*NURSING > QUESTIONS & ANSWERS > MATERNITY QUESTIONS AND ANSWERS, 2022/2023. GRADED A+. (All)
MATERNITY QUESTIONS AND ANSWERS, 2022/2023. GRADED A+.
Document Content and Description Below
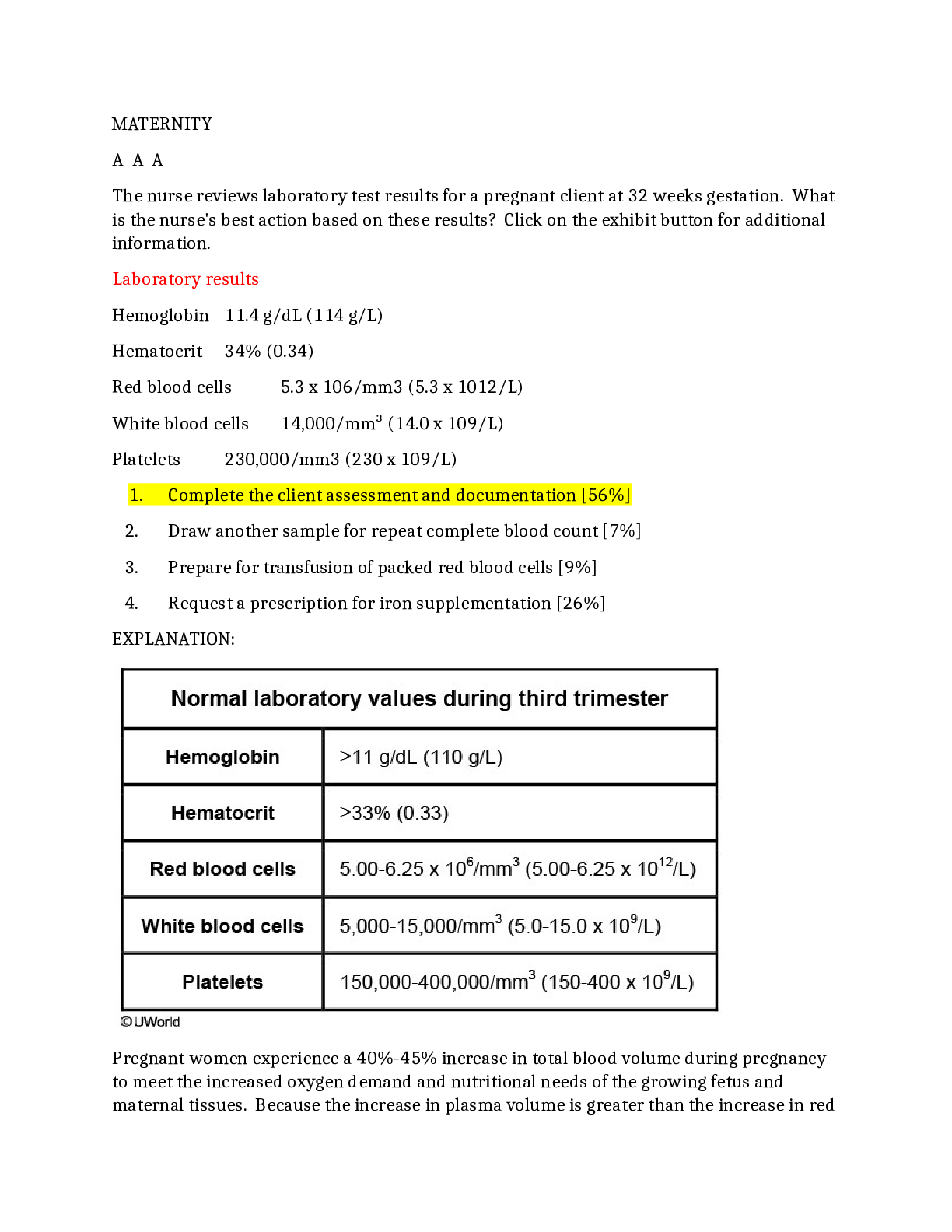
MATERNITY A A A The nurse reviews laboratory test results for a pregnant client at 32 weeks gestation. What is the nurse's best action based on these results? Click on the exhibit button for additi ... onal information. Laboratory results Hemoglobin 11.4 g/dL (114 g/L) Hematocrit 34% (0.34) Red blood cells 5.3 x 106/mm3 (5.3 x 1012/L) White blood cells 14,000/mm³ (14.0 x 109/L) Platelets 230,000/mm3 (230 x 109/L) 1. Complete the client assessment and documentation [56%] 2. Draw another sample for repeat complete blood count [7%] 3. Prepare for transfusion of packed red blood cells [9%] 4. Request a prescription for iron supplementation [26%] EXPLANATION: Pregnant women experience a 40%-45% increase in total blood volume during pregnancy to meet the increased oxygen demand and nutritional needs of the growing fetus and maternal tissues. Because the increase in plasma volume is greater than the increase in redblood cells, a hemodiluted state called physiologic anemia of pregnancy occurs, and is reflected in lower hemoglobin and hematocrit values. It is also normal for the white blood cell count to increase during pregnancy; counts can be as high as 15,000/mm3 (15.0 x 109/L). These laboratory results are within the normal ranges for a pregnant client in the third trimester, and no intervention is required (Options 1 and 2). (Option 3) A blood transfusion should not be considered in pregnancy unless severe anemia (hemoglobin <7.0 g/dL [<70 g/L]) is suspected. (Option 4) Iron is frequently prescribed for pregnant women to prevent or treat iron deficiency anemia (hemoglobin ≤11 g/dL [110 g/L] and hematocrit ≤33% [0.33]). However, this pregnant client's laboratory results are within normal ranges, and iron supplementation is not necessary. Educational objective: Pregnant women experience an increase in total blood volume to meet the increased oxygen demand and nutritional needs of the growing fetus and maternal tissues. The increase in plasma volume is greater than the increase in red blood cells, creating a hemodiluted state termed physiologic anemia of pregnancy, which is reflected in decreased hemoglobin (>11.0 g/dL [>110 g/L]) and hematocrit (>33% [0.33]) values. A A A The nurse is preparing a nutritional teaching plan for a client planning to become pregnant. Which foods would best prevent neural tube defects? 1. Calcium-rich snacks [7%] 2. Fortified cereals [68%] 3. Organ meats [16%] 4. Wild salmon [7%] Explanation: Women who are planning on becoming pregnant should consume 400-800 mcg of folic acid daily. Food options that are rich in folic acid include fortified grain products (eg, cereals, bread, pasta) and green, leafy vegetables (Option 2). Inadequate maternal intake of folic acid during the critical first 8 weeks after conception (often before a woman knows she is pregnant) increases the risk of fetal neural tube defects (NTDs), which inhibit proper development of the brain and spinal cord. Common NTDs are spina bifida and anencephaly (lack of cerebral hemispheres and overlying skull). (Option 1) Adequate calcium intake is especially important during the last trimester for mineralization of fetal bones and teeth, but it does not prevent NTDs.(Option 3) Organ meats (eg, liver) may contain moderately high levels of folate but are consumed more for their high iron content, which can promote red blood cell formation and prevent maternal anemia. (Option 4) A prenatal diet rich in omega-3 fatty acids is important for fetal neurologic function and is linked to a lower risk of preterm birth. Dietary sources include wild salmon, anchovies, flaxseed, and walnuts. Educational objective: Women who are planning to become pregnant should consume 400-800 mcg of folic acid daily to prevent neural tube defects (eg, spina bifida, anencephaly). Food options that are rich in folic acid include fortified grain products (eg, cereals, bread, pasta) and green, leafy vegetables. A A A A pregnant client at 30 weeks gestation comes to the prenatal clinic. Which vaccines may be administered safely at this prenatal visit? Select all that apply. 1. Influenza injection 2. Influenza nasal spray 3. Measles, mumps, and rubella 4. Tetanus, diphtheria, and pertussis 5. Varicella Explanation: Health promotion during pregnancy includes the administration or avoidance of certain vaccines to decrease risks to mother and fetus. Pregnant women have suppressed immune systems and are at increased risk for illness and subsequent complications. Some viruses (eg, rubella, varicella) can cause severe birth defects if contracted during pregnancy. Inactivated vaccines contain a "killed" version of the virus and pose no risk of causing illness from the vaccine. Some vaccines contain weakened (ie, attenuated) live virus and pose a slight theoretical risk of contracting the illness from the vaccine. For this reason, women should not receive live virus vaccines during pregnancy or become pregnant within 4 weeks of receiving such a vaccine. The tetanus, diphtheria, and pertussis (Tdap) vaccine is recommended for all pregnant women between the beginning of the 27th and the end of the 36th week of gestation as it provides the newborn with passive immunity against pertussis (whooping cough) (Option 4).During influenza season (October-March), it is safe and recommended for pregnant women to receive the injectable inactivated influenza vaccine regardless of trimester (Option 1). (Options 2, 3, and 5) The influenza nasal spray; measles, mumps, and rubella (MMR) vaccine; and varicella vaccine contain live viruses and are contraindicated in pregnancy. Educational objective: Inactivated vaccines (eg, inactivated influenza; tetanus, diphtheria, and pertussis) may be given during pregnancy to protect pregnant clients from illness and provide the fetus with passive immunity. Live virus vaccines are contraindicated in pregnancy. A A A A client at 39 weeks gestation with preeclampsia has a blood pressure of 170/100 mm Hg, 2+ proteinuria, and moderate peripheral edema. Immediately after hospital admission, she develops seizures and uterine contractions. Magnesium sulfate is prescribed. Which finding indicates that the drug has achieved the desired therapeutic effect? 1. Blood pressure <130/80 mm Hg [24%] 2. Seizure activity stops [55%] 3. Urine has 1+ protein [1%] 4. Uterine contractions stop [18%] Explanation: Preeclampsia is a systemic disease characterized by hypertension and proteinuria after the 20th gestational week with unknown etiology. Eclampsia is the onset of convulsions or seizures that cannot be attributed to other causes in a woman with preeclampsia. Delivery is the only cure for preeclampsia-eclampsia syndrome. Magnesium sulfate is a central nervous system depressant used to prevent/control seizure activity in preeclampsia/eclampsia clients. During administration, the nurse should assess vital signs, intake and output, and monitor for signs of magnesium toxicity (eg, decreased deep-tendon reflexes, respiratory depression, decreased urine output). A therapeutic magnesium level of 4-7 mEq/L (2.0-3.5 mmol/L) is necessary to prevent seizures in a preeclamptic client. (Option 1) Hypertension is a sign of preeclampsia. Hydralazine (Apresoline), methyldopa (Aldomet), or labetalol (Trandate) is used to lower blood pressure (BP) if needed (usually considered when BP is >160/110 mm Hg). (Option 3) Proteinuria is a symptom of preeclampsia. Control of hypertension and delivery will reduce the protein level. Magnesium sulfate is not prescribed to decrease proteinuria.(Option 4) Tocolytic drugs (eg, terbutaline, magnesium sulfate, indomethacin, nifedipine) are used to suppress uterine contractions in preterm labor, allowing pregnancy to be prolonged for 2-7 days so that corticosteroid administration can improve fetal lung maturity. This client is at term, and there is no need to delay delivery. Educational objective: Magnesium sulfate is prescribed for clients with preeclampsia to prevent seizure activity. A therapeutic magnesium level of 4-7 mEq/L (2.0-3.5 mmol/L) is necessary to prevent seizures in a preeclamptic client. A A A A nurse is admitting a client at 42 weeks gestation to the labor and delivery unit for induction of labor. What is a predictor of a successful induction? 