Genitourinary, gynecologic, renal and acid/base conditions
o Carcinoma of the Cervix
Increased risk in women who smoke and those with HIV or high-risk HPV types.
Considered a sexually transmitted disease as both sq
...
Genitourinary, gynecologic, renal and acid/base conditions
o Carcinoma of the Cervix
Increased risk in women who smoke and those with HIV or high-risk HPV types.
Considered a sexually transmitted disease as both squamous cell and adenocarcinoma of the cervix are secondary to infection with HPV; squamous cell accounts for 80 percent of cervical cancers, 15 % adenocarcinoma, and 3-5 % neuroendocrine.
Prevention through vaccination- recombinant 4 or 9-valent HPV vaccination which target HPV types that pose the greatest risk.
Prognosis- overall 5- year relative survival rate is 68 % for white women and 55 % in black women- survival rates are inversely proportionate to the stage of cancer.
Signs/Symptoms-
Metrorrhagia, postcoital spoting, and cervical ulceration. Gross edema of the legs may be indicative of vacular and lymphatic stasis due to tumor. Pain in the back (lumbosacral plexus region) indicates neurologic involvement. Bladder and rectal dysfunction or fistulas are severe late symptoms. Two to 10 years are required for carcinomas to penetrate the basement layer of the membrane and become invasive- screening has decreased mortality.
Diagnostic Tools-
Cervical Biopsy- After a positive papnicolaou smear biopsy or endocervical curettage is necessary to determine the extent and depth of the cancer cells. Surgery and radiation should be delayed until biopsy results.
Imaging- CT, MRI, lymphangiography, fine-needle aspiration, ultrasound, and laparoscopy are utilized for staging of invasive cancer. Allows for more specific treatment planning.
Complications-
Metastases to regional lymph nodes occurs with increasing frequency from Stage I to Stage IV. Extension occurs in all directions from the cervix.
Hydronephrosis (urine-filled dilation of the renal pelvis due to obstruction) and hydroureters (dilation of the ureter), is a result of the ureters becoming obstructed lateral to the cervix which can lead to impaired kidney function.
Treatment/Management- Refer all patients to Gynecologic Oncologist
Carcinoma in situ (Stage 0)- women whom child-bearing is not a consideration, total hysterectomy is definitive treatment.
Retain uterus- cryosurgery, laser surgery, LEEP, or cervical conizations are options. Close follow-up with pap smears every 3 months for 1 year and every 6 months for another year after cryo/laser surgery.
Invasive Carcinoma- treated with hysterectomy. Stage IA1, IBI, and IIA hysterectomy and concomitant radiation and chemotherapy or with radiation and chemo alone; Stages IB2, IIB, III, and IV cancers treated with radiation therapy plus concurrent chemotherapy.
Emergency presentation- vaginal hemorrhage- due to gross ulceration and cavitation of cervix- late stage- packing, cautery, tranexamic acid to stop bleeding temporarily. Ligation and suturing not an option due to diffused ulceration.
o Fibroid Tumor
Uterine leiomyomas are the most common neoplasm in the female genital tract- it is a round, firm, often multiple uterine tumor composed of smooth muscle and connective tissue.
Classification by anatomical location- 1. Intramural, 2. Submucous, 3. subserious, 4. Intraliagmentous, 5. Parasitic (blood supply from an organ to which its attached) 6. cervical
In non-pregnant women, myomas are frequently asymptomatic- symptoms which prompt for treatment include AUB and pelvic pain or pressure. Complications of fibroids include miscarriage if they block the uterine cavity or preterm delivery and malpresentation.
Diagnostic-
Patients may present with iron deficiency anemia (blood loss). Imaging to include a pelvic ultrasound and monitor growth. MRI can be delineate intramural and submucous myomas and is required prior to uterine artery embolization to assess the blow flow to the fibroid.
R/O: subserous myomas from oviarian tumors
Treatment/Management
Small asymptomatic myomas can be evaluated annually- Patients who defer surgery, non-hormonal therapies (NSAIDs and tranexamic acid) have been show to decrease menstrual blood loss.
Hormonal therapies- GnRH agonists and SPRMs, shown to reduce myoma volume, uterine size, and menstrual blood loss.
Surgical intervention should be based on patient’s symptoms and desire for future fertility- uterine size is not an indication alone for surgery- cervical myomas 3-4 cm in diameter that protrude through cervix, can cause infection, bleeding, pain, or urinary retention, which require removal.
Emergency Surgery- indicated for acute torsion of the pendunculated myoma. Marked anemia, heavy menstrual period post-operative treatment includes DMPA IM q3 months. Only indication for emergency surgery during pregnancy is torsion of a pendunculated fibroid.
Prognosis- Surgery is curative, however, women should be counseled regarding future fertility- reoccurrence is common, and post-operative pelvic adhesions can impact fertility and may require a cesarean delivery.
o Pelvic inflammatory disease-
PID is a polymicrobial infection of the upper genital tract associated the sexually transmitted organism Neisseria gonorrhoeae and chlamydia trachomatis, as well as endogenous organisms, including anaerobes, H. influenza, enteric gram-negative rods, and streptococci.
Most common in young, nulliparous, sexually active women with multiple partners.
Signs/Symptoms
Lower abdominal pain, chills, fever, menstrual disturbances, purulent cervical discharge and cervical and adnexal tenderness. Right upper quadrant pain (Fitz-Hugh & Curtis sign) may indicate associated peri-hepatitis.
Most women present with subtle or mild symptoms, such as urinary frequency, low back pain, or postcoital bleeding.
Diagnostic Criteria
Women with cervical motion, urterine or adnexal tenderness should be treated as if they have PID with antibiotics unless there is a competing diagnosis.
Symptoms including temp >38.3, abnormal cervical or vaginal discharge with white cells on saline microscopy, elevated ESR, elevated CRP, and laboratory documentation of infection by N. gonorrhea or C trachomatis, should prompt treatment with antibiotics while endocervical cultures are processing.
Differential Diagnosis
Appendicitis, ectopic pregnancy, septic abortion, hemorrhagic or unrupture ovarian cyst. PID is more likely to occur if there is a history of recent sexual contact, history of sexually transmitted disease, recent onset of menses, sexual contact with someone with a sexually transmitted disease.
Acute PID is unlikely if sexual intercourse has not occurred within the last 60 days.
Obtain a pregnancy test to rule out ectopic pregnancy, septic abortion,
Pelvic ultrasound can rule out ovarian cyst and ectopic pregnancy
Laparoscopy is often utilized to diagnose PID and imperative if symptoms do not respond to antibiotic therapy within 48 hours of imitating
Treatment/Management
Antibiotic coverage
Mild to moderative infection- treat outpatient
1. Single dose of cefoxitin, 2g IM, with probenecid 1g orally, plus doxycycline 100mg orally twice a day for 14 days
OR
2. Ceftriaxone 250mg IM plus doxycycline 100 mg orally twice daily for 14 days.
3. Metronidazole 500 mg orally twice daily for 14 days can be added to either regimen.
Severe disease- meet criteria for hospitalization
1. Cefotetan 2g IV every 12 hours
OR
2. Cefoxitin 2g IV every 6 hours, plus doxycycline 100mg orally or intravenously every 12 hours.
OR alternative regiment is
3. Clindamycin 900 mg intravenously every 8 hours, plus gentamicin loading dose of 2mg/kg intravenously or IM followed by maintenance dose every 8 hours.
Either regiment should be continued for at least 24 hours after patient shows symptom improvement and then transitioned to oral regimen for a total of 14 days
Surgical Management-
Tubo-ovarian abscess is a complication of PID and may require surgical intervention, unless rupture is suspected high dose antibiotics can be initiated. Monitor therapy response with ultrasound. 70 percent of cases respond to ABX, 30 percent require surgical intervention.
Admission criteria-
Tubo-ovarian abscess, pregnancy, patient is unable to follow outpatient regimen, patient has not clinically improved with 72 hours from outpatient initiation of ABX, serve illness symptoms including nausea/vomiting, or high fever.
o Uterine bleeding
Normal menstrual bleeding is 5-7 days as an average blood loss of 40mL per cycle.
Menorrhagia is considered blood loss over 80mL
Metrorrhagia is bleeding between cycles
Polymonorrhea is bleeding that occurs more often than every 21 days
Oligomenorrhea bleeding less frequently than 35 days.
Abnormal Uterine Bleeding (AUD) is defined by the bleeding pattern, heavy, light, menstrual, intrermenstural and etiology PALM-COEIN
P- polp
A- Adenomyosis
L- leiomyoma
M- malignancy
C coagulopathy
O- ovulatory dysfunction
E- endometrial
I iatrogenic
N- not classified.
Adolescents- AUB is often a result of persistent anovulation due to immaturity of the hypothalamic-pituitary-ovarian axis and normal
Once menses has been established during adolescence ovulatory dysfunction AUB is most common.
Signs/Symptoms
1. History of duration and amount of flow, associated pain, and relationship to the LMP, with presence of blood clots and degree of inconvenience caused by the bleeding
2. History of pertinent illness, such as recent systemic infection, physical or emotional stressors.
3. History of medication such as warfarin or heparin, herbal remedies (ginko, ginsing) that may cause AUB
4. History of coagulation disorders in patient or family members
5. Evaluate for excessive weight and signs of PCOS, thyroid disease, insulin resistance, or bleeding disorder
6. Pelvic examination, rule out vulvar, vaginal, or cervical lesions or pregnancy
Laboratory Studies
1. CBC, pregnancy test and thyroid test
2. History of coagulopathy or history- coagulation study
3. Vaginal or urine sample to rule out chlamydia
4. Transvaginal ultrasound- rule out ectopic pregnancy, adnexal or uterine masses
5. Cervical biopsy- myomas or polps
Treatment- AUB depends on etiology of the bleeding.
AUB ovulatory dysfuction
1. Treated hormonally with progestin
a. Irregular or light bleeding- medroxyprogesterone acetate 10mg/day orally or norethindrone acetate 5 mg/day for 10 days. If successful, treatment can be repeated for several cycles
2. NSAIDS- Naproxen will often reduce blood loss in menorrhagia
3. Oral contraceptives- taper of oral contraceptives to control bleeding.
4. GnRH (depo) can be used for up to 6 months to temporarily stop menstruation.
If bleeding in is not controlled by hormonal treatment, hysteroscopy with tissue sampling to evaluate for structure lesions-
In absence of pathology bleeding unresponsive to medical treatment treated with endomentrail ablation, IUD, or hysterectomy.
o Sexual violence-
- Sexual violence is considered penetration vaginally, anally, or orally and may be by the penis, hand, or a foreign object. The absence of genital injury does not imply consent by the victim.
Rape Trauma Syndrome is comprised of two principles
1- Immediate or acute, shaking, sobbing, restless activity that may last from a few days to a few weeks. The patient may experience anger, guilt, shame, or repress these emotions. Every patient responds differently
2- Late or chronic- problems related to the attack may develop weeks or months later, lifestyle and work patterns may change, sleep disorders or phobias often develop. Loss-self-esteem can lead to suicide.
Treatment- initial presentation
1. Tetanus Toxoid if deep lacerations contain soil or dirt.
2. Consider analgesics or sedatives if needed
3. Ceftriaxone 125mg IM prevent fonorrhea- Metronidazole 2g, and aazithromycin 1g orally OR doxycycline 100mg orall BID for 7 days to treat chlamydial infection- repeat syphilis test 6 weeks after assault.
4. Prevent pregnancy using emergency contraception method
5. Vaccinate against Hep B, conasider HIV prophylaxis
6. Refer for counselling support on psychological support.
o Ectopic pregnancy-
Ectopic implantation occurs in 2 % of pregnancies with 98 % being tubal- Any condition that prevents or retards migration of the ovum to the uterus can predispose to an ectopic pregnancy, including history of infertility, PID, prior tubal surgeries, and ruptured appendix.
Signs/Symptoms
Severe lower quadrant pain, sudden onset, stabbing, intermittent and DOES NOT radiate. Back ache may occur- 2/3rd report history of abnormal menstruation. Slight but persistent vaginal spotting, palpable pelvic mass. Abdominal distension (collection of blood in peritoneum) and mild paralytic ileus.
Labs/Imaging
CBC- anemia and mild leulocytosis
HCG- will show levels slightly lower than normal pregnancies of similar length
Progesterone level can also be measured for pregnancy viability
Normal pregnancy-**Ultrasound will display a gestational sac 5-6 weeks from last menstruation and fetal pole is located in uterus**
An empty uterine cavity leads to strong suspicion of an ectopic pregnancy- especially in conjunction with HCG levels. Consider rising HCG levels with an empty uterus- for example a beta-HCG of 6500 milli-unit/mL and an empty uterine cavity.
Treatment/Management
Differentials including PID, acute appendicitis, ruptured corpus luteum cyst or ovarian follicle
Patient with normal liver and renal function- Methotrexate 50 mg/m2 IM- given as single or multiple dose- pregnancy should be less than 3.5 cm and unruptured
Unstable- patient is hospitalized, blood type and crossed- goal is to diagnose and operate prior to rupture (prevent intra-abdominal hemorrhage)
Surgery- Diagnostic Laparoscopy followed by a salpingostomy with removal of the ectopic pregnancy or a partial/complete salpingectomy. Iron therapy for anemia may necessary- Rh immune globulin should be given to Rh- patients
Fluid/Electrolyte Imbalance
2/3 body weight intracellular, 1/3 extracellular. Effective circulating volume may be assess by physical examination, blood pressure, pulse, jugular venous distention.
Urine- urine concentration of an electrolyte is helpful to determine whether the kidney is appropriately excreting or retaining an electrolyte in response to high or low serum levels.
24 hour urine- most appropriate to assess electrolyte excretion, however, time consuming.
Fractional excretion- FE %= (urine X/serum X)/urine CR/Serum CR x 100.
Low fraction excretion indicates renal reabsorption (electrolyte retention or high avidity)
High fraction- renal wasting (electrolyte excretion or low avidity)
Serum Osmolality- solute concentration- normal 285-295 mmol/kg. Differences in osmolyte concentration across cell membranes lead to osmosis and fluid shifts, stimulation of thirst, and secretion of ADH
Osmolality = 2 (Na+ meq/L) + glucose/ 18 + BUN/2.8
o Hyponatremia- volume status and serum osmolality are essential to determine etiology- usually reflects excess water retention relative to sodium.
HYPOTONIC fluids commonly cause hyponatremia in hospitalized patients.
Serum sodium > 135mEg/L
Evaluation of the patient should include
1. Urine sodium (normal 10-20 mEg/L)
2. Serum osmolality (usually 2 x NA)
3. Clinical status
Measuring urine sodium helps distinguish renal from non-renal causes. Example
Urine sodium >20 suggests renal salt wasting (problem with kidneys)
Urine sodium <10 suggests renal retention of sodium to compensate for extra-renal fluid loss (problem outside of the kidney)
Isotonic Hyponatremia (Pseudohyponatremia)
Serum Osmolality 284-295
Occurs with extreme hyperlipidemia or hyperproteinemia
Body water is normal and the patient is asymptomatic
Treatment- cut down fat (no fluid restriction)
Hypotonic Hyponatremia (serum osmolality <280)- state of body water excess diluting all body fluids, clinical signs arise from water excess
1. Assess if patient is hypovolemic or hypervolemic
2. If hypovolemic, assess whether hyponatremia is due to extrarenal salt losses or renal salt wasting
Hypovlemic/urine NA+ <10
1. Dehydration
2. Diarrhea (c.diff)
3. Vomiting (NG tube suctioning)
Hypovolemic w/urine NA+ >20: low volume and kidneys cannot conserve NA
1. Diuretics
2. ACE inhibitors
3. Mineralcorticoid deficiency.
Hypervolemic, hypotonic hyponatremia (need to restrict water)
1. Edematous state
2. CHD
3. Liver disease
4. Advanced renal failure
Hypertonic Hyponatremia- (serum osmolality >290)
1. Hyperglycemia- usually from HHNK (DM2)
2. Osmolality is high and NA is low
Management of Hyponatremia
Replacement has to be slow and calculated- risk for cerebral osmotic demyelination.
o Hypernatremia
Usually due to excess water loss- always indicates hyperosmolality (deficit of water), excessive sodium intake is rare. Causes include increases NG output, diarrhea, vomting.
Management-
1. Severe hypernatremia with hypovolemia should be treated with NS IV followed by ½ NS
2. Hypernatremia with euvolemia should be treated with free water (D5W)
3. Hypernatremia with hypervolemia should be treated with gree water and loop diuretics- may need dialysis
o Hypokalemia
Causes include chronic use of diuretics, GI loss, excess renal loss and alkalosis. Elevated serum epinephrine in trauma patient may contribute to hypokalemia
Signs and Symptoms
1. Muscular weakness, fatigue, and muscle cramps
2. Constipation or ileus due to smooth muscle involvement
3. If severe (<2.5 mEg/L) may see flaccid paralysis, tetany, hyporeflexia and rhabdomylosis (check serum CK + urine myoglobin)
Laboratory Findings/Diagnostic
1. Decreased amplitude on ECG
2. Broad T waves
3. Prominent U waves
4. PVC, V-Tach, or V-Fib
Management
1. Oral replacement if >2.5 mEq and no ECG abnormalities
2. IV replacement at 10 mEq/hr if cannot take orally
3. If <2.5 mEq or severe signs and symptoms are present, may give 40 mEg/L/hour IV- check every 3 hours and institute continuous ECG monitoring
*Magnesium deficiency frequently impairs K correction
*Replacement of 20 mEq generally raises .2 mEq
o Hyperkalemia
Causes include excess intake, renal failure, drugs (NSAIDs), hypoaldosertonism, and cellular death. Shifts of intracellular K+ into the extracellular space occurs with acidosis. K+ increase .7mEq/L with each 0.1 drop in pH.
Signs/Symptoms
1. Weakness, flaccid paralysis
2. Abdominal distension
3. Diarrhea
Laboratory Findings/Diagnosis
1. ECG not particularly sensitive- 50% of patient with K+ >6.5 will not have ECG changes, however, tall pealed T waves are classic finding
Management
1. Exchange resins (Kayexalate)
2. If >6.5 or cardiac toxicity or muscle paralysis is present, consider
a. Insulin 10 U with one amp D50 (pushes K into cells)
Calcium
Major cellular ion and important as a mediator of neuromuscular and cardiac function.
Normal total calcium of 2.2-2.6 mmol/L (8.5-10.5 mg/dL) and normal ionized calcium of 1.1-1.4mmol/L (4.5-5.5 m/dL).
1. Ionized calcium does not vary with albumin level (useful to measure the ionized calcium level with the serum albumin is not within normal range)
2. Calcium is maintained by Vitamin D, parathyroid hormone, and calcitonin.
3. Acidemia increase ionized calcium and alkalemia decrease
4. The total amount of total calcium varies with the level of serum albumin (since 50 % of calcium is bound to albumin, a normal calcium level in the presence of low albumin level suggests that the patient in hypercalcemic.
5. Corrected calcium (mg/dl) = measured total Ca (mg/dl) +0.8 or [4.0- serum albumin (gldl)], where 4.0 represents the average albumin level
o Hypocalcemia
Causes include hypoparathyroidism, hypomagnesemia, pancreatitis, renal failure, severe trauma, and multiple blood transfusions.
Signs/Symptoms
1. Increase deep tendon reflexes, muscle/abdominal cramps
2. Carpopedal spams (Trousseaus sign) or Chvostek’s sign (sustained cheek)
3. Convulsions, prolonged OT interval
Management
1. Check blood pH- look for alkalosis
2. If acute, IV calcium gluconate
3. If chronic, oral supplements, vitamin D, albumin hydroxide
o Hypercalcemia
causes include hyperparathyroidism, hyperparathyroidism, vitamin D intoxication, prolonged immobilization- rarely thiazide diuretics will promote hypercalcemia.
Signs/Symptoms
1. Fatiguability, muscle weakness, anorexia, depression
2. Nausea/vomiting/diarrhea/constipation
3. Severe hypercalcemia can cause coma and dealth
Management
1. May need calcitonin if impaired cardiovascular or renal function
2. May need NS with loop diuretics – dialysis in severe cases.
o Hypophosphatemia
Causes include malabsorption, vitamin D deficiency, starvation, parental alimentation with inadequate phosphate content, electrolyte abnormalities (hypercalcemia, hypomagnesemia) metabolic alkalosis, recovery from starvation, inadequate DM control, hyperparathyroidism, hyperthyroidism. Alcohol, acute alcohol withdrawal (promotes intracellular shift of phosphate)
Serum phosphate levels decrease after food intake, fasting samples are recommended for accuracy
Moderate hypophosphatemia- 1.02.4 mg/dL
Severe hypophosphatemia- less than 1 mg/dL . Impairs tissue oxygenation and cell metabolism – resulting in muscle weakness or even rhabdomyolysis.
Specific Patient Populations
Alcohol withdrawal- increased plasma insulin and epinephrine along with respiratory alkalosis promotes intracellular shift of phosphate
Chronic alcohol use decreases renal threshold of phosphate excretion- renal dysfunction reverses after a month of abstinence.
COPD- attributed to xanthine derivatives causing shifts oh phosphate intracellularly and the phosphaturic effects of beta-adrenergic agonists, loop diuretics, corticosteroids.
Refeeding or glucose administration to phosphate-depleted patient may causes fatal hypophosphatemia.
Signs/Symptoms
1. Severe can lead to rhabdomyolysis paresthesia, and encephalopathy (confusion, irritability, dysarthria, seizures)
2. Respiratory failure, or failure to wean from vent from diaphragmatic weakness
3. Arrhythmias and heart failure
4. Acute hemolytic anemia from erythrocyte fragility, platelet dysfunction
5. Impaired chemotaxis of leukocytes (increased susceptibility to gram – sepsis)
Laboratory Findings
Urine phosphate excretion- normal renal response to hypophosphatemia is decreased urinary phosphate excretion to less than 100mg/day
Treatment/Management
1. Can be prevented with phosphate repletion in maintenance fluids- rapid decline of calcium can occur with parenteral administration.
