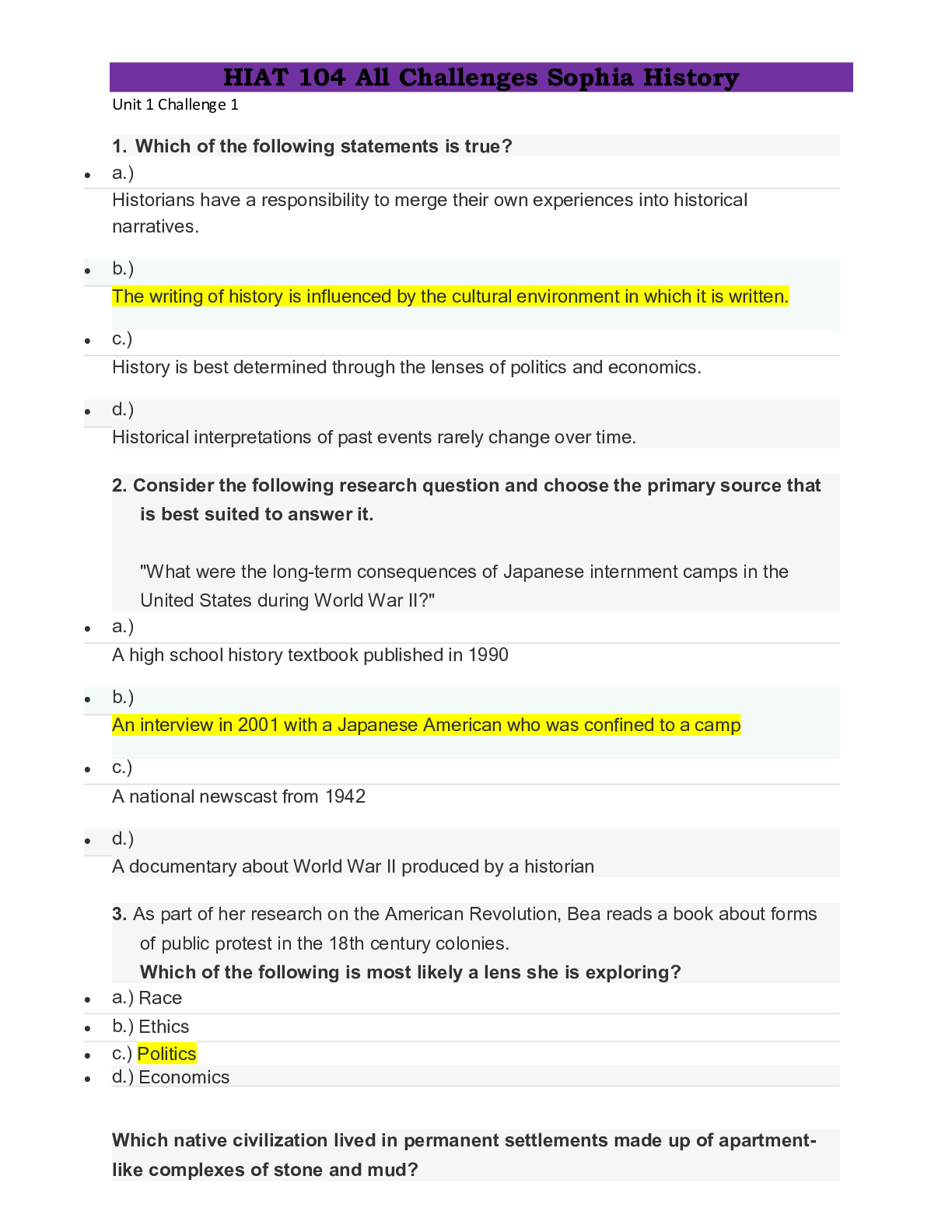
*NURSING > CASE STUDY > Airway/Breathing (Oxygenation) Pneumonia/Chronic Obstructive Pulmonary Disease Clinical Reasoning Ca (All)
Airway/Breathing (Oxygenation) Pneumonia/Chronic Obstructive Pulmonary Disease Clinical Reasoning Case Study
Document Content and Description Below
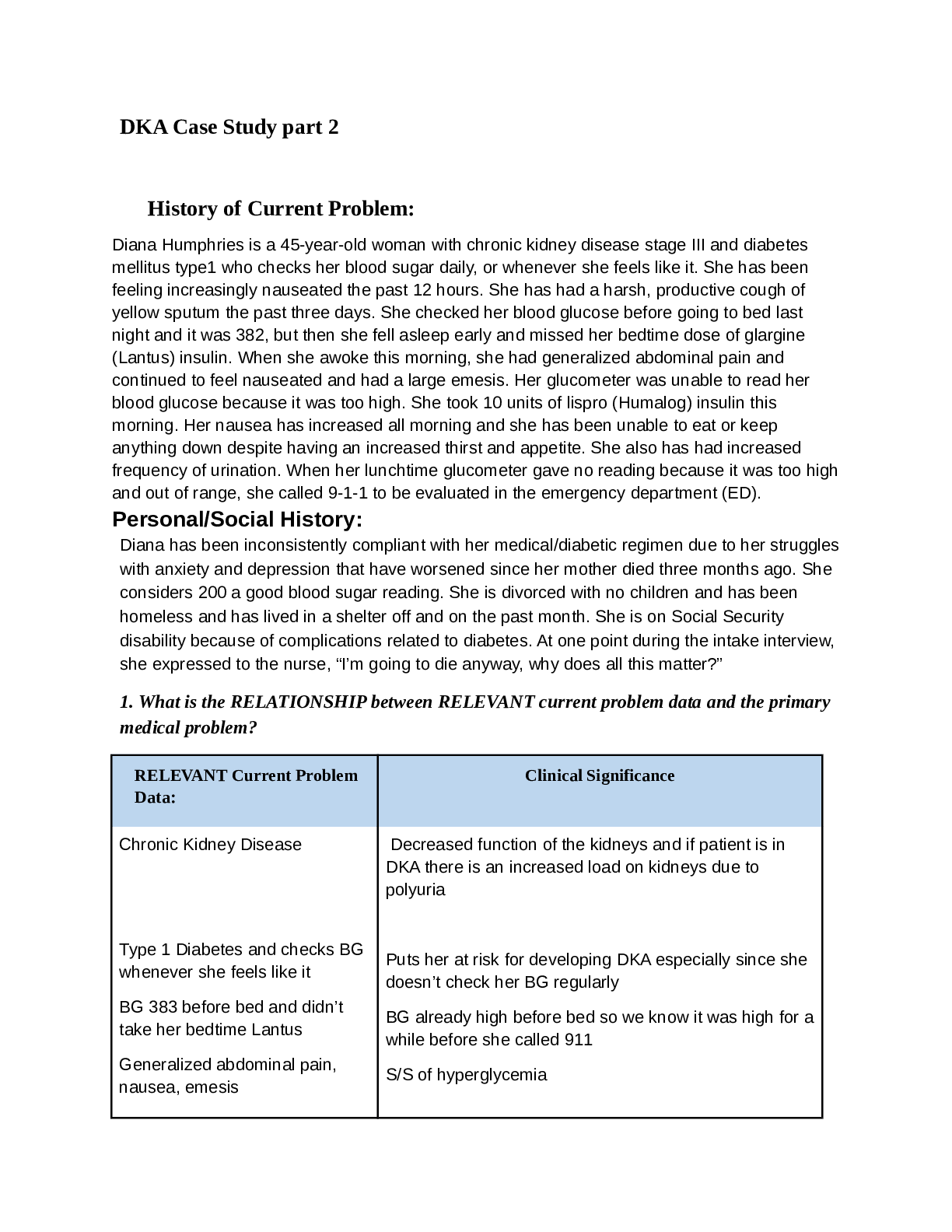
Airway/Breathing (Oxygenation) Pneumonia/Chronic Obstructive Pulmonary Disease Clinical Reasoning Case Study Airway/Breathing (Oxygenation) Pneumonia/Chronic Obstructive Pulmonary Disease Clinical R ... easoning Case Study STUDENT Worksheet JoAnn Walker, 84 years old Overview This case study incorporates a common presentation seen by the nurse in clinical practice: community acquired pneumonia with a history of COPD causing an acute exacerbation. Principles of spiritual care are also naturally situated in this scenario to provide rich discussion of “how to” practically incorporate this into the nurse’s practice. Concepts (in order of emphasis) I. Gas Exchange II. Infection III. Acid-Base Balance IV. Thermoregulation V. Clinical Judgment VI. Pain VII. Patient Education VIII. Communication IX. Collaboration I. Data Collection History of Present Problem: Pneumonia-COPDJoAnn Walker is an 84-year-old female who has had a productive cough of green phlegm 4 days ago that continues to persist. She was started 3 days ago on prednisone 60 mg po daily and azithromycin (Zithromax) 250 mg po x5 days by her clinic physician. Though she has had intermittent chills, she first noticed a fever last night of 102.0. She has had more difficulty breathing during the night and has been using her albuterol inhaler every 1-2 hours with no improvement. Therefore she called 9-1-1 and arrives at the emergency department (ED) by emergency medical services (EMS) where you are the nurse who will be responsible for her care. Personal/Social History: JoAnn was widowed 6 months ago after 64 years of marriage and resides in assisted living. She is a retired elementary school teacher. She called her pastor and he has now arrived and came back with the patient. The nurse walked in the room when the pastor asked Joan if she would like to pray. The patient said, “Yes, this may the beginning of the end for me.” What data from the histories is important & RELEVANT; therefore it has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: Fever, difficulty breathing, no improvement with the inhaler, productive cough of green phlegm. This is important because we need to look at the relevant data and realize that she seems to be in distress and first take care of that. Also realize that she seems to have an infection. With this information we are able to prioritize RELEVANT Data from Social History: Clinical Significance: She was widowed 6 months ago after being married for 64 years, and she feels like it is the beginning of the end for her. This is important because when caring for her we need to keep in mind her age, stressors in her life and any limitations What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect) PMH: Home Meds: Pharm. Classification: Expected Outcome: COPD/asthma Hypertension Hyperlipidemia Cor-pulmonale Anxiety disorder 1ppd smoker x40 years. Quit 