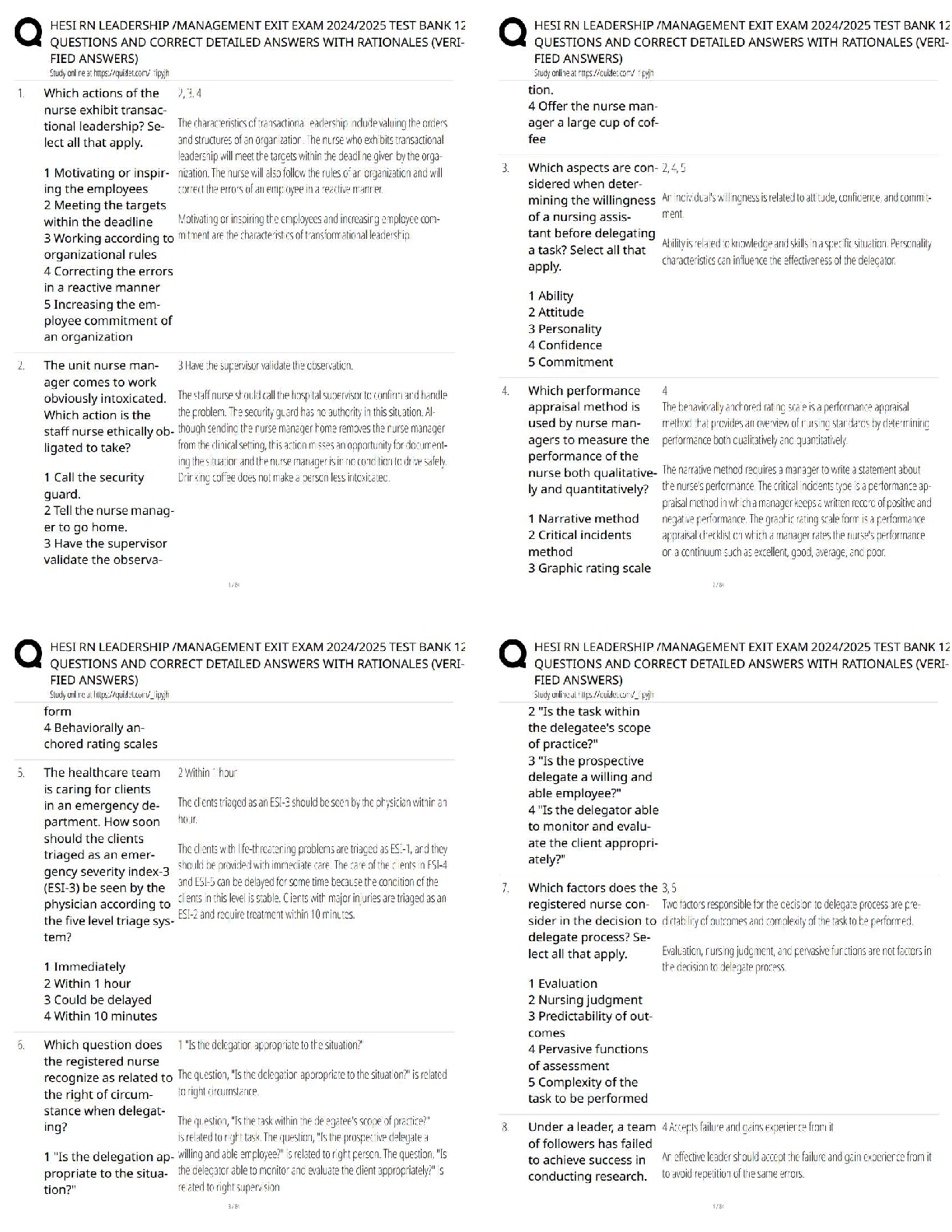
Computer Science > QUESTIONS & ANSWERS > USMLE Step 2 CK-OB/GYN Exam Study Questions 2022/23 COMPLETE SOLUTION. 100% proven pass rate. (All)
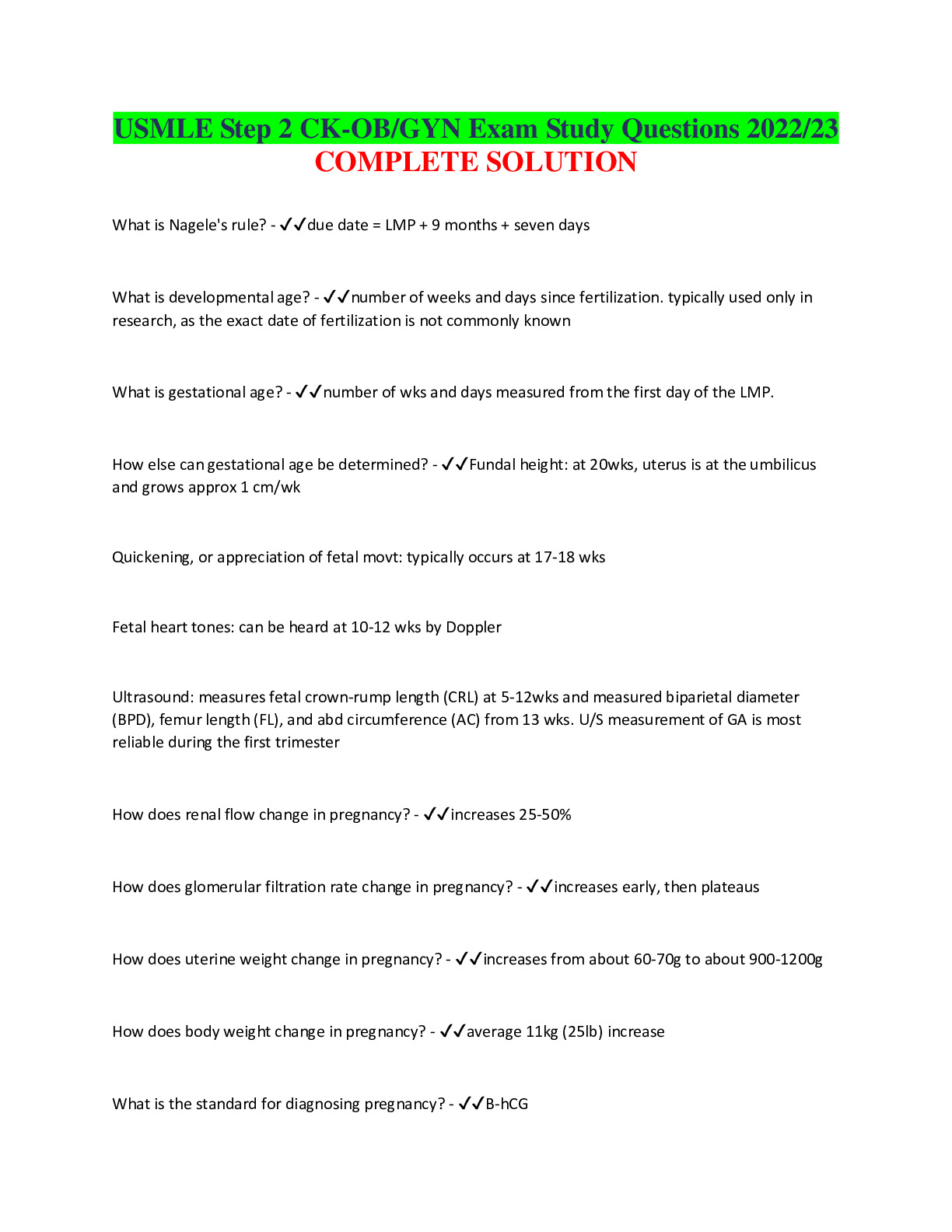
USMLE Step 2 CK-OB/GYN Exam Study Questions 2022/23 COMPLETE SOLUTION. 100% proven pass rate.
Document Content and Description Below
USMLE Step 2 CK-OB/GYN Exam Study Questions 2022/23 COMPLETE SOLUTION What is Nagele's rule? - ✔✔due date = LMP + 9 months + seven days What is developmental age? - ✔✔number of weeks and da ... ys since fertilization. typically used only in research, as the exact date of fertilization is not commonly known What is gestational age? - ✔✔number of wks and days measured from the first day of the LMP. How else can gestational age be determined? - ✔✔Fundal height: at 20wks, uterus is at the umbilicus and grows approx 1 cm/wk Quickening, or appreciation of fetal movt: typically occurs at 17-18 wks Fetal heart tones: can be heard at 10-12 wks by Doppler Ultrasound: measures fetal crown-rump length (CRL) at 5-12wks and measured biparietal diameter (BPD), femur length (FL), and abd circumference (AC) from 13 wks. U/S measurement of GA is most reliable during the first trimester How does renal flow change in pregnancy? - ✔✔increases 25-50% How does glomerular filtration rate change in pregnancy? - ✔✔increases early, then plateaus How does uterine weight change in pregnancy? - ✔✔increases from about 60-70g to about 900-1200g How does body weight change in pregnancy? - ✔✔average 11kg (25lb) increase What is the standard for diagnosing pregnancy? - ✔✔B-hCG- produced by placenta; peaks at 100,000 mIU/mL by 10wks of gestation - decreases throughout the second trimester; levels off in the third trimester - hCG levels double approx every 48hrs during early pregnancy. This is often used to diagnose ectopic pregnancy when doubling is abnormal What is a quantitative B-hCG used for? - ✔✔- to diagnose and follow ectopic pregnancy - to monitor trophoblastic disease - to screen for fetal aneuploidy What is a quad screen? - ✔✔1) Maternal serum alpha-fetoprotein - produced by the fetus, crosses the placenta in small amounts and enters the maternal circulation - Elevated: assoc w/ open neural tube defects (anencephaly, spina bifida), abd wall defects (gastroschisis, omphalocele), multiple gestation, incorrect gestational dating, fetal death, and placental abnormalities (e.g. placental abruption) - Decreased: assoc w/ trisomy 21 and 18, fetal demise, and inaccurate gestational dating. 2) inhibin A 3) estriol 4) B-hCG What quad screen results suggest Trisomy 18? - ✔✔ALL four decreased What quad screen results suggest Trisomy 21 - ✔✔decreased AFP and estriol Increased B-hCG and inhibin A How does heart rate change in pregnancy? - ✔✔gradually increases 20% How does blood pressure change in pregnancy? - ✔✔gradually decreases 10% by 34 wks, then increases to prepregnancy values How does stroke volume change in pregnancy? - ✔✔increases to maximum at 19wks, then plateausHow does cardiac output change in pregnancy? - ✔✔rises rapidly by 20%, then gradually increases an additional 10% by 28wks How does peripheral venous distention change in pregnancy? - ✔✔progressive increase to term How does peripheral vascular resistance change in pregnancy? - ✔✔progressive decrease to term How does respiratory rate change in pregnancy? - ✔✔unchanged How does tidal volume change in pregnancy? - ✔✔increases by 30-40% How does expiratory reserve change in pregnancy? - ✔✔gradual decrease How does vital capacity change in pregnancy? - ✔✔unchanged How does respiratory minute volume change in pregnancy? - ✔✔increases by 40% How does blood volume change in pregnancy? - ✔✔increases by 50% in second trimester How does hematocrit change in pregnancy? - ✔✔decreases slightly How does fibrinogen change in pregnancy? - ✔✔increases How do electrolytes change in pregnancy? - ✔✔unchanged How does sphincter tone change in pregnancy? - ✔✔decreasesHow does gastric emptying time change in pregnancy? - ✔✔increases What is the recommended amount of weight women should gain in pregnancy? - ✔✔an additional 100- 300 kcal/day; 500 kcal/day during breastfeeding Excessive gain: >1.5kg/mo Inadequate gain: <1 kg/mo What are the nutritional guidelines for pregnancy? - ✔✔folic acid supplements (decrease neural tube defects for all reproductive-age women): 0.4 mg/day Iron: 30mg/day of elemental iron Calcium: 1300 mg/day for women <19yo; 1000mg/day >19yo Vitamin D: 10ug or 400IU/day Vitamin B12: 2ug/day What is PAPP-A? - ✔✔pregnancy-assoc plasma protein A recommended at wks 9-14 to detect Down Syndrome and Trisomy 18 risk combined with ultrasound-determined nuchal transparency (fluid in the fetal neck) + B-hCG What is CVS? - ✔✔chorionic villus sampling recommended at wks 10-12 involves transcervical or transabd aspiration of placental (chorionic villi) tissue What are the advantages and disadvantages of CVS? - ✔✔Ads - diagnostic accuracy comparable to that of amnio, available at 10-12wks Disads - carries risk of fetal loss (1-2%); cannot detect open neural tube defects What are complications of CVS? - ✔✔limb defects have been assoc w/ CVS performed </= 9wksHow often should prenatal visits occur? - ✔✔Wks 0-28: every four wks Wks 29-35: every 2 wks Wks 36-birth: every wk What kind of testing should be completed at the initial prenatal visit? - ✔✔Heme: CBC, Rh factor, type and screen ID: UA and culture, rubella ab titer, HBsAg, RPR/VDRL, cervical gonorrhea and chlamydia, PPD, HIV, Pap smear (to check for dysplasia) If indicated: HbA1c, sickle cell screening Discuss genetic screening: Tay-Sachs, CF What kind of prenatal testing should be completed at 9-14wks? - ✔✔offer Triple Screen - PAPP-A - nuchal transparency - free B-hCG +/- CVS What kind of prenatal testing should be completed at 15-20wks? - ✔✔Offer Quad Screen - AFP - estriol - B-hCG - inhibin A +/- amniocentesis What kind of prenatal testing should be completed at 18-20wks? - ✔✔ultrasound for full anatomic screen What kind of prenatal testing should be completed at 24-28 wks? - ✔✔1hr glu challenge test for gestational diabetes screenWhat kind of prenatal testing should be completed at 28-30 wks? - ✔✔RhoGAM for Rh (-) women (after ab screen) What kind of prenatal testing should be completed at 32-36wks? - ✔✔GBS; repeat CBC What kind of prenatal testing should be compeleted at 34-40wks? - ✔✔cervical chlamydia and gonorrhea cultures, HIV, RPR in high-risk pts What is an amniocentesis? - ✔✔recommended 15-20wks consists of transabdominal aspiration of amniotic fluid using an ultrasound guided needle and eval of fetal cells for genetic studies What are the advantages and disadvantages of an amniocentesis? - ✔✔Ads - detects ~80% of open neural tube defects, ~85% of cases of Down syndrome, and ~60% of cases of trisomy 18 Disads - risks: premature rupture of membranes, chorioamnionitis, and fetal-maternal hemorrhage, which can result in fetal loss (0.5%) When is an amniocentesis indicated? - ✔✔- women who will be >35yo at time of delivery - conjunction w/ an abnormal quad screen - Rh-sensitized pregnancy to obtain fetal blood type or to detect fetal hemolysis - to evaluate fetal lung maturity via a lecithin-to-sphingomyelin ratio >/=2.5 or to detect the presence of phosphatidylglycerol (done during the third trimester) What does FDA Risk Category A suggest of drugs used during pregnancy? - ✔✔adequate and wellcontrolled studies in women fail to demonstrate a risk to the fetus in the 1st trimester (and there is no risk in later trimesters). Possibility of fetal harm seems remote. Ex) Vita B6, Vita E, folic acid (w/in recommended daily allowances)What does FDA Risk Category B suggest of drugs used during pregnancy? - ✔✔either animal reproduction studies have not demonstrated risk to the fetus but no adequate and well-controlled studies in pregnant women have been reported, or animal reproduction studies have shown an adverse effect that was not confirmed in controlled studies in women in the 1st trimester (and there is no evidence of risk in later trimesters). Ex) ampicillin, acetaminophen, buproprion What does FDA Risk Category C suggest of drugs used during pregnancy? - ✔✔either studies in animals have revealed adverse effects on the fetus but no controlled studies in women have been reported, or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus Ex) diphenhydramine, rifampin, AZT What does FDA Risk category D suggest of drugs used during pregnancy? - ✔✔positive evidence of human fetal risk exists, but the benefits from use in pregnancy women may be acceptable despite risk Ex) alcohol, phenytoin, tetracycline What does FDA Risk Category X suggest of drugs used during pregnancy/ - ✔✔studies in animals or humans have demonstrated fetal abnormalities, or evidence exists of fetal risk based on human experience, or both, and the risk in pregnant women clearly outweighs any possible benefit Ex) isotretinoin, thalidomide, warfarin What kinds of fetal defects are assoc w/ ACEIs? - ✔✔fetal renal tubular dysplasia and neonatal renal failure, oligohydramnios, IUGR, lack of cranial ossification What kinds of fetal defects are assoc w/ alcohol? - ✔✔FAS - growth restriction before and after birth- MR - midfacial hypoplasia - renal and cardiac defects Consumption of >6 drinks per day is assoc w/ a 40% risk of FAS What kinds of fetal defects are assoc w/ androgens? - ✔✔virilzation of females; advanced genital development in males What kinds of fetal defects are assoc w/ carbamazepine? - ✔✔neural tube defects, fingernail hypoplasia, microcephaly, developmental delay, IUGR what kinds of fetal defects are assoc w/ cocaine? - ✔✔bowel atresias, congenital malformations of the heart, limbs, face, and