2. Oral replacement is preferred
3. IV replacement, consider the potassium and sodium level- IV K- Phos versus IV Na-Phos replacement. Check Na, K, Phos levels q6h
4. Magnesium deficiency often coexists and should be corrected.
Contraindications to treatment
Hypoparathyroidism, advanced CKD, tissue damage and necrosis, and hypercalcemia. When an associated hyperglycemia is treated, phosphate accompanies glucose into the cells and hypophosphatemia may ensue.
o Hyperphosphatemia
Causes include CKD, decreased excretion into the urine, laxatives or enemas containing phosphate, metabolic acidosis, respiratory acidosis, IV phosphate supplement.
Phosphate concentration greater than 4.5 mg/dL
Most patients are asymptomatic however others may develop calcium deposits into the soft tissue (chronic hypephosphatemia). Similar to hypocalcemia symptoms, muscle cramps, tetany, numbness/tingling
Treatment/Management
Treat the cause
1. Caused by tumor lysis, responds to forced saline diuresis to enhance urinary loss
2. Limit phosphate intake- renal failure is the clinical condition most often requiring curtailment of phosphate ingestion- advanced renal insufficiency require phosphate binders to inhibit gastrointestinal absorption of phosphate
3. Enhance renal excretion- use volume repletion with saline coupled with forced diuresis with loop diuretics
Magnesium
Normal plasma magnesium level is 1.83.0 mg/dL, with about 1/3 bound to protein and 2/3 existing as free cation. Excreted via the kidney, physiologic effects on the nervous system resembles those of calcium. Altered magnesium concentration usually provokes an associated alteration of Ca. Both hypo/hyper can decrease PTH secretion or action
o Hypomagnesemia
Causes include malabsorption, laxative abuse, PPT, prolonged gastrointestinal suction, malnutrition, alcoholism, increased renal loss
Signs/Symptoms
- Weakness and muscle cramps, CNS hyperirritability may produce tremors, athetiod movements, jerking, nystagmus, Babinski response, confusion, disorientation.
- EKG may show prolonged QT interval, due to lengthening of the ST segment.
- PTH secretion is suppressed
Management/Treatment
- 250-500mg orally once or twice a day for chronic hypomagnesemia
- IV 1-2 g over 5-60 minutes for symptomatic hypomagnesemia
- Cautious replacement in patients with CKD to avoid hypermagnesemia- reduced doses
o Hypermagnesemia
Almost always the result of advanced CKD and impaired magnesium excretion. Antacids and laxatives. Pregnant patients may have severe hyper-magnesemia from IV magnesium for preeclampsia and eclampsia.
Signs/Symptoms
- Muscle weakness, decreased deep tendon reflexes, mental obtundation, confusion. Weakness, flaccid paralysis, ileus, urinary retention, and hypotension.
- EKG may show broadened QRS complex and peaked T-waves (related to hyperkalemia)
Treatment
-Sources of magnesium should be discontinued
- Calcium antagonizes Mg+ and can be given intravenously as calcium chloride
- Hemodialysis or peritoneal dialysis may be required for CKD patients \
Acid-Base Disorders
Metabolic (decreased or increased HCO3-)
Respiratory (decreased or increased PCO2)
If pH is <7.4 the primary process is acidosis, either respiratory (pCO2 >40 ) or metabolic (HCO <24)
If the pH is >7.4 the primary process is alkalosis, either respiratory (pCO2 <40) or metabolic (HCO > 24)
Once the primary acid base disturbance has been determined, assess whether the compensatory response is appropriate. An inadequate or exaggerated response indicates the presence of another primary acid-base disturbance.
Anion gap should always be calculated0 >20 mEgq/L suggests a primary metabolic acid-base disturbance regardless of the pH or serum bicarb because an anion gap is never a compensatory response to a respiratory disorder.
Anion gap- Na – (HCO3 +Cl)
o Metabolic acidosis
Hallmark is low serum HCO3 and low pH. Measurement of anion gap helps to evaluate cause and treatment options. Normal anion gap is 7-17
Anion Gap Treatment- Treat the cause, such as insulin or fluid therapy, volume resuscitation.
Non-Anion Gap- treatment with administration of bicarbonate or citrate to correct metabolic abnormalities.
Anion Gap Non Anion Gap
“MUDPILERS” “HARDUPS”
Methanol Hyperalimentation
Uremia Acetazolamide
DKA/Alocholic KA Renal tubular acidosis
Paradehyde Diarrhea
Isoniazid Uretero-pelvic shunt
Lactic acidosis Post-hypocapnia
Etoh/Ethylene glycol Spironolactone
Rhabdo/Renal Failure
Salicylates
o Metabolic alkalosis
Metabolic Alkalosis is characterized by high HCO3-
Abnormalities that generate HCO3- are called initiation factors, whereas abnormalities that promote renal conservation of HCO3 are called maintenance factors.
Two causes of metabolic alkalosis is “saline responsiveness” using the urine Cl- as a marker for volume status- saline responsiveness is a sign of extracellular volume contraction, and saline-unresponsive alkalosis implies excessive total body bicarbonate with either euvolemia or hypervolemia.
Metabolic alkalosis is generally associated with hypokalemia due to the direct effect of alkalosis on renal potassium excretion and secondary hypoaldosteronism from volume depletion- hypokalemia exacerbates with metabolic alkalosis by increasing bicarb reabsorption in the proximal tubule and hydrogen ion secretion in the distal tubule.
“CLEVER PD”
Contraction
Licorice * assocated with hight urine Cl levels
Endo: Cushings/Bartters
Vomiting, NG suction
Excess Alkali
Refeeding Syndrome
Post- Hypercapnia
Diuresis
Treatment for Saline Responsive Metabolic Alkalosis
- Correction of the extracellular volume deficit with isotonic saline. Diueretics should be discontinued. H2 blockers or PPIs may be helpful in patients with M.A. from NG suctioning. Pulmonary or cardiovascular status limits resuscitation; acetazolamide will increase renal bicarb excretion.
Treatment for Saline Unresponsive Metabolic Alkalosis
- Surgical removal of the mineralcorticoid-producing tumor and blockage of aldosterone effect with an ACE inhibitor or spironolactone. Caused by primary aldosteronism, can be treated by potassium repletion
o Respiratory acidosis (Hypercapnia)
Results from hypoventilation and subsequent hypercapnia. Arterial pH is low and PCO2 increased. Serum HCO3 is elevated but does not full correct the pH.
Treatment is aimed at improving the underlying disorder and improving ventilation.
Hypoventilation- anything that causes hypoventilation
CNS depression
Airway obstruction
Pneumonia
Pulmonary Edema
Hemo/Pneumothorax
Myopathy
Chronic Respiratory acidosis is caused by COPD and restrictive lung disease.
o Respiratory alkalosis
Occurs when hyperventilation reduces the PCO2, increasing the serum pH-. Serum bicartb is decreased in chronic respiratory alkalosis.
Determination of appriate metabolic compensation may reveal an associated metabolic disorder- metabolic compensation is greater if the respiratory alkalosis is chronic.
Treatment is aimed at the underlining causes for the hyperventilation- rapid correction may lead to metabolic acidosis.
Anything that causes hyperventilation
CNS disease
Hypoxia
Anxiety
Mechanical ventilators
Progesterone (pregnancy)
Salicylates/Sepsis.
Endocrine System and Infections
• Evaluation, differential diagnosis, diagnostic studies, and treatment options
o Hypopituitarism
Evaluation
• Variable presentation depending on cause
• Symptoms include headache, amenorrhea, galactorrhea and visual field defects
• Causes: neoplastic, vascular, inflammatory/infiltrative disorders, infections, congenital, postradiation, postsurgical, traumatic brain injury, empty sella syndrome, hypothalamic diseases, medications (opiods, megestrol)
DDx
• Addison’s disease, primary hypothyroidism, cardiogenic shock, septic shock
Diagnostic studies
• Serum electrolytes, serum and urine osmolarity, 8am cortisol and adrenocorticotropic hormone, thyroid function tests, (8am testosterone, follicle-stimulating hormone, luteinizing hormone in men), (estradiol, follicle-stimulating hormone, and luteinizing hormone in women), prolactin, insulin-like growth factor-1, cosyntropin/tetracosactide stimulation test
Treatment Options
• Underlying cause must be addressed, where causes are not correctable, treatment focuses on replacing target hormones
o ACTH deficiency
o Thyroid deficiency
o Gonadotropin deficiency
o Prolactin deficiency
o Growth hormone deficiency
o ADH deficiency
o Hypophysitis associated with anti-cytotoxic T-lymphocyte antigen-4 (CTLA-4) therapy
o Diabetes Insipidus
Evaluation
• Characterized by polydipsia, polyuria, increased thirst, and formation of hypotonic urine, volume depletion
• Central Diabetes Insipidus – due to defective synthesis or release of arginine vasopressin (AVP) from the hypothalamo-pituitary axis
o Pituitary surgery
o Craniopharyngioma
o Posttraumatic head injury
o Pituitary stalk lesions – Langerhans cell histiocytosis
o Congenital malformations
o Genetic mutations – Wolfram syndrome, AVP-neurophysin gene mutations
o Autoimmune disorders – Hashimoto thyroiditis, DM1
o CNS infections – late complication of meningitis or encephalitis
o Cerebrovascular accident – subarachnoid hemorrhage
o Medications - phenytoin
o Recognized causes- temozolomide, IgG4
• Nephrogenic Diabetes Insipidus – due to renal insensitivity or resistance to AVP, with a resultant lack of permeability of the collecting duct to water.
o Risk factors include lithium therapy, chronic renal disease, and chronic hypercalcemia or hypokalemia
DDx
• Psychogenic polydipsia, DM, hyperosmolar hyperglycemic state, hyperaldosteronism, diuretic use, hypercalcemia
Diagnostic studies
• Urine osmolality, serum osmolality, serum sodium, serum calcium serum potassium, urine dipstick, 24-hour urine collection for volume, serum BUN, serum glucose
Treatment options
• Treatment goals are correction of any pre-existing water deficits and reduction in ongoing excessive urinary water losses.
• Central DI, desmopressin is the treatment of choice.
• Nephrogenic DI is treated with adequate fluid intake; salt restriction and diuretics may help reduce polyuria
•
o Acromegaly
Evaluation
• Rare, chronic disease caused by excessive secretion of growth hormone (GH), usually die to a pituitary somatotroph adenoma.
• Must be screened for in the presences of pituitary adenoma, profuse sweating, acral growth, coarsening of facial features, and when suspected in conjunction with commonly associated conditions such as carpal tunnel syndrome, arthralgia,, glucose intolerance or diabetes, amenorrhea, hypertension, and sleep apnea.
DDx
• Acromegaloidism
• Pseudoacromegaly
Diagnostic studies
• Serum insulin-like growth factor (IGF-1), oral glucose tolerance test, random serum growth hormone (GH)
• Consider MRI or CT of pituitary
Treatment options
• Goals of treatment are to:
o Restore life expectancy to normal
o Relieve symptoms of the condition
o Completely remove the causative tumor, if possible; if not possible, control its growth and related mass effects
o Preserve normal pituitary functioning
o Hyperprolactinemia
Evaluation
• Condition of elevated serum prolactin. Most common endocrine disorder of the hypothalamus-pituitary axis.
• Usually found during the evaluation of presenting complaints such as amenorrhea, galactorrhea, erectile dysfunction, or headaches
• Predominant clinical consequence of hyperprolactinemia is hypogonadotropic hypogonadism, which is due to an interruption in the pulsatile secretion of gonadotropin-releasing hormone by the elevated PRL.
• Symptoms that present are headaches, visual loss or visual field defects, cranial nerve neuropathies, and seizures.
DDx
• Prolactinoma, primary hypothyroidism, acromegaly, chronic kidney disease, cirrhosis, lymphocytic hypophysitis, multiple endocrine neoplasia syndrome type 1, pregnancy
Diagnostic studies
• Serum prolactin, liver and renal function, thyroid function, macroprolactin levels, pregnancy test
• MRI of pituitary if physiologic, drug-induced and secondary hyperprolactinemia have been excluded
Treatment options
• Supportive therapy with IV fluids and corticosteroids
• Transsphenoidal surgical decompression of the tumor if necessary
• Long term follow up to treat any residual tumor and/or pituitary dysfunction may be required
o Thyroiditis
Evaluation
• Thyroiditis is an inflammation of the thyroid gland that may be painful and tender when caused by infection, radiation, or trauma, or painless when caused by autoimmune conditions, medications, or an idiopathic fibrotic process
• The most common forms are Hashimoto's disease, subacute granulomatous thyroiditis, postpartum thyroiditis, subacute lymphocytic thyroiditis, and drug-induced thyroiditis (caused by amiodarone, interferon-alfa, interleukin-2, or lithium
• Diagnosis is by clinical context and findings, including the presence or absence of pain, tenderness, and autoantibodies. In addition, the degree of radioactive iodine uptake by the gland is reduced in most patients with viral, radiation-induced, traumatic, autoimmune, or drug-induced inflammation of the thyroid
DDx
• Hashimoto thyroiditis, Graves disease, toxic multinodular goiter, factitious ingestion of thyroid hormone, Struma ovarii, subacute thyroiditis, iodine-induced hyperthyroidism
Diagnostic studies
• TSH, serum free T4 and T3, thyroid peroxidase antibodies, TSH-receptor antibodies, CRP, CBC
• 4-, 6-, or 24-hour radioiodine uptake
• T3/T4 ratio
Treatment options
• Treatment primarily is directed at symptomatic relief of thyroid pain and tenderness, if present, and restoration of euthyroidism.
• Acute thyroiditis requires abx treatment, PCN or ampicillin 10-14 days
• Subacute thyroiditis goal is to relieve discomfort and control abnormal thyroid function. Low dose ASA and if this does not help prednisone for 1 week then taper.
o Hypothyroid/myxedema
Evaluation
• Present with nonspecific symptoms of weakness, lethargy, depression and mild weight gain. Physical exam may show dry skin, thick tongue, eyelid edema, and bradycardia
• Elevated TSH and low T4
•
DDx
• Central or secondary hypothyroidism, depression, alzheimers dementia, anemia
Diagnostic studies
• Serum TSH, free T4, serum cholesterol, CBC, fasting blood glucose, serum CK, serum sodium, antithyroid peroxidase antibodies
Treatment options
• Levothyroxine at starting dose of 1.6mcg/kg daily or 25mcg daily in older patients or those with CAD
• TSH should be measured 4-6 weeks after initiation of therapy or dosage changes
o Hyperthyroid
Evaluation
• Overactive thyroid when thyroid gland produces too much thyroxine. Accelerates body’s metabolism, causing unintentional weight loss and a rapid or irregular heartbeat.
• Heart palpitations, increased appetite, nervousness, anxiety and irritability, tremor, sweating, changes in menstrual patterns, increased sensitivity to heat, changes in bowel patterns, goiter, fatigue, muscle weakness, difficulty sleeping, skin thinning, fine brittle hair.
• Can be caused by Graves disease, Plummer’s disease and thyroiditis
DDx
• Graves disease, euthyroid hyperthyroxinemia, goiter, struma ovarii, thyrotoxicosis
Diagnostic studies
• TSH, radioiodine uptake test, thyroid scan, thyroid US
Treatment options
• Radioactive iodine – causes gland to shrink
• Anti-thyroid medications – tapazole and propylithiouracil
• Beta blockers – ease the symptoms of hyperthyroidism
• Thyroidectomy
o Thyroid nodules
Evaluation
• Most do not cause symptoms and are typically discovered during routine physical exam or on imaging tests like CT or US.
• Thyroid tests are typically normal, even when cancer is present in a nodule
• https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879398/
DDx
• Thyroid cancer
Diagnostic studies
• Thyroid US, fine needle biopsy, nuclear thyroid scan
Treatment options
• Surgical removal if cancerous
• Monitor if small and benign
o Thyroid cancer
Evaluation
• Most commonly presents as an asymptomatic thyroid nodule
DDx – benign thyroid nodule
Diagnostic studies
• Fine needle aspiration
Treatment options
• Surgical removal of thyroid, followed by radioactive iodine ablation and TSH suppression
• Thyroid hormone replacement
• TSH checked 4-6 weeks after hormone treatment starts
o Iodine deficiency disorder
Evaluation
• Associated with diffuse and nodular goiter
• Iodine is an essential component of thyroxine (T4) and triiodothyronine (T3) and must be provided in the diet.
DDx
• Goiter, hypothyroidism, thyroiditis, infertility, pericardial effusion, thyroid nodule, thyroid cancer
Diagnostic studies
• Test for iodine by urine
Treatment options
• Iodized salt intake increased
• Iodine tablets
• Iodized water
o Hypoparathyroidism
Evaluation
• Presentation varies: asymptomatic with low serum calcium to acutely symptomatic with neuromuscular irritability, tetany, painful muscle cramps, stridor, and even seizures with low serum calcium
• Majority are post-surgery for benign and malignant thyroid disorders, hyperparathyroidism, and laryngeal or other head and neck cancers.
DDx
• Hypovitaminosis D, Hypomangnesemia, hypoalbuminemia, pseudohypoparathyroidism, renal failure, chronic kidney disease
Diagnostic studies
• Serium calcium, serum albumin, EKG, plasma intact PTH, serum magnesium, serum phosphorus, serum 25-hydroxyvitamin D, serum creatinin
Treatment options
• Calcium gluconate 90mg IV over 10 min (can be repeated), followed by 0.5-1.5mg/kg/hr infusion
• Magnesium sulfate 1g IV q6hrs until normal range
o Hyperparathyroidism
Evaluation
• Diagnosis confirmed with serum calcium and inappropriate evaluation of PTH
• Depression, cognitive changes, change in sleep pattern, and myalgias are common complaints
• Physical exam typically normal but exam of neck is essential to look for hard, dense mass, suggestive of parathyroid carcinoma
DDx
• Familial hypocalciuric hypercalcemia, humoral hypercalcemia of malignancy, multiple myeloma, milk-alkali syndrome, sarcoidosis, hypervitaminosis D, thyrotoxicosis, chronic or acute leukemia, immobilization, thiazides
Diagnostic studies
• Serum calcium, serum intact PTH w/immunoradiometric assay, 25-hydroxyvitamin D level, serum ALKP, serum phosphorus
Treatment options
• Parathyroidectomy is definitive cure
• Ergocalciferol replacement
o Osteoporosis
Evaluation
• Typically, asymptomatic until fracture occurs
• Characterized by low bone density and microarchitectural defects in bone tissue, resulting in increased bone fragility and susceptibility to fracture
DDx
• Multiple myeloma, chronic kidney disease – bone and mineral disorder, primary hyperparathyroidism, metastatic bone malignancy, vertebral deformities
Diagnostic studies
• DXA scan, XR, quantitative CT, serum ALKP, serum Ca, serum albumin, serum Cr, serum Phos, serum 25-hydroxy vitamin D, serum parathyroid hormone, thyroid function tests, urinary free cortisol, serum testosterone (men), serum protein electrophoresis
Treatment options
• Fall prevention is first-line therapy
• Bisphosphonates first-line therapy for postmenopausal men and women
• Estrogen for those at high-risk where nonestrogen medications are inappropriate
o Osteomalacia
Evaluation
• Vitamin D deficiency is the most common cause
• Acquired or inherited
• Complain about diffuse bony pain with hx of limited sunlight exposure
• Proximal muscle weakness, spinal tenderness to percussion, pseudofractures, and skeletal deformities are found commonly
DDx
• Osteoporosis, Paget disease
Diagnostic studies
• Diagnosis is made via laboratory results with a low vitamin D level in the setting of low or normal calcium and an elevated intact PTH level
• Serum Ca, serum 25-hydroxyvitamin D, serum Phos, serum Bun & Cr, Intact PTH, serum ALKP, 24-hour urine calcium
Treatment options
• Once underlying cause is addressed, a successful treatment regimen is possible: increased sunlight exposure, oral vitamin
D, and calcium replacement.
o Paget’s disease
Evaluation
• Chronic localized bone remodeling disorder characterized by increased bone resorption, bone formation, and remodeling, which may lead to major long bone and skull deformities
• Majority are asymptomatic. Symptomatic patients experience pain localized to the bone or join, either from pagetic lesion, secondary osteoarthritis, deformity, or pathological fracture.
DDx
• Osteomalacia, fibrous dysplasia
Diagnostic studies
• Diagnosis is incidental, with elevated ALKP raising suscpicion for disease.
• Bone biopsy is the only confirmatory diagnostic test but is rarely indicated
• Plain XR, bone scan, total serum ALKP, bone specific ALKP, serum Ca, serum precollagen 1 N-terminal peptide, serum C-terminal propeptide of type 1 collagen (CTX), LFT’s, serum 25-hydroxyvitamin D
Treatment options
• Bisphosphonates are first-line therapy to retard excessive osteoclastic activity.
• Adjunctive therapy includes physical therapy, orthoses, and walking and hearing aids
• Analgesics are indicated for pain and inflammatory symptoms
o Addison’s disease
Evaluation
• Presentation may be acute or insidious, with substantial fatigue and weakness associated with mucocutaneous hyperpigmentation, hypotension and/or postural hypotension, and salt craving.
DDx
• Adrenal suppression due to corticosteroid therapy, secondary or tertiary adrenal insufficiency, hemochromatosis, hyperthyroidism, occult malignancy, anorexia nervosa
Diagnostic studies
• Adrenocorticotropic hormone stimulation test is performed to confirm or exclude the diagnosis of Addison’s disease.
