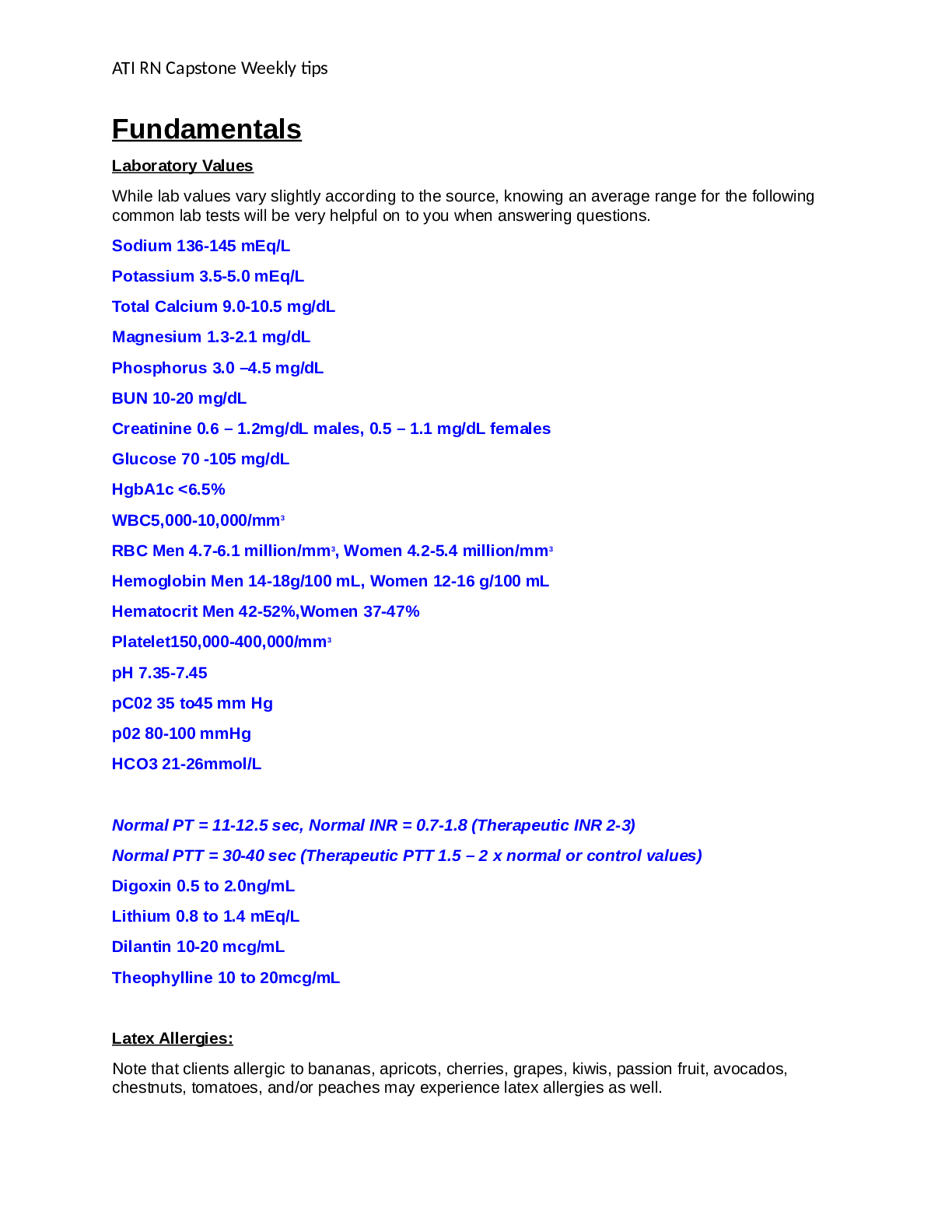
ATI Fundamentals Exam Prep./Review
$ 19
.png)
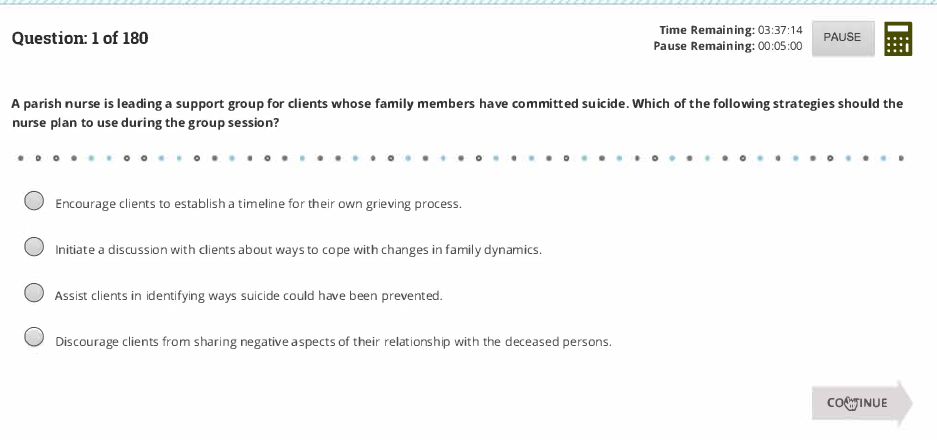
PMHNP certification Exam 2022 (Actual test verified A+)
$ 8

NURS 1102
$ 30
NURS 1102
$ 28

NURS 1102
$ 30

NURS 1102
$ 35
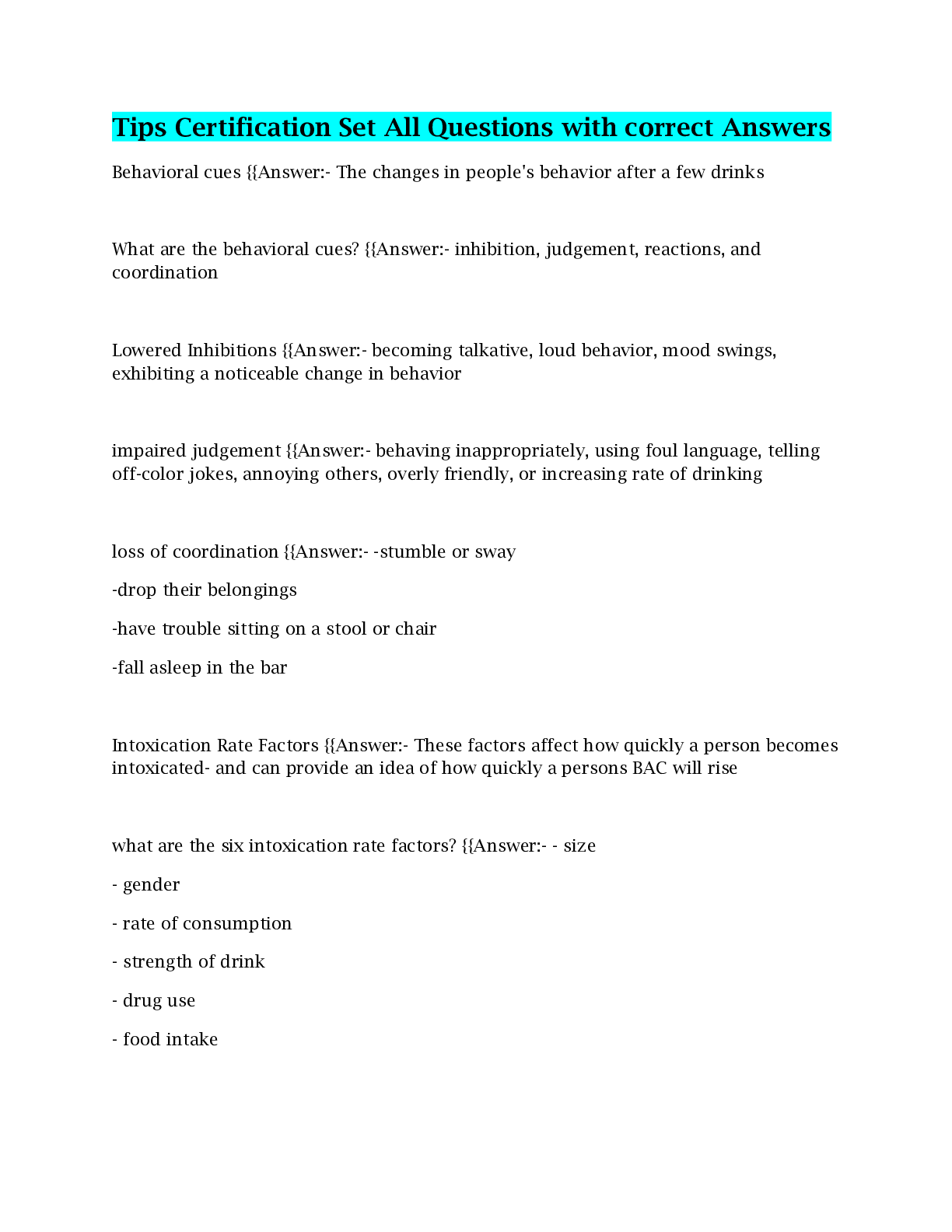
