*NURSING > QUESTIONS & ANSWERS > Educode_4 HIM 432 complete correct questions and answers (All)
Educode_4 HIM 432 complete correct questions and answers
Document Content and Description Below
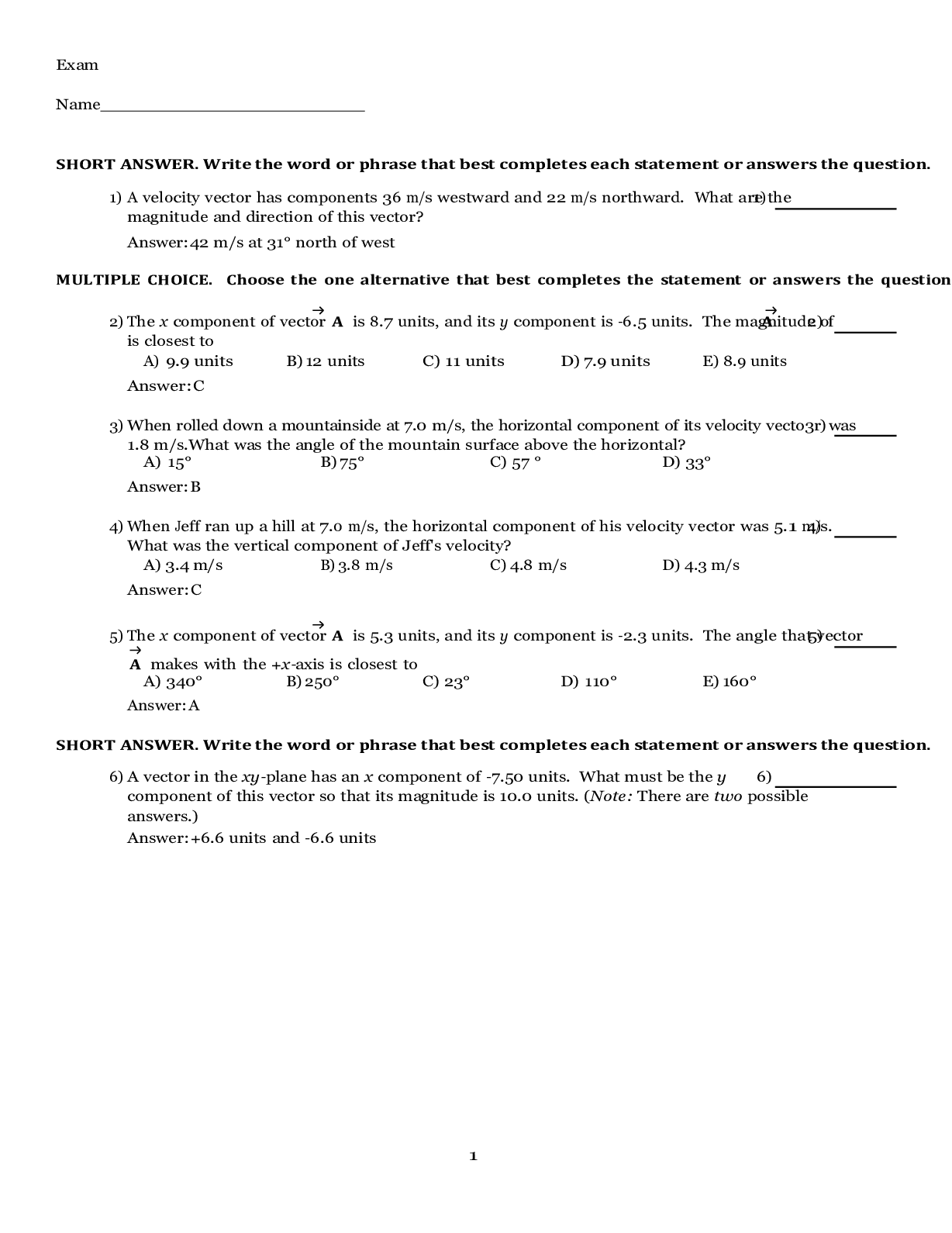
Educode_4 HIM 432 Lesson 1 ________________________________________ Question 1: How many lobes are in each lung? Question 2: What codes are assigned to the diagno... sis "acute and chronic maxillary sinusitis due to Enterococcus infection?" Question 3: For Chapter 10, if a provider documents tobacco use, code Z72.0 should be assigned as a secondary code following which codes? Select all that apply. Question 4: What is the correct coding for the diagnosis "suspected novel influenza A with laryngitis and associated acute frontal sinusitis?" Question 5: What is the coding and sequencing for the diagnosis "Pneumonia due to H. influenza with novel influenza A complicated by viral gastroenteritis?" Question 6: What is the ICD-10-CM coding for "pneumonia due to Streptococcus pneumoniae?" Question 7: What is the diagnosis coding for "Chronic obstructive asthma with acute exacerbation?" Question 8: Which tests or devices are used to measure the level of oxygen and carbon dioxide in the blood? Select all that apply. Question 9: A patient is admitted with status asthmaticus and immediately placed on mechanical ventilation. On the fourth day, the progress notes state "pneumonia." A sputum culture shows Pseudomonas. The final diagnosis is "ventilator-associated pneumonia due to Pseudomonas mallei, severe persistent status asthmaticus." What is the correct diagnosis coding and sequencing for this case? Question 10: Which diagnostic statement for the type of influenza could be coded and reported as confirmed with a specific code from category J09 or J10? Select all that apply. Chapter 10 chapter-specific guideline I.C.10.c of the ICD-10-CM Official Guidelines for Coding and Reporting, Influenza due to certain identified influenza viruses, instructs to code only confirmed cases of influenza due to certain identified influenza viruses (category J09), and due to other identified influenza virus (category J10). Cases reported as suspected are coded to category J11and SARS-associated coronaviral influenza pneumonia is reported in category J12. Lesson 2 ________________________________________ Question 1: A patient is diagnosed with "asthmatic bronchitis with acute exacerbation." What code is assigned for this diagnosis? Question 2: Which of these codes is an unlikely reason for inpatient admission? Question 3: COPD is a major cause of disability and the third-leading cause of death in the United States. What are the major causes of COPD in the United States? Question 4: A patient receives a diagnosis of "exacerbation of extrinsic asthma." What code is assigned to this patient? Question 5: What are the components of mucopurulent chronic bronchitis? Select all that apply. Question 6: An older patient who is severely allergic to cat dander visits his niece. He didn't know she is currently fostering three cats and he subsequently develops an acute exacerbation, resulting in a trip to the emergency department and short-stay admission. His diagnosis is "allergic bronchitis with exacerbation." What is the coding for this case? Question 7: A patient, age 65 with known chronic bronchitis, is admitted with chest pain, which the patient states has been ongoing. He is admitted to rule out a myocardial infarction. After study, the chest pain is documented as due to chronic tracheitis, and the patient is discharged with the diagnosis "chronic tracheobronchitis, simple chronic bronchitis." What code is assigned for this case? Question 8: A patient with known emphysema is admitted with extreme breathlessness. He continues to smoke cigarettes, despite being on home oxygen therapy, claiming "everyone has to die someday." A CT scan shows alveolar destruction in the upper half of the lungs and bullous emphysema. The diagnosis is "nicotine-induced bullous centrilobular emphysema, nicotine dependence, depressive neurosis." Which sequence of codes is assigned to this case? Question 9: What is the clinical definition of chronic bronchitis? Question 10: An emergency department patient is admitted for observation. The provider documents "acute bronchitis with bronchiectasis with exacerbation of bronchiectasis." Which sequence of codes should be assigned? Lesson 3 ________________________________________ Question 1: A