Treatment options
• Hydrocortisone sodium succinate 50-100mg IV q6-8hrs for 1-3 days
• NS to correct hypotension and dehydration
• Glucose when necessary to correct hypoglycemia
• Treatment of underlying cause
o Cushing syndrome
Evaluation
• Clinical manifestation of pathologic hypercortisolism from any cause
• Caused by adrenocorticotropic hormone (ACTH)-secreting pituitary adenoma (most common cause)
• Features more specific to Cushing syndrome include proximal muscle weakness, supraclavicular fat pads, facial plethora, violaceous striae, easy bruising, and premature osteoporosis
DDx
• Metabolic syndrome
Diagnostic studies
• Urine pregnancy, serum glucose, late-night salivary cortisol, 1mg overnight dexamethasone suppression test, 24-hour urinary free cortisol, 48-hour 2mg dexamethasone suppression test
Treatment options
• First line therapy is transsphenoidal resection of the causative pituitary adenoma
• Medical therapy before surgery: mifepristone 300mg daily initially, increase in 300mg/day increments every 2-4 weeks according to the response, max 1200mg/day
• Post-surgical tx: hydrocortisone 10-25mg per meter sqare body surface area/daily in 2-3 divided doses
• Levothyroxine 1.8mcg/kg/day and/or testosterone transdermal 2.5-7.5mg daily, titrate according to response
o Primary aldosteronism
Evaluation
• Most common treatable and curable form of HTN
• Aldosterone production exceeds the body’s requirements
•
DDx
• Essential HTN, thiazide-induced hypokalemia in patient with essential HTN, secondary HTN, syndrome of apparent mineralocorticoid excess, hypertensive forms of congenital adrenal hyperplasia, primary glucocorticoid resistance, Ectopic ACTH syndrome
Diagnostic studies
• Optimal detection involves screening all hypertensive patients using the plasma aldosterone/renin ratio
• Plasma potassium, aldosterone/renin ratio
Treatment options
• Unilateral PA
o Unilateral adrenalectomy
Immediately before sx, potassium supplementation should be withdrawn, aldosterone antagonists discontinued and other antihypertensive therapy reduced, if appropriate. Post-operative IV fluids should be given, generous sodium diet recommended
Spironolactone 12.5-50mg PO daily
Amiloride 2.5-10mg daily
o Non-surgical candidates
Amiloride 2.5-10mg daily
• Bilateral PA
o No adrenal lesion> or equal to 2.5cm
Amiloride 2.5-10mg daily
Unilateral adrenalectomy if bilateral cannot be removed with post and preop meds as above
o Adrenal lesion > or equal to 2.5cm
Unilateral adrenalectomy
Post and preop meds as above
o Pheochromocytoma
Evaluation
• Presents with palpations, diaphoresis, pallor, and paroxysmal hypertension
• Risk factors include multiple endocrine neoplasia type 2, Von Hipple-Lindau syndrome, and neurofibromatosis type 1
• Complications include hypertensive crisis, myocardial infarction, and hypotension
DDx
• Anxiety and panic attacks, essential or intractably hypertension, hyperthyroidism, consumption of illicit substances, carcinoid syndrome, cardiac arrhythmias, menopause, preeclampsia
Diagnostic studies
• Diagnosed by increased levels of urine and serum catecholamines, metanephrines and normetanephrines
• Serum free metanephrines and normetanephrines, plasma catecholamines, genetic testing
Treatment options
• Hypertensive crisis
o Phentolamine 5-20mg IV as single dose
• Without hypertensive crisis
o Surgical candidate with benign tumor
Phenoxybenzamine 10mg PO BID, increase by 10mg/day every other day, max 240mg/day
Atenolol 25-100mg PO daily after alpha blockade
Hydration with isotonic saline and high salt diet
Nifedipine 10-20mg PO TID
Surgical excision of tumor
o Surgical candidate with malignant tumor
Phenoxybenzamine 10mg PO BID, increase by 10mg/day every other day, max 240mg/day
Atenolol 25-100mg PO daily after alpha blockade
Hydration with isotonic saline and high salt diet
Nifedipine 10-20mg PO TID
Surgical excision of tumor
Post-surgical chemo and radiation
o Non-surgical candidate with benign tumor
Phenoxybenzamine 10mg PO BID, increase by 10mg/day every other day, max 240mg/day
Atenolol 25-100mg PO daily after alpha blockade
Hydration with isotonic saline and high salt diet
Nifedipine 10-20mg PO TID
o Non-surgical candidate with malignant tumor
Phenoxybenzamine 10mg PO BID, increase by 10mg/day every other day, max 240mg/day
Atenolol 25-100mg PO daily after alpha blockade
Hydration with isotonic saline and high salt diet
Nifedipine 10-20mg PO TID
Post-surgical chemo and radiation
o Diabetes Mellitus Type 2
Evaluation
• Chronic syndrome of impaired carbohydrate, protein, and fat metabolism, owing to insufficient secretion of insulin and/or target-tissue insulin resistance.
• Complications include both macrovascular and microvascular sequelae.
DDx
• Prediabetes, DM1, latent autoimmune diabetes, monogenic diabetes, ketosis-prone diabetes, gestational diabetes
Diagnostic studies
• HbA1c, fasting plasma glucose, random plasma glucose, 2-hour post-load glucose after 75g oral glucose, fasting lipid profile, urine ketones, random C-peptide
Treatment options
• Initially try lifestyle changes, glycemic management, blood pressure management, lipid management and antiplatelet therapy
• HbA1c above goal at diagnosis
o Metformin 500mg daily, increase by 500mg.day increments every week, max 1000mg BID
• HbA1c above goal on metformin
o Add glipizide 2.5-5mg PO daily, increase by 2.5 to 5mg/day increments every 1-2 weeks, max 10mg BID
o Can add insulin glargine at HS
• HbA1c above goal on metformin and insulin
o Add insulin lispro premeal
o Diabetic Ketoacidosis
Evaluation
• Biochemical triad of hyperglycemia, ketonemia, and acidemia with rapid symptom onset
• Common symptoms and signs include polyuria, polydipsia, polyphagia, weakness, weight loss, tadycardia, dry mucous membranes, poor skin turgor, hypotension, and in severe cases, shock.
•
DDx
• Hyperosmolar hyperglycemic state (HHS), lactic acidosis, starvation ketosis, alcoholic ketoacidosis, salicylate poisoning, ethylene glycol/methanol intoxication, uremic acidosis
Diagnostic studies
• Serum glucose level, serum electrolyte levels, bicarbonate level, amylase and lipase, urine dipstick, ketone levels, serum beta-hydroxy, ABG, CBC, BUN, Cr, urine culture, blood culture if infection suspected, EKG,CXR
Treatment options
• Successful treatment includes correction of volume depletion, hyperglycemia, electrolyte imbalances, and comorbid precipitating events with frequent monitoring.
• Complications of treatment include hypoglycemia, hypokalemia, hypoxemia, and rarely pulmonary edema.
• Fluid resuscitation – isotonic saline infused at 1-1.5L (or 15-20ml/kg) for first hour. When plasma glucose reaches 200mg/dL, fluid therapy should be changed to 5% Dextrose with 0.45% NS at 150-250ml/hr. Potassium chloride 20-30meq/L/hr added.
• Reversal of acidosis or ketosis
• Reduction of plasma glucose
• Replenishment of electrolyte and volume losses
• Identify underlying cause
• Insulin therapy should not be started until serum K+ reaches 3.3
• Dopamine 5-10 mcg/kg/min IV, adjust according to BP and other hemodynamic parameters
• Sodium bicarbonate for serum pH 6.9-7.0: 50mmol IV over 1 hr at a rate of 200ml/hr for 2hrs or until pH>7.0
o Hyperglycemia hyperosmolar state
Hyperosmolar hyperglycemic state is a life-threatening emergency manifested by marked elevation of blood glucose, hyperosmolarity, and little or no ketosis
Physical findings of hyperosmolar hyperglycemic state include those associated with profound dehydration and various neurologic symptoms such as coma. The first step of treatment involves careful monitoring of the patient and laboratory values
Precipitating factors may be divided into six categories: infections, medications, non-compliance, undiagnosed diabetes, substance abuse, and coexisting diseases. Myocardial infarction, cerebrovascular accident, pulmonary embolus, and mesenteric thrombosis have been identified as causes of hyperosmolar hyperglycemic state.
DDx
• DKA, lactic acidosis, alcohol ketoacidosis, ingestion of toxic substances, acetaminophen overdose, salicylate overdose, seizures, stroke
Diagnostic studies
• Plasma glucose level, serum or urinary ketone level, serum BUN, serum Cr, serum Na, K, Cl, Mg, Ca, Phos, serum osmolality anion gap, serum lactate, blood gas, UA, LFT, CBC, EKG, CXR, cardiac panel
Treatment options
o Lactic acidosis
Evaluation
• Severe lactic acidosis is often associated with poor prognosis. Recognition and correction of the underlying process is the major step in the treatment of this serious condition. Intravenous administration of sodium bicarbonate has been the mainstay in the treatment of lactic acidosis.
• S/s – fruity-smelling breath, jaundice, confusion, difficulty breathing, exhaustion, muscle cramps, body weakness, abdominal pain, diarrhea, decrease in appetite, headache, rapid heart rate
• Causes: heart disease, sepsis, HIV, cancer, short bowel syndrome, acetaminophen use, chronic alcoholism, intense exercise or physical activity, common in diabetics
• Type A – related to tissue hypoxia where the body is deficient in O2. Also a characteristic of critical illness, such as sepsis and septic shock or acute medical disease states, including those involving the cardiovascular system and liver
• Type B – not related to tissue hypoxia and can be due to health conditions, such as renal disease and certain cancers, some medications, including those for treating type 2 diabetes and HIV, as well as chronic alcoholism and chronic liver disease.
DDx
• Alcoholic ketoacidosis, anemia, bacterial sepsis, distributive shock, hemorrhagic shock, metabolic acidosis, respiratory failure, salicylate toxicity, septic shock, shock and pregnancy
Diagnostic studies
• Anion gab, lactate, serum lactate level, ABG,
Treatment options
• Directed towards correcting the underlying cause and optimizing tissue oxygen delivery
o IV fluids to promote circulation
o O2 or use of cpap
o Vitamin therapy
o Hemodialysis with bicarb
o Hypoglycemia
Evaluation
• Symptoms may include irregular heart rhythm, fatigue, pale, shakiness, anxiety, diaphoresis, hunger, irritability, tingling sensation around the mouth, confusion, visual disturbances, seizures, loss of consciousness
• Diabetics – too much insulin for food consumed, increased physical activity
• Non-diabetics -medications, excessive ETOH consumption, some critical illnesses, insulin overproduction, hormone deficiencies
• Consider these when evaluating pt with hypoglycemia
DDx
• Addison disease, adrenal crisis, alcoholism, anxiety disorders, cardiogenic shock, hypopituitarism, insulinoma, pseudohypoglycemia
Diagnostic studies
• Blood cultures to search for source of infection to rule out, UA, LFT, serum insulin level, cortisol and thyroid level,
Treatment options
• 15g of carbs to raise blood glucose and check after 15 min
o Glucose tablets, gel tube, 4oz. juice or regular soda, 1 tbsp sugar, honey or corn syrup, hard candies
o Glucagon injection IM
o Fever of unknown origin
https://emedicine.medscape.com/article/217675-treatment
https://www.aci.health.nsw.gov.au/networks/eci/clinical/clinical-resources/clinical-tools/infectious-diseases/fever-of-unknown-origin
o Infections in immunocompromised patient
https://emedicine.medscape.com/article/973120-overview
http://www.pidsphil.org/home/wp-content/uploads/2017/02/08Lec-PREVENTION-OF-INFECTIONS-IN-THE-IMMUNOCOMPROMISED.pdf
o Infections in the CNS
o Animal and human bites
Skin and Musculoskeletal System
• Evaluation, differential diagnosis, diagnostic studies, and treatment options
o Cellulitis: Evaluation: Usually caused by gram-positive cocci/A beta-hemolytic streptococci and S aureus, diffuse infection usually in lower legs, infection of the dermis and subcutaneous tissues. Pain, chills and fever present and possible septicemia can develop. Swelling erythema and pain, lymphangitis and lymphadenopathy can be present. Differentials: DVT and necrotizing fasciitis, sclerosing panniculitis and acute severe contact dermatitis. Diagnostic studies: leukocytosis or neutrophilia left shift, positive blood cultures, aspiration of the advancing edge (not common) and full thickness skin biopsy. Treatment: IV antibiotics (the first 2-5 days) to cover strep/staph, MSSA can be treated with nafcillin, cefazolin, clindamycin, dicloxacillin, cephalexin, doxycycline, or TMP-SMZ. MRSA: vancomycin, linezolid, clindamycin, daptomycin, doxycycline, or TMP-SMZ. Mild cases or following IV treatment, dicloxacillin or cephalexin, 250-500 mg four times a day for 5-10 days. Recurrent cellulitis: PO PCN 250 BID daily or erythromycin can delay reoccurrence.
o Necrotizing fasciitis: Evaluation: infection of the deep soft tissues that results in progressive destruction of the muscle fascia and overlying subcutaneous fat, infection can be polymicrobial or monomicrobial. Fulminant tissue destruction, systemic signs of toxicity and high mortality, and absence of gas in the tissues. SIGNS: very toxic appearance, bullae, crepitus or anesthesia of the involved skin, overlying skin necrosis and laboratory evidence of rhabdomyolysis-elevated CK or disseminated intravascular coagulation. Diagnostic studies: surgical debridement, diagnosis is established via surgical exploration of the soft tissues in the OR, physical examination and specimen/tissue cultures. Elevated CK or disseminated intravascular coagulation, CT scan can be helpful to detect gas in soft tissues. Obtain BC. Differentials: Cellulitis, pyoderma gangrenosum, gas gangrene, Pyomyositis, and DVT. TREATMENT: Surgical exploration and debridement of necrotic tissue, Broad-spectrum empiric antibiotic therapy and hemodynamic support. ABX for both gram positive/gram negative/ and anaerobic organisms. Carbapenem (imipenem, meropenem, or ertapenem) or beta-lactam-beta-lactamase inhibitor plus MRSA agent like vancomycin or daptomycin, and clindamycin for strep/staph. Depending on BC sensitivities and type of organism.
o Pressure ulcers/Pressure Injury: Evaluation: Pressure injury is classified into 1-6 categories: Stage 1: non-blanchable erythema of intact skin, Stage 2: partial-thickness skin loss with exposed dermis, Stage 3: full-thickness skin loss, stage 4: full-thickness skin and tissue loss, unstageable: obscured full-thickness skin and tissues loss and Deep tissue pressure injury: persistent non-blanchable deep red, marron, or purple discoloration. Risk factors: immobility, reduced sensory perception, moisture-incontinence, poor nutritional status, and friction/shear forces. Differential Diagnosis: cellulitis, other ulcer related to DM, arterial insufficiency or venous insufficiency. TREATMENT: Table 4-5 page 68: Stage 1-polyurethan film/hydrocolloid wafer, semipermeable foam dressing, Stage 2: hydrocolloid wafers/semipermeable foam dressing/polyurethane film. Stages 3-4: absorptive dressing or packing, necrotic debris must be debrided (autolytic, enzymatic or surgical), hydrocolloid wafers/semipermeable foam/polyurethane film for shallow wounds, deep wounds need packing with gauze. Heel injury, do not remove eschar to help promote healing. Unstageable, debridement. Deep tissue injury, avoid pressure to the area.
o Dermatitis: Evaluation: Atopic dermatitis: diagnostic criteria for atopic dermatitis includes: pruritus, typical morphology and distribution, onset in childhood and chronicity, personal or family HX of atopy, xerosisichthyosis, facial pallor with infraorbital darkening, elevated serum IgE, and repeated skin infections. Pruritic, xerotic, exudative or lichenified eruption on face/neck/upper trunk/wrists and hands/antecubital and popliteal folds. Differentials: seborrheic dermatitis, psoriasis, secondary staphylococcal or herpetic infections-infra-auricular fissure. Dermatologist consult for atypical dermatitis after the age of 30. Diagnostics: itching, and clinicals findings, discrete plaques with weeping, Eosinophilia and increased serum IgE levels may be present. TREATMENT: determined by the pattern and stage of the dermatitis-acute/weepy, subacute/scaly, or chronic/lichenified. Mainly emollient and corticosteroids/topical. Acute weeping lesions: r/o infection, water/aluminum subacetate solution or colloidal oatmeal for soaks, wet dressing for 10-30 minutes 2-4 times daily, high-potency corticosteroids after soaking, Tacrolimus ointment, or systemic corticosteroids-only indicated for severe acute exacerbation, PO prednisone over 2-4 weeks taper off. Systemic corticosteroids are not indicated for maintenance therapy. Subacute or scaly lesions: Mid-to-High potency corticosteroids in ointment form, 2-4-week taper from twice a day to daily dosing with topical corticosteroids to reliance on emollients, then switch to low-potency. Chronic dry/lichenified lesions: high-potency to ultra-high potency corticosteroid ointments, nightly occlusion for 2-6 weeks may enhance the initial response, add tar preparation such as liquor carbonis detergents 10% in Aquaphor or 2% crude coal tar. Maintenance: effective moisturizers to prevent flairs, use of topical anti-inflammatories only on weekend or three times a week. VITAL to taper off corticosteroids and substitute emollients to avoid steroid side effects.
Also/other types of dermatitis: Seborrheic dermatitis (dry scales with underlying erythema/body folds), Exfoliative dermatitis (scaling/erythema over most of the body, itching fever/chills, and contact dermatitis (erythema and edema, often followed by vesicle’s, bullae, weeping or crusting in area of contact with suspected agent).
o Malignant melanoma: Evaluation: leading cause of death due to skin disease. ABCDE rule: asymmetry, border irregularity, color variegation, diameter greater than 6 mm and evolution-change in mole is the single most important historical reason for close evaluation and possible referral. Different types of melanomas: lentigo maligna melanoma, superficial spreading malignant melanoma, nodular malignant melanoma, acral-lentiginous melanomas, ocular melanomas, malignant melanomas on mucous membranes and acral lentiginous melanomas. Differential diagnosis: common melanocytic nevus, atypical melanocytic nevus, blue nevus, traumatized nevus, lentigo, sptiz nevus, pigmental basal cell carcinoma, pigmented actinic keratosis, seborrheic dermatosis, pyogenic granuloma, cherry hemangioma, dermatofibroma, keratoacanthoma. Diagnostic studies: histologic diagnosis, clinical findings. TREATMENT: excision, re-excision is recommended with margins dictated by the thickness of the tumor, margins of 0.5-1 cm for melanoma in situ and 1 cm for lesions less than 1 mm in thickness are recommended. Sentinel lymph node biopsy for staging melanoma. New immunotherapy treatments PD-1, and referral for high risk patients.
o Psoriasis: Evaluation: common benign, chronic inflammatory skin disease with both a genetic basis and known environmental triggers. Silvery scales/plaques, pitting and onycholysis nail findings, associated with psoriatic arthritis, and patients have increased risk of cardiovascular events, DM2, metabolic syndrome and lymphoma. Obesity worsens psoriasis, several variants of psoriasis, most common (4 types) plaque type, eruptive psoriasis, generalized pustular and erythrodermic psoriasis. Itching may occur, common sites scalp, elbows, knees palms and soles and nails. (inverse psoriasis). Differentials: atopic dermatitis, candidiasis, intertrigo, and cutaneous features of reactive arthritis, pityriasis rosea, SLE, and syphilis mimic psoriasis. Diagnostics: Combination of red plaques with silvery scales on elbow and knees with scaliness in the scalp or nail findings is diagnostic. TREATMENT: systemic corticosteroids should NEVER be used to treat flares. Topical corticosteroids (twice daily) are the mainstay for limited disease. Vitamin D analogs like Calcipotriene or calcitriol ointment twice daily for plaque psoriasis-apply at different time as incompatible with other topical corticosteroids and could cause hypercalcemia. Tar shampoo for scalp daily or 6% salicylic acid gel, P&S solution or fluocinolone acetonide in oil, tacrolimus ointment or pimecrolimus cream in intertriginous areas. Moderate disease (10-30% BSA) UV phototherapy or systemic agent. Generalized disease (more than 30% BSA): OP narrowband UVB TID weekly. Goeckerman regimen (crude oil/UVB light for several hours). Psoralen plus UVA photochemotherapy associated with risk of skin cancer. Methotrexate 25 mg once weekly but can be associated with cirrhosis; add folic acid 1-2 mg daily can eliminated nausea with methotrexate. Acitretin/synthetic retinoid for pustular psoriasis 0.5-0.75 mg/kg/day, check liver enzymes and serum lipids, teratogen agent. Cyclosporine for severe cases; tumor necrosis factor inhibitors etanercept (Enbrel), infliximab (remicaid), and adalimmab (Humira) are effective in pustular and chronic plaque psoriasis and for associated arthritis. Oral phosphodiesterase 4 inhibitors apremilast approved option for plaque-type psoriasis with minimal immunosuppressive effects.
o Rosea: Pityriasis Rosea: Evaluation: common mild acute inflammatory disease that is 50% more common in females. Itching, oval fawn-colored, scaly eruption following cleavage lines of trunk, herald patch precedes eruption by 1-2 weeks. Eruption lasts 6-8 weeks. Diagnostic: finding one or more classic lesions: oval, fawn-colored plaques up to 2 cm in diameter, centers have a crinkled or cigarette paper appearance and collarette scale, lesions follow cleavage lines on the trunk/Christmas tree pattern, and proximal portions of the extremities are often involved. Inverse pityriasis rosea affects the flexures, papular variant can occur especially in black patients. Herald patch-often larger lesion, initial lesion that precedes eruption by 1-2 weeks. **check for serologic testing for syphilis. Differentials: Tinea corporis, seborrheic dermatitis, tinea verisicolor, certain medications (ACEi and metronidazole) and immunizations can mimic this disease. TREATMENT: often requires no treatment unless symptomatic. UVB treatments, short course of prednisone, topical corticosteroids of medium strength, triamcinolone 0.1%, and oral antihistamines. Macrolide antibiotic are controversial.
o Tinea Corporis or Tinea Circinata (ringworm): Evaluation: Trichophyton rubrum is most common pathogen, ring-shaped lesions with scaly boarder, central clearing or scaly patches with a distinct boarder. Exposure to pets/microsporum infections, face arms, trunk. Diagnostics: diagnosis confirmation by KOH preparation or culture. Positive fungal studies distinguish tinea corporis from other skin lesions. Differentials: annular lesions of psoriasis, lupus erythematosus, syphilis, granuloma annulare, and pityriasis rosea. TREATMENT: topical antifungals like econazole, miconazole, clotrimazole, butenafine, and terbinafine. Treatment for 1-2 weeks after clinical clearing. Betamethasone diporpionate with clotrimazole (Lotrisone) is not recommended. Systemic measures: Itraconazole 200 mg daily for one week or Terbinafine 250 mg daily for one month.
