NR602 MIDTERM study guide
Document Content and Description Below
MIDTERM STUDY GUIDE: PART-1
TOPICS Covered
o Chalazions
o Blepharitis
o Conjunctivitis
o Hand-foot-mouth syndrome
o Strep pharyngitis
o Kawasaki disease
o Rheumatic fever
o Milia
o Port-wine
...
stain/Nevus flammeus
o Salmon patch
o Café-au lait spot
o Impetigo
o Molluscum Contagiosum
o Verruca Vulgaris
o Herpetic Whitlow
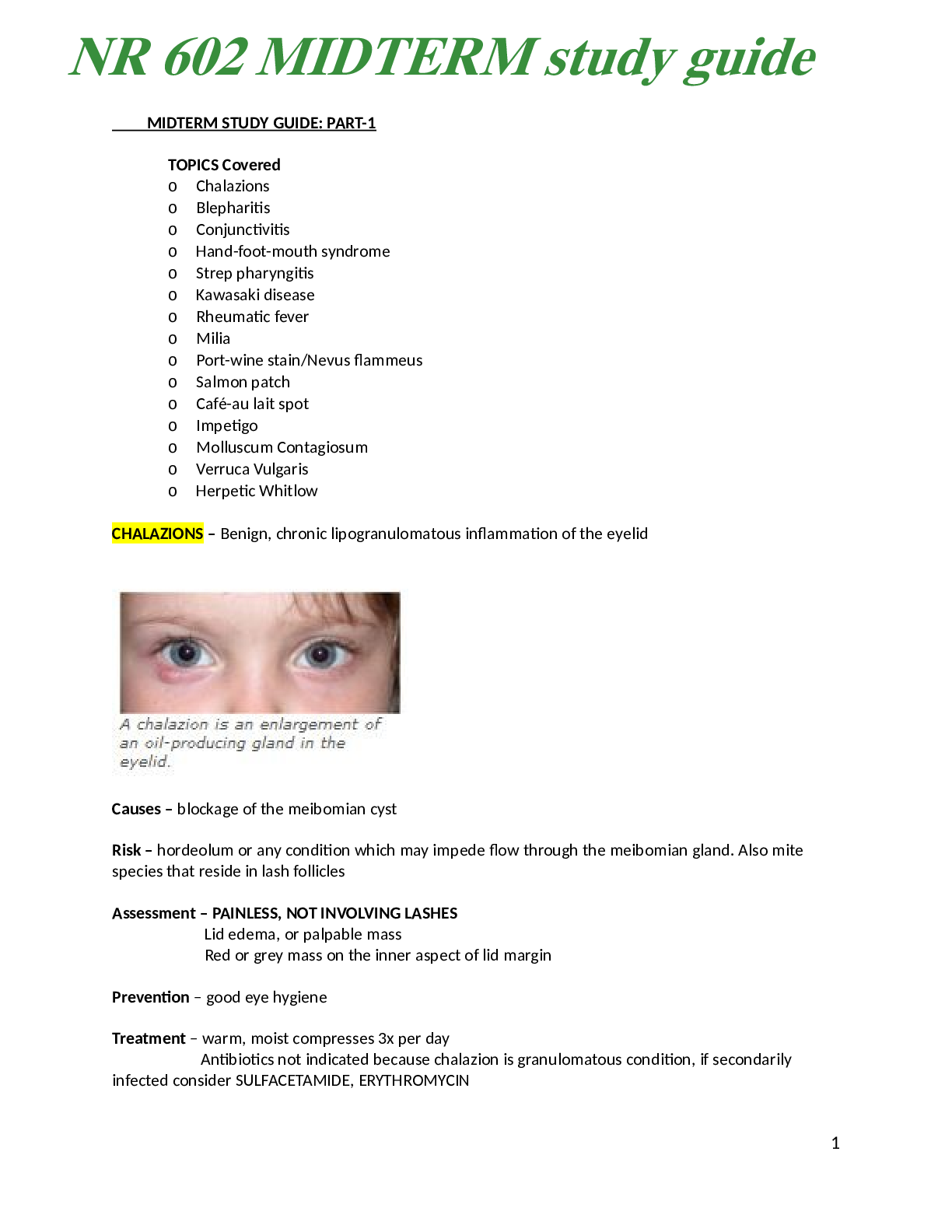
CHALAZIONS – Benign, chronic lipogranulomatous inflammation of the eyelid
Causes – blockage of the meibomian cyst
Risk – hordeolum or any condition which may impede flow through the meibomian gland. Also mite
species that reside in lash follicles
Assessment – PAINLESS, NOT INVOLVING LASHES
Lid edema, or palpable mass
Red or grey mass on the inner aspect of lid margin
Prevention – good eye hygiene
Treatment – warm, moist compresses 3x per day
Antibiotics not indicated because chalazion is granulomatous condition, if secondarily
infected consider SULFACETAMIDE, ERYTHROMYCIN
1
NR 602 MIDTERM study guide
Follow up – 2-4 weeks, if still present after 6 weeks follow up with ophthalmologist
BLEPHARITIS – Inflamation/infection of the lid margins (chronic problem)
2 types – seborrheic (non ulcerative) : irritants (smoke, make up, chemicals)
s&s – chronic inflammation of the eyelid, erythema, greasy scaling of anterior eyelid,
loss of eyelashes, seborrhea dermatitis of eyebrows and scalp
Ulcerative- infection with staphylococcus or streptococcus
s&s – itching, tearing, recurrent styes, chalazia, photophobia, small
ulceration at eyelid margin, broken or absent eyelashes
● the most frequent complaint is ongoing eye irritation and conjunctiva redness
Treatment – clean with baby shampoo 2-4 times a day, warm compresses, lid massage (right after warm
compress)
For infected eyelids – antistaphyloccocal antibiotics BACITRACIN, ERYTHROMYCIN 0.05% for 1 week AND
QUIONOLONE OINTMENTS
For infection resistant to topical – TETRACYCLINE 250 MG PO X4
DOXYCYCLINE 100 MG PO X2
CONJUCTIVITIS – inflammation or irritation of conjuctiva
Bacterial (PINK EYE) – in peds bacteria is the mosts common cause, contact lens, rubbing eyes, trauma,
S&S – purulent exudate, initially unilateral, then bilateral
2
Sensation of having foreign body in the eye is common
Key findings – redness, yellow green, puru,ent discharge, crust and matted eyelids in am
Self limiting 5-7 days. Eye drops – polytrim, erythromycin, tobramycin or cipro
Improvement 2-4 days
Most common organism H. influenza <7
Viral – adenovirus, coxsackie virus, herpes, molluscum
S&S – profuse tearing, mucous discharge, burning, concurrent URI, enlarged or tender
