NURS 301 - Health Assessment Exam 1 Review.
Document Content and Description Below
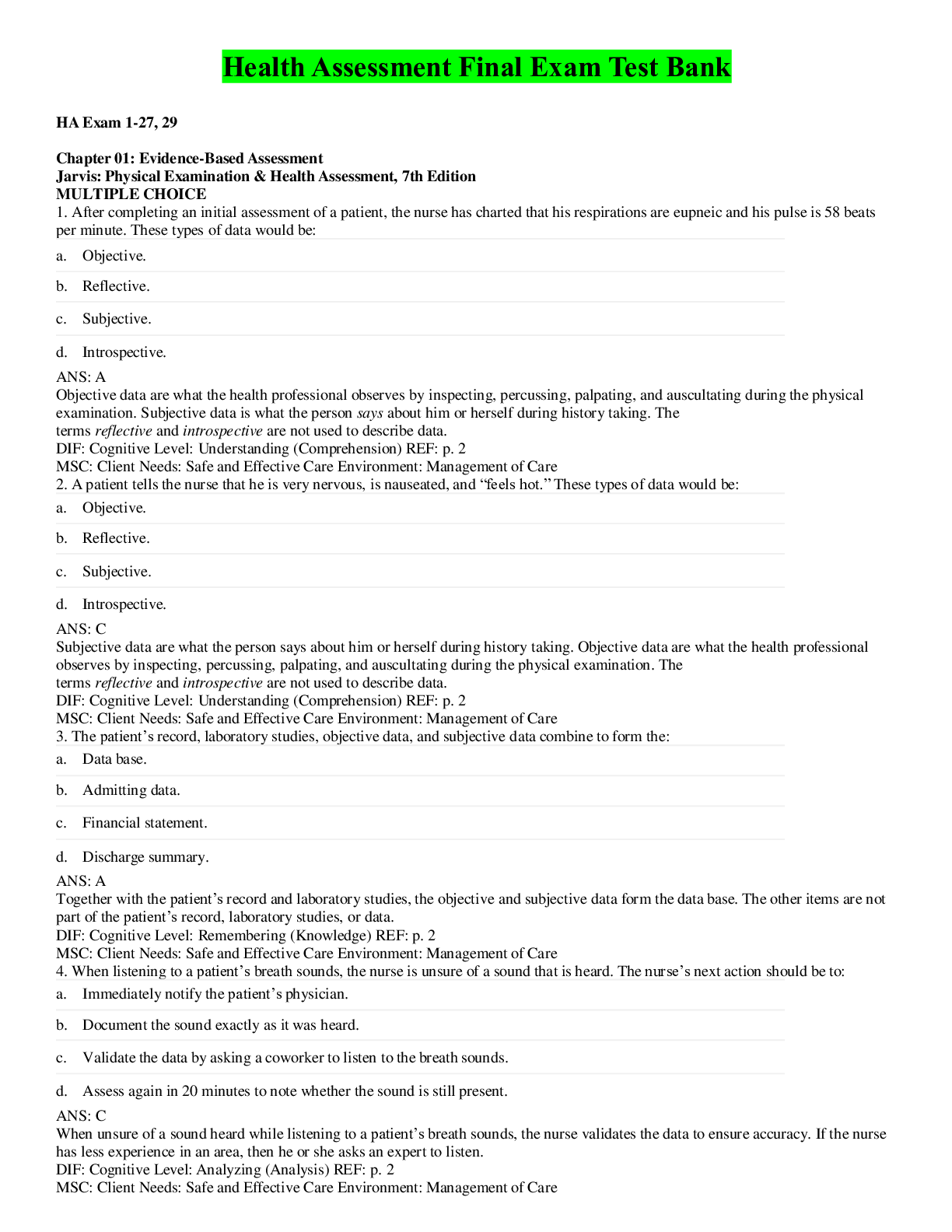
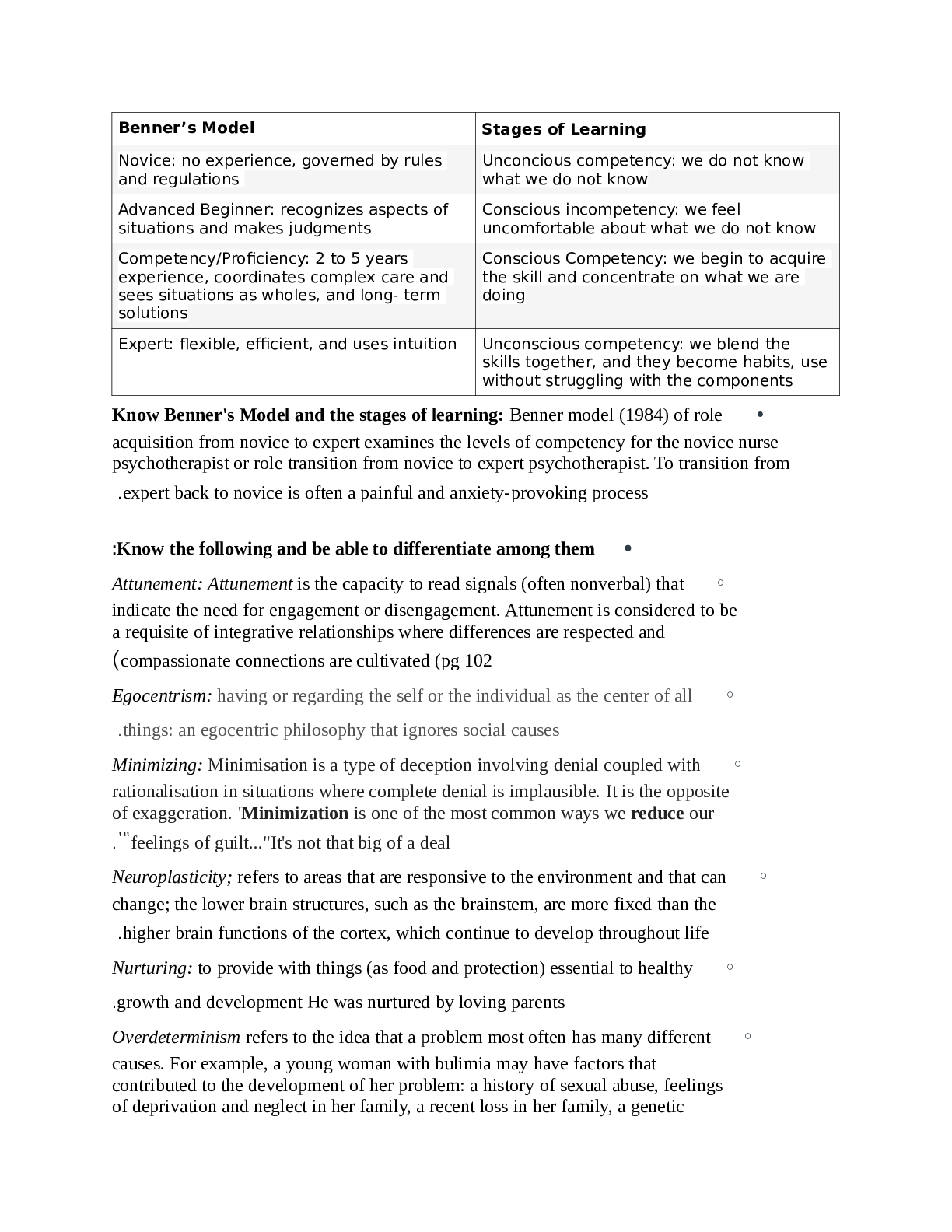
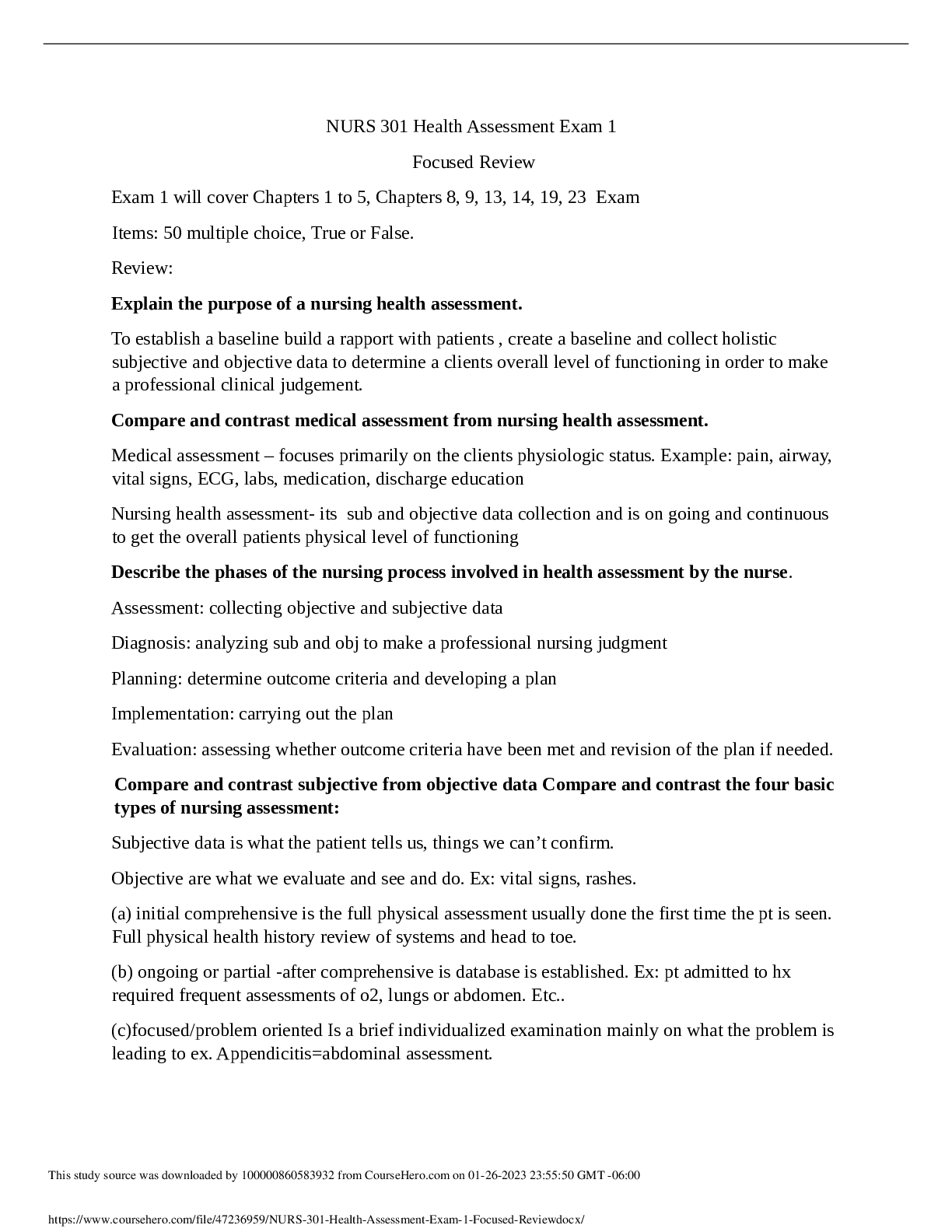
Exam 1 will cover Chapters 1 to 5, Chapters 8, 9, 13, 14, 19, 23 Exam Items: 50 multiple choice, True or False. Review: Explain the purpose of a nursing health assessment. To establish a baseline ... build a rapport with patients , create a baseline and collect holistic subjective and objective data to determine a clients overall level of functioning in order to make a professional clinical judgement. Compare and contrast medical assessment from nursing health assessment. Medical assessment – focuses primarily on the clients physiologic status. Example: pain, airway, vital signs, ECG, labs, medication, discharge education Nursing health assessment- its sub and objective data collection and is on going and continuous to get the overall patients physical level of functioning Describe the phases of the nursing process involved in health assessment by the nurse. Assessment: collecting objective and subjective data Diagnosis: analyzing sub and obj to make a professional nursing judgment Planning: determine outcome criteria and developing a plan Implementation: carrying out the plan Evaluation: assessing whether outcome criteria have been met and revision of the plan if needed. Compare and contrast subjective from objective data Compare and contrast the four basic types of nursing assessment: Subjective data is what the patient tells us, things we can’t confirm. Objective are what we evaluate and see and do. Ex: vital signs, rashes. (a) initial comprehensive is the full physical assessment usually done the first time the pt is seen. Full physical health history review of systems and head