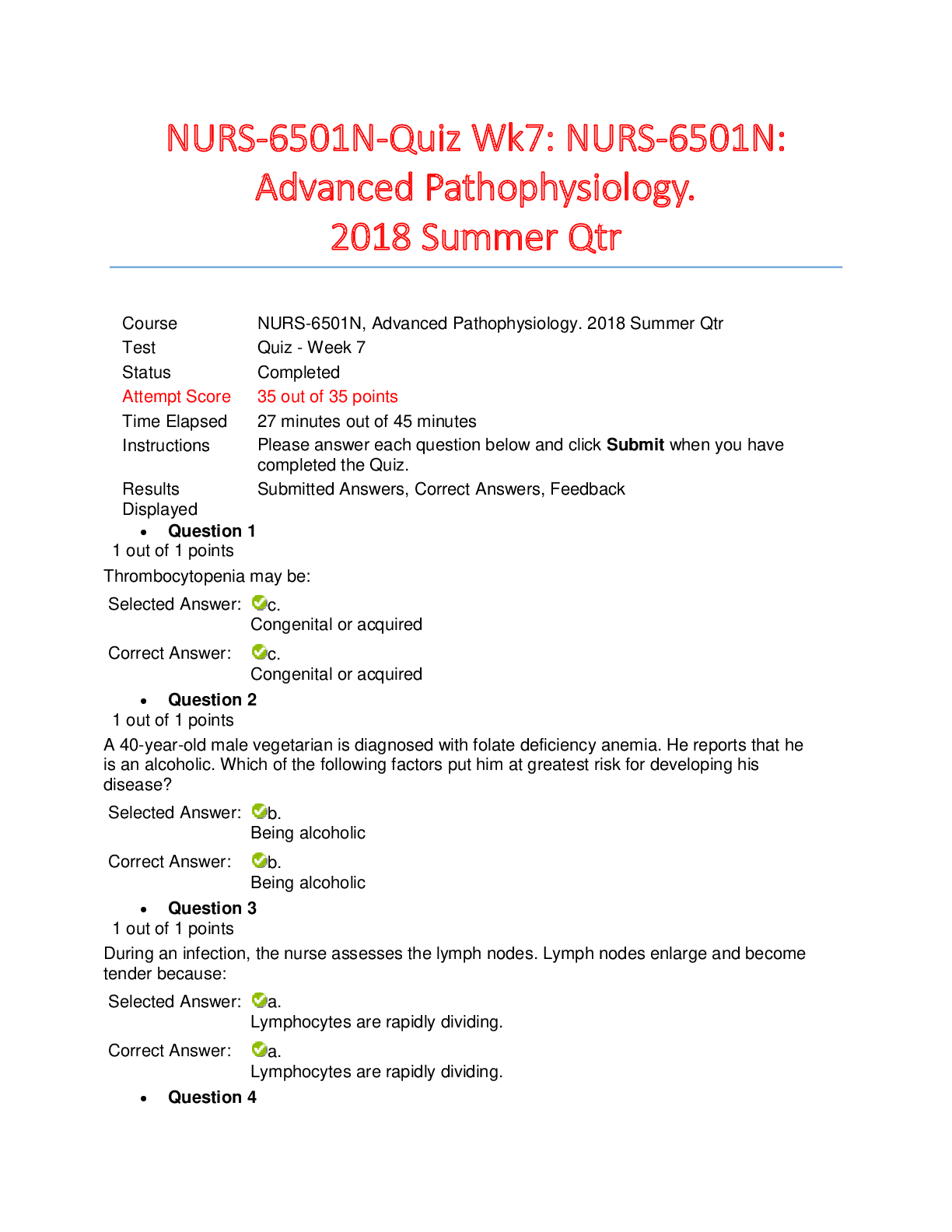
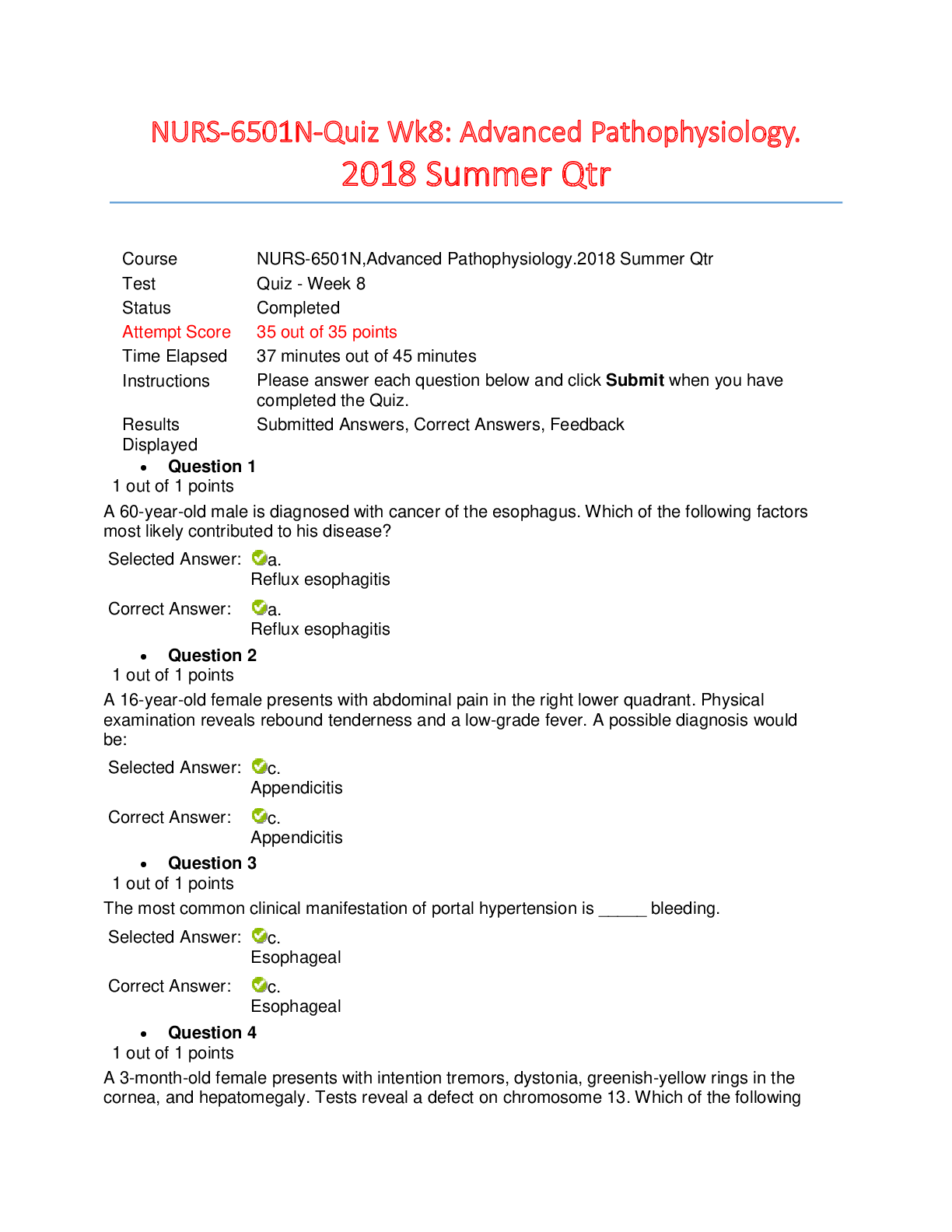
*NURSING > QUESTIONS & ANSWERS > AHIMA CCA: Exam Study Questions 1025 Questions with 100% Correct Answers – COMPLETE SOLUTION (All)
AHIMA CCA: Exam Study Questions 1025 Questions with 100% Correct Answers – COMPLETE SOLUTION
Document Content and Description Below
AHIMA CCA: Exam Study Questions 1025 Questions with 100% Correct Answers – COMPLETE SOLUTION 1. A 65-year-old white male was admitted to the hospital on 1/15 complaining of abdominal pain. The a... ttending physician requested an upper GI series and laboratory evaluation of CBC and UA. The x-ray revealed possible cholelithiasis, and the UA showed an increased white blood cell count. The patient was taken to surgery for an exploratory laparoscopy, and a ruptured appendix was discovered. The chief complaint was: a. Ruptured appendix b. Exploratory laparoscopy c. Abdominal pain d. Cholelithiasis - ✔✔c. Abdominal pain The nature and duration of the symptoms that caused the patient to seek medical attention as stated in the patient's own words (Odom-Wesley et al. 2009, 331). 2. 84. An individual stole and used another person's insurance information to obtain medical care. This action would be considered: a. Violation of bioethics b. Fraud and abuse c. Medical identity theftd. Abuse - ✔✔c. Medical identity theft Correct Answer: 84. c. Medical identity theft occurs when someone uses a person's name and sometimes other parts of their identity without the victim's knowledge or consent to obtain medical services or goods (Johns 2011, 773). 3. Identify the ICD-9-CM diagnostic code(s) for acute osteomyelitis of ankle due to Staphylococcus. a. 730.06 b. 730.07 c. 730.07, 041.1 d. 730.07, 041.10 - ✔✔d. 730.07, 041.10 Correct Answer: D Index Osteomyelitis, acute or subacute. Refer to the table in the Index for the fifth digit 5, ankle and foot. Infection, staphylococcal NEC (Schraffenberger 2012, 305-306). 4. A system that provides alerts and reminders to clinicians is a(n): a. Clinical decision support system b. Electronic data interchange c. Point of care charting systemd. Knowledge database - ✔✔Correct Answer: A Clinical decision support includes providing documentation of clinical findings and procedures, active reminders about medication administration, suggestions for prescribing less expensive but equally effective drugs, protocols for certain health maintenance procedures, alerts that a duplicate lab test is being ordered, and countless other decisionmaking aids for all stakeholders in the care process (Johns 2011, 138). 5. What does an audit trail check for? a. Unauthorized access to a system b. Loss of data c. Presence of a virus d. Successful completion of a backup - ✔✔Correct Answer: A Audit trails can provide tracking information such as who accessed which records and for what purpose (Johns 2011, 403). 6. This is a condition with an imprecise diagnosis with various characteristics. The condition may be diagnosed when a patient presents with sinus arrest, sinoatrial exit block, or persistent sinus bradycardia. This syndrome is often the result of drug therapy, such as digitalis, calcium channel blockers, beta-blockers, sympatholytic agents, or antiarrhythmics. Another presentation includes recurrent supraventricular tachycardias associated with bradyarrhythmias. Prolonged ambulatory monitoring may be indicated to establish a diagnosis of this condition. Treatment includes insertion of a permanent cardiac pacemaker. a. Atrial fibrillation (427.31) b. Atrial flutter (427.32)c. Paroxysmal supraventricular tachycardia (427.0) d. Sick sinus syndrome (SSS) (427.81) - ✔✔d. Sick sinus syndrome (SSS) (427.81) Correct Answer: D SSS is the imprecise diagnosis with various characteristics treated with the insertion of a permanent cardiac pacemaker. The other three conditions are treated with cardioversion and different pharmacological therapy (Schraffenberger 2012, 194-195). 7. Identify the ICD-9-CM diagnostic code for primary localized osteoarthrosis of the hip. a. 715.95 b. 715.15 c. 721.90 d. 715.16 - ✔✔b. 715.15 Correct Answer: B Index Osteoarthrosis, localized, primary. For category 715, refer to the table for the fifth digit of 5 for pelvic region and thigh (Schraffenberger 2012, 303-304). 8. A health record with deficiencies that is not complete within the timeframe specified in the medical staff rules and regulations is called a(n): a. Suspended record b. Delinquent recordc. Pending record d. Illegal record - ✔✔Correct Answer: B An incomplete record not rectified within a specific number of days as indicated in the medical staff rules and regulations is considered to be delinquent (Johns 2011, 412). 9. A hospital HIM department wants to purchase an electronic system that records the location of health records removed from the filing system and documents the date of their return to the HIM department. Which of the following electronic systems would fulfill this purpose? a. Chart deficiency system b. Chart tracking system c. Chart abstracting system d. Chart encoder - ✔✔Correct Answer: B With an automated tracking system, it is easy to track how many records are charged out of the system, their location, and whether they have been returned on the due dates indicated (Johns 2011, 402). 10. Identify the appropriate ICD-9-CM diagnosis code for Lou Gehrig's disease. a. 335.20 b. 334.8c. 335.29 d. 335.2 - ✔✔Correct Answer: A Index Disease, Lou Gehrig's or Lou Gehrig's disease. Amyotrophic lateral sclerosis is another name for Lou Gehrig's disease. Many diseases carry the name of a person or an eponym. The main terms for eponyms are located in the Alphabetic Index under the eponym or the disease, syndrome, or disorder (Schraffenberger 2012, 13). 11. In the laboratory section of CPT, if a group of tests overlaps two or more panels, report the panel that incorporates the greatest number of tests to fulfill the code definition. What would a coder do with the remaining test codes that are not part of a panel? a. Report the remaining tests using individual test codes, according to CPT. b. Do not report the remaining individual test codes. c. Report only those test codes that are part of a panel. d. Do not report a test code more than once regardless whether the test was performed twice. - ✔✔Correct Answer: A Reporting additional test codes that overlap codes in a panel allows the coder to assign all appropriate codes for services provided. It is inappropriate to assign additional panel codes when all codes in the panel are not performed. Reporting individual lab codes is appropriate when all codes in a panel have not been provided (AMA 2012b, 402). 12.An electrolyte panel (80051) in the laboratory section of CPT consists of tests for carbon dioxide (82374), chloride (82435), potassium (84132), and sodium (84295). If each of the component codes are reported and billed individually on a claim form, this would be a form of: a. Optimizing b. Unbundling c. Sequencing d. Classifying - ✔✔Correct Answer: B Unbundling occurs when a panel code exists and the individual tests are reported rather than the panel code (AMA 2012b, 402). 13. Coronary arteriography serves as a diagnostic tool in detecting obstruction within the coronary arteries. Identify the technique using two catheters inserted percutaneously through the femoral artery. a. Combined right and left (88.54) b. Stones (88.55) c. Judkins (88.56) d. Other and unspecified (88.57) - ✔✔Correct Answer: C The Judkins technique provides x-ray imaging of the coronary arteries by introducing one catheter into the femoral artery with maneuvering up into the left coronary artery orifice, followed by a second catheter guided up into the right coronary artery, and subsequent injection of a contrast material (Schraffenberger 2012, 206).Ensuring the continuity of future care by providing information to the patient's attending physician, referring physician, and any consulting physicians is a function of the: a. Discharge summary b. Autopsy report c. Incident report d. Consent to treatment - ✔✔Correct Answer: A The discharge summary is a concise account of the patient's illness, course of treatment, response to treatment, and condition at the time the patient is discharged (Johns 2011, 78). 15. This document includes a microscopic description of tissue excised during surgery: a. Recovery room record b. Pathology report c. Operative report d. Discharge summary - ✔✔Correct Answer: B The pathology report describes specimens examined by the pathologist (Johns 2011, 77). 16.CMS developed medically unlikely edits (MUEs) to prevent providers from billing units of services greater than the norm would indicate. These MUEs were implemented on January 1, 2007, and are applied to which code set? a. Diagnosis-related groups b. HCPCS/CPT codes c. ICD-9-CM diagnosis and procedure codes d. Resource utilization groups - ✔✔Correct Answer: B CMS developed MUEs to prevent providers from billing units in excess and receiving inappropriate payments. This new editing was the result of the outpatient prospective payment system which pays providers passed on the HCPCS/CPT code and units. Payment is directly related to units for specified HCPCS/CPT codes assigned to an ambulatory payment classification (CMS 2012b). 17. Identify the ICD-9-CM diagnostic code for other specified aplastic anemia secondary to chemotherapy. a. 284.9 b. 284.89 c. 285.9 d. 285.22 - ✔✔Correct Answer: B Index Anemia, aplastic, due to, antineoplastic chemotherapy. A coder should always assign the most specific type of anemia. Anemia due to chemotherapy is often aplastic (Schraffenberger 2012, 133-135 ).18. When the physician does not specify the method used to remove a lesion during an endoscopy, what is the appropriate procedure? a. Assign the removal by snare technique code. b. Assign the removal by hot biopsy forceps code. c. Assign the ablation code. d. Query the physician as to the method used. - ✔✔Correct Answer: D It is not appropriate for the coder to assume the removal was done by either snare or hot biopsy forceps. The ablation code is only assigned when a lesion is completely destroyed and no specimen is retrieved. The coding professional must query the physician to assign the appropriate code (AHIMA 2012a, 607). 