1. Bishop score of 10 [54%] 2. Firm and posterior cervix [11%] 3. History of precipitous labor [5%] 4. Reactive nonstress test [28%] Explanation: The Bishop score is a system for the assessment and rating of cervical favorability and readiness for induction of labor. The cervix is scored (0-3) on consistency, position, dilation, effacement, and station of the fetal presenting part. A higher Bishop score indicates an increased likelihood of successful induction that results in vaginal birth. For nulliparous women, a score ≥8 usually indicates that induction will be successful (Option 1). (Option 2) A cervix that is firm and posterior is associated with a low Bishop score, which reflects a low likelihood of successful labor induction. (Option 3) A history of precipitous labor (<3 hours from onset of contractions to birth) may indicate that the client will again experience precipitous labor once labor is established. However, such a history is not an independent predictor of successful induction. (Option 4) A reactive nonstress test indicates that the fetus is well oxygenated and establishes fetal well-being. It does not provide information about the likely success or failure of labor induction. Educational objective: The Bishop score is a system for the assessment and rating of cervical favorability and readiness for induction of labor. A score >8 in nulliparous women is associated with successful induction and subsequent vaginal birth.A A A The nurse is teaching a client, gravida 1 para 0, at 8 weeks gestation about expected weight gain in pregnancy. The client's prepregnancy BMI is 21 kg/m2. Which statement made by the client indicates an understanding about weight gain? 1. "I should gain 10-15 lb (4.5-6.8 kg) during the first trimester." [14%] 2. "I should gain a total of about 30 lb (13.6 kg) during my pregnancy." [65%] 3. "I should gain no more than 0.5 lb (0.2 kg) per week during the third trimester." [17%] 4. "If I gain <20 lb (9.1 kg) during pregnancy, it will be easier to lose weight postpartum." [2%] Explanation BMI (kg/m2): Weight gain <18.5 (underweight) 28-40 LB 18.5-24.9(appropriate weight) 25-35 lb 25-29.9 (overweight) 15-25 lb ≥30 (obese) 11-20 lb Weight gain during pregnancy should be determined by prepregnancy BMI. Underweight clients need to gain more weight (1 lb [0.5 kg]/wk) during the second and third trimesters of pregnancy than do obese clients (0.5 lb [0.2 kg]/wk). However, weight gain in the first trimester should be 1.1-4.4 lb (0.5-2.0 kg) regardless of BMI. With a prepregnancy BMI of 21 kg/m2, this client is classified as an appropriate weight and should gain 25-35 lb (11.3-15.9 kg) (Option 2). (Option 1) Weight gain during the first trimester should be approximately 1.1-4.4 lb (0.5- 2.0 kg). A 10-lb (4.5-kg) weight gain during the first 3 months of pregnancy would be too much in any client. (Option 3) A client of normal weight should gain approximately 1 lb (0.5 kg)/wk during the second and third trimesters of pregnancy. A weight gain of only 0.5 lb (0.2 kg)/wk is recommended for obese clients. (Option 4) A weight gain of 20 lb (9.1 kg) during pregnancy is inadequate for a client of normal weight. Restricting weight gain places the fetus at risk for low birth weight (<5.5 lb [<2500 g]) and preterm birth. Educational objective: Appropriate total weight gain during pregnancy decreases risks to the client and fetus. Weight gain in the first trimester should be 1.1-4.4 lb (0.5-2.0 kg)regardless of BMI. The optimal total weight gain during pregnancy should be determined by the client's prepregnancy BMI. A A A A client with diabetes visits the clinic reporting breast tenderness, vaginal discharge, and urinary frequency. Which action is most important for the nurse to perform? 1. Ask if the client performs breast self-exams [0%] 2. Ask the client about characteristics of vaginal discharge [18%] 3. Assess the date of the client's last menstrual period [71%] 4. Review the client's home blood sugar logs [9%] Incorrect Correct answer 3 Answered correctly 71% Time: 37 seconds Updated: 08/18/2017 Explanation: Subjective (presumptive): - Amenorrhea, Nausea & vomiting, Urinary frequency, Breast tenderness, Quickening, Excessive fatigue Objective (probable): -Uterine & cervical changes, Goodell sign, Chadwick sign, Hegar sign, Uterine enlargement, Braxton Hicks contractions, Ballottement, Fetal outline palpation, Uterine & funic soufflé, Skin pigmentation changes, Chloasma, Linea nigra, Areola darkening, Striae gravidaru, Positive pregnancy tests Positive (diagnostic): -Fetal heartbeat heard with Doppler device -Fetal movement palpated by health care provider or visible fetal movements -Visualization of fetus by use of ultrasoundSubjective (presumptive) signs of pregnancy are self-reported by a client. This client's symptoms could originate from pathologic causes (eg, urinary tract infection [UTI], sexually transmitted infection), but collectively these symptoms may be indicative of early pregnancy. Any client with possible signs/symptoms of early pregnancy should be asked about menstrual history (Option 3). (Option 1) Regular breast self-exams are an important part of breast self-awareness and may alert the client to early pathologic breast changes. However, breast tenderness is a common sign of early pregnancy, which should be ruled out first. (Option 2) Leukorrhea (ie, whitish, mucoid vaginal discharge) increases during pregnancy in response to rising hormone levels. The client should be questioned about color, odor, and consistency of discharge to rule out infection, but this response from the nurse does not address the larger picture. (Option 4) Increased urinary frequency may result from hyperglycemia, and clients with diabetes are at increased risk for infections (eg, UTI, yeast infection). Reviewing home blood sugar logs would help the nurse assess the client's level of glycemic control over time but would not address the complete picture of the client's acute symptoms. Educational objective: Subjective (self-reported) signs of pregnancy may include leukorrhea, breast tenderness, and urinary frequency. Any client with possible signs/symptoms of early pregnancy should be asked about menstrual history. A A A A 28-year-old client is admitted to the labor and delivery unit for severe preeclampsia. She is started on IV magnesium sulfate. Which signs indicate that the client has developed magnesium sulfate toxicity? Select all that apply. 1. 0/4 patellar reflex 2. Blood pressure is 156/84 mm Hg 3. Client voided 600 mL in 8 hours 4. Respirations are 10/min 5. Serum magnesium level is 5 mEq/L (2.5 mmol/L) Explanation: Normal blood level of magnesium is 1.5-2.5 mEq/L (0.75-1.25 mmol/L). However, a therapeutic magnesium level of 4-7 mEq/L (2.0-3.5 mmol/L) is necessary to prevent seizures in a preeclamptic client (Option 5). Magnesium toxicity causes central nervous system depression because toxic magnesium levels (>7 mEq/L) [3.5 mmol/L]) block neuromuscular transmission. Absent or decreased deep-tendon reflexes (DTRs) are the earliest sign of magnesium toxicity. DTRs are scoredon a scale of 0-4+ and should be assessed during magnesium infusion; normal findings are 2+ (Option 1). If toxicity is not recognized early (eg, decreasing DTRs), clients can progress to respiratory depression, followed by cardiac arrest (Option 4). Assessments (including vital signs) should be performed every 5-15 minutes during the loading dose, followed by 30- to 60-minute intervals until the client stabilizes, then every 2 hours. Treatment for magnesium toxicity is immediate discontinuation of the infusion. Administration of calcium gluconate (antidote) is recommended only in the event of cardiorespiratory compromise. (Option 2) Hypertension is a sign of preeclampsia, not of magnesium toxicity. Hydralazine (Apresoline), methyldopa (Aldomet), or labetalol (Trandate) is used to lower blood pressure (BP) if needed (typically when BP is >160/110 mm Hg). (Option 3) Urine output <30 mL/hr is a sign of magnesium toxicity. Educational objective: The therapeutic level of magnesium for preeclampsia-eclampsia treatment is 4-7 mEq/L (2.0-3.5 mmol/L). Signs of magnesium toxicity are decreased or absent deep-tendon reflexes, respiratory depression, decreased urine output (<30 mL/hr), and cardiac arrest. Calcium gluconate (antidote) should be readily available in the event of cardiorespiratory compromise. A A A A client at 38 weeks gestation is brought to the emergency department after a motor vehicle crash. She reports severe, continuous abdominal pain. The nurse notes frequent uterine contractions and mild, dark vaginal bleeding. What actions should the nurse take? Select all that apply. 