Pathophysiology > HESI > HESI PATHOPHYSIOLOGY TEST BANK 27 LATEST VERSIONS VERIFIED QUESTIONS AND ANSWERS AND STUDY S (All)
HESI PATHOPHYSIOLOGY TEST BANK 27 LATEST VERSIONS VERIFIED QUESTIONS AND ANSWERS AND STUDY SETSS BEST DOCUMENT FOR EXAM PREPARATION 100% SATISFACTION GUARANTEED COMPLETE AND LATEST GUIDE FOR ATI NUTRITION 2022 1000+ Questions with answers Hesi Pathophysiology Practice Exam Questions with answers, rated A. 2022/2023
Document Content and Description Below
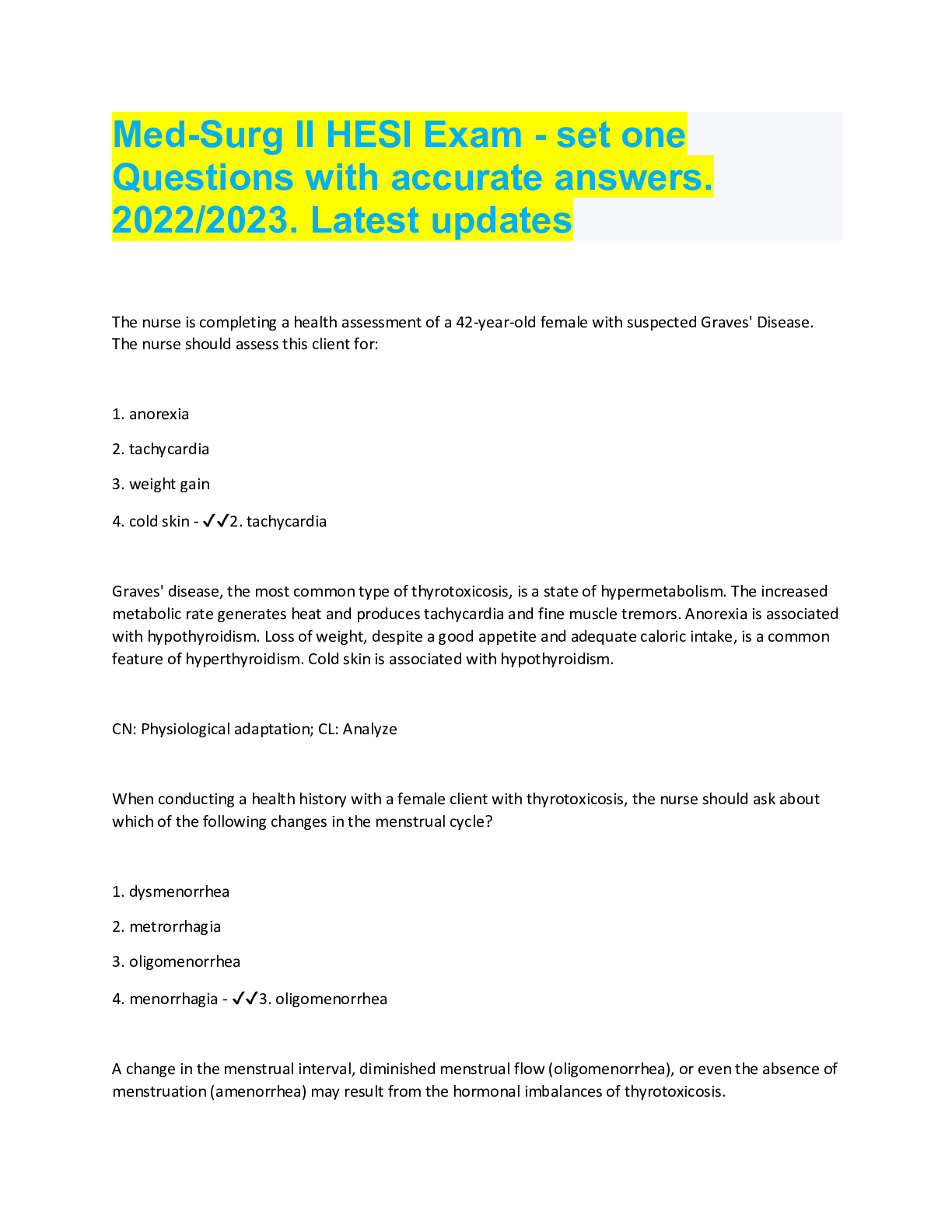
HESI PATHOPHYSIOLOGY TEST BANK 27 LATEST VERSIONS VERIFIED QUESTIONS AND ANSWERS AND STUDY SETSS BEST DOCUMENT FOR EXAM PREPARATION 100% SATISFACTION GUARANTEED COMPLETE AND LATE... ST GUIDE FOR ATI NUTRITION 2022 1000+ Questions with answers Hesi Pathophysiology Practice Exam Questions with answers, rated A. 2022/2023 After talking w/ the HCP, a male pt continues to have questions about the results of a prostatic surface antigen (PSA) screening test and asks the nurse how the PSA levels become elevated. The nurse should explain which pathophysiological mechanism? - ✔✔As the prostate gland enlarges, its cells contribute more PSA in the circulating blood PSA is a glycoprotein found in prostatic epithelial cells, and elevations are used as a specific tumor markers. Elevations in PSA are r/t gland volume, ie. benign BPH, prostatitis, and cancer of the prostate, indicating tumor cell load. PSA levels are also used to monitor response to therapy A 26 yr old male client w/ Hodgkin's disease is scheduled to undergo radiation therapy. The clinet expresses concern about the effect of radiation on his ability to have children. What info should the nurse provide? - ✔✔Permanent sterility occurs in the male client who receive radiation Low sperm count and loss of motility are seen in males w/ Hodgkin's disease b/f any therapy. Radiotherapy often results in permanent aspermia, or sterility The nurse hears short, high-pitched sounds just b/f the end of inspiration in the right and left lower lobes when auscultating a client's lungs. How should this finding be recorded? - ✔✔Crackles in the right and left lower lobes Fine crackles - short, high-pitched sounds heard just b/f the end of inspiration that are the result of rapid equalization of pressure when collaped alveoli or terminal bronchioles suddenly snap open Wheezing is a continuous high-pitched squeaking or musical sound caused by rapid vibration of bronchial walls that are 1st evident on expiration and may be audible A client is admitted to the ER w/ a tension pneumothorax. Which assessment should the nurse expect to ID? - ✔✔A deviation of the trachea toward the side opposite of the pneumothorax Tension pneumothorax is caused by rapid accumulation of air in the pleural space, causing severely high intrapleural pressure. This results in collapse of the lung, and the mediastinum shifts toward the unaffected side, which is subsequently compressed A client who is receiving a whole blood transfusion dv's chills, fever, and a HA 30 min after the transfusion is started. The nurse shold recognize these sx as characteristic of what rxn? - ✔✔A febrile transfusion reaction Sx of a febrile reaction include sudden chills, fever, HA, flushing, and muscle pain. An allergic rxn is the response of histamine release which is characterized by flushing, itching, and urticaria. It exhibits an exaggerated allergic response that progresses to shock and possible cardiac arrest an acute hemolytic reaction presents w/ fever, chills, but is hallmarked by the onset of low back pain, tachycardia, tachypnea, vascular collapse, hemoglobinuria, dark urine, ARF, shock, cardiac arrest, and even death The nurse is analyzing the waveforms of a client's ECG. What finding indicates a disturbance in electrical conduction in the ventricles? - ✔✔QRS interval of 0.14 second the normal duration of the QRS is 0.04 - 0.12 sec T wave is 0.16 sec; PR is 0.12 - 0.20 sec; QT is 0.31-0.38 sec Several hrs after surgical repair of an AAA, the client dvps left flank pain. the nurse determines the client's urinary output is 20 m.;hr for the past 2 hrs. The nurse should conclude that these findings support which complication? - ✔✔Renal artery embolization Post-op complications of surgical repair of AAA are r/t the location of resection, graft, or stent placement along the abd'l aorta. Embolization of a fragment of thrombus or plaque from the aorta into a renal artery can compromise blood flow in 1 of the renal arteries, resulting in renal ischemia that precipitates unilateral flank pain A client w/ markedly distended bladder is dx w/ hydronephroosis and left hydroureter after an IV pyelogram. The nurse catheterizes the client and obtains a residual urine vol of 1650 ml. this finding supports which pathophysiological cause of the client's urinary tract obstruction? - ✔✔Obstruction at the urinary bladder neck Hydroureter (dilation of the renal pelvis), vesicoureteral reflux (backward mvmt of urine from the lower to upper urinary tracts), and hydronephrosis (dilation or enlargement of the renal pelvis and calyces) result from post-renal obstruction which can consequently result in chronic pyelonephritis and renal atrophy. Ascending urinary reflux occurs when normal ureteral peristaltic pressure is met w/ an increase in urinary pressure occurring during bladder filling if the urinary bladder neck is obstructed The nurse is planning care for a client who has a right hemispheric stroke. Which nsg dx should the nurse include in the POC? - ✔✔Risk for injury r/t denial of deficits and impulsiveness Right-brain damage - a client experience difficulty in judgment and spatial perception and is more likely to be impulsive and move quickly, which placing the client at risk for falls the nurse is teaching a client w/ maple syrup urine disease, an autosomal recessive DO about the inheritance pattern. Which info should the nurse provide? - ✔✔both genes of a pair must be abnormal for the DO to occur A female client tells the nurse that she does not know which day of the month is best to do breast self exams. Which instruction should the nurse provide? - ✔✔5-7 days after menses cease this is because the physiologic alterations in breast size and activity reach their minimal level after menses A client reports unprotected sex 1 wk ago and is worried about HIV exposure. An initial HIV antibody screen (ELISA) is obtained. The nurse teaches the client that seroconversion to HIV positive relies on antibody production by B lymphocytes after exposure to the virus. When should the nurse recommend the client return for repeat blood testing? - ✔✔6-12 wks although the HIV antigen is detectable appx 2 wks after exposure, seroconversion to HIV positive may take up to 6-12 wks after exposure A nurse is planning to teach self care measures to a female client about prevention of yeast infections. Which instructions should the nurse provide? - ✔✔avoid tight fitting clothing and do not use bubble bath or bath salts Which rxn should the nurse ID in a client who is responding to stimulation of the sympathetic nervous system (SNS)? - ✔✔Increased HR any stressor that is perceived as threatening to homeostasis acts to stimulate the SNS and manifests as a flight or flight response, which includes an increased HR Parasympathetic Nervous System: pupil constriction, bronchial constriction, decreased BP A client w/ asthma receives a prescription for high BP during a clinic visit. Which prescription should the nurse anticipate the client to receive that is least likely to exacerbate asthma? - ✔✔Metoprolol the nurse is preparing to administer atropine, an anticholinergic, to a client who is scheduled for a cholecystectomy. The client asks the nurse to explain the reason for the prescribed med. What response is best for the nurse to provide? - ✔✔decrease the risk of bradycardia during sugery it us used to increase the automaticity of the sinoatrial node and prevent a dangerous reduction in HR during surgical anesthesia A deficiency of intrinsic factor should alert the nurse to assess a client's hx for which condition? - ✔✔Pernicious anemia the most common cause is lack of instrinsic factor, a glucoprotein produced by the parietal cells of the gastric lining the nurse is assessing an older client and determines that the client's left upper eyelid droops, covering more of the iris than the right eyelid. Which description should the nurse use to document this finding? - ✔✔ptosis on the left eyelid A client w/ aortic valve stenosis dvps HF. Which pathophys finding occurs in the myocardial cells as a result of the increased cardiac workload? - ✔✔Increase in size HTN and incompetent or stenotic heart valves cause an increase in the workload of the heart by increasing afterload which requires an increase in the force of cxn to pump blood out of the heart. Myocardial hypertrophy results because the cells increase in surface area or size by increasing the amt of contractile proteins, but the quantity of fibers remain constant. As myocardial hypertrophy progresses, the heart becomes ineffective as a pump because the ventricular wall cannot dvp enough tension to cause effective contraction, which causes myocardial irritability due to hypoxia The nurse is measuring BP on all 4 ext's of a child w/ coarctation of the aorta. Which BP finding should the nurse expect to obtain? - ✔✔Lower in thelegs than in the arms In coarctation of the aorta, a congenital constriction is found at the aorta near the ductus arteriosus region that lies past the left subclavian arteries, which perfuses the