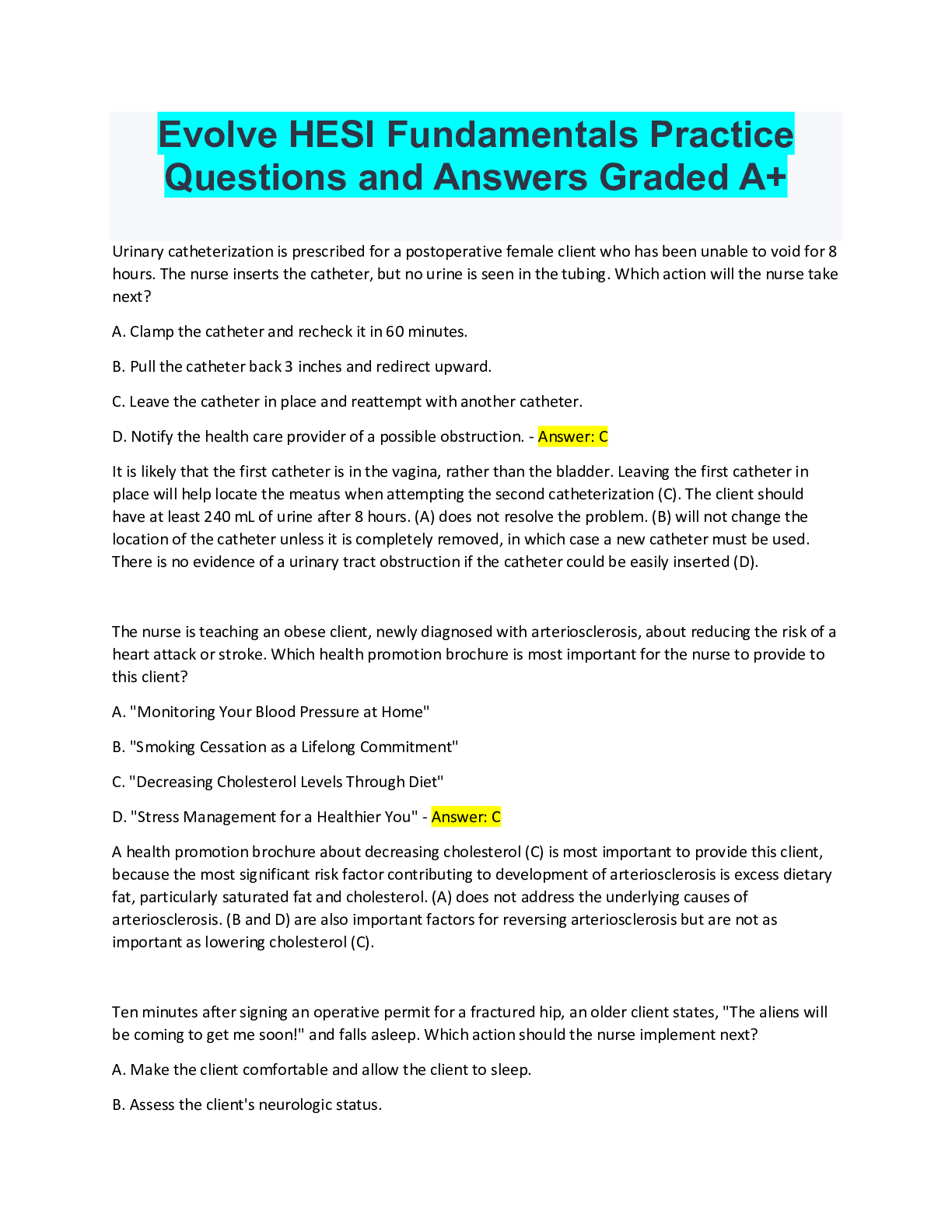
Evolve HESI Fundamentals Practice
Questions and Answers Graded A+
Urinary catheterization is prescribed for a postoperative female client who has been unable to void for 8
hours. The nurse inserts the catheter, but no
...
Evolve HESI Fundamentals Practice
Questions and Answers Graded A+
Urinary catheterization is prescribed for a postoperative female client who has been unable to void for 8
hours. The nurse inserts the catheter, but no urine is seen in the tubing. Which action will the nurse take
next?