1. Anticipate emergent cesarean birth 2. Apply continuous external fetal monitoring 3. Assess routine vital signs every 4 hours 4. Draw blood for type and crossmatch 5. Initiate IV access with a 22-gauge catheter Explanation: Placental abruption occurs when the placenta separates prematurely from the uterine wall, causing hemorrhage beneath the placenta. Abruptions are classified as partial, complete, or marginal and may be overt (visible vaginal bleeding) or concealed (bleeding behind placenta). Risk factors include abdominal trauma, hypertension, cocaine use, history of previous abruption, and preterm premature rupture of membranes.Symptoms and their severity depend on extent of abruption and include abdominal and/or back pain, uterine contractions, uterine rigidity, and dark red vaginal bleeding. Tachysystole (ie, excessive uterine contractions), with or without fetal distress, is often present, and continuous fetal monitoring is necessary (Option 2). A type and crossmatch should be drawn as treatment may include blood transfusion (Option 4). In severe cases, emergent cesarean birth is indicated (Option 1). Although blood loss is maternal, the loss of functional placental surface area can result in decreased placental perfusion, impaired fetal oxygenation, and fetal death. (Option 3) Maternal vital signs should be assessed frequently for signs of shock (eg, tachycardia, hypotension) as client condition can decline rapidly. In this acute scenario, assessment of vital signs every 4 hours is not sufficient. (Option 5) Abruption may require rapid volume replacement with IV fluid and blood products, requiring large-bore IV access. Peripheral IV access with a 16- or 18-gauge catheter should be initiated. Educational objective: Placental abruption usually presents with abdominal pain and dark red vaginal bleeding. The main concerns are maternal blood loss resulting in hypotension and shock and fetal compromise. Maternal stabilization and expedited birth are indicated.A A A The nurse is providing education to several first-trimester pregnant clients. Which client requires priority anticipatory teaching? 1. Client who gardens and eats homegrown vegetables [53%] 2. Client who has gained 4 lb (1.8 kg) from prepregnancy weight [22%] 3. Client who has noticed thin, milky white vaginal discharge [18%] 4. Client who practices yoga and swims in a pool 3 times a week [5%] Explanation: Toxoplasmosis is a parasitic infection caused by Toxoplasma gondii, which may be acquired from exposure to infected cat feces or ingestion of undercooked meat or soil-contaminated fruits/vegetables. Pregnant clients who contract toxoplasmosis can transfer the infection to the fetus and potentially cause serious fetal harm (eg, stillbirth, malformations, blindness, mental disability). Pregnant clients should be advised to take precautions when gardening and thoroughly wash all produce to decrease exposure risk. (Option 2) Weight gain recommendations vary by prepregnancy BMI. A 1.1- to 4.4-lb (0.5- to 2.0-kg) weight gain in the first trimester and approximately 1 lb (0.5 kg) per week thereafter is normal and expected for women with a healthy BMI. (Option 3) Leukorrhea is a thin, milky white vaginal discharge that is normal during pregnancy and is due to increased levels of progesterone and estrogen. If discharge changes color, becomes malodorous, or causes itching/burning, further investigation is needed. (Option 4) Exercise, particularly low-impact activities such as walking, swimming, and yoga, is recommended during pregnancy. Contact sports or activities with a risk for falls (eg, soccer, downhill skiing) should be avoided to prevent abdominal injuries. Educational objective: Toxoplasmosis is a parasitic infection acquired by exposure to infected cat feces or ingestion of undercooked meat or soil-contaminated fruits/vegetables. Pregnant clients who contract toxoplasmosis may transfer the infection to the fetus and potentially cause serious fetal harm. Pregnant clients should take precautions when gardening and thoroughly wash all produce to decrease exposure risk. A A A The initial prenatal laboratory screening results of a client at 12 weeks gestation indicate a rubella titer status of nonimmune. What will the nurse anticipate as the plan of care for this client?1. Administer measles-mumps-rubella (MMR) vaccine now [15%] 2. Administer MMR vaccine immediately postpartum [57%] 3. Administer MMR vaccine in the third trimester [8%] 4. An MMR vaccine is not indicated for this client [18%] Explanation: In a pregnant client, a serum sample is collected at the first prenatal visit to determine immunity to the rubella virus. A positive immune response indicates immunity to the rubella virus, attributed to either past infection or vaccination. A negative, or nonimmune, response indicates that the client is susceptible to rubella disease and requires vaccination. An equivocal response indicates partial immunity to rubella and is treated clinically the same as nonimmune status. Measles-mumps-rubella (MMR) is a live attenuated vaccine. Live vaccines are contraindicated in pregnancy due to the theoretical risk of contracting the disease from the vaccine. Maternal rubella infection can be teratogenic for the fetus. The fetal effects of congenital rubella syndrome include congenital cataracts, deafness, heart defects (patent ductus arteriosus), and cerebral palsy. The best time to administer an MMR vaccine to a nonimmune client is in the postpartum period just prior to discharge (Option 2). The MMR vaccine can safely be administered to breastfeeding clients. (Options 1 and 3) MMR vaccine is contraindicated in pregnancy. Also, pregnancy should be avoided for at least 1–3 months after the immunization is given. (Option 4) This client is rubella nonimmune and is susceptible to rubella if exposed. The vaccine should be offered in the postpartum period. Educational objective: The measles-mumps-rubella vaccine is a live attenuated vaccine and is contraindicated in pregnancy due to the risk of teratogenic effects to the fetus. Clients who are nonimmune to rubella should receive the vaccine in the postpartum period. Pregnancy should be avoided for at least 1-3 months after immunization. A A A Which finding is most important for the nurse to report to the health care provider? 1. 24 weeks gestation, hemoglobin is 9 g/dL (90 g/L) [44%] 2. 24 weeks gestation, 1-hour (50 g) oral glucose screen is 120 mg/dL (6.7 mmol/L) [8%] 3. 27 weeks gestation, vaginal secretion is pH 5 [10%] 4. 36 weeks gestation, white blood cell count is 13,000/mm3 (13.0 x 109/L) [35%]Explanation: Iron deficiency anemia is a common complication during pregnancy. It is related to low iron stores and diets low in iron. During pregnancy, clients are considered anemic when hemoglobin is <11 g/dL (110 g/L) in the first or third trimesters, or <10.5 g/dL (105 g/L) in the second trimester. A pregnant client with a hemoglobin level of 9 g/dL (90 g/L) should be evaluated for symptoms of anemia (eg, fatigue, weakness) and may require additional laboratory work (eg, serum ferritin level) to determine the cause. An iron supplement may need to be prescribed. (Option 2) A 1-hour (50 g) oral glucose screen is considered abnormal if the result is ≥140 mg/dL (7.8 mmol/L). (Option 3) During pregnancy, the vagina maintains an acidic state to inhibit the growth of bacteria. (Option 4) During pregnancy, it is normal for the white blood cell count to increase; counts can be as high as 15,000/mm3 (15.0 x 109/L). Educational objective: Clients are diagnosed with anemia when hemoglobin is <11 g/dL (110 g/L) in the first or third trimesters, or <10.5 g/dL (105 g/L) in the second trimester. Iron deficiency is the most common cause. A A A A nurse on the antepartum unit is caring for a pregnant client at 30 weeks gestation who was admitted with reports of vaginal bleeding. A diagnosis of placenta previa was confirmed by ultrasound. What should the nurse tell the client to anticipate? Select all that apply. 