10 years ago 1. Fluticasone/salmeterol (Advair) diskus 1 puff every 12 hours 2. Albuterol (Ventolin) MDI 2 puffs every 4 hours prn 3. Lisinopril (Prinivil) 10 mg po daily 4. Gemfribrozil (Lopid) 600 mg po bid 5. Diazepam (Valium) 2.5 mg po every 6 hours as needed 6. Triamterene-HCTZ (Dyazide) 1 tab daily 1. corticosteroid 2. bronchodilator 3. ACE inhibitor 4. cholesterol 5. benzodiazepine 6. potassium sparing diuretic 1. improve breathing 2. open up airway in the lungs 3. decrease blood pressure and open up blood vessels 4. decrease fatty acids 5. decrease anxiety and calm down 6. help body from not absorbing too much salt and keep potassium level from getting too low. One disease process often influences the development of other illnesses. Based on your knowledge of pathophysiology, (if applicable), which disease likely developed FIRST that then initiated a “domino effect” in their life? Circle what PMH problem likely started FIRST Underline what PMH problem(s) FOLLOWED as domino(s) II. Patient Care Begins:Current VS: WILDA Pain Scale (5th VS): T: 103.2 (oral) Words: Ache P: 110 (regular) Intensity: 3/10 R: 30 (labored) Location: Generalized over right side of chest with no radiation BP: 178/96 Duration: Intermittent-lasting a few seconds O2 sat: 86% 6 liters n/c Aggreviate: Alleviate: Deep breath Shallow breathing What VS data is RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT VS Data: Clinical Significance: Temperature, pulse, respirations, blood pressure, O2 sat, location of pain, and what aggravates and alleviates pain. The temperature is high which signifies infection. Pulse is also high which could be due to infection, fever or anxiety. Respriations are very high and O2 is very low this is a main concern, she is not getting enough oxygen into her system and can become hypoxic and go into resp acidocis. Blood pressure is elevated and she has a history of elevated BP and heart failure so it needs to be monitored. Patient is in pain and seem to be related to her lungs. Current Assessment: GENERAL APPEARANCE: Appears anxious and in distress RESP: Dyspnea with intercostal retractions, breath sounds very diminished bilaterally with scattered expiratory wheezing CARDIAC: Pale, hot & dry, no edema, heart sounds regular-S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert & oriented to person, place, time, and situation (x4) GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants GU: Voiding without difficulty, urine clear/yellow SKIN: Skin integrity intact What assessment data is RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT Assessment Data: Clinical Significance: General appearance, respiratory, and cardiac Her general appereance is important because we can see that she is having difficulty breathing and is anxious. Her respiratory assessment is important because again we can see that she is in distress and having a possible asthma exacerbation. Also by listening we can hear that she has some fluid on her lungs With her cardiac assessment we can see that she has a fever12 Lead EKG: Interpretation: Sinus tachycardia Clinical Significance: Tachycardia can be due to many possible explanations such as infection, anxiety or fever. All of which are all very