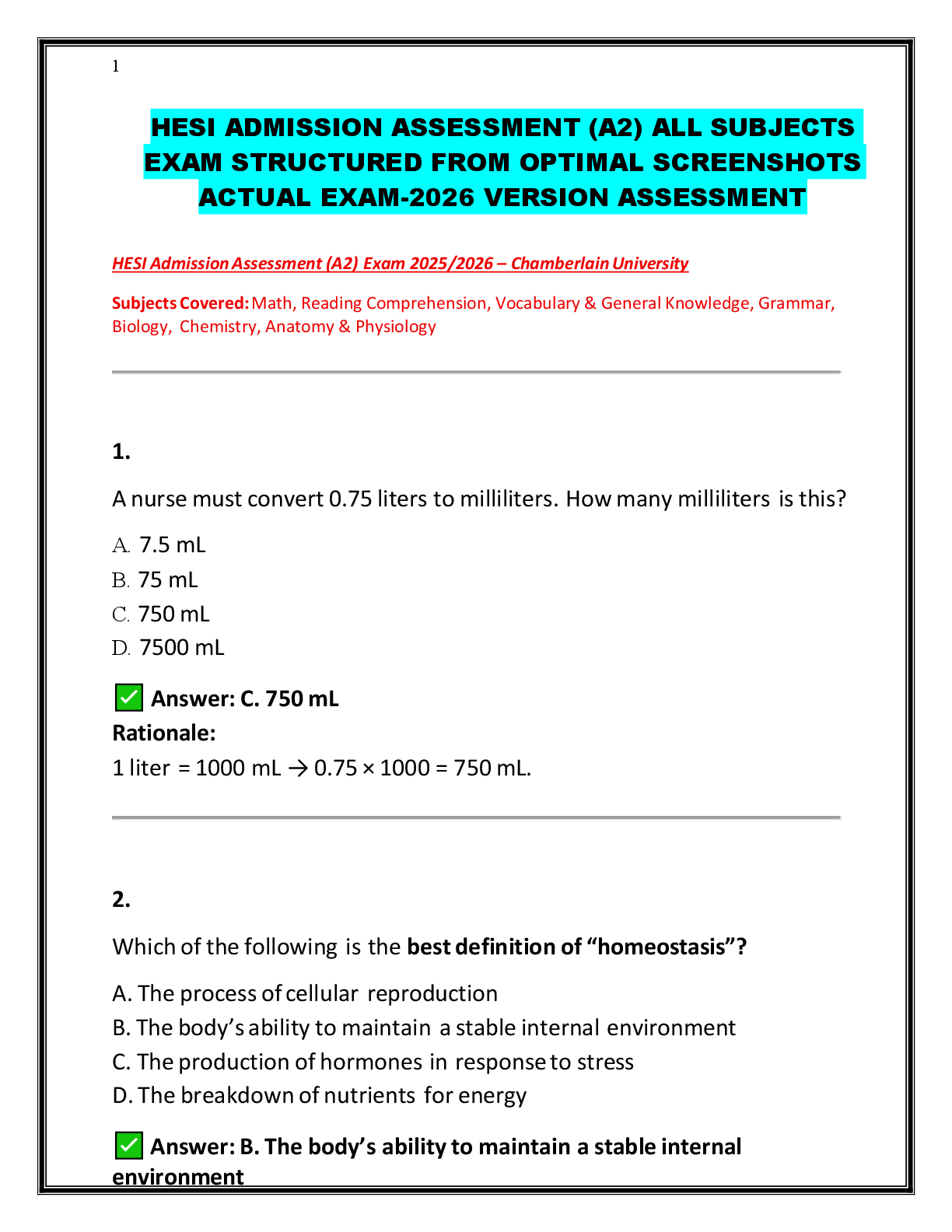
*NURSING > HESI > HESI-SUPER-CONDENSED PORTABLE HESI STUDY GUIDE| HESI Concepts From Start To Finish in 220 Pages (The (All)
HESI-SUPER-CONDENSED PORTABLE HESI STUDY GUIDE| HESI Concepts From Start To Finish in 220 Pages (The complete HESI Guide)
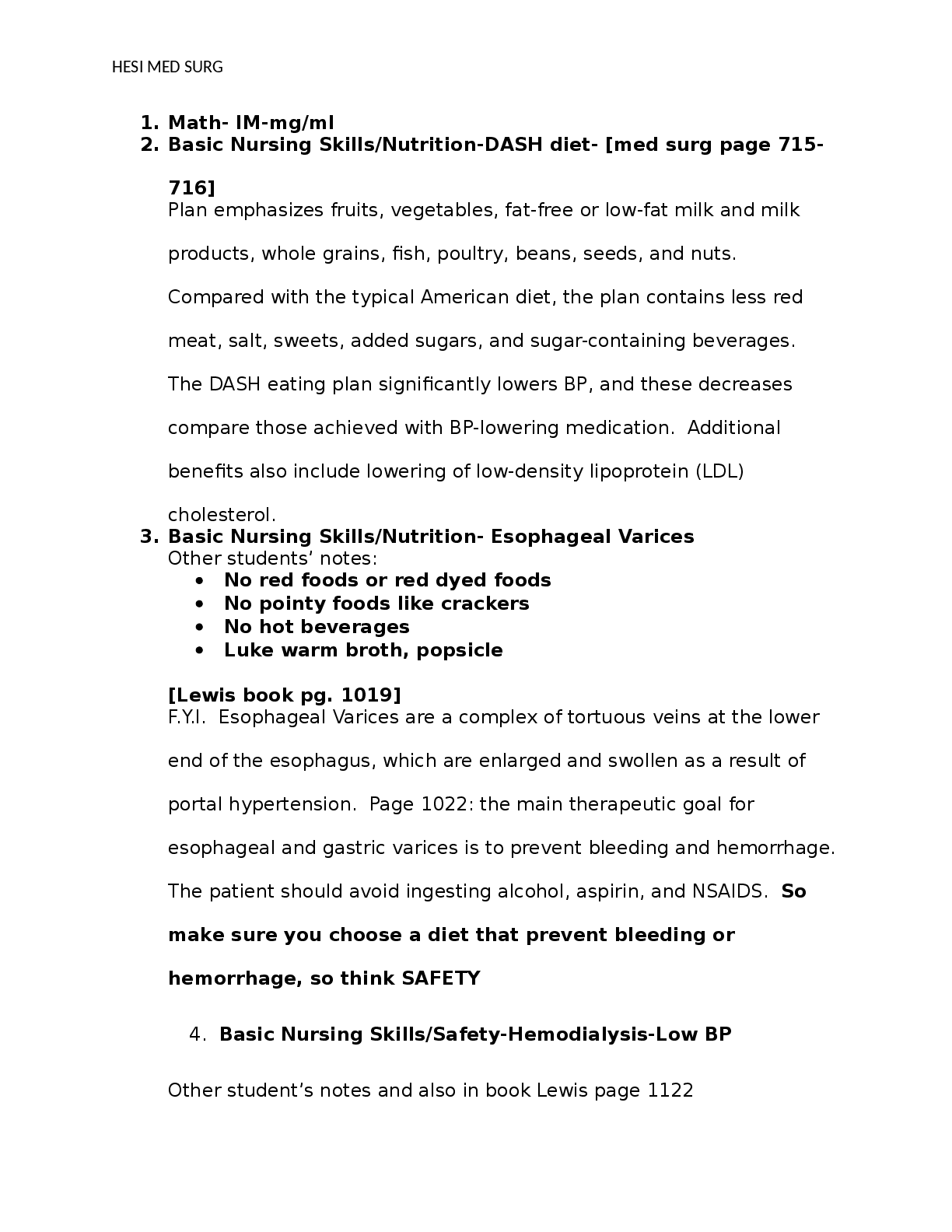
Document Content and Description Below
SUPER CONDENSED PORTABLE HESI STUDY GUIDE HESI Concepts From Start To Finish Your Name Here: _______________________________ Collected Works To Help Facilitate Success. Intended to Supplement E ... xisting Literature, Not Replace It. Preliminary VersionGeneral Usage Instructions/How to Use This Document: ·0 Read your HESI BOOK!, textbooks, and notes. ·1 If viewing this in MS Word, hit “Ctrl-F” on your keyboard and then type in whatever you are looking for into the box and hit the “Enter” key on your keyboard until you find what you are looking for. ·2 If you are scrolling through this document each applicable section is listed “Key Points”, “#” (which key point number), “subject matter title” ·3 Rinse and repeat.HESI NURSING SUBJECT AND EXIT TEST PREPARATION INSTRUCTIONS To prepare for the exam (whether a subject exam or exit exam) use and have the following materials/resources available: 1) HESI study book from evolve (ISBN# 9781416047759) 2) HESI case studies from evolve 3) HESI practice test CD which comes with the HESI book 4) HESI Practest 2009 questions from evolve 5) HESI related flashcards, not from evolve 6) HESI study notes compiled by faculty and previous ADN students (lab values, meds, etc.) 7) HESI related powerpoints for remediation and instructional purposes, not from evolve To prepare for the test itself: 1) Become an expert at the nursing process r/t questions, answers, and related processes 2) Determine my optimum learning style 3) Practice visualization and guided imagery 4) Practice and refine test taking skills 5) Stress relief and coping skills developed and utilized 6) Determine areas of weakness in previous HESI exams (via the statistical report provided after taking the test) 7) Practice the practice tests on the computer until i memorize/understand the questions and related material (until I have it down cold via repetition) 8) Review the rationales on the Practest questions, case studies, and practice test CD relentlessly (usually start with this first... essentially reverse engineer the questions starting with the rationales and working backwards)9) Memorize hints, meds, ranges, lab values, etc. as outlined in the HESI study book (with an intent to not be caught off guard by material you haven't seen before and to not forego any easy points) 10-A) Block off two weeks or more to constantly review the HESI book 10-B) Alternatively, study the HESI book as the semester progresses. 11) Foregoing studying from other non-evolve resources such as the saunders book temporarily (rationale: HESI test comes from HESI/Evolve related products, normally). 12) Host/goto HESI review sessions with other students about to take the test (rationale: If you can teach it, you get a better understanding=proficiency, eventually) Where to get some of the above resources: Austin Community College. Test taking strategies. Available at: http://www2.austin.cc.tx.us/adnlev2/Tutoring_Web/Documents/Testtaking.htm Link for the hesi book + practice test 2009: http://portals.elsevier.com/portal/hesi/ProductAction?isbn=9780323055710 HESI online case studies only: https://evolve.elsevier.com/productPages/s_994.html HESI case studies + practice test 2009: https://evolve.elsevier.com/productPages/s_1641.html HESI study book only: http://search.barnesandnoble.com/Evolve-Reach-Comprehensive-Review-forthe-NCLEX-RNExamination/Hesi/e/9781416047759Sunday Monday Tuesday Wednesday Thursday Friday Saturday Accountability: You only have yourself and your success or failure to account to. 100 questions (you may have to get up extra early to complete them). Goal: is to complete 800- 1000 questions by Sunday before 5 p.m. Do not worry so much about your grade for the exams— the most important thing is to understand why you answered the question(s) incorrectly. Do 3 HESI case studies Review Meds-Pub Therapeutic Communication Practicum ?? After practicum No more than 50 questions. It will not be productive on a long day. e.g. 25 MedSurg; 25 Pedi Do 4 HESI case studies Review Meds-Pub Dosage Calculations After practicum 50 questions e.g. 25 Med-Surg; 25 Pedi Books to have next to you: Med-Surg Lab Ref. Drug book Fundamentals Med. Dictionary In addition to reviewing rationales, go back to your texts to read up if you were not familiar with the disorder/disease. Do 5 HESI case studies Review Meds-Pub NCLEX review prep. No Practicum: 200 questions throughout the day. Not in one sitting 50-med surg 50-pedi 50-psych 50-women’s health In addition to reviewing rationales, go back to your texts to read up if you were not familiar with the disorder/disease. Due 3 HESI case studies After practicum 50 questions e.g. 25 MedSurg; 25 Pedi In addition to reviewing rationales, go back to your texts to read up if you were not familiar with the disorder/disease Due 6 HESI case studies Review MedsPub on Nursing Process No Practicum: 200 questions throughout the day. Not in one sitting 50-med surg 50-pedi 50-psych 50-women’s health In addition to reviewing rationales, go back to your texts to read up if you were not familiar with the disorder/disease Due 2 HESI case studies Review MedsPub on Nursing Process No Practicum: 200 questions throughout the day. Not in one sitting 50-med surg 50-pedi 50-psych 50-women’s health In addition to reviewing rationales, go back to your texts to read up if you were not familiar with the disorder/disease. Due 6 HESI case studies Review Meds-Pub on Nursing Process SAMPLE HESI STUDY AND REMEDIATION SCHEDULE Note: “Fear” of the unknown only serves us from moving forward. Your self-discipline, commitment to working hard and faith will help get you through this.Before the test: The HESI and NCLEX tests use the steps of the nursing process (assessment, nursing diagnosis, planning, intervention, and evaluation) to evaluate how you critically think about and apply your knowledge about nursing principles and skills during the care of patients. Do the following before the test: ·4 Review the nursing process and critical thinking. You need to be very familiar with the stages of the process and the nursing actions associated with each stage, and be prepared to identify whether a certain action is used in the planning or evaluation phase of the nursing process. ·5 Review material which will refresh your knowledge on developmental issues at all stages of life which will help with pediatric health questions. ·6 Use an NCLEX study book to familiarize yourself with the type of questions to expect and review the answers to understand why they are correct. Know the common electrolyte values and signs of abnormal levels, common drugs. Don't read things into the questions or assume things that are not part of the question. After you read the test question only, close your eyes. Think about what the question said and what you know about it, and only then, look at the answers. Practice the questions with same time limit used in the NCLEX testing: 90 seconds per question. During the test be careful about: ·7 Reading too much into the questions. Look at what is there, what you know. Unless it is specified, don't assume that you know the patient's gender, age, diagnoses, situation or where the interaction is occurring (home, street, nursing unit). ·8 Reading too much into the answers. See above. 3. Using the answer choices to search your brain for information. a. Try covering up the answers and read the question. Think about the distracters (unneeded/ irrelevant information and words like "all of the following”, ”except", "not", etc). b. Think about what you know about the subject. If you can't recall anything, look at the words and think about their meaning (dys=not or abnormal, anti=against), or what they sound like (sarcoma sounds like carcinoma, so a sarcoma is a type of cancer), or what body system they might be a part of (autonomic=nervous system). c. Then, think again about what you know and look at each answer to see if it relates to what you know.4. Becoming anxious. If you are feeling overwhelmed, discouraged, tired: STOP for a minute or two. Do deep breathing or relaxation or visualization. Use positive, affirmational self talk- NO negativity! You need your mental energy to concentrate, just like you do in the hospital when patient care situations get tough, like severe bleeding or a code. 5. Be sure to print out the test analysis at the end to have as proof of completion of the test and to help guide future review work. TEST TAKING TIPS: Initial = Assess Essential = Safety Base your Assessment on Malsow’s Hierarchy Absolute Words– These words tend to make answers wrong: ·9 Deadly Words ·10 All ·11 Wholly ·12 Every ·13 Total ·14 Alone ·15 Sole ·16 Lone ·17 Nothing ·18 Always ·19 Forever ·20 Entire ·21 Whole ·22 Completely ·23 Each ·24 Only ·25 Any nobody ·26 Never ·27 None ·28 Everywhere Dangerous Words– are words are strong words. These are words that are strong but not as absolute as the “deadly” words. If you see these words look carefully at the answer. There is a strong chance it isincorrect: ·29 Main ·30 Paramount ·31 Primarily ·32 Inevitable ·33 Eliminate ·34 Regardless ·35 Impossible ·36 Too ·37 Chief ·38 Avoid ·39 Major ·40 Shall ·41 Will rarely ·42 Lack Safe Words – Are qualified answers or hedging words make answers correct. These words are usually “safe” to choose: ·43 Usually ·44 Frequently ·45 Potentially ·46 Sometimes ·47 Some ·48 Occasionally ·49 Essentially ·50 Generally ·51 Maybe ·52 Commonly ·53 Seldom ·54 Normally ·55 Almost ·56 Probably ·57 May ·58 Partial ·59 Might ·60 Should ·61 Few ·62 Nearly ·63 Could ·64 Average ·65 Often Parts of the question ·66 The case (scenario) – description of client or what is happening to the client·67 The stem – the part that ask the question ·68 Response – choosing correct response ·69 Distracters - incorrect but feasible choices ·70 Key word – determine the key words related to the client, problem or specific/aspect of the problem Client – age, sex, marital status may be relevant Who is the focus of the question: nurse, client, spouse, child, family, etc. Test taking tips & techniques: UMBRELLA ANSWERS ·71 Problem solving applies to nursing ·72 Assess signs & symptoms ·73 Determining the nursing diagnosis ·74 Evaluating the outcome criteria ODD MAN WINS ANSWER ·75 Three obvious incorrect answers leaving the odd man wins OPPOSITES ANSWERS ·76 “High blood pressure”, “Low blood pressure” ·77 “Increase IV drip”, “Stop IV” ·78 “Turn to the left”, “Turn to the right” When there are two answers that are opposite, the two automatically eliminates the other two choices but the downside is which of the two opposite answers is correct. SAME ANSWER DIFFERENT WORDING ANSWERS ·79 Client has tachycardia, Client has a rapid heart beat ·80 Client has difficulty breathing, Client has dyspnea Do not choose these answers, eliminate both, leaving the other two choices to be the correct answers. LIKE WORD ANSWERS·81 Words in the question are found in the answer ·82 Caring in the question and the word caring is in the answer Maslow’s Hierarchy Use Maslow’s Hierarchy to answer your questions. Physiology needs will always be your first choice when answering a question with the exception of Psychological questions. Priority ·83 “What actions take priority” ·84 “What should the nurse do first” ·85 “What should the nurse do initially” ·86 “What is essential for the nurse to do?” COMMUNICATION Advising is always incorrect: ·87 “What you really ought to know…..?” ·88 “You shouldn’t have left……..?” ·89 “If I were you I……?” ·90 “What you really should do…..?” Use the word DON’T: (incorrect answers) ·91 Don’t be sad ·92 Don’t cry ·93 Don’t be concerned You should say instead: (correct answers)·94 You seem sad ·95 I noticed you are crying, want to talk about it ·96 You sound concerned More incorrect answers: ·97 I know what you mean ·98 “Why are you upset?” (why in quotation marks is always the wrong answer) ·99 Everything will be alright (everything is an absolute ABSOLUTES Wrong Answers Right Answers Qualified answers or heading words make answers correct. These words are usually are “safe” to choose. “Safe” words are words such as: usually, almost. Therapeutic – goal directed professional framework ·100 Silence – sitting quietly with client ·101 Offering Self – “I will stay with you.”, “Let me help you.” (conveys caring) ·102 Reinstatement & Reflection ·103 Client: “I had a terrible night last night” ·104 Nurse: “You didn’t sleep well?” ·105 Giving information ·106 Client: “Where is the bathroom?” ·107 Nurse: “Second door on the left” (Inappropriate response: “Do you need to go to the bathroom?”) ·108 Focusing/Exploring ·109 “You seem to be upset over your mother’s visit.” ·110 Empathy ·111 “It must be difficult to be away from your family”·112 “It must be hard to be here in the hospital” ·113 “What should the nurse say initially?” questions ·114 Empathy ·115 Reinstatement ·116 Reflection HESI: Pharmacology Half-Life: Time it takes to excrete half the amt of drug from body. Shorter half-life drugs are given more often – approx. 5 half-lives and drug removed from body. First pass: Amt of metabolism of drug before entering the bloodstream Absorption: Getting medication into the bloodstream. (Liquids metabolized quickest; enteric coated takes longest) Distribution: Moving medication to their specific sites Metabolism: Breaking down medications (liver) √ALT (1-21) √AST (7-27) (biotransformation) Excretion: Elimination medication from body (kidney) √BUN (10-20) √Serum Creatinine (0.6 – 1.5) Teratogen: Substances that cause birth defects. 1st Trimester all major organs forming. Weeks 3-8 are most critical. Drugs cross placenta easier in the 3rd trimester however. Known Teratogens: Thalomid, Lithium, Coumadin, Accutane, Dilantin, Tetracycline Hemolytic Reaction: Happens when patient received wrong blood type (cells lyse and gluconate (clump together). Often apparent within the first 50 mL of administration. S/S: Fever, chills, Low back pain, Chest Tightness, Anxiety. STOP INFUSION IMMEDIATELY! Therapeutic index: Relationship between the desired effect and toxicity. Therapeutic effect is the “desired effect”. Tolerance: Increased amounts of a drug are needed to produce the same effect.Polypharmacy: Multiple drugs taken at the same time for multiple conditions. This increases the risk of drug interactions. Parenteral: Medication given via IV or injection. (IV, IM, SubQ, Intradermal) Idiosyncratic reaction or paradoxical reaction: Unexpected reaction to a medication. NOT an allergic reaction. Additive effect: Taking 2 or more drugs that have similar actions. Cross Sensitivity: When allergic to one drug, a similar type drug will cause the same sensitivity. EX: Penicillin and Cephalosporin’s. Cell-Cycle Specific: Anti-neoplastic drug only works in a “specific” cycle of the tumor-cell reproduction. Cell-Cycle nonspecific: Anti-neoplastic drug that works in any cycle of the tumor-cell cycle. Redman Syndrome: Caused by infusion VANCOMYCIN too quickly. Must infuse over 60 minutes. S/S: Sudden drop in BP, Rash on face, neck, chest, Tachycardia, Fever and chills. Caused by a sudden release of Histamine. Treat by slowing infusion and give Benadryl. Anterograde Amnesia: a form of amnesia, or memory loss, where new events are not transferred to long-term memory. Reye’s Syndrome: Fatal complication if a patient, ages 0-16, is given ASA whilst experiencing a viral infection Pseudo membranous Colitis: Super infection of the GI tract. Caused by Clostridium Difficil. S/S Diarrhea, abd pain, cramping and low-grade fever. Take stool culture and treat with VANCOMYCIN. Medications and Antidotes: Heparin - Protamine Streptokinase - Aminocaproic Acid Coumadin - Vitamin K Morphine - NarcanValium - Flumazicon Tylenol- Mucomist Digoxin - Digibind Conditions and Medications MRSA - Vancomycin C. Difficil (Pseudomemb. Colitis) - Vancomycin Neuroleptic Syndrome - Physostigmine Fatal HTN Crisis - Nipride Selected Values Serum Creatinine 0.6 – 1.5 pH 7.35 – 7.45 BUN 10 – 20 PCO2 35 - 45 AST 7 – 27 HCO3 22 - 28 ALT 1 – 21 PaO2 80 - 100 Na 135 – 145 K+ 3.5 – 5.3 Magnesium 1.5 – 2.3 Calcium 8.5 – 10.5 Chloride 95 – 105 Phosphate 2.5 – 4.5 Normal Urine output 30 mL/hr minimumDRUG TABLES: Alzheimer’s Ammonia Detoxicant/Stimulant Laxative AnalgesicsDRUG CODEINE ROUTE PO IM – SQ/SC ONSET *30-45 MINUTES *10-30 MINUTES COMMENTS *do not administer if solution is discolored *used as antidiarrheal or antitussuve DILIAUDID (Hydromorphone) PO IM IV *30 MINUTES *15 MINUTES *10-15 MINUTES *fast acting, potent narcotic *increase likely to cause appetite loss DEMEROL (Meperidine) PO IM IV *15 MINUTES *10-15 MINUTES * 1 MINUTE *use in clients allergic to morphine *Caution in renal failure-metabolites accumulate *S&S of toxicity CNS irritability *most commonly used for post op pain, sickle cell *children 48 hours or less DRUG MORPHINE SULFATE ROUTE PO IM IV ONSET *60-90 MINUTES *10-30 MINUTES *10 MINUTES COMMENTS *drug of choice for pain relief associated with Myocardial Infarction *monitor for hypotension *drug of choice for chronic cancer pain PROPOXYPHENE HCL PO *15-60 MINUTES *can cause false decrease in urinary steroid secretion test (adrenal gland testing)FENTANYL CITRATE (Duragesic) IM IV INTRADERMAL INTRABUCCAL INTRATHECAL *7-15 MINUTES *in 5 MINUTES *IN 12 HOURS *5-15 MINUTES **IMMEDIATE** *synthetic narcotic like morphine *quicker action and less duration than morphine DRUG ADMINISTRATION ROUTES AND RELATED METHODS ROUTE *ORAL ADMINISTRATION *preferred method *drug level peak 1-2 hours *INTRAMUSCULAR *management of acute & short term pain *onset 30 minutes – peak 1-3 hours – duration 4 hours *RECTAL *for client with nausea or unable to take oral medication *useful in home care & elderly as an alternative to oral and (IV) administration *reduced effectiveness with constipation *IV BOLUS (OR) IV PUSH *most rapid onset (5 minutes) with shortest duration (1hour) *management of acute pain *CONTINUOUS EPIDURAL *catheter threaded into epidural space by physician with a continuous infusion of Fentanyl, Morphine or other analgesic *”high risk” for respiratory depression ROUTE PATIENT-CONTROLLED ANALGESIA (PCA) ADMINISTRATION *pain control allowing the client to prevent or manage pain *physician prescribes drug, dose, lockout interval, & maximum dose *pump records all data related to interactions by the nurse, physician, client*risk of drug overdose if someone other than the client regulates the dosage TRANSDERMAL PATCHES *applied to clean, dry skin *remove old patch & clean skin before applying new patch to new site *document patch removal, new patch site *document on patch date, time when applying patch *duration of patch is based on the type of medication & usage CONTINUOUS SUBCUTANEOUS NARCOTIC INFUSION (CSI) *client who cannot take oral medications & require long term pain management (parental narcotics) *provides a continuous level of analgesia *sites are inspected every 8 hours *sites rotated every 7 days HESI COMMUNITY HEALTH NURSING STUDY GUIDE: Population Groups across the Lifespan & Health Risks Infants Number 1 cause of injury or death is suffocation followed by Motor Vehicle Accident then Homicide. Sudden Infant Death Syndrome Infection is the most significant cause of illness in infants and children. Children Obesity – Healthy people objectives have addressed youth fitness and obesity Defined by using BMI which is a ratio of weight to height Risks for childhood obesity were related to obesity in the parents Obesity rates higher populations such as Native American, Hispanic, and African Americans groups. Lower socioeconomic groups in urban settings have been associated with higher rates Injuries and Accidents- Number one cause of death in ages 1 – 24 yrs. Motor vehicles accidents are the leading cause of death among children and teenagers. Toddlers experience a large number of falls, poisonings, and motor vehicle accidents School age children has the lowest injury death rate; however, this group has difficulty judging speed and distance, placing them at risk for pedestrian and bicycle accidents. Adolescents injury accounts for 75% of all deaths and risk-taking becomes more conscious at this time especially among males. Suicide is the second leading cause of death among youths between the ages of 15 and 24. Suicide s the third leading cause of death among youth between the ages of 10 and 24 years.Acute Illness- also a significant cause of illness in children. Chronic Health Problems- improved medical technology has increased the number of children surviving with chronic health problems. Examples: Down Syndrome, spina bifida, cerebral palsy, asthma, diabetes, congenital heart disease, cancer, hemophilia, broncopulmonary dysplasia, and AIDS Routine immunizations have been very successful in preventing selected diseases. Good nutrition is essential for healthy growth and development and influences disease prevention in later life. Women The women’s health movement was pivotal in bringing national recognition to women’s health issues. Women have a longer life expectancy than men Women are more likely to have acute and chronic conditions that require them to use more services than men. Women of color are more statistically more likely to have poor health outcomes because of poor understanding of health, lack of access to health care, and lifestyle practices. Heart disease leading cause of death in women Lung Cancer leading cause of cancer in women and 2nd leading cause of death Men Men are physiologically the more vulnerable gender, shorter life span and higher infant mortality rate Life expectancy of men in the US is one of the lowest in the developed countries Men engage in more risk-taking behaviors than women Men tend to avoid diagnosis and treatment of illnesses that may result in serious health problems Elderly Steadily growing population Increase in chronic conditions, demand for services, and strained health care budgets More older adults live in the community Nurses address the chronic health concerns of elders with a focus on maintaining or improving self-care and preventing complications to maintain the highest possible quality of life. Assessing the elderly incorporates physical, psychological, social, and spiritual domains. Individual and community focused interventions involve all three levels of prevention through collaborative practice. U.S. Healthcare problems More than 43 million people in the United States are uninsured, and many more simplylack access to adequate health care. Health care reform measures seek to make changes in the cost, quality, and access of the present system. The integration of primary care and public health is necessary for the future health of the nation To achieve the specific health goals of programs such as healthy People 2010, primary care and public health must work within the community for community-based care. The most sustainable individual and system changes come when people who live n the community have actively participated. Nurses are more than able to fill the gap between personal care and public health because they have skills in assessment, health promotion, and disease and injury prevention; knowledge of community resources; and ability to develop relationships with community members and leaders. Home Visits- give a more accurate assessment of the following than do clinical visits: ·117 the family structure ·118 the natural or home environment ·119 behavior in that environment Home visits provide opportunities to identify both barriers and supports for reaching family health promotion goals. Home visits afford the opportunity to gain a more accurate assessment of the family structure and behavior in the natural environment. Home visits also provide opportunities to observe the home environment and to identify both barriers and supports to reducing health risks and reaching family health goals. Parish nurses: nurses who respond to health and wellness needs within the faith context of population of faith communities and are partners with the church in fulfilling the mission of health ministry. Parish nursing: a community-based and population-focused professional nursing practice with faith communities to promote whole person health to its parishioners usually focused on primary prevention. Parish nurse coordinator: a parish nurse who has completed a certificate program designed to develop the nurse as a coordinator of a parish nursing service. Parish nurse services respond to health, healing, and wholeness within the context of the church. Although the emphasis is on health promotion and disease preventionthroughout the life span, the spiritual dimension of nursing is central to the practice. The parish nurse partners with the wellness committee and volunteers to plan programs and consider health-related concerns within faith communities To promote a caring faith community, usual functions of the parish nurse include personal health counseling, health teaching, facilitating linkages and referrals to congregation and community resources, advocating and encouraging support resources, and providing pastoral care. Parish nurses collaborate to plan, implement, and evaluate health promotion activities considering the faith community’s beliefs, rituals, and polity. Healthy People 2010 guidelines are basic to the partnering for the programs. Nurses working in the parish nursing specialty must seek to attain adequate educational and skill preparation for the accountability to those served and to those who have entrusted the nurse to serve Nurses are encouraged to consider innovative approaches to creating caring communities. These may be in congregations as parish nurses, among several faith communities in a single locale, or regionally; or in partnership with other community agencies or models such as block nursing. To sustain oneself as a parish nurse healer, the nurse takes heed to heal and nurture self while supporting individuals, families, and congregation communities in their healing process. Hospice: palliative system of health care for terminally ill people; takes place in the home with family involvement under the direction and supervision of health professionals, especially the visiting nurse. Hospice care takes place in the hospital when sever complications of terminal illness occur or when family becomes exhausted or does not fulfill commitments. Professional Preparedness ·120 Requires nurses and other personnel to be aware of and understand the disaster plans at their workplace and community- participate in mock drills ·121 Adequately prepared nurses will function in leadership capacity and assist towards smoother recovery phase ·122 Fieldwork, shelter management requires creativeness and willingness ·123 American Red Cross provides training for health professionals to adapt existing skills to disaster settingRole of Community Health Nurse ·124 Can initiate or update disaster plans at workplace and community and ensure education, drill participation ·125 Knowledge of vulnerable populations, available community resources ·126 Assessing and reporting of environmental hazards, unsafe equipment, faulty structures, disease outbreaks, e.g., measles, flu Before anything happens: Prepare for Safety in a Disaster : Four steps ·127 Find out what could happen to you: ·128 Determine what types of disasters are most likely to happen ·129 Learn about warning signals in community ·130 Ask about care for pets ·131 Review the disaster plans at workplace, and other places where families spend time together ·132 Determine how to help the elderly or disabled ·133 Create a disaster plan ·134 Discuss types of disasters that are likely to happen and review what to do ·135 Pick 2 types of places to meet ·136 Choose an out-of-state friend to contact ·137 Review evac. Plans ·138 Complete this checklist ·139 Post emergency numbers next to phone ·140 Teach how to call 911 ·141 Determine when and how to turn of water, gas, and electricity ·142 Check adequacy of insurance coverage ·143 Locate and review use of fire extinguishers ·144 Install and maintain smoke detectors ·145 Conduct a home hazard hunt ·146 Stock emergency supplies ·147 CPR certification ·148 Locate all escape routes ·149 Find safe spots ·150 Practice and maintain your plan ·151 Review every 6 mos. ·152 Conduct drills ·153 Replace stored water every 3 mos. and stored food every 6 mos. ·154 Test and recharge fire extinguisher ·155 Test smoke detectors Personal PreparednessNurses who are disaster victims themselves and provide care to others will experience considerable stress. American Red Cross and Federal Emergency Management Agency (FEMA) are two well known authorities on disaster preparedness, response, and recovery Three levels 1st level – Personal Preparedness 2nd level- Professional Preparedness 3rd level- Community Preparedness Most states and counties have an Office of Emergency Management (OEM) that is responsible for developing and coordinating emergency response plans within their defined area. The state office supports local OEMs and other state agencies that participate in disaster response. It provides planning and training services to local governments, including financial and technical assistance. During an actual emergency or disaster, the state OEM coordinates a state response and recovery program if necessary. County OEMs are in charge of creating a comprehensive, all-hazard plan that should address realistic dangers to the community and list available resources. **Nurses need to review the disaster history of community, including how past disasters have affected the health care delivery system, how their particular organizations fit into the plan, and what role they and their organizations are expected to play in a disaster. Stages: Preparedness, Response, and Recovery Preparedness: Know who is at risk, Personal, Professional and Community Preparedness Personal Preparedness ·156 Entails plan for keeping oneself ready for disaster, both mentally and physically ·157 Individuals not personally prepared will have less to give to family, community, job, and other disaster victims ·158 Nurses can be disaster victims- personal preparation needed to attend to patients ·159 Checklist helpful to prepare Professional Preparedness ·160 Requires nurses and other personnel to be aware of and understand the disaster plans at their workplace and community- participate in mock drills ·161 Adequately prepared nurses will function in leadership capacity and assist towards smoother recovery phase ·162 Fieldwork, shelter management requires creativeness and willingness·163 American Red Cross provides training for health professionals to adapt existing skills to disaster setting Community Preparedness ·164 Level of preparedness only as high as people/ organizations in the community make it ·165 Well-prepared communities have written disaster plans, conduct drills, have adequate warning system, and backup evacuation plan ·166 Office of Emergency Management- state/ county office coordinating regional plans ·167 Understanding past disasters can influence planning for future, liabilities in resources Response The primary objective of disaster response is to minimize morbidity and mortality. The level of disaster determines FEMA’s response. Levels are not determined by the number of casualties but by the amount of resources needed. FEMA Levels of Disaster Response ·168 Level III- a minor disaster, involves a minimal level of damage but could result in the president declaring an emergency. A minimal request for federal help ·169 Level II- moderate disaster- likely to result in major disaster being declared. Regional federal resources engaged, other outside area may be called on ·170 Level I- massive disaster, severe damage or multistate scope. Full engagement of federal regional and national resources ·171 Citizens and health professionals must be attached to official agencies with disaster management responsibilities to avoid further risk American Red Cross 3 ways to classify a disaster : ·172 Type- agent that caused the event, such as hurricane, hazmat, transportation ·173 Level- anticipated or actual Red Cross response and relief costs Level I. costs less than $10,000 Level II costs $10,000 or more, but less than $50,000 Level II costs $50,000 or more, but less than $250,000 Level IV costs $250,000 or more but less than $2.5 million Level V costs $2.5 million or more·174 Scope- magnitude of the event, units affected and responding ,e.g., single-family, local, state, major, federally declared Single family – affects an individual or single family- occurs within the jurisdiction of a single Red Cross chapter Local Disaster- Affects more than one family, occurs within the jurisdiction of a single Red Cross chapter State Disaster- Affects multiple families, occurs within the jurisdiction of one or More Red Cross chapters within a single state Major Disaster- has one or more of the following characteristics -coordinated response of multiple Red Cross units - affects more than a single state - creates national news - result in emergency or disaster declaration by the President etc. Presidentially Declared Disaster- requires full or partial implementation of the National Response Plan The National Response Plan Once a federal emergency has been declared, the National Response Plan may take effect, depending on specific needs arising from the disaster. The NRP is a concerted effort to prevent terrorist attacks within the US; reduce American’s vulnerability to terrorism, major disasters, and other emergencies; and minimize the damage and recover from attacks, major disasters, and other emergencies that occur. Role of the Nurse ·175 Role in disaster response depends on nurse’s past experience, role in community disaster preparedness, specialized training, special interest ·176 Community health nurses valued for skills in community assessment, case finding, prevention, education, surveillance, working with aggregates ·177 Plans for triage must begin as soon as rescue workers arrive- highest priority given to life-threatening injuries with high probability of survival- nurse’s accurate assessment info will help match available resources to population’s emergency needs Recovery The recovery stage of disaster occurs as all involved agencies pull together to restore the economic and civic life of the community. For example: the government takes the lead in rebuilding efforts whereas the business community tries to provide economic support. Nurse’s Role in Recovery·178 Multifaceted responsibilities- flexibility required to assist in successful recovery ·179 Teaching health promotion, disease prevention, assessment of physical, psychological problems incurred in cleanup efforts, as well as threat of communicable disease ·180 Case finding, referral for mental distress ·181 Assessment and reporting of environmental health hazards resulting from event Get community back to normal, deal with emotional matters and after effects Assess what might be going on in community using primary, secondary and tertiary care Terrorism Role of the Nurse: ·182 Help people cope with the aftermath of terrorism ·183 Allay public concerns and fears of bioterrorism ·184 Identify the feelings that you and others may be experiencing ·185 Assist victims to think positively and move to the future ·186 Prepare nursing personnel to be effective in a crisis situation Nurses are concerned with anthrax and small pox and should have awareness of these diseases Need to have vaccine for small pox Levels of prevention r/t Disaster Management Primary Prevention- Participate in developing a disaster management plan for the community Secondary Prevention- Assess disaster victims and triage for care Tertiary Prevention- Participate in home visits to uncover dangers that may cause additional injury to victim or cause other problems (e.g. house fires from faulty wiring). Population at Greatest Risk for Disruption After a Disaster Persons with disabilities Persons living on a low income, including the homeless Non-English speaking persons and refugees Persons living alone Single-parent families Persons new to the area Institutionalized persons or those with chronic mental illness Previous disaster victims or victims of traumatic events People who are not citizens or legally documented immigrantsSubstance abusers The five components to a comprehensive public health response to outbreaks of illness are the following ·187 Detecting the outbreak ·188 Determining the cause ·189 Identifying factors that place people at risk ·190 Implementing measures to control the outbreak ·191 Informing the medical and public communities about treatments, health consequences, and preventative measures Triage: the process of separating casualties and allocating treatment on the basis of the victims’ potentials for survival. ·192 Highest priority is always given to victims who have life threatening injuries but who have a high probability of survival once stabilized ·193 Second priority is given to victims with injures that have systemic complications that are not yet life threatening and could wait 45 – 60 minutes for treatment ·194 Last priority is given to those victims with local injuries without immediate complications and who can wait several hours for medical attention. Rationale from Saunders In an emergency department, triage is classifying clients according to their need for care and includes establishing priorities of care. The kind of illness, the severity of the problem, and the resources available govern the process. Clients with trauma, chest pain, severe respiratory distress or cardiac arrest, limb amputation, acute neurological deficits, and those who sustained chemical splashes to the eyes are classified as emergent and are the number 1 priority. Clients with conditions such as a simple fracture, asthma without respiratory distress, fever, hypertension, abdominal pain, or the client with a renal stone have urgent needs and are classified as number 2 priorities. Clients with conditions such as a minor laceration, sprain, or cold symptoms are classified as nonurgent and are the number 3 priority. Older adult health risks Nutrition, safety, social isolation, and depression Need to assess the health literacy of the client first Program outcomes: smoking cessation, weight management, diabetic management ·195 look at the evaluation of the specific outcome·196 Identifying changes in the client’s health status that result from nursing care provides nursing data that demonstrate the contribution of nursing to the health care delivery system. Research studies using the tracer or sentinel method to identify clients’ outcomes and client satisfaction surveys can be used to measure outcome standards. From data, strengths and weaknesses in nursing care delivery can be determined. The most common measurement methods are direct physical observations and interviews. Primary Care- refers to organized community efforts designed to prevent disease and promote health (education). Secondary Care- an intermediate level of health care that includes diagnosis and treatment. Screening. Tertiary Care- rehabilitation and return of a patient to a status of maximum usefulness and a minimum risk of recurrence of a physical or mental disorder Levels of Prevention Primary Prevention- Counsel clients in health behaviors related to lifestyle Secondary Prevention- Implement a family-planning program to prevent unintended pregnancies or young couples who attend the primary clinic Tertiary Prevention- Provide a self-management asthma program for children with chronic asthma to reduce their need for hospitalization (prevent from getting worse) Federal Agencies Many federal agencies are involved in government health care functions. The agency most directly involved with the health and welfare of Americans is the U.S. Department of Health and Human Services U.S. Department of Health and Human Services (USDHHS) Largest health program in the world, its mission is to enhance the health and well-being of the American people through the following: ·197 Alcohol, drug abuse, and mental health programs ·198 Disease tracking and identification ·199 Health care access for all and integrity of the nation’s health entitlement and safety net programs·200 Identification and correction of health hazards ·201 Medical assistance after disasters ·202 Medical research ·203 Promotion of exercise and healthy habits ·204 Protection of the nation’s food and drug supply The Health Resources and Services Administration of the USDHHS contains the Bureau of Health Professions, this bureau includes separate divisions for nursing, medicine, dentistry, public health, and allied health professions The Division of Nursing administers nurse education legislation, interprets trends and nursing needs of the nation’s health care delivery system, and serves as a liaison with the nursing community and with international, state, regional, and local health interests Two other agencies with the DHHS: The National Institute for Nursing Research (NINR) and Healthcare Research and Quality (AHRQ) This institution is the focal point of the nation’s nursing research activities. It promotes the growth and quality of research in nursing and patient care, provides important leadership, expands the pool of experienced nurse researchers, and serves as a point of interaction with other bases of health care research Nurses can apply for support for research, projects, or training from a variety of agencies within the federal government besides the NINR of the Division of Nursing. Other federal agencies: Dept. of Commerce, Dept. of Defense, Dept. of Labor (includes OSHA), Dept. of Agriculture (includes WIC), Dept. of Justice, Food and Drug Administration. Voluntary and Private Nonprofit Agencies Voluntary and private agencies are grouped together as nonprofit home health agencies, voluntary agencies are supported by charities such as United Way, Medicare, Medicaid, other third-party payers, and client payment. The amount of financial assistance the voluntary agency receives depends on the community it serves. With Medicare, the private nonprofit agency emerged as an alternative agency to the public-supported program. These agencies included rehabilitation agencies, based in either rehabilitation facilities or skilled facilities. Nurses use assessment skills to detect potential and actual exposure pathways and outcomes for clients cared for in the acute, chronic, and healthy communities of practice. Risk communication is an important skill and must acknowledge the outrage factorexperienced by communities with environmental hazards. Vulnerable populations- are those groups who have an increased risk to develop adverse health outcomes, vulnerable populations often experience multiple cumulative risks and they are particularly sensitive to the effects of those risks. Vulnerable populations often are more likely than the general populations to suffer from health disparities. Examples of areas that show health disparities across populations groups are infant mortality, childhood immunization rates, and disease-specific mortality rates. Vulnerable Population Groups of Special Concern to Nurses ·205 Poor and homeless people ·206 Pregnant adolescents ·207 Migrant workers and immigrants ·208 Severely mentally ill individuals ·209 Substance abusers ·210 Abused individuals and victims of violence ·211 Persons with communicable disease and those at risk ·212 Persons who are human immunodeficiency virus (HIV positive) or have Hep B or sexually transmitted disease. Behavioral (Lifestyle) Health Risk Assessment Families are the major source of factors that can promote or inhibit positive lifestyles. It is important to look at risks for the family as a unit. Critical dimensions of lifestyle risks include the following: ·213 Value placed on behavior ·214 Knowledge of the behavior and its consequences ·215 Effect of the behavior on the family ·216 Effect of the behavior on the individual ·217 Barriers to performing the behavior ·218 Benefits of the behavior It is important to assess the frequency, intensity, and regularity of specific behaviors. It also is important to evaluate the resources available to the family for implementing the behaviors. Modifiable Risk and Unmodifiable Risks Risk factors that are "unmodifiable," are things that neither you nor your patients can do anything about. You need to know the "unmodifiable" risk factors, because they help you to define high-risk individuals and groups for whom treating or controlling the "modifiable" risk factors is a priority.Modifiable risks can be changed such as smoking. Epidemiology – how to calculate a rate ·219 The denominator includes the numerator Example Crude birth rate Number of live births during 1 year X1000 Midyear population Evaluating Outcomes Outcomes can be measured by looking at changes from before and after the intervention to solve the problems. Changes in the following can be used to see the outcomes of the interventions: ·220 Demographics ·221 Socioeconomic factors ·222 Environmental factors ·223 Individual and community health status ·224 Use of health services In the example of infant malnutrition, one would look for the number of cases of infant malnutrition in the community before providing education to other health providers about assessment of infant development. A time period for evaluation would be chosen and perhaps 1 year later (the time frame). The number of cases of infant malnutrition would be measured to see if a change had occurred and there were fewer cases. Incidence rate- the frequency or rate of new cases of an outcome in a populations; provides an estimate of the risk of disease in that population over the period of observation Prevalence: number of existing cases in a population at a given time Nursing Process- Always assess before starting an intervention Community assessment Most nurses are familiar with the nursing process as it applies to individually focused nursing care. Using it to promote community health makes this same nursing process community focused. Community assessment- the process of critically thinking about the community and involves getting to know and understand the community as partner. The community assessment phase involves a logical, systematic approach to the initial phase of the nursing process. Community assessment helps as follows: ·225 To identify community needs·226 To clarify problems ·227 To identify strengths and resources Assessing the community health requires the following three steps: ·228 Gathering relevant existing data and generating missing data ·229 Developing a composite database ·230 Interpreting the composite database to identify community problems and strengths Data Collection and Interpretation The primary goal of data collection is to get usable information about the community and its health. The systematic collection of data about community health requires the following: ·231 Gathering or compiling existing data ·232 Generating missing data ·233 Interpretation of data ·234 Identifying community health problems and community abilities Data gathering is the process of obtaining existing, readily available data. The following data usually describe the demography of a community ·235 Age of residents ·236 Gender distribution of residents ·237 Socioeconomic characteristics ·238 Racial distributions ·239 Vital statistics, including selected mortality and morbidity data Identify needs, problems, strengths, resources and apply what you know. Windshield survey- are the motorized equivalent of simple observation. They involve the collection of data that “will help define the community, the trends, stability, and changes that will affect the health of the community” School Nurse: ·240 Primary -The school nurse monitors the children for all of their statemandated immunizations for school entry. ·241 Secondary- School nurse is involved in screening children for illnesses and providing direct nursing care ·242 Tertiary – The school nurse cares for children with long-term health needs, including asthma and disabling conditions School nurses carry out catheterizations, suctioning, gastrostomy tube feedings, and other skills in school. The concern for health promotion of adolescents is safety because of their propensity totake part in risky behavior. To effectively reach a population group you must connect with someone in the community and establish trust. Occupational Exposure Job categories Exposure Work-related diseases and conditions Farm workers pesticides, infectious HTN, mood disorders, cardiovascular Agents, gases, sunlight disease Medicare Provides hospital insurance and medical insurance to persons ages 65 years and older, permanently disabled persons, and persons with end-stage renal failure Part A – covers: hospital care and home care (home care or hospice – can’t have both), skilled nursing care Part B- covers: (non-institutional care insurance) Medical care, diagnostic services and physiotherapy. Medicaid- Financial assistance to states and counties to pay for medical services for poor older adults, the blind, the disabled, and families with dependent children. WIC- a special supplemental food program administered by the Department of Agriculture through the state health departments; provides nutritious food that add to the diets of pregnant and nursing women, infants, and children younger than 5 years. Eligibility is based on income and nutritional risk as determined by a health professional Outreach worker: a health worker who makes a special, focused effort to find people with specific health problems for the purpose of increasing their access to health services ·243 evaluate effectiveness find out if successful and use ways to measure success Epidemiologic triangle – agent, host, and environment – changes in one of the elements of the triangle can influence the occurrence of disease by increasing or decreasing a person’s risk for disease. Risk is the probability that an individual will experience an event. Agent: an animate or inanimate factor that must be present or lacking for a disease or condition to develop Host: a living species (human or animal) capable of being infected or affected by an agent Environment- all that is internal or external to a given host or agent and that is influenced and influences the host and/or agent Agent- an animate or inanimate factor that must be present or lacking for a disease orcondition to develop ·244 causive – example: E. coli ·245 Infectious agents (bacteria, viruses, fungi, parasites) ·246 Chemical agents (heavy metal, toxic chemicals, pesticides) ·247 Physical agents (radiation, heat, cold, machinery) Host- a living species (human or animal) capable of being infected or affected by an agent ·248 anything capable of being infected ·249 Genetic susceptibility ·250 Immutable characteristics (age, sex) ·251 Acquired characteristics (immunologic status) ·252 Lifestyle factors (diet, exercise) Environment- all that is internal or external to a given host or agent and that is influences the host and or agent ·253 anything external ·254 climate (temperature, rainfall) ·255 Plant and animal life (agents or reservoirs or habitats for agents) ·256 Human population distribution (crowding, social support) ·257 Socioeconomic factors (education, resources, access to care) ·258 Working conditions (levels of stress, noise, satisfaction) Relationship between the above 3 cause disease, try to break the connection, if a break then there will be no disease. Web of Causality- complex interrelations of factors interacting with each other to influence the risk for or distribution outcomes. ·259 recognizes the complex interrelationships of many factors interacting, sometimes in subtle ways, to increase (or decrease) the risk of disease. ·260 Associations are sometimes mutual, with lines of causality going in both directions Family assessment Ecomap- represents the family’s interactions with other groups and organizations, accomplished by using a series of circles and lines. ·261 It is represented by a circle in the middle of the page ·262 Other groups and organizations are then indicated by circles ·263 Lines representing the flow of energy are drawn between the family circle and the circles representing other groups and organizations ·264 An arrowhead at the end of each line indicates the direction of the flow of energy (into or out of the family) ·265 The weight of the line indicates the intensity of the energyGenogram- is a pictorial display of a person's family relationships and medical history. It goes beyond a traditional family tree by allowing the user to visualize hereditary patterns and psychological factors that punctuate relationships. It can be used to identify repetitive patterns of behavior and to recognize hereditary tendencies. Prevention Strategies for Violence Individual and Family levels ·266 Assess during routine examination (secondary) ·267 Assess for marital discord (secondary) ·268 Educate on developmental stages and needs of children (primary) ·269 Counsel for at-risk parents (secondary) ·270 Teach parenting techniques (primary) ·271 Assist with controlling anger (secondary) ·272 Treat for substance abuse (tertiary) ·273 Teach stress-reduction techniques (primary) Community Level ·274 Develop policy ·275 Conduct community resource mapping ·276 Collaborate with community to develop systematic response to violence ·277 Develop media campaign ·278 Develop resources such as transition housing and shelters High school students and middle school students- steer away from violence and teach to work on their own skills and build their self-esteem.HESI QUESTIONS AND ANSWERS COMPLIATION: Please refer to HESI book. MEDICAL SURGICAL NURSING RESPIRATORY SYSTEM: ·279 List 4 common symptoms of pneumonia the nurse might note on a physical exam. ·280 Tachypnea, fever with chills, productive cough, bronchial breath sounds. ·281 State 4 nursing interventions for assisting the client to cough productively. ·282 Deep breathing, fluid intake increased to 3 liters/day, use humidity to loosen secretions, suction airway to stimulate coughing. ·283 What symptoms of pneumonia might the nurse expect to see in an older client? ·284 Confusion, lethargy, anorexia, rapid respiratory rate. ·285 What should the O2 flow rate be for the client with COPD? ·286 1-2 liters per nasal cannula, too much O2 may eliminate the COPD client’s stimulus to breathe, a COPD client has hypoxic drive to breathe. ·287 How does the nurse prevent hypoxia during suctioning? ·288 Deliver 100% oxygen (hyperinflating) before and after each endotracheal suctioning. ·289 During mechanical ventilation, what are three major nursing intervention? ·290 Monitor client’s respiratory status and secure connections, establish a communication mechanism with the client, keep airway clear by coughing/suctioning. ·291 When examining a client with emphysema, what physical findings is the nurse likely to see? ·292 Barrel chest, dry or productive cough, decreased breath sounds, dyspnea, crackles in lung fields. ·293 What is the most common risk factor associated with lung cancer? ·294 Smoking ·295 Describe the pre-op nursing care for a client undergoing a laryngectomy. ·296 Involve family/client in manipulation of tracheostomy equipment before surgery, plan acceptable communication method, refer to speech pathologist, discuss rehabilitation program. ·297 List 5 nursing interventions after chest tube insertion. ·298 Maintain a dry occlusive dressing to chest tube site at all times. Check all connections every 4 hours. Make sure bottle III or end of chamber is bubbling. Measure chest tube drainage by marking level on outside of drainage unit. Encourage use of incentive spirometry every 2 hours. ·299 What immediate action should the nurse take when a chest tube becomes disconnected from a bottle or a suction apparatus? What should the nurse do if a chest tube is accidentally removed from the client?·300 Place end in container of sterile water. Apply an occlusive dressing and notify physician STAT. ·301 What instructions should be given to a client following radiation therapy? ·302 Do NOT wash off lines; wear soft cotton garments, avoid use of powders/creams on radiation site. ·303 What precautions are required for clients with TB when placed on respiratory isolation? ·304 Mask for anyone entering room; private room; client must wear mask if leaving room. ·305 List 4 components of teaching for the client with tuberculosis. ·306 Cough into tissues and dispose immediately into special bags. Long-term need for daily medication. Good handwashing technique. Report symptoms of deterioration, i.e., blood in secretions. RENAL SYSTEM: ·307 Differentiate between acute renal failure and chronic renal failure. ·308 Acute renal failure: often reversible, abrupt deterioration of kidney function. Chronic renal failure: irreversible, slow deterioration of kidney function characterized by increasing BUN and creatinine. Eventually dialysis is required. ·309 During the oliguric phase of renal failure, protein should be severely restricted. What is the rationale for this restriction? ·310 Toxic metabolites that accumulate in the blood (urea, creatinine) are derived mainly from protein catabolism. ·311 Identify 2 nursing interventions for the client on hemodialysis. ·312 Do NOT take BP or perform venipunctures on the arm with the A-V shunt, fistula, or graft. Assess access site for thrill or bruit. ·313 What is the highest priority nursing diagnosis for clients in any type of renal failure? ·314 Alteration in fluid and electrolyte balance. ·315 A client in renal failure asks why he is being given antacids. How should the nurse reply? ·316 Calcium and aluminum antacids bind phosphates and help to keep phosphates from being absorbed into blood stream thereby preventing rising phosphate levels, and must be taken with meals. ·317 List 4 essential elements of a teaching plan for clients with frequent urinary tract infections. ·318 Fluid intake 3 liters/day; good handwashing; void every 2-3 hours during waking hours; take all prescribed medications; wear cotton undergarments. ·319 What are the most important nursing interventions for clients with possible renal calculi? ·320 Strain all urine is the MOST IMPORTANT intervention. Other interventions include accurate intake and output documentation and administer analgesics as needed. ·321 What discharge instructions should be given to a client who has had urinary calculi? ·322 Maintain high fluid intake 3-4 liters per day. Follow-up care (stones tend to recur). Follow prescribed diet based in calculi content. Avoid supine position.·323 Following transurethral resection of the prostate gland (TURP), hematuria should subside by what post-op day? ·324 Fourth day ·325 After the urinary catheter is removed in the TURP client, what are 3 priority nursing actions? ·326 Continued strict I&O; continued observations for hematuria; inform client burning and frequency may last for a week. ·327 After kidney surgery, what are the primary assessments the nurse should make? ·328 Respiratory status (breathing is guarded because of pain); circulatory status (the kidney is very vascular and excess bleeding can occur); pain assessment; urinary assessment most importantly, assessment of urinary output. CARDIOVASCULAR SYSTEM: ·329 How do clients experiencing angina describe that pain? ·330 Described as squeezing, heavy, burning, radiates to left arm or shoulder, transient or prolonged. ·331 Develop a teaching plan for the client taking nitroglycerin. ·332 Take at first sign of anginal pain. Take no more than 3, five minutes apart. Call for emergency attention if no relief in 10 minutes. ·333 List the parameters of blood pressure for diagnosing hypertension. ·334 >140/90 ·335 Differentiate between essential and secondary hypertension. ·336 Essential has no known cause while secondary hypertension develops in response to an identifiable mechanism. ·337 Develop a teaching plan for the client taking antihypertensive medications. ·338 Explain how and when to take med, reason for med, necessary of compliance, need for follow-up visits while on med, need for certain lab tests, vital sign parameters while initiating therapy. ·339 Describe intermittent claudication. ·340 Pain related to peripheral vascular disease occurring with exercise and disappearing with rest. ·341 Describe the nurse’s discharge instructions to a client with venous peripheral vascular disease. ·342 Keep extremities elevated when sitting, rest at first sign of pain, keep extremities warm (but do NOT use heating pad), change position often, avoid crossing legs, wear unrestrictive clothing. ·343 What is often the underlying cause of abdominal aortic aneurysm? ·344 Atherosclerosis. ·345 What lab values should be monitored daily for the client with thrombophlebitis who is undergoing anticoagulant therapy? ·346 PTT, PT, Hgb, and Hct, platelets. ·347 When do PVCs (premature ventricular contractions) present a grave danger?·348 When they begin to occur more often than once in 10 beats, occur in 2s or 3s, land near the T wave, or take on multiple configurations. ·349 Differentiate between the symptoms of left-sided cardiac failure and right-sided cardiac failure. ·350 Left-sided failure results in pulmonary congestion due to back-up of circulation in the left ventricle. Right-sided failure results in peripheral congestion due to back-up of circulation in the right ventricle. ·351 List 3 symptoms of digitalis toxicity. ·352 Dysrhythmias, headache, nausea and vomiting ·353 What condition increases the likelihood of digitalis toxicity occurring? ·354 When the client is hypokalemic (which is more common when diuretics and digitalis preparations are given together). ·355 What life style changes can the client who is at risk for hypertension initiate to reduce the likelihood of becoming hypertensive? ·356 Cease cigarette smoking if applicable, control weight, exercise regularly, and maintain a lowfat/low-cholesterol diet. ·357 What immediate actions should the nurse implement when a client is having a myocardial infarction? ·358 Place the client on immediate strict bedrest to lower oxygen demands of heart, administer oxygen by nasal cannula at 2-5 L/min., take measures to alleviate pain and anxiety (administer prn pain medications and anti-anxiety medications). ·359 What symptoms should the nurse expect to find in the client with hypokalemia? ·360 Dry mouth and thirst, drowsiness and lethargy, muscle weakness and aches, and tachycardia. ·361 Bradycardia is defined as a heart rate below ___ BPM. Tachycardia is defined as a heart rate above ___ BPM. ·362 bradycardia 60 bpm; tachycardia 100 bpm ·363 What precautions should clients with valve disease take prior to invasive procedures or dental work? ·364 Take prophylactic antibiotics. GASTROINTESTINAL SYSTEM: ·365 List 4 nursing interventions for the client with a hiatal hernia. ·366 Sit up while eating and one hour after eating. Eat small, frequent meals. Eliminate foods that are problematic. ·367 List 3 categories of medications used in the treatment of peptic ulcer disease. ·368 Antacids, H2 receptor-blockers, mucosal healing agents, proton pump inhibitors. ·369 List the symptoms of upper and lower gastrointestinal bleeding. ·370 Upper GI: melena, hematemesis, tarry stools. Lower GI: bloddy stools, tarry stools. Similar: tarry stools. ·371 What bowel sound disruptions occur with an intestinal obstruction?