1. Additional ultrasound around 36 weeks gestation 2. Clearance for sexual activity if bleeding stops 3. Discharge home if bleeding stops and fetal status is reassuring 4. Scheduled cesarean birth before onset of labor 5. Weekly vaginal examinations to assess for cervical change Explanation: In placenta previa, the placenta is implanted over or very near the cervix. This causes placental blood vessels to be disrupted during cervical dilation and effacement, which may result in massive blood loss and maternal/fetal compromise. Because of the increased risk of hemorrhage if contractions result in cervical change, a cesarean birth is planned for after 36 weeks gestation and prior to the onset of labor (Option 4). A stable client with no active bleeding and reassuring fetal status may be discharged home andmanaged in an outpatient setting (Option 3). However, the client must be closely monitored and instructed to return to the hospital immediately if bleeding recurs. As pregnancy progresses, the placenta grows in size and can potentially migrate away from the cervical opening, resulting in complete resolution of the previa. Therefore, an additional ultrasound is usually performed around 36 weeks gestation to assess placental location (Option 1). (Options 2 and 5) Clients with placenta previa should be instructed to remain on pelvic rest. Vaginal examinations, douching, and vaginal intercourse are contraindicated due to the risk of disruption of the placental vessels and subsequent hemorrhage. Modified bed rest (ie, decreasing any physical activity that could cause contractions) is also recommended. Educational objective: Clients with placenta previa are at risk for hemorrhage. Vaginal examinations are contraindicated, and pelvic rest is recommended to prevent disruption of placental vessels. A cesarean birth is planned prior to onset of labor. A A A A client at 30 weeks gestation is hospitalized for preeclampsia. Which assessment finding requires priority intervention? 1. Elevated liver enzymes [17%] 2. Lower abdominal pain and vaginal bleeding [45%] 3. Swelling of the hands, feet, and face [19%] 4. Urine output of 25 mL/hr [17%] Explanation: Placental abruption is a possible complication of preeclampsia that can be lifethreatening to mother and baby. It occurs when the placenta tears away from the wall of the uterus due to stress, causing significant bleeding to the mother and depriving the baby of oxygen. Bleeding can be concealed inside the uterus. This may require immediate delivery of the baby. (Option 1) Elevated liver enzymes can indicate the start of a more serious condition called HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets), another complication of preeclampsia. This client will need additional laboratory work. If HELLP is diagnosed, the only treatment is delivery. (Option 3) Swelling of the hands, feet, and face are expected findings of preeclampsia and should be assessed frequently. (Option 4) Normal urine output is 30 mL/hr; anything less represents a potential problem. Oliguria and elevated creatinine levels indicate kidney failure and require intervention.This client's urine output of 25 mL/hr does not represent an immediate, life-threatening condition. Educational objective: Preeclampsia in pregnancy manifests with high blood pressure and protein in the urine. Edema is expected, although it is not part of the criteria. Complications of preeclampsia include eclampsia, placental abruption, and HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets) syndrome. A A A The obstetric nurse is reviewing phone messages. Which client should the nurse call first? 1. Client at 18 weeks gestation taking ceftriaxone and reporting mild diarrhea [10%] 2. Client at 22 weeks gestation with twins who is taking acetaminophen twice a day [23%] 3. Client at 28 weeks gestation taking metronidazole and reporting dark-colored urine [27%] 4. Client at 32 weeks gestation taking ibuprofen for moderate back pain [38%] Explanation: Nonsteroidal anti-inflammatory drugs (NSAIDs) (eg, ibuprofen, indomethacin, naproxen) inhibit prostaglandin synthesis and can be taken to decrease pain and inflammation or to reduce fever. NSAIDs are pregnancy category C in the first and second trimesters and pregnancy category D in the third trimester. NSAIDs must be avoided during the third trimester due to the risk of causing premature closure of the ductus arteriosus in the fetus (Option 4). During the first and second trimesters, NSAIDs should be taken only if benefits outweigh risks and under the supervision of a health care provider (HCP). (Option 1) Beta lactam antibiotics (eg, amoxicillin, ceftriaxone [Rocephin]) are pregnancy category B. Diarrhea is a common side effect of beta lactams. Although diarrhea should be reported to the HCP, as it could indicate pseudomembranous (Clostridium difficile) colitis or lead to dehydration if prolonged, this client is not the priority. (Option 2) Acetaminophen (pregnancy category B) is a common pain reliever and/or fever reducer used during pregnancy. Acetaminophen intake should not exceed 4 g per day, including any over-the-counter or prescription combination medications that contain acetaminophen. (Option 3) Metronidazole (Flagyl) is an anti-infective and pregnancy category B. Darkcolored urine is an expected side effect of metronidazole and not cause for concern. Educational objective:Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided in the third trimester due to risk of premature closure of the fetal ductus arteriosus. NSAIDs should be taken only under the direction and supervision of a health care provider during the first and second trimesters. A A A A client is at 20 weeks gestation. The client reports having to "run to the bathroom all the time," "it hurts to pee," and my urine "smells bad." Which statement by the nurse is the most appropriate?1. "Drink cranberry juice to relieve the symptoms." [1%] 2. "Make sure to wipe from the front to the back after voiding." [3%] 3. "Most women have urinary frequency at this stage and it is normal." [1%] 4. "You may need to be checked for a urinary tract infection." [93%] Explanation: The most common bacterial infection during pregnancy is a urinary tract infection (UTI). Pregnant women are predisposed to UTIs due to physiological changes (urine stasis) in the renal system. Symptoms include frequency, dysuria, urgency, foulsmelling urine, sediment/pus/blood in the urine, or sensation of bladder fullness. Diagnosis is made on signs/symptoms and urinalysis. The prescribed antibiotic course must be completed to treat the infection appropriately. The priority is to deal with the current infection. If the UTI is untreated, the infection can lead to pyelonephritis or premature labor. (Option 1) Cranberry juice works by preventing the attachment of bacteria to the epithelial cells in the bladder wall. It is recommended that clients drink 8 ounces of unsweetened juice 3 times a day. Although this is reasonable teaching, it is not the priority at this time. (Option 2) This is good general advice to help prevent UTIs as the most common causative organism is Escherichia coli. However, completing a urinalysis and initiating antibiotic therapy should be implemented before instructions related to UTI prevention. Actual over potential is always the priority. (Option 3) Most women experience urinary symptoms of frequency (voiding >7 times/day), urgency, and nocturia (voiding >2 times/night) beginning early in pregnancy and continuing to some degree throughout pregnancy. These are primarily a result of hormonal changes and may be due to anatomical changes in the renal system. They are not indicative of UTI. However, the client has new, additional symptoms of a UTI (dysuria, foulsmelling urine). The client should be tested and treated with an antibiotic. Educational objective: Signs/symptoms of a UTI in pregnancy include new-onset dysuria and sediment/cloudy, foul-smelling urine. This differentiates it from the common urinary frequency throughout pregnancy. The priority for the nurse is to identify the need for a urinalysis and to provide instructions to finish the course of antibiotics to prevent the untreated infection from causing pyelonephritis or premature labor. A A A A client at 34 weeks gestation reports constipation. The client has been taking 325 mg ferrous sulfate tid for anemia since the last appointment 4 weeks ago. Which recommendations should the nurse make for this client? Select all that apply.1. Decreased daily dairy intake 2. Increased fruit and vegetable intake 3. Moderate-intensity regular exercise 4. One laxative twice daily for a week 5. Two cups of hot coffee each morning Explanation Constipation is a common discomfort of pregnancy and is due to an increase in the hormone progesterone, which causes decreased gastric motility. Ferrous sulfate (iron) supplementation may also cause constipation. Interventions to prevent or treat constipation include: High-fiber diet: High amounts of fruits, vegetables, breakfast cereals, whole-grain bread, prunes High fluid intake: 10-12 cups of fluid daily Regular exercise: Moderate-intensity exercise (eg, walking, swimming, aerobics) Bulk-forming fiber supplements: Psyllium, methylcellulose, wheat dextrin (Option 1) Dairy is a great source of calcium, which is essential for fetal bone development. However, dairy products should be consumed at least 2 hours before or 1 hour after iron supplements as they bind to iron and decrease absorption. (Option 4) Laxatives are not recommended during pregnancy due to the risk of dehydration and electrolyte imbalance, which can lead to uterine cramping and contractions. The client should consult with the health care provider before using any overthe-counter stool softeners or laxatives. (Option 5) Caffeine consumption in pregnancy should be limited to 200-300 mg/day. Coffee may contain 100-200 mg caffeine per cup and should therefore be consumed in moderation during pregnancy. Educational objective: Constipation in pregnancy may be caused by increased progesterone levels and iron supplementation. It is best treated with 10-12 cups of fluid daily, a high-fiber diet/supplementation, and regular exercise. Clients should not take laxatives without first discussing this with the health care provider. A A AA pregnant client in the first trimester tells the clinic nurse she will be traveling to an area with a known Zika virus outbreak and expresses concern regarding disease transmission. Which statement by the nurse is most appropriate? 