19. What is the best reference tool to determine how CPT codes should be assigned? a. Local coverage determination from Medicare b. American Medical Association's CPT Assistant newsletter c. American Hospital Association's Coding Clinic d. CMS website - ✔✔Correct Answer: B CPT Assistant provides additional CPT coding guidance on how to assign a CPT code by providing intent on the use of the code and explanation of parenthetical instructions. The American Medical Association publishes the guidance monthly (AMA 2012b).20. Identify the appropriate ICD-9-CM diagnosis code(s) for right and left bundle branch block. a. 426.3, 426.4 b. 426.53 c. 426.4, 426.53 d. 426.52 - ✔✔Correct Answer: B Index Block, left, with right bundle branch block. Right and left bundle branch block is inclusive of one code. It is inappropriate to assign a code for right (426.4) and left (426.3) bundle branch block when a combination code includes both the right and left (Schraffenberger 2012, 201-207). 21. A software interface is a: a. Device to enter data b. Protocol for describing data c. Program to exchange data d. Standard vocabulary - ✔✔Correct Answer: C A software interface is a computer program that allows different applications to communicate and exchange data (Johns 2011, 137).22. What did the Centers of Medicare and Medicaid Services develop to promote national correct coding methodologies and to control improper coding leading to inappropriate payment in Part B claims? a. Outpatient Perspective Payment System (OPPS) b. National Correct Coding Initiative (NCCI) c. Ambulatory Payment Classifications (APCs) d. Comprehensive Outpatient Rehab Facilities (CORFs) - ✔✔Correct Answer: B CMS developed the NCCI to control improper coding practices leading to inappropriate payments in Part B claims (CMS 2012a). 23. Identify the appropriate diagnostic and/or procedure ICD-9-CM code(s) for reprogramming of a cardiac pacemaker. a. V53.31 b. 37.85 c. V53.02 d. V53.31, 37.85 - ✔✔Correct Answer: A Index Fitting (of) pacemaker (cardiac). No procedure code exists in ICD-9-CM to describe reprogramming (Schraffenberger 2012, 204-205).24. Which of the following hospitals are excluded from the Medicare acute-care prospective payment system? a. Children's b. Small community c. Tertiary d. Trauma - ✔✔Correct Answer: A Children's hospitals are excluded from PPS because the PPS diagnosis-related groups do not accurately account for the resource costs for the types of patients treated (Johns 2011, 321). 25. Which of the following programs has been in place in hospitals for years and has been required by the Medicare and Medicaid programs and accreditation standards? a. Internal DRG audits b. Peer review c. Managed care d. Quality improvement - ✔✔Correct Answer: D Quality improvement (QI) programs have been in place in hospitals for years and have been required by the Medicare/Medicaid programs and accreditation standards. QI programs have covered medical staff as well as nursing and other departments or processes (LaTour and Eichenwald Maki 2010, 33).26. Identify the code for a patient with a closed transcervical fracture of the epiphysis. a. 820.09 b. 820.02 c. 820.03 d. 820.01 - ✔✔Correct Answer: D Index Fracture, femur, epiphysis, capital. Fifth digits are required for further classification of a specific condition. Many publishers include special symbols and/or color highlighting to identify codes that require a fourth or fifth digit (Schraffenberger 2012, 7). 27. What is the best source of documentation to determine the size of a removed malignant lesion? a. Pathology report b. Post-acute care unit record c. Operative report d. Physical examination - ✔✔Correct Answer: C The total size of a removed lesion, including margins, is needed for accurate coding. This information is best provided in the operative report. The pathology report typically provides the specimen size ratherthan the size of the excised lesion. Because the specimen tends to shrink, this is not an accurate measurement (Kuehn 2012, 110-111). 28. Which of the following definitions best describes the concept of confidentiality? a. The right of individuals to control access to their personal health information b. The protection of healthcare information from damage, loss, and unauthorized alteration c. The expectation that personal information shared by an individual with a healthcare provider during the course of care will be used only for its intended purpose d. The expectation that only individuals with the appropriate authority will be allowed to access healthcare information - ✔✔Correct Answer: C Confidentiality refers to the expectation that the personal information shared by an individual with a healthcare provider during the course of care will be used only for its intended purpose (Johns 2011, 49). 29. Identify the ICD-9-CM diagnosis code for Paget's disease of the bone (no bone tumor noted). a. 170.9 b. 213.9 c. 238.0 d. 731.0 - ✔✔Correct Answer: DIndex Paget's disease, bone. The main terms for eponyms are located in the Alphabetic Index under the eponym or the disease, syndrome, or disorder (Schraffenberger 2012, 13). 30. Which of the following fails to meet the CMS classification of a hospital-acquired condition? a. Foreign object retained after surgery b. Air embolism c. Gram-negative pneumonia d. Blood incompatibility - ✔✔Correct Answer: C Gram-negative pneumonia (Johns 2011, 326). 31. Which of the following is (are) the correct ICD-9-CM procedure code(s) for cystoscopy with biopsy? a. 57.34 b. 57.32, 57.33 c. 57.33 d. 57.39 - ✔✔Correct Answer: C Index Cystoscopy (transurethral), with biopsy (Schraffenberger 2012, 251).32. Identify the ICD-9-CM diagnosis code for chondromalacia of the patella. a. 717.7 b. 733.92 c. 748.3 d. 716.86 - ✔✔Correct Answer: A Index Chondromalacia, patella (Schraffenberger 2012, 303-304). 33. Identify the ICD-9-CM diagnosis code for blighted ovum. a. 236.1 b. 661.00 c. 631.8 d. 634.90 - ✔✔Correct Answer: C Index Ovum, blighted (Schraffenberger 2012, 282-283). 34.Each year the OIG develops a work plan that details areas of compliance it will be investigating for that year. What is the expectation of the hospital in relation to the OIG work plan? a. Hospitals are required to follow the same work plan and deploy audits based on that work plan. b. Hospitals should plan their compliance and auditing projects around the OIG work plan to ensure they are in compliance with the target areas in the plan. c. Hospitals must not develop their audits based on the OIG work plan; rather, they must develop their own and look for high-risk areas that need improvement. d. Hospitals must use the plan developed by their state hospital association that is specific to state laws and compliance activities. - ✔✔Correct Answer: B Hospitals are encouraged but not required to follow the same work plan as the OIG. Hospitals should review the plan carefully and plan their compliance program around the target areas (Johns 2011, 275). 35. The _____ may contain information about diseases among relatives in which heredity may play a role. a. Physical examination b. History c. Laboratory report d. Administrative data - ✔✔Correct Answer: B A complete medical history documents the patient's current complaints and symptoms and lists the patient's past medical, social, and family history (Johns 2011, 63).36. There are several codes to describe a colonoscopy. CPT code 45378 describes the most basic colonoscopy without additional services. Additional codes in the colonoscopy section of CPT further define removal of foreign body (45379); biopsy, single or multiple (45380); and others. Reporting the basic form of a colonoscopy (45378) with a foreign body (45379) or biopsy code (45380) would violate which rule? a. Unbundling b. Optimizing c. Sequencing d. Maximizing - ✔✔Correct Answer: A The coder should assign the most comprehensive code to describe the entire procedure performed. When a code describes the entire service provided, the coder should not code each component separately. Assigning additional codes inherent to the main code would be a form of unbundling (Hazelwood and Venable 2012, 336). 37. Corporate compliance programs were released by the OIG for hospitals to develop and implement their own compliance programs. All of the following except _____ are basic elements of a corporate compliance program. a. Designation of a Chief Compliance Officer b. Implementation of regular and effective education and training programs for all employees c. Medical staff appointee for documentation compliance d. The use of audits or other evaluation techniques to monitor compliance - ✔✔Correct Answer: CSeven elements are required as part of the basic elements of a corporate compliance program and a medical staff appointee is not one of them (Johns 2011, 274). 38. The electronic claim format (837I) replaces which paper billing form? a. CMS-1500 b. CMS-1450 (UB-04) c. UB-92 d. CMS-1400 - ✔✔Correct Answer: B The electronic claim form (screen 837I) replaced the UB-04 (CMS 1450) paper billing form (Johns 2011, 343). 39. According to the Joint Commission Accreditation Standards, which document must be placed in the patient's record before a surgical procedure may be performed? a. Admission record b. Physician's order c. Report of history and physical examination d. Discharge summary - ✔✔Correct Answer: CAccording to the Joint Commission, except in emergency situations, every surgical patient's chart must include a report of a complete history and physical conducted no more than seven days before the surgery is to be performed (Odom-Wesley et al. 2009, 150). 40. The right of an individual to keep information about himself or herself from being disclosed to anyone is a definition of: a. Confidentiality b. Privacy c. Integrity d. Security - ✔✔Correct Answer: B Privacy is the right of an individual to be left alone. It includes freedom from observation or intrusion into one's private affairs and the right to maintain control over certain personal and health information (Johns 2011, 755). 41. Standardizing medical terminology to avoid differences in naming various medical conditions and procedures (such as the synonyms bunionectomy, McBride procedure, and repair of hallus valgus) is one purpose of: a. Transaction standards b. Content and structure standards c. Vocabulary standardsd. Security standards - ✔✔Correct Answer: C Vocabulary standards establish common definitions for medical terms to encourage consistent descriptions of an individual's condition in the health record (Johns 2011, 227). 42. An outpatient clinic is reviewing the functionality of a computer system it is considering purchasing. Which of the following datasets should the clinic consult to ensure all the federally required data elements for Medicare and Medicaid outpatient clinical encounters are collected by the system? a. DEEDS b. EMEDS c. UACDS d. UHDDS - ✔✔Correct Answer: C Uniform Ambulatory Care Data Set (Odom-Wesley et al. 2009, 310). 