·372 Early mechanical obstruction: high-pitched sounds; late mechanical obstruction: diminished or absent bowel sounds. ·373 List 4 nursing interventions for post-op care of the client with a colostomy. ·374 Irrigate daily at same time; use warm water for irrigations; wash around stoma with mild soap/water after each colostomy bag change; pouch opening should extend at least 1/8 inch around the stoma. ·375 List the common clinical manifestations of jaundice. ·376 Sclera-icteric (yellow sclera), dark urine, chalky or clay-colored stools ·377 What are the common food intolerances for clients with cholelithiasis? ·378 Fried/spicy or fatty foods. ·379 List 5 symptoms indicative of colon cancer. ·380 Rectal bleeding, change in bowel habits, sense of incomplete evacuation, abdominal pain with nausea, weight loss. ·381 In a client with cirrhosis, it is imperative to prevent further bleeding and observe for bleeding tendencies. List 6 relevant nursing interventions. ·382 Avoid injectons, use small bore needles for IV insertion, maintain pressure for 5 minutes on all venipuncture sites, use electric razor, use soft-bristle toothbrush for mouth care, check stools and emesis for occult blood. ·383 What is the main side effect of lactulose, which is used to reduce ammonia levels in clients with cirrhosis? ·384 Diarrhea. ·385 List 4 groups who have a high risk of contracting hepatitis. ·386 Homosexual males, IV drug users, recent ear piercing or tattooing, and health care workers. ·387 How should the nurse administer pancreatic enzymes? ·388 Give with meals or snacks. Powder forms should be mixed with fruit juices. ENDOCRINE SYSTEM: ·389 What diagnostic test is used to determine thyroid activity? ·390 T3 and T4 ·391 What condition results from all treatments for hyperthyroidism? ·392 Hypothyroidism, requiring thyroid replacement ·393 State 3 symptoms of hyperthyroidism and 3 symptoms of hypothyroidism. ·394 Hyperthyroidism: weight loss, heat intolerance, diarrhea. Hypothyroidism: fatigue, cold intolerance, weight gain. ·395 List 5 important teaching aspects for clients who are beginning corticosteroid therapy. ·396 Continue medication until weaning plan is begun by physician, monitor serum potassium, glucose, and sodium frequently; weigh daily, and report gain of >5lbs./wk; monitor BP and pulse closely; teach symptoms of Cushing’s syndrome ·397 Describe the physical appearance of clients who are Cushinoid.·398 Moon face, obesity in trunk, buffalo hump in back, muscle atrophy, and thin skin. ·399 Which type of diabetic always requires insulin replacement? ·400 Type I, Insulin-dependent diabetes mellitus (IDDM) ·401 What type of diabetic sometimes requires no medication? ·402 Type II, Non-insulin dependent diabetes mellitus (NIDDM) ·403 List 5 symptoms of hyperglycemia. ·404 Polydipsia, polyuria, polyphagia, weakness, weight loss ·405 List 5 symptoms of hypoglycemia. ·406 Hunger, lethargy, confusion, tremors or shakes, sweating ·407 Name the necessary elements to include in teaching the new diabetic. ·408 Teach the underlying pathophysiology of the disease, its management/treatment regime, meal planning, exercise program, insulin administration, sick-day management, symptoms of hyperglycemia (not enough insulin) ·409 In less than ten steps, describe the method for drawing up a mixed dose of insulin (regular with NPH). ·410 Identify the prescribed dose/type of insulin per physician order; store unopened insulin in refrigerator. If opened, may be kept at room temperature for up to 3 months. Draw up regular insulin FIRST. Rotate injection sites. May reuse syringe by recapping and storing in refrigerator. ·411 Identify the peak action time of the following types of insulin: rapid-acting regular insulin, intermediate-acting, long-acting. ·412 Rapid-acting regular insulin: 2-4 hrs. Immediate-acting: 6-12 hrs. Long-acting: 14-20 hrs. ·413 When preparing the diabetic for discharge, the nurse teaches the client the relationship between stress, exercise, bedtime snacking, and glucose balance. State the relationship between each of these. ·414 Stress and stress hormones usually increase glucose production and increase insulin need; exercise can increase the chance for an insulin reaction, therefore, the client should always have a sugar snack available when exercising (to treat hypoglycemia); bedtime snacking can prevent insulin reactions while waiting for long-acting insulin to peak. ·415 When making rounds at night, the nurse notes that an insulin-dependent client is complaining of a headache, slight nausea, and minimal trembling. The client’s hand is cool and moist. What is the client most likely experiencing? ·416 Hypoglycemia/insulin reaction. ·417 Identify 5 foot-care interventions that should be taught to the diabetic client. ·418 Check feet daily & report any breaks, sores, or blisters to health care provider, wear well-fitting shoes; never go barefoot or wear sandals, never personally remove corns or calluses, cut or file nails straight across; wash daily with mild soap & warm water. MUSCULOSKELETAL SYSTEM: ·419 Differentiate between rheumatoid arthritis and degenerative joint disease in terms of joint involvement. ·420 Rheumatoid arthritis occurs bilaterally. Degenerative joint disease occurs asymmetrically.·421 Identify the categories of drugs commonly used to treat arthritis. ·422 NSAIDs (nonsteroidal anti-inflammatory drugs) of which salicylates are the cornerstones (used when arthritic symptoms are severe). ·423 Identify pain relief interventions for clients with arthritis. ·424 Warm, moist heat (compresses, baths, showers), diversionary activities (imaging, distraction, self-hypnosis, biofeedback), and medications. ·425 What measures should the nurse encourage female clients to take to prevent osteoporosis? ·426 Estrogen replacement after menopause, high calcium and vitamin D intake beginning in early adulthood, calcium supplements after menopause, and weight-bearing exercise. ·427 What are the common side effects of salicylates? ·428 GI irritation, tinnitus, thrombocytopenia, mild liver enzyme elevation. ·429 What is the priority nursing intervention used with clients taking NSAIDs? ·430 Administer or teach client to take drugs with food or milk. ·431 List 3 of the most common joints that are replaced. ·432 Hip, knee, finger. ·433 Describe post-op stump care (after amputation) for the 1st 48 hours. ·434 Elevate stump first 24 hours. Do not elevate stump after 48 hours. Keep stump in extended position and turn prone three times a day to prevent flexion contracture. ·435 Describe nursing care for the client who is experiencing phantom pain after amputation. ·436 Be aware that phantom pain is real and will eventually disappear. Administer pain medication; phantom pain responds to medication. ·437 A nurse discovers that a client who is in traction for a long bone fracture has a slight fever, is short of breath, and is restless. What does the client most likely have? ·438 Fat embolism, which is characterized by hypoxemia, respiratory distress, irritability, restlessness, fever and petechiae. ·439 What are the immediate nursing actions if fat embolization is suspected in a fracture/orthopedic client? ·440 Notify physician STAT, draw blood gas results, assist with endotracheal intubation and treatment of respiratory failure. ·441 List 3 problems associated with immobility. ·442 Venous thrombosis, urinary calculi, skin integrity problems. ·443 List 3 nursing interventions for the prevention of thromboembolism in immobilized clients with musculoskeletal problems. ·444 Passive range of motion exercises, elastic stockings, and elevation of foot of bed 25 degrees to increase venous return. NEUROSENSORY/NEUROLOGICAL SYSTEMS: ·445 What are the classifications of the commonly prescribed eye drops for glaucoma? ·446 Parasympathominetics for pupillary constriction. Beta-adrenergic receptor-blocking agents toinhibit formation of aqueous humor. Carbonic anhydrase inhibitors to reduce aqueous humor production, and prostaglandin agonists to increase aqueous humor outflow. ·447 Identify 2 types of hearing loss. ·448 Conductive (transmission of sound to inner ear is blocked) and sensorineural (damage to 8th cranial nerve) ·449 Write 4 nursing interventions for the care of the blind person and 4 nursing interventions for the care of the deaf person. ·450 Care of the blind: announce presence clearly, call by name, orient carefully to surroundings, guide by walking in front of client with his/her hand in your elbow. Care of deaf: reduce distraction before beginning conversation, look and listen to client, give client full attention if they are a lip reader, face client directly. ·451 In your own words describe the Glasgow Coma Scale. ·452 An objective assessment of the level of consciousness based on a score of 3 to 15, with scores of 7 or less indicative of coma. ·453 List 4 nursing diagnoses for the comatose client in order of priority. ·454 Ineffective breathing pattern, ineffective airway clearance, impaired gas exchange, and decreased cardiac output. ·455 State 4 independent nursing interventions to maintain adequate respirations, airway, and oxygenation in the unconscious client. ·456 Position for maximum ventilation (prone or semi-prone and slightly to one side), insert airway if tongue obstructing; suction airway efficiently, monitor arterial pO2 and pCO2 and hyperventilate with 100% oxygen before suctioning. ·457 Who is at risk for cerebral vascular accidents? ·458 Persons with history of hypertension, previous TIAs, cardiac disease (atrial flutter/fibrillation), diabetes, oral contraceptive use, and the elderly. ·459 Complications of immobility include the potential for thrombus development. State 3 nursing interventions to prevent thrombi. ·460 Frequent range of motion exercises, frequent (q2h) position changes, and avoidance of positions which decrease venous return. ·461 List 4 rationales for the appearance of restlessness in the unconscious client. ·462 Anoxia, distended bladder, covert bleeding, or a return to consciousness ·463 What nursing interventions prevent corneal drying in a comatose client? ·464 Irrigation of eyes PRN with sterile prescribed solution, application of opthalmic ointment q8h, close assessment for corneal ulceration/drying. ·465 When a comatose client on IV hyperalimentation begin to receive tube feedings instead? ·466 When peristalsis resumes as evidenced by active bowel sounds, passage of flatus or bowel movement. ·467 What is the most important principle in a bowel management program for a neurologic client? ·468 Establishment of REGULARITY·469 Define cerebral vascular accident. ·470 A disruption of blood supply to a part of the brain, which results in sudden loss of brain function. ·471 A client with a diagnosis of CVA presents with symptoms of aphasia, right hemiparesis, but no memory or hearing deficit. In what hemisphere has the client suffered a lesion? ·472 Left ·473 What are the symptoms of spinal shock? ·474 Hypotension, bladder and bowel distention, total paralysis, lack of sensation below lesion. ·475 What are the symptoms of autonomic dysreflexia? ·476 Hypertension, bladder and bowel distention, exaggerated autonomic responses, headache, sweating, goose bumps, and bradycardia ·477 What is the most important indicator of increased ICP? ·478 A change in the level of responsiveness ·479 What vital sign changes are indicative of increased ICP? ·480 Increased BP, widening pulse pressure, increased or decreased pulse, respiratory irregularities and temperature increase. ·481 A neighbor calls the neighborhood nurse stating that he was knocked hard to the floor by his very hyperactive dog. He is wondering what symptoms would indicate the need to visit an emergency room. What should the nurse tell him to do? ·482 Call his physician now and inform him/her of the fall. Symptoms needing medical attention would include vertigo, confusion or any subtle behavioral change, headache, vomiting, ataxia (imbalance), or seizure. ·483 What activities and situations should be avoided that increase ICP? ·484 Change in bed position, extreme hip flexion, endotracheal suctioning, compression of jugular veins, coughing, vomiting, or straining of any kind. ·485 How do Hyperosmotic agents (osmotic diuretics) used to treat intracranial pressure act? ·486 Dehydrate the brain and reduce cerebral edema by holding water in the renal tubules to prevent reabsorption, and by drawing fluid from the extravascular spaces into the plasma. ·487 Why should narcotics be avoided in clients with neurologic impairment? ·488 Narcotics mask the level of responsiveness as well as pupillary response. ·489 Headache and vomiting are symptoms of many disorders. What characteristics of these symptoms would alert the nurse to refer a client to a neurologist? ·490 Headache which is more severe upon awakening and vomiting not associated with nausea are symptoms of a brain tumor. ·491 How should the head of the bed be positioned for post-craniotomy clients with infratentorial lesions? ·492 Infratentorial – FLAT; Supratentorial – elevated ·493 Is multiple sclerosis thought to occur because of an autoimmune process? ·494 YES·495 Is paralysis always a consequence of spinal cord injury? ·496 NO ·497 What types of drugs are used in the treatment of myasthenia gravis? ·498 Anticholinesterase drugs, which inhibit the action of cholinesterase at the nerve endings to promote the accumulation of acetylcholine at receptor sires, which should improve neuronal transmission to muscles. HEMATOLOGY/ONCOLOGY: ·499 List 3 potential causes of anemia. ·500 Diet lacking in iron, folate and/or vitamin B12; use of salicylates, thiazides, diuretics; exposure to toxic agents such as lead or insecticides. ·501 Write 2 nursing diagnoses for the client suffering from anemia. ·502 Activity intolerance and altered tissue perfusion. ·503 What is the only intravenous fluid compatible with blood products? ·504 Normal saline ·505 What actions should the nurse take if a hemolytic transfusion reaction occurs? ·506 Turn off transfusion. Take temperature. Send blood being transfused to lab. Obtain urine sample. Keep vein patent with normal saline. ·507 List 3 interventions for clients with a tendency to bleed. ·508 Use a soft toothbrush, avoid salicylates, do not use suppositories. ·509 Identify 2 sites, which should be assessed for infection in immunosuppressed clients. ·510 Oral cavity and genital area. ·511 Name 3 food sources of vitamin b12. ·512 Glandular meats (liver), milk, green leafy vegetables. ·513 Describe care of invasive catheters and lines. ·514 Use strict aseptic technique. Change dressings 2 to 3 times/week or when soiled. Use caution when piggybacking drugs, check purpose of line and drug to be infused. Use lines for obtaining blood samples to avoid “sticking” client when possible. ·515 List 3 safety precautions for the administration of antineoplastic chemotherapy. ·516 Double check order with another nurse. Check for blood return prior to administration to ensure that medication does not go into tissue. Use a new IV site daily for peripheral chemotherapy. Wear gloves when handling the drugs, and dispose of waste in special containers to avoid contact with toxic substances. ·517 Describe the use of Leucovorin. ·518 Leucovorin is used as an antidote with methotrexate to prevent toxic reactions. ·519 Describe the method of collecting the trough and peak blood levels of antibiotics. ·520 Collection of trough: draw blood 30 minutes prior to administration of antibiotic. Collection of peak: draw blood 30 minutes after administration of antibiotic.·521 What is the characteristic cell found in Hodgkin’s disease? ·522 Reed-Sternberg ·523 List 4 nursing interventions for care of the client with Hodgkin’s disease. ·524 Protect from infection. Observe for anemia. Encourage high-nutrient foods. Provide emotional support to client and family. ·525 List 4 topics you would cover when teaching an immunosuppressed client about infection control. ·526 Handwashing technique. Avoid infected persons. Avoid crowds. Maintain daily hygiene to prevent spread of microorganisms. REPRODUCTIVE SYSTEM: ·527 What are the indications for a hysterectomy in the client who has fibromas? ·528 Severe menorrhagia leading to anemia, severe dysmenorrhea requiring narcotic analgesics, severe uterine enlargement causing pressure on other organs, severe low back and pelvic pain. ·529 List the symptoms and conditions associated with cystocele. ·530 Symptoms include incontinence/stress incontinence, urinary retention, and recurrent bladder infections. Conditions associated with cystocele include multiparity, trauma in childbirth, and aging. ·531 What are the most important nursing interventions for the postoperative client who has had a hysterectomy with an A&P repair? ·532 Avoid rectal temps and/or rectal manipulation; manage pain; and encourage early ambulation. ·533 Describe the priority nursing care for the client who has had radiation implants. ·534 Do not permit pregnant visitors or pregnant caretakers in room. Discourage visits by small children. Confine client to room. Nurse must wear radiation badge. Nurse limits time in room. Keep supplies and equipment within client’s reach. ·535 What screening tool is used to detect cervical cancer? What are the American Cancer Society’s recommendations for women ages 30 to 70 with three consecutive normal results? ·536 Pap smear. Women ages 30 to 70 with 3 consecutive normal results may have pap smear every 2 to 3 years. ·537 Cite 2 nursing diagnoses for a client undergoing a hysterectomy for cervical cancer. ·538 Altered body image related to uterine removal. Pain related to postoperative incision. ·539 What are the 3 most important tools for early detection of breast cancer? How often should these tools be used? ·540 Breast self-exam monthly; mammogram baseline at age 35 followed by exams every 1 to 2 years in 40s and every year after age 50; physical examination by a professional skilled in examination of the breast. ·541 Describe 3 nursing interventions to help decrease edema post mastectomy. ·542 Position arm on operative side on pillow. Avoid BP measurements, injections, or venipunctures in operative arm. Encourage hand activity and use. ·543 Name 3 priorities to include in a discharge plan for the client who has had a mastectomy.·544 Arrange for Reach-to-Recovery visit. Discuss the grief process with the client. Have physician discuss with the client the reconstruction options. ·545 What is the most common cause of nongonococcal urethritis? ·546 Chlamydia trachomatis ·547 What is the causative agent for syphilis? ·548 Treponema pallidum (spirochete bacteria) ·549 Malodorous, frothy, greenish-yellow vaginal discharge is characteristic of which STD? ·550 Trichomonas vaginalis ·551 Which STD is characterized by remissions and exacerbations in both males and females? ·552 Herpes Simplex Type II ·553 Outline a teaching plan for the client with an STD. ·554 Signs and symptoms of STD. Mode of transmission. Avoid sex while infected. Provide concise written instructions regarding treatment and request a return verbalization to ensure the client understands. Teach “safer sex” practices. BURNS: ·555 List 4 categories of burns. ·556 Thermal, radiation, chemical, electrical ·557 Burn depth is a measure of severity. Describe the characteristics of superficial partialthickness, deep partial-thickness, and full-thickness burns. ·558 Superficial partial-thickness: 1st degree = pink to red skin (i.e., sunburn), slight edema, and pain relieved by cooling. Deep partial-thickness: 2nd degree = destruction of epidermis and upper layers of dermis; white or red, very edematous, sensitive to touch and cold air, hair does not pull out easily. Full-thickness: 3rd degree = total destruction of dermis and epidermis; reddened areas do not blanch with pressure, not painful, inelastic, waxy white skin to brown, leathery eschar. ·559 Describe fluid management in the emergent phase, acute phase, and rehabilitation phase of the burned client. ·560 Stage I (Emergent phase): Replacement of fluids is titrated to urine output. Stage II (Acute phase): Maintain patent infusion site in case supplemental IV fluids are needed; heparin lock is helpful; may use colloids. Stage III (Rehabilitation phase): No extra fluids needed, but high-protein drinks are recommended. ·561 Describe pain management of the burned client. ·562 Administer pain medication, especially prior to dressing wound (usually Morphine 10 mg). Teach distraction/relaxation techniques. Teach use of guided imagery. ·563 Outline admission care of the burned client. ·564 Provide a patent airway as intubation may be necessary. Determine baseline data. Initiate fluid and electrolyte therapy. Administer pain medication. Determine depth and extent of burn. Administer tetanus toxoid. Insert NG tube. ·565 Nutritional status is a major concern when caring for a burned client. List 3 specific dietary interventions used with burned clients. ·566 High-calorie, high-protein, high-carbohydrate diet. Medications with juice or milk. NO “free” water. Tube feeding at night. Maintain accurate, daily calorie counts. Weigh client daily.·567 Describe the method of extinguishing each of the following burns: thermal, chemical and electrical. ·568 Thermal: remove clothing, immerse in tepid water. Chemical: flush with water or saline. Electrical: separate client from electrical source. ·569 List 4 signs of an inhalation burn. ·570 Singed nasal hairs, circumoral burns; sooty or bloody sputum, hoarseness, and pulmonary signs including: assymetry of respirations, rales or wheezing. ·571 Why is the burned client allowed NO “free” water? ·572 Water may interfere with electrolyte balance. Client needs to ingest food products with highest biological value. ·573 Describe an autograft. ·574 Use of client’s own skin for grafting. PSYCHIATRIC NURSING THERAPEUTIC COMMUNICATION TREATMENT MODALITIES: ·575 After the 4th group meeting, the informal leader makes a statement that she believes she can help the group more than the assigned facilitator and has better credentials. Identify the group dynamics and stage of development. ·576 The informal leader is “testing,” which is a behavior indicative of a new group trying to establish trust. This group is still in the orientation phase of development. ·577 On an in-patient psychiatric unit, clients are expected to get up at a certain time, attend breakfast at a certain time, and come for their medication at the correct time. What form of therapy is incorporated into this unit? - Milieu. ·578 The wife of a man killed in a motor vehicle accident has just arrived at the emergency room and is told of her husband’s death. What nursing actions are appropriate for dealing with this crisis? ·579 Take woman to a quiet room, ask her if there are family, friends, or clergy you can call for her. Assess her need for medication and discuss with physician. Stay with her, be firm and directive, and assess previous successful coping strategies. ·580 A 10 yr. old is admitted to the children’s unit of the psychiatric facility after stabbing his sister. His behavior is extremely aggressive with the other children on the unit. Using a behavior modification approach with positive reinforcement, design a treatment plan for this child. ·581 Assess what activities he enjoys. Set up a token system – when he displays non-aggressive behavior, he earns a token good towards participating in the activity selected. He loses a token when he becomes aggressive. ·582 The 10 yr. old, his sister, mother, and the mother’s live in boyfriend are asked to attend a therapy meeting. Who is the “client” that will be treated during this session? ·583 The entire family. ·584 A 66 yr. old woman is admitted to the psychiatric unit with agitated depression. She has not responded to antidepressants in the past. What would be the medical treatment of choice for this client? ·585 Electroconvulsive therapy (ECT).·586 Describe the nurse’s role in preparing clients for electroconvulsive therapy (ECT). ·587 Give accurate, non-judgmental information about the treatment. Explore client’s concerns. Administer the following as ordered: Atropine sulfate to dry oral secretions, a quick-acting barbiturate to induce anesthesia such as Brevital Sodium, and a muscle relaxant such as Anectine. Check emergency equipment and O2 are available. ·588 Describe the nursing interventions used to care for a client during and after electroconvulsive therapy. ·589 Maintain patent airway. Check vital signs every 15 minutes until alert. Remain with client following treatment until conscious. Reorient, if confused. ANXIETY DISORDERS: ·590 State 5 autonomic responses to anxiety. ·591 Shortness of breath, heart palpitations, dizziness, diaphoresis, frequent urination. ·592 Identify the defense mechanism used by a person who feels guilty about masturbating as a child, and develops a hand-washing compulsion as an adult. ·593 Undoing. ·594 Identify anxiety-reducing strategies the nurse can teach. ·595 Deep breathing techniques, visualization, relaxation techniques, exercise, biofeedback. ·596 Which levels of anxiety facilitate learning? ·597 Mild to moderate. ·598 A Vietnam veteran is plagued by nightmares and is found trying to strangle his roommate one night. List, in order of priority, the appropriate nursing interventions. ·599 Protect roommate from harm. Stay with client. If the client is agitated, administer anti-anxiety medications as ordered. Arrange for private room. Place client on homicidal precautions at night. ·600 A client displays a phobic response to flying. Describe the desensitization process, which would probably be implemented. ·601 Talk about planes. Look at pictures of planes. Make plans to accompany client during a visit to airport. Accompany client into a plane. Allow the client to board a plane alone. Accompany the client on a short flight while listening to a relaxation tape. ·602 A client is in the middle of an extensive ritual, which focuses on food during lunch. However, the client is scheduled for group therapy, which is about to start. What action should the nurse take? ·603 Allow client to complete the ritual. Discuss with the group leader the possibility of allowing the client to enter the group late. Arrange for client to begin lunch either so that the ritual can be completed prior to scheduled activities. SOMATOFORM DISORDERS: ·604 Describe the difference between primary and secondary gains. ·605 Primary gain is a decrease in anxiety, which results from some effort made to deal with stress. Secondary gain is the advantage, other than reduced anxiety, which occurs from the sick role. ·606 Explain the difference between somatization and hypochondriasis. ·607 Somatization is used to describe a person who has many recurrent complaints with no organic basis as opposed to someone with hypochondriasis who has unrealistic or exaggerated that theyinterfere with social and occupational functioning. ·608 An air traffic controller suddenly suddenly develops blindness. All physical findings are negative. The client’s history reveals an increased anxiety about job performance and fear about job security. What type of disorder is this? What purpose is the blindness serving? What nursing interventions are indicated? ·609 Conversion reaction. Decreases the anxiety about job. Assist with ADL, encourage expression of anger, teach relaxation techniques, and assist with the identification of anxiety related to job security and performance. ·610 A 42 yr. old secretary has visited 7 different doctors in the last year with a complaint of chest pain, heart palpitations, and shortness of breath. She is certain she is having a heart attack in spite of the physician’s reassurance that all tests are normal. What type of disorder is this? What nursing actions are indicated? ·611 Hypochondriacal disorder. Decrease anxiety, teach relaxation techniques, explore relationship between the symptoms and past experiences with heart disease. Focus interactions away from bodily concerns. ·612 Five years ago, a woman was involved in a motor vehicle accident that killed her friend who was a passenger in the car she was driving. Since that time, she has been unable to work because of sever back pain. The pain in unrelieved by prescribed medications. What type of disorder is this? What are the contributing causes? Describe the nursing care. ·613 Somatization disorder. Unresolved grief, anxiety. Evaluate pain medication use and/or abuse. Document duration and intensity of pain. Assist client to identify precipitating factors related to request for medication. DISSOCIATIVE DISORDERS: ·614 Describe the difference between psychogenic amnesia and a psychogenic fugue. ·615 Psychogenic amnesia is the sudden inability to recall certain events in one’s life. A psychogenic fugue state is characterized by the individual leaving home and being unable to recall their identity or their past. ·616 What is a multiple personality disorder? ·617 Presence of two or more distinct personalities within an individual. The personalities emerge during stress. ·618 List 3 possible causes of psychogenic amnesia. ·619 Traumatic event such as a threat of death or injury, an intolerable life situation, or a natural disaster. ·620 Describe depersonalization disorder. ·621 A temporary loss of one’s reality, a loss of the ability to feel and express emotions, or a sense of “strangeness” in the surrounding environment. These individuals express a fear of “going crazy.” PERSONALITY DISORDERS: ·622 Obsessive-Compulsive Personality = Orderliness, rigid. ·623 Passive-Aggressive Personality = Passively resistant ·624 Antisocial Personality = Inability to conform to social norms ·625 Borderline Personality = Needy, always in a crisis, self-mutilating, unable to sustain relationships, splitting behavior ·626 Dependent Personality = Unable to make decisions for self, allows others to assumeresponsibility for his/her life. ·627 Narcissistic Personality = Feelings of self-importance and entitlement. May exploit others to get own needs met. ·628 Histrionic Personality = Dramatic, flamboyant, needs to be the center of attention ·629 Paranoid Personality = Suspicious, shows, mistrust of others, is watchful and secretive ·630 Schizoid Personality = Isolated and introverted, has no close friends ·631 Maladaptive Personality = Does not think anything he/she does is wrong, e.g., authorities are “out to get them.” EATING DISORDERS: ·632 Describe the clinical symptoms of anorexia nervosa. ·633 weight loss of at least 15% of ideal/original body weight; hair loss; dry skin; irregular heart rate; decreased pulse; decreased blood pressure; Amenorrhea; dehydration; electrolyte imbalance. ·634 State 2 psychodynamic differences between anorexia and bulimia. ·635 Anorexia nervosa deals with issues of control and a struggle between dependence and independence. Bulimia deals with loss of control (Binge eating) and guilt (purging). ·636 An anorectic client has her friend bring her several cookbooks so she can plan a party when she is discharged. What nursing intervention is appropriate in addressing this behavior? ·637 Discuss activities that don’t involve food, which may take place after discharge. Discuss the cookbooks with the treatment team and, if the treatment plan indicates, take books from client. ·638 Anorexia nervosa may be precipitated by what etiologic factors? ·639 Mother-daughter conflicts usually focusing on independence/dependence issues; discomfort with maturation; need for control; desire for perfection ·640 What might the initial treatment include for a client admitted to the hospital with a diagnosis of bulimia nervosa? ·641 Blood work to evaluate electrolyte status; replenish electrolytes and fluids as indicated; carefully monitor for evidence of vomiting. AFFECTIVE DISORDERS: ·642 Identify physiologic changes, which often occur with depression. ·643 Weight change (loss or gain), constipation, fatigue, lack of sexual interest, somatic complaints, and sleep disturbances. ·644 A client, who has been withdrawn and tearful, comes to breakfast one morning smiling and interacting with her peers. Prior to breakfast, she gave her roommate her favorite necklace. What actions should the nurse take and why? ·645 Assess for suicidal ideation, plan and means to carry out plan. Place on precautions as indicated. A sudden change in mood and giving away possessions are two possible signs that a suicide plan has been developed. ·646 Name the components of a suicide assessment. ·647 Existence of a plan, method, availability of method chosen, lethality of method chosen, identified support system, and history of previous attempts. ·648 A client on your unit refuses to go to group therapy. What is the most appropriatenursing interventions? ·649 Accompany client to the group; do not give client option. Client needs to be mobilized. ·650 A client is standing on a table loudly singing the “Star Spangled Banner” encircled by sheets, which have been set afire. In order of priority, describe appropriate nursing actions. ·651 Remove client and other persons in the vicinity to a safe area and activate hospital fire plan. When area is safe, place client in quiet environment with low stimulation and medicate as indicated. SCHIZOPHRENIC/PARANOID DISORDERS: ·652 A client is sitting alone, talking quietly. There is no one around. What nursing action should be taken? ·653 Quietly approach client and note the behavior. Assess content of the hallucinations, e.g., “I noticed you talking. Are you hearing voices? Can you tell me about the voices you are hearing?” ·654 A client dials 222-2222 and asks for his fiance, Candice Bergen. This is an example of what type of thought disorder? ·655 Delusion of grandeur ·656 A client has been sitting in the same position for 2 hours. He is mute. What type of schizophrenia is this client experiencing? Describe appropriate nursing interventions for this client? ·657 Catatonic: Spend time with client; assist with ADL; be alert to potential for violence toward self/others; be aware of fluid and nutrition needs. ·658 A client is very agitated. He believes that the CIA has tapped the phone, is sending messages through the television, and that you are an agent who has been planted by the agency. In order of priority, list the appropriate nursing actions to intervene in this situation. What type of delusion is this client experiencing? ·659 Approach client and offer solitary activity to distract. Assess need for medication. Encourage verbalization of feelings and promote outlet for expression. Paranoid disorder with delusions of reference (CIA). ·660 The nurse asks the client, “What brought you to the hospital?” The client’s response is, “The bus.” What type of thinking is this client exhibiting? ·661 Concrete. SUBSTANCE ABUSE: ·662 Three days ago, a client was admitted to the medical unit for a GI bleed. His BP and pulse rate gradually increased, and he developed a low-grade fever. What assessment data should the nurse obtain? What kind of anticipatory planning should the nurse develop? ·663 Obtain a drug and alcohol consumption assessment including type, frequency, and time of last dose/drink. Call the physician and report findings. Anticipate withdrawal/delirium tremens. Provide a quiet, safe environment. Place on seizure precautions. Anticipate giving a medication like Librium. ·664 What physical signs might indicate that a client is abusing intravenous medications? ·665 Needle track marks; cellulitis at puncture site; poor nutritional status. ·666 What behaviors would indicate to the nurse manager that an employee has a possible substance abuse problem?·667 Change in work performance, withdrawal, increase in absences (especially Monday or Friday), increase in number of times tardy, long breaks, late returning from lunch. ·668 A client becomes extremely agitated, abusive, and very suspicious. He is currently undergoing detoxification from alcohol with Librium 25 mg q6h. What nursing actions are indicated? ·669 Notify the physician immediately and anticipate an increase in dose or frequency of Librium. Provide a quiet, safe environment. Approach in a quiet, calm manner. Avoid touching client. ·670 A client, in the third week of cocaine rehabilitation program, returns from an unsupervised pass. The nurse notices that he is euphoric and is socializing with the other clients more than he has in the past. What nursing actions are indicated? ·671 Notify the physician of observed behavior change. Get a urine drug screen as ordered. Confront client with observed behavior change. ABUSE: ·672 What family dynamics are often seen in child abuse cases? ·673 Parent sees child as “different” from other children. Parent sees child to meet their own needs. Parent seldom touches or responds to child. Parent may be very critical of child. Family history of frequent moves, unstable employment, marital discord, and family violence. One parent answers all the questions. ·674 What behavior might the nurse observe in a child who is abused? ·675 Child may appear frightened and withdrawn in the presence of parent or adult. ·676 Identify nursing interventions for dealing with an abused child. ·677 Must report all cases of suspected abuse to appropriate local/state agency. Take color photographs of injuries. Document factual, objective statements of child’s physical condition, child-family interactions, and interviews with family. Establish trust, and care for the child’s physical problems. These are the PRIMARY and IMMEDIATE needs of these children. Recognize own feelings of disgust and contempt for the parents. Teach basic child development and parenting skills to family. ·678 When does battering of women often begin or escalate? ·679 During pregnancy. ·680 What dynamics prevent a battered spouse from leaving the battering situation? ·681 A woman in a battering relationship usually lacks self-confidence and feels trapped. She is often embarrassed to tell friends and family, so she becomes isolated and dependent upon the abuser. ·682 Why is elder abuse so under reported? ·683 It is difficult for an elderly person to admit abuse for fear of being placed in a nursing home or being abandoned. ·684 What types of abuse are seen in the elderly? ·685 Abuse can be physical, verbal, psychosocial, exploitive, or physical neglect. ·686 Identify nursing interventions for working with a rape survivor? ·687 Communicate non-judgmental acceptance. Provide physical care to treat injuries. Give clear, concise explanations of all procedures to be performed. Notify police, encourage victim to prosecute. Collect and label evidence carefully in the presence of a witness. Document factual,objective statements of physical condition; record client’s EXACT WORDS in describing the assault. Notify Rape Crisis Team or counselor if available in the community. Allow discussion of feelings about the assault. Advise of potential for venereal disease, HIV, or pregnancy and describe medical care available. ORGANIC MENTAL DISEASES: ·688 List 5 causes of delirium. ·689 Infection, alcohol withdrawal, electrolyte imbalance, sleep deprivation, brain injury, i.e., subdural hematomas ·690 Describe the nursing care for a client with Alzheimer’s disease. ·691 Provide a safe, consistent environment. (Do not make changes if possible. Change increases anxiety and confusion.) Stick to routines. If client wanders, make sure they have a nametag. Provide assistance as needed with ADL. Make sure bathroom is clearly labeled. ·692 Identify 3 or more causes of dementia. ·693 Alzheimer’s disease, multi-infarcts (brain), Huntington’s chorea, multiple sclerosis, Parkinson’s disease. CHILDHOOD AND ADOLESCENT DISORDERS: ·694 A 7 yr. old boy is disruptive in the classroom and is described by his parents as “hyperactive.” What is the most probable psychiatric disorder? What are the signs and symptoms of this disorder? What drug is usually prescribed for this disorder? ·695 Attention deficit disorder (ADD/ADHD). More prevalent in boys, failure to listen or follow instructions. Difficulty playing quietly, disruptive, impulsive behavior, difficulty sitting still, distractibility to external stimuli, excessive talking, shifts from one unfinished task to another, and underachievement in school performance. Ritalin. ·696 A 15 yr. old boy is threatening to drop out of school. His parents, both alcoholics, say they can’t stop him. He has just been arrested for stealing a car and breaking into a house. What is the most probable disorder? Develop nursing diagnoses and interventions for this disorder. ·697 Conduct disorder. ·698 Potential for violence related to…depending on client. ·699 Disturbance in self-esteem related to…depending on client. ·700 Ineffective family coping related to…depending on client. ·701 Assess verbal/nonverbal cues for escalating behavior to decrease outbursts. Use a non-authoritarian approach. Avoid asking “why” questions. Initiate a “show of force” for a child who is out of control. Initiate suicide precautions when assessment indicates risk. Use “quiet room” when external control is needed. Clarify expressions or jargon if meaning is unclear. Redirect angry feelings to “safe” alternative such as pillow or punching bag. Implement behavior modification therapy if indicated. Role-play new coping strategies. PEDIATRIC NURSING GROWTH AND DEVELOPMENT: ·702 When does birth length double? = by 4 years ·703 When does the child sit unsupported? = 8 months ·704 When does a child achieve 50% of adult height? = 2 years·705 When does a child throw a ball overhand? = 18 months ·706 When does a child speak 2-3 word sentences? = 2 years ·707 When does a child use scissors? = 4 years ·708 When does a child tie his/her shoes? = 5 years CHILD HEALTH PROMOTION: ·709 List 2 contraindications for live virus immunization. ·710 Immunocompromised child or a child in a household with an immunocompromised individual. ·711 List 3 classic signs and symptoms of measles. ·712 Photophobia, confluent rash that begins on the face and spreads dowward, and Koplik’s spots on the buccal mucosa. ·713 List the signs and symptoms of iron deficiency. ·714 Anemia, pale conjunctiva, pale skin color, atrophy of papillae on tongue, brittle/ridged/spoonshaped nails, and thyroid edema. ·715 Identify food sources for Vitamin A. ·716 Liver, sweet potatoes, carrots, spinach, peaches, and apricots. ·717 What disease occurs with vitamin C deficiency? ·718 Scurvy. ·719 What measurements reflect present nutritional status? ·720 Weight, skinfold thickness, and arm circumference. ·721 List the signs and symptoms of dehydration in an infant. ·722 Poor skin turgor, absence of tears, dry mucous membranes, weight loss, depressed fontanel and decreased urinary output. ·723 List the laboratory findings that can be expected in a dehydrated child. ·724 Loss of bicarbonate/decreased serum pH, losso f sodium (hyponatremia), loss of potassium (hypokalemia), elevated Hct, and elevated BUN. ·725 How should burns in children be assessed? ·726 Use the Lund-Browder chart, which takes into account the changing proportions of the child’s body. ·727 How can the nurse BEST evaluate the adequacy of fluid replacement in children? ·728 Monitor urine output. ·729 How should a parent be instructed to “child proof” a house? ·730 Lock all cabinets, safely store all toxic household items in locked cabinets, and examine the house from the child’s point of view. ·731 What interventions should the nurse do FIRST in caring for a child who has ingested apoison? ·732 Assess the child’s respiratory, cardiac, and neurological status. ·733 List 5 contraindications to administering syrup of ipecac. ·734 Coma, seizures, CNS depression, ingestion of petroleum-based products, and ingestion of corrosives. ·735 What instructions should be given by phone to a mother who knows her child has ingested a bottle of medication? ·736 Administer syrup of ipecac if the child is conscious. Bring any emesis or stool to the emergency room. Bring the container in which the medicine was stored to the emergency room. RESPIRATORY DISORDERS: ·737 Describe the purpose of bronchodilators. ·738 Reverse bronchospasm ·739 What are the physical assessment findings for a child with asthma? ·740 Expiratory wheezing, rales, right cough, and signs of altered blood gases. ·741 What nutritional support should be provided for the child with cystic fibrosis? ·742 Pancreatic enzyme replacement, fat-soluble vitamins, and a high carbohydrate, high protein, moderate fat diet. ·743 Why is genetic counseling important for the cystic fibrosis family? ·744 The disease is autosomal recessive in its genetic pattern. ·745 List 7 signs of respiratory distress in a pediatric client. ·746 Restlessness, tachycardia, tachypnea, diaphoresis, flaring nostrils, retractions, and grunting ·747 Describe the care of a child in a mist tent. ·748 Monitor child’s temperature. Keep tent edges tucked in. Keep clothing dry. Assess child’s respiratory status. Look at child inside tent. ·749 What position does the child with epiglottis assume? ·750 Upright, sitting, with chin out and tongue protruding (“tripod” position). ·751 Why are IV fluids important for the child with an increased respiratory rate? ·752 The child is at risk for dehydration and acid/base imbalance. ·753 Children with chronic otitis media are at risk for developing what problem? ·754 Hearing loss ·755 What is the most common post-operative complication following a tonsillectomy? Describe the signs and symptoms of this complication. ·756 Hemorrhage; frequent swallowing, vomiting fresh blood, and clearing throat. CARDIOVASCULAR DISORDERS: ·757 Differentiate between a right to left and left to right shunt in cardiac disease. ·758 A left to right shunt moves oxygenated blood back through the pulmonary circulation. A right to left shunt bypasses the lungs and delivers unoxygenated blood to the systemic circulationcausing cyanosis. ·759 List the 4 defects associated with Tetralogy of Fallot. ·760 VSD, overriding aorta, pulmonary stenosis and right ventricular hypertrophy ·761 List the commons signs of cardiac problems in an infant. ·762 Poor feeding, poor weight gain, respiratory distress/infections, edema and cyanosis ·763 What are the 2 objectives in treating congestive heart failure? ·764 Reduce the workload of the heart and increase cardiac output. ·765 Describe nursing interventions to reduce the workload of the heart. ·766 Small, frequent feedings or gavage feedings. Plan frequent rest periods. Maintain a neutral thermal environment. Organize activities to disturb child only as indicated. ·767 What position would best relieve the child experiencing a “tet” spell? ·768 Knee-chest position, or squatting. ·769 What are common signs of digoxin toxicity? ·770 Diarrhea, fatigue, weakness, nausea and vomiting. The nurse should check for bradycardia prior to administration. ·771 List 5 risks of cardiac catheterization. ·772 Arrythmia, bleeding, perforation, phlebitis, and obstruction of the arterial entry site. ·773 What cardiac complications are associated with rheumatic fever? ·774 Aortic valve stenosis and mitral valve stenosis. ·775 What medications are used to treat rheumatic fever? ·776 Penicillin, erythromycin, and aspirin. NEUROMUSCULAR DISORDERS: ·777 What are the physical features of a child with Down syndrome? ·778 Simian creases of palms, hypotonia, protruding tongue, and upward/outward slant of eyes. ·779 Describe “scissoring.” ·780 A common characteristic of spastic cerebral palsy in infants. The legs are extended and crossed over each other, the feet are plantar flexed. ·781 What are 2 nursing priorities for a newborn with myelomeningocele? ·782 Prevention of infection of the sac and monitoring for hydrocephalus (measure head circumference; check fontanel; assess neurological functioning). ·783 List the signs and symptoms of increased ICP in older children. ·784 Irritability, change in LOC, motor dysfunction, headache, vomiting, unequal pupil response, and seizures. ·785 What teaching should parents of a newly shunted child receive? ·786 Signs of infection and increased ICP (decreased pulse, increased blood pressure). Shunt should not be pumped. Child will need revisions due to growth. Provide guidance for growth and development.·787 State the 3 main goals in providing nursing care for a child experiencing a seizure. ·788 Maintain patent airway, protect from injury, and observe carefully. ·789 What are the side effects of Dilantin? ·790 Gingival hyperplasia of the gums, dermatitis, ataxia, and GI distress. ·791 Describe the signs and symptoms of a child with meningitis? ·792 Fever, irritability, vomiting, neck stiffness, opisthotonos, positive Kernig’s sign, positive Brudzinski’s sign. Infant does not show all classic signs, but is very ill. ·793 What antibiotics are usually ordered for bacterial meningitis? ·794 Ampicillin, penicillin, and/or Chloramphenicol. ·795 How is a child usually positioned after brain tumor surgery? ·796 Flat on his/her side. ·797 Describe the function of an osmotic diuretic. ·798 Osmotic diuretics remove water from the CNS to reduce cerebral edema. ·799 What nursing interventions increase intracranial pressure? ·800 Suctioning and positioning/turning. ·801 Describe the mechanism of inheritance for Duchenne muscular dystrophy. ·802 Duchenne muscular dystrophy is inherited as an X-linked recessive trait. ·803 What is “Gower’s sign?” ·804 Gower’s sign is an indicator of muscular dystrophy. The child has to “walk” up legs using hands to stand. RENAL DISORDERS: ·805 Compare the signs and symptoms of acute glomerulonephritis (AGN) with nephrosis. ·806 AGN: gross hematuria, recent strep infection, hypertension, and mild edema. Nephrosis: severe edema, massive proteinuria, frothy-appearing urine, anorexia. ·807 What antecedent event occurs with acute glomerulonephritis? ·808 Beta-hemolytic strep infection ·809 Compare the dietary interventions for acute glomerulonephritis and nephrosis. ·810 AGN: low-sodium diet with no added salt. Nephrosis: high-protein, low-salt diet. ·811 What is the physiologic reason for the lab finding of hypoproteinemia in nephrosis? ·812 Hypoproteinemia occurs because the glomeruli are permeable to serum proteins. ·813 Describe safe monitoring of prednisone administration and withdrawal. ·814 Long term prednisone should be given every other day. Signs of edema, mood changes, and GI distress should be noted and reported. The drug should be tapered, not discontinued suddenly. ·815 What interventions can be taught to prevent urinary tract infections in children? ·816 Avoid bubble baths, void frequently; drink adequate fluids especially acidic fluids such as apple or cranberry juice, and clean genital area from front to back.·817 Describe the pathophysiology of vesicoureteral reflux. ·818 a malfunction of the valves at the end of the ureters allowing urine to reflux out of the bladder into the ureters and possibly the kidneys. ·819 What are the priorities for a client with Wilms’ tumor? ·820 Protect the child from injury to the encapsulated tumor. Prepare the family/child for surgery. ·821 Explain why hypospadias correction is done before the child reaches preschool age. ·822 Preschoolers fear castration, are achieving sexual identity, and acquiring independent toileting skills. GASTROINTESTINAL DISORDERS: ·823 Describe feeding techniques for the child with cleft lip or palate. ·824 Lamb’s nipple, or prosthesis. Feed child upright with frequent bubbling. ·825 List the signs and symptoms of esophageal atresia with TEF. ·826 choking, coughing, cyanosis, and excess salivation. ·827 What nursing actions are initiated for the newborn with suspected esophageal atresia with TEF? ·828 NPO immediately and suction secretions. ·829 Describe the post-op nursing care for an infant with pyloric stenosis. ·830 Maintain Iv hydration and provide small, frequent oral feedings of glucose and/or electrolyte solutions within 4-6 hours. Gradually increase to full strength formula. Position on right side in semi-Fowler’s position after feeding. ·831 Describe why a barium enema is used to treat intussusception. ·832 A barium enema reduces the telescoping of the intestine through hydrostatic pressure without surgical intervention. ·833 Describe the pre-op nursing care for a child with Hirschsprung’s disease. ·834 Check vital signs and take axillary temps. Provide bowel cleansing program and teach about colostomy. Observe for bowel perforation; measure abdominal girth. ·835 What care is needed for the child with a temporary colostomy? ·836 Family needs education about skin care and appliances. Referral to an enterostomal therapist is appropriate. ·837 What are the signs of anorectal malformation? ·838 A newborn who does not pass meconium within 24 hours, meconium appearing from a fistula or in the urine, or an unusual appearing anal dimple. ·839 What are the priorities for a child undergoing abdominal surgery? ·840 Maintain fluid balance (I&O, NG suction, monitor electrolytes), monitor vital signs, care of drains if present, assess bowel function, prevent infection of incisional area and other post-op complications, and support child/family with appropriate teaching. HEMATOLOGICAL DISORDERS: ·841 Describe what information families should be given when a child is receiving oral iron preparations.·842 Give oral iron on an empty stomach and with vitamin C. Use straws to avoid discoloring teeth. Tarry stools are normal. Increase dietary sources of iron. ·843 List dietary sources of iron. ·844 Meat, green leafy vegetables, fish, liver, whole grains, legumes. ·845 What is the genetic transmission pattern of hemophilia. ·846 It is an X-linked recessive chromosomal disorder, transmitted by the mother and expressed in male children. ·847 Describe the sequence of events in a vaso-occlusive crisis in sickle cell anemia. ·848 A vaso-occlusive crisis is caused by clumping of red blood cells which cannot get through the capillaries, causing pain and tissue/organ ischemia. Lowered oxygen tension affects the HgbS, which causes sickling of the cells. ·849 Explain why hydration is a priority in treating sickle cell disease. ·850 Hydration promotes hemodilution and circulation of the red blood cells through the blood vessels. ·851 What should families and clients do to avoid triggering sickling episodes? ·852 Keep child well hydrated. Avoid known sources of infections. Avoid high altitudes. Avoid strenuous exercise. ·853 Nursing interventions and medical treatment for the child with leukemia are based on what 3 physiological problems? ·854 Anemia (decreased erythrocytes). Infection (neutropenia). Bleeding thrombocytopenia (decreased platelets). SKELETAL DISORDERS: ·855 List normal findings in a neurovascular assessment. ·856 Warm extremity, brisk capillary refill, free movement, normal sensation of the affected extremity, and equal pulses. ·857 What is compartment syndrome? ·858 Damage to the nerves and vasculature of an extremity due to compression. ·859 What are the signs and symptoms of compartment syndrome? ·860 Abnormal neurovascular assessment: cold extremity, severe pain, inability to move the extremity, and poor capillary refill. ·861 Why are fractures of the epiphyseal plate a special concern? ·862 Fractures of the epiphyseal plate (growth plate) may affect the growth of the limb. ·863 How is skeletal traction applied? ·864 Skeletal traction is maintained by pins or wires applied to the distal fragment of the fracture. ·865 What discharge instructions should be included for a child with spica cast? ·866 Check circulatio. Keep cast dry. Do not stick anything under cast. Prevent cast soilage during toileting or diapering. DO NOT TURN with abductor bar. ·867 What are the signs and symptoms of congenital dislocated hip in infants?·868 Unequal skin folds of the buttocks, ortalani sign, limited abduction of the affected hip, and unequal leg lengths. ·869 How would the nurse conduct scoliosis screening? ·870 Ask the child to bend forward from the hips with arms hanging free. Examine the child for a curve of the spine, rib hump, and hip asymmetry. ·871 What instructions should the child with scoliosis receive about the Milwaukee brace? ·872 Wear the brace 23 hours per day. Wear t-shirt under brace. Check skin for irritation. Perform back and abdominal exercises. Modify clothing. Encourage the child to maintain normal activities as able. ·873 What care is indicated for a child with juvenile rheumatoid arthritis? ·874 Prescribed exercise to maintain mobility, splinting of affected joints, and teaching medication management and side effects of drugs. ADVANCED CLINICAL CONCEPTS RESPIRATORY FAILURE: ·875 What PO2 value indicates hypoxemia? ·876 Below 50 mmHg ·877 What blood value indicates hypercapnia? ·878 PCO2 above 45 mmHg ·879 Identify the condition that exists when the PO2 is less than 50 mmHg and FiO2 is greater than 60%. ·880 Hypoxemia ·881 List 3 symptoms of respiratory failure in the adult. ·882 Dyspnea/tachypnea, intercostal retractions, cyanosis. ·883 List 4 common causes of respiratory failure in children. ·884 Congenital heart disease, infection or sepsis. Respiratory distress syndrome, aspiration, fluid overload or dehydration. ·885 What percentage of O2 should a child in severe respiratory distress receive? ·886 100% O2 SHOCK/DIC (DISSEMINATED INTRAVASCULAR CLOTTING): ·887 Define shock. ·888 Widespread, serious reduction of tissue perfusion which leads to generalized impairment of cellular function. ·889 What is the most common cause of shock? ·890 Hypovolemia ·891 What cause septic shock? ·892 Release of endotoxins from bacteria which act on nerves in vascular space in periphery, causing vascular pooling, reduced venous return, and decreased cardiac output, resulting in poorsystemic perfusion. ·893 What is the goal of treatment for hypovolemic shock? ·894 Quick restoration of cardiac output and tissue perfusion ·895 What intervention is used to restore cardiac output when hypovolemic shock exists? ·896 Rapid infusion of volume-expanding fluids ·897 It is important to differentiate between hypovolemic and cardiogenic shock. How might the nurse determine the existence of cardiogenic shock? ·898 History of MI with left ventricular failure or possible cardiomyopathy, with symptoms of pulmonary edema. ·899 If a client is in cardiogenic shock, what might result from administration of volume expanding fluids, and what intervention can the nurse expect to perform in the event of such an occurrence? ·900 Pulmonary edema, administer cardiotonic drugs such as digitalis preparations ·901 List 5 assessment findings found in most shock victims. ·902 Tachycardia. Tachypnea. Hypotension. Cool clammy skin. Decrease in urinary output. ·903 What is the normal central venous pressure for an adult? ·904 4 to 10 cm of H2O ·905 Once circulating volume is restored, vasopressors may be prescribed to increase venous return. List the main drugs that are used. ·906 Epinephrine (Bronkaid). Dopamine (Dopram). Dobutamine (Dobutrex). Norepinephrine (Levophed). Isoproterenol (Isuprel). ·907 What is the established minimum renal output per hour? ·908 30 cc/hr ·909 List 4 measurable criteria that are the major expected outcomes of a shock crisis. ·910 BP mean of 80 to 90 mmHg. PO2 >50 mmHg. CVP above 6 cm of H2O. Urine output at least 30 cc/hr. ·911 Define DIC. ·912 A coagulation disorder in which there is paradoxical thrombosis and hemorrhage ·913 What is the effect of DIC on PT, PTT, platelets, FSPs (FDPs)? ·914 PT: prolonged. PTT: prolonged. Platelets: decreased. Fribin split products: increased. ·915 What drug is used in the treatment of DIC? ·916 Heparin ·917 Name 4 nursing interventions to prevent injury in clients with DIC. ·918 Gently provide oral care with mouth swabs. Minimize needle sticks and use the smallest gauge needle possible when injections are necessary. Eliminate pressure by turning the client frequently. Minimize the number of BPs taken by cuff. Use gentle suction to prevent trauma to mucosa. Apply pressure to any oozing site. RESUSCITATION:·919 What is the first priority when a client with an unwitnessed cardiac arrest is found? ·920 Begin CPR ·921 Define myocardial infarction. ·922 Necrosis of the heart muscle due to poor perfusion of the heart. ·923 What criteria should alert a client with known angina who takes nitroglycerin tablets sublingually to call the EMS? ·924 Unrelieved chest pain after 3 nitroglycerin tabs in 15 minutes. ·925 After calling out for help and asking someone to dial for emergency services, what is the next action in CPR? ·926 According to American Heart Association guidelines published September 2000, you should call for help first for unresponsive adults and then begin the ABC’s of CPR. For unresponsive infants & children, CPR should be performed for 1 minute before placing a 911 call for help. ·927 True or False: In feeling of presence of a carotid pulse, no more than 5 seconds should be used. ·928 FALSE: palpate for at least 5 to 10 seconds, recognizing that arrythmias or bradycardia could be occurring. ·929 During one-rescuer CPR, what is the ratio of compressions to ventilations for an adult? During one-rescuer CPR, what is the ratio of compressions to ventialations for a child? ·930 15:2 X 4 cycles for adult. 