NR 602 Week 3 iHuman SOAP
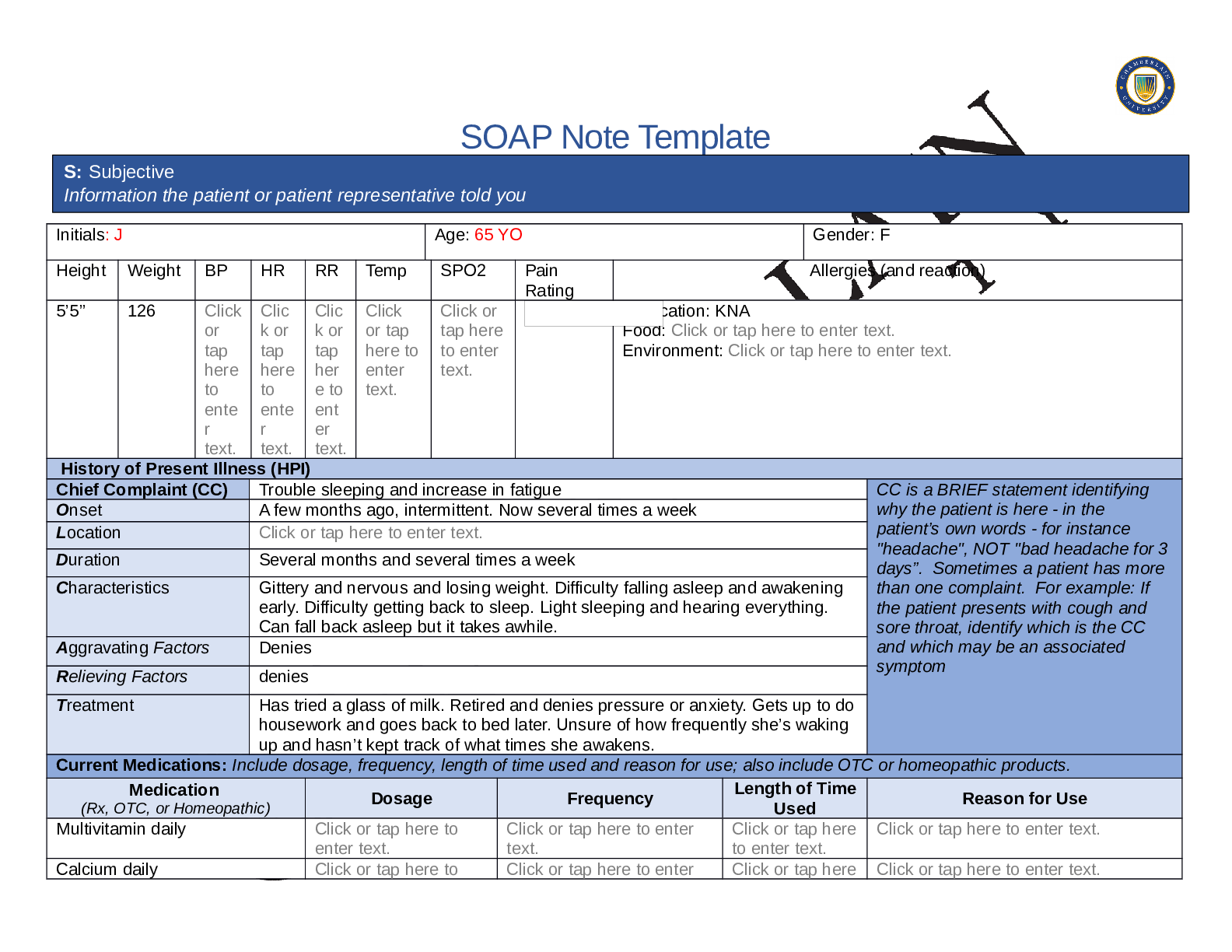
SOAP Note Template
Initials: J Age: 65 YO Gender: F
Height Weight BP HR RR Temp SPO2 Pain
Rating
Allergies (and reaction)
5’5” 126 Click
or
tap
here
to
ente
r
text.
Clic
k or
tap
...