43. Identify the ICD-9-CM diagnostic code for diastolic dysfunction. a. 428.1 b. 428.30 c. 428.9 d. 429.9 - ✔✔Correct Answer: DIndex Dysfunction, diastolic (Schraffenberger 2012, 182-183). 44. Identify the appropriate ICD-9-CM procedure code(s) for a double internal mammary-coronary artery bypass. a. 36.15, 36.16 b. 36.15 c. 36.16 d. 36.12, 36.16 - ✔✔Correct Answer: C Index Bypass, internal mammary-coronary artery (single), double vessel (36.16). Internal mammarycoronary artery bypass is accomplished by loosening the internal mammary artery from its normal position and using the internal mammary artery to bring blood from the subclavian artery to the occluded coronary artery. Codes are selected based on whether one or both internal mammary arteries are used, regardless of the number of coronary arteries involved (Schraffenberger 2012, 203-204). 45. Identify the CPT code(s) for the following patient: A 2-year-old male presented to the emergency room in the middle of the night to have his nasogastric feeding tube repositioned through the duodenum under fluoroscopic guidance. a. 43752 b. 43761 c. 43761, 76000d. 49450 - ✔✔Correct Answer: C Code 43761 is assigned to report repositioning of a nasogastric or orogastric feeding tube through the duodenum. An instructional note guides the coder to report code 76000 when image guidance is performed (AMA 2012b, 235). Which of the following is the correct ICD-9-CM procedure code for a Mayo operation known as a bunionectomy? a. 77.54 b. 77.69 c. 77.59 d. 77.51 - ✔✔Correct Answer: C Index Bunionectomy or Mayo operation, bunionectomy. The main terms for eponyms are located in the Alphabetic Index under the eponym or the disease, syndrome, operation, or disorder (Schraffenberger 2012, 13). 47. Whereas the focus of inpatient data collection is on the principal diagnosis, the focus of outpatient data collection is on: a. Reason for admission b. Reason for encounter c. Discharge diagnosis d. Activities of daily living - ✔✔Correct Answer: BThe Uniform Ambulatory Care Data Set (UACDS) includes data elements specific to ambulatory care, such as the reason for the encounter with the healthcare provider (LaTour and Eichenwald Maki 2010, 166). 48. How do accreditation organizations such as the Joint Commission use the health record? a. To serve as a source for case study information b. To determine whether the documentation supports the provider's claim for reimbursement c. To provide healthcare services d. To determine whether standards of care are being met - ✔✔Correct Answer: D Surveyors review the documentation of patient care services to determine whether the standards for care are being met (Johns 2011, 40). 49. Mildred Smith was admitted from an acute-care hospital to a nursing facility with the following information: "Patient is being admitted for organic brain syndrome." Underneath the diagnosis, her medical information along with her rehabilitation potential were also listed. On which form is this information documented? a. Transfer or referral b. Release of information c. Patient rights acknowledgementd. Admitting physical evaluation - ✔✔Correct Answer: A The transfer or referral form provides document communication between caregivers in multiple healthcare settings. It is important that a patient's treatment plan be consistent as the patient moves through the healthcare delivery system (Odom-Wesley et al. 2009, 131). 50. Which of the following statements is true? a. The higher the relative weight, the higher the payment rates. b. The lower the relative weight, the higher the payment rates. c. The lower the relative weight, the sicker the patient. d. The higher the relative weight, the lesser reimbursement due the facility. - ✔✔Correct Answer: A Higher relative weights link to higher payment rates (Casto and Layman 2011, 13). 51. A coder needs to locate electronic health records for a patient across a health information exchange (HIE). What tool(s) should the coder use? a. Certification b. Identity-matching algorithm and record locator service c. Interoperability and certification d. Meaningful use - ✔✔Correct Answer: BAn HIE organization requires an identity-matching algorithm and record locator service (RLS). An identity-matching algorithm must be used by the HIE to identify any patient for whom data are to be exchanged. This algorithm uses sophisticated probability equations to identify patients. The RLS, then, is a process that seeks information about where a patient may have a health record available to the HIE organization (Johns 2011, 151). 52. All documentation entered in the medical record relating to the patient's diagnosis and treatment is considered this type of data: a. Clinical b. Identification c. Secondary d. Financial - ✔✔Correct Answer: A Clinical information is data related to the patient's diagnosis or treatment in a healthcare facility (Odom-Wesley et al. 2009, 55). 53. What type of data is exemplified by the insured party's member identification number? a. Demographic data b. Clinical data c. Certification datad. Financial data - ✔✔Correct Answer: D Financial data include details about the patient's occupation, employer, and insurance coverage (OdomWesley et al. 2009, 42). 54. What is the best reference tool for ICD-9-CM coding advice? a. AMA's CPT Assistant b. AHA's Coding Clinic for HCPCS c. AHA's Coding Clinic for ICD-9-CM d. National Correct Coding Initiative (NCCI) - ✔✔Correct Answer: C AHA's Coding Clinic for ICD-9-CM is a quarterly publication of the Central Office on ICD-9-CM, which allows coders to submit a request for coding advice through the coding publication. 55. Identify the ICD-9-CM diagnostic code(s) for the following: A 6-month-old child is scheduled for a clinic visit for a routine well child exam. The physician documents, "well child, expreemie." a. V20.1, 765.10 b. V20.2 c. V20.2, 765.10 d. V20.2, 765.19 - ✔✔Correct Answer: CIndex Exam, well baby. Premature, infant NEC. Refer to table in Tabular for fifth digit of "0" to note unspecified birth weight (Schraffenberger 2012, 324-328, ). 56. Identify the ICD-9-CM diagnostic code(s) and procedure code(s) for the following: term pregnancy with failure of cervical dilation; lower uterine segment cesarean delivery with single liveborn female. a. 661.01, V27.0, 74.1 b. 661.21, 74.1 c. 661.01, 74.0 d. 661.21, V27, 74.1 - ✔✔Correct Answer: A Index Delivery, cesarean, poor dilation, cervix (661.0). Refer to the ICD-9-CM Tabular (660-669) for the correct fifth digit of "1," delivered, with or without mention of antepartum condition. Outcome of delivery, single, liveborn. Cesarean section, low uterine segment (Schraffenberger 2012, 282-283). 57. A hospital receives a valid request from a patient for copies of her medical records. The HIM clerk who is preparing the records removes copies of the patient's records from another hospital where the patient was previously treated. According to HIPAA regulations, was this action correct? a. Yes; HIPAA only requires that current records be produced for the patient. b. Yes; this is hospital policy over which HIPAA has no control. c. No; the records from the previous hospital are considered part of the designated record set and should be given to the patient.d. No; the records from the previous hospital are not included in the designated record set but should be released anyway. - ✔✔Correct Answer: C The designated record set includes health records that are used to make decisions about the individual (Johns 2011, 822). 58. As recommended by AHIMA, HIM compliance policies and procedures should ensure all of the following except: a. Compensation for coders and consultants does not provide any financial incentive to code claims improperly b. The proper selection and sequencing of diagnoses codes c. Proper and timely documentation obtained prior to and after billing d. d The correct application of official coding rules and guidelines - ✔✔Correct Answer: C Proper and timely documentation of all physician and other professional services must be obtained prior to billing. Facilities should not provide any financial incentive that may tempt a coder to code claims improperly such as upcoding to higher DRGs, which result in higher pay (Johns 20011, 275). 59. What reimbursement system uses the Medicare fee schedule? a. APCs b. MS-DRGsc. RBRVS d. RUG-III - ✔✔Correct Answer: C The resource-based relative value scale (RBRVS) system was implemented by CMS in 1992 for physicians' services such as office visits covered under Medicare Part B. The system reimburses physicians according to a fee schedule based on predetermined values assigned to specific services (Johns 2011, 326). 60. The CIA of security includes confidentiality, data integrity, and data _____. a. Accessibility b. Authentication c. Accuracy d. Availability - ✔✔orrect Answer: D Security measures not only provide for confidentiality, but data integrity and data availability—the CIA of security (Johns 2011, 184). 61. Valley High, a skilled nursing facility, wants to become certified to take part in federal government reimbursement programs such as Medicare. What standards must the facility meet in order to become certified for these programs? a. Joint Commission Accreditation Standards b. Accreditation Association for Ambulatory Healthcare Standardsc. Conditions of Participation d. Outcomes and Assessment Information Set - ✔✔Correct Answer: C Participating organizations must follow the Medicare Conditions of Participation to receive federal funds from the Medicare program for services rendered (Johns 2011, 61). 62. What software will prompt the user through a variety of questions and choices based on the clinical terminology entered to assist the coder in selecting the most appropriate code? a. Logic-based encoder b. Automated code book c. Speech recognition d. Natural-language processing - ✔✔Correct Answer: A Encoders come in two distinct categories: logic-based and automated codebook formats. A logic-based encoder prompts the user through a variety of questions and choices based on the clinical terminology entered. The coder selects the most accurate code for a service or condition (and any possible complications or comorbidities). An automated codebook provides screen views that resemble the actual format of the coding system (LaTour and Eichenwald Maki 2010, 269). 