MUSCULOSKELETAL NURSING MANAGEMENT
Nursing Care of Fractures
Important concepts to keep in mind when caring for patients with fractures are mobility, pain, and perfusion. Fractures result in immobility, painful, and
...
MUSCULOSKELETAL NURSING MANAGEMENT
Nursing Care of Fractures
Important concepts to keep in mind when caring for patients with fractures are mobility, pain, and perfusion. Fractures result in immobility, painful, and result in impaired perfusion.
Fractures are disruptions or breaks in the continuity of bone structure. The majority of fractures result from traumatic injuries, however some fractures are secondary to disease processes such as cancer or osteoporosis.
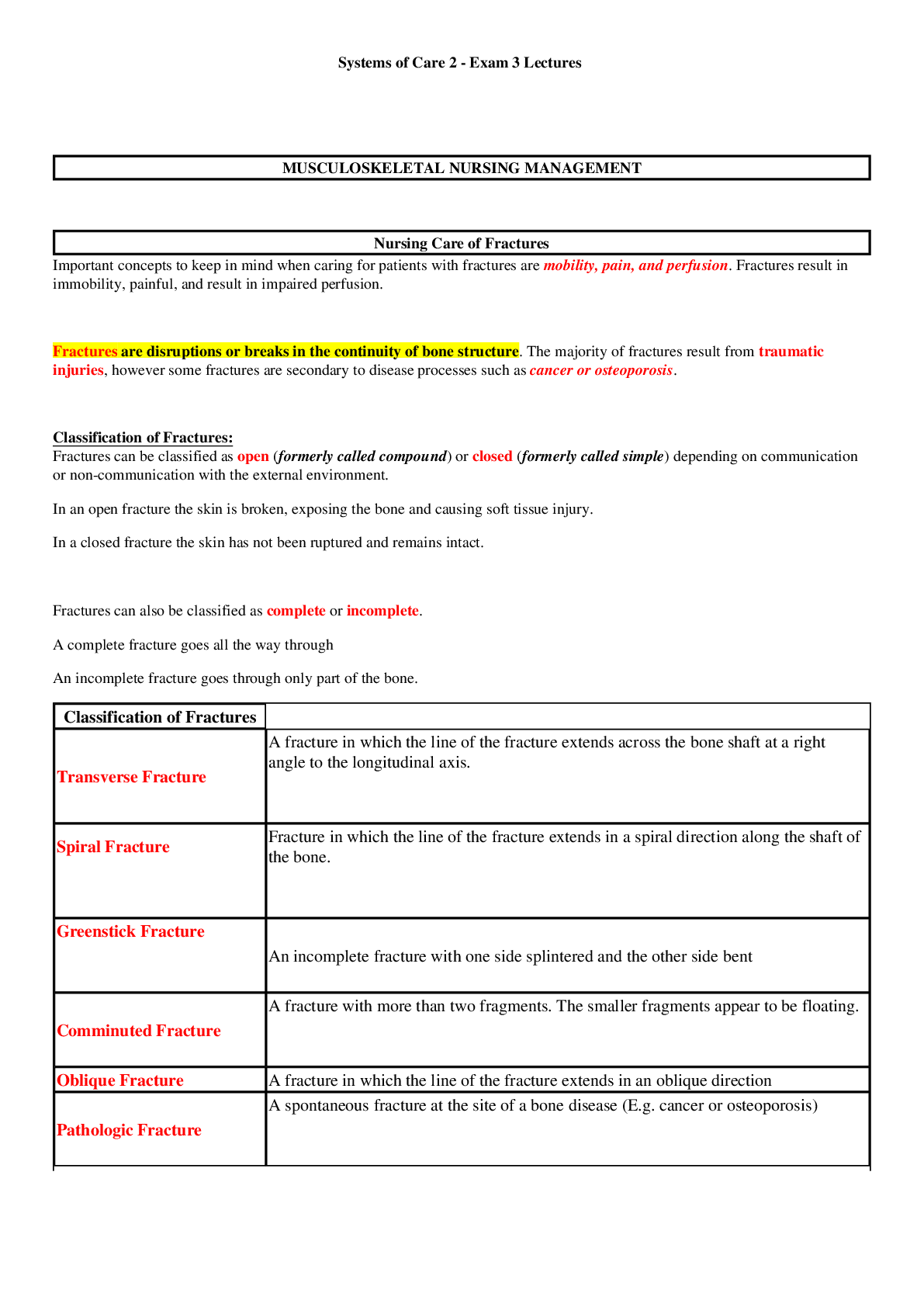
Classification of Fractures:
Fractures can be classified as open (formerly called compound) or closed (formerly called simple) depending on communication or non-communication with the external environment.
(1) In an open fracture the skin is broken, exposing the bone and causing soft tissue injury.
(2) In a closed fracture the skin has not been ruptured and remains intact.
Fractures can also be classified as complete or incomplete.
(1) A complete fracture goes all the way through
(2) An incomplete fracture goes through only part of the bone.