NR 602 Week 3 iHuman SOAP
SOAP Note Template
Initials: J Age: 65 YO Gender: F
Height Weight BP HR RR Temp SPO2 Pain
Rating
Allergies (and reaction)
5’5” 126 Click
or
tap
here
to
ente
r
text.
Clic
k or
tap
here
to
ente
r
text.
Clic
k or
tap
her
e to
ent
er
text.
Click
or tap
here to
enter
text.
Click or
tap here
to enter
text.
Medication: KNA
Food: Click or tap here to enter text.
Environment: Click or tap here to enter text.
History of Present Illness (HPI)
Chief Complaint (CC) Trouble sleeping and increase in fatigue CC is a BRIEF statement identifying
why the patient is here - in the
patient’s own words - for instance
"headache", NOT "bad headache for 3
days”. Sometimes a patient has more
than one complaint. For example: If
the patient presents with cough and
sore throat, identify which is the CC
and which may be an associated
symptom
Onset A few months ago, intermittent. Now several times a week
Location Click or tap here to enter text.
Duration Several months and several times a week
Characteristics Gittery and nervous and losing weight. Difficulty falling asleep and awakening
early. Difficulty getting back to sleep. Light sleeping and hearing everything.
Can fall back asleep but it takes awhile.
Aggravating Factors Denies
Relieving Factors denies
Treatment Has tried a glass of milk. Retired and denies pressure or anxiety. Gets up to do
housework and goes back to bed later. Unsure of how frequently she’s waking
up and hasn’t kept track of what times she awakens.
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
(Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use
Multivitamin daily Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Calcium daily Click or tap here to Click or tap here to enter Click or tap here Click or tap here to enter text.
S: Subjective
Information the patient or patient representative told youenter text. text. to enter text.
Metamucil daily Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to
enter text.
Click or tap here to enter
text.
Click or tap here
to enter text.
Click or tap here to enter text.
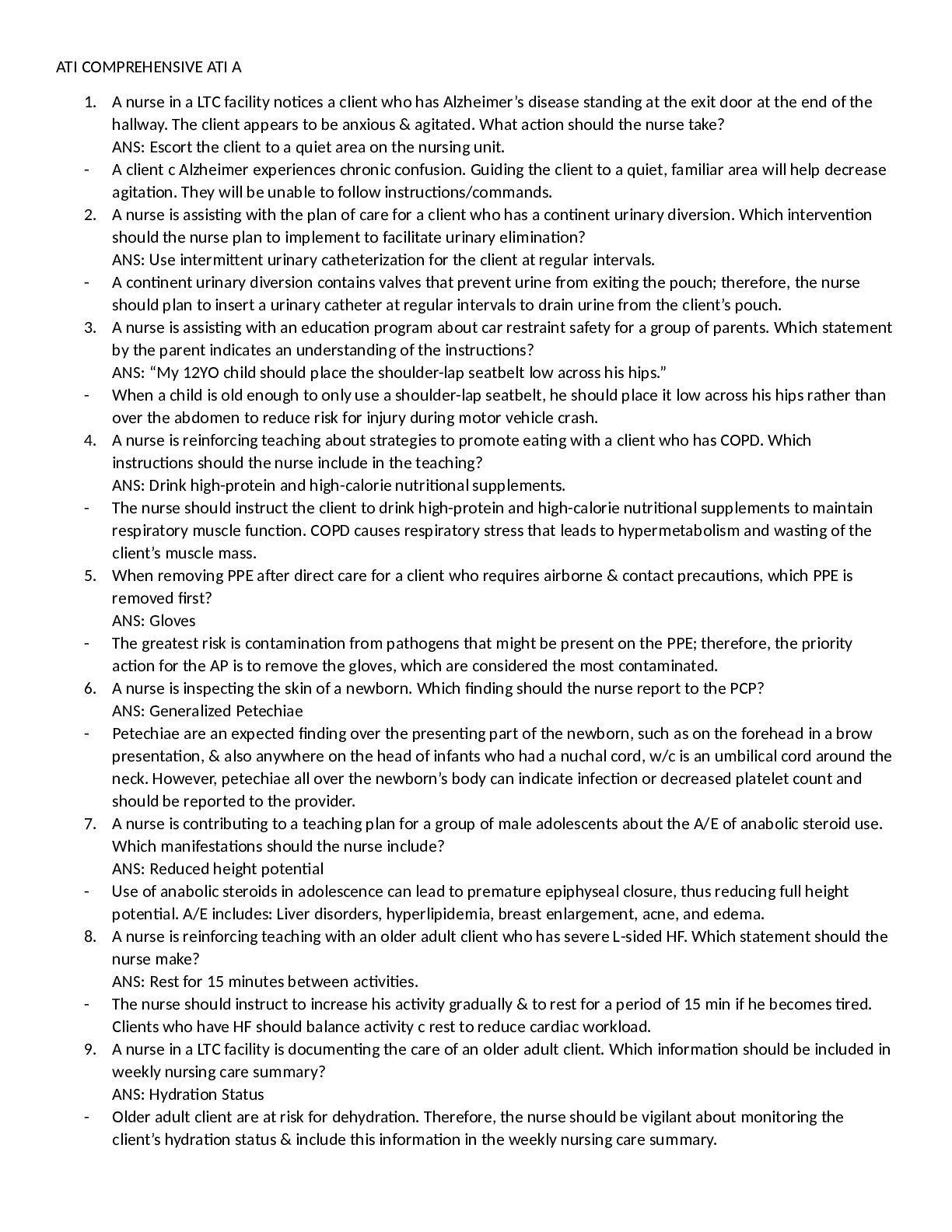
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
Denies current or past medical problems. Occasional headaches. Occasional GERD. Chronic constipation. Hospitalized during the birth of her two
children. Childhood illnesses: mumps, measles, rubella
Immunizations: tetanus within the last 10 years, varicella
