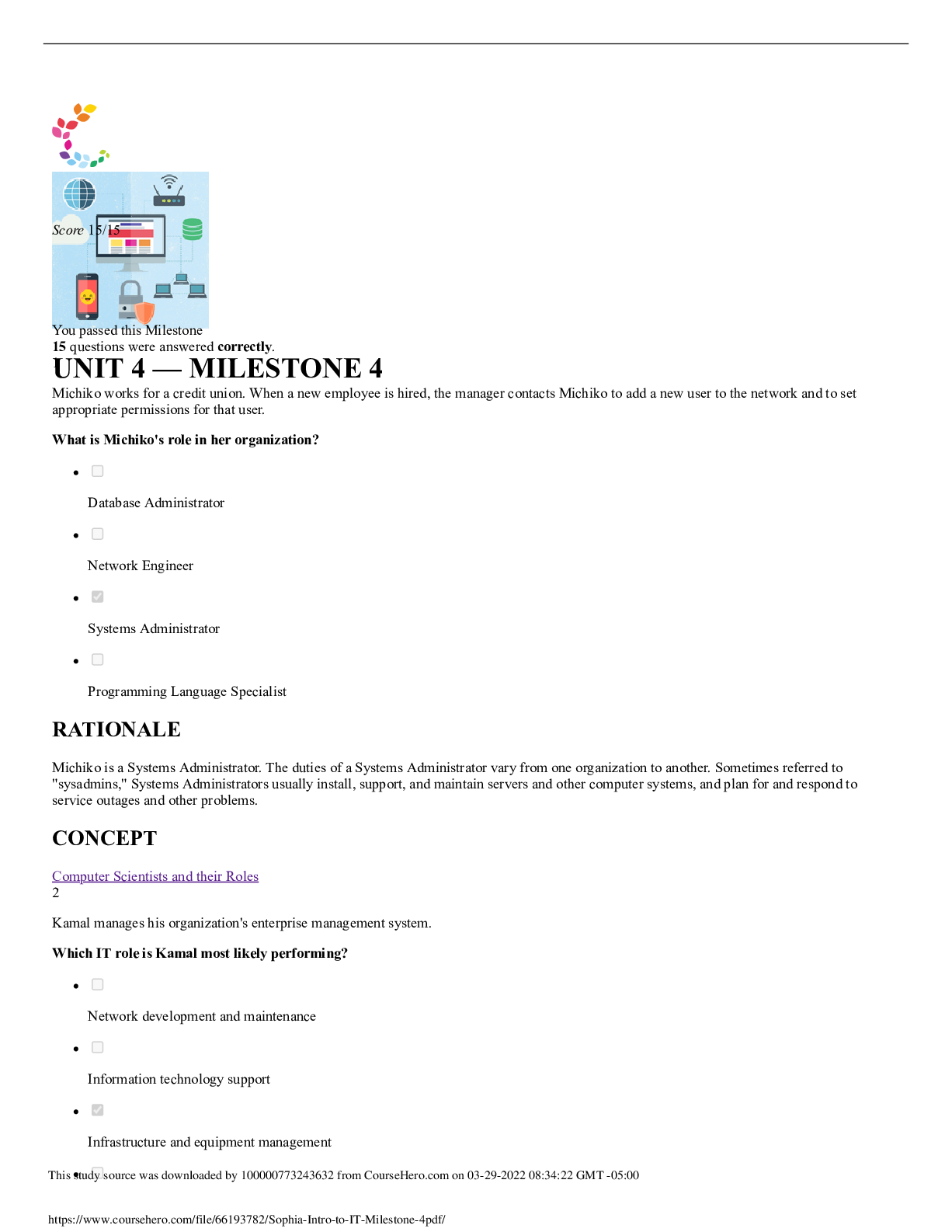
IT 100 Intro to IT Sophia UNIT 4 Milestone 4. Score 15/15
$ 10.5
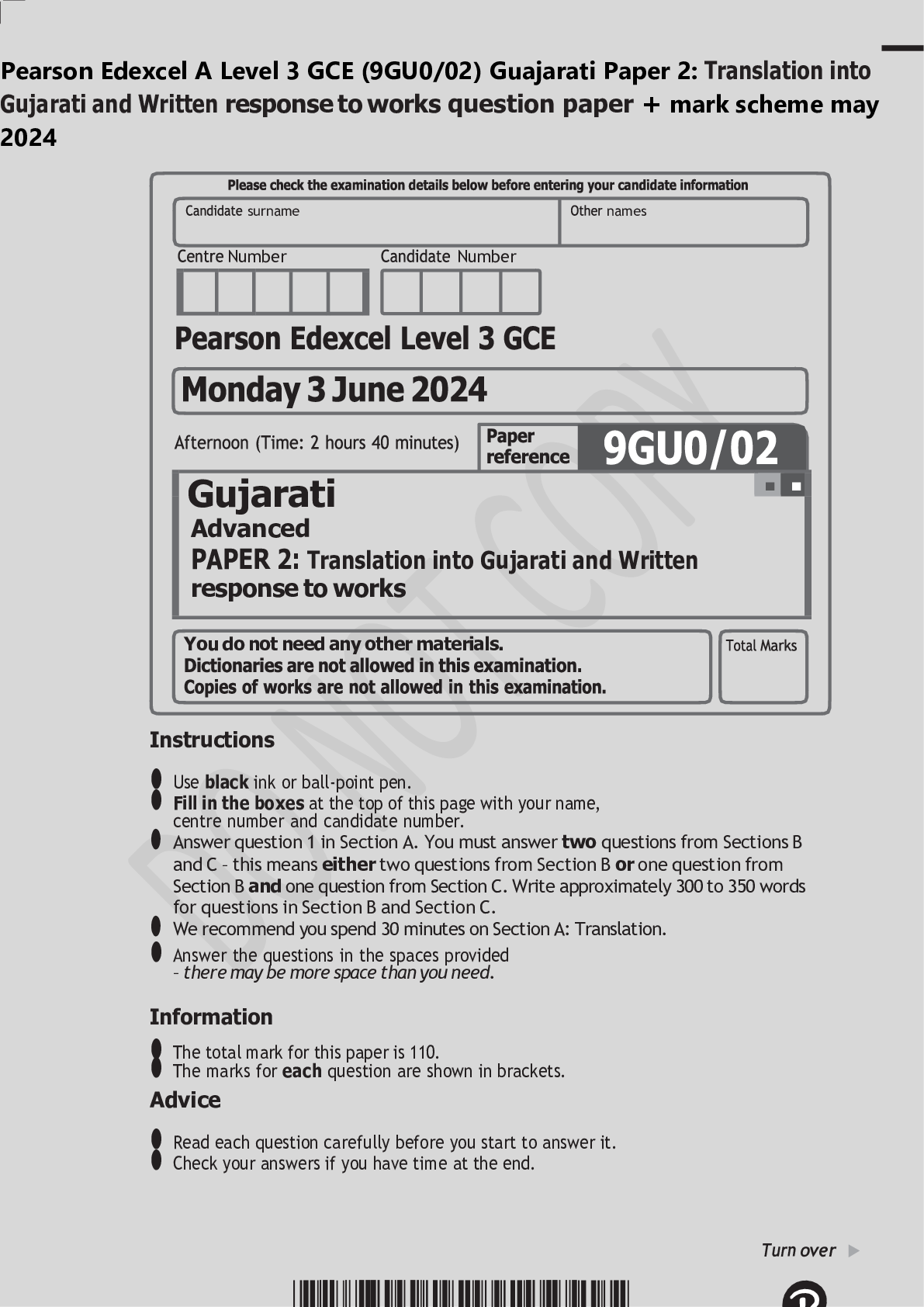
Pearson Edexcel A Level 3 GCE (9GU0/02) Guajarati Paper 2: Translation into Gujarati and Written response to works question paper + mark scheme may 2024
$ 6