1. "If you experience Zika symptoms, notify your health care provider." [1%] 2. "Take precautions against mosquito bites throughout the trip." [34%] 3. "You are not far enough along for the Zika virus to affect your baby." [0%] 4. "You should consider postponing your trip until after you have the baby." [62%] Explanation: Zika virus is transmitted via mosquitoes, sexual contact, and infected bodily fluids. Zika causes viral symptoms (eg, low-grade fever, arthralgias) and has been shown to cause microcephaly, developmental dysfunction, and encephalitis in babies born to Zika-infected women. Women who are attempting to conceive and those who are pregnant are encouraged to avoid travel to areas affected by Zika until after birth (Option 4). For clients currently living in a Zika-affected area, proper mosquito precautions (eg, insect repellant containing DEET) and safe sex practices (eg, barrier methods) should be utilized, and routine Zika testing may be provided. (Option 1) Although this statement is true, it does not provide education on avoiding Zika infection. Waiting until symptoms are present does not address preventing fetal exposure and possible birth defects. (Option 2) Current guidelines recommend that pregnant women avoid travel to Zikaaffected areas completely. In addition, mosquitoes are not the only mode of transmission for the virus. (Option 3) Zika virus can affect women in all stages of pregnancy. Educational objective: Zika infection in a pregnant woman can cause birth defects and developmental dysfunction. Current guidelines recommend that pregnant women avoid travel to Zika-affected areas. A A A A client who is being evaluated for suspected ectopic pregnancy reports sudden-onset, severe, right lower abdominal pain and dizziness. Which additional assessment findings will the nurse anticipate if the client is experiencing a ruptured ectopic pregnancy? Select all that apply. 1. Blood pressure 82/64 mm Hg 2. Crackles on auscultation 3. Distended jugular veins4. Pulse 120/min 5. Shoulder pain Explanation: Ectopic pregnancy occurs when a fertilized ovum implants outside the uterine cavity. The majority of ectopic pregnancies occur in the fallopian tubes. Risk factors include recurrent sexually transmitted infections, tubal damage or scarring, intrauterine devices, and previous tubal surgeries (eg, tubal ligation for sterilization). Clinical manifestations are lower-quadrant abdominal pain on one side, mild to moderate vaginal bleeding, and missed or delayed menses. Signs of subsequent hypovolemic (hemorrhagic) shock from ruptured ectopic pregnancy include dizziness, hypotension, and tachycardia. Free intraperitoneal blood pooling under the diaphragm can cause referred shoulder pain. Peritoneal signs (eg, tenderness, rigidity, low-grade fever) may develop subsequently. (Options 2 and 3) Distended jugular veins and lung crackles indicate volume overload. The main risk with ectopic pregnancy is hypovolemic (hemorrhagic) shock. Jugular veins would be flat in hypovolemic shock. Educational objective: The fallopian tubes are the most common site for an ectopic pregnancy. As the ectopic pregnancy grows and expands, rupture may occur, resulting in active bleeding that progresses to life-threatening hypovolemic (hemorrhagic) shock. Signs of ruptured ectopic pregnancy may include severe abdominal pain, dizziness, and referred shoulder pain. A A A A client who is 8 weeks pregnant reports morning sickness. What is the most appropriate response by the nurse? 1. Advise the client to consume hot, versus cold, foods [7%] 2. Instruct the client to drink 2 glasses of water with each meal [7%] 3. Suggest the client consume high-protein snacks on awakening [53%] 4. Tell the client that morning sickness should pass in a few weeks [32%] Explanation: Morning sickness, characterized by nausea with or without vomiting, is a common problem during the first trimester of pregnancy. Although it is referred to as "morning" sickness, it can happen anytime throughout the day. It is thought to be due to rising hormone levels (ie, estrogen, progesterone, human chorionic gonadotropin). Initial interventions, focusing on diet management and triggering avoidance, include:Eating several small meals during the day (ie, high in protein or carbohydrates and low in fat) Drinking fluids (preferably clear, cold, carbonated beverages) between, rather than with, meals Having a high-protein snack before bedtime and on awakening (Option 3) Consuming foods/drinks with ginger (eg, ginger tea, ginger lollipops, ginger chews) Consuming foods high in vitamin B6 (eg, nuts, seeds, legumes) (Option 1) Hot foods will not relieve morning sickness; cold foods/drinks are usually recommended. (Option 2) Fluids should be consumed at least 30 minutes before or after meals to avoid abdominal distension. (Option 4) This response may provide false reassurance and does not help the client manage symptoms. Morning sickness typically resolves after the first trimester, although some clients experience nausea through the second or third trimester. Educational objective: Morning sickness can usually be relieved through lifestyle and dietary changes, including eating small and frequent meals, drinking cold fluids between meals, having a high-protein snack before bedtime and on awakening, and consuming foods/drinks containing ginger and vitamin B6. A A A A client at 21 weeks gestation has intense heartburn (pyrosis). What should the nurse recommend? Select all that apply. 1. Avoid dairy products 2. High-protein, low-fat diet 3. Lie on the left side after meals 4. Six small meals a day 5. Sodium bicarbonate antacid Explanation: Pyrosis, also known as heartburn, occurs during pregnancy from an increase in the hormone progesterone. Progesterone causes the esophageal sphincter to relax, leading to pyrosis. Interventions to reduce heartburn include: Upright position after meals to reduce gastroesophageal reflux Small, frequent meals rather than 3 large meals a day (Option 4)Keeping the head of the bed elevated using pillows Drinking smaller amounts of fluid while eating Eliminating dietary triggers, including fried and fatty foods, caffeine/chocolate, spicy foods, carbonated drinks, and peppermint (Option 2) (Option 1) Dairy products do not lead to heartburn and should not be avoided during pregnancy. Clients should avoid fried and fatty foods, coffee, and carbonated beverages. (Option 3) Clients should stay upright 2-3 hours after meals. Lying down immediately after eating will cause heartburn to increase and lead to more discomfort. (Option 5) Most antacids are safe during pregnancy. However, those containing sodium bicarbonate (Alka-Seltzer) or magnesium trisilicate should be avoided during pregnancy. Educational objective: Heartburn (pyrosis) is caused by the hormone progesterone, which causes the esophageal sphincter to relax. Methods the pregnant client can take to reduce pyrosis include maintaining an upright position after meals, eating small meals, taking approved antacids, and avoiding causative foods and beverages. A A A A pregnant client arrives in the labor and delivery unit with mild contractions and brisk, painless vaginal bleeding. The client received no prenatal care and reports being "about 7- 8 months." Which actions should the nurse anticipate? Select all that apply. 