likely for this patient. III. Clinical Reasoning Begins… 1. What is the primary problem that your patient is most likely presenting with? Pneumonia with COPD exacerbation and possible sepsis 2. What is the underlying cause/pathophysiology of this problem? Pneumonia is an infection in which the lungs contain fluid or piss caused by many different things such as bacteria, fungi, parasites and more. 3. What nursing priority(s) will guide your plan of care? (if more than one-list in order of PRIORITY) Breathing, O2, BP, HR, temperature4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome: Increase oxygen (8-10 L on mask or nonrebreather). Place on a cooling blanket. Inform doctor of BP. 6L was not enough because he sat was only 86%. To decrease the temperature without having to give too much medication for it. To see if they want to give any medication for it. Increase O2 to at least 90%. decrease her temperature. decrease her BP. 5. What body system(s) will you most thoroughly assess based on the primary/priority concern? Respiratory 6. What is the worst possible/most likely complication to anticipate? Sepsis or pneumothorax 7. What nursing assessment(s) will you need to initiate to identify this complication if it develops? Sepsis- Temp, HR, BP, lactic acid. Pneumothorax-SOB, CP 8. What nursing interventions will you initiate if this complication develops? Sepsis- follow hospital procedure. Pneumothorax- call DR and prepare to insert a chest tube. (this is emergent) Medical Management: Rationale for Treatment & Expected Outcomes Care Provider Orders: Rationale: Expected Outcome: albuterol-ipratropium (Combivent) 2.5 mg neb Establish peripheral IV Lorazepam (Ativan) 1 mg IV push Methylprednisolone (Solumedrol) 125 mg IV push Levofloxacin (Levaquin) 750 mg IVPB (after blood cultures drawn) Acetaminophen (Tylenol) 1000mg oral Chest x-ray (CXR) Complete cell count (CBC) Basic metabolic panel Bronchodilator. Access for medications. Help with anxiety. Decrease bronchoconstriction. Antibiotic. Decrease temperature. Check the lungs to see what is going on. Help detect if there is an infection going on. Look at the electrolytes, BUN, Creat, glucose, etc. Open up airway to increase O2. Have IV access Decrease anxiety Increase oxygen going to lungs. Decrease WBC and temp Decrease temp Pleural effusion Increase in WBC, RBC and lactate Increase in glucose(BMP) Lactate Arterial blood gas (ABG) Sputum culture with gram stain Blood culture x2 sites Urine analysis (UA) Urine culture (UC) PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: 1. Albuterol-ipratropium (Combivent) 2.5 mg neb 2. Establish peripheral IV 3. Lorazepam (Ativan) 1 mg IV push 4. Methylprednisolone (Solumedrol) 125 mg IV push 5. Levofloxacin (Levaquin) 750 mg IVPB (after blood cultures drawn) 6. Acetaminophen (Tylenol) 1000mg oral 1. 1 2. 2 3. 3 4. 4 5. 5 6. 6 1. airway first r/t ABC’s 2. have access for medications 3. to help calm down and breathe easier 4. breathing is always one of the top priorities 5. start broad spectrum antibiotics to get in the system and help fight infection. 