63. Which of the following is not a function of the discharge summary? a. Providing information about the patient's insurance coverageb. Ensuring the continuity of future care c. Providing information to support the activities of the medical staff review committee d. Providing concise information that can be used to answer information requests - ✔✔Correct Answer: A The discharge summary provides an overview of the entire medical encounter to ensure the continuity of future care by providing information to the patient's attending physician, referring physician, and any consulting physicians, to provide information to support the activities of the medical staff review committee and to provide concise information that can be used to answer information requests from authorized individuals or entities (Johns 2011, 78). 64. MS diagnostic-related groups are organized into: a. Case-mix classifications b. Geographic practice cost indices c. Major diagnostic categories d. Resource-based relative values - ✔✔Correct Answer: C Major diagnostic categories (MDCs), of which there are 25. The principal diagnosis determines the MDC assignment (Johns 2011, 322). 65. Identify ICD-9-CM diagnosis code for atypical ductal hyperplasia. a. 610.1b. 610.4 c. 610.8 d. 610.9 - ✔✔Correct Answer: C Use this code when the diagnosis is specified as a certain type of "benign mammary dysplasia," and in this case, "ductal" hyperplasia. Index Hyperplasia, breast, ductal, atypical (Schraffenberger 2012, 253). 66. The Medical Record Committee is reviewing the privacy policies for a large outpatient clinic. One of the members of the committee remarks that he feels the clinic's practice of calling out a patient's full name in the waiting room is not in compliance with HIPAA regulations and that only the patient's first name should be used. Other committee members disagree with this assessment. What should the HIM director advise the committee? a. HIPAA does not allow a patient's name to be announced in a waiting room. b. There is no HIPAA violation for announcing a patient's name, but the committee may want to consider implementing practices that might reduce this practice. c. HIPAA allows only the use of the patient's first name. d. HIPAA requires that patients be given numbers and only the number be announced. - ✔✔Correct Answer: B It is suggested that covered entities use PHI with certain specified direct identifiers removed as a guideline for disclosing only minimum necessary information while providing the amount needed to accomplish the intended purpose (Johns 2011, 822). 67.CMS identified conditions that are not present on admission and could be "reasonably preventable," and therefore hospitals are not allowed to receive additional payment for these conditions that do present. What are these conditions called? a. a Conditions of Participation b. Present on admission c. Hospital-acquired conditions d. Hospital-acquired infection - ✔✔Correct Answer: C CMS identified hospital-acquired conditions (not present on admission) as "reasonably preventable," and hospitals do not receive additional payment for cases in which these cases are present (Johns 2011, 326). 68. Which of the following is (are) the correct ICD-9-CM code(s) for laparoscopic cholecystectomy? a. 51.21 b. 51.22, 54.21 c. 51.23, 54.21 d. 51.23 - ✔✔Correct Answer: D Index Cholecystectomy (total), laparoscopic (Schraffenberger 2012, 237-238). 69.The HIM manager is concerned about whether the data transmitted across the hospital network is altered during the transmission. The concept that concerns the HIM manager is: a. Admissibility b. Disclosures c. Availability d. Data integrity - ✔✔Correct Answer: D Data integrity services ensure the data are not altered as they are stored or transmitted electronically (Johns 2011, 184). 70. Medical record completion compliance is a problem at Community Hospital. The number of incomplete charts often exceeds the standard set by the Joint Commission, risking a type I violation. Previous HIM committee chairpersons tried multiple methods to improve compliance, including suspension of privileges and deactivating the parking garage keycard of any physician in poor standing. To improve compliance, which of the following would be the next step to overcoming noncompliance? a. Discuss the problem with the hospital CEO. b. Call the Joint Commission. c. Contact other hospitals to see what methods they use to ensure compliance. d. Drop the issue because noncompliance is always a problem. - ✔✔Correct Answer: C The HIM manager may compare organizational data with external data from peer groups to determine best practices (Johns 2011, 609).71. Identify CPT code(s) for the following Medicare patient. A 67-year-old female undergoes a fine needle aspiration of the left breast with ultrasound guidance to place a localization clip during a breast biopsy. a. 10022 b. 10022, 19295-LT c. 10022, 19295-LT, 76942 d. 10022, 76942 - ✔✔Correct Answer: C Fine needle aspiration with image guidance is coded with 10022. Instructional note directs coder to assign 19295 for placement of localization clip during a breast biopsy. Add radiology code 76942 for supervision and interpretation of ultrasound guidance for localization clip guidance. See instructional notes following code 10022 (AMA 2012b, 59). 72. Identify the ICD-9-CM code for diaper rash, elderly patient. a. 690.10 b. 691.0 c. 782.1 d. 705.1 - ✔✔Correct Answer: BIndex Rash, diaper. ICD-9-CM classifies dermatitis to categories 690-694. Atopic dermatitis and related conditions are specific to category 691. Fourth-digit subcategories include diaper or napkin rash and other atopic dermatitis and related conditions (Schraffenberger 2012, 292). 73. Identify the ICD-9-CM diagnostic code(s) for the following: threatened abortion with hemorrhage at 15 weeks; home undelivered. a. 640.01, 640.91 b. 640.03 c. 640.83 d. 640.80 - ✔✔Correct Answer: B Index Abortion, threatened 640.0. Refer to the ICD-9-CM Tabular List (640-649) for the correct fifth digit of 3, antepartum condition, not delivered (Schraffenberger 2012, 274-275). 74. To comply with Joint Commission standards, the HIM director wants to ensure that history and physical examinations are documented in the patient's health record no later than 24 hours after admission. Which of the following would be the best way to ensure the completeness of health records? a. Retrospectively review each patient's medical record to make sure history and physicals are present. b. Review each patient's medical record concurrently to make sure history and physicals are present and meet the accreditation standards. c. Establish a process to review medical records immediately on discharge.d. Do a review of records for all patients discharged in the previous 60 days. - ✔✔Correct Answer: B The benefit of concurrent review is that content or authentication issues can be identified at the time of patient care and rectified in a timely manner (Johns 2011, 410). 75. A patient requests copies of her personal health information on CD. When the patient goes home, she finds that she cannot read the CD on her computer. The patient then requests the hospital provide the medical records in paper format. How should the hospital respond? a. Provide the medical records in paper format b. Burn another CD because this is hospital policy c. Provide the patient with both paper and CD copies of the medical record d. Review the CD copies with the patient on a hospital computer - ✔✔Correct Answer: A The covered entity must provide access to the personal health information in the form or format requested when it is readily producible in such form for format. When it is not readily producible in the form or format requested, it must be produced in a readable hard-copy form or such other form or format agreed upon by the covered entity and the individual (Johns 2011, 831). 76. Which payment system was introduced in 1992 and replaced Medicare's customary, prevailing, and reasonable (CPR) payment system? a. Diagnosis-related groups b. Resource-based relative value scale systemc. Long-term care drugs d. Resource utilization groups - ✔✔Correct Answer: B The RBRVS system is the federal government's payment system for physicians. It is a system of classifying health services based on the cost of furnishing physicians' services in different settings, the skill and training levels required to perform the services, and the time and risk involved (Casto and Layman 2011, 151). 77. Identify the CPT code(s) for the following patient: A 2-year-old male presented to the hospital to have his gastrostomy tube changed under fluoroscopic guidance. a. 43752 b. 43760 c. 43761, 76000 d. 49450 - ✔✔Correct Answer: D Code 49450 includes replacement of gastrostomy or cecostomy tube, percutaneous, under fluoroscopic guidance including contrast injections(s), image documentation, and report. Therefore, it would not be appropriate to add code 76000 for fluoroscopic guidance, which is already included in the procedure code (AMA 2012b, 258). 78. A family practitioner requests the opinion of a physician specialist in endocrinology who reviews the patient's health record and examines the patient. The physician specialist records findings, impressions, and recommendations in which type of report? a. Consultationb. Medical history c. Physical examination d. Progress notes - ✔✔Correct Answer: A The consultation report documents the clinical opinion of a physician other than the primary or attending physician. The report is based on the consulting physician's examination of the patient and a review of his or her health record (Johns 2011, 78). 79. Which of the following is (are) the correct ICD-9-CM code(s) for thoracoscopic lobectomy of left lung? a. 32.30 b. 32.41 c. 32.49 d. 34.02, 32.41 - ✔✔Correct Answer: B Index Lobectomy, lung, segmental (with resection of adjacent lobes), thoracoscopic. Segmental includes the complete excision of a lobe of the lung (Schraffenberger 2012, 227-228). 80. An individual designated as an inpatient coder may have access to an electronic medical record to code the record. Under what access security mechanism is the coder allowed access to the system? a. Role-basedb. User-based c. Context-based d. Situation-based - ✔✔Correct Answer: A Role-based access control (RBAC) is a control system in which access decisions are based on the roles of individual users as part of an organization (Brodnik et al. 2009, 211). 