preauricular nose
Antihistamines/decongestant
Improvement, self limiting, 7-14 days
Chlamydial – chlamydia trachomatis
S&S – profuse exudate, associated with genitourinary symptoms, 1-2 weeks after birth
Gonococcal – 2-4 days after birth, most concern can cause blidness
PO azithromycin, doxycycline (tetracyclines increase photosensitivity, don’t use in pregnancy)
Improvement 2-3 weeks
Allergic – IgE mast cell reaction, environmental, cosmetics
S&S – marked conjuctival edema, severe itching, tearing, sneezing
Topical antihistamine or topical steroids
Improvement 2-3 days
Chemical –thimerosal, erythromycin, silver nitrate
S&S conjuctival erythema, 30 minutes afer prophylactic antibiotics drops
Avoid contact
Can consider steroids
Conjunctivitis never accompany vision changes
Diagnostic studies: swap and scraping must be done, gram and Giemsa staining, ELISA, PCR testing,
newborn < 2 weeks needs to be tested for gonorrhea
Non –pharm – clean towels, change pillows, warm compress, no contacts, no eye make up – mascara
Gonococcal conjunctivitis: newborn – give Ceftriaaxone IM once (don’t give if hyperbilirubinemia,
Non-gonococcal – erythromycin 0.5% ointment
Consider fluorescein staining if abrasion suspected
CDC recommends prophylactic administration of antibiotic eye ointment (ERYTHROMYCIN) 1 hour after
delivery
Refer to ophthalmologist if herpes, hemorrhagic conjunctivitis or ulcerations present
May return to work/school 24 hours after topical
HAND-FOOT-AND-MOUTH DISEASE – HIGHLY CONTAGIOUS, viral illness
3
clinical entity evidenced by fever, vesicular eruptions in the oropharynx that may ulcerate and a
maculopapular rash involving hands and feet, the rash evolves to vesicles, especially on the dorsa of the
hands and feet. Last 1 to 2 weeks.
lesions appear on the buccal mucosa, palate, palms of hands, soles of feet and buttocs
most common cause – COXSACKIE A 16
common in children <5
S&S – low grade fever, malaise, abdominal pain, enlarged anterior cervical nodes or submandibular
Oral – small red papules on the tongue and buccal mucosa, which will progress to ulcerative vesicles
EXANTHEM (papulovesicular) – occurs 1-2 days after oral lesions
Differential – herpangina, Stevens- Johnson syndrome
Treatment – maintain hydration, cool liquids, avoid spicy food, rest
Topical aluminum hydroxide/ magnesium hydroxide gel with diphenhydramine applied to painful lesions
Topical anesthetics – Kank A, Orabase
Resolution with 7 days
STREP PHARYNGITIS – An acute inflam
[Show More]
Last updated: 3 years ago
Preview 1 out of 66 pages







.png)