GU tract; microcephaly; IUGR, cerebral infarctions What kinds of fetal defects are assoc w/ DES? - ✔✔clear cell adenocarcinoma of the vagina or cervix, vaginal adenosis, abnormalities of the cervix and uterus or testes, possible infertility What kinds of fetal defects are assoc w/ lead? - ✔✔increased spontaneous abortion (SAB) rate; still births What kinds of defects are assoc w/ lithium? - ✔✔congenital heart disease (Ebstein's anomaly) What kinds of defects are assoc w/ methotrexate? - ✔✔increased SAB rate What kinds of defects are assoc w/ organic mecury? - ✔✔cerebral atrophy, microcephaly, MR, spasticity, seizures, blindness What kinds of fetal defects are assoc w/ phenytoin? - ✔✔IUGR, MR, microcephaly, dysmorphic craniofacial features, cardiac defects, fingernail hypoplasiaWhat kinds of fetal defects are assoc w/ radiation? - ✔✔microcephaly, MR, medical dx radiation delivery <0.05 Gy to the fetus has no teratogenic risk What kinds of fetal defects are assoc w/ streptomycin and kanamycin? - ✔✔hearing loss; CN VIII damage what kinds of fetal defects are assoc w/ tetracycline? - ✔✔premanent yellow-brown discoloration of deciduous teeth; hypoplasia of tooth enamel What kinds of fetal defects are assoc w/ thalidomide? - ✔✔bilateral limb deficiencies, anotia, microtia, cardiac and GI anomalies What kinds of fetal defects are assoc w/ Trimethadione and paramethadione? - ✔✔cleft lip or clef palate, cardiac defects, microcephaly, MR What kinds of fetal defects are assoc w/ valproic acid? - ✔✔neural tube defects (spinal bifida); minor cranial defects What kinds of fetal defects are assoc w/ vitamin A and derivatives? - ✔✔increased SAB rate, thymic agenesis, cardiovascular defects, craniofacial dysmorphism, microphthalamia, cleft lip, or clef phrase, MR What kinds of fetal defects are assoc w/ warfarin? - ✔✔nasal hypoplasia and stippled bone epiphyses, developmental delay, IUGR ophthalmologic abnormalities What are common sequelae of maternal-fetal infxns? - ✔✔premature delivery, CNS abnormalities, anemia, jaundice, hepatosplenomegaly, growth retardation What are the TORCH infxns? - ✔✔most common pathogens causing maternal-fetal infxns - Toxoplasmosis - Other (parvovirus, varicella, Listeria, TB, malaria, fungi) - Rubella- CMV - Herpes - HIV - Syphilis What kinds of animals should pregnant women avoid? - ✔✔cats they shouldn't change a cat's litterbox Which is more common, toxo during the first or third trimester? - ✔✔1st trimester: less common, more severe 3rd trimester: more common, less severe How does toxoplasmosis affect pregnant women? - ✔✔transplacental transmission w/ primary infxn occuring via consumption of raw meat or contact w/ cat feces. Specific findings: hydrocephalus, intracranial calcifications, chorioretinitis, ring-enhancing lesions on head CT How does rubella affect pregnant women? - ✔✔transplacental transmission in the 1st trimester. Specific findings: purpuric "blueberry muffin" rash, cataracts, MR, hearing loss, patent ductus arteriosus (PDA) How does CMV affect pregnant women? - ✔✔most common congenital infxn primarily transmitted transplacentally specific findings: petechial rash (similar to "blueberry muffin" rash) and periventricular calcifications How does herpes affect pregnant women? - ✔✔intrapartum transmission if the mother has active lesions Causes skin, eye, and mouth infxns or life-threatening CNS/systemic infxnHow does HIV affect pregnant women? - ✔✔Transmission can occur in utero, at the time of delivery, or via breast milk Occurs in 13-39% of births to infected mothers Combination of AZT tx (prenatally, intrapartum, and neonatally for the first six wks of life) and C-section can lower transmission to 2%. Newborns w/ congenitally acquired HIV are often ASx, failure to thrive, bacterial infxns w/ common organisms, and an increased incidence of upper and lower respiratory diseases may appear early or may be delayed for months to years. HIV + mothers should not breastfeed How does syphilis affect pregnant women? - ✔✔Primarily intrapartum transmission Specific findings: maculopapular skin rash, lymphadenopathy, hepatomegaly, "snuffles" mucopurulent rhinitis, osteitis Childhood findings: saber shins, saddle nose, CNS involvement and Hutchinson's traid: peg-shaped upper central incisors, deafness, and interstitial keratitis (photophobia, lacrimation) What is the definition of SAB? - ✔✔loss of products of conception prior to the 20th wk of pregnancy. Approx 60% of chemically evident pregnancies and 15-20% of clinically dx pregnancies terminate in a SAB. More than 80% occur in first trimester What are the risk factors for an SAB? - ✔✔Chromosomal abnormalities Maternal factors - maternal trauma, increased maternal age, infxn, dietary deficiencies - inheritied thrombophilias: Factor V Leiden, prothrombin, antithrombin, proteins C and S, methylene tetrahydrofolate reductase (hyperhomocysteinemia) - immunologic issues: antiphospholipids abs, alloimmune factors - anatomic issues: uterine abnormalities, incompetent cervix, cervical conization, loop electrosurgical excision procedure, cervical injury, DES exposure, anatomical abnormalities of the cervix - endocrine issues: DM, hypothyroidism, progesterone deficiency Environmental factors: Tabacco, alcohol, caffeine, toxins, drugs, radiationFetal factors: anatomic malformation How is SAB dx? - ✔✔decreasing level of hCG U/S: identify the gestational sac 5-6 wks from LMP, a fetal pole at six wks, fetal cardiac activity 6-7wks; accurate dating, a small, irregular intrauterine sac w/o fetal pole on transvaginal U/S is diagnostic of abnormal pregnancy Maternal Rh type should be determined and RhoGAM given if the type is Rh neg What is included in a normal obstetric exam? - ✔✔1) Leopold's maneuvers: determine fetal lie (longitudinal or transverse) and if possible, fetal presentation (breech or cephalic) 2) Cervical examination: evaluate dilation, effacement, station, cervical position, cervical consistency. Use Bishop score. Confirm or determine fetal presentation. Determine fetal position through palpation of the fetal sutures and fontanelles. Conduct a sterile speculum exam if rupture of membranes is suspected What is the Bishop score? - ✔✔used to evaluate the favorability of delivery and the probability of succeeding w/ an induction. Scoring: 0-4: indicates 45-50% chance of failure. Give prostaglandins for induction 5-9: points to a 10% chance of failure. Give pitocin for induction 10-13: assoc w/ very high probability of success. There is no need for intervention for induction What are the different types of SAB? - ✔✔- Complete - Incomplete - Threatened - Inevitable - Missed - Septic - Intrauterine fetal demise- Recurrent What is a complete SAB? - ✔✔POC is expelled. Pain ceases, but spotting may persist. CLOSED OS U/S shows empty uterus POC should be sent to pathology to confirm fetal tissue No further intervention needed What is an incomplete SAB? - ✔✔some POC expelled, bleeding/mild cramping. Visible tissue on exam. OPEN OS U/S shows retained fetal tissue Intervention: manual uterine aspiration (MUA) or D&C What is a threatened SAB? - ✔✔No POC expelled. Uterine bleeding +/- abd pain CLOSED OS intact membranes, fetal cardiac motion on U/S Intervention: pelvic rest for 24-48hrs and follow-up U/S to assess the viability of conceptus What is an inevitable SAB? - ✔✔No POC expelled. Uterine bleeding and cramps OPEN OS +/- ROM Intervention: MUA, D&C, misoprostol, or expectant mgmt What is a missed SAB? - ✔✔No POC expelled, No fetal cardiac motion, No uterine bleeding. Brownish vaginal discharge CLOSED OSNo fetal cardiac activity, retianed fetal tissue on U/S Intervention: MUA, D&C, or misoprostol What is a septic SAB? - ✔✔endometritis leading to septicemia. Maternal mortality is 10-15% Hypotension, hypothermia, increased WBC count Intervention: MUA, D&C, IV abx What is an intrauterine fetal demise? - ✔✔absence of fetal cardiac activity Uterus is small for GA; no fetal heart tones or movt on U/S Intervention: induce labor; evacuate the uterus (D&E) to prevent DIC at GA >16wks What is recurrent SAB? - ✔✔Early pregnancy: often due to chromosomal abnormalities Late pregnancy: due to hypercoagulable states (SLE, factor V Leiden, protein S deficiency) Incompetent cervix: should be suspected w/ hx of painless dilation of cervix and delivery of a normal fetus btw 8 and 32 wks Karyotype both parents. Hypercoagulability work-up in mom. Evaluate for uterine abnormalities Intervention: surgical cerclage procedures to suture the cervix closed until labor or ROM occurs w/ subsequent removal prior to delivery. Restrict activities what is the medical procedures for a first trimester therapeutic abortion? - ✔✔1) oral mifepristone (low dose) + oral/vaginal misoprostol UP TO 49 days GA 2) IM/oral methotrexate + oral/vaginal misoprostol UP TO 49 days GA 3) vaginal or sublingual or buccal misoprostol (high dose), repeated up to three times UP TO 56 days GAWhat is the surgical procedure for a first trimester therapeutic abortion? - ✔✔1) manual aspiration 2) D&C w/ vacuum aspiration BOTH UP TO 13 wks GA What is the obstetric mgmt for a second trimester therapeutic abortion? - ✔✔induction of labor (typically w/ prostaglandins, amniotomy, and oxytocin) UP TO 13-24 wks GA (depending on state laws) What is the surgical option for a second trimester therapeutic abortion? - ✔✔D&E UP TO 13-24 wks GA (depending on state laws) What are the recommendations for FHR monitoring in pts w/o complications? - ✔✔Review FHR tracings every 30 min in the first stage of labor and every 15 min in the second stage of labor What are the recommendations for FHR monitoring in pts w/ complications - ✔✔Review FHR tracings every 15 min in the first stage of labor and every 