patient is admitted with pneumonia and placed on intravenous antibiotics. Three days later, he develops respiratory distress and is placed on mechanical ventilation for acute respiratory failure. The acute respiratory failure was not present on admission, but the patient is on the ventilator for 4 days. The final diagnosis is "pneumonia and acute hypoxemic respiratory failure requiring intubation and mechanical ventilation." Which sequence of codes should be assigned? Question 2: After being admitted with acute hypercapnic respiratory failure, a patient is intubated and placed on mechanical ventilation. Work-up reveals gram-negative Pseudomonas in her blood, and she is diagnosed with sepsis due to Pseudomonas and septic shock. What is the coding and sequencing for this case? Question 3: A patient is admitted with a diagnosis of "respiratory failure." His ABG test results show a low oxygen level, which clinically corresponds to his acute lung disease (pneumonia). The patient is treated with antibiotics and BiPAP. Without any further information available, what code should be assigned for "respiratory failure"? Question 4: A patient, age 55, is diagnosed with acute hypercapnic respiratory failure. Which finding is a characteristic of acute hypercapnic respiratory failure? Select all that apply. Question 5: A patient with a history of COPD and chronic respiratory failure is admitted for treatment of lobar pneumonia, and acute respiratory failure develops after admission. Her final diagnosis is pneumonia with additional diagnoses of acute exacerbation of COPD, acute and chronic hypoxemic respiratory failure. Which sequence of codes should be applied? Question 6: Respiratory failure is not a disease but results from other conditions or diseases that cause impaired lung function. When treating respiratory failure, it is important to treat the underlying cause and the threat to organ function. Question 7: A patient who sustained a traumatic brain injury after falling off a cliff has completed treatment of the acute conditions he suffered. He has chronic respiratory failure with hypercapnia and has had a tracheostomy tube inserted. Because he requires mechanical ventilation for the foreseeable future, he is transferred to a rehabilitation facility with a ventilator unit. What codes are assigned for the respiratory and respiratory-related diagnoses? Question 8: A patient is admitted to the ICU with traumatic injuries to the chest and abdominal organs that were sustained in an automobile accident. Twelve hours after admission, the patient experiences respiratory distress. ABG test results indicate a low oxygen level in the blood. The patient is intubated and placed on mechanical ventilation and receives a diagnosis of "acute respiratory distress syndrome." What code is assigned for this condition? Question 9: A patient is admitted from same-day surgery with acute respiratory failure. The provider documents "acute postprocedural respiratory failure." How is this coded? = Question 10: A patient with a history of cigarette smoking has COPD. She is dependent on supplementary oxygen at home and continues to smoke. While at the provider's office for a routine pulmonary function test (PFT), the patient is suddenly unable to complete the test, turns cyanotic, and reports difficulty breathing. She is immediately brought to the ED and admitted with the provisional diagnosis of "acute respiratory failure." The patient is placed on oxygen, given an intravenous anticoagulant, and after 2 days is discharged home to resume supplementary oxygen. The final diagnosis is "acute respiratory failure, exacerbation of COPD." How is this coded? Lesson 4________________________________________ Question 1: Which cells or structures listed below are classified as skin appendages? Select all that apply. Question 2: Given the diagnostic statement "Acute cyanotic respiratory failure and severe hives due to adverse effect of skeletal muscle relaxant," what conditions would be reported with an individual diagnosis code? Select all that apply. Question 3: What is the coding sequence for the following diagnostic statement: "Healed stage 3 pressure ulcer of the right lower back, stage 4 pressure ulcer of the sacral region with gangrene?" Question 4: What is the correct coding and sequencing for the following diagnostic statement: "Abscess of the left hand due to a MRSA infection"? Question 5: A patient has a nonhealing skin ulcer of the right heel due