upper extremities. What is the underlying phathophys process b/w free radicals and destruction of a cell membrane? - ✔✔Enzyme release from lysosomes Oxidative damage to cells is thought to be a causative factor in disease and aging. If free radicals bind to polyunsaturated fatty acids found in the lysosome membrane, the lysosome, nicknamed "suicide bags" leaks its protein catalytic enzymes intracellularly and the cell is destroyed Which clinical finding shojuld the nurse ID in a client who is admitted w/ cardiac cirrhosis? - ✔✔Peripheral edema 4 types of cirrhosis: alcoholic, post-necrotic, biliary, and cardiac. Cardiac is associated w/ severe right sided heart failure, so peripheral edema is most consistant While the nurse obtains a male client's hx, review of systems, and physical exam, the client tells the nurse that his breast drains fluid secretions from the nipple. The nurse should seek further eval of which endocrine land fxn? - ✔✔Hypothalamus and anterior pituitary Breast fluid and milk production are induced by the presence of prolactin secreted from the anterior pituitary gland, which is regulated by the hypothalmus' secretion of prolactin-inhibiting hormone in both men and women. further eval of the hypothalamus and anterior pituitary gland should provide additional info about the secretions or lactation The nurse is assessing the lab results for a client who is admitted w/ renal failure and osteodystrophy. Which findings are consistent w/ the client's clinical picture? - ✔✔K+ 5.5 mEq and total Ca+ 6 mg/dL In renal failure, normal serum electrolyte balance is altered because the kidneys fail to acitvate vitamin D, Ca+ absorption is impaired, and serum Ca+ decreases, which stimulates the release of PTH causing resorption of Ca+ and phosphate from the bone. A decreased tubular excretion and a decreased glomerular filtration rate results in hypocalcemia, hyperphosphatemia, and hyperkalemia Which HC practice is most important for the nurse to teach a postmenapausal client? - ✔✔consume adequate foods rich in Ca+ A mid-aged male client asks the nurse what findings from his digital rectal exam prompted the HCP to prescribe a repeat serum prostatic surface antigen (PSA) level. What info should the nurse provide? - ✔✔stony, irregular nodules palpated on the prostate should be further evaluated Which condition is associated w/ an over-secretion of renin? - ✔✔Hypertension renin is an enzyme synthesized and secreted by the juxtaglomerular cells of the kidney in response to renal artery blood volume and pressure chgs. Low renal perfusion stimulates the release of renin, which is converted by angiotensinogen into angiotensin 1, which causes the secretion of aldosterone, resulting in renal reabsorption of sodium, water, and subsequently increases BP What info should the nurse include in a teaching plan about the onset of menopause? - ✔✔a. Smoking b. Oophorectomy w/ hysterectomy c. Early menarche d. Genetic influence e. Chemotherapy exposure A client is brought to the ER after a snow skiing accident. Which intervention is most important for the nurse to implement? - ✔✔Review the ECG tracing Airway, Breathing, and Circulation are priorities in client assessment and tx. Continuous cardiac monitoring is indicated because hypothermic clients have an increased risk for dysrhythmias Which client is at highest risk for CKD secondary to DM? - ✔✔Type 1 DM and retinopathy and mild vision loss Diabetic retinopathy and nephropathy are r/t prolonged hhyperglycemia and HTN which damage the microvasculature of the eyes and kidneys , so a client w/ DM1 and retinopathy is most likely to dvp nephropathy and CDK A male client who has never smoked but has had COPD for the past 5 yrs is now being assessed for CA of the lung. The nurse knows that he is most likely to dvp which type of lung CA? - ✔✔Adenocarcinoma this is the only lung CA not r/t cigarette smoking. It has been found to be directly r/t to lung scarring and fibrosis from preexisting and pulmonary disease such as TB or COPD The nurse reviews the CBC findings of an adolescent w/ acute myelogenous leukemia. the Hgb is 13.8, Hct is 36.7, WBC is 8,200, and platelet count is 115,000. Based on these findings, what is the priority nsg dx for this client's POC? - ✔✔Risk for injury a client w/ AML is at risk for anemia, neutropenia, and thrombocytopenia. These CBC findings indicate that the platelet count is low, which places him at an increased risk for injury The parents of a child w/ hemophillia A ask the nurse about their probability of having another child w/ it. Which info is the basis for the nurse's response? - ✔✔a. Sons of female carriers have a 50% chance of inheriting hemophillia b. Hemophillia is an X-linked recessive disorder Hemophillia is an inherited disease that manifests in male children whose mom is a carrier. With each pregnancy there is a 50% chance that a male child will inherit the defective gene and manifest hemophillia A The nurse is caring for a client who had an excision of malignant pituitary tumor. Which findings should the nurse document that indicate the client is dvp'g Syndrome of Inappropriate Antidiuretic Hormone (SIADH) ? - ✔✔Wt gain w/ low serum sodium SIADH most frequently occurs when cancer cells manufacture and release ADH, which is manifested by water retention causing wt gain and hyponatremia A man who was recently dx'd w/ Huntington's disease asks the nurse if his adolescent son should be tested for the disease. What response is best for the nurse to provide? - ✔✔Genetic counseling should be obtained prior to undertaking any genetic testing procedure A mom is crying as she holds and rocks her child w/ tetanus who is having muscular spasms and crying. After administering diazepam to the child, what action should the nurse implement? - ✔✔Lay the child down and ask the mom to stay near the child in the crib Controlling environmental stimulation such as noise, light, or tactile stimuli helps reduce CNS irritability r/t acute tetanus. The mom shoujld be instructed to minimize handling of the child during episodes of muscle spasticity and to stay calmly near the child. Her presence w/ the child provides security and support Which rationale best supports an older client's risk of complications r/t dysrhythmia? - ✔✔An older client is intolerant of decreased cardiac output which may cause dizziness and falls In an older client, CO is decreased and a loss of contractility and elasticity reduces systemic and cerebral blood flow, so dysrhythmias, such as bradycardia or tachycardia is poorly tolerated, and increases the client's risk for syncope, falls, transient ischemic attacks, and possibly dementia MD is characterized by which pathophys condition? - ✔✔Skeletal muscle degeneration The nurse is assessing a client w/ a ruptured small bowel and determines that the client has a temp of 102.8F. Which assessment finding provides the earliest indication that the client is experiencing septic shock? - ✔✔Hyperpnea the interrelated pathophys chgs associated w/ the hypermetabolic state of sepsis and septic shock produce a pathologic imbalance b/w cellular O2 demand, supply, and consumption. Which s/s are associated w/ arterial insufficiency? - ✔✔Pallor, intermittent claudication these are 2 signs r/t stage 2 peripheral vascular disease, which results in arterial insufficiency the severity of diabetic retinopathy is directly r/t which condition? - ✔✔Poor glucose control a client w/ a fx'd right radius reports severe, diffuse pain that has not responded to the prescribed analgesics. The pain is greater w/ passive mvmt of the limb than w/ active mvmt by the client. The nurse recognizes that the client is most likely exhibiting sx of which condition? - ✔✔Acute compartment syndrome When observing a client for sx of a large bowel obstruction, the nurse should assess for which finding? - ✔✔Distention of the lower abd The nurse is caring for a client w/ SIADH (syndrome of inappropriate antidiuretic hormone), which is manifested by which sx? - ✔✔loss of thirst, wt gain SIADH occurs when the posterior pituitary gland releases too much ADH, causing water retention, a urine output of less than 20 ml/hr, and dilutional hyponatremia. Other indications are loss of thirst, wt gain, irritability, muscle weakness, and decreased LOC The nurse is caring for a client w/ SIADH. this condition is most often r/t to which predisposing condition? - ✔✔Small cell lung CA The nurse is assessing a postmenapausal woman who is c/o urinary urgency and frequency and stress incontinence. She also reports difficulty in emptying her bladder. These c/o are most likely due to which condition? - ✔✔cystocele Which pathophys response supports a client's vomiting experience? - ✔✔Spasmodic reflex of respiratory and gastric mvmts results from stimulation of the chemoreceptor trigger zone Vomiting is a reflex of spasmodic respiratory mvmts against the glottis causing the forceful expulsion of the contents of the stomach thru the mouth. Stimulation of the emetic center results from afferent vagal and sympathetic nerve pathways that activate the chemoreceptor trigger zone (CTZ) A client's family asks why their mom w/ HF needs a pulmonary artery (PA) catheter now that she is in the ICU. What info should the nurse include in the explanation to the family? - ✔✔A PA catheter measures central pressures for monitoring fluid replacement What histologic finding in an affected area of the body would suggest the presence of chronic inflammation? - ✔✔Increase in monocytes and macrophages A predominance of monocytes and macrophages in