81. Which part of the problem-oriented medical record is used by many facilities that have not adopted the whole problem-oriented format? a. Problem list as an index b. Initial plan c. SOAP form of progress notes d. Database - ✔✔Correct Answer: C The Subjective, Objective, Assessment, Plan (SOAP) notes are part of the problem-oriented medical records (POMR) approach most commonly used by physicians and other healthcare professionals. SOAP notes are intended to improve the quality and continuity of client services by enhancing communication among healthcare professionals (Odom-Wesley et al. 2009, 217). 82. Which of the following software applications would be used to aid in the coding function in a physician ' s office?a. Grouper b. Encoder c. Pricer d. Diagnosis calculator - ✔✔Correct Answer: B An encoder is a computer software program designed to assist coders in assigning appropriate clinical codes and helps ensure accurate reporting of diagnoses and procedures (LaTour and Eichenwald Maki 2010, 318-319). 83. Which of the following fails to meet the CMS classification of a hospital-acquired condition? a. Stage I pressure ulcers b. Falls and trauma c. Catheter-associated infection d. Vascular catheter-associated infection - ✔✔Correct Answer: A Stage I and II pressure ulcers are not considered hospital-acquired conditions but stage III and IV are (Johns 2011, 326). 84. HIM coding professionals and the organizations that employ them have the responsibility to not tolerate behavior that adversely affects data quality. Which of the following is an example of behavior that should not be tolerated?a. Assign codes to an incomplete record with organizational policies in place to ensure codes are reviewed after the records are complete. b. Follow-up on and monitor identified problems. c. Evaluate and trend diagnoses and procedure code selections. d. Report data quality review results to organizational leadership, compliance staff, and the medical staff. - ✔✔Correct Answer: A The coder is not following established policies (Johns 2011, 265-267). 85. Which classification system is in place to reimburse home health agencies? a. MS-DRGs b. RUGs c. HHRGs d. APCs - ✔✔Correct Answer: C Home health resource groups (HHRGs) represent the classification system established for the prospective reimbursement of covered home care services to Medicare beneficiaries during a 60-day episode of care (Johns 2011, 334). 86.Identify CPT code(s) for the following patient. A 35-year-old female undergoes an excision of a 3.0-cm tumor of her forehead. An incision is made through the skin and subcutaneous tissue. The tumor is dissected free of surrounding structures. The wound is closed in layers with interrupted sutures. a. 21012 b. 21012, 12052 c. 21014 d. 21014, 12052 - ✔✔Correct Answer: A CPT code 21012 describes excision of a subcutaneous soft tissue tumor of the face or scalp greater than 2 cm and is appropriately coded when the tumor is removed from the subcutaneous tissue rather than subgaleal or intramuscular. Simple and intermediate closure of the wound is included in the procedure for the excision in the musculoskeletal section of CPT (AMA 2010a, 28-29; AMA 2012b, 88, 94-95). 87. Identify the correct diagnosis ICD-9-CM code(s) for a patient who arrives at the hospital for outpatient laboratory services ordered by the physician to monitor the patient's Coumadin levels. A prothrombin time (PT) is performed to check the patient's long-term use of his anticoagulant treatment. a. V58.83, V58.61 b. V58.83, V58.63 c. V58.61, 790.92 d. V58.61 - ✔✔Correct Answer: AV58.83, Encounter for therapeutic drug monitoring, is the correct code to use when a patient visit is for the sole purpose of undergoing a laboratory test to measure the drug level in the patient's blood or urine or to measure a specific function to assess the effectiveness of the drug. V58.83 may be used alone if the monitoring is for a drug that the patient is on for only a brief period, not long term. However, there is a Use Additional Code note after code V58.83 to remind the coder to use the additional code for any associated long-term drug use with codes V58.61-V58.69 (Schraffenberger 2012, 450-451). 88. Identify the ICD-9-CM procedure code(s) for insertion of dual chamber cardiac pacemaker and atrial and ventricular leads. a. 37,83, 37.73 b. 37.83, 37.71 c. 37.81, 37.73, 37.71 d. 37.83, 37.72 - ✔✔Correct Answer: D ICD-9-CM classifies cardiac pacemakers to code 37.8: Insertion, replacement, removal, and revision of pacemaker device. In coding initial insertion of a permanent pacemaker, two codes are required—one for the pacemaker (37.80-37.83) and one for the lead (37.70-37.74) (Schraffenberger 2012, 204-205). 89. Several key principles require appropriate physician documentation to secure payment from the insurer. Which answer (listed here) fails to impact payment based on physician responsibility? a. The health record should be complete and legible. b. The rationale for ordering diagnostic and other ancillary services should be documented or easily inferred.c. Documenting the charges and services on the itemized bill. d. The patient's progress and response to treatment and any revision in the treatment plan and diagnoses should be documented. - ✔✔Correct Answer: C The documentation of the charges and itemized bill is not the responsibility of the physician (Smith 2012, 7-8). 90. The technology commonly used for automated claims processing (sending bills directly to third-party payers) is: a. Optical character recognition b. Bar coding c. Neural networks d. Electronic data interchange - ✔✔Correct Answer: D EDI allows the transfer (incoming and outgoing) of information directly from one computer to another by using flexible, standard formats (Johns 2011, 348). 91. Two patients were hospitalized with bacterial pneumonia. One patient was hospitalized for three days and the other patient was hospitalized for 30 days. Both cases result in the same DRG with different lengths of stay. Which answer most closely describes how the hospital will be reimbursed? a. The hospital will receive the same DRG for both patients but additional reimbursement will be allowed for the patient who stayed 30 days because the length of stay was greater than the geometric length of stay for this DRG.b. The hospital will receive the same reimbursement for the same DRG regardless of the length of stay. c. The hospital can appeal the payment for the patient who was in the hospital for 30 days because the cost of care was significantly higher than the average length of stay for the DRG payment. d. The hospital will receive a day outlier for the patient who was hospitalized for 30 days. - ✔✔Correct Answer: B The hospital will receive the same reimbursement regardless of the length of stay (Casto and Layman 2011, 12). 92. This is a statement sent by third-party payers to the patient to explain services provided, amounts billed, and payments made by the health plan. a. Coordination of benefits (COB) b. Explanation of benefits (EOB) c. Medicare summary notice (MSN) d. Remittance advice (RA) - ✔✔Correct Answer: B An EOB is a statement sent by a third-party payer to the patient to explain the services provided (Johns 2011, 343). 93. Identify the ICD-9-CM code(s) for infected ingrown nail.a. 703.0 b. 703.8, 681.11 c. 681.11 d. 681.9 - ✔✔Correct Answer: A Index Ingrowing, nail (finger) (toe) (infected) (Schraffenberger 2012, 295). 94. The patient had a total abdominal hysterectomy with bilateral salpingo-oophorectomy. The coder assigned the following codes: 58150, Total abdominal hysterectomy, with/without removal of tubes and ovaries 58700, Salpingectomy, complete or partial, unilateral/bilateral (separate procedure) What error has the coder made by using these codes? a. Maximizing b. Upcoding c. Unbundling d. Optimizing - ✔✔Correct Answer: CUnbundling is the practice of coding services separately that should be coded together as a package because all parts are included within one code and, therefore, one price. Unbundling, done deliberately, could be considered fraud (Kuehn 2012, 347). 95. Bob Smith was admitted to Mercy Hospital on June 21. The physical was completed on June 23. According to Joint Commission standards, which statement applies to this situation? a. The record is not in compliance because the physical examination must be completed within 24 hours of admission. b. The record is not in compliance because the physical examination must be completed within 48 hours of admission. c. The record is in compliance because the physical examination must be completed within 48 hours. d. The record is in compliance because the physical examination was completed within 72 hours of admission. - ✔✔Correct Answer: A According to the Joint Commission, the physical examination must be completed within 24 hours of admission (Odom-Wesley et al. 2009, 353). 96. The Medicare Modernization Act of 2003 (MMA) launched a Medicare payment and recovery demonstration project that would later develop into recovery audit contractors (RACs) serving as a means to ensure correct payments under Medicare. During the demonstration program, the contractors were able to identify _____ of dollars in improper payments. a. Hundreds b. Thousandsc. Millions d. Billions - ✔✔Correct Answer: D The RAC demonstration uncovered $1.03 billion of improper payments, of which 96% were overpayments and 4% were underpayments (Casto and Layman 2011, 39). 97. The documentation of each patient encounter should include the following to secure payment from the insurer except: a. The reason for the encounter and the patient's relevant history, physical exam, and prior diagnostic test results b. A patient assessment, clinical impression, or diagnosis c. A plan of care d. The identity of the patient's nearest relative and emergency contact number - ✔✔Correct Answer: D The identity of the patient's nearest relative and an emergency contact number are not relative to securing payment from the insurer. The encounter should include the date of the encounter and the identity of the observer (Smith 2012, 8). 98. Identify the ICD-9-CM diagnosis code(s) for neonatal tooth eruption. a. 525.0 b. 520.6, 525.0c. 520.9 d. 520.6 - ✔✔Correct Answer: D Index Eruption, teeth/tooth, neonatal. Some main terms are followed by a list of indented subterms (modifiers) that affect the selection of an appropriate code for a given diagnosis. The subterms form individual line entries arranged in alphabetical order and printed in a regular type beginning with a lowercase letter. Subterms are indented on standard indention to the right under the main term. More specific subterms are further indented after the preceding subterm (Schraffenberger 2012, 12). 