*NURSING > QUESTIONS & ANSWERS > U WORLD PEDDIATRIA A A A. QUESTIONS AND ANSWERS, 100% PROVEN PASS RATE. GRADED A+ (All)
U WORLD PEDDIATRIA A A A. QUESTIONS AND ANSWERS, 100% PROVEN PASS RATE. GRADED A+
Document Content and Description Below
PEDDIATRIA A A A The nurse planning teaching for the parents of a child newly diagnosed with hemophilia will include information about which long-term complication? 1. Heart valve injury [33%] 2.... Intellectual disability [3%] 3. Joint destruction [54%] 4. Recurrent pneumonia [8%] Explanation: Hemophilia is a bleeding disorder caused by a deficiency in coagulation proteins. Clients with classic hemophilia, or hemophilia A, lack factor VIII. Clients with hemophilia B (Christmas disease) lack factor IX. When injured, clients with hemophilia should be monitored closely for external as well as internal bleeding. The most frequent sites of bleeding are the joints (80%), especially the knee. Hemarthrosis can occur with minimal or no trauma, with episodes beginning during toddlerhood when the child is active and ambulatory. Over time, chronic swelling and deformity can occur. (Option 1) Heart valve injury is common with rheumatic heart disease not hemophilia. (Option 2) Intellectual disability in children is commonly seen with fetal alcohol syndrome, Down syndrome, hypothyroidism, and lead poisoning. In rare cases, hemophilia can cause life-threatening intracranial bleeding. However, isolated intellectual disability is not seen. (Option 4) Recurrent pneumonia is commonly seen with cystic fibrosis not hemophilia. Educational objective: Clients with hemophilia are at risk for permanent joint destruction due to frequent bleeds into the joint spaces. Assisting clients with decreasing the incidence of bleeding episodes and prompt treatment when bleeding occurs can help minimize joint destruction. A A A The clinic nurse supervises a graduate nurse who is teaching the parents of a 2-year-old with acute diarrhea about home management. The nurse would need to intervene when the graduate nurse provides which instruction? 1. "Do not administer antidiarrheal medications to your child." [26%] 2. "Follow the bananas, rice, applesauce, and toast diet for the next few days." [32%]3. "Record the number of wet diapers and return to the clinic if you notice a decrease." [28%] 4. "Use a skin barrier cream such as zinc oxide in the diaper area until diarrhea subsides." [12%] Explanation: During bouts of acute diarrhea and dehydration, treatment focuses on maintaining adequate fluid and electrolyte balance. The first-line treatment is oral rehydration therapy, using oral rehydration solutions (ORSs) to increase reabsorption of water and sodium. Even if the diarrhea is accompanied by vomiting, ORS should still be offered in small amounts at frequent intervals. Continuing the child's normal diet (solid foods) is encouraged as it shortens the duration and severity of the diarrhea. The BRAT (bananas, rice, applesauce, and toast) diet is not recommended as it does not provide sufficient protein or energy. (Option 1) Use of antidiarrheal medications is discouraged as these have little effect in controlling diarrhea and may actually be harmful by prolonging some bacterial infections and causing fatal paralytic ileus in children. (Option 3) Parents should be taught to monitor their child for signs of dehydration by checking the amount of fluid intake, number of wet diapers, presence of sunken eyes, and the condition of the mucous membranes. (Option 4) Protecting the perineal skin from breakdown during bouts of diarrhea can be accomplished by using skin barrier creams (eg, petrolatum or zinc oxide). Educational objective: When a child is experiencing acute diarrhea, the priority is to monitor for dehydration. Treatment is accomplished with oral rehydration solutions and early reintroduction of the child's normal diet (usual foods). A A A The mother of a 6-year-old child with cystic fibrosis (CF) has received instruction on the use of pancreatic enzymes. Which statement made by the mother indicates a need for further teaching? 1. "I need to monitor the total amount of this medication that I give to my child every day." [6%] 2. "I should give this medication with or just before my child has a meal or snack." [10%]3. "It is okay for my child to chew this medication." [61%] 4. "It is okay to open the capsule and sprinkle the medicine on a tablespoon of applesauce." [21%] Explanation: In CF, unusually thick mucus obstructs the pancreatic ducts, preventing pancreatic enzymes (amylase, trypsin, and lipase) from reaching the small intestine. The result is malabsorption of carbohydrates, fats, and proteins; the inability to absorb fatsoluble vitamins (A, D, E, and K) is of particular concern. Gastrointestinal signs and symptoms of CF include flatulence, abdominal cramping, ongoing diarrhea, and/or steatorrhea. Nutritional therapy includes the administration pancreatic enzyme supplements with or just before every meal or snack (Option 2). These enzymes are enteric-coated beads designed to dissolve only in an alkaline environment similar to that of the small intestine. They must not be mixed with a substance that would cause them to dissolve prior to reaching the jejunum. Capsule contents may be sprinkled on applesauce, yogurt, or acidic, soft, room-temperature foods with pH <4.5. Capsules should be swallowed whole and not crushed or chewed; chewing the capsules could cause irritation of the oral mucosa. Excessive intake of pancreatic enzymes can result in fibrosing colonopathy (Option 1). (Option 4) This is a true statement; some children have difficulty taking a whole capsule. Capsule contents can be sprinkled in acidic substances such as applesauce. Capsules should not be taken with milk as they can cause it to curdle. Educational objective: Pancreatic enzyme supplements are used to aid the absorption of carbohydrates, fats, and proteins in a child with CF. They are taken with or just before every meal (not as needed); should be swallowed whole or sprinkled on an acidic food; and should not be crushed or chewed. They should not be taken with milk. Excessive intake could result in fibrosing colonopathy. A A A An 8-month-old infant is scheduled for a balloon angioplasty of a congenital pulmonic stenosis in the cardiac catheterization laboratory. Which finding should the nurse report to the health care provider (HCP) that could possibly delay the procedure? 1. Auscultation of a loud heart murmur [8%] 2. Infant has been NPO for 4 hours [9%] 3. Infant has polycythemia [52%]4. Infant has severe diaper rash [29%] Explanation: The presence of severe diaper rash should be reported to the HCP. This could potentially delay the procedure if the rash is in the groin area where access is planned for arterial cannulation. Candida, yeast, or bacteria may be present on the rash and could be introduced into the bloodstream with the arterial stick. (Option 1) A loud heart murmur can be an expected finding in a child with pulmonic stenosis. (Option 2) Children are allowed nothing by mouth for 4-6 hours or longer before the procedure. Younger children and infants may have a shorter period of NPO status and should be feed right up to the time recommended by the HCP. (Option 3) Infants and children with polycythemia may need IV fluids to prevent dehydration and hypoglycemia. Polycythemia will not cause a delay in the procedure. Educational objective: The nurse should report the presence of severe diaper rash to the HCP in an infant who has an interventional catheterization procedure planned. If the rash is near the groin area, the procedure may be delayed due to possible contamination at the insertion site. A A A When monitoring an infant with a left-to-right-sided heart shunt, which findings would the nurse expect during the physical assessment? Select all that apply. 1. Clubbing of fingertips 2. Cyanosis when crying 3. Diaphoresis during feedings 4. Heart murmur 5. Poor weight gain Explanation: Congenital heart defects that cause blood to shunt from the higher pressure left side of the heart to the lower pressure right side (eg, patent ductus arteriosus, atrial septal defect, ventricular septal defect) increase pulmonary blood flow. Left-to-right shunting results in pulmonary congestion, causing increased work of breathing and decreased lung compliance. Compensatory mechanisms (eg, tachycardia,diaphoresis) result from sympathetic stimulation. Clinical manifestations of acyanotic defects may include: Tachypnea Tachycardia, even at rest Diaphoresis during feeding or exertion (Option 3) Heart murmur or extra heart sounds (Option 4) Signs of congestive heart failure Increased metabolic rate with poor weight gain (Option 5) (Option 1) Clubbing of the fingertips is associated with chronic hypoxia caused by decreased pulmonary circulation as occurs with right-to-left heart defects. (Option 2) Right-to-left congenital heart defects (eg, cyanotic defects) impede pulmonary blood flow (eg, tetralogy of Fallot, transposition of the great vessels) and cause cyanosis, which is evident shortly after birth and during periods of physical exertion. Educational objective: Left-to-right cardiac shunts (eg, patent ductus arteriosus, atrial septal defect, ventricular septal defect) result in excess blood flow to the lungs. Manifestations include heart murmur, poor weight gain, diaphoresis with exertion, and signs of heart failure. A A A A 12-month-old with Kawasaki disease received IV immunoglobulin (IVIG) 2 months ago. The child is in the clinic for follow-up and scheduled immunizations. Which vaccine should be delayed? Select all that apply. 1. Haemophilus influenzae type b (Hib) 2. Hepatitis B (Hep B) 3. Measles, mumps, rubella (MMR) 4. Pneumococcal conjugate (PCV) 5. Varicella Explanation: Kawasaki disease is treated with aspirin and IVIG to prevent coronary artery aneurysms. Antibodies acquired from the IVIG therapy will remain in the body for up to 11 months and may interfere with the desired immune response to live vaccines. Therefore,live vaccines (eg, varicella, MMR) should be delayed for 11 months after IVIG administration as this therapy may decrease the child's ability to produce the appropriate amount of antibodies to provide lifelong immunity (Options 3 and 5). (Option 1) Hib vaccine is not a live vaccine, and final dose (fourth) is recommended between age 12-15 months, according to the Centers for Disease Control and Prevention (CDC). (Option 2) Hep B vaccine is not a live vaccine; the CDC recommends that the final dose (third) be administered between age 6-18 months. (Option 4) PCV is also not a live vaccine, and the final dose (fourth) is recommended between age 12-15 months, according to the CDC. Educational objective: Live vaccines (eg, varicella, MMR) should be delayed for up to 11 months after IVIG administration as IVIG therapy may decrease the child's ability to produce the appropriate amount of antibodies to provide lifelong immunity A A A Several clients check into the emergency department at the same time. Which client should be seen first? 1. 6-year-old with blood-streaked stools [19%] 2. 10-year-old with epilepsy who had a short seizure at home and is asleep [26%] 3. 15-year-old with dental trauma and tooth avulsion [25%] 4. Newborn who spits up after every feed [28%] Explanation: At age 15, clients should have their permanent teeth. If tooth avulsion occurs, there is limited time (≤1 hour, longer if placed in cold milk) until death of the tooth. This is a time-sensitive condition and the client should be seen first to avoid loss of a permanent tooth. (Option 1) This client needs to be assessed for the cause of blood in the stool. However, this is not considered a medical emergency as long as only streaks and not large volumes of blood are present. Large volumes can represent a gastrointestinal bleed, which is an emergency.(Option 2) A client who is not currently seizing is considered stable. It is normal for a child to be sleepy following a seizure. The child should be assessed to ensure that air exchange is appropriate. (Option 4) It is normal for newborns to spit up after every feed as they are still adapting to eating. The client should be assessed for hydration status and appropriate weight gain. Educational objective: In tooth avulsion, there is a limited amount of time (≤1 hour) before death of the affected tooth. These clients need prompt treatment to save a permanent tooth. A A A The nurse in the emergency department is assessing a 12-month-old diagnosed with intussusception. Which findings should the nurse expect? Select all that apply. 