*NURSING > QUESTIONS & ANSWERS > AHIP Practice Test, Questions with accurate answers,. Graded A+ (All)
AHIP Practice Test, Questions with accurate answers,. Graded A+
Document Content and Description Below
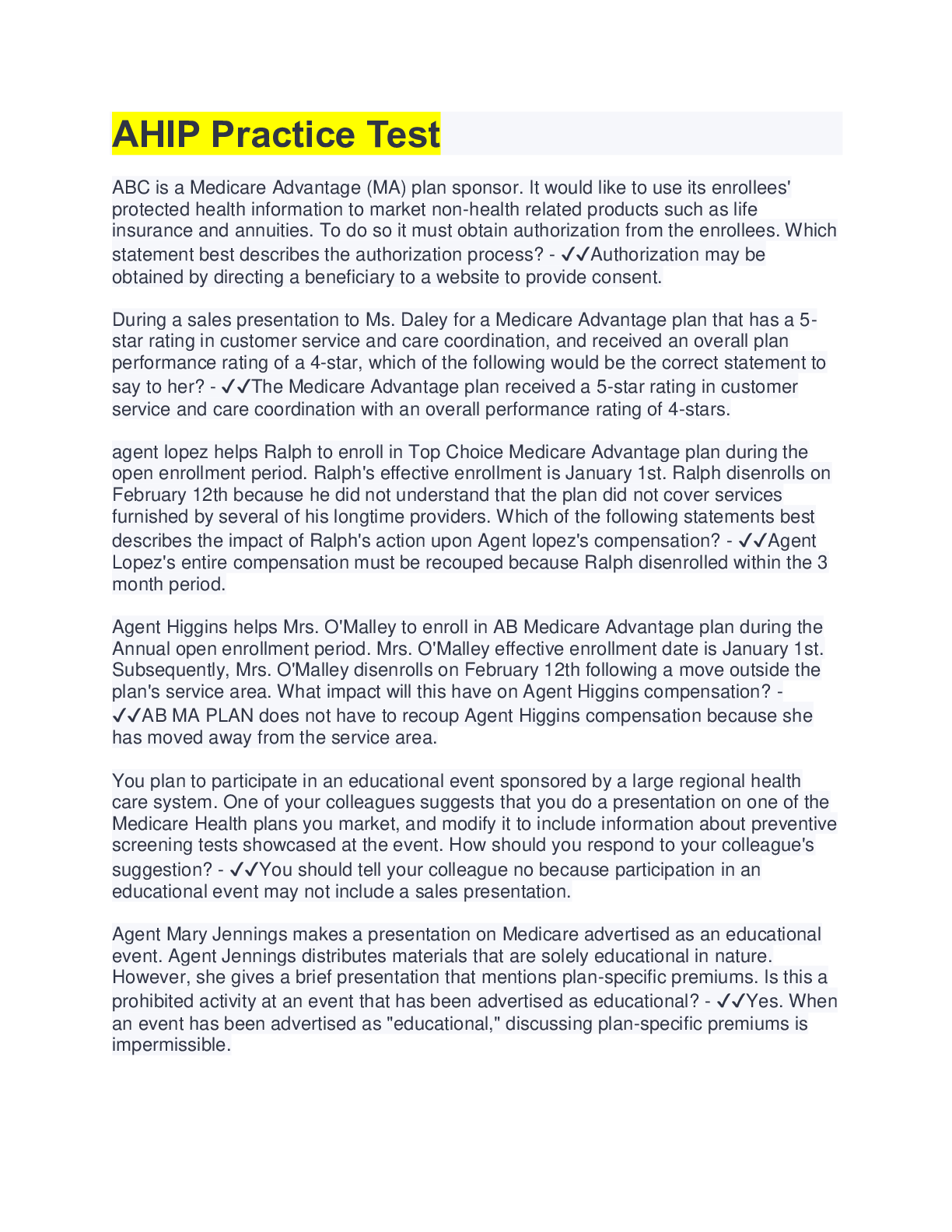
AHIP Practice Test ABC is a Medicare Advantage (MA) plan sponsor. It would like to use its enrollees' protected health information to market non-health related products such as life insurance and a ... nnuities. To do so it must obtain authorization from the enrollees. Which statement best describes the authorization process? - ✔✔Authorization may be obtained by directing a beneficiary to a website to provide consent. During a sales presentation to Ms. Daley for a Medicare Advantage plan that has a 5- star rating in customer service and care coordination, and received an overall plan performance rating of a 4-star, which of the following would be the correct statement to say to her? - ✔✔The Medicare Advantage plan received a 5-star rating in customer service and care coordination with an overall performance rating of 4-stars. agent lopez helps Ralph to enroll in Top Choice Medicare Advantage plan during the open enrollment period. Ralph's effective enrollment is January 1st. Ralph disenrolls on February 12th because he did not understand that the plan did not cover services furnished by several of his longtime providers. Which of the following statements best describes the impact of Ralph's action upon Agent lopez's compensation? - ✔✔Agent Lopez's entire compensation must be recouped because Ralph disenrolled within the 3 month period. Agent Higgins helps Mrs. O'Malley to enroll in AB Medicare Advantage plan during the Annual open enrollment period. Mrs. O'Malley effective enrollment date is January 1st. Subsequently, Mrs. O'Malley disenrolls on February 12th following a move outside the plan's service area. What impact will this have on Agent Higgins compensation? - ✔✔AB MA PLAN does not have to recoup Agent Higgins compensation because she has moved away from the service area. You plan to participate in an educational event sponsored by a large regional health care system. One of your colleagues suggests that you do a presentation on one of the Medicare Health plans you market, and modify it to include information about preventive screening tests showcased at the event. How should you respond to your colleague's suggestion? - ✔✔You should tell your colleague no because participation in an educational event may not include a sales presentation. Agent Mary Jennings makes a presentation on Medicare advertised as an educational event. Agent Jennings distributes materials that are solely educational in nature. However, she gives a brief presentation that mentions plan-specific premiums. Is this a prohibited activity at an event that has been advertised as educational? - ✔✔Yes. When an event has been advertised as "educational," discussing plan-specific premiums is impermissible.What types of tools can Medicare Part D prescription drug plans use that affect the way their enrollees can access medications? - ✔✔Part D plans do not have to cover all medications. As a result, their formularies, or lists of covered drugs, will vary from plan to plan. In addition, they can use cost containment techniques such as tiered copayments and prior authorization. Mrs. Allen has a rare condition for which two different brand name drugs are the only available treatment. She is concerned that since no generic prescription drug is available and these drugs are very high cost, she will not be able to find a Medicare Part D prescription drug plan that covers either one of them. What should you tell her? - ✔✔Medicare prescription drug plans are required to cover drugs in each