1. Blood draw for type and screen 2. Electronic fetal monitoring 3. Initiation of 2 large-bore IV catheters 4. Pad counts to assess bleeding 5. Vaginal examination for cervical dilation Explanation: Placenta previa is an abnormal implantation of the placenta resulting in partial or complete covering of the cervical os (opening). The condition is diagnosed by ultrasound. In clients reporting painless vaginal bleeding after 20 weeks gestation, placenta previa should be suspected. Placenta previa found early in pregnancy may resolve by the third trimester, but women with persistent placenta previa or hemorrhage require cesarean birth. A type and screen to determine blood type and Rh status is appropriate due to the potential for excessive blood loss and need for blood transfusion (Option 1). Fetal well-being is assessed via continuous electronic fetal monitoring to help determine appropriate timing for birth (Option 2). Large-bore IV access is established in anticipation of fluidresuscitation and administration of blood products (Option 3). The client should also be monitored frequently for any changes in bleeding via pad counts (Option 4). (Option 5) Digital vaginal examinations are contraindicated in the presence of vaginal bleeding of unknown origin. When placenta previa is present, manual manipulation of the cervix can damage placental blood vessels, causing subsequent bleeding that can progress to hemorrhage. Clients with placenta previa are on pelvic rest (ie, no intercourse, nothing per vagina). Educational objective: Placenta previa is suspected in clients reporting painless vaginal bleeding after 20 weeks gestation. Clients with placenta previa are at high risk for hemorrhage. The nurse should initiate electronic fetal monitoring and pad counts, draw a type and screen, and initiate large-bore IV access. Digital vaginal examinations are contraindicated. A A A The nurse is caring for a client in the first trimester during an initial prenatal clinic visit. Based on the information provided by the client, which factor places the client at an increased risk for preterm labor? 1. Age 25 [4%] 2. Periodontal disease [65%] 3. Vegetarian diet [27%] 4. White ethnicity [2%] Explanation: Preterm birth is defined as birth before 37 weeks and 0 days gestation. Infection (eg, periodontal disease, urinary tract infection) is strongly associated with preterm labor, particularly when untreated (Option 2). Infection causes release of inflammatory mediators such as prostaglandins, which are uterotonic (ie, promote contractions) and contribute to cervical softening. Some risk factors for preterm birth may be modifiable with lifestyle changes and early treatment. Risk factors should be addressed at the initial and each subsequent prenatal visit to allow for early identification and management. Some risk factors for preterm birth include: History of spontaneous preterm birth in a previous pregnancy (single largest independent risk factor) Previous cervical surgery, such as a cone biopsy (weakens cervical support) Tobacco and/or illicit drug use(Option 1) Maternal ages <17 and >35 are associated with increased risk for preterm birth. Maternal age of 25 is not a risk factor. (Option 3) Maternal undernutrition can increase the risk for preterm birth and low infant birth weight. However, a balanced vegetarian diet with adequate pregnancy weight gain does not increase preterm birth risk. (Option 4) Non-Hispanic black women have the highest rates of preterm labor and birth. Non-Hispanic white ethnicity is not a risk factor for preterm birth. Educational objective: Infection (eg, periodontal disease, urinary tract infection) places pregnant clients at increased risk for preterm labor and birth. Other risk factors include history of preterm birth, previous cervical surgery, tobacco/illicit drug use, and maternal age <17 or >35. A A A Which meal should the nurse recommend for a pregnant client at 13 weeks gestation? 1. Baked chicken, turnip greens, peanut butter cookie, and grape juice [62%] 2. Baked swordfish, fries, baked apples, and fat-free milk [4%] 3. Chilled ham and cheese sandwich, broccoli, orange slices, and water [18%] 4. Fried liver and onions, pasteurized cheese squares, fresh fruit cup, and water [14%] Explanation: During pregnancy, it is important for the client to consume a balanced diet with appropriate nutrients, vitamins, and minerals. Foods containing folic acid, protein, whole grains, iron, and omega-3 fatty acids are especially important. Due to the risk for bacterial contamination (eg, Listeria, toxoplasmosis), pregnant clients should avoid consuming unpasteurized milk products, unwashed fruits and vegetables, deli meat and hot dogs (unless heated until steaming hot), and raw fish/meat. They should also avoid intake of fish high in mercury (eg, shark, swordfish, king mackerel, tilefish). (Option 2) This meal contains swordfish, which is high in mercury and should be avoided during pregnancy. (Option 3) This meal contains cold deli meat, which should be avoided during pregnancy due to the risk of listeriosis from Listeria monocytogenes. (Option 4) Liver should be avoided during pregnancy due to high amounts of vitamin A. Although liver is a good source of iron, the excessively high amounts of vitamin A can be teratogenic. Educational objective: An appropriate diet is essential to meet the needs of the pregnant client and growing fetus. Pregnant clients should avoid deli meats and hot dogs (unlesssteaming hot), liver, unpasteurized milk products, unwashed fruits and vegetables, raw fish, and fish high in mercury. A A A When triaging 4 pregnant clients in the obstetric clinic, the nurse should alert the health care provider to see which client first? 1. First-trimester client reporting frequent nausea and vomiting [0%] 2. Second-trimester client with dysuria and urinary frequency [6%] 3. Second-trimester client with obesity reporting decrease in fetal movement [47%] 4. Third-trimester client with right upper quadrant pain and nausea [45%] Explanation: Right upper quadrant (RUQ) or epigastric pain can be an indicator of HELLP syndrome, a severe form of preeclampsia. HELLP syndrome (Hemolysis, Elevated Liver enzymes, and Low Platelet count) is often mistaken for viral gastroenteritis due to its variable and nonspecific presentation. Misdiagnosis may lead to severe complications (eg, placental abruption, liver failure, stroke) and/or maternal/fetal death. Clients may have RUQ pain, nausea, vomiting, and malaise. Headache, visual changes, proteinuria, and hypertension may or may not be present. (Option 1) Nausea and vomiting during the first trimester are normal, expected findings. Vomiting that continues past the first trimester or that is accompanied by fever, pain, or weight loss is considered abnormal and requires intervention. (Option 2) Although urinary frequency is common in pregnancy, dysuria could indicate a urinary tract infection. This client should be evaluated but does not take priority over a client with symptoms of HELLP. (Option 3) Maternal perception of fetal movement can be altered by obesity, maternal position, fetal sleep cycle, fetal position, anterior placenta, and amniotic fluid volume (increased or decreased). This client should be evaluated to determine the cause of decreased fetal movement; however, this is not the priority. Educational objective: HELLP syndrome (Hemolysis, Elevated Liver enzymes, and Low Platelet count) is a severe form of preeclampsia. Its clinical presentation can be quite variable and may include nonspecific symptoms such as right upper quadrant/epigastric pain, nausea, vomiting, and malaise. Complications including placental abruption, stroke, and death may occur if HELLP syndrome is not treated immediately. ---A client at 39 weeks gestation is brought to the emergency department after a motor vehicle crash. The client, who is secured supine on a backboard, suddenly becomes pale with a blood pressure of 88/50 mm Hg. What action should the nurse take first?1. Administer normal saline fluid bolus [17%] 2. Assess cervix for presenting part [3%] 3. Obtain fetal heart rate [14%] 4. Turn client laterally [64%] Explanation: Supine hypotensive syndrome results from compression of the maternal inferior vena cava by the large gravid uterus in mid to late pregnancy when the client is in the supine position. The venous return is reduced, causing maternal hypotension from reduced cardiac output. The client can also report feeling dizzy and faint. The first step is to rectify the cause by turning the client laterally while still strapped on the backboard. (Option 1) The etiology is not hypovolemia but perfusion. A fluid bolus of isotonic fluids (normal saline or lactated Ringer's) can be administered if the position change does not relieve the symptoms. Mean arterial pressure (MAP) should be >60 mm Hg for effective organ perfusion. Normal MAP is 70-105 mm Hg. (Option 2) The client does not have classic signs of a precipitous or impending delivery. Classic signs or symptoms of the second stage of labor/delivery of the baby include feeling the need to push, an intense urge to bear down, or a sensation of cervical pressure. A pelvic examination can be performed, but it is not the first priority. (Option 3) The etiology is related not to the fetus, but to the maternal circulation. Because the client does not have adequate cardiac output, circulation to the fetus could be compromised. The first priority is to rectify the client's perfusion issue and check the fetus. The best indicators of fetal health are heart rate and movement. Educational objective: Supine hypotensive syndrome results from compression of the maternal inferior vena cava by the large gravid uterus in mid to late pregnancy when the client is in the supine position. It can be corrected by first positioning the client laterally A A A A nurse is caring for a pregnant client who has hyperemesis gravidarum. Which assessment findings should the nurse anticipate? Select all that apply. 