1. Palpable olive-shaped mass in epigastrium 2. Palpable sausage-shaped mass in upper right quadrant 3. Projectile vomiting containing blood 4. Screaming and drawing the knees up to the chest 5. Stool mixed with blood and mucus Explanation: Intussusception is a common obstructive disorder in infancy that occurs when one segment of the bowel telescopes into another. The classic clinical triad is intermittent, severe, crampy abdominal pain; a palpable "sausage-shaped" mass on the right side of the abdomen; and "currant jelly" stools. Other manifestations include inconsolable crying, drawing the knees up to the chest during episodes of pain, and vomiting. The child may appear normal and comfortable between episodes. (Option 1) Infants with infantile hypertrophic pyloric stenosis often present with excessive hunger (frequent feeder), a palpable olive-shaped mass in the epigastrium to the right of the umbilicus, and projectile vomiting (can be up to 3 feet). (Option 3) Projectile vomiting (without blood) is seen with pyloric stenosis and elevated intracranial pressure. Bloody vomiting is seen with gastric ulcers and variceal bleed. Intussusception causes non-projectile vomiting that is usually non-bloody, but stools mixed with mucus and blood are seen. Educational objective:The classic clinical triad of intussusception is intermittent, severe, crampy abdominal pain; a palpable sausage-shaped mass on the right side of the abdomen; and currant jelly stools. A A A The nurse is caring for a pediatric client with end-stage leukemia who is on comfort care and is unresponsive. The child's parent asks, "How can you tell if my child is in pain?" Which of these would the nurse describe as signs of discomfort? Select all that apply. 1. Blank facial expression 2. Facial grimacing 3. Groaning 4. Knees bent up near chest 5. Lying still Explanation: FLACC scale (face, legs, activity, cry, consolability) The nurse will provide teaching on signs that should prompt the parent to administer asneeded pain medication to the child. (Option 1) A child who is comfortable will usually have a neutral facial expression. A child in pain is likely to exhibit grimacing, frowning, or clenching of the jaw, based on the FLACC face assessment. (Option 5) A child who is comfortable will be lying quietly. A child who is squirming and moving is more likely to be in pain, based on the FLACC activity assessment. Educational objective: It is difficult to assess for pain in the nonverbal client, particularly if the person is unresponsive at the end of life. The FLACC scale is an accurate method of assessing pain in the nonverbal child. This tool should be used to teach parents how to promote comfort for their nonverbal child A A A A 2-month-old infant is brought to the pediatric emergency department due to vomiting and diarrhea for 4 days. Assessment findings include lethargy, poor feeding, sunken fontanel, temperature 100.4 F (38 C), heart rate 134/min, and respiratory rate 28/min. Which prescription from the health care provider would be the priority? 1. Acetaminophen elixir 50 mg by mouth every 6 hours [1%]2. Intravenous (IV) ampicillin 240 mg every 12 hours [2%] 3. IV normal saline bolus 20 mL/kg over 1 hour [92%] 4. Obtain a stool culture [4%] Explanation: Infants and young children have a higher body water percentage than older children and adults. As a result, they become dehydrated quickly with fluid losses caused by vomiting and diarrhea. Signs of severe dehydration include lethargy, sunken fontanel, poor feeding, increased heart rate, and increased respiratory rate. When an infant's basic vital signs are intact and there is severe dehydration, the priority is to rehydrate. Normal saline is the fluid of choice for a bolus in an infant. Electrolytes may be added to the maintenance IV fluids if needed. (Option 1) A temperature of 100.4 F (38 C) is a mild fever in an infant and may indicate the need for acetaminophen. However, hydration of the infant takes priority over this action. (Option 2) Antibiotics may be indicated due to the infant's increased temperature. The fluid bolus is of higher priority due to the severe dehydration. (Option 4) The history of vomiting and diarrhea for 4 days would indicate a stool culture to determine a causative agent. This may be obtained after administration of the fluid bolus Educational objective: Severe dehydration occurs more rapidly in infants and young children than in adults due to increased body water percentage. When severe dehydration occurs in an infant, the priority is to rehydrate as appropriate. A A A A nurse is leading a discussion with a group of new parents. A parent asks about the first food to introduce to a 5-month-old infant. What is the best response by the nurse? 1. "Finely mashed fruit, such as bananas, is given." [8%] 2. "Iron-fortified cereal, such as rice cereal, is offered." [82%] 3. "Mashed egg yolk is a good choice." [0%] 4. "Pureed carrots are well tolerated." [8%] Explanation Before age 6 months, an infant should receive only breast milk or formula. The infant is ready physiologically and developmentally for the addition of solid foods to the diet at age 4-6 months as iron stores have declined. Iron-fortified cereals (rice, barley,oatmeal, high protein) should be offered. Rice cereal is preferred due to the low risk of allergy and ease of digestion (Option 2). (Options 1, 3, and 4) Fruit juices and pureed fruit are typically offered next as a source of vitamin C. Vitamin C increases iron absorption. These are followed by strained vegetables, with yellow preferred due to the higher vitamin content. Foods are introduced one at a time to identify any allergies. Foods known to commonly induce allergy (eg, peanuts, eggs, seafood, whole milk) should not be introduced before age 1 year. Educational objective: Solid foods are introduced at age 4-6 months, with iron-fortified cereals (usually rice) offered first due to their low allergy potential and ease of digestion. Fruit juices and pureed fruits containing vitamin C are then offered, followed by strained vegetables. Egg yolks and whites are introduced at age 1 year. A A A The health care provider (HCP) prescribes an oral iron suspension for 3 months for a 2- year-old with iron deficiency anemia. Which instructions should be given to the parent? Select all that apply. 1. Administer doses between meals 2. Administer doses with citrus juice 3. Obtain a full 3-month supply from the pharmacy 4. Place medicine at the back of the mouth 5. Report black, tarry stools to the HCP immediately Explanation: Iron deficiency anemia, the most common chronic nutritional disorder, often occurs in toddlers due to insufficient intake of dietary iron or excessive consumption of milk. It is treated with increased consumption of iron-rich foods (eg, leafy green vegetables, red meats, poultry, dried fruit, fortified cereal) and oral iron supplementation. Key instructions for safe, effective administration of oral iron supplements include: Administer between meals - Concentrations of stomach acid are higher between meals, breaking down the iron to an easily absorbed state (Option 1) Give with citrus juice - Absorption is enhanced when taken with a good source of vitamin C, such as orange juice or other citrus fruit (Option 2)Place medicine at the back of the mouth - Liquid iron can cause temporary staining of the teeth. Using a dropper or straw to direct the iron toward the back of the mouth can reduce this risk (Option 4). Avoid giving with milk - Milk and other products with high amounts of calcium reduce adequate absorption of iron supplements Keep no more than a 1-month supply on hand - When ingested in extreme quantities, iron can be toxic or even lethal. Only short-term amounts should be stored in the home, in a child-proof location (Option 3). (Option 5) Black or green tarry stools are an expected effect of oral iron supplements and are considered an indicator of proper compliance. Educational objective: Oral iron supplements should be given between meals and consumed with citrus juice to promote absorption, and administered to the back of the mouth to prevent tooth staining. No more than a 1-month supply of supplements should be kept on hand to reduce the risk of accidental poisoning. Oral iron should not be taken with milk. A A A The nurse cares for an 11-lb (5-kg) infant admitted with dehydration and prepares to calculate intake and output over an 8-hour shift. Using the data in the exhibit, calculate the total output in milliliters for the 8-hour shift. Record your answer as a whole number. Click on the exhibit button for additional information. Intake and output record Emesis 120 mL Wet diaper 1 50 g Wet diaper 2 52 g Wet diaper 3 46 g *Weight of a dry diaper = 30 g Answer: 178 (mL) Explanation: To measure the urinary output of an infant in diapers, subtract the weight of the diaper when dry from its weight when wet. One (1) gram of weight is equal to one (1) milliliter of fluid. Adequate urinary output for an infant is 2 mL/kg/hr. Calculation:Urine output in diapers: Diaper 1: 50 − 30 = 20 g Diaper 2: 52 − 30 = 22 g Diaper 3: 46 − 30 = 16 g Total mg of urine: 58 g = 58 mL Total output (Emesis) + (Urine) = 120 mL + 58 mL = 178 mL Educational objective: Urinary output for a child in diapers is calculated by subtracting the dry weight of the diaper from its weight when wet. One (1) gram of weight is equal to one (1) milliliter of fluid. A A A What is the best activity for a school-aged child hospitalized for vaso-occlusive sickle cell crisis? 1. Finger painting [18%] 2. Playing a game of Chinese checkers in the activity room [16%] 3. Playing video games [12%] 4. Watching a favorite movie [52%] Explanation: A child in vaso-occlusive sickle cell crisis will be experiencing a high level of pain due to the occlusion of small blood vessels from increased red blood cell sickling. Supportive and symptomatic treatment includes round-the-clock pain management with opioids, intravenous fluids for hydration, and bed rest to decrease energy expenditure and oxygen demand. Age-specific nonpharmacologic strategies should also be implemented to manage pain and help limit the amount of needed narcotic analgesia. For a school-aged child, such activities include distraction (watching TV, listening to music, reading), relaxation, guided imagery, warm soaks, positioning, and gentle massage. (Option 1) Finger painting is messy and best done in the activity room; it is not appropriate for a child confined to bed.(Option 2) A child must be on bed rest when in vaso-occlusive sickle cell crisis. Playing a game in the activity room does not maintain bed rest and would be too stimulating for the child. (Option 3) Playing video games may be too exciting and stimulating for the child; an environment low in stimuli will promote rest. Educational objective: Supportive and symptomatic treatment for vaso-occlusive sickle cell crisis includes pain management and bed rest. Nonpharmacologic measures to alleviate pain include distraction (watching TV, listening to music, reading), relaxation, guided imagery, warm soaks, positioning, and gentle massage. A A A A 2-year-old in the emergency department is suspected of having intussusception. Which assessment finding should the nurse expect? 1. Black, sticky stools [2%] 2. Greasy, foul-smelling stools [6%] 3. Stools mixed with blood and mucus [56%] 4. Thin, "ribbon-like" stools [34%] Explanation: Intussusception is an intestinal obstruction that occurs when a segment of the bowel folds (ie, telescopes) into another segment. Pressure gradually increases within the bowel, causing ischemia and leakage of blood and mucus into the lumen, which produces the characteristic stool mixed with blood and mucus (ie, red, "currant jelly"). Initially, some infants may have only general symptoms (eg, irritability, diarrhea, lethargy). Subsequently, episodes of sudden abdominal pain (cramping), drawing the knees up to the chest, and inconsolable crying are seen. After an episode, the infant may vomit and then appear otherwise normal. Assessment may show a sausage-shaped abdominal mass. (Option 1) Melena (dark red or black, sticky stool) is an indication of an upper gastrointestinal (UGI) bleed. Gastritis is a common cause of UGI bleeding in infants and toddlers. (Option 2) Oily or bulky, foul-smelling stool is an indication of excess fat in the stool (steatorrhea) from malabsorption. This is characteristic of pancreatic insufficiency, cystic fibrosis, or celiac disease.(Option 4) Thin, ribbon-like stool is characteristic of Hirschsprung disease (congenital aganglionic megacolon). Bowel obstruction is caused by failure of the internal sphincter to relax. Educational objective: The classic symptom triad of intussusception is abdominal pain, "currant jelly" stools, and a sausage-shaped abdominal mass. However, it is more common for clients to have episodes of sudden abdominal pain, inconsolable crying, and vomiting followed by periods of normal behavior. A A A The registered nurse is performing triage at a pediatric emergency department. Which client should be seen first? 