6. won’t act as fast so you can do last. Medication Dosage Calculation: Medication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: lorazepam (Ativan) 1 mg IV push Normal Range: Average Depress CNS by GABA IV Push: Volume every 15 sec? 2-5 minutes Fall risk, possible addiction, monitor respirations. Medication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: methylprednisolone (Solumedrol) 125 mg IV push Normal Range: high Corticosteroid decreases inflammation of the bronchial IV Push: Volume every 15 sec? None Adrenal insufficient, monitor I&O, weight patient daily. Possible sepsis Tell you if there is pneumonia Tell you if the infection is in the blood Check the urine for cells, protein, sugar or blood See if the infection is a UTI Increase in lactate Decrease ph, co2, respiratory acidosis. Positive Positive Negative NegativeMedication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: levofloxacin (Levaquin) 750 mg IVPB Normal Range: average Broad spectrum antibiotic 150 mL over 90 minutes Hourly rate on pump: 100ml/hr Photo toxicity, muscle weakness, and hepatic toxic. Radiology Reports: What diagnostic results are RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT Results: Clinical Significance: Left lower lobe infiltrate. Hypoventilation present in both lung fields Buildup of fluid, bacterial infection. Hypoventilation- COPD Lab Results: What lab results are RELEVANT that must be recognized as clinically significant to the nurse? Complete Blood Count (CBC:) Current: High/Low/WNL? Most Recent: WBC (4.5-11.0 mm 3) 14.5 High 8.2 Hgb (12-16 g/dL) 13.3 WNL 12.8 Platelets(150-450x 103/µl) 217 WNL 298 Neutrophil % (42-72) 92 High 75 Band forms (3-5%) 5 WNL 1 What lab results are RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: WBC Neutrophil Band forms Infection WBC increasing Neutrophil increasing Band forms improving Basic Metabolic Panel (BMP:) Current: High/Low/WNL? Most Recent: Sodium (135-145 mEq/L) 138 WNL 142 Potassium (3.5-5.0 mEq/L) 3.9 WNL 3.8 Chloride (95-105 mEq/L) 98 WNL 96 CO2 (Bicarb) (21-31 mmol/L) 35 High 31 Anion Gap (AG) (7-16 mEq/l) 15 WNL 16 Glucose (70-110 mg/dL) 112 High 102 Calcium (8.4-10.2 mg/dL) 8.9 WNL 9.7 BUN (7 - 25 mg/dl) 32 High 28 Creatinine (0.6-1.2 mg/dL) 1.2 WNL 1.0 Misc. Labs: Current High/Low/WNL? Most Recent Lactate (0.5-2.2 mmol/L) 3.2 HighRELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Bicarb Glucose BUN Lactate COPD Prednisone Renal Sepsis Increasing Increasing Increasing N/A Arterial Blood Gas: Current: High/Low/WNL? pH (7.35-7.45) 7.25 Low pCO2 (35-45) 68 High pO2 (80-100) 52 Low HCO3 (18-26) 36 High O2 sat (>92%) 84% low RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: All of them Partially compensated respiratory acidosis N/A Urine Analysis (UA:) Current: High/Low/WNL? Color (yellow) Yellow WNL Clarity (clear) Clear WNL Specific Gravity (1.015-1.030) 1.015 WNL Protein (neg) Neg WNL Glucose (neg) Neg WNL Ketones (neg) Neg WNL Bilirubin (neg) Neg WNL Blood (neg) Neg WNL Nitrite (neg) Neg WNL LET (Leukocyte Esterase) (neg) Neg WNL MICRO: RBC’s (<5) 1 WNL WBC’s (<5) 3 WNL Bacteria (neg) Few High Epithelial (neg) Few high RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Bacteria Epithelial They are OK since it is few N/ALab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal value: Why Relevant? Nursing Assessments/Interventions