NURS 6550 Midterm Exam Review (Week 1-6)
Medicolegal Considerations and the Role of the Advanced Practice Nurse
• Coding and billing in nursing practice
o ICD-10, CPT, and E&M codes
• Role of the acute care nurse p
...
NURS 6550 Midterm Exam Review (Week 1-6)
Medicolegal Considerations and the Role of the Advanced Practice Nurse
• Coding and billing in nursing practice
o ICD-10, CPT, and E&M codes
• Role of the acute care nurse practitioner
o populations, limitations, common practice settings
• Certification exam content areas
• Informed consent
• HIPPA and patient confidentiality
• Radiology – appropriate orders and interpreting reports
• Evaluation, differential diagnosis, diagnostic studies, and treatment options for common symptoms
o Cough
o Dyspnea
o Hemoptysis
o Chest pain
o Palpitations
o Lower extremity edema
o Fever and hyperthermia
o Involuntary weight loss
o Fatigue
o Acute headache
o Dysuria
• Assessment of the older adult
• Evaluation, differential diagnosis, and treatment of geriatric disorders
o Dementia
Types, differentiating different types, treatment
o Delirium (how to differentiate between dementia and delirium)
Common causes, assessment, treatment
o Urinary incontinence
o Skin pressure injuries
• Care of patients at the end of life
o Symptom treatment / pain control
o Decision making
o DNR orders
• Pain Management
o Differentiate types of pain (acute, chronic, cancer)
o Classes of medications to treat pain (opioids, NSAIDS, adjuvant)
o Side effects and adverse effects of the medications
• Medications that treat neuropathic pain
o complications
Psychosocial Health Conditions
• Evaluation, differential diagnosis, and treatment of psychiatric disorders (review medication indications of treatment and medication complications)
o Trauma and stress related trauma disorders
o Anxiety disorders / panic attack
treatment
o Somatic symptom disorders
o Chronic pain
o Personality disorders
o Bipolar disorder
Long term treatment, monitoring, complications
o Schizophrenia
o Depression and mania (Initial treatment and common side effects to monitor for)
o Substance use disorders
Conditions of the Eye, Ear, Nose, and Throat
• Evaluation, differential diagnosis, and treatment of eye, ENT disorders
o Conjunctivitis
Differentiate between viral, bacterial, gonococcal
o Infectious keratitis
o Glaucoma
Acute vs chronic
Diagnosis – use tonometry
treatment
o Cataract
o Retinal detachment
o Macular degeneration
o Optic disc swelling
o Ocular trauma
o Corneal abrasion
o Orbital cellulitis
o Orbital trauma
o Hearing loss
Conductive vs sensorineural
o Otitis media
o Cholesteatoma
o Vertigo
Evaluation and treatment
o Sinusitis
o Nasal trauma / bleeding
Use of nasal packing
o Pharyngitis / peritonsillar abscess
o Epiglottitis
o Salivary gland disorders
o Bell’s palsy
• Procedures – review the indications, procedure, and patient instructions