5 min in the second stage of labor What are the components of reading FHR? - ✔✔Rate (normal = 110-160) - <110 = bradycardia ---caused by congenital heart malformations or severe hypoxia (secondary to uterine hyperstimulation, cord prolapse, or rapid fetal descent) - >160 = tachycardia ---can be caused by hypoxia, maternal fever, fetal anemia Variability (normal beat to beat variability = 6-25 bpm) - undetectable variability indicates severe fetal distress - minimal variability (<6) indicates fetal distress or effects of opioids or mag - marked variability (>25) indicates fetal distress; or may occur before a decrease in variability- sinusoidal variability: points to serious fetal anemia; may also occur during maternal meperidine use - accelerations: onset of increase in FHR to a peak in <30sec. Reassuring b/c they indicate fetal ability to appropriately respond to the environment - decelerations: several types (early, late, variable) What are the stages of labor? - ✔✔First stage - latent - active Second Third What occurs during the first stage of labor? - ✔✔Latent: onset of labor to 3-4cm dilation - primiparous: 6-11hrs - multiparous: 4-8hrs - prolonged if excessive sedation and hypertonic uterine contractions Active: 4cm to complete cervical dilation (10cm) - primiparous: 4-6hrs (1.2cm/hr) - multiparous: 2-3hrs (1.5cm/hr) - prolongation seen w/ cephalopelvic disproportion what occurs during the second stage of labor? - ✔✔complete cervical dilation to delivery of infant - primparous: 0.5-3.0hrs - multiparous: 5-30min When baby goes through all cardinal mvts of delivery What occurs during the third stage of labor? - ✔✔delivery of infant to delivery of placenta - primparous and multiparous: 0-0.5 hr uterus contracts and placenta separates to establish hemostasisWhat is an early fetal deceleration? - ✔✔visually apparent, gradual (onset to nadir in >30sec) decrease in FHR w/ a return to baseline that mirrors the uterine contraction Etiology: head compression from uterine contraction (normal) What is a late fetal deceleration? - ✔✔WORRISOME visually apparent, gradual (onset to nadir in >30 sec) decrease in FHR w/ return to baseline whose onset, nadir, and recovery occur after the beginning, peak, and end of uterine contraction, respectively Etiology: uteroplacental insufficiency and fetal hypoxemia What is a variable fetal deceleration? - ✔✔an abrupt (onset to nadir in <30sec), visually apparent decrease in FHR below baseline lasting >/= 15 sec but <2 min Etiology: umbilical cord compression What are the indications for antepartum fetal surveillance? - ✔✔used in pregnancies w/ increased risk for fetal demise. Begin 32-34wks for at risk pts 26-28 if there are multiple worrisome risks What are the components of antepartum fetal surveillance? - ✔✔Fetal movt assessment: - # movts in an hr; assessed by mom - average is 10 movts q20min - if decreased movt... Nonstress Test (NST) - mom is resting in lateral tilt position (prevent supine hypotension) - FHR monitored externally by Doppler along w/ a tocodynamometer to detect uterine contractions - Acoustic stimulation can be used - Results:---"reactive" (normal response): two accelerations of >/=15 bpm above baseline lasting for at least 15 sec over a 20min period ---"nonreactive": fewer than two accelerations over a 20 min period. Perform further tests (e.g. biophysical profile). Lack of FHR accelerations may occur w/ any of the following: -----GA<32 wks -----fetal sleping -----fetal CNS anomalies -----maternal sedative or narcotic administration Contraction Stress Test (CST) - mom in lateral recumbent position - FHR monitored during spontaneous or induced (via nipple stimulation or oxytocin) contractions - reactivity is determined from fetal heart monitoring, as w/ NST - procedure CI in women w/ preterm membrane rupture or known placenta previa; women w/ history of uterine surgery; women who are at high risk for preterm labor - Results: ---"Positive" CST: late decelerations following 50% or more of contractions in a 10min window; raises concerns about fetal compromise. DELIVERY NEEDED ---"Negative" CST: no late or significant variable decelerations w/in 10 min and at least 3 contractions. Highly predictive of fetal well-being in conjunction w/ a normal NST ---"Equivocal" CST: defined by intermittent late decelerations or significant variable decelerations Biophysical profile (BPP) - real-time U/S to assign a score of 2 (normal) or 0 (abnormal) to five parameters --fetal tone --breathing --movement --amniotic fluid volume --NST - Scoring:---8-10: reassuring for fetal well-being ---6: considered equivocal. Term pregnancies delivered w/ this profile ---0-4: Extremely worrisome for fetal asphyxia; strong consideration should be given to immediate delivery if no other explanation is found Modified BPP (mBPP) - combines NST w/ amniotic fluid index (AFI). Normal