to toe. (b) ongoing or partial -after comprehensive is database is established. Ex: pt admitted to hx required frequent assessments of o2, lungs or abdomen. Etc.. (c)focused/problem oriented Is a brief individualized examination mainly on what the problem is leading to ex. Appendicitis=abdominal assessment. This study source was downloaded by 100000860583932 from CourseHero.com on 01-26-2023 23:55:50 GMT -06:00 https://www.coursehero.com/file/47236959/NURS-301-Health-Assessment-Exam-1-Focused-Reviewdocx/ (d) emergency is a physical examination done when time is a factor treatment must begin immediately. Describe the three phases of a client interview process. Give examples on what occurs in each phase. Introductory: introduction, explaining the purpose, types of questions that will be asked, assuring confidentiality, making sure the client is comfortable and privacy. Developing trust and rapport Working: bio data, reason for seeking care, past health history and family history, review of body systems. Lifestyle and health practices. Summary and closing-summarizing information validating problems and goals, identifying and discussing plans to resolve problems with clients, is there anything else the client needs or any questions. Describe effective verbal and nonverbal communication techniques to collect subjective client data. Identify verbal communication to avoid during a client interview. Describe ways to adapt the interview for the older client. Verbal: open-ended questions “how or “what” Ex: how have you been feeling today? Closed ended questions “when or did” only can answer to that question Ex: when did the nausea start?, rephrasing, providing information. Non-verbal- appearance, demeanor, facial expressions, silence, listening, posture and attitude. Things to AVOID: biased or