5:1 for a child and neonate. ·931 What is the FIRST drug most likely to be used for an in-hospital cardiac arrest? ·932 Epinephrine ·933 A client in cardiac arrest is noted on bedside monitor to be in pulseless ventricular tachycardia. What is the first action that should be taken? ·934 Defibrillation with 200 to 360 joules. ·935 True or False: A precordial thump is routine activity for an in-hospital cardiac arrest. ·936 FALSE: only indicated in pulseless VT or VF or when ventricular asystole on monitor responds to a thump with a QRS complex. ·937 How would the nurse assess the adequacy of compressions during CPR? How would the nurse assess for adequacy of ventilations during CPR? ·938 Check for a pulse. Watch for chest excursion and auscultate bilaterally for breath sounds. ·939 If a person is choking, when should the rescuer intervene? ·940 When the person points to his/her throat and can no longer cough, talk, or make sounds. ·941 One should NEVER make blind sweeps into the mouth of a choking child or infant. Why? ·942 Because the object might be pushed further down into the throat. ·943 Why do ACLS guidelines recommend a decreased reliance on the use of bicarbonate during adult CPR? ·944 Because acidosis should be relieved with improved ventilation. Bicarbonate administration can actually contribute to increased CO2.FLUID AND ELECTROLYTE BALANCE: ·945 List 4 common caused of fluid volume deficit. ·946 GI causes: vomiting, diarrhea, GI suctioning. Decrease in fluid intake. Increase in fluid output such as sweating. Massive edema. Ascites. ·947 List 4 common causes of fluid volume overload. ·948 CHF, renal failure; cirrhosis; excess ingestion of table salt or over-hydration with sodiumcontaining fluids. ·949 Identify 2 examples of isotonic fluids. ·950 Ringer’s lactate. Normal saline. ·951 List 3 systems which maintain acid-base balance. ·952 Lungs. Kidneys. Chemical buffers. ·953 Cite the ABG normals for the following: pH, pCO2, HCO3. ·954 pH: 7.35-7.45. pCO2: 35 to 45 mmHg. HCO3: 22-26 mEq/L ·955 Determine the following acid-base disorders: ·956 pH- 7.50, pCO2 – 30, HCO3 – 26 = Respiratory alkalosis ·957 pH- 7.30, pCO2 – 42, HCO3 – 20 = Metabolic acidosis ·958 pH- 7.48, pCO2 – 42, HCO3 – 32 = Metabolic alkalosis ·959 pH- 7.29, pCO2 – 55, HCO3 – 26 = Respiratory acidosis PERIOPERATIVE CARE: ·960 List 5 variables that increase surgical risk. ·961 Age: very young and very old, obesity and malnutrition, preoperative dehydration/hypovolemia, preoperative infection, use of anticoagulants preoperative (aspirin) ·962 Why is a client with liver disease at increased risk for operative complications? ·963 Impairs ability to detoxify medications used during surgery. Impairs ability to produce prothrombin to reduce hemorrhage. ·964 Preoperative teaching should include demonstration and explanation of expected postoperative client activities. What activities should be included? ·965 Respiratory activities: breathing, use of spirometer. Exercises: range of motion, leg exercises, turning. Pain management: medications, splinting. Dietary restrictions: NPO to progressive diet. Dressings and drains. Orientation to recovery room environment. ·966 What items should the nurse assist the client in removing before surgery? ·967 Contact lenses, glasses, dentures, partial plates, wigs, jewelry, prosthesis, make-up and nail polish. ·968 How and why is the client positioned in the immediate postoperative period? ·969 Usually on the side or with head to side in order to prevent aspiration of any emesis. ·970 List 3 nursing actions to prevent postoperative wound dehiscence/evisceration. ·971 Splint incision when coughing, encourage coughing/deep breathing in EARLY postoperative period when sutures are STRONG. Monitor for signs of infection, malnutrition, and dehydration.Encourage high-protein diet. ·972 Identify 3 nursing interventions to prevent postoperative urinary tract infections. ·973 Avoid postoperative catheterization. Increase oral fluid intake. Empty bladder q4 to 6 hours, early ambulation. ·974 Identify nursing/medical interventions to prevent postoperative paralytic ileus. ·975 Early ambulation. Limit use of narcotic analgesics. NG tube decompression. ·976 List 4 nursing interventions to prevent postoperative thrombophlebitis. ·977 Perform in-bed leg exercises. Early ambulation. Apply antiembolus stockings. Avoid positions/pressure which obstruct venous flow. ·978 During the intraoperative period, what activities should the operating room nurse do to ensure safety during surgery? ·979 Ascertain correct sponge, needle, and instrument count. Position client to avoid injury. Apply ground during electrocautery use. Strict use of surgical asepsis. HIV INFECTION: ·980 Identify the way HIV is transmitted. ·981 Transmitted through blood and body fluids, e.g., unprotected sexual contact with an affected person, sharing needles among drug abusing persons, infected blood products (rare), maternal to fetus transmission through breast milk, or breaks in universal precautions (needle sticks or similar occurrences). ·982 Vertical transmission (from mother to fetus) occurs how often if mother is treated during pregnancy? ·983 Vertical transmission occurs 30 to 50% of the time. ·984 Describe universal precautions. ·985 Protection from blood and body fluids is the goal of standard precautions. Standard precautions initiate barrier protection between caregiver and client through: Hand washing, use gloves, use gown and masks, eye protection as indicated, depending on activity of care and the likelihood of exposure. Prevent needle sticks by not capping needles. ·986 What are the side effects of Amphotericin B? ·987 Side effects of amphotericin B (can be quite severe) include: Anorexia, Chills, Cramping, Muscle and joint pain, Circulatory problems. ·988 What does the CD4 T cell count describe? ·989 CD4 T cell count describes the number of infection-fighting lymphocytes the person has. ·990 Why does the CD4 T cell count drop in HIV infections? ·991 CD4 T cell count drops because the virus destroys CD4 T cells as it invades them and replicates. ·992 Describe the ways a pediatric client might acquire HIV infection. ·993 Through infected blood products. Through sexual abuse. Through breast milk. PAIN: ·994 What modalities are associated with the Gate control pain theory?·995 Massage, heat and cold, acupuncture, TENS. ·996 How does past experiences with pain influence current pain experience? ·997 The more pain experienced in childhood, the greater the perception of pain in adulthood or with current pain experience. ·998 What modalities are thought to increase the production of endogenous opiates? ·999 Acupuncture, administration of placebos, TENS. ·1000 What 6 factors should the nurse include when assessing the pain experience? ·1001 Location, intensity, comfort measures, quality, chronology and subjective view of pain. ·1002 What mechanism is involved in the reduction of pain through the administration of NSAIDs meds? ·1003 NSAIDs act by a peripheral mechanism at the level of damaged tissue by inhibiting prostaglandin synthesis and other chemical mediators involved in pain transmission. ·1004 If narcotic agonist/antagonist drugs are administered to a client already taking narcotic drugs, what may be the result? ·1005 Initiation of withdrawal symptoms ·1006 List 4 side effects of narcotic medications. ·1007 Nausea/vomiting. Constipation. CNS depression. Respiratory depression. ·1008 What is the antidote for narcotic-induced respiratory depression? ·1009 Narcan (Naloxone). ·1010 What is the 1st sign of tolerance to pain analgesics? ·1011 Decreased duration of drug effectiveness ·1012 Which route of administration for pain medications has the quickest onset and the shortest duration? ·1013 IV push or bolus. ·1014 List the 6 modalities that are considered non-invasive, non-pharmacologic pain relief measures. ·1015 Heat and cold applications. Transcutaneous electrical nerve stimulation (TENS). Massage. Distraction. Relaxation techniques. Biofeedback techniques. DEATH AND GRIEF: ·1016 Identify the 5 stages of death and dying. ·1017 Denial. Anger. Bargaining. Depression. Acceptance. ·1018 A client has been told of a positive breast biopsy report. She asks no questions and leaves the healthcare provider’s office. She is overheard telling her husband, :the doctor didn’t find a thing.” What coping style is operating at this stage of grief? ·1019 Denial ·1020 Your client, an incest survivor, is speaking of her deceased father, the perpetrator. “He was a wonderful man, so good and kind. Everyone thought so.” What would be the most useful intervention at this time?·1021 Gently point out both the positive and negative aspects of her relationship wit her father. Try to minimize the idealization of the deceased. ·1022 Your client feels responsible for his sister’s death because he took her to the hospital where she died. “If I hadn’t taken her there, they couldn’t have killed her.” It has been one month since her death. Is this response indicative of a normal or complicated grief reaction? ·1023 This is a normal expression of anger and guilt, which occurs. Try to minimize the rumination of these thoughts. ·1024 Mrs. Green lost her husband 3 years ago. She has not disturbed any of his belongings and continues to set a place at the table for him nightly. Is this response indicative of a normal or complicated grief reaction? ·1025 This is a dysfunctional grief reaction. Mrs. Green has never moved out of the denial stage of her grief work. ELECTROCARDIOGRAM: ·1026 Identify the waveforms found in a normal EKG? ·1027 P wave, QRS complex, T wave, ST segment, PR interval ·1028 In an EKG reading, which wave represents depolarization of the atrium? ·1029 P wave ·1030 In an EKG reading, what complex represents depolarization of the ventricle? ·1031 QRS complex ·1032 What does the PR interval represent? ·1033 The time rquired for the impulse to travel from the atria through the A-V node ·1034 If the U wave is most prominent, what condition might the nurse suspect? ·1035 Hypokalemia ·1036 Describe the calculation of the heart rate using an EKG rhythm strip. ·1037 Count the number of the R-R intervals in the 30 large squares and multiply by 10 ·1038 What is the most important assessment data for the nurse to obtain on a client with arrythmia? ·1039 Ability of the client to tolerate the arrhythmia ·1040 Calculate the rate of this rhythm strip. ·1041 90 to 100 depending on which set of 6 squares you use. GERONTOLOGICAL NURSING: ·1042 What are normal memory changes that occur as one ages? ·1043 Short-term memory declines while long-term memory undergoes minimal change. ·1044 What symptoms might the nurse expect to see in an older person who has had an overload of changes as well as a respiratory infection? ·1045 Confusion. ·1046 Why can the BP of older adults be expected to increase? ·1047 Heart work increases in response to increased peripheral resistance.·1048 What is the major cause of respiratory disability in the elderly? ·1049 COPD ·1050 List 5 nursing interventions to promote adequate bowel functioning for older persons. ·1051 Determine what is normal GI functioning for each individual, increase fiber and bulk in the diet, provide adequate hydration, encourage regular exercise, and encourage eating, small, frequent meals. ·1052 How can a female nurse increase the older client’s ability to hear her speak? ·1053 Lower the pitch or tone of her voice. ·1054 What is the most common visual problem occurring in the elderly? ·1055 Cataracts. ·1056 Describe the following conditions which occur in the elderly: Presbyopia, Arcus senilis, Presbycusis. ·1057 Presbyopia – decreased ability of the eye to accommodate for close work. ·1058 Arcus senilis – glossy white ring encircling the periphery of the cornea ·1059 Presbycusis – decrease in hearing acuity, auditory threshold, pitch and tone discrimination, and speech intelligibility. ·1060 Describe the onset of Alzheimer’s disease. ·1061 Slow, insidious onset with progressive downward course. ·1062 What is the purpose of a reality orientation group? ·1063 To keep the client oriented to time, place, and person. ·1064 What are the 2 factors that cause decrease in excretion of drugs by the kidneys? ·1065 Decrease in glomerular filtration and slowed organ functioning. OB-MATERNITY ANATOMY & PHYSIOLOGY OF REPRODUCTION: ·1066 State the objective signs that signify ovulation ·1067 abundant, thin, clear cervical mucus; open cervical os; slight drop in BBT and then 0.5-1.0 F rise; ferning under the microscope ·1068 Ovulation occurs how many days before the next menstrual period? ·1069 14 days. ·1070 State three ways to identify the chronological age of a pregnancy (gestation)? ·1071 10 lunar months, 9 calendar months consisting of 3 trimesters of 3 months each, 40 weeks, 280 days. ·1072 What maternal position provides optimum fetal maternal/placental perfusion during pregnancy? ·1073 The knee-chest position, but the ideal position of COMFORT for the mother which supports fetal/maternal/placental perfusion is the side-lying position off the abdominal vessels (vena cava, aorta)·1074 Name the major discomforts of the first trimester and one suggestion for amelioration of each. ·1075 Nausea and vomiting: crackers before rising. Fatigue: teach the need for rest periods/naps and 7-8 hours sleep at night. ·1076 If the first day of a woman’s last normal menstrual period was May 28, what is the estimated delivery date (EDD) using Nagele’s rule? ·1077 Count back 3 months and add 7 days: March 7 (always give February 28 days). ·1078 At twenty weeks gestation, the fundal height would be ______ , the fetus would weigh approximately _______ and look like _____ . ·1079 At the umbilicus; 300-400 grams; a baby with hair, lanugo and verniz, but without subcutaneous fat. ·1080 State the normal psychosocial responses to pregnancy in the 2nd trimester ·1081 Ambivalence wanes and acceptance of pregnancy occurs; pregnancy becomes “real;” signs of maternal-fetal bonding occur. ·1082 Hemodilution of pregnancy peaks at ______ weeks and results in a/an ______ in a women’s Hct. ·1083 28-32 weeks; increase in Hct ·1084 State three principles relative to the PATTERN of weight gain in pregnancy. ·1085 Total gain should average 24-30 lbs. Gain should be consistent throughout pregnancy. An average of 0.9 lb/week should be gained in the 2nd & 3rd trimester. ·1086 During pregnancy a woman should add ____ calories to her diet, and drink ____ of milk/day. ·1087 300 calories; 1 quart of milk ·1088 Fetal heart rate can be auscultated by Doppler at ____ weeks gestation. ·1089 10-12 weeks ·1090 Describe the schedule for prenatal visits for a low-risk pregnant woman. ·1091 Once a month until 28 weeks, then once every week until delivery. FETAL-MATERNAL ASSESSMENT TECHNIQUES: ·1092 Name 5 maternal variables associated with diagnosis of a high risk pregnancy ·1093 Age (under 17 years or over 34 years of age), parity (over 5), <3 months between pregnancies, diagnosis of PIH, diabetes mellitus, or cardiac disease. ·1094 Is one ultrasound examination useful in determining the presence of intrauterine growth retardation (IUGR)? ·1095 no, serial measurements are needed to determine IUGR. ·1096 What does the biophysical profile (BPP) determine? ·1097 Fetal well-being ·1098 List 3 necessary nursing actions prior to an ultrasound exam for a woman in the first trimester of pregnancy. ·1099 Have client fill bladder. Do not allow client to void. Position supine with uterine wedge.·1100 State the advantage of CVS over amniocentesis. ·1101 Can be done between 8-12 weeks gestation with results returned within one week, which allows for decision about termination while still in 1st trimester. ·1102 Why are serum or amniotic AFP levels done prenatally? ·1103 To determine if alpha-fetoprotein levels are elevated which may indicate the presence of neural tube defects; or low levels, which may indicate trisomy 21. ·1104 What is the most important determinant of fetal maturity for extrauterine survival? ·1105 L/S ratio (lung maturity, lung surfactant development) ·1106 Name the 3 most common complications of amniocentesis. ·1107 Spontaneous abortion, fetal injury, infection. ·1108 Name the 4 periodic changes of the fetal heart rate, their causes, and one nursing treatment for each. ·1109 Acceleration: caused by burst of sympathetic activity; they are reassuring and require no treatment. Early decelerations: caused by head compression, are benign and caution the nurse to monitor for labor progress and fetal descent. Variable decelerations: caused by cord compression; change of position should be tried first. Late decelerations: are caused by UPI (uteroplacental insufficiency) and should be treated by placing client on her side and administering O2. ·1110 What is the most important indicator of fetal autonomic nervous system integrity/health? ·1111 Fetal heart rate variability ·1112 Name 4 causes of decreased FHR variability. ·1113 Hypoxia, acidosis, drugs, fetal sleep ·1114 State the most important action to take when a cord prolapse is determined. ·1115 Examiner should position mother to relieve pressure on the cord with fingers until emergency delivery is accomplished. ·1116 What is a “reactive” non-stress test? ·1117 FHR acceleration of 15 beats per minute for 15 seconds in response to fetal movement. ·1118 What are the dangers of nipple-stimulation stress test? ·1119 The inability to control “oxytocin” dosage and the chance of tetany/hyperstimulation. ·1120 Normal fetal scalp pH in labor is ____ and values below ____ indicate true acidosis. - 7.25-7.35 normal pH; 7.2 indicates true acidosis. INTRAPARTUM: ·1121 List five prodromal signs of labor the nurse might teach the client. ·1122 lightening, braxton-hicks contractions increase, bloody show, loss of mucous plug, burst of energy, and nesting behaviors. ·1123 How is true labor discriminated from false labor? ·1124 true labor: regular, rhythmic contractions that intensify with ambulation, pain in the abdomen sweeping around from the back, and cervical changes. False labor: irregular rhythm, abdominalpain (not in back) that decreases with ambulation. ·1125 State 2 ways to determine if the membranes have truly ruptured (ROM). ·1126 Nitrazine testing: paper turns dark blue or black. Demonstration of fluid “ferning” under microscope. ·1127 Are psychoprophylactic breathing techniques prescribed for use by the stage and phase of labor? ·1128 No, clients should use these techniques according to their discomfort level and change techniques when one is no longer working for relaxation. ·1129 Identify two reasons to withhold anesthesia and analgesia until the mid-active phase of Stage 1 labor. ·1130 if given too early, can retard labor; if given too late, can cause fetal distress ·1131 Hyperventilation often occurs to the laboring client. What results from hyperventilation and what actions should the nurse take to relieve the condition? ·1132 Respiratory alkalosis occurs which is caused by blowing off CO2 and is relieved by breathing into a paper bag or cupped hands. ·1133 Describe maternal changes that characterize the transition phase of labor. ·1134 irritability, unwillingness to be touched but does not want to be left alone, nausea and vomiting, and hiccupping. ·1135 When should a laboring client be examined vaginally? ·1136 Vaginal exams should be done prior to analgesia/anesthesia, to rule out cord prolapse, to determine labor progress if it is questioned, and to determine when pushing can begin. ·1137 Define cervical effacement. ·1138 the taking up of the lower cervical segment into the upper segment; shortening of the cervix expressed in percent from 0-100% or complete effacement. ·1139 Where is the fetal heart rate best heard? ·1140 through the fetal back in vertex, OA positions. ·1141 Normal fetal heart rate in labor is _____ = 110-160 bpm Normal maternal BP in labor is _____ = <140/90 Normal maternal pulse in labor is _____ = <100 bpm Normal maternal temperature in labor is _____ = <100.4 F ·1142 List four nursing actions for the 2nd stage of labor. ·1143 make sure cervix is completely dilated before pushing is allowed. Assess FHR with each contraction. Teach woman to hold breath for no longer than 5 seconds. Teach pushing technique. ·1144 List 3 signs of placental separation. ·1145 gush of blood; lengthening of cord, and globular shape of uterus ·1146 When should the postpartum dosage of Pitocin be administered? Why is it administered? ·1147 give immediately after placenta is delivered to prevent postpartum hemorrhage/atony. ·1148 State one contraindication to the use of ergot drugs (Methergine).·1149 Hypertension ·1150 State 5 symptoms of respiratory distress in the newborn. ·1151 tachypnea, dusky color, flaring nares, retractions, and grunting. ·1152 If meconium was passed in utero, what action must the nurse take in the delivery room? ·1153 arrange for immediate endotracheal tube observation to determine the presence of meconium below the vocal cords (prevents pneumonitis/meconium aspiration syndrome) ·1154 What score is considered a good Apgar score? ·1155 7 to 10 ·1156 What is the purpose of eye prophylaxis for the newborn? ·1157 prevent opthalmia neonatorum, which results from exposure to gonorrhea in vagina. ·1158 What is the danger associated with regional blocks? ·1159 hypotension resulting from vasodilation below the block, which pools blood in periphery reducing venous return. ·1160 What is the major cause of maternal death when general anesthesia is administered? ·1161 Aspiration of gastric contents ·1162 Why are PO medications avoided in labor? ·1163 gastric activity stops or slows in labor, decreasing absorption from PO route, may cause vomiting. ·1164 State the best way to administer IV drugs in labor. ·1165 at beginning of contraction, push a little medication in while uterine blood vessels are constricted, thereby reducing dose to fetus. ·1166 When is it dangerous to administer butorphanol (Stadol), an agonist/antagonist narcotic? ·1167 when the client is an undiagnosed drug abuser of narcotics, it can cause immediate withdrawal symptoms. ·1168 Hypotension often occurs after the laboring client receives a regional block. What is one of the first signs the nurse might observe? ·1169 Nausea ·1170 State three actions the nurse should take when hypotension occurs in a laboring client. ·1171 turn client to left side. Adminsiter O2 by mask at 10L/min. increase speed of intravenous infusion (if it does not contain medication). ·1172 The fourth stage is defined as: ·1173 the first 1 to 4 hours after delivery placenta. ·1174 What actions can the nurse take to assist in preventing postpartum hemorrhage? ·1175 massage the fundus (gently) and keep the bladder emptied. ·1176 To promote comfort, what nursing interventions are used for a 3rd degree episiotomy, which extends into the anal sphincter?·1177 ice pack, withc hazel compresses, and no rectal manipulation ·1178 What nursing interventions are used to enhance maternal-infant bonding during the 4th stage of labor? ·1179 withhold eye prophylaxis up to 2 hours. Perform newborn admission/routine procedures in room with parents. Encourage early initiation of breastfeeding. Darken room to encourage newborn to open eyes. ·1180 List 3 nursing interventions to ease the discomfort of afterpains. ·1181 keep bladder empty. Provide warm blanket to abdomen. Administer analgesics ordered by doctor. ·1182 List symptoms of a full bladder, which might occur in the 4th stage of labor. ·1183 fundus above umbilicus, dextroverted (to the right side of abdomen), increased bleeding (uterine atony). ·1184 What action should the nurse take first when a soft, boggy, uterus is palpated? ·1185 perform fundal massage ·1186 What are the symptoms of hypovolemic shock? ·1187 pallor, clammy skin, tachycardia, lightheadedness, and hypotension ·1188 How often should the nurse check the fundus during the 4th stage of labor? ·1189 q15 minutes X 4 (1 hour), q30 minutes X 2 hours if normal. NORMAL PUERPERIUM (POSTPARTUM): ·1190 A nurse discovers a postpartum client with a boggy uterus, displaced above and to the right of the umbilicus. What nursing action is indicated? ·1191 Perform immediate fundal massage. Ambulate to the bathroom or use bedpan to empty bladder because cardinal signs of bladder distention are present. ·1192 Which women experience afterpains more than others? ·1193 Breastfeeding women, multiparas, and women who experienced over distention of the uterus. ·1194 Upon admission to the postpartum room, 3 hours after delivery, a client has a temperature of 99.5F. What nursing actions are indicated? ·1195 Probably elevated due to dehydration and work of labor; force fluids and retake temperature in an hour; notify physician if above 100.4F. ·1196 A client feels faint on the way to the bathroom. What nursing assessments should be made? ·1197 Assess BP sitting and lying, assess Hgb and Hct for anemia. ·1198 What factor places the postpartum client at risk for thromboembolism? ·1199 Increased clotting factors. ·1200 A breastfeeding mother complains of very tender nipples. What nursing actions should be taken? ·1201 Have her demonstrate infant position on breast (incorrect positioning often causes tenderness). Leave bra open to air-dry nipples for 15 minutes 3X daily. Remove all “smothering” creams.·1202 Three days postpartum, a lactating mother has full, warm, taut, tender breasts. What nursing actions should be taken? ·1203 She is engorged; have newborn suckle frequently; use measures to increase milk flow; warm water, breast massage and supportive bra. ·1204 What information should be given to a client regarding resumption of sexual intercourse after delivery? ·1205 Avoid until postpartum exam. Use water soluble jelly. Expect slight discomfort due to vaginal changes. ·1206 A woman has decided to take birth control pills as her contraceptive method. What should she do if she misses taking the pill two consecutive days? ·1207 Take two pills for two days and use an alternate form of birth control. ·1208 A woman asks why she is urinating so much in the postpartum period. The nurse bases the response on what information. ·1209 Up to 3,000 cc per day can be voided due to the reduction of the 40% plasma volume increase during pregnancy. ·1210 A woman’s white blood count returns 17,000; she is afebrile and has no symptoms of infection. What nursing action is indicated? ·1211 Continue routine assessments; normal leukocytosis occurs during postpartal period because of placental site healing. ·1212 What is the most common cause of uterine atony in the first 24 hours postpartum? ·1213 full bladder ·1214 What is the purpose of giving docusate sodium (Colace) to the postpartum client? ·1215 to soften the stool in mother’s with 3rd and 4th degree episiotomies, hemorrhoids, or Cesarean section delivery. ·1216 What should the fundal height be at three days postpartum for a woman who has had a vaginal delivery? ·1217 3 fingerbreadths/cm below the umbilicus. ·1218 List 3 signs of positive bonding between parents and newborn? ·1219 Calling infant by name, exploration of newborn head to toe, en face position. THE NORMAL NEWBORN: ·1220 The newborn transitional period consists of the first ____ of life. ·1221 6 to 8 hours of life ·1222 The nurse anticipates which newborn will be more at risk for problems in the transitional period. State 3 predisposing factors to respiratory depression in the newborn. ·1223 Cesarean delivery; magnesium sulfate given to mother in labor; asphyxia/fetal distress in labor. ·1224 What is the danger of heat loss to the newborn in the first few hours of life? ·1225 Leads to depletion of glucose (very little glycogen storage in immature liver); begins to use brown fat for energy producing ketones causing subsequent ketoacidosis and shock.·1226 Normal newborn temperature is ____ = 97.7 – 99.4F Normal newborn heart rate is ____ = 110-160 bpm Normal newborn respiratory rate is ____ = 30-60 bpm Normal blood pressure is ____ = 80/50 ·1227 The nurse records a temperature below 97F on admission of the newborn. What nursing actions should be taken? ·1228 Place newborn in isolette or under radiant warmer and attach a temperature skin probe to regulate isolette or radiant warmer temperature. Wrap newborn double if no isolette or warmer available and put cap on head. Watch for signs of hypothermia and hypoglycemia. ·1229 True or False: the newborn’s head is usually smaller than the chest. ·1230 FALSE: head is usually 2 cm larger unless severe molding occurred. ·1231 During the physical exam of the newborn, the nurse notes the cry is shrill, highpitched, and weak. What are the possible causes? ·1232 CNS anomalies, brain damage, hypoglycemia, drug withdrawal. ·1233 The nurse notes a swelling over the back part of the newborn head. Is this normal newborn variation? ·1234 It depends on the exam. If it crosses suture lines and is a caput (edema), it is normal. If it does not cross suture lines, it is a cephalhematoma with bleeding between the skull and periosteum. This could cause hyperbilirubinemia. This is an abnormal variation. ·1235 What symptoms are common to most newborns with Down Syndrome? ·1236 Low set ears, simian crease on palm, protruding tongue, Brushfield’s spots in iris, epicanthal folds. ·1237 Identify 3 ways t determine presence of congenital hip dislocation in the newborn. ·1238 Hip click determination, asymmetrical gluteal folds, unequal limb lengths. ·1239 Should the normal newborn have a positive or negative Babinski reflex? ·1240 Positive. The transient reflex is present until 12-18 months of age. ·1241 A small-for-gestational age newborn is identified as one who ____. ·1242 Has a weight below the 10th percentile for estimated weeks of gestation. ·1243 When suctioning the newborn with a bulb syringe, which should be suctioned first, the mouth or the nose? ·1244 Mouth; stimulating the nares can initiate inspiration which could cause aspiration of mucus in oral pharynx. ·1245 A new mother asks the nurse if circumcision is medically indicated in the newborn. How should the nurse respond? ·1246 There is controversy concerning this issue, but we do know it causes pain and trauma to the newborn, and the medical indication may be unfounded. ·1247 Normal blood glucose in the term neonate is ____. = 40-80 mg/dl. ·1248 Why does the newborn need vitamin K in the 1st hour after birth? ·1249 Sterile gut at delivery lacks intestinal bacteria necessary for the synthesis of vitamin K; vitamin K is needed in the clotting cascade to prevent hemorrhagic disorders.·1250 Physiologic jaundice in the newborn occurs _____. It is caused by _____. ·1251 Jaundice occurs at 2-3 days of life and is caused by immature liver’s inability to keep up with bilirubin production of normal RBC destruction. ·1252 When is the screening test for phenylketonuria done? ·1253 At 2-3 days of life or after enough milk ingestion to determine body’s ability to metabolize amino acid phenylalanine. ·1254 A term newborn needs to take in _____ calories per pound per day. After the initial weight loss is sustained, the newborn should gain _____ per day. ·1255 50 calories; 1 ouncce or 30 grams. ·1256 List 5 signs and symptoms new parents should be taught to report immediately to a doctor or clinic. ·1257 Lethargy; temperature >100F, vomiting, green stools, refusal of 2 feeds in a row. HIGH-RISK DISORDERS: ·1258 What instructions should the nurse give the woman with a threatened abortion? ·1259 Maintain strict bedrest for 24-48 hrs. Avoid sexual intercourse for two weeks. ·1260 Identify the nursing plans and interventions for a woman hospitalized with hyperemesis gravidarum. ·1261 Weight daily; uring ketone checks 3X daily; progressive diet; check FHR q8h; monitor for electrolyte imbalances. ·1262 Describe discharge counseling for a woman after hydatidiform mole evacuation by D&C. ·1263 Prevent pregnancy for one year. Return to clinic/MD for monthly hCG levels for 1 yr. Post-op D&C instructions; call if bright red vaginal bleeding or foul smelling vaginal discharge occurs, or temperature spike over 100.4F. ·1264 What condition should the nurse suspect if a woman of childbearing age presents to an emergency room with bilateral or unilateral abdominal pain with or without bleeding? ·1265 Ectopic pregnancy ·1266 List 3 symptoms of abruptio placentae and 3 symptoms of placenta previa. ·1267 Abruption: fetal distress; rigid, board-like abdomen; pain; dark red or absent bleeding. Previa: painless, bright red vaginal bleeding; fetal heart rate normal; soft uterus. ·1268 What specific information should the nurse include when teaching human papillomavirus detection & treatment? ·1269 Detection of dry; wart-like growths on vulva or rectum. Need for pap smear in the prenatal period. Treatment with laser ablation (cannot use Podophyllin in pregnancy). Associated with cervical carcinoma in mother and respiratory papillomatosis in neonate. ·1270 State 3 principles pertinent to counseling and/or teaching a pregnant adolescent. ·1271 Nurse must establish trust/rapport before counseling/teaching begins. Adolescents do not respond to an authoritarian approach. Consider the developmental tasks of identity and social/individual intimacy. ·1272 What complications are pregnant adolescents more prone to develop? ·1273 PIH, IUGR, CPD, STDs, Anemia.·1274 All pregnant women should be taught preterm labor recognition. Describe the warning symptoms of preterm labor. ·1275 More than 5 contractions/hour, cramps, low, dull backache; pelvic pressure; change in vaginal discharge. ·1276 List the predisposing factors to preterm labor. ·1277 Urinary tract infection; over distention of uterus; diabetes; PIH; cardiac disease; placenta previa, psychosocial factors, i.e., stress ·1278 When is preterm labor able to be arrested? ·1279 Cervix is <4cm dilated, <50% effacement, and membranes intact and not bulging out of the cervical os. ·1280 What is the major side effect of beta-adrenergic (Terbutaline, Ritodrine) tocolytic drugs? ·1281 Tachycardia ·1282 What special actions should the nurse take in the intrapartum period if preterm labor is unable to be arrested? ·1283 Monitor the FHR continuously and limit drugs, which cross placental barriers to prevent fetal depression or further compromise. ·1284 A prolonged latent phase for a multipara is ____ and for a nullipara is ____. Multiparas average cervical dilatation is ____cm/hr in the active phase and nulliparas average cervical dilatation is ____cm/hr in the active phase. ·1285 >14 hours, >20 hours, 1.5 cm/her; 1.2 cm/hr. ·1286 What are the major goals of nursing care related to pregnancy-induced hypertension with preeclampsia? ·1287 Maintenance of uteroplacental perfusion; prevention of seizures; prevention of complications such as HELLP syndrome, DIC and abruption. ·1288 Magnesium sulfate is used to treat PIH. A) What is the purpose for administration of magnesium sulfate? B) What is the main action of magnesium sulfate? C) The antidote for magnesium sulfate? D) List the 3 main assessment findings indicating toxic effects of magnesium sulfate. ·1289 A) Prevent seizures by decreasing CNS irritability B) Central nervous system depression (seizure prevention) C) Calcium Gluconate D) Reduced urinary output, reduced respiratory rate, and decreased reflexes. ·1290 What are the major symptoms of pregnancy induced hypertension (preeclampsia)? ·1291 Increase in BP of 30mmHg systolic and 15 mmHg diastolic over previous baseline; hyperflexia; proteinuria (albuminuria); CNS disturbances; headache, and visual disturbances; epigastric pain. ·1292 What is the priority nursing action after spontaneous or artificial rupture of membranes? ·1293 Assessment of the fetal heart rate. ·1294 What is the most common complication of oxytocin augmentation or induction of labor? List 3 actions the nurse should take if such a complication occurs. ·1295 Tetany. Turn off Pitocin. Turn pregnant woman to side. Administer O2 by face mask.·1296 List the symptoms of water intoxification from the antidiuretic hormone (ADH) effect of Pitocin (oxytocin). ·1297 Nausea and vomiting, headache, and hypotension. ·1298 State 3 nursing interventions during FORCEPS delivery. ·1299 Ensure empty bladder. Auscultate FHR before application, during, and between traction periods. Observe for maternal lacerations and newborn cerebral/facial trauma. ·1300 What is the cause of pregnancy induced hypertension? ·1301 The person who determines the exact cause will be our next NOBEL prize winner! However, the underlying pathophysiology appears to be generalized vasospasm with increased peripheral resistance and vascular damage. This decreased perfusion results in damage to numerous organs. ·1302 What interventions should the nurse implement to prevent further CNS irritability in the PIH client? ·1303 Darken room, limit visitors, maintain close 1:1 nurse/client ratio, place in private room, plan nursing interventions all together so client is disturbed as little as possible. ·1304 A woman on Orinase (oral hypoglycemic) asks the nurse if she can continue this medication in pregnancy. How should the nurse respond? ·1305 No, oral hypoglycemic medications are teratogenic to the fetus. Insulin will be used. ·1306 Name 3 maternal & 3 fetal complications of gestational diabetes. ·1307 Maternal: hypoglycemia, herperglycemia, ketoacidosis; Fetal: macrosomia, hypoglycemia at birth, fetal anomalies ·1308 When should the nurse hold the dose of magnesium sulfate and call the physician? ·1309 When the client’s respirations are <12/minute, DTRs are absent, or urinary output is <100cc/4 hours ·1310 State 3 priority nursing actions in the postdelivery period for the client with PIH. ·1311 Monitor for signs of blood loss. Continue to assess BP and DTRs q4 hours. Monitor for uterine atony. ·1312 When are the 2 most difficult times for control for the pregnant diabetic? ·1313 Late in the 3rd trimester and in the postpartum period when insulin needs to drop sharply (the diabetogenic effects of pregnancy drop precipitously). ·1314 Why is regular insulin used in labor? ·1315 It is short-acting, predictable, can be infused intravenously and discontinued quickly if necessary. ·1316 List 3 conditions clients with diabetes mellitus are more prone to develop. ·1317 PIH, hydramnios; infection ·1318 When is cardiac disease in pregnancy most dangerous? ·1319 At peak plasma volume increase, 28-32 weeks gestation and during Stage II labor. ·1320 Does insulin cross the placental/breast barrier? ·1321 No, therefore insulin-dependent women may breastfeed.·1322 The goal for diabetic management during labor is euglycemia. How is it defined? ·1323 60-100 mg/dl. ·1324 What contraceptive technique is recommended for diabetic women? ·1325 Diaphragm with spermicide. Avoid birth control pills that contain estrogen and IUDs, which are an infection risk. ·1326 List the symptoms of cardiac decompensation in the laboring client with cardiac disease. ·1327 Tachycardia, tachypnea, dry cough, rales in lung bases, dyspnea, and orthopnea. ·1328 What interventions can the nurse implement to maintain cardiac perfusion in a laboring cardiac client? ·1329 Position client in a semi or high-Fowler’s position. Prevent Valsalva’s maneuvers. Position client in a supine or R/T for regional anesthesia. Avoid stirrups because of possible popliteal vein compression and decreased venous return. ·1330 Gentle counterpressure against the perineum during an emergency delivery prevents ____ and ____. ·1331 Maternal lacerations, fetal cerebral trauma. ·1332 When may a vaginal birth after Cesarean (VBAC) be considered by a woman with a previous c-section? ·1333 If a low uterine transverse incision was performed and can be documented AND if the original complication does not recur, i.e., CPD. ·1334 Prior to anesthesia for C-section delivery, the mother may be given an antacid or a gastric antisecretory drug (histamine receptor antagonist). State the reasons why these drugs are given. ·1335 Antacid buffers alkalize the stomach secretions. If aspiration occurs, less lung damage ensues. An antisecretory drug reduces gastric acid, reducing the risk of gastric aspiration. ·1336 Clients who have had a C-section are prone to what post-op complications? ·1337 Paralytic ileus, infection, thromboembolism, respiratory complications, and impaired maternal infant bonding. POSTPARTUM HIGH-RISK DISORDERS: ·1338 May women with a positive HIV antibody test breastfeed? ·1339 No, HIV has been found in breast milk. ·1340 What are the common side effects of antibiotics used to treat puerperal infection? ·1341 GI adverse reactions: nausea, vomiting, diarrhea, and cramping. Hypersensitivity reactions: rashes, urticaria, and hives ·1342 How does the nurse differentiate symptomatology of cystitis from pylonephritis? ·1343 Pyelonephritis has the same symptoms as cystitis (dysuria, frequency, and urgency) with the addition of flank pain, fever, and pain at costovertebral angle. ·1344 What are the signs of endometritis? ·1345 Subinvolution (boggy, high uterus), lochia returns to rubra with possible foul smell, temperature 100.4F or higher, unusual fundal tenderness.·1346 What are the nursing actions for endometritis and parametritis? ·1347 Measures to promote lochial drainage; antipyretic measures (acetaminophen, cool baths); administration of analgesics and antibiotics as ordered; increase fluids with attention to high protein/high vitamin C diet. ·1348 State 4 risk factors or predisposing factors t opostpartum infection. ·1349 Operative delivery, intrauterine manipulation , anemia or poor physical health, traumatic delivery, and hemorrhage. ·1350 State 4 risk factors or predisposing factors to postpartum hemorrhage. ·1351 Dystocia or prolonged labor, over distention of the uterus, abruptio placentae, and infection ·1352 What immediate nursing actions should be taken when a postpartum hemorrhage is detected? ·1353 Fundal massage. Notify MD if massage does NOT firm fundus. Count pads to estimate blood loss. Assess/record vital signs. Increase IV fluids and administer oxytocin infusion as ordered. ·1354 Must women diagnosed with mastitis stop breastfeeding? ·1355 No, women who abruptly stop breastfeeding may make the situation worse by increasing congestion/engorgement and providing further media for bacterial growth. Client may HAVE to discontinue breastfeeding if pus is present or if antibiotics are contraindicated for neonate. NEWBORN HIGH-RISK DISORDERS: ·1356 List the major CNS danger signals, which occur in the neonate. ·1357 Lethargy, high-pitched cry, jitteriness, seizures, and bulging fontanels. ·1358 A baby is delivered blue, limp, and with a heart rate <100. The nurse dries the infant, suctions the oropharynx and gently stimulates the infant while blowing O2 over the face. The infant still does not respond. What is the next nursing action? ·1359 Begin oxygenation by bag and mask at 30-50 breaths/minute. Assist physician in setting up for intubation procedure. ·1360 What does the Silverman-Anderson index measure? ·1361 Respiratory difficulty ·1362 What are the two major complications of O2 toxicity? ·1363 Retrolental fibroplasias and bronchopulmonary dysplasia. ·1364 Necrotizing enterocolitis results from ____ and is manifested by ____. Ischemia/hypoxia results in ____. ·1365 Ischemis hypoxia; abdominal distention, sepsis and a lack of absorption from intestines. Injury to the intestinal mucosa. ·1366 Intraventricular hemorrhage is more common in ____ and results in symptoms of ____. ·1367 Premature neonates and VLBW babies. ·1368 What conditions make oxygenation of the newborn more difficult? ·1369 Respiratory distress syndrome; alveolar prematurity/lack of surfactant, anemia and polycythemia. ·1370 In order to prevent problems with oxygenating the newborn, what parameters can the nurse observe?·1371 PO2 50-90, SVO2 60-80 mmHg. ·1372 What are the cardinal symptoms of sepsis in a newborn? ·1373 Lethargy, temperature instability, difficulty feeding, subtle color changes, subtle behavioral changes and hyperbilirubinemia. ·1374 A premature baby is born and develops hypothermia. State the major nursing interventions to treat hypothermia. ·1375 Place under radiant warmer or in incubator with temperature skin probe over liver. Warm all items touching the newborn. Place plastic wrap over neonate. ·1376 Nurses often weigh diapers in order to determine exact urine output in the high-risk neonate. Explain this procedure. ·1377 Diaper is weighed in grams before applying. Weigh diaper after wetting. Calculate and record each gram or added weight as one cc of urine. ·1378 What factors does the nurse look for in determining the newborn’s ability to take in nourishment by nipple/mouth? ·1379 Good suck, coordinated suck-swallow, takes less than 20 minutes to feed, gaining 20-30 gm/day. ·1380 What complications are associated with total parenteral nutrition (TPN)? ·1381 Hyperglycemia, electrolyte imbalance, dehydration, and infection. ·1382 In order to prevent rickets in the preterm newborn, what supplement is given? ·1383 Calcium and vitamin D. ·1384 List 4 nursing interventions to enhance family/parent adjustment to a high-risk newborn. ·1385 Initiate early visitation at ICU. Provide daily information to family. Encourage participation in support group for parents. Encourage all attempts at care-giving (enhances bonding). ·1386 List risk factors for hyperbilirubinemia. ·1387 Rh incompatibility, ABO incompatibility, prematurity, sepsis, perinatal asphyxia. ·1388 List symptoms of hyperbilirubinemia in the neonate. ·1389 Bilirubin levels rising 5mg/day, jaundice, dark urine, anemia, high reticulocyte (RBC) count, and dark stools. ·1390 Write one nursing diagnosis generated from the data pertinent to hyperbilirubinemia. ·1391 Potential for injury related to predisposition of bilirubin for fat cells in brain. ·1392 List 3 nursing interventions for the neonate undergoing phototherapy. ·1393 Apply opaque mask over eyes. Leave diaper loose so stools/urine can be monitored. Turn every 2 hours. Watch for dehydration. ·1394 List the symptoms of neonatal narcotic withdrawal. ·1395 Irritability, hyperactivity, high-pitched cry, frantic sucking, coarse flapping tremors, and poor feeding. ·1396 Neonates who are “sick” are prone to receive too much stimulation in the form of invasive procedures and handling too little developmentally-appropriate stimulation andaffection. How might such an infant respond? ·1397 Failure to thrive, lack of crying. ·1398 How should the nurse determine the length of a tube needed for oral gavage feeding of a newborn? ·1399 From the bridge of the nose, to the earlobe, to a point halfway between the xiphoid and the umbilicus. ·1400 What are the 2 best ways to test for correct placement of the gavage tube in the infant’s stomach? ·1401 Aspiration of stomach contents with pH testing, and auscultation of air bubble injected into stomach. ·1402 What characteristics would the nurse expect to see in a neonate with fetal alcohol syndrome? ·1403 Microcephaly, growth retardation, short palpebral fissures, and maxillary hypophysia. ALL HESI HINTS ADVANCED CLINICAL CONCEPTS ·1404 ARDS is an unexpected, catastrophic pulmonary complication occurring in a person with no previous pulmonary problems. The mortality rate is high (50%) ·1405 In ARDS, a common laboratory finding is lowered PO2. However, these clients are not very responsive to high concentrations of oxygen. ·1406 Think about the physiology of the lungs by remembering PEEP: Positive End Expiratory Pressure is the instillation and maintenance of small amounts of air into the alveolar sacs to prevent them from collapsing each time the client exhales. The amount of pressure can be set with the ventilator and is usually around 5 to 10 cm of water. ·1407 Suction only when secretions are present. ·1408 Before drawing arterial blood gases from the radial artery, perform the Allen test to assess collateral circulation. Make the client’s hand blanch by obliterating both the radial and ulnar pulses. Then release the pressure over the ulnar artery only. If flow through the ulnar artery is good, flushing will be seen immediately. The Allen test is then positive, and the radial artery can be used for puncture. If the Allen test is negative, repeat on the other arm. If this test is also negative, seek another site for arterial puncture. The Allen test ensures collateral circulation to the hand if thrombosis of the radial artery should follow the puncture. ·1409 If the client does not have O2 to his/her brain, the rest of the injuries do not matter because death will occur. However, they must be removed from any source of imminent danger, such as a fire. ·1410 PC)2 >45 or PO2 <60 on 50% O2 signifies respiratory failure. ·1411 A child in severe distress should be on 100% O2. ·1412 Early signs of shock are agitation and restlessness resulting from cerebral hypoxia.·1413 If cardiogenic shock exists with the presence of pulmonary edema, i.e., from pump failure, position client to REDUCE venous return (HIGH FOWLER’s with legs down) in order to decrease venous return further to the left ventricle. ·1414 Severe shock leads to widespread cellular injury and impairs the integrity of the capillary membranes. Fluid and osmotic proteins seep into the extra vascular spaces, further reducing cardiac output. A vicious cycle of decreased perfusion to ALL cellular level activities ensues. All organs are damaged, and if perfusion problems exist, the damage can be permanent. ·1415 All vasopressors/vasodilator drugs are potent and dangerous and require weaning on and off. Do not change infusion rates simultaneously. ·1416 A client is brought into the hospital suffering shock symptoms as a result of a bee sting. What is the first priority? Maintaining an open airway (the allergic reaction damages the lining of the airways causing edema). Also, keep the client warm without constricting clothing; keep legs elevated (not Trendelenburg because the weight of the lower organs restricts breathing). ·1417 Epinephrine: 1:1000, 0.2 to 0.5ml subq for mild ·1418 Epinephrine: 1:10,000, or 5ml IV for severe ·1419 Volume expanding fluids are usually given to clients in shock. However, if the shock is cardiogenic, pulmonary edema may result. ·1420 Drugs of choice for shock ·1421 Digitalis preparations: Increase the contractility of the heart muscle ·1422 Vasoconstrictors (Levophed, Dopamine): Generalized vasonconstriction to provide more available blood to the heart to help maintain cardiac output. ·1423 A common volume-expanding substance is plasma and possibly whole blood. ·1424 You are caring for a woman who was in severe automobile accident several days ago. She has several fractures and internal injuries. The exploratory laparotomy was successful in controlling the bleeding. However, today you find that this client is bleeding from her incision, short of breath, has a weak thready pulse, has cold and clammy skin, and hematuria. ·1425 What do you think is wrong with the client, and what would you expect to do about it? ·1426 These are typical signs and symptoms of DIC crisis. Expect to administer IV heparin to block the formation of thrombin (Coumadin does not do this). However, the client described is already past the coagulation phase and into the hemorrhagic phase. Her management would be administration of clotting factors along with palliative treatment of the symptoms as they arise. (Her prognosis is poor). ·1427 NCLEX-RN questions on CPR often deal with prioritization of actions. Question: What actions are required for each of the following situations? ·1428 A 24-year old motorcycle accident vistim with a ruptured artery if the leg is pulseless and apneic. ·1429 A 36-year old first time pregnant woman who arrests during labor. ·1430 A 17-year old with no pulse or respirations who is trapped in an overturned car, which is starting to catch fire. ·1431 A 40-year old businessman who arrests two days after a cervical laminectomy. ·1432 WHEN TO SEEK EMERGENCY MEDICAL SERVICE (EMS)·1433 The American Heart Association recommends that those with known angina pectoris seek emergency medical care if chest pain is NOT relieved by three nitroglycerin tablets 5 minutes apart over a 150minute period. ·1434 A person with previously unrecognized coronary disease experiencing chest pain persisting for 2 minutes or longer should seek emergency medical treatment. ·1435 It is important for the nurse to stay current with the American Heart Association’s guidelines for Basic Life Support (BLS) by being certified every two years as required. ·1436 If one rescuer is performing CPR, 1 15:2 ratio of compression to ventilations is performed for 4 cycles, then reassess for breathing and pulse. If two rescuers are performing CPR, a 15:2 ratio is now recommended for compressions to ventilations. Perform for 15 cycles with a 100/min compression rate. When trading off, start with compressions. ·1437 Initiate CPR with BLS guidelines immediately, then move on to Advanced Cardiac Life Support (ACLS) guidelines. ·1438 When significant arterial acidosis is noted, try to reduce PCO2 by increasing ventilation, which will correct arterial, venous, and tissue acidosis. Bicarbonate may exacerbate acidosis b producing CO2. Thus, the ACLS guidelines have recommended bicarbonate NOT be used unless hyperkalemia and/or preexisting acidosis is documented. ·1439 Infants/prematures may have problems with the following that can predispose to arrest: Beware of the “H’s” – hypoxia, hypoglycemia, hypothermia, increased H+ (metabolic and/or respiratory acidosis), hypercoagulability (if polycythemia exists). ·1440 Changes is osmolarity cause shifts in fluid. The osmolarity of the extracellular fluid (ECF) is almost entriely due to sodium. The osmolarity of intracellular fluid (ICF) is related to many particles, with potassium being the primary electrolyte. The pressures in the ECF and the ICF are almost identical. If either ECF or ICF change in concentration, fluid shifts from the area of lesser concentration to the area of greater concentration. ·1441 Dextrose 10% is a hypertonic solution and should be administered IV. ·1442 Normal saline is an isotonic solution and is used for irrigations, such as bladder irrigations or IV flush lines with intermittent IV medication. ·1443 Use only isotonic (neutral) solutions in irrigations, infusions, etc., unless the specific aim is to shift fluid into intracellular or extracellular spaces. ·1444 Potassium imbalances are potentially life-threatening, must be corrected immediately. A low magnesium often accompanies a low K+, especially with the use of diuretics. ·1445 Fluid Volume Deficit: Dehydration ·1446 Elevated BUN: The BUN measures the amount of urea nitrogen in the blood. Urea is formed in the liver as the end product of protein metabolism. The BUN is directly related to the metabolic function of the liver and the excretory function of the kidneys. ·1447 Creatinine, as with BUN, is excreted entirely by the kidneys and is therefore directly proportional to renal excretory function. However, unlike BUN, the creatinine level is affected very little by dehydration, malnutrition, or hepatic function. The daily production of creatinine depends on muscle mass, which fluctuates very little. Therefore, it is a better test of renal function than is the BUN. Creatinine is generally used in conjunction with the BUN test and they normally are in a 1:20 ratio. ·1448 Serum osmolality measures the concentration of particles in a solution. It refers to the fact that the same amount of solute is present, but the amount of solvent (fluid) is decreased.Therefore, the blood can be considered “more concentrated.” ·1449 Urine osmolality and specific gravity increase. ·1450 Check the IV tubing container to determine the drip factor because drip factors vary. The most common drip factors are 10, 12, 15, and 60 drops per milliliter. A microdrip is 60 drops per milliliter. ·1451 Flushing a saline lock requires approximately 1 ½ times the amount of fluid that the tubing will hold in order to efficiently flush the tubing. REMEMBER to use sterile technique to prevent complications such as infiltration, emboli and infection. ·1452 A pH of less than 6.8 or more than 7.8 is NOT COMPATIBLE WITH LIFE. ·1453 The acronym ROME can help you remember: Respiratory, Opposite, Metabolic, Equal. ·1454 Review the order of blood flow to the heart: ·1455 Unoxygenated blood flows from the superior and inferior vena cava into the right atrium, then to the right ventricle. It flows out of the heart through the pulmonary artery, to the lungs for oxygenation. The pulmonary vein delivers oxygenated blood back to the left atrium, then to the left ventricle (largest, strongest chamber) and out the aorta. ·1456 Review the three structures that control the one-way flow of blood through the heart: ·1457 Valves→ Atrioventricular valves → Tricuspid (right side) → Mitral (left side) Semilunar valves → Pulmonary (in pulmonary artery) → Aortic (in aorta) ·1458 Cordae Tendinae ·1459 Papillary muscles ·1460 Since the T waves represents repolarization of the ventricle, this is a critical time in the heartbeat. This action represents a resting and regrouping stage so that the next heartbeat can occur. If defibrillation occurs during this phase, the heart can be thrust into a life-threatening dysrhythmia. ·1461 Observe the client for tolerance of the current rhythm. This information is the most important data the nurse can collect on the client with an arrythmia. ·1462 REMEMBER to monitor the client as well as the machine! If the EKG monitor shows a severe dysrhythmia, but the client is sitting up quietly watching a TV without any sign of distress, assess to determine if the leads are attached properly. ·1463 Marking the operative site is required for procedures involving right/left distinctions, multiple structures (fingers, toes), or levels (spinal procedures). Site marking should be done with the involvement of the client. ·1464 Wound dehiscence is separation of the wound edges and is more likely to occur with vertical incisions. It usually occurs after the early postoperative period, when the client’s own granulation tissue is “taking over” the wound, after absorption of the sutures has begun. Evisceration of the wound is protrusion of intestinal contents (in an abdominal wound) and is more likely in clients who are older, diabetic, obese, or malnourished and have prolonged paralytic ileus. ·1465 NCLEX-RN items will focus on the nurse’s role in terms of the entire perioperative process. Sample: A 43-year old mother of 2 teenage daughters enters the hospital to have her gallbladder removed in a same-day surgery using a scope instead of an incision. What nursing needs will dominate each phase of her short hospital stay? ·1466 Preparation phase: Education about postoperative care, NPO, assist with meeting family needs.·1467 Operative phase: Assessment, management of the operative suite. ·1468 Post-anesthesia phase: Pain management, post-anesthesia precautions. ·1469 Post-operative phase: Prevent and assess for complications, pain management, dietary restrictions, activity. ·1470 HIV clients with tuberculosis require respiratory isolation. Tuberculosis is the only real risk to non-pregnant caregivers that is not related to a break in universal precautions (i.e., needle sticks, etc.). ·1471 STANDARD PRECAUTIONS: ·1472 Wash hands, even if gloves have been worn to give care ·1473 Wear gloves (latex) for touching blood or body fluids, or any non-intact body surface. ·1474 Wear gowns during any procedure that might generate splashes (changing clients with diarrhea). ·1475 Use masks and eye protection during activity which might disperse droplets (suctioning). ·1476 Do not recap needles, dispose of in puncture-resistant containers. ·1477 Use mouth piece for resuscitation efforts. ·1478 Refrain from giving care if you have open skin lesions. ·1479 Caregivers who are pregnant may choose not to care for a client with Cytomegalovirus (CMV). ·1480 Pediatric HIV is often evidenced by lymphoid interstitial pneumonitis. ·1481 The focus of NCLEX-RN questions is likely to be assessment of early signs of the disease and management of complications associated with HIV. ·1482 For narcotic induced respiratory depression, administer Naloxone 0.1mg to 0.4mg IV every 2- 3 minutes as needed, until 1.0mg is achieved. ·1483 Use non-invasive methods for pain management when possible: ·1484 Relaxation techniques ·1485 Distraction ·1486 Imagery ·1487 Biofeedback ·1488 Interpersonal skills ·1489 Physical care: altering positions, touch, hot and cold applications. ·1490 Narcotic analgesics are prepared for pain relief because they bind to the various opiate receptor sites in the CNS. Morphine is often the preferred narcotic (REMEMBER: it causes respiratory depression). ·1491 Other agonists are meperidine and methadone. Narcotic antagonists block the attachment of narcotics to the receptors, such as Narcan (naloxone). Once Narcan has been given, additional narcotics cannot be given until the Narcan effects have passed. ·1492 Do not take away the coping style used in a crisis state…DENIAL. It is a useful and needed tool at the initial stage for some. Support, do not challenge, unless it hinders/blocks treatment – endangering the patient.MEDICAL –SURGICAL NURSING RESPIRATORY SYSTEM ·1493 Fever can cause dehydration from excessive fluid loss in diaphoresis. Increased temperature also increases metabolism and the demand for oxygen. ·1494 High risk for pneumonia: ·1495 Any person, who has altered level of consciousness, has depressed or absent gag reflex and cough reflexes, is susceptible to aspirating oropharyngeal secretions. (Alcoholics, anesthesized individuals, those with brain injury, drug overdose, or stroke victims). ·1496 When feeding, raise the head of the bed and position the client on side – not on back. ·1497 Bronchial breath sounds are heard over areas of density or consolidation. Sound waves are easily transmitted over consolidated tissue. ·1498 Hydration – enables liquification of mucous trapped in the bronchioles and alveoli, facilitating expectoration. Essential for the client experiencing fever. Important because 300 to 400 ml of fluid are lost daily by the lungs through evaporation. ·1499 Irritability and restlessness are early signs of cerebral hypoxia – the client is not getting enough oxygen to the brain. ·1500 Pneumonia preventatives: ·1501 Elderly: flu shots; pneumonia immunizations; avoiding sources of infection and indoor pollutants (dust, smoke, and aerosols); do not smoke. ·1502 Immunosuppressed and debilitated persons: infection avoidance, sensible nutrition, adequate intake, balance of rest and activity. ·1503 Comatose and immobile persons: elevate head of bed to feed; turn frequently. ·1504 Compensation occurs over time in clients with chronic lung disease, and arterial blood gases (ABGs) are altered. It is imperative that baseline data are obtained on the client. ·1505 Productive cough and comfort can be facilitated by Semi-Fowler’s or high Fowler’s positions, which lessen pressure on the diaphragm from abdominal organs. Gastric distention becomes a priority in these clients because it elevates the diaphragm and inhibits lung expansion. ·1506 Pink puffer: Barrel chest is indicative of emphysema and is caused by use of accessory muscles to breathe, which causes the person to work harder to breathe, but the amount of O2 taken in in adequate to oxygenate the tissues. ·1507 Blue bloater: insufficient oxygenation occurs with chronic bronchitis and leads to generalized cyanosis and often right-sided heart failure. ·1508 Cells of the body depend on oxygen to carry out their functions. Inadequate arterial oxygenation is manifested by cyanosis and slow capillary refill (<3 seconds). A chronic sign is clubbing of the fingernails, and a late sign is clubbing of the fingers. ·1509 Caution must be used in administering O2 to COPD client. The stimulus to breathe is hypoxia (hypoxic drive) not the usual hypercapnia, the stimulus to breathe for healthy persons. Therefore, if too much oxygen is given, the client may stop breathing!