if reactive NST and AFI>5cm Umbilical artery Doppler Velocimetry - IUGR: reduction and even reversal of umbilical artery diastolic flow. Test is of benefit only when IUGR is suspected Oligohydramnios (AFI <5 cm) ALWAYS warrants further work-up Where is the pain in uterine contractions and cervical dilation? - ✔✔visceral pain at T10-L1 Where is the pain when the fetal head descends and pressure is placed on vagina and perineum? - ✔✔somatic pain at S2-S4 What are absolute CI to regional anesthesia during delivery? - ✔✔refractory maternal hypotension maternal coagulopathy maternal use of once-daily dose of LMW Heparin w/in 12hrs untreated maternal bacteremia skin infxn over the site of needle placement Increased ICP caused by mass lesion What is hyperemesis gravidarum? - ✔✔persistent vomiting not related to other causes, acute starvation (usually large ketonuria), and weight loss Evaluate Severity:- ketonemia, ketonuria, hyponatremia, and hypokalemic, hypochloremic metabolic alkalosis - measure LFTs, serum bilirubin, serum amylase/lipase More common in first pregnancy, multiple gestations, and molar pregnancies. - check B-hCG and U/S to r/o molar pregnancy If "morning sickness" persists after the first trimester, think hyperemesis gravidarum Increased B-hCG and estradiol implicated R/O acid reflux, gastroenteritis, hyperthyroidism, neuro conditions What are the different types of pain relief offered to delivery moms? - ✔✔Nonpharmacologic Opiods Local block (lidocaine) Epidural Spinal Combined spinal epidural General What is included in nonpharmacologic pain relief and what are the advantages of this method? - ✔✔social support, massages, breathing, aromatherapy, ambulation, and repositioning - no known neg side effects - works by increasing coping w/ pain rather than eliminating pain BUT offers limited pain relief What are the advantages/disadvantages of using opiods for obstetric analgesia/anesthesia? - ✔✔ADS: provide an adequate level of pain relief for some women w/o risks assoc w/ regional anesthesiaDISADS: sedative effect of opiods decreases FHR variability and increases the possible need for neonatal naloxone admin and five-min APGAR scores <7 What are the advantages/disadvantages of using local blocks for obstetric analgesia/anesthesia? - ✔✔ADS: excellent anesthesia before episiotomy and during repair of lacerations; can be used to perform a pudendal block DISADS: rarely, may cause seizures, hypotension, and cardiac arrhythmias What are the advantages/disadvantages of using epidural for obstetric analgesia/anesthesia? - ✔✔ADS: MOST effective form of pain relief; can also be used for C-section or postpartum tubal ligation DISADS: can result in pruritis, fever, hypotension, and transient FHR deceleration What are the advantages/disadvantages of using spinal for obstetric analgesia/anesthesia? - ✔✔ADS: rapid onset analgesia that provides excellent pain relief for procedures of limited duration (30-250min) DISADS: Limited duration. Puts pts at risk for hypotension, postdural puncture headache, and transient neuro sx What are the advantages/disadvantages of using combined spinal epidural for obstetric analgesia/anesthesia? - ✔✔ADS: offers rapid onset of spinal analgesia combined w/ ability to prolong duration of analgesia w/ continuous epidural infusion DISADS: carries risk of both procedures; may increase risk of bradycardia and emergent cesarean delivery over epidural analgesia alone What are the advantages/disadvantages of using general anesthesia for obstetric analgesia/anesthesia? - ✔✔ADS: used in emergent c-section and indicated in some cases of FHR abnormality; can be useful in cases where regional anesthesia is absolutely CI or failsDISADS: requires airway control; carries significant risk of maternal aspiration and neonatal depression (inhaled anesthetic agents readily cross placenta); assoc w/ higher maternal morbidity rates than epidural anesthesia How is hyperemesis gravidum tx? - ✔✔1) Admin Vitamin B6 2) doxylamine (antihistamine) PO 3) Promethazine or deminhydrinate PO/PR 4) If severe: metoclopramide, ondansetron, prochlorperazine, or promethazine IM/PO 5) If dehydrated: IV fluids, IV nutritional supplementation, dimenhydrinate IV What is the difference btw gestational diabetes and pregestational diabetes? - ✔✔gestational = onset occurs during pregnancy What classification system is used to risk stratify women with diabetes assoc w/ pregnancy? - ✔✔White Classification A1: gestational; insulin not required A2: gestational; insulin required B: age of onset 20yrs or older or duration <10yrs C: age of onset 10-19yrs or duration 10-19yrs D: age of onset<10yrs or duration >20yrs F: nephropathy H: cardiomyopathy R: proliferating retinopathy RF: proliferating retinopathy T: renal transplant How does gestational diabetes present? - ✔✔typically ASx Edema, polyhydramnios, or a large-for-GA