1. Blood pressure 160/94 mm Hg 2. Large urine protein 3. Positive urine ketones (moderate) 4. Pulse 106/min 5. Urine specific gravity 1.010Explanation: Hyperemesis gravidarum is a disorder that causes pregnant clients to have severe nausea and vomiting. This leads to fluid and electrolyte imbalances, nutritional deficiencies, ketonuria, and weight loss. On assessment, the nurse should expect signs and symptoms of dehydration, which include dry mucous membranes, poor skin turgor, decreased urine output, tachycardia, and low blood pressure. Ketonuria indicates that the body is breaking down fat to use for energy due to the client's starvation state. (Options 1 and 5) The client with hyperemesis gravidarum is dehydrated. Blood pressure is expected to be low due to lack of blood volume. The urine specific gravity will be increased (>1.030) as the urine is in a concentrated state. Blood urea nitrogen is also elevated (>20 mg/dL [7.1 mmol/L]). (Option 2) Proteinuria is associated with kidney disease or preeclampsia. Hyperemesis does not cause proteinuria. Educational objective: Excessive vomiting (hyperemesis gravidarum) leads to fluid and electrolyte imbalances (hypokalemia, metabolic alkalosis), weight loss, nutritional deficiencies, and ketonuria. The signs and symptoms of dehydration include poor skin turgor, decreased urine output, tachycardia, low blood pressure, and dry mucous membranes. A A A The nurse is preparing to assess a client visiting the women's health clinic. The client's obstetric history is documented as G5T1P2A1L2. Which interpretation of this notation is correct? 1. The client had 1 birth at 37 wk 0 d gestation or beyond [66%] 2. The client had 3 births between 20 wk 0 d and 36 wk 6 d gestation [16%] 3. The client has 3 currently living children [8%] 4. The client is currently not pregnant [8%] Explanation: The GTPAL system is a shorthand system of documenting a client's obstetric history. This client (G5T1P2A1L2) has been pregnant 5 times (G5); had 1 term birth (T1), 2 preterm births (P2), and 1 abortion (A1); and has 2 currently living children (L2). The client's term birth is indicated by the T1 portion of the GTPAL notation (Option 1). (Option 2) The client had 2 preterm births, indicated by the P2 portion of the GTPAL notation. (Option 3) The client has 2 currently living children, as indicated by the L2 portion of the GTPAL notation. If a child born full- or preterm is not living (due to stillbirth from 20 wk 0 d and beyond or infant/child death after birth), that birth and subsequent death is countedtoward T or P (term or preterm) but is not notated under L (currently living children); T and P record total number of births without regard to current living status. This client has 2 currently living children (L2), which is 1 less than the client's total notation for term + preterm (T1 + P2 = 3). Therefore, the client has experienced the death of 1 child who had been born at 20 wk 0 d gestation or beyond. (Option 4) If a client is currently pregnant, the number of pregnancies (gravida) will be greater than the number of births (term, preterm, and abortions combined). This client is a G5, and T1 + P2 + A1 = 4. Therefore, the client is currently pregnant. Educational objective: The GTPAL system notational components are G - gravida (number of pregnancies, regardless of outcome and including current pregnancies), T - term (37 wk 0 d gestation and beyond), P - preterm (20 wk 0 d through 36 wk 6 d gestation), A - abortions (before 20 wk 0 d gestation; spontaneous or induced), and L - currently living children. A A A A nurse is measuring a uterine fundal height for a client who is at 36 weeks gestation in supine position. The client suddenly reports dizziness and the nurse observes pallor and damp, cool skin. What should the nurse do first? 1. Assess fetal heart rate and pattern [5%] 2. Assess heart and lung sounds [2%]3. Notify the health care provider (HCP) immediately [1%] 4. Reposition the client into a lateral position [90%] Explanation: Supine hypotensive syndrome occurs when the weight of the abdominal contents compresses the vena cava causing decreased venous return to the heart. This results in low cardiac output (maternal hypotension) and reflex tachycardia. Manifestations include dizziness, pallor, and cold and clammy skin. The client should be immediately repositioned onto the right or left side until the symptoms subside. Prevention of this condition includes using a wedge under the client's hip while in a supine position. (Option 1) Decreased maternal cardiac output can result in decreased placental blood flow and fetal heart rate (FHR) abnormalities. FHR assessment also follows after the client is placed in the right or left lateral position. (Option 2) When supine hypotension is suspected, the client should first be placed in a lateral position. Blood pressure and pulse are checked to confirm the diagnosis. Assessing lung and heart sounds is not a priority. (Option 3) The HCP is notified after placing the client in a lateral position and completing the assessment. Educational objective: Supine hypotensive syndrome is usually seen in the third trimester of pregnancy when the weight of the uterine contents compresses the inferior vena cava. The resultant maternal hypotension is best treated initially by turning the client to the right or left side to relieve pressure on the vena cava. A A A The clinic nurse is collecting data on a pregnant client in the first trimester. Which finding is most concerning and warrants priority intervention? 1. Client has not been taking prenatal vitamins [13%] 2. Client is taking lisinopril to control hypertension [53%] 3. Client reports a whitish vaginal discharge [3%] 4. Client reports mild cramping pain in the lower abdomen [29%] Explanation: Angiotensin-converting enzyme (ACE) inhibitors (eg, enalapril, lisinopril, ramipril) and angiotensin II receptor blockers (eg, losartan, valsartan, telmisartan) should be avoided in clients who are planning to become pregnant. These drugs are teratogenic, leading to fetal renal and cardiac abnormalities, and are contraindicated in all stages of pregnancy.