A. Clamp the catheter and recheck it in 60 minutes.
B. Pull the catheter back 3 inches and redirect upward.
C. Leave the catheter in place and reattempt with another catheter.
D. Notify the health care provider of a possible obstruction. - Answer: C
It is likely that the first catheter is in the vagina, rather than the bladder. Leaving the first catheter in
place will help locate the meatus when attempting the second catheterization (C). The client should
have at least 240 mL of urine after 8 hours. (A) does not resolve the problem. (B) will not change the
location of the catheter unless it is completely removed, in which case a new catheter must be used.
There is no evidence of a urinary tract obstruction if the catheter could be easily inserted (D).
The nurse is teaching an obese client, newly diagnosed with arteriosclerosis, about reducing the risk of a
heart attack or stroke. Which health promotion brochure is most important for the nurse to provide to
this client?
A. "Monitoring Your Blood Pressure at Home"
B. "Smoking Cessation as a Lifelong Commitment"
C. "Decreasing Cholesterol Levels Through Diet"
D. "Stress Management for a Healthier You" - Answer: C
A health promotion brochure about decreasing cholesterol (C) is most important to provide this client,
because the most significant risk factor contributing to development of arteriosclerosis is excess dietary
fat, particularly saturated fat and cholesterol. (A) does not address the underlying causes of
arteriosclerosis. (B and D) are also important factors for reversing arteriosclerosis but are not as
important as lowering cholesterol (C).
Ten minutes after signing an operative permit for a fractured hip, an older client states, "The aliens will
be coming to get me soon!" and falls asleep. Which action should the nurse implement next?
A. Make the client comfortable and allow the client to sleep.
B. Assess the client's neurologic status.C. Notify the surgeon about the comment.
D. Ask the client's family to co-sign the operative permit. - Answer: B
This statement may indicate that the client is confused. Informed consent must be provided by a
mentally competent individual, so the nurse should further assess the client's neurologic status (B) to be
sure that the client understands and can legally provide consent for surgery. (A) does not provide
sufficient follow-up. If the nurse determines that the client is confused, the surgeon must be notified (C)
and permission obtained from the next of kin (D).
The nurse-manager of a skilled nursing (chronic care) unit is instructing UAPs on ways to prevent
complications of immobility. Which intervention should be included in this instruction?
A. Perform range-of-motion exercises to prevent contractures.
B. Decrease the client's fluid intake to prevent diarrhea.
C. Massage the client's legs to reduce embolism occurrence.
D. Turn the client from side to back every shift. - Answer: A
Performing range-of-motion exercises (A) is beneficial in reducing contractures around joints. (B, C, and
D) are all potentially harmful practices that place the immobile client at risk of complications.
The nurse is assisting a client to the bathroom. When the client is 5 feet from the bathroom door, he
states, "I feel faint." Before the nurse can get the client to a chair, the client starts to fall. Which is the
priority action for the nurse to take?
A. Check the client's carotid pulse.
B. Encourage the client to get to the toilet.
C. In a loud voice, call for help.
D. Gently lower the client to the floor. - Answer: D
(D) is the most prudent intervention and is the priority nursing action to prevent injury to the client and
the nurse. Lowering the client to the floor should be done when the client cannot support his own
weight. The client should be placed in a bed or chair only when sufficient help is available to prevent
injury. (A) is important but should be done after the client is in a safe position. Because the client is not
supporting himself, (B) is impractical. (C) is likely to cause chaos on the unit and might alarm the other
clients.
A female nurse is assigned to care for a close friend, who says, "I am worried that friends will find out
about my diagnosis." The nurse tells her friend that legally she must protect a client's confidentiality.
Which resource describes the nurse's legal responsibilities?A. Code of Ethics for Nurses
B. State Nurse Practice Act
C. Patient's Bill of Rights
D. ANA Standards of Practice - Answer: B
The State Nurse Practice Act (B) contains legal requirements for the protection of client confidentiality
and the consequences for breaches in confidentiality. (A) outlines ethical standards for nursing care but
does not include legal guidelines. (C and D) describe expectations for nursing practice but do not
address legal implications.
The nurse is teaching a client how to perform progressive muscle relaxation techniques to relieve
insomnia. A week later the client reports that he is still unable to sleep, despite following the same
routine every night. Which action should the nurse take first?
A. Instruct the client to add regular exercise as a daily routine.
B. Determine if the client has been keeping a sleep diary.
C. Encourage the client to continue the routine until sleep is achieved.
D. Ask the client to describe the routine that the client is currently following. - Answer: D
The nurse should first evaluate whether the client has been adhering to the original instructions (D). A
verbal report of the client's routine will provide more specific information than the client's written diary
(B). The nurse can then determine which changes need to be made (A). The routine practiced by the
client is clearly unsuccessful, so encouragement alone is insufficient (C).