infant (>90th percentile) may be warning signs occurs in 3-5% of all pregnancies, usually in late pregnancyHow is gestational diabetes dx? - ✔✔1) One hr 50g glu challenge test; venous plasma glucose is measured one hr later (at 24-48wks). Values >/=140mg/dL are considered abnormal 2) Confirm w/ an oral three hr 100g glu tolerance test showing any two of the following: fasting >95mg/dL; one hr>180mg/dL; two hr>155mg/dL, three hrs >140mg/dL How is gestational diabetes tx? - ✔✔Mom: 1) start on ADA diet, regular exercise, strict glu monitoring (4x/day). Tight maternal glu control (fasting glu <100; one to two hr postprandial glu <150) improves outcomes 2) add insulin if dietary control is insufficient Give intrapartum insulin and dextrose to maintain tight control during delivery Fetus: - Obtain periodic U/S and NSTs to assess fetal growth and well being (30-32wks) - may be necessary to induce labor at 39-40wks What are complications of gestational diabetes? - ✔✔more than 50% pts go on to develop glucose intolerance and/or type 2DM later in life What are risks of pregestational diabetes? - ✔✔poorly controlled DM is assoc w/ increased risk of congenital malformations, fetal loss, and maternal/fetal morbidity during labor and delivery How is pregestational diabetes tx? - ✔✔Mother: - renal, ophthalmologic, and cardiac evaluation to assess for end-organ damage. - strict glu control (w/ diet, exercise, insulin tx, and frequent self-monitoring for type 1 and type 2 DM) to minimize fetal defects --Fasting AM<90mg/dL --two-hr postprandial<120mg/dL Fetus:- 18-20wks: u/s to determine fetal age and growth: evaluate for cardiac anomalies and polyhydramnios; quad screen to screen for developmental anomalies - 32-4wks: close fetal surveillance (NST, CST, BPP). Admit if maternal DM has been poorly controlled for fetal parameters are a concern. Serial U/S for fetal growth Delivery and postpartum - maintain normoglycemia (80-100mg/dL) during labor w/ an IV insulin drip and hourly glu measurements - consider early delivery in the setting of poor maternal glu control, preeclampsia, macrosomia, evidence of fetal lung maturity - c-section should be considered for EFW> 4500g - encourage breastfeeding w/ appropriate increase in caloric intake - continue glu monitoring postpartum. Insulin needs rapidly decrease after delivery What lab tests in mom suggest pregestational diabetes? - ✔✔HgbA1c>8% UA before 20wks reveals glycosuria Hyperglycemia in 1st trimester What is the difference btw gestational and chronic HTN? - ✔✔Gestational HTN: - aka PIH - idiopathic HTN w/o significant proteinuria (<300mg/L) that develops at >20wks' gestation. 25% will develop preeclampsia Chronic HTN: - present before conception and at <20wks gestation, may persist >12wks postpartum - 1/3 may develop superimposed preeclampsia How are gestational and chronic HTN tx? - ✔✔Monitor BP closely and tx w/ appropriate anti-HTN (methyldopa, labetalol, nifedipine). DO NOT give ACEIs or diureticsWhat are complications that can occur if pregnant pts receive ACEIs or diuretics? - ✔✔ACEIs: uterine ischemia Diuretics: low plasma volume to point of uterine ischemia What are complications of gestational and chronic HTN? - ✔✔similar to preeclampsia What is preeclampsia? - ✔✔new onset HTN (SBP>140 or DBP> 90) and proteinuria (>300mg in 24hrs) occuring at >20wks gestation What is eclampsia? - ✔✔new onset grand mal seizures in women w/ preeclampsia What is HELLP syndrome? - ✔✔Hemolytic anemia Elevated liver enzymes Low platelet Variant of preeclampsia w/ poor prognosis Clinical manifestations explained by vasospasm leading to hemorrhage and organ necrosis What are maternal complications of pregestational DM? - ✔✔DKA (type 1) HHNK (type 2) preeclampsia/eclampsia cephalopelvic disproportion (from macrosomia) and need for C-section preterm labor infxn polyhydramnios postpartum hemorrhage maternal mortality What are fetal complications of pregestational DM? - ✔✔macrosomia or IUGR cardiac and renal defectsneural tube defects (sacral agenesis) hypocalcemia polycythemia hyperbilirubinemia IUGR hypoglycemia from hyperinsulinemia respiratory distress syndrome birth injury (shoulder dystocia) perinatal mortality What are risk factors for preeclampsia/eclampsia? - ✔✔nulliparity, African-American ethnicity, extremes of age (<20 or >35), multiple gestation, molar pregnancy, renal disease (due to SLE or type I DM), FHx of preeclampsia, chronic HTN What are the s/sx of mild preeclampsia? - ✔✔usually ASx BP>/= 140/90 on 2 occasions >6hrs apart Proteinuria (>300mg/24hrs or 1-2 + urine dipsticks) Edema What are the s/sx of severe preeclampsia? - ✔✔BP>160/110 on two occasions >6hrs apart Renal: proteinuria (>5g/24hrs or 3-4+urine dipsticks) or oliguria (<500 mL/24hrs). Cerebral changes: headache, somnolence Visual changes: blurred vision, scotoma Hyperactive reflexes/clonus RUQ pain Hemolysis, elevated liver enzymes, thrombocytopenia (HELLP) What are the s/sx of eclampsia? - ✔✔signs preceding eclamptic attack - HA, visual changes, RUQ/epigastric painSeizures are severe if not controlled w/ anticonvulsant tx What is the classic triad for preeclampsia? - ✔✔HTN proteinuria edema What is the ONLY cure for preeclampsia/eclampsia? - ✔✔delivery of fetus How is preeclampsia tx? - ✔✔if pts is close to term or preeclampsia worsens, induce delivery w/ IV oxytocin, prostaglandin, amniotomy if far from term, tx w/ modified bed rest and expectant mgmt How is severe preeclampsia tx? - ✔✔1) Control BP w/ labetalol and/or hydralazine (goal <160/110, DBP btw 90-110 to maintain fetal blood flow). 