1. Child with history of cystic fibrosis (CF) has new yellow sputum and cough today [18%] 2. Crying infant with fiery redness and moist papules in the diaper region [6%] 3. Grade-school client with swollen ecchymotic ankle after playing basketball [2%] 4. Adolescent client with abdominal pain, heart rate 120/min, and respirations 26/min [72%] Explanation: The client with abdominal pain has abnormal vital signs, which is a sign of a systemic condition. Adult criteria apply to adolescent clients in terms of physiological signs/symptoms. A pulse of 120/min signals dehydration and this client's respirations are above normal. This is the most serious acuity. (Option 1) The client with a history of CF would be treated second as clients with CF have chronic respiratory issues related to the thick mucus plugging the airways. This client will probably need antibiotics but is stable and can wait. The severity of the situation is considered when prioritizing client care based on airway, breathing, and circulation (ABC). The seriousness of the adolescent client's condition related to "C" (dehydration) is a priority over a relatively stable "B." There is nothing indicating that this client is in respiratory distress. (Option 2) The infant has diaper dermatitis from irritation of urine and stool on the skin. A secondary infection with Candida albicans can occur. Diaper dermatitis is most common in infants age 9-12 months. Ointment will be provided. Mild diaper dermatitis is treated with a topical water-impermeable barrier (eg, zinc oxide). If the infant has an infection with Candida albicans, an antifungal topical medication is also used. When care must beprioritized, young children do not automatically go first. Prioritization is decided by the client's acuity. (Option 3) The grade-school client has a limited extremity injury and the priority principle is always "life before limb." Therefore, the client with abdominal pain is more important. Educational objective: In prioritization, the severity of ABC is more important than absolute order. As a result, a severe "C" client comes before a stable "B" client. The priority principle is to take "life before limb" in this order. When care must be prioritized, young children do not automatically go first. A A A The nurse is reviewing anticipatory guidance with the parents of a 6-month-old infant with phenylketonuria. Which statements by the nurse are appropriate? Select all that apply. 1. "A low-phenylalanine diet is required." 2. "Meat and dairy products should not be introduced into the diet." 3. "Phenylketonuria is self-limiting and usually resolves by adulthood." 4. "Special infant formula is required." 5. "Tyrosine should be removed from the diet." Explanation: Phenylketonuria (PKU) is one of a few genetic inborn errors of metabolism. Individuals with PKU lack the enzyme (phenylalanine hydroxylase) required for converting the amino acid phenylalanine into the amino acid tyrosine. As unconverted phenylalanine accumulates, irreversible neurologic damage can occur. A low-phenylalanine diet is essential in the treatment of PKU (Option 1). Phenylalanine cannot be entirely eliminated from the diet as it is an essential amino acid and necessary for normal development. The diet must meet nutritional needs while maintaining phenylalanine levels within a safe range (2-6 mg/dL [120-360 µmol/L] for clients age <12). There is no known age at which the diet can be discontinued safely, and lifetime dietary restrictions are recommended for optimal health (Option 3). Management of the client with PKU includes: Monitoring serum levels of phenylalanineIncluding synthetic proteins and special formulas (eg, Lofenalac, Phenyl-Free) in the diet (Option 4) Eliminating high-phenylalanine foods (eg, meats, eggs, milk) from the diet (Option 2) Encouraging the consumption of natural foods low in phenylalanine (most fruits and vegetables) (Option 5) Restriction of dietary tyrosine is not necessary. Tyrosine levels in clients with PKU may be normal or slightly decreased. Educational objective: Phenylketonuria requires lifetime dietary restrictions. Infants should be given special formulas (eg, Lofenalac). For children and adults, high-phenylalanine foods (eg, meats, eggs, milk) should be restricted and replaced with protein substitutes. A A A A nurse is assessing a 1-month-old infant with an atrial septal defect (ASD). Which assessment finding does the nurse expect? 1. Muffled heart tones [19%] 2. Murmur [53%] 3. Cyanosis [19%] 4. Weak femoral pulses [6%] Explanation: The nurse would expect to hear a murmur with an atrial septal defect. This defect is an abnormal opening between the right and left atria, allowing blood from the higher pressure left atrium to flow into the lower pressure right atrium. The back-andforth flow of blood between the 2 chambers causes a vibration that is heard as a murmur on auscultation. ASD has a characteristic systolic murmur with a fixed split second heart sound. Some clients may also have a diastolic murmur. (Option 1) Muffled heart tones are not typical in ASD. Muffled heart tones that are heard postsurgical intervention are concerning for cardiac tamponade. (Option 3) Atrial and ventricular septal defects are acyanotic congenital heart defects because the blood from the high pressure left side (oxygenated blood) goes to the low pressure right side.(Option 4) Weak lower and strong upper extremity pulses are present in coarctation of the aorta. Educational objective: In a child with atrial septal defect, the nurse would expect to hear a heart murmur on auscultation of heart sounds. A A A The nurse is caring for an infant diagnosed with Hirschsprung disease who is awaiting surgery. Which assessment finding requires the nurse's immediate action? 1. Abdominal distension with no change in girth for 8 hours [6%] 2. Did not pass meconium or stool within 48 hours after birth [26%] 3. Episode of foul-smelling diarrhea and fever [26%] 4. Excessive crying and greenish vomiting [39%] Explanation: Hirschsprung disease (HD) occurs when a child is born with some sections of the distal large intestine missing nerve cells, rendering the internal anal sphincter unable to relax. As a result, there is no peristalsis and stool is not passed. These newborns exhibit symptoms of distal intestinal obstruction. They have a distended abdomen and will not pass meconium within the expected 24-48 hours. They also have difficulty feeding and often vomit green bile. Surgical removal of the defective section of bowel is necessary and colostomy may be required. A potentially fatal complication is Hirschsprung enterocolitis, an inflammation of the colon, which can lead to sepsis and death. Enterocolitis will present with fever; lethargy; explosive, foul-smelling diarrhea; and rapidly worsening abdominal distension. (Option 1) Mild to moderate abdominal distension is an expected finding with a diagnosis of HD; however, increasing abdominal girth is a serious finding that must be reported. (Option 2) Failure to pass meconium or stool within 24-48 hours after birth is an expected finding of HD. (Option 4) Bilious vomiting and excessive crying are expected findings of HD. In enterocolitis, vomiting can occur more frequently and the client appears more ill. Educational objective:Enterocolitis, a potentially fatal complication of Hirschsprung disease, is characterized by explosive, foul-smelling diarrhea; fever; and worsening abdominal distension. A A A The clinic nurse interviews the parents of a 6-month-old about the child's diet and feeding schedule. Which parent statement causes the nurse the most concern? 1. "Apples are a healthy food, so we often make apple pie for our child." [5%] 2. "Chopped pears are one of our child's favorite foods." [8%] 3. "Oatmeal with fresh honey is our child's favorite breakfast." [57%] 4. "We have found TV dinners to be convenient as they have both meat and vegetables." [28%] Explanation: Although more than one of these parent comments are concerning, the most concerning is feeding honey to a child under age 1 year. Honey (especially raw or wild) is not recommended for children under age 1 due to the risk for infant botulism. An infant under age 1 has an immature gut system that can allow Clostridium botulinum spores contaminated in honey to colonize the gastrointestinal tract and release toxin that causes botulism. Botulinum toxin produces muscle paralysis by inhibiting the release of acetylcholine at the neuromuscular junction. Infants often present with constipation, diminished deep tendon reflexes, and generalized weakness. Additional symptoms are lack of head control, difficulty in feeding, and decreased gag reflex, which can progress to respiratory failure. Isolation of the organism from the child's stool can take several days; therefore, diagnosis is usually made by history, and treatment with botulism immune globulin is started before laboratory results are known. (Option 1) Apple pie is not the best way to serve apples to a 6-month-old as the other ingredients add too much fat and sugar. This would need to be addressed but is not a priority over the use of honey. (Option 2) Raw fruits are appropriate for a 6-month-old. (Option 4) Although TV dinners contain meat and vegetables, they are not the best source of food for an infant due to the high sodium content. This would need to be addressed after the use of honey is addressed. Educational objective:Due to the risk of infant botulism, honey should not be given to children under age 1 year. A A A The home health nurse is visiting an infant who recently had surgery to repair tetralogy of Fallot. The nurse should teach the parents to report which findings indicative of heart failure to the health care provider (HCP)? Select all that apply. 1. Cool extremities 2. Increase in appetite 3. Puffiness around the eyes 4. Reduction in number of wet diapers 5. Weight loss Explanation: Heart failure may develop after surgical repair of tetralogy of Fallot, and infants and children can quickly decompensate hemodynamically when it occurs. Clinical manifestations are grouped into 3 primary categories— impaired myocardial pumping, pulmonary congestion, and systemic venous congestion. (Option 2) The infant would have a decrease in appetite with heart failure symptoms. (Option 5) The infant would more likely have experienced weight gain due to fluid retention. Educational objective: The nurse should teach parents of an infant or child with a repaired congenital heart defect to recognize and report signs and symptoms of heart failure to the HCP. These may include rapid breathing rate; rapid heart rate at rest; dyspnea; activity intolerance (especially during feeding in infants); pale, cool extremities; weight gain; reduction in wet diapers; and puffiness around the eyes.A A A The nurse receives 4 prescriptions for a child diagnosed with hemophilia A who was brought to the emergency department following an injury on the school playground. The child has vomited once and has a headache. Which prescription should the nurse carry out first? 1. Administer IV factor VIII [39%] 2. Administer IV ondansetron [9%] 3. Blood draw for hemoglobin [8%] 4. CT scan of the head [42%] Explanation: Hemophilia is a bleeding disorder caused by a deficiency in coagulation proteins. Treatment consists of replacing the missing clotting factor and teaching the client about injury prevention. Clients with hemophilia who are injured should be monitored closely for bleeding (eg, intracranial bleeds, bleeding into joints). Signs of an intracranialbleed include lethargy, headache, irritability, and vomiting. An intracranial bleed is lethal if unchecked, so administration of factor VIII to a client with hemophilia A is the first order of action, followed by a CT scan. (Option 2) Ondansetron (Zofran) can be given to treat nausea/vomiting, but administration of factor VIII is the priority. (Option 3) Laboratory studies, particularly hemoglobin and hematocrit levels, are necessary, but the priority is to administer factor VIII. (Option 4) A CT scan should be performed for diagnostic purposes, but the bleeding must be stopped emergently. Even if bleeding is evident on CT scan and the client is taken to the operating room, surgery cannot be performed without simultaneous factor VIII replacement. Educational objective: A client with hemophilia A and a head injury is at risk for intracranial bleeding (which sometimes occurs spontaneously). When intracranial or another form of bleeding is suspected, administration of factor VIII is a priority as the client's body cannot form a clot without it. A A A The school nurse is teaching a class of 10-year-old children about prevention of dental caries. Which recommendations would be part of the nurse's teaching plan? Select all that apply. 