A 65-year-old client who attends an adult daycare program and is wheelchair-mobile has redness in the
sacral area. Which instruction is most important for the nurse to provide?
A. Take a vitamin supplement tablet once a day.
B. Change positions in the chair at least every hour.
C. Increase daily intake of water or other oral fluids.
D. Purchase a newer model wheelchair. - Answer: B
The most important teaching is to change positions frequently (B) because pressure is the most
significant factor related to the development of pressure ulcers. Increased vitamin and fluid intake (A
and C) may also be beneficial promote healing and reduce further risk. (D) is an intervention of last
resort because this will be very expensive for the client.When turning an immobile bedridden client without assistance, which action by the nurse best ensures
client safety?
A. Securely grasp the client's arm and leg.
B. Put bed rails up on the side of bed opposite from the nurse.
C. Correctly position and use a turn sheet.
D. Lower the head of the client's bed slowly. - Answer: B
Because the nurse can only stand on one side of the bed, bed rails should be up on the opposite side to
ensure that the client does not fall out of bed (B). (A) can cause client injury to the skin or joint. (C and
D) are useful techniques while turning a client but have less priority in terms of safety than use of the
bed rails.
A female client with frequent urinary tract infections (UTIs) asks the nurse to explain her friend's advice
about drinking a glass of juice daily to prevent future UTIs. Which response is best for the nurse provide?
A. Orange juice has vitamin C that deters bacterial growth.
B. Apple juice is the most useful in acidifying the urine.
C. Cranberry juice stops pathogens' adherence to the bladder.
D. Grapefruit juice increases absorption of most antibiotics. - Answer: C
Cranberry juice (C) maintains urinary tract health by reducing the adherence of Escherichia coli bacteria
to cells within the bladder. (A, B, and D) have not been shown to be as effective as cranberry juice (C) in
preventing UTIs.
The nurse is aware that malnutrition is a common problem among clients served by a community health
clinic for the homeless. Which laboratory value is the most reliable indicator of chronic protein
malnutrition?
A. Low serum albumin level
B. Low serum transferrin level
C. High hemoglobin level
D. High cholesterol level - Answer: A
Long-term protein deficiency is required to cause significantly lowered serum albumin levels (A).
Albumin is made by the liver only when adequate amounts of amino acids (from protein breakdown) are
available. Albumin has a long half-life, so acute protein loss does not significantly alter serum levels. (B)
is a serum protein with a half-life of only 8 to 10 days, so it will drop with an acute protein deficiency.
Neither (C or D) are clinical measures of protein malnutrition.The nurse identifies a potential for infection in a patient with partial-thickness (second-degree) and fullthickness (third-degree) burns. What intervention has the highest priority in decreasing the client's risk
of infection?
A. Administration of plasma expanders
B. Use of careful hand washing technique
C. Application of a topical antibacterial cream
D. Limiting visitors to the client with burns - Answer: B
Careful hand washing technique (B) is the single most effective intervention for the prevention of
contamination to all clients. (A) reverses the hypovolemia that initially accompanies burn trauma but is
not related to decreasing the proliferation of infective organisms. (C and D) are recommended by
various burn centers as possible ways to reduce the chance of infection. (B) is a proven technique to
prevent infection.
Which serum laboratory value should the nurse monitor carefully for a client who has a nasogastric (NG)
tube to suction for the past week?
A. White blood cell count
B. Albumin
C. Calcium
D. Sodium - Answer: D
Monitoring serum sodium levels (D) for hyponatremia is indicated during prolonged NG suctioning
because of loss of fluids. Changes in levels of (A, B, or C) are not typically associated with prolonged NG
suctioning.
In completing a client's preoperative routine, the nurse finds that the operative permit is not signed. The
client begins to ask more questions about the surgical procedure. Which action should the nurse take
next?
A. Witness the client's signature to the permit.
B. Answer the client's questions about the surgery.
C. Inform the surgeon that the operative permit is not signed and the client has questions about the
surgery.
D. Reassure the client that the surgeon will answer any questions before the anesthesia is administered.
- Answer: CThe surgeon should be informed immediately that the permit is not signed (C). It is the surgeon's
responsibility to explain the procedure to the cliesxnt and obtain the client's signature on the permit.