Also/Other Tinea: Tinea cruris (jock itch), tinea manuum and tinea pedis (interdigital tinea pedis is the most common predisposing cause of lower extremity cellulitis in health individuals), and tinea versicolor (malassezia infection of the skin-usually upper trunk).
o Impetigo: Evaluation: contagious and autoinoculable infection of the skin/epidermis caused by staphylococci or streptococci. Superficial blisters filled with purulent material that rupture easily, crusted superficial erosions, and positive gram stain and bacterial culture. Often in face, ecthyma is a deeper form of impetigo with ulceration and scarring that happens on extremities. Diagnostics: gram stain and cultures confirm diagnosis. Differentials: acute allergic contact dermatitis and herpes simplex. TREATMENT: first line treatment: topical agents like bacitracin, mupirocin, and retapamulin for small areas. Systemic antibiotics for wide-spread cases. Cephalexin 250 mg four times a day or Doxycycline 100 mg BID. CA-MRSA coverage with doxycycline or TMP-SMZ, 50% of CA-MRSA are quinolone resistant. Recurrent impetigo/S Aureus treated with rifampin 600 mg daily for 5 days intranasal mupirocin ointment twice daily for 5 days clears the nasal carriage of MRSA strains. Bleach baths 3-4 times weekly ¼ to ½ cup per 20 liters of bathwater for 15 minutes. Household bleach to clean surfaces and reduce spread.
o Acne Vulgaris: Evaluation: most common skin condition, polymorphic, open/closed comedones, papules, pustules, and cysts, more common in younger adults and males. Comedones are the hallmark of acne, affects face and upper trunk, and can cause scarring. Hyperandrogenism may be a cause of acne in women. Differential diagnosis: Rosacea, gram-negative folliculitis, tinea infections, staphylococcal folliculitis, miliaria/heat rash, or malassezia folliculitis or eosinophilic folliculitis. TREATMENT: education on use of medications and cosmetics, Diet-low glycemic diet/hyperinsulinemia has been associated. Comedonal acne: Proper hygiene, topical retinoids 0.25% cream use first twice weekly at night and then to nightly. Benzoyl peroxide/different concentrations, water-based gels, other topical agents like adapalene and topical antibiotics (erythromycin, clindamycin phosphate). Papular or cystic inflammatory acne: (3 weeks to 3 months) with topical or oral antibiotics, clindamycin phosphate and erythromycin in combination with benzoyl peroxide. Common oral antibiotics are doxycycline 100 mg BID, minocycline 50-100 mg once or BID daily, Bactrim (one double strength tab BID, or cephalosporin/cefadroxil or cephalexin 500 mg BID, and used in combination with benzoyl peroxide to reduce resistance. Once clear tapering dose by 50% every 6-8 weeks to lowest system dose to maintain clearing. Topical retinoids for long-term maintenance after antibiotics. Sub antimicrobial dosing of doxycycline can be used for long-term and contraceptives or spironolactone 50-200 mg/day are effective alternatives for women with treatment-resistant acne. For severe cystic acne, isotretinoin/vitamin A analog/Accutane can be used 0.5-1 mg/kg/day for 20 weeks, teratogenicity. Contradicted in pregnancy, can cause elevated liver enzymes and triglyceride levels. Intralesional injections for lesions/cysts, and cosmetic corrective surgery for scare revision.
o Rosacea: Evaluation: usually presents itself in adulthood, pathogenesis is unknown, usually has a neurovascular component (erythema and telangiectasias and a tendency to flush easily); acneiform component (papules and pustules however no comedones) and a glandular component-hyperplasia of the soft tissue of the nose rhinophyma. Differentials: acne. Diagnostics: rosy hue of rosacea and telangiectasias will pinpoint the diagnosis, lupus is often misdiagnosed, **presence of neurovascular component and absence of comedone. TREATMENT: education on avoiding triggers for exacerbations, sunscreen with zinc or titanium-based sunscreens, chronic condition. Local therapy: Metronidazole creams/gels 0.75% applied twice daily or 1% applied once daily, ivermectin 1% cream applied once daily are effective topical treatments. Clindamycin 1% lotion applied twice daily or sulfur-sodium sulfacetamide -containing topicals if only partial response to topical antibiotic. Systemic therapy: oral tetracyclines, minocycline or doxycycline 50-100 mg once or twice daily, metronidazole or amoxicillin 250-500 mg orally twice daily or rifaximin 400 mg orally three times daily for 10 days for refractory period. Long-term maintenance with sub antimicrobial dosing. If failed treatment, possible isotretinoin.
o Rheumatoid arthritis (RA): Evaluation: Morning stiffness and joint pain, symmetric polyarthritis, ulnar deviation, rheumatoid nodules, insidious onset, symmetrical swelling of multiple joints/tenderness, and pain. Chronic systemic inflammatory disease whose major manifestation is synovitis of multiple joints. More common in women than men, cause is unknown, genetic determinant, chronic synovitis with formation of a pannus which erodes cartilage bone ligaments and tendons, effusion are common signs of inflammation. Symptoms include dryness of mouth, eyes, and other mucous membranes, and scleritis. Other symptoms include interstitial lung disease, pericarditis, pleural disease, palmar erythema, vessel vasculitis, narcotizing arteritis, and Felty syndrome. Diagnostics: Anti-CCP antibodies and rheumatoid factor are present in 70-80 percent of cases, ESR/C-reactive protein are typically elevated and antinuclear antibodies are found in about 20% of RA patients. Arthrocentesis is needed to diagnose superimposed septic arthritis-common complication. Imaging: radiographic changes are the most specific to RA. Differentials: osteoarthritis, CPPD disease, gouty tophi, spondyloarthropathies, Chronic Lyme arthritis, acute viral infections like chikungunya virus and parvovirus B19, chronic infection with hepatitis C, SLE, polymyalgia rheumatica, granulomatosis with polyangiitis, rheumatic fever, carditis and erythema marginatum, variety of cancers, hypertrophic pulmonary osteoarthropathy. TREATMENT: (corticosteroids, synthetic disease-modifying antirheumatic drugs (DMARDs), biologic DMARDs, and DMARD combinations) Low-dose corticosteroids like oral prednisone 5-10 mg daily, intra-articular corticosteroids may be helpful, triamcinolone 10-40 mg intra-articular. Methotrexate/synthetic DMARDs, 7.5 mg initially orally once weekly, increase by 15 mg once per week if initial does is not therapeutic, max dos is 20-25 mg/wk. Sulfasalazine, second line agent 0.5 BID, increase by 0.5 up to 3 g. Leflunomide/pyrimidine synthesis inhibitor, FDA approved for RA treatment, daily dose of 20 mg. Antimalarials, hydroxychloroquine sulfate 200-400 mg/day orally and tofacitinib/inhibitor of janus kinase 3 for refractory RA to methotrexate and dose includes tofacitinib 5-10mg twice daily. Biologic DMARDs: Tumor necrosis factor inhibitors, abatacept, rituximab, tocilizumab. DMARD combinations: methotrexate and TNF, methotrexate, sulfasalazine, and hydroxychloroquine, methotrexate plus etanercept.
o Osteoarthritis (OA): Evaluation: Degenerative disorder with minimal articular inflammation, no systemic symptoms, pain relieved by rest, most common form of joint disease, disease of aging. Age, obesity, and sex (more females than males) are risk factors, degeneration of cartilage and by hypertrophy of bone at the articular margins. Hereditary and mechanical factors for pathogenesis. Causes Heberden nodes and Bouchard nodes. Primary (most commonly affects DIP and proximal interphalangeal joints in fingers, hip, knee MTP joint and cervical/lumbar spine) vs secondary (occurs in any joints). Onset insidious. Diagnostics: No lab signs of inflammation, Radiographs can reveal narrowing, osteophyte formation, thickened subchondral bone, and bone cysts. DIFFERENTIALS: arthritides, RA, metastatic neoplasia, osteoporosis, multiple myeloma and other bone disease. TREATMENT: Acetaminophen, NSAIDS (GI/renal toxicity), and intra-articular injections (triamcinolone 20-40 mg).
o Rhabdomyolysis: Evaluation: acute necrosis of skeletal muscle associated with myoglobinuria and markedly elevated creatine kinase levels. Complication: acute tubular necrosis is common, oliguric renal failure, compartment syndrome, disseminated intravascular coagulation and cardiac arrhythmias are serious but less common. Cocaine use, alcohol intoxication, crush injuries to muscle, prolonged immobility, drug toxicities, hypothermia, and medication/statins. Diagnostics: Elevated creatine kinase levels, elevated serum levels of AST, ALT and lactate dehydrogenase, and UA positive for blood. TREATMENT: Fluid resuscitation 4-6 L/day, infusion of mannitol 100 mg/day urine alkalization.
o Giant cell arteritis: EVALUATION: elevated ESR, age over 50 years, headache, jaw claudication, polymyalgia rheumatica, visual abnormalities. Systemic panarteritis affecting medium-sized and large vessels, AKA temporal arteritis, can cause blindness and large artery complications and requires high-dose prednisone (40-60 mg/day). Cause unknown. Diagnostics: over the age of 50, will also have polymyalgia rheumatica, varicella-zoster found in 75% of cases, headache, scalp tenderness, visual symptoms, jaw claudication or throat pain. Can cause fever of unknown origin over the age of 65, and 90% of patients with giant cell arteritis have ESRs higher than 50 mm/h, biopsy proves giant cell arteritis, mild normochromic normocytic anemia and thrombocytosis, elevated alkaline phosphatase. DIFFERENTIALS: malaise, anemia, rheumatic disease/RA, plasma cell myeloma, malignant disorder, and chronic infections like endocarditis and osteomyelitis. Treatment: Prednisone 60 mg/day (1 month) then taper.
o Reactive arthritis/formerly Reiter Syndrome: Evaluation: usually follows dysentery or STI, HLA-B27-positive in 50-80% of patients, oligoarthritis, conjunctivitis, urethritis, and mouth ulcers are most common features. Precipitated by antecedent gastrointestinal and genitourinary infection (1-4 weeks) and manifests as an asymmetric sterile oligarthritis typically lower extremities. Diagnostics: HLA-B27-positive in 50-80% of patients, radiographic sings of permanent or progressive joint disease seen in sacroiliac as well as peripheral joints. Differentials: Gonococcal arthritis, RA, ankylosing spondylitis, and psoriatic arthritis, Behcet disease and HIV common with reactive arthritis. Treatment: NSAIDs or individuals who do not response to NSAIDs can use sulfasalazine 1000 mg PO BID or methotrexate 7.5-20 mg PO per week, or if that is ineffective than anti-TNF agents.
o Poisonings – symptoms / antidotes: Symptoms: Coma/airway protection, Hypothermia, hypotension, hypertension, arrhythmias, seizures, hyperthermia. Antidotes: Naloxone-opioid antagonists, and Flumazenil-for benzodiazepine overdose. TABLE 38-3 page 1594; Chapter 38; page 1591-1619
o Acetaminophen overdose: Specific antidote: N-Acetylcysteine (based on serum level). Overdose-greater than 150-200 mg/kg, or 8-10 g in an average adult. Causes hepatotoxicity, recommended maximum dose of 4g/day for several days. Causes nausea or vomiting, signs of toxicity may not show until 24-48 hours after ingestion. Fulminant hepatic necrosis can occur, jaundice, hepatic encephalopathy, AKI and death. Could cause acute comma, seizures, hypotension and metabolic acidosis. Diagnosis: Based on measurement of the serum acetaminophen level. TREATMENT: activated charcoal if it can be given 1-2 hours of ingestion; if serum or plasma acetaminophen level falls above the line on monogram/Figure 38-1 page 1599, treatment with N-acetylcysteine is indicated. PO or IV, PO 140 mg/kg followed by 70 mg/kg Q4H, 72-hour treatment. IV 150 mg/kg over 60 minutes, then 4-hour infusion 50 mg/kg and then 16-hour IV infusion of 100 mg/kg. Call poison control center.
o Amphetamine/Cocaine overdose: euphorigenic and stimulant properties, causes anxiety, tremulousness, tachycardia, HTN, diaphoresis, dilated pupils, agitation, muscular hyperactivity and psychosis. TREATMENT: maintain patent airway, assist if necessary, treat for seizures, lower body temperature, give IVF to prevent myoglobinuric kidney injury in patient with rhabdomyolysis. Treat symptoms with benzodiazepines such as diazepam 5-10 mg or lorazepam 2-3 mg IV. Phenobarbital 15 mg/kg IV for persistent seizures. Phentolamine 1-5 mg IV for HTN or nitroprusside, treat arrhythmias with short-acting BB such as esmolol.
o Shoulder impingement syndrome: EVAULATION: subacromial impingement syndrome-shoulder pain with overhead motion, night pain while sleeping on shoulder; a collection of diagnosis that cause mechanical inflammation in the subacromial space, can be caused due to muscle strength imbalances, poor scapula control, rotator cuff tears, and subacromial bursitis/bone spurs. Clinically presents with one or more of the following: pain with overhead activities, nocturnal pain with sleeping on the shoulder or pain on internal rotation (putting on a jacket or bra). Atrophy in the supraspinatus or infraspinatus fossa, dyskinesis, rolled-forward shoulder posture of head forward posture, tenderness over anterolateral shoulder, lack full active range of motion but should have preserved passive ROM, + NEER and +HAWKINS impingement signs. Diagnostics: AP scapula, AP acromioclavicular joint, lateral scapula, and axillary lateral radiographs. MRI/US show tears or tendinosis, US can also show thickening of rotator cuff tendons and tendinosis. TREATMENT: conservative: first-line treatment: Education and PT, activity modification. No evidence for ICE/NSAIDS, some relief with corticosteroid injections.
o Rotator cuff tear: Evaluation: common cause of shoulder impingement syndrome after age 40 (partial tears), difficulty lifting the arm with limited active ROM, weakness with resisted strength testing, caused by trauma or can be degenerative. Common with falls, outstretched arm or pulling on the shoulder, overhead movement or lifting. Full thickness rotator cuff tears may require surgical treatment. Tears at supraspinatus. Weakness or pain with overhead movement and night pain. Clinical findings include impingement syndrome except that full-thickness rotator cuff tears there may be more obvious weakness noted with light resistance testing of specific rotator cuff muscles. Supraspinatus tendon strength +OPEN CAN test. Will also have +NEER/HAWKINS tests. Diagnostics: AP scapula, axillary lateral, supraspinatus outlet, and AP acromioclavicular joint views. MRI is the best method for visualizing rotator cuff tears, or US. TREATMENT: Partial tears: PT and scapular/rotator cuff muscle strengthening. Full-thickness rotator cuff tears: do not heal well, **most young active patients with acute, full-thickness tears should be treated with operative fixation. If no surgery, could lead to OA.
o Adhesive Capsulitis: AKA Frozen shoulder Evaluation: Acute inflammation of the capsule followed by scarring and remodeling; very painful shoulder triggered by minimal or no trauma, pain out of proportion to clinical findings during the inflammatory phase, stiffness during the freezing phase and resolution during the thawing phase. Patients 40-65 y/o, more common in women than men, debilitation disease, especially with endocrinology disorders. Limited ROM for both passive and active movements, Limited or +external rotation exam. Three phases: (a) inflammatory (4-6 months, very painful), (b) freezing (4-5 months, stiffer and stiffer, pain improving), and (c) thawing phase (1-year, shoulder slowly regains motion). Diagnostics: Standard AP, axillary, and lateral glenohumeral radiographs, and clinical diagnosis. TREATMENT: NSAIDs and PT during freezing stage.
o Lumbar disk herniation: Evaluation: Usually due to bending or heavy loading/lifting with the back in flexion causing herniation or extrusion of disk contents into the spinal cord area. Pain with back flexion or prolonged sitting, radicular pain into the leg due to compression of neural structurers, and lower extremity numbness and weakness. Disk herniations with Degenerative disk disease, compression of neural structures will cause pain, cauda equina syndrome -surgical emergency. Sciatica, worsen with back flexion/bending/sitting. Differential: r/o cauda equina syndrome, bowel/bladder incontinence. Diagnostic: plain radiographs, MRI to assess level and morphology of the herniation and recommended for surgery. TREATMENT: bed rest for 48 hours, first-line treatment: NSAIDs and analgesics, PT, McKenzie exercises, and oral Prednisone 1mg/kg daily and tapering over 10-15 days, neuropathic pain-calcium channel alfph-2-delta ligands like gabapentin, and tricyclic antidepressants. Other treatments include Epidural and transforaminal corticosteroids injections. Microdiscectomy, percutaneous endoscopic discectomy, disk replacement surgery, spine fusion surgery.
o Hip fractures: Evaluation: increased mortality in elders, osteoporosis, female sex, height greater than 5’8” and over 50 y/o are risk factors. Secondary to fall, internal rotation of hip, require surgical repair, patient may not be able to bear weight, Pain with internal rotation of the hip is the most sensitive test to identify intra-articular hip pathology. + Trendelenburg test can examine weakness or instability of the hip abductors. Diagnostics: AP views of the pelvis and bilateral hips, and frog-leg-lateral views of the painful hip. MRI/CT for hip fracture pattern. TREAMENT: most hip FX need surgery, surgery is recommended with the first 24 hours. Stress FX-protected weight bearing immobilizer and gradual return to activities. Femoral neck FX, hemiarthroplasty or total hip replacement. Peritrochanteric hip FX treatment with ORIF, plate and screw construct or intramedullary devices
o Knee injuries: ACL injury (+Lackman test, anterior drawer test, and Pivot tests), MCL injuries (+valgus stress test, and varus stress test), and PCL injuries (+safe sign and posterior drawer test). Meniscus injuries (+McMurray test, Modified McMurray test, and Thessaly test). Patellofemoral pain, AKA runner’s knee (+apprehension sign and patellar grind test). TREATMENT: ACL Most people with need surgery, MCL injuries can be treated with protected weight bearing and PT, Isolated PCL injuries can be treated nonoperatively, immobilization with knee brace and knee extension, crutches, PT, however, PCL associated with other injuries that require operative reconstruction. Conservative treatment with Meniscus injuries, analgesics and PT. Conservative treatment ice/anti-inflammatory medication for runner’s knee and surgical treatment is last resort.
o Ankle injuries: Both Inversion (localized pain/swelling, majority of ankle injuries/lateral ligaments) and Eversion-high ankle sprains (severe and prolonged pain, limited ROM, mild swelling, difficulty with weight bearing). Inversion +anterior drawer test, subtaler tilt test. Imaging: Ottawa ankle rules. Eversion +external rotation stress test, affects anterior tibiofibular ligament, more painful than typical ankle sprain. TREATMENT: Inversion-MICE: modified activities, ice, compression, and elevation. PT and early motion. Eversion: Conservative with a cast or walking boot for 4-6 weeks, then weight bearing with crutches and PT.
o Bone density: Bone density screening: Identify patients at risk for osteopenia or osteoporosis. Calcium and vitamin D intake, bone health-bone densitometry serum calcium and 25-OH vitamin D levels.