1. Chew sugar-free gum 2. Drink fruit drinks/juices instead of sugary, carbonated beverages 3. Include milk, yogurt, and cheese in dietary intake 4. Minimize consumption of sweet, sticky foods 5. Rinse mouth with water after meals when brushing is not possible Explanation: Dental caries (ie, cavities) form when bacteria (eg, Streptococcus mutans) digest carbohydrates in the mouth, producing acids that break down tooth enamel and cause mineral loss. Oral hygiene and dietary intake are significant factors contributing to the development of caries. Clients should increase intake of cariostatic foods, which have an inhibitory effect on the progression of dental caries (eg, dairy products, whole grains, fruits and vegetables, sugarfree gum containing xylitol) (Options 1 and 3). Cariogenic foods increase the risk for cavities and should be avoided. These include refined, simple sugars; sweet, sticky foods such as dried fruit (eg, raisins) and candy; and sugary beverages (eg, colas and other carbonated beverages, fruit drinks/juices) (Option 4). Additional practices to prevent dental caries include: Brushing after meals Flossing at least twice a day Rinsing the mouth with water after meals or snacks (Option 5) Drinking tap water rather than bottled water (most tap water sources add fluoride to promote dental health, whereas most bottled water does not contain fluoride) Finishing meals with a high-protein food (Option 2) Fruit drinks/juices contain high amounts of simple sugars; substituting these for other sugary beverages does not prevent dental caries. Whole fruits are better choices. Educational objective: Risk for dental caries can be reduced by avoiding highly cariogenic foods (eg, refined, simple sugars; sugary beverages; sweet, sticky foods), increasing intake of cariostatic foods (eg, dairy products, whole grains, fruits and vegetables), and maintaining oral hygiene (eg, brushing teeth, rinsing after meals). A A A The nurse is caring for a child with Kawasaki disease who is receiving IV immunoglobulin. The child's parent wants to know why this treatment is required. The nurse explains that this therapy is given to: 1. Fight the infection [47%] 2. Minimize rash [5%] 3. Prevent heart disease [36%] 4. Reduce spleen size [11%] Explanation: Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is characterized by ≥5 days of fever, bilateral nonexudative conjunctivitis, mucositis, cervical lymphadenopathy, rash, and extremity swelling. Coronary artery aneurysms are the most serious potential sequelae in untreated clients, leading to complications such asmyocardial infarction and death. Echocardiography is used to monitor these cardiovascular complications. Intravenous immunoglobulin (IVIG) along with aspirin is used to prevent coronary aneurysms and subsequent occlusion. KD is one of the few pediatric illnesses in which aspirin therapy is warranted due to its antiplatelet and anti-inflammatory properties. However, parents should be cautioned about the risk of Reye syndrome. Cardiopulmonary resuscitation should also be taught to parents of children with coronary artery aneurysms. (Option 1) KD is a vasculitis of unknown etiology, but it is not an infectious process. Because the child will often have a similar clinical presentation to that of an infection (eg, persistent fever, inflammatory immune response), KD may be mistaken for a bacterial or viral illness. (Option 2) Polymorphous rash of the trunk and extremities is an expected finding in a child with KD. Cool compresses, unscented lotions, and loose-fitting clothing can minimize discomfort. IVIG is not given to control rash. (Option 4) Lymphadenopathy (usually a single palpable anterior cervical node >1.5 cm) and splenomegaly are included in the clinical presentation of KD. IVIG therapy is not indicated to reduce incidence of these findings. Educational objective: IVIG along with aspirin is the recommended initial treatment for Kawasaki disease, with the primary goal of coronary disease prevention. A A A The nurse is planning care for a child being admitted with Kawasaki disease and should give priority to which nursing intervention? 1. Apply cool compresses to the skin of the hands and feet [10%] 2. Monitor for a gallop heart rhythm and decreased urine output [60%] 3. Prepare a quiet, non-stimulating, and restful environment [21%] 4. Provide soft foods and liberal amounts of clear liquids [7%] Explanation: Kawasaki disease (KD) is a childhood condition that causes inflammation of arterial walls (vasculitis). The coronary arteries are affected in KD, and some children develop coronaryaneurysms. The etiology of KD is unknown; there are no diagnostic tests to confirm the disease, and it is not contagious. KD has 3 phases: Acute - sudden onset of high fever that does not respond to antibiotics or antipyretics. The child becomes very irritable and develops swollen red feet and hands. The lips become swollen and cracked, and the tongue can also become red (strawberry tongue). Subacute - skin begins to peel from the hands and feet. The child remains very irritable. Convalescent - symptoms disappear slowly. The child's temperament returns to normal. Initial treatment consists of IV gamma globulin (IVIG) and aspirin. IVIG creates high plasma oncotic pressure, and signs of fluid overload and pulmonary edema develop if it is given in large quantities. Therefore, the child should be monitored for symptoms of heart failure (eg, decreased urinary output, additional heart sounds, tachycardia, difficulty breathing). (Option 1) During the acute phase (swollen hands and feet), skin discomfort can be eased with cool compresses and lotions. No treatment is needed in the subacute phase (skin peeling), but the new skin might be very tender. (Option 3) The child will be very irritable during the acute phase of KD. A non-stimulating, quiet environment will help to promote rest. After a KD episode, it is important for parents to understand that their child's irritability may last for up to 2 months and that follow-up appointments for cardiac evaluation are important. (Option 4) During the acute phase (painful swollen lips and tongue), the child should be given soft foods and clear liquids as these are tolerated best Educational objective: Kawasaki disease causes inflammation of the arterial walls and can lead to scarring of the coronary arteries or development of coronary aneurysms. Treatment consists of aspirin and substantial infusion of IV gamma globulin. The affected child must be monitored for signs of heart failure. A A A A school-age child is brought to the emergency department due to nausea, vomiting, and severe right lower quadrant pain. The child's white blood cell count is 17,000/mm3 (17.0 x 109/L). Which statement by the child is of most concern to the nurse? 1. "I am hungry and they will not let me eat." [5%] 2. "I don't like hospitals and I want to go home." [1%]3. "I'm so tired." [15%] 4. "My belly doesn't hurt anymore." [77%] Explanation: A child with acute-onset right lower quadrant abdominal pain, nausea, and vomiting and a high white blood cell count likely has acute appendicitis. Appendicitis is a serious condition that usually requires emergency surgery due to the risk of appendix rupture. The pain results from swelling and inflammation of the appendix. However, once the appendix ruptures, pain is relieved only temporarily and will return with full-blown peritonitis and sepsis. (Option 1) Clients diagnosed with appendicitis often need immediate surgery. The client will be placed NPO until surgery is performed to remove the appendix. (Option 2) This is a normal statement that will be made by many children. (Option 3) Tiredness is nonspecific and could be due to many reasons (eg, pain medication). Educational objective: Appendicitis is an acute condition that needs immediate surgical intervention to prevent appendix rupture and subsequent peritonitis and sepsis A A A A nurse is providing education to the parents of a child diagnosed with chronic allergic rhinitis that is triggered by household and environmental allergies. Which statements by the parents indicate that the teaching has been effective? Select all that apply. 1. "My wife plans to wipe down our child's furniture with a damp rag every other day." 2. "Our child needs plastic covers for the mattress and pillow." 3. "We must give away the family dog." 4. "We will keep the windows open during warm weather to air out the house." 5. "We will replace the carpet with hardwood floors throughout the house." Explanation: Symptoms of allergic rhinitis include sneezing, nasal drainage, nasal congestion, and pruritus of the eyes or nose. Clients and their families can help prevent these symptoms byidentifying individual triggers (eg, dust, mold, pollen, dander) and implementing strategies to reduce or avoid exposure to known allergens. Key measures to reduce exposure to household and environmental allergens include the following: Installing high-efficiency particulate air filters in the home air conditioning system Keeping windows closed and staying indoors, particularly during times of heavy pollen Using hypoallergenic pillow and mattress covers to prevent exposure to dust mites (Option 2) Reducing or eliminating carpet and area rugs from the home (Option 5) Regularly mopping hard floors and damp-dusting furniture (at least weekly) (Option 1) (Option 3) If the client is not allergic to animal dander, keeping a household pet may be acceptable. However, to prevent pets from bringing environmental allergens into the home, further precautions may need to be implemented, such as more frequent baths or additional doormats. (Option 4) Open windows allow environmental allergens, such as pollen, to enter the home. To prevent exposure to these particles, susceptible clients should keep exterior windows closed and avoid spending long periods of time outdoors. Educational objective: Prevention of symptoms plays an important role in the management of chronic allergic rhinitis. Preventive measures to reduce exposure include using hypoallergenic pillow and mattress covers, eliminating carpet in the home, keeping windows closed, installing highefficiency air filters, regularly mopping hard floors, and frequently damp-dusting furniture A A A A 3-month-old infant has irritability, facial edema, a 1-day history of diarrhea with adequate oral intake, and seizure activity. During assessment, the parents state that they have recently been diluting formula to save money. Which is the most likely cause for the infant's symptoms? 1. Hypernatremia due to diarrhea [9%] 2. Hypoglycemia due to dilute formula intake [16%] 3. Hypokalemia due to excess gastrointestinal output [11%]4. Hyponatremia due to water intoxication [63%] Explanation: Water intoxication (water overload) resulting in hyponatremia may occur in infants when formula is diluted to "stretch" the feeding to save money. Hyponatremia may also result from ingestion of plain water (eg, caregiver attempting to rehydrate an infant who has been ill). Infants have immature renal systems with a low glomerular filtration rate, which decreases their ability to excrete excess water and makes them susceptible to water intoxication. Symptoms of hyponatremia include irritability, lethargy, and, in severe cases, hypothermia and seizure activity. Breast milk and/or formula are the only sources of hydration an infant needs for the first 6 months of life. Formula should be prepared per the manufacturer's instructions. (Option 1) Hypernatremia may be caused by dehydration (eg, decreased oral intake, vomiting, diarrhea) and presents with similar neurological symptoms (eg, restlessness, seizures). The infant's history indicates adequate oral intake and signs of fluid overload (eg, facial edema), not dehydration. (Option 2) Hypoglycemia may present with irritability and seizures, but facial edema and recent history of over-diluting the formula should alert the nurse that water intoxication with hyponatremia is the most likely cause. (Option 3) Hypokalemia secondary to diarrhea may present with irritability, muscle weakness, and cardiac arrhythmias. Educational objective: Infants are susceptible to hyponatremia secondary to water intoxication, which can present with neurological symptoms (eg, lethargy, irritability, seizures). Breast milk and/or formula provide sufficient hydration for the first 6 months of life. Formula should not be diluted to save money. A A A The nurse just administered routine immunizations to a healthy 15-month-old. What information should the nurse provide the caregivers before they leave the clinic? 1. Call the office if the toddler's temperature is higher than 100 F (37.7 C) [18%] 2. Fussiness and anorexia are common for 1 week after immunizations [3%] 3. Redness at the injection sites and a mild fever are common [76%] 4. The toddler's activity level should be restricted for 24 hours [1%]Explanation: Common side effects of immunizations include a mild fever and soreness and redness at the injection site. Caregivers should be instructed to apply a warm compress to the injection site and taught how to correctly calculate the dose of acetaminophen or ibuprofen needed for these symptoms. (Option 1) The health care provider should be notified if the child's temperature is higher than 100.4 F (38 C). (Option 2) Children may have increased fussiness and anorexia following immunizations. These symptoms should not last more than 24 hours. (Option 4) A child's activity level should not be restricted following immunizations. Being active may actually help decrease any soreness if the child moves the injected extremity. Educational objective: Common side effects of immunizations include a mild fever and soreness and redness at the injection site. Anorexia and fussiness can be present for the first 24 hours. A A A: The nurse has received report on 4 pediatric clients on a telemetry unit. Which client should the nurse assess first? 