an inflamed area indicates the start of a chronic infection. Macrophages are responsible for "cleaning up" the healing wound thru phagocytic and debridement actions and monocytes assist in the healing of the wound after neutrophils have entered the area Physical exam of a comatose client reveals decorticate posturing. Which stmt is accurate regarding this client's status based upon this finding? - ✔✔decorticate posturing (adduction of arms at shoulders, flexion of arms on chest w/ wrists flexed and hands fisted and extension and adduction of extremities) is seen w/ severe dysfunction of the cerebral cortex HESI Pathophysiology questions and answers, rated A. Graded A. 2022/2023 An initial disturbance in a system sets off a chain of events that does not favor stability and often abruptly displaces a system from its steady state: What is that? - ✔✔positive feedback What organ shrinks with age? - ✔✔gums Which of the following is true? a. An infant will have a slower heart rate than an adult b. The elderly has better temperature sensations c. There are more sweat glands in an elderly person d. There is less thirst perception in the elderly - ✔✔d. There is less thirst perception in the elderly Which of the following in true? a. Women snore more than men b. Men have higher calcium levels c. Women have a lower hemoglobin than men d. men have a lower creatinine level than women - ✔✔c. Women have a lower hemoglobin than men An increase in normal adaptive response to the decreased availability of oxygen at high altitude is termed which? a. Circadian b. Acclimatization c. Population d. Diurnal - ✔✔b. Acclimatization What does it mean when the cause of disease is unwanted medical treatment? a. Idiopathic b. Ecogenetic c. Genotypical d. Iatrogenic - ✔✔d. Iatrogenic Which term is used for the first two months of life? a. Infancy b. Childhood c. Prenatal d. Neonatal - ✔✔d. Neonatal What is an objectively identifiable aberration of the disease? a. Symptom b. Syndrome c. Stage d. Sign - ✔✔d. Sign Which of the following is true regarding catecholamines? a. They are from the parasympathetic nervous system b. They cross the blood brain barrier c. They include epinephrine and norepinephrine d. They cause of decrease in heart rate - ✔✔They include epinephrine and norepinephrine Which of the following is a true statement? a. Antidiuretic is not important for blood volume regulation b. Endorphins increase with stress, resulting in a decrease in pain perception c. Epinephrine and cortisol act very differently d. Cortisol negates epinephrine's activity - ✔✔b. Endorphins increase with stress, resulting in a decrease in pain perception By what mechanism do lipid molecules cross cell membranes? a. They use channel proteins as a membrane transport system b. They are transported across the plasma membrane by endocytosis and exocytosis c. They use voltage-gated ion channels d. They cross by diffusion - ✔✔d. They cross by diffusion Which of the following metabolic processes is a component of anabolic metabolism? a. Protein synthesis b. Glycolysis c. Citric acid cycle d. Oxidative phosphorylation - ✔✔a. Protein synthesis Which of the following electrochemical mechanism is responsible for maintaining cell volume? a. The calcium pump b. Glucose transporters c. The sodium-potassium pump d. ATP-binding cassette (ABC) transporters - ✔✔c. The sodium-potassium pump Cellular hypoxia results in: a. Enhanced ATP activity b. Loss of intracellular calcium c. Increased pH d. Failure of the sodium-potassium pump - ✔✔d. Failure of the sodium-potassium pump A 75-y/o women develops weakness in her lower extremities after a prolonged periods of bed rest. This is most likely caused by a. Atrophy of her leg muscles b. Dysplasia of her leg muscles c. Hypertrophy of her leg muscles d. Hyperplasia of her leg muscles - ✔✔a. Atrophy of her leg muscles Which of the following types of cellular adaption is most likely to occur from chronic ischemia? a. Hypertrophy b. Metaplasia c. Atrophy d. Hyperplasia - ✔✔c. Atrophy What is the mechanism of cellular injury that occurs when deep sea divers get 'the bends'? a. Free radicals form abnormal chemical bonds which destroy the cellular membranes b. Carbon monoxide binds tightly to hemoglobin, preventing the RBD's from carrying O2 c. Intracellular calcium accumulation creates muscle tetany d. Gas bubbles from in the blood, blocking circulation and resulting and resulting in ischemia - ✔✔d. Gas bubbles from in the blood, blocking circulation and resulting and resulting in ischemia What type of cellular adaptation would create the greatest concern if found on a biopsy report? a. Dysplasia b. Metaplasia c. Hyperplasia d. Atrophy - ✔✔a. Dysplasia 19. Which of the following is the process by which mRNA is synthesized from single stranded DNA? a. Sense stranding b. Replication c. Translation d. Transcription - ✔✔d. Transcription Which of the following is not one of the 4 cell types found in adult humans? a. Epithelium b. Connective tissue c. Hematopoietic tissue d. Nervous tissue - ✔✔c. Hematopoietic tissue If a patient has a recessive trait, which of the following is the genotype of this patient? i. Recessive trait: a trait that is expressed when an organism has two recessive alleles ii. Lowercase = recessive/ uppercase = dominant b. aa c. AA d. Aa e. aA - ✔✔b. aa Which of the following chromosomal abnormalities has been linked with down syndrome? a. Translocation b. Inversion c. Deletion d. Duplication - ✔✔d. Duplication Which of the following refers to a deficiency of factor VII that causes a bleeding disorder? a. Marfan Syndrome b. Phenylketonuria c. Hemophilia d. Huntington - ✔✔c. Hemophilia Which of the following is a retrovirus that causes cancer? a. Rhinovirus b. Parvovirus c. Epstein-Barr virus d. Poxvirus - ✔✔c. Epstein-Barr virus Which of the following genes contributes specifically to some breast cancer? a. Rb b. BRCA1 c. P53 d. VHL - ✔✔b. BRCA1 Which is used to describe the histologic characteristics of tumor cells? a. Staging b. Cachexia c. Grading d. Angiogenesis - ✔✔c. Grading Which of the following offers the best prognosis for the cure of cancer? a. Early detection b. Aggressive chemotherapy c. Adjunct radiation d. Gene therapy - ✔✔a. Early detection Which of the following is true about cancer? a. Most deaths occur in those over 75 years old b. Men have a 1 in 3 lifetime risk of cancer c. The combined 5-year survival rate for cancer is 62% d. It is the leading cause of death - ✔✔c. The combined 5-year survival rate for cancer is 62% What is the purpose of the TNM classification system? a. It provides information for ongoing research to develop a cure for cancer b. It tracks the progress of the disease and the effectiveness of treatment c. It enables the MD to determine the underlying cause of the malignancy d. It proved tumor data for the centers for disease control and prevention - ✔✔b. It tracks the progress of the disease and the effectiveness of treatment Why do patients with advanced cancer develop cachexia? a. Cancer cells produce an enzyme that robs normal calls of nutrients b. They lack an adequate number of normal cells to support metabolism c. They have an increased basal metabolic rate d. The process of cancer cell destruction utilizes most of the body's nutrients - ✔✔a. Cancer cells produce an enzyme that robs normal calls of nutrients Which of the following explains the genetic basis for cancer development? a. Exposure to ionizing radiation b. Decreased immune function c. Infection by oncogenic bacteria d. Loss or defect of tumor suppressor genes - ✔✔d. Loss or defect of tumor suppressor genes Bacteria are categorized by their: (select all that apply) a. Shape b. Need for oxygen c. Reaction to staining d. Size e. Color - ✔✔a. Shape b. Need for oxygen c. Reaction to staining If the host's immune system is compromised resident florae may become pathogenic resulting in: a. Opportunistic infection b. Salmonella infection c. Otitis media d. Myocarditis - ✔✔a. Opportunistic infection Patient education to reduce emergence of resistant infectious includes: a. Stop taking prescribed antibiotics when fever is gone to avoid overuse b. Take antibiotics for viral infections that cause temperature elevation c. Take all antibiotics ordered even when feeling recovered d. Share antibiotics with susceptible family members to prevent spread of infection - ✔✔c. Take all antibiotics ordered even when feeling recovered Which of the following occurs first after cellular injury? a. Vessel walls rupture b. Neutrophils migrate to the injured area c. Plasma proteins and water move from the intracellular space to the interstitial space d. Vessel walls briefly constrict - ✔✔d. Vessel walls briefly constrict Which of the following is an example of active immunity? a. Injection of pooled gamma globulin b. Breast-feeding c. Passed from mother to infant via the placenta d. Pneumonia vaccine - ✔✔d. Pneumonia vaccine A patient's WBC count indications a shift to the left. What should the nurse asses for? a. Leukemia b. Weakness c. Infection d. Immunosuppression - ✔✔c. Infection The lab analysis on a child with chronic nasal drainage show elevated #s of eosinophils in the blood. What is the likely cause of the drainage? a. Bacterial infection b. Allergies c. Viral infection d. Sinus infection - ✔✔b. Allergies 39. A child with ill-fitting shoes develops a vesicle (small blister) that burst, releasing clear watery fluid. The school nurse would document this drainage as: a. Serous b. Vesicular c. Purulent d. Sanguineous - ✔✔a. Serous Which of the following specialized cells are associated with the immune response? a. Neutrophils b. Monocytes c. Macrophages d. Lymphocytes - ✔✔d. Lymphocytes A severe life-threatening type 1 hypersensitivity reaction is: a. Angioedema b. Urticarial c. Anaphylaxis d. Hives - ✔✔c. Anaphylaxis What pathophysiological abnormality underlies systemic lupus erythematosus (SLE)? a. Immune deficiency b. Type 2 hypersensitivity c. Autoimmunity d. Immunosuppression - ✔✔c. Autoimmunity Which of the following terms best describes the symptoms of petechiae, easy bruising, bleeding gums, occult hematuria or retinal hemorrhage? a. Neutropenia b. Leukopenia c. Anemia d. Thrombocytopenia - ✔✔d. Thrombocytopenia If I get a kidney transplant from my sister, what is it called? a. Allogenic transplant b. 