·1510 Health Promotion: ·1511 Eating consumes energy needed for breathng. Offer mechanically soft diets, which do not require as much chewing and digestion. Assist with feeding if needed. ·1512 Prevent secondary infections – avoid crowds, contact with persons who have infectious diseases, and respiratory irritants (tobacco smoke). ·1513 Teach client to report any change in characteristics of sputum. ·1514 Encourage client to hydrate well and to obtain immunizations needed (flu and pneumonia). ·1515 When asked to prioritize nursing actions, use the ABC rule: ·1516 Airway first ·1517 Then breathing ·1518 Then circulation ·1519 Look and listen. If breath sounds are clear, but the client is cyanotic and lethargic, adequate oxygenation is not occurring. ·1520 The key to respiratory status assessment of breath sounds as well as visualization of the client. Breath sounds are better “described,” not named, e.g., sounds should be described as “crackles,” “wheeze,” “hihg-pitched whistling sound,” rather than “rales,” “rhonchi,” etc., which may not mean the same thing to each clinical professional. ·1521 Watch for NCLEX-RN questions that deal with oxygen delivery. In adults, O2 must bubble through some type of water solution so it can be humidified if given at >4 L/min or delivered directly to the trachea. If given at 1 to 4 L/min or by mask or nasal prongs, the oropharynx and nasal pharynx provide adequate humidification. ·1522 With cancer of the larynx, the tongue and mouth often appear white, gray, dark brown, or black, and may appear patchy. ·1523 Tracheostomy care involves cleaning the inner cannula, suctioning, and applying a clean dressing. ·1524 Air entering the lungs is humidified along the naso-bronchial tree. This natural humidifying pathway is gone for the client who has had a laryngectomy. If the air is not humidified before entering the lungs, secretions tend to thicken and become crusty. ·1525 A laryngectomy tube has a larger lumen and is shorter than the tracheostomy tube. Observe the client for any signs of bleeding or occlusion, which are the greatest immediate postoperative risks (first 24 hours). ·1526 Fear of choking is very real for laryngectomy clients. They cannot cough as before because the glottis is gone. Teach the “glottal stop” technique to remove secretions (take a deep breath, momentarily occlude the tracheostomy tube, cough, and simultaneously remove the finger from the tube). ·1527 TB SKIN TEST: a positive TB skin test is exhibited by an induration 10mm or greater in diameter 48 hours after skin test. Anyone who has received a BCG vaccine will have a positive skin test and must be evaluated using a chest x-ray. ·1528 Teaching is very important with the TB client. Drug therapy is usually long term (9 months or longer). It is essential that the client take the medications as prescribed for the entire time. Skipping doses or prematurely terminating the drug therapy can result in a public health hazard. ·1529 TEACHING POINTS –·1530 Rifampin: Reduces effectiveness of oral contaceptives; should use other birth control methods during treatment; gives body fluids orange tinge; stains soft contacts. ·1531 Isoniazid (INH): Increases Dilantin levels. ·1532 Ethambutal: Vision check before starting therapy and monthly; may have to take 1 to 2 years longer. ·1533 Teach rationale for combination drug therapy to increase compliance. Resistance develops more slowly if several anti-TB drugs given, instead of just one drug at a time. ·1534 Some tumors are so large that they fill entire lobes of the lung. When removed, large spaces are left. Chest tubes are not usually used with these clients because it is helpful if the mediastinal cavity, where the lung used to be, fills up with fluid. This fluid helps prevent a shift of the remaining chest organs to fill the empty space. ·1535 If the chest tube remains disconnected, do not clamp! Immediately place the end of the tube in a container of sterile saline or water until a new drainage system can be connected. ·1536 If the chest tube is accidentally removed from the client, the nurse should apply pressure immediately with an occlusive dressing and notify the healthcare provider. ·1537 Chest Tube NCLEX-RN content: Fluctuations (tidaling) in the fluid will occur if there is no external suction. These fluctuating movements are a good indicator that the system is intact and should move upward with each inspiration and downward with each expiration. If fluctuations cease, check for kinked tubing, accumulation of fluid in the tubing, occlusions, or change in the client’s position, since expanding lung tissue may be occluding the tube opening. Remember, when external suction is applied the fluctuations cease. Most hospitals DO NOT MILK chest tubes as a means of clearing or preventing clots – it is too easy to remove chest tubes. Mediastinal tubes may have orders to be stripped because of location, compared to larger thoracic cavity tubes. ·1538 Various pathophysiological conditions can be related to the nursing diagnosis “Ineffective Breathing Patterns.” ·1539 Inability of air sacs to fill and empty properly (emphysema, cystic fibrosis) ·1540 Obstruction of the air passages (carcinoma, asthma, chronic bronchitis) ·1541 Accumulation of fluid in the air sacs (pneumonia) ·1542 Respiratory muscle fatigue (COPD, pneumonia) RENAL SYSTEM ·1543 Normally, kidney excrete approximately 1ml of urine per kg of body weight per hour, which is about 1 to 2 liters in a 24-hour period. ·1544 Electrolytes are profoundly affected by kidney problems. There must be a balance between extracellular fluid and intracellular fluid to maintain homeostasis. A change in the number of ions or in the amount of fluid will cause a shift in one direction or the other. Sodium and chloride are the primary extracellular ions. Potassium and phosphate are the primary intracellular ions. ·1545 In some cases, persons in ARF may not experience the oliguric phase but may progress directly to diuretic phase during which the urine output may be as much as 10 liters per day. ·1546 Body weight is a good indicator of fluid retention and renal status. Obtain accurate weights on all clients with renal failure – done on the same scale at the same time every day. ·1547 Fluid Volume Alterations Fluid·1548 Excess symptoms: ·1549 Dyspnea ·1550 Tachycardia ·1551 Jugular vein distention ·1552 Peripheral edema ·1553 Pulmonary edema ·1554 Fluid deficit symptoms: ·1555 Decreased urine output ·1556 Reduction in body weight ·1557 Decreased body turgor ·1558 Dry mucous membranes ·1559 Hypotension ·1560 Tachycardia ·1561 Watch for signs of hyperkalemia: dizziness, weakness, cardiac irregularities, muscle cramps, diarrhea, and nausea. ·1562 Potassium has a critical safe range (3.5 to 5.0 mEg/L) because it affects the heart, and any imbalance must be corrected by medications or dietary modification. Limit high potassium foods (bananas, avocados, spinach, fish) and salt substitutes, which are high in potassium. ·1563 Clients with renal failure retain sodium. With water retention, the sodium becomes diluted and serum levels may appear near normal. With excessive water retention, the sodium levels appear decreased dilution). Limit fluid and sodium intake in ARF clients. ·1564 During oliguric phase, minimize protein intake. When the BUN and creatinine return to normal, aRF is determined to be resolved. ·1565 Accumulation of waste products from protein metabolism is the primary cause of uremia. Protein must be restricted in CRF clients. However, if protein intake is inadequate, a negative nitrogen balance occurs causing muscle wasting. The glomerular filtration rate (GFR) is most often used as an indicator of level of protein consumption. ·1566 DIALYSIS COVERED BY MEDICARE: ·1567 All persons in the United States are eligible for Medicare as of their first day of dialysis under special End Stage Renal Disease funding. ·1568 Medicare card will indicate ESRD. ·1569 Transplantation is covered by Medicare procedure; coverage terminates six months postoperative if dialysis is no longer required. ·1570 Protein intake is restricted until blood chemistry shows ability to handle protein catabolites: urea, creatinine. Ensure high calorie intake so protein is spared for its own work: give hard candy, jelly beans, flavored carbohydrate powders. ·1571 As kidneys fail, medications must often be adjusted. Of particular importance is digoxin toxicity since digitalis preparations are excreted by the kidneys. Signs of toxicity in adults include nausea, vomiting, anorexia, visual disturbances, restlessness, headache, cardiac arrythmias, and pulse <60 beats per minute (bradycardia). ·1572 The major difference between dailysate for hemodialysis and peritoneal dialysis is the amount of glucose. Peritoneal dialysis dialysate is much higher in glucose. For this reason, if the dialysate is left in the peritoneal cavity too long, hyperglycemia may occur.·1573 The key to resolving UTI with most antibiotics is to keep the blood level of the antibiotic constant. It is important to tell the client to take the antibiotics round-the-clock and not skip doses so that a consistent blood level can be maintained for optimal effectiveness. ·1574 Location of the pain can help determine location of the stone. ·1575 Flank pain usually means the stone is in the kidney or upper ureter. If it radiates in the abdomen or scrotum, the stone is likely to be in the ureter or bladder. ·1576 Excruciating, spastic-type pain is called colic. ·1577 During kidney stone attacks, it is preferable to administer pain medications at regularly scheduled intervals rather than PRN to prevent spasm and optimize comfort. ·1578 Percutaneous nephrostomy: A needle/catheter is inserted through the skin into the calyx of the kidney. The stone may be dissolved by percutaneous irrigation with a liquid which will dissolve the stone, or ultrasonic sound waves (lithotripsy) can be directed through the needle/catheter to break up the stone which then can be eliminated through the urinary tract. ·1579 Bladder spasms frequently occur after TURP. Inform the client that the presence of the oversized balloon on the catheter (30 to 45 cc inflate) will cause a continuous feeling of needing to void. The client should not try to avoid around the catheter since this can precipitate bladder spasms. Medications to reduce or prevent spasms should be given. ·1580 Instillation of hypertonic or hypotonic solution into a body cavity will cause a shift in cellular fluid. Use only sterile saline for bladder irrigation after TURP since the irrigation must be isotonic to prevent fluid and electrolyte imbalance. ·1581 Inform the client prior to discharge that some bleeding is expected after TURP. Large amounts of blood or frank bright bleeding should be reported. However, it is normal for the client to pass small amounts of blood during the healing process as well as small clots. He should rest quietly and continue drinking large amounts of fluid. CARDIOVASCULAR SYSTEM ·1582 What is the relationship of the kidneys to the cardiovascular system? ·1583 The kidneys filter about a liter of blood per minute ·1584 If cardiac output is decreased, the amount of blood going through the kidneys is decreased; urinary output is decreased. Therefore, a decreased urinary output may be a sign of cardiac problems. ·1585 When the kidneys produce and excrete 0.5 ml of urine per kg of body weight or average 30 ml/hr output, the blood supply is considered to be minimally adequate to perfuse the vital organs. ·1586 Angina is caused by myocardial ischemia. Which cardiac medications would be appropriate for acute angina? ·1587 Digoxin – Not appropriate – Increases the strength and contractility of the heart muscle; the problem in angina is that the muscle is not receiving enough oxygen. Digoxin will not help. ·1588 Nitroglycerin – Appropriate – Causes dilation of the coronary arteries, allowing more oxygen to get to the heart muscle. ·1589 Atropine – Not appropriate – Increases heart rate by blocking vagal stimulation, which suppresses the heart rate. Does not address the lack of O2 to the heart muscle. ·1590 Propanolol (Inderal) – Not appropriate – for acute angina attack; however, is appropriate for long-term management of stable angina because it acts as a beta-blocker to control vasoconstriction.·1591 Blood pressure is created by the difference in the pressure of the blood as it leaves the heart and the resistance it meets flowing out to the tissues. Therefore, any factor that alters cardiac output or peripheral vascular resistance will alter blood pressure. Diet and exercise, smoking cessation, weight control, and stress management can control many factors that influence the resistance blood meets as it flows from the heart. ·1592 Remember the risk factors for hypertension: heredity, race, age, alcohol abuse, increased salt intake, obesity, and use of oral contraceptives. ·1593 The number one cause of CVA with hypertensive clients is non-compliance with medication regime. Hypertension is often symptomless, and antihypertensive medications are expensive and have side effects. Studies have shown that the more clients know about their antihypertensive medications, the more likely they are to take them – teaching is important. ·1594 Decreased blood flow results in diminished sensation in the lower extremities. Any heat source can cause severe burns before the client actually realizes the damage is being done. ·1595 A client is admitted with severe chest pain and states that he feels a terrible, tearing sensation in his chest. He is diagnosed with a dissecting aortic aneurysm. What assessment should the nurse obtain in the first few hours? ·1596 Vital signs q1 hour ·1597 Neurological vital signs ·1598 Respiratory status ·1599 Urinary output ·1600 Peripheral pulses ·1601 During aortic aneurysm repair, the large arteries are clamped for a period of time and kidney damage can result. Monitor daily BUN and creatinine levels. Normal BUN is 10 to 20 mg/dl and normal creatinine is 20:1. When this ratio increases or decreases, suspect renal problems. ·1602 A positive Homen’s sign is considered an early indication of thrombophlebitis. However, it may also indicate muscle inflammation. If a deep vein thrombosis has been confirmed, a Homan’s sign should not be elicited because of the increased risk of embolization. ·1603 Heparin prevents conversion of fibrinogen to fibrin and prothrombin to thrombin, thereby inhibiting clot formation. Since the clotting mechanism is prolonged, do not cause tissue trauma which may lead to bleeding when giving heparin subcutaneously. Do not massage area or aspirate; give in the abdomen between the pelvic bones; 2 inches from umbilicus; rotate sites. ·1604 HEPARIN: ·1605 Antagonist: Protamine Sulfate ·1606 LAB: PTT or APTT determines efficacy ·1607 Keep 1.5 to 2.5 times normal control ·1608 COUMADIN: ·1609 Antagonist: Vitamin K ·1610 LAB: PT determines efficacy ·1611 Keep 1.5 to 2.5 times normal control ·1612 INR: Desirable therapeutic level usually 2 to 3 seconds (reflects how long it takes a blood sample to clot). ·1613 A holter monitor offers continuous observation of the client’s heart rate. To make assessmentof the rhythm strips, most meaningful, teach the client to keep a record of: ·1614 Medication times and doses ·1615 Chest pain episodes – type and duration ·1616 Valsalva maneuver (straining at stool, sneezing, coughing) ·1617 Sexual activity ·1618 Exercise ·1619 Cardioversion is the delivery of synchornized electrical shock to the myocardium. ·1620 Differentiate in synchronous and asynchronous pacemakers: ·1621 Synchronous or demand pacemaker fires only when the client’s heart rate falls below a rate set on the generator. ·1622 Asynchronous or fixed pacemaker fires at a constant rate. ·1623 Restricting sodium reduces salt and water retention, thereby reducing vascular volume and preload. ·1624 DIGITALIS: ·1625 Side effects of digitalis are increased when the client is hypokalemic. ·1626 Has a negative chronotropic effect, i.e., it shows the heart rate. Hold the digitalis if the pulse rate is <60, >120, or has markedly changed rhythm. ·1627 Bradycardia, tachycardia, or dysrhythmias may be signs of digitalis toxicity: these signs include nausea, vomiting, and headache in adults. ·1628 If withheld, consult with physician. ·1629 Infective endocarditis damage to heart valves occurs with the growth of vegetative lesions on valve leaflets. These lesions pose a risk of embolization; erosion/perforation of the valve leaflets; or abscesses within adjacent myocardial tissue. Valvular stenosis or regurgitation (insufficiency), most commonly of the mitral valve, can occur depending upon the type of damage inflicted by the lesions, leading to symptoms of left – or right-sided heart failure. ·1630 Acute and Subacute Infective Endocarditis - There are 2 types of infective endocarditis: ·1631 Acute, which often affects individuals with previously normal hearts and healthy valves, and carries a high mortality rate ·1632 Subacute, which typically affects individuals with preexisting conditions, such as rheumatic heart disease, mitral valve prolapse, or immunosuppression. Intravenous drug abusers are at risk for both acute and subacute bacterial endocarditis. When this population develops Subacute Infective Endocarditis, the valves on the right side of the heart (tricuspid and pulmonic) are typically affected due to the introduction of common pathogens which colonize on the skin (S. epidermis and Candida) into the venous system. ·1633 Pericarditis – presence of a friction rub is an indication of pericarditis (inflammation of the lining of the heart). ST segment elevation and T wave inversion are also signs of pericarditis. ·1634 With mitral valve stenosis, blood is regurgitated back into the left atrium from the left ventricle. In early period, there may be no symptoms; but, as the disease progresses, the client will exhibit excessive fatigue, dyspnea on exertion, orthopnea, dry cough, hemoptysis, or pulmonary edema. There will be a rumbling apical diastolic murmur, and atrial fibrillation is common. GASTROINTESTINAL SYSTEM ·1635 A Fowler’s or semi-Fowler’s position is beneficial in reducing the amount of regurgitation aswell as preventing the encroachment of the stomach tissue upward through the opening in the diaphragm. ·1636 Stress can cause or exacerbate ulcers. Teach stress reduction methods and encourage those with a family history of ulcers to obtain medical surveillance for ulcer formation. ·1637 CLINICAL MANIFESTATIONS OF GI BLEEDING: ·1638 Pallor: conjuctival, mucous membranes, nail beds ·1639 Dark, tarry stools ·1640 Bright red or coffee-ground emesis ·1641 Abdominal mass or bruit ·1642 Decreased BP, rapid pulse, cool extremities (shock). ·1643 The GI tract usually accounts for only 100 to 200 ml fluid loss per day, although it filters up to 8 liters per day. Large fluid losses can occur if vomiting and/or diarrhea exists. ·1644 Opiate drugs tend to depress gastric motility. However, they should be given with care, and those receiving them should be closely monitored because a distended intestinal wall accompanied by decreased muscle tone may lead to intestinal perforation. ·1645 Diverticulosis is the presence of pouches in the wall of the intestine. There is usually do discomfort, and the problem goes unnoticed unless seen on radiological examination (usually prompted by some other condition). ·1646 Diverticulitis is an inflammation of the diverticula (punches), which can lead to perforation of the bowel. ·1647 A client admitted with complaints of severe lower abdominal pain, cramping, and diarrhea is diagnosed with diverticulitis. What are the nutritional needs of this client throughout recovery? ·1648 Acute phase – NPO graduating to liquids. ·1649 Recovery phase – no fiber or foods that irritate the bowel. ·1650 Maintenance phase – high-fiber diet, with bulk-forming laxatives to prevent pooling of foods in the pouches where they can become inflamed. Avoid small, poorly digested foods such as popcorn, nuts, seeds, etc. ·1651 Bowel obstructions: ·1652 Mechanical: due to disorders outside the bowel (hernia, adhesions), due to disorders within the bowel (tumors, diverticulitis), or due to blockage of the lumen in the intestine (intussusception, gall stone). ·1653 Non-mechanical: paralytic ileus, which does not involve any actual physical obstruction, but results from inability of the bowel itself to function. ·1654 Blood gas analysis will show alkalotic state if the bowel obstruction is high in the small intestine where gastric acid is secreted. If the obstruction is in the lower bowel where base solutions are secreted, the blood will be acidic. ·1655 A client admitted with complaints of constipation, thready stools and rectal bleeding over the past few months is diagnose with a rectal mass. What are the nursing priorities for this client? ·1656 NPO ·1657 NG tube (possibly an intestinal tube such as a Miller-Abbott) ·1658 IV fluids ·1659 Surgical preparations of bowel (if obstruction is complete)·1660 Teaching (preoperative, nutrition, etc.) ·1661 Diet recommended by the American Cancer Society to prevent bowel cancer: ·1662 Eat more cruciferous vegetables (from the cabbage family such as broccoli, cauliflower, Brussels sprouts, cabbage, and kale). ·1663 Increase fiber intake. ·1664 Maintain average body weight ·1665 Eat less animal fat. ·1666 AMERICAN CANCER SOCIETY RECOMMENDATIONS for early detection of Colon Cancer: ·1667 A digital rectal examination every year after 40. ·1668 A stool blood test every year after 50. ·1669 A sigmoidoscopy examination every 3 to 5 years after the age of 50, based on the advice of a physician. ·1670 Cancer of the colon is the most common cancer in the US when considering men and women together. An early sign is the rectal bleeding. Encourage patients 50 years of age or older, or those with increased risk factors, to be screened yearly with fecal occult blood testing. Routine colonoscopy at 50 is also recommended. ·1671 CLINICAL MANIFESTATIONS OF JAUNDICE ·1672 Yellow skin, sclera, and/or mucous membranes (bilirubin in skin) ·1673 Dark-colored urine (bilirubin in urine) ·1674 Chalky or clay-colored stools (absence of bilirubin in stools) ·1675 Fetor hepaticus is a distinctive breath odor of chronic liver disease. It is characterized by a fruity or musty odor which results from the damaged liver’s inability to metabolize and detoxify mercaptan which is produced by the bacterial degradation of metionine, a sulfurous amino acid. ·1676 For treatment of ascities, paracentesis and peritoneovenous shunts (LaVeen and Denver shunts) may be indicated. ·1677 Esophageal varices may rupture and cause hemorrhage. Immediate management includes insertion of an esophagogastric balloon tamponade – a Blakemore-Sengstaken or Minnesota tube. Other therapies include vasopressors, vitamin K, coagulation factors, and blood transfusions. ·1678 Ammonia is not broken down as usual in the damaged liver; therefore, the serum ammonia level rises. ·1679 PROVIDE AN ENVIRONMENT CONDUCIVE TO EATING for clients who are anorexic and/or nauseated: ·1680 Remove strong odors immediately; they can be offensive and increase nausea. ·1681 Encourage client to sit up for meals; this can decrease the propensity to vomit. ·1682 Serve small, frequent meals. ·1683 Liver tissue is destroyed by hepatitis. Rest and adequate nutrition are necessary for regeneration of liver tissue being destroyed by the disease. Since many drugs are metabolized in the liver, drug therapy must be scrutinized carefully. Caution the client that recovery takes many months, and previously taken medications should not be resumed without the healthcare provider’s directions.·1684 Acute pancreatic pain is located retroperitoneally. Any enlargement of the pancreas causes the peritoneum to stretch tightly. Therefore, sitting up or leaning forward will reduce the pain. ·1685 Following an endoscopic retrogade cholangiopancreatography (ERCP), the client may feel sick. The scope is placed in the gallbladder and the stones are crushed and left to pass on their own. These clients may be prone to pancreatitis. ·1686 Non-surgical management of the client with cholecystitis includes: ·1687 Low-fat diet ·1688 Medications for pain and clotting if required ·1689 Decompression of the stomach via NG tube ENDOCRINE SYSTEM ·1690 Thyroid storm is a life-threatening event that occurs with uncontrolled hyperthyroidism due to Grave’s disease. Symptoms include fever, tachycardia, agitation, anxiety, and hypertension. ·1691 Primary nursing interventions include maintaining an airway and adequate aeration. ·1692 Propylthiouracil (PTU) or methimazole (Tapazole) are antithyroid drugs used to treat thyroid storm. Propanolol (Inderal) may be given to decrease excessive sympathetic stimulation. ·1693 Post-operative thyroidectomy: be prepared for the possibility of laryngeal edema. Put a tracheostomy set at bedside along with oxygen and a suction machine; Ca++ gluconate easily accessible. ·1694 Normal serum calcium is 9.0 to 10.5 mEq/L. The best indicator of parathyroid problems is a decrease in the client’s calcium compared to the preoperative value. ·1695 If two or more parathyroid glands have been removed, the chance of tetany increases dramatically: ·1696 Monitor serum calcium levels (9.0 to 10.5 mg/dl is normal range) ·1697 Check for tingling of toes, fingers, and around the mouth. ·1698 Check for Chvostek’s sign (tap over the parotid gland and which for twitching of lip = positive) ·1699 Check Trousseau’s sign (carpopedal spasm after inflating BP cuff above systolic pressure = positive). ·1700 Myxedema coma can be precipitated by acute illness, withdrawal of thyroid medication, anesthesia, use of sedatives, or hypoventilation (with the potential for respiratory acidosis and carbondioxide narcosis). The airway must be kept patent, and ventilator support as indicated. ·1701 Many people take steroids for a variety of conditions. NCLEX-RN questions often focus on the need to teach clients the importance of precisely following the prescribed regimen. They should be cautioned against suddenly stopping the medications and be informed that it is necessary to taper off taking steroids. ·1702 ADDISON”S CRISIS IS A MEDICAL EMERGENCY: Brought on by sudden withdrawal of steroids or a stressful event (trauma, severe infection) ·1703 Vascular Collpase: Hypotension and tachycardia occur; administer IV fluids at rapid rate until stabilized. ·1704 Hypoglycemia: Administer IV glucose ·1705 ADMINISTER PARENTERAL HYDROCORTISONE: Essential for reversing the crisis.·1706 ALDOSTERONE REPLACEMENT: Administer fludrocortisone acetate(Florinef) PO (only available as oral preparation) with simultaneous administration of salt (sodium chloride) if client has a sodium deficit. ·1707 Teach clients to take steroids with meals to prevent gastric irritation. They should never skip doses. If they have nausea or vomiting for more than 12 to 24 hours, they should contact the physician. ·1708 Why do diabetics have trouble with wound healing? High blood glucose contributes to damage of the smallest vessels, the capillaries. This damage causes permanent capillary scarring, which inhibits the normal activity of the capillary. This phenomenon causes disruption of capillary elasticity and promotes problems such as diabetic retinopathy, poor healing or breaks in the skin, cardiovascular abnormalities, etc. ·1709 Glycosylated Hgb (Hgb A1C) ·1710 Indicates glucose control over previous 120 days (life of RBC) ·1711 Valuable measurement of diabetes control. ·1712 The body’s response to illness/stress is to produce glucose. Therefore, any illness results in hyperglycemia. ·1713 If in doubt whether the client is hyperglycemic or hypoglycemic, treat for hypoglycemia. ·1714 SELF-MONITORING BLOOD GLUCOSE (SMBG) ·1715 Provides tight glucose control thereby decreasing the potential for long-term complications ·1716 Technique is specific to each meter if meter is used. ·1717 Monitor before meals, at bedtime, and any time symptoms occur. ·1718 Record results and report to healthcare provider at time of visit. MUSCULOSKELETAL SYSTEM ·1719 A client comes to the clinic complaining of morning stiffness, weight loss, and swelling of both hands and wrists. Rheumatoid arthritis is suspected. Which methods of assessment might the nurse use and which methods would the nurse not use? ·1720 Use inspection, palpation, and strength testing. ·1721 Do not use range of motion (this activity promotes pain because ROM is limited). ·1722 In the joint, the normal cartilage becomes soft, fissures and pitting occur, and the cartilage thins. Spurs form and inflammation sets in. The result is deformity marked by immobility, pain, and muscle spasm. The prescribed treatment regimen is corticosteroids for the inflammation; splinting, immobilization, and rest for joint deformity; and NSAIDS for the pain. ·1723 Synovial tissues line the bone of the joints. Inflammation of this lining causes destruction of tissue and bone. Early detection of rheumatoid arthritis can decrease the amount of bone and joint destruction. Often the disease will go into remission. Decreasing the amount of bone and joint destruction will reduce the amount of disability. ·1724 What activity recommendations should the nurse provide a client with rheumatoid arthritis? ·1725 Do not exercise painful, swollen joints. ·1726 Do not exercise any joint to the point of pain.·1727 Perform exercises slowly and smoothly; avoid jerky movements. ·1728 NCLEX-RN questions often focus on the fact that avoiding sunlight is key in management of lupus erythematosus – this is what differentiates it from other connective tissue diseases. ·1729 Degenerative joint disease (DJD) and osteoarthritis are often described as the same disease, and indeed they both result in hypertrophic changes in the joints. However, they differ in that osteoarthritis is an inflammatory disease and DJD is characterized by non-inflammatory degeneration of the joints. ·1730 Postmenopausal, thin, Caucasian women are at highest risk for development of osteoporosis. Encourage exercise, a diet high in calcium, and supplemental calcium. While TUMS is an excellent source of calcium, it is also high in sodium and hypertensive or edematous individuals should seek another source for supplemental calcium. ·1731 The main cause of fractures in the elderly, especially women, is osteoporosis. The main fracture sites seem to be hip, vertebral bodies, and Colles’ fracture of forearm. ·1732 NCLEX-RN questions focus on safety precautions. Improper use of assistive devices can be very risky. When using a non-wheeled walker, the client should lift and move the walker forward, then take a step into it. The client should avoid scooting the walker or shuffling forward into it which takes more energy and is less stable than a single movement. ·1733 What type of fracture is more difficult to heal, an extra capsular fracture (below the neck of the femur) or an intracapsular fracture (in the neck of the femur)? ·1734 The blood supply enters the femur below the neck of the femur. Therefore, an intra-capsular fracture is much more harder to heal and has a greater likelihood of necrosis since it is cut off from the blood supply. ·1735 The risk of a fat embolism, a syndrome in which fat globules migrate into the bloodstream and combine with platelets to form emboli, is greatest in the first 36 hours after a fracture. It is more common in clients with multiple fractures, fractures of long bones, and fractures of the pelvis. The initial symptom of a fat embolism is confusion due to hypoxemia (check blood gases for PO2). Assess for respiratory distress, restlessness, irritability, fever, and petechiae. If an embolus is suspected, notify physician STAT, draw blood gases, administer oxygen, and assist with endotracheal intubation. ·1736 In clients with hip fractures, thromboembolism is the most common complication. Prevention includes passive range of motion exercises, elastic stocking use, elevation of the foot of the bed 25 degrees to increase venous return, and low-dose hepatin therapy. ·1737 Clients with fractures, casts, or edema to the extremities need frequent neurovascular assessment distal to the injury. Skin color, temperature, sensation, capillary refill, mobility, pain and pulses should be assessed. ·1738 Assess the “5 Ps” of neurovascular functioning: pain, paresthesia, pulse, pallor and paralysis. ·1739 Orthopedic wounds have a tendency to ooze more than other wounds. A suction drainage device usually accompanies the client to the postoperative floor. Check drainage often. ·1740 A big problem after joint replacement is infection. ·1741 Fractures of bone predispose the client to anemia, especially if long bones are involved. Check hemtocrit every 3 to 4 days to monitor erythropoiesis. ·1742 Instruct the client not to lift the leg upward from a lying position or to elevate the knee when sitting. This upward motion can pop the prosthesis out of the socket.·1743 Immobile clients are prone to complications: skin integrity problems, formation of urinary calculi (may limit milk intake), and venous thrombosis (may be on prophylactic anticoagulants). ·1744 The residual limb should be elevated on one pillow. If the residual limb (stump) is elevated too high, the elevation can cause contracture. NEUROSENSORY SYSTEM ·1745 Glaucoma is often painless and symptom-free. It is usually picked up as part of a regular eye exam. ·1746 Eye drops are used to cause pupil constriction since movement of the muscles to constrict the pupil also allows aqueous humor to flow out, thereby decreasing the pressure in the eye. Pilocarpine is often used. Caution client that vision may be blurred 1 to 2 hours after administration of pilocarpine and adaptation to dark environments is difficult because of pupillary constriction (desired effect of the drug). ·1747 There is an increased incidence of glaucoma in the elderly population. Older clients are prone to problems associated with constipation. Therefore, the nurse should assess these clients for constipation and postoperative complications associated with constipation, and implement a plan of care directed at prevention, and, if necessary, treatment for constipation. ·1748 The lens of the eye is responsible for projecting light, which enters onto the retina so that images can be discerned. Without the lens, which becomes opaque with cataracts, light cannot be filtered and vision is blurred. ·1749 When the cataract is removed, the lens is gone, making prevention of falls important. If the lens is replaced with an implant, vision is better than if a contact lens is used (some visual distortion) or if glasses are used (greater visual distortion – everything has a curved shape). ·1750 The ear consists of three parts: the external ear, middle ear, and the inner ear. Inner ear disorders, or disorders of the sensory fibers going to the CNS., often are neurogenic in nature and may not be helped with a hearing aid. External and middle ear problems (conductive) may result from infection, trauma or wax buildup. These types of disorders are treated more successfully with hearing aids. ·1751 NCLEX-RN questions often focus on communicating with older adults who are hearing impaired. ·1752 Speak in a low-pitched voice, slowly, and distinctly. ·1753 Stand in front of the person with the light source behind the client. ·1754 Use visual aids if available. NEUROLOGICAL SYSTEM ·1755 Use of the Glasgow Coma Scale eliminates ambiguous terms to describe neurologic status such as lethargic, stuporous, or obtunded. ·1756 Almost every diagnosis in the NANDA format is applicable, as severely neurologically impaired persons require total care. ·1757 Clients with an altered state of consciousness are fed by enteral routes since the likelihood of aspiration with oral feedings is great. Residual feeding is the amount of previous feeding still in the stomach. The presence of 100 ml residual in adults usually indicates poor gastric emptying and the feeding should be held.·1758 Paralytic ileus is common in comatose clients. Gastric tube aids in gastric decompression. ·1759 Any client on bedrest/immobilized must have range of motion exercises often and very frequent position changes. Do not leave the client in any one position for longer than 2 hours. Any position that decreases venous return is dangerous, i.e., sitting with dependent extremities for long periods. ·1760 If temperature elevates, take quick measures to decrease it since fever increases cerebral metabolism and can increase cerebral edema. ·1761 Safety measures for immobilized clients: ·1762 Prevent skin breakdown with frequent turning. ·1763 Maintain adequate nutrition. ·1764 Prevent aspiration with slow, small feedings or NG feedings. ·1765 Monitor neurological signs to detect the first signs that intracranial pressure may be increasing. ·1766 Provide range of motion exercises to prevent deformities. ·1767 Prevent respiratory complications – frequent turning and positioning for optimal drainage. ·1768 Restlessness may indicate a return to consciousness but can also indicate anoxia, distended bladder, covert bleeding, or increasing cerebral anoxia. Do not over-sedate, and report any symptoms of restlessness. ·1769 The forces of impact influence the type of head injury. They include acceleration injury, which is caused by the head in motion, and deceleration injury, which occurs when the head stops suddenly. Helmets are a GREAT preventive measure for motorcyclists and bicyclists. ·1770 Even subtle behavior changes, such as restlessness, irritability, or confusion, may indicate increased ICP. ·1771 CSF leakage carries the risk of meningitis and indicates a deteriorating condition. Because of CSF leakage, the usual signs of increased ICP may not occur. ·1772 Try not to use restraints; they only increase restlessness. AVOID narcotics since they mask level of responsiveness. ·1773 Physical assessment should concentrate on respiratory status, especially in clients with injury at C-3 to C-5, as cervical plexus innervates diaphragm. ·1774 It is imperative to reverse spinal shock as quickly as possible. Permanent paralysis can occur if a spinal cord is compressed for 12 to 24 hours. ·1775 A common cause of death after spinal cord injury is urinary tract infection. Bacteria grow best in alkaline media, so keeping urine diluted ad acidic is prophylactic against infection. Also, keeping the bladder emptied assists in avoiding bacterial growth in urine, which is stagnated in the bladder. ·1776 Benign tumors continue to grow and take up space in the confined area of the cranium causing neural and vascular compromise for the brain, increased intracranial pressure, and necrosis of brain tissue – even benign tumors must be treated as they may have malignant effects. ·1777 Craniotomy post-operative medications: ·1778 Corticosteroids to reduce swelling·1779 Agents and osmotic diuretics to reduce secretions (atropine, robinul) ·1780 Agents to reduce seizures (phenytoin) ·1781 Prophylactic antibiotics ·1782 Symptoms involving motor function usually begin in the upper extremities with weakness progressing to spastic paralysis. Bowel and bladder dysfunction occurs in 90% of the cases. MS is more common in women. Progression is not “orderly.” ·1783 Drug therapy for MS clients: ACTH, cortisone, Cytoxan, and other immunosuppressive drugs. Nursing implications for administration of these drugs should focus on prevention of infection. ·1784 In clients with Myasthenia Gravis, be alert for changes in respiratory status – the most severe involvement may result in respiratory failure. ·1785 Bedrest often relieves symptoms. Bladder and respiratory infections are often a recurring problem. Need for health promotion teaching. ·1786 Myasthenic crisis is associated with a positive edrophonium (Tensilon) test, while a cholinergic crisis is associated with a negative test. ·1787 NCLEX-RN questions often focus on the features of Parkinson’s disease – tremors (a coarse tremor of fingers and thumb on one hand which disappears during sleep and purposeful activity – also called “pill rolling”), rigidity, hypertonicity, and stooped posture. Focus: SAFETY! ·1788 An important aspect of Parkinson’s treatment is drug therapy. Since the pathophysiology involves an imbalance between acetylcholines and dopamine, symptoms can be controlled by administering dopamine precursor (Levodopa). ·1789 CNS involvement related to cause of CVA: ·1790 Hemorrhagic: caused by a slow or fast hemorrhage into the brain tissue – often related to hypertension. ·1791 Embolytic: caused by a clot, which has broken away from some vessel and has lodged in one of the arteries of the brain, blocking the blood supply. It is often related to atherosclerosis (may happen again). ·1792 Atrial flutter/fibrillation has a high incidence of thrombus formation following arrythmias due to turbulence of blood flow through all valves/heart chambers. ·1793 A woman who had a stroke two days ago has left-sided paralysis. She has begun to regain some movement in her left side. What can the nurse tell the family about the client’s recovery period? ·1794 The quicker movement is recovered, the better the prognosis is for more or full recovery. She will need patience and understanding from her family as she tries to cope with the stroke. Mood swings can be expected during the recovery period, and bouts of depression and tearfulness are likely. ·1795 Words that describe losses from CVA: ·1796 Apraxia: inability to perform purposeful movements in the absence of motor problems. ·1797 Dysarthria: difficulty articulating ·1798 Dysphasia: impairment of speech and verbal comprehension ·1799 Aphasia: loss of the ability to speak ·1800 Agraphia: loss of the ability to write ·1801 Alexia: loss of the ability to read·1802 Dysphagia: dysfunctional swallowing ·1803 Steroids are administered after a stroke to decrease cerebral edema and retard permanent disability. H2 inhibitors are administered to prevent peptic ulcers. HEMATOLOGY/ONCOLOGY ·1804 Physical symptoms occur as a compensatory mechanism when the body is trying to make up for a deficit somewhere in the system. For instance, cardiac output increases when hemoglobin levels drop below 7g/dl. ·1805 ONLY use normal saline to flush IV tubing or to run with blood. NEVER add medications to blood products. TWO registered nurses should simultaneously check the physician’s prescription, client’s identity, and blood bag label. ·1806 A 24-year old is admitted with large areas of ecchymosis on both upper and lower extremities. She is diagnosed with acute myeologenous leukemia. What are the expected laboratory findings for this client and what is the expected treatment? ·1807 Lab: Decreased Hgb, decreased Hct, decreased platelet count, altered WBC (usually quite high). ·1808 Treatment: Prevention of infection; prevention and/or control of bleeding; high protein, high calorie diet; assistance with ADL; drug therapy. ·1809 Infection in the immunosuppressed person may not be manifested with an elevated temperature. It is imperative, therefore, that the nurse performs a total and thorough assessment of the client frequently. ·1810 Most oncologic drugs cause immunosuppression. Prevention of secondary infections is vital! Advise client to stay away from persons with known infections such as colds. In the hospital, maintain an environment as sterile and as clean as possible. These persons should not eat raw vegetables or fruits – only cooked to destroy any bacteria. ·1811 Hodgkin’s is one of the most curable of all adult malignancies. Emotional support is vital. Career development is often interrupted for treatment. Chemotherapy renders many male clients sterile. May bank sperm prior to treatment, if desired. REPRODUCTIVE SYSTEM ·1812 Menorrhagia (profuse or prolonged menstrual bleeding) is the most important factor relating to benign uterine tumors. Assess for signs of anemia. ·1813 What is the anatomical significance of a prolapsed uterus? When the uterus is displaced, it impinges on other structures in the lower abdomen. The bladder, rectum, and small intestine can protrude through the vaginal wall. ·1814 Laser therapy or cryosurgery is used to treat cervical cancer when the lesion is small and localized. Invasive cancer is treated with radiation, conization, hysterectomy, or pelvic exenteration (a drastic surgical procedure where the uterus, ovaries, fallopian tubes, vagina, rectum, and bladder are removed in an attempt to stop metastasis). Chemotherapy is not useful with this type of cancer. ·1815 Pap smears should begin within 3 years of having intercourse or no later than age 21, whichever comes first. Should be done annually until age 30 and then may be done every 2 to 3 years if a woman has 3 consecutive normal results. After age 70 may stop if woman has 3 consecutive normal and no abnormal pap smears in last 10 years. Women at high risk shouldhave annual screenings. ·1816 Ovarian cancer is the leading cause of death from gynecologic cancers in the US. Growth is insidious, so it is not recognized until it is at an advanced stage. ·1817 The major emphasis in nursing management of cancers of the reproductive tract is early detection. ·1818 The importance of teaching female clients how to do self-breast examination cannot be overemphasized. Early detection is related to positive outcomes. ·1819 The presence or absence of hormone receptors is paramount in selecting clients for adjuvant therapy. ·1820 Men whose testes have not descended into the scrotum or whose testes descended after age 6 are at high risk for developing testicular cancer. The most common symptom is the appearance of a small, hard lump about the size of a pea on the front or side of the testicle. Manual testicular examination should be done after a shower by gently palpating the testes and cord to look for a small lump. Swelling may also be a sign of testicular cancer. ·1821 STDs in infants and children usually indicate sexual abuse and should be reported. The nurse is legally responsible to report cases of child abuse. Chlamydia is the most reported communicable disease in the United States. ·1822 Pelvic inflammatory disease (PID) involves one more of the pelvic structures. The infection can cause adhesions and eventually result in sterility. Manage the pain associated with PID with analgesics and warm sitz baths. Bedrest in a semi-Fowler’s position may increase comfort and promote drainage. Antibiotic treatment is necessary to reduce inflammation and pain. ·1823 A client comes to the clinic with a chancre on his penis. What is the usualy treatment? ·1824 IM dose of penicillin (such as Benzathine penicillin G 2.4 million units). ·1825 Obtain sexual history, including the names of his sex partners, so that they can receive treatment. BURNS ·1826 Massive volumes of IV fluids are given. It is not uncommon to give over 1,000 cc/hr during various phases of burn care. Hemodynamic monitoring must be closely observed to be sure the client is supported with fluids but is not overloaded. ·1827 Infection is a life-threatening risk for those with burns. Dressing changes are VERY PAINFUL! Medicate client prior to procedure. ·1828 Pre-existing conditions that might influence burn recovery are age, chronic illness, diabetes, cardiac problems, etc.), physical disabilities, disease, medications used routinely, and drug and/or alcohol abuse. PEDIATRIC NURSING GROWTH AND DEVELOPMENT: ·1829 When does birth length double? = by 4 years ·1830 When does the child sit unsupported? = 8 months·1831 When does a child achieve 50% of adult height? = 2 years ·1832 When does a child throw a ball overhand? = 18 months ·1833 When does a child speak 2-3 word sentences? = 2 years ·1834 When does a child use scissors? = 4 years ·1835 When does a child tie his/her shoes? = 5 years ·1836 Be aware that a girl’s growth spurt during adolescence begins earlier than boys (as early as 10 years old). ·1837 Temper tantrums are common in the toddler, i.e., considered “normal,” or average behavior. ·1838 Be aware that adolescence is a time when the child forms his/her identity and that rebellion against family values is common for this age group. ·1839 Normal growth and development knowledge is used to evaluate interventions and therapy. For example, “What behavior would indicate that thyroid hormone therapy for a 4-month-old is effective?” You must know what milestones are accomplished by a 4-month-old. One correct answer would be “has steady head control” which is an expected milestone for a 4-month-old and indicates that replacement therapy is adequate for growth. ·1840 Use facts and principles related to growth and development in planning teaching interventions. For example: “What task could a 5-year-old diabetic boy be expected to accomplish by himself?” One correct answer would be to pick the injection sites. This is possible for a preschooler to do and gives the child some sense of control. ·1841 School-age children are in Erikson’s stage of industry, meaning they like to do and accomplish things. Peers are also becoming important for this age child. ·1842 Age groups concepts of bodily injury: ·1843 Infants: After 6 months, their cognitive development allows them to remember pain. ·1844 Toddlers: Fear intrusive procedures. ·1845 Preschoolers: Fear body mutilation. ·1846 School Age: Fear loss of control of their body. ·1847 Adolescent: Major concern is change in body image. CHILD HEALTH PROMOTION ·1848 Subcutaneous injection, rather than intradermal, invalidates the Mantoux test. ·1849 The common cold is not a contraindication for immunization. ·1850 Following immunization, what teaching should the nurse provide to the parents? ·1851 Irritability, fever (<102F), redness and soreness at injection site for 2 to 3 days are normal side effects of DPT and IPV administration. ·1852 Call health care provider if seizures, high fever, or high-pitched crying occur. ·1853 A warm washcloth on the thing injection site and “bicycling” the legs with each diaper change will decrease soreness. ·1854 Acetaminophen (Tylenol) is administered orally 4 to 6 hours (10 to 15 mg/Kg).·1855 Children with German measles pose a serious threat to their unborn siblings. The nurse should counsel all expectant mothers, especially those with young children, to be aware of the serious consequences of exposure to German measles during pregnancy. ·1856 Common childhood problems are encountered by nurses caring for children in the community or hospital settings. The child’s age directly influences the severity and management of these problems. ·1857 Teach proper cooking and storage to preserve potency, i.e., cook vegetables in small amount of liquid. Store milk in opaque container. ·1858 Add potassium to IV fluids ONLY with adequate urine output. ·1859 Urinary output for infants and children should be 1 to 2 ml/kg/hr. ·1860 Use of syrup of ipecac is no longer recommended by the American Academy of Pediatrics. Teach parents that it is NOT recommended to induce vomiting in any way as it may cause more damage. RESPIRATORY DISORDERS ·1861 Child needs 150% of the usual calorie intake for normal growth and development. ·1862 Do not examine the throat of a child with epiglottis due to the risk of completely obstructing the airway, i.e., do not put a tongue blade or any object in the throat. ·1863 In planning and providing nursing care, a patent airway is always a priority of care, regardless of age! ·1864 Respiratory disorders are the primary reason most children and their families seek medical care. Therefore, these disorders are frequently tested on the NCLEX-RN. Knowing the normal parameters for respiratory rates and the key signs of respiratory distress in children is essential! ·1865 The nurse should be sure a PT and PTT have been determined prior to a tonsillectomy. More importantly, the nurse should ask if there has been a history of bleeding, prolonged/excessive, or if there is a history of any bleeding disorders in the family. ·1866 When calculating a pediatric dosage, the nurse must often change the child’s weight from pounds to kilograms. ·1867 HINT: weight expressed in kilograms should always be a smaller number than weight expressed in pounds. CARDIOVASCULAR DISORDERS ·1868 Polycythemia is common in children with cyanotic defects. ·1869 The heart rate of a child will increase with crying or fever. ·1870 Infants may require tube feeding to conserve energy. ·1871 Basic difference between cyanotic and acyanotic defects: ·1872 Acyanotic: Has abnormal circulation, however, all blood entering the systemic ciruclation is oxygenated.·1873 Cyanotic: Has abnormal circulation with unoxygenated blood entering systemic circulation. ·1874 Congestive heart failure is more often associated with acyanotic defects. ·1875 CHF is a common complication of congenital heart disease. It reflects the increased workload of the heart resulting from shunts or obstructions. The two objectives in treating CHF are to reduce the workload of the heart and increase cardiac output. ·1876 When frequent weighings are required, weigh client on the same scale at same time of day so that accurate comparisons can be made. NEUROMUSCULAR DISORDERS ·1877 The nursing goal in caring for children with Down syndrome is to help the child reach his/her OPTIMAL level of functioning. ·1878 Feed infant or child with cerebral palsy using nursing interventions aimed at preventing aspiration. Position child upright and support the lower jaw. ·1879 The signs of ICP are the opposite of those of shock. ·1880 Shock: Increased pulse, Decreased blood pressure. ·1881 Increased ICP: Decreased pulse, Increased blood pressure. ·1882 Baseline data on the child’s USUAL behavior and level of development is essential so changes associated with increased ICP can be detected EARLY. ·1883 Do not pump shunt unless specifically prescribed. The shunt is made up of delicate valves, and pumping changes pressures within the ventricles. ·1884 Medication noncompliance is the most common cause of increased seizure activity. ·1885 Do NOT use tongue blade, padded or not, during a seizure. It can cause traumatic damage to mouth/oral cavity. ·1886 Monitor hydration status and IV therapy carefully. With meningitis, there may be inappropriate ADH secretions causing fluid retention (cerebral edema) and dilutional hyponatremia. ·1887 Headache upon awakening is the most presenting symptom of brain tumors. ·1888 Most postoperative clients with infratentorial tumors are prescribed to lie flat and turn to either side. A large tumor may require that the child NOT be turned to the operative side. ·1889 Suctioning, coughing, straining, and/or causes increased ICP. RENAL DISORDERS ·1890 Decreased urinary output is FIRST sign of renal failure. ·1891 Surgical correction for hypospadias is usually done before preschool years due to achieving sexual identity, castration anxiety and toilet training.GASTROINTESTINAL DISORDERS ·1892 Typical parent/family reaction to a child with an obvious malformation such as cleft lip/palate are quilt, disappointment, grief, sense of loss, and anger. ·1893 Children with cleft lip/palate and those with pyloric stenosis both have a nursing diagnosis “alteration in nutrition; less than body requirements.” ·1894 Cleft lip/palate is related to decreased ability to suck. ·1895 Pyloric stenosis is related to frequent vomiting. ·1896 Nutritional needs and fluid and electrolyte balance are key problems for children with GI disorders. The younger the child, the more vulnerable they are to fluid and electrolyte imbalances and greater is the need for caloric intake required for growth. ·1897 Take axillary temperature on children with congenital megacolon. HEMATOLOGICAL DISORDERS ·1898 Remember the Hgb norms: ·1899 Newborn: 14 to 24 g/dl ·1900 Infant: 10 to 15 g/dl ·1901 Child: 11 to 16 g/dl ·1902 Teach family about administration of oral iron: ·1903 Give on empty stomach (as tolerated for better absorption) ·1904 Give with citrus juices (vitamin C) for increased absorption ·1905 Use dropper or straw to avoid discoloring teeth ·1906 Stools will become tarry ·1907 Iron can be fatal in severe overdose; keep away from children. Do not give with dairy products. ·1908 Inherited bleeding disorders (hemophilia and sickle cell anemia) are often used to test knowledge of genetic transmission patterns. Remember: ·1909 Autosomal recessive: Both parents must be heterozygous, or carriers of the recessive trait, for the disease to be expressed in their offspring. With each pregnancy, there is a 1:4 chance of the infant having the disease. However, all children of such patterns CAN get the disease – NOT 25% of them. This is the transmission for sickle cell anemia, cystic fibrosis, and phenylketonuria (PKU). ·1910 X-linked recessive trait: The trait is carried on the X chromosome, therefore, usually affects male offspring, e.g., hemophilia. With each pregnancy of a woman who is a carrier there is a 25% chance of having a child with hemophilia. If the child is male, he has a 50% chance of having hemophilia. If the child is female, she has a 50% chance of being a carrier. ·1911 Hydration is very important in treatment of sickle cell disease because it promotes hemodilution and circulation of red cells through the blood vessels. ·1912 Important terms: ·1913 Heterozygous gene (HgbAS) sickle cell trait ·1914 Homozygous gene (HbSS) sickle cell disease ·1915 Abnormal hemoglobin (HGBS) disease and trait ·1916 Supplemental iron is not given to clients with sickle cell anemia. The anemia is not caused by iron deficiency. Folic acid is given only to stimulate RBC synthesis.·1917 Have epinephrine and oxygen readily available to treat anaphylaxis when administering lasparaginase. ·1918 Prednisone is frequently used in combination with antineoplastic drugs to reduce the mitosis of lymphocytes. Allopurinol, a xanthine-oxidase inhibitor, is also administered to prevent renal damage from uric acid build up during cellular lysis. METABOLIC AND ENDOCRINE DISORDERS ·1919 An infant with hypothyroidism is often described as a “good, quiet baby” by the parents. ·1920 Early detection of hypothyroidism and phenylhetonuria is essential in preventing mental retardation in infants. Knowledge of normal growth and development is important, since a lack of attaintment can be used to detect the existence of these metabolic/endocrine disorders and attainment can be used for evaluating the treatment’s effect. ·1921 Nutrasweet (aspartame) contains phenylalanine and should not therefore, be given to a child with phenylketonuria. ·1922 Diabetes mellitus (DM) in children was typically diagnosed as insulin dependent diabetes (Type I) until recently. A marked increase in Type II DM has occurred recently in the US, particularly among Native-American, African-American, and Hispanic children and adolescents. Adolescence frequently causes difficulty with management since growth is rapid and the need to be like peers makes compliance difficult. Remember to consider the child’s age, cognitive level of development, and psychosocial development when answering NCLEX-RN questions. ·1923 When child is in ketoacidosis, administer regular insulin IV as prescribed in normal saline. ·1924 There has been an increase in the number of children diagnosed with Type II diabetes. The increasing rate of obesity in children is thought to be a contributing factor. Other contributing factors include lack of physical activity and a family history of Type II diabetes. SKELETAL DISORDERS ·1925 Fractures in older children are common as they fall during play and are involved in motor vehicle accidents. ·1926 Spiral fractures (caused by twisting) and fractures in infants may be related to child abuse. ·1927 Fractures involving the epiphyseal plate (growth plate) can have serious consequences in terms of growth of the affected limb. ·1928 Skin traction for fracture reduction should not be removed unless prescribed by healthcare provider. ·1929 Pin sites can be sources of infection. Monitor signs of infection. Cleanse and dress pin sites as prescribed. ·1930 Skeletal disorders affect the infant’s or child’s physical mobility, and typical NCLEX-RN questions focus on appropriate toys or activities for the child who is on bedrest and/or immobilized.·1931 Children do not like injections and will deny pain to avoid “shots.” ·1932 A brace does not correct the curve of a child with scoliosis, it only stops or slows the progression. ·1933 Corticosteroids are used short term in low doses during exacerbations. Long-term use is avoided due to side effects and their adverse effect on growth. MATERNITY NURSING ANATOMY & PHYSIOLOGY OF REPRODUCTION ·1934 The menstrual phase varies in length for most women. ·1935 From ovulation to the beginning of the next menstrual cycle is usually exactly 14 days. In other words, ovulation occurs 14 days before the next menstrual period. ·1936 Sperm lives approximately 3 days and eggs live about 24 hours. A couple must avoid unprotected intercourse for several days before the anticipated ovulation and for 3 days after ovulation in order to prevent pregnancy. ·1937 Because some women experience implantation bleeding or spotting, they do not know they are pregnant. ·1938 Look for signs of maternal-fetal bonding during pregnancy. For example: talking to fetus in utero, massaging abdomen, nicknaming fetus are all healthy psychosocial activities. ·1939 For many women, BATTERING (emotional or physical abuse) begins during pregnancy. Women should be assessed for abuse in private, away from the male partner, by a nurse who knows local resources and how to determine the safety of the client. ·1940 Practice determining gravidity and parity: A woman who is 6 weeks pregnant has the following maternal history: ·1941 Has a 2 yr. old healthy daughter. ·1942 Had a miscarriage at 10 weeks, 3 years ago. ·1943 Had an elective abortion at 6 weeks, 5 years ago. With this pregnancy, she is a gravida 4, para 1 (only 1 delivery after 20 weeks gestation). ·1944 Practice calculating EDB (estimated date of birth). If the first day of a women’s last normal menstrual period was October 17, what is her EDB using Nagele’s rule? July 24. Count back 3 months and add 7 days (always give February 28 days). ·1945 At approximately 28 to 32 weeks gestation, the maximum plasma volume increase of 25 to 40% occurs, resulting in normal hemodilution of pregnancy and Hct values of 32 to 42%. High Hct values may look “good,” but in reality represent pregnancy-induced hypertension and a depleted vascular space. ·1946 Hgb/Hct data can be used to evaluate nutritional status. Example: a 22-year old primigravida at 12 weeks gestation has a high Hgb of 9.6 g/dl and a Hct of 31%. She has gained 3 pounds during the first trimester. A weight gain of3.5 to 5 pounds during the first trimester is recommended and this client is anemic. Supplemental iron and a diet higher in iron are needed. ·1947 Foods high in iron: fish and red meats; cereal and yellow vegetables; green leafy vegetablesand citrus fruits; egg yolks and dried fruits. ·1948 As pregnancy advances, the uterus presses on abdominal vessels (vena cava and aorta). Teach the woman that a side-lying position increases perfusion to uterus, placenta, and fetus. Recent research indicates that the knee-chest position is best for increasing perfusion and that the side-lying position (either left or right side-lying) is the second most desirable position to increase perfusion. Prior to this research, the left side-lying position was usually encouraged. ·1949 Fetal well-being is determined by assessing fundal height, fetal heart tones/rate, fetal movement and uterine activity (contractions). Changes in fetal heart rate are the first and most important indicator of compromised blood flow to the fetus, and these changes require action! Remember, the normal FHR is 110 to 160 bpm. ·1950 Danger signs during pregnancy. Teach clients to immediately report any of the following danger signs. Early intervention can optimize maternal and fetal outcome. ·1951 Possible indications of preeclampsia/eclampsia: ·1952 Visual disturbances ·1953 Swelling of face, fingers or sacrum ·1954 Severe, continuous headache ·1955 Persistent vomiting ·1956 Signs of infection: ·1957 Chills ·1958 Dysuria ·1959 Temperature over 100.4 F ·1960 Pain in abdomen ·1961 Fluid discharge from vagina (anything other than normal leukorrhea) ·1962 Change in fetal movement and/or increased FHR ·1963 Most providers prescribe prenatal vitamins to ensure that the client receives an adequate intake of vitamins. However, only the healthcare provider can prescribe prenatal vitamins. It is the nurse’s responsibility to teach about proper diet and taking prescribed vitamins, if prescribed by the healthcare provider. ·1964 It is recommended that pregnant women drink one quart of milk/day. This will ensure that the daily calcium needs are met an help to alleviate the occurrence of leg cramps. FETAL/MATERNAL ASSESSMENT TECHNIQUES ·1965 In some states, the screening for neural tube defects through either maternal serum AFP levels or amniotic fluid AFP levels is mandated by state law. This screening test is highly associated with both false positives and false negatives. ·1966 When an amniocentesis is done in early pregnancy, the bladder must be full to help support the uterus and to help push the uterus up in the abdomen for easy access. When an amniocentesis is done in late pregnancy, the bladder must be empty to avoid puncturing the bladder. ·1967 Early decelerations, caused by head compression and fetal descent, usually occur between 4 and 7 cm and in the 2nd stage. Check for labor progress if early decelerations are noted. ·1968 If cord prolapse is detected, the examiner should position the mother to relieve pressure onthe cord (i.e., knee-chest position) or push the presenting part off the cord until IMMEDIATE Cesarean delivery can be accomplished. ·1969 Late decelerations indicate uteroplacental insufficiency and are associated with conditions such as postmaturity, preeclampsia, diabetes mellitus, cardiac disease, and abruptio placentae. ·1970 When deceleration patterns (late or variable) are associated with decreased or absent variability and tachycardia, the situation is OMINOUS (potentially disastrous) and requires immediate intervention and fetal assessment. ·1971 A decrease in uteroplacental perfusion results in late decelerations; cord compression results in a pattern of variable decelerations. Nursing interventions should include changing maternal position, discontinuing Pitocin infusion, administering oxygen and notifying the healthcare provider. ·1972 The danger of nipple stimulation lies in controlling the “dose” of oxytocin stimulated from the posterior pituitary. The chance of hyper-stimulation or tetany (contractions over 90 seconds or contractions with less than 30 seconds in between) is increased. ·1973 Percutaneous umbilical blood sampling (PUBS) can be done during pregnancy under ultrasound for prenatal diagnosis and therapy. Hemoglobinopathies, clotting disorders, sepsis, and some genetic testing can be done using this method. ·1974 The most important determinant of fetal maturity for extra-uterine survival is the L/S ratio (2:1 or higher). INTRAPARTUM NURSING CARE ·1975 Be able to differentiate true labor from false labor. ·1976 True labor: ·1977 Pain in lower back that radiates to abdomen ·1978 Accompanied by regular, rhythmic contractions ·1979 Contractions that intensify with ambulation ·1980 Progressive cervical dilation and effacement ·1981 False labor: ·1982 Discomfort is localized in abdomen ·1983 No lower back pain ·1984 Contractions decrease in intensity and/or frequency with ambulation ·1985 Know normal findings for clients in labor: ·1986 Normal FHR in labor: 110 to 160 bpm ·1987 Normal maternal BP: <140/90 ·1988 Normal maternal pulse: <100 bpm ·1989 Normal maternal temperature: <100.4 F ·1990 Slight elevation is often due to dehydration and the work of labor. Anything higher indicates infection and must be reported immediately. ·1991 Admission procedures: ·1992 vulvar/perineal shave (may not be done)·1993 enema: may be refused by woman due to pre-labor diarrhea or recent, large bowel movement. An enema should not be administered to a client in active labor. If head is floating, watch for cord prolapse. ·1994 Meconium-stained fluid is yellow-green and may indicate fetal stress. ·1995 Breathing techniques such as deep chest, accelerated, and cued are not prescribed by the stage and phase of labor, but by the discomfort level of the laboring woman. If coping is decreasing, switch to a new technique. ·1996 Hyperventilation results in respiratory alkalosis due to blowing off too much CO2. Symptoms include: ·1997 Dizziness ·1998 Tingling of fingers ·1999 Stiff mouth ·2000 Have woman breathe into her cupped hands or a paper bag in order to rebreathe CO2. ·2001 Determine cervical dilation before allowing client to push. Cervix should be completely dilated (10 cm) before the client begins pushing. If pushing starts too early, the cervix can become edematous and never fully dilate. ·2002 Give the oxytocin after the placenta is delivered because the drug will cause the uterus to contract. If the oxytocic drug is administered before the placenta is delivered, it may result in a retained placenta, which predisposes the client to hemorrhage and infection. ·2003 Application of perineal pads after delivery: ·2004 Place two on perineum ·2005 Do NOT touch inside of pad ·2006 DO apply from front to back, being careful not to drag pad across the anus. ·2007 Methergine is NOT given to clients with hypertension due to its vasoconstrictive action. Pitocin is given with caution to those with hypertension. ·2008 FULL BLADDER is one of the most common reasons for uterine atony and/or hemorrhage in the first 24 hours after delivery. If the nurse finds the fundus soft, boggy, and displaced above and to the right of the umbilicus, what action should be taken first? First, perform fundal massage; then have the client empty her bladder. Recheck fundus q15 minutes X 4 (1 hour); q30 minutes X 2 hours. ·2009 If narcotic analgesics (codeine, meperidine) are given, raise side rails and place call light within reach. Instruct client not to get out of bed or ambulate without assistance. Caution client about drowsiness as a side effect. ·2010 A 1st degree tear involves only the epidermis. A 2nd degree tear involves dermis, muscle, and fascia. A 3rd degree tear extends into the anal sphincter, and a 4th degree extends up the rectal mucosa. Tears cause pain and swelling. Avoid rectal manipulations. ·2011 If it was documented that the fetus passed meconium in utero or the nurse noted LATE passage of meconium in delivery room, the neonate MUST be attended by a pediatrician, neonatologist, and/or nurse practitioner to determine, through endotracheal tube observation and suction, the presence of meconium below the cords. It can result in pneumonitis/meconium aspiration syndrome, which will necessitate a sepsis workup including a chest x-ray early in the transitional newborn period.