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Mother of two children. Normal American Diet Exercises – plays tennis on weekends. Colonscopy at age 58 normal. Yearly mammograms all
negative with dense breast tissue. Non-smoker (smoked occasionally in college). Drinks alcohol socially (1-2x per month; goes out with girlfriends).
Denies recreational drug use. Married, monogamous, no history of STDS or herpes. Retired high school science teacher.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
Father: deceased at 90 from pneumonia, history of asthma and osteoarthritis
Mother: died in hit and run car accident at age 71.
Maternal grandmother: deceased and died of a stroke, history of being “nervous” and was told it was her thyroid
Maternal grandfather: died in war, no medical problems
Paternal grandmother: died of breast cancer
Paternal grandfather: died of prostate cancer
No siblingsReview of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive
symptom and provide additional details.
Constitutional
If patient denies all
symptoms for this system,
check here: ☐
Skin
If patient denies all
symptoms for this
system, check here: ☐
HEENT
If patient denies all symptoms for this system, check here: ☐
☒Fatigue Click or tap here
to enter text.
☐Weakness Click or tap
here to enter text.
☐Fever/Chills Click or tap
here to enter text.
☐Weight Gain denies
☒Weight Loss Click or tap
here to enter text.
☒Trouble Sleeping Click or
tap here to enter text.
☐Night Sweats denies
☐Other:
Click or tap here to enter
text.
☐Itching Click or tap
here to enter text.
☐Rashes Click or tap
here to enter text.
☒Nail Changes Click
or tap here to enter
text.
☐Skin Color Changes
Click or tap here to
enter text.
☒Other:
Hair thinning
☐Diplopia Click or tap
here to enter text.
☐Eye Pain Click or tap
here to enter text.
☐Eye redness Click or
tap here to enter text.
☐Vision changes Click or
tap here to enter text.
☐Photophobia Click or
tap here to enter text.
☐Eye discharge Click or
tap here to enter text.
☐Earache Click or tap here
to enter text.
☐Tinnitus Click or tap here
to enter text.
☐Epistaxis Click or tap
here to enter text.
☐Vertigo Click or tap here
to enter text.
☐Hearing Changes Click
or tap here to enter text.
☐Hoarseness Click or tap here
to enter text.
☐Oral Ulcers Click or tap here
to enter text.
☐Sore Throat Click or tap here
to enter text.
☐Congestion Click or tap here
to enter text.
☐Rhinorrhea Click or tap here
to enter text.
☐Other:
Click or tap here to enter text.