'Gift of life' c. Autologous transplant d. Peripheral stem cell transplant - ✔✔a. Allogenic transplant Which of the following is a malignant disorder of mature antibody-secreting B lymphocytes or plasma cells? a. Multiple myeloma b. Hairy cell leukemia c. ALL d. CML - ✔✔Multiple myeloma Which disease has the presence of Reed-Sternberg cells? a. B-cell lymphoma b. NK-cell lymphoma c. Hodgkin lymphoma d. T-cell lymphoma - ✔✔c. Hodgkin lymphoma Which of the following assists in the diagnosis of multiple myeloma? a. Elevated liver enzymes b. Bence Jones proteins c. Hyperkalemia d. Erythrocytosis - ✔✔b. Bence Jones proteins What statement is true regarding HIV -1? a. It is a causative agent in the US b. It produces a milder form of the disease c. It is most commonly found in west Africa d. The latency period is longer than in HIV-2 - ✔✔a. It is a causative agent in the US What is the result of increased hydrostatic pressure in blood vessels? a. Increased levels of albumin b. Fluid movement into interstitial space c. Vasoconstriction d. Hypertension - ✔✔b. Fluid movement into interstitial space Which is a manifestation of left heart failure? a. Peripheral edema b. Increased exercise tolerance c. Pulmonary edema d. Paroxysmal nocturnal dyspnea (PND) - ✔✔c. Pulmonary edema A patient develops compartment syndrome. Which of the following are expected manifestations? (select all that apply) a. Pain b. Paresthesia c. Rubor d. Ischemia e. Inflammation f. Coolness g. Edema - ✔✔a. Pain b. Paresthesia d. Ischemia f. Coolness Which are manifestations of increased intracranial pressure (ICP)? a. Intense thirst b. Projectile vomiting c. Pinpoint pupils d. Altered mental status e. Decerebrate positioning f. Bradycardia g. Hypotension - ✔✔b. Projectile vomiting d. Altered mental status e. Decerebrate positioning f. Bradycardia What may unusual thirst in a diabetic patient indicate? a. Nephropathy b. Hyperglycemia c. Polyuria d. Fluid overload - ✔✔b. Hyperglycemia Which of the following is true about chronic airway disease? a. Chronic obstructive pulmonary disease COPD) is characterized by progressive increase in ciliary function b. Asthmatic attacks produce edema and increased mucus c. COPD produces reversible constriction of airways d. Asthma results in hyperinflation of alveoli - ✔✔b. Asthmatic attacks produce edema and increased mucus Which hormone is elevated in early pregnancy, and is detected by pregnancy screening tests? a. Estrogen b. Follicle stimulating hormone c. Beta chorionic gonadotrophin d. Prolactin - ✔✔c. Beta chorionic gonadotrophin A patient with peripheral artery disease experiences intermittent pain with walking. What is the mechanism responsible? a. Vein engorgement resulting in tissue compression b. Hyperglycemic damage to arterioles, resulting in intimal destruction c. Arteriole occlusion results in ischemia to muscles d. Thromboembolism in capillaries causes inflammation of blockage of blood drainage from legs - ✔✔c. Arteriole occlusion results in ischemia to muscles Which is the initial vital sign alteration expected when a patient has acute hypovolemia? a. Tachypnea b. Hypotension c. Tachycardia d. Elevated temperature - ✔✔c. Tachycardia A patient has episodes of chest pain, shortness of breath with activity, and it is relieved by rest. What is this called? a. Stable angina b. Unstable angina c. Myocardial infarction d. Pericarditis - ✔✔a. Stable angina Which of the following may be risk factors associated with the development of gastric cancer? (select all that apply) a. Eating bacon and other cured meats b. Celiac disease c. Ulcerative colitis d. Helicobacter pylori infection e. High carbohydrate diet - ✔✔a. Eating bacon and other cured meats d. Helicobacter pylori infection What immunologic activity is seen in the development of chronic obstructive pulmonary disease (COPD)? a. T cells attack healthy goblet cells in epithelium of trachea b. B cells produce excessive immunoglobulins causing inflammation in lung parenchyma c. Macrophages cause destruction of alveolar walls, resulting in loss of overall alveolar surface area d. Antigen-antibody complexes are deposited in small airways causing widespread inflammation - ✔✔c. Macrophages cause destruction of alveolar walls, resulting in loss of overall alveolar surface area Why would protein be restricted for patients with liver and kidney disease? a. Protein has a pro inflammatory effect on live tissue b. Protein will be excreted by damaged nephrons and result in proteinuria c. Less protein is needed as organ dysfunction results in reduced metabolic needs d. Protein breakdown produces nitrogenous wastes that are excreted by liver and kidneys - ✔✔d. Protein breakdown produces nitrogenous wastes that are excreted by liver and kidneys What is the mechanism of end organ disease with diabetes mellitus? a. Hyperglycemia results in microvascular damage to capillaries b. Episodic hypoglycemia causes intermittent reduction of blood flow to organs c. Buildup of nitrogenous wastes in blood is toxic to organs d. Reduction in blood viscosity results in enhanced perfusion of organs - ✔✔a. Hyperglycemia results in microvascular damage to capillaries What is a way to diagnose pancreatitis? a. Hard, dry stools b. Right lower quadrant (RLQ) pain c. Elevated serum lipase and amylase levels d. Thrombocytopenia - ✔✔c. Elevated serum lipase and amylase levels Which of the following is caused by elevated plasma glucose? a. Release of glucagon b. Release of insulin c. Release of glycogen d. Release of potassium - ✔✔b. Release of insulin Which of the following lab values reflect NORMAL (expected) levels? a. Low density lipoprotein (LDL) of 100 mg/dL b. Potassium of 3.5-5.0 mEq/l c. Hemoglobin of 12-17 gm/dL d. Hematocrit < 30 % e. High density lipoprotein (HDL) > 40 mg/dL f. Blood urea nitrogen of 15 mg/dL - ✔✔a. Low density lipoprotein (LDL) of 100 mg/dL b. Potassium of 3.5-5.0 mEq/l c. Hemoglobin of 12-17 gm/dL e. High density lipoprotein (HDL) > 40 mg/dL f. Blood urea nitrogen of 15 mg/dL What is true of open angle glaucoma? a. The angle of Schlemm is constricted, preventing drainage b. It is sudden and acutely painful c. The trabecular meshwork becomes blocked over time d. There is reduced production of aqueous humor, resulting in eye ischemia - ✔✔c. The trabecular meshwork becomes blocked over time What is an expected feature of adult respiratory distress syndrome (ARDS)? a. Extreme hypercapnia b. Metabolic alkalosis c. Hypoxia d. Green or yellow sputum - ✔✔c. Hypoxia Which form of leukemia may be suppressed but is not likely to be cured? a. Acute lymphocytic leukemia (ALL) b. Chronic lymphocytic leukemia (CLL) c. Hodgkin's lymphoma d. Acute myelogenous leukemia (AML) - ✔✔b. Chronic lymphocytic leukemia (CLL) Why might a patient with benign prostatic hypertrophy (BPH) have urinary symptoms? a. Inflammatory changes in bladder b. Metastasis of tumor cells into urinary tract c. Compression of urethra causing difficulty voiding d. Formation of calculi resulting in urinary pain - ✔✔c. Compression of urethra causing difficulty voiding What is an expected finding in acute renal failure? a. Decreased specific gravity of urine b. Reduced blood urea nitrogen (BUN) c. Increased serum potassium d. Normal blood creatinine level - ✔✔c. Increased serum potassium What is the mechanism of the development of extreme edema after a burn? a. Burns cause heat damage to blood vessels and cause them to constrict b. Burns cause tissue damage and initiate the inflammatory response c. Burns cause increase in cardiac output, resulting is increased perfusion of kidneys d. Burns cause pain with movement, causing decreased Mobily and dependent edema - ✔✔b. Burns cause tissue damage and initiate the inflammatory response What is the type of tissue injury caused by prolonged pressure on tissues, causing inflammation and ischemia? a. Eczema b. Psoriasis c. Decubitus ulcers d. Abrasions - ✔✔c. Decubitus ulcers A patient living with HIV has a non-reactive TB skin test (induration 5 mm) but is found to have active disease by sputum testing. What is the reason for the discrepancy? a. Presence of HIV virus interferes with skin reaction b. Anergic response because of immune system damage c. Increase in T cells suppressed response d. Sputum testing not accurate with HIV - ✔✔b. Anergic response because of immune system damage A patient-travels to a country with possibly contaminated water. Which infection (s) might be expected? (select all that apply) a. Hepatitis B b. Hepatitis A c. Acute amoebic dysentery d. Ulcerative colitis e. Gluten enteropathy - ✔✔b. Hepatitis A c. Acute amoebic dysentery Which of the following are true? (select all that apply) a. Osteoporosis results in increased bone reabsorption and demineralization b. Rheumatoid arthritis results in antigen-antibody