o Eyebrow laceration repair
o Woods light evaluation of the eye
o Eyelid eversion
o Tooth avulsion and fracture
Cardiovascular Conditions
• Evaluation, differential diagnosis, treatment options, and complications
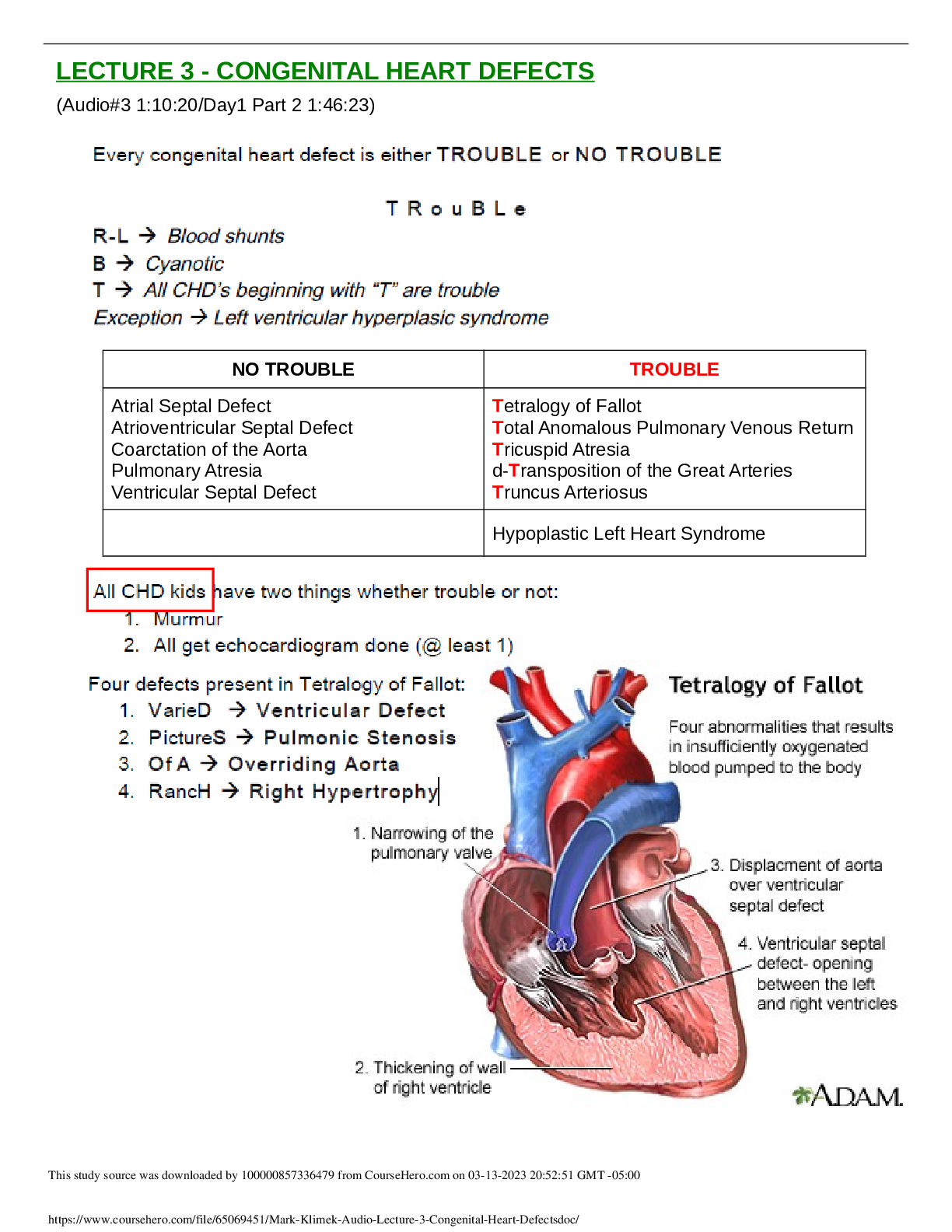
o Congenital heart disease
Pulmonary valve stenosis
Coarctation of the aorta
Atrial septal defect
Ventricular septal defect
Tetralogy of fallot
Patent ductus arteriosus
o Valvular heart disease (differentiate each of these from the others, diagnosis, treatment, murmurs location)
Mitral stenosis
Mitral regurgitation
Mitral valve prolapse
Aortic stenosis
Aortic regurgitation
Tricuspid stenosis
Tricuspid regurgitation
Pulmonary valve regurgitation
o Coronary artery disease
o Angina
o Coronary vasospasm (what drug class NOT to use for this dx)
o Acute Coronary syndromes (NSTEMI)
o Acute Myocardial infarction (STEMI)
Initial treatment
When is fibrinolytic therapy indicated
Contraindications to fibrinolytic therapy
o Arrythmias
Different classes of medications
Medication indications for specific rhythms
Be able to recognize arrythmias on 12 lead EKG – review book and simulator (http://www.skillstat.com/tools/ecg-simulator#/-home)
Bradycardia / tachycardia
Superventricular tachycardia
Atrial fibrillation
• Treatments including indication for anticoagulation
• Be familiar with the clinical practice guideline on anticoagulation management
Ventricular tachycardia / fibrillation
Syncope
o Heart failure
Differentiate systolic / diastolic failure
Review heart murmurs and their association with pathology
NY Heart rating scale
First line treatment
How treatment differs based on ejection fraction
o Myocarditis
o Cardiomyopathies
Differentiate between types
How assessment and treatment differs between types
o Pericarditis
12 lead EKG changes seen in pericarditis
Diagnostic criteria
treatment
o Endocarditis
Duke criteria
Common causes
Common symptoms
o Pericardial effusion / tamponade
o Pulmonary Hypertension
o Hypertension
Be very familiar with practice guideline JNC 9
Target BP by age
Treatment based on co-morbidities
Hypertensive urgency / emergency – diagnostic criteria
o Atherosclerotic peripheral vascular disease (symptoms)
Aortic and iliac occlusions
Femoral and popliteal occlusions
Tibial and pedal occusions
o Occlusive cerebrovascular disease
Diagnosis and treatment
o Abdominal aortic aneurysms
o Thoracic aortic aneurysms
Monitoring and treatment guidelines
o Peripheral artery aneurysms
o Aortic dissection
o Shock
How to differentiate between the types of shock
Be familiar with the shock guidelines via Surviving Sepsis
Hemodynamic readings related to each shock type
treatment
o Thrombophlebitis
o Venous insufficiency
Diagnosis and treatment
o Lipid disorders
Be familiar with the 2018 practice guideline on management of blood cholesterol
Be able to use the risk calculator
• Procedures
o Be able and familiar with EKG interpretation