Tips Certification Set All Questions with correct Answers
$ 8
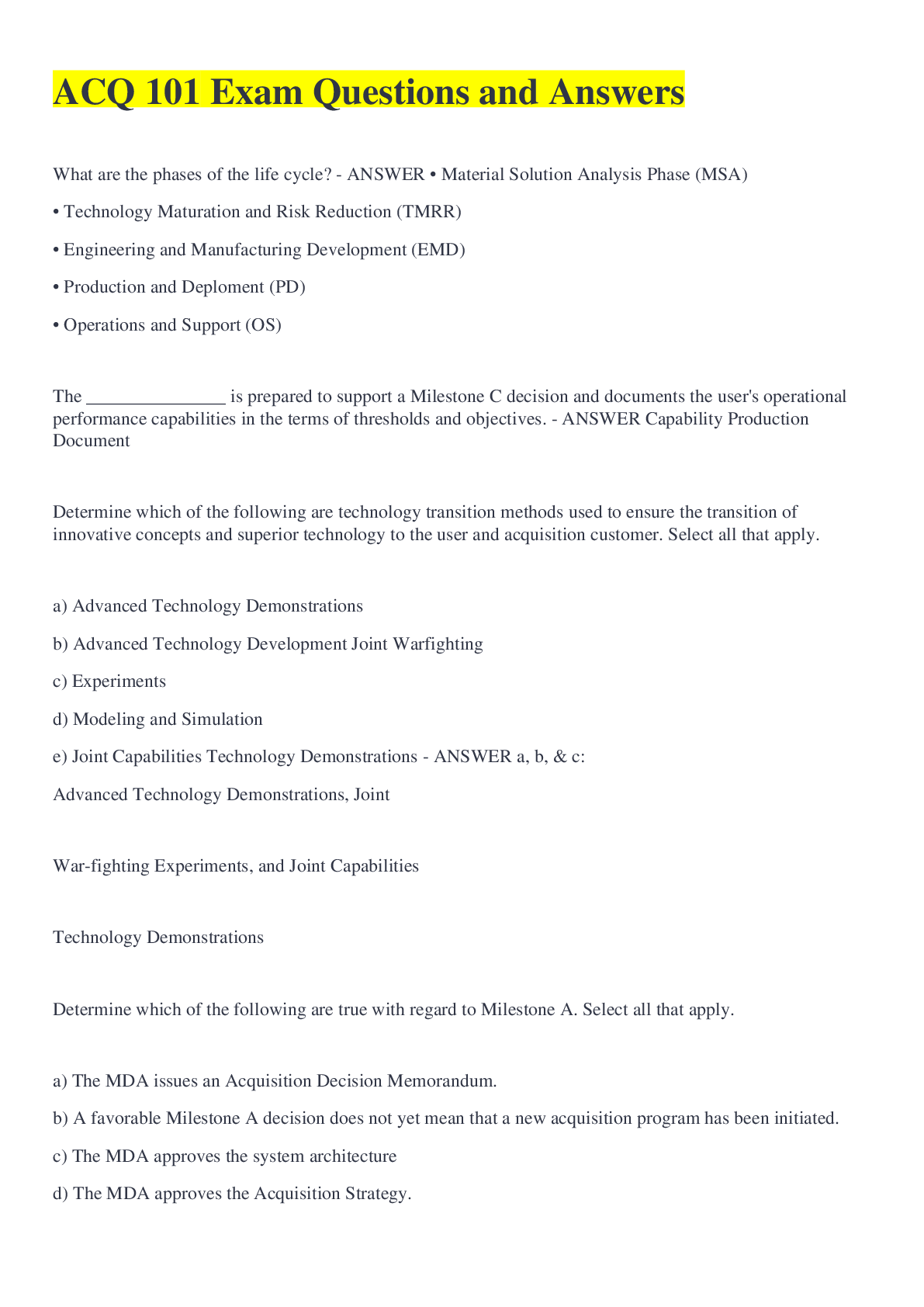
ACQ 101 Exam Questions and Answers
$ 7
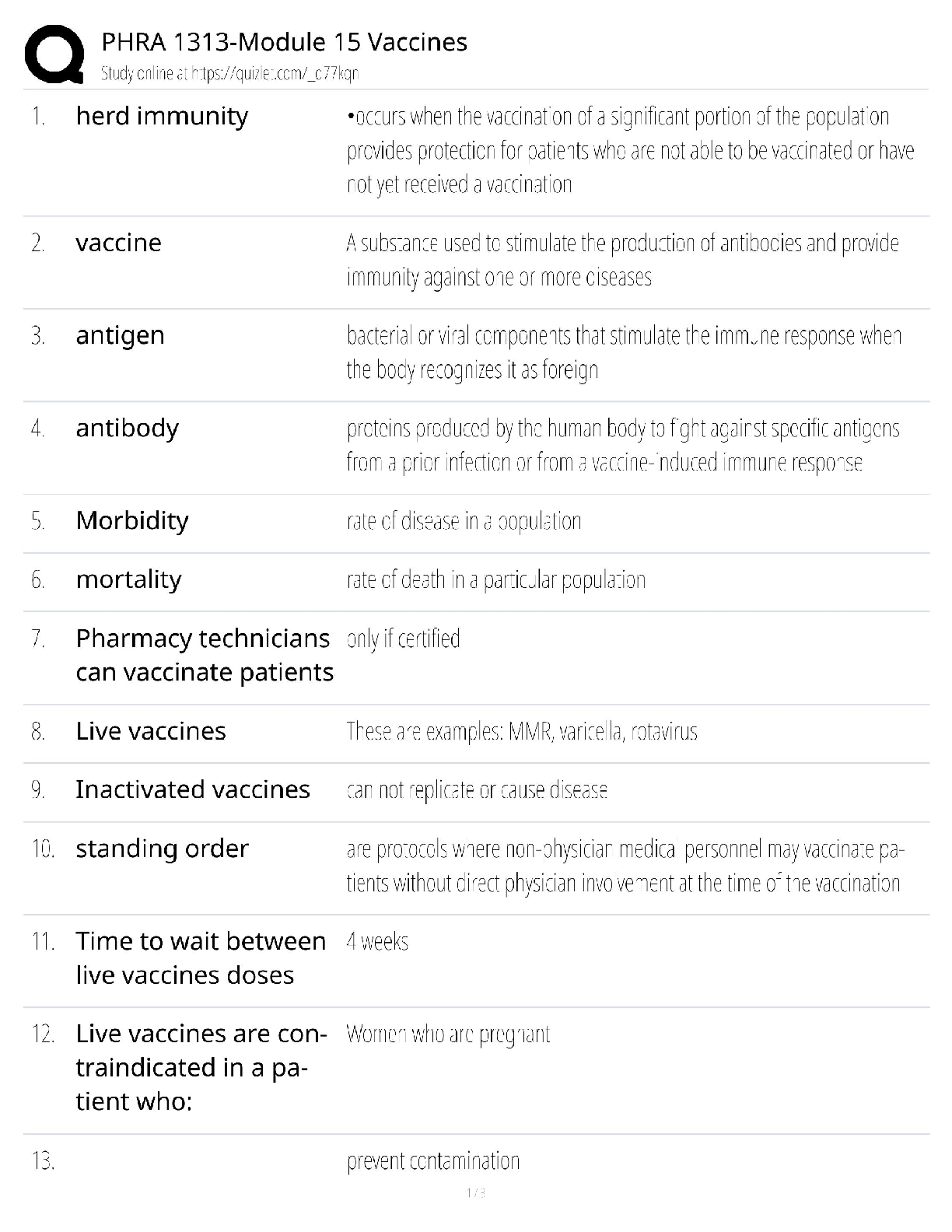
PHRA 1313 Module 15 / Vaccines Study Guide / Pharmacy Tech / 2025 Update / Score 100%
$ 15

NURS 1102
$ 28