deposition and inflammation of joint c. Acute gout results in repetitive stress and destruction of articular cartilage d. Osteoarthritis is always affects joints symmetrically, and causes fevers and fatigue - ✔✔a. Osteoporosis results in increased bone reabsorption and demineralization b. Rheumatoid arthritis results in antigen-antibody deposition and inflammation of joint What kind of cells are associated with the development of atherosclerosis? a. Foam cells (fatty macrophages) b. Pluripotent stem cells c. Reticulocytes d. Myocytes - ✔✔a. Foam cells (fatty macrophages) Which patient should receive an emergency infusion of factor Vlll? a. Patient with von Willebrand's disease having surgery b. Patient with gunshot wound to chest c. Patient with pernicious anemia d. Patient with polycythemia vera - ✔✔a. Patient with von Willebrand's disease having surgery Which patient would be an appropriate candidate for a transfusion of whole blood? a. Elderly woman with iron deficiency anemia b. Septic patient with disseminated intravascular coagulopathy (DIC) c. Trauma patient who is hemorrhaging d. Patient with hemophilia A who is getting routine infusion - ✔✔c. Trauma patient who is hemorrhaging What is the expected progression of amyotrophic lateral sclerosis (ALS)? a. Dysfunction of substance nigra in the brain causes reduction in dopamine and development of progressive movement disorder b. Acute inflammation of meninges causes nuchal rigidity, pain, headache and high fever c. Loss of cholinergic receptors in muscles leads to early muscle fatigue and weakness d. Destruction of motor neurons in brain and spinal cord cause progressive muscle weakness - ✔✔d. Destruction of motor neurons in brain and spinal cord cause progressive muscle weakness What would be expected if a patient with an abdominal aortic aneurysm (AAA) experiences a rupture of the aneurysm? a. Sudden loss of circulation to one leg b. Acute respiratory distress c. Hypotension and shock d. Proteinuria and edema - ✔✔c. Hypotension and shock Which of the following are risk factors for osteoporosis? a. Repetitive stress to joint b. Being overweight c. Low BMI (body mass index) d. Being Caucasian e. Smoking f. Being male - ✔✔c. Low BMI (body mass index) d. Being Caucasian e. Smoking What hormone, released in a stressful situation, will cause alteration in glucose metabolism? a. Epinephrine b. Renin c. Erythropoietin d. Cortisol - ✔✔d. Cortisol What is a true statement about the difference between diabetic ketonuria (DKA) and Hyperosmolar hyperglycemic state (HHS)? a. DKA occurs with diabetics, HHS occurs in anyone b. DKA is characterized by hyperglycemia, HHS is characterized by hypoglycemia c. DKA patients have ketones in the urine and blood; HHS patients do not d. DKA is very dangerous; HHS is less serious. - ✔✔c. DKA patients have ketones in the urine and blood; HHS patients do not Exophthalmos is caused by what mechanism? a. Decreased cardiac output results in activation of RAAS system and increased blood pressure b. Increased inflammation of eyes affecting muscles and fatty tissue around eye c. Increased pressure in anterior chamber of eye causes hardening of eyeball and blurring of vision d. Inflammation of cornea causes intense pressure and pain in eye - ✔✔b. Increased inflammation of eyes affecting muscles and fatty tissue around eye For what condition would a nurse teach a patient about 'stress dosing' of steroids? a. Cushing's disease b. Acromegaly c. Addison's disease d. Hypothyroidism - ✔✔c. Addison's disease 86. What is seen in early infections ('shift to the left')? a. Increased B cells b. Lymphocytosis c. Thrombocytopenia d. Bandemia - ✔✔d. Bandemia What does Frank-Starling law predict about heart function? a. More afterload, less perfusion b. More preload, increased contraction c. Less afterload, more ischemia d. More contraction, less output - ✔✔b. More preload, increased contraction What is the function of the glomerulus? a. Filter blood b. Activate vitamin D c. Actively reabsorb glucose d. Regulate sodium excretion - ✔✔a. Filter blood What neurotransmitter changes in brain are associated with mood depression? a. High dopamine b. Low serotonin c. Increase acetylcholine (ACh) d. Low norepinephrine - ✔✔b. Low serotonin Which is true about HIV transmission? (select all that apply) a. it is transmitted via breast milk b. it has been transmitted via aerosol route c. it cannot be transmitted during pregnancy until delivery d. it can be transmitted by sharing needles e. saliva is a common route for transmission f. it can live for 48 hrs on surfaces outside the body - ✔✔a. it is transmitted via breast milk d. it can be transmitted by sharing needles Which of the following is associated with initial HIV infection? a. flulike symptoms and rash b. decreased CD4 T cells c. seroconversion within 3-6 days d. CD4 T cell count < 200 per mcg/L - ✔✔a. flulike symptoms and rash Which of the following statement is true regarding HIV testing? a. the first test is the electrophoresis b. the new rapid finger stick tests give results in 20 min c. all patient's w/a positive test must have the ELISA performed d. the Western blot is the initial test - ✔✔b. the new rapid finger stick tests give results in 20 min Which of the following are required for erythropoieses? (select all that apply) a. vitamin K b. vitamin B12. c. Folate. d. vitamin E. e. niacin. f. Ascorbic acid (Vitamin C). - ✔✔b. vitamin B12. c. Folate. e. niacin. f. Ascorbic acid (Vitamin C). What causes a shift of the oxyhemoglobin curve to the right? a. chronic disease. b. increased pH c. decreased H+ ions d. decreased temperature - ✔✔a. chronic disease. What is the term used for an excess of RBCs? a. anemia b. polycythemia c. pancytopenia d. granulocytosis - ✔✔b. polycythemia What is false regarding aplastic anemia? a. it runs in families b. it causes overproduction of hematopoietic tissue c. it is characterized by pancytopenia d. it is caused by viral infections - ✔✔b. it causes overproduction of hematopoietic tissue Which of the following is a macrocytic anemia? a. thalassemia b. anemia of chronic renal failure c. Iron deficiency anemia d. Pernicious anemia - ✔✔d. Pernicious anemia Which of the following are appropriate for sickle cell anemia? a. early spleen removal b. acetaminophen (Tylenol) for fever c. dehydration to prevent vaso-occlusive crises d. maintain cool room temperature to prevent fever - ✔✔b. acetaminophen (Tylenol) for fever Anemia of chronic disease is caused by lack of what hormone? a. estrogen b. erythropoietin c. parathyroid hormone d. adrenaline - ✔✔b. erythropoietin 100. S/Sx of anemia are: (select all that apply) a. pallor b. bradycardia c. shortness of breath d. reduced activity tolerance e. dry mucous membranes - ✔✔a. pallor c. shortness of breath d. reduced activity tolerance How do platelets contribute to hemostasis? a. cause vasoconstriction b. stimulate fibrinolysis c. clumping d. intrinsic pathway - ✔✔c. clumping What is true of petechiae in vascular and platelet disorders? a. red, raised and macular b. flat and purple with vesicles c. Flat, pinpoint and non-blanching d. raised, red and blanching - ✔✔c. Flat, pinpoint and non-blanching What is true about disseminated intravascular coagulation (DIC)? a. it is both a bleeding and a clotting disorder b. the acute form has more thrombotic episodes c. fibrinogen level is increased d. fibrin split products are decreased - ✔✔a. it is both a bleeding and a clotting disorder Allergic purpura lesions include all of the flowing except: a. fever, itching, arthralgias b. very palpable lesions c. bleeding from lesions d. lesions located mainly on the trunk and face - ✔✔d. lesions located mainly on the trunk and face Which statement is true about the lymphatic system? a. the arrangement of the lymphatic system is very similar to that of the circulatory system b. one of the functions of the lymphatic system is to reabsorb fluid that leaks out of he vascular network into the interstitium and to return it to the general circulation c. Lymphatic vessels are more like arteries in that they are thick-walled and have no valves d. lymphatic tissue and lymph nodes are found deep within muscles nto connective tissue - ✔✔b. one of the functions of the lymphatic system is to reabsorb fluid that leaks out of he vascular network into the interstitium and to return it to the general circulation What findings are expected with arterial thrombosis of the legs? a. intermittent claudication, cool and cyanotic skin, toe ulcer. b. pain with activity, hot and dry skin, very pink c. intermittent claudication and pinkness of skin, bounding pulse d. pain with activity, leg cool to warm, (+) Homan's sign usually - ✔✔a. intermittent claudication, cool and cyanotic skin, toe ulcer. Which of the following CANNOT produce signs and symptoms of a stroke? a. varicose veins b. atherosclerosis c. cerebral aneurysm d. cerebral AV malformation - ✔✔a. varicose veins Which is the upper acceptable level of cholesterol in the blood? a. total cholesterol of 40 mg/dL, HDL of 200 mg/dL and LDL of 160 mg/dL b. total cholesterol of 40 mg/dL, HDL of 160 mg/dL and LDL of 200 mg/dL c. total cholesterol of 200 mg/dL, HDL of 140 mg/dL and LDL of 60 mg/dL d. total cholesterol of 200 mg/dL, HDL of 40 mg/dL and LDL of 100 mg/dL - ✔✔d. total cholesterol of 200 mg/dL, HDL of 40 mg/dL and LDL of 100 mg/dL Which of the following is considered a modifiable risk factor for prevention of atherosclerosis? a. smoking b. age c. gender d. genetics - ✔✔a. smoking Which of the flowing is a major determinant of diastolic blood pressure? a. heart rate (HR) b. systemic vascular resistance (SVR). c. stroke volume (SV) d. preload - ✔✔b. systemic vascular resistance (SVR). Which does NOT stimulate the release of renin? a. renal hypoperfusion b. parasympathetic activation c. 