to postthrombotic syndrome. Bone necrosis due to the ulcer is documented. What is the coding and sequencing for this case? Question 6: During evaluation for admission for congestive heart failure, a patient complained of an extremely uncomfortable skin irritation covering the palms of both hands. Before admission earlier in the day, he had petted his friend's cats. The provider ordered a topical steroid cream to relieve the itching and swelling for this contact dermatitis. The provider documented that the patient likely was suffering from this condition due to having touched the cat. Which code is assigned for this condition? Question 7: What is the purpose of a skin culture? Question 8: During an inpatient stay, a medication order for a topical ointment is noted in the physician orders. On further investigation, the coder determines that this particular ointment is prescribed for fungal infections of the skin. The history and physical report notes a reddened, foul-smelling area of the right big toe. What is reported for this condition treated with the ointment? Question 9: If a patient is admitted with a stage 1 pressure ulcer of the sacral region and during their stay the sacral pressure ulcer progressed to stage 3, assign the code for the highest stage of pressure ulcer for that site. Question 10: Jon is a 35-year-old morbidly obese male with a body mass index of 42. He has a stage 4 pressure ulcer with an area of gangrene located on his right heel. What is the coding and sequencing for these conditions? Lesson 5 ________________________________________ Question 1: Which tissue layer anchors the skin to the other organs, is composed of fat and connective tissue, and also contains nerves and blood vessels? Question 2: Which stage of a pressure ulcer is described as an ulcerated area that extends below the surface of the skin, forming a crater? Question 3: Common underlying conditions that can lead to non-pressure ulcers are which of the following? Select all that apply. Question 4: A patient is admitted with a stage 3 pressure ulcer of the right hip with gangrene surrounding the area. He also has a stage 2 sacral decubitus ulcer. What is the coding and sequencing for this case? Question 5: A patient is diagnosed with atherosclerosis of native arteries of the lower extremities, with a nonhealing ulcer with associated skin breakdown over the left ankle. What is the coding for this case? Question 6: A 65-year-old man who developed a stage 4 decubitus ulcer on his left buttock while immobilized following major surgery presents to the ED with fever and chills. He reports the lesion has worsened over a 6-week period and, during the course of the hospitalization, is found to be infected with methicillin-resistant Staphylococcus aureus (MRSA). What is the coding for this case? Question 7: A 67-year-old man with a long history of chronic nonhealing venous right calf ulceration is a cigarette smoker with tobacco dependence and also has hypertension. The skin surrounding the ulceration is dry and scaly, with a degree of hyperpigmentation and inflammation around the wound margins. He is admitted for IV antibiotics and surgical consultation for possible debridement. What is the diagnosis coding and sequencing for this case? Question 8: A patient is admitted from a nursing home with pneumonia following a long period of immobilization due to hip surgery for a fracture. Also noted in the history and physical is "an area over the sacrum with partial-thickness skin loss of epidermis." Admission diagnoses: Pneumonia, dementia, sacral decubitus ulcer. How will the coder report this case? Question 9: A 55-year-old woman with type 2 diabetes is a direct admission from her physician's office because of gangrenous toes with necrotic muscle on the left foot due to non-healing ulcers. She has a long history of diabetic peripheral vascular disease. After a surgical consult, the patient is scheduled for amputation of the toes. What is the coding and sequencing for this case? Question 10: The patient is an elderly woman with dementia who was brought to the ED for a suspected hip fracture. She is evaluated and found to have a left trochanteric fracture, dementia, malnourishment, stage 1 pressure ulcer on right buttock. She undergoes surgical repair of the fracture. On Day 5, the ulcer is noted to be stage 2 and the wound care staff begins treatment. Which of the following statements is correct for this case? Lesson 6 ________________________________________ Question 1: A patient was discharged from the hospital with the diagnosis of acute left humeral osteomyelitis due to the hematogenous spread of Staphylococcus aureus. What is the correct diagnosis coding for this case? Question 2: A 29-year-old woman presents to the ED after she felt a pop in her hip and was unable to ambulate due to pain. The patient reports that approximately 3 weeks before admission, she had experienced a sudden and significant thigh pain while climbing a ladder. An x-ray taken at that time was normal, but the pain continued to worsen. Upon examination, a CT scan and x-ray show a right femur fracture, destruction of the outer layer of the bone, and a mass in the soft tissue next to the fracture. A biopsy of the bone and soft tissue leads to a diagnosis of osteomyelitis with an abscess caused by Streptococcus (S.) milleri. The patient may have bruised her thigh, causing the accumulation of blood, which may have become infected with S. milleri from tooth decay. The bacterial infection caused bone destruction, which resulted in the fracture and abscess. The fracture is surgically stabilized and subsequently healed. Which of the following codes would be reported for the fracture? Question 3: A 45-year-old sedentary man presents to the office with a painless hard lump in the medial aspect of the right knee. He has no history of trauma, and further workup results in the lump being diagnosed preoperatively as a benign soft tissue tumor. On the day of surgery, the patient is found to have an old vertical bucket-handle tear of the posterior horn of the medial meniscus. The fragment had detached at the posterior horn, everted, and presented as a subcutaneous lesion over the anteromedial parapatellar region of the knee. Which of the following codes would be reported for the tear? Question 4: The following conditions are assigned the same code, M51.16: Degeneration of L5 with radiculopathy Displacement of L5 with radiculopathy Question 5: Rheumatoid arthritis is a chronic, systemic, inflammatory disease of unknown cause. Which code block contains the code for rheumatoid arthritis for sites other than the spine? Question 6: Which tests may be used to diagnose a musculoskeletal condition? Select all that apply. Question 7: The patient is a man with a history of longstanding back, buttock, and bilateral leg pain. He was evaluated and found to have bilateral pars defects at L5-S1 with spondylolysis, and spinal instability with radiculopathy in the same area. What is the diagnosis coding for this case? Question 8: The patient has a long-standing ongoing diagnosis of systemic lupus erythematosus with musculoskeletal system involvement. Exam today reveals positive tenderness in the lateral epicondyles of both elbows, no effusion, which is consistent with the diagnosis of epicondylitis, both elbows secondary to a flare up of the patient's systemic lupus erythematosus. What is the diagnosis coding for this case? Question 9: Code the following diagnosis: Acute nontraumatic slipped upper femoral epiphysis with chondrolysis of the left hip. Question 10: The patient has a 6 year history of gout presented in the ED complaining of swollen and tender right great toe and right knee. Exam remarkable for a small effusion over right knee and tophi noted over right great toe. X-rays of her knees noted narrowing of joint space with effusion on right side. UA 8.3mg/dL, aspiration of her right knee demonstrated cell count of 15K and presence of urate crystals consistent with the diagnosis of idiopathic chronic gout of lower extremity involving both knees and right great toe. What is the correct diagnosis code for this case? Lesson 7 ________________________________________ Question 1: Which tests are used to diagnose osteomyelitis? Select all that apply. ] Question 2: Smoking and heavy use of alcohol are risk factors for osteoporosis. Question 3: The patient is a 15-year-old girl who sustained a trivial fall while playing volleyball. She presents to the emergency department complaining of severe right thigh pain and inability to bear weight. There is an obvious deformity and significant edema in the right thigh. She also keeps the right lower extremity externally rotated. Her mother reports that she had an episode of pain in the right thigh about 3 months ago that resolved. No other injuries are reported. There is no significant past medical history. She does not take any medication and denies