1. Adolescent client with coarctation of the aorta and diminished femoral pulses [34%] 2. Infant client with ventricular septal defect with reported grunting during feeding [22%] 3. Newborn client with patent ductus arteriosus and a loud machinery-like systolic murmur [8%] 4. Preschool client with tetralogy of Fallot who has finger clubbing and irritability [34%] Explanation: Ventricular septal defect (VSD) is a congenital abnormality in which a septal opening between ventricles causes left-to-right shunting, leading to excess blood flow to the lungs. This places the client at risk for congestive heart failure (CHF) and pulmonary hypertension. Clinical manifestations of VSD include a systolic murmur auscultated near the sternal border at the third or fourth intercostal spaces, and hallmark CHF signs (eg, diaphoresis, tachypnea, dyspnea). The client is currently showing signs of increased respiratory exertion (eg, grunting) and requires further assessment for CHF (Option 2). (Option 1) Coarctation of the aorta (COA) is an abnormal aortic narrowing that results in decreased cardiac output. The client will exhibit elevated pulse pressure in the upperextremities and diminished pressures in the lower extremities. Further assessment is needed, but this client is not the current priority. (Option 3) A systolic murmur with a machine sound and poor feeding are expected, nonurgent findings in clients with patent ductus arteriosus (PDA). PDA commonly resolves within 48 hours and requires no intervention in full-term newborns. (Option 4) Tetralogy of Fallot (TOF) is a cyanotic congenital heart defect commonly manifested by signs of irritability and clubbing of fingers due to oxygen saturation chronically remaining between 65-85% until the client can undergo surgical repair. Further evaluation of the client's oxygenation is necessary but not urgently required. Educational objective: Ventricular septal defect is a cardiac abnormality, with a septal opening between ventricles, that may progress to congestive heart failure (CHF). The client should be closely monitored for respiratory exertion and signs of CHF (eg, dyspnea, tachypnea). A A A The parent of a 3-year-old calls and tells the nurse of finding the child in the bathroom with an empty bottle of mouthwash. The parent thinks that the bottle was about one quarter full. What is the nurse's priority response? 1. "Call the poison control center. I will give you the number." [29%] 2. "Give your child about a cup of water to dilute the mouthwash." [7%] 3. "How did your child get hold of the mouthwash?" [0%] 4. "What is your child doing right now?" [62%] Explanation: Many mouthwashes have an ethanol (alcohol) content ranging from the equivalent of wine to half the strength of hard liquor. Because children's bodies absorb alcohol quickly, the symptoms of alcohol poisoning can occur within 30 minutes or less after consumption. Clinical indications include confusion, vomiting and seizures, difficulty breathing, flushed or pale skin, and coma secondary to low blood sugar. The exact amount of alcohol that this child presumably ingested is unknown. It is most important to assess the child's condition (eg, behavior, mental status, physical signs and symptoms) to determine if immediate emergency measures (eg, calling 911, cardiorespiratory support) are necessary or if the parent should be instructed to contact the poison control center (Option 4). (Option 1) It is the nurse's professional responsibility to provide instruction and guidance to the parent. Although caregivers should have the number of the poison control centerreadily available, referral might delay care and place the child at further risk of a negative outcome if the child is already deteriorating. If the child's condition is stable, the nurse should instruct the parents to contact the center for further evaluation and instructions. (Option 2) Giving the child water or any other liquid will not change the amount of alcohol ingested. In addition, alcohol can impair swallowing, placing the child at risk for choking and aspiration. Parents should be advised not to perform any interventions before contacting the poison control center (Option 3) This response does not address the immediacy of the situation and suggests that the parent is to blame for the child's possible ingestion. Educational objective: When a child accidentally ingests a poisonous substance, it is most important to assess the child's condition, including physical signs and symptoms, mental status, and behavior. Based on the condition of the child, the nurse can provide guidance and instructions to contact the appropriate agency (eg, emergency services, poison control center). A A A A nurse in the neonatal intensive care unit discovers a cyanotic newborn with excessive frothy mucus in the mouth. What should be the nurse's first action? 1. Administer 100% oxygen [7%] 2. Auscultate the lungs [4%] 3. Place infant in knee-chest position [11%] 4. Suction the infant's mouth [76%] Explanation: The initial nursing action for a client experiencing cyanosis and excess oral secretions is suctioning the mouth (ie, oropharynx) to clear the airway (Option 4). Excessive frothy mucus and cyanosis in a newborn could be due to esophageal atresia (EA) and tracheoesophageal fistula (TEF). If EA/TEF is suspected, the infant should be kept supine with the head elevated at least 30 degrees to prevent aspiration. A nasogastric tube should be inserted and connected to continuous or intermittent suction until surgical repair. (Option 1) Oxygen cannot be delivered to the lungs if secretions obstruct the airway. Therefore, suctioning is a priority.(Option 2) This infant is aspirating and in immediate distress, which should be addressed without delay. After suctioning the excess saliva and ensuring a clear airway, the nurse may perform further assessments. (Option 3) This infant's cyanosis is a result of aspirating secretions and does not indicate a circulatory problem. The knee-chest position is appropriate to increase pulmonary blood flow in infants with a cyanotic heart defect (eg, tetralogy of Fallot). Educational objective: The initial nursing action for a client experiencing cyanosis and excess oral secretions is oropharyngeal suctioning to ensure airway patency. A A A The nurse is teaching a class on nutrition and feeding practices for young children. What would the nurse recommend as the best snack for a toddler? 1. ½ cup orange juice [7%] 2. Animal cracker cookies [26%] 3. Raw carrot sticks [18%] 4. Strips of cheese [46%] Explanation: When choosing snacks and meals for toddlers (age 1–3), 3 factors must be considered: Safety – small, hard, sticky and/or slippery foods pose a choking risk and should not be offered to children under age 3. Examples include hot dogs, grapes, nuts, raw carrot sticks, popcorn, peanut butter, hard candy, and raisins. Nutrient density (the nutrients a food provides relative to the number of calories it contains). The snack should be of high nutritional value rather than "empty calories." Potential for food-borne illness – children are at higher risk for developing a food-related infection if given raw, unpasteurized foods such as juice, partially cooked eggs, raw fish, or raw bean sprouts. Examples of healthy snacks for children under age 3 include pieces of cheese, whole-wheat crackers, banana slices, yogurt, cooked vegetables, mini pizzas, and cottage cheese with cutup fruit.(Option 1) Although orange juice is a source of vitamin C, it is considered a "sugary" beverage and lacks the fiber of whole fruit. It is recommended that young children have no more than 4–6 ounces of fruit juice per day. It is best to serve juice with a meal so the child does not become accustomed to snacking on sugary foods. (Option 2) Cookies do not have high nutritional value. Graham crackers or whole-wheat crackers with cream cheese would be better snack choices. (Option 3) Raw carrot sticks pose a choking risk. Carrots and other hard vegetable should be served grated or cooked. Educational objective: Food choices for young children should be of high nutritional value and pose little risk of choking or food-borne infection. Examples of healthy snacks for children under age 3 include pieces of cheese, whole-wheat crackers, banana slices, yogurt, cooked vegetables, mini pizzas, and cottage cheese with cut-up fruit. A A A For the past month, the nurse has been providing care to a 7-year-old client recently diagnosed with type 1 diabetes mellitus. Initially, the family seemed devastated over the diagnosis. The client's parent stated, "Our lives will never be the same." What statement now made by the parent best indicates that nursing interventions have been effective? 1. "Our child will not be able to participate in sporting events." [0%] 2. "Our whole family will have to make sacrifices to deal with this disease." [5%] 3. "We have set aside a place in the pantry for our child's special foods." [26%] 4. "We will not let this disease take control of our child's life." [66%] Explanation: It is normal for parents to feel devastated when their child is diagnosed with a chronic illness (eg, diabetes). Reactions include shock, denial, helplessness, anger, fear, and anxiety. They may have feelings of guilt that they contributed to or failed to prevent the development of the disease. The parents' emotional response, adaptation, and coping strategies will greatly impact the child's perception of self and the ability to self-manage the disease. In providing diabetes education, the nurse needs to emphasize and reinforce that with planning and preparation, diabetes can be managed and controlled, regular day-to-day activities can be resumed, and the child can have a normal life.When clients feel in control rather than victimized and dependent, it increases the likelihood that they will be actively engaged in diabetes self-management activities. (Option 1) This is not a true statement. Clients with diabetes can participate in a wide variety of sports. (Option 2) The diagnosis and management of diabetes in a child will affect the whole family. The use of the word "sacrifice" suggests that the parent is feeling victimized by the disease. (Option 3) Nutritional management of diabetes does not require special foods. Nutrition education should emphasize healthy food choices and balancing food choices with medications and exercise for blood sugar control. Educational objective: The diagnosis of a chronic illness (eg, diabetes) in a child will have an impact on the entire family. When the parents see themselves and their child as capable of being independent and in control of the condition, there is an increased likelihood that the disease will be better managed and controlled. A A A A nurse is assisting a new mother as she is breastfeeding her infant. The infant has been diagnosed with tetralogy of Fallot. During feeding, the infant becomes cyanotic and is having difficulty breathing. What should be the nurse's first action? 1. Administer morphine to the infant [0%] 2. Administer oxygen via mask [19%] 3. Assess infant's vital signs and pulse oximetry [7%] 4. Place the infant in the knee-chest position [73%] Explanation: Tetralogy of Fallot is a congenital cardiac defect that typically has 4 characteristics: pulmonary stenosis, right ventricular hypertrophy, overriding aorta, and ventricular septal defect. This infant is experiencing a hypercyanotic episode, or "tet spell," which is an exacerbation of tetralogy of Fallot that can happen when a child cries, becomes upset, or is feeding. The child should first be placed in a knee-to-chest position. Flexion of the legs provides relief ofdyspnea as this angle improves oxygenation by reducing the volume of blood that is shunted through the overriding aorta and the ventricular septal defect. (Option 1) Morphine may be considered if the dyspnea is not relieved by the knee-to-chest position. (Option 2) If oxygen saturation remains low, oxygen may need to be administered. (Option 3) Vital signs and pulse oximetry may be checked after the infant has been placed in the knee-chest position. Educational objective: To relieve a hypercyanotic episode, or "tet spell," the nurse should place the infant or child in the knee-chest position. A A A The registered nurse is teaching the parent of a 6-year-old about behavioral strategies for treating fecal incontinence due to functional constipation. Which statement by the parent indicates a need for further teaching? 