ATI Nutrition Proctored Study Guide Updated
$ 14
.png)
bobs_meltdown_case_study Final
$ 11
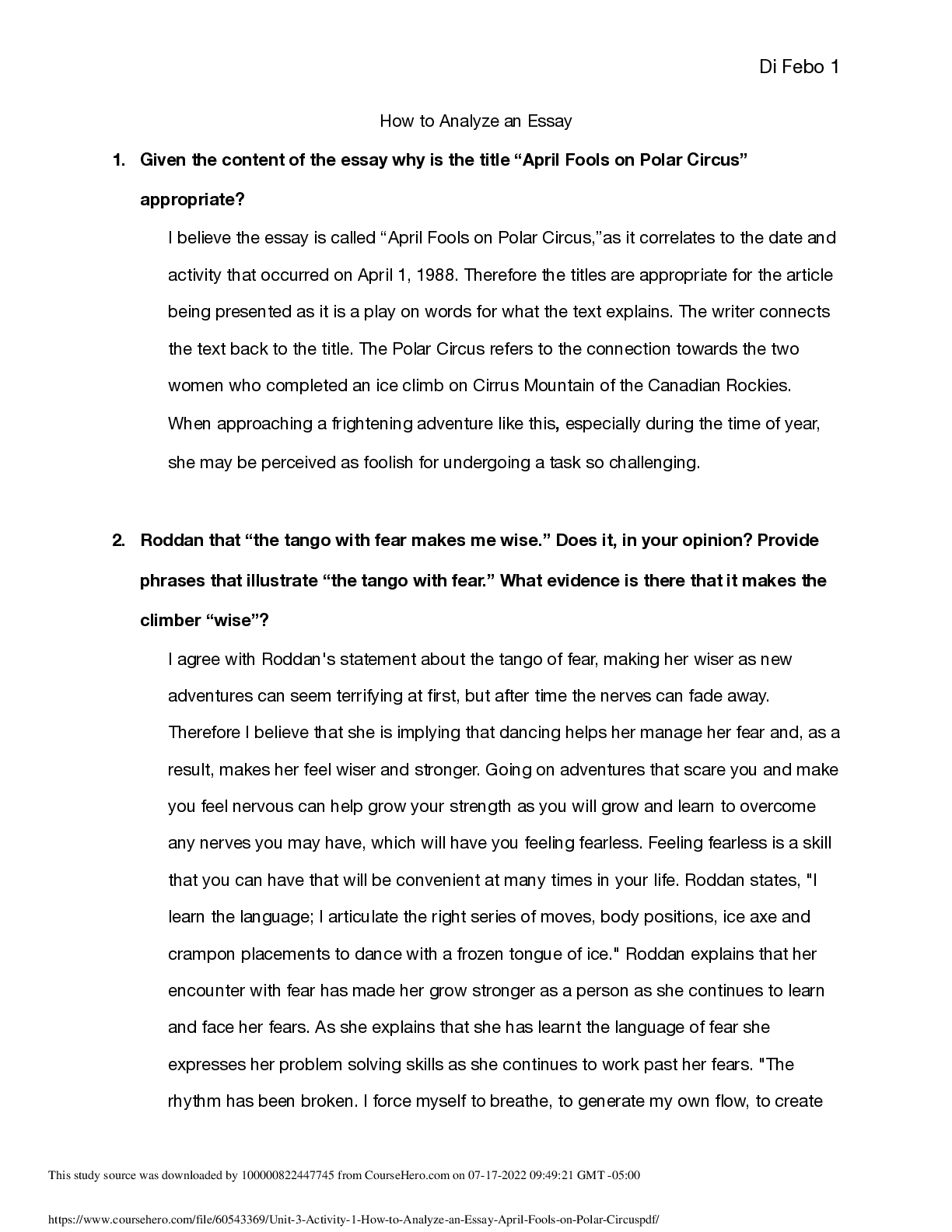
How to Analyze an Essay
$ 6.5
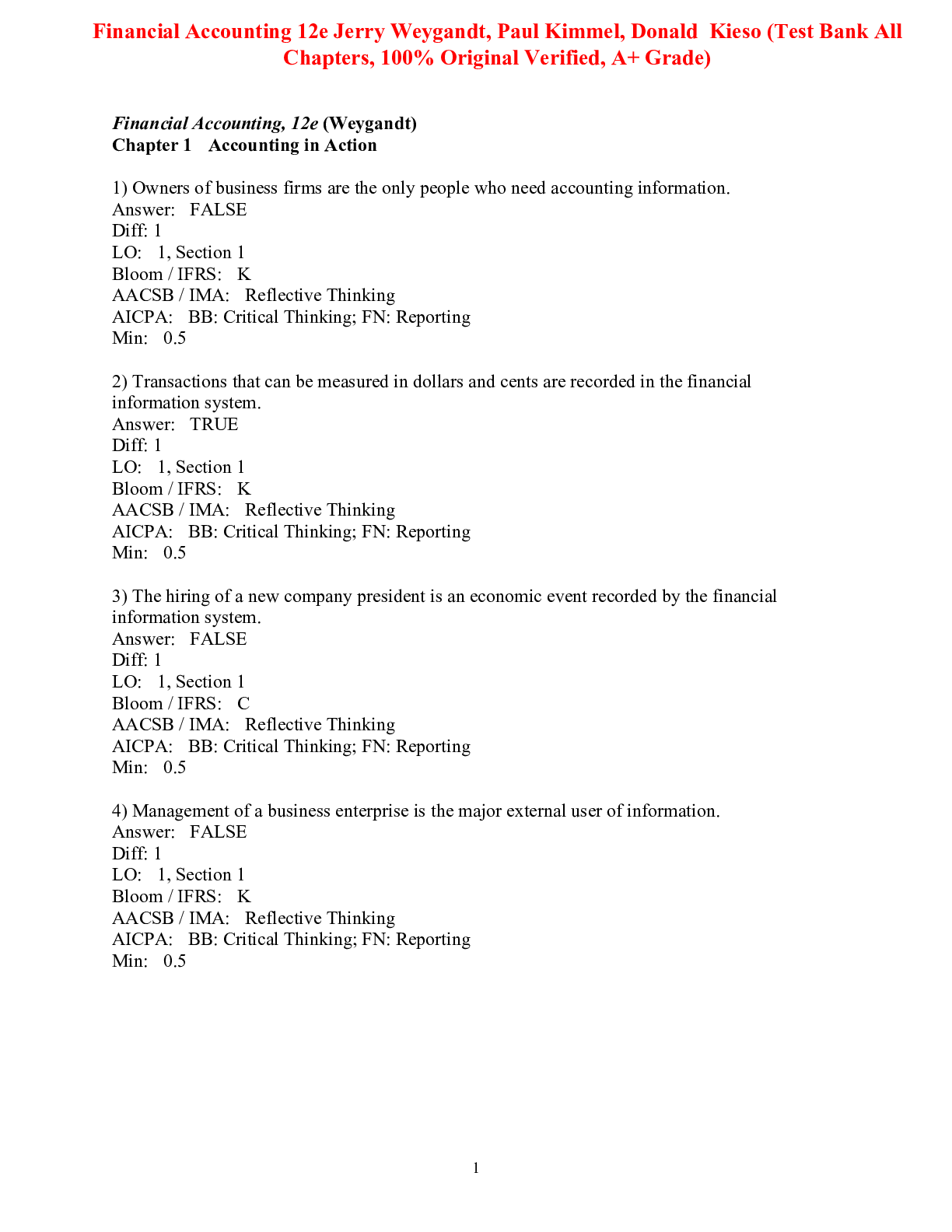
Test Bank For Financial Accounting 12th Edition By Jerry Weygandt, Paul Kimmel, Donald Kieso (All Chapters, 100% Original Verified, A+ Grade)
$ 25
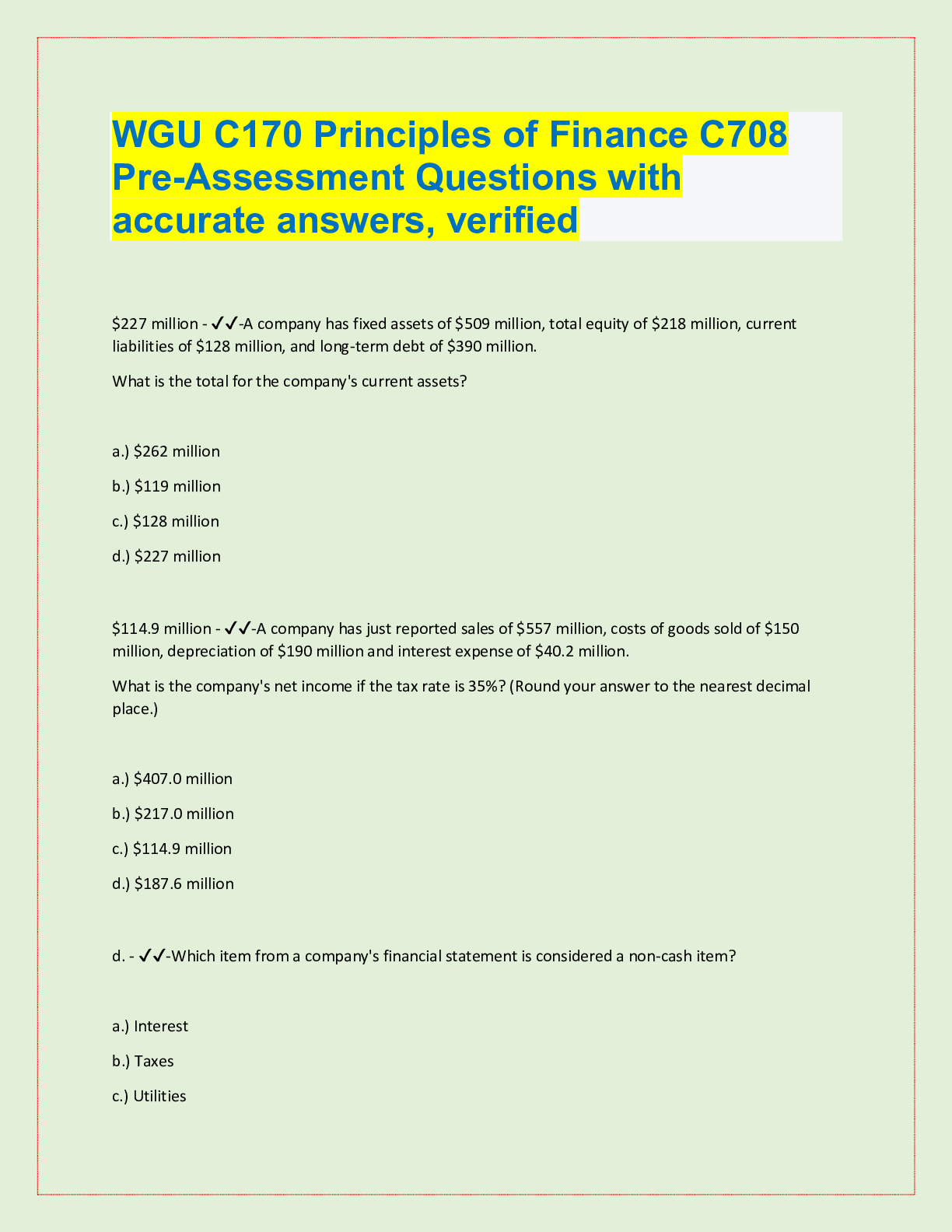
WGU C170 Principles of Finance C708 Pre-Assessment Questions with accurate answers, verified
$ 10
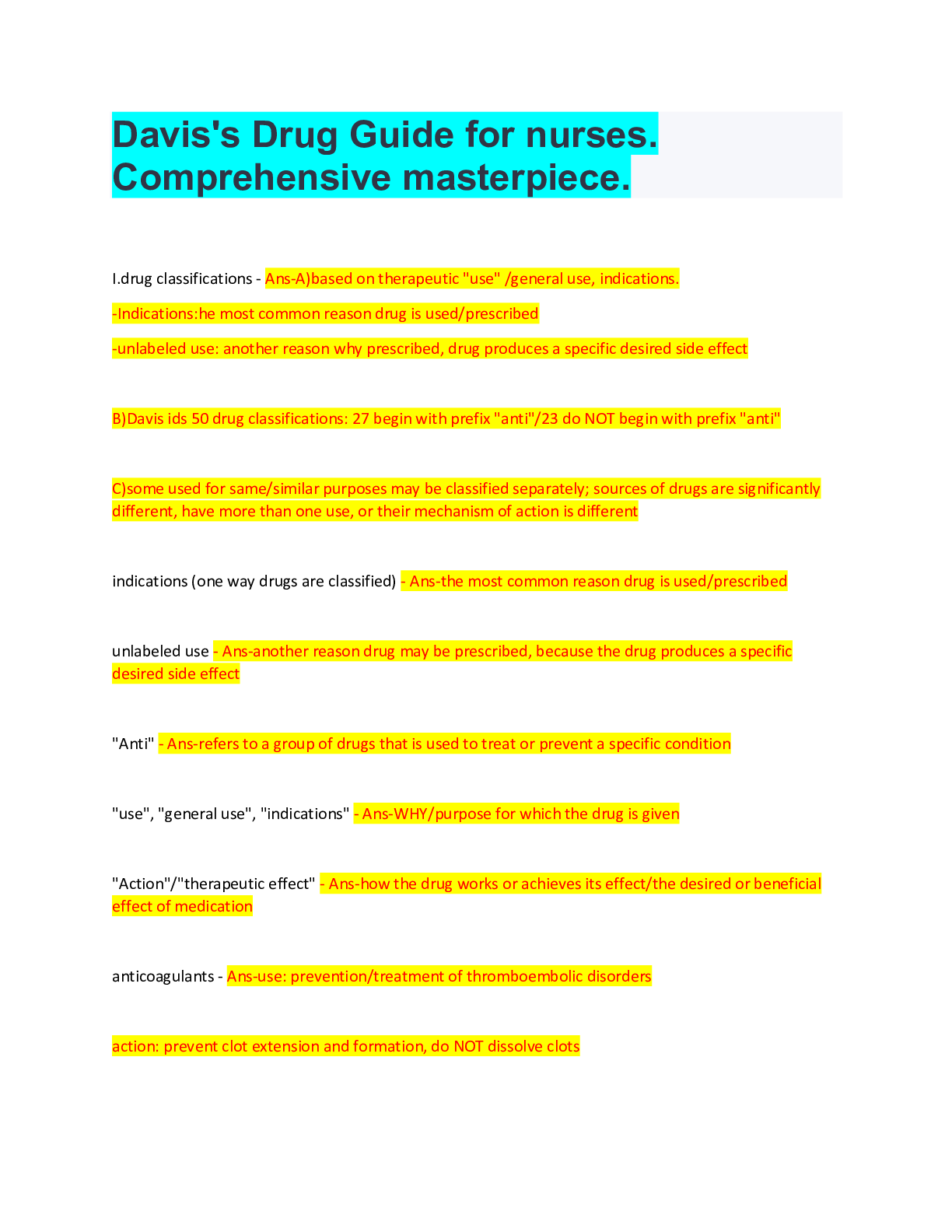
Davis's Drug Guide for nurses. Comprehensive masterpiece.