·2012 Do not wait until a 1 minute Apgar is assigned to begin resuscitation of the compromised neonate. ·2013 Apgar scores of 6 or < at 5 minutes require an additional Apgar assessment at 10 minutes. ·2014 IV administration of analgesics is preferred to IM for the client in labor because the onset and peak occurs more quickly and duration of the drug is shorter. ·2015 IV administration: ·2016 Predictable onset: 5 minutes ·2017 Peak: 30 minutes ·2018 Duration: 1 hour ·2019 IM administration: ·2020 Onset: within 30 minutes ·2021 Peak: 1 to 3 hours after injection ·2022 Duration: 4 to 6 hours ·2023 Tranquilizers (ataractics and/or phenothiazines) Phenergan, Vistaril, are used in labor as analgesic-potentiating drugs to decrease maternal anxiety. ·2024 Agonist narcotic drugs (Demerol, morphine) produce narcosis and have a higher risk for maternal/fetal respiratory depression. Antagonist drugs (Stadol, Nubain) have less respiratory depression but MUST be used with caution in a mother with preexisting narcotic dependency since withdrawal symptoms occur immediately. ·2025 Pudendal block and subarachnoid (saddle block) are used only for second stage of labor. Peri/epidural may be used for all stages of labor. ·2026 The first sign of block effectiveness is usually warmth and tingling of ball/big toe of foot. ·2027 Discontinue continuous infusion at end of Stage I or during transition to increase pushing effectiveness. ·2028 Regional block anesthesia and fetal presentation ·2029 Internal rotation is harder to achieve when the pelvic floor is relaxed by anesthesia resulting in persistent occiput posterior position of fetus. ·2030 Monitor for fetal position. REMEMBER, mother cannot tell you she has back pain, which is the cardinal sign of persistent posterior fetal position. ·2031 Regional blocks, especially epidural and caudal, often result in assisted (forceps or vacuum) delivery due to the inability to push effectively in 2nd stage. ·2032 Nerve block anesthesia (spinal or epidural) during labor blocks motor as well as nerve fibers. Vasodilation below the level of the block results in blood pooling in the lower extemities and maternal hypotension. Approximately 20 minutes prior to nerve block anesthesia, the client should be hydrated with 500 to 1000 cc of lactated ringers IV. Monitor maternal vital signs and FHR q5 to 15 minutes. If hypotension occurs – turn the client to her side, administer O2 at 10 L/min by facemask, and increase IV rate. NORMAL PUERPERIUM ·2033 Normal leukocytosis of pregnancy averages 12,000 to 15,000 mm3. The first 10 to 12 dayspost-delivery, values of 25,000 mm3 are common. Elevated WBC and the normal elevated ESR may confuse interpretation of acute postpartal infections. For example, if the nurse assesses a client’s temperature to be 101 F on the client’s second postpartum day, what assessments should be made before notifying the physician? Assess fundal height and firmness, perineal integrity, check for a positive Homan’s sign and other symptoms, i.e., burning on urination, pain in leg, excessive tenderness of uterus. ·2034 Client/family teaching is a common area for NCLEX-RN questions. Remember, when teaching the first step is to assess the client’s (parent’s) level of knowledge and identify their readiness to learn. Client teaching regarding lochia changes, perineal care, breastfeeding, sore nipples are commonly tested content. ·2035 After the 1st PP day, the most common cause of uterine atony is retained placental fragments. The nurse must check for presence of fragments in lochial tissue. ·2036 Women can tolerate blood loss, even slightly excessive blood loss, in the postpartal period due to the 40% increase in plasma volume during pregnancy. In postpartal period can void up to 3,000 cc/day to reduce this volume increase that occurred during pregnancy. ·2037 Client should void within 4 hours of delivery. Monitor closely for urine retention. Suspect retention if voiding is frequent and <100 cc per voiding. ·2038 Women often have a syncopal spell (faint) on the first ambulation after delivery (usually related t ovasomotor changes, orthostatic hypotension). The astute nurse will check for client’s Hgb and Hct for anemia and the blood pressure, sitting and lying for orthostatic hypotension. ·2039 Kegel exercises: increase integrity of introitus and improve urine retention. Teach client to alternate contraction and relaxation of the pubococcygeal muscles. ·2040 Assess for thromboembolism: Examine legs of PP client daily for pain, warmth, and tenderness or a swollen vein which is tender to touch. Client may or may not exhibit a positive Homan’s sign (dorsiflexion of foot causes compression of tibial veins and pain if thrombus is present). ·2041 “Postpartum blues” are usually normal, especially 5 to 7 days after delivery (unexplained tearfulness, feeling “down,” and a decreased appetite). Encourage use of support persons to help with housework for first two postpartum weeks. Refer to community resources. ·2042 Remember RhoGAM is given to a Rh-negative mother who delivers a Rh-positive fetus and has a negative direct Coombs. If the mother has a positive Coombs, there is no need to give RhoGAM since the mother is already sensitized. ·2043 Because Rh Immune Globulins suppress the immune system, the client who receives both RhoGAM and the Rubella vaccine should be tested for rubella immunity at 3 months. THE NORMAL NEWBORN ·2044 PHYSICAL ASSESSMENT: A detailed physical assessment is performed by the nurse or physician. Regardless of who performs the physical assessment, the nurse must know normal versus abnormal variations of the newborn. Observations must be recorded and the physician and the physician notified regarding abnormalities. ·2045 It is difficult to differentiate between caput succedaneum (edema under the scalp) and cephalhematoma (blood under the periosteum). The caput crosses suture lines and is usually present at birth, while the cephalhematoma does NOT cross suture lines and manifests a fewhours after birth. The danger of cephalhematoma is increased by hyperbilirubinemia due to excess RBC breakdown. ·2046 These neurological reflexes are transient, and, as such, disappear usually within the first year of life. In the pediatric client, prolonged presence of these reflexes can indicate CNS defects. Anticipate NCLEX-RN questions regarding normal newborn reflexes. Physical assessment questions focus on normal characteristics of the newborn and the differentiation of conditions such as caput succedaneum and cephalhematoma. ·2047 The umbilical cord should always be checked at birth. It should contain 3 vessels, 1 vein which carries oxygenated blood to the fetus and 2 arteries which carry unoxygenated blood back to the placenta. This is the opposite of normal circulation in the adult. Cord abnormalities usually indicate cardiovascular or renal anomalies. ·2048 Postnatally, the fetal structures of foramen ovale, ductus arteriosus and ductus venosus should close. If they do not, cardiac and pulmonary compromise will develop. ·2049 Suctioning the mouth first and then the nose. Stimulating the nares can initiate inspiration which could cause aspiration of mucus in oral pharynx. ·2050 Circumcision has become controversial since there is no real medical indication for the procedure and it does not cause trauma and pain to the newborn. It was once thought to decrease the incidence of penile and cervical cancer, but some researchers say this is unfounded. ·2051 HYPOTHERMIA (heat loss) leads to depletion of glucose and, therefore, the use of brown fat (special fat deposits fetus puts on in last trimester which are important to thermoregulation) for energy, resulting in ketoacidosis and possible shock. Prevent by keeping neonate warm! ·2052 Physiologic jaundice (normal inability of the immature liver to keep up with normal RBC destruction) occurs at 2 to 3 days of life. If it occurs before 24 hours or persists beyond 7 days, it becomes pathologic. Typically, NCLEX-RN questions ask about normal problem of physiologic jaundice which occurs 2 to 3 days after birth due to the liver’s inability to keep up with RBC destruction and bind bilirubin. Remember, unconjugated bilirubin is the culprit. ·2053 Do not feed a newborn when the respiratory rate is over 60. Inform the physician and anticipate gavage feedings in order to prevent further energy utilization and possible aspiration. ·2054 A 7 lb. 8 oz. baby would need 50 calories X 7 lbs = 350 calories plus 25 calories (1/2 lb. or 8 oz.) = 375 calories per day. Most infant formulas contain 20 calories/ounce. Dividing 375 by 20 = 18.75 ounces of formula needed per day. ·2055 Teach parents to take infant’s temperature BOTH axillary and rectally. While axillary is recommended, some pediatricians will request a rectal temperature (core). ·2056 AXILLARY: Place thermometer under arm and hold thermometer in place 5 minutes. ·2057 RECTALLY: Use thermometer with BLUNT end. Insert thermometer ¼ to ½ inch and hold in place for 5 minutes. Hold feet and legs firmly. HIGH-RISK DISORDERS ·2058 Clients with prior traumatic delivery, history of D&C, multiple abortions (spontaneous or induced), or daughters of DES mothers may experience miscarriage or preterm labor related to INCOMPETENT CERVIX. The cervix may be surgically repaired prior to pregnancy, or DURING gestation. A CERCLAGE (McDonald’s suture) is placed around the cervix to constrict the internal os. The cerclage may be removed prior to labor if labor is planned or left in place if cesarean birthis planned. ·2059 Suspect ectopic pregnancy in any woman of childbearing age who presents at an emergency room, clinic, or office with unilateral or bilateral abdominal pain. Most are misdiagnosed with appendicitis. ·2060 A client who is 32 weeks gestation calls the healthcare provider because she is experiencing dark, red vaginal bleeding. She is admitted to the emergency room where the nurse determines the FHR to be 100 bpm. The client’s abdomen is rigid and boardlike, and she is complaining of severe pain. What action should the nurse take first? First, the nurse must use knowledge base to differentiate between abruptio placentae (this client) from placenta previa (painless bright red bleeding occurring in the third trimester). The nurse should immediately notify the healthcare provider and no abdominal or vaginal manipulation or exams should be done. Administer O2 per face mask. Monitor for bleeding at IV sites and gums due to the increased risk of DIC. Emergency Cesarean section is required since uteroplacental perfusion to the fetus is being compromised by early separation of the placenta from the uterus. ·2061 Clients with abruptio placentae or placenta previa (actual or suspected) should have NO abdominal or vaginal manipulation. NO Leopold’s maneuvers. NO vaginal exams. NO rectal exams, enemas, or suppositories. NO internal monitoring. ·2062 Disseminated intravascular coagulation (DIC) is a syndrome of abnormal clotting that is systematic and pathologic. Large amounts of clotting factors, especially fibrinogen, are depleted causing widespread external and/or internal bleeding. DIC is related to fetal demise, infection/sepsis, pregnancy-induced hypertension (Preeclampsia) and abruptio palcentae. ·2063 Podophyllin, which is usually used to treat HPV, is contraindicated in pregnancy because it is associated with fetal death, preterm labor, and cervical carcinoma. ·2064 Toxoplasmosis is usually related to exposure to cats, gardening (where cat feces may be found), or eating raw meat. ·2065 Rubella is teratogenic to the fetus during the FIRST trimester, causing congenital heart disease and/or congenital cataracts. All women should have their titers checked during pregnancy. If a women’s titer’s are low, she should receive the vaccine AFTER delivery and be instructed not to get pregnant within 3 months. Breastfeeding mothers may take the vaccine. ·2066 Although Metronidazole (Flagyl) is the treatment of choice for some vaginal infections, its use is contraindicated in the first trimester of pregnancy, and its use during the second trimester is controversial. Medications usually recommended for the non-pregnant client with STDs may be CONTRAINDICATED for the pregnant client due to effect on the fetus. ·2067 The outcome of adolescent pregnancy depends on prenatal care. NUTRITION is a key factor since the adolescent’s physiological needs for growth are already increased, plus the additional stress of pregnancy. ·2068 Although the toxic side effects of magnesium sulfate are well known and watched for, it is just as important to get serum blood levels of magnesium sulfate above 4 mg/dl in order to prevent convulsions and reach therapeutic range. ·2069 Hold next dose of magnesium sulfate and notify healthcare provider if any toxic symptoms occur (<12 respirations/minute, urine output <100 cc/4 hours, absent DTRs, Magnesium sulfate > 8 mg/dl). ·2070 When administering magnesium sulfate. ALWAYS have antidote available (calcium gluconate, 20 ml vial of 10% solution).·2071 Tachycardia is the major side-effect of tocolytic drugs, which are bete adrenergic agents such as terbutaline (Brethine) or ritodrine (Yutopar) used to stop preterm labor. Teach the client to take her pulse prior to administration and withhold medication if pulse is not within the prescribed parameters (usually whitheld if pulse >120 to 140). If administration is via a continuous pump, teach client to monitor pulse periodically. ·2072 In 1978, the FDA banned the use of oxytocin for ELECTIVE inductions. The healthcare provider must provide, for the record, the medical reason for oxytocin use. ·2073 Dystocia frequently requires the use of oxytocin for augmentation or induction of labor. Uterine tetany is a harmful complication and careful monitoring is required. The desired effect is contractions q2 to 3 minutes, with duration of contractions no longer than 90 seconds. Continuously monitor FHR and uterine resting tone. If tetany occurs, turn off Pitocin, turn client to a side-lying position, and administer O2 by facemask. Check output (should be at least 100 cc/4 hours). Oxytocin’s most important side effects is its antidiuretic (ADH) effect, which can cause water intoxification. Using IV fluids containing electrolytes decreases the risk of water intoxification. ·2074 The uterus is most sensitive to becoming tetanic at the beginning of infusion. The client must ALWAYS be attended and contractions monitored. Contractions should last NO longer than 90 seconds to prevent fetal hypoxia. ·2075 Women with previous uterine scars are prone to uterine rupture especially if oxytocin or forceps are used. If a woman complains of a sharp pain accompanied by the abrupt cessation of contractions, suspect uterine rupture, a MEDICAL EMERGENCY. Immediate surgical delivery is indicated to save the fetus and the mother. ·2076 Rarely are antihypertensive drugs used in the preeclamptic client. They are given only in the event of diastolic blood pressure over 110 mmHg. (CVA danger). Drug of choice is Hydralazine HCL (Apresoline). ·2077 Altough delivery is often described as the “cure” for preeclampsia, the client can convulse up to 48 hours after delivery. ·2078 The major goal of nursing care for a client with preeclampsia is to maintain uteroplacental perfusion and prevent seizures. This requires the administration of magnesium sulfate. Withhold administration of magnesium sulfate if signs of toxicity exist: respirations <12/minute, absence of DTRs, and urine output <30 ml/hour. ·2079 Nursing care during labor and delivery for the client with cardiac disease is focused on prevention of cardiac embarrassment, maintenance of uterine perfusion, and alleviation of anxiety. ·2080 Should these clients experience preterm labor, the use of beta-adrenergic agents such as terbutaline (Brethine) and ritodrine HCL (Yutopar) are contraindicated due to the chance of myocardial ischemia. ·2081 Normal diuresis, which occurs in the postpartum period, can pose serious problems to the new mother with cardiac disease because of the increased cardiac output. ·2082 Coumadin may NOT be taken during pregnancy due to its ability to cross the placenta and affect the fetus. HEPARIN is the drug of choice; it does NOT cross the placental membrane. ·2083 Recent research has found that Helicobacter pylori, (the bacterium that causes stomach ulcers) infection is another possible causative factor in hyperemesis. Other pregnancy and nonpregnancy risk factors for hyperemesis gravidarum include first pregnancy, multiple fetuses, age under 24, history of this condition in other pregnancies, obesity, and high fat diets. ·2084 In severe cases of hyperemesis gravidarum, the healthcare provider may prescribe antihistamines, vitamin B6, or phenothiazines to relieve nausea. The provider also prescribe metoclopramide (Reglan) to increase the rate the stomach moves food into the intestines, or antacids to absorb stomach acid and help prevent acid reflux. ·2085 Women who suffer from hyperemesis gravidarum are often deficient in thiamin, riboflavin, vitamin B6, vitamin A, and retinol-binding proteins. ·2086 GLUCOSE SCREEN: Client does NOT have to fast for this test. 50 gm of glucose is given and blood is drawn after one hour. If the blood glucose is greater than 135 mg/dl, the na threehour glucose tolerance test (GTT) is done. ·2087 High incidence of fetal anomalies occurs in pregnant diabetic women. Therefore, fetal surveillance is very important. Ultrasound exam. Alpha-fetoprotein (to determine neural tube anomalies). Non-stress and contraction stress tests. ·2088 Oral hypoglycemics are not taken in pregnancy due to potential teratogenic effects on fetus. Insulin is used for therapeutic management. ·2089 When a woman is admitted in labor with diagnosis of diabetes mellitus. She is more prone to preeclampsia, hemorrhage and infection. Delivery is often scheduled between 37 to 38 weeks gestation to avoid the end of the 3rd trimester of pregnancy because this is a VERY difficult time to maintain diabetic control. ·2090 It is useful to discontinue long-acting insulin administration on the day before the delivery is planned since insulin requirements are less in labor and drop precipitously after delivery. ·2091 Estrogen-containing birth control pills affect glucose metabolism by increasing resistance to insulin. The intrauterine device may be associated with an increased risk of infection in these already vulnerable women. ·2092 If a woman is medicated, the responsible adult accompanying her must sign the necessary consent forms. State laws differ as to the acceptability of a friend signing the consent form rather than a relative. ·2093 Babies delivered abdominally miss out on the vaginal squeeze and are born with more fluid in the lungs, predisposing the newborn to transient tachypnea (TTN) and respiratory distress. ·2094 The preferable low-transverse uterine incision usually results in less postoperative pain, less bleeding, and less incidents of ruptured uterus. The classical, vertical incision on the uterus may involve part of the fundus, resulting in more postoperative pain, bleeding, and an increased chance of uterine rupture. ·2095 Due to the exploration and cleansing of the uterus just after delivery of the placenta, the amount of lochia may be scant in the recovery room. However, pooling in the vagina and uterus while on bedrest may result in blood running down the client’s leg when she first ambulates. Cesarean birth clients have the same lochial changes, placental site healing, and aseptic needs as do vaginal birth clients. ·2096 A laparotomy of any kind, including cesarean birth, predisposes the client to postoperative paralytic ileus. When the bowel is manipulated in surgery, it ceases preistalsis, which may persist. Symptoms include: absent bowel sounds, abdominal distention, tympany on percussion, nauseaand vomiting, and of course, obstipation (intractible constipation). Early ambulation is an effective nursing intervention. POSTPARTUM HIGH-RISK DISORDERS ·2097 Nurse must be especially supportive of postpartum client with infection because it usually implies isolation from newborn until organism is identified and treatment begun. Arrange phone calls to nursery and window viewing. Involve family, spouse, significant others in teaching, and encourage other family members to continue neonatal attachment activities. ·2098 Most common iatrogenic cause of UTI is urinary catheterization. Encourage clients to void frequently and not ignore the urge. IV antibiotic are usually administered to clients with pyelonephritis. ·2099 Remember, the risk of postpartum infections increases for clients who experienced problems during pregnancy (e.g., anemia, diabetes) or experienced trauma during labor and delivery. ·2100 Clients taking anticoagulants can usually expect to have heavy menstrual periods. ·2101 In most cases, a mother who is on antibiotic therapy can continue to breastfeed unless the healthcare provider thinks the neonate is at risk for sepsis by maternal contact. Sulfa drugs are used cautiously in lactating mothers because they can be transferred to the infant in breast milk. ·2102 Many times mastitis can be confused with a blocked milk sinus, which is treated by nursing closer to the lump and by rotating the baby on the breast. Breastfeeding is not contraindicated for women with mastitis, unless pus is in the breast milk, or the antibiotic of choice is harmful to the infant. If either of these occurs, milk production can still be fostered by manual expression. ·2103 During medical emergencies such as bleeding episodes, clients need calm, direct explanations and assurance that all is being done that can be done. If possible, allow support person at bedside. Risk-management principles state that the suit-prone client is one who feels things are being hidden from her or that adequate attention is NOT being give to HER problem. ·2104 Risk factors for hemorrhage include: dystocia, prolonged labor, over distended uterus, abruptio placentae, and infection. ·2105 What immediate nursing actions should be taken when a postpartum hemorrhage is detected? ·2106 Perform fundal massage ·2107 Notify the healthcare provider if the fundus does not become firm with massage ·2108 Count pads to estimate blood loss ·2109 Assess and record vital signs ·2110 Increase IV fluids (additional IV line may be indicated) ·2111 Administer oxytocin infusion as prescribed NEWBORN HIGH-RISK DISORDERS ·2112 “Jitteriness” is a clinical manifestation of hypoglycemia and hypocalcemia. Laboratory analysis is indicated to differentiate between two etiologies. ·2113 To avoid metabolic problems brought on by cold stress, the first step and number one priority, in management of the newborn is to prevent loss of body heat, followed by ABCs. Neonatesproduce heat by non-shivering thermogenesis, by burning brown fat. The neonate is easily stressed by hypothermia and develops acidosis from hypoxia. Prevent chilling (keep under radiant warmer or in isolette). If cold, the first signs exhibited are prolonged acrocyanosis, skin mottling, tachycardia, and tachypnea. If cold stressed, warm slowly over 2 to 4 hours since rapid warming may produce apnea. The neonate needs glucose, he/she has little glycogen storage and needs to be fed. ·2114 The lower the score on the Silverman-Anderson index of Respiratory Distress, the better the respiratory status of the neonate. A score of 10 indicates that a newborn is in severe respiratory distress. This is the exact opposite of the method used for Apgar scoring. ·2115 WATCH the newborn Hct; it is difficult to oxygenate either an anemic newborn (lack of oxygencarrying capacity) or a newborn with polycythemia (Hct >80%, thich, sluggish circulation). ·2116 The PO2 should be maintained between 50 to 90 mmHg. PO2 <50 signifies hypoxia, PO2 > 90 signifies oxygen toxicity problems. ·2117 Antibiotic dosage is based on the neonate’s weight in kilograms. Peak and trough drug levels are drawn to evaluate if therapeutic drug levels have been achieved. Closely monitor the neonate for adverse effects of ALL drugs. ·2118 Sepsis can be indicated by both a temperature increase and a temperature decrease. ·2119 Drugs used to treat neonatal infections can be ototoxic and nephrotoxic. Close monitoring of therapeutic levels and observation for side effects are required. ·2120 Renal immaturity in the preterm infant makes the monitoring of IV fluid administration and drug therapy crucial. Closely monitor BUN and creatinine levels when administering the “mycin” antibiotics to treat infections in the neonate. ·2121 If tube passes into trachea, newborn can make NO noise, i.e., no crying. Newborn may gag, cough, or become cyanotic. ·2122 To assess for skin jaundice, apply with thumb over bony prominences to blanch skin. After removing thumb, area will look yellow before normal skin color reappears. The best areas for assessment are the nose, forehead, and sternum. In dark-skinned infants, observe conjunctival sac and oral mucosa. ·2123 Lab tests measure total and direct (conjugated, excretable, non-fat soluble) bilirubin levels. The dangerous bilirubin is the unconjugated, indirect (fat-soluble), which is measured by subtracting the direct from the total bilirubin. ·2124 Maintenance of hydration is crucial for all infants. The preterm infant is already at risk for fluid and electrolyte imbalances due to increased body surface area from extended body positioning and larger body area in related to body weight. Phototherapy treatment for hyperbilirubinemia (level > 12 mg/dl) increases the risk for dehydration. PSYCHIATRIC NURSING THERAPEUTIC COMMUNICATION / TREATMENT MODALITIES ·2125 The purpose of therapeutic interaction with clients is to allow them the autonomy to make choices when appropriate. Keep statements value free, advice free, and reassurance free. Remember, JUST THE FACTS! NO OPINIONS!·2126 What action should the nurse take in a “psychiatric situation” when the client describes a physical problem? Assess, assess, assess! If the client with paranoid schizophrenia on the psychiatric unit complains of chest pain, take his/her blood pressure. If the OB client who has delivered a dead fetus complains of perineal pain – look at the perineal area (she may have a hematoma). Just because the focus of the client’s situation is on his/her psychological needs, it does not mean that the nurse can ignore physiological needs. ·2127 Remember, nurses are “nice” people, but they are also therapeutic. ·2128 Basic communication principles can be applied to all clients: ·2129 Establish trust. ·2130 Demonstrate a non-judgmental attitude ·2131 Offer self; be emphathetic, NOT sympathetic ·2132 Use active listening ·2133 Accept and support client’s feelings ·2134 Clarify and validate client’s statement ·2135 Use matter-of-fact approach ·2136 Remember, a nurse’s nonverbal communication may be more important that his/her verbal communication. ·2137 A question concerning nurse-client confidentiality often appears on the NCLEX-RN. For the nurse to tell a client she/he will not tell anyone about their discussion, puts the nurse in a difficult position. Some information MUST be shared with other team members for the client’s safety (e.g., suicide plan) and optimal therapy. ·2138 Nausea is a common complaint after ECT. Vomiting by the unconscious client can lead to aspiration. Because post-ECT clients are unconscious, the nurse must observe closely for the possibility of aspiration, i.e., MAINTAIN A PATENT AIRWAY! ANXIETY DISORDERS ·2139 Common physiological responses to anxiety include increased heart rate and blood pressure; rapid, shallow respirations; dry mouth, tight feeling in throat; tremors, muscle tension; anorexia; urinary frequency; palmar sweating. ·2140 Anxiety is very contagious and is easily transferred from client to nurse AND from nurse to client. FIRST, the nurse must assess his/her own level of anxiety and remain calm. A calm nurse assists the client to gain control, decrease anxiety, and increase feelings of anxiety. ·2141 When a client described a phobia or expresses an unreasonable fear, the nurse should acknowledge the feeling (fear) and refrain from exposing the client to the identified fear. After trust is established, a desensitization process may be prescribed. Desensitization is the nursing intervention for phobia disorders. The nurse should: ·2142 Assist client to recognize factors associated with feared stimuli that precipitate a phobic response. ·2143 Teach and practice with client alternative adaptive coping strategies such as the use of thought substitution (replacing a fearful thought with a pleasant thought), and relaxation techniques. Role-playing is useful when the client is in a calm state. ·2144 Expose client progressively to feared stimuli, offering support with the nurse’s presence. ·2145 Provide positive reinforcement whenever a decrease in phobic reaction occurs. ·2146 NOTE: In all likelihood, the desensitization process will be overseen by a mental healthpractitioner (NP psych CNS, or psychologist). ·2147 The nurse should place an anxious client where there are reduced environmental stimuli – a quiet area of the unit, away from the nurse’s station. ·2148 The best time for interaction with a client is at the completion of the performed ritual. The client’s anxiety is lowest at this time; therefore, it is an optimal time for learning. ·2149 Compulsive acts are used in response to anxiety, which may or may not be related to the obsession. It is the nurse’s responsibility to help alleviate anxiety. Interfering will increase anxiety. These acts should be allowed as long as the client’s acts are free of violence. The nurse should: ·2150 Actively listen to the client’s obsessive themes ·2151 Acknowledge effects that ritualistic acts have on the client ·2152 Demonstrate empathy ·2153 Avoid being judgmental ·2154 For clients with postraumatic stress disorder, the nurse should: ·2155 Actively listen to client’s stories of experiences surrounding the traumatic event ·2156 Assess suicide risk ·2157 Assist client to develop objectivity about the event and problem solve regarding possible means of controlling anxiety related to the event ·2158 Encourage group therapy with other clients who have experienced the same or related traumatic events SOMATOFORM DISORDERS ·2159 Be aware of your own feelings when dealing with this type of client. It is a challenge to be non-judgmental. The pain is real to the person experiencing it. These disorders cannot be explained medically: they result from internal conflict. The nurse should: ·2160 Acknowledge the symptom or complaint ·2161 Reaffirm that diagnostic test results reveal no organic pathology ·2162 Determine the secondary gains acquired by the client DISSOCIATIVE DISORDERS ·2163 The nurse should be aware that ALL behavior has meaning. ·2164 Avoid giving clients with dissociative disorders too much information about past events at one time. The various types of amnesia, which accompany dissociative disorders, provide protection from pain. Too much, too soon, may cause decompensation. PERSONALITY DISORDERS ·2165 Personality disorders are long-standing behavioral traits that are maladaptive responses to anxiety and cause difficulty in relating and working with other individuals. NCLEX-RN questions test personality disorder content by describing management situations. ·2166 Persons with a personality disorder are usually comfortable with their disorder and believe that they are right and the world is wrong. These individuals usually have very little motivation to change. Think of them as a CHALLENGE.EATING DISORDERS ·2167 People with Anorexia gain pleasure from providing others with food and watching them eat. These behaviors reinforce their perception of self-control. Do not allow these clients to plan or prepare food for unit-based activities. ·2168 People with Bulimia often use syrup of ipecac to induce vomiting which may cause cardiovascular problems such as congestive heart failure (CHF). Because CHF is not usually seen in young people, it is often overlooked. Assess for edema and listen to breath sounds. ·2169 Physical assessment and nutritional support are a priority; the physiological implications are great. Nursing interventions should increase self-esteem and develop a positive body image. Behavior modification is useful and effective. Family therapy is most effective since issues of control are common in these disorders. (Therapy is usually long term). MOOD DISORDERS ·2170 Depressed clients have difficulty hearing and accepting compliments because of their lowered self-concept. Comment on signs of improvement by noting the behavior, e.g., “I noticed you cobed your hair today” NOT, “You look nice today.” ·2171 The most important signs and symptoms of depression are a depressed mood with a loss of interest or pleasure in life. The client has sustained a loss. Other symptoms include: ·2172 Significant change in appetite often accompanied by a change in weight – either weight loss or gain ·2173 Insomnia or hyperinsomnia (usually sleeping during the day – often because the client is not sleeping at night due to anxiety). ·2174 Fatigue or a lack of energy ·2175 Feelings of hopelessness, worthlessness, guilt, or over-responsibility ·2176 Loss of ability to concentrate or think clearly ·2177 Preoccupation with death or suicide ·2178 The nurse knows depressed clients are improving when they begin to take an interest in their appearance or begin to perform self-care activities, which were previously of little or no interest. ·2179 The nurse should suspect an imminent suicide attempt if a depressed client becomes “better,” e.g., happy or even elated. Be aware – a happy affect may signify that the client feels relieved that a plan has been made and he/she is ready for the suicide attempt. ·2180 When dealing with a depressed client, the nurse should assist with personal hygiene tasks and encourage the client to initiate grooming activities even when he/she does not feel like doing so. This helps promote self-esteem and a sense of control. ·2181 An important intervention for the depressed client is to sit quietly with the client. When answering NCLEX-RN questions, remember that you are working at Utopia General and there is plenty of time and staff to provide ideal nursing care. Do not let realities of clinical situations deter you from choosing the best nursing intervention. The best intervention is to sit quietly with the client, offering support with your presence. ·2182 There are always drug questions on the NCLEX-RN. Here are some tips: Know common side effects for drug groups. For example:·2183 Anti-anxiety drugs = sedation, drowsiness ·2184 Antidepressant drugs = anticholinergic effects, postural hypotension ·2185 MAO inhibitors = hypertensive crisis ·2186 Know specific problems or concerns for drug therapy. For example: ·2187 Lithium requires renal function assessment and monitoring ·2188 Phenothiazines cause extrapyramidal effects (EPS); tardive dyskinesia can be permanent if client is not assessed regularly for signs of tardive dyskinesia! ·2189 Know specific client teaching for drug therapy. For example: ·2190 Phenothiazines = photosensitivity, need to wear protective clothing, sunglasses ·2191 MAO inhibitors = dietary restrictions to prevent hypertensive crisis ·2192 Monitor serum lithium levels carefully. The therapeutic range is between 0.5 and 1.5 mEq/L. the therapeutic and toxic levels are very close in reading. Signs of toxicity are evident when lithium levels are more than 1.5 mEq/L. Blood levels should be drawn 12 hours after LAST dose. ·2193 Manic clients can be very caustic toward authority figures. Be prepared for personal “put downs.” Avoid arguing or becoming defensive. ·2194 What activities are appropriate for a manic client? = Noncompetitive physical activities, which require the use of large muscle groups. ·2195 Where should a manic client be placed on the unit? = Make every attempt to reduce stimuli in the environment. Place the client in a quiet part of the unit. ·2196 What interventions should the nurse use if a client becomes abusive? ·2197 Redirect negative behavior or verbal abuse in a calm, firm, non-judgmental, non-defensive manner ·2198 Suggest a walk or physical activity ·2199 Set limits on intrusive behavior. For example, “When you interrupt, I cannot explain the procedure to the others; please wait your turn.” ·2200 If necessary, seclude or administer medication if client becomes totally out of control. Always remember to use compassion because nurses are “nice” people. ·2201 Two atypical antipsychotic drugs are also indicated for mania (risperidone and olanzapine). THOUGHT DISORDERS: SCHIZOPHRENIA ·2202 There are five types of schizophrenia specified under the DSM-IV-TR. The DSM-IV-TR is a diagnostic manual prepared by the American Psychiatric Association that provides diagnostic criteria for all psychiatric disorders. ·2203 Observe for increased motor activity and/or erratic response to staff and other clients. The client may be experiencing an increase in command hallucinations. When this occurs, there is an increased potential for aggressive behavior. THINK PRN! ·2204 When evaluating client behaviors, consider the medications the client is receiving. Exhibited behaviors may be manifestations of schizophrenia or a drug reaction. ·2205 Use Bleuler’s four As to help remember the important characteristics of schizophrenia:·2206 Autism (preoccupied with self) ·2207 Affect (flat) ·2208 Association (loose) ·2209 Ambivalence (difficulty making decisions) ·2210 Do not argue with a client about their delusions. Logic does NOT work, it only increases the client’s anxiety. Be matter-of-fact and divert delusional thought to reality. Trust is the basis for all interactions with these clients. Be supportive and non-judgmental. Stress increases anxiety and the need for delusions and hallucinations. Do not agree you hear voices (you should be the client’s contact to reality), but acknowledge your observation of the client, for example, “You look like you’re listening to something.” ·2211 Know the side effects of drugs commonly used to treat schizophrenia since client behavioral changes may be due to drug reactions instead of schizophrenia. SUBSTANCE ABUSE ·2212 Know what defense mechanisms are used by chemically dependent clients. Denial and rationalization are the two most common coping styles used – their use must be confronted so accountability for the client’s own behavior can be developed. ·2213 What basic needs have priority when working with chemically dependent clients? Nutrition is a priority. Alcohol and drug intake has superseded the intake of food for these clients. ·2214 What behaviors are expected during withdrawal? In the alcoholic, delirium tremens (DT) occurs 12 to 36 hours after the last intake of alcohol. Know the symptoms (tachycardia, tachypnea, diaphoresis, marked tremors, hallucinations, paranoia). In drug abuse, withdrawal symptoms are specific to the type of drug. ·2215 What medications can the nurse expect to administer to chemically dependent clients? In treating alcohol withdrawal, Librium or Ativan are commonly used. Antabuse is often used as s deterrent to drinking alcohol. Client teaching should include the effects of consuming any alcohol while on Antabuse. Encourage client to read all labels of over-the-counter medications and food products, which may contain small amounts of alcohol. ·2216 What type of therapy is used with chemically dependent clients? Group therapy is effective as well as support groups such as Alcoholics Anonymous, Narcotics Anonymous, etc. ·2217 Harm reduction is a community health strategy designed to reduce the harm of substance abuse to families, individuals, community, and society. ·2218 More compassionate drug treatment options including abstinence and drug substitution models. ·2219 HIV related interventions such as needle exchanges ·2220 Directed drug use management should the client wish to continue use ·2221 Changes in laws concerning possession of paraphernalia ABUSE ·2222 Select only one nurse to care for an abused child. Abused children have difficulty establishing trust. The child will be less anxious with one consistent caregiver. ·2223 Women who are abused may rationalize the spouse’s behavior and unnecessarily accept theblame for his actions. The woman may or may not choose to press charges. Be sure to give her the number of a shelter for “help line” for future occurrences, as well as develop a safety plan. ·2224 It is difficult for an elderly person to admit abuse for fear being placed in a nursing home or being abandoned. Therefore, it is imperative to establish a trusting relationship with the elderly client. ·2225 Rape victims are at high risk for Post Traumatic Stress Disorder (PTSD). Immediate intervention to diminish distress is vital. The nurse should also assess for and intervene for sequellae such as unwanted pregnancy, sexually transmitted diseases, and HIV risk. ·2226 Questions on the NCLEX-RN regarding physical/sexual abuse usually focus on three aspects: ·2227 Physical manifestations of abuse ·2228 Client safety ·2229 Legal responsibilities of the nurse – In children, the nurse is legally responsible to report all suspected cases of abuse. In intimate partner abuse, it is the adult’s decision; the nurse should be supportive of their decision. Remember to document objective factual assessment data and the client’s exact words in cases of sexual abuse/rape. ORGANIC MENTAL DISORDERS ·2230 Confusion in the elderly is often “accepted” as part of growing old. This confusion may be due to dehydration with resulting electrolyte imbalance. Think “sudden change” when obtaining a history. Such changes are usually due to a specific stressor, and treatment for the causative stressor will usually result in correcting the confusion. ·2231 Confabulation is not lying. It is used by the client to decrease anxiety and protect the ego. ·2232 Nursing interventions for the confused elderly should focus on: ·2233 Maintaining the client’s health and safety ·2234 Encouraging self care ·2235 Reinforcing reality orientation (e.g., “Today is Monday,” and call the client by name). ·2236 Providing a consistent, safe environment – engage client in simple tasks, activities to build self-esteem ·2237 Providing consistent caregiver is a priority in planning nursing care for the confused older client. Change increases anxiety and confusion. ·2238 May also use atypical antipsychotics such as resperidine, quetiapine, olanzapine, Clozaril is not a front-line agent due to side-effects. May also give mood stabilizers and antianxiety medications as indicated. ·2239 The basic difference between delirium and dementia is that delirium is acute, and reversible, whereas dementia is gradual and permanent. CHILDHOOD AND ADOLESCENT DISORDERS ·2240 Children also experience depression, which often presents as headaches, stomachaches, and other somatic complaints. Be sure to assess suicidal risks, especially in the adolescent. ·2241 The client’s lack of remorse or guilt about their antisocial behavior represents a malfunction ofthe superego or conscience. The id functions on the basic instinct level and strives to meet immediate needs. The ego is in touch with external reality and is the part of the personality that makes decisions. ·2242 Important points to remember when answering NCLEX-RN questions: ·2243 These children may be involved in self-fulfilling prophecy (e.g., “Mom says that he/she is a trouble-maker, therefore, he/she must live up to Mom’s expectations”). ·2244 Confront the client with his/her behavior, e.g., lying. This gives the client a sense of security. ·2245 Provide consistent interventions – helps to prevent manipulation. Inconsistency does not help the client develop self-control. GERONTOLOGICAL NURSING ·2246 Changes in the heart and lungs result in less efficient utilization of O2, which reduces an individual’s capacity to maintain physical activity for long periods of time. Physical training for older persons can significantly reduce blood pressure and increase aerobic capacity. NCLEX-RN questions ask about teaching and designing rehab programs for the elderly – they should contain something about exercise and nutrition. ·2247 Older persons often complain that they cannot get to sleep at night and do not sleep soundly even after they fall asleep. This is because they have shorter stages of sleep, particularly shorter cycles from stages 1 to 4 and REM sleep (stage 4 is deep sleep). They are easily awakened by environmental stimuli. They often compensate by napping during the day, which leads to further disruptions of night sleep. A common response is use of prescription sleeping pills which can create still further problems of disorientation, etc. ·2248 Both systolic and diastolic blood pressure tend to increase with normal aging, but the elevation of the systolic is greater. REMEMBER the physiologic of blood pressure, which is expressed as a ratio of systolic to diastolic pressure. Systolic refers to the level of blood pressure during the contraction phase whereas diastolic refers to the stage when the chambers of the heart are filling with blood. ·2249 Dysrhythmias in the elderly are particularly serious since older persons cannot tolerate decreased cardiac output, which can result in syncope, falls, and transient ischemic attacks (TIAs). Pulse may be rapid, slow, or irregular. ·2250 Angina symptoms may be absent in the elderly or they may be confused with GI symptoms. ·2251 With aging, the muscles that operate the lings lose elasticity so that respiratory efficiency is reduced. Vital capacity (the amount of air brought into the lungs at one time) decreases. Breathing may become more difficult after strenuous exercise or after climbing up several flights of stairs. The rate of decline has been found to be slower in more active persons. The nurse should encourage older persons to remain physically active for as long as possible. Declining muscle strength may impair cough efficiency. This fact makes older persons more susceptible to chronic bronchitis, emphysema, and pneumonia. ·2252 COPD is the major cause of respiratory disability in the elderly. ·2253 Aging changes that contribute to chronic constipation: ·2254 The number of enzymes in the small intestine is reduced and simple sugars are absorbed more slowly, resulting in decreased efficiency of the digestive process. ·2255 The smooth muscle content and muscle tone of the wall of the colon decrease. Anatomical changes in the large intestine result in decreased intestinal motility. ·2256 Psychological factors, as well as abuse of over-the-counter laxatives·2257 Decreases in fluid intake and mobility contribute to constipation ·2258 Tooth loss is NOT a normal aging process. Good dental hygiene, good nutrition, and dental care can prevent tooth loss. ·2259 Older persons appear to eat small quantities of food at mealtimes. This is because the digestive system of older persons features a decrease in contraction time of the muscles and more time is needed for the cardiac sphincter to open. Therefore, it takes more time for the food to be transmitted to the stomach. Thus, the sensation of fullness may occur before the entire meal is consumed. ·2260 Older persons have a higher risk of developing renal failure because normal age-related changes result in compromised renal functioning. The nurse should pay careful attention to urinary output in older clients because it is the first sign of loss of renal integrity. ·2261 Kegel exercises consist of tightening and relaxing the vaginal and urinary meatus muscles. These exercises have been very successful in reducing the incidence of incontinence. They must be done consistently, and they can be done unobtrusively at home. ·2262 The elderly with incontinence may seek isolation, thereby predisposing themselves to loneliness. ·2263 15 to 30% of community-based elderly and almost 50% of elderly living in nursing homes suffer from difficulties with bladder control. Older persons may be more sensitive to alcohol and caffeine since these substances inhibit the production of antidiuretic hormone (ADH). An assessment of sensitivity to bladder problems is essential when planning nursing care. ·2264 MEDICATION ALERT: ·2265 As one ages, the total number of functioning glomeruli decreases until function has been reduced by nearly 50%. This decrease in the filtration efficiency of the kidneys has grave implications for persons who are taking medication. Of particular importance are penicillin, tetracycline, and digoxin, which are primarily cleared from the blood stream by the kidneys. These drugs remain active longer in an older person’s system. Therefore, they may be more potent, indicating a need to adjust the dosage frequency of administration. ·2266 Alzheimer’s disease is the most common irreversible dementia of old age. It is characterized by deficits in attention, learning, memory, and language skills. Discuss the problems family members have in dealing with Alzheimer’s clients in relation to the following disease manifestations: ·2267 Depression ·2268 Night wandering ·2269 Aggressive or passiveness ·2270 Failure to recognize family members ·2271 Strokes from cerebral thrombosis are more common in older persons than are strokes from cerebral hemorrhage. Clots tend to develop when patient is awake or just arousing. ·2272 Normal loss of brain cells is compounded by alcohol, smoking, and breathing polluted air. In relation to such losses, the nurse should teach to shop at uncrowded times in stores that are familiar to them, slow down well in advance of traffic signals, stay in the slower lane of the freeway, avoid freeways during rush hours, and leave for appointments well ahead of time. ·2273 The most common endocrine disorders in the older adult are thyroid dysfunctions and diabetes.·2274 Impaired mobility, impaired skin integrity, decreased peripheral circulation, and a lack of physical activity place the elderly at risk for developing decubitus ulders. ·2275 Ways to help prevent/decrease the occurrence of falls: ·2276 Adequate lighting ·2277 Pain the edges of stairs a bright color ·2278 Place a bell on the elderly person’s cat (since cats move quickly and get underfoot) ·2279 Wear proper footwear that supports the foot and contributes to balance (made of non-slippery materials). ·2280 Peripheral circulation decreases as one ages. Regular assessment of the feet is very important because it increases the opportunity to discover and treat skin care problems early. These problems could become more serious because of decreased circulation. ·2281 Older persons have a dry, wrinkled skin because they lose subcutaneous fat and the second layer of skin, the dermis, becomes less elastic. ·2282 Diminished eyesight results in: ·2283 A loss of independence (ADL and driving) ·2284 A lack of stimulation ·2285 The inability to read ·2286 A fear of blindness ·2287 Lower the tone of your voice when talking to an older person who is hearing-impaired. Highpitched tones (i.e., women’s voices) are the first hearing to go, therefore, lowering the pitch of your voice increases the likelihood that an older person with a hearing loss will be able to hear you speak. ·2288 Presbycusis (age-related hearing loss) can result in decreased socialization, avoidance of friends and family, decreased sensory stimulation, and hazardous conditions when driving. ·2289 Use frequent touch to decrease the sense of isolation and to compensate for visual and sensory loss. ·2290 Older persons undergo a great many changes, which are usually associated with LOSS (loss of spouse, friends, career, home, health, etc.). therefore, older persons are extremely vulnerable to emotional and mental stress. ·2291 INTEGRITY VS. DESPAIR is Erikson’s final stage of growth and development. Reminiscing is a means of setting one’s life in order (accepting life and self), which is the task of this stage of Erikson’s development theory. The goal of this stage is to feel a sense of meaning in one’s life, rather than to feel despair or bitterness that life was wasted. The major task of old age is to redefine self in relation to a changed role. Those persons who had been in charge of situations most of their lives may now fund themselves in dependent positions. The role adjustment is a major task of old age. ·2292 Think about the following situations and discuss the nursing care for each. ·2293 A nursing supervisor who has had a stroke and is sent to a long term facility for rehabilitation. ·2294 An oil company executive retires after 42 years with the company to travel in his recreational vehicle wit his wife and dog. ·2295 Shortly after their 53rd wedding anniversary, a woman who has never worked outside the home loses her husband to brain cancer.·2296 There are many conditions that can imitate dementia in the older adult. A key role for the nurse is to complete assessment to rule out other possible causes. Important HESI/NCLEX Terms/Glossary: abruptio placentae Premature separation of a normally positioned placenta in a pregnancy of at least 20 weeks' gestation either before labor or during labor but before delivery. This serious complication of pregnancy, occurring in one of every 200 births and often resulting in hemorrhage, may lead to the death of the mother, the fetus, or both. Also called ablatio placentae, accidental hemorrhage. abuse 1. Behavior toward another that is offensive, harmful, or injurious. 2. Misuse or particularly excessive use of a substance, service, or equipment; commonly refers to improper use of a drug or similar substance. accommodation 1. The act or process of adapting to changes in the physiologic or psychological environment to maintain homeostasis. 2. In ophthalmology: adjustment of the lens of the eye for various distances. 3. In sociology: the use of compromise, arbitration, or negotiation to resolve conflicts between persons or groups that arise from differences in customs or cultural norms. Also called adjustment. acquired immunodeficiency syndrome (AIDS) A disorder of the immune system characterized by an inability to mount a successful defense against infection such as by organisms that usually aren't pathogenic (opportunistic infections). The syndrome is caused by infection with the human immunodeficiency virus, which causes a marked depletion in the number of helper T cells. AIDS is currently incurable and fatal. However, recently developed drug treatments and regimens seem to be effective in prolonging the lives of clients with AIDS. active immunity Acquired immunity caused by the production of antibodies, either after infection or as a result of vaccination. acute lymphocytic leukemia (ALL) A form of leukemia, most commonly occurring in children, marked by large numbers of immature leukocytes in the blood and blood-forming tissues (including the bone marrow, spleen, liver, and lymph nodes). The disease has a sudden onset and rapid clinical course. Signs and symptoms include fever,pallor, fatigue, loss of appetite, anemia, bleeding, bone pain, spleen enlargement and, because the immune function is disturbed, frequent infection. Also called acute lymphoblastic leukemia. acute nephritis Acute inflammation of the kidney, possibly involving the glomerulus, tubules, and interstitial tissues. Addison's disease A life-threatening condition characterized by fatigue, hypotension, loss of appetite and weight, nausea or vomiting, and increased hyperpigmentation of the skin and mucous membranes. It results from partial or complete loss of glucocorticoid, mineralocorticoid, and androgenic function of the adrenal glands caused by tuberculosis, an autoimmune process, or other disease. Also called Addisonism, Addison's syndrome, chronic adrenocortical insufficiency. Addisonian crisis An emergency situation occurring with adrenal hypofunction and exposure to trauma, surgery, or other severe physiologic stress that exhausts the body's stores of glucocorticoids. adrenergic 1. Activated or transmitted by epinephrine, norepinephrine, or a similar substance. 2. Also called a sympathomimetic, a drug that stimulates alpha or beta receptors (thus mimicking the effects of epinephrine or norepinephrine) or acts primarily on receptors in the sympathetic nervous system that are stimulated by dopamine. advance directive Documented written or verbal instructions by the client about his wishes for life-sustaining medical care in the event he becomes incapacitated (for example, living wills, durable powers of attorney for health care, or any document that states the client's wishes). agonist 1. In anatomy: any muscle in a state of contraction whose action is opposed by another muscle with which it’s paired (called the antagonist). 2. In pharmacology: a drug that has an affinity for and stimulates physiologic activity at cell receptors. agoraphobia An intense, irrational fear of being in open spaces or of venturing out from the home or other familiar setting. The anxiety may be generalized to any setting beyond the home or may be specific for certain types of situations and environments, such as open spaces or crowded places. akinesia 1. Loss of the ability to move voluntarily. 2. The rest period after systole in the normal heart rhythm. 3. In psychiatry: a neurotic condition characterized by symptoms of paralysis.Allen's test A test designed to evaluate a client's collateral circulation in the arm before an invasive arterial procedure such as arterial blood gas analysis. While the client's radial and ulnar arteries are occluded, he clenches his fist, causing the hand to blanch. The client then unclenches his fist while the pressure on the ulnar artery is released (but the radial artery remains occluded). The hand should become pink, indicating a patent ulnar artery. amblyopia Decreased visual acuity in one eye in the absence of detectable structural or pathologic changes. amenorrhea The absence or cessation of menstruation. Except in preadolescents and in pregnant and postmenopausal women, amenorrhea may reflect dysfunction of the hypothalamus, pituitary gland, ovary, or uterus; congenital absence or surgical removal of both ovaries or the uterus; or an adverse effect of medication. amniocentesis Withdrawal of a sample of amniotic fluid by transabdominal puncture and needle aspiration, usually performed during the fifth month of pregnancy to detect such genetic disorders as Down syndrome, neural tube defects, and Tay-Sachs disease; if the clinician suspects sex-linked genetic defects, the procedure may be done to determine fetal gender. amniotomy Artificial rupture of the membranes. analgesic 1. Having the ability to relieve pain. 2. A medication that relieves pain. anaphylaxis A systemic reaction to a previously encountered antigen. anastomosis A surgical procedure in which two blood vessels, ducts, or other tubelike structures are joined to allow the flow of substances between them. Types of anastomoses are end-to-end and side-to-side. angina pectoris Severe chest pain characterized by sensations of spasm, constriction, and crushing weight, classically radiating from the area over the heart to the left shoulder and arm and possibly accompanied by a feeling of choking or suffocation. Angina usually results from myocardial oxygen deprivation secondary to atherosclerosis of the coronary arteries. anorexia Loss of appetite. anorexia nervosa An eating disorder, most common among adolescent girls, that ischaracterized by an aversion to eating, a morbid fear of becoming obese despite significant weight loss, a disturbed body image that results in a feeling of being fat even when extremely thin, and amenorrhea (in females). antagonist 1. In pharmacology: a drug that nullifies the action of another drug. 2. In anatomy: a muscle whose effects counteract the effects of another muscle. 