99. Identify the correct ICD-9-CM procedure code(s) for replacement of an old dual pacemaker with a new dual pacemaker. a. 37.87 b. 37.85 c. 37.87, 37.89 d. 37.85, 37.89 - ✔✔Correct Answer: A When a pacemaker is replaced with another pacemaker, only the replaced pacemaker is coded (37.85- 37.87). Removal of the old pacemaker is not coded (Schraffenberger 2012, 204-205). 100. The release of information function requires the HIM professional to have knowledge of: a. Clinical coding principlesb. Database development c. Federal and state confidentiality laws d. Human resource management - ✔✔Correct Answer: C Because federal regulations such as HIPAA and state laws govern the release of health record information, HIM department personnel must know what information needs to be included on the authorization for it to be considered valid (Johns 2011, 443). 1. Data security policies and procedures should be reviewed at least: a. Semi-annually b. Annually c. Every two years d. Quarterly - ✔✔Correct Answer: B All data security policies and procedures should be reviewed and evaluated at least every year to make sure they are up-to-date and still relevant to the organization (Johns 2011, 995). 2. Identify the correct ICD-9-CM diagnosis code(s) for a patient with near-syncope event and nausea. a. 780.2 b. 780.2, 787.02c. 780.2, 787.01 d. 780.4, 787.02 - ✔✔Correct Answer: B Near-syncope and nausea are both signs and symptoms and therefore not integral to the other. Both conditions should be coded (Hazelwood and Venable 2012, 71). 3. The codes in the musculoskeletal section of CPT may be used by: a. Orthopedic surgeons only b. Orthopedic surgeons and emergency department physicians c. Any physician d. Orthopedic surgeons and neurosurgeons - ✔✔Correct Answer: C Any physician may use the codes in any section of CPT (AHIMA 2012a, 587). 4. In an EHR, what is the risk of copying and pasting? a. Reduction in the time required to document b. The system not recording who entered the data c. Quicker overall system response timed. System thinking that the original documenter recorded the note - ✔✔Correct Answer: B The system not recording who entered the data (Johns 2011, 433). 5. Mr. Smith is seen in his primary care physician's office for his annual physical examination. He has a digital rectal examination and is given three small cards to take home and return with fecal samples to screen for colorectal cancer. Assign the appropriate CPT code to report this occult blood sampling. a. 82270 b. 82271 c. 82272 d. 82274 - ✔✔Correct Answer: A CPT code 82270 describes a test for occult blood using feces source for the purpose of neoplasm screening with the use of three cards or single triple card for consecutive collection (AMA 2012b, 417). 6. Identify the punctuation mark that is used to supplement words or explanatory information that may or may not be present in the statement of a diagnosis or procedure in ICD-9-CM coding. The punctuation does not affect the code number assigned to the case. The punctuation is considered a nonessential modifier, and all three volumes of ICD-9-CM use them. a. Parentheses ( ) b. Square brackets [ ]c. Slanted brackets [ ] d. Braces { } - ✔✔Correct Answer: A Parentheses enclose supplementary words or explanatory information that may or may not be present in the statement of a diagnosis or procedure. They do not affect the code number assigned in the case. Terms in parentheses are considered nonessential modifiers, and all three volumes of ICD-9-CM use them. Bronchiectasis (fusiform) (postinfectious) (recurrent) is an example of a diagnosis statement with nonessential modifiers noted with parentheses (Schraffenberger 2012, 26-28). 7. Documentation regarding a patient's marital status; dietary, sleep, and exercise patterns; and use of coffee, tobacco, alcohol, and other drugs may be found in the: a. Physical examination record b. History record c. Operative report d. Radiological report - ✔✔Correct Answer: B A complete medical history documents the patient's current complaints and symptoms and lists his or her past medical, personal, and family history (Johns 2011, 63). 8. If an orthopedic surgeon attempted to reduce a fracture but was unsuccessful in obtaining acceptable alignment, what type of code should be assigned for the procedure? a. A "with manipulation" codeb. A "without manipulation" code c. An unlisted procedure code d. An E/M code only - ✔✔Correct Answer: A The "with manipulation" code is used because the fracture was manipulated, even if the manipulation did not result in clinical anatomic alignment. See Musculoskeletal Guidelines, Definitions (AHIMA 2012a, 597). 9. What is the maximum number of diagnosis codes that can appear on the UB-04 paper claim form locator 67 for a hospital inpatient principal and secondary diagnoses? a. 35 b. 25 c. 18 d. 9 - ✔✔Correct Answer: B As of January 1, 2011, CMS allows a total of 25 ICD-9-CM diagnosis codes (one principal and 24 additional diagnoses) for 837 Institutional claims filing (Schraffenberger 2012, 66). 10. What type of standard establishes methods for creating unique designations for individual patients, healthcare professionals, healthcare provider organizations, and healthcare vendors and suppliers? a. Vocabulary standardb. Identifier standard c. Structure and content standard d. Security standard - ✔✔Correct Answer: B Identifier standards establish methods for assigning a unique identifier to individual patients, healthcare professionals, healthcare provider organizations, and healthcare vendors and suppliers (Odom-Wesley et al. 2009, 311). 11. Identify the correct ICD-9-CM diagnosis code for a patient with anterolateral wall myocardial infarction, initial episode. a. 410.11 b. 410.01 c. 410.02 d. 410.12 - ✔✔Correct Answer: B Index Infarction, myocardium, anterolateral (wall) with fifth digit for initial episode (Schraffenberger 2012, 26-28). 12. A patient has two health insurance policies: Medicare and a Medicare supplement. Which of the following statements is true?a. The patient receives any monies paid by the insurance companies over and above the charges. b. Monies paid to the healthcare provider cannot exceed charges. c. The decision on which company is primary is based on remittance advice. d. The patient should not have a Medicare supplement. - ✔✔Correct Answer: B The monies collected from third-party payers cannot be greater than the amount of the provider's charges (Johns 2011, 343). 13. Identify the ICD-9-CM diagnosis code(s) for uncontrolled type II diabetes mellitus; mild malnutrition. a. 250.02 b. 250.01, 263.1 c. 250.02, 263.1 d. 250.01, 263.0 - ✔✔Correct Answer: C Diabetes (without complication) with fifth digit of 2 = type II, uncontrolled. 263.1 Malnutrition, mild, not stated as related to diabetes (Schraffenberger 2012, 122-124). 14. Identify the correct sequence and ICD-9-CM diagnosis code(s) for a patient with a scar on the right hand secondary to a laceration sustained two years ago. a. 709.2b. 906.1 c. 709.2, 906.1 d. 906.1, 709.2 - ✔✔Correct Answer: C The residual condition or nature of the late effect is sequenced first, followed by the cause of the late effect (Hazelwood and Venable 2012, 60-61). 15. Which of the following is the concept responsible for limiting disclosure of private matters including the responsibility to use, disclose, or release such information only with the knowledge and consent of the individual? a. Privacy b. Bioethics c. Security d. Confidentiality - ✔✔Correct Answer: D Confidentiality is the responsibility for limiting disclosure (Johns 2011, 755). 16. Tissue transplanted from one individual to another of the same species but different genotype is called a(n): a. Autograftb. Xenograft c. Allograft or allogeneic graft d. Heterograft - ✔✔Correct Answer: C Tissue transplanted from one individual to another of the same species but different genotype is called an allograft or allogeneic graft (AHIMA 2012a, 592-593). 17. Where would a coder who needed to locate the histology of a tissue sample most likely find this information? a. Pathology report b. Progress notes c. Nurse's notes d. Operative report - ✔✔Correct Answer: A Histology refers to the tissue type of a lesion. The histology of tissue is determined by a pathologist and documented in the pathology report (Johns 2011, 77). 18. A patient with known COPD and hypertension under treatment was admitted to the hospital with symptoms of a lower abdominal pain. He undergoes a laparoscopic appendectomy and develops a fever. The patient was subsequently discharged from the hospital with a principal diagnosis of acute appendicitis and secondary diagnoses of postoperative infection, COPD, and hypertension. Which of the following diagnoses should not be tagged as POA?a. Postoperative infection b. Appendicitis c. COPD d. Hypertension - ✔✔**Correct Answer: A Present on admission is defined as present at the time the order for inpatient admission occurs (CMS 2011c, 97). 19. A hospital needs to know how much Medicare paid on a claim so they can bill the secondary insurance. What should the hospital refer to? a. Explanation of benefits b. Medicare Summary Notice c. Remittance advice d. Coordination of benefits - ✔✔Correct Answer: C Remittance advice (RA) is sent to the provider to explain payments made by third-party payers (Johns 2011, 346). 20. Which of the following would be the best technique to ensure that registration clerks consistently use the correct notation for assigning admission date in an electronic health record (EHR)?a. Make admission date a required field b. Provide an input mask for entering data in the field c. Make admission date a numeric field d. Provide sufficient space for input of data - ✔✔Correct Answer: B When several people enter data in an EHR, you can define how users must enter data in specific fields to help maintain consistency. For example, an input mask for a form means that users can only enter the date in a specified format (MacDonald 2007, chapter 4). 21. Which of the following threatens the "need-to-know" principle? a. Backdating progress notes b. Blanket authorization c. HIPAA regulations d. Surgical consent - ✔✔Correct Answer: B A blanket authorization is a common ethical problem when misused. Patients often sign a blanket authorization, which authorizes the release of information from that point forward, without understanding the implications. The problem is the patient is not aware of what information is being accessed (Johns 2011, 778-779). 