• Procedures (review the indications, procedure steps, and education)
o Nerve block: digital nerve block for nail removal or ingrown toenails procedures, paronychia sutures dislocation or removal of foreign body. 1% lidocaine, 2-3 mL, and 3 mL syringe, 27-30 gauge, ½-1 inch. Procedure: Position patient, cleanse with antiseptic skin cleanser, and put on gloves. Fingers: insert needle at 45-degree angle, along palmar crease on either side of digit, on anterior surface of the digit close to the bone. Toes: insert needle toward the plantar surface of both sides of the toe, aspirate the syringe before injecting lidocaine, if no blood returns, lidocaine can be injected safely, then redirect the needle across the extensor surface and insert needle further, inject 0.5 mL of lidocaine while withdrawing needle, repeat and wait 5-10 minutes.
o Fish hook: three methods: pull-through, barb sheath, or angler’s string-yank. For pull-through method: 1-position client, 2-put on gloves and cleanse skin with antiseptic, 3-inject 1% lidocaine using the 27-30-gauge needle at the point of the hook, 4-using pliers or hemostat, force the fishhook tip through the skin. 5-cut off the eye of the fishhook close to the skin with wire cutters. 6-attach pliers or hemostats to the sharp end of the hook and pull the hook out. Tetanus prophylaxis if more than 5 years ago, observe for s/s of infection, 5 days of antibiotics including cephalexin 500 mg TID, pain medications, soak in warm salt water for 2 days, return follow up in 28 hours.
o Nail removal: for ingrown toenails and paronychia, education-cut nails straight across, notch center of nail with a V, absorbent socks. TWO methods: cotton wick insertion or partial avulsion with phenolization. Cotton wick insertion procedure: supine, feet flat, sanitize with antiseptic cleanser, file middle third of nail on the affected side with a nail file or emery board, roll cotton to forma. Wick, gently push cotton wick under the distal portion of the lateral nail groove on the affected side using splinter forceps, identify the offending spicule and remove it, continue to insert cotton wick to separate the nail for the groove, apply tincture of iodine to the cotton wick, cauterize granulomatous tissue with silver nitrate stick, bandage the toe. Check toe circulation, pain medication, oral antibiotics for 5 days, like cephalexin, and return to office in two days.
o Skin closure: using Dermabond (tissue adhesive), only about 1/3 of wounds meet criteria for tissue adhesive closure, 5-0 or smaller diameter sutures. Procedure: Access wound, irrigate with saline, apply povidone-iodine to the wound beginning at the wound edges and expanding out in a circular pattern, let dry, remove with alcohol prep pad, put on gloves, topical anesthetic if needed, oppose the wound edges with good approximation, crush the dermabond vial and invert, apply to the approximated would edges with a gently brush motion to the edges-avoids oozing into the wound. Hold wound edges in place for 30 seconds, 10 seconds to make any corrects, apple a total of three layers of adhesive, and optional-steri-strips may be applied. Education: can shower within 6 hours after application, no topical antibiotics s/s of infection, return within 48 hours for follow up
o Skin lesion: (removal) two methods, cautery and cryosurgery (superficial lesions-seborrheic keratoses). Indications for removing skin tags, BCC, actinic keratosis, lentigo, and warts. Contraindications-face or melanomas. Cautery: Position patient, cleanse area, inject under lesion with 1% lidocaine or perform a field block, drap lesion, gloves, cauterize the lesion with the disposable cautery pen, wipe off the burned area, apple topical antibiotic and gauze. For Keloids either cryotherapy, corticosteroid injection or surgical excision. Skin tag/Acrochordon removal: either Snip or cryogenic techniques.
o Suture placement and management: repairs lacerations of the skin. Lidocaine or Bupivacaine used. Complications include infection with gram-positive bacteria (staph aureus or strep) or Gram-negative bacteria (proteus/kelbsiella/pseudomonas). Procedure: Position, apply povidone-iodine, gloves, infiltrate wound with 1% lidocaine-insert needle parallel along each side of the edge of the laceration to the farthest point, carefully explore wound, irrigate with sterile normal saline, trim with iris scissors if wound edges are ragged, place suture needle in needle holder, with opposite hand use forceps with teeth to grasp wound edge and evert the edges, penetrate the wound edge with the suture needing, tie suture off as determined by chosen technique, trim leftover suture to a length suitable for grasping with forceps for easy removal. Once completed, cleanse area with 0.9% sodium chloride, pate dry apply dressing. Keep clean/dry for 24 hours, then dressing can be removed. Bathing after 48 hours, pain management, s/s of infection, clean off crusts, wound check by 48 hours.
o Immobilizations: Clavicle immobilization for clavicle FX. Three methods: clavicle strap technique, figure eight technique or sling and swath technique. Procedure: Clavicle strap technique: Place the straps over the client’s shoulder, one strap over each shoulder, pull straps gently toward the middle of the back and fasten, palpate the fractured clavicle checking that the displaced clavicle is pulled into alignment and obtain x-ray of the chest.
o Bursa injection: Bursa Corticosteroid injection: decrease pain, promote joint function. Procedure: draw up lidocaine and corticosteroid into the syringe, mix by rolling/rocking syringe, mark the injection site with thumbnail, position patient-joint slightly flexed, gloves, clean site with povidone-iodine, insert needle 45-90 degree angle, aspirate-if blood remove needle, should be cloudy bursal fluid, inject corticosteroid, remove needle, apply pressure and cover with band aide.
o Splint: temporary methods of immobilization a joint after joint inflammation or injury, used in place of casting. Ankle, overuse syndrome of wrist and thumb. Ankle splinting (Posterior splint and air cast technique), knee immobilization: use with grade II and II knee strains, wrist splinting (premade wrist splint or volar splinting), and thumb splinting-use for adductor pollicis tendinitis (premade wrist splint with thumb support, aluminum thumb splint and thumb spica).
o Trigger finger: (stenosing flexor tenosynovitis) if persistent symptoms not relieved by splinting or use of NSAIDs, glucocorticoid injections with methylprednisolone or triamcinoloine with lidocaine can be used. Injection can be repeated in six weeks if symptoms have not improved. If this does not work, then ultra-sound guided percutaneous and open surgical release of the first annular (A1) pulley ligament are both effective. Trigger point injections page 202
NEURO
After heart disease and cancer, stroke has been ranked as the third leading cause of death in the United States. Stroke, defined as a sudden onset of focal neurologic deficiency, is due to interruption of blood flow to the brain. Blood flow may be impaired due to structural abnormalities in blood vessels or blockage of vessels due to thrombi. The two major categories of stroke include hemorrhagic (intracerebral, subarachnoid) and ischemic.
During the stroke patient’s stay in the hospital, the major concern is to limit the neurologic deficit due to the acute stroke by placing patients on the proper treatments to prevent the reoccurrence of strokes. In addition, prevention of complications from the acute stroke is also a major concern. Complications may include hemorrhagic transformation, ischemic cerebral edema, infections, venous thrombosis, or pulmonary embolisms.
Impact of Stroke
• 3rd leading cause of death in the U.S.
• Leading cause of adult disability
• Over 700,000 new stroke cases per year in U.S. with 150,000 stroke deaths per year
• 85% are ischemic
• Less than 25% of eligible thrombolytic candidates receiving therapy
The most common cause of non-traumatic intracerebral hematoma is hypertensive hemorrhage. Other causes include amyloid angiopathy, a ruptured vascular malformation, coagulopathy, hemorrhage into a tumor, venous infarction, and drug abuse.
Stroke Assessment Scales Overview
TYPE NAME AND SOURCE APPROXIMATE TIME TO ADMINISTER STRENGTHS WEAKNESSES
Level-of-consciousness scale Glasgow Coma Scale [a]
2 minutes Simple, valid, reliable. None observed.
Stroke deficit scales NIH Stroke Scale [b]
2 minutes Brief, reliable, can be administered by non-neurologists. Low sensitivity.
Canadian Neurological Scale [c]
5 minutes Brief, valid, reliable. Some useful measures omitted.
Global disability scale Rankin Scale [d, e]
5 minutes Good for overall assessment of disability. Walking is the only explicit assessment criterion. Low sensitivity.
Measures of disability/activities of daily
living (ADL) Barthel Index [f]
5-10 minutes Widely used for stroke. Excellent validity and reliability. Low sensitivity for high-level functioning.
Functional Independence Measure
(FIM) [g]
40 minutes Widely used for stroke. Measures
mobility, ADL, cognition, functional communication. “Ceiling” and “floor”
effects.
Mental status screening Folstein Mini-Mental State Examination [h]
10 minutes Widely used for screening. Several functions with summed score. May
misclassify patients with aphasia.
Neurobehavioral
Cognition Status Exam (NCSE) [i]
10 minutes Predicts gain
in Barthel Index scores. Unrelated to age. Does not distinguish
right from left hemisphere. No reliability studies in stroke.
No studies of factorial structure. Correlates with education.
Assessment of motor function Fugl-Meyer [j]
30-40 minutes Extensively evaluated measure. Good validity and reliability
for assessing sensorimotor function and balance. Considered too complex and time-consuming by many.
Motor Assessment Scale [k]
15 minutes Good, brief assessment of movement
and physical mobility. Reliability assessed only in stable
patients. Sensitivity not tested.
Motricity Index [l]
5 minutes Brief assessment of motor function
of arm, leg, and trunk. Sensitivity not tested.
Balance assessment Berg Balance Assessment [m]
10 minutes Simple, well established with stroke patients,
sensitive to change. None observed.
Mobility assessment Rivermead Mobility Index [n]
5 minutes Valid, brief, reliable test of physical mobility. Sensitivity not tested.
Assessment of speech and
language functions Boston Diagnostic
Aphasia Examination [o]
1-4 hours Widely used, comprehensive,
good standardization data, sound theoretical rationale. Time to administer
long; half of patients cannot be classified.
Porch Index of
Communicative Ability (PICA) [p]
1/2-2 hours Widely used, comprehensive,
careful test development and standardization. Time to administer
long. Special training required to administer. Inadequate sampling
of language other than one word and single sentences.
Western aphasia
Battery [q]
1-4 hours Widely used, comprehensive. Time to administer
long. “Aphasia quotients” and “taxonomy”
of aphasia not well validated.
Depression scales Beck Depression Inventory (BDI) (BDI) [r]
10 minutes Widely used, easily administered. Norms available. Good
with somatic symptoms. Less useful in elderly and in patients with aphasia or neglect.High
rate of false positives. Somatic items may not be due
to depression.
Center for Epidemiologic Studies
Depression (CES-D) [s]
< 15 minutes Brief, easily administered, useful
in elderly, effective for screening in stroke population. Not appropriate for aphasic patients.
Geriatric Depression Scale (GDS)
[t]
10 minutes Brief, easy to use with elderly,
cognitively impaired, and those with visual or physical problems
or low motivation. High false negative rates in minor
depression.
Hamilton Depression Scale [u]
< 30 minutes Observer rated; frequently used
in stroke patients. Multiple differing versions compromise
interobserver reliability.
Quick Inventory of Depressive Symptomatology (QIDS) 5-10 minutes Good internal consistency, correlates significantly with clinician ratings of depression severity, and is sensitive to change
Measures of instrumental
ADL PGC Instrumental Activities of Daily Living
[v]
5-10 minutes Measures broad base of information necessary
for independent living. Has not been tested in stroke patients.
Frenchay Activities
Index [w]
10-15 minutes Developed specifically
for stroke patients; assesses broad array of activities. Sensitivity and
interobserver reliability not tested; sensitivity probably limited.
Family assessment Family Assessment Device (FAD) [x]
30 minutes Widely used in stroke. Computer scoring available. Excellent
validity and reliability. Available in multiple languages. Assessment subjective; sensitivity not tested; “ceiling”
and “floor” effects.
Health status/ quality of
life measures Medical Outcomes Study (MOS) 36-Item Short-Form
Health Survey [y]
10-15 minutes Generic health status scale SF36 is improved
version of SF20. Brief, can be self – administered or administered
by phone or interview. Widely used in the United States. Possible “floor” effect in seriously
ill patients (especially for physical functioning), suggests
it should be supplemented by an ADL scale in stroke patients.
Sickness Impact
Profile (SIP) [z]
20-30 minutes Comprehensive
and well-evaluated. Broad range of items reduces “floor”
or “ceiling” effects. Time to administer
somewhat long. Evaluates behavior rather than subjective health;
needs questions on well-being, happiness, and satisfaction.
Stroke Syndromes
(See pg 1003 in Papadakis for “Features of Major Stroke Subtypes”)
Lobes of the Brain
The three main components of the brain—the cerebrum, the cerebellum, and the brainstem—have distinct functions. The cerebrum is the largest and most developmentally advanced part of the human brain. It is responsible for several higher functions, including higher intellectual function, speech, emotion, integration of sensory stimuli of all types, initiation of the final common pathways for movement, and fine control of movement.
The cerebellum, the second largest area, is responsible for maintaining balance and further control of movement and coordination.
The brain stem is the final pathway between cerebral structures and the spinal cord. It is responsible for a variety of automatic functions, such as control of respiration, heart rate, and blood pressure, wakefullness, arousal and attention.
The cerebrum is divided into a right and a left hemisphere and is composed of pairs of frontal, parietal, temporal, and occipital lobes.
The left hemisphere controls the majority of functions on the right side of the body, while the right hemisphere controls most of functions on the left side of the body The crossing of nerve fibers takes place in the brain stem. Thus, injury to the left cerebral hemisphere produces sensory and motor deficits on the right side, and vice versa.
One hemisphere has a slightly more developed, or dominant, area in which written and spoken language is organized. Over 95% of right-handed people and even the majority of left handed people have dominance for speech and language in the left hemisphere. Thus, a left hemisphere stroke will be more likely to produce aphasia and other language deficits.
Layers of the Cerebrum – Gray and White Matter
The entire cerebrum is composed of two layers. The 20-millimeter thick outermost layer, called the cerebral cortex (or gray matter), contains the centers of cognition and personality and the coordination of complicated movements. As shall be seen, the gray matter is also organized for different functions.
The white matter is a network of fibers that enables regions of the brain to communicate with each other.
Cerebellum and Brainstem
A stroke involving the cerebellum may result in a lack of coordination, clumsiness, shaking, or other muscular difficulties. These are important to diagnose early, since swelling may cause brainstem compression or hydrocephalus.
Strokes in the brainstem are usually due to basilar occlusion, although in many cases the clinical syndrome may fit the criteria for a lacunar stroke [Mohr JP and Sacco RL, 1992]. Brainstem strokes can be serious or even fatal. People who survive may be left with severe impairments or remain in a vegetative state.
Blood Vessels of the Brain
The common carotid arteries have two divisions. The external carotid arteries supply the face and scalp with blood. The internal carotid arteries supply blood to most of the anterior portion of the cerebrum. The vertebrobasilar arteries supply the posterior two-fifths of the cerebrum, part of the cerebellum, and the brain stem.
Any decrease in the flow of blood through one of the internal carotid arteries brings about some impairment in the function of the frontal lobes. This impairment may result in numbness, weakness, or paralysis on the side of the body opposite to the obstruction of the artery.
Occlusion of one of the vertebral arteries can cause many serious consequences, ranging from blindness to paralysis.
At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis. From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerebral artery (MCA), the posterior cerebral artery (PCA)—arise and travel to all parts of the brain.
Because the carotid and vertebrobasilar arteries form a circle, if one of the main arteries is occluded, the distal smaller arteries that it supplies can receive blood from the other arteries (collateral circulation).
The anterior cerebral artery extends upward and forward from the internal carotid artery. It supplies the frontal lobes, the parts of the brain that control logical thought, personality, and voluntary movement, especially of the legs. Stroke in the anterior cerebral artery results in opposite leg weakness. If both anterior cerebral territories are affected, profound mental symptoms may result (akinetic mutism).
The middle cerebral artery is the largest branch of the internal carotid. The artery supplies a portion of the frontal lobe and the lateral surface of the temporal and parietal lobes, including the primary motor and sensory areas of the face, throat, hand and arm, and in the dominant hemisphere, the areas for speech.
***The middle cerebral artery is the artery most often occluded in stroke.
The posterior arteries supply the temporal and occipital lobes of the left cerebral hemisphere and the right hemisphere. When infarction occurs in the territory of the posterior cerebral artery, it is usually secondary to embolism from lower segments of the vertebral basilar system or heart.
Clinical symptoms associated with occlusion of the posterior cerebral artery depend on the location of the occlusion and may include thalamic syndrome, thalamic perforate syndrome, Weber’s syndrome, contralateral hemplegia, hemianopsia and a variety of other symptoms, including including color blindness, failure to see to-and-fro movements, verbal dyslexia, and hallucinations. The most common finding is occipital lobe infarction leading to an opposite visual field defect.
Small, deep penetrating arteries known as the lenticulostriate arteries branch from the middle cerebral artery Occlusions of these vessels or penetrating branches of the Circle of Willis or vertebral or basilar arteries are referred to as lacunar strokes. About 20% of all stokes are lacunar and have a high incidence in patients with chronic hypertension.
Left (Dominant) Hemisphere Stroke: Common Pattern
• Aphasia
• Right hemiparesis
• Right-sided sensory loss
• Right visual #eld defect
• Poor right conjugate gaze
• Dysarthria
• Difficulty reading, writing, or calculating
Right (Non-dominant) Hemisphere Stroke: Common Pattern
• Neglect of left visual field
• Extinction of left-sided stimuli
• Left hemiparesis
• Left-sided sensory loss
• Left visual #eld defect
• Poor left conjugate gaze
• Dysarthria
• Spatial disorientation
Brain Stem / Cerebellum / Posterior Hemisphere Stroke: Common Patterns
• Motor or sensory loss in all four limbs
• Crossed signs
• Limb or gait ataxia
• Dysarthria
• Dysconjugate gaze
• Nystagmus
• Amnesia
• Bilateral visual field defects
Small Subcortical Hemisphere or Brain Stem (Pure Motor) Stroke:
• Weakness of face and limbs on one side of the body without abnormalities of higher brain
function, sensation, or vision
Small Subcortical Hemisphere or Brain Stem (Pure Sensory) Stroke:
• Decreased sensation of face and limbs on one side of the body without abnormalities of higher
brain function, motor function, or vision
Tests for the Emergent Evaluation of the Patient with Acute Ischemic Stroke
• 1st test: CT of the brain without contrast (relatively insensitive to acute ischemic strokes within the first 6-12 hrs); subsequent MRI with diffusion-weighted sequences helps define the distribution and extent of infarction as well as exclude tumor or other differentials
• Electrocardiogram
• Chest x-ray
• Hematologic studies (complete blood count, platelet count, prothrombin time, partial thromboplastin time)
• Serum electrolytes
• Blood glucose
• Renal and hepatic chemical analyses
• National Institutes of Health Scale (NIHSS) score
TREATING A STROKE
HEPARIN: Binds to platelets and plasma proteins
“Patients who may be candidates for "fibrinolytic therapy should be transported to hospitals identified as capable of providing acute stroke care, including 24-hours availability of CT scan and interpretation.” “Stroke presenting with 3 hours should be triaged on an emergent basis with urgency similar to acute ST-elevation myocardial infarction.”
Intravenous fibrinolysis for acute ischemic stroke
• Class I IV - t-PA within 3 hours of onset
• Class Indeterminate IV - t-PA between 3 and 6 hours of onset
Intra-arterial fibrinolysis
• Class IIb IA prourokinase within 3 to 6 hours after symptom onset
NIH National Symposium Recommendations
• Door-to-MD: < 10 minutes
• Door-to-Neurologic Expertise: < 15 minutes
• Door-to-CT scan: < 25 minutes
• Door-to-CT Interpretation: < 45 minutes
• Door-to-Drug: (80% compliance) < 60 minutes
• Door-to-Admission: < 3 hours
Cincinnati Pre-Hospital Stroke Scale
Facial Droop
• Normal: Both sides of face move equally
• Abnormal: One side of face does not move at all
Arm Drift
• Normal: Both arms move equally or not at all
• Abnormal: One arm drifts compared to the other
Speech
• Normal: Patient uses correct words without slurring
• Abnormal: Slurred or inappropriate words or mute
Know your stroke team before you need them
• Check glucose
• Two large IV lines
• Oxygen as needed
• Cardiac monitor
• Continuous pulse-ox
• Stat non-contrast CT scan
• ECG
• CXR
• Get rt-PA > Prepare to mix > Have pharmacy alerted
• Discuss options with patient and family
• Contact primary care provider
American Heart Association Recommendations
Oxygen - Use to correct hypoxia; Suggestion that supernormal levels may hurt > one-year survival 69% 3L NC vs 73% control
Glucose - Maintain euglycemia; Treat glucose > 300 mg/dl with insulin
MODIFIABLE R/F:
High blood pressure • Cigarette smoking • Transient ischemic attacks • Heart disease • Diabetes mellitus • Hypercoagulopathy • Carotid stenosis • Other
NON-MODIFIABLE R/F:
Age • Gender • Race • Prior stroke • Heredity
Early CT Changes in Ischemic Stroke
• Loss of insular ribbon
• Loss of gray-white interface
• Loss of sulci
• Acute hypo density
• Mass effect
• Dense MCA sign
Differential Diagnosis: Intracerebral hemorrhage • Hypoglycemia / Hyperglycemia • Seizure • Migraine headache • Hypertensive crisis • Epidural / Subdural • Meningitis / Encephalitis / Brain abscess • Tumor
Exclusions to Thrombolytics
• Stroke or head trauma in 3 mos
• Major surgery within 14 days
• Any history of intracranial hemorrhage
• SBP > 185 mm Hg
• DBP > 110 mm Hg
• Rapidly improving or minor symptoms
• Symptoms suggestive of subarachnoid hemorrhage
• Glucose < 50 or > 400 mg/dl
• GI hemorrhage within 21 days
• Urinary tract hemorrhage within 21 days
• Arterial puncture at non-compressible site past 7 days
• Seizures at the onset of stroke
• Patients taking oral anticoagulants
• Heparin within 48 hours AND an elevated PTT
• PT >15 / INR >1.4
• Platelet count <100 X 10/L
“Patients were also excluded if aggressive measures were required to lower the blood pressure to within specified limits”
Pretreatment BP Treatment
“Gentle” management if thrombolytic candidate:
• SBP > 180 mm Hg
• DBP > 110 mm Hg
Choices:
• Labetalol 10 - 20 mg IV
• Enalapril 1.25 mg IV
• Nitropaste 1” to chest wall
*****No nipride or nitroglycerin gtts
Treatment Considerations: Who Will Benefit from rt-PA?