'fight or flight' response d. decreased Na+ delivery - ✔✔b. parasympathetic activation Another name for vasopressin? a. arterial natriuretic peptide b. angiotensin c. antidiuretic hormone d. aldosterone - ✔✔c. antidiuretic hormone Which of the following causes increases in blood pressure? a. dehydration b. intracerebral hemorrhage. c. blood loss d. prolonged bed rest - ✔✔b. intracerebral hemorrhage. Which of the following is NOT an endocrine disorder that causes elevated BP? a. coarctation of the aorta b. Cushing syndrome c. Acromegaly d. Pheochomocytoma - ✔✔a. coarctation of the aorta The renin-angiotensisn system (RAS) alters blood pressure in response to: a. decreased perfusion of the kidney b. decreased flow to the brain c. decreased perfusion to the arm d. decreased perfusion to the liver - ✔✔a. decreased perfusion of the kidney What is the arrangement in which separate cells of the myocardium can function together? a. autoregulation b. ischemia c. myocyte d. syncytium - ✔✔d. syncytium Which electrolytes are necessary for muscle contraction? a. sodium b. calcium c. magnesium d. potassium e. selenium - ✔✔a. sodium b. calcium d. potassium Blood flows in the human body: a. from the L side of the heart to the lungs to the R side of the heart from which it is ejected to the body b. from the R ventricle to the R atrium to the lungs, then to the L atrium to the L ventricle to the body c. from the R atrium to the R ventricle to the lungs, back to the L atrium to the L ventricle to the body, then back through the venous system to the R atrium again d. none of the above - ✔✔c. from the R atrium to the R ventricle to the lungs, back to the L atrium to the L ventricle to the body, then back through the venous system to the R atrium again During which part of the cardiac cycle does the cardiac muscle obtain its O2 and get rid of wastes? a. systole b. ventricular contraction c. atrial repolarization d. diastole - ✔✔d. diastole Which of the following describes myocardial infarction, not angina pectoris? a. chest pain that is worse with cough and deep breath b. chest pain initiated by exercise or stress c. radiating chest pain, ST segment changes, elevated troponin d. chest pain worsened with deep breathing, but relieved by rest - ✔✔c. radiating chest pain, ST segment changes, elevated troponin What factor causes a congenital heart disease to produce cyanosis? a. left-to-right shunting of blood b. right-to-left shunting of blood c. ventricular septal obstruction d. atherosclerotic plaques - ✔✔b. right-to-left shunting of blood A patient with heart failure complains of awakening intermittently during the night with shortness of breath. Which term describes this? a. dyspnea b. orthopnea c. paroxysmal dyspnea d. cyanosis - ✔✔c. paroxysmal dyspnea 123. A patient is admitted to the hospital with L heart failure. Which symptoms is NOT expected? a. pedal edema b. cough c. dyspnea d. crackles in lungs - ✔✔a. pedal edema A patient is in hypovolemic shock. What compensatory mechanism will help preserve adequate circulation? a. renin-angiotensin-aldosterone cascade. b. increased parasympathetic nervous system activity c. vasodilation d. decreased secretion of antidiuretic hormone (ADH) - ✔✔a. renin-angiotensin-aldosterone cascade. Which kind of shock is NOT characterized by vasodilation and peripheral pooling of blood? a. cardiogenic b. septic c. anaphylactic d. neurogenic - ✔✔a. cardiogenic What is the underlying problem in ALL shock states? a. tachycardia b. cardiac failure c. faulty compensatory mechanisms d. inadequate cellular oxygenation - ✔✔d. inadequate cellular oxygenation When cells get hypoxic, they switch to anaerobic metabolism. What is produced? a. excess energy b. lactic acid c. carbon monoxide d. bilirubin - ✔✔b. lactic acid Which of the following is NOT a type of dead space? a. anatomic b. cartilaginous c. alveolar d. physiologic - ✔✔b. cartilaginous Compliance is a measure of: a. how easily the lung can be inflated b. how easily gas exchange occurs at the alveoli c. how much dead space the lung has d. shunting - ✔✔a. how easily the lung can be inflated Which of the following increase lung compliance? a. pneumonia b. emphysema. c. ARDS d. pulmonary edema - ✔✔b. emphysema. What occurs with hypoventilation? a. the amount of air entering the alveoli increases b. the PaCO2 exceeds 45 mm Hg c. it is a normal response to high altitude d. hypocapnia occurs - ✔✔b. the PaCO2 exceeds 45 mm Hg Which of the following is not a major obstructive airway disease? a. bronchitis b. asthma c. pneumonia d. emphysema - ✔✔c. pneumonia Which of the following is NOT a pathogenic change associated with bronchitis? a. inflamed airways b. swelling from exudation of fluid c. decreased mucous production d. Loss of ciliary function - ✔✔c. decreased mucous production Which of the following is the most common cause of chronic bronchitis? a. viral infection b. Bacterial infection c. air pollution d. smoking - ✔✔d. smoking A 24 yo male presents with emphysema. He has never smoked and is not exposed to second hand smoke. What hereditary disease may be responsible for his condition? a. intrinsic asthma b. alpha-1 antitrypsin deficiency c. Duchenne muscular dystrophy d. pulmonary fibrosis - ✔✔b. alpha-1 antitrypsin deficiency Which value is consistent with acute respiratory failure? a. PaO2 of 100 mm Hg b. PaCO2 of 40 mm Hg c. pH < 7.3 d. hypocapnia - ✔✔c. pH < 7.3 Which of the following abnormality is characteristic of emphysema? a. extensive inflammation of the lower airways b. trapping of air in distal air sacs c. widespread occurrence of bronchial plugs d. collapse of proximal airways - ✔✔b. trapping of air in distal air sacs Which triad suggests epiglottitis? a. sore throat, difficulty swallowing, drooling b. hoarseness, sore throat, productive cough c. Persistent productive cough, vomiting, fever reted by the adrenal glands and gonads. Thyroid hormone is secreted by the thyroid gland. Oxytocin is secreted by the posterior pituitary. It is TRUE that the parathyroid gland: A. is made up of at least 6 to 10 pairs of glands. B. is large and makes up the majority of the thyroid gland. C. influences the production of thyroid hormone. D. secretes the most important factor in Ca++ regulation. - ✔✔D. secretes the most important factor in Ca++ regulation. PTH is the most important regulator of Ca++. While there are two pairs of parathyroid glands normally present, there may be two to six. They are small and located behind the thyroid gland. Thyroid hormone is produced by the thyroid gland and is unaffected by the parathyroid gland. A patient is diagnosed with type 1 diabetes and is unable to produce insulin. The pancreatic cells that are most likely damaged are the: A. beta. B. alpha. C. C-peptide. D. delta. - ✔✔A. beta. The beta cells synthesize insulin. The alpha cells secrete glucagon. The delta cells secrete somatostatin and gastrin. C-peptide is the bond that connects the two peptides of proinsulin. If the outer two layers of the adrenal cortex are removed, the patient will experience: A. hypernatremia. B. hyperkalemia. C. hyperglycemia. D. decreased epinephrine. - ✔✔B. hyperkalemia. The outer two layers of the adrenal cortex produce aldosterone and glucocorticoids. Aldosterone deficiency would cause hyponatremia and hyperkalemia. A deficiency in glucocorticoids would result in hypoglycemia. Epinephrine would only decrease if the adrenal medulla was damaged or removed. The posterior pituitary gland secretes: A. antidiuretic hormone (ADH). B. prolactin-releasing factor (PRF). C. thyrotropin-releasing hormone (TRH). D. gonadotropin-releasing hormone (GnRH). - ✔✔A. antidiuretic hormone (ADH). ADH is secreted by the posterior pituitary gland. The hypothalamus secretes the remaining substances. A characteristic of a hormone includes: Select all that apply. A. having specific rates and rhythms of secretion. B. operating independently of feedback systems. C. affecting only cells with appropriate receptors. D. being excreted by the kidneys. E. having little integration with the nervous system. - ✔✔A. having specific rates and rhythms of secretion. C. affecting only cells with appropriate receptors. D. being excreted by the kidneys. Hormones do operate within feedback systems that may be positive or negative in nature. Hormones convey specific regulatory information between cells and organs and are integrated with the nervous system to maintain communication and control. The posterior pituitary is composed of the: Select all that apply. A. median eminence. B. isthmus. C. stalk. D. pars distallis. E. infundibular process. - ✔✔A. median eminence. C. stalk. E. infundibular process. The median eminence, stalk, and infundibular process are parts of the posterior pituitary. The pars distallis is part of the anterior pituitary, while the isthmus is found in the thyroid gland. The thyroid gland contains: Select all that apply. A. C-cells. B. follicles. C. isthmus. D. somatostatin. E. chromophils. - ✔✔A. C-cells. B. follicles. C. isthmus. E. chromophils. C-cells secrete calcitonin and somatostatin. Follicles secrete thyroid hormone. The isthmus joins the two lobes of the thyroid. Chromophils are found in the anterior pituitary. The effects of glucocorticoids includes: Select all that apply. A. metabolic