leading questions, rushing, reading the questions. Too much or too little eye contact, distraction, or standing. Describe the purpose of performing genogram. Helps organize and illustrates the clients family history. It helps us see if there are health problems that run in the family and those of genetic predisposition. Summarize the ways that the nurse can prepare the client for a physical examination Keep room temp comfortable, private area, quiet and adequate lighting, firm examination table or bed, bedside table/tray to hold equipment Explain the 4 physical assessment techniques and sequence of physical assessment. Inspection, Palpation, percussion, Auscultation. Abdomen is: Inspection, Auscultation, percussion, and palpation Describe ways to validate data Explain the purposes of documenting assessment data Ways to validate repeat the assessment, clarify data with the client, verify with another health care professional, compare obj and subj findings. This study source was downloaded by 100000860583932 from CourseHero.com on 01-26-2023 23:55:50 GMT -06:00 https://www.coursehero.com/file/47236959/NURS-301-Health-Assessment-Exam-1-Focused-Reviewdocx/ Purpose for documenting establishes a basis for screening and validating, acts as a source of information to help diagnose new problems, helps to determine educational needs of the client and family, provides eligibility of care and reimbursement. Constitutes a permanent legal record of care that was or was not given to client. Compare and contrast Health Promotion, Risk, Actual and Collaborative Diagnoses Health promotion- they are ready to learn or enhance their well-being Risk- they don’t have the disease or problem, but they can be at risk for it Actual- is the actual problem that they have and are being cared for Collaborative