• Patient age and past medical history (diabetes)
• Time from onset
• Blood pressure
• Stroke severity
• Stroke subtype
• CT findings
Factors Associated with Increased Risk of ICH
• Treatment initiated > 3 hours
• Increased thrombolytic dose
• Elevated blood pressure
• NIHSS > 20 *
• Acute hypodensity or mass effect *
(* Even though increased r/o ICH, still with benefit vs. placebo)
rt-PA Dosing
• 0.9 mg/kg (max = 90 mg)
• 10% bolus (over 1 minute)
• Remainder as a 1-hour infusion
• Have rt-PA in the Emergency Department
Post Treatment Care - Antihypertensive Therapy (SBP 180 - 230 or DBP 105-120 mm Hg)
• Labetalol 10 mg IV, may repeat / double to 150 mg max
• Labetalol drip 2-8 mg / min
SBP > 230 or DBP 121 - 140 mm Hg
• Above
• Sodium nitroprusside
DBP > 140 mm Hg
• Sodium nitroprusside (0.5 ug/kg per minute)
May consider enalapril in patients with CHF, asthma, abnormal cardiac conduction
Management of Seizures
Prophylactic anticonvulsant medication not recommended
Recurrent seizures require treatment
• Diazepam 5 mg over 2 minutes
• Lorazepam 1-4 mg over 2–10 minutes
• Follow benzodiazepines with longer acting anticonvulsant (phenytoin, phenobarbital, etc.)
Pneumonia After Stroke
• One third of stroke patients develop a pneumonia within 1 month
• 3rd leading cause of death in the first month
• Estimated cost per event $10,000 and a 7-day length of stay
• Laryngeal cough reflex cough tests can identify patients at risk.
SUBARACHNOID HEMORRHAGE
Possible complications after subarachnoid hemorrhage include chemical meningitis, vasospasm, hydrocephalus, rebleeding, and brain edema.
Subarachnoid hemorrhage is sudden bleeding into the subarachnoid space. The most common cause of spontaneous bleeding is a ruptured aneurysm. Symptoms include sudden, severe headache, usually with loss or impairment of consciousness. Secondary vasospasm (causing focal brain ischemia), meningismus, and hydrocephalus (causing persistent headache and obtundation) are common. Focal deficits frequently absent. Diagnosis is by CT (1st test) or MRI; if neuroimaging is normal, diagnosis is by CSF analysis. Treatment is with supportive measures and neurosurgery or endovascular measures, preferably in a comprehensive stroke center.
Arteriovenous malformations (AVMs): AVMs are tangled, dilated blood vessels in which arteries flow directly into veins. AVMs occur most often at the junction of cerebral arteries, usually within the parenchyma of the frontal-parietal region, frontal lobe, lateral cerebellum, or overlying occipital lobe. AVMs also can occur within the dura. AVMs can bleed or directly compress brain tissue; seizures or ischemia may result.
Neuroimaging may detect them incidentally; contrast or noncontrast CT can usually detect AVMs > 1 cm, but the diagnosis is confirmed with MRI. Occasionally, a cranial bruit suggests an AVM. Conventional angiography is required for definitive diagnosis and determination of whether the lesion is operable.
Superficial AVMs > 3 cm in diameter are usually obliterated by a combination of microsurgery, radiosurgery, and endovascular surgery. AVMs that are deep or < 3 cm in diameter are treated with stereotactic radiosurgery, endovascular therapy (eg, preresection embolization or thrombosis via an intra-arterial catheter), or coagulation with focused proton beams.
Aneurysms may bleed into the subarachnoid space, causing subarachnoid hemorrhage. Before rupture, aneurysms occasionally cause sentinel (warning) headaches due to painful expansion of the aneurysm or to blood leaking into the subarachnoid space. Actual rupture causes a sudden severe headache called a thunderclap headache.
If < 7 mm, asymptomatic aneurysms in the anterior circulation rarely rupture and do not warrant the risks of immediate treatment. They can be monitored with serial imaging. If aneurysms are larger, are in the posterior circulation, or cause symptoms due to bleeding or due to compression of neural structures, endovascular therapy, if feasible, can be tried.
Blood in the subarachnoid space causes a chemical meningitis that commonly increases intracranial pressure for days or a few weeks. Secondary vasospasm may cause focal brain ischemia; about 25% of patients develop signs of a transient ischemic attack(TIA) or ischemic stroke. Brain edema is maximal and risk of vasospasm and subsequent infarction (called angry brain) is highest between 72 h and 10 days. Secondary acute hydrocephalus is also common. A 2nd rupture (rebleeding) sometimes occurs, most often within about 7 days.
S/S of CHEMICAL MENINGITIS: Headache is usually severe, peaking within seconds. Loss of consciousness may follow, usually immediately but sometimes not for several hours. Severe neurologic deficits may develop and become irreversible within minutes or a few hours. Sensorium may be impaired, and patients may become restless. Seizures are possible. Usually, the neck is not stiff initially unless the cerebellar tonsils herniate. However, within 24 h, chemical meningitis causes moderate to marked meningismus, vomiting, and sometimes bilateral extensor plantar responses. Heart or respiratory rate is often abnormal.
Fever, continued headaches, and confusion are common during the first 5 to 10 days. Secondary hydrocephalus may cause headache, obtundation, and motor deficits that persist for weeks. Rebleeding may cause recurrent or new symptoms.
If subarachnoid hemorrhage is suspected clinically but not identified by neuroimaging or if neuroimaging is not immediately available, lumbar puncture is done. Lumbar puncture is contraindicated if increased intracranial pressure is suspected because the sudden decrease in CSF pressure may lessen the tamponade of a clot on the ruptured aneurysm, causing further bleeding.
CSF findings suggesting subarachnoid hemorrhage include
• Numerous RBCs
• Xanthochromia
• Increased pressure
Treatment in a comprehensive stroke center
• Nicardipine if mean arterial pressure is > 130 mm Hg
• Nimodipine to prevent vasospasm - Vasospasm is prevented by giving nimodipine 60 mg po q 4 h for 21 days to prevent vasospasm, but BP needs to be maintained in the desirable range (usually considered to be a mean arterial pressure of 70 to 130 mm Hg and a systolic pressure of 120 to 185 mm Hg).
• Occlusion of causative aneurysms
PARKINSONISM:
Parkinson disease is a slowly progressive, degenerative disorder characterized by resting tremor, stiffness (rigidity), slow and decreased movement (bradykinesia), and gait and/or postural instability.
S/S:
Tremors - Usually, the hands or feet are affected first, most often asymmetrically. The jaw and tongue may also be affected, but not the voice. Tremor may become less prominent as the disease progresses.
Rigidity develops independently of tremor in many patients. When a clinician moves a rigid joint, semirhythmic jerks due to variations in the intensity of the rigidity occur, having a ratchet-like effect (cogwheel rigidity).
Slow movements (bradykinesia) are typical. Movement also becomes decreased in amplitude (hypokinesia) and difficult to initiate (akinesia).
Rigidity and hypokinesia may contribute to muscle aches and sensations of fatigue. The face becomes masklike (hypomimic), with an open mouth and reduced blinking. Excessive drooling (sialorrhea) may contribute to disability. Speech becomes hypophonic, with characteristic monotonous, sometimes stuttering dysarthria.
Hypokinesia and impaired control of distal muscles cause micrographia (writing in very small letters) and make activities of daily living increasingly difficult. Without warning, voluntary movement, including walking, may suddenly halt (called freezing of gait).
Postural instability may develop, resulting in falls, which occur later in Parkinson disease. Patients have difficulty starting to walk, turning, and stopping. They shuffle, taking short steps, holding their arms flexed to the waist, and swinging their arms little or not at all with each stride. Steps may inadvertently quicken, while stride length progressively shortens; this gait abnormality, called festination, is often a precursor to freezing of gait. A tendency to fall forward (propulsion) or backward (retropulsion) when the center of gravity is displaced results from loss of postural reflexes. Posture becomes stooped.
Dementia develops in about one third of patients, usually late in Parkinson disease. Early predictors of its development are visuospatial impairment (eg, getting lost while driving) and decreased verbal fluency.
Sleep disorders are common. Insomnia may result from nocturia or from the inability to turn in bed. Rapid eye movement (REM) sleep behavior disorder may develop; in this disorder, violent bursts of physical activity occur during REM sleep because the paralysis that normally occurs during REM sleep is absent. Sleep deprivation may exacerbate depression and cognitive impairment, as well as contribute to excessive daytime sleepiness. Recent studies have shown that REM sleep behavior disorder is a marker of synucleinopathies and indicates higher risk of developing Lewy body dementia or Parkinson disease dementia.
Neurologic symptoms unrelated to parkinsonism commonly develop because synucleinopathy occurs in other areas of the central, peripheral, and autonomic nervous systems. The following are examples:
• Almost universal sympathetic denervation of the heart, contributing to orthostatic hypotension
• Esophageal dysmotility, contributing to dysphagia and increased risk of aspiration
• Lower bowel dysmotility, contributing to constipation
• Urinary hesitancy and/or urgency, potentially leading to incontinence (common)
• Anosmia (common)
In some patients, some of these symptoms occur before the motor symptoms of Parkinson disease and frequently worsen over time.
Seborrheic dermatitis is also common.
Diagnosis is clinical, based on motor symptoms
Treatment aims to restore dopaminergic function in the brain with levodopa plus carbidopa and/or other drugs (eg, dopamine agonists, MAO type B [MAO-B] inhibitors, amantadine). For refractory, disabling symptoms in patients without dementia, stereotactic deep brain stimulation or lesional surgery and levodopa and an apomorphine pump may help.
The pathologic hallmark of Parkinson disease is
• Synuclein-filled Lewy bodies in the nigrostriatal system
HUNTINGTON DISEASE:
Huntington disease is an autosomal dominant disorder characterized by chorea, neuropsychiatric symptoms, and progressive cognitive deterioration, usually beginning during middle age. Diagnosis is by genetic testing. First-degree relatives should be offered genetic counseling before genetic tests are done. Treatment is supportive.
DIFFERENCES OF CLINICAL FEATURES FOR ALZHEIMER’S, DEMENTIA W/LEWY BODIES, AND FRONTOTEMPORAL DEMENTIA ON PG 1028 IN PAPADAKIS
MULTIPLE SCLEROSIS:
Multiple sclerosis (MS) is characterized by disseminated patches of demyelination in the brain and spinal cord. MS is believed to involve an immunologic mechanism. One postulated cause is infection by a latent virus (possibly a human herpesvirus such as Epstein-Barr virus), which, when activated, triggers a secondary autoimmune response. An increased incidence among certain families and presence of human leukocyte antigen (HLA) allotypes (HLA-DR2) suggests genetic susceptibility.
Typical patterns of progression:
• Relapsing-remitting pattern: Exacerbations alternate with remissions, when partial or full recovery occurs or symptoms are stable. Remissions may last months or years. Exacerbations can occur spontaneously or can be triggered by an infection such as influenza.
• Primary progressive pattern: The disease progresses gradually with no remissions, although there may be temporary plateaus during which the disease does not progress. Unlike in the relapsing-remitting pattern, there are no clear exacerbations.
• Secondary progressive pattern: This pattern begins with relapses alternating with remissions (relapsing-remitting pattern), followed by gradual progression of the disease.
• Progressive relapsing pattern: The disease progresses gradually, but progression is interrupted by sudden, clear relapses. This pattern is rare.
The most common initial symptoms of multiple sclerosis are the following:
• Paresthesias in one or more extremities, in the trunk, or on one side of the face
• Weakness or clumsiness of a leg or hand
• Visual disturbances (eg, partial loss of vision and pain in one eye due to retrobulbar optic neuritis, diplopia due to internuclear ophthalmoplegia, scotomas)
Other common early symptoms of MS include slight stiffness or unusual fatigability of a limb, minor gait disturbances, vertigo, and mild affective disturbances; all usually indicate scattered CNS involvement and may be subtle. Most patients with MS have difficulty with bladder control (eg, frequency, urgency, hesitancy, incontinence, retention). Fatigue is common. Excess heat (eg, warm weather, a hot bath, fever) may temporarily exacerbate symptoms and signs (Uhthoff phenomenon).
Mild cognitive symptoms are common. Apathy, poor judgment, or inattention may occur. Affective disturbances, including emotional lability, euphoria, or, most commonly, depression, are common. Depression may be reactive or partly due to cerebral lesions of MS. A few patients have seizures.
Dx:
Multiple sclerosis is suspected in patients with optic neuritis, INO, or other symptoms that suggest MS, particularly if deficits are multifocal or intermittent. If MS is suspected, brain MRI and spinal MRI are done.
MRI is the most sensitive imaging test for MS and can exclude other treatable disorders that may mimic MS,
Tx: (pg 1034 Papadakis shows Tx medications as well)
• Corticosteroids
• Immunomodulators to prevent exacerbations and delay eventual disability
• Baclofen or tizanidine for spasticity
• Gabapentin or tricyclic antidepressants for pain
• Supportive care
Tx of Exacerbations and Relapses:
Corticosteroids, given in brief courses, are used to treat acute onset of symptoms or exacerbations that cause objective deficits sufficient to impair function (eg, loss of vision, strength, or coordination); regimens include
• Methylprednisolone 500 to 1000 mg IV once/day for 3 to 5 days
• Less commonly, prednisone 1250 mg po per day (eg, 625 mg po bid or 1250 mg po once/day) for 3 to 5 days
Symptom Control:
• Spasticity is treated with escalating doses of baclofen 10 to 20 mg po tid to qid or tizanidine 4 to 8 mg po tid. Gait training and range-of-motion exercises can help weak, spastic limbs.
• Painful paresthesias are usually treated with gabapentin 100 to 800 mg po tid or pregabalin 25 to 150 mg po bid; alternatives include tricyclic antidepressants (eg, amitriptyline 25 to 75 mg po at bedtime, desipramine 25 to 100 mg po at bedtime ifamitriptyline has intolerable anticholinergic effects), carbamazepine 200 mg po tid, as well as other anticonvulsants, and opioids.
• Depression is treated with counseling and antidepressants.
• Bladder dysfunction is treated based on its underlying mechanism.
• Fatigue can be treated with amantadine 100 mg po tid, modafinil 100 to 300 mg po once/day, armodafinil 150 to 250 mg po once/day, or extended-release amphetamine 10 to 30 mg once/day.
**Acute Cerebral Sequelae of Head Injuries & GCS found on pg 1039 in Papadakis
SPINAL TRAUMA:
The most common causes of spinal cord injuries are
• Motor vehicle crashes (48%)
• Falls (16%) - In the elderly, falls are the most common cause
Effects of Spinal Cord Injury by Location
Location of Injury* Possible Effects†
At or above C5 Respiratory paralysis
Quadriplegia
Between C5 and C6 Paralysis of legs, wrists, and hands
Weakened shoulder abduction and elbow flexion
Loss of brachioradialis deep tendon reflex
Between C6 and C7 Paralysis of legs, wrists, and hands, but shoulder movement and elbow flexion usually possible
Loss of biceps jerk reflex
Between C7 and C8 Paralysis of legs and hands
Loss of triceps jerk reflex
At C8 to T1 With transverse lesions, Horner syndrome (ptosis, miotic pupils, facial anhidrosis)
Paralysis of legs
Between T1 and T12 Paralysis of leg muscles above and below the knee
At T12 to L1 Paralysis below the knee
Cauda equina (usually about L2 to S5) Hyporeflexic or areflexic paresis of the lower extremities
Usually pain and hyperesthesia in the distribution of the affected nerve roots
Usually loss of bowel and bladder control
At S3 to S5 or conus medullaris at L1 Complete loss of bowel and bladder control
*Abbreviations refer to vertebrae; the cord is shorter than the spine, so that moving down the spine, the cord segments and vertebral levels are increasingly out of alignment.
†Priapism, reduced rectal tone, and changes in caudal reflexes may occur with injury at any level.
KEY POINTS:
• In addition to patients with obvious spinal trauma, suspect spinal cord injuries in patients at increased risk for spinal injury, including elderly patients who may have had a fall and patients with an altered sensorium, neurologic deficits suggesting cord injury, or localized spinal tenderness.
• To ensure recognition of incomplete spinal cord injuries, test motor function and sensory function (including light touch, pinprick, and position sensation) and check for disproportionate weakness in the upper extremities.
• Immediately immobilize the spine in patients at risk.
• Arrange for immediate CT or, if available, MRI.
• Arrange for surgery within 24 h of injury if patients have incomplete cord injuries.
• Treat irreversible spinal cord injury with multimodal rehabilitation and drugs that control spasticity.
Guillain-Barre Syndrome:
Guillain-Barré syndrome is an acute, usually rapidly progressive but self-limited inflammatory polyneuropathy characterized by muscular weakness and mild distal sensory loss. Cause is thought to be autoimmune. Guillain-Barré syndrome is the most common acquired inflammatory neuropathy. In some variants, demyelination predominates; other variants affect the axon.
In about two thirds of patients, Guillain-Barré syndrome begins 5 days to 3 wk after a banal infectious disorder, surgery, or vaccination. Infection is the trigger in > 50% of patients; common pathogens include
• Campylobacter jejuni
• Enteric viruses
• Herpesviruses (including cytomegalovirus and Epstein-Barr virus)
• Mycoplasma spp
S/S:
• Flaccid weakness - Relatively symmetric weakness with paresthesias usually begins in the legs and progresses to the arms, but it occasionally begins in the arms or head. In 90% of patients, weakness is usually maximal at 3 to 4 wk
• Deep tendon reflexes are lost
• Facial and oropharyngeal muscles are weak in > 50% of patients with severe disease
• Dehydration and undernutrition may result
• Respiratory paralysis severe enough to require endotracheal intubation and mechanical ventilation occurs in 5 to 10%
• A few patients (possibly with a variant form) have significant, life-threatening autonomic dysfunction causing BP fluctuations, inappropriate ADH secretion, cardiac arrhythmias, GI stasis, urinary retention, and pupillary changes.
Dx:
• Clinical evaluation
• Electrodiagnostic testing
• CSF analysis
Diagnosis of Guillain-Barré syndrome is primarily clinical.
If Guillain-Barré syndrome is suspected, patients should be admitted to a hospital for electrodiagnostic testing (nerve conduction studies and electromyography), CSF analysis, and monitoring by measuring forced vital capacity every 6 to 8 h. Initial electrodiagnostic testing detects slow nerve conduction velocities and evidence of segmental demyelination in two thirds of patients; however, normal results do not exclude the diagnosis and should not delay treatment.
CSF analysis may detect albuminocytologic dissociation (increased protein but normal WBC count), but it may not appear for up to 1 wk and does not develop in 10% of patients.
Tx:
Guillain-Barré syndrome is a medical emergency, requiring constant monitoring and support of vital functions, typically in an ICU. Forced vital capacity should be measured frequently so that respiration can be assisted if necessary; if vital capacity is < 15 mL/kg, endotracheal intubation is indicated. Inability to lift the head off the pillow by flexing the neck is another danger sign; it frequently develops simultaneously with phrenic nerve (diaphragm) weakness.
If oral fluid intake is difficult, IV fluids are given as needed to maintain a urine volume of at least 1 to 1.5 L/day. Extremities should be protected from trauma and from the pressure of bed rest.
Heat therapy helps relieve pain, making early physical therapy possible. Immobilization, which may cause ankylosis and contractures, should be avoided. Passive full-range joint movement should be started immediately, and active exercises should be initiated when acute symptoms subside. Heparin 5000 units sc bid helps prevent deep venous thrombosis in bedbound patients.
Given early, IVIG 400 mg/kg IV once/day for 5 consecutive days is the treatment of choice; it has some benefit up to 1 mo from disease onset.
Plasma exchange helps when done early; it is used if IVIG is ineffective. Plasma exchange is relatively safe, shortens the disease course and hospital stay, and reduces mortality risk and incidence of permanent paralysis. Plasma exchange removes any previously administered IVIG, negating its benefits, and so should never be done during or soon after use of IVIG. Waiting at least 2 to 3 days after stopping IVIG is recommended.
***Do not give corticosteroids in Guillain-Barré syndrome because they may worsen outcome.
BELL’s PALSY:
AKA: Facial nerve (7th cranial nerve) palsy is often idiopathic (formerly called Bell palsy). Idiopathic facial nerve palsy is sudden, unilateral peripheral facial nerve palsy. Symptoms of facial nerve palsy are hemifacial paresis of the upper and lower face. Paresis, often with complete paralysis, develops within hours and is usually maximal within 48 to 72 hours. Patients may report a numb or heavy feeling in the face. The affected side becomes flat and expressionless; the ability to wrinkle the forehead, blink, and grimace is limited or absent. In severe cases, the palpebral fissure widens and the eye does not close, often irritating the conjunctiva and drying the cornea.
Tests (eg, chest x-ray, serum angiotensin-converting enzyme [ACE] level, tests for Lyme disease, serum glucose) are done to diagnose treatable causes.
Treatment may include lubrication of the eye, intermittent use of an eye patch, and, for idiopathic facial nerve palsy, corticosteroids.
KEY POINTS:
• In facial nerve palsy, patients cannot move the upper and lower part of their face on one side; in contrast, central facial nerve lesions (eg, due to stroke) affect primarily the lower face.
• Evidence that the mechanism for what was previously thought to be idiopathic facial nerve palsy is increasingly implicating herpes viruses.
• Diagnosis is clinical, but if onset is not clearly acute, MRI should be done.
• If given early, corticosteroids are helpful for idiopathic facial nerve palsy; antivirals probably provide no benefit.
MYASTHENIA GRAVIS:
Myasthenia gravis involves episodic muscle weakness and easy fatigability caused by autoantibody- and cell-mediated destruction of acetylcholine receptors. It is more common among young women and older men but may occur in men or women at any age.
Precipitating factors for myasthenia gravis include
• Infection
• Surgery
• Certain drugs (eg, aminoglycosides, quinine, magnesium sulfate, procainamide, calcium channel blockers)
The most common symptoms of myasthenia gravis are
• Ptosis
• Diplopia
• Muscle weakness after use of the affected muscle
Weakness resolves when the affected muscles are rested but recurs when they are used again.