22.A fee schedule is: a. Developed by third-party payers and includes a list of healthcare services, procedures, and charges associated with each b. Developed by providers and includes a list of healthcare services provided to a patient c. Developed by third-party payers and includes a list of healthcare services provided to a patient d. Developed by providers and lists charge codes - ✔✔Correct Answer: A A fee schedule is a list of healthcare services and procedures and charges associated with each (Johns 2011, 350). 23. Identify the correct ICD-9-CM diagnosis code for a male patient with stress urinary incontinence. a. 625.6 b. 788.30 c. 788.32 d. 788.39 - ✔✔Correct Answer: C Index Incontinence, stress, male, NEC 788.32. Category 788.3x indicates incontinence of urine with the fifth digit specific to different types such as urge, stress, mixed, and others (Hazelwood and Venable 2012, 73). 24.Identify the correct ICD-9-CM diagnosis codes and sequence for a patient who was admitted to the outpatient chemotherapy floor for acute lymphocytic leukemia. During the procedure, the patient developed severe nausea with vomiting and was treated with medications. a. 204.00, 787.01, V58.11 b. V58.11, 204.00, 787.01 c. V58.11, 204.00 d. 204.22, 787.01 - ✔✔Correct Answer: B When a patient is admitted for the purpose of radiotherapy, chemotherapy, or immunotherapy and develops a complication, such as uncontrolled nausea and vomiting or dehydration, the principal diagnosis is the admission for radiotherapy (V58.0), the admission for the antineoplastic chemotherapy (V58.11), or the admission for the antineoplastic immunotherapy (V58.12). Additional codes would include the cancer and the complication(s) (Hazelwood and Venable 2012, 103). 25. Category II codes cover all but one of the following topics. Which is not addressed by Category II codes? a. Patient management b. New technology c. Therapeutic, preventative, or other interventions d. Patient safety - ✔✔Correct Answer: B New technology is addressed by the Category III codes (AHIMA 2012a, 584).26. The hospital is revising its policy on medical record documentation. Currently, all entries in the medical record must be legible, complete, dated, and signed. The committee chairperson wants to add that, in addition, all entries must have the time noted. However, another clinician suggests that adding the time of notation is difficult and rarely may be correct since personal watches and hospital clocks may not be coordinated. Another committee member agrees and says only electronic documentation needs a time stamp. Given this discussion, which of the following might the HIM director suggest? a. Suggest that only hospital clock time be noted in clinical documentation b. Suggest that only electronic documentation have time noted c. Inform the committee that according to the Medicare Conditions of Participation, all documentation must be authenticated and dated d. Inform the committee that according to the Medicare Conditions of Participation, only medication orders must include date and time - ✔✔Correct Answer: C All entries must be legible and complete, and must be authenticated and dated promptly by the person (identified by name and discipline) who is responsible for ordering, providing, or evaluating the service furnished (42 CFR 482.24). 27. How are amendments handled in an EHR? a. Automatically appended to the original note; no additional signature is required. b. Amendments must be entered by the same person as the original note. c. Amendments cannot be entered after 24 hours of the event's occurrence. d. The amendment must have a separate signature, date, and time. - ✔✔Correct Answer: DThe addendum must have a separate signature, date, and time from the original entry (Johns 2011, 437). 28. What penalties can be enforced against a person or entity that willfully and knowingly violates the HIPAA Privacy Rule with the intent to sell, transfer, or use PHI for commercial advantage, personal gain, or malicious harm? a. A fine of not more than $10,000 only b. A fine of not more than $10,000, not more than 1 year in jail, or both c. A fine of not more than $5,000 only d. A fine of not more than $250,000, not more than 10 years in jail, or both - ✔✔Correct Answer: D When a person or entity willfully and knowingly violates the HIPAA Privacy Rule, a fine of not more than $250,000, not more than 10 years in jail, or both may be imposed (LaTour and Eichenwald Maki 2010, 292). 29. Which of the following reports includes names of the surgeon and assistants, date, duration and description of the procedure, and any specimens removed? a. Operative report b. Anesthesia report c. Pathology reportd. Laboratory report - ✔✔Correct Answer: A An operative report describes the surgical procedures performed on the patient (Johns 2011, 73). 30. A provision of the law that established the resource-based relative value scale (RBRVS) stipulates that refinements to relative value units (RVUs) must maintain: a. Moderate rate increases b. Market basket increases c. Budget neutrality d. Sustainable growth rate - ✔✔Correct Answer: C Budget neutrality must be maintained annually when the RVUs are adjusted (Casto and Layman 2011, 156). 31. CPT was developed and is maintained by: a. CMS b. AMA c. Cooperating parties d. WHO - ✔✔Correct Answer: BThe AMA developed and maintains CPT. CMS developed and maintains HCPCS Level II codes (AHIMA 2012a, 586). 32. Identify the correct ICD-9-CM diagnosis code for a patient with an elevated prostate specific antigen (PSA) test result. a. 796.4 b. 790.6 c. 792.9 d. 790.93 - ✔✔Correct Answer: D Review Tabular List: Findings, abnormal, without diagnosis, prostate specific antigen (PSA), 790.93, or Elevation, prostate specific antigen (PSA), 790.93 (Hazelwood and Venable 2012, 69). 33. Identify the correct ICD-9-CM diagnosis code(s) and proper sequencing for urinary tract infection due to E. coli. a. 599.0 b. 599.0, 041.49 c. 041.49 d. 041.49, 599.0 - ✔✔Correct Answer: BConnecting words or connecting terms are subterms that indicate a relationship between the main term and an associated condition or etiology in the Alphabetic Index. The connecting term "due to" connects the organism E. coli to the urinary tract infection. The instructional note "Use additional code" is found in the Tabular List of ICD-9-CM. This notation indicates that use of an additional code may provide a more complete picture of the diagnosis or procedure. The additional code should always be assigned if the health record provides supportive documentation. Infection, urinary (tract) Tabular List— use additional code to identify organism. Infection, Escherichia coli (Schraffenberger 2012, 22-23, 79). 34. What is it called when a Medicare hospital inpatient admission results in exceptionally high costs when compared to other cases in the same DRG? a. Rate increase b. Charge outlier c. Cost outlier d. Day outlier - ✔✔Correct Answer: C To qualify for a cost outlier, a hospital's charges for a case (adjusted to cost) must exceed the payment rate for the MS-DRG by a specific threshold amount determined by CMS for each fiscal year (Johns 2011, 374). 35. Health insurance for spouses, children, or both is known as: a. Dependent (family) coverage b. Individual (single) coveragec. Group coverage d. Inclusive coverage - ✔✔Correct Answer: A Health insurance for spouses, children, or both is known as dependent (family) coverage (Casto and Layman 2011, 5). 36. In a routine health record quantitative analysis review, it was found that a physician dictated a discharge summary on 1/26/20XX. The patient, however, was discharged two days later. In this case, what would be the best course of action? a. Request that the physician dictate another discharge summary. b. Have the record analyst note the date discrepancy. c. Request the physician dictate an addendum to the discharge summary. d. File the record as complete because the discharge summary includes all of the pertinent patient information. - ✔✔Correct Answer: C An addendum may be included in the medical record to update or supplement documentation that has been recorded (AHIMA 2008b, 83-88). 37. Observation E/M codes (99218-99220) are used in physician billing when: a. A patient is admitted and discharged on the same date. b. A patient is admitted for routine nursing care following surgery.c. A patient does not meet admission criteria. d. A patient is referred to a designated observation status. - ✔✔Correct Answer: D See instructional notes preceding code 99217. In order to report these codes, the admission order must designate observation status. Whether the patient meets admission criteria or is admitted following surgery does not affect the observation code selection. If the patient is admitted and discharged on the same date, codes 99234-99236 are appropriate (AMA 2012b, 13). 38. When coding a selective catheterization in CPT, how are codes assigned? a. One code for each vessel entered b. One code for the point of entry vessel c. One code for the final vessel entered d. One code for the vessel of entry and one for the final vessel, with intervening vessels not coded - ✔✔Correct Answer: C The only vessel coded is the final vessel entered. See instructional note preceding code 36000. Intermediate steps along the way are not reported (AHIMA 2012a, 604). 39. The Privacy Rule establishes that a patient has the right of access to inspect and obtain a copy of his or her PHI: a. For as long as it is maintainedb. For six years c. Forever d. For 12 months - ✔✔Correct Answer: A An individual's right extends for as long as the record is maintained (Johns 2011, 827). 40. Assignment of benefits is a contract between a physician and Medicare in which the physician agrees to bill Medicare directly for covered services and to bill the beneficiary only for ________ , and to accept the Medicare payment as payment in full. a. Coinsurance or deductible b. Deductible only c. Coinsurance only d. Balance of charges - ✔✔Correct Answer: A When a physician accepts assignment of benefits, the physician can only collect any applicable deductible and/or coinsurance from the patient (Casto and Layman 2011, 156). 41. The purpose of a physician query is to: a. Identify the MS-DRG b. Identify the principal diagnosisc. Improve documentation for patient care and proper reimbursement d. Increase reimbursement as form of optimization - ✔✔Correct Answer: C Improve documentation to support services billed (Johns 2011, 348). 