therapeutic category. She should be able to enroll in a Medicare prescription drug plan that covers the medications she needs. Mr. and Mrs. Vaughn both take a specialized multivitamin prescription each day. Mr. Vaughn takes a prescription for helping to regrow his hair. They are anxious to have their Medicare prescription drug plan cover these drug needs. What should you tell them? - ✔✔Medicare prescription drug plans are not permitted to cover the prescription medications the Vaughns are interested in under Part D coverage, however, plans may cover them as supplemental benefits and the Vaughn's could look into that possibility All plans must cover at least the standard Part D coverage or its actuarial equivalent. What costs would a beneficiary incur for prescription drugs in 2018 under the standard coverage? - ✔✔Standard Part D coverage would require payment of an annual deductible, 25% cost-sharing up to the coverage gap, a portion of costs for both generics and brand-name drugs in the coverage gap, and co-pays or co-insurance after the coverage gap. Mrs. Andrews was preparing a budget for next year because she takes quite a few prescription drugs, she will reach the coverage gap, and wants to be sure she has enough money set aside for those months. She received assistance calculating her projected expenses from her daughter who is a pharmacist, but she doesn't think the calculations are correct because her out-of-pocket expenses would be lower than last year. She calls to ask if you can help. What might you tell her? - ✔✔It would not be unusual for her costs to be a bit less because the Bipartisan Act of 2018 moved up the date for closing the so-called "donut hole" for brand name drugs to 2019. You are mailing invitations to new Medicare beneficiaries for a marketing event. You want an idea of how many people to expect, so you would like to request RSVPs. What should you keep in mind? - ✔✔You may request RSVPs, but you are not permitted to require contact information. Agent Antonio is preparing for a presentation on Medicare and Medicare Advantage before a local senior citizen civic group where he hopes to enroll some attendees. Which of the following steps should he take in order to be in compliance with Medicaremarketing rules? - ✔✔Antonio should include on the invitation a statement that a salesperson will be present with information and applications. Agent Armstrong is employed by XYZ Agency, which is under contract with ABC Health Plan, a Medicare Advantage (MA) plan that offers plans in multiple states. XYZ Agency maintains a website marketing the MA plans with which it has contracts. Agent Armstrong follows up with individuals who request more information about ABC MA plans via the website and tries to persuade them to enroll in ABC plans. What statement best describes the marketing and compliance rules that apply to Agent Armstrong? - ✔✔Agent Armstrong needs to be licensed and appointed in every state in which beneficiaries to whom he markets ABC MA plans are located. Another agent you know has engaged in misconduct that has been verified by the plan she represented. What sort of penalty might the plan impose on this individual? - ✔✔The plan may withhold commission, require retraining, report the misconduct to a state department of insurance or terminate the contract. BestCare Health Plan has received a request from a state insurance department in connection with the investigation of several marketing representatives licensed by the state who sell Medicare Advantage plans. What action(s) should BestCare take in response? - ✔✔Cooperate with the state and supply requested information. Mrs. Burton is in an MA-PD plan and was disappointed in the service she received from her primary