$ 10

ATI PROCTORED REMEDIATION NUTRITION VERIFIED SOLUTION LATEST UPDATE
$ 5
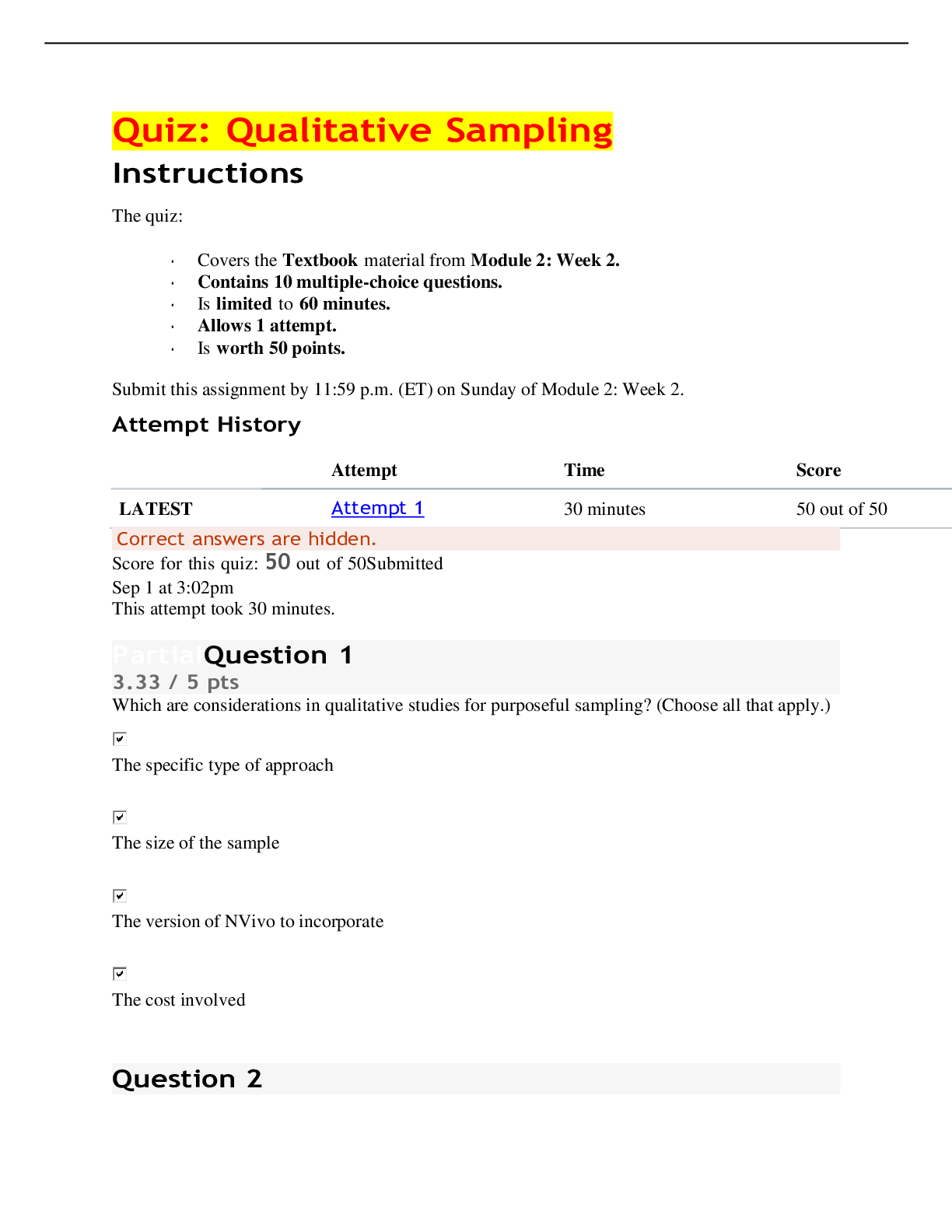
EDUC 817 Quiz 817 Qualitative Sampling Score for this quiz: 50 out of 50:-Liberty University Online Academy
$ 9.5
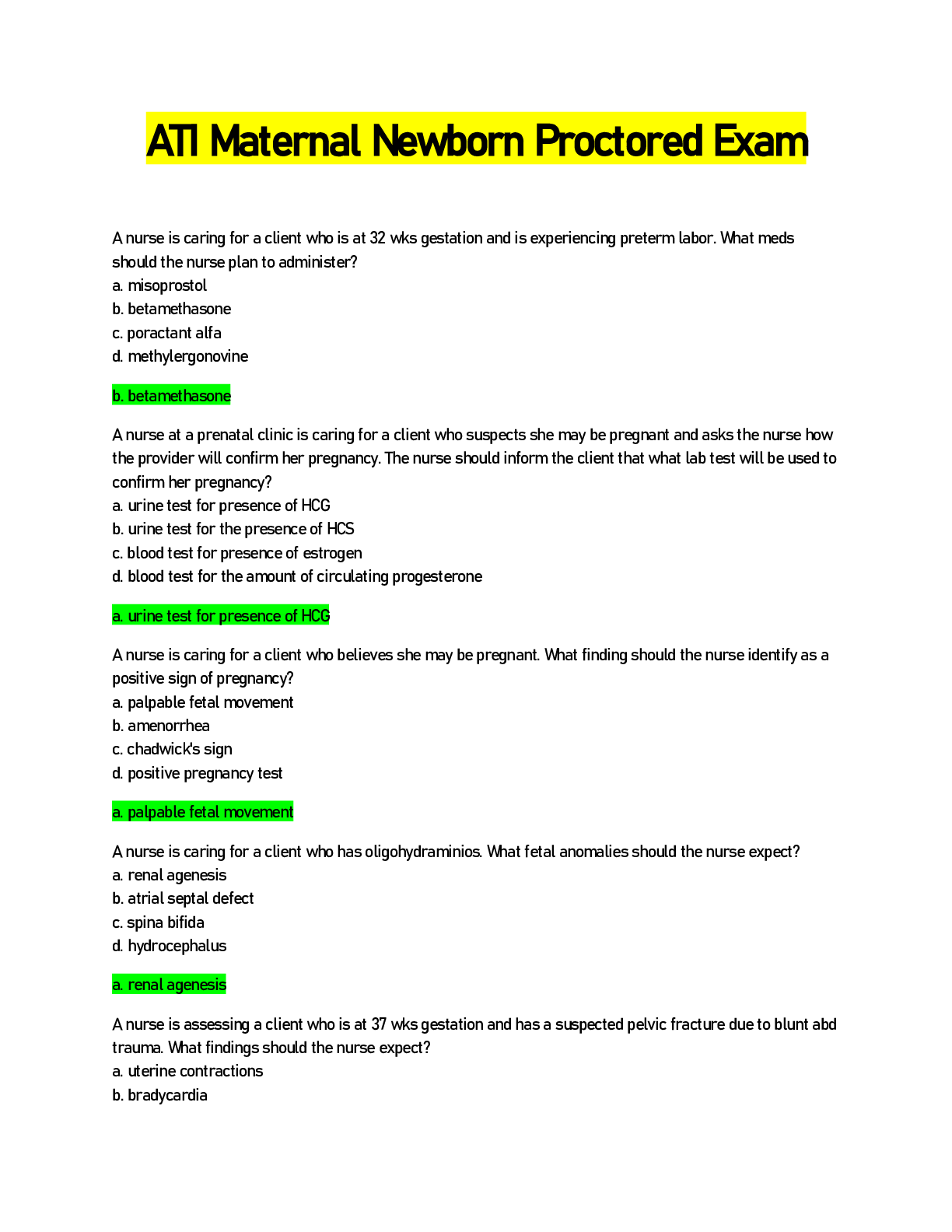
ATI Maternal Newborn Proctored Exam 2022
$ 15
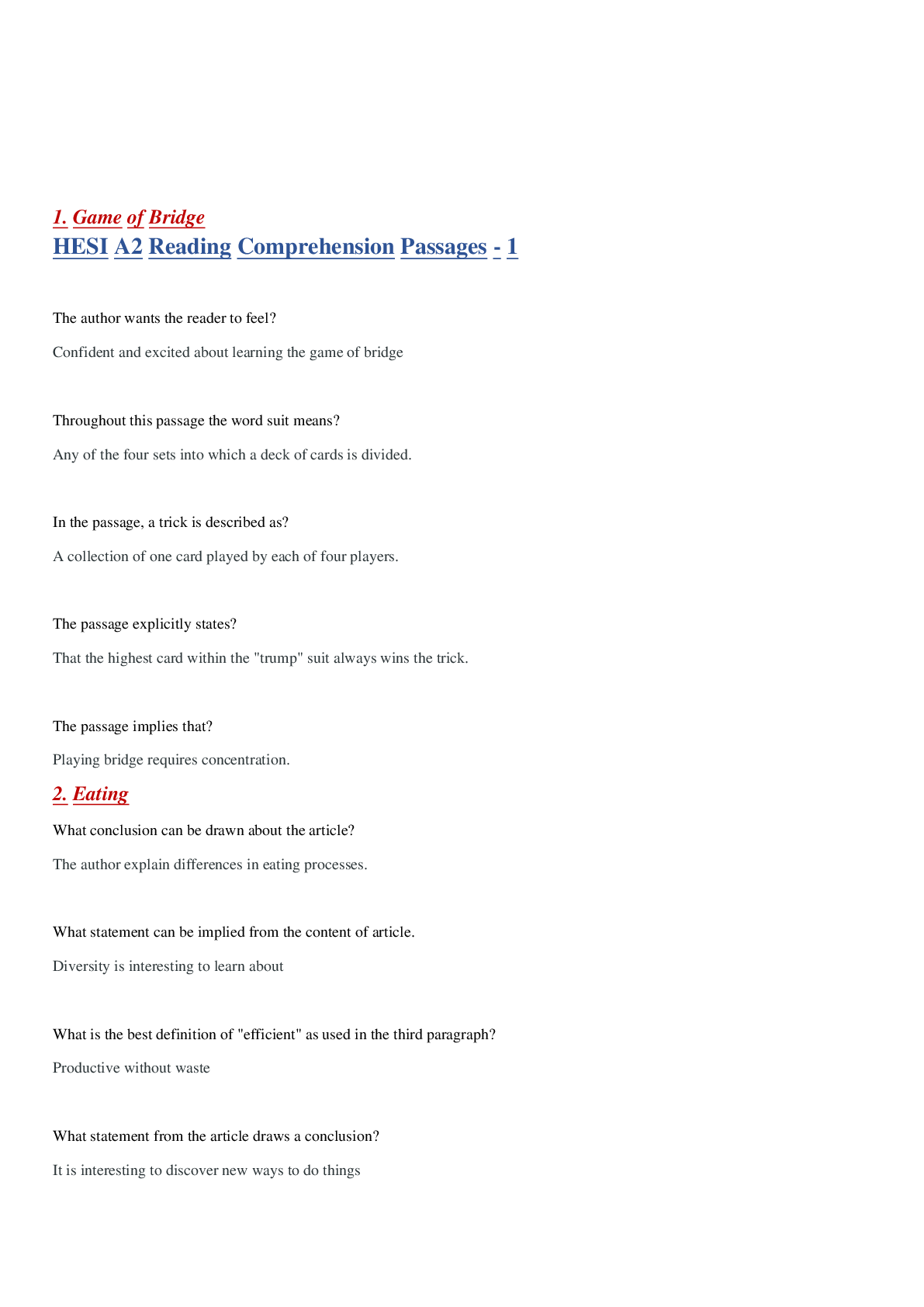
HESI - A2 Reading & Writing V1 Latest 2022
$ 14

COS1512 Introduction to Programming II Semester II
$ 12
NAMS Exam Study Guide for Menopause Practitioners
$ 12.5

HESI Review (Adult Health II Final) Questions and Answers Rated A+
$ 10

ATI FUNDAMENTALS PROCTORED EXAM 2019 RETAKE
$ 21.5
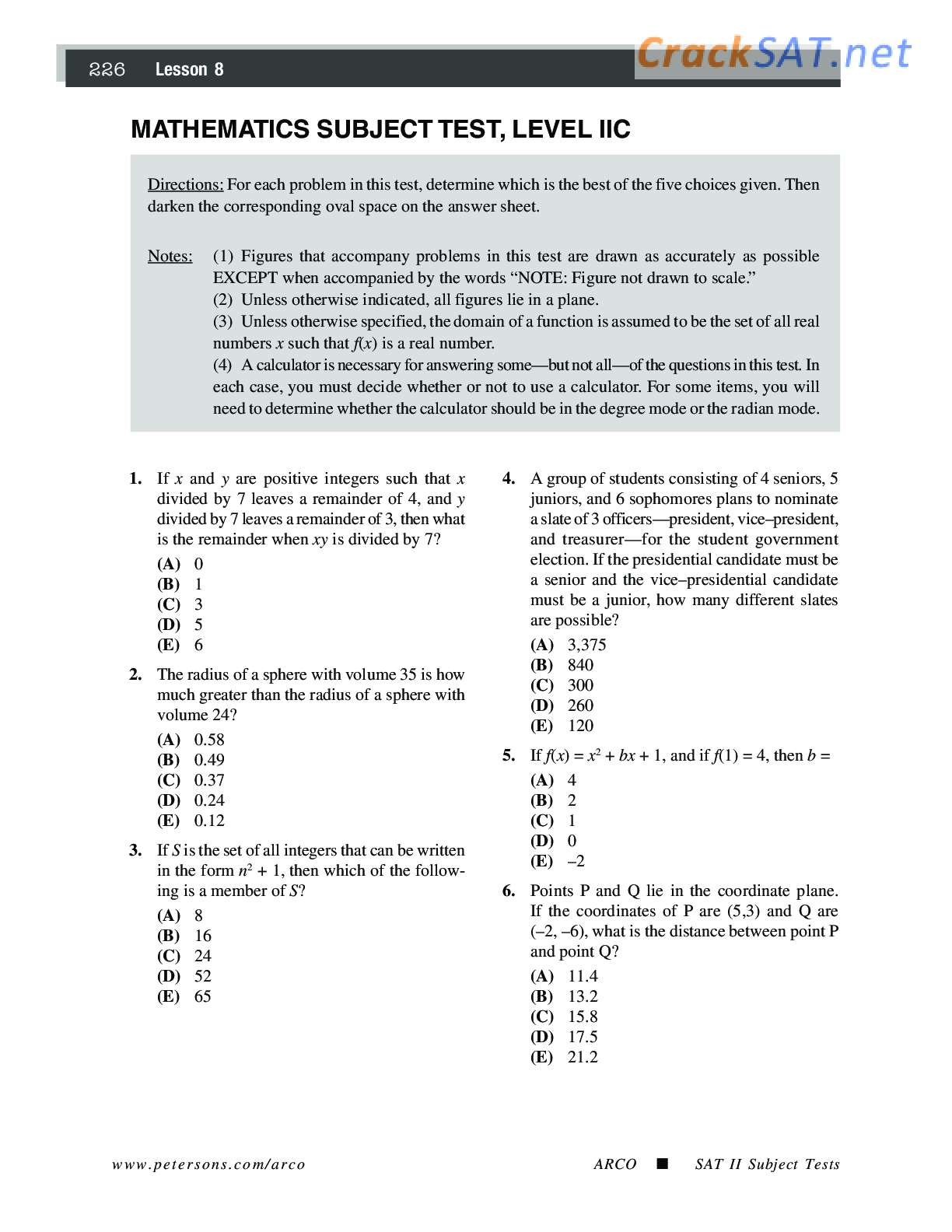