1. "I will give my child a picture book to look at during toilet time." [29%] 2. "I will give my child a reward for each bowel movement while sitting on the toilet." [34%] 3. "I will keep a log of my child's bowel movements, laxative use, and episodes of soiling." [23%] 4. "I will schedule regular toilet sitting time for my child." [11%] Explanation: Fecal incontinence (ie, encopresis, soiling) refers to the repeated passage of stool in inappropriate places by children age ≥4 years. In more than 80% of cases, it is due to functional constipation (retentive type); in about 20% of cases, it may be caused by psychosocial triggers (nonretentive type). Management of fecal incontinence/constipation primarily includes 3 components: Disimpaction followed by prolonged laxative therapy, dietary changes (increased fiber and fluid intake), and behavior modification. Behavioral strategies are used to promote and restore regular toileting habits and to gain the child's cooperation and participation in the treatment program.Behavioral interventions include the following: Regularly schedule toilet sitting times 5-10 minutes after meals for 10-15 minutes (Option 4) Provide a quiet activity for the child during toilet sitting, which will help pass the time and make the experience more "enjoyable" (Option 1) Initiate a reward system to boost the child's participation in the treatment program; the reward would be given for effort, not for success of evacuation in the toilet (children with retentive encopresis have dysfunctional anal sphincters and little control over bowel movements; giving a reward for something the child has no control over would not be effective) (Option 2) Keep a diary or log of toilet sitting times, stooling, medications, and episodes of soiling to evaluate the success of the treatment (Option 3) Educational objective: A reward system is one of the behavioral strategies used in the treatment of functional incontinence (due to constipation). The reward is given to encourage the child's involvement in the treatment to restore normal bowel function. Rewards are given for the child's effort and participation, not for having bowel movements while sitting on the toilet. A A A The nurse teaching the parents of a child diagnosed with cystic fibrosis will advise the parents to choose foods that satisfy which recommended diet? 1. Gluten-free with added protein [7%] 2. High calorie, high protein, high fat [55%] 3. High protein, low fat, low phosphate [9%] 4. High protein, low fat, low sodium [27%] Explanation: In cystic fibrosis (CF), a protein responsible for transporting sodium and chloride is defective and causes the secretions from the exocrine glands to be thicker and stickier than normal. These abnormal secretions plug smaller airway passages and ducts in the gastrointestinal (GI) tract. The thick secretions block pancreatic ducts, resulting in a deficient amount of pancreatic enzymes entering the bowel to aid in digestion and nutrient absorption. Clients require multiple vitamin supplements and supplemental pancreaticenzymes that are administered with meals. To meet the growth needs of clients with CF, a diet high in calories, fat, and protein is required. (Options 1, 3, and 4) A gluten-free diet is required for clients with celiac disease who cannot tolerate barley, rye, oats, or wheat (mnemonic: BROW). Low-phosphate diets are indicated for clients with certain kidney disorders. Low-sodium diets are indicated for volume overload states (eg, heart failure, ascites) and hypertension. Educational objective: Cystic fibrosis causes damage to the GI tract and pancreas, leading to impaired absorption of nutrients and resulting growth deficits. Clients must consume a diet high in calories, fat, and protein. A A A The parent of a 7-month-old reports that the child has been crying and vomiting with a distended belly for the past 4 hours. The infant is now lying quietly in the parent's arms with a pulse of 200/min and respirations of 60/min. Which of the following components of SBAR (situation, background, assessment, recommendation/read-back) communication is most important for the nurse to report to the health care provider? 1. Client has been ill for approximately 4 hours [4%] 2. Client has improved from apparent earlier distress [3%] 3. Client is now lethargic with abnormal vital signs [88%] 4. Does the health care provider want to order a laxative? [3%] Correct Answered correctly 88% Time: 37 seconds Updated: 07/27/2017 Explanation: SBAR (situation, background, assessment, recommendation/read-back) is an established reporting format used to communicate with the health care provider (HCP). Use of SBAR ensures that the HCP receives the necessary information to make a clinical judgment regarding treatment or need for immediate assessment. In this situation, the client's presentation indicates worsening symptoms that require immediate intervention. The client's lethargy represents a declining level of consciousness.The client also has significantly abnormal vital signs (normal infant pulse rate is 110- 160/min, respirations generally around 40/min). These are ominous signs that should be reported immediately (Option 3). (Option 1) Although it is helpful to know that the change is fairly recent, it is most important to report the current concerning change in the client's clinical presentation and vital signs. (Option 2) Abnormal vital signs with a decreased level of consciousness are not improvements; rather, these findings indicate deterioration. (Option 4) It would not be appropriate to assume and treat potential constipation in this client without further assessment and diagnostic procedures. The nurse needs to assess additional aspects, including bowel sounds, abdominal characteristics, and temperature. Vital signs this significantly abnormal would not be caused by constipation. Educational objective: SBAR (situation, background, assessment, recommendation/read-back) is used to transmit complete essential information to the health care provider. Any abnormal vital signs or current deterioration should be communicated immediately. A A A Several children seen at a local pediatric clinic are found to have a hemoglobin level of 10- 11 g/dL (100-110 g/L). Which strategy would most likely help increase the hemoglobin levels in these clients? 1. Encouraging intake of milk and other dairy products [3%] 2. Ensuring adequate intake of meat, fish, poultry, and legumes [80%] 3. Increasing consumption of fruits and vegetables [8%] 4. Using orange juice fortified with vitamin D [7%] Explanation: Iron deficiency (ID) is the most common nutritional deficiency of children and adolescents in the United States and worldwide. In most individuals with ID, the cause is inadequate intake of foods high in iron. In this type of anemia, the red blood cells are small (microcytes) and have reduced hemoglobin, appearing paler (hypochromic) under a microscope.The richest dietary sources of iron include meat, fish, poultry, eggs, and legumes. Iron occurs as heme iron in these foods and is better absorbed than the non-heme iron found in plant foods. Heme iron sources also contain a factor that promotes the absorption of iron, including iron from other foods eaten at the same time. Other dietary sources of iron include dried fruits, nuts, green leafy vegetables, and whole grains. However, the iron from these sources is not absorbed as completely as heme iron. Fruit and fruit juices high in vitamin C may enhance the absorption of both heme and nonheme iron and should be included in a meal (Option 1) Milk and milk products are poor sources of dietary iron. Overconsumption of milk along with little or no consumption of other foods is a leading cause of iron deficiency (milk anemia) in young children. (Option 3) Fruits and vegetables are not the best sources of dietary iron. (Option 4) Vitamin D is not a common nutritional deficiency in children and adolescents, and the deficiency does not result in anemia. Educational objective: A diet rich in iron can prevent iron deficiency anemia (hypochromic and microcytic) in children and adolescents. The best sources of iron are those that contain heme iron, which has a higher bioavailability; these foods include meat, fish, poultry, eggs, and legumes. Fruit and fruit juices high in vitamin C may enhance the absorption of both heme and non-heme iron and should be included in a meal. A A A A parent has brought her 6-month-old to the clinic for routine immunizations. The nurse administers which of the following to the client? Select all that apply. 1. Hepatitis B (Hep B) 2. Inactivated poliovirus (IPV) 3. Measles, mumps, rubella (MMR) 4. Pneumococcal conjugate vaccine (PCV) 5. Varicella zoster virus (VZV) Explanation:The schedule of recommended routine immunizations for a 6-month-old client includes Hep B, DTaP, RV, Hib, IPV, and PCV; a mnemonic is Be DR HIP (Hep B, DTaP, RV, Hib, IPV, PCV). (Options 3 and 5) The first MMR and VZV vaccines are given at age 12-15 months. Educational objective: The recommended immunization schedule for a 6-month-old client includes Hep B, DTaP, RV, Hib, IPV, and PCV. MMR and varicella vaccines are given at age 12-15 months.A A A The nurse in the pediatric clinic is triaging telephone messages. The nurse should call the parent of which child first? 1. 2-year-old with bilateral tympanostomy tubes who has a small piece of plastic in the right outer ear [18%] 2. 4-year-old post adenotonsillectomy who is now reporting ear pain [53%]3. 6-year-old with strep throat who needs a note to return to school 24 hours after starting antibiotics [3%] 4. 7-year-old 5 days post tonsillectomy who wants to return to soccer practice today [24%] Explanation: The child with a recent tonsillectomy is at highest safety risk. Postoperative hemorrhage from tonsillectomy is uncommon but may occur up to 14 days after surgery. During the healing process, white scabs will form at the surgical sites. Sloughing then occurs approximately 7 days after the procedure, increasing the risk for bleeding. Caregivers should be taught to observe for signs of bleeding (eg, frequent swallowing or throat clearing). The child may also experience increased pain. The nurse should instruct this parent that the child should not resume strenuous activity or contact sports for at least 7- 14 days post surgery. (Option 1) Tympanostomy tubes or grommets are pressure-equalizing tubes placed in the tympanic membrane to facilitate drainage of middle ear fluid (eg, for eustachian tube dysfunction or recurrent otitis media with effusion). One of this child's tubes has most likely fallen out of the eardrum. No immediate intervention is required; however, the health care provider should be notified. (Option 2) Clients often report ear pain (otalgia) following adenotonsillectomy due to irritation of the 9th cranial nerve (glossopharyngeal) in the throat, causing referred pain to the ears. This is a normal, expected finding. (Option 3) The contagious period for strep throat starts at the onset of symptoms and lasts through the first 24 hours of beginning antibiotic treatment. This client is able to return to activities and does not require an immediate call back. Educational objective: The risk of post-tonsillectomy hemorrhage persists for up to 14 days after surgery, and resuming strenuous activity too early increases this risk. The potential for bleeding is higher 7-10 days postoperatively while sloughing occurs. A A A A nurse auscultates a loud cardiac murmur on a newborn with suspected trisomy 21 (Down syndrome). A genetic screen and an echocardiogram are scheduled that day. The neonate's vital signs are shown in the exhibit. What would be an appropriate action for the nurse to complete next? Click on the exhibit button for additional information.Vital signs Temperature 98.6 F (37 C) Heart rate 146/min Respirations 42/min O2 saturation 98% 1. Call the health care provider (HCP) immediately [6%] 2. Document the assessment finding [76%] 3. Place the neonate in a knee-chest position [10%] 4. Provide oxygen to the neonate [6%] Explanation: Atrioventricular (AV) canal defect is a cardiac anomaly often associated with trisomy 21 (Down syndrome). As an echocardiogram is already scheduled for that day, documenting the assessment finding would be the appropriate action for the nurse to complete at this time. (Option 1) The neonate has stable vital signs and the echocardiogram will be completed. This is not an emergency and the HCP does not need to be contacted immediately. (Option 3) A knee-chest position is used to treat episodes of hypoxia and cyanosis in infants and young children with tetralogy of Fallot (TOF). This neonate likely has an AV canal defect, not TOF. There is also no indication of cyanosis or hypoxia that would necessitate knee-chest positioning. (Option 4) The normal respiratory rate in a neonate is 30-60/min; pulse can be up to 160/min. The vital signs are stable and the oxygen saturation level is appropriate for a neonate. Educational objective: Trisomy 21 (Down syndrome) is often associated with the cardiac anomaly AV canal defect. Assessment typically includes a loud murmur that requires no immediate action when vital signs are stable. Surgery will correct the anomaly when the neonate grows in size and can tolerate the invasive procedure better Block Time Remaining: 00:31:01A A A A 3-month-old who weighs 8.8 lb (4 kg) has just returned to the intensive care unit after surgical repair of a congenital heart defect. Which finding by the nurse should be reported immediately to the health care provider (HCP)? 