care physician because she was told she would have to wait five weeks to get an appointment when she was feeling ill. She called you to ask what she could do so she wouldn't continue to have to put up with such poor access to care. What could you tell her? - ✔✔She could file a grievance with her plan to complain about the lack of timeliness in getting an appointment. Mr. Barker had surgery recently and expected that he would have certain services and items covered by the plan with minimal out-of-pocket costs because his MA-PD coverage has been very good. However, when he received the bill, he was surprised to see large charges in excess of his maximum out-of-pocket limit that included a number of services and items he thought would be fully covered. He called you to ask what he could do? What could you tell him? - ✔✔You can offer to review the plans appeal process to help him ask the plan to review the coverage decision. Mr. Garcia was told he qualifies for a Special Election Period (SEP), but he lost the paper that explains what he could do during the SEP. What can you tell him? - ✔✔If the SEP is for MA coverage, he will generally have one opportunity to change his MA coverage. Mrs. Schmidt is moving and a friend told her she might qualify for a "Special Election Period" to enroll in a new Medicare Advantage plan. She contacted you to ask what a Special Election Period is. What could you tell her? - ✔✔It is a time period, outside ofthe Annual Election Period, when a Medicare beneficiary can select a new or different Medicare Advantage and/or Part D prescription drug plan. Typically the Special Election Period is beneficiary specific and results from events, such as when the beneficiary moves outside of the service area. Mr. Wendt suffers from diabetes which has progressively gotten worse during the last year. He is currently enrolled in Original Medicare (A AND B) and a part D prescription drug plan and did not enroll in a Medicare Advantage plan during the last annual open enrollment period which just closed. Mr. Wendt has heard that there are certain MA plans that might provide him with more specialized coverage for his diabetes and wants to know if he must wait until the next Annual open enrollment period before enrolling in such a plan. What should you tell him? - ✔✔If there is a special needs plan (SNP) in Mr. Wendt's area that specializes in caring for individuals with diabetes, he may enroll in the SNP at any time under a special enrollment period (SEP). Mr. Carlini has heard that Medicare prescription drug plans are only offered through private companies under a program known as Medicare Advantage (MA), not by the government. He likes Original Medicare and does not want to sign up for an MA product, but he also wants prescription drug coverage. What should you tell him? - ✔✔Mr. Carlini can stay with Original Medicare and also enroll in a Medicare prescription drug plan through a private company that has contracted with the government to provide only such drug coverage to eligible Medicare beneficiaries. Mrs. Mulcahy is concerned that she may not qualify for enrollment in a Medicare prescription drug plan because, although she is entitled to Part A, she is not enrolled under Medicare Part B. What should you tell her? - ✔✔Everyone who is entitled to Part A or enrolled under Part B is eligible to enroll in a Medicare prescription drug plan. As long as Mrs. Mulcahy is entitled to Part A, she does not need to enroll under Part B before enrolling in a prescription drug plan. Mrs. Chou likes a PFFS plan available in her area that does not offer drug coverage. She wants to enroll in the plan and enroll in a stand-alone prescription drug plan. What should you tell her? - ✔✔She could enroll in