Respiratory
If patient denies all symptoms for this
system, check here: ☐
Neuro
If patient denies all symptoms
for this system, check here:
☐
Cardiac and Peripheral Vascular
If patient denies all symptoms for this system, check here: ☐
☐Cough Click or tap here to enter
text.
☐Syncope or
Lightheadedness Click or tap
☐Chest pain Click or tap here to enter
text.
☒Palpitations over the past
few years☐Hemoptysis Click or tap here to
enter text.
☐Dyspnea Click or tap here to enter
text.
☐Wheezing Click or tap here to enter
text.
☐Pain on Inspiration Click or tap here
to enter text.
☐Sputum Production
☐Other: Click or tap here to enter
text.
here to enter text.
☒Headache Click or tap here
to enter text.
☐Numbness Click or tap here
to enter text.
☐Tingling Click or tap here to
enter text.
☐Sensation Changes
☐Speech Deficits Click or tap
here to enter text.
☐Other: Click or tap here to
enter text.
☒SOB breathing harder and heart
beats faster with
☒Exercise Intolerance exhausted with
weekly tennis
☐Orthopnea Click or tap here to enter
text.
☐Edema Click or tap here to enter text.
☐Murmurs Click or tap here to enter
text.
☒Faintness struggles with
heat
☐Claudications Click or tap
here to enter text.
☐PND Click or tap here to
enter text.
☐Other: Click or tap here to
enter text.
MSK
If patient denies all symptoms for
this system, check here: ☒
GI
If patient denies all symptoms for this
system, check here: ☒
GU
If patient denies all symptoms
for this system, check here: ☒
PSYCH
If patient denies all symptoms
for this system, check here: ☐
☐Pain Click or tap here to enter
text.
☐Stiffness Click or tap here to
enter text.
☐Crepitus Click or tap here to enter
text.
☐Swelling Click or tap here to enter
text.
☐Limited ROM
☐Redness Click or tap here to
enter text.
☐Misalignment Click or tap here to
enter text.
☐Other: Click or tap here to enter
text.
☐Nausea/Vomiting Click or tap here to
enter text.
☐Dysphasia Click or tap here to enter
text.
☐Diarrhea Click or tap here to enter
text.
☐Appetite Change Click or tap here to
enter text.
☐Heartburn Click or tap here to enter
text.
☐Blood in Stool Click or tap here to
enter text.
☐Abdominal Pain Click or tap here to
enter text.
☐Excessive Flatus Click or tap here to
enter text.
☐Urgency Click or tap here to
enter text.
☐Dysuria Click or tap here to
enter text.
☐Burning Click or tap here to
enter text.
☐Hematuria Click or tap here
to enter text.
☐Polyuria Click or tap here to
enter text.
☐Nocturia Click or tap here to
enter text.
☐Incontinence Click or tap
here to enter text.
☐Other: Click or tap here to
enter text.
☐Stress Click or tap here to
enter text.
☐Anxiety Click or tap here to
enter text.
☐Depression Click or tap here
to enter text.
☐Suicidal/Homicidal Ideation
Click or tap here to enter text.
☐Memory Deficits Click or tap
here to enter text.
☐Mood Changes Click or tap
here to enter text.
☐Trouble Concentrating Click
or tap here to enter text.
☐Other: Click or tap here to
enter text.☐Food Intolerance Click or tap here to
enter text.
☐Rectal Bleeding Click or tap here to
enter text.
☐Other:
GYN
If patient denies all symptoms for this
system, check here: ☒
Hematology/Lymphatics
If patient denies all symptoms for this system,
check here: ☒
Endocrine
If patient denies all symptoms for this system,
check here: ☐
☐Rash Click or tap here to enter text.
☐Discharge Click or tap here to enter text.
☐Itching Click or tap here to enter text.
☐Irregular Menses Click or tap here to
enter text.
☐Dysmenorrhea Click or tap here to enter
text.
☐Foul Odor Click or tap here to enter text.
☐Amenorrhea Click or tap here to enter
text.
☐LMP: Click or tap here to enter text.
☐Contraception Click or tap here to enter
text.
☐Other:Click or tap here to enter text.
☐Anemia Click or tap here to enter text.