Required: Lactate Value: 3.2 0.5- 2.2 Critical Value: Over 2.2 Indicated hypoxia which leads to spesis Hospital sepsis protocol, monitor temp, HR, and BP IV. Evaluation: One hour later… You have been able to implement all orders and it has been 30 minutes since the nebulizer treatment. Your collect the following clinical reassessment data: Current VS: Most Recent: T: 100.8 (oral) T: 103.2 (oral) P: 88 (regular) P: 110 (regular) R: 24 (slight labored) R: 30 (labored) BP: 128/90 BP: 178/96 O2 sat: 92% 4 liters n/c O2 sat: 86% 6 liters n/c Current Assessment: GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds improved aeration bilaterally, coarse crackles with diminished aeration in left lower lobe (LLL) CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert & oriented to person, place, time, and situation (x4) GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants GU: Voiding without difficulty, urine clear/yellow SKIN: Skin integrity intact 1. What clinical data is RELEVANT that must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: VS are fine and improving There is improvement, I would still continue to monitor vital signs RELEVANT Assessment Data: Clinical Significance: Slight labored breathing and crackles There is improvement in the patients condition, I would continue treatment, see how she does with weaning of O2You report your assessment findings to the primary care provider who decides to repeat the ABG. You obtain the following results: Arterial Blood Gas: Current: Most Recent: pH (7.35-7.45) 7.31 7.25 pCO2 (35-45) 55 68 pO2 (80-100) 78 52 HCO3 (18-26) 35 36 O2 sat (>92%) 91% 84% 2. Has the status improved or not as expected to this point? Improved 3. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? Yes 4. Based on your current evaluation, what are your nursing priorities and plan of care? More specific antibiotics, have patient use an incentive spirometer. It is now time to transfer your patient to the floor. Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the nurse who will be caring for this patient: Situation: 84 year old female who has possible pneumonia with COPD exacerbation and possible sepsis Background: COPD, asthma, HTN, heart failure, anxiety Assessment: GENERALAPPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds improved aeration bilaterally, coarse crackles with diminished aeration in left lower lobe (LLL) CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert & oriented to person, place, time, and situation (x4) GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants GU: Voiding without difficulty, urine clear/yellow SKIN: Skin integrity intact Recommendation: Continue treatment plan, monitor vitals, and schedule PT.V. Education Priorities/Discharge Planning 1. What will be the most important discharge/education priorities you will reinforce with their medical condition to prevent future readmission with the same problem? Get up and moving, wash hands, coughing etiquette 2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient? [Show More]
Last updated: 3 years ago
Preview 1 out of 11 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
11
Written in
All
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
95