ARCO SAT Subject Math Level 2 Practice Test
$ 7.5
Psychological Testing Principles, Applications, And Issues 9th Edition By Robert M. Kaplan Chapter 1_21 TEST BANK
$ 27.5
Permanent Makeup VA Regulations 2023
$ 13
Test Bank for Art Matters, 1st edition Pam Gordon
$ 29
QBO 2023 Certification Exam / Practice Exam #2 / QuickBooks Online Test Bank / Score 100% 2025
$ 23
NAB Test Exam Test Bank With Complete Solution
$ 16
Ebook PDF Environmental Data Management at NOAA: Archiving, Stewardship, and Access
$ 15
TEAS ALL SECTIONS PREP: EVERYTHING YOU NEED (100% Guarantee)
$ 17.5
TIPS Certification Study Guide with complete solution
$ 8
ACC 410 Week 5 Assignment Audit Report Modifications Paper
$ 8

Macro Topic 2.6 Real v. Nominal GDP | Real_vs_Nominal_GDP
$ 5.5
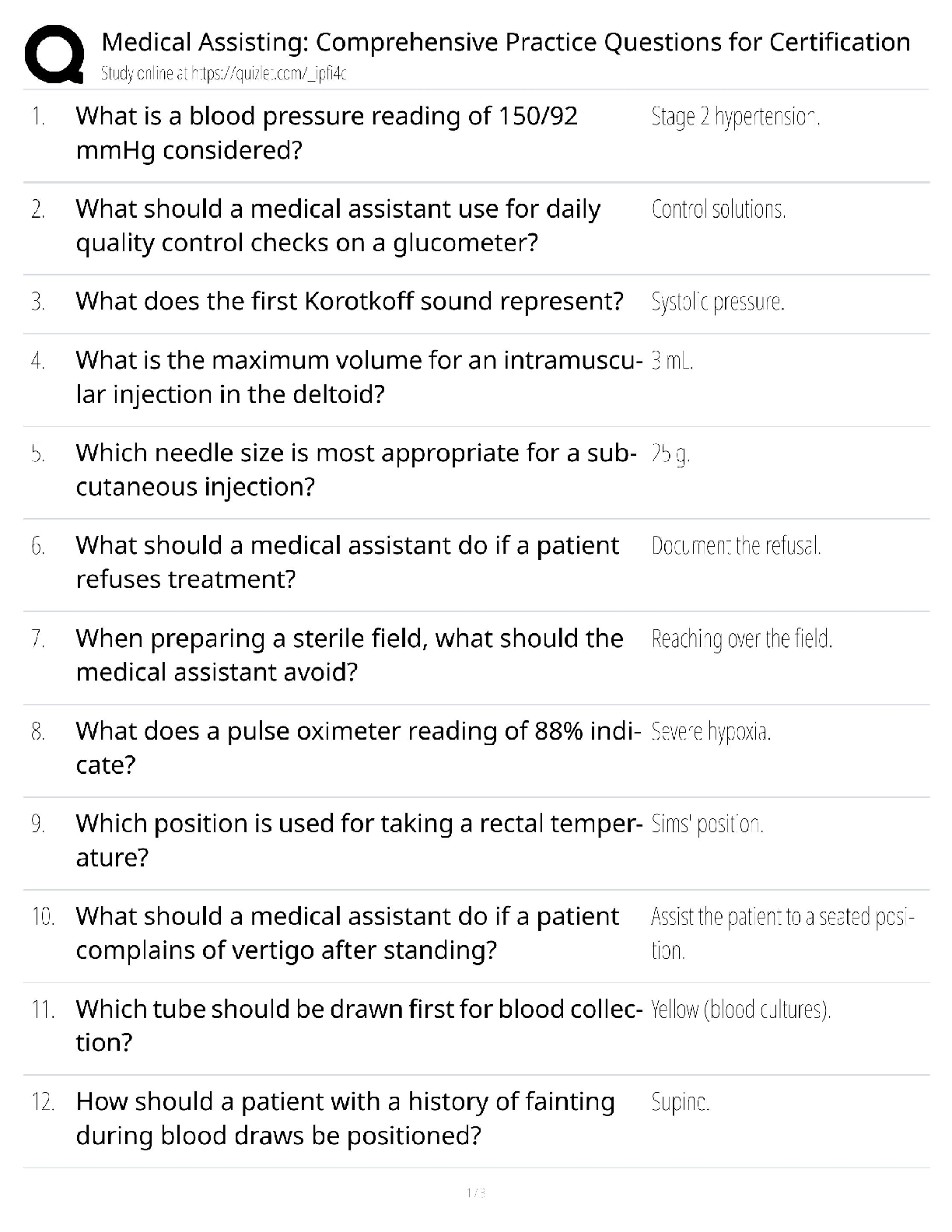
Medical Assisting Comprehensive Practice Questions for Certification / score 100% / new version / 2025 update / Study Guide & Exam Prep
$ 19
eBook [PDF] Getting to Yes Negotiating Agreement Without Giving In 1th Edition By (Updated & Revised Edition) By Roger Fisher, William Ury, Bruce Patton
$ 30

BTEC Applied Science Titration and Colorimetry Unit 2 Assignment 1
$ 12
RN ATI Comprehensive Predictor 2025 New Version
$ 18
Brunner Suddarth Chapter 06 Transcultural Nursing Test 2023
$ 6
TIPS Certification Exam Questions and Answers 100%
$ 8

Final Project Health Information.docx Final Project: Health Information Technology Reco