B. hypertensive. C. anti-inflammatory. D. growth suppression. E. tumor growth. - ✔✔A. metabolic C. anti-inflammatory. D. growth suppression. The hypertensive response and tumor growth are not a result of glucocorticoids. The other three answers are all effects of glucocorticoids. Abnormalities in endocrine function may be caused by a(n): A. decrease in hormone levels. B. altered metabolism of the hormones. C. absence of antibodies against specific receptors. D. faulty feedback systems. E. hormone production by nonendocrine tissue. - ✔✔C. absence of antibodies against specific receptors. Elevated or depressed hormone levels result from: (a) faulty feedback systems, (b) dysfunction of the gland, (c) altered metabolism of hormones, or (d) production of hormones from nonendocrine tissues. There is actually a presence of antibodies against specific receptors that either reduce available binding sites or mimic hormone action. A symptom of SIADH is: A. hyponatremia. B. hypernatremia. C. hyperosmolality (serum). D. hypoosmolality (urine). - ✔✔A. hyponatremia. The cardinal features of SIADH are symptoms of water intoxication. These include hyponatremia (low serum sodium), serum hypoosmolality, and urine that is inappropriately concentrated (hyperosmolar) with respect to serum osmolality. It is true that DI: A. results from low levels of ADH. B. occurs with organic lesion of the hypothalamus or pituitary. C. may be demonstrated by excessively concentrated urine. D. is caused by low levels of ADH. - ✔✔B. occurs with organic lesion of the hypothalamus or pituitary. The neurogenic form of DI occurs when a lesion of the hypothalamus, pituitary stalk, or posterior pituitary interferes with ADH synthesis, transport, or release. While the neurogenic form is caused by low levels of ADH, the nephrogenic form is caused by inadequate response of the renal tubules to available ADH. Urine is usually very diluted. A patient experiences nausea, vomiting, loss of body hair, fatigue, weakness, and hypoglycemia. The hormone deficiency the patient is most likely experiencing is that of: A. TSH. B. ACTH. C. FSH. D. LH. - ✔✔B. ACTH. Within 2 weeks of complete absence of ACTH, symptoms of nausea, vomiting, anorexia, fatigue, and weakness develop. With absence of TSH, there is cold intolerance, dry skin, mild myxedema, lethargy, and decreased metabolic rate. FSH and LH deficiencies are associated with amenorrhea, atrophic vagina, uterus, breasts, decrease in body hair, and diminished libido. It is correct to assume that pituitary adenomas: A. will experience rapid growth. B. are generally metastatic. C. arise from the anterior pituitary. D. have a pathogenesis due to infarction. - ✔✔C. arise from the anterior pituitary. They arise from the anterior pituitary, are benign, and are usually slow growing in nature. The pathogenesis is not a result of infarction. A patient with visual changes that begin in one eye then progress to the second eye is likely experiencing: A. pituitary infarct. B. ACTH insufficiency. C. Growth hormone (GH) insufficiency. D. pituitary adenoma. - ✔✔D. pituitary adenoma. With a pituitary adenoma, there can be increased pressure on the optic chiasm, and growth of the tumor can cause visual changes in both eyes. The other conditions do not present with optic nerve involvement. Awarded 0.0 points out of 1.0 possible poi It is correct to assume that acromegaly: A. occurs due to excessive levels of ACTH. B. is the result of a GH-secreting pituitary adenoma. C. occurs more frequently in men. D. is a relatively common condition. - ✔✔B. is the result of a GH-secreting pituitary adenoma. Acromegaly is a condition caused by excess of GH, not ACTH, as a result of GH-secreting pituitary adenoma. It occurs more commonly in women and is a relatively uncommon condition occurring in about 40 per 1 million. A symptom of a prolactinoma would include: A. galactorrhea. B. alopecia. C. excessive menses. D. pregnancy. - ✔✔A. galactorrhea. Galactorrhea is the spontaneous flow of milk from the breast, unassociated with childbirth or nursing. Amenorrhea (absence of menses), hirsutism (excessive body hair), and osteopenia can all be caused by a prolactinoma. Pregnancy is a normal cause of galactorrhea. Symptoms of Graves disease includes: A. hypothyroid. B. goiter. C. sunken eyeballs. D. atrial fibrillation. - ✔✔B. goiter. Graves disease is an autoimmune disease that can cause hyperthyroidism, goiter (diffuse thyroid enlargement), and ophthalmopathy (protruding eyeballs). Atrial fibrillation is not generally viewed as a symptom of Graves disease. Two siblings are diagnosed with a thyroid disorder due to destruction of thyroid tissue by lymphocytes and circulating thyroid autoantibodies. This pathology is likely the result of: A. subacute thyroiditis. B. Hashimoto disease. C. painless thyroiditis. D. postpartum thyroiditis. - ✔✔B. Hashimoto disease. Hashimoto disease is also called autoimmune thyroiditis. It results in the gradual destruction of thyroid tissue by infiltration or lymphocytes and circulating thyroid autoantibodies. Painless thyroiditis has a similar course to subacute thyroiditis, but is pathologically identical to Hashimoto disease. Subacute thyroiditis is a nonbacterial inflammation of thyroid often preceded by a viral infection. Postpartum thyroiditis generally occurs within 6 months of delivery and occurs in up to 7% of all women. Myxedema coma is generally associated with: A. hyperthyroidism. B. hyperthermia. C. lactic acidosis. D. hyperglycemia. - ✔✔C. lactic acidosis. Myxedema coma is a medical emergency involving lactic acidosis. It is associated with a diminished level of consciousness due to severe hypothyroidism. Signs and symptoms include hypothermia, hypoventilation, hypotension, hypoglycemia, and lactic acidosis. It is correct to assume that primary hypothyroidism: A. is commonly observed. B. occurs in children aged 5 to 10 years. C. is the result of absent thyroid tissue. D. occurs more frequently in male infants. - ✔✔C. is the result of absent thyroid tissue. Primary hypothyroidism is a rare form of hypothyroidism caused by the absence of thyroid tissue. It occurs in infants, and more commonly in female infants. Diabetic ketoacidosis (DKA) is a result of: A. an increase in insulin production. B. a decrease in catecholamine secretion. C. impaired metabolism seen in the elderly. D. increased fat mobilization. - ✔✔D. increased fat mobilization. DKA develops when there is an absolute or relative deficiency of insulin or increase in insulin counterregulatory hormones and fat is burned for fuel. This includes an increase in catecholamines, cortisol, glucagon, and GH. Emotional factors and stress, especially in children, can contribute to the development of DKA, and there is increased glucose production, decreased peripheral glucose usage, and increased fat mobilization. A patient develops severe dehydration and hyperglycemia in the absence of ketosis. Which of the following conditions does this patient have? A. Hyperosmolar hyperglycemic nonketotic syndrome (HHNKS) B. DKA C. Hypoglycemia D. Somogyi effect - ✔✔A. Hyperosmolar hyperglycemic nonketotic syndrome (HHNKS) HHNKS is different from DKA in the degree of insulin deficiency and fluid deficiency. It is also characterized by a lack of ketosis. Somogyi effect occurs when hypoglycemia stimulates glucose counterregulation of hormones, causing a rebound hyperglycemia. A newly diagnosed diabetic patient will exhibit symptoms of: Select all that apply. A. polydipsia. B. anuria. C. polyphagia. D. weight loss. E. loss of muscle mass. - ✔✔A. polydipsia. C. polyphagia. D. weight loss. Excessive thirst and hunger as well as weight loss will likely be seen in a diabetic patient. Polyuria, not anuria, is seen. Loss of muscle mass is not a symptom of diabetes mellitus. Risk factors for insulin resistance include: Select all that apply. A. obesity. B. inactivity. C. low-fat diet. D. age. E. medications. - ✔✔A. obesity. B. inactivity. D. age. E. medications. Resistance of the receptors to insulin is heightened by obesity, inactivity, illnesses, medications, and age. A carbohydrate-rich diet, not low-fat, puts an obese person at risk for insulin resistance. Complications experienced by patients with chronic uncontrolled type 2 diabetes are: Select all that apply. A. peripheral vascular disease. B. orthostatic hypotension. C. thickened capillary membranes. D. increased glomerular filtration rate (GFR). E. visual difficulties. - ✔✔A. peripheral vascular disease. B. orthostatic hypotension. C. thickened capillary membranes. E. visual difficulties. GFR decreases due to destruction of the nephrons and thickening of the filtration barrier. All other options occur with uncontrolled hyperglycemia. Which form of anemia is caused by altered heme synthesis in erythroid cells? A. Iron deficiency B. Microcytic-hypochromic C. Sideroblastic D. Megaloblastic - ✔✔C. Sideroblastic Sideroblastic anemias are a heterogeneous group of disorders characterized by anemia of varying severity due to a dysfunction in the erythroid cells that results in a faulty production of heme. Iron deficiency anemia is usually a result of pregnancy or caused by a continuous loss of blood. Microcytichypochromic anemia is caused by small erythrocytes that contain reduced amounts of hemoglobin. Megaloblastic anemia is caused by unusually large erythrocytes. Which term refers to an abnormally high production of red blood cells? A. Anemia B. Hemolytic crisis C. Polycythemia D. Apoferritin - ✔✔C. Polycythemia Polycythemia is the medical term for abnormally high