Although the nurse can witness an operative permit (A), the procedure must first be explained by the
health care provider or surgeon, including answering the client's questions (B). The client's questions
should be addressed before the permit is signed (D).
The nurse is preparing an older client for discharge. Which method is best for the nurse to use when
evaluating the client's ability to perform a dressing change at home?
A. Determine how the client feels about changing the dressing.
B. Ask the client to describe the procedure in writing.
C. Seek a family member's evaluation of the client's ability to change the dressing.
D. Observe the client change the dressing unassisted. - Answer: D
Observing the client directly (D) will allow the nurse to determine if mastery of the skill has been
obtained and provide an opportunity to affirm the skill. (A) may be therapeutic but will not provide an
opportunity to evaluate the client's ability to perform the procedure. (B) may be threatening to an older
client and will not determine his ability. (C) is not as effective as direct observation by the nurse.
A client in a long-term care facility reports to the nurse that he has not had a bowel movement in 2 days.
Which intervention should the nurse implement first?
A. Instruct the caregiver to offer a glass of warm prune juice at mealtimes.
B. Notify the health care provider and request a prescription for a large-volume enema.
C. Assess the client's medical record to determine the client's normal bowel pattern.
D. Instruct the caregiver to increase the client's fluids to five 8-ounce glasses per day. - Answer: C
This client may not routinely have a daily bowel movement, so the nurse should first assess this client's
normal bowel habits before attempting any intervention (C). (A, B, or D) may then be implemented, if
warranted.
The nurse is instructing a client with cholecystitis regarding diet choices. Which meal best meets the
dietary needs of this client?
A. Steak, baked beans, and a salad
B. Broiled fish, green beans, and an apple
C. Pork chops, macaroni and cheese, and grapes
D. Avocado salad, milk, and angel food cake - Answer: BClients with cholecystitis (inflammation of the gallbladder) should follow a low-fat diet, such as (B). (A) is
a high-protein diet and (C and D) contain high-fat foods, which are contraindicated for this client.
When bathing an uncircumcised boy older than 3 years, which action should the nurse take?
A. Remind the child to clean his genital area.
B. Defer perineal care because of the child's age.
C. Retract the foreskin gently to cleanse the penis.
D. Ask the parents why the child is not circumcised. - Answer: C
The foreskin (prepuce) of the penis should be gently retracted to cleanse all areas that could harbor
bacteria (C). The child's cognitive development may not be at the level at which (A) would be effective.
Perineal care needs to be provided daily regardless of the client's age (B). (D) is not indicated and may
be perceived as intrusive.
The nurse who is preparing to give an adolescent client a prescribed antipsychotic medication notes that
parental consent has not been obtained. Which action should the nurse take?
A. Review the chart for a signed consent for hospitalization.
B. Get the health care provider's permission to give the medication.
C. Do not give the medication and document the reason.
D. Complete an incident report and notify the parents. - Answer: C
The nurse should not give the medication and should document the reason (C) because the client is a
minor and needs a guardian's permission to receive medications. Permission to give medications is not
granted by a signed hospital consent (A) or a health care provider's permission (B), unless conditions are
met to justify coerced treatment. (D) is not necessary unless the medication had previously been
administered.
A nurse is working in an occupational health clinic when an employee walks in and states that he was
struck by lightning while working in a truck bed. The client is alert but reports feeling faint. Which
assessment will the nurse perform first?
A. Pulse characteristics
B. Open airway
C. Entrance and exit wounds
D. Cervical spine injury - Answer: ALightning is a jolt of electrical current and can produce a "natural" defibrillation, so assessment of the
pulse rate and regularity (A) is a priority. Because the client is talking, he has an open airway (B), so that
assessment is not necessary. Assessing for (C and D) should occur after assessing for adequate
circulation.
The mental health nurse plans to discuss a client's depression with the health care provider in the
emergency department. There are two clients sitting across from the emergency department desk.
Which nursing action is best?
A.
Only refer to the client by gender.
B.
Identify the client only by age.
C.
Avoid using the client's name.
D.
Discuss the client another time. - Answer: D
The best nursing action is to discuss the client another time (D). Confidentiality must be observed at all
times, so the nurse should not discuss the client when the conversation can be overheard by others.
Details can identify the client when referring to the client by gender (A) or age (B), and even when not
using the client's name (C).
The nurse is assessing several clients prior to surgery. Which factor in a client's history poses the
greatest threat for complications to occur during surgery?