42. Identify the correct ICD-9-CM diagnosis code(s) for a patient with seizures; epilepsy ruled out. a. 780.39 b. 345.9 c. 780.39, 345.9 d. 345.90 - ✔✔Correct Answer: A Code signs and symptoms when a condition is ruled out, which means the condition has been proven not to exist. The code for seizures (780.39) is assigned when a more specific diagnosis cannot be made even after all the facts bearing on the case have been investigated (Hazelwood and Venable 2012, 68- 73). 43. The Privacy Rule applies to: a. All covered entities involved with transmitting or performing any electronic transactions specified in the act b. Healthcare providers onlyc. Only healthcare providers that receive Medicare reimbursement d. Only entities funded by the federal government - ✔✔Correct Answer: A The Privacy Rule is applicable to all covered entities involved, either directly or indirectly, with transmitting or performing any electronic transactions specified in the act (Johns 2011, 823). 44. Which answer FAILS to provide a requirement for assignment of the MS-DRG? a. Diagnoses and procedures (principal and secondary) b. Attending and consulting physicians c. Presence of major or other complications and comorbidities (MCC or CC) d. Discharge disposition or status - ✔✔**Correct Answer: B Attending and consulting physicians have no bearing on the assignment of the MS-DRG and payment to the hospital (Schraffenberger 2012, 471-473). 45. Who is responsible for writing and signing discharge summaries and discharge instructions? a. Attending physician b. Head nursec. Primary physician d. Admitting nurse - ✔✔Correct Answer: A The physician principally responsible for the patient's hospital care writes and signs the discharge summary (Odom-Wesley et al. 2009, 200). 46. Under the HIPAA privacy standard, which of the following types of protected health information (PHI) must be specifically identified in an authorization? a. History and physical reports b. Operative reports c. Consultation reports d. Psychotherapy notes - ✔✔Correct Answer: D The distinction of psychotherapy notes is important due to HIPAA requirements that these notes may not be released unless specifically specified in an authorization (Odom-Wesley et al. 2009, 440). 47. In hospitals, automated systems for registering patients and tracking their encounters are commonly known as ______ systems. a. MIS b. CDSc. ADT d. ABC - ✔✔Correct Answer: C Automated systems for registering patients and tracking their encounters are commonly known as admission-discharge-transfer (ADT) systems (Johns 2011, 947). 48. Community Hospital implemented a clinical document improvement (CDI) program six months ago. The goal of the program was to improve clinical documentation to support quality of care, data quality, and HIM coding accuracy. Which of the following would be best to ensure that everyone understands the importance of this program? a. Request that the CEO write a memorandum to all hospital staff. b. Give the chairperson of the CDI committee authority to fire employees who don't improve their clinical documentation. c. Include ancillary clinical and medical staff in the process. d. Request a letter from the Joint Commission. - ✔✔Correct Answer: C Staff participation in the process of developing and implementing a program will contribute to the staff understanding of the importance of the program (Russo 2010, chapter 6). 49. Statements that define the performance expectations and/or structures or processes that must be in place are: a. Rulesb. Policies c. Guidelines d. Standards - ✔✔Correct Answer: D Standards are fixed rules that must be followed, which is different from a guideline that provides general direction (Johns 2011, 416). 50. What was the goal of the MS-DRG system? a. To improve Medicare's capability to recognize severity of illness in its inpatient hospital payments. The new system is projected to increase payments to hospitals for services provided to sicker patients and decrease payments for treating less severely ill patients. b. To improve Medicare's capability to recognize poor quality of care and pay hospitals on an incentive grid that allows hospitals to be paid by performance. c. To improve Medicare's capability to recognize groups of data by patient populations, which will further allow Medicare to adjust the hospitals wage indexes based on the data. This adjustment will be a system to pay hospitals fairly across all geographic locations. d. To improve Medicare's capability to recognize practice patterns among hospitals that are inappropriately optimizing payments by keeping patients in the hospital longer than the median length of stay. - ✔✔**Correct Answer: A For fiscal year 2008, Medicare adopted a severity-adjusted diagnosis-related groups system called Medicare Severity-DRGs (MS-DRGs). This was the most drastic revision to the DRG system in 24 years. The goal of the new MS-DRG system was to significantly improve Medicare's ability to recognize severity of illness in its inpatient hospital payments. The new system is projected to increase payments to hospitals for services provided to the sicker patients and decrease payments for treating less severely ill patients (Schraffenberger 2012, 471-473).51. A hospital is planning on allowing coding professionals to work at home. The hospital is in the process of identifying strategies to minimize the security risks associated with this practice. Which of the following would be best to ensure that data breaches are minimized when the home computer is unattended? a. User name and password b. Automatic session terminations c. Cable locks d. Encryption - ✔✔Correct Answer: B Automatic session termination will help to control access to the computer when unattended by automatically ending the session when not in use, preventing unauthorized access (HHS 2006a). 52. What healthcare organizations collect UHDDS data? a. All outpatient settings including physician clinics and ambulatory surgical centers b. All outpatient settings including cancer centers, independent testing facilities, and nursing homes c. All non-outpatient settings including acute-care, short-term care, long-term care, and psychiatric hospitals; home health agencies; rehabilitation facilities; and nursing homes d. All inpatient settings and outpatient settings with a focus on ambulatory surgical centers - ✔✔Correct Answer: CThe Uniform Hospital Discharge Data Set was promulgated by the US Department of Health, Education, and Welfare in 1974 as a minimum, common core of data on individual acute-care, short-term hospital discharges in Medicare and Medicaid programs. It sought to improve the uniformity and comparability of hospital discharge data. In 1985, the data was expanded to include all nonoutpatient settings (Schraffenberger 2012, 63-65). 53. What should a hospital do when a state law requires more stringent privacy protection than the federal HIPAA privacy standard? a. Ignore the state law and follow the HIPAA standard b. Follow the state law and ignore the HIPAA standard c. Comply with both the state law and the HIPAA standard d. Ignore both the state law and the HIPAA standard and follow relevant accreditation standards - ✔✔Correct Answer: C When a state law is more stringent than a federal law, hospitals must comply with both (Odom-Wesley et al. 2009, 68). 54. What should be done when the HIM department's error or accuracy rate is deemed unacceptable? a. A corrective action should be taken. b. The problem should be treated as an isolated incident. c. The formula for determining the rate may need to be adjusted.d. Re-audit the problem area. - ✔✔Correct Answer: A Corrective action should be taken when error or accuracy rates are deemed to be at an unacceptable rate (Johns 2011, 417). 55. Identify the correct ICD-9-CM diagnosis code(s) for a patient with sepsis due to Staphylococcus aureus septicemia. a. 038.11, 995.91 b. 995.91, 038.11 c. 038.11 d. 038.11, 995.92 - ✔✔Correct Answer: A 038.11, Septicemia, Staphylococcus aureus, and 995.91, Sepsis. The "Code first" note following code 995.91 directs the coder to assign the code for the underlying infection first (Schraffenberger 2012, 80- 81). 56. An HIM professional's ethical obligations: a. Apply regardless of employment site b. Are limited to the employer c. Apply to only the patientd. Are limited to the employer and patient - ✔✔Correct Answer: A HIM ethical obligations apply regardless of employment site (Johns 2011, 754). 57. Which of the following provides organizations with the ability to access data from multiple databases and to combine the results into a single questions-and-reporting interface? a. Client-server computer b. Data warehouse c. Local area network d. Internet - ✔✔Correct Answer: B A data warehouse is a special type of database that consolidates and stores data from various databases (Johns 2011, 909). 58. During a review of documentation practices, the HIM director finds that nurses are routinely using the copy-and-paste function of the hospital's new EHR system for documenting nursing notes. In some cases, nurses are copying and pasting the objective data from the lab system and intake-output records as well as the patient's subjective complaints and symptoms originally documented by another practitioner. Which of the following should the HIM director do to ensure the nurses are following acceptable documentation practices? a. Inform the nurses that "copy and paste" is not acceptable and to stop this practice immediately. b. Determine how many nurses are involved in this practice.c. Institute an in-service training session on documentation practices. d. Develop policies and procedures related to cutting, copying, and pasting documentation in the EHR system. - ✔✔Correct Answer: D In order to thoughtfully and appropriately manage copy functionality, organizations must have sound documentation integrity policies within their organization. HIM professionals should lead their organizations in developing copy policies and procedures that address operational processes, utilization of copy functionality, documentation guidelines, responsibility, and auditing and reporting (AHIMA 2012b, 9-10, 18-21). Documentation policies are used to define the acceptable practices that should be followed by all applicable staff to ensure consistency and [Show More]
Last updated: 2 years ago
Preview 1 out of 460 pages
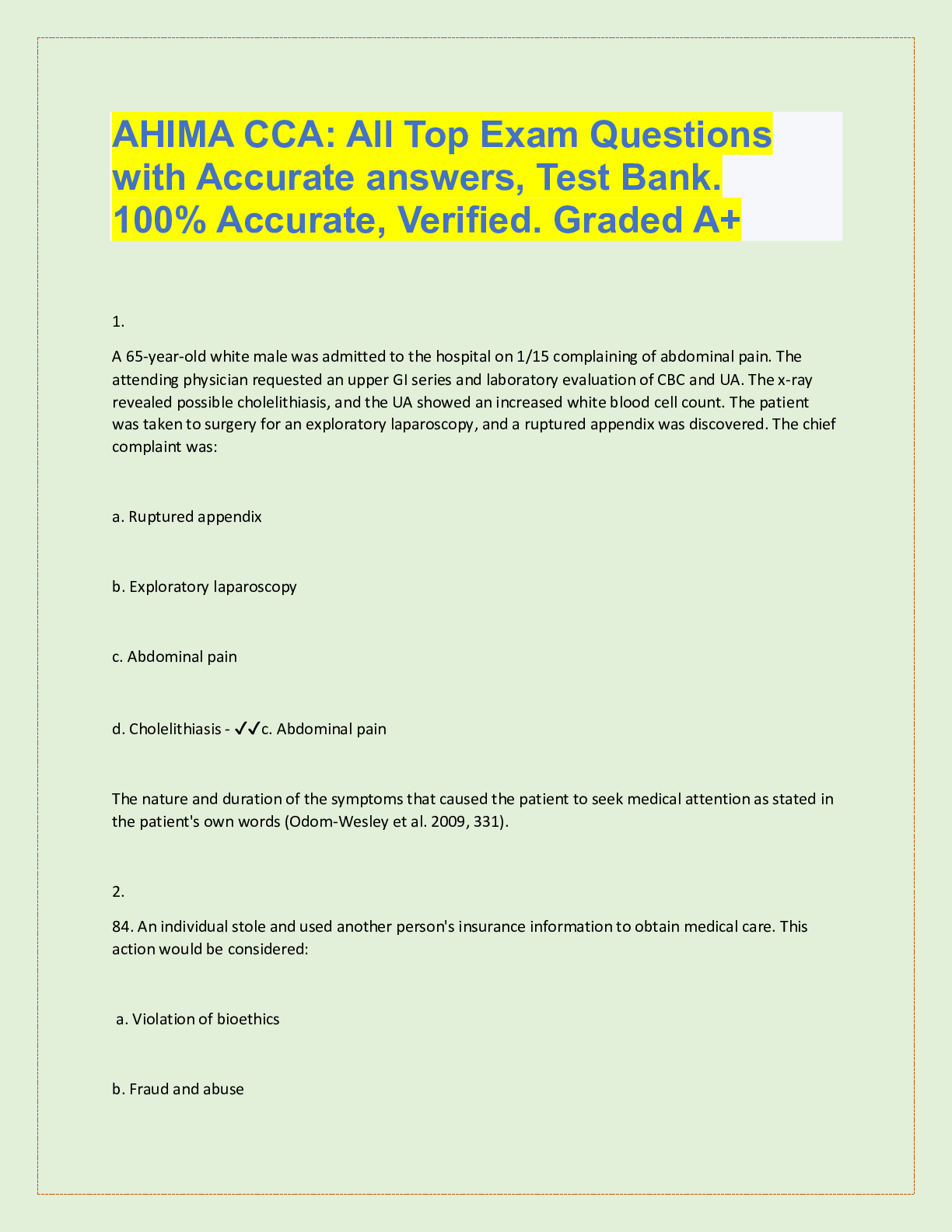
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 04, 2022
Number of pages
460
Written in
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Sep 04, 2022
Downloads
0
Views
121