Ocular muscles are affected initially in 40% of patients and eventually in 85% and are the only muscles affected in 15%. If generalized myasthenia is going to develop after ocular symptoms, it usually does so within the first 3 yr.
Hand grip may alternate between weak and normal (milkmaid’s grip). Neck muscles may become weak. Proximal limb weakness is common. Some patients present with bulbar symptoms (eg, altered voice, nasal regurgitation, choking, dysphagia). Sensation and deep tendon reflexes are normal. Manifestations fluctuate in intensity over minutes to hours to days.
Myasthenic crisis, a severe generalized quadriparesis or life-threatening respiratory muscle weakness, occurs in about 15 to 20% of patients at least once in their life. It is often due to a supervening infection that reactivates the immune system. Once respiratory insufficiency begins, respiratory failure may occur rapidly.
Cholinergic crisis is muscular weakness that can result when the dose of anticholinesterase drugs (eg, neostigmine, pyridostigmine) is too high. A mild crisis may be difficult to differentiate from worsening myasthenia. Severe cholinergic crisis can usually be differentiated because it, unlike myasthenia gravis, results in increased lacrimation and salivation, tachycardia, and diarrhea.
Dx:
• Bedside tests - The traditional anticholinesterase test, done at bedside and using the short-acting (< 5 min) drug edrophonium, is positive in most patients who have myasthenia with overt weakness. However, this test should only be done in patients with obvious ptosis or ophthalmoparesis; these deficits must be present to be able to clearly see improvement to normal strength and thus provide unequivocal objective evidence of a positive test result. For the test, patients are asked to exercise the affected muscle until fatigue occurs (eg, to hold the eyes open until ptosis occurs); then, edrophonium 2 mg IV is given. If no adverse reaction (eg, bradycardia, atrioventricular block) occurs within 30 sec, another 8 mg is given. Rapid (< 2 min) recovery of muscle function is a positive result. However, this test is not ideal for the following reasons:
A positive result is not definitive for myasthenia gravis because such improvement may occur in other neuromuscular disorders.
Results may be equivocal, particularly if the test is done in patients without obvious ptosis or ophthalmoparesis.
During the test, weakness due to cholinergic crisis may worsen; thus, resuscitation equipment and atropine (as an antidote) must be available during the test.
Because weakness due to myasthenia lessens in cooler temperature, patients with ptosis can be tested using the ice pack test. For this test, an icepack is applied to a patient's closed eyes for 2 min, then removed. A positive result is full or partial resolution of ptosis. The ice pack test usually does not work if patients have ophthalmoparesis.
Patients with opthalmoparesis can be tested using the rest test. For this test, patients are asked to lie quietly in a dark room for 5 min with their eyes closed. If ophthalmoparesis resolves after this rest, the result is positive.
****Try the ice pack or rest test before the anticholinesterase test. Do the anticholinesterase test only if patients have obvious ptosis or ophthalmoparesis (to get unequivocal results), and have resuscitation equipment and atropine (as an antidote) on hand.
• AChR antibody levels, electromyography, or both - Even if a bedside test is unequivocally positive, one or both of the following are required to confirm the diagnosis:
^ Serum AChR antibody levels
^ Electromyography (EMG)
AChR antibodies are present in 80 to 90% of patients with generalized myasthenia but in only 50% with the ocular form. Antibody levels do not correlate with disease severity. Up to 50% of patients without AChR antibodies test positive for anti-MuSK antibodies.
EMG using repetitive stimuli (2 to 3/sec) shows a > 10% decrease in amplitude of the compound muscle action potential response in 60% of patients. Single-fiber EMG can detect abnormal neuromuscular transmission in > 95%.
***The diagnosis of myasthenia gravis is suggested by symptoms and signs and confirmed by tests.
Tx:
• Anticholinesterase drugs to relieve symptoms - Anticholinesterase drugs are the mainstay of symptomatic treatment but do not alter the underlying disease process. Moreover, they rarely relieve all symptoms, and myasthenia may become refractory to these drugs. Pyridostigmine is begun at 60 mg po q 3 to 4 h and titrated up to a maximum of 120 mg/dose based on symptoms. When parenteral therapy is necessary (eg, because of dysphagia), neostigmine (1 mg = 60 mg of pyridostigmine) may be substituted. Anticholinesterase drugs can cause abdominal cramps and diarrhea, which are treated with oral atropine 0.4 to 0.6 mg (given with pyridostigmine or neostigmine) or propantheline 15 mg tid to qid. Patients who have been responding well to treatment and then deteriorate require respiratory support because they may have cholinergic crisis, and anticholinesterase drugs must be stopped for several days.
• Corticosteroids, immunomodulating treatments (eg, IV immune globulin [IVIG], plasma exchange), immunosuppressant drugs, and thymectomy to lessen the autoimmune reaction - Corticosteroids are necessary as maintenance therapy for many patients but have little immediate effect in myasthenic crisis. Over half of patients worsen acutely after starting high-dose corticosteroids. Initially, prednisone 10 mg po once/day is given; dose is increased by 10 mg weekly up to 60 mg, which is given for about 2 mo, then tapered slowly. Improvement may take several months; then, the dose should be reduced to the minimum necessary to control symptoms. Azathioprine 2.5 to 3.5 mg/kg po once/day may be as effective as corticosteroids, although significant benefit may not occur for many months. Cyclosporine 2 to 2.5 mg/kg po bid may allow the corticosteroid dose to be reduced. These drugs require the usual precautions. Other drugs that may be beneficial include methotrexate, cyclophosphamide, and mycophenolate mofetil. For patients with refractory disease, monoclonal antibodies (eg, rituximab, eculizumab) may be beneficial but are costly. Plasma exchange or IVIG is useful for myasthenic crisis and, for patients unresponsive to drugs, before thymectomy.
• Supportive care
***In patients with congenital myasthenia, anticholinesterase drugs and immunomodulating treatments are not beneficial and should be avoided.
MUSCULAR DYSTROPHIES EXPLAINED ON PG 1057 IN PAPADAKIS
Hematologic/Lymphatic/Immune System
• Iron Deficiency Anemia
o Most common cause of anemia world wide
o Signs and Symptoms
Fatigue
Tachycardia
Palpations
Dyspnea on exertion
Severe deficiency causes skin and mucosal changes (smooth tongue, brittle nails, spooning of nails)
Pica (craving non-iron foods
o Laboratory Findings
Develops in stages
o First is depletion of iron stores without anemia followed by anemia with normal red blood cell size (normal MCV) followed by anemia with reduced MCV
Ferritin: value of less than 12 ng/mL is a highly reliable indicator of reduced iron stores. Anyone who is less than 30 ng/mL almost always indicates iron deficiency in anyone who is anemic.
Platelet: commonly increased but usually remains under 800,000 mcL
o Differential Dx: anemia of chronic disease, thalassemia, lead poisoning, congenital X-linked sideroblastic anemia
o Treatment:
Oral Iron: 325 mg ferrous sulfate on empty stomach. Results usually seen within 2 weeks. Continue treatment for 3-6 months
Parenteral Iron: Indicated for intolerance of or refractoriness to oral iron. Most patients require 1-1.5 g
• Anemia of Chronic Disease
o Signs and Symptoms
Clinical features are those of the causative condition
o Labs
Hct rarely falls below 60% of baseline
MCV usually normal or slightly reduced
Red blood cell morphology is usually normal
Reticulocyte count is mildly decreased or normal
Ferritin normal or increased
o Treatment
In most cases no treatment of anemia is necessary, and the primary management is to address the condition causing the anemia
RBC transfusions
Epoetin alfa or darbepoetine (goal hgb between 10-12)
• Thalassemia
o Herediatry disorders characterized by reduction in the sysnthesis of globin chains (alpha or beta).
o Alpha is due primarily to gene deletions causing reduced alpha-globin chain synthesis.
o Beta is usually caused by point mutations rather than deletions.
o Alpha Signs and Symptoms
Normally adults have 4 copies of the alpha-globin chain.
When 3 aplha-globin chains are present the patient is hematologically normal (silent carrier).
When 2 alpha-globin chains are present will have mild microcytic anemia
When only 1 alpha-globin chain is present (Hemoglobin H disease) physical exam may reveal pallor and splenomegaly.
o Beta signs and symptoms
Homozygous for beta thalassemia have thalassemia major.
• Affected children will show signs after 6 months including stunted growth, bony deformities, hepatosplenomegaly, jaundice, and thrombophilia. Transfusions are needed but be watchful for transfusional iron overload.
Patients homozygous for a milder form of beta thalassemia have thalassemia intermedia. Have chronic hemolytic anemia but do not require transfusions except under periods of stress or during aplastic crisis.
o Labs
Hallmark features are small (low MCV) and pale (low mean corpuscular hemoglobin MCH) red blood cells, anemia and a normal to elevated red blood cell count (ie, a large number of the small and pale red blood cells are being produced)
Alpha-thalassemia trait. Mild anemia with Hct between 28-40%, MCV low 60-75 fL and red blood cell count is normal or increased.
Hemoglobin H disease. More marked anemia with Hct 22-32%, MCV low at 60-70 fL, and peripheral blood smear is markedly abnormal with hypochromia, microcytosis, target cells and poikilosytosis.
Beta-thalassemia minor. Modest anemia with Hct between 28-40%, MCV ranges from 55-75 fL., red blood cell is normal to increased.
Beta-thalassemia intermedia. Hct 17-33%, MCV 55-75 and red blood count is normal or increased. Reticulocyte count is elevated.
Beta thalassemia major. Severe anemia and without transfusion the Hct will fall to less than 10%. Peripheral blood smear is bizarre showing severe poikilocytosis, hypochromia, microcytosis, target cells, basophilic stripping and nucleated red blood cells.
o Differential Dx
Iron deficiency anemia
Dx of beta-thalassemia is made by the above findings and hemoglobin electrophoresis showing elevated levels of hemoglobins A2 and F.
o Treatment
Mild thalassemia (alph-thalassemia or beta-thalassemia minor): no treatment, evaluate regularly for iron deficiency.
Hemoglobin H disease: folic acid, avoid medicinal iron, and oxidative drugs such as sulfonamides.
Severe thalassemia: regular transfusion schedule, folic acid. Splenectomy is performed if hypersplenism causes a marked increase in the transfusion requirement or refractory symptoms.
Patients with regular transfusions should be treated with iron chelation (oral or parenteral) in order to prevent life limiting organ damage from iron overload.
• B12 Deficiency
o Signs and symptoms
Slow onset anemia, glossitis, anorexia, diarrhea, neurologic syndrome.
o Labs
Low serum B level. (Normal greater than 210, most with overt deficiency levels less than 170)
o Differential Dx
Folic acid deficiency, myelodysplastic syndrome, acute erythrocytic leukemia.
o Treatment
IM or subcu injections of 100mcg B12. Replacement is usually given daily for the 1 st week, weekly for a month and monthly for life. Oral or sublingual methylcobalamin (1 mg/day) may be used after correction is made.
• Hemolytic Anemia
• Hemolytic anemia is a disorder in which red blood cells are destroyed faster than they can be made. The destruction of red blood cells is called hemolysis.
• 2 types including intrinsic or extrinsic factor
The treatment for hemolytic anemia will vary depending on the cause of the illness. Treatment may include:
• Blood transfusions
• Corticosteroid medicines
• Treatment to strengthen your immune system (using intravenous immune globulin)
• Rituximab
In more severe cases, the following treatments may be needed:
• Surgery to remove the spleen
• Medicine to reduce the strength of your immune system (immunosuppressive therapy)
• Neutropenia
• Causes
o Bone marrow disorders: cyclic neutropenia, congenital neutropenia, hairy cell leukemia, myelodysplasia
o Non-Bone marrow: medications (sulfonamides, chlorpromazine, procainamide, PCN, cephalosporins), aplastic anemia, myelosuppressive cytotoxic chemotherapy, hypersplenism, sepsis, HIV
• Clinical findings
o Results in stomatitis and in infections due to gram-positive or gram-negative bacteria or fungi such as candida or aspergillus. Most common infection syndromes are septicemia, cellulitis, pneumonia, and neutropenic fever of unknown origin.
• Treatment
o Stop potential causative medications
o Autoimmune neutropenia often responds to immunosuppression with corticosteroids.
o Fevers during neutropenia should be considered infectious until proven otherwise.
o Enteric gram-negative bacteria are primary concern and should be treated empirically with fluoroquinolones or third- or fourth-generation cephalosporins.
o Fungal infections are treated with “azoles” (fluconazole for yeast and voriconazole, itraconazole for molds)
• Acute Leukemia
• Classifications
o Acute Myeloid (AML)
o Acute Promyelocytic
o Acute Lymphoblastic
o Mixed Phenotype Acute Leukemias
• Signs and symptoms
o Most ill for only few days or weeks
o Bleeding occurs in the skin and mucosal surfaces
o Infection due to neutropenia
o Gum hypertrophy
o Bone and joint pain
o Purpura and petechiae
• Labs
o Hallmark combination of pancytopenia with circulating blasts.
o Hyperuricemia
o Patients with ALL may have mediastinal mass visible on chest radiograph
• Differential Dx
• CML, toxic insult recovery, CLL, lymphoma, hairy cell leukemia.
• Treatment
o AML: combination of anthracycline plus cytarabine.
o ALL: combination chemotherapy including daunorubicin, vincristine, prednisone, and asaraginase. This treatment produces 90% remission in patients.
• Chronic Leukemia
o Symptoms and signs
CLL is a disease of older patients; 90% after age 50.
Fatigue
Lymphadenopathy
Enlargement of liver or spleen
o Labs
Hallmark sign is isolated lymphocytes. WBC count is usually greater than 20,000 and may be markedly elevated to several hundred thousand
o Differential Dx
Viral infections, lymphoma, hairy cell leukemia, Walden-strom macroglobulinemia
o Treatment
Most early cases require no treatment, just monitor
Indications for treatment include progressive fatigue, symptomatic lymphadenopathy, anemia or thrombocytopenia.
Initial Tx for patients under 70 is chemotherapy with either fludarabine with cyclophosphamide and rituximab or bendamustine with rituximab.
For older patients or young patients with significant co-morbidities, chlorambucil 0.6-1 mg/kg orally every 2-3 weeks has been standard. Watch for bleeding in patients taking coumadin
• Non-Hodgkin Lymphoma
• Signs and symptoms
o Isolated or wide spread lymphandeonpathy
o Fever
o Drenching night sweats
o Weight loss greater than 10%
• Treatments
o Indolent Lymphomas
Most common in this group are follicular lymphoma, marginal zone lymphomas, and small lymphocytic lymphoma.
Depend on the stage and clinical status of the patient
Rituximab 375 mg IV weekly x 4 weeks.
o Aggressive lymphomas
o Patients with diffuse large B cell lymphoma are treated with curative intent
o Most treated with six cycles of immunochemotherapy such as R-CHOP
(R) rituximab (Rituxan)
(C) cyclophosphamide
(H) doxorubicin hydrochloride
(O) vincristine (Oncovin, Vincasar PFS)
(P) prednisolone
• Prognosis
o Median survival of patients with indolent lymphomas is 10-15 years
• Hodgkin Lymphoma
• Clinical findings
o Bimodial age distribution peaking at age 20 and again at age 50
o Often seek medical care due to painless mass in neck
o Fever
o Weight loss
o Drenching night sweats
o Generalized pruritis
• Treatment
o Chemotherapy is the mainstay treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine
o Relapse after initial treatment is treatable with high dose chemotherapy and autologous hematopoietic stem cell transplantation
• Prognosis
o Cure rate is 75% with 0-2 risk factors and 55% with 3 or more risk factors including stage, age, gender, hemoglobin, albumin, white blood cell count, and lymphocyte count
• Transfusion
• Preparations
o Whole blood
o Packed red blood cells
o Leukocyte poor blood
o Autologous packed red blood cells
• Compatibility Testing
o A and B antigens are the most important
o In emergencies type O/ Rh negative blood can be given to anyone
• Hemolytic transfusion reaction
o Most severe reaction
o May last up to 5-10 days after transfusion
o Signs and symptoms
Fever, chills, backache and headache, dyspnea, hypotension and cardiovascular collapse. Patients under anesthesia will not manifest such symptoms and the 1st indication may be tachycardia, generalized bleeding or oliguria.
o Labs
Coagulation studies may reveal AKI or DIC
Delayed hemolytic reaction will have unexpected Hgb drop, increase in the total and direct bilirubin
o Treatment
Stop transfusion immediately.
Hydrate vigorously
Forced diuresis with mannitol may help prevent or minimize AKI
• Leukoaggutinin Reactions
o Occurs due to transfusion products relatively rich in leukocyte-rich plasma, especially platelets.
o Fever and chills within 12 hours. In severe cases cough and dyspnea.
o Acetaminophen, Benadryl, corticosteroids
• Hypersensitivity Reaction
o Urticaria or bronchospasm may develop during or soon after transfusion.
o These reactions are almost always due to exposure to allergic plasma proteins rather than leukocytes
o May require transfusion of washed or even frozen red blood cells to avoid future reactions
• Contaminated blood
o Blood products can be contaminated with bacteria, platelets being the most prone since they are unable to be refrigerated
o Recipient of blood product contaminated with gram negative bacteria often causes septic shock, acute DIC and AKI due to the transfused endotoxin and is often fatal.
o Blood from both recipient and blood bag need to be cultured and antibiotics started immediately
• Infectious disease transmission through transfusion
o Any blood can still transmit viral disease including Hep B & C, HIV, west nile virus and zika
• Transfusion graft vs host disease
o Allogenic passenger lymphocytes within transfused blood products will engraft in some recipients and mount an alloimmune attack against tissues expressing discrepant HLA antigens causing graft-versus-host disease (GVHD).
o Symptoms include fever, rash, diarrhea, hepatitis, lymphadenopathy, and severe pancytopenia.
o Normally fatal
• Transfusion related acute lung injury
o Occurs in 1 in every 5000 units transfused
o Clinically defined as noncardiac pulmonary edema after receiving blood.
o No specific treatment, just supportive care
• Platelet Transfusion
o A single donor should raise the platelet count by 50,000 to 60,000 per mcL
o Transfused platelets typically last for 2-3 days
• Transfusion of plasma components
o Fresh frozen plasma (FFP): used to correct coagulation factor deficiencies and to treat thrombotic thrombocytopenia purpura or hemolytic uremic syndrome. Also used to correct or prevent coagulopathy in trauma patients with a ratio of 1 FFP to every 2 PRBC
o Cryoprecipitate: made from FFP by cooling plasma to 4 degrees C and collecting the precipitate. 1 unit has a volume of approx. 250 mg of fibrinogen and between 80 to 100 units of factor VIII and von Wille-brand factor. Commonly used in DIC.
• Increased Platelet Destruction (ITP)
o Signs and Symptoms
Mucocutaneous bleeding may be present depending on platelet count.
Spontaneous bruising, nosebleeds, gingival bleeding or other types of hemorrhage generally do not occur until the platelet count has fallen below 10,000-20,000
o Labs
Isolated thrombocytopenia
Anemia if bleeding has occurred
Hep B & C and HIV infections should be excluded by serologic testing
Bone marrow biopsy in patients older than 60 or in those who do not respond to treatment
If there are clinical findings suggestive of lymphoproliferative malignancy, a CT should be done
o Treatment
Mainstay treatment of new onset primary ITP is short course of corticosteroids with or without IV immunoglobin (IVIG) or anti-D (WinRho)
Platelet transfusion if bleeding present
May add rituximab to corticosteroids to improve initial response rate
Chronic ITP treated with Romiplostim (subcu) weekly and eltrombopag (taken orally daily) are approved for those who have not responded to corticosteroids, IVIG or splenectomy.
Pregnancy related ITP goals include 10,000-30,000 in first trimester, greater than 30,000 in the 2nd and 3rd trimester and greater than 50,00 prior to ceseran or vaginal delivery. Moderate oral dose of prednisone or infusions of IVIG intermittent are standard.
• Heparin Induced Thrombocytopenia (HIT)
o Signs and symptoms
Generally asymptomatic
Bleeding does not generally occur
Thrombosis develops in 50% of patients, up to 30 days post op
o Labs
New onset thrombocytopenia detected within 5-14 days of exposure to heparin
A 50% decline is common from baseline count
o Treatment
Immediate d/c of heparin containing products
Doppler US to rule out DVT
Platelet transfusions should be avoided
A direct thrombin inhibitor such as argatroban or bivalirudin and should be continued until platelet count is greater than 100,000 and then initiate warfarin.
In all patients with HIT, some form of anticoagulation should be continued for at least 30 days and in patients who have thrombosis treatment for 3-6 months
• Disseminated Intravascular Coagulation (DIC)
o Signs and symptoms
Bleeding usually occurs at multiple sites including IV sites or incisions.
Malignancy related DIC may manifest principally as thrombosis.
o Labs
In early DIC, platelet counts, and fibrinogen levels may remain normal
There Is a progressive thrombocytopenia, prolongation of the prothrombin time, decrease in fibrinogen levels, and eventually elevation in the activated partial thromboplastin time
D-dimer levels typically are elevated
Laboratory abnormalities in the HELLP syndrome (hemolysis, elevated liver enzymes, low platelets) a severe form of DIC with a high mortality rate
o Treatment
The underlying causative disorder must be treated (eg. Antimicrobials, chemotherapy, surgery, or delivery of conceptus).
Blood transfusion for significant hemorrhage
FFP for prolonged APTT and PT.
Cryoprecipitate for fibrinogen less than 80-100
• Hemophilia A & B
o Symptoms and signs
Severe hemophilia presents in infant males or in early childhood with spontaneous bleeding into joints, soft tissues, or other locations.