Classification of Fractures
Transverse Fracture A fracture in which the line of the fracture extends across the bone shaft at a right angle to the longitudinal axis.
Spiral Fracture
Fracture in which the line of the fracture extends in a spiral direction along the shaft of the bone.
Greenstick Fracture
An incomplete fracture with one side splintered and the other side bent
Comminuted Fracture A fracture with more than two fragments. The smaller fragments appear to be floating.
Oblique Fracture A fracture in which the line of the fracture extends in an oblique direction
Pathologic Fracture A spontaneous fracture at the site of a bone disease (E.g. cancer or osteoporosis)
Stress Fracture
A fracture that occurs in normal or abnormal bone that is subject to repeated stress, such as from jogging/running or gymnastics.
Fractures can also be classified as displaced or nondisplaced.
Further Classification of Fractures
Displaced Fractures The two ends of the broken bone are separated from one another and out of their normal positions. Displaced fractures are usually:
• Comminuted (more than two fragments)
• Oblique.
Nondisplaced Fractures the periosteum is intact across the fracture, and the bone is still in alignment. Nondisplaced fractures are usually:
• Transverse
• Spiral
• Greenstick.
Neurovascular Assessment
Six P’s of Acute Neurovascular Compromise
Paresthesia Numbness and tingling of extremity
Pain Distal to injury that is not relieved by analgesics and pain on passive stretch of muscle traveling through compartment
Poikliothermia Coolness of extremity
Pallor Loss of normal color of extremity
Paralysis Loss of function and ability to move extremity (fingers/toes)
Pulselessness Diminished/absent peripheral pulses
CMS of Distal Neurovascular Status
Circulation Assess for pulses, temp, delayed cap refill, color
Movement Assess for movement of fingers/toes
Sensation Assess for sensation; paresthesia or anesthesia
Whenever a fracture is suspected, the extremity is immobilized in the position in which it is found. Unnecessary movement increases soft tissue damage and may convert a closed fracture to an open fracture or create further injury to adjacent neurovascular structures. Immobilization decreases the risk of fat embolism. Any extra movements will also be very painful and can potentially worsen the injury. Splints can be implemented to immobilize the limb.
For musculoskeletal injuries such as sprains or strains, the protocol is RICE:
(1) Rest
(2) Ice for 15-20 minutes several times a day
(3) Compression with an elastic wrap to help control swelling/excess inflammation
(4) Elevate the ankle or extremity above the heart to minimize swelling
For fractures, the protocol RIIE is used:
(1) Rest
(2) Ice for 15-20 minutes several times a day
(3) Immobilize
(4) Elevate the ankle or extremity above the heart to minimize swelling
Fracture Healing
Bone goes through a complex multistage healing process termed union that occurs through 6 stages.
1. Fracture Hematoma
Bleeding creates a hematoma, which surrounds the ends of the fragments. The hematoma is extravasated blood that changes from a liquid to a semisolid clot.
• This occurs in the initial 72 hours after injury.
2. Granulation Tissue During this stage, active phagocytosis absorbs the products of local necrosis. The hematoma converts to granulation tissue. Granulation tissue (consisting of new blood vessels, fibroblasts, and osteoblasts) produces the basis for new bone substance called osteoid during days 3 to 14 post injury.
3. Callus Formation As minerals (calcium, phosphorus, and magnesium) and new bone matrix are deposited in the osteoid, an unorganized network of bone is formed that is woven about the fracture parts. Callus is primarily composed of cartilage, osteoblasts, calcium, and phosphorus. It usually appears by the end of the second week after injury. Evidence of callus formation can be verified by x-ray.
4. Ossification Ossification of the callus occurs from 3 weeks to 6 months after the fracture and continues until the fracture has healed. Callus ossification is sufficient to prevent movement at the fracture site when the bones are gently stressed. However, the fracture is still evident on x-ray. During this stage of clinical union, the patient may be allowed limited mobility or the cast may be removed.
5. Consolidation As callus continues to develop, the distance between bone fragments diminishes and eventually closes. During this stage ossification continues. It can be equated with radiologic union. Radiologic union occurs when there is x-ray evidence of complete bony union. This phase can occur up to a year following injury.
6. Remodeling Excess bone tissue is reabsorbed in the final stage of bone healing, and union is completed. Gradual return of the injured bone to its preinjury structural strength and shape occurs. Bone remodels in response to physical loading stress or Wolf’s law. Initially, stress is provided through exercise. Weight bearing is gradually introduced. New bone is deposited in sites subjected to stress and resorbed at areas where there is little stress. Remodeling is accomplished as excess callus is reabsorbed and trabecular bone is laid down.
A, Bleeding at fractured ends of the bone with subsequent hematoma formation.
B, Organization of hematoma into fibrous network.
C, Invasion of osteoblasts, lengthening of collagen strands, and deposition of calcium.
D, Callus formation: new bone is built up as osteoclasts destroy dead bone.
E, Remodeling is accomplished as excess callus is reabsorbed and trabecular bone is laid down
[Show More]