☐ Easy bruising/bleeding Click or tap here to
enter text.
☐ Past Transfusions Click or tap here to enter
text.
☐ Enlarged/Tender lymph node(s) Click or tap
here to enter text.
☐ Blood or lymph disorder Click or tap here to
enter text.
☐ Other Click or tap here to enter text.
☐ Abnormal growth Click or tap here to enter
text.
☐ Increased appetite Click or tap here to enter
text.
☐ Increased thirst denies
☐ Thyroid disorder Click or tap here to enter text.
☐ Heat/cold intolerance heat intolerant
☐ Excessive sweating Click or tap here to enter
text.
☐ Diabetes Click or tap here to enter text.
☐ Other Click or tap here to enter text.O: Objective
Information gathered during the physical examination by inspection, palpation, auscultation, and percussion. If unable to assess a
body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. Pertinent positive are the
“abnormal” findings and pertinent “negative” are the expected normal findings. Separate the assessment findings accordingly and be
detailed.Body System Positive Findings Negative Findings
General
Pleasant 65-year-old female appropriately dressed and appropriate
responses to questions
Click or tap here to enter text.
Skin
Warm and dry. Palms moist. No obvious skin lesions seen. Normal
skin turgor. Hair is dry but typical for age. Normal thickness and
distribution pattern for patient gender. Eyebrows: sparse; missing
lateral aspect. No swelling of extremities or deformities. No
cyanosis, clubbing or edema.
Click or tap here to enter text.
HEENT
Eyes: no erythema or swelling; positive for lid retraction and mild lid
lag; no proptosis. Conjunctivae: pink, no discharge. Sclerae:
anicteric. Orbital area: no edema, redness, tenderness or lesions
noted. Lateral outside third of eyebrow is missing bilaterally. Neck
has no visible scars, deformities or other lesions and trachea is
midline. Thyroid is soft, 45gm in size. Isthmus ropey, easily
palpable, slight bilateral asymmetry R>L, no nodules palpated.
Thyroid moves with swallowing and no nodules are felt.
Click or tap here to enter text.
Respiratory
Chest is symmetrical and the anterior-posterior diameter is normal.
The excursion with respiration is symmetrical and there are no
abnormal retractions or use of accessory muscles. No distention,
scars, masses or rashes.
Click or tap here to enter text.
Neuro
No fasiculations. Slightly coarse tremor in extended hand.
Hyperreflexia of biceps and brachioradialis tendons.
Click or tap here to enter text.
Cardiovascular
PMI is in the 5th intercostal space at the mid-clavicular line. RRR. Click or tap here to enter text.
Musculoskeletal
Normal muscle bulk and tone. Click or tap here to enter text.
Gastrointestinal
Abdomen is flat and symmetric with no scars, deformities, striae or
lesions. Hyperactive bowel sounds.
Click or tap here to enter text.Problem List
1. Click or tap here to enter text. 6. Click or tap here to enter text. 11. Click or tap here to enter text.
2. Click or tap here to enter text. 7. Click or tap here to enter text. 12. Click or tap here to enter text.
3. Click or tap here to enter text. 8. Click or tap here to enter text. 13. Click or tap here to enter text.
4. Click or tap here to enter text. 9. Click or tap here to enter text. 14. Click or tap here to enter text.
5. Click or tap here to enter text. 10. Click or tap here to enter text. 15. Click or tap here to enter text.
Diagnosis ICD-10 Code Pertinent Findings
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
A: Assessment
Medical Diagnoses. Provide 3 differential diagnoses (DDx) which may provide an etiology for the CC. The first diagnosis
(presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each
diagnosis.Diagnostics: List tests you will order this visit
Test Rationale/Citation
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text.
Medications: List medications/treatments including OTC drugs you will order and “continue meds” if pertinent.
Drug Dosage Length of Treatment Rationale/Citation
P: Plan
Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write
“None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for
each intervention.Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.
Referral/Consults:
Click or tap here to enter text. Rationale/Citation Click or tap here to enter text.
Education:
Click or tap here to enter text. Rationale/Citation Click or tap here to enter text.
Follow Up: Indicate when patient should return to clinic and provide detailed symptomatology indicating if the patient should return sooner than
[Show More]