A. Taking birth control pills for the past 2 years
B. Taking anticoagulants for the past year
C. Recently completing antibiotic therapy
D. Having taken laxatives PRN for the last 6 months - Answer: BAnticoagulants (B) increase the risk for bleeding during surgery, which can pose a threat for the
development of surgical complications. The health care provider should be informed that the client is
taking these drugs. Although clients who take birth control pills (A) may be more susceptible to the
development of thrombi, such problems usually occur postoperatively. A client with (C or D) is at less of
a surgical risk than (B).
When assisting a client from the bed to a chair, which procedure is best for the nurse to follow?
A. Place the chair parallel to the bed, with its back toward the head of the bed and assist the client in
moving to the chair.
B. With the nurse's feet spread apart and knees aligned with the client's knees, stand and pivot the
client into the chair.
C. Assist the client to a standing position by gently lifting upward, underneath the axillae.
D. Stand beside the client, place the client's arms around the nurse's neck, and gently move the client to
the chair. - Answer: B
(B) describes the correct positioning of the nurse and affords the nurse a wide base of support while
stabilizing the client's knees when assisting to a standing position. The chair should be placed at a 45-
degree angle to the bed, with the back of the chair toward the head of the bed (A). Clients should never
be lifted under the axillae (C); this could damage nerves and strain the nurse's back. The client should be
instructed to use the arms of the chair and should never place his or her arms around the nurse's neck
(D); this places undue stress on the nurse's neck and back and increases the risk for a fall.
The nurse is instructing a client in the proper use of a metered-dose inhaler. Which instruction should
the nurse provide the client to ensure the optimal benefits from the drug?
A. "Fill your lungs with air through your mouth and then compress the inhaler."
B. "Compress the inhaler while slowly breathing in through your mouth."
C. "Compress the inhaler while inhaling quickly through your nose."
D. "Exhale completely after compressing the inhaler and then inhale." - Answer: B
The medication should be inhaled through the mouth simultaneously with compression of the inhaler
(B). This will facilitate the desired destination of the aerosol medication deep in the lungs for an optimal
bronchodilation effect. (A, C, and D) do not allow for deep lung penetration.
The nurse finds a client crying behind a locked bathroom door. The client will not open the door. Which
action should the nurse implement first?
A. Instruct an unlicensed assistive personnel (UAP) to stay and keep talking to the client.B. Sit quietly in the client's room until the client leaves the bathroom.
C. Allow the client to cry alone and leave the client in the bathroom.
D. Talk to the client and attempt to find out why the client is crying. - Answer: D
The nurse's first concern should be for the client's safety, so an immediate assessment of the client's
situation is needed (D). (A) is incorrect; the nurse should implement the intervention. The nurse may
offer to stay nearby after first assessing the situation more fully (B). Although (C) may be correct, the
nurse should determine if the client's safety is compromised and offer assistance, even if it is refused.
Which step(s) should the nurse take when administering ear drops to an adult client? (Select all that
apply.)
A. Place the client in a side-lying position.
B. Pull the auricle upward and outward.
C. Hold the dropper 6 cm above the ear canal.
D. Place a cotton ball into the inner canal.
E. Pull the auricle down and back. - Answer: A, B
The correct answers (A and B) are the appropriate administration of ear drops. The dropper should be
held 1 cm (½ inch) above the ear canal (C). A cotton ball should be placed in the outermost canal (D).
The auricle is pulled down and back for a child younger than 3 years of age, but not an adult (E).
The nurse is using the Glasgow Coma Scale to perform a neurologic assessment. A comatose client
winces and pulls away from a painful stimulus. Which action should the nurse take next?
A. Document that the client responds to painful stimulus.
B. Observe the client's response to verbal stimulation.
C. Place the client on seizure precautions for 24 hours.
D. Report decorticate posturing to the health care provider. - Answer: A
The client has demonstrated a purposeful response to pain, which should be documented as such (A).
Response to painful stimulus is assessed after response to verbal stimulus, not before (B). There is no
indication for placing the client on seizure precautions (C). Reporting (D) is nonpurposeful movement.
A hospitalized client has had difficulty falling asleep for 2 nights and is becoming irritable and restless.
Which action by the nurse is best?
A. Determine the client's usual bedtime routine and include these rituals in the plan of care as safety
allows.B. Instruct the UAP not to wake the client under any circumstances during the night.