a PFFS plan and a stand-alone Medicare prescription drug plan. Mrs. Walters is enrolled in her state's Medicaid program in addition to Medicare. What should she be aware of when considering enrollment in a Medicare Health Plan? - ✔✔She can enroll in any type of Medicare Advantage plan except an MA medical savings plan MSA Mrs. Lee is discussing with you the possibility of enrolling in a Private Fee-for-Service (PFFS) plan. As part of that discussion, what should you be sure to tell her? - ✔✔PFFS plans may choose to offer part D prescription drug plans but are not required to do so. Ms. Claggett is sixty-six (66) years old. She has been covered under both Parts A and B of Original Medicare for the last six years due to her disability, has never been enrolledin a Medicare Advantage or a Part D plan before. She wants to enroll in a Part D plan. She knows that there is such a thing as the "Part D Initial Enrollment Period" and has concluded that, since she has never enrolled in such a plan before, she should be eligible to enroll under this period. What should you tell her about how the Part D Initial Enrollment Period applies to her situation? - ✔✔It occurs three months before and three months after the month when a beneficiary meets the eligibility requirements for Part B, so she will not be able to use it as a justification for enrolling in a Part D plan now. When Myra first became eligible for Medicare, she enrolled in Original Medicare (Parts A and B). She is now 67 and will turn 68 on July 1. She would now like to enroll in a Medicare Advantage (MA) plan and approaches you about her options. What advice would you give her? - ✔✔She should remain in Original Medicare until the annual election period running from October 15 to December 7, during which she can select an MA plan Daniel is a middle-income Medicare beneficiary. He has chronic bronchitis, putting him at severe risk for pneumonia. Otherwise he has no problems functioning. Which type of SNP is likely to be most appropriate for him? - ✔✔C-SNP Dr. Elizabeth Brennan does not contract with the PFFS plan but accepts the plans terms and conditions for payment, Mary Rodgers sees Dr. Brennan for treatment. How much may Dr. Brennan charge? - ✔✔Dr. Brennan can charge Mary Rodgers no more than the cost sharing specified in the PFFS plan's terms and conditions of payment which may include balance billing up to 15 percent of the Medicare rate. Mr. Sinclair has diabetes and heart trouble and is generally satisfied with the care he has received under Original Medicare, but he would like to know more about Medicare Advantage Special Needs Plans (SNPs). What could you tell him? - ✔✔SNPs have special programs for enrollees with chronic conditions, like Mr. Sinclair, and they provide prescription drug coverage that could be very helpful as well. Mrs. Disraeli is enrolled in Original Medicare (Parts A and B) and a standalone part D prescription drug plan. She has recently developed diabetes and has suffered from heart disease for several years. She has also recently learned that her area is served by a SNP for individuals suffering from a combination of chronic diseases. Mrs. Disraeli is concerned however that she will have few rights or protections if she enrolls in a CSNP. How would you respond? - ✔✔Enrollees in a SNP must have access to provider networks that include enough doctors, specialists, and hospitals to provide to all covered services necessary to meet enrollees need [Show More]
Last updated: 3 years ago
Preview 1 out of 9 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 10, 2022
Number of pages
9
Written in
All
Seller

Reviews Received
Additional information
This document has been written for:
Uploaded
Sep 10, 2022
Downloads
0
Views
102