o Use the simulator to practice
o Know the criteria for each arrhythmia, AV block, STEMI with associated location
o Defibrillation - indications and procedure
Respiratory System
• Evaluation, differential diagnosis, treatment options, and complications
o Asthma
Be familiar with the Global Initiative for Asthma, diagnostic criteria, step wise approach to treatment
Be familiar with the FEV monitoring and intervention
o COPD
GOLD classification and treatment recommendations
Indication for supplemental oxygen
Smoking cessation / stages of change
o Bronchiectasis
o Cystic fibrosis
o Bronchitis
o Pneumonia
Differentiate CAP, HAP, and VAP along with treatment changes
VAP prevention / risk factors
CURB-65 criteria
o Pulmonary tuberculosis
Monitoring, when to treat, how to treat, when to report
o Pulmonary neoplasms
o Interstitial lung disease
o Sarcoidosis
o Pulmonary Embolism
Treatment – be familiar with the CHEST guidelines for anticoagulation management (2016)
Diagnosis – effectiveness of D-dimer / what effects result
Congenital risk factors
o Pulmonary hypertension
o Smoke inhalation
o Aspiration syndromes
o Pleuritis
o Pleural effusion
Lab findings related to the pleural fluid
o Pneumothorax
o Obstructive sleep apnea
o Acute Respiratory Failure
Different types of respiratory support
Ventilator management / blood gases
o ARDS
Phases
Clinical symptoms
o Hypothermia
o Drowning
o Burns
o Altitude sickness
o Sepsis
Be familiar with the Surviving Sepsis guidelines
Diagnosis
Monitoring
Treatment
Differentiate SIRS/Sepsis/MODS
• Procedures
o Peak flow meter
o Pulmonary function tests
Be familiar with how to differentiate different disease
Determine baseline and disease progreassion
o Stress tests
o Chest xray interpretation
Review and be able to do some basic interpretation
Gastrointestinal System
• Evaluation, differential diagnosis, treatment options, and complications
o Dyspepsia
o Nausea / vomiting
o Constipation /diarrhea
o GI Bleeding
o Ascites
o Bacterial Peritonitis
o GERD
o Esophagitis
o Esophageal lesions
treatment
o Esophageal varices
o Achalasia
o Gastritis
o PUD
o Zollinger-Ellison Syndrome
o Celiac disease
o Acute paralytic ileus
o Appendicitis
o Irritable bowel syndrome
o Colitis
o Inflammatory bowel disease
o Crohns disease
o Ulcerative colitis
o Diverticulitis
o Jaundice
o Hepatitis
Differentiate between all types
Know the serologic testing
o Acute liver failure
o Alcoholic liver disease
o Non alcoholic fatty liver disease
o Cirrhosis
o Non cirrhotic portal hypertension
o Cholelithiasis
o Cholecystitis
o Choledocholithiasis
o Pancreatitis
o Protein energy malnutrition
o Obesity
o Anorexia
o Bulimia
o Vitamin deficiencies
o Enteral nutrition
When to use
o Parenteral nutrition
When to use
complications
• Procedures
o Abdominal xray interpretation
o Nasogastric tube insertion
[Show More]








.png)
