(Option 1) Prenatal supplements, especially folic acid and iron, are recommended during pregnancy. Although important, this is not a priority over discontinuing ACE inhibitors. (Option 3) Leukorrhea, a whitish vaginal discharge, is common during the prenatal period. The client should be instructed to call the health care provider if the discharge is accompanied by other signs or symptoms, such as a foul odor, redness, or itching. (Option 4) As the uterus enlarges, cramping may occur in the lower abdomen and inguinal region. This common finding can be caused by stretching of the round ligaments, and is usually not concerning in the absence of vaginal bleeding. Educational objective: Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are teratogenic and need to be discontinued when planning pregnancy. A A A A 37-weeks-pregnant woman comes to the emergency department with a fractured ankle. Which assessment finding is most concerning and requires the nurse to follow up? 1. Fetal heart rate remains 206/min [84%] 2. Fetus kicked 4 times in the past hour [2%] 3. Mother reports feeling 2 contractions every hour [5%] 4. Mother's hemoglobin is 11 g/dL (110 g/L) [7%] Explanation: Fetal tachycardia is a baseline of >160 beats/min for >10 minutes. Tachycardia needs evaluation and continued surveillance. The most sensitive indicators of fetus health are fetal movement and fetal heart rate. (Option 2) This is an expected finding. Monitoring fetal movement/kick counts is a primary method of fetal surveillance. The reassuring finding is when the movement equals or exceeds the established baseline. In general, 4 movements/hour or 10 distinct fetal movements within 2 hours is a reassuring finding. (Option 3) Braxton-Hicks contractions are felt mid-pregnancy onward. These painless, occasional physiological contractions are normal. The contractions are a concern if they become regular and persist. (Option 4) During pregnancy, hemoglobin can drop to 11 g/dL (110 g/L), a condition known as physiological anemia of pregnancy. Due to the increased oxygen requirements of pregnancy, the red blood cell count increases 30%. However, anemia can result from an increase in the plasma volume that is relatively larger than the increase in red blood cells. This lowered maternal hemoglobin is within the expected range.Educational objective: Sustained fetal tachycardia (>160/min for >10 minutes) is a concerning finding that requires further follow-up. A A A During the first prenatal assessment, the client reports the last normal menstrual period starting on March 1 and ending on March 5, but also slight spotting on March 23. The client had unprotected intercourse on March 15. Using Naegele's rule, what is the estimated date of birth? 1. December 8 [57%] 2. December 12 [22%] 3. December 22 [13%] 4. December 30 [6%] Explanation: Various methods to determine the estimated date of birth (EDB) include use of Naegele's rule, ultrasound, uterine height measurement (McDonald's measurement), and auscultation of fetal heart rate with a Doppler device. The most accurate dating of pregnancy involves use of ultrasound around the 16th-18th week of pregnancy. However, Naegele's rule can be used to quickly determine an EDB early in the pregnancy. This calculation uses the date of the first day of the last normal menstrual period (LMP) for determination of EDB. EDB = (LMP minus 3 months) + 7 days This client's LMP is March 1, minus 3 months = December 1. Add 7 days to obtain EDB = December 8. Clients who conceive in January, February, and most of March will deliver in the current year. Those who conceive after March will deliver in the following year; as a result, a third step is adding 1 to the current year to determine the estimated date of birth. For example, LMP of May 10, 2014, would have an EDB of February 17, 2015. It is important to note that Naegele's rule is based on a client having a menstrual cycle of 28 days. It therefore may not be as accurate if the client has a shorter or longer menstrual cycle. (Option 2) Using the last day of the LMP to calculate EDB provides an inaccurate due date as clients may have varying lengths of menstrual bleeding. (Option 3) Conception occurs around the time of ovulation and is about 14 days from the beginning of the LMP. Eggs are fertile for about 12-24 hours after ovulation with sperm able to remain fertile for 24-72 hours. Implantation of the trophoblast occurs about 7-10 days after fertilization. Using the conception date calculates the gestational age of the embryo approximately 2 weeks later than the true gestational age.(Option 4) Spotting around the time the next menstrual period is due may be considered normal and is probably caused by implantation of the trophoblast into the uterine endometrial lining. This is not considered a problem, but using this occurrence to date the pregnancy erroneously delays the EDB by 4 weeks. It is important to calculate EDB from the beginning of the last normal menstrual period. Educational objective: Naegele's rule provides a quick determination of the estimated date of birth (EDB). EDB = (LMP minus 3 months) + 7 days. If the LMP occurs in January, February, or March, the EDB will be in the current year. If the LMP occurs after March, the EDB will be in the next year. A A A Which client in a prenatal clinic should the nurse assess first? 1. Client at 11 weeks gestation with backache and pelvic pressure [13%] 2. Client at 16 weeks gestation with earache and sinus congestion [3%] 3. Client at 27 weeks gestation with headache and facial edema [78%] 4. Client at 37 weeks gestation with white vaginal discharge and urinary frequency [4%] Explanation: Gestational hypertension is new-onset high blood pressure (≥140/90 mm Hg) that occurs after 20 weeks gestation without proteinuria. The development of proteinuria with hypertension indicates preeclampsia, which may manifest with symptoms such as headache, visual disturbances, and facial swelling. This client is exhibiting symptoms of preeclampsia and should be assessed first (Option 3). Complications of preeclampsia may include thrombocytopenia, liver dysfunction, and renal insufficiency. Clients with preeclampsia must be monitored closely for sudden worsening, which can lead to serious complications, including eclampsia and/or HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets). (Option 1) Backache and pelvic pressure are common discomforts of pregnancy. The enlarging uterus stretches the supporting ligaments and may cause increased backache. Fluid retention from increasing blood volume causes pelvic congestion, which may be reported as pelvic pressure. (Option 2) Earache and sinus congestion are common discomforts during pregnancy that result from increased blood volume and fluid retention. This client should be assessed to rule out sinus and/or ear infection, but this is not the highest priority. (Option 4) The increase in estrogen and progesterone during pregnancy often results in leukorrhea, a mucoid, white vaginal discharge. Pressure on the bladder from the fetal head during the third trimester may cause diminished bladder capacity and urinary frequency without dysuria. These are common and expected findings.Educational objective: The nurse should assess the client with symptoms of potentially serious complications first before assessing the remaining clients. Signs of hypertensive disorders during pregnancy may include headache and facial edema. A A A A couple is excited about finding out the sex of their baby during ultrasound at 14 weeks gestation. What is the nurse's best response? 1. "Basic structures of major organs are not yet formed." [7%] 2. "External genitalia are not usually visualized until 21-24 weeks." [47%] 3. "If the baby is in the right position, the genitalia may be visualized." [42%] 4. "Sex cannot be determined until fetal movement is felt." [1%] Explanation: By the end of 12 weeks gestation, fetal sex can often be determined by the appearance of the external genitalia on ultrasound, depending on the quality of the image. (Option 1) By the end of 8 weeks gestation, all major organ systems are in place, and many are functioning in a simple way. By 7 weeks gestation, fetal heart tones can be detected. (Options 2 and 4) Clients typically begin feeling fetal movements in the second trimester at around 16-20 weeks gestation. Parous (have been pregnant before) clients can notice thisearlier than the nulliparous (first pregnancy). Fetal sex can be determined as early as the end of 12 weeks gestation. Educational objective: Fetal heart tones can be detected by 7 weeks gestation. Fetal sex may be determined on ultrasound as early as the end of 12 weeks gestation. Fetal movements are typically felt at around 16-20 weeks gestation. A A A The nurse is admitting a client at 41 weeks gestation for induction of labor due to oligohydramnios. Considering the client's indication for induction, what should the nurse anticipate? 1. Additional neonatal personnel present for birth [37%] 2. Intermittent fetal monitoring during labor [26%] 3. Need for forceps-assisted vaginal birth [13%] 4. Need for uterotonic drugs for postpartum hemorrhage [21%] Explanation: Amniotic fluid is produced by the fetal kidney and serves 2 major purposes - to prevent cord compression and promote lung development. Oligohydramnios is a condition characterized by low amniotic fluid volume. This can occur due to fetal kidney anomalies (eg, renal agenesis or urine flow obstruction) or fluid leaking through the vagina (eg, undiagnosed ruptured membranes). Fluid volume also declines gradually after 41 weeks. Small uterine size for gestational age or a fe [Show More]
Last updated: 3 years ago
Preview 1 out of 96 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 30, 2022
Number of pages
96
Written in
All
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Aug 30, 2022
Downloads
0
Views
146