1. Chest tube output of 30 mL in the past hour [18%] 2. Heart rate of 180/min [47%] 3. Temperature of 97.5 F (36.4 C) [4%] 4. Urine output of 12 mL in the past hour [28%] Explanation: Chest tube drainage >3 mL/kg/hr for 3 consecutive hours or 5-10 mL/kg in 1 hour should be reported immediately to the HCP. This could indicate postoperative hemorrhage and needs immediate intervention. Cardiac tamponade can develop rapidly in children and can be life-threatening. This child weighs 4 kg and an output of 30 mL in 1 hour is excessive. (Option 2) For infants age 1-12 months, the normal heart rate is 100-160/min. However, this can be increased slightly with crying or surgery. (Option 3) Hypothermia is common after surgery and warmers are often used. (Option 4) Hourly urine output should be measured in the postoperative infant. A urinary catheter is often placed during surgery. Urine output should be between 1-2 mL/kg/hr. Educational objective: The nurse should immediately report chest tube drainage >3 mL/kg/hr over 3 consecutive hours or 5-10 mL/kg over 1 hour. This could indicate postoperative hemorrhage. Cardiac tamponade can occur rapidly in children and can be life-threatening. A A A A nurse manager on a pediatric oncology unit is leading a discussion about personal coping strategies that nurses can use to remain effective when caring for dying children. What should be included in the discussion? 1. Attending a child's memorial service can be helpful [45%] 2. Avoid expressing personal feelings of grief or loss directly with the family [28%]3. Personal contact with the family of the deceased should end after they leave the hospital [18%] 4. The length of daily exercise routines should be increased [7%] Explanation: Nurses who care for dying children experience many of the same feelings that the child's family does, resulting in stress that may lead to compassion fatigue. To remain positive in the caring role, nurses must implement appropriate coping strategies to enhance self-care and grief resolution. Attending a memorial service can demonstrate care for the grieving family while also providing closure for the nurse. Other helpful strategies for coping include: taking time off from work if distancing is needed, utilizing personal and professional support systems (eg, spouse, employee assistance programs, experienced mentors), and maintaining good health through adequate rest, regular exercise, and proper nutrition. (Option 2) The nurse should maintain a level of objectivity to make effective care decisions, but it is sometimes appropriate to share personal emotions of loss or sadness with the family of a dying child. Honesty and personal connection support the coping process for the nurse and the family. (Option 3) Personal contact with the family of the deceased child for an extended period after their loss is helpful for the nurse and the family during the grieving process, particularly if a close relationship was established during hospitalization. (Option 4) Although exercise is an important part of maintaining overall health, there is no evidence that increasing the length of daily exercise routines is an effective coping strategy. Educational objective: Nurses who care for dying children experience many of the same feelings that the family of the dying child does, resulting in stress that may lead to compassion fatigue. To remain effective in the care-giving role, nurses should utilize professional and personal support systems, share in end-of-life celebration rituals, and take time off from work when distancing is needed. The family and the nurse can gain support by remaining in contact during the grieving process. A A A An overweight toddler is diagnosed with iron deficiency anemia. Which is the most likely explanation for the anemia? 1. Excessive intake of meat products [3%]2. Excessive intake of milk [64%] 3. Gastrointestinal blood loss [18%] 4. Impaired iron transfer from the mother [13%] Explanation: Iron deficiency anemia is the most common chronic nutritional disorder in children. There are many risk factors for iron deficiency, including insufficient dietary intake, premature birth, delayed introduction of solid food, and consumption of cow's milk before age 1 year. One common cause in toddlers is excessive milk intake, over 24 oz/day. In addition to becoming overweight, toddlers who consume too much milk develop iron deficiency due to the likely exclusion of iron-rich foods in favor of milk, a poor source of available iron. Treatment of iron deficiency anemia includes oral iron supplementation and increased consumption of iron-rich foods (eg, leafy green vegetables, red meats, poultry, dried fruit, fortified cereal). It is also important to limit milk intake (16-24 oz/day) in toddlers to ensure a balanced diet. (Option 1) Red meat and other meat products are considered good sources of dietary iron. However, clients may be at risk for obesity if meat consumption exceeds protein and caloric needs. (Option 3) Gastrointestinal blood loss, which can occur if infants under age 1 year are fed cow's milk, is a potential cause of iron deficiency anemia. However, excessive milk intake is a more common cause, particularly in clients over age 1 year. (Option 4) Impaired or decreased iron transfer is a potential cause of iron deficiency anemia, particularly in preterm infants or infants born in multiples. However, iron stores received from the mother are typically depleted by age 5-6 months (2-3 months for preterm infants); after this point, iron must be acquired through dietary sources. Because this client is a toddler (age 1-3 years), impaired iron transfer is not a likely cause of the current anemia. Educational objective: Iron deficiency anemia is the most common nutritional disorder in children. Risk factors include premature birth, cow's milk before age 1 year, and excessive milk intake in toddlers. Prevention and treatment are achieved through proper nutrition (eg, meat, leafy green vegetables, fortified cereal) and supplementation. A A AA 3-month-old client has stopped breathing. Identify the area where the nurse should check the client's pulse. Left-clicking the mouse will place an X to show the answer before submitting the question. Explanation: The American Heart Association's guidelines for infant cardiopulmonary resuscitation (CPR) are used on children age <1 year. To check a pulse on an infant, the nurse should palpate the brachial artery by placing 2 or 3 fingers halfway between the shoulder and elbow on the medial aspect of the arm. The pulse should be assessed for 5-10 seconds to determine its presence and quality before CPR is initiated. The brachial pulse is preferred in infants as the brachial artery is close to the surface and is easily palpable. The carotid pulse can be difficult to assess due to a child's shorter neck. Extending an infant's neck to attempt to palpate the carotid pulse can cause injury. This pulse is recommended for clients age >1 year. The femoral pulse may be used for all clients; however, it is often not easily accessible for palpation due to diapers and clothing. The radial pulse is used in responsive clients age >1 year. It is not a recommended method of pulse detection in an unresponsive client as a weak or thready pulse is difficult to palpate at this location Educational objective: According to the infant cardiopulmonary resuscitation guidelines of the American Heart Association, the brachial artery is used to detect a pulse in an unresponsive client age <1 year.A A A The nurse is gathering data on a 5-week-old admitted with a suspected diagnosis of pyloric stenosis. The nurse should expect to find which laboratory value? 1. Blood pH of 7.1 [34%] 2. Hematocrit of 57% (0.57) [22%] 3. Potassium of 5.2 mEq/L (5.2 mmol/L) [24%] 4. White blood cells of 28,500/mm3 (28.5 x 109/L) [19%] Explanation: In pyloric stenosis, a hypertrophied pyloric muscle causes postprandial projectile vomiting secondary to an obstruction at the gastric outlet. An olive-shaped mass may be palpated in the epigastric area just to the right of the umbilicus. Emesis is nonbilious (formula in/formula out) and leads to progressive dehydration. Infants will be hungry constantly despite regular feedings. A hematocrit of 57% (0.57) is elevated and indicative of hemoconcentration caused by dehydration (Option 2). Elevated blood urea nitrogen is also a sign of dehydration. (Option 1) The stomach contains acid, which becomes depleted with excess vomiting (or during nasogastric [NG] suctioning), leading to metabolic alkalosis (increased bicarbonate and pH of >7.45). (Option 3) A potassium level of 5.2 mEq/L (5.2 mmol/L) is considered slightly elevated. However, vomiting or prolonged NG suctioning would cause hypokalemia, not hyperkalemia. (Option 4) A white blood cell count of 28,500/mm3 (28.5 x 109/L) is elevated, indicating infection. However, pyloric stenosis is not an infectious process. Educational objective: Hypertrophic pyloric stenosis results in recurrent projectile vomiting, which leads to dehydration and hypokalemic metabolic alkalosis. Dehydration is manifested by hemoconcentration (elevated hematocrit) and elevated blood urea nitrogen. A A A A newborn is being evaluated for possible esophageal atresia with tracheoesophageal fistula. Which finding is the nurse most likely to observe?1. Choking and cyanosis during feeding [77%] 2. Concave (scaphoid) abdomen [2%] 3. Diminished lung sounds [2%] 4. Projectile vomiting after feeding [18%] Explanation: Esophageal atresia (EA) and tracheoesophageal fistula (TEF) consist of a variety of congenital malformations that occur when the esophagus and trachea do not properly separate or develop. In the most common form of EA/TEF, the upper esophagus ends in a blind pouch and the lower esophagus connects to the primary bronchus or the trachea through a small fistula. EA/TEF can usually be corrected with surgery. Clinical manifestations of EA/TEF include frothy saliva, coughing, choking, and drooling. Clients may also develop apnea and cyanosis during feeding (Option 1). Aspiration is the greatest risk for clients with EA/TEF, and newborns who demonstrate signs of the condition are immediately placed on nothing by mouth (NPO) status. (Option 2) A newborn with EA/TEF may have a distended abdomen due to the buildup of air in the stomach via the fistula from the trachea to the lower esophagus. A concave (ie, scaphoid) abdomen is associated with a congenital diaphragmatic hernia due to the migration of abdominal organs to the thoracic space. (Option 3) Diminished lung sounds are not an ordinary sign of EA/TEF unless aspiration pneumonia develops. These may be an indication of a diaphragmatic hernia or pneumothorax. (Option 4) A newborn with EA/TEF may experience apnea, choking, and cyanosis due to aspiration of fluid while eating. Projectile vomiting after feeding is a classic manifestation of hypertrophic pyloric stenosis. Educational objective: Clinical manifestations of EA/TEF include frothy saliva, coughing, choking, drooling, and a distended abdomen. Clients may also develop apnea and cyanosis while feeding. These findings must be reported to the health care provider for further evaluation. A A A A nurse is admitting a child who has leukemia. Several rooms are available on the pediatric unit. Which client could share a room with this child?1. A client recovering from a ruptured appendix [25%] 2. A client with cystic fibrosis [20%] 3. A client with minimal change nephrotic syndrome [49%] 4. A client with rheumatic fever [4%] Explanation: Leukemia is characterized by unrestricted proliferation of abnormal white blood cells (lymphoblasts), resulting in depression of normal bone marrow activity. This disorder is the most common form of childhood cancer. Infection is a major concern due to neutropenia. In addition, anemia occurs due to decreased red blood cell production, and bleeding is common as a result of decreased platelet production. It would be appropriate for this client with leukemia to share a room with a client with minimal change nephrotic syndrome (MCNS). MCNS is a non-infectious condition of the glomeruli and poses no risk to a client with leukemia. (Option 1) Appendicitis is a result of viral or infectious processes and can lead to rupture of the appendix. A client recovering from a ruptured appendix poses a threat of infection to the child who has leukemia. (Option 2) A client with cystic fibrosis has pulmonary complications due to thick mucus that traps bacteria. The tracheobronchial tree is colonized with bacteria and respiratory infections are a lifelong problem. This client poses a threat of infection to the child with leukemia. (Option 4) Rheumatic fever occurs following pharyngitis caused by group A -hemolytic β Streptococcus. A client with this condition poses a threat of infection to the child with leukemia. Educational objective: Leukemia is a cancer of the blood and organs involved in hematologic function. Due to myelosuppression, clients are at risk for problems related to infection, anemia, and bleeding. A A A The nurse who is caring for a 1-month-old with Tetralogy of Fallot will report which finding to the health care provider as a priority? 