C. Place a "Do Not Disturb" sign on the door and change assessments from every 4 to every 8 hours.
D. Encourage the client to avoid pain medication during the day, which might increase daytime napping.
- Answer: A
Including habitual rituals that do not interfere with the client's care or safety may allow the client to go
to sleep faster and increase the quality of care (A). (B, C, and D) decrease the client's standard of care
and compromise safety.
While reviewing the side effects of a newly prescribed medication, a 72-year-old client notes that one of
the side effects is a reduction in sexual drive. Which is the best response by the nurse?
A. "How will this affect your present sexual activity?"
B. "How active is your current sex life?"
C. "How has your sex life changed as you have become older?"
D. "Tell me about your sexual needs as an older adult." - Answer: A
(A) offers an open-ended question most relevant to the client's statement. (B) does not offer the client
the opportunity to express concerns. (C and D) are even less relevant to the client's statement.
The health care provider has changed a client's prescription from the PO to the IV route of
administration. The nurse should anticipate which change in the pharmacokinetic properties of the
medication?
A. The client will experience increased tolerance to the drug's effects and may need a higher dose.
B. The onset of action of the drug will occur more rapidly, resulting in a more rapid effect.
C. The medication will be more highly protein-bound, increasing the duration of action.
D. The therapeutic index will be increased, placing the client at greater risk for toxicity. - Answer: B
Because the absorptive process is eliminated when medications are administered via the IV route, the
onset of action is more rapid, resulting in a more immediate effect (B). Drug tolerance (A), protein
binding (C), and the drug's therapeutic index (D) are not affected by the change in route from PO to IV.
In addition, an increased therapeutic index reduces the risk of drug toxicity.
A male client is laughing at a television program with his wife when the evening nurse enters the room.
He says his foot is hurting and he would like a pain pill. How should the nurse respond?
A. Ask him to rate his pain on a scale of 1 to 10.
B. Encourage him to wait until bedtime so the pill can help him sleep.C. Attend to an acutely ill client's needs first because this client is laughing.
D. Instruct him in the use of deep breathing exercises for pain control. - Answer: A
Obtaining a subjective estimate of the pain experience by asking the client to rate his pain (A) helps the
nurse determine which pain medication should be administered and also provides a baseline for
evaluating the effectiveness of the medication. Medicating for pain should not be delayed so that it can
be used as a sleep medication (B). (C) is judgmental. (D) should be used as an adjunct to pain
medication, not instead of medication.
The nurse determines that a postoperative client's respiratory rate has increased from 18 to 24
breaths/min. Based on this assessment finding, which intervention is most important for the nurse to
implement?
A. Encourage the client to increase ambulation in the room.
B. Offer the client a high-carbohydrate snack for energy.
C. Force fluids to thin the client's pulmonary secretions.
D. Determine if pain is causing the client's tachypnea. - Answer: D
Pain, anxiety, and increasing fluid accumulation in the lungs (D) can cause tachypnea (increased
respiratory rate). Encouraging (A) when the respiratory rate is rising above normal limits puts the client
at risk for further oxygen desaturation. (B) can increase the client's carbon metabolism, so an alternative
source of energy, such as Pulmocare liquid supplement, should be offered instead. (C) could increase
respiratory congestion in a client with a poorly functioning cardiopulmonary system, placing the client at
risk of fluid overload.
A 20-year-old female client with a noticeable body odor has refused to shower for the last 3 days. She
states, "I have been told that it is harmful to bathe during my period." Which action should the nurse
take first?
A. Accept and document the client's wish to refrain from bathing.
B. Offer to give the client a bed bath, avoiding the perineal area.
C. Obtain written brochures about menstruation to give to the client.
D. Teach the importance of personal hygiene during menstruation with the client. - Answer: D
Because a shower is most beneficial for the client in terms of hygiene, the client should receive teaching
first (D), respecting any personal beliefs such as cultural or spiritual values. After client teaching, the
client may still choose (A or B). Brochures reinforce the teaching (C).Based on the nursing diagnosis of Risk for infection, which intervention is best for the nurse to
implement when providing care for an older incontinent client?
A. Maintain standard precautions.
B. Initiate contact isolation measures.
C. Insert an indwelling urinary catheter.
D. Instruct client in the use of adult diapers. - Answer: A
The best action to decrease the risk of infection in vulnerable clients is hand washing (A). (B) is not
necessary unless the client has an infection. (C) incre
[Show More]