2) Prevent seizures w/ continuous MgSO4 drip - watch for signs of mg toxicity (Loss of DTRs, respiratory paralysis, coma). Continue seizure prophy for 24hrs postpartum. Tx mg toxicity w/ IV calcium gluconate 3) Delivery by induction of C-section when mother is stable How is eclampsia tx? - ✔✔1) ABCs w/ O2 2) seizure control/prophy w/ mg. If seizures recur, give IV diazepam. Monitor mg blood levels and mag toxicity; monitor fetus status. Control BP (labetalol and/or hydralazine). Limit fluids; Foley for strict I/Os. 3) Initiate delivery if pt is stable and convulsions are controlled. Postpartum mgmt is the same as that for preeclampsia. Seizures may occur antepartum, intrapartum, or postpartum. Most w/in 48hrs after delivery What are complications of preeclampsia? - ✔✔prematurity fetal distress stillbirth placental abruptionseizure DIC cerebral hemorrhage serous retinal detachment fetal/maternal death What are complications of eclampsia? - ✔✔cerebral hemorrhage aspiration pneumonia hypoxic encephalopathy thromboembolic events fetal/maternal death What are possible causes of third trimester bleeding? - ✔✔Vagina: bloody show, trauma Cervix: cervical cancer, cervical/vaginal lesion Placenta: placental abruption, placenta previa Fetus: fetal bleeding What is antepartum bleeding? - ✔✔bleeding that occurs after 20wks gestation (bleeding before 20wks = threatened abortion) most common causes: placental abruption, placenta previa other causes: abnormal placentation (placenta accreta), ruptured uterus, genital tract lesions, and trauma What is placental abruption? - ✔✔premature (before delivery) separation of normally implanted placenta What are risk factors for placental abruption? - ✔✔HTN abd/pelvic trauma tobacco or cocaine useprevious abruption rapid decompression of an overdistended uterus excessive stimulation What are sx of placental abruption? - ✔✔PAINFUL Dark vaginal bleeding that does not spontaneously cease Abd pain, uterine hypertonicity Fetal distress How is placental abruption dx? - ✔✔Clinical dx Transabdominal/transvaginal U/S sensitivity : 50% Look for retroplacental clot; most useful for ruling out previa How is placental abruption tx? - ✔✔Stabilize pt w/ mild abruption and a premature fetus-->manage expectantly --hospitalize --start IV and fetal monitoring --type and cross blood --bed rest Moderate to severe abruption-->IMMEDIATE delivery -- vaginal delivery w/ amniotomy if mother and fetus are stable and delivery is expected soon --C-section for maternal or fetal distress What are complications of placental abruption? - ✔✔Hemorrhagic shock Coagulopathy: DIC in 10% Recurrence risk is 5-16% and rises to 25% after 2 previous abruptions Fetal hypoxiaWhat is placenta previa? - ✔✔Abnormal placental implantation - total: covers cervical os - marginal: placenta extends to margin of the os - low-lying: placenta is in close proximity to os What are risk factors for placenta previa? - ✔✔prior C-sections, grand multiparity, advanced maternal age, multiple gestation, prior placenta previa How does placenta previa present? - ✔✔PAINLESS bright red blood that often ceases in 1-2 hrs w/ or w/o uterine contractions Usually no fetal distress How is placenta previa dx? - ✔✔transabdominal/transvaginal U/S sensitivity is >95% Look for an abnormally positioned placenta How is placenta previa tx? - ✔✔NO VAGINAL EXAMS! stabilize pts w/ a premature fetus-->mgmt expectantly Give tocolytics Serial U/S to assess fetal growth; resolution of partial previa Give betamethasone to help w/ fetal lung maturity Delivery by C-section --Indications for delivery ---labor ---life-threatening bleeding ---fetal distress ---documented fetal lung maturity ---36wks GA What are complications of placenta previa? - ✔✔increased risk of placenta accretavasa previa (fetal vessels crossing the internal os preterm delivery, PROM, IUGR, congenital anomalies [Show More]
Last updated: 3 years ago
Preview 1 out of 87 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$7.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 03, 2022
Number of pages
87
Written in
All
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Sep 03, 2022
Downloads
0
Views
281