3. In dentistry, a tooth that meets another in the opposite jaw during chewing or clenching of the teeth. anteroposterior-to-lateral Direction referring from front to back and side to side. anticholinergic 1. Of or relating to blockade of the impulses of parasympathetic or other cholinergic nerve fibers. 2. Any agent with anticholinergic properties. anticipatory guidance Information about a disorder or about the normal growth and development expectations of a specific age-group given at an appropriate time before an event in order to provide the client with support and strategies for dealing with potential problems before they occur. antiembolism stockings Elasticized stockings prescribed for some postoperative or bedridden clients to enhance venous blood flow from the lower extremities and thus prevent thromboembolism resulting from pooling of blood in the veins and dilation of veins. antisocial personality disorder A disorder that manifests after age 15 as a pervasive disregard for and violation of the rights of others. anuria Absence of urine production. aortic stenosis An abnormal narrowing of the orifice of the aortic valve, which prevents normal flow of blood from the left ventricle into the aorta. The constriction may result from a congenital malformation or pathologic fusion of the valve cusps. Aortic stenosis causes decreased cardiac output and pulmonary vascular congestion. Apgar score A numerical evaluation of a neonate's condition in which a rating of 0, 1, or 2 is assigned to each of five criteria: heart rate, respiratory effort, muscle tone, reflex responses, and skin color. The five scores are then combined: A score of 7 to 10 is considered normal, 4 to 7 indicates moderate distress, and 3 or less indicates acute distress. The Apgar score is usually obtained at 1 minute and 5 minutes after birth. aphasiaLoss or impairment of the ability to communicate through speech, written language, or signs, resulting from brain disease or trauma. aphthous stomatitis A recurring disease of unknown cause marked by the eruption of ulcers on the mucous membranes of the mouth. Also called canker sore. appendicitis Inflammation of the vermiform appendix. When acute, appendicitis commonly necessitates an appendectomy to prevent perforation of the appendix and subsequent peritonitis. apraxia Complete or partial inability to perform purposeful movements in the absence of sensory or motor impairment. asepsis The absence of living, disease-producing organisms. Medical asepsis refers to the removal or destruction of disease organisms or infected material. Surgical asepsis refers to protection against infection before, during, or after surgery by means of sterile technique. asthma A respiratory disorder characterized by recurrent attacks of paroxysmal dyspnea, bronchospasm, wheezing on expiration, and coughing. Conditions that may trigger an asthma attack include inhalation of allergens or pollutants, vigorous exercise, emotional stress, and infection. ataxia Impairment of the ability to coordinate voluntary muscle movement. atopic dermatitis A skin inflammation occurring in individuals with a genetic predisposition to allergies, characterized by intense itching, maculopapular lesions, and excoriation (rash pattern varies with age but usually occurs on the face). audiometry Evaluation of hearing using an audiometer. Various audiometric tests identify the lowest intensity of sound at which a client can perceive an auditory stimulus, hear different frequencies, and differentiate speech sounds. Pure tone audiometry evaluates the ability to hear frequencies, usually ranging from 125 to 8,000 Hz, and can determine whether a hearing loss results from a problem in the middle ear, inner ear, or auditory nerve. auditory hallucinations Perceptual experiences occurring in the absence of actual external sensory stimuli (for example, hearing voices telling one to do something). auscultatory gap Absence of Korotkoff sounds between phases I (onset of faint, clear tapping sound that gradually intensifies) and II (onset of swishing-like sound) while obtaining a blood pressure reading.Austin Flint murmur A mid-diastolic aortic regurgitation murmur usually heard best using the bell of the stethoscope over the mitral area. It’s a low-pitched, rumbling murmur. autograft The surgical transfer of tissue (commonly skin) from one location of the body to another location in the same individual. autoimmune disorder A disorder resulting from an inappropriate immune response that is directed against the self. Antigens normally found in the internal cells stimulate the development of antibodies; these antibodies can’t distinguish antigens of the internal cells from external antigens and act against the internal cells to cause various reactions. autoimmunity A condition in which the immune system mounts an attack against the individual's own body tissues. One theory proposes that autoimmunity reflects an inability of the immune system to distinguish between autoantigens and foreign substances, caused by some change in the cellular components of the immune system. Autoimmunity may lead to hypersensitivity and autoimmune disease. autonomic dysreflexia Reaction that may occur in clients with spinal cord injury above T6. Dysreflexia results in profuse diaphoresis, pounding headache, blurred vision, and dramatically elevated blood pressure. This life-threatening reaction may occur even from seemingly minor stimuli, such as lying on a wrinkled sheet or having a full bladder. autosomal recessive disorder Genetic disorder involving two expressed abnormal autosomal genes (not expressed in the parents) in which the individual affected receives one copy of the altered gene from each parent; thus the individual is homozygous for that trait. bacterial meningitis Inflammation of the meninges of the brain and spinal cord caused by bacteria such as Neisseria meningitidis, Haemophilus influenzae, Streptococcus pneumoniae, or Escherichia coli. Battle's sign Discoloration of the skin behind the ear after the fracture of a bone in the lower skull. bipolar disorder A mood disorder characterized by major depression and full manic episodes. body surface area Means for calculating the amount of drug to be given to a client (typically a child) using a nomogram or for estimating the extent of a burnborderline personality disorder A disorder characterized by unstable relationships, potentially self-damaging impulsiveness, difficulty in controlling anger, recurrent suicidal threats, and chronic feelings of boredom and emptiness. bradyarrhythmias Irregularity in heart rate or rhythm characterized by slowness. bradycardia A slow but steady heartbeat at a rate of less than 60 beats per minute. Bradycardia is normal during sleep and in well-conditioned athletes. In other circumstances, it may indicate an abnormal condition, such as brain tumor or digitalis toxicity. Braxton Hicks contraction Light, painless, irregular uterine tightening during pregnancy, arising during the first trimester and increasing in frequency, duration, and intensity by the third trimester. Also called false labor. Strong Braxton Hicks contractions occurring near term may be mistaken for true labor. breast engorgement Distention of the milk ducts and surrounding tissue as breast milk is formed, causing the breasts to become fuller, larger, and firmer. bronchiolitis A lung inflammation that usually begins in the terminal bronchioles, occurring mainly in infants and debilitated persons. Also called bronchopneumonia. Commonly, bronchiolitis results from upper respiratory infection, specific infectious fevers, and other debilitating diseases. bronchoscopy Visual examination of the tracheobronchial tree using a bronchoscope. Broviac catheter Single-lumen silicone central venous catheter used for long-term venous access. Brudzinski's sign Flexion of the hips and knees in response to passive flexion of the neck; signals meningeal irritation. bruit An abnormal vascular "swishing" sound heard on auscultation as a result of turbulent blood flow through dilated, irregular, torturous, or stenotic vessels. buccal Of or relating to the inside of the cheek; may also refer to a tooth surface or the gum next to the cheek. bulimia An eating disorder characterized by episodes of binge eating that may end in self-induced vomiting, alternating with periods of normal eating or fasting. Depression and awareness of the abnormal behavior are part of this illness.cardiac catheterization A diagnostic procedure in which a cardiac catheter is inserted into a large vein (usually of an arm or leg) and then threaded through the vein to the client's heart. cardiac output The volume of blood ejected by the heart per minute (normally ranging from 4 to 8 L). Cardiac output equals the stroke volume (the difference between end-diastolic volume and end-systolic volume) multiplied by the heart rate. cardiogenic shock A condition of low cardiac output that results from heart pump failure, such as in acute myocardial infarction, heart failure, or severe cardiomyopathy. cardiomyopathy Primary noninflammatory disease of the myocardium. catatonic A stuporous or unresponsive state commonly characterized by an inability to move or talk. catecholamine Any of a group of compounds having a sympathomimetic action and composed of a catechol molecule and the aliphatic portion of an amine. Some catecholamines are produced by the body and function as key neurologic chemicals. Others are synthesized as drugs for use in the treatment of such disorders as asthma, shock, and heart failure. cauda equina The aggregation of spinal roots, resembling the tail of a horse, that descend from the first lumbar vertebrae and occupy the vertebral canal below the cord. celiac disease A chronic disease in which an individual can’t tolerate foods containing gluten or wheat protein. Signs and symptoms include abdominal distention, vomiting, diarrhea, muscle wasting, and extreme lethargy. cellulitis An infection of deep subcutaneous tissue and sometimes muscle that may be associated with infection of an operative or traumatic wound. Cellulitis is characterized by local heat, pain, redness, and swelling. cerebral aneurysm A saclike dilation of the wall of a cerebral artery, typically resulting from weakness of the wall. A cerebral, or berry, aneurysm usually occurs in the circle of Willis and is prone to rupture. cerebral contusion A bruising of the brain tissue as a result of a severe blow to the head. A contusion disrupts normal nerve function in the bruised area and may cause loss of consciousness, hemorrhage, edema, and even death.cerebral palsy A permanent disorder of motor function resulting from nonprogressive brain damage or a brain lesion. Cerebral palsy usually appears before age 3. chelation therapy Administration of agents that bind to metals; administered to aid in the removal of excess metals, such as lead or iron in the body. chemotherapy Treatment of a disease using chemicals that exert a toxic effect on the pathogen or abnormal cell growth. chest physiotherapy An array of physical techniques, including postural drainage, chest percussion and vibration, and coughing and deep-breathing maneuvers. Chest physiotherapy is used to loosen and help eliminate lung secretions, reexpand lung tissue, and promote optimal use of respiratory muscles. cholelithiasis The presence or formation of gallstones in the gallbladder. cholinergic 1. Of or relating to nerve fibers that are stimulated to free acetylcholine at a synapse. 2. An agent that frees acetylcholine. chronic bronchitis A persistent respiratory disease marked by increased production of mucus by the glands of the trachea and bronchi. This common disease is characterized by a cough (with expectoration) at least 3 months of the year for more than 2 consecutive years. Chvostek's sign A spasm of the facial muscles elicited by light taps on the facial nerve. This spasm signals tetany and is seen in clients with hypocalcemia. circumcised Involving the removal of the foreskin of the penis. circumferential Area encircling or concerning the periphery of an object or body part. cirrhosis A chronic, degenerative liver disease in which the lobes are covered with fibrous tissue, the liver parenchyma degenerates, and the lobules are infiltrated with fat. clarification Communication technique used to help the client identify inconsistencies in his statements. clinical depression Syndrome characterized by persistent sadness and dysphoria accompanied by disturbances in sleep and appetite, lethargy, and an inability to experiencepleasure. clubfoot A congenital foot deformity in which the foot is twisted out of shape or position. cognitive development Ability to learn from experience, gain and maintain knowledge, respond to new situations, and solve problems. colonoscopy Examination of the colon using a flexible endoscope to visualize internal body areas or to remove tissue samples or small growths. communicable disease A disease that may be transmitted directly or indirectly from one person to another. compartment syndrome A neurovascular complication commonly associated with fractures of the limb; constricting or occlusive dressings, sutures, or casts; poor positioning; and any injury causing ischemia, swelling, or bleeding into the tissues that ultimately can lead to permanent dysfunction and deformity. It’s characterized by increasing limb pain unrelieved by analgesics, pallid or dusky skin color changes, absent pulse or edema distal to the injury site, decreased active and passive muscle movement distal to the injury site, pain with passive muscle stretching, and sensory changes. compliance 1. Adherence to a therapeutic regimen. 2. A tissue's or organ's ability to yield to pressure without disruption, commonly used to describe the distensibility of an air- or fluid-filled organ. compulsion A ritualistic, repetitive, and involuntary defensive behavior. concussion A violent shock or jarring, such as from an explosion or a blow. Concussion of the brain is characterized by loss of consciousness. Severe concussion may also cause impairment of brain stem functions. congenital hip dislocation Improper formation and function of the hip socket, commonly involving subluxation (where the femoral head is high in the acetabulum) or dislocation (where the femoral head is above the acetabulum). consolidation Solidification of the lungs that occurs with pneumonia. contracture Abnormal flexion and fixation of a joint, possibly permanent, which is typically caused by muscle wasting and atrophy or by loss of normal skin elasticity such as from extensive scar tissue.controlled substance Any substance that is strictly regulated or outlawed because of its potential for abuse or addiction. conversion disorder A disorder in which the client attempts to resolve a psychological conflict through the loss of a specific physical function -- for example, by paralysis, blindness, or inability to swallow. Corrigan's pulse Short, forceful, bounding pulse typically associated with aortic insufficiency. couvade The experience of physical symptoms associated with pregnancy, such as nausea, vomiting, and backache, by the husband of a pregnant woman; the response often results from stress, anxiety, and empathy for the pregnant woman. crackles Short, explosive or popping sounds usually heard during inspiration. They may be coarse (loud and low in pitch) or fine (less intense and high in pitch) and resemble the sounds heard when rolling hair between the fingers near the ear. Crohn's disease A chronic inflammatory bowel disease of unknown cause, usually involving the terminal ileum, with scarring and thickening of the bowel wall. Signs and symptoms include frequent episodes of diarrhea, severe abdominal pain, nausea, fever, chills, anorexia, and weight loss. croup An acute viral infection of the respiratory tract that causes acute upper airway obstruction. Characterized by stridor, a barking cough, and hoarseness, it primarily affects infants and young children ages 3 months to 3 years and follows an upper respiratory tract infection. crowning Appearance of the presenting part of the fetus at the perineum and seen when the vulva are separated. crystalloid fluid Clear solutions (usually in reference to I.V. solutions) containing electrolytes and water. Cushing's syndrome A metabolic disorder caused by chronic, excessive production of adrenocortical hormones or by prolonged high-dose glucocorticoid therapy. It’s characterized by such signs and symptoms as hypertension, diabetes mellitus, dusky complexion with purple striae, muscle wasting, weakness, and sudden development of fat around the face, neck, and trunk. cyanosisBluish discoloration of the skin and mucous membranes resulting from an excessive amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule such as in methemoglobin. cyanotic Referring to the bluish or bluish black discoloration of the skin and mucous membranes that results from excessive concentration of unoxygenated hemoglobin in the blood. cystic fibrosis An inherited disorder of the exocrine glands that affects multiple organ systems, causing such conditions as chronic pulmonary disease, pancreatic deficiency, sweat gland dysfunction, malabsorption, and liver obstruction. cystoscopy Direct visualization of the urinary tract by inserting a cystoscope in the urethra. debridement Removal of dead or damaged tissue or foreign material from a wound to prevent the growth of microorganisms and further damage and to promote healing. deceleration A drop in baseline fetal heart rate as indicated by the fetal monitor. Early deceleration is a drop in fetal heart rate that coincides with uterine contraction. Variable deceleration is a drop in fetal heart rate that doesn't occur at a consistent point during contractions. Prolonged deceleration is a drop in fetal heart rate that occurs for an extended period of time. deep vein thrombosis A condition involving the development of a blood clot in the deep veins of the pelvis, groin, or legs that disrupts venous blood flow and leads to swelling and edema. dehiscence The partial or complete separation of a wound's edges. dehydrated Having insufficient water in the body or tissues. delusions False ideas or beliefs accepted as real by the client. delusions of grandeur Distorted or false idea or belief that one has exceptional powers, wealth, skill, influence, or destiny. Denver Developmental Screening Test An assessment tool used to evaluate the development of a child in four categories: personal social, fine motor-adaptive, language, and gross motor skills.dependent personality disorder A disorder that begins in early adulthood and is characterized by an excessive need to be taken care of that leads to submissive and clinging behavior and fear of separation. depolarization Neutralization of electrical polarity; reversal of the resting potential in excitable cell membranes when stimulated. An example is the reduction of the ion differential of sodium and potassium across the nerve cells at the neuromuscular junction. diabetes insipidus A metabolic disorder marked by extreme polyuria and polydipsia and resulting from deficient secretion or production of antidiuretic hormone (ADH) or inability of the renal tubules to respond to ADH. (Rarely, excessive water intake causes signs and symptoms.) The condition may be acquired (secondary to disease or drug therapy), inherited, idiopathic, or nephrogenic. diabetes mellitus A chronic disorder of carbohydrate metabolism characterized by hyperglycemia and glycosuria resulting from inadequate production or utilization of insulin. diabetic ketoacidosis An acute, life-threatening form of metabolic acidosis that may arise as a complication of uncontrolled diabetes mellitus. Accumulation of ketone bodies leads to urinary loss of water, potassium, ammonium, and sodium, resulting in hypovolemia, electrolyte imbalances, an extremely high blood glucose level and, commonly, coma. Signs and symptoms include flushed, hot, dry skin; confusion; nausea; diaphoresis; restlessness; and fruity breath odor. dislocated Displacement of any body part, primarily a bone from its normal position in a joint. disseminated intravascular coagulation (DIC) A life-threatening disorder of excessive clot formation caused by overstimulation of the body's clotting and anticlotting processes in response to disease or injury. Such overstimulation is followed by a deficiency in clotting factors with hypocoagulability and hemorrhaging. diuretic 1. Tending to increase the formation and excretion of urine. 2. An agent that promotes the formation and excretion of urine. diverticulitis Inflammation of one or more diverticula, or saclike herniations, in the muscular layer of the colon. diverticulosis The presence of saclike herniations through the muscular layer of the colon without accompanying inflammation. Most clients with this condition havefew signs or symptoms except for occasional rectal bleeding. drip factor An indication of the number of drops needed to obtain one milliliter of solution delivered by a manufacturer's I.V. tubing based on the drop size. dumping syndrome A condition of nausea, weakness, profuse sweating, and dizziness occurring in clients who have had a subtotal gastrectomy. Signs and symptoms arise soon after eating when the contents of the stomach empty too rapidly into the duodenum. Also called postgastrectomy syndrome. Eating small, frequent, high-protein, high-calorie meals may help prevent discomfort and ensure adequate nutrition. dysphagia Difficulty swallowing, commonly resulting from obstructive or motor disorders of the esophagus. Obstructive disorders, such as an esophageal tumor or lower esophageal ring, interfere with the ability to swallow solids; motor disturbances such as achalasia impair swallowing of solids and liquids. dyspnea Shortness of breath, difficulty breathing, or labored breathing resulting from certain heart conditions, anxiety, or strenuous exercise. dystonic reaction Severe tonic contractions of the muscles in the neck, mouth, and tongue; dystonic reaction is a common adverse reaction to antipsychotic drugs. dysuria Painful or difficult urination, which is usually caused by a bacterial infection or an obstruction in the urinary tract. echolalia Parrotlike and inappropriate repetition of another's words. ectopic pregnancy Implantation of the fertilized ovum outside the uterine cavity. Types of ectopic pregnancy are abdominal pregnancy, interstitial pregnancy, and tubal pregnancy. effacement Shortening of the vaginal portion of the cervix and thinning of its walls during labor due to stretching and dilation caused by the fetus. Full effacement obliterates the constrictive neck of the uterus. The extent of effacement is expressed as a percentage of full effacement. elbow restraints Type of restrictive device attached to the client's body at the elbow to restrict movement or access to another body part; may be applied after cleft palate repair to reduce the risk of injury to the suture line. electrocardiogram interpretation Analysis of the waveforms seen on an electrocardiogramelectroconvulsive therapy (ECT) The induction of a brief seizure and loss of consciousness by applying a lowvoltage alternating current to the brain through scalp electrodes. ECT is used in the treatment of affective disorders (primarily acute depression), especially in clients resistant to psychoactive drugs. On awakening, the client has no memory of the shock. electromyogram (EMG) A record of the electrical activity of skeletal muscles, obtained by surface electrodes or needle electrodes and devices that amplify, transmit, and record the signals. The technique is helpful in diagnosing neuromuscular disorders, pinpointing motor nerve lesions, and measuring electrical potentials induced by voluntary muscle contraction. electromyography Diagnostic test that records the electrical activity of selected skeletal muscle groups at rest and during voluntary contraction. It involves percutaneous insertion of a needle electrode into a muscle with measurement of the muscle's electrical discharge through an oscilloscope. endocarditis An abnormal condition of the endocardium and heart valves marked by vegetations on the valves and endocardium. It may occur as a primary disorder or arise in association with another disease. endotracheal intubation Passage of a wide-bore tube through the mouth or nose into the trachea. It may be used to maintain a patent airway, administer anesthesia, aspirate secretions, prevent aspiration of foreign material into the tracheobronchial tree of an unconscious or paralyzed person, or administer positive pressure ventilation that can’t be given effectively by a mask. enteral Referring to administration by mouth, rectum, or directly into the intestinal system. enteral feedings Delivery of nutrients directly into the GI tract through a feeding tube. enteric precautions A category-specific type of infection precautions established by the Centers for Disease Control and Prevention involving infections transmitted by intestinal secretions. These have since been replaced with standard precautions and transmission-based precautions. enuresis Involuntary passage or release of urine after the age when bladder control would have been normally achieved. epiglottis The lidlike, cartilaginous structure that overhangs the larynx and prevents food from entering the larynx and trachea during swallowing.epiglottitis Inflammation of the epiglottis. Acute epiglottitis, a severe form of the condition that primarily affects children, causes stridor, fever, sore throat, croupy cough, and a reddened, swollen epiglottis. epilepsy A group of neurologic disorders marked by uncontrolled electrical discharge from the cerebral cortex and typically manifested by seizures with clouding of consciousness. Epilepsy is most commonly of unknown cause (idiopathic) but is sometimes associated with head trauma, intracranial infection, brain tumor, vascular disturbances, intoxication, or chemical imbalance. episiotomy Surgical incision into the perineum to enlarge the vaginal opening for delivery. It’s performed to prevent traumatic tearing of the perineum, to hasten or promote delivery, or to prevent stretching of perineal muscles and connective tissue. Erikson Psychosocial development theorist who described eight developmental stages across the life span, each of which is characterized by a conflict between two opposing forces. erythroblastosis fetalis Hemolytic anemia of the neonate caused by placental transmission of maternally formed antibodies against the incompatible antigens of fetal blood. It results from maternal-fetal blood group incompatibility, specifically involving the rhesus (Rh) factor and the ABO blood groups, and is characterized by accelerated destruction of red blood cells and resulting jaundice. In Rh factor incompatibility, the hemolytic reaction appears only when the mother is Rh-negative and the infant is Rh-positive. Isoimmunization rarely occurs with the first pregnancy, but the risk increases with each succeeding pregnancy. eschar A thick scab or dry crust that appears after a thermal or chemical burn. esophageal atresia A congenital anomaly involving closure of the esophagus at some point, often ending in a blind pouch. evaporation The change of a liquid to a vapor at a temperature below the boiling point of the liquid. Evaporation occurs at the surface of the liquid, hastened by an increase in temperature and a decrease in atmospheric pressure. evisceration 1. Pushing out or removal of the viscera, especially through a surgical incision. 2. In ophthalmology: excision of the contents of the eyeball (except the sclera). exacerbationAn increase in the seriousness of a disease or disorder or in its signs and symptoms. extrapyramidal 1. Describing the tissues and structures of the brain located outside the pyramidal tract and not running through the medullary pyramid -- excluding the motor neurons, motor cortex, and corticospinal and corticobulbar tracts. 2. Of or relating to the function of these tissues and structures. extravasation Escape, usually of blood, lymph, or I.V. solution, from a vessel into surrounding tissues. failure to thrive Condition in which an infant's height and weight fall below the third percentile on a standard growth chart; also called reactive attachment disorder. fantasy play Type of play involving imaginary playmates typically associated with preschoolers. febrile seizure Typically, a tonic-clonic seizure of relatively short duration (usually less than 1 minute) occurring with an acute illness and fever. fifth disease A contagious, relatively benign disease caused by the Parvovirus B19; most commonly occurs in children ages 2 to 12 and is characterized by a red rash on the cheeks. Also called erythema infectiosum. fontanel A soft spot, such as the spaces covered by tough membranes remaining between the bones of an infant's skull. full-term Pregnancy that has continued for a period of 38 to 42 weeks. fundus The base of an organ; the portion of a hollow organ farthest from its mouth, such as the fundus of the uterus. gastritis Inflammation of the stomach and stomach lining. gastroenteritis Inflammation of the lining of the stomach and intestines that accompanies numerous GI disorders; characterized by anorexia, weakness, abdominal pain, nausea, and diarrhea. gastrostomy Opening created into the stomach. gestational diabetesThe development of diabetes during pregnancy, usually during the second trimester. gestational trophoblastic disease Failure of an embryo to develop beyond a primitive state due to proliferation and degeneration of the trophoblastic villi becoming filled with fluid and appearing as grape-sized vesicles Also called a hydatidiform mole, molar pregnancy. glaucoma A group of eye diseases characterized by abnormally elevated pressure within the eye due to obstruction of the outflow of aqueous humor. glomerular filtration rate Rate at which the glomeruli in the kidneys filter blood (normally, 125 ml/minute). glomerulonephritis Inflammation of the glomeruli in the kidneys. gout A group of disorders associated with inborn errors of metabolism that affect purine and pyrimidine use; results in increased production of uric acid or interferes with its excretion. Manifested by hyperuricemia, recurrent acute inflammatory arthritis, deposition of urate crystals in the joints of the extremities, and uric acid urolithiasis. Graham Steell's murmur A pulmonary regurgitation murmur resulting from pulmonary hypertension; usually loud with a blowing quality and variable in duration, it’s heard best along the left sternal border over the third and fourth intercostal spaces. granulation tissue Tissue that develops during collagen production; capillaries form as budlike structures from nearby vessels, penetrating the wound, growing into loops, and providing a nutritional source for the newly generated tissue; the loops give the tissue a "granular" appearance. Graves' disease A disorder of the thyroid gland characterized by pronounced thyrotoxicosis usually associated with an enlarged thyroid gland, exophthalmos, or pretibial myxedema. gravida A pregnant woman. gynecomastia Enlargement and development of the mammary glands in men, usually temporary and benign. hallucinations Sensory perceptions that don't result from external stimuli and that occur during wakefulness.health care power of attorney A legal document in which an individual designates another person, called an "attorney-in-fact," to act on the individual's behalf if the principal person becomes disabled or incapacitated. The document becomes void when the principal person dies or recovers. heart failure Inability of the heart to pump an adequate amount of blood to the tissues. hemarthrosis Bleeding into a joint cavity. hematuria The presence of blood in the urine. hemicolectomy Surgical removal of one-half of the colon. hemiparesis Paralysis on one side of the body or a part of it that indicates an injury to the motor area of the brain. hemiplegia Paralysis of one side of the body. hemogram Written recording of the blood count differential. hemolytic reaction Type of blood transfusion reaction occurring when the donor's blood is incompatible with the recipient's blood; the most serious type of transfusion reaction. hemophilia A bleeding disorder characterized by a failure of the blood clotting mechanism. It’s an inherited condition occurring almost exclusively in males. hemoptysis The coughing or spitting up of blood caused by hemorrhage in the lungs or bronchi. Minor amounts of blood may appear in the sputum of individuals with bronchitis or upper respiratory tract infections. hepatic encephalopathy A serious complication of liver failure affecting a client's neurologic status; believed to result from the accumulation of toxins, such as ammonia, in the blood. hepatojugular reflux Distention of the neck veins when manual pressure is applied over the right upper quadrant of the abdomen; it suggests heart failure. hepatomegaly Enlargement of the liver.heterozygous Having two different genes at corresponding loci on homologous chromosomes. hiatal hernia Protrusion of part of the stomach through the esophageal opening in the diaphragm. homonymous hemianopia Blindness or visual deficit in one-half of the field of vision of both eyes. Either the right halves or the left halves of each eye are affected. hopelessness State of severe despair associated with feelings of inadequacy and isolation, an inability to act on one's behalf, and a belief that the situation is highly unlikely to improve. hospice A system of family-centered care using a multidisciplinary approach designed to assist the chronically ill person to maintain a satisfactory lifestyle through the terminal phases of dying. human immunodeficiency virus (HIV) A retrovirus identified as the primary cause of acquired immunodeficiency syndrome (AIDS). hydatidiform mole A usually benign neoplasm that occurs at the end of a degenerating pregnancy and arises from enlarged chorionic villi and the proliferation of trophoblastic tissue. hydramnios Presence of an excess volume of amniotic fluid during pregnancy. hydrotherapy Treatment involving the use of water, such as tub or shower baths and whirlpools. hyperemesis gravidarum Severe and prolonged vomiting during pregnancy to such a degree that weight loss and an imbalance of fluids and electrolytes occur. hyperphosphatemia Elevated serum level of phosphorus above 2.6 mEq/L or 4.5 mg/dl. hypersomnolence Excessive sleepiness. hyperthermia A severe elevation in body temperature. hyperthyroidism Disorder involving overproduction of thyroid hormone, leading to a metabolicimbalance. hypertonic 1. A solution that has greater osmotic pressure compared to another solution; a fluid in which cells shrink. 2. In reference to muscles or arteries, having a greater than normal degree of tension. hypertrophic cardiomyopathy Primary disease of the cardiac muscle characterized by disproportionate, asymmetrical thickening of the interventricular septum, particularly in the anterior-superior region. Also called idiopathic hypertrophic subaortic stenosis. hyperventilate To increase the rate or depth of one's inspirations or expirations, or both; may occur with anxiety. hypochondriasis Preoccupation with the fear that one has a serious illness despite medical reassurance to the contrary; fear interferes with psychosocial functioning. hypoglycemia Low serum glucose levels. hypospadias A congenital abnormality in males in which the urethral opening is on the underside, rather than at the tip, of the penis; in females, the defect is manifested by a urethral opening into the vagina. hypotonic 1. A solution that has a decreased osmotic pressure compared to another solution; a fluid in which cells swell. 2. In reference to muscles or arteries, having a less than normal degree of tension. hypoxia A decreased level of oxygen in inspired air. iatrogenic Introduced inadvertently by a medical practitioner or resulting from a diagnostic procedure or treatment. impetigo A contagious, inflammatory skin infection that usually occurs on the face. Characterized by the appearance of small, itchy blisters that rupture and form a crusty scab; usually caused by streptococcal or staphylococcal bacteria or a combination of both types of organisms. incentive spirometer A device that requires the client to deep breathe, hold the breath for approximately 3 seconds, and then exhale in an effort to expand the lungs. incompatibility Unsuitability for combination, often due to antagonistic action.induration Area of hardened tissue. infection The invasion and multiplication of pathogenic organisms within the body. informed consent Permission obtained from a client to perform a specific test or procedure after the client has been fully informed about the test or procedure. intelligence quotient (IQ) Measurement of a person's ability to comprehend relationships, think, problem solve, and adjust to new situations; usually expressed as a score and based on standardized intelligence tests. intermittent claudication Pain that occurs with activity or exercise but that is relieved with rest. This pain results from the body's inability to supply arterial blood (blood rich in nutrients) to the tissues that experience an increase in demand during exercise or activity. interpretation The deep analysis of the meaning and significance of what a client is saying and doing in an effort to gain insight into his behavior. intertrigo Dermatitis that occurs at moist, warm sites where skin surfaces rub together, such as the armpits, the inner surfaces of the thighs, and between the buttocks; caused by an overgrowth of normal flora. intra-aortic balloon pump A device consisting of a balloon attached to a catheter that is introduced into the descending thoracic aorta through the femoral artery. Alternating inflation (during diastole) and deflation (during systole) of the balloon alters resistance to aortic blood flow and both decrease the heart's workload and increase the supply of blood to the coronary arteries. intracranial pressure Pressure exerted by the brain tissue, cerebrospinal fluid, and blood. intradermal injection Injection of any substance into the skin between the dermis and epidermis. The technique is typically used to produce a local drug effect (such as in local anesthesia for procedures such as suturing wounds) or during allergy testing. Also called intracutaneous injection. intraosseous infusion Administration of fluid, blood, or drugs into the bone marrow cavity of a long bone; typically used in children for emergency situations when I.V. access is difficult or unavailable. intussusception Telescoping or invagination of a portion of the bowel into an adjacent portion;most commonly seen in infants. iron deficiency anemia Anemia characterized by an insufficient amount of iron in the serum, decreased stores of iron in the bone marrow, and elevated serum ironbinding. irritability Excitability or excessive responsiveness to a stimulus. isotonic Of or relating to a solution that has the same osmotic pressure as another solution; a solution in which cells neither swell nor shrink. juvenile hypothyroidism A condition involving a deficiency of thyroid hormone secretion in children. Kawasaki disease A febrile, multisystem disorder affecting the small to medium-size vessels, primarily of the lymph nodes, most commonly in children before puberty; usually follows exposure to an infection. Also called mucocutaneous lymph node syndrome. Kegel exercises Exercises involving alternate contraction and relaxation performed to strengthen the perineal muscles. kernicterus A neurologic syndrome resulting from deposition of unconjugated bilirubin in the brain cells and characterized by severe neural symptoms. Kernig's sign Elicitation of resistance and hamstring muscle pain when the examiner attempts to extend the knee while the hip and knee are both flexed 90 degrees. Kussmaul's respirations Abnormally deep, gasping type of respirations resulting from air hunger; associated with severe diabetic acidosis and coma. laminectomy Surgical removal of the bony arches of one or more vertebrae; performed to relieve spinal cord compression or to remove a displaced intervertebral disk. lead poisoning Poisoning caused by the ingestion or absorption of lead or one of its salts. Signs and symptoms include loss of appetite and weight, anemia, constipation, insomnia, headache, dizziness, irritability, a blue line at the margin of the gums, and peripheral neuropathy. lethargy A feeling or condition of sluggishness, apathy, or inactivity.lipodystrophy Any disturbance in fat metabolism. living will A witnessed document indicating a client's desire to be allowed to die a natural death rather than be kept alive by heroic, life-sustaining measures. The will applies to decisions that will be made after a terminally ill client is incompetent and has no reasonable possibility of recovery. lochia The vaginal discharge present during the first several weeks after delivery. lochia alba A creamy white, brown, or colorless discharge consisting mainly of serum and white blood cells; typically stops flowing at about 6 weeks postpartum. lochia rubra Present during the first 3 to 4 postpartal days; it’s bloody and may contain mucus, tissue, debris, and small clots. lochia serosa A pink or brownish discharge persisting for 5 to 7 days postpartum. Logan bar Apparatus used to protect the surgical incision after cleft lip repair. Logan bow A wire U-shaped apparatus taped to both cheeks of an infant or toddler following cleft lip repair to protect the surgical site. lumbar puncture Fluid withdrawal from the subarachnoid space of the lumbar region of the spinal canal, usually between the third and fourth lumbar vertebrae, for diagnostic or therapeutic purposes. Also called spinal tap. lymphangiography A diagnostic radiographic evaluation of lymphatic system filling after injection of a contrast medium into a lymphatic vessel of each foot or hand. lymphedema Edema of an arm or leg caused by the buildup of interstitial fluid as a result of lymphatic inflammation or obstruction or a lymph node disorder. mammogram A radiograph of the breast; used for diagnostic purposes. mammography Radiography of the mammary gland to identify benign and malignant neoplastic processes. mastectomy The surgical resection of a breast; usually performed to remove a malignant tumor.mastitis Inflammation of the mammary gland; usually caused by streptococcal or staphylococcal infection and infrequent breast-feeding. meconium A dark, greenish black material that occurs in the intestines of a fetus that forms the first stools of a neonate. The fluid is thick and sticky and is composed of intestinal gland secretions, some amniotic fluid, and intrauterine debris. megaloblastic anemia A hematologic disorder that is characterized by the production and peripheral proliferation of megaloblasts. Ménière's disease A labyrinthine dysfunction that produces severe vertigo, sensorineural hearing loss, and tinnitus. metabolic acidosis A condition resulting from excessive accumulation of acid or depletion of bicarbonate. metabolic alkalosis A clinical state marked by decreased amounts of acid or increased amounts of base bicarbonate. milieu A therapeutic environment, typically used as part of inpatient psychiatric therapy. mitral stenosis Obstruction of blood flow from the left atrium to the left ventricle due to thickening and contracting of the mitral valve leaflets; consequently, left atrial volume and pressure rise and the chamber dilates. Greater resistance to blood flow causes pulmonary hypertension, right ventricular hypertrophy, and right-sided heart failure. muscular dystrophy A group of degenerative genetic diseases characterized by weakness and the progressive atrophy of skeletal muscles with no evidence of nervous system involvement. myalgia Diffuse muscle pain or tenderness associated with many infectious diseases. myasthenia gravis An abnormal muscle weakness and fatigability, especially in the muscles of the face and throat, resulting from a defect in the conduction of nerve impulses at the myoneural junction. mycoplasmal pneumonia A contagious respiratory disease caused by Mycoplasma pneumoniae, characterized by a sore throat, dry cough, fever, malaise, and myalgia.myeloma Osteolytic neoplasm consisting of a protrusion of cells typical of the bone marrow. myelomeningocele The protrusion of a hernial sac containing a portion of the spinal cord, its meninges, and cerebrospinal fluid through a congenital defect in the vertebral column. myxedema A disorder that results from hypofunction of the thyroid. Signs and symptoms include enlarged tongue, slowed speech, moon face, drowsiness, cold intolerance, hair loss, and anemia. myxedema coma A rare, serious form of hypothyroidism that usually results from lack of treatment or mistreatment, severe stress (from infection, exposure to cold, or trauma), or the use of sedatives or anesthetics in a client being treated for hypothyroidism. nebulizer A device that employs a baffle to produce a fine aerosol spray consisting of particles less than 30 micrometers in diameter. necrotizing enterocolitis GI disorder commonly associated with premature infants and characterized by diffuse or patchy intestinal necrosis and sometimes accompanied by sepsis. negative nitrogen balance Increased rate of protein breakdown when compared to protein synthesis; nitrogen excretion that exceeds nitrogen intake. neglect A form of abuse involving the failure to protect a person from injury or meet the person's physical, emotional, or medical needs. nephrectomy The surgical removal of a kidney, usually done to remove a tumor, drain an abscess, or treat hydronephrosis. nephrotic syndrome A clinical classification including all kidney diseases characterized by marked proteinuria, hypoalbuminemia, and edema. neurotransmitter Any one of a group of substances that act on a target nerve cell to excite or inhibit transmission of nerve impulses; substances include norepinephrine, acetylcholine, and dopamine. nystagmus Involuntary, rapid movements of the eyeball that may be horizontal, rotatory, vertical, or mixed.obsessive-compulsive disorder A disorder characterized by obsessive thoughts and compulsive behaviors that represent recurring efforts to control overwhelming anxiety, guilt, or unacceptable impulses that persistently enter the consciousness. oliguria A diminished flow of urine in relation to fluid intake; usually less than 400 ml in 24 hours. Also called hypouresis. ophthalmia neonatorum Eye infection occurring at birth or in the first month; most commonly caused by gonorrhea or chlamydia. opioids Opium-derived or synthetically produced drugs that alter pain perception, induce mental changes, promote deep sleep, depress respirations, constrict pupils, and decrease GI motility. orthostatic hypotension Abnormally low blood pressure that occurs when a person stands up. Also called postural hypotension. osmolality The concentration or osmotic pressure of a solution; expressed in osmoles of solute per kilogram of solvent. osmolarity The osmotic pressure of a solution expressed in osmoles of solute per liter of solution. osteomalacia Delayed or poor mineralization of bone; the adult equivalent of rickets. This condition is associated with anorexia, fracture, pain, weakness, and weight loss. osteomyelitis Inflammation of bone that results from a local or general infection of bone and bone marrow. The bacterial infection is caused by trauma or surgery, by direct extension from a nearby infection, or by introduction from the bloodstream. osteoporosis A disorder in which bone mass is reduced and fractures occur after minimal trauma. It occurs most commonly in postmenopausal women, sedentary or immobilized individuals, and persons on long-term steroid or heparin therapy. otorrhea A discharge from the ear, which may be serous, sanguineous, or purulent if the external or middle ear is infected. ototoxicity Harmful effect on the function of the eighth cranial nerve or hearing organs; most commonly associated with prescribed drugs.Paget's disease A common bone disease that usually affects middle-aged and elderly people. It’s marked by inflammation of the bones, softening and thickening of the bones, excessive bone destruction, and unorganized bone repair; the result is bowing of the long bones. The cause is unknown. palilalia Repetition of words or phrases with increasing rapidity. pancreatitis Acute or chronic inflammation of the pancreas. paralysis An abnormal condition characterized by the loss or impairment of motor function or the impairment of sensory function. paralytic ileus A decrease in or absence of bowel motility that may occur following abdominal surgery or may be caused by numerous other conditions, most commonly by peritonitis. paranoid schizophrenia Disorder involving disordered thinking with delusional thought content characterized by preoccupation with delusions or auditory hallucinations, lack of organized speech, disorganized or catatonic behavior, or flat or inappropriate affect. paraplegia An abnormal condition characterized by the loss of sensation and motor function in the lower limbs, which may result in either complete or incomplete paralysis. parenteral Not in or through the digestive system, but rather by injection through some other route, such as subcutaneously, I.V., I.M., or intradermally. paresthesia Abnormal or heightened touch sensations, such as burning, numbness, prickling, and tingling, that commonly occur without external stimulus. perceptions Awareness of objects and the ability to differentiate between them. percutaneous transluminal coronary angioplasty (PTCA) A technique to open stenosed atherosclerotic arteries. A balloon catheter is inserted through the skin and into the vessel to the site of narrowing; the balloon is inflated, thus flattening the plaque against the arterial walls. pericarditis Inflammation of the pericardium; may be caused by trauma, neoplasm, infection, uremia, myocardial infarction, or collagen disease. perineum1. The pelvic floor and its associated structures; located between the symphysis pubis and the coccyx and on the sides by the ischial tuberosities. 2. The body area between the thighs; bounded by the anus and scrotum in males and by the anus and vulva in females. peristaltic waves Alternating involuntary contraction and relaxation of the smooth muscle fibers of a structure in a wavelike fashion to propel the contents forward; commonly associated with the GI tract. peritoneal dialysis A procedure performed to remove toxins, drugs, or other wastes normally excreted by the kidney; transfers these substances across the peritoneum by intermittently introducing and removing a dialysate from the peritoneal cavity. peritonitis An inflammation of the peritoneum; can be produced by bacteria or irritating substances introduced into the abdominal cavity by a penetrating wound or perforation of an organ. pernicious anemia A megaloblastic anemia characterized by decreased gastric production of hydrochloric acid from the parietal cells of the stomach essential for vitamin B12 absorption; results in vitamin B12 deficiency. phagocytosis The process by which cells engulf and digest solid substances, such as microorganisms and cell debris. phenylketonuria (PKU) An inborn metabolic disorder caused by absence or deficiency of phenylalanine hydroxylase, the enzyme responsible for the conversion of phenylalanine to tyrosine; results in accumulation of phenylalanine and its metabolites, causing mental retardation and other neurologic problems, light pigmentation, eczema, and a distinctive mousy odor. pheochromocytoma A chromaffin-cell tumor of the adrenal medulla that secretes an excessive amount of the catecholamines epinephrine and norepinephrine, which results in severe hypertension, increased metabolism, and hyperglycemia. phototherapy The treatment of disease by the use of light, especially ultraviolet light or other concentrated rays; used to treat acne, psoriasis, and hyperbilirubinemia. pituitary dwarfism A condition characterized by a deficiency in secretion of the growth hormone from the anterior pituitary gland. placenta accretaAbnormal adherence of the placenta to the uterine wall. placenta previa Implantation of the placenta so that it adjoins or covers the internal os of the uterine cervix. The most common symptom is painless hemorrhage in the last trimester. pneumonia An acute infection of the lung parenchyma that commonly impairs gas exchange. pneumothorax A collection of air in the pleural space; may result from an open chest wound that permits the entrance of air or from the rupture of a vesicle on the surface of the lung. Common types of pneumothorax are open, closed, and tension. polydipsia Chronic, excessive thirst. polymyositis The simultaneous inflammation of a number of voluntary muscles. polyneuritis Degeneration of peripheral nerves primarily supplying the distal muscles of the extremities. It results in muscle weakness, with sensory loss and atrophy, and decreased or absent deep tendon reflexes. polyphagia Voracious or excessive eating before becoming satiated. polyuria The excessive excretion of urine from the kidneys. postterm neonate A neonate born after the onset of the 43rd week of pregnancy. preeclampsia An abnormal condition characterized by the development of hypertension during pregnancy, accompanied by edema or proteinuria, usually after the 20th week of gestation. pressure ulcer Localized area of skin breakdown occurring secondary to prolonged pressure. Necrotic tissue develops because the vascular supply to the area is diminished. preterm neonate A neonate born before the beginning of the 38th week of pregnancy. primigravid A woman who is pregnant for the first time.Prinzmetal's angina A variant of angina pectoris, a form of unstable angina, in which the attacks occur during rest. Attacks are indicated by an ST-segment elevation on an electrocardiogram. productive cough A mechanism by which the body clears the airway passages of secretions that normal mucociliary action doesn't remove; usually sudden, forceful, noisy expulsion of air from the lungs that contains sputum or blood (or both). projection False attribution of one's unacceptable feelings, impulses, or thoughts onto another. pruritus Itching; an unpleasant sensation that leads to rubbing or scratching the skin in an effort to obtain relief. Scratching the skin may lead to secondary infection. pseudoparkinsonism The development of a Parkinson-like disorder (neuromuscular disorder involving progressive muscle rigidity, akinesia, and involuntary tremors) due to psychotropic drug therapy. puerperal 1. Of or pertaining to the period from the end of childbirth until involution of the uterus is complete (usually 3 to 6 weeks). 2. Of or pertaining to a woman (puerpera) who has just given birth to an infant. pulmonary edema An abnormal condition in which extravascular fluid is accumulated in lung tissues and alveoli. pulse pressure The numeric difference between the systolic and diastolic pressures, usually 30 to 40 mm Hg. purulent Containing or forming pus. pyelonephritis Inflammation of the kidney and its pelvis. pyuria The presence of pus in the urine, commonly a sign of urinary tract infection. quickening The first notable fetal movement in utero, usually occurring at 16 to 20 weeks' gestation. radical mastectomy Surgical removal of an entire breast, pectoral muscles, axillary lymph nodes, and all fat, fascia, and adjacent tissues; usually used in the treatment ofbreast cancer. reaction formation Substitution of behavior, thoughts, or feelings that are completely opposed to one's own unacceptable behavior, thoughts, or feelings. rectal route Use of the rectum to administer medication reflection A technique in which the listener interprets the feelings of the client and repeats them back to the client; encourages the client to clarify his feelings. repolarization Part of the cardiac conduction cycle in which the cell returns to its resting state, a more negatively charged state. Calcium ions move into the cell and potassium ions move out, followed by the extrusion of sodium and calcium ions from the cell and the restoration of potassium ions into the cell by the sodium potassium pump. respiratory acidosis Caused by reduced alveolar ventilation; is marked by increased partial pressure of arterial carbon dioxide, excess carbonic acid, and increased plasma hydrogen-ion concentration. Hypoventilation inhibits the excretion of carbon dioxide, which consequently produces excessive carbonic acid and thus lowers blood pH. respiratory alkalosis Caused by both respiratory and nonrespiratory factors, this condition is marked by decreased partial pressure of arterial carbon dioxide, decreased hydrogen-ion concentration, and increased blood pH. Extreme anxiety can precipitate hyperventilation associated with respiratory alkalosis. resuscitation A method used to support a client's breathing and circulation until the body can do so on its own or the client is mechanically supported. It involves maintaining an open airway, providing artificial ventilation through rescue breathing, and promoting artificial circulation through external cardiac compression. Reye's syndrome Acute encephalopathy and fatty infiltration of the internal organs following acute viral infections, such as influenza B, chickenpox (varicella), the enteroviruses, and the Epstein-Barr virus; has also been associated in children with administration of aspirin and other salicylates. Rh incompatibility In hematology: two blood groups that are antigenically different and, therefore, aren't compatible because one group lacks the Rh factor. rheumatic fever An inflammatory disease sometimes occurring if group A beta-hemolyticstreptococcal infection is inadequately treated. rheumatoid arthritis A chronic, systemic collagen disease marked by inflammation, stiffness, and pain in the joints and related structures that result in crippling deformities. ritodrine therapy A prescribed treatment that uses the beta-receptor agonist ritodrine to halt preterm labor. Romberg’s sign A swaying (or falling) when a person stands with feet together and eyes closed. It’s an indication that the person has lost a sense of position. Also called rombergism. rooting reflex A response in neonates to the cheek being touched or stroked. The infant turns the head toward the stimulated side and begins to suck. The reflex usually disappears by 3 to 4 months of age. Russell traction An orthopedic device that combines suspension and traction to align and immobilize the legs; used to treat diseases of the hip and knee and fractured femurs as well as hip and knee contractures. scabies A contagious skin disease caused by the itch mite, Sarcoptes scabiei. schizotypal personality disorder A disorder characterized by acute discomfort with and reduced capacity for close relationships and by cognitive or perceptual distortions and eccentricities of behavior, beginning in early adulthood. scoliosis An appreciable lateral curvature of the spine resulting from numerous causes, including congenital malformations of the spine, muscle paralysis, poliomyelitis, sciatica, and unequal leg length. sensorineural hearing loss Hearing loss caused by a defect or lesion of the inner ear or the acoustic nerve resulting in a distortion of sound that makes discrimination difficult. sensory perceptions Awareness of one's surroundings through the use of vision, hearing, taste, touch, and smell. serosanguineous Of a discharge containing both serum and blood. shock An abnormal physiologic state characterized by reduced cardiac output, circulatory insufficiency, tachycardia, hypotension, restlessness, pallor, and diminished urinary output. Shock may be caused by a variety of conditions,including trauma, infection, hemorrhage, poisoning, myocardial infarction, and dehydration. sickle cell anemia A chronic and incurable hereditary disorder occurring in people homozygous for hemoglobin S (Hb S). The presence of Hb S results in distortion and fragility of erythrocytes. sickle cell crisis Episode of widespread cellular sickling in which the client's red blood cells containing hemoglobin S are exposed to conditions in which oxygen supply to the cells is decreased. This leads to cellular contraction and piling within the cell, altering the shape of the red blood cells (sickling). These sickled cells become rigid and clump together to form clusters, ultimately obstructing capillary blood flow and causing tissue ischemia. simple fracture An uncomplicated, closed bone fracture in which the skin isn't broken. skin turgor Skin characteristic determined by pinching a small area of skin on the medial arm or anterior chest and noting how quickly it returns to its position when released. somatoform pain Development of the symptom of pain as a result of psychological stress. spinal shock Loss of autonomic reflex, motor, and sensory activity below the level of a lesion. Signs of spinal shock include flaccid paralysis, loss of deep tendon and perianal reflexes, and loss of motor and sensory function. standard precautions Infection control guidelines established by the Centers for Disease Control and Prevention requiring all health care personnel to use gloves, gowns, and goggles to prevent contact with a client's blood or body fluids and to adhere to strict safety measures when handling needles, scalpels, and other sharp instruments. status asthmaticus A severe and prolonged asthma attack in which bronchospasm fails to respond to oral medication, sometimes resulting in hypoxia, cyanosis, and unconsciousness. Stokes-Adams attack Episode of confusion and light-headedness accompanying syncope with or without seizures due to inadequate cerebral perfusion secondary to heart block. stoma 1. A minute pore, orifice, or surface opening. 2. An artificial, surgically created opening of an internal organ on the body surface, such as for acolostomy or tracheostomy. 