Ohio Notary Test Questions and answers, Rated A. 2022 version
$ 5
eBook [PDF] Manufacturing Strategies and Systems: Technologies, Processes, and Machine Tools 1st Edition | Print ISBN: 9781032715414 and 1032715413 and eText ISBN: 9781040303115 and 1040303110 | by Ajay Kumar | Published by CRC Press in 2025
$ 36.5
 Graded A.png)
SCIENCE 101_ CARBON CYCLE GIZMO (Complete Questions and Full Answers to Questions from Activities A, B, and C) Graded A
$ 15
[eTextBook] (EPUB) [PDF] (ISE) Essential Statistics 3rd Edition By William Navidi, Barry Monk
$ 29
Elementary Statistics A Step By Step Approach, 10th Edition By Allan Bluman [eBook][PDF]
$ 19

Sophia Statistics Fundamentals Unit 5 Milestone
$ 18.5

2022 Rules Quiz Questions and Answers
$ 14
.png)
PMP Certification Questions and Answers Latest 2022 A+ Work (Recommended)
$ 11
eBook BDS/GPS Dual-Mode Software Receiver 1st Edition By Yu Lu
$ 29

GIZMOs - Student Exploration: Radiation - ANSWER KEY
$ 7
Information Systems, Organizations, and Strategy
$ 2
IHUMAN CASE STUDY KASEY GAINES GASTROINTESTINAL CONDITIONS 2024-25 QUESTIONS AND ANSWERS
$ 17
TEST BANK For Berne and Levy Physiology 8th Edition by Koeppen & Stanton, Verified Chapters 1 - 44, Complete Newest Version
$ 13
eBook Introduction to the New Statistics 1st Edition By Geoff Cumming,Robert Calin-Jageman
$ 25
PATHO 370 Test 1 (QUESTIONS AND CORRECT SOLUTIONS) ASSURED GRADE A SCORE
$ 10.5
APEA 3P Predictor Exam 2025 Test Questions with Answers and Rationales
$ 12
ATI Predictor Comprehensive Assessment 2019 A