having any recent fevers or illnesses. Biopsy of the lesion is done, and histology is consistent with osteosarcoma. Diagnosis: Pathological mid-shaft right femur fracture. What is the coding for this visit? (Do not code the external causes codes.) Question 4: A 71-year-old woman is admitted to the hospital with an admitting diagnosis of acute hip pain. There is no history of trauma. She states that she stood up from a chair and immediately experienced acute pain in the left leg. She has known osteoporosis and is a type 2 diabetic. An x-ray reveals a fracture of the upper left femur. The physician documents a spontaneous fracture secondary to osteoporosis. What are the diagnosis codes for this visit? Question 5: The patient is an 85-year-old man who is admitted for chest pain to rule out acute myocardial infarction. Two weeks prior to admission, he had a respiratory infection that caused excessive coughing. On evaluation, there is no evidence of cardiac infarction, and his chest pain is ruled to be due to costochondritis secondary to excessive coughing. Discharge diagnosis: Costochondritis. What is the coding for this encounter? Question 6: A 57-year-old right-hand-dominant Caucasian gentleman presents with history of a painful boil located on the dorsum of the left distal forearm that has been discharging intermittently for over 6 months. The patient reports the problem started with pain, redness, and swelling, and then progressed to form an abscess. He underwent multiple incision and drainage procedures under local anesthetic in the office of his primary care physician, along with at least eight courses of oral antibiotics. On physical examination, a discharging sinus on the dorsum of the distal left forearm is noted. There is an area of surrounding erythema with serous discharge noted from the sinus. Plain radiographs of the left wrist reveal a radiolucent area in the distal radius metaphysis measuring 2.7 mm in diameter. The lesion is well-circumscribed with some surrounding sclerosis. Routine laboratory investigations reveal elevated white count and erythrocyte sedimentation rate. The patient subsequently is admitted for surgical treatment. Final diagnosis: Brodie's abscess, left forearm. What is the coding for this case? Question 7: The patient is a 58-year-old woman who is admitted for a planned right total hip replacement. About 2 years ago, the patient suffered a fractured femoral neck as the result of a motor vehicle accident. The fracture was repaired at the time with an intramedullary nail. The nail was causing pain and was removed about 4 months ago. Since then the patient has had pain in the hip, and most recently the pain has become severe. Admission diagnosis: Osteonecrosis right hip due to previous injury. What is the coding for this visit? Question 8: The patient is a 49-year-old obese man with type 2 diabetes who takes Actos to control his hemoglobin A1c. He is 6 feet, 1 inch tall and weighs 275 pounds, and his BMI is 36.3. His physician recently diagnosed him with drug-induced osteoporosis secondary to the Actos. He presents to the emergency department after tripping on his carpet and experiencing immediate pain in his left foot. X-rays indicate a foot fracture. The patient is admitted for surgical repair of the fracture. Admission diagnoses: Pathological metatarsus fracture due to osteoporosis, uncontrolled diabetes. What are the diagnosis codes for this admission? Question 9: The patient is a 66-year-old woman who experienced a small blister on her right hand several weeks ago after raking leaves in her yard. She did not seek treatment at that time but noticed the blister progressively getting worse. She tried putting topical ointments on the wound, but it failed to improve. This morning, the patient awoke with a high fever, chills, malaise, and the right hand is warm and erythematous, with a deep open wound. A CT shows possible bone involvement, and she is admitted now for possible acute osteomyelitis due to suspected methicillin-resistant Staphylococcus aureus (MRSA), because she has a history of MRSA infections in the past. What is the coding for this visit? Question 10: Osteochondritis in diabetes is coded in the M90 category with an additional code for the diabetes. [Show More]
Last updated: 2 years ago
Preview 1 out of 25 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 14, 2021
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Jan 14, 2021
Downloads
0
Views
112

.png)