Bleeding rare in mild hemophilia
Female carriers are asymptomatic
o Labs
Isolated reproductively low factor VIII or factor IX activity level, in the absence of other conditions
APTT may or may not be prolonged
o Treatment
Plasma derived or recombinant factor VIII or IX products are the mainstay of treatment
Severe hemophilia patients by age 4 are started on infusions of factor 2-3x weekly.
Those who are nonsevere are treated periprocedural prior to high risk bleeding activities such as sports
DDAVP for mild hemophilia either IV or intra-nasal PRN
• Factor Deficiency
• Rare clotting factor deficiencies are bleeding disorders in which one of the other clotting factors (i.e. factors I, II, V, V + VIII, VII, X, XI, or XIII)
• HIV
o Signs and Symptoms
Many asymptomatic approx. 10 years
Physical exam may be normal
Hairy leukoplakia tongue, Kaposi sarcoma, cutaneous bacillary angiomatiosis
o Labs
HIV enzyme-linked immunosorbent assay (ELISA)
Western blot (confirmatory test)
HIV rapid antibody
CBC
Absolute CD4 lymphocyte count
CD4 lymphocyte percentage
HIV viral load tests
o Differential DX
Cancer, chronic infection such as TB or endocarditis, hyperthyroidism
o Complications
Systemic complaints
• Weight loss, wasting syndrome, nausea
Pulmonary disease
• Pneumocystis pneumonia (treat with trimethoprim-sulfamethoxazole), community acquired pneumonia (most common), Kaposi sarcoma, non-Hodgkin lymphoma, lung cancer, sinusitis
Central nervous system disease
• Encephalopathy, meningitis, spinal cord processes, toxoplasmosis, central nervous system lymphoma, HIV associated dementia, cryptococcal meningitis, meningococcal meningitis, HIV myelopathy, progressive multifocal leukoencephalopathy
Peripheral nervous system
• Inflammatory polyneuropathies, sensory neuropathies, mononeuropathies
Rheumatologic and bone manifestations
• Arthritis, SLE, sicca syndrome, psoriatic arthritis, osteoporosis, osteopenia
Myopathy
• Proximal muscle weakness is common
Retinitis
• CMV retinitis : characterized by perivascular hemorrhages and white fluffy exudates
Oral lesions
• Oral candidias (caused from Epstein-barr virus), hairy leukopenia (white lesions on lateral aspect of tongue)
GI manifestations
• Candidal esophagitis, hepatic diease, biliary disease, enterocolitis, malabsorption, gastropathy
Endocrinology
• Hypogonadism (most common endocrine abnormality in men)
Skin manifestations
• Viral dermatitides (herpes simplex infection, herpes zoster, Molluscum contagiosum), bacterial dermatitides (staph infection, bacillary angiomatosis), Fungal rashes (candida, seborrheic dermatitis), neoplastic dermatitides, non-specific dermatitides (Xerosis, psoriasis)
HIV related malignances
• Kaposi sarcoma, non-hodgkin lymphoma, primary lymphoma of the brain, invasive cervical carcinoma.
Inflammatory responses
• Fever, sweats, and malaise
Gynecologic manifestations
• Vaginal candidiasis, cervical dysplasia and neoplasia, pelvic inflammatory diease
Coronary artery disease
• HIV infected persons are more at risk for CAD
o Treatment
Prophylaxis against: pneumocystis pneumonia, M avium complex, toxoplasmosis
Antiretroviral therapy (Table 31-7 Papadakis)
Adjunctive therapy: epoetin alfa for HIV related anemia
Integrase inhibitors
• Raltegravir, elvitegravir
Entry inhibitors
• Enfuvirtide, maraviroc
Protein inhibitors
• Indinavir, saquinavir, ritonavir, nelfinavir, amprenavir, fosamprenavir, lopinavir, atazanavir
Nonnucleotide reverse transcriptase inhibitors
• Efavirenz, rilpivirine, nevirapine, delavirdine, etravirine
Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs)
• Zidovudine, lamivudine, emtricitabine, emtricitabine, abacavir, tenfovir, didanosine, stavudine
o Prevention
HIV screening and counseling, decreasing transmission to others, postexposure prophylaxis for sexual and drug use exposure to HIV
o Monitoring ART
• Goals: evaluate toxicity and measure efficacy using objective markers to determine whether to maintain or change regimens. Should be done every 3-4 months
• Cancer Staging
The TNM Staging System
The TNM system is the most widely used cancer staging system. Most hospitals and medical centers use the TNM system as their main method for cancer reporting. You are likely to see your cancer described by this staging system in your pathology report, unless you have a cancer for which a different staging system is used. Examples of cancers with different staging systems include brain and spinal cord tumors and blood cancers.
In the TNM system:
• The T refers to the size and extent of the main tumor. The main tumor is usually called the primary tumor.
• The N refers to the number of nearby lymph nodes that have cancer.
• The M refers to whether the cancer has metastasized. This means that the cancer has spread from the primary tumor to other parts of the body.
o Once the TNM designations have been determined, an overall stage is assigned, stage I, II, III or IV.
• Lung Cancer
o Leading cause of cancer deaths in both men and women
o Cigarette smoking causes 85-90% of cases
o Signs and symptoms
Weight loss, asthenia, anorexia, cough or change in chronic cough, hemoptysis, chest pain, change in voice
o Labs
Examination of tissue or cytology specimen
Sputum cytology is highly specific but intensive; the yield is highest when there are lesions in the central airway
Thoracentesis can establish lung cancer in those with malignant pleural effusions
Fiberoptic bronchoscopy allows for visualization of the major airways, cytology brushings of visible lesions or lavage of specimens
o Imaging
Cxr or chest CT
o Special examinations
1. Staging: There are 2 essential principles for staging non-small cell lung cancer 1. The more extensive the disease the worse the prognosis 2. Surgical resection offers the best chance for cure. Small cell lung cnacer is divided into two categories. 1. Limited or 2. Extensive (when the tumor extends past the hemithorax)
All pts should have measurement of CBC, electrolytes, calcium, creatinine, liver tests, lactate dehydrogenase and albumin.
PET scan is an important modality for identifying metastatic foci. Disadvantages to a PET scan include false positive results due to sarcoidosis, TB or fungal infections. Also, not great tool for brain mets.
2. Pulmonary function testing: many pts with non-small cell lung ca have moderate to severe chronic severe lung disease that increases risk for perioperative complications as well as long term pulmonary insufficiency
Low risk pats have a FEV1 2L or more, high risk pts have postoperative FEV1 less than 700 ml
3. Screening: screening with low dose helical CT scans has been shown to improve mortality rates for lung cancer
o Treatment
Non-small cell
• Cure is unlikely without resection.
• Patients who are stage 1 who are not able to have resection due to comorbidity or other issues may be candidates for stereotactic body radiotherapy
• Neo adjuvant chemotherapy consists of giving antineoplastic drugs in advance to surgery or radiation therapy, more widely used in pts with stage IIIA or IIIB
• Adjuvant chemotherapy consists of administering antineoplastic drugs following surgery or radiation therapy.
Small cell
• Response rates to cisplatin and etoposide are excellent with 80-90% response in limited stage disease
• Remissions tend to be short lived of 6-8 months
• Once disease has reoccurred median survival is 3-4 months
o 5 histologic categories of lung cancer
Squamous cell carcinoma
Adenocarcinoma (most common)
Large cell
Small cell
Adenocarcinomas in situ
• Liver Cancer
o Symptoms and signs
Cachexia, weakness, weight loss, ascites
Tender enlargement of the liver occasionally with palpable mass
Auscultation may reveal a bruit over the tumor
o Labs
Leukocytosis, anemia, sudden and sustained elevation of the serum alkaline phosphatase, elevated alpha-fetoprotein
Cytology of ascitic fluid rarely shows malignant cells
o Imaging
Multiphasic helical CT and MRI with contrast
o Liver biopsy and staging
For lesions under 1 cm, US may be repeated every 3 months to watch for enlarging
For lesions over 1 cm biopsy can be deferred when characteristic arterial hypervascularity and delayed washout are demonstrated on either multiphasic helical CT or MRI with contrast
o Screening and prevention
Recommended in pts with Hep B or those with a family history of hepatocellular carcinoma, or cirrhosis caused by HCV, HBV or alcohol.
o Treatment
Surgical resection for those who have a solitary lesion and portal vein thrombosis is not present
Liver transplant
Chemotherapy, hormonal therapy with tamoxifen, and long-acting octreotide have not been shown to prolong life but trans arterial chemoembolization (TACE), TACE with drug eluting beads, trans arterial chemo infusion (TACI) and trans arterial radioembolization (TARE) via the hepatic artery are palliative and may prolong survival in pts with large or multifocal tumors
Radiofrequency ablation is superior to ethanol injection for tumors larger than 2 cm
Opioids for pain management
• Pancreatic Cancer
o Symptoms and signs
Pain located in the epigastric or left upper quad
Weight loss, depression, jaundice
o Labs
Anemia, glycosuria, hyperglycemia, and impaired glucose tolerance or true diabetes mellitus are found in 10-20% of cases.
Serum amylase or lipase level are occasionally elevated
Liver tests suggestive of obstructive jaundice
Occult blood in stool suggestive of carcinoma of ampulla of Vater
o Imaging
Multiphase thin-cut helical CT is generally the initial diagnostic procedure and detects a mass in 80% of cases.
MRI or CT
Ultrasound not reliable
MRCP or ERCP
o Staging
TNM classification is used
T1: limited to pancreas
T2: limited to pancreas but greater than 2 cm
T3: beyond pancreas without involvement of the celiac axis or superior mesenteric artery
T4: involve celiac axis or superior mesenteric artery
N1: regional lymph node metastasis
M1: distant metastasis
o Treatment
Surgical resection is choice
Metastatic disease may be controlled with long-acting somatostatin analogs, interferon, peptide-receptor radionuclide therapy and chemoembolization
Asymptomatic pancreatic cysts 2 cm or smaller are at low risk for harboring invasive carcinoma; the cysts may be monitored by MRI in 1 year and then every 2 years for 5 years
o Prognosis
Poor prognosis, 5-year survival rate
• Gastric Cancer
o Signs and symptoms
Generally asymptomatic until quite advanced
Dyspepsia, vague epigastric pain, anorexia, early satiety and weight loss
Ulcerating lesions can cause GI bleeding with hematemesis or melena
Pyloric obstruction causing postprandial vomiting
Physical exam is rarely useful
o Labs
Iron deficiency anemia due to chronic blood loss or anemia of chronic disease. Live test abnormalities, particularly elevation of alkaline phosphatase
o Endoscopy
Upper endoscopy should be obtained on all pts over age 55 years with new onset epigastric symptoms
Biopsy of suspicious lesions
o Imaging
Preoperative with CT of chest and abdomen (including pelvis in females) and EUS
EUS is superior to CT in determining depth of tumor penetration
PET for identifying mestastasis
o Screening
Screening for H pylori infection and treating is not recommended for asymptomatic adults
Screening is not recommended in the US
o Treatment
Curative surgical resection: only therapy with curative potential
Perioperative chemotherapy or chemoradiation: improved survival rates for those with localized or locoregional gastric adenocarcinoma who undergo surgical resection
Palliative modalities: surgery that is not curative but alleviate pain, bleeding or blockage
• Rectal Cancer
o Risk factors
Age: rises after age 45
Family history
IBD: ulcerative colitis and Crohns disease
Dietary and lifestyle: diets rich in fats and red meats increased risk. Low dose ASA associated with reduced risk of cancer
Other: higher rates in blacks than whites
o Symptoms and signs
Chronic blood loss from right sided colonic cancers
Change in bowel habits, abdominal pain, constipation, stool streaked with blood
o Labs
CBC, elevated liver enzymes, carcinoembryonic antigen (CEA) should be measured in all pts with proved colorectal cancer. A CEA level of greater than 5 preoperative is indicative for poor outcome
o Colonoscopy
Diagnostic procedure of choice
o Imaging
Chest, abdominal and pelvic CT scans with contrast are required for preoperative staging.
o Treatment
Surgery: resection of the primary colonic or rectal cancer is the treatment of choice
Systemic chemotherapy for colon cancer: chemotherapy has been demonstrated to improve overall and tumor free survival in select patients with colon cancer depending on stage
• Stage 1: excellent 5 year survival rate, no adjuvant therapy Is recommended
• Stage 2: higher risk for reoccurrence, may benefit from adjuvant chemotherapy
• Stage 3: treat 6 months post-operatively with a combo of oxaliplatin, 5-fluorouracil and leucovorin
• Stage 4: metastatic disease. Most do not have resectable (curable) disease. Without Tx the median survival rate is 12 months. Goal is to slow tumor progression.
• Prostate Cancer
o Symptoms and signs
Focal nodules or areas of induration within the prostate at the time of DRE
Most are found with elevated serum PSA
Urinary retention or neurologic symptoms from epidural metastases and cord compression
o Labs
Serum tumor markers: PSA
Misc: elevated BUN or creatinine
Prostate biopsy
o Imaging
Transrectal US
MRI
Radionucleotide bone scans
o Screening for prostate cancer
DRE, PSA, and transrectal US
o Treatment
Active surveillance
Radical prostatectomy
Radiation therapy
Cryosurgery
Locally and regionally advanced disease
Metastatic disease: androgen deprivation therapy
Ketoconazole: use in those with spinal cord involvement
Bisphosphates: prevent osteoporosis associated from androgen deprivation
Docetaxel: first cytotoxic chemotherapy agent to improve survival in pts with castration resistant prostate cancer
• Renal Cancer
o Symptoms and signs
Gross or microscopic hematuria, flank pain, abdominal mass, fever
o Labs
Hematuria, erythrocytosis, anemia, hypercalcemia
o Imaging
CT and MRI are the most valuable imaging tests
CXR to exclude metastasis
o Treatment
Surgical extirpation is primary treatment for localized carcinoma.
No effective chemotherapy is available for metastatic renal cell carcinoma
• CNS Cancer
o Symptoms and signs
Back pain at the level of the tumor that may be aggravated by lying down, sneezing, coughing
Progressive weakness, sensory changes, bowel and bladder symptoms
o Imaging
MRI is the initial imaging procedure of choice
PET scan
o Treatment
Corticosteroids immediately: dexamethasone 10-100 mg IV followed by 4-6 mg Q6H
Pts without a known history of cancer should have emergent surgery to relieve the impingement and obtain a pathologic specimen
Surgery followed by radiation
If multiple vertebra are involved, radiation is choice
[Show More]




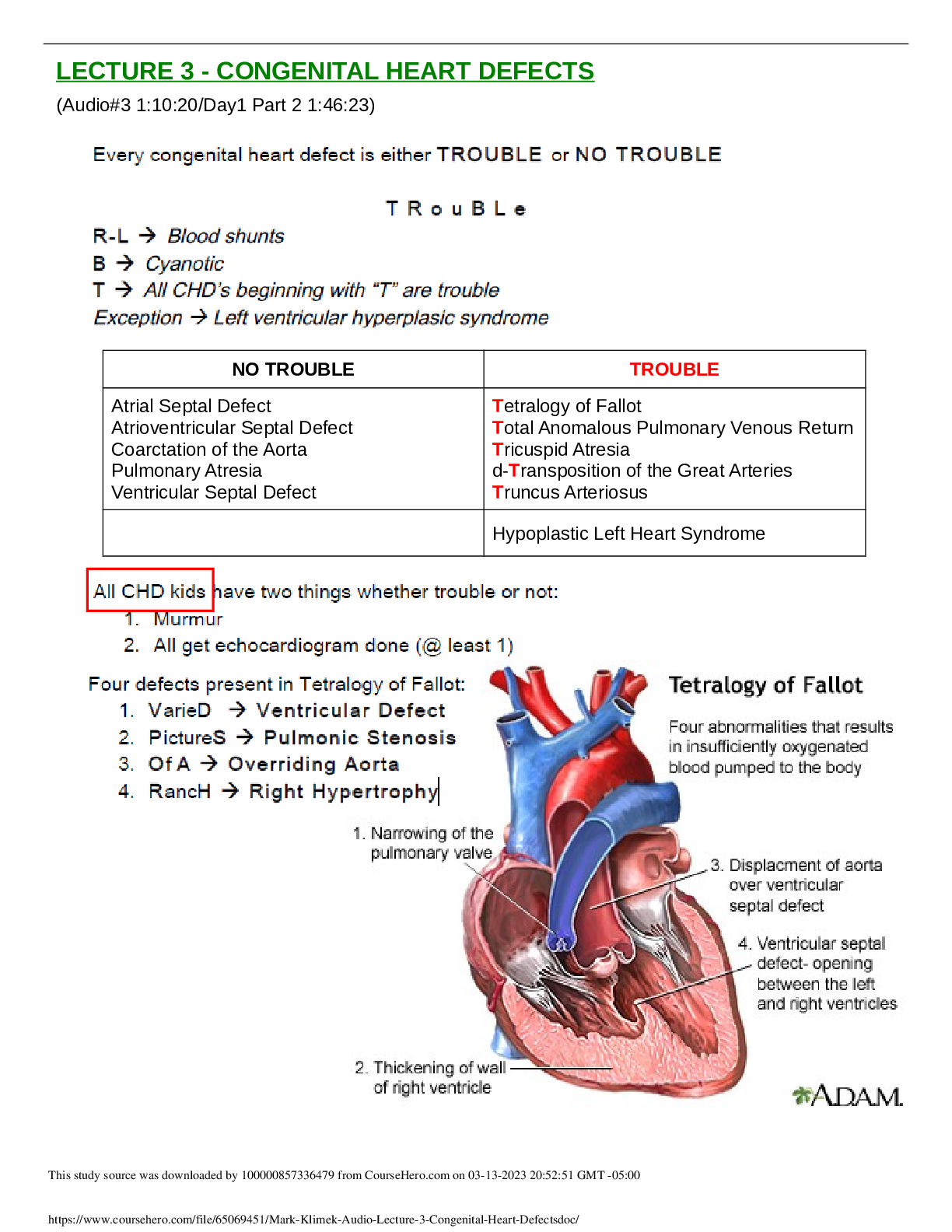




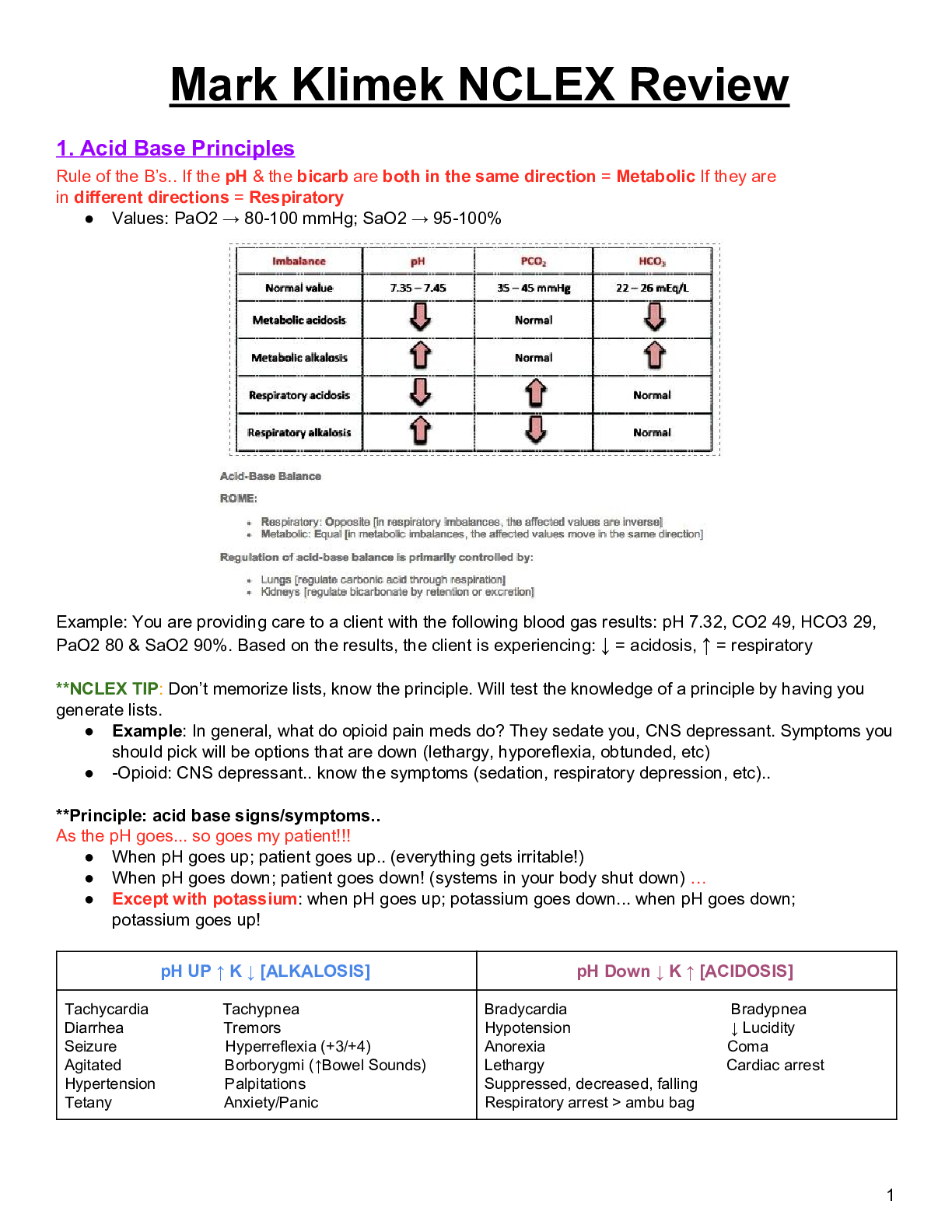
.png)
