diagnosisIdentify safe guidelines for documentation of client data. Keep confidential all documented information, make sure its legible or printed neatly. Use correct grammar and spelling. Record findings, not how they were obtained. Avoid using NORMAL. What is SBAR? Sbar is used to translate information to one personal to the next. Situation- what is going on Background- what led to the situation Assessment- actual documentation and usually includes the vitals your subjective and objective data. Recommendation- what do you recommend or what should the provider do or who should you send the pt to, that is, a specialist. Describe how to perform the general status assessment. Compare and contrast normal from abnormal findings. Explain the significance of the abnormal findings. Its usually a head to toe assessment and general characteristics and impressions of the client. Observing significant abnormalities. Discuss the assessment of pain as a fifth vital sign. How is pain assessed? When does the nurse perform a pain assessment? What is COLDSPA? Pain is subjective and is what the person tells us. Observing the client for grimacing or holding onto an area or guarding is signs of pain as well. The nurse will perform the pain assessment initially in the general assessment and periodically assess the pain. We use a numerical scale from 0-10. COLDSPA is used to get more information regarding the pain. Characteristic how does it feel? This study source was downloaded by 100000860583932 from CourseHero.com on 01-26-2 [Show More]
Last updated: 2 years ago
Preview 1 out of 6 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$9.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 27, 2023
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Jan 27, 2023
Downloads
0
Views
96



.png)
.png)









.png)