1. Hemoglobin level of 24.9 g/dL (249 g/L) [18%]2. Murmur on heart auscultation [8%] 3. Oxygen saturation of 82% on room air [66%] 4. Poor weight gain [6%] Explanation: The normal range for hemoglobin in a 1-month-old is 12.5-20.5 g/dL (125-205 g/L). Hemoglobin of 24.9 g/dL (249 g/L) is diagnostic of polycythemia (elevated hemoglobin levels). Infants with cyanotic cardiac defects can develop polycythemia as a compensatory mechanism due to prolonged tissue hypoxia. Polycythemia will increase blood viscosity, placing an infant at risk for stroke or thromboembolism (Option 1). Clubbing is another manifestation of prolonged hypoxia. (Option 2) Cardiac murmur is expected in heart defects. This is not a priority to report. (Option 3) Tetralogy of Fallot (TOF) is a cyanotic cardiac defect. Infants with TOF will normally maintain oxygen saturations of 65%-85% until the defect is surgically corrected. (Option 4) Poor weight gain is common with congenital heart defects. This finding is not a priority. Feeding intolerance, tachypnea, and dyspnea usually indicate severe hypoxemia. Educational objective: Poor oxygenation can cause elevated levels of hemoglobin (polycythemia), which increase blood viscosity. Thickened serum puts infants at risk for stroke or thromboembolism. An infant with polycythemia must stay hydrated. A A A A teenage client with sickle cell disease reports having a vaso-occlusive crisis (pain crisis). Family members say that the client is just "drug seeking." Which expected laboratory findings would help confirm the presence of a sickle cell crisis? Select all that apply. 1. Elevated bilirubin 2. Elevated eosinophils 3. Elevated reticulocyte count 4. Hemoglobin <10 g/dL (100 g/L) 5. Potassium <3.5 mEq/L (3.5 mmol/L) Explanation:During a sickle cell crisis, there is an elevation in bilirubin above normal due to hemoglobin breakdown (from the excessive hemolysis). When bilirubin is 2-3 times the normal level, jaundice results (Option 1). Elevated reticulocytes demonstrate the bone marrow's activity in response to the anemia (due to red blood cells sickling with destruction) (Option 3). A normal hemoglobin level for an adolescent male is 13.0-16.0 g/dL (130-160 g/L) and for an adolescent female is 12.0-16.0 g/dL (120-160 g/L). Acute anemia usually occurs during sickle cell crisis and is due to the increased hemolysis. Transfusions may be required (Option 4). (Option 2) Eosinophils are part of a white blood cell count differential; a rise indicates an allergic response. It is not related to sickle cell crisis. (Option 5) Potassium is an intracellular electrolyte. Therefore, bursting of red blood cells would most likely result in hyperkalemia, not hypokalemia, if there is any change in the potassium level (normal 3.5-5.0 mEq/L [3.5-5.0 mmol/L]). Educational objective: Laboratory results that support a vaso-occlusive crisis (pain crisis) in a client with sickle cell disease include elevated reticulocytes, elevated bilirubin, and anemia. A A A The nurse provides discharge teaching for the parents of a child newly diagnosed with hemophilia A. Which statements by the parents indicate that teaching has been effective? Select all that apply. 1. "A high-calorie, high-protein diet is best for our child." 2. "It is extremely important that we do not allow our child to become dehydrated." 3. "Our child should wear a medical alert bracelet at all times." 4. "We should avoid giving our child over-the-counter medicine containing aspirin." 5. "We should encourage a noncontact sport such as swimming." Explanation: Hemophilia is a hereditary bleeding disorder caused by a deficiency in coagulation proteins. Treatment consists of replacing the missing clotting factor and teaching the client about injury prevention, including:Avoid medications such as ibuprofen and aspirin that have platelet inhibition properties (Option 4). Avoid intramuscular injections; subcutaneous injections are preferred. Avoid contact sports and safety hazards; noncontact activities (eg, swimming, jogging, tennis) and use of protective equipment (eg, helmets, padding) are encouraged (Option 5). Dental hygiene is necessary to prevent gum bleeding, and soft toothbrushes should be used. MedicAlert bracelets should be worn at all times (Option 3). (Option 1) Malnutrition is not commonly associated with hemophilia; a regular diet is indicated. Clients with cystic fibrosis are at risk for malnutrition and need a high-calorie diet. (Option 2) Dehydration is not commonly associated with hemophilia. Avoiding dehydration is important for those with sickle cell anemia. Educational objective: Parents of a child with hemophilia should encourage noncontact sports, avoid giving medications that inhibit platelet aggregation, know how to control bleeding when it occurs, and ensure that the child wears a MedicAlert bracelet at all times. A A A The nurse is caring for a newborn with patent ductus arteriosus. Which assessment finding should the nurse expect? 1. Harsh systolic murmur [14%] 2. Loud machine-like murmur [44%] 3. Soft diastolic murmur [18%] 4. Systolic ejection murmur [22%] Correct Answered correctly 44% Time: 17 seconds Updated: 06/12/2017 Explanation:Patent ductus arteriosus (PDA) is an acyanotic congenital defect more common in premature infants. When fetal circulation changes to pulmonary circulation outside the womb, the ductus arteriosus should close spontaneously. This closure is caused by increased oxygenation after birth. If a PDA is present, blood will shunt from the aorta back to the pulmonary arteries via the opened ductus arteriosus. Many newborns are asymptomatic except for a loud, machine-like systolic and diastolic murmur. The PDA will be treated with surgical ligation or IV indomethacin to stimulate duct closure. (Option 1) A harsh systolic murmur is heard in the setting of ventricular septal defect, an opening between the ventricles of the heart. Ventricular septal defect is an acyanotic defect. (Option 3) A diastolic murmur is heard in mitral stenosis and aortic regurgitation but not in PDA. (Option 4) A systolic ejection murmur is heard in pulmonic stenosis. Right ventricular hypertrophy will develop if this defect is not repaired. In adults, systolic ejection murmur is usually due to aortic stenosis. Educational objective: The ductus arteriosus of a newborn should close spontaneously when fetal circulation changes to pulmonary circulation. If the ductus arteriosus remains open, blood will shunt from the aorta to the pulmonary arteries. The child will be acyanotic but will have a machine-like murmur heard on both systole and diastole. A A A Which of the following statements made by the mother of a child recently diagnosed with celiac disease indicates a need for further teaching? 1. "I will need to read the labels of all processed foods." [1%] 2. "It is okay if my child eats rice, corn, and potatoes." [12%] 3. "My child can have small amounts of foods containing wheat as long as she remains symptom free." [80%] 4. "My child will need to be on a gluten-free diet for the rest of her life." [5%] Explanation: The following are important principles to teach clients with celiac disease:All gluten-containing products should be eliminated from the diet. These include wheat, barley, rye, and oats. Rice, corn, and potatoes are gluten free and are allowed on the diet. Deficient vitamins (mainly fat-soluble vitamins), iron, and folic acid should be replaced. Processed foods (eg, chocolate candy, hot dogs) may contain "hidden" sources of gluten such as modified food starch, malt, and soy sauce. Food labels should indicate that the product is gluten free. Clients will need to be on a gluten-free diet for the rest of their lives. Eliminating gluten from the diet reduces the risk of nutritional deficiencies and intestinal cancer (lymphoma). Eating even small amounts of gluten will damage the intestinal villi although the client may have no clinical symptoms. All sources of gluten must be eliminated from the diet (Option 3). Educational objective: All sources of gluten must be eliminated from the diet of a client with celiac disease; consuming small amounts, even in the absence of clinical symptoms, will increase the risk of damage to the intestinal villi. Clients can have foods containing rice, corn, and potatoes. They should read food labels and follow the diet for the rest of their lives. A A A A parent brings a 6-month-old child to the primary health care provider after the child abruptly started crying and grabbing intermittently at the abdomen. The client's stool has a red, currant jelly appearance. What intervention does the nurse anticipate? 1. Administer epoetin alfa (erythropoietin) [7%] 2. Give air (pneumatic) enema [32%] 3. Have the parent give 2 ounces of extra juice a day for constipation [1%] 4. Perform hemoccult test on stool [58%] Explanation: Intussusception is a process in which one part of the intestine prolapses and then telescopes into another part. It is one of the most frequent causes of intestinal obstruction during infancy. Initially, the telescoping is intermittent, resulting in periodic pain in association with the legs drawn up toward the abdomen. Pain is severe, progressive, andassociated with inconsolable crying. Ongoing obstruction can compromise circulation, causing mucosal ischemia, occult bleeding, and, if untreated, grossly bloody "currant jelly" stools (mixture of blood and mucus). A contrast enema is used for diagnostic purposes and often reduces the intussusceptions. An air enema is considered safer than a barium enema. (Option 1) Human recombinant erythropoietin (epoetin alfa [Epogen, Procrit]) stimulates bone marrow to form red blood cells and is used to combat the effects of chemotherapy (due to bone marrow suppression) and/or kidney disease (erythropoietin is secreted by the kidneys). Human recombinant erythropoietin is not indicated in this client. (Option 3) Constipation during infancy usually can be corrected by increasing fluids or adding 2 ounces of pear or apple juice to the daily diet. In addition, eliminating constipating foods and increasing high-fiber foods can help. In this client, it is more important to treat the intussusception as there is no evidence of constipation. (Option 4) A hemoccult test is performed typically when occult (hidden) blood is suspected due to a dark and tarry stool. Blood is evident in intussusception, and so the priority in this client is to treat the cause of the bloody mucus stool. Educational objective: Intussusception (the intestine telescoping into itself) causes intermittent cramping and progressive abdominal pain, inconsolable crying, and currant jelly stool (from blood or mucus). It is often treated successfully with an air enema. A A A The nurse assesses a child with intussusception. Which assessment findings require priority intervention? 1. Abdominal rigidity with guarding [42%] 2. Absence of tears in crying child with IV start [16%] 3. Blood-streaked mucous stool in diaper [13%] 4. Sausage-shaped right-sided mass on palpation [26%] Explanation: Intussusception occurs when part of the intestine telescopes into another adjacent part and causes a blockage. This leads to swelling and decreased blood supply to the intestine. Tissue death as well as perforation to the bowel may result. If perforation occurs, the clientcould develop peritonitis in which the peritoneum in the abdomen becomes inflamed due to infection. This can quickly lead to sepsis and multiple organ failure. Peritonitis is characterized by fever, abdominal rigidity, guarding, and rebound tenderness. This condition can be fatal if it is not treated quickly. (Option 2) Absence of tears in a painful procedure during which the client is crying is a sign of dehydration. This is very common in clients with intussusception and should be treated. IV fluids should be started, and the client's hydration status (vital signs, mucus membranes, capillary refill) should be assessed frequently. (Option 3) A classic sign of intussusception is blood-streaked mucous stool, sometimes referred to as "currant jelly-like" stool. This is expected with intussusception. Treatment is an enema of either air or barium to unfold the intestine. (Option 4) A "sausage-shaped" right-sided mass is commonly felt on palpation in clients with intussusception. This is an expected finding for this condition. Educational objective: Intestinal perforation and peritonitis are common complications of intestinal obstruction (eg, intussusception). Peritonitis is characterized by fever, abdominal rigidity, guarding, and rebound tenderness and is a surgical emergency [Show More]
Last updated: 2 years ago
Preview 1 out of 231 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 30, 2022
Number of pages
231
Written in
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Aug 30, 2022
Downloads
0
Views
125













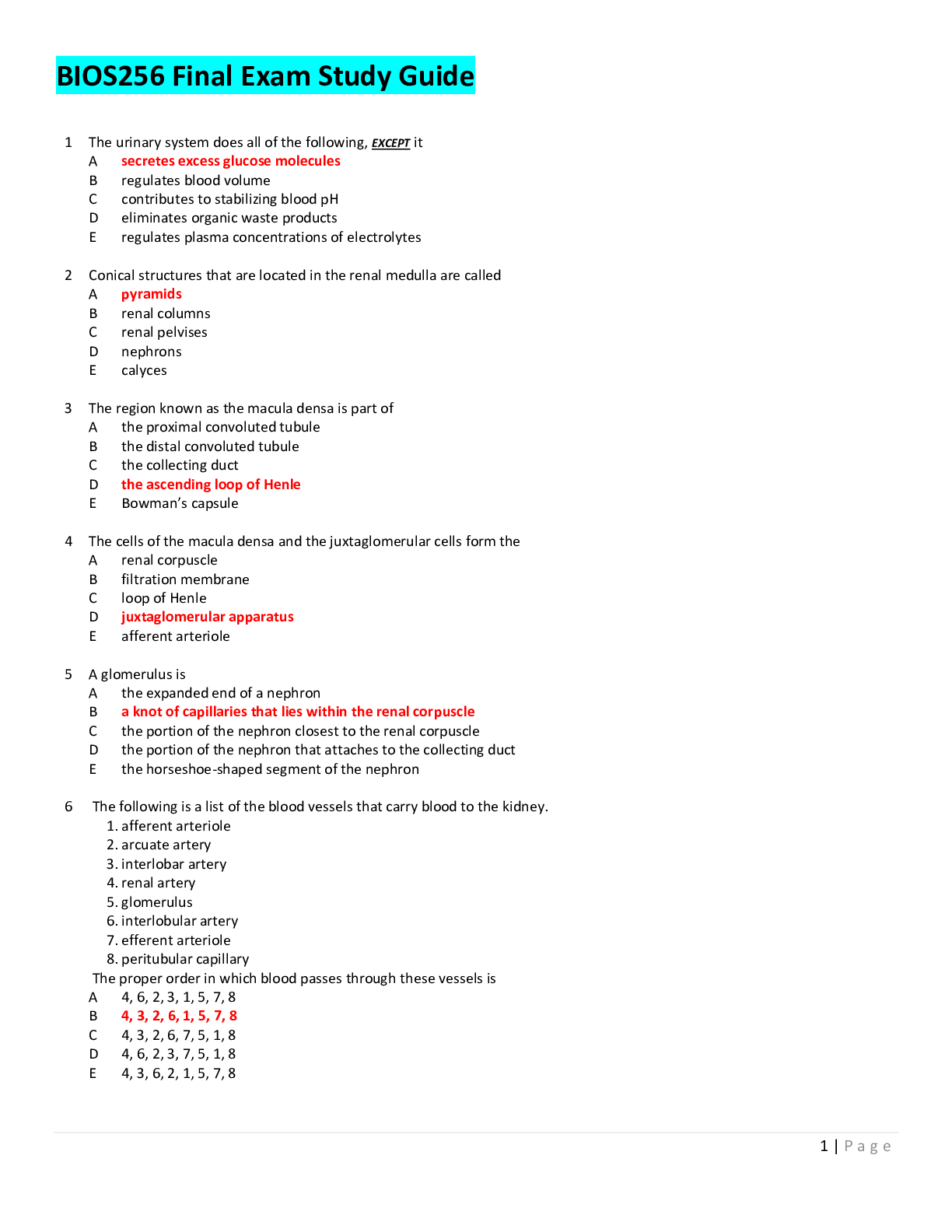


, Question Answers, 100% Correct , Correct Answers.png)

.png)

, Question Answers, Correct , Correct Answers.png)