3. A new opening surgically created between two structures, such as for a gastroenterostomy or pancreaticogastrostomy. stomatitis An inflammation of the mouth that may result from bacterial, viral, or fungal infection; exposure to chemicals or drugs; vitamin deficiency; or a systemic inflammatory disease. stridor A high-pitched respiratory sound, usually heard during inspiration, caused by an obstruction of the trachea or larynx. stroke A condition of sudden onset in which a cerebral blood vessel is occluded by an embolus or cerebrovascular hemorrhage. The resulting ischemia of brain tissue that is normally perfused by the affected vessel may lead to permanent neurologic damage. subdural hematoma A condition involving the collection of blood between the dura mater and the brain. sublingual Under the tongue. sudden infant death syndrome (SIDS) The sudden, unexpected, and inexplicable death of an infant who appears to be healthy. It occurs during sleep, typically in infants between the ages of 3 weeks and 5 months. Also called crib death. supratentorial Located above the tentorium of the brain. suspension A liquid that contains solid particles that aren't dissolved; stirring or shaking the liquid maintains the dispersal. sympathomimetics Group of drugs that mimic the effects of impulses conveyed by adrenergic postganglionic fibers of the sympathetic nervous system. synchronized cardioversion Delivery of an electrical shock to the client in conjunction with the R wave on his ECG, just as the heart muscle contracts. Delivery is timed to avoid the T wave because an electrical discharge at this time may cause ventricular fibrillation. synergistic effect Administration of two drugs producing the same qualitative effect together to produce a greater response than either drug alone. systemic lupus erythematosus (SLE) A chronic inflammatory multisystemic disorder of connective tissue,characterized principally by involvement of the skin, joints, kidneys, and serosal membranes. tachycardia A condition characterized by a regular but accelerated action of the heart, usually l00 to 150 beats per minute. tactile fremitus Vibration in the chest wall that can be felt when a hand is applied to the thorax while the patient is speaking. It's most commonly due to consolidation of a lung or a part of a lung but may also be caused by congestion, inflammation, or infection. tardive dyskinesia A neurological syndrome marked by slow, rhythmical, automatic movements that occur as an adverse effect of extended phenothiazine use. tension pneumothorax A condition in which air enters the pleural space through a tear in lung tissue but can't exit through the same vent, thereby trapping air in the pleural space with each inspiration and producing positive pleural pressure. This in turn causes the ipsilateral lung to collapse. tenting An indication of decreased skin turgor, as exhibited by a fold of skin remaining or holding in the pinched position after being released. teratogenic Causing harm to the developing fetus. tetany Hyperexcitability of nerves and muscles as a result of a lessened concentration of extracellular ionized calcium; symptoms include convulsions, muscle twitching and cramps, and sharp flexion of the wrist and ankle joints. tetralogy of Fallot A combination of congenital cardiac defects consisting of pulmonic stenosis, interventricular septal defect, dextroposition of the aorta so that it overrides the interventricular septum and receives venous as well as arterial blood, and right ventricular hypertrophy. thrombocytopenia A reduction in the number of blood platelets; usually caused by destruction of erythroid tissue in bone marrow. The condition may be a result of neoplastic disease or an immune response to a drug. thrombophlebitis Inflammation of a vein, often involving clot formation. Common causes include chemical irritation, blood hypercoagulability, immobilization, infection, postoperative venous stasis, prolonged sitting or standing, trauma to the vessel wall, or a long period of I.V. catheterization. tonic-clonic seizureParoxysmal, uncontrolled discharge of central nervous system neurons extending to the entire brain and characterized by stiffening (tonic phase) and then rapid synchronous muscle jerking and hyperventilation (clonic phase). Also called a major or grand mal seizure. tonsillectomy The surgical removal of the palatine tonsils. total parenteral nutrition (TPN) The administration of total caloric needs in a nutritionally adequate solution of glucose, protein hydrolysates, minerals, and vitamins through a catheter inserted into the superior vena cava. tracheoesophageal fistula Abnormal opening between the esophagus and trachea that may lead to aspiration. tracheostomy The surgical creation of an opening through the neck into the trachea; used to relieve upper airway obstruction and aid breathing. traction 1. The action of pulling a part of the body along the long axis. 2. In orthopedics: the act of exerting force through a system of weights and pulleys to align, immobilize, or relieve pressure in a limb, bone, or group of muscles. transdermal Method or route of topical drug administration; provides continuous drug delivery through the skin to achieve a constant, steady blood concentration level. transsphenoidal adenohypophysectomy Surgery involving the pituitary gland, most commonly performed to remove a pituitary tumor. The physician enters from the inner aspect of the upper lip through the sphenoid sinus. transsphenoidal hypophysectomy Microsurgery in which an incision is made at the junction of the gums and upper lip. A surgical microscope is advanced and a special surgical instrument is used to excise all or part of the pituitary gland. Trendelenburg's position Position in which the client's head is lower than the trunk; typically, the body and legs are elevated on an incline. Trousseau's sign An assessment technique for evaluating neuromuscular irritability (tetany) associated with hypocalcemia. When Trousseau's sign is positive, the client develops a carpopedal spasm (adducted thumb, flexed wrist and metacarpophalangeal joints, and extended interphalangeal joints) after a blood pressure cuff is applied to the client's upper arm and inflated to apressure above systolic pressure for approximately 1 to 4 minutes. tuberculosis An acute or chronic infection from exposure to Mycobacterium tuberculosis or another strain of mycobacteria characterized by pulmonary infiltrates and formation of granulomas with caseation, fibrosis, and cavitation. type 1 diabetes An endocrine disorder involving disturbances in carbohydrate, protein, and fat metabolism, usually occurring before age 30 and requiring the use of exogenous insulin and dietary management. Also called insulin-dependent diabetes mellitus. type 2 diabetes An endocrine disorder involving disturbances in carbohydrate, protein, and fat metabolism; characterized by insulin resistance with varying degrees of insulin secretory defects. May be treated with diet, exercise, and oral antidiabetic agents. Exogenous insulin is sometimes necessary. type 2 herpes simplex A type of herpes simplex virus transmitted primarily through contact with genital secretions and affecting the genital structures. ulcerative colitis A chronic, recurrent ulceration of the colon of unknown cause in which there is abdominal cramping, rectal bleeding, and diarrhea containing blood, pus, and mucus. urinary incontinence Inability to prevent urine discharge. urinary tract infection (UTI) A bacterial infection, most commonly caused by Escherichia coli or a species of Klebsiella, Proteus, Pseudomonas, or Enterobacter, affecting one or more parts of the urinary tract. urticaria A vascular reaction caused by dilation and increased permeability of the capillaries. Symptoms include the development of transient wheals with pale centers and well-defined erythematous margins. variability Differing rhythmicity or changes in condition; often used to describe fetal heart rate reflected on the fetal heart rate tracing as a slight irregularity or jitteriness. vaso-occlusive crisis The most common type of sickle cell crisis resulting from blood vessel obstruction by rigid, tangled sickle cells leading to tissue anoxia and possibly necrosis. Also called a painful crisis or infarctive crisis. vastus lateralis The largest of the four muscles that make up the quadriceps femoris; locatedon the outside of the thigh, extending from the hip joint to the common quadriceps tendon and inserted in the patella; extends the leg. venography A radiographic test using a contrast medium to identify thrombi or obstruction in the veins of the lower extremities or the kidneys. ventricular septal defect (VSD) An abnormal opening in the septum separating the ventricles, usually resulting from failure of the fetal interventricular foramen to close; results in blood flow from the left ventricle to the right ventricle and recirculation of blood through the pulmonary artery and lungs. ventricular tachycardia A life-threatening arrhythmia that occurs when the ventricles produce several premature ventricular contractions in succession; usually due to a problem with the heart's conduction system and increased myocardial contractility. vertigo A sensation of movement in which the client feels himself revolving in space (subjective vertigo) or his surroundings revolving about him (objective vertigo); may result from diseases of the inner ear or from disturbances of the vestibular pathways in the central nervous system. vesicle 1. Any small anatomic sac that contains liquid. 2. A small blister that contains clear fluid. wet-to-dry dressings Type of wound covering (dressing) in which gauze moistened with normal saline is applied wet to the wound and removed once the gauze becomes dry and adheres to the wound bed; used for debridement. Wilms' tumor A rapidly growing malignant kidney tumor that occurs most commonly in children younger than age 5, although it sometimes develops before birth. Rare cases occur later in life. Also called adenomyosarcoma. X-linked recessive disorders Genetic disorders in which the abnormal gene exists on the X chromosome; only males exhibit clinical signs of the disorder because they have no offsetting X chromosome. Z-track An I.M. injection technique in which the client's skin is pulled in such a way that the needle track is sealed off after the injection. The technique is done to minimize subcutaneous irritation and discoloration.Comprehensive HESI Exit and Subject Exam Flashcards Question Answer Hint Blood functions: transports nutrients, O2, hormones & enzymes to tissues, carries CO2 and waste products away from tissues, helps regulate temp, fluid electrolytes & pH, protects body from bacteria and foreign substances, coagulates to prevent excess fluid loss What is total blood volume? Volume of blood present in the circulatory system (arteries, veins, capillaries) Total blood volume is approximately.... 4-5 L in females 5-6 L in males Normal pH range is... 7.35-7.45 (arterial blood) Whole blood refers to... the formed elements and plasma (Blood as a whole) What kind of tissue is blood classified as... Connective tissue (Blood consists of cells and cell fragments surrounded by a liquid intercellular matrix) Cellular elements comprise ____% of the blood volume? 45% Plasma comprises ___% of the blood volume 55% Approximately 95% of the volume of the formed elements consists of..... red blood cells Cell fragments are called.... platelets Approximately 5% of the volume of the formed elements consists of.... WBC and platelets The formed elements account for ____% to ___% of the total blood volume in females. (AKA Hematocrit) 38% to 48% The formed elements account for ____% to ___% of the total blood volume in males. (AKA Hematocrit) 44% to 54% The % of total blood volume composed of formed elements in the blood sample is the... Hematocrit Red Blood Cells or RBC functions: transport O2 and CO2 throughout body White Blood cells or WBC functions... body's defense against microorganisms and foreign material. Platelets are essential for... preventing blood loss (hemostasis) In a healthy person, only _______ blood cells are found in blood circulation. mature In persons with disease states, immature and abnormal cells may be present. What is plasma? Is a viscous (sticky) pale yellow colloidal fluidaccounting for slightly more than half the total blood volume. What is plasma made of? 92% water and 8% dissolved or proteins such as albumin, globulins and fibrinogen, salts, nutrients, gases, waster products, hormones and enzymes. Plasma without the proteins that clot blood is called.... serum How does water enter plasma? from digestive tract, interstitial fluids and as a by-product of metabolism. How does water leave plasma? Kidneys, lungs, intestinal tract and skin Where do the solutes come from in the plasma? liver, kidneys, intestines, endocrine glands and immune tissues such as the spleen. What are other terms for circulatory system? vascular space or vascular system. Blood or fluid within the vascular system is referred to as.... intravascular Blood or fluid outside the vascular system is referred to as.... extravascular What is the interstitial space? the space surrounding the cells outside the vascular system. The exchange of nutrients, gases, hormones, waste products takes place between blood and tissues occurs where? at the capillary level (the walls are one cell thick) (microvasculature) The process by which nutrients and other substance cross the capillary wall is called.... diffusion How does the lymphatic system differ from the circulatory system? It is not a closed loop system. What does the lymphatic system do? 1.)picks up fluids and large complex substances that have left the circulatory system and entered the tissues 2.)returns them to the vascular system (helps maintain normal blood volume) What do lymph nodes do? filter lymphatic vessels What are two large lymph vessels? the thoracic duct on the left side of body the right lymphatic duct on the right side What do the thoracic duct and right lymphatic duct do? empty into veins in the upper chest and return fluid to the vascular system. What would happen to a person if fluid remains in the interstital space? would develop a balloon-like appearance. Their blood volume is depleted (fluid lost from their circulation) Vascular system includes both: peripheral and cardiopulmonary systems Peripheral system refers to... circulatory system but not thecardiopulmonary system What are the major veins in the body? superior vena cava (receives blood from head and upper part of body) inferior vena cava (blood from lower part of body) Both vessels enter the Right atrium of the heart. (RA) Cardiopulmonary system refers to.... heart and lungs as they function together. Blood going into right atrium from both vena cavae is.... deoxygenated From the right atrium, blood is pumped to the right ventricle through which valve? tricuspid From the right ventricle (RV), deoxygenated blood is pumped out through which valve? pulmonary blood goes to pulmonary arteries to go to lungs What happens in the aveolar capillary newtwork in the lungs? O2 and CO2 are exchanged. (CO2 is the waste product of cellular metabolism) Where does the oxygenated blood go from the lungs? through pulmonary veins to the left atrium (LA)of the heart. Where does blood go from left atrium (LA)? pumped into the left ventricle (LV) through the mitral or biscuspid valve. Where does blood go from left ventricle (LV))? ejected through aortic valve to the aorta. What is Alkaline Phosphatase (ALP)? enzyme produced mainly in liver, bone, intestine, kidney & placenta. What does Alkaline Phosphatase (ALP)test? differentiates between liver and bone disorders when other enzyme tests are done (ALP isoenzymes 1 & 2, GGTP and/or 5'N) ALP isoenzyme, ALP1 is of what origin? liver ALP isoenzyme, ALP2 is of what origin? bone What could a decreased ALP level mean? alkaline phosphatase hypothyroidism, malnutrition, scurvy, hypophosphatasia, pernicious anemia, placental insufficiency What drugs may decrease alkaline phosphatase (ALP)values? flouride, oxalate, propranolol (Inderal) What could an increased ALP level mean? alkaline phosphatase obstructive biliary disease (juandice), cancer of the liver, hepatocellular cirrhosis, hepatitis, leukemia, cancer of the bone, breast or prostate, Paget's disease (osteitis deformans) healing fx, multiple myeloma, osteomalacia, GI ulcerative dx, late pregnancy, hyperthyroidism, hyperparathyroidsim, rheumatoid arthritis, CHF What drugs may increase alkaline ABX, cochicine, methyldopa(Aldomet),phosphatase (ALP)values? allopurinol, phenothiazines, indomethacin (Indocin) procainamide, some oral contraceptives, tolbutamine, INH (isoniazid) and IV albumin Procedure for ALP test? Collect 5-10ml of venous blood in red-top tube. No food or fluid restrictions are required. Withhold drugs that may elevate ALP for 8-24 hrs w/Dr's permission. List client's age & drugs that may affect results on lab slip. Nursing implications for ALP test: Know factors that can elevate serum ALP levels (drugs, IV albumin), age of client, late pregnancy to 3 weeks postpartum, blood drawn 2-4 hrs after fatty meal. record info on lab slip. inform pt that other enzyme tests may be ordered to verify dx, assess for s/s of liver dx or bone dx. Normal ALP levels for adult 20-90 U/L at 30 C, 24-97 U/L at 37 C, 2-4 U/dL, 4-13 U/dL elderly-slightly higher What is amylase? enzyme that is derived from the pancreas, salivary gland and liver. increases in acute pancreatitis. Normal ALP levels for child: 0-12 yr = 40-300 U/L 13-18 yr = 30-165 U/L What cause increase amylase levels? acute pancreatitis (can be 2X normal at peak at 20-30 hrs and returns to normal in 2-4 days), abdominal surgery involving gallbladder and stomach What are the two major types of amylase isoenzymes and what do they relate to? P-type, occur more frequently in acute pancreatitis. elevated S-type can be d/t ovarian and bronchogenic tumors. Why is the urine amylase helpful to know? determines the significance of a normal or slightly elevated serum amylase, esp when pt has sxs of pancreatitis. Urine amylase can remain elevated up to 2 wks after acute pancreatitis. What are normal serum levels of amylase? adult - 60-160 Somogyi U/dL pregnancy: slightly increased child: usually not done elderly: could be slightly higher than adult What are normal lvels of serum amylase isoenzymes? S (salivary) type 45-70% P (pancreatic) type 30- 55% What is normal urine amylase level? adult: 4-37 U/L2h What can a decreased level of amylase indicate? IV D/W, advanced chronic pancreatitis, acute and subacute necrosis of the liver, chronic alcoholism, toxic hepatitis, severe burns, severe thyrotoxicosis What drugs can decrease amylase glucose, citrates, flourides, oxalatesvalues? What can an elevated level of amylase indicate? acute pancreatitis, chronic pancreatitis (acute onset), partial gastrectomy, peptic ulcer perforation, obstruction of pancreatic duct, acute cholecystitis, CA of pancreas, DKA, DM, acute alcoholic intoxication, mumps, RF, BPH, burns, pregnancy What drugs may increase amylase value? narcotics, ethyl alcohol (large amts) ACTH, guanethidine, thiazide diuretics, salicylates, tetracycline What is the ANA test? is a screening test for diagnosing systemic lupus erythematosis (SLE) and other collagen diseases. Scleroderma, RA, cirrhosis, leukemia, infectious mononucleosis and malignancy. What is reference value for ANA test? Adult: negative What is an elevated level of ANA? >1:20 What drugs may increase ANA value? abx, HTN meds, methyldopa (Aldomet) isoniazide (INH) diuretics, thiazides, phenytoin (Dilantin) oral contraceptives, antiarrhythmics Why are arterial blood gases (ABGs) assessed? to assess disturbances of acid-base balance caused by a respiratory disorder or a metabolic disorder or both. a pH of less than 7.35 indicates.... acidosis a pH greater than 7.45 indicates.... alkalosis a decreased pH (<7.35) and an elevated PaCO2 (>45) indicates... respiratory acidosis An elevated pH (>7.45) and a decreased PaCO2 (<35) indicates.... respiratory alkalosis To determine whether an acid-base imbalance has a metabolic cause, you should look at... bicarbonate (HCO3) A decreased pH (<7.35) and a decreased HCO3 (<24) indicates... metabolic acidosis An elevated pH (>pH 7.45) and an elevated HCO3 (>28> indicates.... metabolic alkalosis Adult ABG reference values... pH 7.35-7.45 PaCO2 35-45 PaO2 75-100 HCO3 24-28 BE +2 to -2 (base excess) Child ABG reference values... pH 7.36-7.44 PaCO2 35-45 PaO2 75-100 HCO3 24-28 BE +2 to -2 (base excess) What can cause respiratory acidosis? (pH <7.35, PaCO2 >45) COPD, (emphysema, chronic bronchitis, severe asthma)ARDS, Guillian-Barre syndrome, anesthesis, pneumonia What can cause metabolic acidosis? (pH <7.35, HCO3 <24) DKA, severe diarrhea, starvation/malnutrition, kidney failure, burns, shock, acure myocardial infarctionWhat drugs may cause a low pH? narcotics, barbiturates What can cause respiratory alkalosis? (pH >7.45, PaCO2 <35) salicylate toxicity (early phase) anxiety, hysteria, tetany, strenuous exercise, (swimming, running) fever, hyperthyroidism, delirium tremens, PE What can cause metabolic alkalosis? (pH >7.45, HCO3 >28) severe vomiting, gastric suction, peptic ulcer, potassium loss (hypokalemia) excess administration of sodium bicarbonate, cystic fibrosis, hepatic failure. What drugs may cause an elevated pH? sodium bicarbonate, sodium oxalate, potassium oxalate What is bilirubin? is formed from the breakdown of hemoglobin by the reticuloendothelial sytem and is carried in the plasma to the liver where it is conjugated or unconjugated. If the total bilirubin (serum bilirubin) is within normal range, then what? direct and indirect bilirubin levels do not need to be analyzed. If total bilirubin elevated, look at direct bilirubin. If one value of bilirubin is reported, what does it represent? the total bilirubin Jaundice is frequently present when serum bilirubin (total) is greater than.... 3 mg/dL Remember to check sclera of the eyes and inner aspects of the arm for jaundice. Increased direct or conjugated bilirubin is usually the result of ... obstructive jaundice, either extrahepatic (from stones or tumor) or intrahepatic (damaged liver cells) Indirect or onconjugated bilirubin is associated with... increased destruction of RBCs (hemolysis) Adult Reference values for Bilirubin (Total, Direct, Indirect) serum: Total: 0.1-1.2 mg/dL Direct(conjugated): 0.0- 0.3 mg/dL Indirect (unconjugated):0.1-1.0 mg/dL Newborn Reference values for Bilirubin (Total) serum: Total: 1-12 mg/dL Child Reference values for Bilirubin (Total) serum: Total: 0.2-0.8 mg/dL What can cause a decreased direct bilirubin level? iron deficiency anemia What drugs may decrease bilirubin value? barbituates, ASA (in large amts), PCN, caffeine What can cause an increased direct bilirubin level? obstructive jaundice caused by stones or neoplasms, hepatits, cirrhosis of the liver, infectious mononucleosis, liver CA, Wilson's disease What can cause an increased indirect bilirubin level? erythroblastosis fatalis, sickle cell anemia, transfusion reaction, hemolytic anemias,pernicious anemia, malaria, septicemia, CHF, decompensated cirrhosis What drugs may increase bilirubin value: ABX, sulfonamides, diuretics, INH, valium, narcotics, barbiturates, Dalmane, Indocin, Aldomet, Pronestyl, steroids, oral contraceptives, orinase, vitamins A, C and K How do you figure out the indirect bilirubin? subtract the direct bilirubin from the total bilirubin. What should a nurse remember when drawing a bilirubin sample? Avoid hemolysis. Pt to be NPO except for water. List drugs pt is taking protect sample from sun and light. Blood should be sent asap to lab. Tell pt to NOT eat carrots or foods high in fat the night before test. What should a nurse remember when drawing ABGs? Collect blood in heparinized needle and syringe place syringe with arterial blood in an ice bag and deliver to lab asap. indicate on lab slip if pt is receiving O2 and what rate. apply pressure for 2-5 min. blood not to be drawn from same arm as IV No food or fluid restriction. What should a nurse remember when drawing an amylase test? restrict food for 1-2 hours before the blood sample is drawn. if pt ate or received a narcotic 2 hrs before test, may be invalid. What are 2 methods to test bleeding times? Ivy and Duke method Why are bleeding time tests done? to determine whether bleeding time is normal or prolonged. frequently done when pt has a hx of bleeding (easy bruising) familial bleeding or peroperative screening. Describe Ivy method: cleanse below the antecubital space w/alcohol and allow to dry. inflate BP cuff to 40mm Hg and leave inflated during test.puncure skin 2.5 mm deep. start timing on stopwatch. blot blood q 30 sec until bleeding stops. the time required for bleeding to stop is recorded. When should Ivy test method not be done? more popular than Duke method when pt is taking anticoagulants or ASA. Pt should stop these meds 3-7 days prior to test w/ Drs permission. ASA therapy will prolong bleeding time. Describe Duke method: earlobe is used. no food or fluid restriction. What can disorders can increase bleeding times (prolonged time)? thrombocytopenia (decreased platelet count <50,000), platelet function abnormality, vascular abnormalities, severe liver dx, disseminated intravascular coagulation (DIC) aplastic anemia, factor deficiencies (V, VII, XI)Christmas disease, hemophilia, leukemia What drugs may increase bleeding time? salicylates, (ASA, others) warfarin (Coumadin) dextran, streptokinase (fibrinolytic agent) What are adult reference values for Ivy method? 3-7 minutes What are adult reference values for Duke method? 1-3 minutes What is urea? Urea is an end product of protein metabolism. If both BUN and Creatinine levels are elevated, nurse should suspect what? kidney disease What should nurse do w/Dr's permission if pt's BUN is 26-35? Encourage fluids. serum calcium (Ca) normal range for Adults adult: 4.5-5.5 mEq/L, 9-11 mg.dL serum calcium (Ca) normal range: newborn, infant, child newborn: 3.7-7.0 mEq/L, 7.4-14.0 mg/dL Infant: 5.0-6.0 mEq/L, 10-12 mg/dL Child: 4.5- 5.8 mEq/L, 9-11.5 mg/dL what is total serum calcium? ionized and nonionized calcium level together. How does pH affect calcium ionization? acidosis-more Ca ionized alkalosis-most of Ca is bound to protein and cannot be ionized. What does a calcium deficit cause? tetany symptoms, unless acidosis is present What can a calcium excess cause? cardiac dysrhythmias What can a 24-urine specimen for calciuria determine? parathyroid disorders In hyperparathyroidism, hyperthyroidism and osteolytic disorders, the urinary calcium excretion is usually... increased. it is decreased in hypoparathyroidism. What can cause a decreased level of serum calcium? malabsorption of Ca from GI tract, lack of Ca & Vit D intake, hypoparathyroidism, CRF caused by PH retention, laxative abuse, extensive infections, burns, pancreatitis, alcoholism, diarrhea, pregnancy What drugs can decrease Ca value? cortisone preparations, ABX (gentamicin, methicillin), Mg products (antacids), excess laxatives, heparin ,insulin, mithramycin, acetazolamide (Diamox) What can cause elevated level of serum calcium? hyperPTH, malignant neoplasm of bone, lung, breast, bladder or kidney, hypervitaminosis Vit D, multiple myeloma, prolonged immobilization, multiple fx, renal calculi, exercise, milk-alkali syndrome What drugs can increase Ca value? thiazide diuretics, alkaline antacids, calcium salts, estrogen preparation, vit D What are sx of decreased level of Ca? tetany: muscular twitching and tremors,spasms of the larynx, parathesis, facial spasms and spasmodic contractions What is Chvostek's sign? a spasm of the facial muscles following a tap on one side of the face over the facial nerve. + in hypocalcemia What is Trousseau's sign? muscular spasm resulting from pressure applied to nerves and vessels of the upper arm such as inflating a BP cuff) + in hypocalcemia Why should nurse look for sx of tetany when pt receives massive transfusions of citrated blood? citrates prevent calcium ionization. serum calcium level may not be affected. What can occur if pt receives ca supplements and a digitalis preparation? digitalis toxicity (sx: N/V, anorexia, bradycardia) What should nurse do when giving IV fluids with 10% Ca gluconate? GIVE SLOWLY. Ca should be administered in D5/W and not in saline solution. Na promotes Ca loss. Why should Ca not be added to solutions containing bicarbonate? rapid precipitation will occur. What are sx of hypercalcemia? lethargy, HA, weakness, muscle flaccidity, heart block, anorexia, N/V What should nurse teach pt who is hypercalcemic? avoid high ca foods, be ambulatory when possible, and increase oral fluid intake. What should nurse promote if pt is bedridden? active and passive exercises. this will prevent ca loss from bone. What happens when pt is hypercalcemic and is taking a thiazide diuretic? thiazide diuretic inhibit ca excretion and promote hypercalcemia. What is normal Chloride serum level for adult? 95-105 mEq/L What is normal serum Chloride level for newborn, infant and child? newborn: 94-113 mEq/L infant: 95-110 mEq/L child: 98-105 mEq/L Where is chloride found, extracellular or intracellular? It is found in the extracellular fluid. What roles does chloride play? maintain body water balance, osmaolality of body fluids (with sodium), and acid-base balance. What causes decreased levels of chloride? vomiting, gastric suction, diarrhea, low serum K+ or Na (or both), Low Na diet, continuous IV D5/W, adrenal gland insufficiency, heat exhaustion, acute infections, burns, excess diaphoresis, metabolic alkalosis, chronic resp acidosis, CHF What drugs may decrease chloride value? thiazide and loop diuretics, bicarbonatesWhat causes increased levels of chloride? dehydration, high serum Na level, adrenal gland hyperfunction, multiple myeloma, head injury, eclampsia, cardiac decompensation, excessive IV saline (0.9% NaCl) kidney dysfunction What drugs may increase chloride level? ammonium chloride, cortisone preparations, ion exchange resins, acetazolamide (Diamox), prolonged use of triamterene (Dyrenium) What should nurse look for in hypochloremia? hyperexcitability of the nervous system and muscles, tetany, slow and shallow breathing, hypotension What should nurse tell Dr can happen with continuous IV D5/W? a chloride deficit can occur. What should nurse encourage the pt who is Cl deficient to do? drink fluids containing sodium and chloride (ex. broth, tomato juice) NO PLAIN WATER) What other labs should nurse look at if pt's Cl is decreased? serum K+ and Na levels. Cl is frequently lost with Na and K+. What are sx of overhydration when pt is receiving several L of normal saline for Na and Cl replacement? Na holds water. Sx of overhydration: constant, irritating cough, dyspnea, neck&hand vein engorgement, chest rales. What are sx of hyperchloremia? Sx similar to acidosis; weakness, lethargy and deep, rapid vigorous breathing What should nurse instruct pt to do if hyperchloremic? tell pt to avoid drinking or eating salting foods and to use a salt substitute. (avoid Ca chloride and K+ chloride substitutes) If pt is hyperchloremic, what IV fluid would be a concern? NS. Nurse should check for sx of overhydration. If pt is hyperchloremic, what could be monitored to determine fluid retention? daily weight and intake and output What is desirable serum Cholesterol level for adult? < 200 mg/dL What serum cholesterol level for adult is a risk? 200-240 mg/dL moderate risk >240 mg/dL What may happen to cholesterol levels during pregnancy? may go to high risk levels (>240 mg/dL) but returns to prepregnancy values 1 month after delivery. What are infant serum level of cholesterol? 90-130 mg/dL What are child (age 2-19 yr)serum level of cholesterol? normal and risky levels desirable level: 130-170 mg/dL moderate risk: 171-184 mg/dL high risk: > 184 mg/dL Why should nurse look for sx of tetany when pt receives massive transfusions of citrated blood? citrates prevent calcium ionization. serum calcium level may not be affected.What can occur if pt receives ca supplements and a digitalis preparation? digitalis toxicity (sx: N/V, anorexia, bradycardia) What should nurse do when giving IV fluids with 10% Ca gluconate? GIVE SLOWLY. Ca should be administered in D5/W and not in saline solution. Na promotes Ca loss. Why should Ca not be added to solutions containing bicarbonate? rapid precipitation will occur. What are sx of hypercalcemia? lethargy, HA, weakness, muscle flaccidity, heart block, anorexia, N/V What should nurse teach pt who is hypercalcemic? avoid high ca foods, be ambulatory when possible, and increase oral fluid intake. What should nurse promote if pt is bedridden? active and passive exercises. this will prevent ca loss from bone. What happens when pt is hypercalcemic and is taking a thiazide diuretic? thiazide diuretic inhibit ca excretion and promote hypercalcemia. What is normal Chloride serum level for adult? 95-105 mEq/L What is normal serum Chloride level for newborn, infant and child? newborn: 94-113 mEq/L infant: 95-110 mEq/L child: 98-105 mEq/L Where is chloride found, extracellular or intracellular? It is found in the extracellular fluid. What roles does chloride play? maintain body water balance, osmaolality of body fluids (with sodium), and acid-base balance. What causes decreased levels of chloride? vomiting, gastric suction, diarrhea, low serum K+ or Na (or both), Low Na diet, continuous IV D5/W, adrenal gland insufficiency, heat exhaustion, acute infections, burns, excess diaphoresis, metabolic alkalosis, chronic resp acidosis, CHF What drugs may decrease chloride value? thiazide and loop diuretics, bicarbonates What causes increased levels of chloride? dehydration, high serum Na level, adrenal gland hyperfunction, multiple myeloma, head injury, eclampsia, cardiac decompensation, excessive IV saline (0.9% NaCl) kidney dysfunction What drugs may increase chloride level? ammonium chloride, cortisone preparations, ion exchange resins, acetazolamide (Diamox) prolonged use of triamterene (Dyrenium) What s&s should nurse look for in hypochloremia? hyperexcitabillity of the nervous system and muscles, tetany slow and shallow breathing, hypotensionsWhy should nurse inform Dr when pt is receiving IV D5/W continuously? a chloride deficit could occur. what should nurse encourage to do with hypochloremia? drink fluids containing sodium and chloride (broth, tomato juice) NO PLAIN WATER! Why should nurse check serum potassium and sodium levels in pt that is hypochloremic? chloride is frequently lost with sodium and potassiu. What should nurse look for when pt is receiving several L of NS for sodium and chloride replacement? Sx of overhydration. Sodium holds water. Sx include: constant irritating cough, dyspnea, neck and hand vein engorgement, chest rales. What are s&s of hyperchloremia? similar to acidosis, (weakness, lethargy and deep, rapid, vigorous breathing) What should nurse instruct pt do when hyperchloremic? avoid drinking or eating salty foods and to use a salt substitute (avoid calcium chloride and potassium chloride substitutes) Why should nurse notify dr when pt receiving NS IV fluids and has an elevated serum chloride? NS increases chloride level more. check for overhydration. What should nurse do when pt hyperchloremic? Monitor daily weights and intake and output to determine whether fluid retention is present. What is desirable level for cholesterol in adults? <200 mg/dL What are risky levels for cholesterol in adults? moderate risk: 200-240 mg/dL high risk: >240 mg/dL What can happen to cholesterol levels in pregnancy? can be a high risk levels but returns to prepregnancy values 1 month after delivery. What are desirable cholesterol levels in infant? 90-130 mg/dL What are cholesterol levels in child (2- 19yr)? desirable: 130-170 mg/dL moderate risk: 171- 184 mg/dL High risk: >184 mg/dL What is cholesterol and where is it produced? blood lipid synthesized in liver. used by body to form bile salts for fat digestion and for formation of hormones by the adrenal glands, ovaries and testes. What hormones decrease the concentration of cholesterol? thyroid and estrogen What causes decreased level of serum cholesterol? hyperthyroidism, starvation, malabsorption What drugs may decrease cholesterol level? thyroxine, estrogens, ASA, ABX (tetracycline, neomycin) nicotinic acid, heparin, colchicine what causes increased level of serum cholesterol? hypercholesterolemia, atherosclerosis, hypothyroidism, AMI, uncontrolled DM, biliary cirrhosis, pancreatectomy, pregnancy (3rd sem) heavy stress periods, nephrotic syndrome, high cholesterol diet.What drugs may increase cholesterol level? oral contraceptives, vit A & D, phenothiazines, epinephrine, sulfonamides, phenytoin (Dilantin) What should nurse instruct pt with hyperchlesterolemia? decrease the intake of foods rich in cholesterol (i.e. bacon, eggs, fatty meats, seafood, chocolate and coconut) encourage weight loss. What is the Coombs' indirect (serum) antibody screen test? detects free circulating antibodies in the serum. checks for antibodies in recipients's and donor's serum prior to transfusions to avoid a reaction. does not identify specific antibodies. is part of cross-match blood test. When is the Coombs' indirect antibody screen test positive? (+1 TO +4) When incompatible cross-matched blood, specific antibody (previous transfusion) anti-Rh antibodies, acquired hemolytic anemia. What drugs may increase Coombs' indirect? ABX (cephalosporins (Keflin) PCN, tetracycline, streptomycin, amnopyrine (Pyradone) Dilantin, Thorazine, sulfonamides, antiarrhythmics, quinidine, pronestyl) L-dopa, Aldomet, INH, rifampin What result do we want with the Coombs' indirect antibody screen test? Negative in both adult and children What is the Coombs' direct antiglobulin test? detects antibodies other than the ABO group which will attach to RBCs. The RBCs are tested and if sensitized will agglutinate. When is the Coombs' direct antiblobulin test positive? (+1 to +4) when antibodies are present on RBCs. erythroblastosis fetalis, hemolytic anemia, transfusion hemolytic reactions, leukemias, SLE What drugs may increase the Coombs' direct test? ABX (cephalosporins (Keflin) PCN, tetracycline, streptomycin, amnopyrine (Pyradone) Dilantin, Thorazine, sulfonamides, antiarrhythmics, quinidine, pronestyl) L-dopa, Aldomet, INH, rifampin What are sx of blood transfusion reactions? chills, fever (slight temp elevation) rash What is CRP? (C-Reactive Protein) CRP appears in blood 6-10 Hrs after an acute inflammatory process or tissue destruction (necrosis), or both, peaks within 48-72 Hrs. is a non-specific test. What are reference values for CRP serum in adults and children? (CReactive Protein) Not usually present in both. >1:2 titer = positive When is CRP (C-Reactive Protein) elevated? during bacterial infections but not viral infections. RA, rheumatic fever, acutemyocaridal infarction (AMI) pyelonephritis, SLE, inflammatory bowel disease, CA with metastasis, late pregnancy, Burkitt's lymphoma What drugs may increase CRP value? (C-Reactive Protein) oral contraceptives If CRP positive, (C-Reactive Protein), what should nurse look for in pt? s&s of an acute inflammatory process (pain, swelling in joints, heat, redness, increased body temp) What is creatinine? a by-product of muscle catabolism, is derived from the breakdown of muscle creatine and creatine phosphate. amt of creatinine produced is proportional to muscle mass. kidneys excrete creatinine. When 50% or > nephrons destroyed, serum Cr level increases. evaluates glomerular function. What are normal reference values for adult serum and urine creatinine? serum: 0.5-1.5 mg/dL Females may have slightly lower values d/t less muscle mass. urine: 1-2 g/24 hr What are normal reference values for newborn, infant, 2-6 yo, older child and elderly? newborn: 0.8-1.4 mg/dL infant: 0.7-1.7 mg/dL 2-6yo: 0.3-0.6 mg/dL older child: 0.4-1.2 mg/dL elderly: may have decreased values d/t decreased muscle mass and decreased creatinine production. Question Answer Hint Albumin normal levels 3.5 - 5.0 mg/dl Albumin Increased serum values? Decreased: cystic fibrosis, chronic glomerulonephritis, alcoholic cirrhosis, Hodkin's disease, malnutrition, nephrotic syndrome, multiple myeloma, inflammatory bowel disease, leukemia, collagen-vascular diseases Aldosterone Increased in which pathologies Increased: hyperaldosterism (primary or secondary). Aldosterone Decreased in which pathologies Decreased: adrenal insufficiency, panhypopituitarism. Amylase Increased in which pathologies Increased: acute pancreatitis, pancreatic duct obstruction, alcohol ingestion, mumps, parotitidis, renal disease, cholecystitis, peptic ulcers, intestinal obstruction, mesenteric thrombosis, postop abdominal surgery Amylase Decreased in which pathologies Decreased: Liver damage, pancreatic destruction (pancreatitis, cystic fibrosis) Bilirubin Normal Serum values Total: 0.2 - 1.2 mg/dl Bilirubin Increased in which pathologies Increased total: hepatic damage (hepatitis, toxins, cirrhosis), biliary obstruction,hemolysis, fasting. Increased direct (conjugated): biliary obstruction / cholestasis, drug induced cholestasis. BUN Normal Serum values 7-20 mg/dl BUN Increased in which pathologies Increased: renal failure, pre-renal azotemia, shock, volume depletion, postrenal (obstruction), GI bleeding, stress, drugs (aminoglycosides, vanco etc). BUN decreased serum values Decreased: starvation, liver failure, pregnancy, infancy, nephrotic syndrome, overhydration. Calcium serum values 8.8 - 10.3 mg/dl Calcium Increased serum values Increased: primary hyperthyroidism, parathyroid hormone secreting tumors, vitamin D excess, metastatic bone tumors, chronic renal failure, milk-alkali syndrome, osteoporosis, thiazide drugs, pagets disease, multiple myeloma, sarcoidosis. Calcium Decreased serum values Decreased: hypoparathyroidism, insufficient vitamin D, hypomagnesemia, renal tubular acidosis, hypoalbuminemia, chronic renal failure (phosphate retention), acute pancreatitis CO2 ABG value 35-45 mm HG CO2 Increased ABG value Increased: respiratory acidosis, compensation for metabolic acidosis, severe vomiting, primary aldosteronism, volume contraction, emphysema CO2 Decreased ABG value Decreased: Respiratory alkalosis, starvation, DKA, lactic acidosis, alcoholic ketoacidosis, severe diarrhea, renal failure, drugs (salicylates etc), dehydration. Chloride Normal Serum values 95-107 meq/l Chloride Increased serum values Increased: diarrhea, renal tubular acidosis, mineralocorticoid deficiency, hyperalimentation, medications (acetazolamide, ammonium chloride). Chloride Decreased serum values Decreased: mineralocorticoid excess, vomiting, diabetes mellitus with ketoacidosis Creatinine Normal Serum values 0.5 - 1.4 mg/dl Creatinine Increased serum values Increased: renal failure including prerenal, drug-induced (aminoglycosides, vancomycin, others), acromegaly. Creatinine Decreased serum values Decreased: loss of muscle mass, pregnancy. Magnesium Normal Serum values 1.6 - 2.6 mg/dl Magnesium Increased serum values Increased: renal failure, hypothyroidism,severe dehydration, lithium intoxication, antacids, Addison's disease. Magnesium Decreased Serum values Decreased: hyperthyroidism, aldosteronism, diuretics, malabsorption, hyperalimentation, nasogastric suctioning, chronic dialysis, renal tubular acidosis, drugs (aminoglycosides, cisplatin, ampho B) Phosphorus Normal Serum values 2.5 - 4.5 mg/dl Phosphorus Increased serum values Increased: hypoparathyroidism, excess vitamin D, secondary hyperparathyroidism, renal failure, bone disease, addisons disease. Phosphorus Decreased Serum values Decreased: hyperparathyroidism, alcoholism, diabetes, hyperalimentation, acidosis, hypomagnesemia, diuretics, vitamin D deficiency, phosphate-binding antacids. Question Answer Hint Birth weight doubled by _____, tripled by _____. 6 months; 12 months Birth length increased by 50% at _____. 12 months Posterior fontanel closes by _____. 8 weeks (2 months) A child can socially smiles at _____. 2 months A child should be able to turn head to locate sounds at _____. 3 months Moro reflex disappears around _____. 4 months A child should be able to achieve steady head control at _____ of age. 4 months A child can turn completely over at _____ of age. 5 to 6 months A child can play peek-a-boo after _____ of age. 6 months A child should be able to transfers objects hand to hand at _____. 7 months A child develops stranger anxiety at _____. 7 to 9 months A child should be able to sit unsupported at _____. 8 months The infant crawls at _____. 10 months Fine pincer grasp appears at _____. 10 to 12 months A child should be able to waves byebye at _____. 10 months A child should be able to walks with assistance at _____. 10 to 12 months The infant says a few words in addition to "mama" or "dada" at 12 months_____. From birth to one year, the baby explores environment by _____ and _____ means. motor; oral From birth to one year is what stage of Erikson's theory? Trust vs Mistrust (Developing a sense of trust) What are some age-appropriate toys for hospitalized infants? mobiles rattles squeaking toys picture books balls colored blocks activity boxes Birth weight quadruples by _____. 30 months Achieves 50% of adult height by ___. 2 years Anterior fontanel closes by _____. 12 - 18 months A child should be able to throw a ball overhand at _____. 18 months The nurse tells a mother that her child should be able to kicks a ball at _____. 24 months A child should be able to feeds self with spoon and cup at _____. 2 years Day time toilet training can usually be started around _____. 2 years of age A child should be able to speak two to three word sentences at _____. 2 years (24 months) A child should be able to speak three to four word sentences at _____ of age. 3 years A child should be able to states his/her own first and last name by _____. 2.5 to 3 years Is temper tantrums common among toddlers (1 to 3 years)? Yes What is the import developmental task of a toddler according to Erikson's theory? Developing a sense of autonomy. What are some age-appropriate toys for the hospitalized toddler? board and mallet push/pull toys toy telephone stuffed animals storybooks with pictures What can the nurse do to promote the developemental task of a toddler? Toddlers benefit from being taken to the hospital playroom, as mobility is very important to their development. What are the average weight and height gain for preschool children (3 to 5 years old)? Each year gain about 5 lbs and grows 2.5 to 3 inches. A child can use sissors at _____ of age. 4 years A child should be able to ties shoelaces at _____ of age. 5 years Visual acuity approaches 20/20 at _____. Preschool age (3 to 5 years)A preschool child thinking is _____ and _____. egocentric; concrete A child should be able to use sentences of 5 to 8 words at _____ of age. 3 to 5 years Preschool At this stage of developement, a child learns sexual identity (curiosity and masturbation common). 3 to 5 years Preschool At this stage of development, imaginary playmates and fears are common. Preschool (3 to 5 years) At child at this development stage begins to stands erect with more slender posture. Preschool (3 to 5 years) At this stage of development, a child learns to run, jump, skip, and hop. Preschool (3 to 5 years) A child at this developmental stage learns colors and shapes. Preschool (3 to 5 years) Imaginary playmates and fears are common at this stage of development: Preschool (3 to 5 years) Aggressiveness at _____ is replaced by more _____ at 5 years. 4 years; independence Preschool child's major developmental taks according to Erikson theory is: Developing a sense of initiative At this stage of development, the child appears to be bowlegged and potbellied. TODDLER (1 TO 3 YEARS) At this stage of development, all primary teeth (20) are present. TODDLER (1 TO 3 YEARS) Nursing implications of hospitalized preschoolers (3-6 years) needs to emphasize understanding of the child's _____. egocentricity; (Explain that he/she did not cause the illness and that painful procedures are not a punishment for misdeeds.) _____ or medical play to allow the child to act out their experiences is helpful for _____. Therapeutic play; Preschoolers At this stage of development, fear of mutilation from procedures is common. Preschool (3 to 5 years) Toys and play for the hospitalized preschooler include: coloring books puzzles cutting and pasting dolls building blocks clay toys that allow the preschooler to work out hospitalization experiences. The _____ needs preparation for procedures. He or she needs to preschooler (3 to 6 years)understand what is and what is not going to be "fixed." Simple explanations and basic pictures are helpful. Let child handle equipment or models of the equipment. _____ are learning to name body parts and are concerned about their bodies. Toddlers (1-3 years) During hospitalization, enforced separation from parents is the greatest threat to the _____ psychological and emotional integrity. toddler's (1 to 3 years) Security objects or favorite toys from home should be provided for _____. toddlers (1 to 3 years) Normal gain in weight and height for school-age child (6 to 12 years) are: Each year gain 4 to 6 pounds and about 2 inches in height. Loss of primary teeth and eruption of most permanent school-age child (6 to 12 years) At this stage of development fine and gross motor skills mature. school-age child (6 to 12 years) During this developmental stage, girls may experience menarche. school-age (6 to 12 years) At this stage of development, a child should be able to dresses selfcompletely. school-age child (6 to 12 years) At this stage of development, egocentric thinking is replaced by social awareness of others. school-age child (6 to 12 years) At this stage of development, a child learns to tell time and understands past, present, and future. school-age child (6 to 12 years) At this stage of development, a child learns cause and effect relationships. school-age child (6 to 12 years) Socialization with peers becomes important at this stage of development: school-age child (6 to 12 years) A child's molars should erupt at _____. 6 years According to Erikson's theory, developing a sense of industry occurs at this stage: school-age child (6 to 12 years) A child should be able to write script at _____. 8 years The hospitalized _____ may need more support from parents than they school-age childwish to admit. Maintaining contact with peers and school activities is important during hospitalization for a _____. school-age child For school-age child, _____ and _____ are important, and should be respected during hospitalization. privacy; modesty e.g., close curtains during procedures, allow privacy during baths, etc. Participation in care and planning with staff fosters a sense of _____ and _____ for a school-age child (6-12 years). involvement; accomplishment Toys for the hospitalized school-age (6 to 12 years) child include: board games card games hobbies (such as stamp collecting, puzzles, and video games) School-age children are in Erikson's stage of _____, meaning they like to do and accomplish things. _____ are also becoming important for this age child. industry; Peers Girls' growth spurt during adolescent begins _____ than boys (may begin as early as ___ for girls). earlier; 10 Boys catch up to girls' growth at age _____ and continue to grow. 14 Girls finish growth around _____, boys around _____. 15; 17 Adult-like thinking begins around age _____. They can _____ and use _____ thinking. 15; problem solve; abstract Secondary sex characteristics begins at this developmental stage: ADOLESCENCE (12 to 19 YEARS) At this stage of development, family connflict commonly occurs. ADOLESCENCE (12 10 19 YEARS) Hospilalization of adolescents disrupts _____ and _____ activities; they need to maintain contact with both. school; peer Illness, treatments, or procedures which alter the body image can be viewed as devastating by the _____. adolescent For this develpmental stage, teaching about procedures should include time without parents present. adolescent (12 to 18 years) For this developmental group, some assessment questions should be asked without parents' presence. adolescent When teaching adolescent needs, the here and now i.e., how will this affect mefocus should be on _____. today? Infants' concept of bodily injury: Infants: After 6 months, their cognitive development allows them to remember pain. Toddlers' concept of bodily injury Toddlers: Fear intrusive procedures. Preschoolers' concept of bodily injury Preschoolers: Fear body mutilation. School ages' concept of bodily injury: School age: Fear loss of control of their body. Adolescents' concept of bodily injury: Adolescent: Major concern is change in body image. MMR VACCINE Generally administered at _____ months of age and repeated at _____ years or by _____ years. 12 to 15; 4 to 6; 11 to 12 In times of measles epidemic, it is possible to give measles protection at _____ and repeat the MMR at _____. 6 months; 15 months Measles vaccine is contraindicated for persons with history of anaphylactic reaction to _____ or _____, those with known altered _____ and _____ women. neomycin; eggs; immunodeficiency; pregnant MMR vaccine may be given to those with HIV and breastfeeding women. T or F True MMR vaccines are administer _____ at separate sites. subcutaneously A child may have a light transient ___ 2 weeks after administration of MMR vaccine. rash DTaP Vaccine administration begins at age ____, administer three doses at _____ intervals. 2 months; 2 months DTaP Vaccine: Booster doses given at _____ to _____; and at _____. 15; 18 months; 4 to 6 years. DTaP Vaccine: administer _____ (separate site from other vaccine). intramuscularly DTaP Vaccine is not given to children past the ______ birthday; they receive _____ which contains full strength protection against tetanus and lesser strength diphtheria protection. 7th; Td When pertussis vaccine is contraindicated, give _____, until 7th birthday. DT (full strength diphtheria and tetanus without pertussis vaccine) Contraindications to pertussis vaccine include: 1. _____ within 7 days of Encephalopathy; seizures; Neurologic; Systemicprevious dose of DTP. 2. History of _____. 3. _____ symptoms after receiving the vaccine. 4. _____ allergic reactions to the vaccine. Parents should be instructed to begin _____ administration after the immunization (normal dosage is _____ mg/kg). acetaminophen (Tylenol); 10 to 15 IPV is recommended for all person under the age of _____. 18 IPV is administer at _____ of age and again at _____ of age. Boosters are given at _____ , and _____. 2 months; 4 months; 6 to 15 months; 4 to 6 years Administer IPV _____ or _____ at separate site. subcutaneously; IM IPV is contraindicated for those with history of anaphylactic reaction to _____ or _____. neomycin; streptomycin PRP-OPMs can be given as early as ____ of age. 2 months DaTP/Hib combinations should not be used as primary immunizations at ages ___, ___, or ___. 2; 4; 6 months Children at high risk who were not immunized with Hib previously should be immunized after age _____. 5 Hib is administer ______. intramuscularly _____ offers protection against bacteria that causes serious illness (epiglottitis, bacterial meningitis, septic arthritis) in small children or those with chronic illnesses such as sickle cell anemia. Hib _____ offers protection against hepatitis B. Typically, given to all _____ prior to hospital discharge. Vaccinate all children _____ to _____ years of age. Hepatitis B vaccine; newborns; 0; 18 Hepatitis B vaccine is contraindicated for persons with anaphylactic reaction to _____. common baker's yeast Hepatitis B vaccine is administer trough _____ site at _____ , _____, and _____ of age. IM; 0 to 2 months; 1 to 4 months; 6 to 18 months _____ offers protection against VARICELLA vaccinechickenpox. It is also a school entry requirement in 33 states. And it is safe for children with asymptomatic HIV infection. VARICELLA vaccine is administer at _____ of age (must beat least _____). 12 to 18 months; 12 months Give _____ and _____ vaccines on same day or >30 days apart (separate site). MMR; varicella Irritability, fever (<102 F), redness and soreness at injection site for 2 to 3 days are normal side effects of _____ and _____ administration. DPT; IPV Following immunization, call health care provider if _____, _____, or _____. seizures; high fever; high-pitched crying occur Following immunization, a _____ on the thigh injection site and _____ the legs with each diaper change will decrease soreness. warm washcloth; "bicycling" Following immunization, acetaminophen (Tylenol) is administered orally every _____ hours (_____ mg/Kg). 4 to 6; 10 to 15 The common cold is not a contraindication for immunization. T or F True A highly contagious, viral disease that can lead to neurologic problems or death. RUBEOLA (Measles) RUBEOLA (Measles) is transmitted by _____. Direct contact with droplets from infected person. RUBEOLA (Measles) is contagious mainly during the _____ which is characterized by _____ and _____ symptoms. prodromal period; fever; upper respiratory Classic symptoms of RUBEOLA (Measles) include: Photophobia Koplik's spots on the buccal mucosa. Confluent rash that begins on the face and spreads downward. Viral disease characterized by skin lesions. VARICELLA ZOSTER (Chicken Pox) Chicken Pox lesions begin on the _____ and spread to the _____ and _____. trunk; face; proximal extremities Chicken Pox progresses through macular; papular; vesicular; pustular_____, _____, _____, and _____ stages. Chicken Pox transmitted by ____, _____, or _____. direct contact; droplet spread; freshly contaminated objects Chicken Pox communicability end when _____. scabs have formed Common viral disease which has teratogenic effects on fetus durina the first trimester of pregnancy. RUBELLA (German Measles) RUBELLA (German Measles) is transmitted by _____ and _____. droplet; direct contact with infected person RUBELLA (German Measles) is charcterized by _____ starts on _____ and rapidly spreads to _____. discrete red maculopapular rash; face; entire body RUBELLA (German Measles) rash disappears within _____. 3 days An acute, infectious respiratory disease usually occurring in infancy. Pertussis (Whooping cough) Pertussis is caused by a _____. gram-negative bacillus PERTUSSIS (Whooping Cough) begins with _____. upper respiratory symptoms _____ is a paroxysmal state of the disease is characterized by prolonged coughing and crowing or whooping upon inspiration. PERTUSSIS (Whooping Cough) PERTUSSIS (Whooping Cough) lasts from _____. 4 to 6 weeks PERTUSSIS (Whooping Cough) is transmitted by _____, _____, or _____. direct contact; droplet spread; freshly contaminated objects PERTUSSIS (Whooping Cough) is treated with _____. erythromycin PERTUSSIS (Whooping Cough) complications include _____, _____, and _____. pneumonia; hemorrhage; seizures Question Answer Hint Which action should the nurse implement when administering a prescription drug that should be given on an empty stomach? Give one hour before or two hours after a meal. Average transit time from stomach to duodenum is 2 hours. The nurse is caring for a client who is unable to void. The plan of care establishes an objective for the client to ingest 1000ml of fluid between 7am and 3pm. Which client response Drinks 240ml of fluid five times during the shift.should the nurse document that indicates a sucessful outcome? A client with metastatic cancer is preparing to make decisions about end of life issues. When the nurse explains a durable power of attorney for health care, which description is accurate? It will identify someone that can make decisions for your health care if you are in a coma or vegetative state. The nurse is caring for a client who is the daughter of a local politician. When the nurse approaches a man who is reading the names on the hall doors, he identifies himself as a reporter for the local newspaper and requests information about the client's status. Which standard of nursing practice should the nurse use to respond? Confidentiality A client with acute hemorrhagic anemia is to receive four units of packed RBC's (red blood cells) as rapidly as possible. Which intervention is most important for the nurse to implement? Ensure the accuracy of the blood type match. A male client who had abdominal surgery has a nasogastric tube to suction, oxygen per nasal cannula, and complains of dry mouth. Which action should the nurse implement? Apply a water soluble lubricant to the lips, oral mucosa, and nares. Petroleum based products are flammable. A client with chronic renal failure selects a scramble egg for his breakfast. Which action should the nurse take? Commend the client for selecting a high biologic value protein. The nurse is administering meds through a NG tube which is connected to suction. After ensuring correct tube placement, what action should the nurse take next? Flush the tube with water. NGT should be flushed before, after, and in between each med adminstered. The nurse notices that the mother of a 9 year old Vietnamese child always looks at the floor when she talks to the nurse. What action should the nurse take? Continue asking the mother questions about the child. When assessing a client with wrist restraints, the nurse observes that the Loosen the right wrist restraint.fingers on the right hand are blue. What action should the nurse implement first? A client who is 5'5 tall and weighs 200lbs is scheduled for surgery the next day. What question is most important for the nurse to include during the preoperative assessment? What vitamin and mineral supplements do you take? Vitamins affect meds. An african american grandmother tells the nurse that 4 year old grandson is suffering with miseries. Based on this statement, which focused assessment should the nurse conduct? Inquire about the source and type of pain. Different cultural have different words. In developing a plan of care for a client with dementia, the nurse should remember that confusion in the elderly often follows relocation to new surroundings. The nurse is instructing a client with high chholesterol about diet and life style modification. What comment from the client indicates that the teaching has been effective? I will limit my intake of beef to 4 ounces per week. saturated fat from animal > cholesterol The nurse is interviewing a female client whose spouse is present. During the nterview, the spouse answers most of the questions for the client. Which action is best for the nurse to implement? Ask the spouse to step out for a few minutes. A young mother of three complains of increased anxiety during her annual physical exam. What information should the nurse obtain first? Nutritional history A nurse takes a female client to the examination room and asks her to remove her clothes and put on an examination gown with the front open. The woman states "I have special undergarments that I do not remove for religious reasons." How should the nurse respond? Tell me about your undergarments so we can discuss how you can have your examination comfortably. The nurse determines that a client's body weight is 105% above teh standardized height-weight scale. Which related factor should the nurse include in the nursing diagnosis, Inadequate lifestyle changes in diet and exercise."Imbalanced nutrition: more than body requirements? A postoperative client will need to perform daily dressing changes after discharge. Which outcome statement best demonstrates the client's readiness to manage his wound care after discharge? The client Demonstrates the wound care procedure correctly An elderly male client who is unresponsive following a cerebral vascular accident (CVA) is receiving bolus enteral feedings though a gastrostomy tube. What is the best client position for administration of the bolus tube feedings? Fowlers' (Semi-sitting) The nurse plans a teaching session with a client but postponses the planned session based on which nursing diagnosis? Activity intolerance related to postoperative pain. The nurse is preparing to adminster IV fluid to a client with a strict fluid restriction. IV tubing with which feature is most important for the nurse to select? Buterol attachment An elderly resident of a long-term care facility is no longer able to perform self care and is becoming progressively weaker. The resident previously requested that no resusciative efforts be performed, and the family requests hospice care. WHat action should the nurse implement first? Notify the healthcare provider of the family's request. Prior to transferring a client to a chair using a mechanical lift, what is teh most important client characteristic the nurse should assess? Tolerance of exertion. Which snack food is best for the nurse to provide a client with myasthenia gravis who is at risk for altered nutritional status? Chocolate pudding The nurse observes that a male client has removed the covering from an ice pack applied to his knee. Which action should the nurse take first? Observe the appearance of the skin under the ice pack.While instructing a male client's wife in the performance of passive range of motion exercises to his contracted shoulder, the nurse observes that she is holding his arm above and below the elbow. What nursing action should the nurse implement? Acknowledge that she is supporting the arm correctly. When evaluating a client's plan of care, the nurse determines that a desired outcome was not achieved. Which action will the nurse implement first? Note which actions were not implemented. The nurse assigns a UAP to obtain vital signs from a very anxious client. What instructions should the nurse give the UAP? Report the vital signs to the nurse. During a visit to the outpatient clinic, the nurse assess a client with severe osteoarthritis using a goniometer. Which finding should the nurse expect to measure? Degree of flexion and extension of the client's knee joint. The nurse is assessing an older client and determines that the client's left upper eyelid droops, covering more of the iris than the right eyelid. Which description should the nurse use to document this finding? Ptosis of the left eyelid. A female client asks the nurse to find someone who can translate into her native language her concerns about a treatment. Which action should the nurse take? Request and document the name of the certified translator. The nurse is teaching a client proper use of an inhaler. When should the client administer the inhaler-delivered medication to demonstrated correct use of the inhaler? During the inhalation. The nurse observes an unlicensed personnel (UAP) taking a client's blood pressure with a cuff that is too small, but the blood pressure reading obtained is within the client's usage range. What action is most important for the nurse to implement? Reassess the client's blood pressure using a larger cuff. A client is brought into the emergency Stop the code immediately.department following a sudden cardiac arrest. A full code is started. FIve minutes later the family arrives with a durable power of attorney signed by the client requesting that no extraordinary measures be taken, including intubation, to save the client's life. What action should the nurse take? The nurse dons gown, mask with eyeshield, and gloves before entering a client's room that has airborne precautions. Upon leaving the client's room, in which sequence should the nurse remove the personal protective equipment? Remove gloves, gown, mask, wash hands When documenting assessment data, which statement should the nurse record in the narrative nursing notes? S1 murmur auscultated in supine position: Objective data An obese male client discusses with the nurse his plans to begin a longterm weight loss regimen. In addition to dietary changes, he plans to begin an intendive aerobic exercise program 3 to 4 times a week and to take stress managment classes. After praising the client for his decision, which instruction is most important for the nurse to provide? Be sure to have a complter physical exam before beginning your planned exercise program. A male client being discharged with a prescription for the bronchodilator theophylline tells the nurse that he understands he is to take three doses of the medication each day. Since, at the time of discharge, timed-release capsules are not available, which dosing schedule should the nurse advise the client to follow? 