production of red blood cells. Anemia is a decrease in the number of red blood cells. Hemolytic crisis is fulminate hemolytic anemia and can present with shock. Apoferritin is a protein implicated in altered iron metabolism. Which statement regarding lymphoma is true? A. The malignancy occurs in the bone marrow. B. It is the result of injury to the RNA of a lymphocyte. C. Palpable, tender lymph nodes are present. D. Lymphomas are the second most common cause of cancer death. - ✔✔C. Palpable, tender lymph nodes are present. Lymphomas are initially identified by the presence of tender, lymph nodes that are enlarged enough to be palpated. They are the sixth most common cause of cancer death and are the result of injury to the DNA of the lymphoid tissue. Malignancy within the lymphatic tissue in the bone marrow is termed lymphocytic leukemia. Spontaneous bleeding without trauma is possible when the platelet count is: A. greater than 100,000. B. between 60,000 and 75,000. C. between 20,000 and 50,000. D. less than 10,000. - ✔✔D. less than 10,000. With a platelet count of less than 10,000, severe bleeding without trauma may result. It is unlikely that such a bleeding will occur at the other levels. Which statement regarding iron deficiency anemia is true? A. Caucasians are more commonly affected. B. Incidence is most common in those children older than 2 years. C. It is common in children due to their extremely high need for iron for normal growth. D. There is decreased risk in children of homeless women. - ✔✔C. It is common in children due to their extremely high need for iron for normal growth. It is common in children due to their extremely high need for iron for growth. Incidence is not related to race but is increased in the children of homeless women most likely due to poor nutrition. It is most commonly found between the ages of 6 months and 2 years. Which statement regarding iron deficiency is true? A. Splenomegaly is present in 90% of those affected. B. Hemoglobin of 7 g/dl to 8 g/dl may be accompanied by pallor. C. Hemoglobin of 10 g/dl is generally accompanied by tachycardia. D. Widening of sutures is an early sign of iron deficiency. - ✔✔B. Hemoglobin of 7 g/dl to 8 g/dl may be accompanied by pallor. Splenomegaly is evident in only 10% to 15% of children with iron deficiency anemia. If the condition is longstanding, the sutures may widen. Mild to moderate iron deficiency (hemoglobin 6 g/dl to 10 g/dl) may show some cellular changes. Hemoglobin less than 8 g/dl can demonstrate pallor, tachycardia, and a systolic murmur. Microcytic-hypochromic anemia is known to be a result of disorders involving: Select all that apply. A. iron metabolism. B. porphyrin synthesis. C. globin synthesis. D. vitamin B12 absorption. E. heme production. - ✔✔A. iron metabolism. B. porphyrin synthesis. C. globin synthesis. E. heme production. Research supports that microcytic-hypochromic anemia is a result of disorders involving iron metabolism, porphyrin synthesis, heme production, and globin synthesis. The inability to absorb vitamin B12 results in pernicious anemia, which is a microcytic-normochromic anemia. Which factors involved in blood clotting are regulated by vitamin K? Select all that apply. A. II B. VII C. VIII D. IX E. X - ✔✔A. II B. VII D. IX E. X Which situation is a characteristic of the triad of Virchow? Select all that apply. A. Injury to endothelium B. Abnormalities of blood flow C. Hypercoagulability of the blood D. Decreased clotting factors E. Impaired vitamin A absorption - ✔✔A. Injury to endothelium B. Abnormalities of blood flow C. Hypercoagulability of the blood Which statement regarding anemia in children is TRUE? A. The most common cause of sickle cell disease is anemia. B. Anemia is the most common blood disorder in children. C. There is only one cause of hemolytic anemia. D. Children rarely present with iron deficiency anemia. - ✔✔B. Anemia is the most common blood disorder in children. Anemia, not sickle cell disease, is the most common blood disorder in children. The most common cause of anemia is iron deficiency. There are two large categories for hemolytic anemia, including increased destruction and disorders related to damaging extraerythrocytic factors. Which statement regarding maternal antibodies is TRUE? A. Placental detachment does not result in fetal erythrocytes crossing the placenta. B. The first Rh-incompatible pregnancy usually presents with severe complications. C. Anti-Rh antibodies are formed only in the response to transfusion. D. ABO incompatibility can cause hemolytic disease without erythrocytes escaping maternal circulation. - ✔✔D. ABO incompatibility can cause hemolytic disease without erythrocytes escaping maternal circulation. Anti-Rh antibodies are formed only in response to the presence of incompatible (Rh-positive) erythrocytes in the blood of an Rh-negative mother. Sources of exposure include fetal blood that is mixed with the mother's blood at the time of delivery, transfused blood, and, rarely, previous sensitization of the mother by her own mother's incompatible blood. ABO incompatibility can cause hemolytic disease of the newborn without erythrocytes escaping maternal circulation. Placental detachment results in a large number of fetal erythrocytes entering the mother's bloodstream. The first Rh-incompatible pregnancy usually presents with no difficulties. Anti-Rh antibodies are formed in response to the presence of incompatible (Rh-positive) erythrocytes in the blood of an Rh-negative mother. Which statement regarding a Coombs test is accurate? A. Indirect Coombs confirms the diagnosis of antibody-mediated hemolytic disease. B. Indirect Coombs measures antibodies to the mother's circulation. C. Direct Coombs indicates if the fetus is at risk for hemolytic disease. D. Direct Coombs measures free antibodies. - ✔✔B. Indirect Coombs measures antibodies to the mother's circulation. The indirect Coombs measures antibody in the mother's circulation and indicates if the fetus is at risk for hemolytic disease. The direct Coombs test measures antibodies already bound to the surfaces of fetal erythrocytes and is used primarily to confirm the diagnosis of antibody-mediated hemolytic disease. Which condition is defined as the "profound anemia caused by decreased erythropoiesis"? A. Vaso-occlusive crisis B. Aplastic crisis C. Sequestration crisis D. Hyperhemolytic crisis - ✔✔B. Aplastic crisis Aplastic crisis is a profound anemia caused by diminished erythropoiesis despite an increased need for new erythrocytes. Vaso-occlusive crisis may develop spontaneously or be precipitated by infection, cold temperatures, dehydration, or low pH. This is when the cells clump and occlude vessels. Sequestration crisis is when large amounts of the blood become pooled in the liver and spleen. Hyperhemolytic crisis is unusual and often occurs with G6PD. Congenital deficiency in which plasma clotting factors is most likely to cause hemophilia? A. V B. VI C. IX D. X - ✔✔C. IX About 90% to 95% of hemorrhagic bleeding disorders are caused by clotting factors VIII, IX, and XI. There is no current research to support the role of the other options in the development of hemophilia. Which statements regarding hemophilia are accurate? Select all that apply. A. There is a dangerous tendency to bleed. B. Transmission of the disorder to sons occurs via the father. C. It is considered a hereditary disorder. D. Blood coagulation is chronically impaired. E. Women are carriers of the disorder. - ✔✔A. There is a dangerous tendency to bleed. C. It is considered a hereditary disorder. D. Blood coagulation is chronically impaired. E. Women are carriers of the disorder. Hemophilia is a condition characterized by impairment of the coagulation of blood and a subsequent tendency to bleed. The classic disease is hereditary and limited to males, being transmitted through the female to the second generation. Which clinical manifestation is suggestive of leukemia? Select all that apply. A. Sudden onset B. Fever present C. Fatigue D. Hemoglobin less than 7 g/dl E. Unaffected white blood counts - ✔✔B. Fever present C. Fatigue D. Hemoglobin less than 7 g/dl Which artery travels in the coronary sulcus between the left atrium and the left ventricle? A. Left anterior descending B. Circumflex C. Right coronary D. Left coronary - ✔✔B. Circumflex The circumflex travels in the coronary sulcus. The left anterior descending travels down the anterior surface of the interventricular septum. The right coronary artery originates from an ostium behind the right aortic cusp and travels behind the pulmonary artery. The left coronary artery passes between the left atrial appendage and the pulmonary artery and generally divides into two branches. Which part of the heart is responsible for electrical impulse stimulation? A. Atrioventricular (AV) node B. Sinoatrial (SA) node C. Bundle of His D. Right bundle branch - ✔✔B. Sinoatrial (SA) node The SA node contains P cells and is the site of impulse formation. The atrioventricular node is the junction of the electrical transmission between the atria and the ventricles. The bundle of His is the next stop, and then the transmission branches to the right and left bundle branches [Show More]
Last updated: 2 years ago
Preview 1 out of 736 pages
_merged.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$18.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 04, 2022
Number of pages
736
Written in
Additional information
This document has been written for:
Uploaded
Oct 04, 2022
Downloads
0
Views
275














.png)