$ 7
ARDMS SPI STUDY GUIDE (LATEST 2022/2023) Correct Q & A, SATISFACTION GUARANTEED
$ 13
eBook Humanism and Resilience in Residency Training A Guide to Physician Wellness 1st Edition By Ana Hategan , Karen Saperson , Sheila Harms , Heather Waters
$ 29
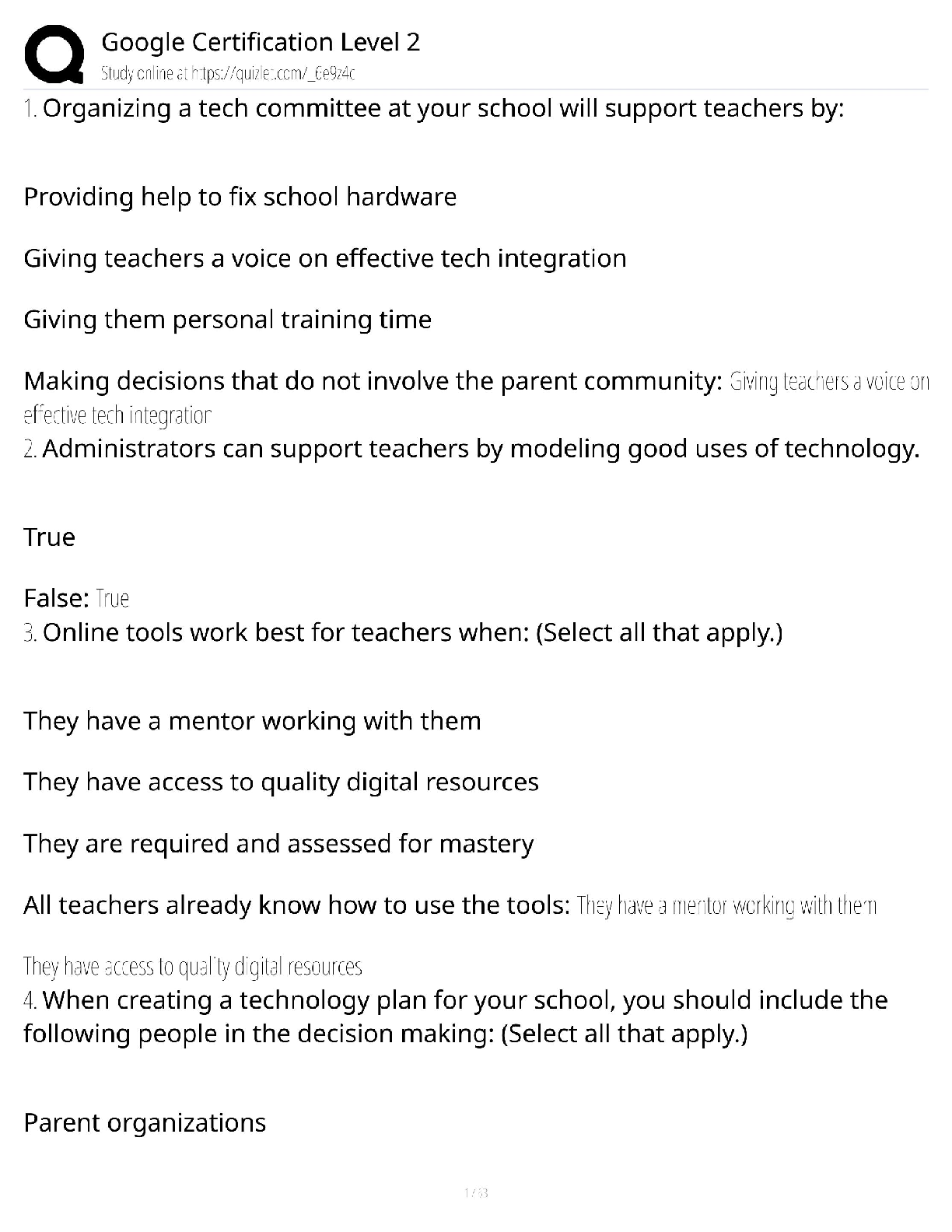
Google Certification Level 2 / Score 100% / Advanced Exam / 2025 Study Guide
$ 20.5
SAT-II-Math-Level-2-Practice-Test-C
$ 6.5
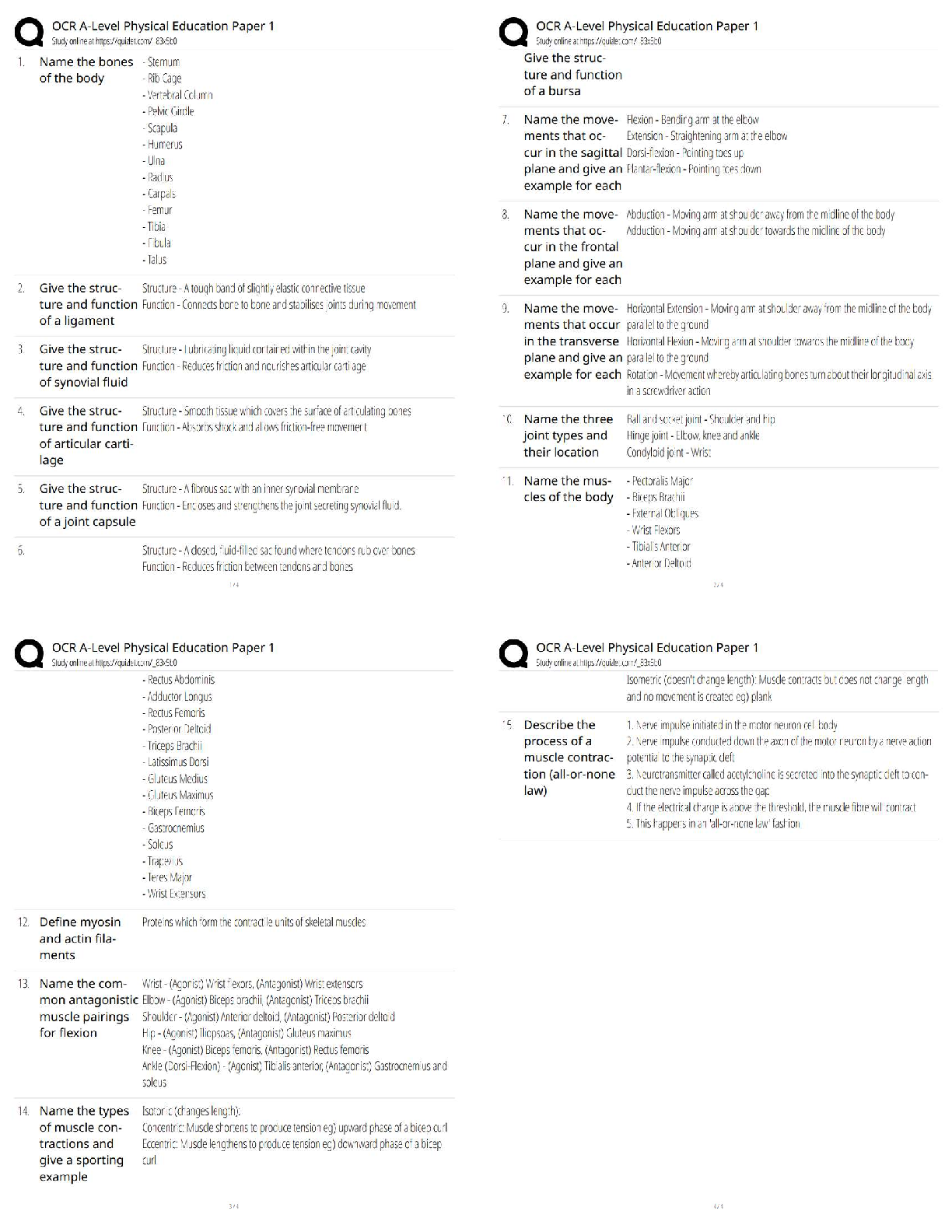
OCR A-Level Physical Education Paper 1 | Physiological Factors Affecting Performance / 2025 Updated
$ 7.5
ANAPHY.
$ 15
Bates' Guide To Physical Examination and History Taking 13thEdition Bickley Test Bank






 (1).png)