8am, 4pm, 1200 midnight. q 8hrs The nurse is preparing to administer a high volume saline enema to a client. Which information is most important for the nurse to obtain prior to administering the enema? History of inflammatory bowel disorder scrymptoms: diarhhea, hematuria, perforation Question Answer Hint ABG Values: pH PaCO2 PaO2 pH: 7.35-7.45 high--alkalosis PaCO2: 35-45high-- acidosis Pa02: 75-100 Ca+ level 9-11 Creatinine: K+: Na+: Creatinine: 0.2-1.0 K+: 3.5-5 Na+: 135-145 Mg: Phos: Mg: 1.5-2.5 Phos: 2.8-4.5 Hgb: Hct: Hgb: 12-18 Hct: 38-55 Platelets WBC'S RBC's (erthrocytes) 150-400 4-11(,000,000) 4-6 PERRLA Cranial Nerve? Smile Cranial Nerve? Gag reflex Cranial Nerve? Shoulder Shrug Cranial Nerve? PERRLA: II (Optic) Smile: VII (Facial) Gag: X (Vagus) XII (Hypoglossal) Shoulder Shrug: XI (Accessory) Normal Values: CCP: MAP: ICP: CCP: 70-100 MAP: 50 ICP: 0-15 What heals slowest? Cartilage, ligaments Upper UTI sx: CVA tenderness ITP (immune thrombocytopenia purpura) tx: Splenectomy (reduced destruction of platelets by macrophages) Urine Specific Gravity: 1.003-1.030 MI Lab Values: elevated Troponin 0.02 normal CK-MB 0-9 normal Band Neutrophils normal 0-8% increased in: acute infection-- shift to the left Cranial Nerves: O olfactory O optic O oculomotor T trochlear T trigeminal A abducens F facial A auditory G glossopharyngeal V vagus A accessory H hypoglossal Question Answer Hint prompt zinc suspension insulin (Semilente) Rapid-Acting human insulin lispro (Humalog) Rapid-Acting insulin aspart (Novolog) Rapid-Acting regular insulin (human) Short acting isophane insulin (NPH) (Iletin) Intermediate acting insulin zinc suspension (Humulin L) Intermediate acting protamine zinc (PZI) Long-Acting extended zinc suspension (Ultralente) Long-Acting insulin glargine (Lantus) Long-Acting prompt zinc suspension insulin (Semilente) Onset Peak 0.5 to 1 hour 2 to 3 hours human insulin lispro (Humalog) Onset Peak 0.5 to 1 hour 2 to 4 hours insulin aspart (Novolog) Onset Peak 5 to 15 minutes 0.75 to 1.5 hour Give within 15 min of a meal. Nursing implications for Lispro (2) Lispro may be given intravenously. Give within 15 min of a meal. isophane insulin (NPH) (Iletin) Onset Peak 1 to 2 hours 6 to 12 hours insulin zinc suspension (Humulin L) Onset Peak 1 to 2 hours 6 to 12 hoursprotamine zinc (PZI) Onset Peak 4 to 8 hours 14 to 20 hours Not to be given IV. extended zinc suspension (Ultralente) Onset Peak 1.1 hours 5 hours insulin glargine (Lantus) Onset Peak 1.1 hours 5 hours regular insulin (human) Onset Peak 30 to 60 minutes 2 to 3 hours Regular insulin may be given IV. Question Answer Hint What are the 5 steps of the nursing process? assessment analysis planning implementation evaluation Define assessment? gather objective and subjective data verify data Define analysis? interpret data collect additional data when necessary identify and communicate nursing diagnoses determine health team's ability to meet client's needs Define planning? determine and prioritize goals of care. Include client, significant others, and health team in setting goals develop and modify plan for delivery of client's care Define implementation? organize and manage the client's care perform or assist in performance of client's care counsel and teach client, significant others, and health team provide care specifically directed toward achieving goals Define evaluation? compare actual outcomes with expected outcomes evaluate compliance with the established regimen or plan record and describe client's response to plan modify plan as indicated, and set priorities What are the 2 components of the nursing diagnosis? response etiology The RESPONSE component of a nursing diagnosis is? includes potential or actual health response describes measurable outcomes that can be derived cites potential for changes based on nursingn actions example: alteration in comfort, pain The ETIOLOGY component of a nursing diagnosis is? includes potential or actual health response addresses independent, inter- dependent, and dependent nursing functions example: related to fractured left ankle Name 13 NANDA-Approved Nursing Diagnoses? activity/rest circulation elimination emotional reactions food/fluid hygiene neurologic pain relationship alterations safety sexuality teaching/learning ventilation Name the Activity/Rest NANDA- Activity Intolerance Activity Intolerance,Approved Nursing Diagnoses? (7) Potential Disuse Syndrome, Potential for Diversional Activity Deficit Fatigue Physical Mobility, Impaired Sleep Pattern Disturbance Name the Circulation NANDAApproved Nursing Diagnoses? (3) Decreased Cardiac Output Tissue Perfusion, Altered (Specify type: renal, cerebral, cardiopulmonary, GI, peripheral) high risk for peripheral neurovascular dysfunction Name the Elimination NANDAApproved Nursing Diagnoses? (12) Constipation Constipation, Colonic Constipation, Perceived Diarrhea Incontinence, Bowel Incontinence, Functional Incontinence, Reflex Incontinence, Stress Incontinence, Total Incontinence, Urge Urinary Elimination, Altered Urinary Retention Name the Emotional Reactions NANDA-Approved Nursing Diagnoses? (22) Adjustment, Impaired Anxiety Body Image Disturbance Individual Coping, Ineffective Defensive Coping Denial, Ineffective Decisional Conflict (Specify) Fear Grieving, Anticipatory Grieving, Dysfunctional Hopelessness PostTrauma Response Powerlessness Personal Identity Disturbance Rape-Trauma Response Rape-Trauma Syndrome Rape-Trauma Syndrome: Compound Reaction Rape-Trauma Syndrome: Silent Reaction Relocation Stress Syndrome Self-Esteem, Chronic Low SelfEsteem, Situational Low Spiritual Distress Name the Food/Fluid NANDAApproved Nursing Diagnoses? (12) Breastfeeding, Ineffective Interrupted Breastfeeding Fluid Volume, Excess Fluid Volume Deficit, Potential Nutrition Less than Body Requirements, Altered Nutrition More than Body Requirements, Altered Nutrition, Potential for more than Body Requirements, Altered Oral Mucous Membrane, Altered Swallowing, Impaired Ineffective Infant Feeding Pattern Name the Hygiene NANDA-Approved Nursing Diagnoses? (2) Health-Seeking Behaviors (Specify) Self-Care Deficit: ---Bathing/Hygiene ---Toileting ---Feeding ---Dressing/Grooming Name the Neurologic NANDAApproved Nursing Diagnoses? (5) Communications, Impaired Verbal Dysreflexia Unilateral Neglect Sensory/Perceptual Alterations (Specify type: visual, auditory, kinesthetic, gustatory, tactile, olfactory) Thought Process, Altered Name the Pain Nanda-Approved Nursing Diagnoses? (2) Pain Pain, Chronic Name the Relationship Alterations Family Coping: Compromised, IneffectiveNANDA-Approved Nursing Diagnoses? (13) Family Coping: Disabling, Ineffective Family Process, Altered Parental Role Conflict Parenting, Altered Role Performance, Altered Self-Esteem, Chronic Low Self-Esteem, Situational Low Self-Esteem Disturbance Social Interaction, Impaired Social Isolation Caregiver Role Strain High Risk for Caregiver Role Name the Safety NANDA-Approved Nursing Diagnoses? (17) Body Temperature, Potential Altered Health Maintenance, Altered Home Maintenance Management, Impaired Hyperthermia Hypothermia Infection, Potential for Injury, Potential for Poisoning, Potential for Suffocation, Potential for Trauma, Potential for Skin Integrity, Impaired Skin Integrity, Potential Impaired Thermoregulation, Ineffective Tissue Integrity, Impaired Violence, Potential for: Selfdirected or directed at others High Risk for Self-Mutilation Name the Sexuality NANDA-Approved Nursing Diagnoses? (2) Sexual Dysfunction Sexual Patterns, Altered Name the Teaching/Learning NANDAApproved Nursing Diagnoses? (5) Growth and development, altered Knowledge deficit (specify) Noncompliance (specify) Ineffective management of therapeutic regimen (individuals) Therapeutic regimen: (community, families): ineffective management Name the Ventilation NANDAApproved Nursing Diagnoses? (6) Airway clearance, ineffective Aspiration, potential for Breathing pattern, ineffective Gas exchange Dysfunctional ventilatory weaning response Inability to sustain spontaneous ventilation Name Maslow's Hierarchy of Needs in order. (6) Physiologic Safety Love and Belonging Esteem and Recognition Self-Actualization Aesthetic What is the definition of Maslow's Physiologic? Biologic needs for food, shelter, water, sleep, oxygen, sexual expression What is the definition of Maslow's Safety? Avoiding harm; attaining security, order, and physical safety What is the definition of Maslow's Love and Belonging? Giving and receiving affection; companionship; and identification with a group What is the definition of Maslow's Esteem and Recognition? Self-esteem and respect of others; success in work; prestige What is the definition of Maslow's Self-Actualization? Fulfillment of unique potential What is the definition of Maslow's Aesthetic? Search for beauty and spiritual goals The priority biologic need is? breathing i.e. open airwayEnsuring that the client's environment is 1____ is a priority, e.g., teaching an older client to remove throw rugs which pose a safety hazard when ambulating would have a greater priority than teaching how to use a walker - FIRST priority is 2____, then 3____ skills. 1 SAFE 2 safety 3 coping Which action has a higher priority...assisting the client in becoming a part of a support group...or assisting him/her in developing self-esteem? sense of belonging comes first, and such a sense might help in developing self-esteem What provides the laws that control the practice of nursing in each state? Nurse Practice Acts A tort is an act involving injury or damage to another (except 1_____ of contract) resulting in 2_____ liability (i.e. the victim can sue) instead of 3_____ liability (see crime). 1 breech 2 civil 3 criminal Two unintentional torts are? negligence malpractice Negligence is a form of ______ tort whereby performing an act that a reasonable and prudent person would not do. Measure of negligence is "_____" (i.e. would a reasonable and prudent nurse act in the same manner under the same circumstance?) unintentional reasonableness Malpractice is a form of ______ tort whereby there is negligence of professional _____, e.g., professional misconduct, or unreasonable lack of skill in carrying out professional duties. unintentional misconduct What four elements are necessary to prove negligence/malpractice and if any element is missing, it cannot be proved? duty breach of duty injury/damages causation What is DUTY? (one of the four elements that proves negligence/malpractice and cannot be missing) The obligation to use due care (what a reasonable, prudent nurse would do) Failure to care for and/or to protect others against unreasonable risk. DUTY (one of four elements of negligence/malpractice) must _______ foreseeable risks. Example: If ANTICIPATEa floor has water on it, the nurse is responsible for anticipating the risk to the client of falling. What is BREACH OF DUTY? (one of the four elements that proves negligence/malpractice and cannot be missing) Failure to perform according to the established standard of conduct in providing nursing care. What is INJURY/DAMAGES? (one of the four elements that proves negligence/malpractice and cannot be missing) Failure to meet standard of care, which causes actual injury or damage to the client, either physical or mental. What is CAUSATION? (one of the four elements that proves negligence/malpractice and cannot be missing) A connection exists between conduct and the resulting injury referred to as "proximate cause" or "remoteness of damage" Hospital policies provide a guide for nursing 1_____. They are NOT 2____, but courts generally rule against nurses who have violated the employer's policies. Hospitals can be liable for poorly formulated or poorly implemented policies. 1 actions 2 laws What alerts administration to possible liability claims and the need for investigation; they do NOT _____ against legal action being taken for negligence or malpractice. Incident report protect Burning a client with a hot water bottle or heating pad is an example of? negligence/malpractice Two forms of intentional tort are? assault battery What is the term used for mental or physical threat, e.g., forcing (without touching) a client to take a medication or treatment? assault What is the term used when touching, with or without the intent to do harm, e.g., hitting or striking a client. If a mentally competent adult is forced to have a treatment and has refused, this occurs? battery Leaving sponges or instruments in a client in surgery is an example of? negligence/malpractice What is the term for encroachment or trespassing on another's body and/or invasion of privacypersonality? Confinement without authorization? false imprisonment Exposure or discussion of the client's case. After death, the client has a right to be unobserved, excluded from unwarranted operations, and protected from unauthorized touching of the body? exposure of a person Performing incompetent assessments is an example of? negligence/malpractice Divulgence of privileged information or communication, e.g., from charts, conversations, or observations? defamation Failing to heed warning signs of shock or impending MI is an example of? negligence/malpractice Willful and purposeful misrepresentation that could cause, or has caused, loss or harm to a person or property? fraud Ignoring signs and symptoms of bleeding is an example of? negligence/malpractice Presenting false credentials for the purpose of entering nursing school, obtaining a license, or obtaining employment is termed? fraud A legal term meaning the accused is not criminally responsible for the unlawful act committed due to mental illness? insanity Forgetting to give a medication or giving the wrong medication is an example of? negligence/malpractice An act contrary to a criminal statute. Wrongs punishable by the state, committed against the state, with intent usually present. crime Legal hearing that is held to determine a person's capability to make responsible decisions about self, dependent, or property? competency hearing Persons declared incompetent have the legal status of a minor, i.e., they cannot? (5) vote make contracts or wills drive a car sue or be sued hold a professional license If a person is incompetent, a _____ is appointed. Declaring a person guardian stateincompetent can be initiated by the ____ or family. An admission whereby any adult may apply for another. However, medical or judicial approval is required to detain anyone beyond 24 hours. emergency admmission Emergency admissions allow persons held against their will to file a ____ _____ to try and get the court to hear their case and release them. habeas corpus With emergency admissions, the court determines the ____ and alleged unlawful restraint of a person. sanity Question Answer Hint 1 km = _ m 1,000 1 m = _ cm 100 1 cm = _ mm 10 1 L = _ ml 1000 1 ml = _ cm3 1 1 kg = _ g 1000 1 g =_ mg 1,000 1 mile = _ yds 1760 yds 1 mile =_ ft 5280 ft 1 yd = _ ft 3 ft 1 ft =_ in 12 in 1 gallon = _ qts 4 qts 1 gallon = _ oz 128 oz 1 qt = _ pints 2 pints 1 pint = _ cups 2 cups 1 cup =_ oz 8 oz 1 oz = _ cm3 30 1 kg =_g 1000 1 g = _ mg 1000 1 ton =_ Ibs 2,000 1 Ib=_ oz 16 oz 1 Kg = __ lbs. 2.2 lbs. 1 oz = __ g 30 g 15 g = __ dr 4 dr 1 g = __ gr 15 gr 1 gr = __ mg 60 mg 1 qt = __ pints 2 pints 1 pint = __ fluid oz 16 fluid oz 1 fluid oz = __ fluid drams 8 fluid drams 1 fluid dram = __ (m) minims 60 m (minims)1 minim = __ drops (gt) 1 drop 1 oz = __ grains 480 gr 1 oz = __ drams 8 drams 1 dram = __ grains 60 grains 1 t = __ drops 60 drops 1 T = __ t 3 t 1 oz = __ T 2 T 1 L = __qt; __oz 1 qt; 32 oz 1 in = __ cm 2.54 cm 1 oz = __ml; __dr; __T; __t 30 ml; 8 dr; 2 T; 6 t Question Answer Hint List the major CNS danger signals that occur in the neonate. Lethargy, high-pitched cry, jitteriness, seizure, and bulging fontanelles. A baby is deleivered blue, and with heart rate <100. The nurse dries the infant, suctions the oropharynx and gently stimulates the infant while blowing O2 over the face. The infant still does not respond. What is the next nursing action? Begin oxygenation by bag and mask at 30 to 50 breaths per minute. If heart rate is <60, start cardiac massage at 120 events per minute. (30 breaths and 90 compressions). Assist health care provider in setting up for intubation procedure. What does the Silverman-Anderson index measure? Respiratory difficulty. What ar two complications of O2 toxicity? Retroplacental fibroplaisas and bronchopulmonary dysplasia Necrotizing enterocolitis results from ___________ and is manifested by_______. Ischemia/hypoxia results in _____-__. Ischemic hypoxia, abdominal distetion, sespis, and a lack of absorption from intestines; injury to the inestinal mucosa. Inraventricular hemorrhage is more common __________and results in symptoms of ___________. premature neonates and VLBW babies; increased intracranial pressure Wht conditions make oxygenation of the newborn more difficult? Respiratory distress syndrome: alveolar prematurity and lack of surfactant; anemia; polycythemia. In order to prevent problems with oxygenating the newborn, what parameters can the nurse observe? Po2 50 to 90; SvO2 60 to 80mmHg What are the cardinal symptoms of sepsis in a newborn? Lethargy, tempetature instability, difficulty feeding, subtle color changes, subtle behavioral changes, and hyperbilirubinemia. A premature baby is born and develops hypothermia. State the major nursing interventions t treat hypothermia. Place under radiant warmer or in incubator with temperature skin probe over liver. Warm all items touching newborn. Place plastic wrap over neonate. Nurses often weigh diapers in order to Daiper is weighed in grams before beingdetermine exact urine output in the high-risk neonate. Explain this procedure. applied to infant. Diaper is weighed after infant has wet it. Each gram of added weight is calculated and recorded as 1 ml of urine. What factors does a nurse look for in determining a newborn's ability to take in nourishment by nipple and mouth? infant has good suck, has coordinated suckswallow, takes less than 20 minutes to feed, gains 20 to 30g/day. What complications are associated with total parenteral nutrition? Hyperglycemia, electrolyte imbalance, dehydration, and infection. In order to prevent rickets in the preterm in the preterm newborn, what supplements are given? Calcium and Vitamin D. List four nursing interventions to enhance family and parent adjustment to a high-risk newborn. Initiate early visittaion at ICU. Provide daily information to family. Encourage partcipation in support group for parents. Encourage all attempts at care giving (enhances bonding). List the factors for Hyperbilirubinemia. Rh incompatibility, ABO incompatibility, prematurity, sepsis, perinatal asphyxia List the symptoms of hyperbilirubinemia in the neonate. Bilirubine levles rising 5mg/day, jaundice, dark urine, anemai, High reticulocyte (RBC) count, and dark stools. Question Answer Hint The nurse is providing instructions to a 68 year old client who is at high risk for development of coronary heart disease (CHD). Which intervention should the nurse include? Increase intake of soluble fiber to 10 to 25 grams per day. An Adult client is admitted to the hospital burn unit with second and third degree burns over 40% of the body surface area. In assessing the potential for skin regeneration, what should the nurse remember about thrid degree burns? Regenerative function of the skin is absent because the dermal layer has bbeen destroyed. Which description of symptoms is charcteristic of a client diagnosed with trigeminal neuralgia (Tic dououreux)? Sudden, stabbing, severe pain over the lip and chin. Prior to a cardiac catherization, which activity should the nurse have the client practice? Valsalva's manuever and coughing. A client is placed on respirator following a cerebral hemmorhage, and vecuronium bromide (Norcuron) . 04mg/kg q 12h IV is prescribed. Which nursing diagnosis is the priority? Impaired communication related to paralysis of skeletal muscles.Which client should the nurse recognize as most likely to experience sleep apnea? Obese older male client with a short, thick neck. A client receiving cholestyramine (Questran) for hyperlipidemia should be evaluated for what vitamin deficency? Vit K (Thse drugs reduce the absorption of the fat soluble vitamins ADEK. The nurse identifies bright red drainage, about 6 cm in diameter, on the dresssing of a client who is one day post abdominal surgery. Which action should the nurse take next? Mark the drainage on the dressing and take vital signs. A client is admitted to the hospital with a diagnosis of severe acute diverticulitis. Which assessment finding should the nurse expect this client ot exhibit? Lower left quadrant pain an da low-grade fever. (sigmoid most common site) The nurse is assessing the lab results for a client who is admitted with renal failure and osteodystrophy. Which findings are consistent with this client's clinical picture? Serum Potassium of 5.5 mEq and total calcium of 6mg/dl. Renal failure (hyperKalemia and Hypocalcemia) The nurse is assessing a client lab values following administration of chemotherapy. Which lab values leads the nurse to suspect that the client is experiencing tumor lysis syndrome? Serum calcium 5.0mg/dl. TLS results in hyperkalemia, hypocalcemia, and hyperuricemia. A client who is HIV positive ask the nurse, "How will I know when I have Aids"? Which response is best for the nurse to provide? Aids is diagnosed when a specifc oppurtunistic infection is found in an other wise healthy individual. A splint is prescribed for nightitme use by a client with rhuematoid arthritis. Which statement by the nurse provides the most accurate explanation for use of the splints. Prevention of deformities. Then nurse is planning care for a client who has a right hemispheric stroke. Which nursing diagnosis should the nurse include in the plan of care? Risk for injury related to denial of deficits and impulsiveness. Right brain damage= difficulty in judgement and spatial perception. Left=speech issues and language deficits Then nurse knows that lab values sometimes vary for the older client. Which data should the nurse expect to find when reveiwing lab values of an 80 year old male? Increased protein in the urine, slightly increased serum glucose levels.The nurse is planning care to prevent complication for a client with multiple myeloma. Which intervention is most important for the nurse to include? Maintain a Fluid fo 3 to 4 l per day. Malignant plasma cells that infiltrate bone casue demineralization>>>promote excretion of calcium The nurse is assessing a client with bacterial meningitis. Which assessment finding indicates the client may have developed septic emboli? Cyanosis of fingertips Emboli lodge in small arterioles of extermities A client who is sexually active with several partners requests an IUD as a contraceptive method. Which information should the nurse provide? Using an IUD offers no protection against sexually transmitted diseases (STD), which increae the risk of pelvic inflammatory disease. In preparing a discharge plan for a 22 year old male client diagnosed with Buerger's disease (thromboangitis oblitrans), which referral is most important? Smoking cessation program. An 81 year old male client has emphysema. He lives at home with his cat and manages self care with no difficulty. When making a home visit, the nurse notices that his tongue is somewhat cracked and his eyeballs are sunken into his head. What nursing intervention is indicated? Help the client to determine ways to increase his fluid intake. Based on the analysis of the client's atrial fibrillation, the nurse should prepare for which treament protocol. Anticoagulant therapy. THe nurse should prepare for anticoag therapy which is prescribed before rhythmn control. A client with cirrhosis develops increasing pedal edema and ascites. What dietary modification is most important for the nurse to teach this client? Restrict salt and fluid intake. Which reaction should the nurse identify in a client who is responding to stimulatiion of the sympathetic nervous system? Increased Heart rate Thenurse is preparing a teaching plan for a client who is newly diagnosed with Type 1 diabetes mellitus. Which signs and symptoms should the nurse describe when teaching the client about hypoglycemia? Sweating, trembling, tachycardia Hyper: Poly uria, dipsia, phagia, fruity breath tachypnea A client who is receiving chemotherapy asks the nurse, "Why is Chemotherapy affects the cells of the body that grow rapidly, both normal and malignant.so much of my hair falling out each day"? WHich response by the nurse best explains the reason for alopecia? Which finding should the nurse identify as most significant for a client diagnosed with polycystic disease? 3+ bacteria in urine A female client receiving IV vasopressin (Pitressin) for esophageal varice rupture reports to the nurse that she feels substernal tightness and pressure across her chest. Which PRN protocol should the nurse initiate? Start an IV nitro infusion The nurse is assessing a client with Chronic Renal Failre. Which finding is most important for the nurse to respond to first? Potassium 6.0 mEQ> A male client receives a local anesthetic during surgery. During the post-operative assessment, the nurse notices the client is slurring his speech. Which action should the nurse take? Evaluate his blood pressure, pulse, and respiratory status. Which assessment finding by the nurse during a client's clinical breast exam requires follow-up? A newly retracted nipple. A client is being admitted to the medical unit from teh emergency dept after having a chest tube inserted. What equipment should be brought to his client's room? Rubber tipped clamp (assesses air leaks) Which information should thenurse give a client with chronic renal failure (CRF)? Avoid salt subsitutes A client who is one week postoperative after an aortic valve replacemnt suddenly develops severe pain in the left leg. On assessment, the nurse determines that the client's leg is pale and cool, and no pulses are palpable in the left leg. After notifying the healthcare provider, which action should the nurse take? Keep client in bed in the supine position (anticoagulan therapy & rest) After the fourth dose of gentamicin sulfate (Garamycin) IV, the nurse plans to draw blood samples to determine 5 m,inutes before and 30 minutes after the next dose.peak and trough levels. When are the best times to draw these samples? When teaching diaphragmatic breathing to a client with chronic obstructive pulmonary (COPD), which information should the nurse provide? Place a small book or magazine on the abdomen and make it rise while inhaling deeply A client taking a thiazide diuretic for the past six months has a serum potassium level of 3. The nurse anticipates which change in prescription for the client? A potassiium supplement will be prescribed. A 20 year old female client calls the nurse to report alump she found in her breast. Which response is the best for the nurse to provide? Most lumps are benign, but it is always best to come in for an examination. Which intervention should the nurse implement for a female client diagnosed with pelvic relaxation disorder? Encourage the client to perform Kegel exercises 10 times daily. During a health fair, a 72 year odl male client tells the nurse that he is experiencing shortness of breath. Auscultation reveals crackles and wheezing in both lungs. Suspecting that the client might have chronic bronchitis, which classic symptom should the nurse expect this clien to have?" productive cough with grayish-white sputum. A client has taken steroids for 12 years to help manage chronic obstructive pulmonary (COPD). When making a home visit, which nursing function is of greatest importnace to this client? Assess the client's C Temperature over skin color and turgor steroids and infection A client has undergone insertion of a permanent pacemaker. When developing a discharge teaching plan, the nurse writes a goal of, "The client will verbalize symptoms of pacemaker failure. "Which symptom are the most important to teach the client? Feelings of dizziness In assessing a client diagnosed with primary hyperaldosteronism, the nurse expects the lab test results to indicate a decreased serum level of Potassiumwhich substance? The healthcare provider prescribes aluminum and magnesium hydroxde (maalox, 1 tablet PO PRN, for a client with chronic renal failure who is complaining of indigestion. What intrevention should the nurse implement? Question the healthcare provider prescription. (it can casue hypermagnesium) An elderly client is admitted with a diagnosis of bacterial pnuemonia. The nurse's assessment of the client is most likely to reveal which sign and symptom? Confusion and tachcardia A 67 year old woman who lives alone is admitted after tripping on a rug in her home and fractures her hip. WHic predisposing factor probably led to the fracture in the proximal end of her femur? Osteoporosis Question Answer Hint Abrubt Sudden Abstain Voluntarily refrain from something Access A means to obtain entry or a means of approach Accountable Responsible Adhere to hold fast or stick together Adverse Undesired, possibly harmful Affect Appearance of observable emotions Annual Once a year Apply To place, put on, or spread something Audible Able to hear Bilateral Present on two sides Cease To some to an end or bring to an end Compensatory To offset or make up for something Complication An undesired problem that is the result of some other event Comply Do as desired Concave Rounded inward Concise Brief, to the point Consistency Degree of viscosity, how thick or thin a fluid is Constrict To draw together or become smaller Contigent Dependant Contour Shape or outline of a shape Contract To draw together or reduce in size Contraindiction A reason why something is not advisable orwhy it shouldnt be done Defecate Expel a bowel movement Deficit A deficiency or lack of something Depress Press downward Depth Downward measurement from the surface Deteriorating Worsening Device Tool or piece of equipment Diameter The distance across the center or an object Dilate To enlarge or expand Dilute To make a liquid less concentrated Discrete Distinct, separate Distended Endlarged or expanded from pressure Elevate To lift up or place in a higher position Endogenous Produce within the body Exacerbate To make worse or more severe Excess More than what is needed or usual Exogenous Produced outside the body Expand To increase in size or amount Question Answer Hint When does birth weight double? 6 months When does birth weight triple? 12 months When does the posterior fontanel close? By 8 weeks When does a baby give its 1st social smile? 2 months When does a baby turn its head toward sounds? 3 months When does the Moro reflex disappear? 4 months When does a child achieve steady head control? 4 months When does a baby turn completely over? 5-6 months When does a baby transfer objects hand to hand? 7 months When does a baby play peek a boo for 1st time? After 6 months When does stranger anxiety develop? 7-9 months When does a child sit unsupported? 8 months When does a child crawl? 10 months When does a child’s fine pincer grasp appear? 10-12 months When does a child wave bye bye? 10 months When does a child walk with 10-12 monthsassistance? When does a child say a few words in addition to mama or dada? 12 months When does birth weight quadruple? 30 months When do you achieve 50% of adult height? 2 years What is the appearance of a toddler? Bowlegged and potbellied What are the teeth of a toddler (1-3 year old) like? All 20 primary teeth are present When does the anterior fontanel close? 12-18 months When does a child throw a ball overhand for 1st time? 18 months When can a child kick a ball? 2 yrs When does a child feed self with cup and spoon? 2 yrs When can daytime toilet training begin? 2 yrs When can kids form 2-3 word sentences? 2 yrs When can kids form 3-4 word sentences? \\ 3 yrs When can child state full name? 2.5-3 years When are temper tantrums common? Toddler (1-3) What is Erickson’s Theory of the toddler (1-3)? Developing a sense of autonomy What type of toys should you give to babies under 1 year old? Mobiles, rattles, squeaking toys, picture books, balls, colored blocks, activity boxes What happens to a baby under 1 whose parents are not able to stay with him? May be inconsolable due to separation anxiety What is Erickson’s Theory of infants under 1? Developing a sense of trust What are the toys appropriate for the toddler (1-3)? Board and mallet, push/pull toys, toy phone, stuffed animals, storybooks with pictures, use of the hospital playroom bc of mobility (which is important to their development). How much weight does a preschool child (3-5) gain each year/ inches grown each year? 5 lbs and 2-3 inches/year When do kids learn to run, skip, jump? Preschool How old are you when you start riding tricycle? 3 years old At what age is standing erect began? Preschool When do you establish handedness? PreschoolAt what age do you use scissors? 4 years old What age ties shoelaces? 5 years old At what stage do you learn colors and shapes? Preschool What is the visual acuity of a preschooler? 20/20 What is the thinking of a preschooler like? Egocentric and concrete When does a child learn sexual identity/curiosity/masturbation? Preschool When are imaginary friends and fears common? Preschool Aggressiveness at ___years old is replaced by independence at ___years old. 4, 5 What should you make sure a preschooler knows about their illness? They did not cause it, painful procedures are not punishment When is fear of mutilation from procedures common? How can you help restore body integrity? Preschool, put on a Bandaid What are appropriate toys for a preschooler? Coloring books, puzzles, cutting/pasting, dolls, clay, toys that let you work out hospital experiences What is Erickson’s Theory of Preschoolers? Developing a sense of initiative School age (6-12 year olds) have what weight/height gain per year? 4-6 lbs and 2 inches per year What is Erickson’s Theory of schoolagers? Developing a sense of industry When are primary teeth lost and permanent teeth established? school age At what age are you able to write script? 8 years Egocentric thinking in the school age child is replaced by _________. Social awareness of others When are cause and effect relationships learned? School age When does socialization with peers become important? School age When do molars erupt? School age (6 year molars) Whose growth spurt develops 1st? As early as what age? Girls-10 years old. Boys at 14. Adult-like thinking begins at what age? 15 When does growth end? Girl-15, boys-17 What is Erickson’s theory for Developing sense of identityadolescents (12 to 19)? After 6 months what is the baby’s concept of bodily injury? They can remember the pain What is the toddler’s concept of bodily injury? Fear of intrusive procedures What is the preschooler’s concept of bodily injury? Fear of body mutilation What is the school age childs concept of bodily injury? Fear of loss of control over their body What is the adolescent’s concept of bodily injury? Change in body image When can you start using the numeric pain scale? 9 and up How can a non verbal child be assessed for pain? Using the FLACC pain assessment tool, that looks at the face, leg movement, activity, cry, and consolability What are the best nondrug measures to reduce pain in infants? Pacifiers, holding, rocking What are the best nondrug measures to reduce pain in toddlers and preschoolers? Distraction What are the best nondrug measures to reduce pain in school age and adolescents? Guided imagery At what age can you teach a child how to use PCA? 5 years old When is MMR vaccine given? 12-15 months and then 1 other time between 4 and 12 years old During a measles epidemic when can you give the MMR? 6 months and then again at 15 months What are contraindications for MMR? Allergy to neomycin or eggs How do you administer the MMR vaccine? SQ at 2 difft sites After the MMR vaccine what is a normal finding? Light rash 2 weeks later When do you give the DTaP vaccine? At 2 months, 4 months, and 6 months. THEN get boosters at 15-18 months and again at 4-6 years. How do you give DTaP vaccine? IM apart from other vaccines When do you have to stop giving DTaP vaccine? At age 7, bc then you switch to Td vaccine After the injection of DTaP what should the nurse tell the parents to do? Give acetaminophen (Tylenol) When do you give the IPV vaccine? At 2 months and 4 months, THEN boosters at6-18months and again at 4-6 years old How do you administer IPV? SQ or IM at separate site from other vaccines What is the contraindication for IPV vaccine? Allergy to neomycin or streptomycin How and when do you administer Hib vaccine? IM at 2, 4, and 6 months When and how do you administer the HepB vaccine? IM at 0-2 months, 1-4 months, 6-18 months When and how do you give the varicella vaccine? 12-18 months –should be given with the MMR vaccine OR over 30 days apart What are normal side effects from DPT and IPV vaccinations? Irritability, fever under 102, redness and soreness at injection site for 2-3 days What can decrease soreness after thigh injections? Warm washcloth on injection sites, bicycling the legs with each diaper change How do you treat fever in a child with a communicable disease? NON-ASPIRIN PRODUCT What can you use for itching in communicable diseases? Diphenhydramine (benadryl) What is Rubeola (Measles)? How is it transmitted? When is it contagious? What are classic symptoms? Highly contagious, viral disease that can cause neurologic problems or death, transmitted by droplets; contagious mainly during prodromal period when they have fever and upper respiratory symptoms; symptoms include photophobia, Koplik’s spots in the mouth, rash starting on face and spreading downward. When is chicken pox no longer contagious? Once scabs have formed on all lesions What is German Measles? A viral disease that can kill babies in 1st trimester; spread by droplets and contact, a red maculopapular rash spreads from face to rest of body and fades in 3 days What is pertussis? Whooping cough; caused by bacteria prolonged coughing for 4-6 weeks; treated with erythromycin; complications are pneumonia, hemorrhage, and seizures How do you measure past nutrition in a child? Height and head circumference How do you measure current nutrition in a child? Weight, skinfold thickness, arm circumference How do you measure the body fat content of a child? Skinfold thickness What does vitamin B2 (riboflavin) deficiency look like? How do you treat it? Redness and itchiness of eyes, magenta tongue, delayed wound healing Give these kids green leafy veggies, liver, cow milk, cheddar cheeseWhat does vitamin A deficiency (retinol) look like? How do you treat these kids? Rough dry skin, cornea problems, retarded growth Give them orange foods (sweet potatoes, peaches, apricots) What are signs of dehydration in an infant/child? Poor turgor, depressed fontanels, no tears, dry mucous membranes, weight loss, decreasued urine output What are lab signs of metabolic acidosis (caused by dehydration)? pH under 7.3, low sodium and potassium, high Hct and BUN When should you add potassium to IV fluids? ONLY when the child has adequeate urine output What is the expected urine output for both infants and children per hour? 1-2 mL/kg/hr How many children die from child abuse each year? 3 to 5 thousand How should burns in children be assessed? Using the Lund-Browder Chart, which takes into account the changing proportions fo the child's body How can the nurse BEST evaluate adequacy of fluid replacement in children? Monitor urine output What interventions should be done FIRST when caring for a child who has ingested poison? Assess repiratory, cardiac, and neuro status What are the cardinal signs of respiratory distress in children, and other signs of resp. distress in kids? Cardinal signs: restless, inc respirations, inc pulse, sweating Other signs: flaring nostrils, retractions, grunting, bad breath sounds, accessory muscle use, head bobbing, low PO2, high PCO2, cyanosis, pallor Which usually occurs 1st: cardiac failure or respiratoy failure in children? Respiratory failure What is epiglottitis caused by? What is the classic position these kids are in? What do you NEVER do in these patients? HIB Upright sitting position with chin out and tongue protruding ("tripod position") NEVER examine the throat of this child!! What causes bronchiolitis? What lung sounds do you hear? What are their respirations like? RSV Wheezing and rales Respirations are shallow and fast What is given to kids under 2 yrs old born either premature or with lung/heart disease to give passive immunity to RSV? Synagis What is a risk of untreated otitis media? What do you see on assessment? What can you do to ear Conductive hearing loss Pulling at ears, fever, pain, enlarged lymph nodes, discharge from ear IF drum is ruptured, V/D Apply warmfor comfort? compress on ear How can you reduce body temperature in children to avoid seizure risk? Tepid bath or Tylenol Tonsillitis can be either bacterial or viral. If related to strep why is treatment so important? bc the child can develop acute glomerulonephritis or rheumatic heart disease Prior to tonsillectomy what lab values must be drawn? PT and PTT, assess for history of bleeding of family hx of bleeding disorders What are signs of postoperative tonsillectomy bleeding? when is highest risk for hemorrhage? These kids should NEVER be given what? Clearing throat, vomiting fresh blood, frequent swallowing 1st 24 hours and 5-10 days post surgery NO STRAWS! What is the drug of choice for an acute asthma attack? Epinephrine bc it is a rapid acting bronchodilator What are the normal PO2 and PCO2 values for kids in an arterial blood gas draw? PO2: 83-100 PCO2: 35-45 What nutritional support should be given to a child with CF? pancreatic enzyme replacement, fat soluble vitamins, low carb, high protein, moderate fat diet What type of genetic disease is CF? autosomal recessive How do you care for a child in a mist tent? Monitor temperature. Keep clothing dry. Keep tent edges tucked in, assess respiratory status. An increased respiratory rate in kids puts them at risk for _____________. dehydration and acid/base imbalance What is a patent ductus arteriosus? Hole between the aorta and pulmonary artery, which normally closes within 72 hours postbirth. If it stays open blood from the aorta returns to the pulmonary artery, resulting in increased blood flow to the lungs and pulmonary hypertension. Describe acyanotic defects. Examples They can be 1 of three things: 1. L to R shunts 2. Increased pulmonary blood flow 3. Obstructive defects VSD, ASD, PDA, AS, and coarctation of the aorta Describe cyanotic heart defects. Examples They can be either: 1. R to L shunts 2. Decreased pulmonary blood flow 3. Mixed blood flow The 3 T's: Tetralogy of Fallot, TA, TGV What is a ventricular septal defect? Acyanotic Blood from the L ventricle is shunted to the R ventricle through a hole and recirculated to the lungs, resulting in increased pulmonary blood flow What is an atrial septal defect? Oxygenated blood from the L atrium is shuntedinto the R atrium and lungs through a hole , resulting in increased pulmonary blood flow. What is a coarctation of the aorta? It is a narrowing of the aorta which causes HTN in the upper extremities and decreased/absent pulses in the lower extremities. What is aortic stenosis? A narrowing at or around the aortic valve; Oxygenation to the systemic circulation is poor bc cardiac output is low. What is a common finding in children with cyanotic heart defects (3 T's)? polycythemia What is truncus arteriosus? When the pulmonary artery and aorta do not separate. The blood from the 2 ventricles mix and causes cyanosis What is transposition of the great vessels? Incompatible with life, a medical emergency where babies recieve prostaglandin E to keep ductus open. Is CHF associated more with cyanotic or acyantoic defects? acyanotic MANAGING DIGOXIN: 1. Before giving digoxin what must the nurse do? 2. What are therapeutic levels? What is an early sign of digoxin toxicity? What electrolyte imbalance increases digoxin toxicity? 1. Take child's apical pulse. If bradycardic do not administer. 2. 0.8-2.0ng/mL 3. Throwing or spitting up 4. Hypokalemia Rheumatic fever is an _______disease. It is the most common cause of ________ in children. It is associated with an infection of ________. Rheumatic fever is a collagen disease that injures _________. Inflammatory Acquired heart disease Bhemolytic strep bacteria Heart, blood vessels, joints, subQ tissue What assessment findings are associated with rheumatic fever? Lab values? Chest pain, SOB, tachycardia ALL the time, joint pain, chorea (involuntary movements), rash, subQ nodules over bony prominences, fever Increased Erythrocyte sedimentation rate, increased ASO titer (anistreptolysin O). What medications are used to treat rheumatic fever? Penicillin, eryhtromycin, and aspirin In ____________ (a type of congenital heart defect) the child often experiences "tet spells" (_________), which are relieved by which position? Tetralogy of Fallot hypoxic episodes squatting or knee chest position What is the nurse's goal in caring for kids with Down Syndrome? help the child reach its OPTIMAL level of functioning What is cerebral palsy? Its major risk factor? An injury to the motor centers of the brain causes neuromuscular problems of spaasticityor dyskinesia (involuntary movements) Low birth weight What is "scissoring" a characteristic of? Cerebral Palsy; it occurs when legs are extended and crossed over each other with feet plantar flexed. If a mother of a Cerebral Palsy child says she is having "difficulty with diapering," what is the mom describing? Spasticity What should the nurse do while feeding a cerebral palsy child? Prevent aspiiration by sitting the child upright and supporting the lower jaw What is the most common allergy of kids with spina bifida? Latex What are 2 nursing priorities for the infant with myelomeningocele? 1. Prevent infection of the sac 2. Monitor for hydrocephalus (measure head circumference, assess fontanel, and neuro functioning). What is hydrocephalus and assessment findings? Accumulation of CSF within the brain and is often associated with spina bifida or meningitis Symptoms: Increased ICP (low pulse, high BP), change in LOC, vomiting, seizures, bulging fontanels, widening suture lines, sunset eyes What is the surgery like for kids with hydrocephalus? A shunt is inserted into the brain ventricle and tubing is then tunneled through skin to the peritoneum where excess CSF is drained out Seizures are more common in what age group? Under 2 yrs old Describe tonic clonic seizures (grand mal). You get an aura. Then you lose consciousness and the body becomes stiff (tonic). Then you stop breathing and become cyonotic before you go into spasms (clonic) and relax. Pupils will be dilated and nonreactive to light, incontinent, and then you lay there sleepy and disoriented Describe absence seizures (petit mal). Usually occur between 4 anbd 12 years old. You lose consciousness for 5-10 seconds and appear to be daydreaming because posture is kept and you get minor face and hand movements. These kids may be doing poorly in school. What is the most common cause of increased seizure activity? Medication noncompliance What do you see in older children with bacterial meningitis (normally caused by HIB)? ICP, fever, chills, neck stiffness, opisthotonos, photophobia, positive Kernig's Sign (inable to extend leg when knee is bent toward chest), positive Brudzinski's sign (neck flexion causesflexion movements of lower extremities) What do you see in infants with bacterial meningitis? BULGING FONTANELS, poor feeding, vomiting, irritable, seizures With meningitis it is important to monitor hydration status and IV therapy. Why? Bc with meningtitis there may be inappropriate secretions of ADH, causing fluid retention (cerebral edema) and dilutional hyponatremia What antibiotics are usually prescribed for bacterial meningitis? Ampicillin, penicillin, chloramphenicol How do kids usually get Reye's syndrome? ASA + chicken pox/influenza What is the most common presenting symptom of brain tumors? Headache upon awakening How is a child usually positioned after brain tumor surgery? flat on his or her side What is the mechanism for inheritance of Duchenne muscular dystrophy? it is an x-linked recessive trait affecting mostly males What is "Gower's sign?" An indicator of muscular dystrophy; difficulty moving to standing position-child has to walk up legs using hands to stand up. What is the first sign of renal failure? Decreased urine output What are the symptoms of acute glomerulonephritis? Dietary interventions? blood in urine, recent strep infection, HTN, mild edema around eyes, positive ASO titer low sodium diet what are the symptoms of nephrosis? dietary interventions? severa edema, massive proteinuria, frothy urine, anorexia, negative ASO titer high protein AND low salt Decribe safe monitoring of prednisone administration and withdrawal? Give prednisone every other day, signs of ededma/mood changes/GI distress should be reported; the drug should always be tapered. How can you prevent Urinary Tract Infections in kids? avoid bubble baths, pee a lot, drink lots of fluids (especially acidic ones), wipe from frant to back what is the vesicoureteral reflex? When urine backflows from the bladder up into the ureters. Recurrent UTIs are common. What do you see in a kid with Wilms Tumor? Mass at midline on abdomen, fever, pallor, lethargy, high BP (bc of excess renin secretion) What is THE MOST IMPORTANT thing for a nurse to do w/ a child who has Wilms Tumor? Prevent injury to the capsulated tumor by making sure noone palpates the abdomen. What is hypospadias? Why is surgical correction usually done before preschool? When the urethra opens on the ventral side of the penis behind the glans To schieve sexual identity, toilet training, and remove the fear of castration anxiety When is closure of cleft lip normally When the baby weighs 10 pounds and has Hgbperformed? After surgery how is child positioned? of 10g/dL. on side or upright in car seat (NOT PRONE) When is closure of cleft palate usually performed? After surgery how is the child positioned? 1 year of age to minimize speech impairment on side or abdomen How can you protect the surgical site on a child with cleft lip/palate? Apply elbow restraints, minimize crying, maintain Logan Bow to lip if applied What is an esophageal atresia with tracheoesophageal fistula? When the upper esophagus ends in a blind pouch with the lower esophagus connected to the trachea. It is a MEDICAL EMERGENCY!! In tracheoesophageal fistula what do you see on assessment? The 3 c's (coughing, choking, cyanosis), exxcess salivation, resp. distress, aspiration pneumonia What nursing actions are initiated for a child suspected of having esophageal atresia with tracheoesophageal fistula? NPO immediately and suction secretions What are the feeding techniques for a child with cleft lip/palate? Feed upright with lamb's nipple or prosthesis. Use frequent bubbling. What assessment findings do you see in kids with pyloric stenosis? Projectile vomiting, constant hunger, weight loss, dehydration, palpable olive shaped mass in RUQ, visible walves of peristalsis What lab values are seen in kids with pyloric stenosis? Low sodium, low potassium, metabolic alkalosis (low chloride, increased ph, increased CO2) What is postoperative nursing care for a child with pyloric stenosis? IV hydration, small frequent feedings of oral glucose or electrolyte solutions, gradually increasing to full strength formula. Position ON RIGHT SIDE in semi fowlers after feedings What assessment findings do you see in a child with intussusception (when 1 part of intestine telescopes into another part of intestine)? Intermittent abdominal pain, screaming when legs are pulled toward abdomen, "currant jelly stools" (blood +mucus), sausage shaped mass in RUQ with empty RLQ (Dance sign) Why is a barium enema used to treat intussusception? It reduces intestinal telescoping via hydrostatic pressure instead of surgery What is Hirschsprung's Disease? Lack of persitalsis in area of colon where ganglion cells are missing. Fecal matter accumulates above this area. What do you see when assessing a Hirschsprung's Disease child? How do you take their temperature? Failure to pass meconium in 1st 24 hours, distended abdomen, ribbon like stools Take axillary temperature. What are signs of anorectal malformation? Failure to pass meconium in 24 hours, meconium appearing from a fistula or in the urine, an unusual anal dimple What are the Hgb norms for: 1. Newborn 2. Infant 3. Child Newborn 14-24 Infant 10-15 Child 11-16What are assessment findings in kids who have iron deficiency anemia? Pale, fatigue, milk intake over 32oz/day, pica, low Hgb, Low serum iron values What is the genetic transmission pattern of hemophelia? x-linked recessive transmitted by the mother and expressed by male offspring. These children are missing factors 8 or 9. What are assessment findings in a child with hemophelia? Never give these kids______. Prolonged bleeding(after circumcision or in general); loss of motion in joints, prolonged PTT Aspirin Describe autosomal recessive transmission and give examples. Both parent must be heterozygous carriers of the trait. Each child has a 1 in 4 chance of having the disease. ex.) sickle cell, CF, PKU Describe X-linked recessive transmission. Give an example. The trait is carried on the X chromosome, so it usually affects male offspring. With each pregnancy of a woman who is a carrier there is a 25% chance of having a child with the disease. If male there is a 50% chance of getting disease. If female there is a 50% chance of being a carrier. ex.) hemophelia What is the sequence of events in a vasooclusive crisis of sickle cell anemia? RBCs clump together and block small blood vessels. Cells cannot get through the capillaries, causing pain and ischemia. Lowered O2 affects the HgbS and causes sickling. Why is hydration a priority in treating sickle cell disease? Hydration promotes hemodilution and circulation of RBCs through the blood vessels What should families and clients do to prevent sickle cell episodes? Keep hydrated, avoid high altitudes, avoid strenuous exercises, avoid unknown sources of infection Do you give supplemental iron to kids with sickle cell anemia? No, bc it is not caused by iron deficiency. You DO give them folic acid, however, to stimulate RBC synthesis. Nursing interventions and medical treatment for a child with leukemia are based on which 3 physiological problems? Anemia (decreased RBCs), Infection (neutropenia), and bleeding thrombocytopenia (decreased platelets) What should you have nearby when administering l-asparaginase to a leukemic patient? Epinephrine and oxygen in case of anaphylaxis An infant with ________is often described as a "good, quiet baby" by the parents. Hypothyroidism What do you see in children with hypothyroidism? sleepy, poor feeders, flat expression, constipations, hypoactive What are the outcomes of untreated congenital hypothyroidism? Mental retardation, growth failure What is phenylketonuria? What is the An autosomal recessive disorder where theresult of PKU? body cannot metabolize the aa phenylalanine The buildup of phe leads to CNS damage (mental retardation) and decreased melanin On assessment of a child with PKU what do you see? Newborn screening using Guthrie test is positive when serum phenylalanine is 4mg/dL or higher. Vomiting, failure to gain weight, hyperactive, musty urine odor What are foods high in phenylalanine (which should be avoided if you have PKU)? high protein foods including meat, dairy, eggs, aspartame. This low protein diet should be done until brain growth is complete (6-8 years old). What 2 formulas are prescribed for kids with PKU? Lofenelac and PKU-1 What are the 3 classic signs of diabetes? Polydipsia, polyuria (including bedwetting-"enuresis"), polyphagia Diabetes is diagnosed if the fasting blood sugar is greater than_____mg/dl. 120+ What do you do if a diabetic child is in ketoacidosis? Provide care for unconscious child, administer REGULAR insulin IV in Normal Saline, monitor blood gases, maintain strict I&O What are the signs and symptoms of hypOglycemia? tremors, sweating, headache, hunger, nausea, lethargy, confusion, slurred speech, anxiety, tingling around mouth, nightmares What are the signs and symptoms of hypERglycemia? polydipsia, polyuria, polyphagia, blurry vision, weight loss, weakness, syncope What is the relationship between hypOglycemia and exercise? During exercise insulin uptake is increased and the risk for hypOglycemia occurs. What is a complete fracture? When bone fragments completely separate What is an incomplete fracture? When bone fragments remain attached Wha is a comminuted fracture? When bone fragments of the bone shaft break free and lie in surrounding tissue. Rare in children. What type of fractures have serious consequences in terms of growth of the affected limb? Fractures involving the epiphyseal (growth) plate What re the 5 "P's" that may indicate ischemia in the fractured limb? pain, pallor, pulselessness, paresthesia (pins and needles), paralysis What is a skin traction? Force is applied to the skin. This should NEVER be removed unless specifically prescribed by the MD What is Buck's Skin Traction? For the lower extremities; keeps legs extended with no hip flexion. What is Dunlop Skin/Skeletal Traction? When there are 2 lines of pull on the arm What is Russell Skin Traction? 2 lines of pull on lower extremity (1perpendicular, 1 longitudinal) What is Bryant's Skin Traction? Both lower extremities are flexed 90 degrees at hips (rarely used bc extreme elevation of legs causes decreased peripheral circulation) What is a skeletal Traction? When a pin or wire applies pull directly to the distal bone fragment What is a 90 degree skeletal traction? 90 degree flexion of the hip and knee. The lower leg is in a boot cast. This can also be used on upper extremities. What is a hip spica? How do you help with toileting a child with a hip spica? A special type of cast used to immobilize the hip joints and/or the thigh Use Bradford frame under the child. NEVER USE abduction bar to turn a child. What is compartment syndrome? Assessment findings? Damage to nerves and vasculature of an extremity due to compression. You see coldness, severe pain, inability to move extremity, poor capillary refill What are the signs and symptoms of congenital hip dysplasia in infants? Unequal skin fold of buttocks, positive Ortalani Sign (clicking with abduction), limited abduction of affected hip, unequal leg lengths What are signs of hip dysplasia in older children? Limp on affected side, positive Trendelenburg Sign (when standing on one leg the pelvis drops on the side opposite to the stance leg. ) How does the nurse conduct scoliosis screening? Ask child to bend forward from hips with arms hanging free. Examine child for curvature of the spine, rib hump, and hip asymmetry What instructions should the child with scoliosis receive about the Milwaukee brace? Wear it 23 hours each day. Wear t-shirt under brace. Check skin for irritation. Perform back and abdominal exercises. Modify clothing. Maintain normal activities as able. A brace does not correct the curve of a child with scoliosis. It only stops or slows the progression. What is the potential outcome for untreated scoliosis? respiratory difficulty What is postoperative nursing care of a child with scoliosis? Frequent neuro assessments, log roll for 5 days, keep npo, monitor NG tube/bowel sounds Describe log rolling. Used postoperatively for scoliosis patients. Requires 2+ people. Client is moved on a draw sheet to the side of the bed away from which they are to be turned (rolled toward the L if they are to face the R). Client is the turned in a simultaneous motion, maintaining the spine in a straight position. Pillows arranged for support and comfortWhat nursing care is indicated for a child with juvenile rheumatoid arthritis? Prescribed exercise to maintain mobility, splinting of affected joints, teach medication management and side effects [Show More]
Last updated: 1 year ago
Preview 1 out of 227 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 07, 2022
Number of pages
227
Written in
All
Additional information
This document has been written for:
Uploaded
Oct 07, 2022
Downloads
0
Views
183